Psychotherapy for dissociative identity disorder
Dissociative disorders - Diagnosis and treatment
Diagnosis
Diagnosis usually involves assessment of symptoms and ruling out any medical condition that could cause the symptoms. Testing and diagnosis often involves a referral to a mental health professional to determine your diagnosis.
Evaluation may include:
- Physical exam. Your doctor examines you, asks in-depth questions, and reviews your symptoms and personal history. Certain tests may eliminate physical conditions — for example, head injury, certain brain diseases, sleep deprivation or intoxication — that can cause symptoms such as memory loss and a sense of unreality.
- Psychiatric exam. Your mental health professional asks questions about your thoughts, feelings, and behavior and discusses your symptoms. With your permission, information from family members or others may be helpful.
- Diagnostic criteria in the DSM-5. Your mental health professional may compare your symptoms to the criteria for diagnosis in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), published by the American Psychiatric Association.
For diagnosis of dissociative disorders, the DSM-5 lists these criteria.
Dissociative amnesia
For dissociative amnesia:
- You've had one or more episodes in which you couldn't remember important personal information — usually something traumatic or stressful — or you can't remember your identity or life history. This memory loss is too extensive to be explained by ordinary forgetfulness.
- Your episodes of memory loss don't occur only during the course of another mental health disorder, such as post-traumatic stress disorder. Also, your symptoms are not due to alcohol or other drugs, and they're not caused by a neurological or other medical condition, such as amnesia related to head trauma.
- You may also experience dissociative fugue, where you purposefully travel or experience confused wandering that involves amnesia — inability to remember your identity or other important personal information.
- Your symptoms cause you significant stress or problems in your relationships, work or other important areas of your life.
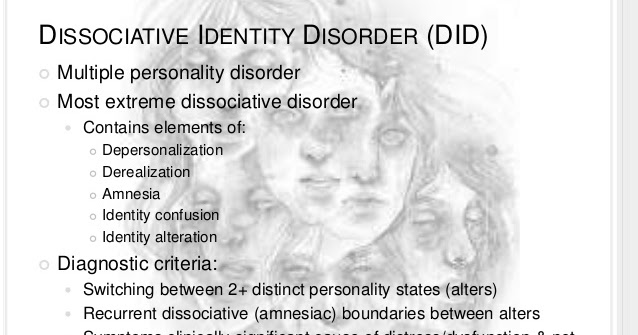
Dissociative identity disorder
For dissociative identity disorder:
- You display, or others observe, two or more distinct identities or personalities, which may be described in some cultures as possession that is unwanted and involuntary. Each identity has its own pattern of perceiving, relating to and thinking about yourself and the world.
- You have recurrent gaps in memory for everyday events, skills, important personal information and traumatic events that are too extensive to be explained by ordinary forgetfulness.
- Your symptoms are not a part of broadly accepted cultural or religious practice.
- Your symptoms are not due to alcohol or other drugs, or a medical condition. In children, symptoms are not due to imaginary playmates or other fantasy play.
- Your symptoms cause you significant stress or problems in your relationships, work or other important areas of your life.
Depersonalization-derealization disorder
For depersonalization-derealization disorder:
- You have persistent or recurrent experiences of feeling detached from yourself, as if you're an outside observer of your thoughts, sensations, actions or your body (depersonalization).
 Or you feel detached or experience a lack of reality for your surroundings as if you're in a dream or the world is distorted (derealization).
Or you feel detached or experience a lack of reality for your surroundings as if you're in a dream or the world is distorted (derealization). - While you're experiencing an episode of depersonalization or derealization, you're aware the experience is not reality.
- Your symptoms do not occur only during the course of another mental disorder, such as schizophrenia or panic disorder, or during another dissociative disorder. Your symptoms are also not explained by the direct effects of alcohol or other drugs, or a medical condition, such as temporal lobe epilepsy.
- Your symptoms cause you significant stress or problems in your relationships, work or other important areas of your life.
Treatment
Dissociative disorders treatment may vary based on the type of disorder you have, but generally include psychotherapy and medication.
Psychotherapy
Psychotherapy is the primary treatment for dissociative disorders. This form of therapy, also known as talk therapy, counseling or psychosocial therapy, involves talking about your disorder and related issues with a mental health professional.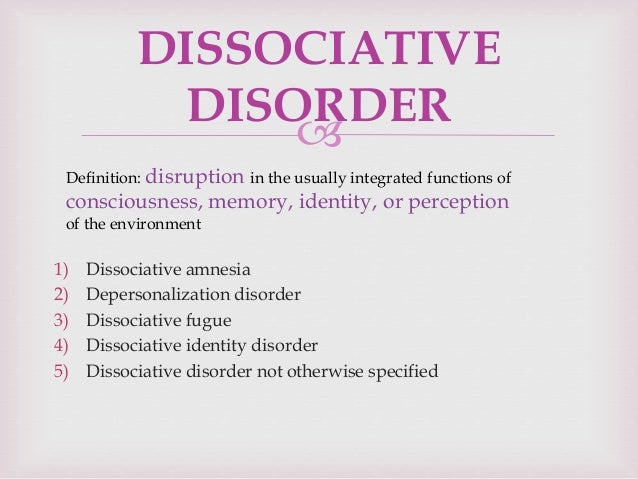 Look for a therapist with advanced training or experience in working with people who have experienced trauma.
Look for a therapist with advanced training or experience in working with people who have experienced trauma.
Your therapist will work to help you understand the cause of your condition and to form new ways of coping with stressful circumstances. Over time, your therapist may help you talk more about the trauma you experienced, but generally only when you have the coping skills and relationship with your therapist to safely have these conversations.
Medication
Although there are no medications that specifically treat dissociative disorders, your doctor may prescribe antidepressants, anti-anxiety medications or antipsychotic drugs to help control the mental health symptoms associated with dissociative disorders.
More Information
- Cognitive behavioral therapy
- Hypnosis
- Psychotherapy
Request an Appointment at Mayo Clinic
Preparing for your appointment
As a first step, your doctor may ask you to come in for a thorough exam to rule out possible physical causes of your symptoms.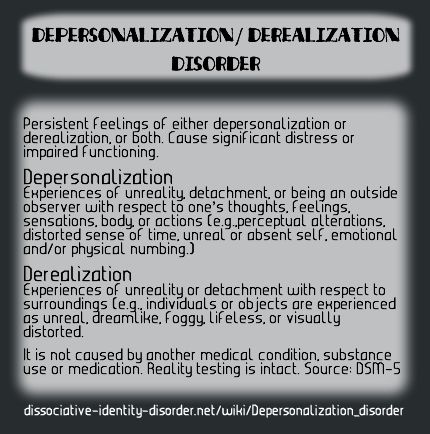 However, in some cases you may be referred immediately to a psychiatrist. You may want to take a family member or friend along, if possible, to help you remember information.
However, in some cases you may be referred immediately to a psychiatrist. You may want to take a family member or friend along, if possible, to help you remember information.
Here's some information to help you prepare for your appointment, and what to expect from your doctor.
What you can do
Before your appointment, make a list of:
- Any symptoms you're experiencing, including any recent behavior that caused confusion or concern for you or your loved ones.
- Key personal information, including any major stresses or recent life changes. Also note events from your past, including your childhood, that caused physical or emotional trauma. If you can't recall some periods of your life, note the time frame and anything you can remember about the period leading up to your amnesia.
- Your medical information, including other physical or mental health conditions you have. Include any medications, vitamins, herbs or other supplements you're taking, and the dosages.
- Questions to ask your doctor to make the most of your time together
Some questions to ask your doctor may include:
- What's likely causing my symptoms or condition?
- What are other possible causes?
- How will you determine my diagnosis?
- Is my condition likely temporary or long term (chronic)?
- What treatments do you recommend for this disorder?
- How much can I expect my symptoms to improve with treatment?
- How will you monitor my progress?
- I have these other health conditions. How can I best manage them together?
- Should I see a specialist?
- Are there any brochures or other printed material that I can have?
- What websites do you recommend?
Don't hesitate to ask other questions during your appointment.
What to expect from your doctor
Your doctor is likely to ask you a number of questions. Be ready to answer them to reserve time to go over any points you want to focus on. Your doctor may ask:
Your doctor may ask:
- What symptoms concern you or your loved ones?
- When did you or your loved ones first notice your symptoms?
- Are there periods of time in your life that you don't remember?
- Have you ever found yourself some distance away from your home or work, and not known how you got there?
- Do you ever feel as if you're outside of your body, observing yourself?
- Do you feel as though there is more than one person, or maybe many people, living inside your head?
- What other symptoms or behaviors are causing you or your loved ones distress?
- How often do you feel anxious or depressed?
- Have your symptoms caused problems in your work or your personal relationships?
- Have you ever thought about harming yourself or others?
- Do you drink alcohol or use recreational drugs?
- Do you now or have you ever served in the military?
- Have you ever been touched against your will?
- Were you physically abused or neglected as a child?
- Was anyone in your family abused during your childhood?
- Are you currently being treated for any other medical conditions, including mental health disorders?
By Mayo Clinic Staff
Related
Associated Procedures
Products & Services
Dissociative Identity Disorder: Treatment and Recovery
The treatment plan for DID centers around talk therapy, where you can learn to understand your symptoms, their causes, and ways to manage dissociative episodes.
Dissociation — when someone temporarily disconnects from their surroundings or emotions — is more common than many people think.
According to a 2004 study, between 26 and 74% of people have symptoms of derealization and depersonalization during their lifetime (two types of dissociation), but only 1–2% meet the criteria for clinically significant episodes.
DID is a mental health condition characterized by extreme dissociation involving “switching” between two or more distinct identities.
Once known as multiple personality disorder, the causes and treatment options for DID haven’t always been well understood. This has lead to stigma and confusion among society and even experts.
That’s all changing though, thanks to more research, a better understanding of neurobiology, and people speaking up about their lived experiences. Now we have a better understanding of the treatments, tools, and self-care strategies that can help when living with DID.
Most treatment plans for people with DID focus on talk therapy (aka psychotherapy). Talk therapy can help you understand why you dissociate and give you the tools to cope.
Talk therapy can help you understand why you dissociate and give you the tools to cope.
Other treatment options include medication for co-occurring issues and hospital visits.
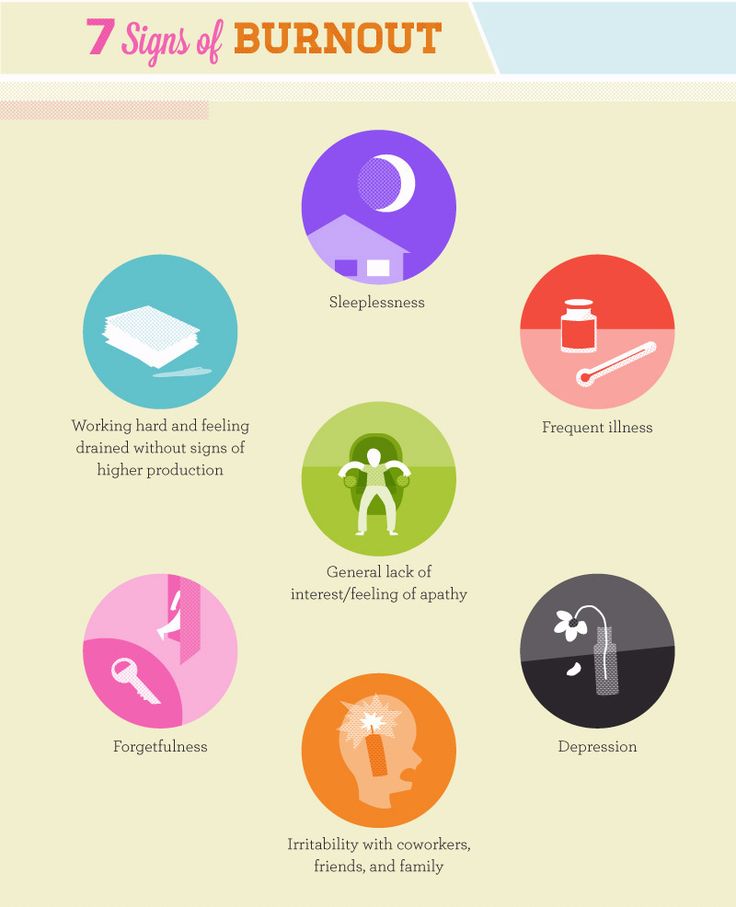
Treatment aims to help you reduce and cope with the symptoms of DID, which include:
- Identity shifts. DID involves switching between at least two identities, also known as personality states, alters, multiples, splits, or plurals.
- Amnesia. This is different from occasional forgetfulness; it refers to a gap in time during everyday events, the inability to recall personal information, or forgetting your activities, such as waking up somewhere and not being able to recall how you got there.
- Depersonalization. This is the feeling of being disconnected from your physical self or having an “out of body” experience, like observing yourself from a passenger’s perspective or watching a movie of yourself.
- Derealization.
 This is the sensation of being disconnected from your physical environment, experiencing your surroundings as dream-like, or feeling like people and events aren’t real.
This is the sensation of being disconnected from your physical environment, experiencing your surroundings as dream-like, or feeling like people and events aren’t real. - Identity confusion. This means you may have a difficult time pinning down your core interests, goals, style, opinions, values, and beliefs.
Your treatment should also aim to help with any co-occurring issues, which might include:
- PTSD
- anxiety
- depression
- borderline personality disorder
- eating disorders
- sleep disturbances
- self-harm or suicidal thoughts
- substance use issues
We take a closer look at the treatment options below.
For some people, living with the symptoms of DID can be frightening, isolating, or confusing.
Research has found that people with DID are more likely to harm themselves, and more than 70% of outpatients have attempted suicide.
For this reason, working closely with a compassionate, knowledgeable mental health professional is considered the first-line treatment for DID. Talk therapy has been shown to improve symptoms of DID in the long term.
Talk therapy has been shown to improve symptoms of DID in the long term.
Your therapist can help you understand what you’re experiencing and why. Therapy also gives you the space to explore and understand the different parts of your identity that have dissociated, and ultimately, to integrate them.
Dissociative disorders often stem from childhood trauma. In fact, as many as 90% of people with DID have a history of childhood abuse or neglect.
Dissociation is your body’s way of distancing you from an intolerable experience, which is an effective survival strategy in the moment — but over time, chronic dissociation can form separate identities from your “core” or “main” personality, leading to the symptoms of DID.
Besides helping you understand the reasons behind your dissociation, your therapist can help you deal with dissociative states and develop useful coping mechanisms.
Your treatment plan will be based on your own unique needs, but may include:
- education about dissociation and DID
- body movement therapy to release trauma that’s held in the body
- relationship support
- trigger management
- impulse control
- mindfulness and self-awareness
- coping methods to tolerate difficult emotions
Some specific therapies used to treat DID include:
- cognitive behavioral therapy (CBT)
- dialectical behavioral therapy (DBT)
- eye movement desensitization and reprocessing (EMDR)
If you need support:
- Text the Crisis Text Line by texting “HOME” to 741741.
- Contact the National Suicide Prevention Lifeline at 800-273-8255, or if not in the U.S., find a crisis line in your country with Befrienders Worldwide.
- Call the NAMI HelpLine at 800-950-6264.
- Use the International Society for the Study of Trauma and Dissociation’s Find a Therapist tool.
There are no medications recommended to directly treat DID, at least not yet. But there are some options to help with co-existing conditions and symptoms, like anxiety, depression, and substance use.
Your doctor may prescribe an antidepressant medication, like a selective serotonin reuptake inhibitor (SSRI). Common ones include:
- fluoxetine (Prozac)
- sertraline (Zoloft)
Anti-anxiety meds may also be recommended, depending on your symptoms.
If psychosis is present, an antipsychotic medication might help you manage symptoms and feel more in control.
If symptoms for you or someone you love are becoming severe, or suicide is a possibility, you can seek emergency medical attention at your nearby hospital right away.
This can help doctors rule out the possibility of an underlying condition, like a brain injury, and provide a safe, stable environment to talk about next steps.
In real life, an inpatient stay at a psychiatric facility is very different from what you’ll see in the media, which is often sensationalized.
An inpatient stay may last a few days to several weeks, which will give doctors ample time to work with you in individual and group therapy settings, discuss medications, and form a solid discharge plan.
Balanced nutrition
There’s no recommended food protocol for DID, but a diet rich in whole, unprocessed foods is a great way to make sure that your body and mind are getting all the nutrients and energy needed.
Get daily movement
Thanks to a rush of endorphins, exercise may boost your mood and help release any stored up tension. It doesn’t have to be intensive, either.
If you’re trying to build a habit, start with just enough to get your heart rate up, like a brisk walk around your neighborhood. The Centers for Disease Control and Prevention (CDC) recommends 30 minutes per day, 5 days a week.
The Centers for Disease Control and Prevention (CDC) recommends 30 minutes per day, 5 days a week.
Get enough sleep
Do your best to maintain a sleep schedule and practice sleep hygiene before bed.
Try to get at least 8 hours of sleep each night so that your brain has time to rest and your tissues have time to repair themselves. In other words, it will help keep you performing at your optimal level.
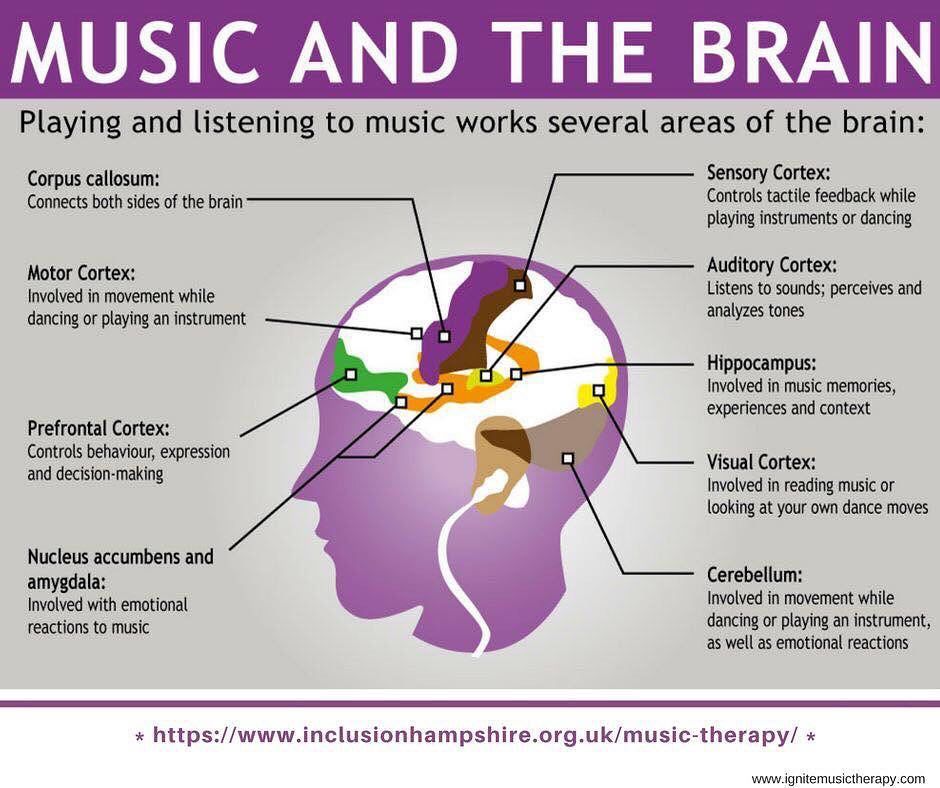
Develop a meditation practice
While more research is needed on complementary treatments for dissociative disorders, a small 2016 study found that some symptoms improved for young participants enrolled in a mindfulness program over the course of 6 weeks. You could start by checking out some meditation apps.
Roll out your yoga mat
Yoga has long been studied for its positive effects on mood. Research has shown that a regular yoga practice can help people with trauma increase their emotional regulation, among other mental health benefits.
It might be important for you to seek a trauma-informed practice, because yoga can feel overwhelming for some people with a history of trauma.
When symptoms of DID impact your everyday routine, it may feel difficult to — as they say — “live your best life.” The good news is, we understand a lot more about this condition than we once did.
Learning more about dissociation and DID can help you manage your symptoms.
To this end, trauma researcher Dr. Janina Fisher published a book in 2017 called “Healing the Fragmented Selves of Trauma Survivors: Overcoming Internal Self-Alienation.” The book offers information on the neurobiological basis of trauma and dissociation, along with treatment information for both therapists and clients.
See if you resonate with any of these resources:
- For an illuminating interview about DID, Med Circle talks with Encina, who has 11 distinct personalities. At the 54:10 minute mark, viewers meet one of her alters, Minnie, a 3-year-old girl.
- The System Speak podcast explores what it’s like for Emma, diagnosed at age 36, to live with DID. She regularly brings on experts to talk about managing symptoms and trauma recovery.
- Comedian Roseanne Barr, musician Adam Duritz, and retired NFL athlete Herschel Walker have all spoken about being diagnosed with DID. Walker wrote a book about it, called “Breaking Free: My Life With Dissociative Identity Disorder.”
Treatment of dissociative personality disorder in St. Petersburg
- Main
- Psychiatry
- Treatment of dissociative disorder
Dissociative personality disorder is a rather rare disease in our country. However, interest in this personality disorder is reflected not only in the Western European community of psychiatrists and psychotherapists, but also in modern cinema (for example, in the film Split, which was released in domestic cinemas in 2016). The disease itself is not associated with schizophrenia, as many still mistakenly believe, and the diagnosis (F44.8 according to ICD-10, 6B64 according to ICD-11) as such appeared in the International Classification of Diseases already in the 80s of the last century.
The disease itself is not associated with schizophrenia, as many still mistakenly believe, and the diagnosis (F44.8 according to ICD-10, 6B64 according to ICD-11) as such appeared in the International Classification of Diseases already in the 80s of the last century.
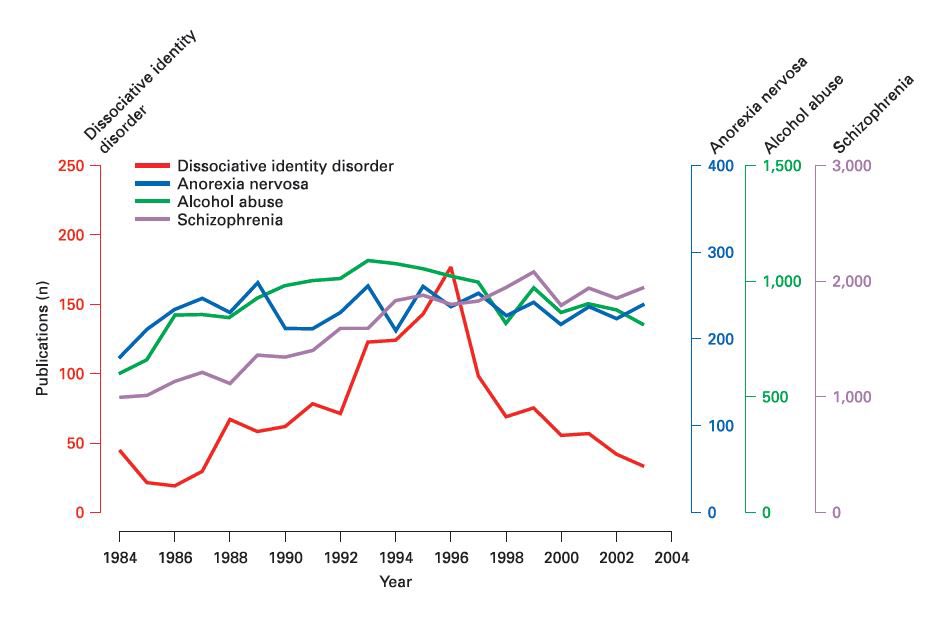
Since 1984, psychiatrists and psychotherapists have begun to form associations for the study of dissociative identity disorder. By 1995, more than 40,000 patients were diagnosed with this disease, previously defined as a subspecies of hysterical neurosis. To date, the treatment of dissociative personality disorder has been successfully carried out with the help of pharmacotherapy and psychotherapeutic treatment.
Dissociative personality disorder is one of the psychological defense mechanisms that occurs after a trauma suffered in childhood. The mechanism helps to cope with stress and, in most cases, represses memories of psychological or sexual abuse. The presence of any factors that contribute to the emergence of painful memories activates the alter ego (“other self”). Depending on the case, there may be several “other selves”. At the same time, the person himself does not know and does not remember what these “other selves” said and did after he comes to his senses.
Depending on the case, there may be several “other selves”. At the same time, the person himself does not know and does not remember what these “other selves” said and did after he comes to his senses.
In childhood, dissociative identity disorder may look like a kind of game and, as a rule, goes unnoticed not only by parents, but also by peers (for example, at school). However, entering adulthood, a person with a dissociative disorder begins to experience difficulties in communicating with other people and in family life. However, today there are examples of happy families with many children, where one of the spouses is diagnosed with a dissociative disorder.
Consultation of a doctor on the treatment of dissociative disorder:
+7 (812) 407-18-00
Thank you for your trust!
- Psychosocial personality correction
- Anonymous treatment without registration
- Assistance to family and relatives
| Service | Price | |
|---|---|---|
| Outpatient treatment | ||
| Psychiatric consultation | 5 000 ₽ | |
| Psychotherapist appointment | 5 000 ₽ | |
Reception of the chief physician Bocharov A. V. (Associate Professor, PhD) V. (Associate Professor, PhD) | 6 000 ₽ | |
| Psychiatric consultation at home | 6 000 ₽ | |
| Treatment in a hospital | ||
| Delivery to hospital | For free | |
| Standard Chamber | 8 900 ₽ | |
| 3-bed superior room | 12 000 ₽ | |
| 2-bed superior room | 15 000 ₽ | |
| 1 local VIP room | 19 500 ₽ | |
| Doctor's appointment 2 weeks after discharge | For free | |
Signs of dissociative personality disorder
Treatment of dissociative identity disorder
Help for family and relatives
Resources
Expert Q&A: dissociative disorders — https://psychiatry.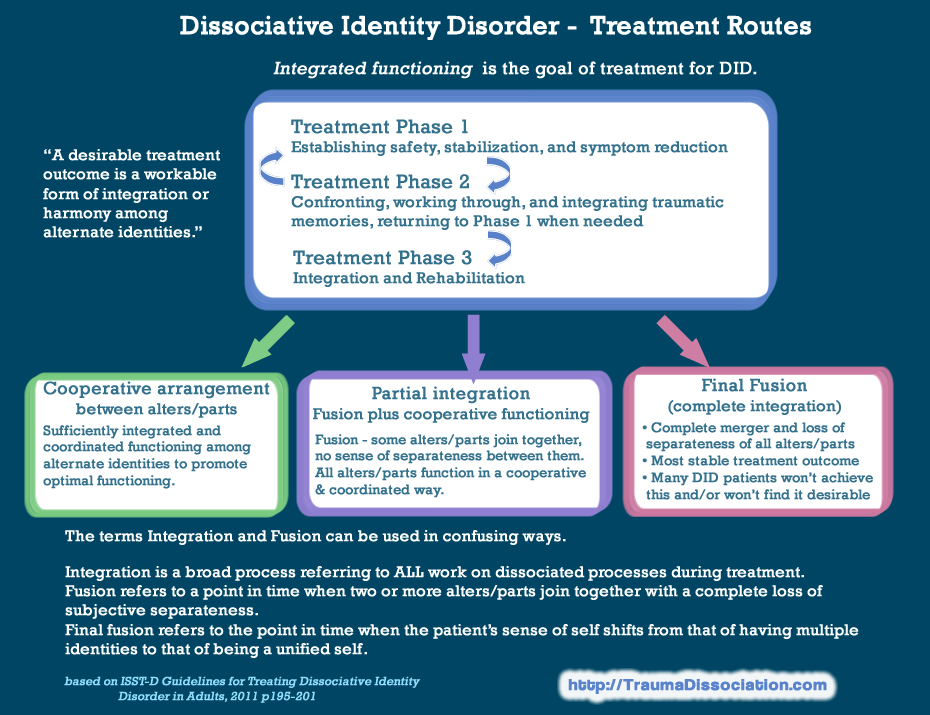 org
org
Clinical handling of patients with dissociative disorders — https://pubmed.ncbi.nlm.nih.gov
Dissociative identity disorder (multiple personality disorder) — https://www.webmd.com
Update date: 10/12/2022
- Depersonalization and derealization
- Suicidal behavior
- Anxiety disorder
Make an appointment
Date and time: (not set)
Make an appointment with a psychiatrist
Make an appointment with a psychiatrist
Select the date and time of your appointment
Tomorrow
February 19
Monday
February 20
Tuesday
February 21
Wednesday
February 22
Thursday
February 23
Friday
February 24
Saturday
February 25
Sunday
February 26
Monday
February 27
Tuesday
February 28
Treatment for dissociative disorder
Bocharov Alexey
Viktorovich
Psychiatrist, psychotherapist
Head physician of clinic
Experience 42 years
Psychiatrist, psychotherapist, sexologist, child psychiatrist
Work experience 42 years
Sinenchenko Andrey
Georgievich
Psychiatrist, psychotherapist
PhD
Work experience 23 years
Psychiatrist, psychotherapist, narcologist
Work experience 23 years
Zun Sergey
Andreevich
Psychiatrist, narcologist
PhD
Experience 34 years
Psychiatrist, narcologist, psychotherapist
Work experience 34 years
Lisitsyna Elena Alekseevna
Psychiatrist
Top category
Experience 34 years
Psychiatrist
Work experience 34 years
Buchelnikova Victoria
Viktorovna
Psychiatrist
Head of amb.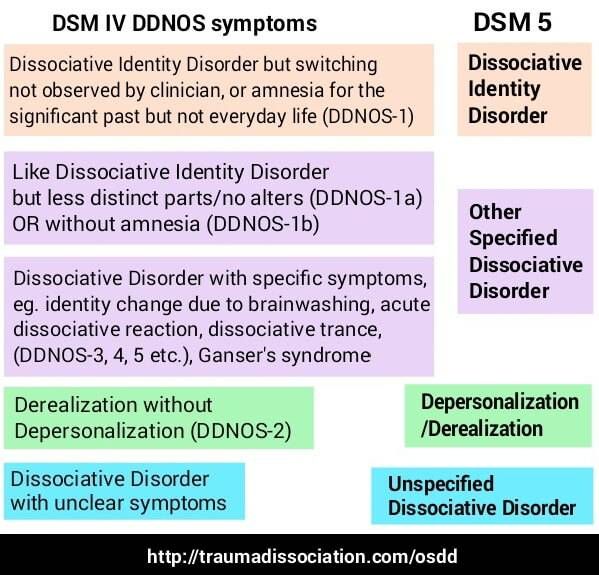 department
department
Work experience 16 years
Psychiatrist
Work experience 16 years
Voronina Elvira
Vladimirovna
Psychiatrist
First category
Experience 28 years
Psychiatrist
Work experience 28 years
Efimova Evgeniya
Vladimirovna
Psychiatrist
Second category
Experience 20 years
Psychiatrist
Experience 20 years
Gorobets Elena
Vasilievna
Psychiatrist
First category
Experience 17 years
Psychiatrist
Work experience 17 years
Travnikova Oksana
Mikhailovna
Psychiatrist
First category
Experience 22 years
Psychiatrist
Work experience 22 years
Kurochkina Nadezhda
Pavlovna
Psychiatrist
First category
Experience 20 years
Psychiatrist
Work experience 20 years
Suslennikova Elena
Viktorovna
Psychiatrist, psychotherapist
First category
Experience 26 years
Psychiatrist, psychotherapist
Work experience 26 years
Chuban Olga
Ivanovna
Psychiatrist, psychotherapist
First category
Work experience 14 years
Psychiatrist, psychotherapist, psychologist
Work experience 14 years
Popov Andrey
Petrovich
Psychiatrist
Top category
Experience 36 years
Psychiatrist
Work experience 36 years
Stetsiv Lyudmila
Gennadievna
Psychiatrist, psychotherapist
PhD
Experience 32 years
Psychiatrist, psychotherapist
Work experience 32 years
Prokhorchev Konstantin
Sergeevich
Psychiatrist, psychotherapist
First category
Work experience 13 years
Psychiatrist, psychotherapist
Work experience 13 years
Gulevsky Roman
Alexandrovich
Psychiatrist, narcologist
Head of hospital
Work experience 26 years
Psychiatrist, narcologist
Work experience 26 years
Konoplin Dmitry Alekseevich
Narcologist, psychiatrist
PhD
Experience 25 years
Narcologist, psychiatrist
Experience 25 years
Stavitskaya Svetlana
Yurievna
Psychiatrist
Top category
Experience 25 years
Psychiatrist
Work experience 25 years
Pylskaya Anna
Nikolaevna
Psychiatrist
Second category
Experience 8 years
Psychiatrist
Work experience 8 years
Trofimova Alexandra
Olegovna
Psychiatrist, child psychiatrist
First category
Experience 29 years
Psychiatrist, child psychiatrist
Work experience 29 years
Zholobetskaya Maria
Sergeevna
Psychiatrist, psychotherapist
Top category
Work experience 23 years
Psychiatrist, psychotherapist
Work experience 23 years
Endrzheevskaya Diana
Vadimovna
Psychiatrist, psychotherapist
Second category
Work experience 15 years
Psychiatrist, child psychiatrist, psychotherapist
Work experience 15 years
Usov Grigory
Mikhailovich
Psychiatrist, psychotherapist
MD
Experience 25 years
Psychiatrist, psychotherapist
Experience 25 years
Ivanov Alexander
Nikolaevich
Psychiatrist, narcologist
Top category
Experience 21 years
Psychiatrist, narcologist
Work experience 21 years
Semenov Andrey
Nikolaevich
Psychiatrist, narcologist
Leading specialist of clinic
Work experience 24 years
Psychiatrist, narcologist, transfusiologist
Work experience 24 years
Leave a request for a call:
+7 (812) 407-18-00
Dissociative disorder, Psychotherapy - Gestalt Club
Dissociative disorders (dissociation) is a group psychological disorders, defined as ".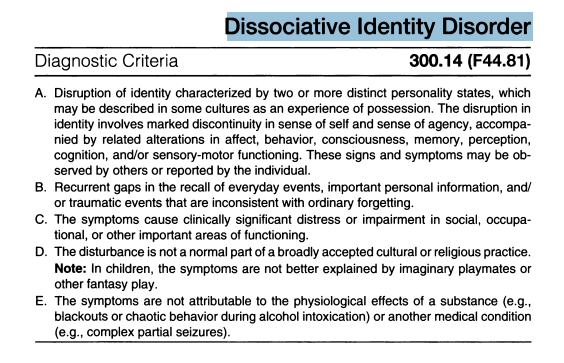 .. a violation habitual functions of consciousness, memory, personal identity or perception of the environment.
.. a violation habitual functions of consciousness, memory, personal identity or perception of the environment.
All dissociative disorders impair general functions patient affect both social relationships and performance.
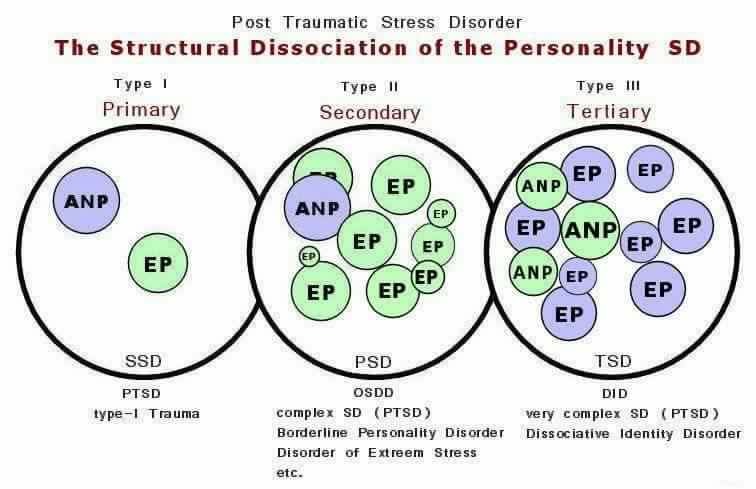
Dissociation (bifurcation) is a mechanism that allows the mind to to separate or divide into parts specific memories or thoughts ordinary consciousness. These bifurcated subconscious thoughts are not are erased. They may resurface spontaneously in consciousness. They are animated by trigger mechanisms (triggers), triggers objects and events surrounding a person during traumatic event.
The process of dissociation (bifurcation) is a serious and long process with a large spectrum of action. If patient (client) has a dissociative disorder, it is not means that this is a manifestation of a mental illness. A moderate degree of dissociation can occur in consequences of stress; in people who have spent a long time without sleep, received a dose of "laughing gas", during a dental operations or suffered a minor accident - often receive short dissociative experience. Another simple example dissociative disorder - a person, sometimes it happens wholly interested in a book or film, what the world around and time pass by unnoticed. Known dissociation is associated with hypnosis, which in turn includes a temporary change in the state of consciousness.
Another simple example dissociative disorder - a person, sometimes it happens wholly interested in a book or film, what the world around and time pass by unnoticed. Known dissociation is associated with hypnosis, which in turn includes a temporary change in the state of consciousness.
People often have dissociative experiences during confession religion (being in special trance states), or other group or individual lessons (meditation practices, the highest level of autogenic training). These cases are not worth perceived as "frequent/usual", considering Ukraine.
Moderate or complex forms of dissociation are observed in individuals with traumatic experiences of childhood abuse, participants in hostilities, robberies, torture or transfer of a natural disaster, a car accident. dissociative symptoms may develop in patients with severe manifestations of post-traumatic stress disorder disorders, or with disorders that have formed in during somatization (diseases of internal organs, as a result of psychological conflicts).
In a state of dissociative amnesia, the patient is unable to remember important personal information to the extent that it cannot be justify by natural forgetfulness. In many cases, this is a reaction in a traumatic event or when a person was a witness cruel crime. Patients with dissociative amnesia may develop depersonalization or trance states, but without changes in personal identity.
In a dissociative flight reaction, the person temporarily loses sense of personal identity and travels to another place where, as it seems to him, you can find a new identity of yourself. Again, such behavior most often follows a major injury or stress. For others, besides the fact that patients with dissociative disorders cannot remember the past or personal information, their behavior does not look strange and does not harm society. cases dissociative flight most commonly encountered in wartime or in areas prone to natural disasters.
The main symptom of depersonalization is separation from own "I".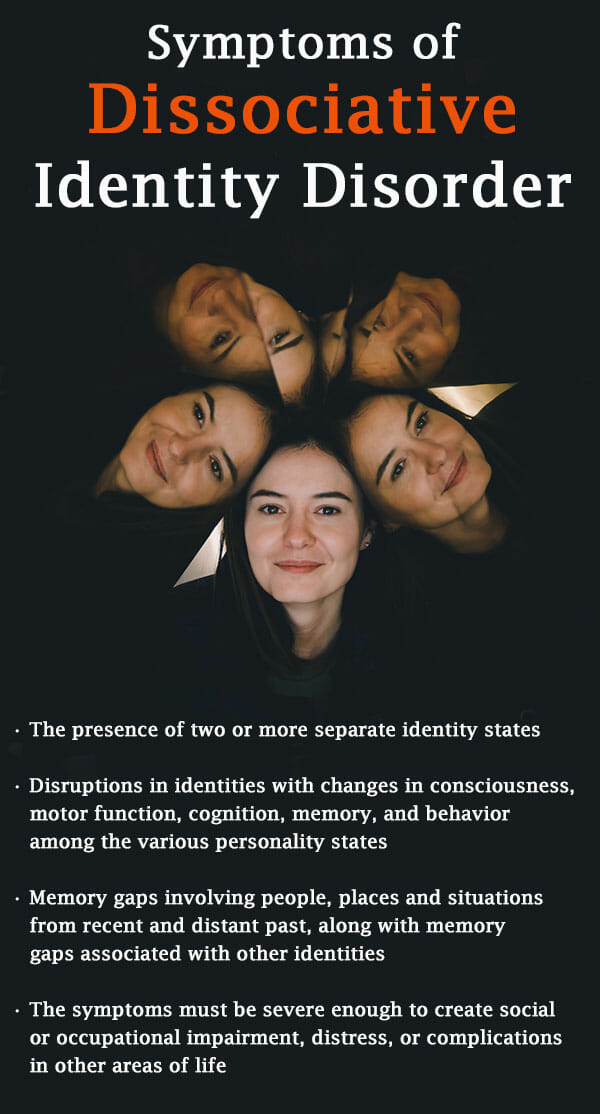
Depersonalization as a symptom (not a disorder), quite a frequent occurrence among the student age group. He is often associated with sleep deprivation or drug use “to have fun" and may be accompanied by "derealization" (disorder perception of the environment, for example, in situations where objects around appear to be modified). Sometimes patients describe depersonalization, like feeling like a robot or watching yourself from the side.
Depersonalization disorder may also include a feeling of immobility, insensibility, or loss of emotional "liveness".
Dissociative Identity Disorder (DID) is new name for habitual multiple personality disorder (MPD). DID considered the most severe dissociative disorder and has most major dissociative symptoms.
DDNOS (dissociative disorder not otherwise specified) place) is attributed to patients with dissociative symptoms, which cannot be included in any of the categories of special dissociative disorder.
Both mild/moderate and complex dissociations that occur in patients with dissociative disorders, occur as a result of a set of causes:
Innate ability to easily dissociate
Recurrent episodes of mental or sexual abuse in childhood
Lack of a person who would support, comfort and protect from abusive relatives
The influence of other family members suffering from dissociative disorders, symptoms.
Association of dissociative disorders with abuse in childhood gave rise to deep discussions and lawsuits in which, under the issue is the accuracy of childhood memories.
Information stored in the brain, recovery functions and interpretation of memory is not yet fully understood.
Main dissociative symptoms:
Amnesia - marked by lapses in the patient's memory for a long time time (observed after traumatic events).
Depersonalization is a state of perception in which the patient feels that his body is not real, unnatural, that it changes or disappears.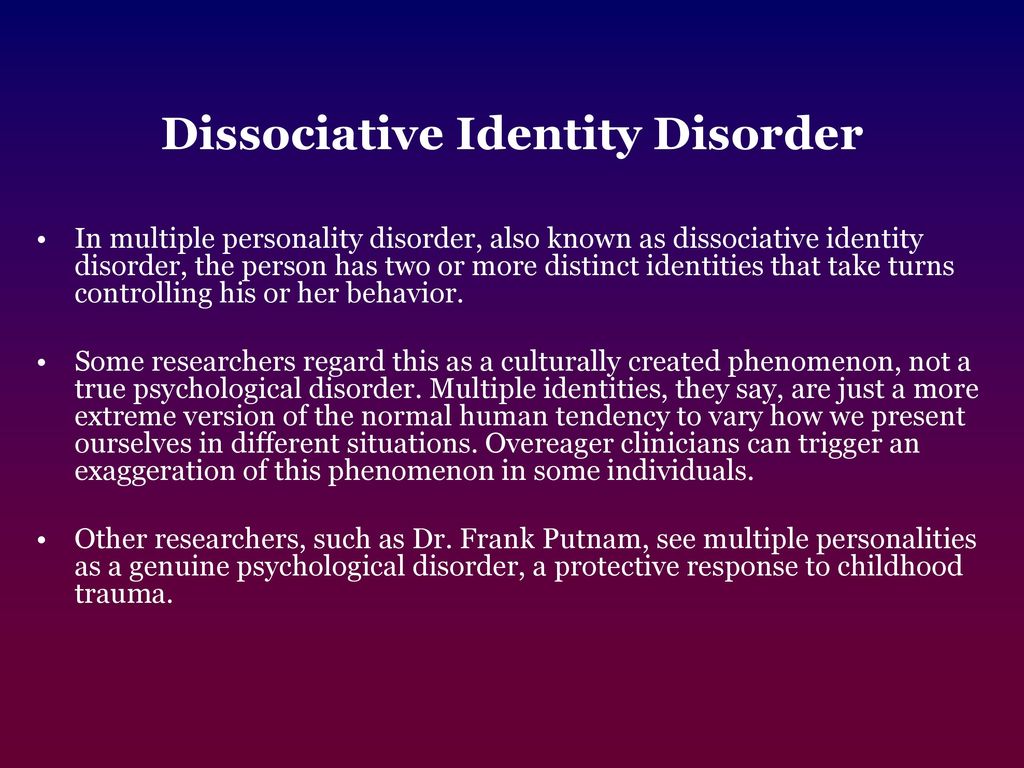 Some patients feel detachment from your body, or watching a movie with your own participation.
Some patients feel detachment from your body, or watching a movie with your own participation.
Derealization - everything around is perceived as fake. The patient sees walls, buildings, or other objects that change shape, size or color. In some cases, the patient may it seems that the people around him are robotic machines, although he himself understands the unreality of such sensations.
Dissociative Flight Reaction Patients with DDNOS or DID are often confused about their identity or invent a new identity for themselves. Subsequently stressful experience, the patient may behave differently than before, respond to different names, or be unaware of what is happening around.
Treatment of dissociative disorders may include psychotherapy, medication, or a combination of both approaches.
In the case of psychotherapy, patients often need help doctor who specializes in this problem and has experience in treatment of dissociative disorders.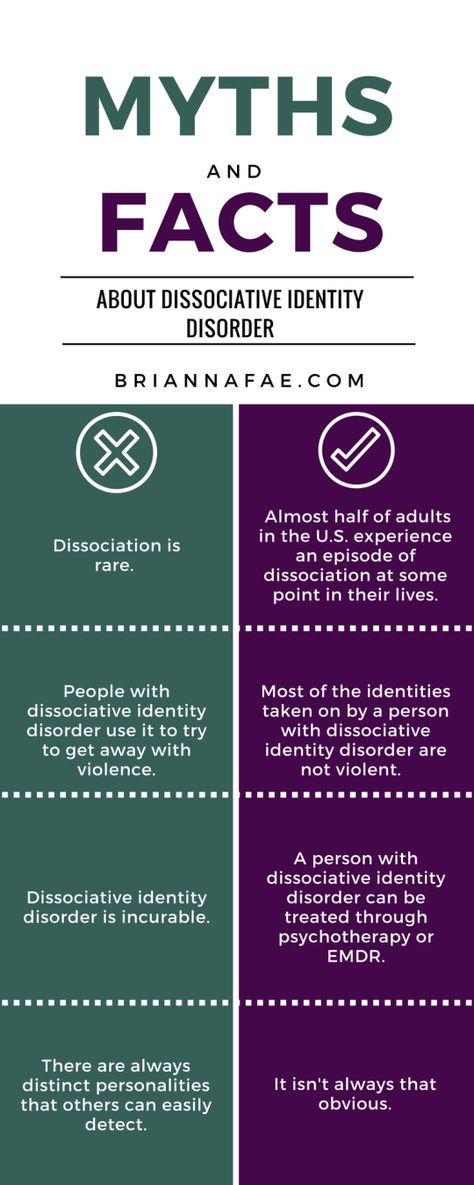 Such knowledge is especially necessary if the patient's symptoms are expressed by problems definitions of personal identity.
Such knowledge is especially necessary if the patient's symptoms are expressed by problems definitions of personal identity.
Some doctors prescribe tranquilizers or antidepressants for excessive activity, anxiety and/or depression, which often occurs along with dissociative disorders. However, patients with dissociative disorders more prone to addiction and dependence on medications.
Hypnosis is often recommended as one of the methods treatment of dissociative disorders, in part because hypnosis associated with the process of dissociation. Hypnosis helps to get rid of depressing ideas or memories. Professionals treating patients with DID, use hypnosis from time to time in the process of "closing" alternative personalities.
Prospects for recovery from dissociative disorders different. Recovery from dissociative flight is usually happens quickly. Dissociative amnesia can be cured quite quickly, but in some patients it can become chronic disorder.