Non medicine treatment for depression
SAMHSA’s National Helpline | SAMHSA
Your browser is not supported
Switch to Chrome, Edge, Firefox or Safari
Main page content
-
SAMHSA’s National Helpline is a free, confidential, 24/7, 365-day-a-year treatment referral and information service (in English and Spanish) for individuals and families facing mental and/or substance use disorders.
Also visit the online treatment locator.
SAMHSA’s National Helpline, 1-800-662-HELP (4357) (also known as the Treatment Referral Routing Service), or TTY: 1-800-487-4889 is a confidential, free, 24-hour-a-day, 365-day-a-year, information service, in English and Spanish, for individuals and family members facing mental and/or substance use disorders.
This service provides referrals to local treatment facilities, support groups, and community-based organizations.
Also visit the online treatment locator, or send your zip code via text message: 435748 (HELP4U) to find help near you. Read more about the HELP4U text messaging service.
The service is open 24/7, 365 days a year.
English and Spanish are available if you select the option to speak with a national representative. Currently, the 435748 (HELP4U) text messaging service is only available in English.
In 2020, the Helpline received 833,598 calls. This is a 27 percent increase from 2019, when the Helpline received a total of 656,953 calls for the year.
The referral service is free of charge. If you have no insurance or are underinsured, we will refer you to your state office, which is responsible for state-funded treatment programs. In addition, we can often refer you to facilities that charge on a sliding fee scale or accept Medicare or Medicaid. If you have health insurance, you are encouraged to contact your insurer for a list of participating health care providers and facilities.
If you have health insurance, you are encouraged to contact your insurer for a list of participating health care providers and facilities.
The service is confidential. We will not ask you for any personal information. We may ask for your zip code or other pertinent geographic information in order to track calls being routed to other offices or to accurately identify the local resources appropriate to your needs.
No, we do not provide counseling. Trained information specialists answer calls, transfer callers to state services or other appropriate intake centers in their states, and connect them with local assistance and support.
-
Suggested Resources
What Is Substance Abuse Treatment? A Booklet for Families
Created for family members of people with alcohol abuse or drug abuse problems. Answers questions about substance abuse, its symptoms, different types of treatment, and recovery.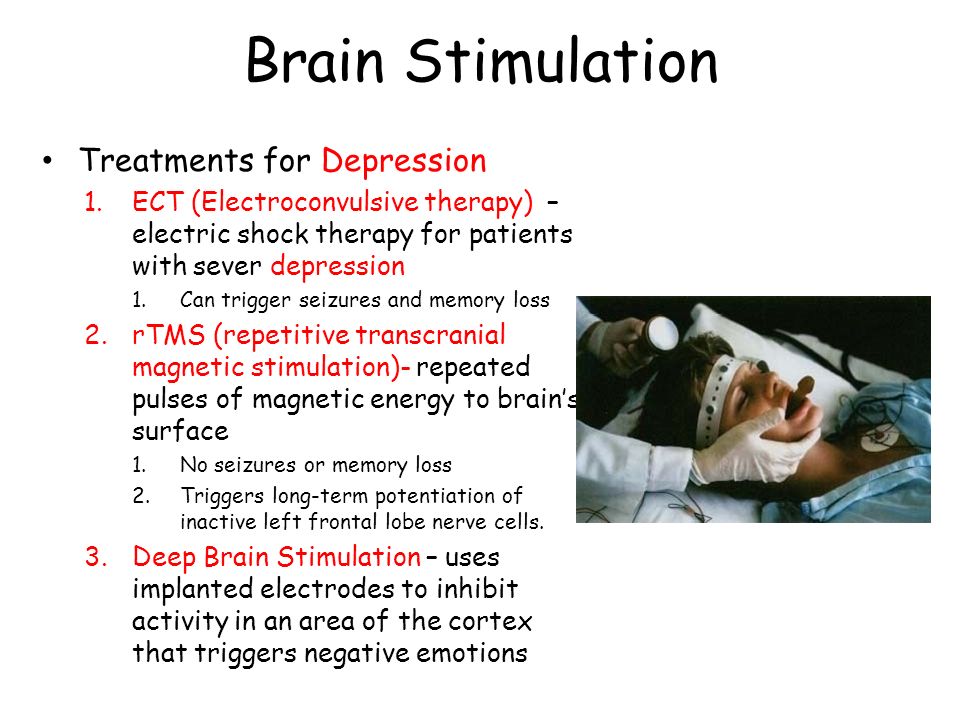 Addresses concerns of children of parents with substance use/abuse problems.
Addresses concerns of children of parents with substance use/abuse problems.It's Not Your Fault (NACoA) (PDF | 12 KB)
Assures teens with parents who abuse alcohol or drugs that, "It's not your fault!" and that they are not alone. Encourages teens to seek emotional support from other adults, school counselors, and youth support groups such as Alateen, and provides a resource list.After an Attempt: A Guide for Taking Care of Your Family Member After Treatment in the Emergency Department
Aids family members in coping with the aftermath of a relative's suicide attempt. Describes the emergency department treatment process, lists questions to ask about follow-up treatment, and describes how to reduce risk and ensure safety at home.Family Therapy Can Help: For People in Recovery From Mental Illness or Addiction
Explores the role of family therapy in recovery from mental illness or substance abuse. Explains how family therapy sessions are run and who conducts them, describes a typical session, and provides information on its effectiveness in recovery.
For additional resources, please visit the SAMHSA Store.
Last Updated: 08/30/2022
Alcohol, Tobacco, and Other Drugs
Your browser is not supported
Switch to Chrome, Edge, Firefox or Safari
Misusing alcohol, tobacco, and other drugs can have both immediate and long-term health effects.The misuse and abuse of alcohol, tobacco, illicit drugs, and prescription medications affect the health and well-being of millions of Americans. NSDUH estimates allow researchers, clinicians, policymakers, and the general public to better understand and improve the nation’s behavioral health. These reports and detailed tables present estimates from the 2021 National Survey on Drug Use and Health (NSDUH).
Alcohol
Data:
- Among the 133.1 million current alcohol users aged 12 or older in 2021, 60.0 million people (or 45.1%) were past month binge drinkers.
 The percentage of people who were past month binge drinkers was highest among young adults aged 18 to 25 (29.2% or 9.8 million people), followed by adults aged 26 or older (22.4% or 49.3 million people), then by adolescents aged 12 to 17 (3.8% or 995,000 people). (2021 NSDUH)
The percentage of people who were past month binge drinkers was highest among young adults aged 18 to 25 (29.2% or 9.8 million people), followed by adults aged 26 or older (22.4% or 49.3 million people), then by adolescents aged 12 to 17 (3.8% or 995,000 people). (2021 NSDUH) - Among people aged 12 to 20 in 2021, 15.1% (or 5.9 million people) were past month alcohol users. Estimates of binge alcohol use and heavy alcohol use in the past month among underage people were 8.3% (or 3.2 million people) and 1.6% (or 613,000 people), respectively. (2021 NSDUH)
- In 2020, 50.0% of people aged 12 or older (or 138.5 million people) used alcohol in the past month (i.e., current alcohol users) (2020 NSDUH)
- Among the 138.5 million people who were current alcohol users, 61.6 million people (or 44.4%) were classified as binge drinkers and 17.7 million people (28.8% of current binge drinkers and 12.8% of current alcohol users) were classified as heavy drinkers (2020 NSDUH)
- The percentage of people who were past month binge alcohol users was highest among young adults aged 18 to 25 (31.
 4%) compared with 22.9% of adults aged 26 or older and 4.1% of adolescents aged 12 to 17 (2020 NSDUH)
4%) compared with 22.9% of adults aged 26 or older and 4.1% of adolescents aged 12 to 17 (2020 NSDUH) - Excessive alcohol use can increase a person’s risk of stroke, liver cirrhosis, alcoholic hepatitis, cancer, and other serious health conditions
- Excessive alcohol use can also lead to risk-taking behavior, including driving while impaired. The Centers for Disease Control and Prevention reports that 29 people in the United States die in motor vehicle crashes that involve an alcohol-impaired driver daily
Programs/Initiatives:
- STOP Underage Drinking interagency portal - Interagency Coordinating Committee on the Prevention of Underage Drinking
- Interagency Coordinating Committee on the Prevention of Underage Drinking
- Talk. They Hear You.
- Underage Drinking: Myths vs. Facts
- Talking with your College-Bound Young Adult About Alcohol
Relevant links:
- National Association of State Alcohol and Drug Abuse Directors
- Department of Transportation Office of Drug & Alcohol Policy & Compliance
- Alcohol Policy Information Systems Database (APIS)
- National Institute on Alcohol Abuse and Alcoholism
Tobacco
Data:
- In 2020, 20.
 7% of people aged 12 or older (or 57.3 million people) used nicotine products (i.e., used tobacco products or vaped nicotine) in the past month (2020 NSDUH)
7% of people aged 12 or older (or 57.3 million people) used nicotine products (i.e., used tobacco products or vaped nicotine) in the past month (2020 NSDUH) - Among past month users of nicotine products, nearly two thirds of adolescents aged 12 to 17 (63.1%) vaped nicotine but did not use tobacco products. In contrast, 88.9% of past month nicotine product users aged 26 or older used only tobacco products (2020 NSDUH)
- Tobacco use is the leading cause of preventable death, often leading to lung cancer, respiratory disorders, heart disease, stroke, and other serious illnesses. The CDC reports that cigarette smoking causes more than 480,000 deaths each year in the United States
- The CDC’s Office on Smoking and Health reports that more than 16 million Americans are living with a disease caused by smoking cigarettes
Electronic cigarette (e-cigarette) use data:
- In 2021, 13.2 million people aged 12 or older (or 4.7%) used an e-cigarette or other vaping device to vape nicotine in the past month.
 The percentage of people who vaped nicotine was highest among young adults aged 18 to 25 (14.1% or 4.7 million people), followed by adolescents aged 12 to 17 (5.2% or 1.4 million people), then by adults aged 26 or older (3.2% or 7.1 million people).
The percentage of people who vaped nicotine was highest among young adults aged 18 to 25 (14.1% or 4.7 million people), followed by adolescents aged 12 to 17 (5.2% or 1.4 million people), then by adults aged 26 or older (3.2% or 7.1 million people). - Among people aged 12 to 20 in 2021, 11.0% (or 4.3 million people) used tobacco products or used an e-cigarette or other vaping device to vape nicotine in the past month. Among people in this age group, 8.1% (or 3.1 million people) vaped nicotine, 5.4% (or 2.1 million people) used tobacco products, and 3.4% (or 1.3 million people) smoked cigarettes in the past month. (2021 NSDUH)
- Data from the Centers for Disease Control and Prevention’s 2020 National Youth Tobacco Survey. Among both middle and high school students, current use of e-cigarettes declined from 2019 to 2020, reversing previous trends and returning current e-cigarette use to levels similar to those observed in 2018
- E-cigarettes are not safe for youth, young adults, or pregnant women, especially because they contain nicotine and other chemicals
Resources:
- Tips for Teens: Tobacco
- Tips for Teens: E-cigarettes
- Implementing Tobacco Cessation Programs in Substance Use Disorder Treatment Settings
- Synar Amendment Program
Links:
- Truth Initiative
- FDA Center for Tobacco Products
- CDC Office on Smoking and Health
- National Institute on Drug Abuse: Tobacco, Nicotine, and E-Cigarettes
- National Institute on Drug Abuse: E-Cigarettes
Opioids
Data:
- Among people aged 12 or older in 2021, 3.
 3% (or 9.2 million people) misused opioids (heroin or prescription pain relievers) in the past year. Among the 9.2 million people who misused opioids in the past year, 8.7 million people misused prescription pain relievers compared with 1.1 million people who used heroin. These numbers include 574,000 people who both misused prescription pain relievers and used heroin in the past year. (2021 NSDUH)
3% (or 9.2 million people) misused opioids (heroin or prescription pain relievers) in the past year. Among the 9.2 million people who misused opioids in the past year, 8.7 million people misused prescription pain relievers compared with 1.1 million people who used heroin. These numbers include 574,000 people who both misused prescription pain relievers and used heroin in the past year. (2021 NSDUH) - Among people aged 12 or older in 2020, 3.4% (or 9.5 million people) misused opioids in the past year. Among the 9.5 million people who misused opioids in the past year, 9.3 million people misused prescription pain relievers and 902,000 people used heroin (2020 NSDUH)
- According to the Centers for Disease Control and Prevention’s Understanding the Epidemic, an average of 128 Americans die every day from an opioid overdose
Resources:
- Medication-Assisted Treatment
- Opioid Overdose Prevention Toolkit
- TIP 63: Medications for Opioid Use Disorder
- Use of Medication-Assisted Treatment for Opioid Use Disorder in Criminal Justice Settings
- Opioid Use Disorder and Pregnancy
- Clinical Guidance for Treating Pregnant and Parenting Women With Opioid Use Disorder and Their Infants
- The Facts about Buprenorphine for Treatment of Opioid Addiction
- Pregnancy Planning for Women Being Treated for Opioid Use Disorder
- Tips for Teens: Opioids
- Rural Opioid Technical Assistance Grants
- Tribal Opioid Response Grants
- Provider’s Clinical Support System - Medication Assisted Treatment Grant Program
Links:
- National Institute on Drug Abuse: Opioids
- National Institute on Drug Abuse: Heroin
- HHS Prevent Opioid Abuse
- Community Anti-Drug Coalitions of America
- Addiction Technology Transfer Center (ATTC) Network
- Prevention Technology Transfer Center (PTTC) Network
Marijuana
Data:
- In 2021, marijuana was the most commonly used illicit drug, with 18.
 7% of people aged 12 or older (or 52.5 million people) using it in the past year. The percentage was highest among young adults aged 18 to 25 (35.4% or 11.8 million people), followed by adults aged 26 or older (17.2% or 37.9 million people), then by adolescents aged 12 to 17 (10.5% or 2.7 million people).
7% of people aged 12 or older (or 52.5 million people) using it in the past year. The percentage was highest among young adults aged 18 to 25 (35.4% or 11.8 million people), followed by adults aged 26 or older (17.2% or 37.9 million people), then by adolescents aged 12 to 17 (10.5% or 2.7 million people). - The percentage of people who used marijuana in the past year was highest among young adults aged 18 to 25 (34.5%) compared with 16.3% of adults aged 26 or older and 10.1% of adolescents aged 12 to 17 (2020 NSDUH)
- Marijuana can impair judgment and distort perception in the short term and can lead to memory impairment in the long term
- Marijuana can have significant health effects on youth and pregnant women.
Resources:
- Know the Risks of Marijuana
- Marijuana and Pregnancy
- Tips for Teens: Marijuana
Relevant links:
- National Institute on Drug Abuse: Marijuana
- Addiction Technology Transfer Centers on Marijuana
- CDC Marijuana and Public Health
Emerging Trends in Substance Misuse:
- Methamphetamine—In 2019, NSDUH data show that approximately 2 million people used methamphetamine in the past year.
 Approximately 1 million people had a methamphetamine use disorder, which was higher than the percentage in 2016, but similar to the percentages in 2015 and 2018. The National Institute on Drug Abuse Data shows that overdose death rates involving methamphetamine have quadrupled from 2011 to 2017. Frequent meth use is associated with mood disturbances, hallucinations, and paranoia.
Approximately 1 million people had a methamphetamine use disorder, which was higher than the percentage in 2016, but similar to the percentages in 2015 and 2018. The National Institute on Drug Abuse Data shows that overdose death rates involving methamphetamine have quadrupled from 2011 to 2017. Frequent meth use is associated with mood disturbances, hallucinations, and paranoia. - Cocaine—In 2019, NSDUH data show an estimated 5.5 million people aged 12 or older were past users of cocaine, including about 778,000 users of crack. The CDC reports that overdose deaths involving have increased by one-third from 2016 to 2017. In the short term, cocaine use can result in increased blood pressure, restlessness, and irritability. In the long term, severe medical complications of cocaine use include heart attacks, seizures, and abdominal pain.
- Kratom—In 2019, NSDUH data show that about 825,000 people had used Kratom in the past month. Kratom is a tropical plant that grows naturally in Southeast Asia with leaves that can have psychotropic effects by affecting opioid brain receptors.
 It is currently unregulated and has risk of abuse and dependence. The National Institute on Drug Abuse reports that health effects of Kratom can include nausea, itching, seizures, and hallucinations.
It is currently unregulated and has risk of abuse and dependence. The National Institute on Drug Abuse reports that health effects of Kratom can include nausea, itching, seizures, and hallucinations.
Resources:
- Tips for Teens: Methamphetamine
- Tips for Teens: Cocaine
- National Institute on Drug Abuse
More SAMHSA publications on substance use prevention and treatment.
Last Updated: 01/05/2023
Biological non-drug treatments for depression
In addition to pharmacological and psychotherapeutic treatment of depression, other methods have been proposed for its treatment.
These methods of treating depression, often effectively combined with pharmacotherapy and psychotherapy, include: intravenous laser blood irradiation, magnetic stimulation (transcranial low-frequency alternating magnetic field therapy, right-sided parapolarization therapy), extracorporeal detoxification (plasmapheresis), periodic normobaric hypoxia, craniocerebral hypothermia, light therapy, sleep deprivation, dietary therapy (including its unloading variants), balneotherapy (warm baths have long been used to alleviate the condition of a person who is depressed), massage and exercise therapy (breathing exercises and physical activity help to relieve symptoms of depression) .
Among the biological treatments for depression, electroconvulsive therapy occupies a special place.
Intravenous laser irradiation of blood
According to the recommendations of domestic scientists, intravenous laser irradiation of blood should be carried out on a low-intensity helium-neon apparatus (FALM-1). The wavelength of laser irradiation is 0.63 µm. The radiation power at the fiber output is 8 mW. The duration of the session is 15 minutes, the course of therapy is 8-12 sessions. It was noted that after laser therapy while taking psychopharmacological drugs, the severity of depressive symptoms almost halved in 60% of people suffering from depression. Patients with manifestations of apathy and melancholy are especially sensitive to laser therapy, a less pronounced effect is observed in complex depressive syndromes, including symptoms of depersonalization, obsessive-compulsive disorders and hypochondria. Laser therapy is ineffective in anxiety-depressive conditions. It should be borne in mind that the effect of laser therapy as a non-drug method of treatment, as well as from treatment with antidepressants, may be delayed and appear some time after the completion of the course of treatment. Currently, there are various upgrades of laser therapy. As an example, a differentiated method of low-intensity magneto-laser therapy can be cited. This method of treatment includes an individual staged program of course combined laser exposure, which is venous irradiation of the skin with continuous red light (0.63 μm) and transcutaneous irradiation with pulsed infrared light (0.89µm) projections of a number of biologically active zones and organs using standard magnetic attachments. Laser irradiation usually does not cause side effects and complications.
It should be borne in mind that the effect of laser therapy as a non-drug method of treatment, as well as from treatment with antidepressants, may be delayed and appear some time after the completion of the course of treatment. Currently, there are various upgrades of laser therapy. As an example, a differentiated method of low-intensity magneto-laser therapy can be cited. This method of treatment includes an individual staged program of course combined laser exposure, which is venous irradiation of the skin with continuous red light (0.63 μm) and transcutaneous irradiation with pulsed infrared light (0.89µm) projections of a number of biologically active zones and organs using standard magnetic attachments. Laser irradiation usually does not cause side effects and complications.
Extracorporeal detoxification
Extracorporeal detoxification as a biological non-drug treatment for depression is used in combination therapy for resistant depression and can be combined with fresh frozen plasma or albumin transfusion to normalize protein metabolism. For this, 2-3 plasmapheresis procedures are usually performed.
For this, 2-3 plasmapheresis procedures are usually performed.
Electroconvulsive therapy
Currently, one of the most effective non-drug methods of treating depression is electroconvulsive therapy, which is used as an independent method of treatment, and in combination with other methods of therapy (Nelson AI, 2002).
Electroshock therapy methods were used in ancient Greece. In the temples of Asclepius, depression was treated with electric snakes. In the Middle Ages, it was believed that a strong shock to the patient could bring him out of depression.
Treatment of depression with electric shock was recommended by Hill in 1814 (commotions electriques) (Kempinski A., 2002). Particular interest in this method of treating depression was noted in the early forties of the twentieth century. At present, electroconvulsive therapy is generally recognized to be highly effective in the treatment of depression.
It is difficult to overestimate the importance of electroconvulsive therapy for those patients for whom pharmacological treatment is contraindicated (pregnancy, certain somatic diseases, etc.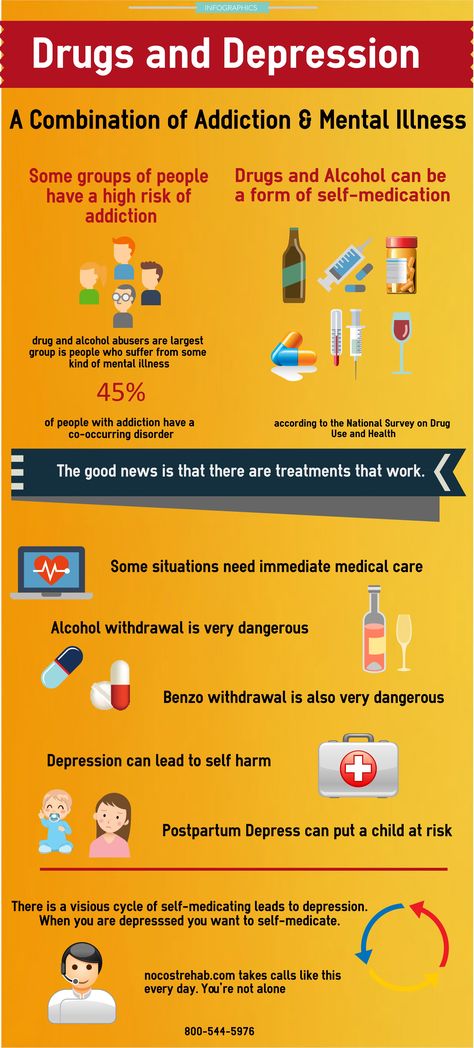 ), as well as in case of need to overcome depression resistant to other types of therapy.
), as well as in case of need to overcome depression resistant to other types of therapy.
Usually, about 8-10 shocks are needed to obtain a therapeutic effect from electroconvulsive therapy, at a frequency of 3 sessions per week.
Subject to monitoring of the condition of patients, it is possible to treat them with ECT in an outpatient setting or in the daytime treatment of depression in a hospital.
In general, the combination of ECT with antidepressants is not recommended, perhaps the use of small doses of tranquilizers.
Complications of electroconvulsive therapy include spinal injury and circulatory disorders, states of confusion after convulsive seizures, as well as periods of anterograde and retrograde memory impairment. The latter can persist for up to a month after the end of ECT. ECT causes a temporary rise in blood pressure (often to fairly high levels) and increases the heart rate.
Relative contraindications for ECT include coronary heart disease and arrhythmias, as well as some localization of a brain tumor.
Most patients are afraid of this method of therapy, so the importance of professional psychotherapeutic work with the patient, as well as its subsequent support during the ECT therapy itself, should be emphasized.
Magnetic stimulation
Repeated transcranial magnetic stimulation (TMS) has been proposed for the non-drug treatment of depression in 1985 (Barcer A., et al., 1985). This treatment for depression, as well as vagus nerve stimulation, are currently new treatments for depressive spectrum disorders.
Low-frequency transcranial magnetic stimulation has been proposed as an alternative treatment to electroconvulsive therapy for depression whose stimuli do not reach the seizure threshold.
In comparison with electroconvulsive therapy, this method of treatment has an important advantage: a more precise effect on those brain structures that are involved in the pathogenesis of depression (the hippocampal region). In addition, there are no cognitive impairments associated with ECT in TMS.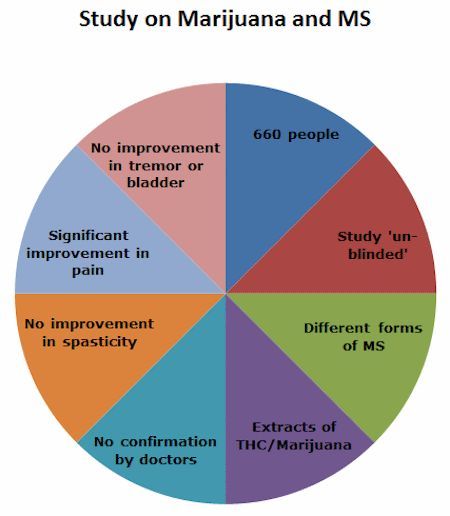 However, if the effect of TMS and ECT treatment is approximately equal in the treatment of mild or moderate depression, then in the case of severe depression, ECT may become a more preferable method (Grunhaus L., et al. 1998).
However, if the effect of TMS and ECT treatment is approximately equal in the treatment of mild or moderate depression, then in the case of severe depression, ECT may become a more preferable method (Grunhaus L., et al. 1998).
Studies have shown that TMS induces changes in beta-adrenergic receptors similar to those that occur after ECT and positively affects the astroglial tissue of the brain.
TMS has proven effective not only in the treatment of depression, but also in the treatment of schizophrenia, obsessive-compulsive disorders, post-traumatic stress disorder (George M., et al., 1999). However, it has been noted that the positive effect of TMS in the treatment of depression is observed in only 50% of cases. In addition, most patients had frequent relapses of depression after several months of remission following TMS. The combination of high-frequency and low-frequency magnetic stimulation is more preferable for the quality of remission and its duration.
From the point of view of the pathogenesis of depression, the method of cyclic transcranial magnetic stimulation seems promising, since weak magnetic fields can reduce circadian rhythms (Mosolov SN, 2002).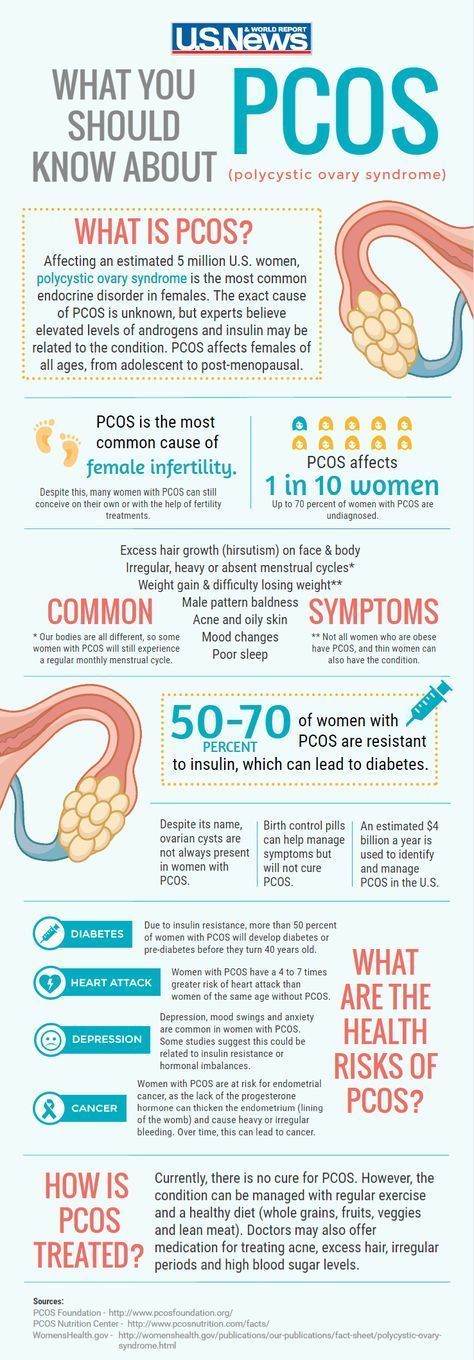 Currently, this method of therapy is used to overcome resistant depression.
Currently, this method of therapy is used to overcome resistant depression.
The first studies of TMS proved the advantage of fast stimulation over slow stimulation, however, the number of such studies was quite limited and the area of influence was not precisely localized. Recent studies show a higher efficiency of low-frequency magnetic stimulation compared to high-frequency (Klein E., et al., 1999).
Usually, magnetic stimulation is carried out according to the unilateral technique: on the projection of the left dorsolateral prefrontal area (high frequency or fast stimulation - < 10 Hz), stimulation of the right prefrontal area is less common. With low-frequency magnetic stimulation, a selective area of the anterolateral prefrontal cortex of the left hemisphere is affected.
The course of low-frequency magnetic stimulation for non-drug treatment of depression is 10 sessions, with an average duration of 30 minutes. Sessions are carried out every other day; stimulation parameters - 1.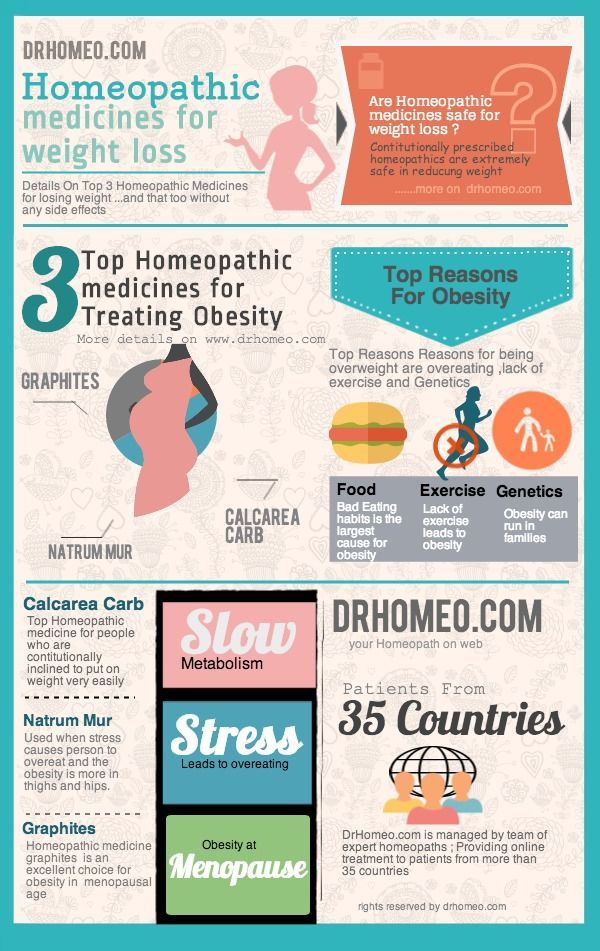 6 T/1 Hz. The therapeutic effect is noticeable after the first session of therapy and is most often manifested by calming, reducing the severity of anxiety, and restoring sleep. This method is of interest due to the development of a rapid effect and the absence of complications. As noted above, unlike ECT, TMS does not require the use of anesthesia.
6 T/1 Hz. The therapeutic effect is noticeable after the first session of therapy and is most often manifested by calming, reducing the severity of anxiety, and restoring sleep. This method is of interest due to the development of a rapid effect and the absence of complications. As noted above, unlike ECT, TMS does not require the use of anesthesia.
Vagus stimulation
Vagal stimulation for the non-drug treatment of depression was proposed in 1994 (Harden C., et al., 1994). During stimulation of the vagus, areas of the lateral and orbital regions of the anterior sections of the brain, as well as the parabrachial nuclei of the nerve and the region of the locus ceruleus are affected. The impact on the last part of the brain provides the influence of this method on the functional activity of the thalamus and hypothalamus.
After the application of vagal stimulation, an increase in the content of biogenic amines in the limbic region of the brain was noted (Ben-Menachem E. , et al., 1995)
, et al., 1995)
Sleep deprivation
A relatively benign non-pharmacological treatment for depression is sleep deprivation, which was actively developed in the early 1970s. Three types of sleep deprivation were used: total, partial, and selective. Total sleep deprivation means being awake for 36-40 hours, partial sleep deprivation - sleeping from 5 pm to 1 am, then awake until the next evening or sleeping from 9 pm to 1 hour 30 minutes, then awake until the next evening - sleep duration 4, 5 hours and selective sleep deprivation focused on selective deprivation of REM sleep only. Combination of total sleep deprivation with light therapy at night proved to be the most effective for treating depression with manifestations of melancholy. It should be noted that with complete sleep deprivation, lethargy and drowsiness are more common. In most cases, sleep deprivation is carried out after two days on the third, the therapeutic course includes an average of 5 sessions.
Sleep deprivation, both partial and complete, changes the structure of sleep, lengthens the latency period and reduces the duration of REM sleep (REM stages). As a rule, an improvement in mood in patients is observed after one sleepless night, however, this effect is usually short-lived and lasts about three days. Improvement in mood occurs gradually, expressed in the form of a feeling of general relief, a decrease in the feeling of lethargy, apathy, the disappearance of experiences of mental pain, bitterness.
As a rule, an improvement in mood in patients is observed after one sleepless night, however, this effect is usually short-lived and lasts about three days. Improvement in mood occurs gradually, expressed in the form of a feeling of general relief, a decrease in the feeling of lethargy, apathy, the disappearance of experiences of mental pain, bitterness.
In a prognostic sense, the ratio between the change in the mood of a depressed patient after the first and second sleepless nights is important.
The mechanism of the therapeutic effect of sleep deprivation is difficult to reduce to simple elimination of one of the sleep phases or resynchronization of a time-shifted circadian rhythm. Probably, one of the mechanisms for improving the condition of a patient with depression after sleep deprivation is the activation of adrenergic structures.
Treatment with light
Non-drug treatment of depression has been tried for more than twenty years with the help of light, counting on the normalization of human biological rhythms altered by the disease. Natural ways to treat depression include taking a temporary vacation in the winter to places where there are more daylight hours. In addition, prolonged exposure to the street on sunny days helps to get out of depression. Light therapy or phototherapy is most indicated for seasonal mood disorders, especially if episodes of exacerbation of depression occur in the winter or spring season. According to some authors, with a course of light therapy from three to fourteen days, the effectiveness of this method reaches 60-70%.
Natural ways to treat depression include taking a temporary vacation in the winter to places where there are more daylight hours. In addition, prolonged exposure to the street on sunny days helps to get out of depression. Light therapy or phototherapy is most indicated for seasonal mood disorders, especially if episodes of exacerbation of depression occur in the winter or spring season. According to some authors, with a course of light therapy from three to fourteen days, the effectiveness of this method reaches 60-70%.
It has been experimentally proven that the change in biological rhythms occurs when the patient is illuminated by a light source of increased intensity. Attempts have been made to prevent the seasonal exacerbation of affective psychosis by "lengthening the daytime period" with the help of artificial lighting and sleep deprivation.
It is assumed that bright and intense light has a multifaceted effect on the centers of circadian rhythms: suppression of the secretion of the pineal hormone melatonin, changes in the concentration of cortisol and adrenocorticotropic hormone, an increase in the synthesis of catecholamines, and normalization of the function of the vegetative system. Most experts associate the positive effect of light therapy with an increase in the regulatory function of the cerebral cortex, as well as with the normalization of the activity of the autonomic system.
Most experts associate the positive effect of light therapy with an increase in the regulatory function of the cerebral cortex, as well as with the normalization of the activity of the autonomic system.
In the course of treatment with light, the patient is daily, preferably in the morning, for several hours (less often half an hour) in a brightly lit room or next to an intense light source specially designed for this purpose.
Previously, it was believed that in order to obtain a therapeutic effect, the illumination of the room should be at least 2600 and not more than 8000 lux. Such illumination was achieved by using incandescent lamps located on the ceiling of the ward at a height of about 2.5 meters. Typically, about 30 200 W incandescent lamps were used. It was noted that the effectiveness of light treatment increases when the therapeutic room is painted white or green, as well as when the patient's body is exposed to the maximum (more than 25%).
Before starting light therapy, the patient is carefully examined, usually paying attention to the state of the autonomic system, indicators of the cardiovascular system.
Long therapy sessions were recommended - from 1.5 to 3 hours, with a total of 15 sessions, however, it was emphasized that these numbers, as well as the duration of the therapy session, should be determined based on the characteristics of the clinical picture of depression. 30 minute phototherapy sessions are currently recommended.
Some researchers advise light treatment at any time of the day, both daily and with breaks of two or three days. Phototherapy sessions are especially effective in the morning, immediately after waking up.
During a therapy session, patients who are only asked not to close their eyes can move freely around the room. To avoid getting used to the light once every 3 minutes. should be periodically watched for 1 sec. on lamps.
After a therapeutic session, there may be an increase in blood pressure, less often its decrease, probably due to the thermal effect, the body temperature usually rises. Quite often, patients report mild drowsiness. The change in the R-R interval on the ECG can be a reliable predictor of the effectiveness of light therapy. The therapeutic effect in some cases is possible both during the session and 2-3 days after its completion.
The change in the R-R interval on the ECG can be a reliable predictor of the effectiveness of light therapy. The therapeutic effect in some cases is possible both during the session and 2-3 days after its completion.
The most common complications of phototherapy are: insomnia, fatigue, irritability, headaches. These complications usually occur in people who try to work hard during light therapy.
It is interesting to note the sensitivity to light therapy of patients with manifestations of anxiety. To a lesser extent, patients with symptoms of melancholy and apathy respond to this type of therapy. Speaking about the mechanism of the therapeutic effect of this therapy, the thermal effect of light should be emphasized. Common contraindications to light therapy are oncological diseases and eye pathology.
Currently, special desktop and stationary devices have been developed for the non-drug treatment of depression with the help of light. Full-spectrum lamps are more efficient because they give light close to natural light.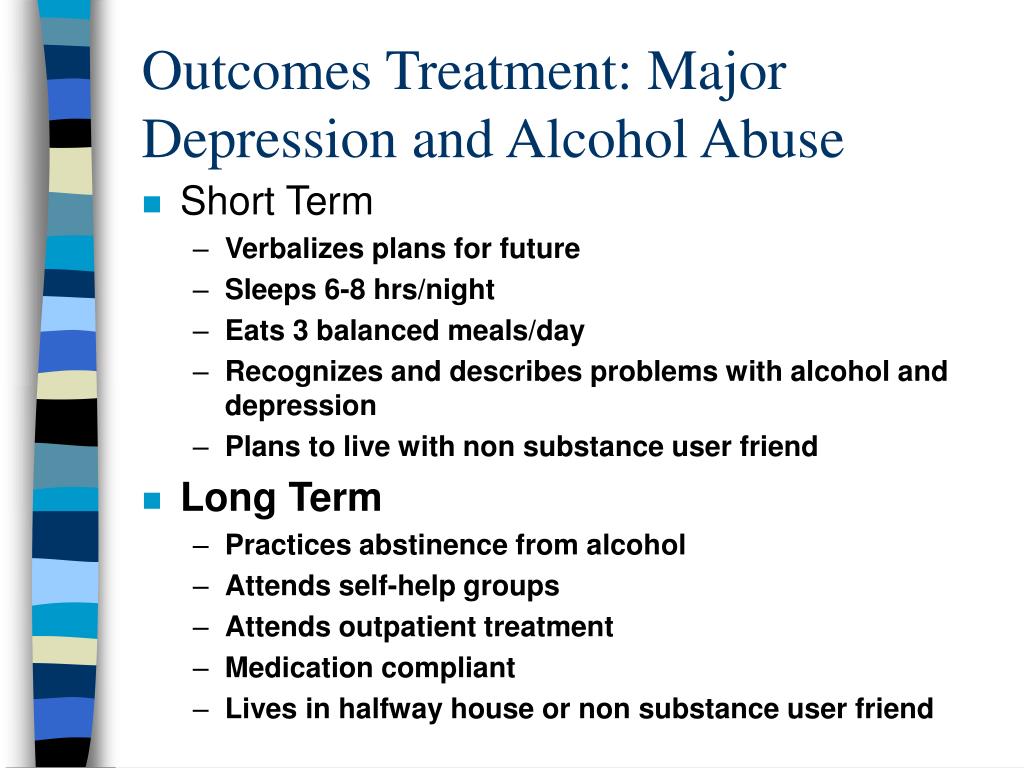 In order for the patient not to suffer from light treatment, special filters are used that block ultraviolet rays and thereby protect the patient's retina from intense radiation (cataract prevention).
In order for the patient not to suffer from light treatment, special filters are used that block ultraviolet rays and thereby protect the patient's retina from intense radiation (cataract prevention).
Recent studies have shown that the effectiveness of light exposure is determined by three characteristics: intensity, spectrum and exposure time. In connection with the above, methods of phototherapy are being developed with the enrichment of the light flux with long-wave ultraviolet radiation, which has a biologically active effect. This technique involves the use of a full spectrum light source, as it approximates natural light as much as possible.
The modern achievements of phototherapy include "artificial dawn" (a special electric lamp at the patient's bedside, which intensifies its illumination before dawn).
Biofeedback
Non-pharmacological methods of treatment should also include biofeedback, which by and large refers to psychotherapeutic methods for the treatment of depression.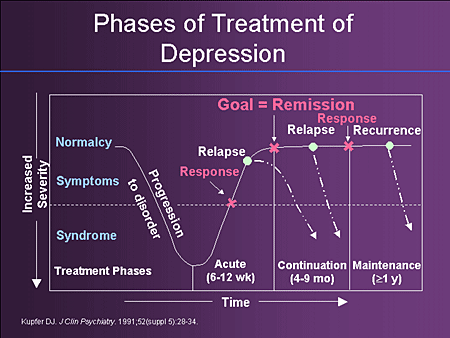 To carry out this method of treatment, special psychophysiological equipment is used, which implies the possibility of polygraphic recording of various psychophysiological indicators: bioelectrical activity of the brain, muscles, heart, galvanic skin reaction, etc. 20-25 sessions of therapy based on the use of biofeedback and aimed at increasing power of alpha waves in the left occipital region. Most patients have a 50% reduction in the severity of depressive symptoms.
To carry out this method of treatment, special psychophysiological equipment is used, which implies the possibility of polygraphic recording of various psychophysiological indicators: bioelectrical activity of the brain, muscles, heart, galvanic skin reaction, etc. 20-25 sessions of therapy based on the use of biofeedback and aimed at increasing power of alpha waves in the left occipital region. Most patients have a 50% reduction in the severity of depressive symptoms.
Therapeutic massage and breathing exercises
Auxiliary methods of treating depression include breathing exercises, therapeutic massage (especially if the onset of depression is provoked by mental trauma) and meditation.
Such breathing is useful on the seashore, in a pine forest, because such breathing increases the amount of oxygen. Massage is usually carried out for 30 minutes and its therapeutic effect is associated with a decrease in the content of stress hormones in the blood. In addition, massage relieves internal tension and normalizes sleep.
Homeopathy
From the point of view of homeopathy, an alternative medical system based on the principle of "like can be healed by like" and using microdoses of medicines, homeopathy can cure depression, however, there is no scientific confirmation of the effectiveness of this non-drug method of treatment. A variant of a homeopathic treatment for depression is the use of flower remedies.
Phytotherapy
St. John's wort (Negrustin) is used as a natural remedy for the treatment of depression, however, their effect in the treatment of depression is very insignificant. S-adenosyl-L-methionine (SAM-e) is undergoing clinical trials.
Dietary nutrition
The effectiveness of dietary nutrition as a non-drug treatment for depression is also not supported by scientific studies. However, it is generally accepted that the diet of a depressed patient must necessarily include complex carbohydrates, which naturally increase the production of serotonin by neurons in the brain, the deficiency of which during depression (especially with anxiety symptoms) is well known.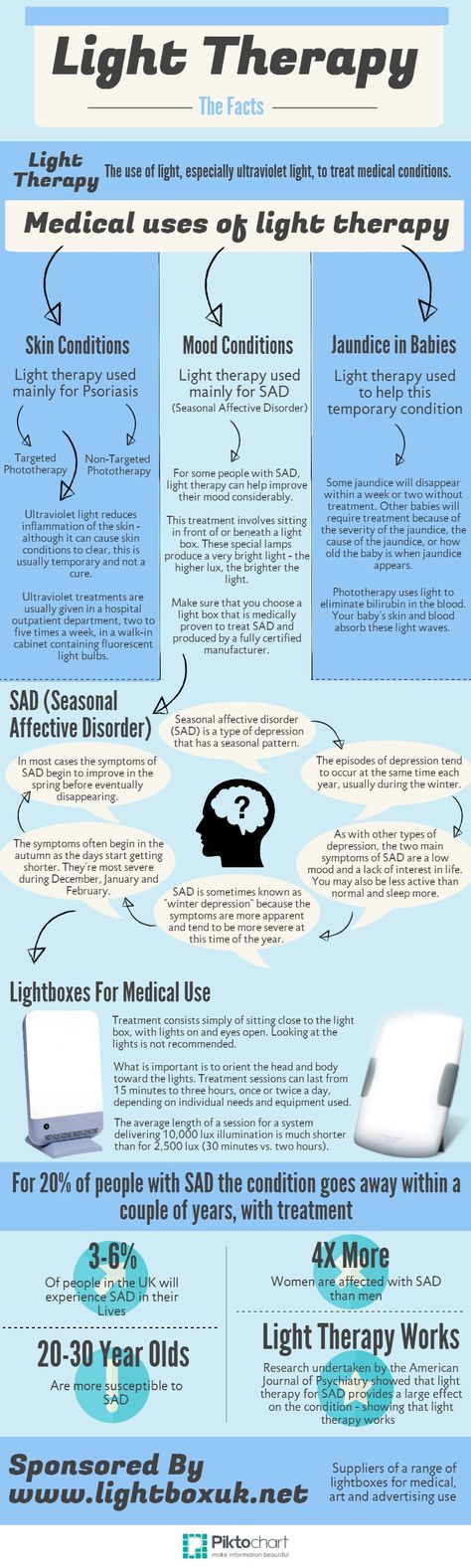 Complex carbohydrates are found in legumes and whole grains. An increase in the production of norepinephrine and dopamine - neurotransmitters, the concentration of which is reduced in depression with symptoms of apathy, is promoted by a diet high in protein (beef, poultry, fish, nuts, eggs). At the same time, there is an opposite point of view about the inadmissibility of high protein content in food, which should be consumed in case of depression. It is recommended to exclude sugar, alcohol, caffeine, convenience foods and canned food. Foods with a high content of saturated fatty acids are undesirable.
Complex carbohydrates are found in legumes and whole grains. An increase in the production of norepinephrine and dopamine - neurotransmitters, the concentration of which is reduced in depression with symptoms of apathy, is promoted by a diet high in protein (beef, poultry, fish, nuts, eggs). At the same time, there is an opposite point of view about the inadmissibility of high protein content in food, which should be consumed in case of depression. It is recommended to exclude sugar, alcohol, caffeine, convenience foods and canned food. Foods with a high content of saturated fatty acids are undesirable.
Back to Table of Contents
Non-Drug Treatment for Depression | Psychosoma
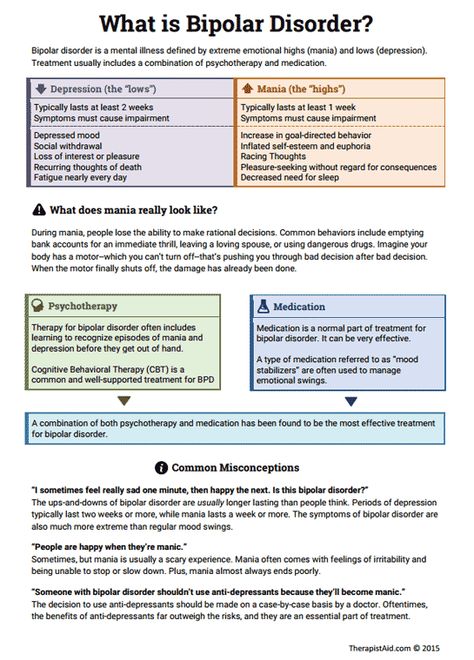
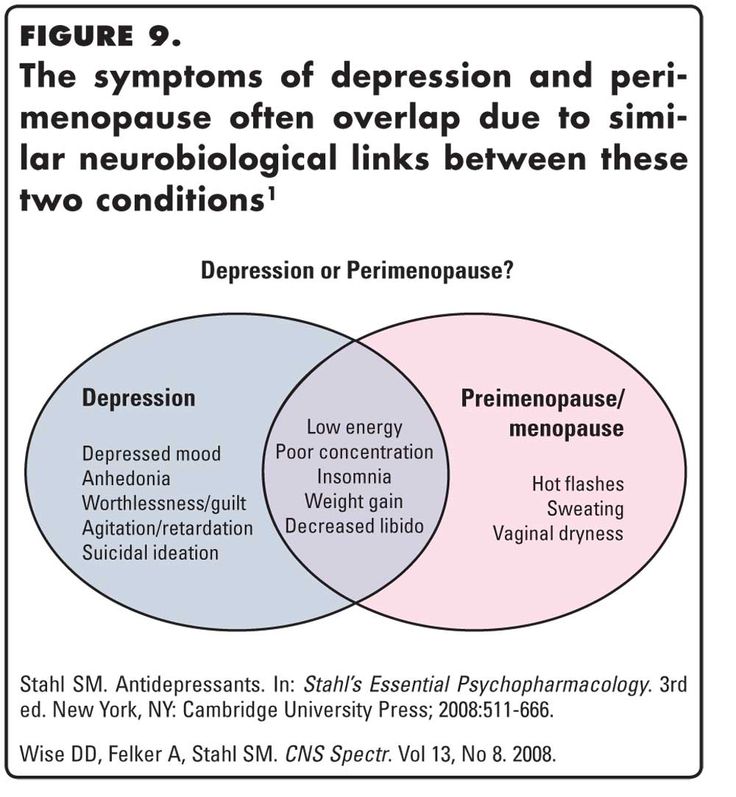
Depression is a decrease in mood, depression of mental activity and motor activity.
Depression can be not only an independent disease (endogenous), a reaction of adaptation to a traumatic situation (psychogenic), but also a syndrome that is observed in various mental illnesses (endogenous depression is an independent mental illness caused by hereditary factors and specific neurotransmitter disorders, psychogenic - due to negative life circumstances, the depressive phase in bipolar affective disorder as a stage in the course of the disease).
Treatment of depression without pills: truth or myth?
In addition to standard methods of treatment (pharmacotherapy), there are also non-drug methods of influence. They are less common, but they have their place in the treatment of adaptation reactions, unexpressed subdepressive states. Also, these techniques are used in combination with medications in the treatment of severe and prolonged depression, which are difficult to treat with medication.
Sleep deprivation
Sleep deprivation is a special treatment for depression. Even in the era of Antiquity, it was noted that after a sleepless night, an oppressed person again became sociable and cheerful. And in the 70s of the last century, the Swiss psychiatrist Walter Schulte discovered the healing properties of sleep deprivation.
The essence of the technique is that a person should not sleep for a day. He spends his day as usual and then stays up in bed, staying awake all night. At the same time, it is not recommended to take psychostimulants, caffeine or energy drinks. It is important to combine passive and active activity. That is, spending the whole night in front of a TV or a book is highly undesirable. You need to do physical exercises or walks.
At the same time, it is not recommended to take psychostimulants, caffeine or energy drinks. It is important to combine passive and active activity. That is, spending the whole night in front of a TV or a book is highly undesirable. You need to do physical exercises or walks.
The next day the person is also awake. He may have episodes of drowsiness, which must be dealt with through physical activity. Then the patient goes to bed. Thus, a patient with depression is in an active state for 36-38 hours, that is, one and a half days. The effect, as a rule, is observed immediately, but it is short-lived. Therefore, 7-8 sessions of sleep deprivation are carried out twice a week, after which they can be reduced to once. The method is effective in the treatment of depression, both endogenous and psychogenic.
Some people find it difficult to understand the paradox of curing depression by additional exhaustion of the body through insomnia. Indeed, with a prolonged lack of sleep, a person may experience symptoms of psychosis: delirium, hallucinations, illusions, etc. As you know, this method was used during the Inquisition and World War II to exhaust prisoners or interrogate criminals. However, psychotic symptoms occur with persistent sleep deprivation. Here, deprivation is carried out periodically, the emphasis is on the cyclicity and normalization of the daily routine.
As you know, this method was used during the Inquisition and World War II to exhaust prisoners or interrogate criminals. However, psychotic symptoms occur with persistent sleep deprivation. Here, deprivation is carried out periodically, the emphasis is on the cyclicity and normalization of the daily routine.
Lack of sleep is recognized by our neuroendocrine system as an existential threat, on par with hunger, hypothermia, injury, and so on. A stressful situation stimulates the production of adrenaline and cortisol by the adrenal glands. The first produces a quick effect, the second - a long one. An increase in their concentration leads to an activation of the body's forces: motor and mental activity accelerates, mood rises (up to euphoria), vascular tone and blood pressure increase, metabolic reserves are activated (gluconeogenesis is triggered - the production of glucose from fats and amino acids). It also normalizes the production of serotonin, the hormone responsible for mood. At the same time, physical activity complements the effectiveness of sleep deprivation.
At the same time, physical activity complements the effectiveness of sleep deprivation.
A similar effect was described by the Austrian psychiatrist W. Frankl during his stay in a concentration camp. He noted that people suffering from neuroses before the war were cured of disorders while in captivity, where they were subjected to inhuman conditions of life. A stressful situation changes the neurotransmitter processes that exist in depression.
Naturally, many would want to treat depression without drugs. However, sleep deprivation has its limitations. People suffering from arterial hypertension, diabetes mellitus, renal failure, oncological pathology and other severe somatic diseases, such treatment is contraindicated.
Non-drug treatment for depression: phototherapy (light therapy)
Phototherapy (light therapy) is a technique , based on regular exposure of the patient to sunlight or artificial light.
This method was originally used to treat seasonal depression.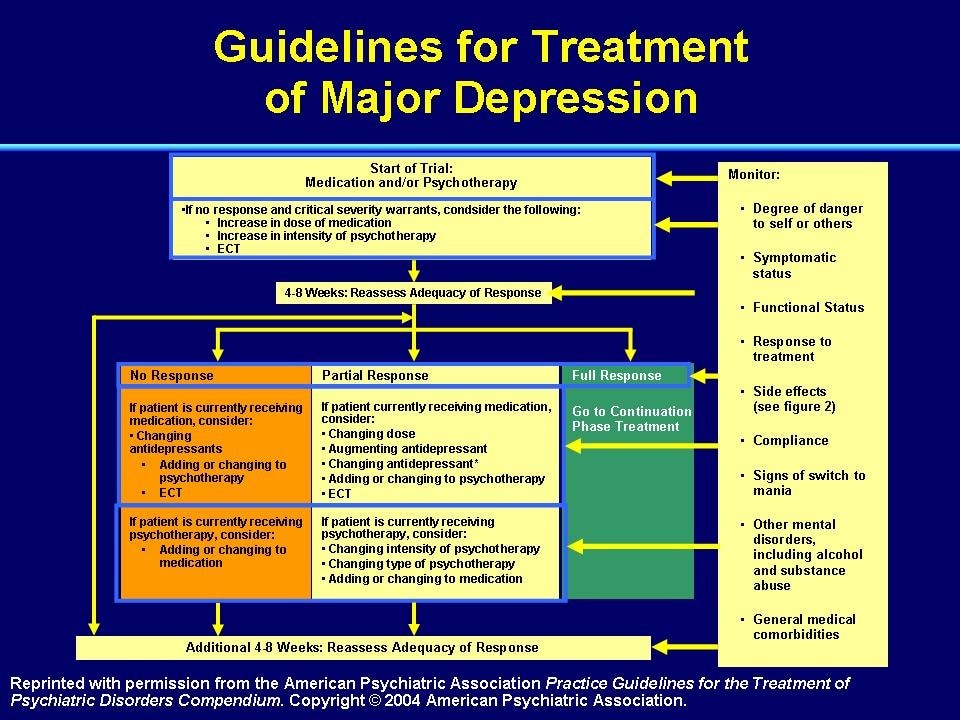 In autumn and winter, the amount of the sleep hormone, melatonin, increases in the human body. It is derived from serotonin (the feel-good hormone). Quantitative fluctuations of both hormones are interconnected. The high content of melatonin inhibits the production of serotonin. In those patients who suffer from a depressive disorder, this provokes the onset of a seasonal exacerbation. Mood and efficiency fall, anxiety and melancholy appear. Regular exposure to light reduces the amount of melatonin in the blood and stimulates the body, respectively, the symptoms of depression are leveled. This has been proven in a study by Lee and Chan 1999 years.
In autumn and winter, the amount of the sleep hormone, melatonin, increases in the human body. It is derived from serotonin (the feel-good hormone). Quantitative fluctuations of both hormones are interconnected. The high content of melatonin inhibits the production of serotonin. In those patients who suffer from a depressive disorder, this provokes the onset of a seasonal exacerbation. Mood and efficiency fall, anxiety and melancholy appear. Regular exposure to light reduces the amount of melatonin in the blood and stimulates the body, respectively, the symptoms of depression are leveled. This has been proven in a study by Lee and Chan 1999 years.
However, phototherapy is not used as an independent method, but in combination with antidepressants. Their combined effect produces the best effect.
Properly use white fluorescent illuminators for the procedure. Each morning, the patient should sit in front of a 10,000 lux light source for 30-40 minutes for 2-3 weeks. With less illumination (2500 lux), the duration of the procedure can be increased up to 2 hours (Lam and Levitt 1999).