Most prescribed antidepressant
Overview - Antidepressants - NHS
Antidepressants are a type of medicine used to treat clinical depression.
They can also be used to treat a number of other conditions, including:
- obsessive compulsive disorder (OCD)
- generalised anxiety disorder
- post-traumatic stress disorder (PTSD)
Antidepressants are also sometimes used to treat people with long-term (chronic) pain.
Read more about when antidepressants are used.
How antidepressants work
It's not known exactly how antidepressants work.
It's thought they work by increasing levels of chemicals in the brain called neurotransmitters. Certain neurotransmitters, such as serotonin and noradrenaline, are linked to mood and emotion.
Neurotransmitters may also affect pain signals sent by nerves, which may explain why some antidepressants can help relieve long-term pain.
While antidepressants can treat the symptoms of depression, they do not always address its causes. This is why they're usually used in combination with therapy to treat more severe depression or other mental health conditions.
How effective are antidepressants?
Research suggests that antidepressants can be helpful for people with moderate or severe depression.
They're not usually recommended for mild depression, unless other treatments like talking therapy have not helped.
Doses and duration of treatment
Antidepressants are usually taken in tablet form. When they're prescribed, you'll start on the lowest possible dose thought necessary to improve your symptoms.
Antidepressants usually need to be taken for 1 or 2 weeks (without missing a dose) before the benefit starts to be felt. It's important not to stop taking them if you get some mild side effects early on, as these effects usually wear off quickly.
If you take an antidepressant for 4 weeks without feeling any benefit, speak to your GP or mental health specialist. They may recommend increasing your dose or trying a different medicine.
A course of treatment usually lasts for at least 6 months after you start to feel better. Some people with recurrent depression may be advised to take them indefinitely.
Read more about antidepressant dosages.
Side effects
Different antidepressants can have a range of different side effects. Always check the information leaflet that comes with your medicine to see what the possible side effects are.
The most common side effects of antidepressants are usually mild. Side effects should improve within a few days or weeks of treatment, as the body gets used to the medicine.
Read more about:
- possible side effects of antidepressants
- cautions and interactions of antidepressants
Coming off antidepressants
Talk to your doctor before you stop taking antidepressants. It's important that you do not stop taking antidepressants suddenly.
Once you're ready to come off antidepressants, your doctor will probably recommend reducing your dose gradually over several weeks – or longer, if you have been taking them for a long time.
This is to help prevent any withdrawal symptoms you might get as a reaction to coming off the medicine.
Read more about stopping or coming off antidepressants.
Types of antidepressants
There are several different types of antidepressants.
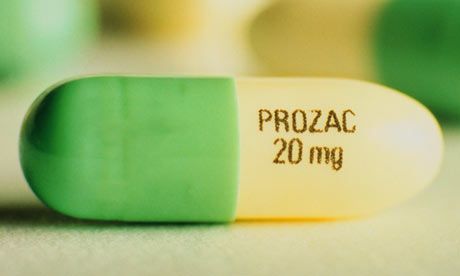
Selective serotonin reuptake inhibitors (SSRIs)
SSRIs are the most widely prescribed type of antidepressants. They're usually preferred over other antidepressants, as they cause fewer side effects. An overdose is also less likely to be serious.
Fluoxetine is probably the best known SSRI (sold under the brand name Prozac). Other SSRIs include citalopram (Cipramil), escitalopram (Cipralex), paroxetine (Seroxat) and sertraline (Lustral).
Serotonin-noradrenaline reuptake inhibitors (SNRIs)
SNRIs are similar to SSRIs. They were designed to be a more effective antidepressant than SSRIs. However, the evidence that SNRIs are more effective in treating depression is uncertain. It seems that some people respond better to SSRIs, while others respond better to SNRIs.
It seems that some people respond better to SSRIs, while others respond better to SNRIs.
Examples of SNRIs include duloxetine (Cymbalta and Yentreve) and venlafaxine (Efexor).
Noradrenaline and specific serotonergic antidepressants (NASSAs)
NASSAs may be effective for some people who are unable to take SSRIs. The side effects of NASSAs are similar to those of SSRIs, but they're thought to cause fewer sexual problems. However, they may also cause more drowsiness at first.
The main NASSA prescribed in the UK is mirtazapine (Zispin).
Tricyclic antidepressants (TCAs)
TCAs are an older type of antidepressant. They're no longer usually recommended as the first treatment for depression because they can be more dangerous if an overdose is taken. They also cause more unpleasant side effects than SSRIs and SNRIs.
Exceptions are sometimes made for people with severe depression that fail to respond to other treatments. TCAs may also be recommended for other mental health conditions, such as OCD and bipolar disorder.
TCAs may also be recommended for other mental health conditions, such as OCD and bipolar disorder.
Examples of TCAs include amitriptyline, clomipramine, dosulepin, imipramine, lofepramine and nortriptyline.
Some types of TCAs, such as amitriptyline, can also be used to treat chronic nerve pain.
Serotonin antagonists and reuptake inhibitors (SARIs)
SARIs are not usually the first choice of antidepressant, but they may be prescribed if other antidepressants have not worked or have caused side effects.
The main SARI prescribed in the UK is trazodone (Molipaxin).
Monoamine oxidase inhibitors (MAOIs)
MAOIs are an older type of antidepressant that are rarely used nowadays.
They can cause potentially serious side effects so should only be prescribed by a specialist doctor.
Examples of MAOIs include tranylcypromine, phenelzine and isocarboxazid.
Other treatments for depression
Other treatments for depression include talking therapies such as cognitive behavioural therapy (CBT).
People with moderate to severe depression are usually treated using a combination of antidepressants and CBT. Antidepressants work quickly in reducing symptoms, whereas CBT takes time to deal with causes of depression and ways of overcoming it.
Regular exercise has also been shown to be useful for those with mild depression.
Read more about alternatives to antidepressants.
Yellow Card Scheme
The Yellow Card Scheme allows you to report suspected side effects from any type of medicine you're taking. It's run by a medicines safety watchdog called the Medicines and Healthcare products Regulatory Agency (MHRA).
It's run by a medicines safety watchdog called the Medicines and Healthcare products Regulatory Agency (MHRA).
See the Yellow Card Scheme website for more information.
Community content from HealthUnlockedThe most effective antidepressants for adults revealed in major review
This is a plain English summary of an original research article
Antidepressants are effective to treat moderate to severe depression in adults. Five antidepressants appear more effective and better tolerated than others.
A major review of 522 antidepressant trials found that all of the 21 drugs studied performed better than placebo, in short-term trials measuring response to treatment. However, effectiveness varied widely.
Researchers ranked drugs by effectiveness and acceptability after eight weeks of treatment. Several drugs were more effective and were stopped by fewer people than others:
- escitalopram
- paroxetine
- sertraline
- agomelatine
- mirtazapine.

The review provides new evidence which may help people decide which antidepressant to choose first-line for moderate to severe depression. However, it did not assess antidepressants compared to other treatments such as cognitive behavioural therapy, or treatments in combination. Though there are some concerns over items not reported by individual trials, this review is likely to be reliable. It is extensive, included only placebo controlled double blind trials and searched successfully for unpublished trials.
Why was this study needed?
Depression is a common condition, affecting an estimated 1 in 10 adults at some point in their lives. Antidepressants are widely prescribed in primary and secondary care, along with psychological interventions such as cognitive behavioural or interpersonal therapy. There is conflicting evidence to guide which antidepressants should be prescribed first-line, although NICE recommends a selective serotonin reuptake inhibitor (SSRI).
There has been uncertainty in recent years about the effectiveness of antidepressants. Their mode of action is poorly understood, and improvement in mood tends to be modest. One 2008 meta-analysis suggested that antidepressants gave little benefit over placebo for mild to moderate depression.
This new analysis went to some lengths to find unpublished studies and additional data from published studies, to give us the best overview of the current state of research.
What did this study do?
This systematic review and network meta-analysis compared 21 antidepressants with placebo or each other, directly within trials and indirectly across trials. They included 522 double-blind randomised controlled trials of 116,477 adults with moderate to severe depression.
More than 100 trials were previously unpublished. As well as publication databases, international trial registers and drug approval websites, the researchers had contacted all pharmaceutical companies marketing antidepressants to ask for unpublished studies.
The antidepressants were compared for effectiveness (at least 50% improvement in symptoms) and acceptability (assessed as drop-out rate). They found 380 trials at possible risk of bias due mainly to lack of reporting of randomisation methods, and 46 at high risk. However, the trials were all placebo controlled.
What did it find?
- All 21 antidepressants were more likely to produce a treatment response after eight weeks treatment than a placebo. The most effective antidepressant compared to placebo was the tricyclic antidepressant amitriptyline, which increased the chances of treatment response more than two-fold (odds ratio [OR] 2.13, 95% credible interval [CrI] 1.89 to 2.41). The least effective was the serotonin and noradrenaline reuptake inhibitor reboxetine, which increased treatment response by 37% (OR 1.37, 95% CrI 1.16 to 1.63).
- Drop-out rates by eight weeks of treatment were similar to placebo for the majority of antidepressants. People were 30% more likely to stop taking the tricyclic clomipramine than placebo (OR 1.
 30, 95% CrI 1.01 to 1.68) and slightly less likely to stop taking agomelatine (an “atypical” antidepressant) or the SSRI fluoxetine (OR for agomelatine 0.84, 95% CrI 0.72 to 0.97; OR for fluoxetine 0.88, 95% CrI 0.8 to 0.96).
30, 95% CrI 1.01 to 1.68) and slightly less likely to stop taking agomelatine (an “atypical” antidepressant) or the SSRI fluoxetine (OR for agomelatine 0.84, 95% CrI 0.72 to 0.97; OR for fluoxetine 0.88, 95% CrI 0.8 to 0.96). - In head-to-head comparisons between the drugs, five were identified as having a combination of better effectiveness and lower drop-out rates, compared to others: the SSRIs escitalopram, paroxetine and sertraline, and atypicals agomelatine and mirtazapine. Reboxetine (atypical), trazodone (similar to a tricyclic) and fluvoxamine (SSRI) were identified as having lower effectiveness and higher drop-out rates.
- Though absolute effect sizes were not reported in the results, the researchers described the effect sizes as “modest”. However, they also said that “non-response to treatment will occur.”
What does current guidance say on this issue?
The NICE 2009 guideline on depression advises that people with moderate to severe depression should be offered an antidepressant and psychological therapy such as cognitive behavioural therapy or interpersonal therapy. It says the antidepressant prescribed “should normally be an SSRI in a generic form because SSRIs are equally effective as other antidepressants and have a favourable risk-benefit ratio.”
It says the antidepressant prescribed “should normally be an SSRI in a generic form because SSRIs are equally effective as other antidepressants and have a favourable risk-benefit ratio.”
The guideline warns that venlafaxine is more associated with risk of death from overdose than other SSRIs, while “tricyclic antidepressants, except for lofepramine, are associated with the greatest risk in overdose.”
The guideline, last updated in 2016, is under review.
What are the implications?
The findings are of interest to GPs and psychiatrists, who need to decide on the best initial treatment for adults with moderate to severe depression. The comparative data may help doctors select drugs with better efficacy and side-effects.
However, treatment choice will be guided by an individual patient's circumstances and preferences. The meta-analysis was unable to look at the potentially different effects of treatment on subgroups based on age, sex, the severity of symptoms or duration of illness.
The review did not consider combined drug and psychological treatments, as recommended by NICE for moderate to severe depression, or long-term effects which limit its applicability.
Citation and Funding
Cipriani A, Furukawa TA, Salanti G, et al. Comparative efficacy and acceptability of 21 antidepressant drugs for the acute treatment of adults with major depressive disorder: a systematic review and network meta-analysis. Lancet. 2018. [Epub ahead of print].
This project was funded by the National Institute for Health Research Oxford Health Biomedical Research Centre (BRC-1215-20005) and the Japan Society for the Promotion of Science.
Bibliography
Parikh SV, Kennedy SH. More data, more answers: picking the optimal antidepressant. Lancet 2018.
NICE. Depression in adults: recognition and management. CG90. London: National Institute for Health and Care Excellence; 2009.
Produced by the University of Southampton and Bazian on behalf of NIHR through the NIHR Dissemination Centre
Fighting depression: 10 modern drugs
{{if type === 'partner-stocks'}}
{{/if}}
{{/if}} {{each list}}${this} {{if isGorzdrav}}
Delete
{{/if}}
{{/each}} {{/if}} Search by drug, disease, substance: DERMAKOSMETIKA, SOLGAR, NaturAge, Voltaren, KagocelHome
Articles
Fighting depression: 10 modern drugs
Depression is an urgent problem, the number of visits to doctors is growing every year. It can be solved by contacting a psychotherapist and taking antidepressants . These are drugs that regulate the production of hormones and biochemical processes in the body. It is strictly forbidden to prescribe them to oneself , as these are complex drugs with certain restrictions, side effects effects . The doctor must authorize their appointment and control the intake. We will tell you which of them are the most effective and common in medicine, how many they have pluses and minuses.
It can be solved by contacting a psychotherapist and taking antidepressants . These are drugs that regulate the production of hormones and biochemical processes in the body. It is strictly forbidden to prescribe them to oneself , as these are complex drugs with certain restrictions, side effects effects . The doctor must authorize their appointment and control the intake. We will tell you which of them are the most effective and common in medicine, how many they have pluses and minuses.
What is meant by
depression Doctors have known it since ancient Greece and Egypt. Hippocrates described it as melancholy - a condition that is accompanied by anxiety, despondency, insomnia, refusal of food, irritability. Most often, the cause is childhood trauma or severe, frequent stress in adulthood. There are many provoking factors: the death of a loved one, deterioration of living conditions, alcoholism, brain diseases.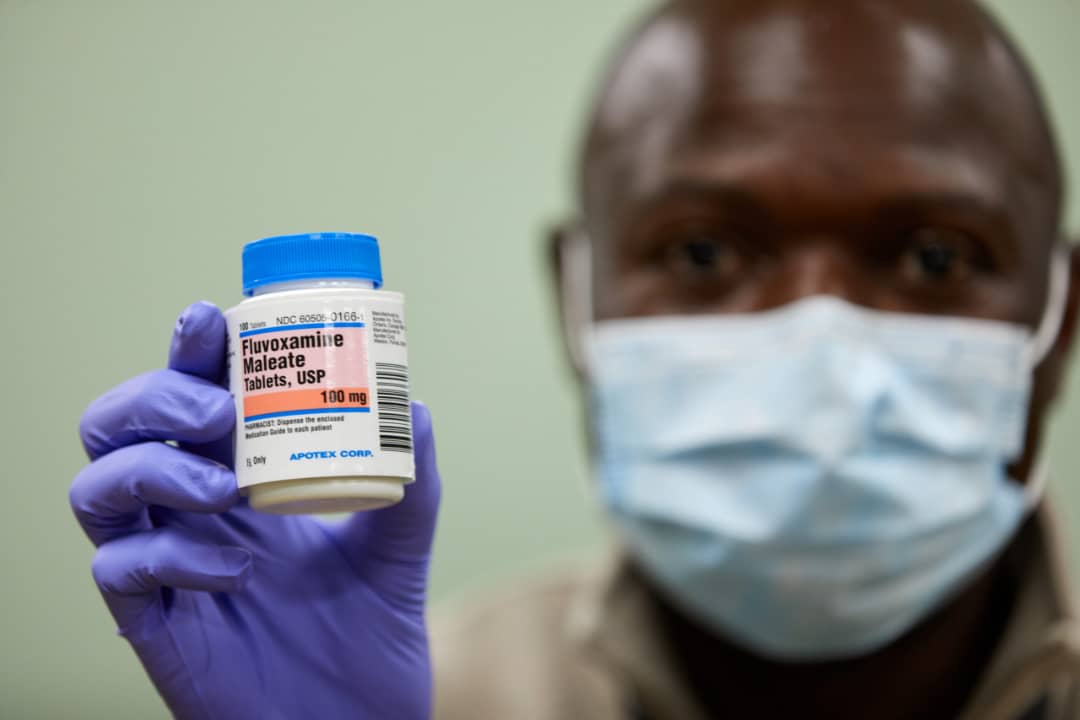 Such cases are referred to as psychogenic depression.
Such cases are referred to as psychogenic depression.
The second type is endogenous. The problem appears not from large external shocks, but because of internal causes. A person is constantly dissatisfied with himself, subjecting himself to criticism. Many patients have panic attacks , haunted by a feeling of fear, anxiety.
How long the period of depression lasts
Many people mistake ordinary periods of low mood for depression. If they do not last long and are quickly replaced by periods of recovery, then we are not talking about a depressive state. The problem is obvious when the symptoms persist for months and dramatically change a person's life. Then you need to see a doctor.
What happens to the body
The most common theory is that there is a malfunction of neurotransmitters located in the brain. These substances transmit signals from neuron to neuron and are responsible for a person's mood. Dysfunction leads to a slowdown in the rate of this transmission and a decrease in the number of neurotransmitters themselves. Serotonin, which is called the "hormone of happiness", suffers the most. For clarity, this biochemical process can be compared, for example, with a drop in blood sugar levels in diabetes mellitus.
How is
treated depressionDepression has been treated in different ways. In the ancient world - emetics and laxatives. In the Renaissance - wine and sunbathing. In the Age of Enlightenment - external stimuli, for example, insects. The 19th century brought new recipes - in particular, a solution of camphor in tartaric acid. The treatment also included the use of drugs, which are now no longer allowed for sale, and some are recognized as narcotic.
Obviously, all these drugs did not affect the increase in the amount of serotonin. And the treatment is precisely to normalize its production. This was done after creating modern antidepressants , which have a minimum of side effects, are safe for the body and are not addictive. These are drugs, whose action is aimed precisely at balancing the disturbed balance of neurotransmitters: serotonin, norepinephrine, dopamine.
These are drugs, whose action is aimed precisely at balancing the disturbed balance of neurotransmitters: serotonin, norepinephrine, dopamine.
Prescription
If a healthy person takes antidepressants , there will be no effect . For a depressed patient, taking them will help:
- improve psychological state;
- get rid of irritability;
- panic fear;
- increase mental and physical activity;
- overcome the dreary mood.
Psychiatrists prescribe antidepressants for chronic back pain, headaches. And also with irritable bowel syndrome, incontinence and other cases when the body stops producing its own painkillers. Medication helps restore pain suppression mechanisms.
You can only take these drugs with a doctor's prescription, as many of them are strong stimulants. Self-administration can cost dearly - the condition may worsen. Only a doctor will correctly calculate how many medicines to take per day. In parallel with the treatment by a psychiatrist, a neurologist, a consultation of a psychotherapist is required.
Self-administration can cost dearly - the condition may worsen. Only a doctor will correctly calculate how many medicines to take per day. In parallel with the treatment by a psychiatrist, a neurologist, a consultation of a psychotherapist is required.
Precautions
- Prescribed drug start drinking from a small dose - the first couple of days they take a quarter of a tablet. Gradually increase the dose to normal. So the body adapts better. Finish the course by reducing the dose.
- The first effect of appears only 2 weeks after the start of administration. Sustained action - after six months. All this time, you need to take remedy, without making passes, breaks.
-
Products are not combined with melatonin, St. John's wort, products and dietary supplements based on sibutramine, 5-HTP. Their combination can raise serotonin to dangerous levels.
 Also, you can not combine them with monoamine oxidase inhibitors, for example, Cipralex. When writing a prescription, the doctor takes these points into account.
Also, you can not combine them with monoamine oxidase inhibitors, for example, Cipralex. When writing a prescription, the doctor takes these points into account. - Drinking antidepressants is better in parallel with visits to a psychotherapist. If the drugs normalize the biochemical processes in the body, then this doctor will help normalize the psychological state after depression.
The best antidepressants
In medicine, they have long argued that some drugs give only a placebo effect. The purpose of the study was to find out which of them are the most effective and valid . The project involved 116 thousand patients, and its results were published by the authoritative edition of the Lancet. We offer a list of the best.
1. Agomelatine
New generation drug. Agomelatine is used for severe depressive disorders, high levels of anxiety. Enhances the release of dopamine and norepinephrine, stimulates melatonin receptors. The standard therapeutic dose is 25-50 mg 1 time / day. Helps to restore the normal structure of sleep, get rid of anxiety and panic attacks attacks
The standard therapeutic dose is 25-50 mg 1 time / day. Helps to restore the normal structure of sleep, get rid of anxiety and panic attacks attacks
Pros
+ Does not adversely affect attention and memory.
+ No lethargy during the day.
+ No sexual deviations.
+ No relation to blood pressure.
+ Do not reduce dosage upon discontinuation.
Cons
— In 1-10% of cases, increased sweating, diarrhea, constipation.
- Possible increased fatigue, drowsiness.
- There are no evidence-based safety studies in people with renal or hepatic insufficiency, therefore, such patients are advised to refrain from taking drugs with active ingredient agomelatine.
2. Amitriptyline
Tricyclic antidepressant. Moreover, the World Health Organization considers Amitriptyline the most reliable in this group. The standard dose is 200-250 mg / day. The action is to block the reuptake of neurotransmitters. A good remedy for moderate to severe disorders of the endogenous type. Additionally, it has a sedative and hypnotic effect. Effective in the treatment of neuropathic pain, for the prevention of migraine.
A good remedy for moderate to severe disorders of the endogenous type. Additionally, it has a sedative and hypnotic effect. Effective in the treatment of neuropathic pain, for the prevention of migraine.
Pluses
+ Preparations with active ingredient amitriptyline are inexpensive.
+ High reliability, minimum side effects.
+ Relatively safe during breastfeeding.
Cons
— Possible side effect in the form of blurred vision, dry mouth.
- Lowering blood pressure.
- Some patients experience constipation.
- Drowsiness.
3. Escitalopram
It belongs to the group of modern serotonin reuptake inhibitors (SSRIs). Most often, it is recommended to take for anxiety, panic attacks. It is taken once, the standard dose is 10 mg per day. Escitalopram has a milder effect and is prescribed to patients for whom tricyclic drugs are contraindicated.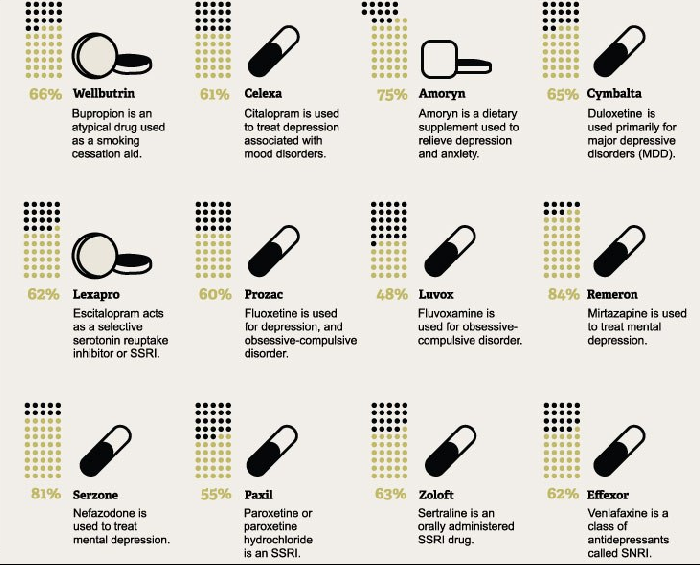
Pluses
+ Lasting effect comes after 3 months.
+ Indicated for patients with disorders of the cardiovascular system.
+ Soft action.
Cons
- In some patients, the functions of the gastrointestinal tract are disturbed, which is most often expressed in diarrhea.
- Anxiety may increase during the first 2 weeks, therefore it is recommended to start treatment with low doses and gradually increase them.
- Contraindicated in pregnancy and lactation.
4. Mirtazapine
A drug of the tetracyclic group. Mirtazapine - good stimulant for anxious depressions, has a moderate sedative effect. The average amount is 30 mg / day, it must be consumed once. Usually it is prescribed to patients who lose interest in life, cease to experience joy, pleasure. Effective in the correction of sleep, in particular, early awakenings.
Pros
+ Earlier onset of action than SSRIs (1 week).
+ Works well with most general medicines.
+ Full effect in 4 weeks.
+ Does not affect sexual function.
Cons
- The active substance mirtazapine is contraindicated in diabetes mellitus, arterial hypotension, increased intraocular pressure.
— During the appointment, you must drive carefully and engage in potentially hazardous types of work.
- 18% of patients experience drowsiness, 15% dry mouth, 5% weight loss. Other side effects occur in 1-3% of cases.
5. Paroxetine
Belongs to the SSRI group, is used most often for severe anxiety, panic, social phobia, nightmares, stress after trauma. Paroxetine can resolve the problems of anxious depression, anxiety-phobic disorders. Take once a day at a dose of 20 mg.
Pros
+ The most powerful stimulant among SSRIs.
+ Anxiety and insomnia pass quickly.
+ Minimal side effects in the form of vomiting, diarrhea.
+ Suitable for patients with cardiovascular problems.
Cons
— Not suitable for patients with severe motor, mental inhibition.
- Reduces libido.
- Harmful to the fetus when taken during pregnancy.
6. Fluoxetine
One of the most commonly used antidepressants in the SSRI group. Known as Prozac. Fluoxetine is also known as a good mood stimulant. Patients have a feeling of fear, tension, anxiety, gloomy dislike for others. Depending on the indications, the average daily dose is 20-60 mg.
Pluses
+ There is practically no effect on the work of the heart.
+ Does not cause sedation.
+ Effective for patients with motor retardation and excessive daytime sleepiness.
Cons
- May cause weight loss.
— Hypoglycemia is possible in diabetes mellitus.
- Contraindicated in severe renal impairment.
7. Fluvoxamine
Another SSRI drug. Fluvoxamine is similar to Prozac Fluoxetine but is fast acting and may cost cheaper. The effect is in a more active slowing down of the reuptake of serotonin by neurons. It is indicated for depression of various origins, as well as obsessive-compulsive disorders. The average daily dose is 100 mg.
Fluvoxamine is similar to Prozac Fluoxetine but is fast acting and may cost cheaper. The effect is in a more active slowing down of the reuptake of serotonin by neurons. It is indicated for depression of various origins, as well as obsessive-compulsive disorders. The average daily dose is 100 mg.
Pros
+ Lower price than traditional Prozac.
+ Faster action than him.
+ Relatively minor side effects (diarrhea, dry mouth, drowsiness).
Cons
- Contraindicated in diabetes.
- Pregnant women - with caution, lactation - prohibited.
- Causes nausea in some patients.
8. Sertraline
One of the widely used and universal drugs of the SSRI group. They treat almost any depressive condition, panic disorder, social phobia. However, in severe clinical cases, sertraline may not be effective enough. The standard dose is 50 mg/day.
Pros
+ No cardiotoxicity.
+ The patient's psychomotor activity does not change.
+ Does not increase body weight.
+ Combines well with other groups of antidepressants.
Cons
— In the first 2 weeks there may be problems with sleep, diarrhea.
- Side effects of a sexual nature.
- Contraindicated in pregnant women.
9. Escitalopram
The drug is classified as an SSRI. Its difference is in its effectiveness in depression, which is accompanied by involuntary movements (tic, tremor, chewing, smacking). Escitalopram is prescribed to patients with panic, anxiety, phobias, obsessive thoughts or actions. The daily dose is 20 mg.
Pluses
+ Effective in tardive dyskinesia.
+ One of the most powerful SSRIs.
+ More pronounced thymoleptic effect (improvement of mood) compared to many antidepressants of the same group.
Cons
- In some patients, anxiety increases within 2 weeks after starting treatment.
— Gastrointestinal disorders, insomnia, agitation are possible.
— Use during pregnancy only in extreme cases, incompatible with feeding.
10. Venlafaxine
Belongs to the SNRI group. In addition to blocking the reuptake of serotonin, venlafaxine has a similar effect on another neurotransmitter, norepinephrine. The medicine is prescribed for depressive conditions of various origins, social phobias, anxiety, panic. Usually take 150 mg per day.
Pros
+ Better tolerated by patients than most tricyclics.
+ More pronounced effect than classic SSRIs.
+ Fewer contraindications.
Cons
- Traditional side effects of most antidepressants: nausea, drowsiness, dry mouth, diarrhea or constipation.
- May increase eye pressure.
- The most severe withdrawal syndrome among antidepressant drugs.
This list is not to be used as a recommendation. In any case, consult your doctor before purchasing. Be healthy!
Venlafaxine (Velaxin) - the most effective antidepressant?
partners Keywords / keywords: Antidepressants, Depression, Demonstrative medicine, Personal experience, Neurons, Recommendations, Effectiveness, Velaxin, Neuropsychiatry
Summary
Evidence-based medicine has failed to provide conclusive evidence that antidepressants differ in their effectiveness in treating depression. Therefore, scientists base their judgments on the effectiveness of drugs on "personal experience." There is another way to determine the most effective antidepressant. To do this, it is necessary to compare data on the activity of neurons in depression and the ability of antidepressants to act on these neurons. This comparison suggests that the most effective antidepressants are amitriptyline, imipramine, and venlafaxine (in high daily doses). But only venlafaxine is used in our country in therapeutic doses. Therefore, venlafaxine is the most effective antidepressant.
Therefore, scientists base their judgments on the effectiveness of drugs on "personal experience." There is another way to determine the most effective antidepressant. To do this, it is necessary to compare data on the activity of neurons in depression and the ability of antidepressants to act on these neurons. This comparison suggests that the most effective antidepressants are amitriptyline, imipramine, and venlafaxine (in high daily doses). But only venlafaxine is used in our country in therapeutic doses. Therefore, venlafaxine is the most effective antidepressant.
Persistent attempts by pharmaceutical companies to prove with the help of evidence-based medicine that their antidepressant is the most effective in the treatment of depression have so far been unsuccessful. This is agreed not only by individual critics of such studies, but also by large teams of scientists who make recommendations for the pharmacotherapy of depressive disorders. In any case, they proceed from the fact that evidence-based medicine data indicate a comparable activity of antidepressants in the treatment of depression (1, 2, 3). Therefore, to determine the most effective drugs, scientists resort to the “personal experience” accumulated in the treatment of patients (4), which is always subjective. This method of determining the most effective antidepressants is vulnerable to criticism. An alternative to "personal experience" is a comparison of the mechanisms of formation of depression (pathogenesis) and the therapeutic properties of drugs.
Therefore, to determine the most effective drugs, scientists resort to the “personal experience” accumulated in the treatment of patients (4), which is always subjective. This method of determining the most effective antidepressants is vulnerable to criticism. An alternative to "personal experience" is a comparison of the mechanisms of formation of depression (pathogenesis) and the therapeutic properties of drugs.
It is known that the symptoms of depression are accompanied by a decrease in the activity of different neurons: norepinephrine (↓H), dopamine (↓D), serotonin (↓C), and melatonin (↓M) neurons (Table 1).
Table 1. Decreased activity of neurons in various symptoms of depression (5, 6, 7).
| Neuronal activity | Symptoms of depression | "Traditional" names for depressions |
| ↓ND | Deterioration of mood - weakening of positive emotions: melancholy, depression, apathy, decreased interest and pleasure in activities usually associated with positive emotions, gloomy and pessimistic vision of the future | Sad, apathetic, anhedonic |
| ↓CH | Deterioration of mood - increased negative emotions: sadness, spleen, irritation, low self-esteem and feelings of self-doubt, ideas of guilt and self-abasement, anxiety, fear, nervousness | Aching, self-torturing, anxious, dysphoric |
| ↓SND | Deterioration of mood - weakening of positive and strengthening of negative emotions: melancholy and anxiety, anxiety and apathy | Sad-anxious, anxious-apathetic |
| ↓N | Psychomotor retardation: loss of energy and increased fatigue, difficulty in concentrating and holding attention, slowing down of information processes, retardation of movements | Asthenic, adynamic |
| ↓SND | Somatic: pain and other discomforts in the body, loss of appetite and weight loss | Somatized, hypochondriacal |
| ↓SNM | Somatic: pathology of circadian rhythms (sleep disturbances, early awakening, peak of feeling unwell in the morning or in the first half of the day). | - |
The main of these symptoms, reflecting deterioration (decrease) in mood (3, 6), are associated with a deterioration in the functioning of norepinephrine and dopamine (↓ND), norepinephrine and serotonin (↓SN), as well as serotonin, norepinephrine and dopamine neurons (↓SND). Accordingly, all depressions can be divided into three classes. The first of these includes ↓ND-depressions. They proceed with the weakening of positive emotions. The second option covers ↓CH-depressions. They are characterized by an increase in negative emotions. Finally, the third one includes ↓SDI-depressions. They are accompanied by both a weakening of positive and an increase in negative emotions. In all three of these variants of depression, phenomena of psychomotor retardation (↓H-symptoms) and / or somatic symptoms (↓SDI or ↓SNM) can be observed. From the presented data, it follows that for the successful treatment of any depression, it is necessary to increase the activity, first of all, of norepinephrine, dopamine and serotonin neurons (↑SND). Accordingly, this is how the most effective antidepressants should act. In other words, they must be ↑SDI drugs.
Accordingly, this is how the most effective antidepressants should act. In other words, they must be ↑SDI drugs.
To increase the activity of serotonin, norepinephrine and dopamine neurons, antidepressants have only three mechanisms. They can be neurotransmitter reuptake inhibitors (RIIs), regulatory receptor-influencing agents (RIARs), or monoamine oxidase type A reversible inhibitors (RIMAO-A) (Table 2).
Table 2. Antidepressants known in Russia, their effect on neurons and the "formula" of the mechanism of action (4, 5, 6, 8).
| INN | Group names | Years of appearance | Growth of neuronal activity* and its mechanism | "Formula" of the drug | |||
| ↑С | ↑N | ↑D | ↑M | ||||
| Imipramine | TcA | 50s | IOZ | IOZ | IOZ | ↑SNd | |
| Amitriptyline | 60s | IOZ | IOZ | IOZ | ↑SNd | ||
| Clomipramine | 60s | IOZ | IOZ | IOZ | ↑Snd | ||
| Pipofezin | 70s | IOZ | IOZ | IOZ | ↑snd | ||
| Trazodone | CMA | 70s | IOZ | SWRR | SWRR | ↑snd | |
| Maprotiline | ChCA | 70s | IOZ | IOZ | ↑cN | ||
| Mianserin | 70s | SWRR | SWRR | ↑sn | |||
| Pirlindol | OIMAO-A | 70s | OIMAO-A | OIMAO-A | OIMAO-A | ↑snd | |
| Moclobemide | 80s | OIMAO-A | OIMAO-A | OIMAO-A | ↑snd | ||
| Fluoxetine | SSRI | 70s | IOZ | ↑С | |||
| Paroxetine | 70s | IOZ | ↑С | ||||
| Citalopram | 70s | IOZ | ↑С | ||||
| Fluvoxamine | 70s | IOZ | ↑С | ||||
| Sertraline | 80s | IOS | ↑С | ||||
| Escitalopram | 2000s | IOZ | ↑С | ||||
| Venlafaxine | SNRI | 80s | IOZ | IOZ | ↑SN | ||
| Venlafaxine** | 80s | IOZ | IOZ | IOZ | ↑SNd | ||
| Duloxetine | 80s | IOZ | IOZ | ↑SN | |||
| Milnacipran | 80s | IOZ | IOZ | SWRR | ↑snd | ||
| Mirtazapine | NaSSA | 80s | SWRR | SWRR | ↑sn | ||
| Agomelatine | MeA | 2000s | SWRR | SWRR | SWRR | ↑ndm | |
| Vortioxetine | mma | 2010s | IOZ | SWRR | SWRR | ↑snd | |
*- white color - the drug does not affect neurons, dark gray - a pronounced increase in activity, light gray - a moderate increase in activity,
**- in high doses
However, the vast majority of antidepressants used in Russia are classified as IOPs (Table 2). It is this pharmacological property that determines the ability to activate neurons in 66.7% of drugs related to tricyclic (TCA) and tetracyclic (TCA) antidepressants, as well as selective serotonin reuptake inhibitors (SSRIs) and selective serotonin and noradrenaline reuptake inhibitors (SNRIs) . Three more drugs (14.3%) combine the properties of IOP and SVR. Trazodone (a serotonin modulating antidepressant - CMA), milnacipran (SNRI) and vortioxetine (a multimodal antidepressant - MMA) have this mixed mechanism of action.
It is this pharmacological property that determines the ability to activate neurons in 66.7% of drugs related to tricyclic (TCA) and tetracyclic (TCA) antidepressants, as well as selective serotonin reuptake inhibitors (SSRIs) and selective serotonin and noradrenaline reuptake inhibitors (SNRIs) . Three more drugs (14.3%) combine the properties of IOP and SVR. Trazodone (a serotonin modulating antidepressant - CMA), milnacipran (SNRI) and vortioxetine (a multimodal antidepressant - MMA) have this mixed mechanism of action.
A similar situation is observed throughout the world. Most antidepressants are PIOs. For example, in the US, these include 8 of the 10 most commonly prescribed drugs (duloxetine, dezvenlafaxine, citalopram, setralin, fluoxetine, escitalopram, paroxetine, venlafaxine) (9). Another one - vilazodone - combines the property of the IOP with a different mechanism of action. In some countries (for example, the USA), the reputation of the PHI is so high that they try not to register antidepressants that do not have such a mechanism of action at all (10).
IOPs are not only allowed to enter the medical services market on a priority basis, but they are also considered a kind of “standard”. After all, their mechanism of action leaves neurotransmitters (serotonin, norepinephrine or dopamine) where they usually realize their effects - “between” neurons in the so-called. "intersynaptic gap" (5). As a result, serotonin, norepinephrine or dopamine act on nerve cells for a longer time, and neurons are activated more than usual. It is also important that this mechanism of action is completely reversible, since it does not contribute to the creation of new neurotransmitters (their synthesis) and does not inhibit their decay (metabolism). And this is very important for the safety of treatment.
But not all antidepressants are strong IODs (4, 5). For some drugs, this mechanism of action is much less pronounced (Table 2). Thus, pipofesin (TcA), which is indicated only for mild to moderate depression (11), most likely moderately activates serotonin, norepinephrine, and dopamine neurons. Trazodone (CmA) and vortioxetine (MmA) are the IOS of serotonin (Table 2). But this mechanism of action is less pronounced in them compared to SSRIs (4, 12).
Trazodone (CmA) and vortioxetine (MmA) are the IOS of serotonin (Table 2). But this mechanism of action is less pronounced in them compared to SSRIs (4, 12).
Antidepressants can only be strong PIDs on serotonin (SSRIs: sertraline, paroxetine, citalopram, escitalopram, fluoxetine, fluvoxamine, TcA: clomipramine), norepinephrine (NcA: maprotiline; SNRI: milnacipran), or both of these neurotransmitters (TcA: amitriptyline, imipramine; SNRIs: venlafaxine and duloxetine) (4, 5, 13, 14). With regard to dopamine, all modern drugs are only weak IODs (TcA: amitriptyline, imipramine, clomipramine, pipofezin; SNRI: venlafaxine in high daily doses), or they do not affect the metabolism of this neurotransmitter at all (4, 5, 6, 13, 14) . In addition, in some IODs, the ability to affect different nerve cells depends on the dose (7).
Thus, venlafaxine (SNRI), especially at low daily doses (75-150 mg), is more of an IOD of serotonin and affects serotonin neurons. At the same time, it has an active metabolite dezvenlafaxine. This substance abroad is itself an antidepressant, and its properties differ from venlafaxine. Dezvenlafaxine is a potent IRI of serotonin and norepinephrine, and at high doses is a weak IRI of dopamine. The amount of dezvenlafaxine is considered to be half of the prescribed daily dose of venlafaxine. With an increase in the dosage of the latter, the concentration in the blood of its active metabolite also increases. Accordingly, venlafaxine, administered at a dose of 150–225 mg/day, is converted by dezvenlafaxine to the IOD of serotonin and norepinephrine. As a result, it effectively activates serotonin and norepinephrine neurons (Table 2). If the daily dose is further increased, then venlafaxine (together with dezvenlafaxine) will acquire the properties of the IOP of dopamine. Then the drug will activate not only serotonin and norepinephrine neurons, but also dopamine neurons, although much weaker (Table 2).
This substance abroad is itself an antidepressant, and its properties differ from venlafaxine. Dezvenlafaxine is a potent IRI of serotonin and norepinephrine, and at high doses is a weak IRI of dopamine. The amount of dezvenlafaxine is considered to be half of the prescribed daily dose of venlafaxine. With an increase in the dosage of the latter, the concentration in the blood of its active metabolite also increases. Accordingly, venlafaxine, administered at a dose of 150–225 mg/day, is converted by dezvenlafaxine to the IOD of serotonin and norepinephrine. As a result, it effectively activates serotonin and norepinephrine neurons (Table 2). If the daily dose is further increased, then venlafaxine (together with dezvenlafaxine) will acquire the properties of the IOP of dopamine. Then the drug will activate not only serotonin and norepinephrine neurons, but also dopamine neurons, although much weaker (Table 2).
Turning now to SVR (mianserin - HcA, mirtazapine - norepinephrine and selective serotonin antidepressant - NaSSA, agomelatine - melatonergic antidepressant), let's point out the reason why they lose at least strong IOPs in the effectiveness of their effect on neurons (Table 2). ). With the help of PP, it is not the excitation of nerve cells, but rather the “fine tuning” of their “tone” (5, 8, 15). Therefore, "pure" SVRs are quite rare among antidepressants.
). With the help of PP, it is not the excitation of nerve cells, but rather the “fine tuning” of their “tone” (5, 8, 15). Therefore, "pure" SVRs are quite rare among antidepressants.
On the other hand, there are many IOPs in which the effect on the RR is an additional mechanism of action. But due to its relative weakness, it is not even mentioned in the drug instructions (16, 17, 18). For example, milnacipran (SNRI) refers to the IOD of serotonin and norepinephrine (16). This property gives the antidepressant the ability to effectively activate norepinephrine neurons and, to a lesser extent, serotonin neurons (6). At the same time, milnacipran, due to its effect on RR, contributes to a moderate increase in the “tone” of dopamine nerve cells (19). However, this property is not mentioned in the drug instructions. And only in some IOPs, the effect on RR is still mentioned in the guidelines for the medical use of antidepressants. This feature is characteristic of trazodone (CmA) and vortioxetine (MmA) (5, 8, 20). Both antidepressants are IOS serotonin. This property allows them to moderately activate serotonin neurons (Table 2). And due to the effect on the RR, they slightly increase the "tone" of norepinephrine and dopamine nerve cells.
Both antidepressants are IOS serotonin. This property allows them to moderately activate serotonin neurons (Table 2). And due to the effect on the RR, they slightly increase the "tone" of norepinephrine and dopamine nerve cells.
Finally, two more drugs (OIMAO-A: pirlindol and moclobemide) to activate neurons inhibit (inhibit) the work of an enzyme - monoamine oxidase, which destroys neurotransmitters (serotonin, norepinephrine, dopamine) (5, 20, 21, 22, 23), as inside neurons, and outside them - in the intersynaptic gap. It would seem that this mechanism of action should be very strong, because as a result, the amount of serotonin, norepinephrine and dopamine increases both inside the neuron and outside it. However, this effect is typical, first of all, for the so-called. irreversible inhibitors of monoamine oxidase, which form stable chemical bonds with this enzyme (24). After that, it can no longer perform its functions and breaks down, and instead the body is forced to synthesize a new enzyme, which usually takes about two weeks. As a result, irreversible monoamine oxidase inhibitors are indeed highly active antidepressants. However, due to the high efficiency of the mechanism of action, they are poorly tolerated, they can even be toxic, and their use in our country has practically ceased.
As a result, irreversible monoamine oxidase inhibitors are indeed highly active antidepressants. However, due to the high efficiency of the mechanism of action, they are poorly tolerated, they can even be toxic, and their use in our country has practically ceased.
A different picture is observed in the case of pirlindol and moclobemide (20, 22). The effect of these drugs on the enzyme is reversible (RIMAO). The fact is that their relationship with the enzyme is only relatively stable. Its gradual disappearance leads to the release of monoamine oxidase, while the enzyme itself remains intact (24). In addition, pirlindol and moclobemide selectively inhibit the activity of only one of the types of monoamine oxide - "A" (OIMAO-A), while the other type "B" continues to work almost with the same strength. All these features significantly reduce the effectiveness of RIMAO-A, which is why the considered mechanism of action is much less common than IOP (Table 2). At the same time, these features make RIMAO-A more tolerable drugs that weakly activate serotonin, norepinephrine, and dopamine neurons.
The presented features of the mechanisms of action of antidepressants can be represented as a letter formula consisting of the first letters of the name of the neuron on which it acts (↑s, ↑n, ↑n, ↑m). Moreover, in the case of pronounced activation of the nerve cell, you can use an uppercase letter (↑С, ↑Н, ↑Д, ↑М), and with a weak one - a lowercase letter (↑s, ↑n, ↑d, ↑m). It turns out an individual "formula" of the mechanism of action of an antidepressant (hereinafter simply "formula"), which reflects its pharmacological activity much more accurately than the name of the group.
Such "formulas" testify to the existence of "triple" action drugs. These include:
- ↑SND-antidepressants (active effect on serotonin and norepinephrine neurons and weaker effect on dopamine neurons):
- amitriptyline (TcA),
- imipramine (TCA)
- venlafaxine (SNRI) in high daily doses
- ↑ SND-antidepressants (active effect on serotonin neurons and weaker effect on noradrenaline and dopamine neurons):
- clomipramine (TCA)
- ↑SND-antidepressants (active effect on norepinephrine neurons and weaker effect on serotonin and dopamine neurons):
- milnacipran (SNRI)
- ↑SND-antidepressants (weak effect on serotonin, norepinephrine and dopamine neurons):
- pipofezin (TCA),
- pirlindol (OIMAO-A),
- moclobemide (OIMAO-A),
- trazodone (CmA),
- vortioxetine (Mma)
- ↑ndm-antidepressants (weak effect on norepinephrine, dopamine and melatonin neurons):
- agomelatine (MeA)
There are drugs "double" action. These include:
These include:
- ↑CH-antidepressants (active effect on serotonin and norepinephrine neurons):
- duloxetine (SNRI)
- venlafaxine (SNRI) at average daily doses
- ↑CH-antidepressants (active effect on serotonin neurons and weak on norepinephrine)
- maprotiline (ncA)
- ↑sn-antidepressants (weak effect on serotonin and norepinephrine neurons)
- mianserin (NZA),
- mirtazapine (HaSSA)
Finally, single-acting drugs include:
- ↑C-antidepressants (active effect on serotonin neurons):
- sertraline (SSRI),
- paroxetine (SSRI),
- citalopram (SSRI),
- escitalopram (SSRI),
- fluoxetine (SSRI),
- fluvoxamine (SSRI).
The presented data make it easy to determine that the most effective antidepressants will be "triple" action, whose formula contains the largest number of capital letters. These are ↑SNd-antidepressants that actively affect serotonin and norepinephrine neurons and, to a lesser extent, dopamine neurons: amitriptyline (TcA), imipramine (TcA), venlafaxine (SNRI) in high daily doses. This set of pharmacological properties allows them to influence all three variants of depression (↓ND with a decrease in positive emotions; ↓SN with an increase in negative emotions; ↓SDI-depression with a decrease in positive and an increase in negative emotions), which may be accompanied by phenomena of psychomotor retardation (↓ H-symptoms) and/or somatic symptoms (↓SNM or ↓SNM).
These are ↑SNd-antidepressants that actively affect serotonin and norepinephrine neurons and, to a lesser extent, dopamine neurons: amitriptyline (TcA), imipramine (TcA), venlafaxine (SNRI) in high daily doses. This set of pharmacological properties allows them to influence all three variants of depression (↓ND with a decrease in positive emotions; ↓SN with an increase in negative emotions; ↓SDI-depression with a decrease in positive and an increase in negative emotions), which may be accompanied by phenomena of psychomotor retardation (↓ H-symptoms) and/or somatic symptoms (↓SNM or ↓SNM).
The presented very short list of the most effective antidepressants correlates well with the "personal experience" of foreign experts who create recommendations. It has already been mentioned above that TcA and SNRIs are recognized as the most powerful drugs there (4). Some recommendations have more precise instructions. It reports that, along with TcA, only one SNRI, venlafaxine, is the most effective (3). But experts always stipulate that they cannot provide any objective evidence of their point of view. One can only regret that they did not want to turn to the features of the formation of symptoms of depression and the mechanism of action of antidepressants. If we take into account the relationship between them, then the "personal experience" of experts becomes quite understandable and even "public".
But experts always stipulate that they cannot provide any objective evidence of their point of view. One can only regret that they did not want to turn to the features of the formation of symptoms of depression and the mechanism of action of antidepressants. If we take into account the relationship between them, then the "personal experience" of experts becomes quite understandable and even "public".
This analysis puts venlafaxine in an exceptional position, especially in our country. It is well known that in Russia TcA (amitriptyline and imipramine) are prescribed very sparingly in low doses, which are usually less than therapeutic doses (25, 26). This is due to the pronounced side effects inherent in amitriptyline and imipramine. Meanwhile, any drug, including TcA, when administered at doses that do not reach the therapeutic range, loses its effectiveness. As a result, in our country, only venlafaxine can claim to be the most effective antidepressant. And this drug is widely used in our country in the form of Velaksin (Egis). He was recommended by leading scientific organizations carrying out cutting-edge research in the field of psychiatry. Among them are the Federal State Budgetary Institutions “State Scientific Center for Social and Forensic Psychiatry named after V.P. Serbsky" and "Moscow Research Institute of Psychiatry" of the Ministry of Health of Russia, St. Petersburg Research Institute. V.M. Bekhterev (27, 28). Long-acting capsules (Velaxin retard) are also well known (29), which have been shown to significantly reduce the side effect of the drug, such as nausea (30). In addition, the study of Velaksin was successfully carried out not only in psychiatry, but also in neurology (31). It remains to recommend that this antidepressant be used as widely as possible in the treatment of depression.
He was recommended by leading scientific organizations carrying out cutting-edge research in the field of psychiatry. Among them are the Federal State Budgetary Institutions “State Scientific Center for Social and Forensic Psychiatry named after V.P. Serbsky" and "Moscow Research Institute of Psychiatry" of the Ministry of Health of Russia, St. Petersburg Research Institute. V.M. Bekhterev (27, 28). Long-acting capsules (Velaxin retard) are also well known (29), which have been shown to significantly reduce the side effect of the drug, such as nausea (30). In addition, the study of Velaksin was successfully carried out not only in psychiatry, but also in neurology (31). It remains to recommend that this antidepressant be used as widely as possible in the treatment of depression.
M.Yu Drobizhev's video on the same topic can be viewed at the link: https://youtu.be/C4J_SaQb1uw
References.
- depression.
 The treatment and management of depression in adults (updated edition). National Clinical Practice Guideline 90. https://www.nice.org.uk/guidance/cg90/evidence/full-guidance-243833293
The treatment and management of depression in adults (updated edition). National Clinical Practice Guideline 90. https://www.nice.org.uk/guidance/cg90/evidence/full-guidance-243833293 - Won E, Park SC, Han KM, Sung SH, Lee HY, Paik JW, Jeon HJ, Lee MS, Shim SH, Ko YH, Lee KJ, Han C, Ham BJ, Choi J, Hwang TY, Oh KS, Hahn SW , Park YC, Lee MS J Evidence-based, pharmacological treatment guideline for depression in Korea, revised edition. Korean Med Sci. 2014 Apr;29(4):468-84. doi: 10.3346/jkms.2014.29.4.468.
- Bauer M., Pfennig A., Severus E., Weibrau P.S., J. Angst, Müller H.-J. Clinical guidelines of the World Federation of Societies of Biological Psychiatry for the biological therapy of unipolar depressive disorders. Part 1: Acute and ongoing treatment of unipolar depressive disorders as of 2013. Modern therapy of mental disorders 2015;4:33-39.
- Antidepressant therapy and other treatments for depressive disorders. Report of the CINP Working Group based on a review of the evidence.
 Ed. V.N. Krasnova. M., 2008. - 215 S.
Ed. V.N. Krasnova. M., 2008. - 215 S. - Stahl S.M. Stahl's essential psychopharmacology: neuroscientific basis and practical application. — 3nd ed. Cambridge University Press, 2008. - 1117P.
- Drobizhev M. Yu., Fedotova A. V., Kikta S. V., Antokhin E. Yu. Between depression and fibromyalgia: the fate of an antidepressant. Journal of Neurology and Psychiatry. S.S. Korsakov. 2016;116(4): 114-120. DOI:10.17116/jnevro201611641114-120.
- Drobizhev M.Yu., Kikta S.V., Fedotova A.V., Serdyuk O.V. Just depression. Questions and answers. LLC "Marketing Machine" M., 2013. 100C.).
- Shagiakhmetov F.Sh., Anokhin P.K., Shamakina I.Yu. Vortioxetine: mechanisms of multimodality and clinical efficacy. Social and Clinical Psychiatry 2016;26(4): 84-96
- Hrenchir T. 10 Most-Prescribed Antidepressant Medications. http://www.newsmax.com/Health/Health-Wire/most-prescribed-antidepressant-medications/2015/09/02/id/673123/
- Pae CU Agomelatine: a new option for treatment of depression? Expert Opin Pharmacother.
 2014 Mar;15(4):443-7. doi:10.1517/14656566.2014.877889.).
2014 Mar;15(4):443-7. doi:10.1517/14656566.2014.877889.). - Azafen MB - official instructions for use. https://medi.ru/instrukciya/azafen-mb_9646/
- Sanchez C, Asin KE, Artigas F. Vortioxetine, a novel antidepressant with multimodal activity: review of preclinical and clinical data. Pharmacol Ther. Jan 2015;145:43-57. Doi:10.1016/j.pharmthera.2014.07.001
- Sharma H, Santra S, Dutta A. Triple reuptake inhibitors as potential next-generation antidepressants: a new hope? Future Medical Chem. 2015;7(17):2385-406. Doi: 10.4155/fmc.15.134.
- Stahl SM, Grady MM, Moret C, Briley M. SNRIs: their pharmacology, clinical efficacy, and tolerability in comparison with other classes of antidepressants. CNS Spectr. 2005;10:732-747.
- Valdoxan - official instructions for use. https://medi.ru/instrukciya/valdoksan_5084/.
- Ixel - official instructions for use. https://medi.ru/instrukciya/iksel_11711/
- Prozac - official instructions for use.
 https://medi.ru/instrukciya/prozak_10337/
https://medi.ru/instrukciya/prozak_10337/ - Saroten - official instructions for use. https://medi.ru/instrukciya/saroten_11880/
- Kohno T, Kimura M, Sasaki M, Obata H, Amaya F, Saito S. Milnacipran inhibits glutamatergic N-methyl-D-aspartate receptor activity in spinal dorsal horn neurons. Mol Pain. 2012 Jun 19;8:45.
- Brintellix (Brintellix). https://www.rlsnet.ru/tn_index_id_87791.htm4
- Mashkovsky M.D., Andreeva N.I., Polezhaeva A.I. Pharmacology of antidepressants - M., Medicine, 1983. -240С.
- Pyrazidol - official instructions for use. https://medi.ru/instrukciya/pirazidol_10633/
- Aurorix (Aurorix) https://www.rlsnet.ru/tn_index_id_419.htm
- Bykov Yu. V., Bekker R. A., Reznikov M. K. Resistant depressions. Practical guide. - Kyiv: Medkniga, 2013. - 400 p. - ISBN 978-966-1597-14-2.
- Serdyuk O.V., Ovchinnikov A.A., Kutuzova N.A., Drobizhev M.Yu., Retyunsky K.
 Yu. The practice of using antidepressants in psychiatry (CIRKADIAN-I program). Doctor. 2010:2; 2-5.15.
Yu. The practice of using antidepressants in psychiatry (CIRKADIAN-I program). Doctor. 2010:2; 2-5.15. - Drobizhev M.Yu., Ovchinnikov A.A. Kikta S.V. Mechanisms of action of antidepressants and pathogenesis of mental disorders. What are the matches? Social and Clinical Psychiatry 2017. 27(3):94-101.
- Krasnov VN, Kryukov VV Velaxin® (venlafaxine) in the modern therapy of depression: results of the first Russian multicenter efficacy and safety study. Psychiatry and psychopharmacotherapy. 2007;9(4), http://www.consilium-medicum.com/magazines/special/psychiatry/article/15426
- Mosolov S.N., Kostyukova E.G., Gorodnichev A.V., Timofeev I.V., Ladyzhensky M.Ya., Serditov O.V. Clinical efficacy and tolerability of venlafaxine (Velaxin) in the treatment of moderate and severe depression. Modern therapy of mental disorders. 2007;3:58-63.
- Avedisova A.S., Zakharova K.V., Kanaeva L.S., Vazagaeva T.I., Aldushin A.A. Psychiatry and psychopharmacotherapy.
 2009;11(1):36-40.
2009;11(1):36-40. - Avedisova A.S. Venlafaxine (velaxin): results of international trials of a third-generation antidepressant. Psychiatrist. and a psychopharmacologist. 2006; 11(2):2-7.
- Mosolov S.N. Clinical use of modern antidepressants. SPb., 1995.-565C.
M.Yu. Drobizhev, Doctor of Medical Sciences, Head of the Educational Department of the Training Center of the Association of Medical and Pharmaceutical Universities of Russia
Contact information – [email protected]
E.Yu. Antokhin, Candidate of Medical Sciences, Associate Professor, Head of the Department of Clinical Psychology and Psychotherapy, Orenburg State Medical University, Ministry of Health of Russia.
R.I. Palaeva – Assistant of the Department of Clinical Psychology and Psychotherapy of FSBEI HE “Orenburg State Medical University” of the Ministry of Health of Russia.