Psychotic break age
Early signs of psychosis | Washington State Health Care Authority
Psychosis is not a diagnosis, but a term used to describe a group of symptoms. Psychosis is a break with reality where the thoughts and perceptions of a person become disrupted. These changes happen gradually, typically in three phases: early, acute, and recovery.
The onset of first episode psychosis typically presents when an individual is between the ages of 18-25, however, may present between the ages of 15-40. It is uncommon for first episode psychosis to present in childhood.
On this page
What should I know about psychosis?
Phases of psychosis
What should I look for?
Have others experienced this?
Is there help?
Tools for you, family, and friends
What should I know about psychosis?
-
Anyone can have a psychotic episode.
-
Psychosis does not discriminate across cultures, races, or social classes.
-
At this time it is still unknown exactly what causes psychosis, but it is known that psychosis is treatable and that the earlier it is identified and treated the more successful remission is.
Phases of psychosis
Psychosis occurs in three phases:
- Early
- Acute
- Recovery
Learn more about the phases of psychosis on the New Journeys website.
What should I look for?
The following are some of the more common signs of psychosis:
- Changes in thinking
-
- Everyday thoughts may be confused/jumbled or don't join up properly
- Sentences may be unclear or don't make sense
- Thoughts are sped up or come very slowly
- Difficulties planning, reasoning, making decisions, completing tasks, following a conversation, remembering details
- Having odd ideas
- Changes in behavior
-
- Shifts in basic personality
- Mood changes (i.
 e., hyperactivity, inactivity, or alternating between the two)
e., hyperactivity, inactivity, or alternating between the two) - Social withdrawal and isolation
- Severe changes in sleep patterns
- Deterioration in personal hygiene
- Excessive writing without meaning
- Unusual sensitivity to stimuli (such as noise, light, colors, textures)
- Suicidal thoughts or behaviors
- Use of alcohol and/or other drugs
- Changes in feelings and perception
-
- Feeling strange and cut off from the world
- Feelings of distrust or suspicion about others and their actions
- Things look or sound different from what others are experiencing
- The tone in a person's speech may change
- Facial expressions and physical movement may change
- Hallucinations
-
- Hearing, seeing, tasting, smelling or feeling things that are not there, but seem very real to the person experiencing them
- Hearing voices: the voices could be threatening to them or telling them to harm themselves
- Delusions
-
- False beliefs such as being followed or monitored, or having special abilities or "powers"
- Thinking they are being controlled by other people or forces, or that their thoughts are being broadcast so others can hear them
- These beliefs are often held firmly, and attempts at reasoning or debating can lead to anger or mistrust
Want more information?
Watch ThriveNYC's video on psychosis.
Have others experienced this?
Yes. According to the National Alliance on Mental Illness (NAMI) approximately 100,000 young people will experience psychosis each year, and as many as 3 in 100 people will experience psychosis in their lifetime.
Watch recent New Journeys graduates share their recovery stories:
Is there help?
Yes. If someone you know is experiencing some of these symptoms, you can get help. Research shows that the longer psychosis goes untreated, the harder it is to control.
- Talk to your doctor.
- Call the Washington Recovery Helpline at 1-866-789-1511.
- Contact New Journeys. The Health Care Authority (HCA) collaborated with the University of Washington and Washington State University to develop New Journeys, a program for first episode psychosis.
 New Journeys is currently available in the following areas:
New Journeys is currently available in the following areas: - Behavioral health resources (Grays Harbor and Olympia)
- Catholic Charities (Chelan, Douglas, and Wenatchee)
- Comprehensive Healthcare (Yakima)
- Comprehensive Life Resources (Pierce County)
- First episode psychosis (FEP) Comprehensive (Franklin County)
- First episode psychosis (FEP) SeaMar (Clark County)
- Frontier Behavioral Health (Spokane)
- Harborview Step Team (King County)
- Kitsap Mental Health services (Kitsap County)
- Ryther (Seattle)
- Valley Cities Behavioral Health Care (Renton)
New Journeys statewide plan
- Read the Washington Council for Behavioral Health and HCA's statewide plan.
Are you, or someone you know, in need of immediate help?
- For a life-threatening emergency: Call 911.
- For suicide prevention:
Contact the National Suicide Prevention Lifeline at 1-800-273-8255 (TRS: 1-800-799-4889).

- For 24-hour emotional support and referrals: Contact the Washington Recovery Help Line or the crisis line in your area.
Tools for you, family, and friends
Video: "We can prevent major mental Illness"
Learn more about early psychosis in this 16-minute TEDxRosenburg talk by Dr. Ryan Melton, clinical director of the EASA Center for Excellence at Portland State University's Regional Research Institute and an Assistant Professor of Clinical Mental Health at Northwest Christian University.
Read the New Journeys fact sheet.
Additional resources
- New Journeys teams site map
- UW Medicine SPIRIT Lab
- Center for Practice Innovations' (CPI's) consumer and family portal: A series of vignettes of consumers and family members. The videos share inspirational and informative recovery stories on a variety of topics. A manual is also available to help integrate the videos into treatment and training.
- Mindmap online psychosis quiz: A three-minute quiz for those who have concerns about psychosis.
Schizophrenia Onset: Age Ranges and Warning Signs
Schizophrenia is a mental health condition that affects about 1% of the U.S. population. That means millions of people nationwide live with the condition. It typically starts in late adolescence or early adulthood.
Schizophrenia can affect people of all different sexes, genders, and backgrounds.
Schizophrenia impacts your ability to connect with other people, organize your thoughts, and manage your emotions.
As much as 80% of people with schizophrenia aren’t aware they’re experiencing symptoms during early psychosis. For this reason, if you notice signs of schizophrenia in someone else, it may be especially important to help them connect with a healthcare professional.
If you’re experiencing unusual thoughts or notice any changes in the way you sense or perceive yourself and the world around you, it may help to speak with a mental health professional about these experiences.
An important thing to note is that the onset of schizophrenia can look different from person to person, as this condition can take a variety of forms.
That said, there are still certain symptoms you can look for.
The onset of schizophrenia usually occurs between the ages 16 and 30. Broken down by sex, the average age of onset tends to be:
- Males: late teens to early 20s
- Females: late 20s to early 30s
There’s a possibility that healthcare professionals may diagnose this condition in children 13 years old and younger. However, the chances of this are much lower. The odds of developing childhood-onset schizophrenia are roughly 1 in 10,000.
Though it’s most common for people to begin experiencing their first symptoms in late adolescence or early adulthood, early or late onset schizophrenia is also possible.
Psychosis affects the way you think and perceive the world around you. A person experiencing psychosis has trouble distinguishing between what is real and what isn’t. Psychosis can be brought on by medical causes or trauma, or by a developmental cause, such as schizophrenia.
Everyone’s experience is different, but most people say that psychosis is frightening and confusing.
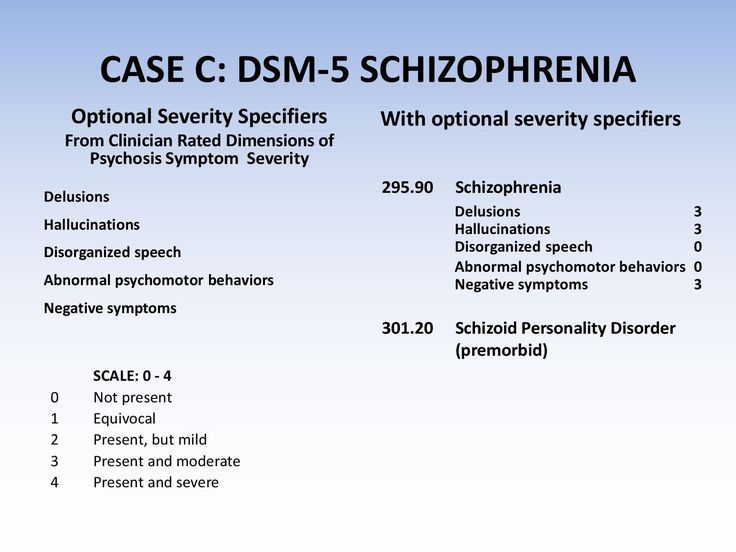
Schizophrenia is a psychotic syndrome that involves positive symptoms, negative symptoms, and thought disorder.
Positive symptoms are symptoms that are present when they usually would not be, such as hallucinations. Negative symptoms are symptoms where something is absent that would usually be present. Examples would include diminished emotional responses or delayed speech development in children.
People with thought disorder may communicate using words and phrases that may not make complete logical sense.
First episode of psychosis
The first episode of psychosis refers to when you first show signs of being unable to distinguish what’s real from what isn’t. It typically involves hallucinations and delusions, which can seem very real to the person experiencing them.
Experts say the average age at which people first experience psychosis is 24 years old. The oldest age of onset was 63 years and the youngest age was 3 years.
The oldest age of onset was 63 years and the youngest age was 3 years.
Acting quickly to connect yourself or your loved one with the right treatment during early psychosis can help dramatically. If you are a family member or friend, consider reaching out to a healthcare professional on behalf of the person you care about.
Healthcare professionals consider someone to have early onset schizophrenia, or childhood onset schizophrenia (COS), when their symptoms begin before the age of 13 years.
Early onset can be harder to diagnose because clinicians have to distinguish between a child’s benign imaginative play and delusions or hallucinations that are related to schizophrenia.
If a child receives a diagnosis of schizophrenia, their hallucinations will most likely be auditory. This means they may hear strange voices, ringing, or other noises that may not actually be occurring.
It’s usually not until later in the teenage years that someone with early onset schizophrenia experiences thought disorder.
Children with COS may also show disordered speech. However, because children sometimes have delayed development of speech for other reasons, it can be difficult for a psychiatrist to say whether this symptom is related to schizophrenia.
Regardless of how difficult it can be for healthcare professionals to diagnose schizophrenia in children, if you believe that someone close to you might be experiencing early onset schizophrenia, it’s important to say something.
The quicker they can receive professional assessment, diagnosis, and treatment, the better their chances of successfully managing their mental health.
Like early onset schizophrenia, late onset schizophrenia is rare. Mental health professionals consider schizophrenia to be late onset when a person begins experiencing symptoms between ages 40 and 60.
Later in life, schizophrenia is associated with other medical risks, such as cardiac issues. People with late onset schizophrenia are less likely to have disorganized thoughts or trouble understanding.
Instead, they’re more likely to experience so-called positive symptoms, like delusions and hallucinations.
Usually, a person with schizophrenia has gradual changes in their thoughts and perceptions. Families are often the first to see early signs of psychosis and schizophrenia in a loved one.
Before the first episode of psychosis, you go through what is known as a “premorbid” period. This is the 6 months before the first symptoms of psychosis. During this period, you might experience gradual changes.
Although sleep disturbances are not included in the diagnostic criteria for schizophrenia, people with the condition consistently report them.
Early warning signs include:
- a concerning drop in grades in school or performance at work
- trouble thinking clearly or concentrating
- suspiciousness of or uneasiness around others
- a decline in self-care or personal hygiene
- inappropriately strong emotions or no feelings at all
- unusual thoughts or beliefs
- hearing, seeing, tasting, or believing things that others don’t
Schizophrenia is a long-lasting mental health condition that tends to become apparent in late adolescence or early adulthood. Earlier and later onsets are also possible, but they’re relatively rare.
Earlier and later onsets are also possible, but they’re relatively rare.
Doctors can’t cure schizophrenia, but they can help you significantly manage and control it. There are different therapies, medications, and support groups that can alleviate some of the uncomfortable symptoms associated with schizophrenia.
It’s possible to live well if you have schizophrenia. Once you or your loved one has spoken with a psychiatrist and been diagnosed with this mental health condition, there are a variety of treatment options available.
For more information, you can visit the National Alliance on Mental Illness (NAMI) and the National Institute of Mental Health (NIMH).
There should be no shame in addressing your mental health or that of a loved one.
You can listen to the Inside Schizophrenia Podcast to learn more about schizophrenia and ending the stigma around mental health.
Mental disorders of late age
Mental disorders of late age are diseases that occur in presenile (presenile, involutional) and senile age. Since there are large differences in the definition of the concept of "late age", in psychiatry, the involutionary period is usually understood as the age from 45 to 55 years, and patients older than 60 years are referred to the old age (V. M. Bleikher, I. V. Kruk "Explanatory Dictionary psychiatric terms", 1995), which is at odds with the WHO classification, according to which patients from 60 to 74 years old are considered elderly, and persons from 75 to 90 years old are classified as old age.
Since there are large differences in the definition of the concept of "late age", in psychiatry, the involutionary period is usually understood as the age from 45 to 55 years, and patients older than 60 years are referred to the old age (V. M. Bleikher, I. V. Kruk "Explanatory Dictionary psychiatric terms", 1995), which is at odds with the WHO classification, according to which patients from 60 to 74 years old are considered elderly, and persons from 75 to 90 years old are classified as old age.
The increase in life expectancy has led to a change in the age structure of the population, manifested in an increase in the proportion of elderly and senile patients and, accordingly, elderly patients who manifest certain somatic disorders, as well as severe mental disorders.
Gerontological mental disorders:
Mental disorders of late age are usually divided into diseases of "organic" origin, which arise on the basis of a certain destructive process and lead to dementia (dementia), and "functional" (reversible and, as a rule, not leading to severe dementia) disorders.
The treatment of affective (manifested by such disorders as depression or manic states) and delusional (manifested mainly by delirium) senile psychoses does not differ from the psychopharmacotherapy of similar conditions in other mental illnesses. At the European Medical Center, we use combined treatment with antipsychotics and antidepressants - depending on the patient's condition, treatment can be started with the use of antipsychotics and, upon reaching a decrease in the patient's anxiety-delusional arousal, it is possible to add antidepressant drugs.
If a patient with affective and affective-delusional senile (senile) psychosis is insensitive to psychotropic drugs, it is possible to prescribe the so-called electroconvulsive therapy (ECT), if there are no contraindications. Since ECT is ineffective in delusional forms of senile psychosis, treatment with antipsychotics is used.
Psychopharmacological treatment of mental disorders of late age is carried out in a multidisciplinary hospital of the European Medical Center, where patients are provided with comprehensive support and treatment - a complete physical examination is carried out, round-the-clock monitoring of the patient's condition during therapy is provided and complications are prevented.
Parkinson's disease is a degenerative-atrophic disease of the brain that manifests itself at a later age and is often accompanied by mental disorders. The most effective treatment for movement disorders currently used to treat Parkinson's disease is L-DOPA, but the drug has side effects (approximately 50% of patients may experience mental disorders such as confusion, psychomotor agitation with anxiety, agitation, drowsiness, increased depression ). The appointment of L-DOPA follows after a thorough assessment of the mental state of the patient and treatment begins with small doses, which are gradually increased. If psychotic disorders occur, along with a gradual decrease in doses of antiparkinsonian drugs (up to temporary cancellation) and detoxification therapy, it is possible to prescribe small doses of psychotropic drugs.
Alzheimer's disease - an atrophic brain disease that manifests itself mainly in presenile age, which leads to dementia and is accompanied by disorders of higher nervous activity. The prognosis of this disease is unfavorable, and today there are no proven effective methods of its treatment. In the later stages of the process, patients, as a rule, need to be hospitalized in psychiatric hospitals or placed in neuropsychiatric boarding schools.
The prognosis of this disease is unfavorable, and today there are no proven effective methods of its treatment. In the later stages of the process, patients, as a rule, need to be hospitalized in psychiatric hospitals or placed in neuropsychiatric boarding schools.
Senile dementia is the most characteristic mental illness of senile age with a progressive breakdown of mental activity, culminating in most cases in total dementia (decrease in all intellectual functions). Some foreign psychiatrists consider senile dementia, a kind of completion of the physiological process of aging of the brain, inevitable in old age. With physiological aging, there is also a decrease in the level of mental activity, reminiscent of the initial symptoms of senile dementia. Proper care and symptomatic therapy are important for the fate of such patients - at the initial stage of the disease, patients are recommended to be left in their usual home environment (if their condition allows). Transfer to an unusual (including hospital) environment can cause an aggravation of the course of the disease. Patients are hospitalized only for special indications (helplessness, lack of care, danger to themselves and others).
Transfer to an unusual (including hospital) environment can cause an aggravation of the course of the disease. Patients are hospitalized only for special indications (helplessness, lack of care, danger to themselves and others).
There are no convincing data indicating the effectiveness of the treatment of senile dementia with nootropic drugs, and therefore such therapy can be recommended only in the initial stages of the disease, as well as in the combination of senile dementia with cerebral atherosclerosis. Psychotropic drugs in very small doses are indicated only when the patient is very agitated, persistent insomnia or psychotic disorders.
Fracture Julia Beldyanovna
About the specialist
Accepts adults from 18 to 70 years old, and children from 5 to 17 years old.
Invites even the most indecisive and closed people to itself thanks to a warm atmosphere and a neutral position in the course of therapy.
It will help you focus on solving the problem, find the source of the resource and believe in changing the situation for the better. This is possible thanks to the solution-oriented method, the experience of the therapist and the supportive environment. Constantly learning and improving his skills.
This is possible thanks to the solution-oriented method, the experience of the therapist and the supportive environment. Constantly learning and improving his skills.
Tactful, understanding specialist.
How it can help
- Decision-making: bouts of loneliness, lack of support from loved ones, impotence, impasse in life, burnout, lack of support, career difficulties, self-discovery.
- Relationships, family: crisis in a couple, quarrels, betrayals, jealousy, mistrust, tantrums, closeness, intimate difficulties, thoughts of divorce, conflicts/scandals, coldness, resentment, pre-divorce/divorce, loneliness.
- Parenthood: frequent quarrels in the family, fears for the child, loss of strength, emotional burnout, conflicts with the child, post-natal depression.
- Children: conflicts with children, isolation, enuresis, encopresis, disobedience, aggression, tantrums, tearfulness.

- Adolescents: rudeness, conflicts, tantrums, adolescent depression, anxiety before exams, poor academic performance, uncontrollability/isolation, depression, communication difficulties.
- Depressive: depression, sadness, procrastination, impotence, forgetfulness, detachment from life, apathy, chronic fatigue, melancholy.
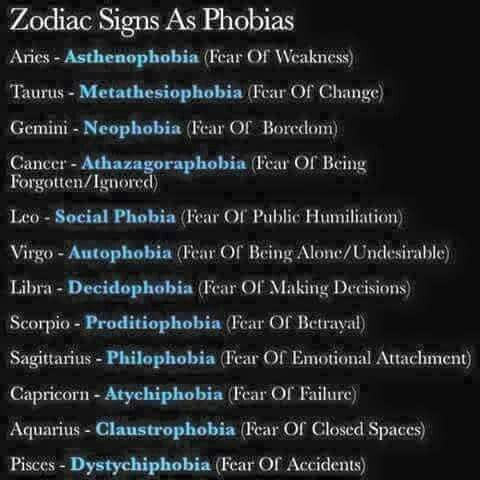
- Anxiety: attacks of terror and panic, anxiety, various phobias.
- Obsessions: OCD, obsessive counting and other calming rituals, obsessive thoughts.
- Trauma: past traumatic experience, emotional highs, abuse, humiliation, criticism, bullying, shaming, cruel or distant parenting, attempted submission or suppression, relationship problems.
What can't help
- Major psychiatry: BAD, MDP, schizophrenia, psychotic spectrum disorders, psychoses.
- Chemical addictions: alcohol, drugs, nicotine.

Learn more