Process of bereavement
SAMHSA’s National Helpline | SAMHSA
Your browser is not supported
Switch to Chrome, Edge, Firefox or Safari
Main page content
-
SAMHSA’s National Helpline is a free, confidential, 24/7, 365-day-a-year treatment referral and information service (in English and Spanish) for individuals and families facing mental and/or substance use disorders.
Also visit the online treatment locator.
SAMHSA’s National Helpline, 1-800-662-HELP (4357) (also known as the Treatment Referral Routing Service), or TTY: 1-800-487-4889 is a confidential, free, 24-hour-a-day, 365-day-a-year, information service, in English and Spanish, for individuals and family members facing mental and/or substance use disorders.
This service provides referrals to local treatment facilities, support groups, and community-based organizations.
Also visit the online treatment locator, or send your zip code via text message: 435748 (HELP4U) to find help near you. Read more about the HELP4U text messaging service.
The service is open 24/7, 365 days a year.
English and Spanish are available if you select the option to speak with a national representative. Currently, the 435748 (HELP4U) text messaging service is only available in English.
In 2020, the Helpline received 833,598 calls. This is a 27 percent increase from 2019, when the Helpline received a total of 656,953 calls for the year.
The referral service is free of charge. If you have no insurance or are underinsured, we will refer you to your state office, which is responsible for state-funded treatment programs. In addition, we can often refer you to facilities that charge on a sliding fee scale or accept Medicare or Medicaid. If you have health insurance, you are encouraged to contact your insurer for a list of participating health care providers and facilities.
If you have health insurance, you are encouraged to contact your insurer for a list of participating health care providers and facilities.
The service is confidential. We will not ask you for any personal information. We may ask for your zip code or other pertinent geographic information in order to track calls being routed to other offices or to accurately identify the local resources appropriate to your needs.
No, we do not provide counseling. Trained information specialists answer calls, transfer callers to state services or other appropriate intake centers in their states, and connect them with local assistance and support.
-
Suggested Resources
What Is Substance Abuse Treatment? A Booklet for Families
Created for family members of people with alcohol abuse or drug abuse problems. Answers questions about substance abuse, its symptoms, different types of treatment, and recovery. Addresses concerns of children of parents with substance use/abuse problems.
Addresses concerns of children of parents with substance use/abuse problems.It's Not Your Fault (NACoA) (PDF | 12 KB)
Assures teens with parents who abuse alcohol or drugs that, "It's not your fault!" and that they are not alone. Encourages teens to seek emotional support from other adults, school counselors, and youth support groups such as Alateen, and provides a resource list.After an Attempt: A Guide for Taking Care of Your Family Member After Treatment in the Emergency Department
Aids family members in coping with the aftermath of a relative's suicide attempt. Describes the emergency department treatment process, lists questions to ask about follow-up treatment, and describes how to reduce risk and ensure safety at home.Family Therapy Can Help: For People in Recovery From Mental Illness or Addiction
Explores the role of family therapy in recovery from mental illness or substance abuse. Explains how family therapy sessions are run and who conducts them, describes a typical session, and provides information on its effectiveness in recovery.
For additional resources, please visit the SAMHSA Store.
Last Updated: 08/30/2022
SAMHSA Behavioral Health Treatment Services Locator
HomeWelcome to the Behavioral Health Treatment Services Locator, a confidential and anonymous source of information for persons seeking treatment facilities in the United States or U.S. Territories for substance use/addiction and/or mental health problems.
PLEASE NOTE: Your personal information and the search criteria you enter into the Locator is secure and anonymous. SAMHSA does not collect or maintain any information you provide.
Please enter a valid location.
please type your address
-
FindTreatment.
 gov
gov Millions of Americans have a substance use disorder. Find a treatment facility near you.
-
988 Suicide & Crisis Lifeline
Call or text 988
Free and confidential support for people in distress, 24/7.
-
National Helpline
1-800-662-HELP (4357)
Treatment referral and information, 24/7.

-
Disaster Distress Helpline
1-800-985-5990
Immediate crisis counseling related to disasters, 24/7.
- Overview
- Locator OverviewLocator Overview
- Locator OverviewLocator Overview
- Finding Treatment
- Find Facilities for VeteransFind Facilities for Veterans
- Find Facilities for VeteransFind Facilities for Veterans
- Facility Directors
- Register a New FacilityRegister a New Facility
- Register a New FacilityRegister a New Facility
- Other Locator Functionalities
- Download Search ResultsDownload Search Results
- Use Google MapsUse Google Maps
- Print Search ResultsPrint Search Results
- Use Google MapsUse Google Maps
- Icon from Find practitioners and treatment programs providing buprenorphine for opioid addiction (heroin or pain relievers).
 Find practitioners and treatment programs providing buprenorphine for opioid addiction (heroin or pain relievers).
Find practitioners and treatment programs providing buprenorphine for opioid addiction (heroin or pain relievers). - Icon from Find practitioners and treatment programs providing buprenorphine for opioid addiction (heroin or pain relievers). Find programs providing methadone for the treatment of opioid addiction (heroin or pain relievers).
The Locator is authorized by the 21st Century Cures Act (Public Law 114-255, Section 9006; 42 U.S.C. 290bb-36d). SAMHSA endeavors to keep the Locator current. All information in the Locator is updated annually from facility responses to SAMHSA’s National Substance Use and Mental Health Services Survey (N-SUMHSS). New facilities that have completed an abbreviated survey and met all the qualifications are added monthly. Updates to facility names, addresses, telephone numbers, and services are made weekly for facilities informing SAMHSA of changes. Facilities may request additions or changes to their information by sending an e-mail to [email protected], by calling the BHSIS Project Office at 1-833-888-1553 (Mon-Fri 8-6 ET), or by electronic form submission using the Locator online application form (intended for additions of new facilities).
Updates to facility names, addresses, telephone numbers, and services are made weekly for facilities informing SAMHSA of changes. Facilities may request additions or changes to their information by sending an e-mail to [email protected], by calling the BHSIS Project Office at 1-833-888-1553 (Mon-Fri 8-6 ET), or by electronic form submission using the Locator online application form (intended for additions of new facilities).
Experience of bereavement — Such cases
For the first time in Russia, the book Fundamentals of Palliative Care, edited by Robert Twycross and Andrew Wilcock, is published — the first fundamental manual on palliative care in Russian, prepared for publication by the Vera Hospice Foundation. "Things Like This" publishes a chapter from this book
Fundamentals of Palliative Care is a comprehensive guide covering all aspects of care for terminally ill people. This manual has been used by European specialists for more than 20 years, and now it is available to Russian-speaking medical students, doctors, and nurses. The book Introducing Palliative Care was first published in 1995 and after it was repeatedly reprinted in different languages of the world. The fifth edition of the book was translated into Russian in the 2016 edition.
The book Introducing Palliative Care was first published in 1995 and after it was repeatedly reprinted in different languages of the world. The fifth edition of the book was translated into Russian in the 2016 edition.
Dr. Robert Twycross is one of the pioneers of the hospice movement in the world. He taught a course in palliative medicine at Oxford and directed the WHO Collaborating Center for Palliative Care for 17 years. In Fundamentals of Palliative Care, Twycross has put together a detailed and comprehensive guide to managing palliative patients: treating painful symptoms associated with their illnesses, as well as communicating with relatives and loved ones. nine0003
Andrew Wilcock is Fellow of the Royal College of Physicians and Fellow in Palliative Medicine and Oncology with the Macmillan Service at the University of Nottingham in the UK. Editor and one of the creators of the International Palliative Care Formulary, scientific consultant on prescribing drugs in palliative care of the British National Formulary.
Bereavement
The experience of loss is one of the most severe crises in life, which affects the health of a significant number of people. Bereavement support is one of the main elements of palliative care. It includes both caring for the patient's body after his death, and helping relatives and friends of the deceased. If the death of a person is expected, some of his relatives may experience "anticipatory (anticipatory) grief", in which case help in experiencing the loss can begin to be provided even before death. nine0003
The period of bereavement is the time of experiencing the death of a loved one, and grief is a reaction to longing and anguish that occurs after death. Grief is a transitional process during which people adjust to the reality of loss and learn to live without a deceased loved one. Grief is not just an emotional experience; it highlights behavioral, cognitive, physical, social and spiritual aspects. Thus, grief requires a holistic approach.
The experience of loss is associated with increased mortality, in particular from cardiovascular diseases, in the first months after the loss of a loved one.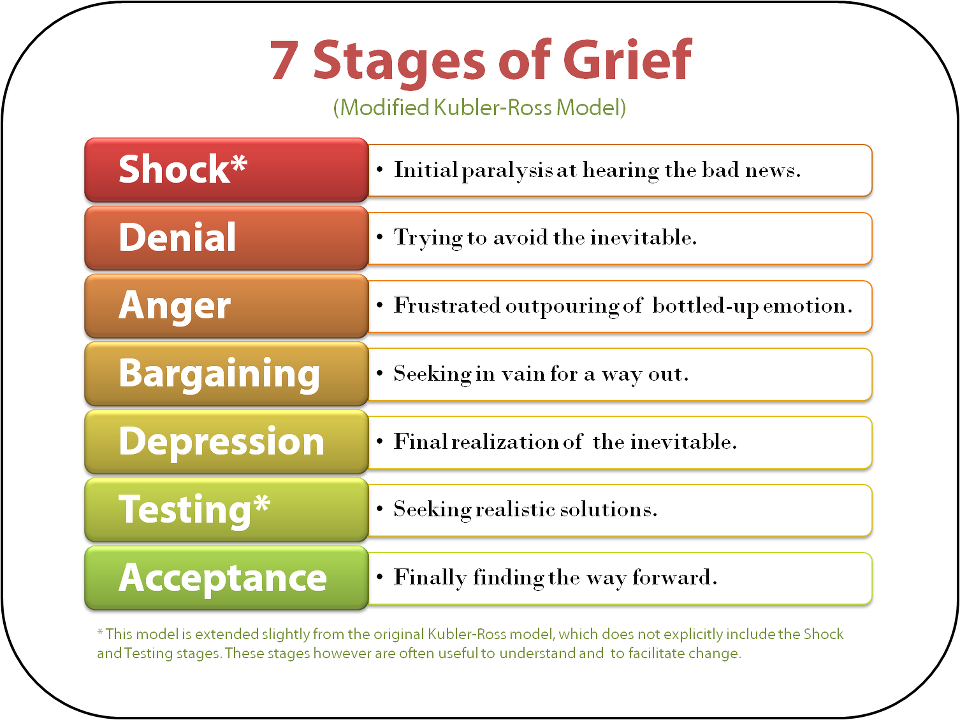 There is an increase in the frequency of somatic and mental illness, infections and alcohol abuse, as well as seeking medical help and psychotropic drugs. nine0003
There is an increase in the frequency of somatic and mental illness, infections and alcohol abuse, as well as seeking medical help and psychotropic drugs. nine0003
Patterns of grief
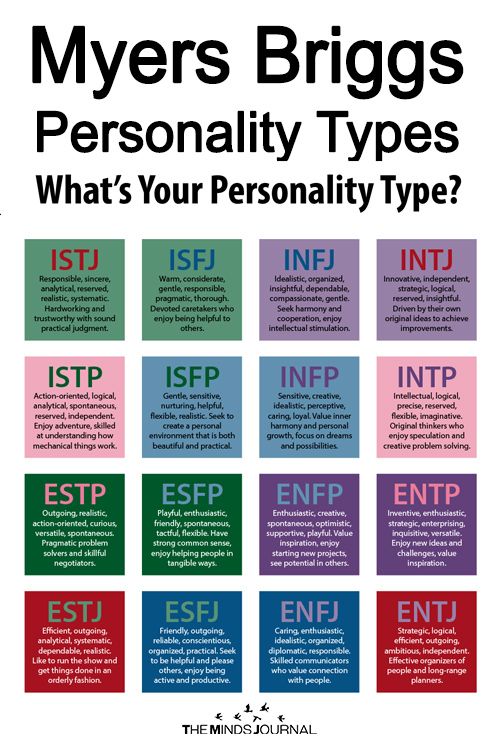
Grief is a deeply personal experience that people experience in different ways. Nevertheless, several typical stages can be distinguished, and on their basis, a number of models of grief experience.
They can be used to support those who are grieving, but the model is always a simplification and should therefore be used with caution. The sequential passage through the stages of experiencing grief is not typical. Usually people vacillate between different stages of such a path, which can lead to confusion both for themselves and those around them. nine0003
Grief is not a stable process. A person goes through a certain stage of this process, but then returns to it again. And so in a circle. All repeats.
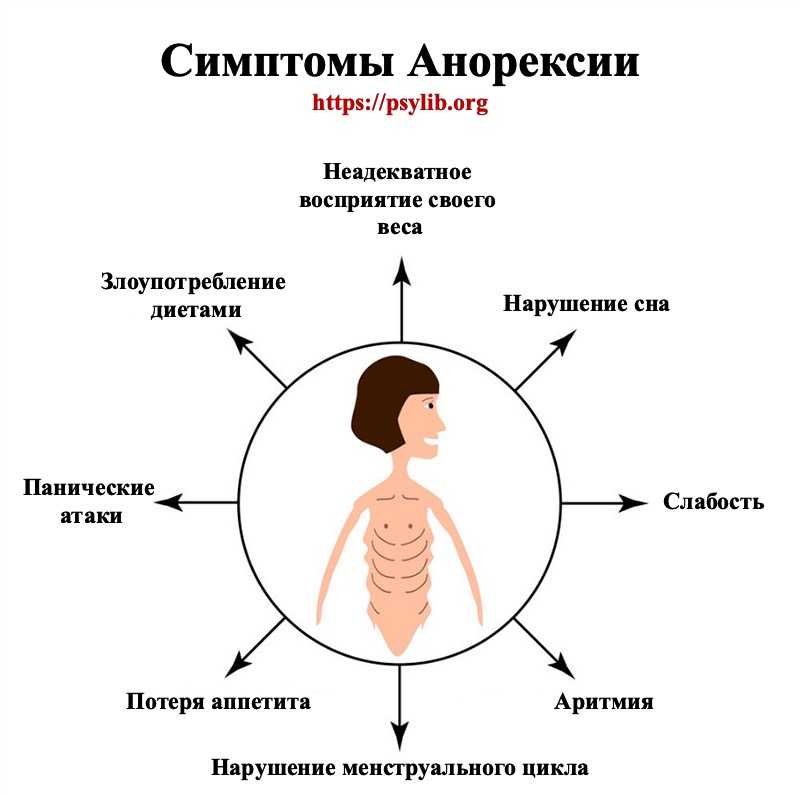
Common reactions to bereavement:
Emotions
Anxiety; anger; anxiety; depression; guilt; feeling of loneliness; sense of relief
attitude
Despair; low self-esteem; self-criticism; a feeling of unreality of what is happening; social isolation; suspicion; longing for the deceased
Behavior
Alcohol abuse; increased fatigue; tearfulness
Physiological changes
Dry mouth; hair loss; headaches; indigestion; insomnia; loss of appetite, weight loss; muscle pain; heart palpitations; dyspnea; stress-induced disease, infection; the use of psychoactive substances; visual impairment
Therefore, one should not make hasty judgments about the stage of grief that a bereaved person is or should be in. Personal characteristics are of great importance. For people who rely primarily on their feelings, the experience of grief tends to be more in line with traditional patterns, while for people who tend to make sense of what is happening first, it becomes more of a cognitive process. To cope with a situation, such people search for information, think about problems, take action, and look for ways to distract themselves - this model is not necessarily associated with difficulties. In addition, the manifestation and expression of grief is culturally determined. In the UK and the US, self-confidence and independence are highly valued, which forces grieving people, especially if they are male, to suppress their emotions and not show that they are suffering. nine0003
Personal characteristics are of great importance. For people who rely primarily on their feelings, the experience of grief tends to be more in line with traditional patterns, while for people who tend to make sense of what is happening first, it becomes more of a cognitive process. To cope with a situation, such people search for information, think about problems, take action, and look for ways to distract themselves - this model is not necessarily associated with difficulties. In addition, the manifestation and expression of grief is culturally determined. In the UK and the US, self-confidence and independence are highly valued, which forces grieving people, especially if they are male, to suppress their emotions and not show that they are suffering. nine0003
The traditional model
The traditional model states that the process of grief consists of certain stages, but in reality one stage can occur simultaneously with another and unexpected changes are possible.
Numbness
The first reaction is shock and distrust, accompanied by a feeling of the unreality of what is happening and the mechanicalness of life (existence "on autopilot"). Somatic symptoms may or may not be present.
Somatic symptoms may or may not be present.
Separation and pain
Stupefaction gradually gives way to intermittent intense melancholy, anxiety, tension, anger and self-criticism. There is an irresistible desire to return the deceased. This can manifest itself in dreams and in the fact that a person hears the deceased and feels his presence, or excessively indulges in memories. There may also be an obsession to re-analyze the circumstances of the death. Somatic symptoms are common.
Despair
This stage occurs when the realization comes that the deceased person will not return. There are signs such as poor concentration, apathy, social withdrawal, lack of purpose, and deep sadness.
Acceptance
Despair gradually gives way to acceptance of the loss. Acceptance of the irreparable situation first occurs at the intellectual level, and later at the level of feelings. Sadness and emotional shifts can last for more than a year.
Decoupling and reorganization
Eventually, the grieving person begins to adapt to life without a deceased loved one: he rebuilds his personality and redefines goals, acquires new skills and assumes new roles. Gradually, lighter feelings appear, energy returns, new hobbies arise and relationships are born. At the memory of a departed loved one, emotions are no longer overwhelmed, however, anniversaries and memorable days cause a temporary aggravation of grief. nine0003
The normal course of life is interrupted by loss, which primarily causes shock, as well as numbness and denial. What follows is protest, accompanied by anger and guilt, followed by disorganization, as well as sadness, a feeling of loneliness and emptiness. And finally, a reorganization takes place, thanks to which a person can return to the original level of functioning, often changing his attitude to life and acquiring new values.
Bilateral process model
This model illustrates that the bereaved person oscillates between two extremes: bereavement activities (e. g., thinking about the deceased, yearning for them, reminiscing, expressing their feelings) and recovery activities, in which a person is looking for a way to distract himself in order to cope with everyday life (for example, suppresses memories, controls emotions, finds a business for himself).
g., thinking about the deceased, yearning for them, reminiscing, expressing their feelings) and recovery activities, in which a person is looking for a way to distract himself in order to cope with everyday life (for example, suppresses memories, controls emotions, finds a business for himself).
Orientation towards restoration allows a person to adapt and acquire a new self-identity, but since in everyday life there are many reminders of loss, he rushes between two types of behavior. The predominant behavior and degree of fluctuation of each individual will depend on personality factors, gender and cultural background. Over time, a person usually shifts from bereavement behavior to recovery behavior. nine0003
This model helps to understand why one day a person can look great and the next day he is grieving. Difficulties arise when a person tends to experience loss exclusively (chronic grief) or only to recovery behavior (absent grief).
Grieving parents may choose different types of bereavement experiences: one will be primarily bereavement-oriented, and the other will be recovery-oriented. This leads to tension between them as they cannot understand how each of them deals with grief. nine0003
This leads to tension between them as they cannot understand how each of them deals with grief. nine0003
Assistance in dealing with bereavement
The basis of support during bereavement is general quality assistance during the life of the patient, well-established communication and trusting relationships built with the family. The promptly carried out procedure for ascertaining and registering death, the removal of equipment and medicines from the house, and the willingness to answer questions help to alleviate the pain of loss in many ways.
Some of the health professionals who can provide bereavement care are general practitioners, community nurses, community palliative care nurses, and various bereavement support organizations. nine0003
There are special support groups for survivors of trauma or suicide of a loved one, stillbirth or death of a child, and support groups for bereaved children. After the death of a patient who was under the care of a hospice, for relatives of a patient with an increased risk of complicated grief, assistance in experiencing loss is officially provided.
For most people, it is enough to give them the opportunity to express their grief and support them by offering to talk about their feelings and listening carefully. This is of great therapeutic value and belongs to the mandatory skills of every medical worker. By far the most beneficial influence on bereavement outcomes is family and friends, who provide the necessary support and allow the person to express grief and speak freely about their experiences for as long as they need it. nine0003
The main task is to help a person find strength in himself and find his own ways to overcome it. Because some people are reluctant to ask for help, it's important to ask how they are coping with the situation. Often they need someone to confirm that their experience of grief is normal.
Bereavement reactions are either immediate or delayed; both short-term and long-term; both moderate and strong. Most bereaved people go through this period with the support of family and friends, and a healthcare professional who is willing to listen to them. About 10% need the help of a volunteer bereavement team or support group, and about 5% have complicated (pathological) grief that requires the participation of a psychologist or psychiatrist. nine0003
About 10% need the help of a volunteer bereavement team or support group, and about 5% have complicated (pathological) grief that requires the participation of a psychologist or psychiatrist. nine0003
In addition, it is important to provide support not only to family members, but also to caregivers, especially if the death was traumatic. For most of them, it is enough to give them the opportunity to express their grief in an atmosphere of support.
Complicated grief
Complicated grief is grief that leads to long-term physical and mental health problems.
His risk factors are listed below:
• premature and sudden death; nine0126
• death too severe;
• highly dependent, conflicting or difficult relationship with the deceased;
• poor social support;
• inability to talk openly with anyone and prepare for
death;
• anger, if it makes it difficult to provide support and leads to social isolation;
;
• Life circumstances that take away time and opportunity to deal with loss, such as financial hardship, lack of employment, needy children or elderly relatives; nine0126
• loss of loved ones in the past;
• the presence of a somatic or mental illness;
• history of alcoholism, drug addiction or suicidal behavior .
Complicated grief usually takes the form of extremes of normal grief. Formal criteria for complicated grief remain controversial. In addition, the fifth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) no longer includes complicated grief as a psychiatric diagnosis, but it also no longer lists bereavement as an exclusion criterion. major depressive disorder. nine0003
Complicated grief requires the help of psychologists and psychiatrists. In particular, the following treatments are possible: guided mourning; interpersonal (interpersonal) psychotherapy, cognitive-behavioral psychotherapy and family-oriented grief therapy.
Short-term treatment with benzodiazepine hypnotics may help, but it is important to carefully monitor these prescriptions to prevent dependence.
For those who develop an apparent psychiatric disorder (eg depression, anxiety disorder, substance abuse, post-traumatic stress disorder, psychosis), treatment will be provided in accordance with standard psychiatric practice. nine0003
nine0003
the electronic version of the book can be read at pro-palliativ.ru
Even more important news and good texts from us and our colleagues - in the telegram channel "Takikh Del." Subscribe!
medicine palliative care psychological care
Sitemap - Surgut City Clinical Hospital
About the clinic  |