Mothers with mental illness
Parenting with a Mental Health Condition
Be the Best Parent You Can Be
Mental health conditions can affect any person regardless of gender, age, health status and income, and that includes people who have or want to have children of their own. Parenting is both greatly rewarding and a daunting task for anyone, but it poses some particular challenges for people with a mental health condition. Here, you will find information about parenting and mental illness, where to go to get help for you and your family, and how to support yourself and your children.
Everyone can improve on their parenting skills. Consider taking a parenting class to learn the basics and lessen the anxiety of being a parent. Parentingwell.org is a web site especially for parents with mental illness. It includes an online community, tips and tools and other resources. For perspective on all of the roles being a parent entails, visit the Parenting section of the Temple University Collaborative on Community Inclusion website.
My Mental Illness and My ChildMy Child's Mental HealthTalking to My ChildCaring for ChildrenCould I Lose My Child? Legal IssuesKeeping Families Intact
What impact does a parent's mental illness have on children?
The effect of a parent's mental illness on children is varied and unpredictable.[1] Although parental mental illness poses biological, psychosocial and environmental risks for children, not all children will be negatively affected, or affected in the same way. The fact that a parent has mental illness alone is not sufficient to cause problems for the child and family. Rather, it is how the mental health condition affects the parent's behavior as well as familial relationships that may cause risk to a child. The age of onset, severity and duration of the parent's mental illness, the degree of stress in the family resulting from the illness, and most importantly, the extent to which parents' symptoms interfere with positive parenting, such as their ability to show interest in their children, will determine the level of risk to a child. The child's age and stage of development is also important.
The child's age and stage of development is also important.
Will my child have a mental health condition as well?
Mental health conditions are not contagious, but research shows that some mental health conditions may have a genetic link. Bipolar disorder, for example, has long been shown to run in families. Other people may pass on hereditary traits that make a mental health disorder more likely without passing on a specific disorder.
Because you have a mental health condition does not mean that your child will have a mental health condition. But because of your own experiences, it may help you be better attuned to the psychological challenges that parenting can bring.
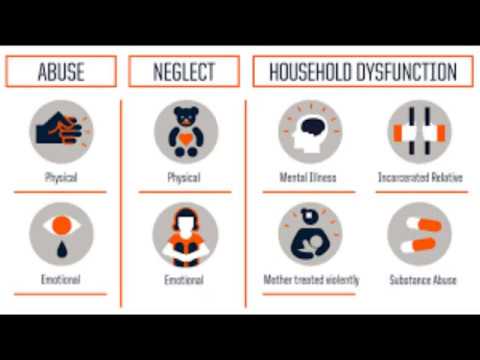
Risk Factors
Children whose parents have a mental illness are at risk for developing social, emotional and/or behavioral problems. An inconsistent and unpredictable family environment, often found in families in which a parent has mental illness, contributes to a child's risk. Other factors that place all children at risk, but particularly increase the vulnerability of children whose parents have a mental illness, include:
- Poverty
- Occupational or marital difficulties
- Poor parent-child communication
- Parent's co-occurring substance abuse disorder
- Openly aggressive or hostile behavior by a parent
- Single-parent families
Families at greatest risk are those in which mental illness, a child with their own difficulties, and chronically stressful family environments are all present. Many of these factors, however, can be reduced through preventive interventions. For example, poor parent-child communication can be improved through skills training, and marital conflict can be reduced through couple's therapy.
Many of these factors, however, can be reduced through preventive interventions. For example, poor parent-child communication can be improved through skills training, and marital conflict can be reduced through couple's therapy.
The Prevention Perspective
Whether or not children of parents with mental illness will develop social, emotional, or behavioral problems depends on a number of factors. These include the child's genetic vulnerability, the parent's behavior, the child's understanding of the parent's illness, and the degree of family stability (for example, the number of parent-child separations). Preventive interventions aimed at addressing risk factors and increasing children's protective factors increase the likelihood that they will be resilient, and grow and develop in positive ways. Effective prevention strategies help increase family stability, strengthen parents' ability to meet their children's needs, and minimize children's exposure to negative manifestations of their parent's illness. [2]
[2]
Protective Factors
Increasing a child's protective factors helps develop his or her resiliency. Resilient children understand that they are not responsible for their parent's difficulties, and are able to move forward in the face of life's challenges. It is always important to consider the age and stage of development when supporting children. Protective factors for children include:
- A parent's warm and supportive relationship with his or her children
- Help and support from immediate and extended family members
- A sense of being loved by their parent
- Positive self-esteem
- Good coping skills
- Positive peer relationships
- Interest in and success at school
- Healthy engagement with adults outside the home
- An ability to articulate their feelings
- Parents who are functioning well at home, at work, and in their social relationships
- Parental employment
References:
1. Joanne Nicholson, Elaine Sweeny, and Jeffrey Geller. Mothers With Mental Illness: I. The Competing Demands of Parenting and Living With Mental Illness. Psychiatric Services. May 1998. Vol. 49. No. 5.
Joanne Nicholson, Elaine Sweeny, and Jeffrey Geller. Mothers With Mental Illness: I. The Competing Demands of Parenting and Living With Mental Illness. Psychiatric Services. May 1998. Vol. 49. No. 5.
2. Ibid.
How do I talk to my child about my mental health condition?
How you talk to your child about your mental health condition will depend on the age and maturity of your child and your willingness to open up to him or her.
In general, children, especially as they grow older, are very astute and knowledgeable about their surroundings. They can sense emotional changes and can often tell if something is hidden from them without their knowledge. Some children may be able to fully understand what it means to have a mental health condition. In talking with children you can help them to know how to cope when you are not feeling well. And, a child may be able to support you in your recovery by reminding you when to take your medications or help you stay on track.
Your decision to talk to your child about your condition should also take into account your readiness. Parents often want to appear invincible and strong to their children, as they think it is the parents' role to care for a sick child and not the other way around. The decisions you make should be made with both parent and child in mind.
Before proceeding, you should always talk to your doctor or therapist about the best ways to bring this information up. You may want to consider the possibility of inviting a child to a session to explore this information.
What can I expect from my child?
Your child might experience some of these feelings:
- Anger - Your child may be angry at you for having a mental health condition. The child may think that it was your fault that you had a mental health condition and that it is your fault that they will experience a harder life. Your child might also be angry at external forces, such as a higher power or the world, for unfairly hurting you or your family.
 Your child may also be angry at him or herself. If you notice anger problems in your child, you should talk to your therapist or doctor about arranging for your child to join in sessions.
Your child may also be angry at him or herself. If you notice anger problems in your child, you should talk to your therapist or doctor about arranging for your child to join in sessions. - Fear - Your child might be scared about what the future will bring. Your child might be afraid about how your mental health condition will change your relationship. They might be afraid about your ability to take care of them. Your child may also be scared about what others will think if they found out that you have a mental health condition. Sit down and talk to your child about these issues, reassure them you still love them.
- Guilt - Your child may blame himself or herself for your mental health condition, especially in cases or anxiety or depression. Your child may express guilt by taking over an inordinate amount of household duties. Your child may try and hide his or her own problems so as not to make your life any worse.
- Shame - Despite efforts to educate the public about mental illness, mental illness is still often a stigmatized and misunderstood condition.
 Your child might be embarrassed. He or she might think that your condition will have negative impacts on his or her social life and might be worried.
Your child might be embarrassed. He or she might think that your condition will have negative impacts on his or her social life and might be worried. - Sadness - Children can become very sad when they learn that a loved one, especially a parent, is hurt or sick. You should talk to your doctor about ways to cope with sadness and ways to know when sadness becomes depression.
- Anxiety - Your child may become overanxious or worried about you if he or she learns that you have a mental health condition. These children tend to be overly helpful and may miss out on their own lives.
- Relief - For some children, learning that you have a mental health condition might be a relief. It might help explain behaviors or incidents that they experienced that they previously could not understand.
- Supportiveness - Your child may be very supportive of your mental health, regardless of his or her previous attitudes toward mental illness.
 Often, having mental illness in a family can change someone's orientation toward mental illness.
Often, having mental illness in a family can change someone's orientation toward mental illness.
How can I care for a child while caring for myself?
In addition to being a parent, you are also a person of your own. Your recovery plans and activities should always include time for yourself that is relaxing and beneficial.
If you have a crisis action plan or a psychiatric advance directive, you should designate someone to help with your parenting duties. If your child is old enough, you should discuss your plan with your child and identify resources and options together for handling things when you are not well.
Could I lose my child because I have a mental health condition?
A higher proportion of parents with serious mental illness lose custody of their children than parents without mental illness. There are many reasons why parents with a mental illness risk losing custody, including the stresses their families undergo, the impact on their ability to parent, economic hardship, and the attitudes of mental health providers, social workers and the child protective system.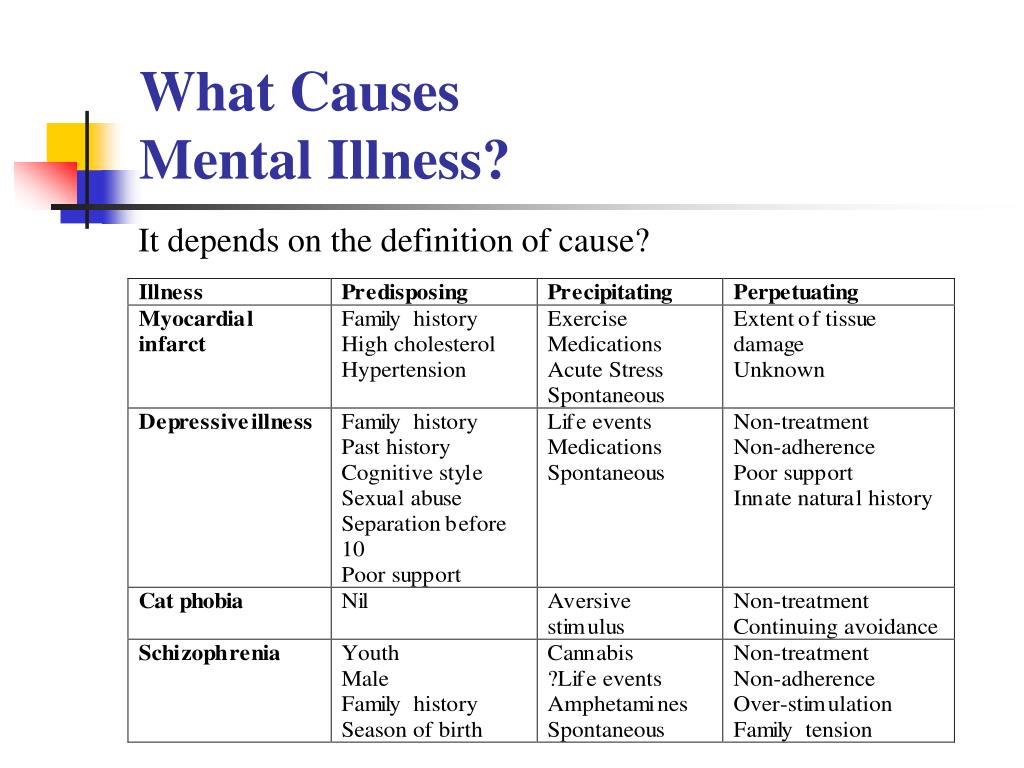 Supporting a family where mental illness is present takes extra resources that may not be available or may not be offered. Also, a few state laws cite mental illness as a condition that can lead to loss of custody or parental rights. One unfortunate result is that parents with mental illness might avoid seeking mental health services for fear of losing custody of their children. Studies that have investigated this issue report that:
Supporting a family where mental illness is present takes extra resources that may not be available or may not be offered. Also, a few state laws cite mental illness as a condition that can lead to loss of custody or parental rights. One unfortunate result is that parents with mental illness might avoid seeking mental health services for fear of losing custody of their children. Studies that have investigated this issue report that:
- Only one-third of children with a parent who has a serious mental illness are being raised by that parent.
- In New York, 16 percent of the families involved in the foster care system and 21 percent of those receiving family preservation services include a parent with a mental illness.
- Grandparents and other relatives are the most frequent caregivers if a parent is psychiatrically hospitalized, however other possible placements include voluntary or involuntary placement in foster care.[1]
The major reason states take away custody from parents with mental illness is the severity of the illness, and the absence of other competent adults in the home. [2] Although mental disability alone is insufficient to establish parental unfitness, some symptoms of mental illness, such as disorientation and adverse side effects from psychiatric medications, may demonstrate parental unfitness. A research study found that nearly 25 percent of caseworkers had filed reports of suspected child abuse or neglect concerning their clients.[3]
[2] Although mental disability alone is insufficient to establish parental unfitness, some symptoms of mental illness, such as disorientation and adverse side effects from psychiatric medications, may demonstrate parental unfitness. A research study found that nearly 25 percent of caseworkers had filed reports of suspected child abuse or neglect concerning their clients.[3]
The loss of custody can be traumatic for a parent and can exacerbate their illness, making it more difficult for them to regain custody. If mental illness prevents a parent from protecting their child from harmful situations, the likelihood of losing custody is drastically increased.
Legal Issues
All people have the right to bear and raise children without government interference. However, this is not a guaranteed right. Governments may intervene in family life in order to protect children from abuse or neglect, imminent danger or perceived imminent danger. When parents are not able, either alone or with support, to provide the necessary care and protection for their child, the state may remove the child from the home and provide substitute care.
Adoption and Safe Families Act
The Federal Adoption and Safe Families Act, Public Law 105-89 (ASFA) was signed into law November 19, 1997. This legislation is the first substantive change in federal child welfare law since the Adoption Assistance and Child Welfare Act of 1980, Public Law 96-272.4 It is intended to achieve a balance of safety, well-being and permanency for children in foster care. It requires that state child welfare agencies make "reasonable efforts" to prevent the unnecessary placement of children in foster care and to provide services necessary to reunify children in foster care with their families. ASFA establishes expedited timelines for determining whether children who enter foster care can be moved into permanent homes promptly-their own familial home, a relative's home, adoptive home, or other planned permanent living arrangement.
While ASFA is designed to protect children, it also includes provisions pertaining to parental rights. For example, under ASFA, parents have the right to receive supports and services to help them retain custody and keep their families intact.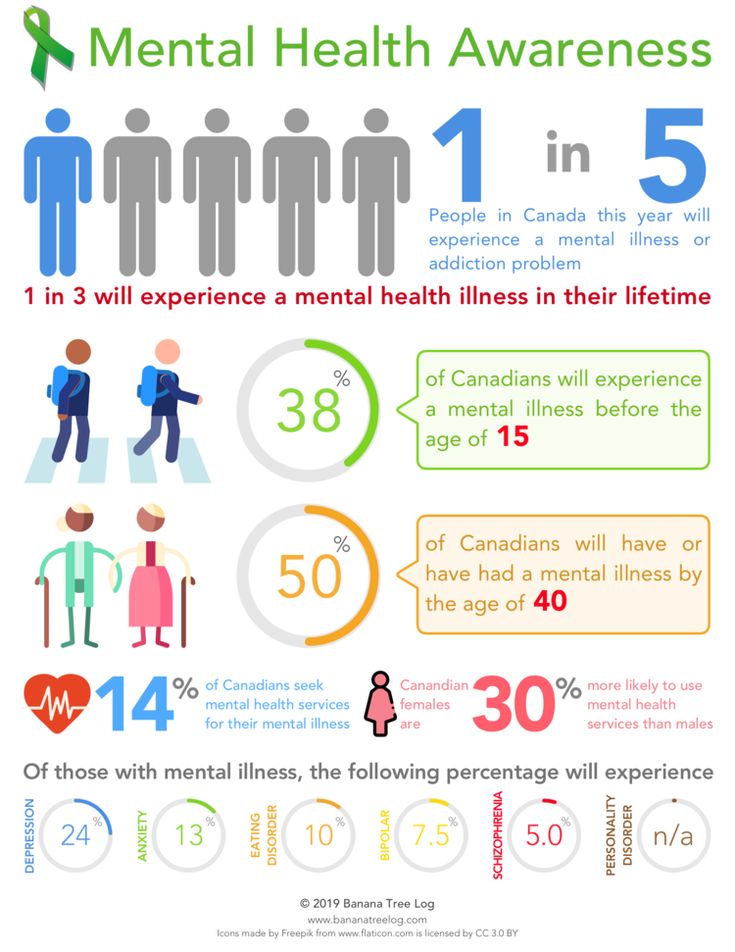 The child welfare system must provide these services according to an individualized plan that has been developed and agreed upon by all parties to ensure parents with mental illnesses are not discriminated against due to their illness. A plan with parental input also helps ensure that, when appropriate, efforts are made by state welfare agencies to promote family permanency, including establishing whether children in foster care can be moved into a permanent living situation.
The child welfare system must provide these services according to an individualized plan that has been developed and agreed upon by all parties to ensure parents with mental illnesses are not discriminated against due to their illness. A plan with parental input also helps ensure that, when appropriate, efforts are made by state welfare agencies to promote family permanency, including establishing whether children in foster care can be moved into a permanent living situation.
Helping Families Stay Intact
Parental mental illness alone can cause strain on a family; parental mental illness combined with parental custody fears can cause even greater strain. Such strain, as well as the lack of specialized services for families in the child welfare system and the overall stigma associated with mental illness, makes it difficult for families to get the help they need. With the right services and supports though, many families can stay together and thrive. The following efforts by advocates can help families living with mental illness maintain custody and stay intact:
- Help parents become educated about their rights and obtain legal assistance and information.

- Advocate for parents as services plans are developed, and assist adult consumers to develop their own self-care plans and advance directives to strengthen their parenting skills and manage their own illness.
- Enable parent-child visitation during psychiatric hospitalization to maintain the bond between parent and child.
- Train child protective services workers to better understand parental mental illness.
- Educate the legal system about advances in the treatment of serious mental illness.
- Advocate for increased specialized services for parents with serious mental illnesses available through the court system.
References:
1. Network practical tools for changing environment. Making the Invisible Visible: Parents with Psychiatric Disabilities. National Technical Assistance Center for State Mental Health Planning. Special Issue Parents with Psychiatric Disabilities. Spring, 2000.
2. Roberta Sands. "The Parenting Experience of Low-Income Single Women with Serious Mental Disorders. Families in Society." The Journal of Contemporary Human Services. 76 (2), 86-89. 1995.
Families in Society." The Journal of Contemporary Human Services. 76 (2), 86-89. 1995.
3. Joanne Nicholson, Elaine Sweeny, and Jeffrey Geller. Mothers With Mental Illness: II. Family Relationships and the Context of Parenting. May 1998. Vol. 49. No. 5.
4. Ibid.
Page Not Found | Mental Health America
- Quick Facts and Statistics
- Mental Health Conditions
- MHA Programs
- News
- Policy Issues
- Research and Reports
- Webinars
- Podcast
- Blog
- The B4Stage4 Philosophy
- Staying Mentally Healthy
- Recovery & Support
- Tools for Mental Wellness
- Get Screened
- Find a Warmline
- Crisis Resources
- Find Help For Myself
- Find Help For Someone Else
- Types of Mental Health Treatments
- Types of Mental Health Professionals
- How Insurance Works
- What To Expect
- Find MHA In Your Area
- FAQs
- Current Legislation
- Position Statements
- Advocacy Network
- Action Alerts
- The State of Mental Health in America
- Regional Policy Council
- Hill Day
- Give
- Shop
- Advocate
- Attend an Event
- Partner with Us
- Share What #mentalillnessfeelslike
- Take an action alert
- Get Your Workplace Bell Seal Certified
- Give Monthly
- Give cryptocurrency
- Memorial Gifts
- Fundraise
- Clifford Beers Society
- Planned Giving
- Bequests
- Other Ways to Give
Search
We’re so sorry; this page doesn’t appear to be working.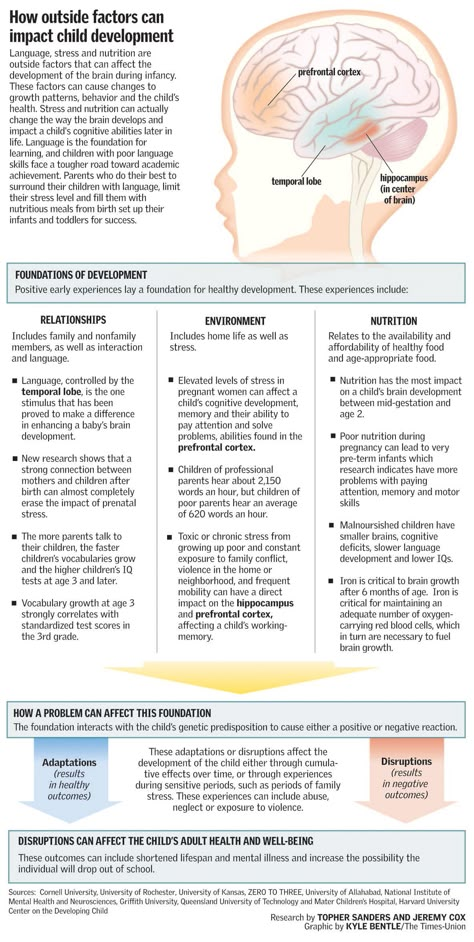
We recently launched a new website at www.mhanational.org. While this is an exciting update for us, it can cause issues for some of our users who are trying to find our content. We tried to fix as many links as possible, but we may have missed some.
Let us try to help you get to where you’re going:
-
Try using our search function at the top of the screen and type in keywords.
-
You can also try some of our more popular features:
-
Fact sheets on mental health conditions and topics are here
-
Our programs, including Mental Health Month, can be found here
-
Get quick access to our policy information here
-
And MHAScreening.org still provides free, confidential, anonymous screens here
-
And if it isn’t too much trouble, please email us and let us know where you were trying to go.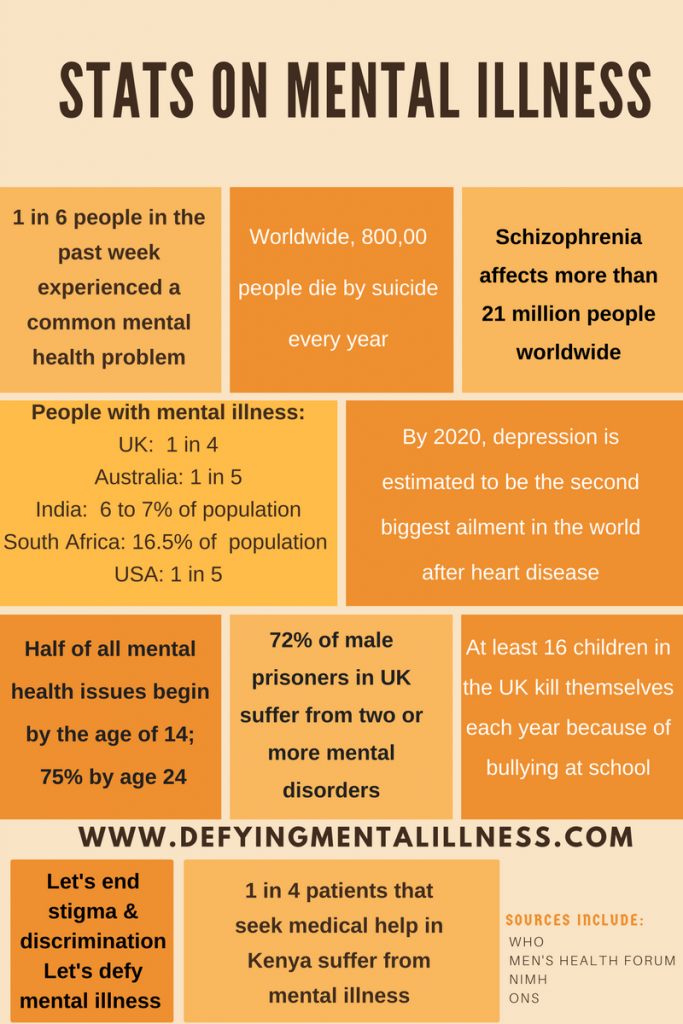 We can get that fixed so it won’t be a problem next time!
We can get that fixed so it won’t be a problem next time!
Thank you so much for your patience with us as we continue to deliver up-to-date modern information and resources on mental health.
Yours in mental health,
The Mental Health America (MHA National) Team
© Copyright 2023 Mental Health America, Inc.
"Why would you give birth." Can women with mental disorders raise children? More often, women do not develop acute postpartum psychosis, but a depressive disorder, said Natalia Treushnikova, President of the Mental Health Union.
“It is worth paying attention to, first of all, to relatives. The woman is very tired, she becomes more tearful, complains of insomnia.
Acute psychotic disorder is difficult to miss, because the patient is clearly agitated, inadequate. And lethargy and apathy are often attributed to a change in the rhythm of life. But this is what leads to depression, and in this state, women can harm the child, ”the expert emphasized.
According to her, a doctor should assess the patient's ability to raise a child. He will find out in what form her disease proceeds and in what condition she is. If the disorder is successfully treated with medication, the woman will be able to perform parental duties, severe or non-remission disease requires hospitalization.
“In this respect, chronic mental disorders do not differ from chronic somatic ones. For example, if a mother has severe diabetes mellitus, we understand that this threatens the life and health of herself and her child no less than a mental illness,” Treushnikova argues.
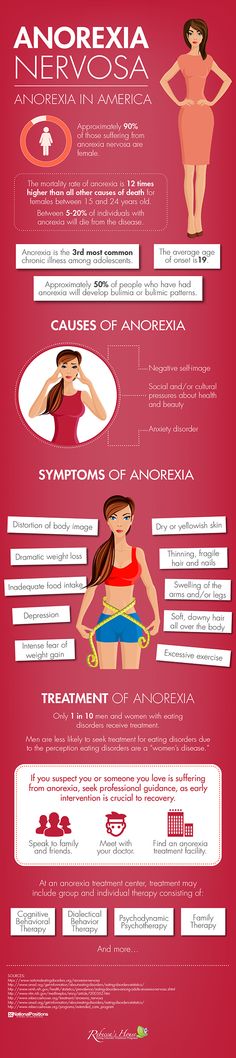
If the mother suffers from some kind of neurotic disorder, such as depression, anxiety, chronic fatigue syndrome, asthenic or obsessive-compulsive disorder, as a rule, she does not lose control over her behavior and fits into the socially acceptable framework of functioning, explained psychiatrist Mikhail Tetyushkin. However, this will create a certain algorithm for the functioning of the psyche, which can have a negative impact on the health of the child.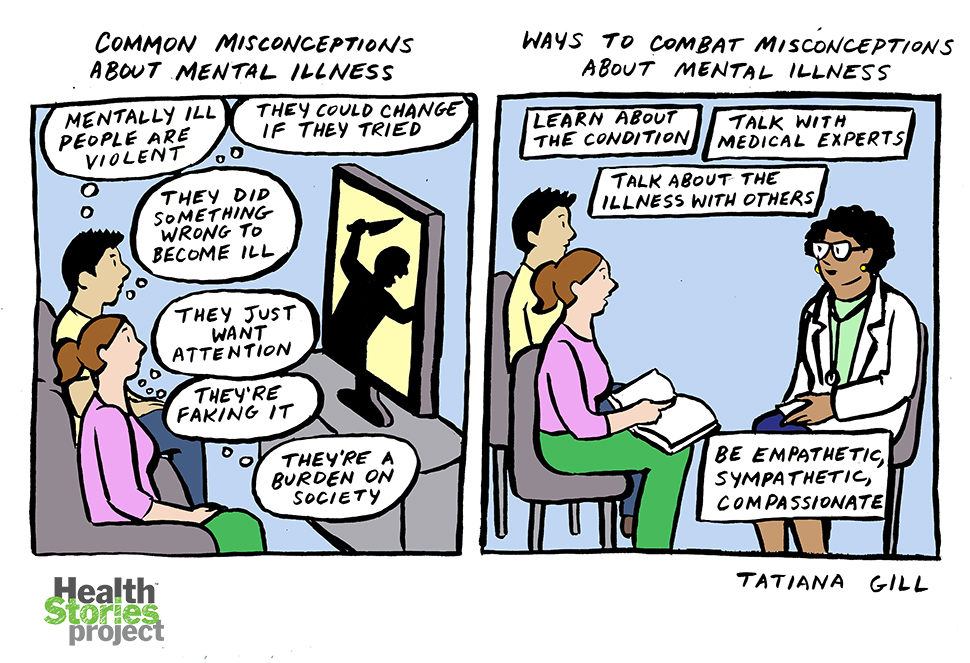
Speaking about mental illnesses in women who have recently given birth, the doctor emphasized that they can develop without being tied to any events or experiences. In pregnant patients and new mothers, psychoses are associated with weakness of the nervous system and past traumatic experiences (suicide attempts, eating disorders, and others).
It is often difficult to make such a diagnosis and motivate a woman to seek help, because in society, mood swings and emotional fluctuations in women during pregnancy and childbirth are considered the norm.
“It is important to look at how painful the reactions of the psyche that appeared after childbirth are and how much they harmonize with the general state of the person. If they fit into the usual system of reactions (a woman is very temperamental in principle), it is logical that during pregnancy she will experience a flurry of emotions. If emotionality is dulled, cardinal changes in behavior appear, this is a reason for contacting a psychiatrist or even hospitalization, ”Tetyushkin explained.
“Children are hostages of the situation”
According to the law, it is impossible to deprive a parent of the rights to a child only on the basis of the presence of a mental illness, the decision is made on the basis of Article No. 69 of the Family Code of the Russian Federation. For example, if a mother suffers from alcoholism or drug addiction, or, having a mental disorder, commits a crime against the life or health of her children or another family member, she may be deprived of her rights.
If there are reports of incidents or suspicious behavior in the family, the guardianship authorities conduct an inspection, said Yulia Zimova, deputy chairman of the commission of the Civic Chamber of the Russian Federation on demography, protection of the family and children. If the actions of the mother pose a threat to the minor, he moves to a shelter or to relatives. After that, a court passes, which can restrict the parent's rights.
They try to leave a child who was removed from the family with one of its members, but they are not always able to arrange temporary custody. Relatives registered in the same territory as a mother with limited rights are prohibited from doing this, Zimova emphasized.
Relatives registered in the same territory as a mother with limited rights are prohibited from doing this, Zimova emphasized.
The mother can continue to take care of her son or daughter if the attacks of her diseases can be successfully stopped with drugs. To do this, the doctor must record that the woman has no exacerbations and she is regularly observed in the neuropsychiatric dispensary and takes prescribed medications.
“In fact, children become hostages of the situation: they develop attachment, and it would be wrong to deprive them of a loved one simply because of her illness - a child needs a mother. This is done in emergency cases, when there was information about precedents proving the danger of a child being with a mentally unhealthy mother. But his transfer to other families is also difficult, no one can adopt him,” Zimova said.
At the same time, the restriction of a parent with a diagnosis of rights does not mean his actual separation from the child.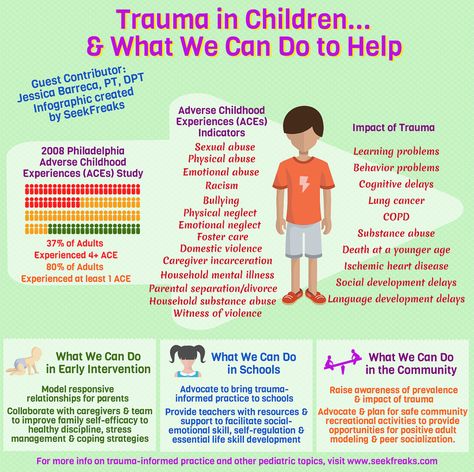 The social worker said that in practice, mother and child often see each other. A woman visits an institution where a minor is kept, data about her visit is recorded there.
The social worker said that in practice, mother and child often see each other. A woman visits an institution where a minor is kept, data about her visit is recorded there.
The format of communication between a mother with a diagnosis and her son or daughter is determined by the court, said Nina Ostanina, chairman of the State Duma Committee on Family, Women and Children. Usually, the meetings are attended by guardianship and guardianship authorities, employees of educational institutions where the minor is located, or an appointed guardian.
Nevertheless, all children should have the right to be brought up by their parents, the politician believes.
“I am categorically against depriving women with mental disorders of the opportunity to take care of a child. Guardianship authorities should try to the last to build such a model in which a child born by such a mother will not suffer, ”she said.
The fact that a woman has a diagnosis should not become a reason for a reproductive restriction, agreed psychiatrist Viktor Lebedev.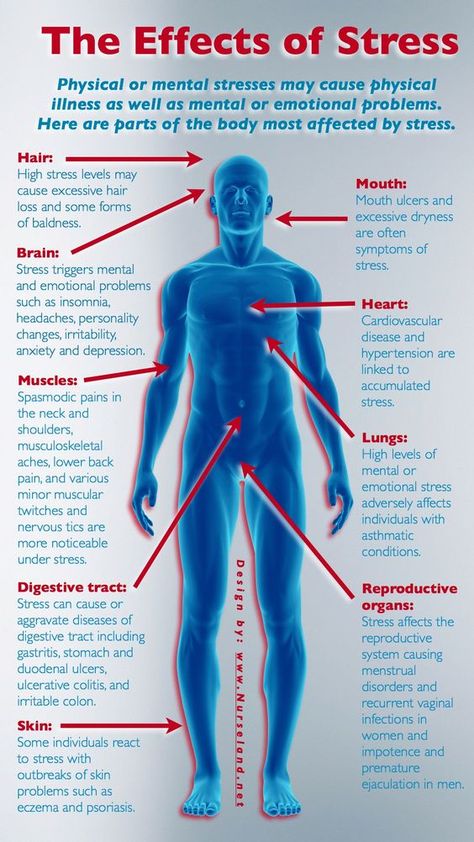 However, some doctors may put pressure on the patient, forcing her to abandon the pregnancy.
However, some doctors may put pressure on the patient, forcing her to abandon the pregnancy.
“Doctors say: “Why do you need to give birth?”, “Think about the state of the child.” Psychiatrists, on the other hand, avoid prescribing drugs to a woman during pregnancy and lactation, although there is evidence of their safety. This is rather the position of the specialists themselves - "no matter how something happens." The moment itself is ethically controversial, ”says the doctor.
Monitoring of mothers with mental illness
To understand how a mother's illness can be dangerous for her child, regular monitoring is necessary. The difficulty lies in the fact that not all patients are aware of their problems and not all, knowing, report them, explained Elena Shidlovskaya, perinatal psychologist, head of the Soul Gift charity project.
“If a woman was on a special register during pregnancy, the data can be transferred to the attending physician. He can independently suspect violations, when a woman at the very reception shows inadequacy or aggression, then she will be sent to a psychologist or psychiatrist for further examination, ”said the psychologist.
Mikhail Tetyushkin added that patients with diseases of this kind should be observed by an obstetrician-gynecologist and a psychiatrist at the same time, since taking medications in the standard regimen is not available to women due to the toxic effect of drugs on the fetal body.
Subsequently, all information about the health of the woman in labor is entered into the card, they are transferred to pediatricians and employees of the psycho-neurological dispensary (PND), who are already alert about possible changes in the condition of the young mother. After discharge, the tactics of further treatment are determined, the specialist said.
The nature of dynamic dispensary observation in a chronic disease, according to Natalia Treushnikova, is determined by the type of its course and the patient's condition.
If she is in remission, it is enough to visit the IPA 1-2 times a year. If a woman has recently been discharged from a hospital, she needs visits to a psychiatrist 1-2 times a month.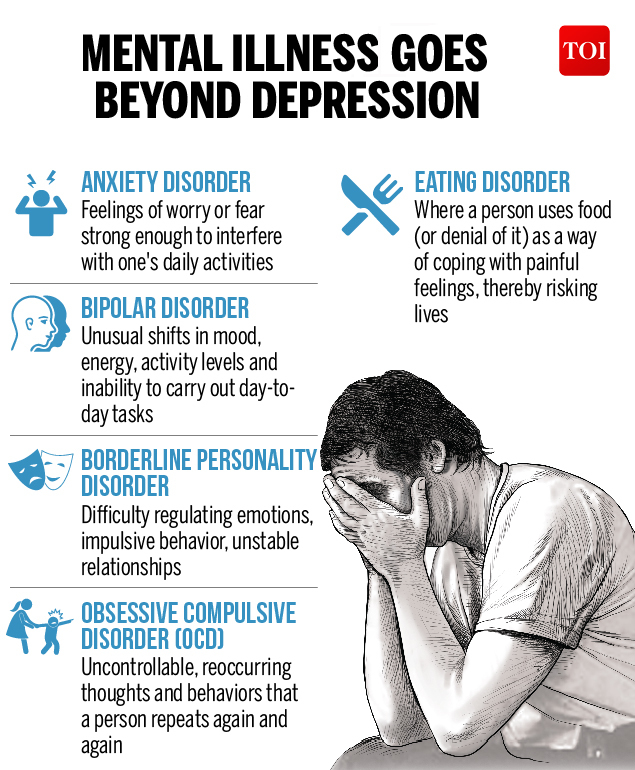
You can notice the prerequisites for the development of acute disorders immediately after childbirth, the expert is sure: the knowledge of a doctor of any specialty should be sufficient.
“I would like pediatricians who take care of a baby to be attentive. How can this be understood? If the mother behaves inappropriately or the doctor suspects that she is not coping with her duties. It is worth offering her the primary help of a clinical psychologist or psychotherapist, ”the expert said.
Psychiatrist Lebedev believes that a standard survey about her psychological state will help to identify a woman's problem, it can be conducted by the attending physician and even a nurse. Thus, a “risk group” is formed that requires attention and which should be informed about the possibility of receiving specialized support.
“This does not mean that a woman should be immediately taken to a dispensary for fear that she might do something to the child. It is important to warn her and teach the algorithm of actions in case of difficulties, not forcing, but creating conditions for the mother in which she will be able to receive information and use it.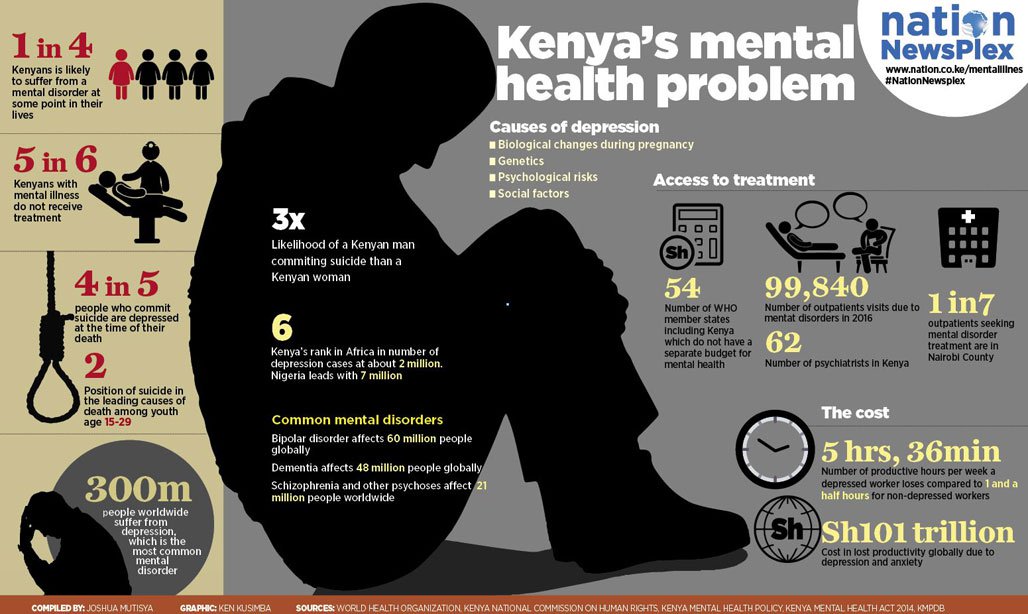 To avoid the possible negative impact of her diagnosis on the baby, competent specialists are needed to inform about the options for receiving assistance, and to destigmatize the use of medications,” the doctor emphasized.
To avoid the possible negative impact of her diagnosis on the baby, competent specialists are needed to inform about the options for receiving assistance, and to destigmatize the use of medications,” the doctor emphasized.
Help during crises
Psychologist Shidlovskaya believes that prolonged postpartum depression can cause exacerbation of serious conditions. The woman's psyche is affected by an increased sense of responsibility for the child, fatigue, unfulfilled expectations, and increases feelings and criticism of the environment.
“Often they say to a new mother: “You are crying and don’t want to live because you don’t do anything”, “Before, no one complained about depression”, “Did you think it would be easy?”, “You should experience only joy from motherhood because children are happiness. Close people should be more attentive to the woman, support her and provide all possible assistance with the baby in order to prevent her condition from worsening, ”the expert emphasized.
She reminded that mothers have the right to apply for psychological support, in many regions of the country various services work on a charitable basis, ready to assist in solving problems that have arisen.
However, in case of severe illness, other specialists may be required.
If the mother’s condition poses a real threat to the life and health of herself and those around her, if the failure to provide assistance leads to a deterioration in her mental health, or if she is unable to meet the needs of life, the woman is forcibly hospitalized on the basis of Article No. 29psychiatric law.
If one of the indicated signs is present, family members should call doctors, advised Mikhail Tetyushkin. The patient will be provided with a psychiatric consultation or taken to a state psychiatric hospital, her family members can also apply to a private medical institution. Moreover, she will not need to undergo treatment for a long time: in most cases, the patient does not even need a permanent stay in the hospital. Standardly, he stays there for 21 days, in some situations - a few months, no more, the doctor said.
Standardly, he stays there for 21 days, in some situations - a few months, no more, the doctor said.
If a woman is being treated at home, mental health services actively contact her. In case of missing a visit to the dispensary, medical and social workers and psychologists will remind the patient of the need to get specialist advice and convince her to come to the appointment, stressed Natalia Treushnikova, President of the Mental Health Union.
What mental illnesses are inherited - Atlant, medical center
Are mental illnesses hereditary? This question worries many parents. After all, it is very scary to “reward” your child with a mental disorder.
How mental illness is transmitted
The fact that mental illness can be inherited has been noticed for a long time. Today, geneticists confirm: indeed, mental disorders are more likely to appear in a child in a family where a relative suffered from a similar illness. And the reason for this are violations in the structure of genes.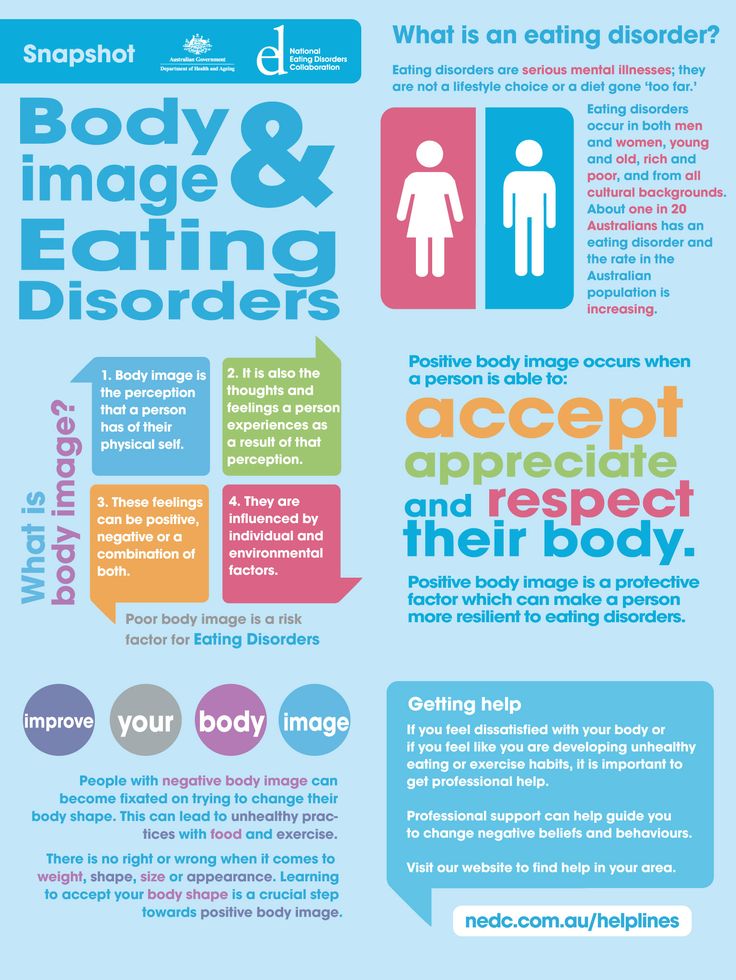
There is such a thing as the coefficient of hereditary risk. The higher this coefficient, the higher the likelihood that the child will inherit the disease of relatives.
Only some mental illnesses are directly related to breakdowns in the genes, for example, Huntington's chorea, the hereditary risk coefficient of which is 5000. For comparison, for such a mental illness as schizophrenia, it is 9.
How does the degree of relationship affect hereditary diseases?
The risk of developing a mental illness depends on the degree of relationship with a sick family member and on the number of sick relatives.
The highest probability of transmission of the disease in identical twins, followed by 1st degree relationship (parents, children, brothers, sisters). In 2nd degree relatives, the risk is significantly reduced
So, with schizophrenia, which is present in the mother and father, the probability of its occurrence in children is 46%, if one parent is sick - about 13%, if the grandfather or grandmother is sick - 5%.
What mental illnesses are most often inherited
1. Disorders of the mental development of children
- Attention deficit hyperactivity disorder (ADHD) is manifested by impulsivity, difficulty concentrating, increased motor activity. Often this disorder is combined with depression, behavioral disorders.
- Dyslexia - the inability to read, compare what is written with speech in some cases is hereditary.
- Autism is a severe mental disorder, which is expressed in violation of social adaptation. An autistic child is closed, he does not want to communicate with the outside world, he exists in his personal space. He does not tolerate any change, he has his own rituals, which he strictly observes. He constantly repeats stereotypical movements (rocking, bouncing) or the same phrases.
Autism is usually diagnosed in the first three years of a child's life.
It is believed that the role of heredity in the occurrence of this disease is great.
2. Schizophrenia
This is a mental illness, which is characterized by disturbances in thinking, perception of the world, inappropriate behavior and an abnormal reaction to stimuli. The disease may be accompanied by agitation, delusions, hallucinations. Patients are prone to depression and suicidal.
As a rule, the onset of the disease falls on the age of 20-22 to 30 years.
Heredity plays a significant role in the occurrence of this disease, but other factors are no less important: complications during gestation, difficult childbirth in the mother, infections, difficult psycho-emotional situations, and even birth in winter.
3. Affective bipolar disorder
Otherwise, this mental illness is called manic-depressive psychosis. It proceeds with an alternation of phases: depression and excitement, sometimes with aggression. There may be gaps between these phases.
4. Alzheimer's disease
This disease develops after the age of 65 and is expressed first in forgetfulness, difficulty concentrating. Then there is confusion, loss of orientation in space. Irritability, unmotivated aggression appear, speech is disturbed. Dementia develops.
Then there is confusion, loss of orientation in space. Irritability, unmotivated aggression appear, speech is disturbed. Dementia develops.
Rarely enough, the disease begins earlier, and here the hereditary factor, the pathological gene, plays a significant role.
Other hereditary mental illnesses:
- epilepsy;
- psychopathy;
- alcohol dependence;
- dementia;
- Down syndrome;
- Huntington's chorea;
- "cat cry" syndrome;
- Klinefelter's syndrome.
All of these mental illnesses can be inherited. At the same time, they can appear in a family where no one has suffered from such disorders. True, the risk of disease in this case is less, but it exists. So, you can get schizophrenia in a completely “healthy” family with a probability of 1%.
If there is a risk
Many people are afraid of passing on hereditary diseases to their children (even if distant relatives suffered from them), especially mental disorders, and therefore prefer not to have a child.