Ocd social anxiety
When Symptoms of OCD and Social Anxiety Overlap
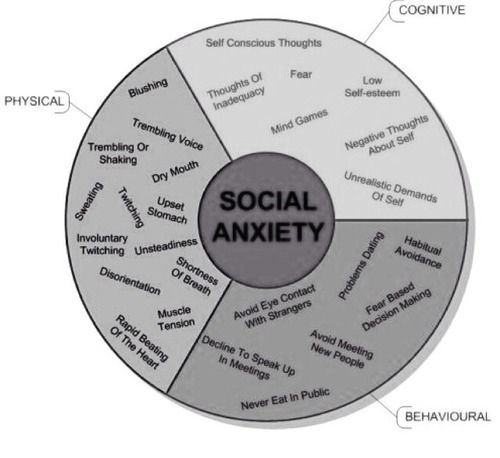
Social OCD refers to experiencing obsessions and compulsions around the fear of being rejected, judged, or humiliated by others. It may also refer to overlapping symptoms of OCD and social anxiety.
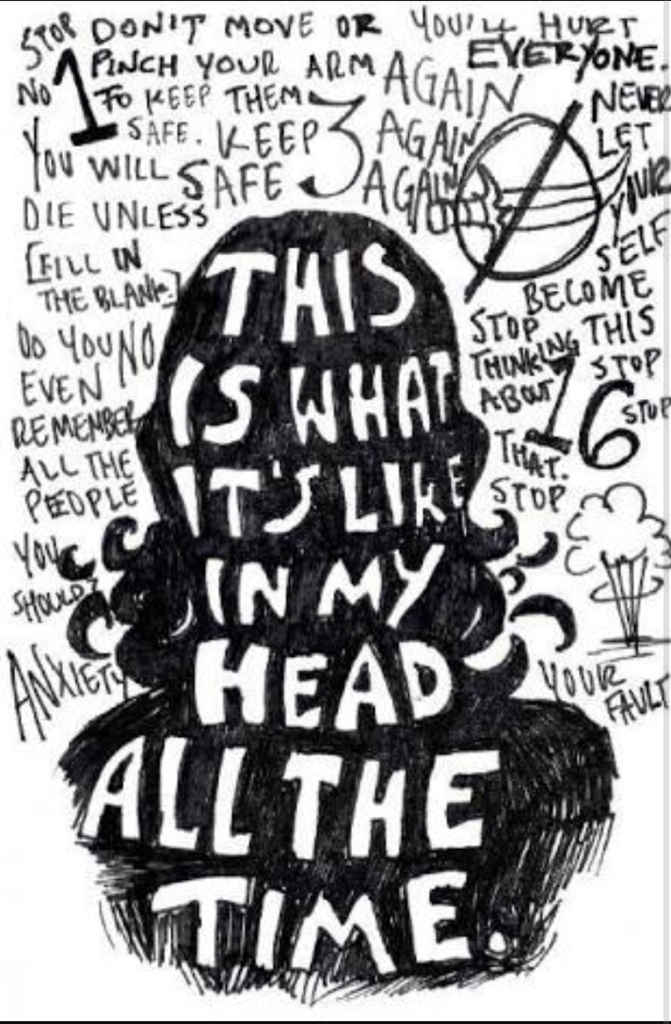
Obsessive-compulsive disorder (OCD) is a mental health condition characterized by two primary symptoms: persistent intrusive thoughts (obsessions) and repetitive behaviors or rituals (compulsions).
Social OCD isn’t an established clinical term or a formal diagnosis. It may refer to overlapping symptoms of OCD and social anxiety.
Social anxiety is one of many anxiety disorders characterized by fear or panic of social interactions and of being criticized and rejected socially.
For people with social OCD, obsessions may be about social interactions or social performance. When this is the case, you may experience uncontrollable thoughts and intrusive images about people making fun of you, rejecting you even without knowing you, or humiliating you.
When this fear of social humiliation and rejection is a persistent symptom and impacts your daily routine, a mental health professional may diagnose both OCD and social anxiety.
Both social anxiety disorder and obsessive-compulsive disorder are chronic conditions that may involve debilitating symptoms. They’re two separate diagnoses.
It’s possible for symptoms of OCD and social anxiety to occur together, though. This would mean that you live with two separate conditions. In fact, research suggests that social anxiety disorder is the most frequently co-occurring disorder for those with OCD.
But it’s also possible for someone with OCD to experience obsessions about social rejection for a period of time without receiving a social anxiety diagnosis.
To receive both diagnoses, you would need to meet the diagnostic criteria for both conditions. Diagnostic criteria are established by the Diagnostic and Statistical Manual of Mental Disorders, 5th edition, text revision (DSM-5-TR), a reference handbook used by most U. S. mental health professionals.
S. mental health professionals.
According to the DSM-5-TR, two main criteria must be met for you to receive an OCD diagnosis:
- You experience repetitive and persistent obsessions and compulsions.
- These obsessions and compulsions take considerable time from your daily routine (more than 1 hour per day) or they cause you significant distress that translates into impairment or inability to function.
According to the DSM-5-TR, the criteria to receive a social anxiety diagnosis are:
- Significant fear about social events where you may be exposed to other people’s judgment and criticism.
- Persistent fear that others may recognize social anxiety symptoms in you that may lead you to be humiliated or embarrassed in public. It may also be fear that you won’t know how to act and offend others.
- Consistent fear about the same social situations.

- Tendency to avoid social situations or experience impairing levels of fear when exposed to those.
- Your fear of these social interactions isn’t proportionate to the threat you face.
- These symptoms last for at least 6 months but typically more than that.
- Your fear of social situations impairs the way you function at work, school, and in relationships.
- These symptoms cannot be explained by an injury, disease, or substance use.
- These symptoms cannot be explained by any other anxiety disorder or mental health condition.
- If you live with any injury, disease, or condition, your fear is unrelated to those or impairing.
A person with both OCD and social anxiety may be more likely to experience obsessions with social themes. This may lead to symptoms commonly seen in people with “responsibility OCD,” also known as “social scrupulosity OCD.”
Responsibility OCD involves feeling an extreme fear of harming someone else’s feelings. For instance, you might worry excessively that you’ll say something in front of your friends that may remind them of a traumatic experience they lived. You experience intrusive images and thoughts about saying what you fear. This may lead you to repeatedly shrug your shoulders when you’re in front of your friends.
For instance, you might worry excessively that you’ll say something in front of your friends that may remind them of a traumatic experience they lived. You experience intrusive images and thoughts about saying what you fear. This may lead you to repeatedly shrug your shoulders when you’re in front of your friends.
Social scrupulosity is a theme in OCD and doesn’t mean you also live with social anxiety, unless you meet all the criteria for this condition.
OCD is not a social disorder nor is it a social disability.
Even though OCD symptoms can be debilitating and highly distressing, many people with the disorder can navigate different aspects of life, including employment, romantic relationships, and social interactions.
OCD doesn’t cause social anxiety disorder, and social anxiety doesn’t cause OCD. However, it’s possible that one may be a contributing factor to the other in some instances. In fact, they often co-occur.
In one study, social anxiety disorder was seen in about 20% of participants with OCD. Those with both OCD and social anxiety disorder were more likely to experience severe depression symptoms and insecure attachment styles.
Those with both OCD and social anxiety disorder were more likely to experience severe depression symptoms and insecure attachment styles.
Both OCD and social anxiety disorder can be managed with the support of a mental health professional.
Cognitive behavioral therapy (CBT) is one of the most effective treatments for both conditions.
CBT for the management of social anxiety disorder may include techniques like exposure therapy, which involves gradually exposing you to your social fears until your anxiety is reduced or gone.
CBT for the management of OCD typically involves exposure and response prevention (ERP) therapy. ERP also gradually exposes you to your fears while helping you not to engage in a compulsion to relieve the anxiety they cause you. In time, you learn that you don’t need to engage in compulsions to decrease anxiety.
In some cases, medication may also be used to treat OCD and social anxiety.
Social anxiety disorder and OCD are two separate mental health diagnoses.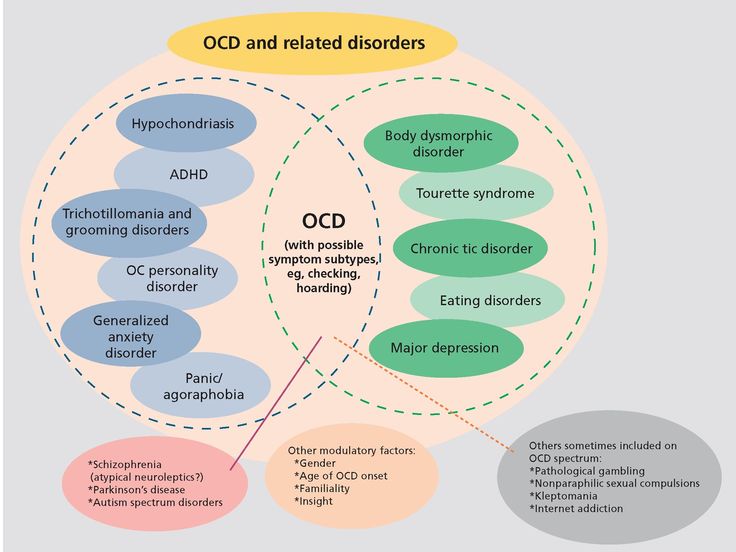 In some instances, someone can live with both conditions.
In some instances, someone can live with both conditions.
It’s also possible for someone with OCD to have obsessions around a fear of social interactions without meeting the criteria for social anxiety.
Only a mental health professional can provide an accurate diagnosis and a management plan for both conditions.
When Symptoms of OCD and Social Anxiety Overlap
Social OCD refers to experiencing obsessions and compulsions around the fear of being rejected, judged, or humiliated by others. It may also refer to overlapping symptoms of OCD and social anxiety.
Obsessive-compulsive disorder (OCD) is a mental health condition characterized by two primary symptoms: persistent intrusive thoughts (obsessions) and repetitive behaviors or rituals (compulsions).
Social OCD isn’t an established clinical term or a formal diagnosis. It may refer to overlapping symptoms of OCD and social anxiety.
Social anxiety is one of many anxiety disorders characterized by fear or panic of social interactions and of being criticized and rejected socially.
For people with social OCD, obsessions may be about social interactions or social performance. When this is the case, you may experience uncontrollable thoughts and intrusive images about people making fun of you, rejecting you even without knowing you, or humiliating you.
When this fear of social humiliation and rejection is a persistent symptom and impacts your daily routine, a mental health professional may diagnose both OCD and social anxiety.
Both social anxiety disorder and obsessive-compulsive disorder are chronic conditions that may involve debilitating symptoms. They’re two separate diagnoses.
It’s possible for symptoms of OCD and social anxiety to occur together, though. This would mean that you live with two separate conditions. In fact, research suggests that social anxiety disorder is the most frequently co-occurring disorder for those with OCD.
But it’s also possible for someone with OCD to experience obsessions about social rejection for a period of time without receiving a social anxiety diagnosis.
To receive both diagnoses, you would need to meet the diagnostic criteria for both conditions. Diagnostic criteria are established by the Diagnostic and Statistical Manual of Mental Disorders, 5th edition, text revision (DSM-5-TR), a reference handbook used by most U.S. mental health professionals.
Diagnostic criteria for OCDAccording to the DSM-5-TR, two main criteria must be met for you to receive an OCD diagnosis:
- You experience repetitive and persistent obsessions and compulsions.
- These obsessions and compulsions take considerable time from your daily routine (more than 1 hour per day) or they cause you significant distress that translates into impairment or inability to function.
According to the DSM-5-TR, the criteria to receive a social anxiety diagnosis are:
- Significant fear about social events where you may be exposed to other people’s judgment and criticism.
- Persistent fear that others may recognize social anxiety symptoms in you that may lead you to be humiliated or embarrassed in public. It may also be fear that you won’t know how to act and offend others.
- Consistent fear about the same social situations.
- Tendency to avoid social situations or experience impairing levels of fear when exposed to those.
- Your fear of these social interactions isn’t proportionate to the threat you face.
- These symptoms last for at least 6 months but typically more than that.
- Your fear of social situations impairs the way you function at work, school, and in relationships.
- These symptoms cannot be explained by an injury, disease, or substance use.
- These symptoms cannot be explained by any other anxiety disorder or mental health condition.
- If you live with any injury, disease, or condition, your fear is unrelated to those or impairing.
A person with both OCD and social anxiety may be more likely to experience obsessions with social themes.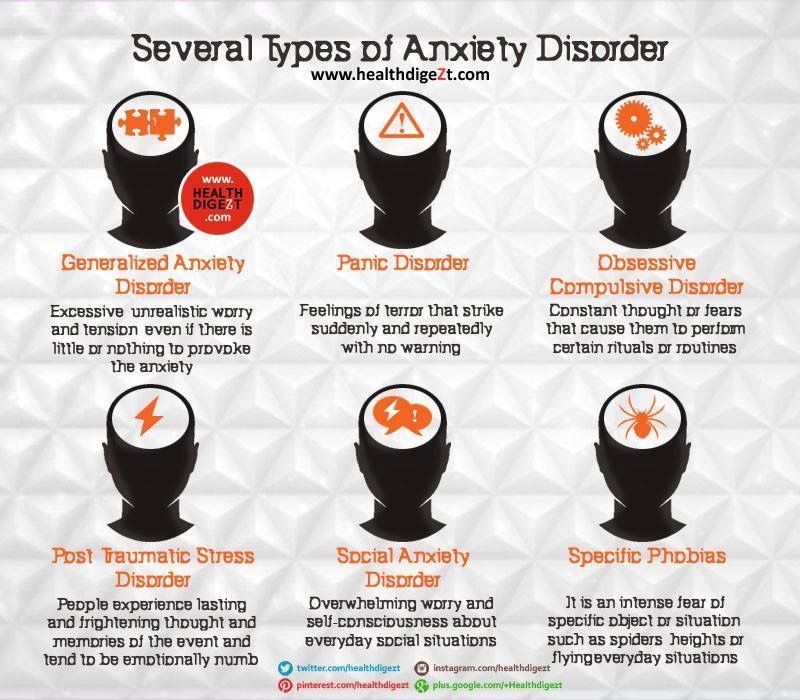 This may lead to symptoms commonly seen in people with “responsibility OCD,” also known as “social scrupulosity OCD.”
This may lead to symptoms commonly seen in people with “responsibility OCD,” also known as “social scrupulosity OCD.”
Responsibility OCD involves feeling an extreme fear of harming someone else’s feelings. For instance, you might worry excessively that you’ll say something in front of your friends that may remind them of a traumatic experience they lived. You experience intrusive images and thoughts about saying what you fear. This may lead you to repeatedly shrug your shoulders when you’re in front of your friends.
Social scrupulosity is a theme in OCD and doesn’t mean you also live with social anxiety, unless you meet all the criteria for this condition.
OCD is not a social disorder nor is it a social disability.
Even though OCD symptoms can be debilitating and highly distressing, many people with the disorder can navigate different aspects of life, including employment, romantic relationships, and social interactions.
OCD doesn’t cause social anxiety disorder, and social anxiety doesn’t cause OCD.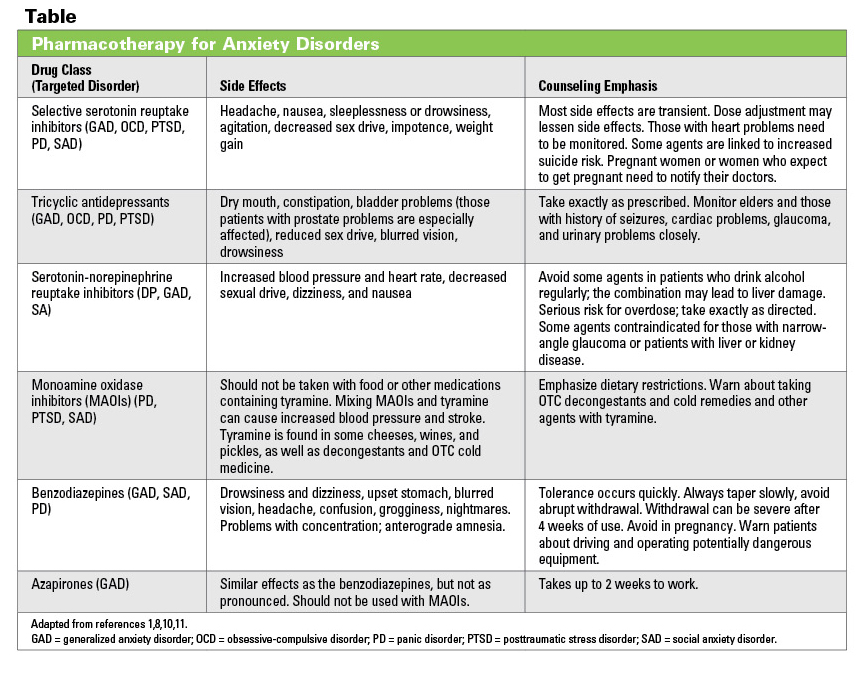 However, it’s possible that one may be a contributing factor to the other in some instances. In fact, they often co-occur.
However, it’s possible that one may be a contributing factor to the other in some instances. In fact, they often co-occur.
In one study, social anxiety disorder was seen in about 20% of participants with OCD. Those with both OCD and social anxiety disorder were more likely to experience severe depression symptoms and insecure attachment styles.
Both OCD and social anxiety disorder can be managed with the support of a mental health professional.
Cognitive behavioral therapy (CBT) is one of the most effective treatments for both conditions.
CBT for the management of social anxiety disorder may include techniques like exposure therapy, which involves gradually exposing you to your social fears until your anxiety is reduced or gone.
CBT for the management of OCD typically involves exposure and response prevention (ERP) therapy. ERP also gradually exposes you to your fears while helping you not to engage in a compulsion to relieve the anxiety they cause you. In time, you learn that you don’t need to engage in compulsions to decrease anxiety.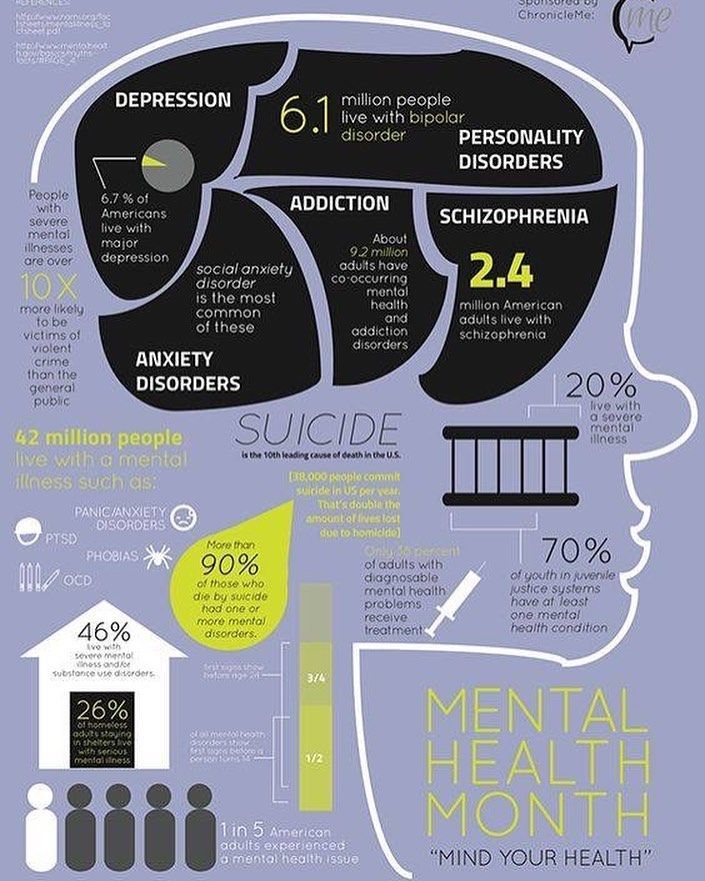
In some cases, medication may also be used to treat OCD and social anxiety.
Social anxiety disorder and OCD are two separate mental health diagnoses. In some instances, someone can live with both conditions.
It’s also possible for someone with OCD to have obsessions around a fear of social interactions without meeting the criteria for social anxiety.
Only a mental health professional can provide an accurate diagnosis and a management plan for both conditions.
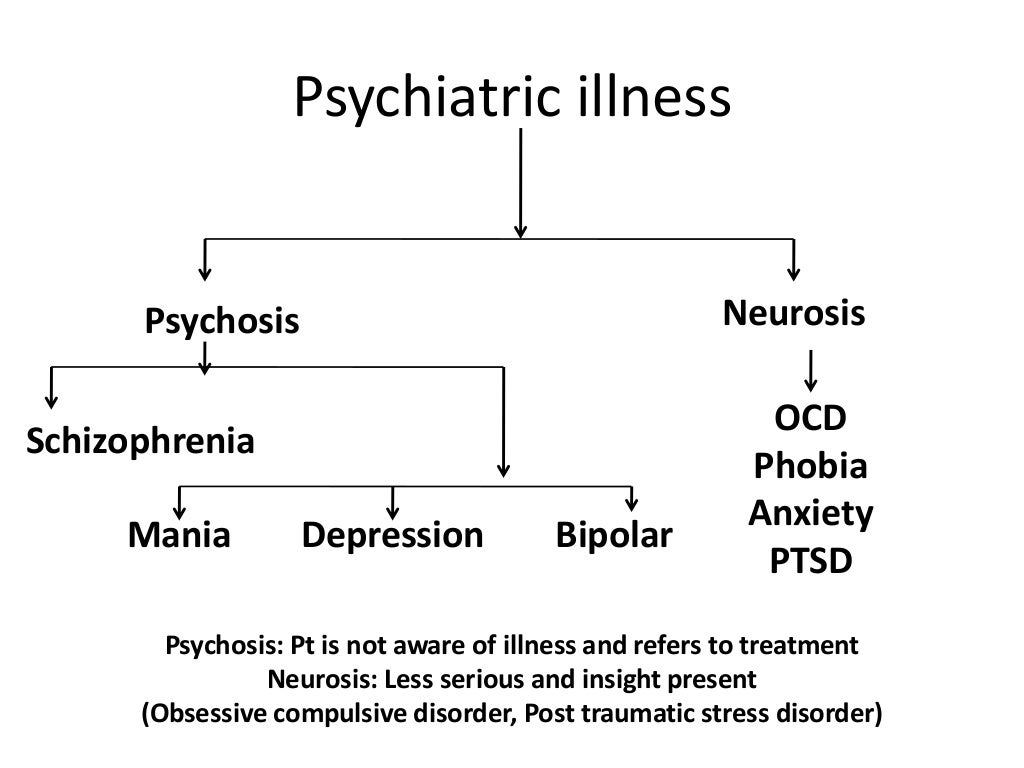
Obsessive Compulsive Disorder (OCD): what it is, symptoms, treatment, advice from a doctor Some people develop symptoms during adolescence, although they are usually diagnosed in adults. Obsessive-compulsive disorder can significantly interfere with a fulfilling life, but treatment can help keep it under control.
Let's figure out together with experts what are the causes of OCD, what therapeutic and drug methods are used by doctors, and how to behave relatives of a person who has been diagnosed with this disorder.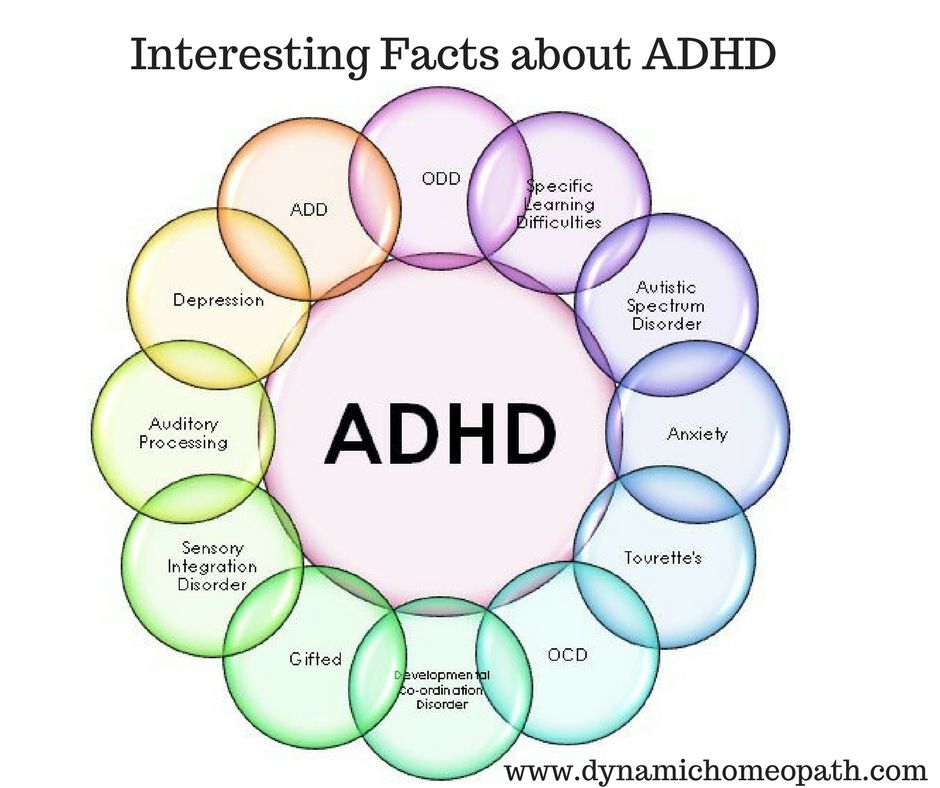 nine0003
nine0003
Contents
- What it is
- Signs and symptoms
- Causes
- Diagnosis
- How to treat
- Advice for relatives 902 support groups
- obsessions - persistent thoughts or impulses, intrusive and unacceptable, causing anxiety;
- compulsions are rituals that are built into the thoughts of a person, he considers it necessary to perform them in response to an obsession. nine0016
- present daily;
- are uncontrollable;
- are not enjoyable;
- affect work and social life.
- Checks if the door is locked, if the iron and oven are switched off.
- Unreasonably suspects undiagnosed health conditions such as pregnancy or schizophrenia.
- Afraid of germs, things that can be dirty, constantly cleaning.
- Strives for excessive symmetry and order, feels the need to arrange things in a certain way: by size, colors or alphabet.
- Cannot drive obsessive thoughts and ideas away from himself. Some of them can be violent or disturbing. nine0016
- Genetics. If you have OCD in your next of kin—father, mother, brother, and sister—the chances are high that you have it too.
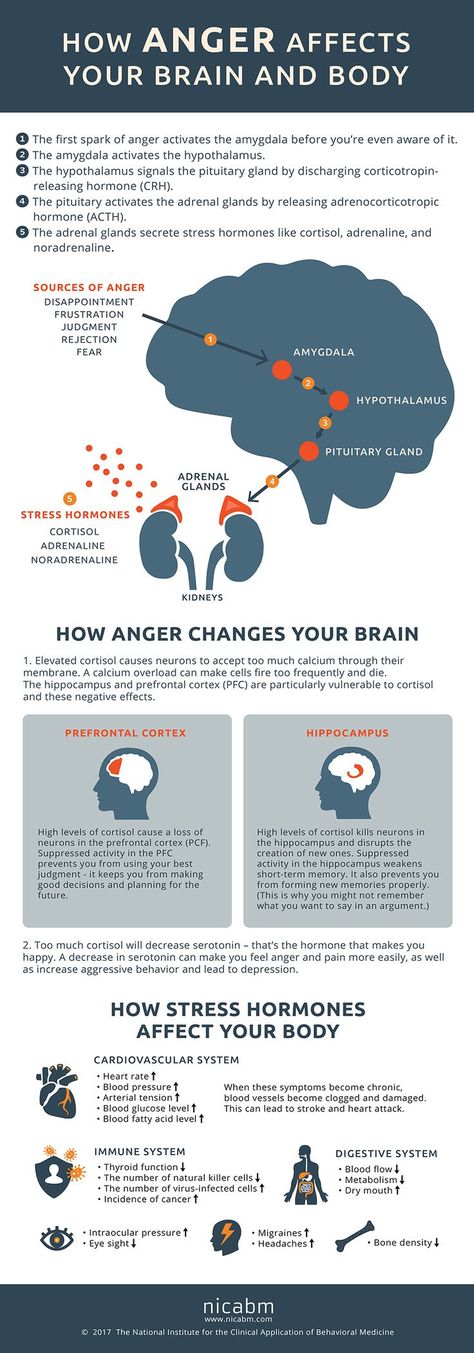
- Structure and function of the brain. In the brain of OCD sufferers, increased activity is recorded in the region of the cortico-striatal-thalamo-cortical loop [5].
- Environment. High levels of stress, increased anxiety can also be a trigger for the development of obsessive-compulsive disorder.
- Concomitant diseases. OCD is often diagnosed in parallel with eating disorders and depression [6]. nine0016
- Traumatic events. The disorder can be the result of difficult circumstances experienced: psychological and sexual abuse, physical trauma, loss of loved ones.
- Infections. Occasionally, OCD is found in children who have had a streptococcal infection. This is called pediatric autoimmune neuropsychiatric disorders.
- Do you have obsessive thoughts about possible tragic events, death, serious illnesses, fires, accidents?
- Are you concerned about the possibility of contamination with germs and chemicals?
- Do you unnecessarily re-read emails or text messages before or after sending them?
- Are you obsessed with keeping everything in order (cataloging books, perfect stacks of clothes in your closet, sized pencils on your desk)? nine0016
- Do you repeat routine activities such as opening a door, putting on your shoes, or getting into bed over and over again until you feel like you've done it "right"?
- Do you have recurring inappropriate thoughts (often of a religious, violent, or sexual nature) that seem intrusive and out of control?
- Do you feel the need to constantly seek confirmation of what you have said or done?
- Do you follow ritualized washing, cleaning or personal grooming habits (eg washing your hands five times in a row)? nine0016
- Do you avoid certain colors or numbers because you consider them "unlucky"?
- Do you check your trash before throwing it away to make sure it's clean?
- Do you worry about doing something out of a senseless urge, like pushing a stranger or hitting a loved one?
- Do you check oven handles, door locks and car brakes over and over again in a short period of time? nine0016
- Anxiety and Depression Association of America (ADAA) - mental health resources, including conferences of the International OCD Foundation.
 There are online support groups for those with the disorder.
There are online support groups for those with the disorder. - OCD Peers - Virtual support groups (6-10 members) using a HIPAA compliant platform. Video conferences with group mentor, open discussions and agenda. All groups are paid.
- 7 cups - on the platform you can find a volunteer who will be in touch and ready to listen to the problem. This is not a qualified professional, but sometimes speaking out to an attentive listener is just as important as working through a problem with a licensed psychotherapist. nine0016
- Support Groups - A free resource with several hundred support groups on a variety of topics, including those for OCD sufferers. Groups are moderated to avoid bullying and inappropriate user reactions.
- HealthUnlocked - literally "health unlocked" - a resource with forums to support people with various diseases. The ROC topic is moderated not only by the portal administrators, but also by representatives of the International ROC Foundation.
- basal ganglia;
- frontal part;
- caudate nucleus;
- amygdala.
- high intelligence;
- adequate thinking; nine0016
- conscientiousness and anxiety;
- high sense of responsibility;
- pedantry;
- desire to be the best.
- intrusive thoughts;
- anxiety and various fears;
- the same rituals that a person performs daily.
- fear of catching an infection;
- causeless anxiety;
- maniacal desire for order and cleanliness; nine0016
- excessive superstition.
- Psychological. OCD occurs when a person develops aggression towards an object. It also includes stressful situations that provoke a violation. The state appears as an exit of emotions, as a marker of anxiety. nine0016
- Biological. The disorder is the result of a disease of the brain or nervous system. It can be provoked by various kinds of injuries, hormonal disorders or anatomical features.
- Genetic. The disease can be inherited.
- Sociological. They arise as a response of the body to external factors.
- Exogenous. They manifest themselves in the form of traumatic situations that can happen at work or in personal life. nine0047
- "Mental chewing gum" or rumination. When a person sets himself unsolvable questions and tasks.
- Arrhythmia. Obsession, which is manifested by the constant re-reading of various objects.
- Intrusive reproduction. It manifests itself in the painful formation of a person to remember everything that is not related to a given period of time, event or conversation. nine0016
- Onomatomania. An obsessive desire to remember all the words, titles and names.
- Misunderstanding. At this stage, intrusive thoughts are mild. A person feels a violation of the habitual consciousness, anxiety, cannot understand the nature of the occurrence of manic impulses.
- Understanding. Accompanied by a visit to a specialist. The patient understands that disturbances are present, but cannot yet realize the changes. Often at this stage there is hope that the state will change and life will return to its previous course.
- Adoption. The patient comes to terms with the mental disorder, agrees to treatment. He ceases to regard obsession and compulsion as a temporary condition. At this stage, it is important to fully interact with the attending physician, to obtain comprehensive information about the disease. nine0016
- Suicidal behavior.
 In a severe stage, the patient may commit suicide or try to cause physical harm to another person.
In a severe stage, the patient may commit suicide or try to cause physical harm to another person. - From constant contact with soap and detergents that a person uses so actively, dermatitis can develop.
- Possible problems in the social sphere. Inability to communicate with society. A person falls out of society - he does not have a hobby, he is afraid to appear in public places, he cannot concentrate on work. nine0016
- There are conflicts with relatives and friends. Some people with OCD are unable to start a family and have difficulty raising children.
- The patient has intrusive thoughts. The frequency of their appearance in this case exceeds the permissible norm for two weeks.
- Obsessive thoughts and actions qualitatively worsen the life of the patient. nine0016
- The implementation of obsessions and compulsions causes discomfort in the patient.
- Actions and thoughts occur regularly and frighten the patient with their frequency.
- There is no specificity in thoughts and actions, their nature is associated with anxiety, generates stress in a person, internal tension.

- Primary. A person learns about a genetic predisposition, corrects his behavior with the help of a specialist, uses various methods to prevent the occurrence of a violation. Primary prevention also includes educational methods.
- Secondary. Used to prevent recurrence of OCD. In this case, you will also need the help of a specialist to correct behavior, calm and sufficient sleep, abstinence from alcoholic beverages and drugs. You can also follow a special diet that is aimed at producing serotonin. nine0016
- Erich Fromm, "The human soul, its capacity for good and evil"
- Karen Horney, Neurosis and Personal Growth: The Struggle for Self-Realization
- Goldsmith G.

What is obsessive-compulsive disorder?
Unsplash
Obsessive-compulsive disorder is a common chronic and long-term condition in which a person has uncontrollable repetitive, obsessive thoughts (ideas) and/or actions (behaviors) [1]. OCD is diagnosed in 1.3% of the world's population [2]. nine0003
Many people confuse OCD with nail biting or negative thinking. Both can be a sign of the disease, but other diagnostic criteria must be taken into account. The obsession is often that a person considers certain numbers or colors to be "good" or "bad". It happens that the habit with OCD is washing your hands repeatedly after touching something that is considered dirty, infected, dangerous. Although the person does not want to think or do it, he is unable to stop [3]. nine0003
nine0003
Vladimir BelovMedical psychologist, child psychologist, consultant suicidologist, leading specialist of the Semeynaya clinic network
“Obsessive Compulsive Disorder is a neuropsychological disorder that always includes two components:
The most common connection between these components is that compulsions are actions whose purpose is to neutralize or reduce the distress caused by obsessions. Rituals include such processes as endless washing of hands, double-checking one's own actions or the state of some objects. For some people, these are specific prayers, rituals when going to work, when returning to an apartment, while waiting for transport.
Signs and symptoms of obsessive-compulsive disorder
Unsplash
Obsessions - involuntary thoughts and ideas: "I shook hands with a person and now I can get infected with something.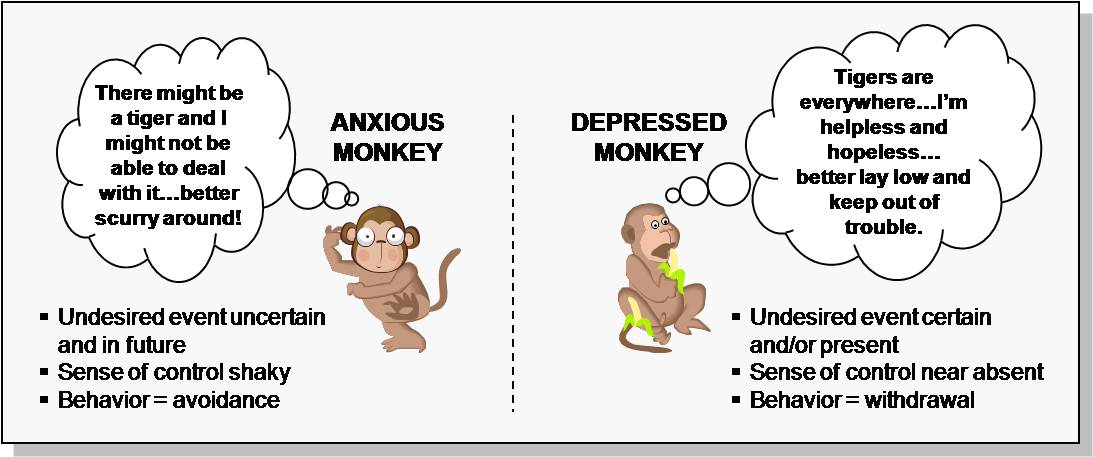 " This rumination in itself is perfectly normal, but the person with OCD will wash their hands again and again, unable to get rid of it. This is already a compulsion - an obsessive behavior, an individual unstoppable ritual. In the short term, it reduces anxiety, but the thought returns and the action must be repeated. A person feels that he must do it, while he cannot stop. Everyone has recurring habits or thoughts that recur frequently. But in the case of OCD they are:
" This rumination in itself is perfectly normal, but the person with OCD will wash their hands again and again, unable to get rid of it. This is already a compulsion - an obsessive behavior, an individual unstoppable ritual. In the short term, it reduces anxiety, but the thought returns and the action must be repeated. A person feels that he must do it, while he cannot stop. Everyone has recurring habits or thoughts that recur frequently. But in the case of OCD they are:
It's not unusual to wonder if the curling iron is unplugged. It’s worth worrying if this thought haunts you every day, makes you return home halfway from work and check (more than once, even if you just made sure that the device is not turned on). Obsessive-compulsive disorder comes in many forms, but most cases fall into at least one of the four main categories. The symptoms of OCD are rooted in the person's obsessive behavior.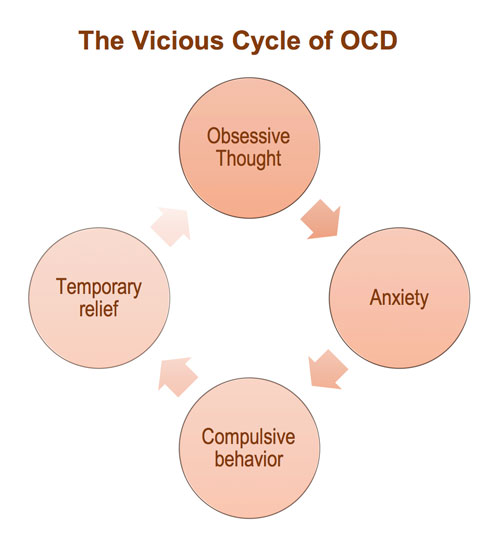 For example, he:
For example, he:
Anastasia AfanasyevaPsychiatrist, psychotherapist, clinical director of the psychological platform Alter
“Intrusive thoughts can occur as part of a variety of disorders, from psychosis to anxiety. To understand what disease these thoughts can be associated with, experts look at how a person treats them. For example, a person in psychosis may not even have a shadow of doubt and discomfort from the fact that the obsessive thought “you can harm your child” is spinning in his head. A person with OCD cannot have this, he will be frightened by such thoughts, and he will try to do everything to prevent this from happening, for example, remove all sharp objects away from him or not approach the child. Discomfort and the feeling that these thoughts are "inadequate", "wrong" will be an important identifying factor that this is OCD. nine0003
A person with OCD cannot have this, he will be frightened by such thoughts, and he will try to do everything to prevent this from happening, for example, remove all sharp objects away from him or not approach the child. Discomfort and the feeling that these thoughts are "inadequate", "wrong" will be an important identifying factor that this is OCD. nine0003
People without disorders can also have obsessive thoughts, but normally we quickly cope with them and they do not disturb life, forcing us to rebuild it for ourselves: the thought appeared - the person brushed it off and moved on.
Causes of OCD
Unsplash
Doctors do not give a specific explanation of the causes of the onset and development of OCD. It is most often diagnosed in adolescence and adulthood, with women 1.6 times more likely than men [4]. The factors for the development of the disease include:
There is a hypothesis that disturbing deviations developed and persisted in the course of evolution [7]. When people did not have access to modern advances in medicine and hygiene, those who had less contact with a possible source of infection and were constantly on the alert, assessing possible risks and double-checking the safety of food and housing, survived.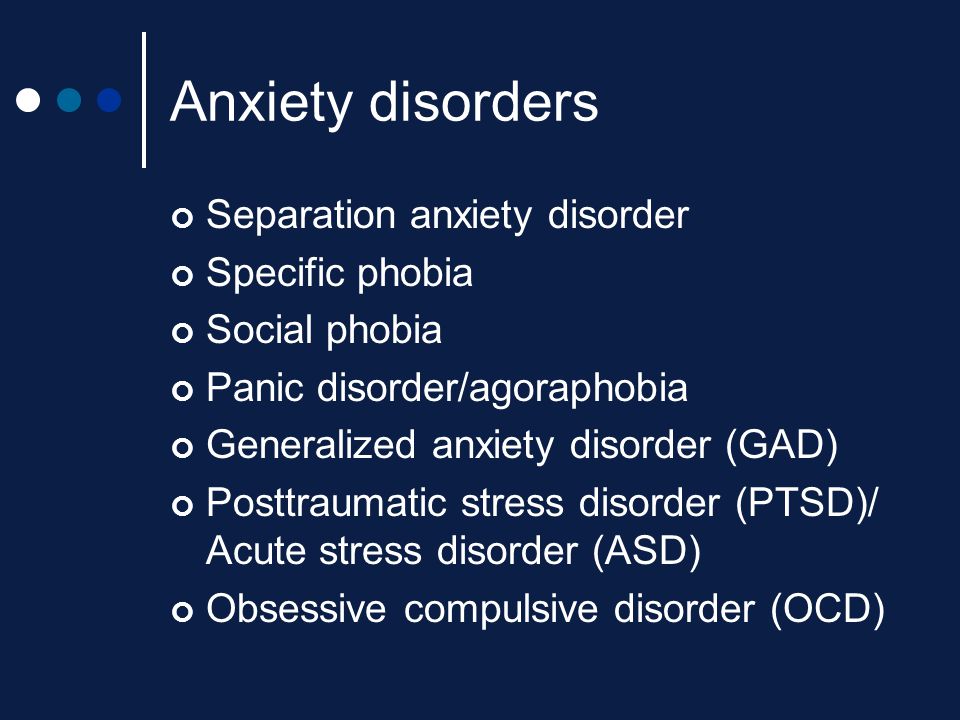 nine0003
nine0003
Obsessive Compulsive Disorder Diagnostics
Unsplash
All people from time to time find themselves in stressful situations, many people find it helpful to put things in order at home or in the closet, everyone at least once caught himself thinking that he had not turned off the coffee maker in a hurry to a meeting. It doesn't mean you have OCD. Only a doctor can make an accurate diagnosis. Contact a specialist if the above symptoms directly affect your relationship with yourself and others, steal time, do not allow you to relax and enjoy life. nine0003
In society, the attitude towards OCD is often superficial and not serious. It is often perceived as a funny feature of a person. But the worsening symptoms cannot be controlled by willpower alone. OCD can be expressed in varying degrees of obsession, and for many it really does not interfere (and may help maintain cleanliness and keep processes under control), but for others it poses a real threat to normal life [8].
There are specialized tests for obsessive-compulsive disorder. Try to answer several questions in the format "often", "rarely", "never", "always":
If most of the described thoughts and situations appear suspiciously often in your daily life, you should consult a general practitioner. He will conduct a physical examination and order blood tests to make sure that the symptoms are not caused by something else. If OCD is suspected, work with a therapist or psychiatrist to talk about life circumstances, feelings, thoughts, and habits.
He will conduct a physical examination and order blood tests to make sure that the symptoms are not caused by something else. If OCD is suspected, work with a therapist or psychiatrist to talk about life circumstances, feelings, thoughts, and habits.
How to treat obsessive-compulsive disorder
Shutterstock
There is no specific drug that can completely eliminate the symptoms of OCD. But medication support and additional psychological techniques for working on oneself help to work through this problem and keep it under control.
Psychotherapy
Cognitive Behavioral Therapy allows you to change your thinking patterns. Anastasia Afanasyeva believes that one of the most important techniques when working with OCD is distancing, exposing and challenging thoughts: “Distancing is a group of techniques in which we teach a person with OCD to notice intrusive thoughts, realize their ineffectiveness and switch from thinking about them to current ones. affairs. It is important here not to try to start controlling and “not thinking” these thoughts, as this is unrealistic and causes even more anxiety. Instead, for example, we can imagine that thoughts are like an annoying radio broadcast that cannot be turned off, but is not worth listening to. nine0003
affairs. It is important here not to try to start controlling and “not thinking” these thoughts, as this is unrealistic and causes even more anxiety. Instead, for example, we can imagine that thoughts are like an annoying radio broadcast that cannot be turned off, but is not worth listening to. nine0003
Exposure is the conscious exposure to uncomfortable situations in order to gradually learn to endure stress and stop using rituals that reduce anxiety in the moment, such as double-checking, washing hands, avoiding sharp objects.
Challenging and checking the reality of thoughts helps to understand that often a thought is just a thought and not every thought that comes to mind is worth believing. To assess how true this idea is, you can write it down on a piece of paper and give facts for and against its correctness. nine0003
Relaxation
Anxiety and obsessive thoughts are inevitably associated with tension in the body. Available meditation techniques, as well as massage and yoga classes, help to consciously look at the circumstances and cope with stress.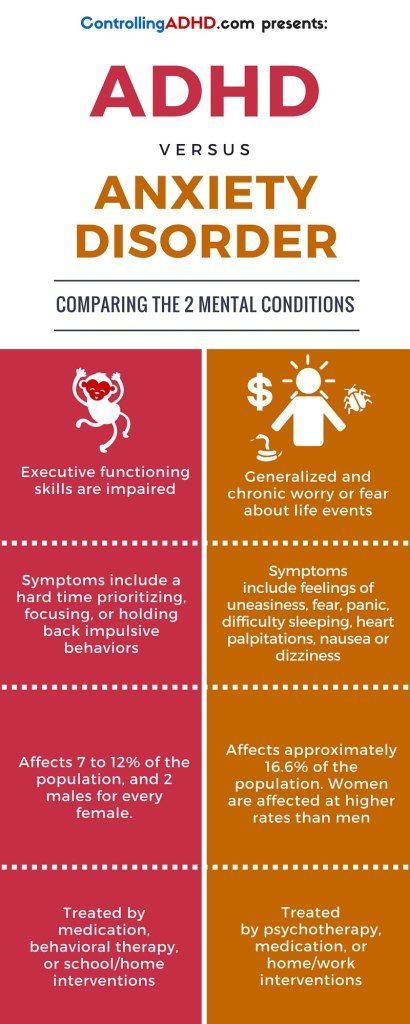
Anastasia Afanasyeva:
“In general, working with anxiety disorders always involves homework, as people learn to cope with their anxiety not only in the psychologist's office, but also in situations that arise in everyday life. Mostly it's working with thoughts and changing behavioral strategies that support OCD or reduce anxiety for only a short time. nine0003
The most common treatment for OCD involves individual sessions with a psychotherapist. There are practically no therapy protocols with proven efficacy for groups.”
Medicines
When taking drugs, you can achieve a stable remission. The timing of drug treatment will be determined by the attending physician. Do not stop taking antidepressants at the first sign of improvement.
Vladimir Belov:
“First of all, we need both a psychiatrist and a medical psychologist/psychotherapist. Because, on the one hand, cognitive-behavioral therapy is used, which is quite effective and has a lot of scientific evidence: exposure and prevention of reactions and rituals. This program goes on for several months and is combined with drugs. First of all, these are antidepressants - selective serotonin reuptake inhibitors and atypical antipsychotic drugs. Much depends on the condition of the patient and the severity of the process in which he is. nine0003
This program goes on for several months and is combined with drugs. First of all, these are antidepressants - selective serotonin reuptake inhibitors and atypical antipsychotic drugs. Much depends on the condition of the patient and the severity of the process in which he is. nine0003
What to do for relatives of a patient with OCD
Unsplash
People who live near a person with OCD often find themselves in difficult conditions. They want to help by interrupting the compulsive manifestations of a loved one, which can create an even more stressful situation for him. But it is also not worth closing your eyes to the disease. Psychologists advise updating it, pronouncing the problem. Develop the emotional intelligence of a loved one: let's understand that he can safely talk to you about any of his feelings. Emphasize that you are always ready to listen and help: “I am with you, we will deal with this problem together.” nine0003
Anastasia Afanasyeva:
“If someone in your family suffers from OCD, one of the important tasks that you face is to stay out of the anxiety maintenance cycle.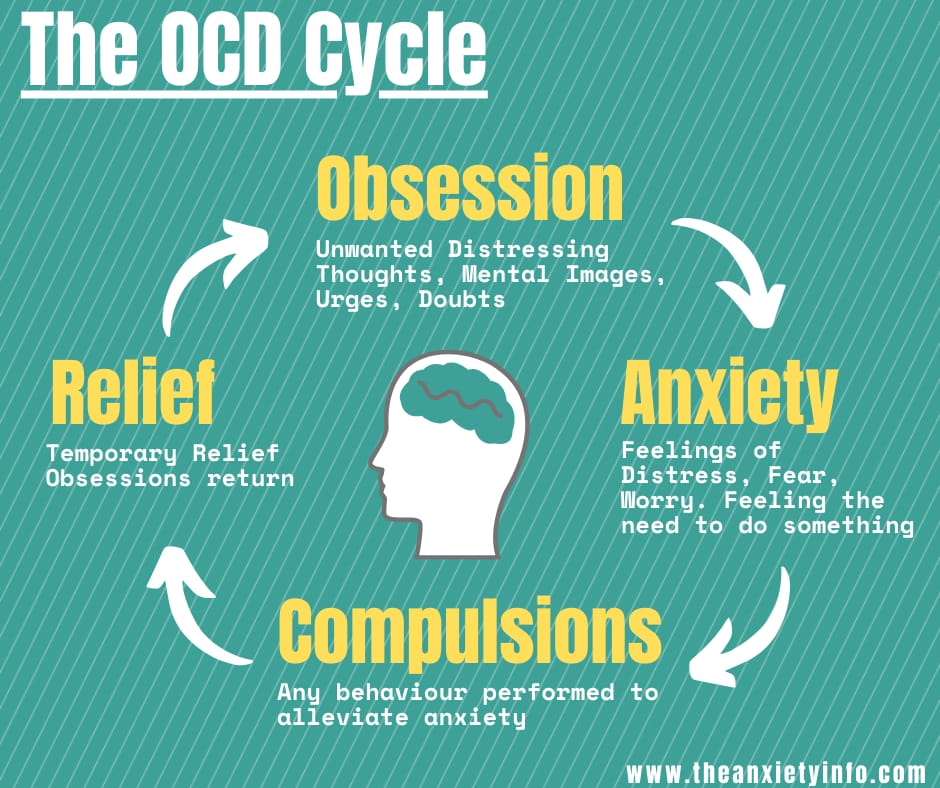 For example, one should not encourage the desire for excessive cleanliness, endless washing of clothes, washing hands, constant fruitless visits to doctors, one should not participate in rechecking any facts. You need to understand that this does not help a loved one cope with anxiety, but reinforces a non-working pattern of behavior and serves as proof that such behavior and thoughts are justified. nine0003
For example, one should not encourage the desire for excessive cleanliness, endless washing of clothes, washing hands, constant fruitless visits to doctors, one should not participate in rechecking any facts. You need to understand that this does not help a loved one cope with anxiety, but reinforces a non-working pattern of behavior and serves as proof that such behavior and thoughts are justified. nine0003
Forums, support groups for people with OCD
Unsplash
The best option is to contact a trusted doctor and treat according to his recommendations. In addition to medicines and work with a specialist, the fulfillment of independent tasks plays an important role. It is important for people with OCD to talk about the problem and see the support of others. Like-minded forums often help. You can join thematic groups on social networks or contact volunteers:
Share
Materials for article
Authors
Tags
Irina Rudevich
OCD: what is obsessive-compulsive mental disorder, diagnosis, treatment
In our time, obsessive-compulsive mental disorder is faced by those who knew this disease only by hearsay. Surprisingly, psychologists note that many OCD patients can find advantages in their illness. Still, it is better to diagnose the disease and try to cope with it. The statistics are disappointing - up to 3% of the world's population is faced with a violation. nine0003
What is OCD (obsessive compulsive disorder)?
OCD, or obsessive-compulsive disorder, is a mental disorder characterized by obsessive thoughts (obsessions) and actions (compulsions). Striking examples include the desire for perfect cleanliness, the fear of catching various diseases, a manic attachment to certain rituals (for example, pressing the doorbell three times, washing hands after each handshake, etc. ).
).
Often, the manifestation of obsessive-compulsive disorder is accompanied by bodily harm to oneself or other people. It is important to diagnose the disease in time so that it does not develop into a pathology. nine0003
Obsessive-compulsive disorder is also called obsessive-compulsive disorder. The disease can be chronic, episodic or progressive. Equally, the disease is present in both men and women. Sometimes the patient himself understands that his thoughts in their manifestation are absurd, and the behavior that follows them is very ineffective. But resisting them is useless. Suppressing these actions only increases the anxiety state.
If we consider the disease from the side of physiology, then it leads to functional disorders in the following parts of the brain: nine0003
The severity of obsessive-compulsive personality disorder in patients can vary and most often depends on the presence of stressful situations in a person's life. Violation can change life for the worse, reduce communication with society. A distinctive feature of obsession can be considered the absence of rationalism, and compulsions - that they cannot be abandoned. nine0003
Violation can change life for the worse, reduce communication with society. A distinctive feature of obsession can be considered the absence of rationalism, and compulsions - that they cannot be abandoned. nine0003
Patients, realizing their situation, are afraid to go crazy, start worrying about their relatives, about their own and their safety. In practice, such neuroses do not lead to serious consequences or mental disorders, and aggressive thoughts do not lead to subsequent actions.
This is what distinguishes a person with OCD from mentally deranged or hallucinating patients. A patient with OCD has the following symptoms:
Symptoms of obsessive-compulsive disorder
The most obvious symptoms include the obsessive and compulsive disorders already mentioned, that is, obsessive thoughts and a manic desire to perform any action.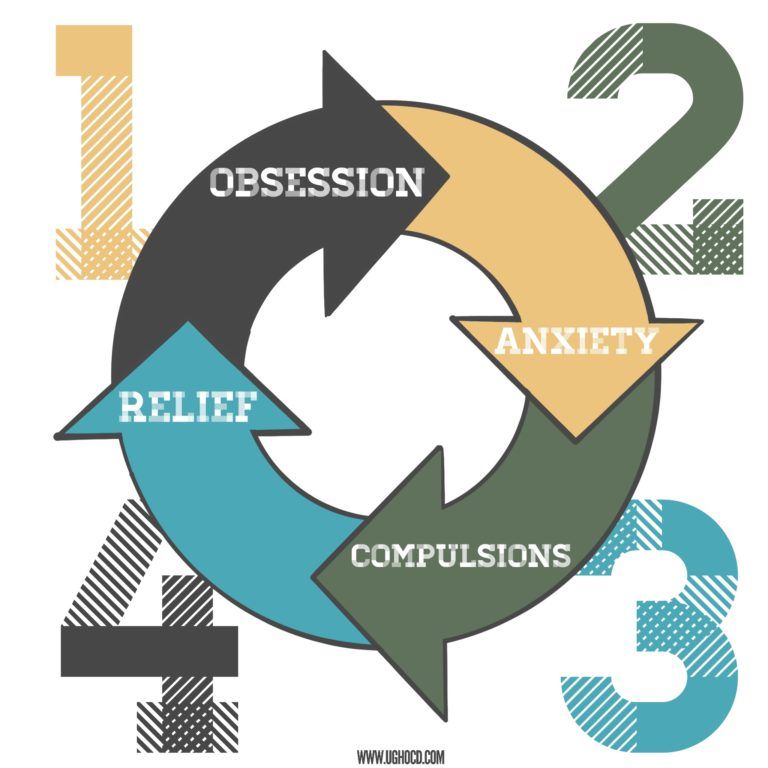 Thoughts can manifest as images, delusional ideas, inexplicable drives. Obsessive-compulsive disorder and its symptoms are observed in the form of the inability to make decisions regarding everyday situations. nine0003
Thoughts can manifest as images, delusional ideas, inexplicable drives. Obsessive-compulsive disorder and its symptoms are observed in the form of the inability to make decisions regarding everyday situations. nine0003
Of the main signs of OCD, the following can be distinguished: obsessive-compulsive disorder:
Among the mental symptoms in patients, the following are observed:
With OCD, the patient appropriates all incoming thoughts, in contrast to the disease of a split personality, when a person hears "foreign" voices.
These actions themselves do not bring pleasure to a person, but they can reduce the level of anxiety and stress. This does not last long and after a while the obsession returns, a phobia sets in and everything starts in a circle. Outwardly, compulsions can resemble ordinary work, for example, a person lays out things, constantly cleans the house, although the house can be perfectly clean anyway. nine0003
This does not last long and after a while the obsession returns, a phobia sets in and everything starts in a circle. Outwardly, compulsions can resemble ordinary work, for example, a person lays out things, constantly cleans the house, although the house can be perfectly clean anyway. nine0003
Sometimes the manifestation of obsessive-compulsive disorder manifests itself physically. A person does not sleep well, he has headaches, heartaches, blinking becomes more frequent, nervous tics and convulsions occur, pressure rises, appetite is disturbed, and sexual desire decreases.
The manifestations of obsessive-compulsive disorder are constant and manic in nature, they cause inconvenience to a person.
Causes of obsessive-compulsive disorder nine0031
Scientists are still conducting various studies to establish the exact causes of the violation.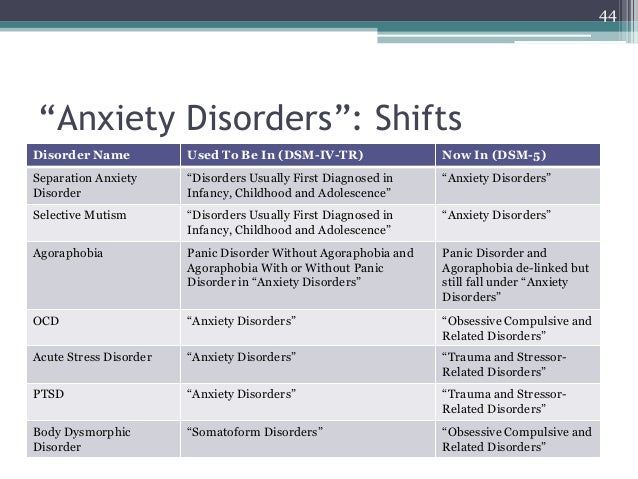 But there are no exact data in this area. Despite this, it is customary to single out several areas that can cause obsessive-compulsive disorder syndrome, the reasons are:
But there are no exact data in this area. Despite this, it is customary to single out several areas that can cause obsessive-compulsive disorder syndrome, the reasons are:
Disease pathogenesis
Despite various theories of the occurrence of OCD, the pathogenesis of obsessive-compulsive disorder has a well-defined nature of occurrence, although not fully understood.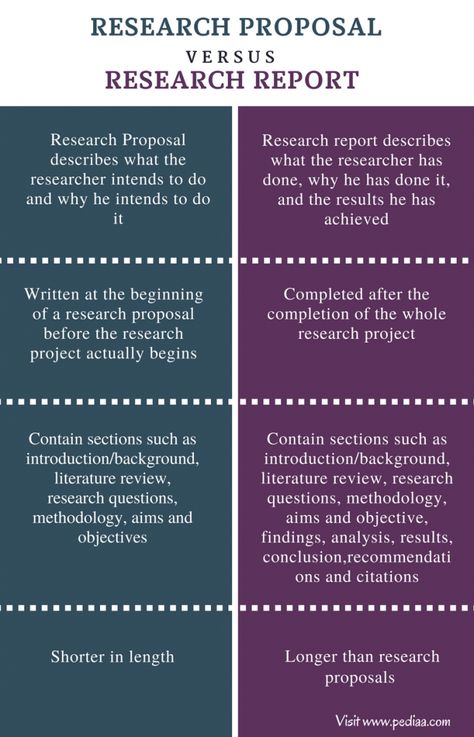 These structures of the body interact with each other through serotonin. The lack of this hormone is due to the heightened effect of neurons on the cerebral cortex. This provokes a blockage of the nerve impulse, which does not reach the next neuron.
These structures of the body interact with each other through serotonin. The lack of this hormone is due to the heightened effect of neurons on the cerebral cortex. This provokes a blockage of the nerve impulse, which does not reach the next neuron.
Classification and stage of development of ROC nine0031
Obsessive-compulsive disorder has different degrees of severity and manifests itself in the following stages:
There are several variants of manifestation. For example, they can be expressed in simple symbolic actions.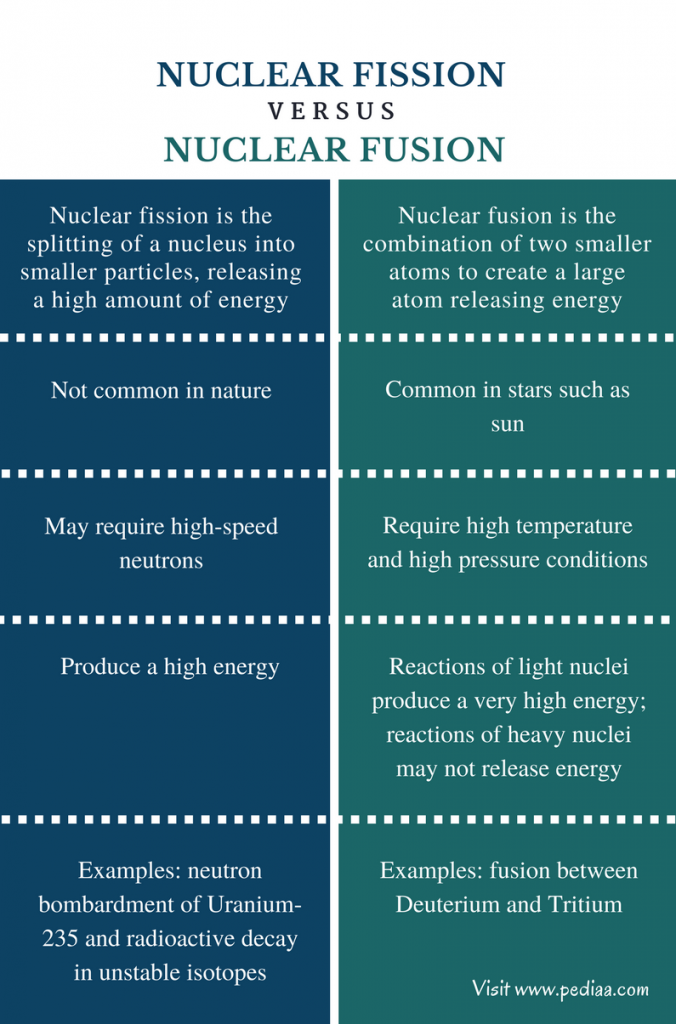 The patient can put a certain prohibition on performing actions, for example, counting steps for failure or success. They can also be expressed in physical actions aimed at self-harm: pulling out body hair and eating it. As a rule, an accurate diagnosis requires complete immersion in the disease in order to understand whether it is different from other mental disorders. nine0003
The patient can put a certain prohibition on performing actions, for example, counting steps for failure or success. They can also be expressed in physical actions aimed at self-harm: pulling out body hair and eating it. As a rule, an accurate diagnosis requires complete immersion in the disease in order to understand whether it is different from other mental disorders. nine0003
The manifestation of obsessive-compulsive disorder is equally observed in both men and women. It is much less common in children, although it is believed that the first signs may appear before the age of 11 years.
Obsessive-compulsive disorder is most common in adolescents. Studies have shown that the disorder affects mainly adolescents aged 11-17 years. Up to 85% of all patients are adolescents.
Each person, as a rule, goes through three stages that are inherent in OCD: nine0003
The obsessive-compulsive disorder scale was introduced to determine the stage of the disorder. It's called the Yale-Brown scale. It was developed at Yale University under the direction of Wayne Goodman. This manual is accepted throughout the world as a traditional method for identifying the stage of OCD.
Complications of obsessive-compulsive disorder
In obsessive-compulsive disorder, the consequences can be irreversible and cover completely different areas of life: nine0003
When to see a doctor?
At the slightest suspicion of the listed symptoms, you should immediately contact a specialist. Often a person with OCD is not able to independently realize and accept that his behavior and way of thinking has changed.
If you have problems with society and loved ones, then you should listen to their advice and make an appointment with a doctor. nine0003
Diagnostics
The violation is included in the International Classification of Diseases (ICD-10). Diagnosis of obsessive-compulsive disorder includes a mandatory visit to a specialist with subsequent diagnosis.
When making a diagnosis, the doctor relies on the following criteria:
The diagnosis is made if the patient has obsessive thoughts or ideas. They adopt an image that prompts them to impulsively perform some kind of action. nine0003
There is a mixed form of the disorder where the patient is equally haunted by obsessive thoughts and there is a manic execution of compulsions.
Treatment
Comprehensive treatment of obsessive-compulsive disorder includes an individual visit to a psychotherapist - a specialist identifies the causes of the disease, helps to recognize the signs of an obsessive-compulsive disorder, and accepts that the patient has OCD. The next step is the CBT method (Cognitive Behavioral Therapy). The psychotherapist teaches the patient to monitor the appearance of OCD, find ways to change negative thoughts, displace them and change them into optimistic actions. Medications in this case are prescribed with the consent of the patient. nine0003
Antidepressants and anxiolytics (drugs that relieve anxiety) are prescribed as medicines.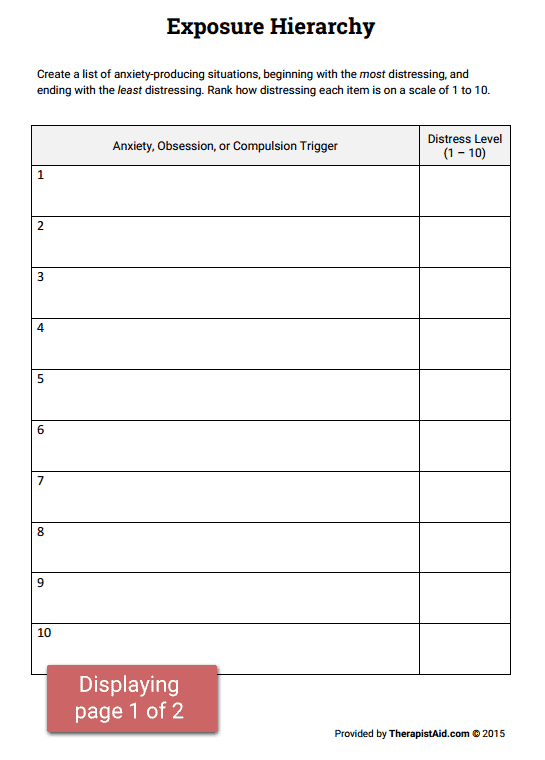 Treatment with sedatives is also possible, which helps relieve depressive thoughts, remove depressed mood.
Treatment with sedatives is also possible, which helps relieve depressive thoughts, remove depressed mood.
Therapy for obsessive-compulsive disorder may include biofeedback therapy. Sensors are installed on the patient, with the help of which breathing, muscle work and heart rate are controlled. This technique helps to control the condition and further cope with emerging obsessive thoughts and negative emotions. nine0003
You can get treatment from private practitioners, but it is better to choose clinics that specialize in the treatment of mental disorders. Such institutions employ doctors with many years of experience who have been practicing and treating obsessive-compulsive disorder for many years.
+7 (495) 121-48-31
Prevention and recommendations for illness
OCD is typical for people who have any other mental disorders. Also, with a stable calm state of patients diagnosed with OCD, its recurrence is possible. Since the specific cause of the violation has not been established, then prevention is advisory in nature. nine0003
nine0003
For obsessive-compulsive disorder, recommendations in terms of prevention can be primary and secondary:
If any signs appear, it is better to consult a doctor, and not try to come to terms with unfamiliar conditions. It is useful to get comprehensive information about OCD from people who have suffered this disorder.
References: