Psychiatric occupational therapist
Occupational Therapy for Mental Health
At the Johns Hopkins Department of Physical Medicine and Rehabilitation, our occupational therapists specialize in helping patients with mental health disorders. Our occupational therapists are experts in performing behavioral health assessments, which offer insight into a patient’s condition. They have strong observation and creative problem-solving skills, and understand human development and function across different diagnoses.
Why Choose Johns Hopkins
Patients may have challenges in the areas of planning tasks, organizing, problem solving and decision making. They may also have difficulties with controlling emotions, which can make it difficult to function and be independent in society. Occupational therapy can help improve on or compensate for these challenges. Our occupational therapists use standardized and nonstandardized screening and assessments to make recommendations for treatment, which may include:
- Patient and caregiver education
- Practicing life management skills
- Adapting tasks or environment to become more independent
- Developing coping mechanisms to deal with emotional problems
Psychiatric Occupational Therapy Team
Our psychiatric occupational therapy team works closely with patients with mental illness. Our therapists help these patients improve their function in work, play, leisure, social life, self-care and community living skills. Our team is highly trained in assessing these skills and making recommendations for treatment and safe discharge.
-
Bobby Walsh, DBH, OTR/L, BCMH | Team Lead
AOTA Board Certification in Mental Health
-
Tess Spence, MS, OTR/L | Clinical Specialist
Helping Patients Enjoy Life to the Fullest
Our occupational therapists are trained to identify difficulties in performing daily activities. They help address these underlying problems through the activities listed above. Our team can work with patients and their loved ones to improve these and other life management skills:
- Creating and following a productive daily schedule
- Taking care of personal hygiene
- Managing one’s own health
- Navigating the community and using public transportation
- Organizing and following a medication regimen
- Interacting appropriately in work or social situations
- Working or volunteering
- Planning and cooking healthy meals
- Managing budget and finances
Developing Habits That Are Important to You
Habit training was the first occupational therapy treatment model. It was introduced by Eleanor Clarke Slagle, with input from psychiatrist Adolf Meyer, when both worked at Johns Hopkins in the early 1900s. Habit training focuses on balancing activities in the areas of work, rest and play, which can be unbalanced in people with mental health disorders. When occupational therapy was fairly new, habit training was heavily focused on arts and crafts. Now, our updated approach emphasizes meaningful activities rooted in independent living and quality of life.
It was introduced by Eleanor Clarke Slagle, with input from psychiatrist Adolf Meyer, when both worked at Johns Hopkins in the early 1900s. Habit training focuses on balancing activities in the areas of work, rest and play, which can be unbalanced in people with mental health disorders. When occupational therapy was fairly new, habit training was heavily focused on arts and crafts. Now, our updated approach emphasizes meaningful activities rooted in independent living and quality of life.
Request an appointment with one of our mental health occupational therapy experts to discuss how we can help you or your loved one.
Locations and Referrals
Our psychiatric occupational therapy team is based in The Johns Hopkins Hospital and offers both inpatient and outpatient services, as well as partial hospitalization. Contact us if you are looking to make an appointment or refer a patient.
Occupational Therapists and Mental Health Interventions
Image credit: BD Hypno Plus
Occupational therapy focuses on the therapeutic use of daily activities (or occupations) with individuals or groups. This is to improve their participation in roles, habits, and routines in the home, school, workplace, community, or other settings. An occupational therapist helps you to get back to your customary activities as much as possible. They work with individuals who have physical and cognitive impairments, psychosocial dysfunction, mental illness, and developmental (or learning) challenges. So let’s discuss the significance of occupational therapists and mental health interventions.
This is to improve their participation in roles, habits, and routines in the home, school, workplace, community, or other settings. An occupational therapist helps you to get back to your customary activities as much as possible. They work with individuals who have physical and cognitive impairments, psychosocial dysfunction, mental illness, and developmental (or learning) challenges. So let’s discuss the significance of occupational therapists and mental health interventions.
Occupational Therapists and Mental Health and Wellness
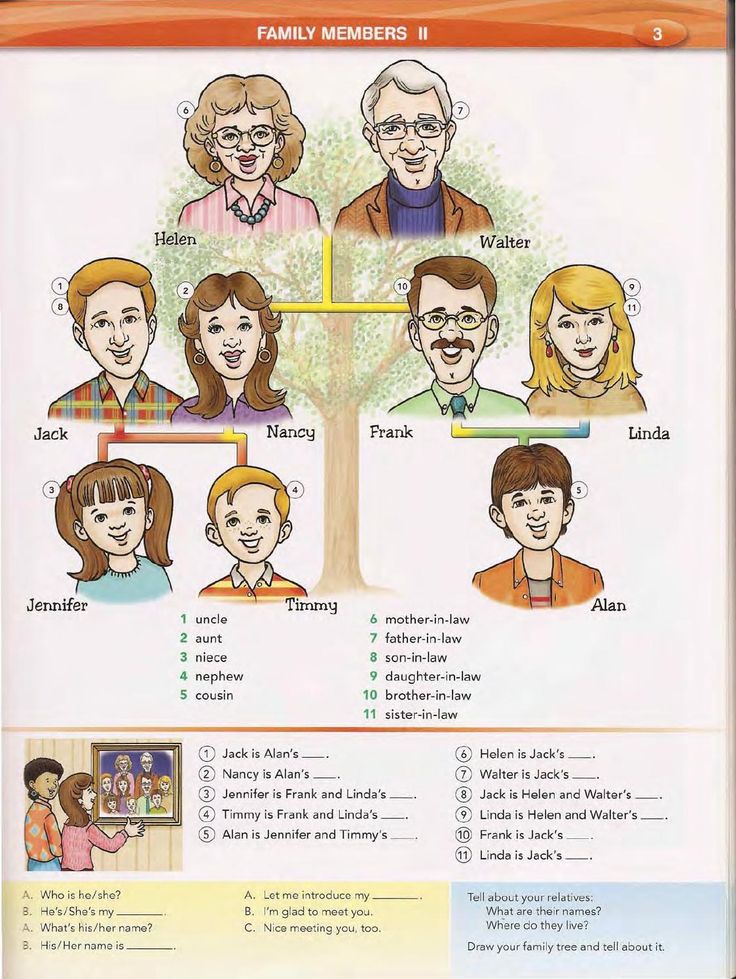
An occupational therapist assesses each client holistically. For each client, they will consider various factors such as:
- Values, beliefs, spirituality, mental function, sensory function, etc.
- Performance skills (or motor, process, and social interaction skills)
- Environment or context
- Performance patterns (or habits, routines, roles, etc.)
Your occupational therapist will work with you to promote, establish (or restore), maintain, or modify tasks to help you participate fully in your daily life. Furthermore, occupational therapists will seek to prevent potential barriers to participation in desired activities.
Furthermore, occupational therapists will seek to prevent potential barriers to participation in desired activities.
Is Occupational Therapy Considered Mental Health Assistance?
Mental health is an essential component of all occupational therapy interventions. Occupational therapists provide mental health treatment and prevention services for all – children, youth, the aged, and people with severe and persistent mental illness. All interventions focus on improving each client’s function and independence.
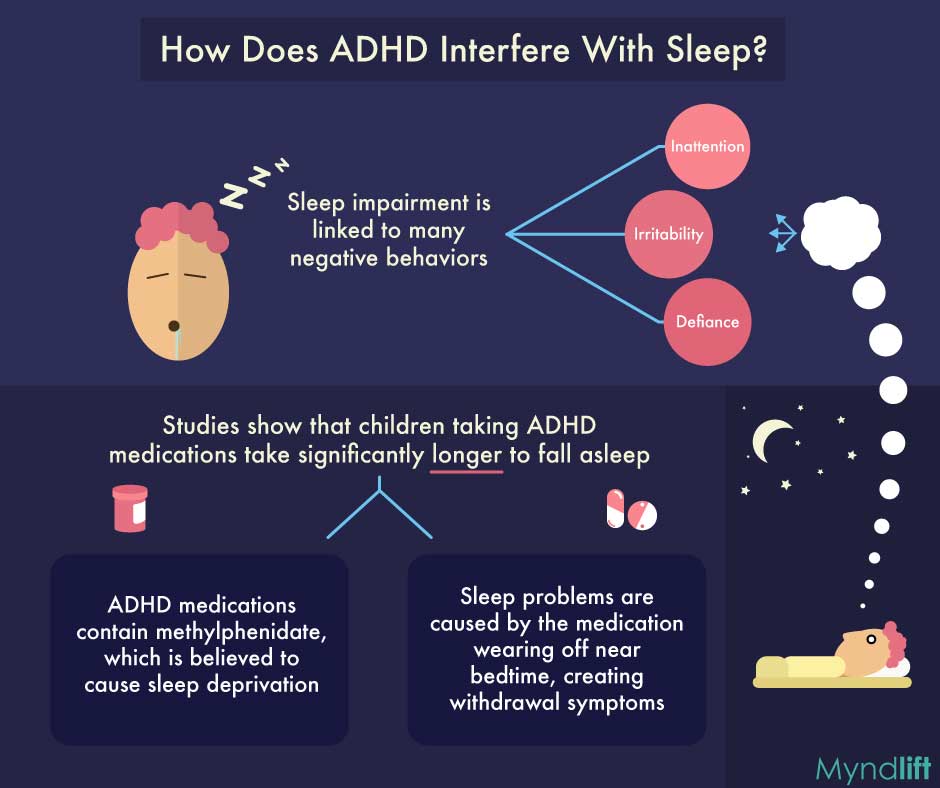
Occupational therapists work in mental health settings and they focus on enabling persons to re-engage in useful occupations. How do they do this? They help each client build a variety of skill sets, establish good habits and routines, set therapy goals, apply cognitive-behavioral techniques (CBT), and understand and counter physiological influences.
Within the settings of children’s and adolescents’ mental health, occupational therapy focuses on these physiological influences. They teach clients how to identify and utilize self-regulation strategies to get them back to participating in meaningful activities like going to school or work and interacting with family and friends.
They teach clients how to identify and utilize self-regulation strategies to get them back to participating in meaningful activities like going to school or work and interacting with family and friends.
Also, occupational therapists serve individuals with sensory processing disorders (SPD) and social-emotional learning dysfunctions. These conditions are usually seen within the children and adolescent segments of the mental health sector.
Occupational Therapy and Community Mental Health
Did you know that occupational therapy has its roots in mental health? It’s true! The creation of the profession coincided with the early 20th century’s mental hygiene movement.
Eventually, the call for deinstitutionalization of people with mental challenges led to the 1963 Community Mental Health Act. This act meant that occupational therapists and their assistants began working in community mental health. Today, occupational therapy within community mental health settings provides services such as:
- Community mental health centers
- Assertiveness community treatment (ACT) teams
- Psychosocial clubhouses
- Homeless and women’s shelters
- Correctional facilities
- Senior centers
- Consumer-operated programs
- After-school programs
- Homes
- Worksites
As mental health services have shifted from the hospital to the community, there has also been a paradigm shift in the service delivery philosophy. Traditionally, there was an emphasis on the medical model, but now the focus is on implementing the recovery model.
Traditionally, there was an emphasis on the medical model, but now the focus is on implementing the recovery model.
This latter model acknowledges that recovery is a long-term process and clients are encouraged to keep participating in community activities until they can do so fully. Therefore, occupational therapy activities include finding and keeping employment, going to school, and living independently.
The philosophical foundation of this recovery model is the integration of occupational therapy with community mental health. The goal of this integration is to increase your ability to live independently, as much as possible, in the community as you engage in productive daily activities.
Occupational therapy facilitates your participation and is client-centered. It also plays a significant role in the success of those recovering within the community. Occupational therapists and occupational therapy assistants are educated to deliver mental and physical health and wellness services, rehabilitation, habilitation, and recovery-focused approaches. They are also trained in clinical fieldwork that’s focused on assessing psychosocial issues.
They are also trained in clinical fieldwork that’s focused on assessing psychosocial issues.
Examples of Occupational Therapy Within Mental Health
Occupational therapy interventions improve the health outcomes of those with mental health challenges. These interventions are found in the areas of education, work, skills training, health, and wellness, as well as cognitive remediation and adaptation. Some examples of occupational therapy interventions in community mental health include:
Evaluating and adapting the home, work, school, and other settings to facilitate your optimal functioning.
- Providing educational programs, experiential learning, and treatment groups or classes to address key issues. These issues include assertiveness, self-awareness, interpersonal and social skills, stress management, and role development (for example, parenting).
- Helping clients develop leisure or avocational interests and pursuits.

- Developing skills for independent living such as using community resources, managing your home, time, and medication, as well as being safe at home and in the community.
- Providing training in daily living activities (for example, hygiene and grooming).
- Consulting with employers about appropriate accommodations for their clients (as required by the 1990 Americans with Disabilities Act).
- Conducting functional evaluations and ongoing monitoring for successful job placement.
- Guiding and consulting with persons in all employment settings (including supportive employment).
- Providing evaluation and treatment for sensory processing deficits.
Occupational therapy benefits individuals of all ages with a variety of mental illnesses. Furthermore, friends and family members also benefit from occupational therapy as they learn how to deal with the stress of caregiving and successfully balance their daily responsibilities in life.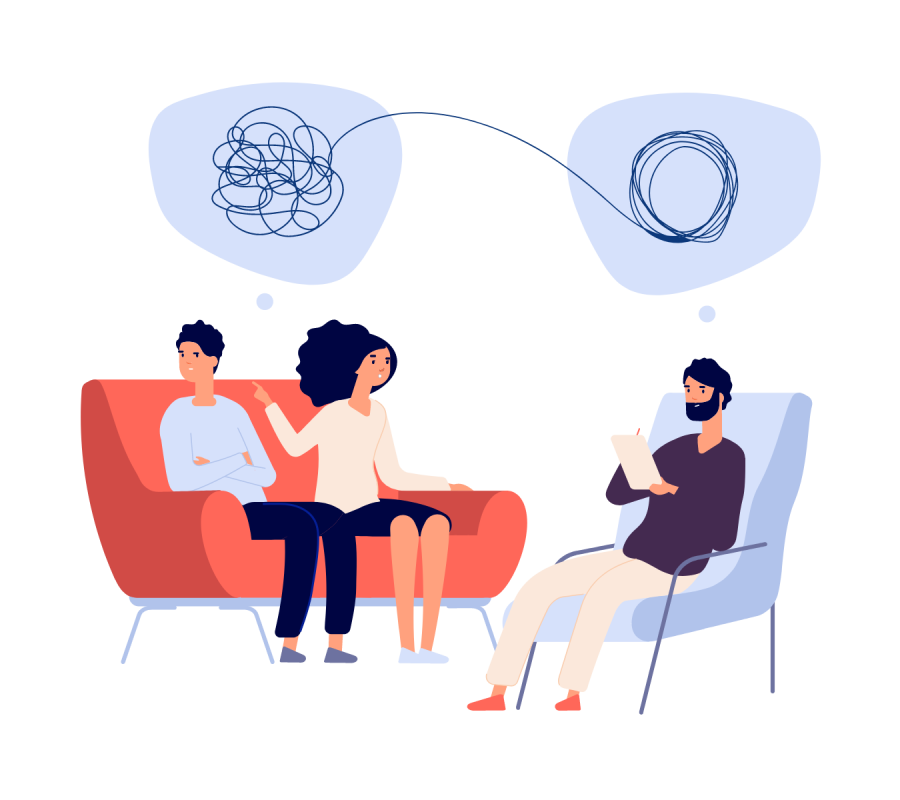
Occupational Therapy Approaches
Occupational therapists use several evidence-based approaches within the mental health environment. They include:
- Teaching coping and self-regulation skills that are useful in a variety of contexts.
- Educating people about sensory exploration and implementing sensory approaches for self-regulation.
- Utilizing CBT approaches to support your participation in desired activities.
- Identifying and implementing healthy, positive habits, and structure into daily routines.
- Supporting the learning and implementation of key skills. These skills include those related to social competence (like making and keeping friends), coping with anger, solving problems, learning about social etiquette, and following rules.
- Evaluating factors that block your success in school, at work, as well as in your home and community.

- Modifying your environment to support improved attention, participation, and decrease sensory overload at school and/or at work.
- Educating parents about important behavioral and psychosocial approaches to enhance their children’s daily functioning.
- Reducing restraints and seclusions within the inpatient setting. This is done via comprehensive assessments to determine what facilitates and bars your participation in:
- Life tasks
- Self-awareness and skills development
- Developing attainable goals
- Modifying your environment for optimal fit.
- Promoting the use of self-regulation and sensory strategies.
- Educating an interdisciplinary team on prevention techniques.
Can an Occupational Therapist Assist With Anxiety?
Occupational therapy plays a significant role in helping clients suffering from anxiety to manage their condition. An occupational therapist will work with you to identify how anxiety is affecting you, teach you valuable coping skills, and help you work towards achieving your future goals.
An occupational therapist will work with you to identify how anxiety is affecting you, teach you valuable coping skills, and help you work towards achieving your future goals.
Can an Occupational Therapist Perform Psychotherapy?
Occupational therapists are authorized to provide psychotherapy services. Furthermore, these psychotherapy services are performed according to the standards of the practice.
What You Can Expect From a Mental Health Occupational Therapist
Many people think of occupational therapy as applicable to pediatric services or physical rehabilitation. So they are often surprised to find occupational therapists working in mental health environments. So if you, a relative, or a friend is seeing a mental health occupational therapist, then keep reading to learn about how they can help you.
An Occupational Therapist’s Contributions to a Mental Health Treatment Team
An occupational therapist undergoes training in holistic approaches that are suitable for work in mental health settings. Their areas of training include:
Their areas of training include:
- Physical wellbeing
- Cognitive assessment
- Sensory strategies
- Therapeutic alliances
- Group activities
- Participation in activities of daily living (ADLs)
- Socio-emotional skills
Occupational therapy assists clients to participate in daily activities as independently as possible.
Mental Health Occupational Therapy Interventions
Some of these interventions include:
Lead GroupsOccupational therapists are trained to create lead groups in areas that focus on:
- Life skills
- Job readiness
- Therapeutic cooking
- Money and time management
- Wellness recovery action plans (WRAPs)
- Therapeutic leisure
- Nutrition
- Sensory groups
- Independent living
Occupational therapists use activities of daily living (ADLs) or occupations to aid in optimal mental health and welfare. They may also help you use coping mechanisms like listening to music, playing cards, writing, drawing, cooking, or cleaning.
They may also help you use coping mechanisms like listening to music, playing cards, writing, drawing, cooking, or cleaning.
They are also experts at applying sensory strategies. Your sensory system helps you process information that you gather from your environment. Clients with mental health challenges have a compromised ability to process sensory input, which can lead to them feeling agitated and unsafe.
Sensory strategies activate your basic processing systems like the vestibular, proprioceptive, and deep pressure touch, to help you process information. These strategies help you to feel safe and calm. These sensory strategies may prove very helpful for persons who may not be able to benefit from talk therapies.
Sensory Rooms
Occupational therapists serve as a part of a larger movement to create sensory rooms in mental health facilities. These sensory rooms are safe havens for clients. These rooms also tend to have tools to help them de-escalate and relax.
Occupational therapists use a series of assessments to see if clients are ready to be discharged. These standardized assessments provide valuable information. In turn, this information helps your treatment team understand the level of care that’s required for discharge and to monitor your treatment progress.
Address Physical WellbeingAnother vital service that an occupational therapist provides is their physical rehabilitation background. Mental health issues are often accompanied by physical health issues.
In a mental health environment, you may find that your occupational therapist:
- Addresses general strengthening
- Adjusts wheelchairs
- Recommends adaptive equipment
- Performs any other activity that’s within the scope of occupational therapy
Your occupational therapist will assist you in mastering your daily activities. If your mental health condition compromises your ability to fully complete your daily activities, then speak to your occupational therapist about your concerns. Even if your occupational therapist doesn’t have the tools necessary to address your mental health requirements, they can advocate on your behalf and assist you to get the help you need.
If your mental health condition compromises your ability to fully complete your daily activities, then speak to your occupational therapist about your concerns. Even if your occupational therapist doesn’t have the tools necessary to address your mental health requirements, they can advocate on your behalf and assist you to get the help you need.
Mental Health Specializations
Many occupational therapists are experts in trauma-informed care and the recovery model. They gain this expertise either through their schooling, workplace training, or independent study. Some occupational therapists will then proceed to earn their Certified Psychiatric Rehabilitation Practitioner (CPRP) certification.
Occupational therapists possess unique knowledge and skills that facilitate effective, holistic mental health interventions. Incorporating occupational therapy skills like sensory approaches and psychosocial techniques help clients to effectively function in their daily lives.
How Long is Rehab After a Mental Health Incident?
After a mental health crisis, hospitalization is often necessary for stabilization and treatment. Some of the reasons for hospitalization include any conversations about suicide or death, self-harm, violence toward others, psychosis symptoms (like hallucinations and delusions), or a complete inability to carry out daily life skills.
Some of the reasons for hospitalization include any conversations about suicide or death, self-harm, violence toward others, psychosis symptoms (like hallucinations and delusions), or a complete inability to carry out daily life skills.
The length and severity of a mental health episode vary and so the length of stabilization also varies. However, most individuals stabilize within a few days of staying in a hospital. Studies have shown that the average length of hospitalization is 10 days. Hospital stays may also last longer when placed in psychiatric care than when in a regular hospital.
However, rehabilitation is different as this phase occurs after a patient has been stabilized. The length of rehabilitation will also vary according to the individual, their prognosis, and how quickly they can learn and effectively implement coping skills.
How Do I Find a Rehabilitation Program for Occupational Therapy for Mental Health?
We have shown that occupational therapists and mental health are intertwined. Are you wondering how to find an occupational therapy rehabilitation program for mental health? We have an outstanding option for you at Moving With Hope in Shelton, CT.
Are you wondering how to find an occupational therapy rehabilitation program for mental health? We have an outstanding option for you at Moving With Hope in Shelton, CT.
We provide the best occupational therapists who effectively assist clients with a variety of mental health challenges. At Moving With Hope, we will also work with your medical team to create an effective treatment plan to suit your needs. We invite you to contact us today to begin your journey to health and wellness, inside and out.
Occupational Therapy
Introduction
What is Occupational Therapy?
The task of occupational therapy is to support people who are at risk of getting or already experiencing difficulties in maintaining themselves in everyday life. The theoretical basis of occupational therapy is that there is a relationship between activity and health and well-being. Participation in meaningful and meaningful activities therefore leads to both better health and better well-being of the patient/client.
The code of ethics for occupational therapists makes it clear: “The goal of occupational therapy is to develop the patient/client's ability to lead a fulfilling life in accordance with their desires and needs, and in proportion to environmental requirements. The occupational therapist's means to achieve these goals is to use occupational therapy to develop the patient/client's ability to be active or to prevent a decrease in this ability, and, if necessary, to compensate for reduced activity so that the client feels satisfaction in his daily life.
The result of ergotherapeutic measures in each case is an improvement in the quality of life, an increase in independence and inclusion in society.
Activity as end and means
During occupational therapy, the activity of the patient/client becomes as therapeutic as possible in relation to the goal he is striving for.
The above concerns, for example, the environment, the degree of activity structure, the degree of intimacy in relationships, and the degrees of difficulty from various points of view. The therapeutic activity is aimed at obtaining new experiences that can provoke and stimulate the patient/client. Often this leads to a new direction in activities and positive changes for the patient/client. Another goal is for the activity to be carried out as naturally as possible, so that outwardly it seems to be random and not a prepared process, although in reality it is the result of constant and active ergotherapeutic diagnosis and intervention.
The therapeutic activity is aimed at obtaining new experiences that can provoke and stimulate the patient/client. Often this leads to a new direction in activities and positive changes for the patient/client. Another goal is for the activity to be carried out as naturally as possible, so that outwardly it seems to be random and not a prepared process, although in reality it is the result of constant and active ergotherapeutic diagnosis and intervention.
For an intervention to be successful, "accuracy in time" is essential. The intervention must take place at the right time, that is, in the right context and when the individual is ready for it. If the intervention occurs earlier than necessary, there is a risk of failure, and if it is delayed, then it becomes irrelevant. The occupational therapist conducts an assessment with the patient/client and analyzes his or her abilities in relation to the levels of difficulty in the activity. An ergotherapist is a professional instructor who helps the patient/client, from the field of psychiatry to adaptation in society. This help happens with the cooperation between the community
This help happens with the cooperation between the community
What does an occupational therapist do in a mental health service?
The occupational therapist always considers the needs of each patient/client. Events are thus developed for each individual. They aim to enable the patient/client to manage self-care, daily activities and free time as independently as possible. These measures vary depending on the problems, needs, wishes and conditions. The timing also varies from short to long.
The first contact with an occupational therapist in psychiatry begins with the diagnosis of the consequences of mental disorders in everyday life and work. In other words, it is determined what level of functional activity the patient has. In ergotherapeutic examination, great importance is attached to the study of the resources of the individual and the difficulties that exist in the space surrounding him. The survey uses different forms of assessment tools.
An examination is sometimes a preparation for an independent evaluation and most often marks the start of a specific treatment. The most important starting point in formulating goals and a treatment plan is what the patient/client himself assesses as a problem or goals for his work. Therefore, a treatment plan or rehabilitation plan, including goals and objectives, is developed together with the patient/client. Sometimes the goal is for the patient/client to regain their former ability to be active. Sometimes the examination is that the performance of an activity or environment requires a change or adjustment. The intervention then aims to develop new personal skills and strategies, to find new roles and to learn new skills while adapting to the social and physical environment (at home, at work, etc.). Throughout the treatment period there is continuous mutual feedback, monitoring and evaluation between the occupational therapist and the patient/client. This leads to the fact that the intermediate goal can sometimes be formulated again.
The most important starting point in formulating goals and a treatment plan is what the patient/client himself assesses as a problem or goals for his work. Therefore, a treatment plan or rehabilitation plan, including goals and objectives, is developed together with the patient/client. Sometimes the goal is for the patient/client to regain their former ability to be active. Sometimes the examination is that the performance of an activity or environment requires a change or adjustment. The intervention then aims to develop new personal skills and strategies, to find new roles and to learn new skills while adapting to the social and physical environment (at home, at work, etc.). Throughout the treatment period there is continuous mutual feedback, monitoring and evaluation between the occupational therapist and the patient/client. This leads to the fact that the intermediate goal can sometimes be formulated again.
In occupational therapy, the patient/client's experience of meaning, context and interaction are important components. The occupational therapist acknowledges and encourages the resources and initiative of the patient/client. At the same time, the occupational therapist should encourage the patient/client to have a realistic vision of their goals and changes in work. This is achieved with hope, but without a lot of promises.
The occupational therapist acknowledges and encourages the resources and initiative of the patient/client. At the same time, the occupational therapist should encourage the patient/client to have a realistic vision of their goals and changes in work. This is achieved with hope, but without a lot of promises.
An occupational therapist is present at every level of care
Psychiatric care in Sweden today is divided into three different levels: primary care, specialized psychiatry and social psychiatry. The level of care a patient/client receives depends on his or her functioning and whether there is a threat or risk to the safety of the patient/client or others. Occupational therapists work at all levels, but to a lesser extent in primary care, as this level is not strictly psychiatric. The division of responsibility between primary care and specialized psychiatry is also quite new.
About 600 (1) occupational therapists currently work in psychiatric care, most of them in specialized psychiatry. However, a minimum of about 1000 occupational therapists is required to cover the existing need.
However, a minimum of about 1000 occupational therapists is required to cover the existing need.
Psychiatry in Primary Care
Primary care, ie polyclinic with community physicians, is responsible for the treatment and rehabilitation of acute crisis reactions, mild depression and mild/moderate anxiety disorders. Occupational therapists work at this level today.
This level of rehabilitation exists in the tradition of providing treatment without psychiatric diagnoses, although many of the patients suffer from mental problems. In many regions of the country, special teams and programs have been established for patients/clients with pain problems or stress-related conditions. There are also psychosomatic problems, where depression and anxiety become a concomitant or secondary diagnosis. Psychiatric diagnosis is therefore not seen as a focus for intervention. Some polyclinics have a psychologist and a social worker (curator), and sometimes even a psychiatrist. However, there is still a lack of resources for early rehabilitation measures. Primary care needs additional resources and professional competence to offer people suffering from mental disorders optimal examination and early rehabilitation, in accordance with existing guidelines.
Primary care needs additional resources and professional competence to offer people suffering from mental disorders optimal examination and early rehabilitation, in accordance with existing guidelines.
Occupational therapists have developed methods in the study of the ability to be active, as well as the functional level of patients in their daily life (personal hygiene, accommodation, free time, work). Therefore, there is a great need for the work of an ergotherapist in polyclinic psychiatry.
Specialist Psychiatry
Specialist Psychiatry is responsible for the treatment and rehabilitation of patients/clients with more severe, difficult to treat or chronic mental disorders. Occupational therapy has traditionally held a central position in specialized psychiatry. Most occupational therapists working in psychiatry practice at this level of psychiatric care.
Simultaneously with the development of psychiatry, new ergotherapeutic methods develop, theoretical developments and explanatory models appear. Therefore, there is already a tradition of accumulating knowledge tested by experience. Validated and credible assessment tools are also being developed. Scientific research in occupational therapy, however, has only begun in recent years, which means many methods are yet to be tested.
Therefore, there is already a tradition of accumulating knowledge tested by experience. Validated and credible assessment tools are also being developed. Scientific research in occupational therapy, however, has only begun in recent years, which means many methods are yet to be tested.
Psychiatric problems should in most cases be treated on an outpatient basis. Treatment in the hospital is limited and therefore the time of stay in the hospital is quite short. The task of an ergotherapist in a hospital is, firstly, to study the need for rehabilitation of the patient/client, and secondly, to assess the patient/client's ability to care for himself independently in everyday life.
A psychiatric outpatient department most often consists of a multi-professional team, including an occupational therapist. The occupational therapist takes part in the examination and treatment plan developed by the team. The occupational therapist is responsible for assessing the patient/client's ability to perform daily life and work responsibilities, and presents an appropriate treatment and rehabilitation plan, or makes recommendations to other members of the rehabilitation and support team.
Social psychiatry in municipalities (communes)
The 1995 reforms in psychiatry were aimed at improving the life situation of people with mental disorders and at increasing their opportunities for communication and involvement in society. The municipal district has the primary responsibility for making change happen by planning, coordinating and implementing the activities that people with mental disabilities need to achieve a decent and independent life in society.
The municipalities are responsible for providing people with mental disorders and receiving treatment with support in daily life, as well as in providing them with employment or work rehabilitation. More than 100 occupational therapists work at this level, often as leaders of this activity.
Social psychiatric care aims to include patients/clients in daily activities, which can take place, for example, in activity centers or meeting rooms with various activities in the social aspect. In addition to psychosocial rehabilitation, classes on adaptation to work are held in worker cooperatives, work centers, etc. This activity is aimed at increasing the social integration of people with mental disorders and their involvement in society. Improved daily living and participation in patient/client activities can improve their health and well-being.
This activity is aimed at increasing the social integration of people with mental disorders and their involvement in society. Improved daily living and participation in patient/client activities can improve their health and well-being.
One of the most important tasks of occupational therapy and a condition for the rehabilitation process is the formation of a supportive, tolerant, empathic and structured environment. In this way, the ergotherapist creates a platform from which the patient/client can develop, gain new knowledge, skills and increase confidence in themselves and in changing their own lives from a positive point of view. This requires the cooperation of all involved in rehabilitation. An ergotherapist in social and psychiatric activities has several roles - an expert, a leader, a role model; he cooperates with all those involved in this work, with the psychiatric service and with other partners in the community.
Explanation of concepts
There are many professional terms in occupational therapy that can be difficult to understand for those who are not associated with this profession. For ease of reading, here are some basic concepts used in occupational therapy and psychiatry. The following section provides examples of occupational therapy tools used in assessment.
For ease of reading, here are some basic concepts used in occupational therapy and psychiatry. The following section provides examples of occupational therapy tools used in assessment.
Performance appraisal
Evaluation of factors relevant to performance capacity, including resources that are lacking; for example, desires, habits, skills, as well as environmental factors.
Activity groups and other occupational therapy groups
Schematic description:
Individual and result oriented. High degree of external structure.
- Task focus; for example, aimed at training a special skill or a special result.
- Focus on social interaction through joint activities.
- Focus on interaction and communication; social skills and creativity training.
- Focus on joint evaluation of experiences and expression of feelings, for example, with the help of an image.
- Focus on the actual group process.
Group orientation and progress.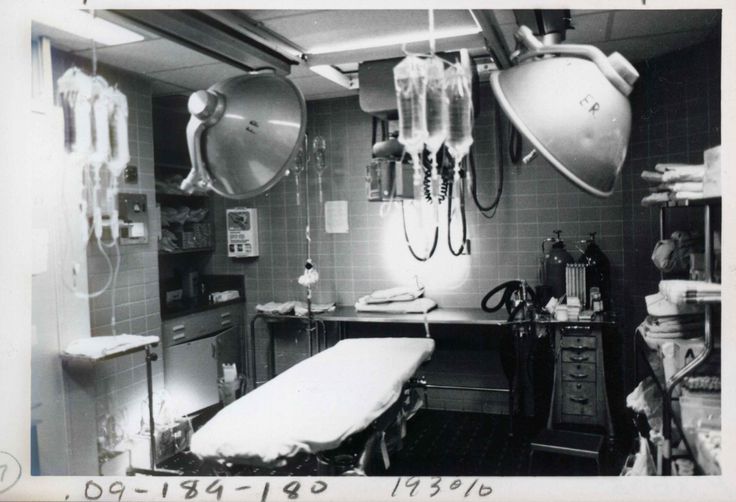 Low degree of external structure.
Low degree of external structure.
Accommodation
Activities or strategies to make the activity as effective as possible, such as different strategies in performing the activity, adjustment of the structure, complexity of the environment and work tasks, degree of intimacy in relationships, cognitive aids and support functions. Adaptation is made during assessment, treatment and directly during daily activities.
Skills
Ability to plan and carry out activities, such as process skills and social skills.
Staging/Initiating
Staging is the strategy used by the occupational therapist when taking the initiative to carry out the rehabilitation process when the patient/client is unable to do so on their own, for example due to fear/fear of change.
Mentally disabled people
Mentally impaired people are patients/clients who, due to mental disorders, have a reduced level of functioning. They may experience difficulties in daily life and therefore require care and/or support, or they may need adjustments to their work situation or long-term work rehabilitation.
Psychosocial rehabilitation
Can be defined as a process that makes it easier for an individual with a mental disorder to achieve an optimal level of functioning in society. Psychosocial rehabilitation aims to develop skills and knowledge through individually tailored support within a democratic, tolerant and stimulating learning environment.
Social worker cooperatives
Social worker cooperatives (hereinafter simply worker cooperative or cooperative) are workplaces where psychosocial rehabilitation and job training/training takes place. Cooperatives are seen as lighter jobs. The goal of psychosocial rehabilitation is to develop the skills and knowledge that are important for the performance of work tasks and social activities in and outside the cooperative itself. Cooperatives have a variety of activities such as handicrafts, service industries, cafeterias, assembly and stacking/packing work. Stress prevention occurs through collective planning, which takes into account the aspect of time; work time and speed are determined for certain patients/clients in order to reduce stress. Varying between two or more work tasks is used to break the monotony of work and mobilize patient/client resources.
Varying between two or more work tasks is used to break the monotony of work and mobilize patient/client resources.
Accuracy in time
Accuracy is an intervention that is adjusted to the rhythm of the patient/client. The ergotherapist waits and analyzes when the client is ready for the next step, that is, when there are better prerequisites/conditions for continuing the rehabilitation process.
Validation
A method by which an occupational therapist helps a client to understand his or her experiences, feelings, thoughts, and behaviors in a nonjudgmental way. This occurs, for example, when showing interest in the patient, acknowledging personal feelings, and also experiencing difficulties and encouraging success. Reasonableness can be the starting point for working on change, that is, it means that the behavior being assessed was not effective in relation to the goal.
Turning point
The concept of turning point or turning point can be related to development, for example, when the patient/client manages to cope with what was difficult for him. A positive turn or turning point may be associated with a change in roles, attitudes, or self-belief in performing an activity.
A positive turn or turning point may be associated with a change in roles, attitudes, or self-belief in performing an activity.
Occupational Therapy Evaluation Tools
Before recommending an adequate intervention to a patient/client, an assessment of the individual's ability to perform daily activities must be made. For this purpose, the occupational therapist uses formalized standardized tools as a complement to informal, situational methods. Such methods include observation of individual abilities in the performance of various activities, interviews in order to identify personal understanding of one's capabilities and / or the use of various self-assessment tools. The assessment may be done in a clinic, at home, at work, or elsewhere.
Examples of tools currently used in psychiatry
- AMPS (Assessment of Motor and Process Skills). Assessment of motor and process skills. With the help of observation, individual skills and abilities are evaluated when performing various activities.

- ACIS (Assessment of Communication and Interactions Skills). Assessment of communication and interaction skills. Through observation, this tool evaluates communication skills.
- OCAIRS (Occupational Circumstance Assessment Interview and Rating Scale). Interview and work environment scale. Through a semi-structured interview, an assessment is made of the work situation and participation in daily life.
- Min Mening (OSA - Occupational Self Assessment). My opinion (Self-assessment of activity). Through self-assessment, the patient/client gains their own understanding of their ability to work and the influence of their environment.
- SORM (Canadian Occupational Performance Measure). Canadian Performance Assessment. The tool measures a patient's/client's own understanding of their abilities and helps organize a treatment plan based on that.
- PRPP (Perceive, Recall, Plan, Reform). Cognition, Remembrance, Planning, Reformation. The tool gives a structured assessment of cognitive aspects in the performance of activities.
 - WRI (Worker Role Interview) and DOA (Dialog om akivitetsfbrmaga-arbete). Two tools that provide insight into the patient/client's work situation. The WRI (Work Role Interview) is based on a semi-structured interview, while the DOA (Application-Work Ability Dialogue) determines personal involvement in work through self-assessment.
- WRI (Worker Role Interview) and DOA (Dialog om akivitetsfbrmaga-arbete). Two tools that provide insight into the patient/client's work situation. The WRI (Work Role Interview) is based on a semi-structured interview, while the DOA (Application-Work Ability Dialogue) determines personal involvement in work through self-assessment.
Adults
Adults
Referrals for the adult department of the Almadea Clinic.
| ultrasound ECG | Intramuscular/periarticular/intravenous administration of drugs Botulinum therapy
| Physician call Rehabilitation after COVID-19 PCR tests |
Name Telephone
By submitting the form, I agree with personal data processing policy.
Write to us
Name Telephone Email address mail Message Attach Document Maximum number of uploaded files: 5 Maximum size of one file: 5 Mb Maximum total size of all uploaded files: fifteen Mb The following file formats are accepted:
jpg,png,pdf, doc, docx, jpeg, xlsx
By submitting the form, I agree with personal data processing policy.
Online booking
Name Telephone Email address mail Specify the specialist/service, convenient date and time of appointmentOur medical coordinator will contact you shortly Comment
Attach Document Maximum number of uploaded files: 5 Maximum size of one file: 5 Mb Maximum total size of all uploaded files: fifteen Mb The following file formats are accepted:
jpg,png,pdf, doc, docx, jpeg, xlsx
By submitting the form, I agree with personal data processing policy.