Mental illness and symptoms
Mental illness - Symptoms and causes
Overview
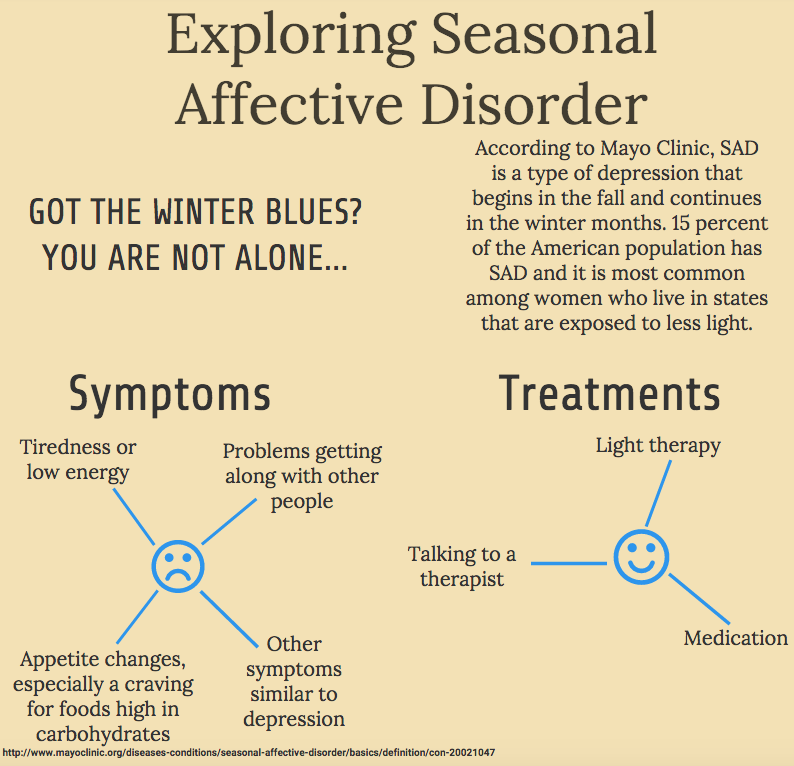
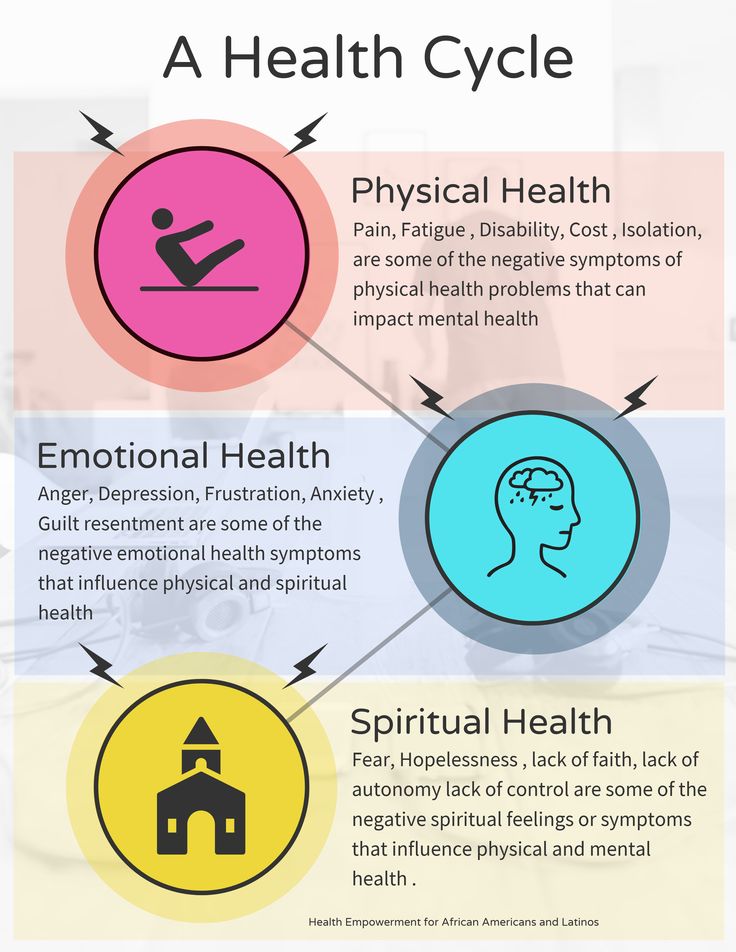
Mental illness, also called mental health disorders, refers to a wide range of mental health conditions — disorders that affect your mood, thinking and behavior. Examples of mental illness include depression, anxiety disorders, schizophrenia, eating disorders and addictive behaviors.
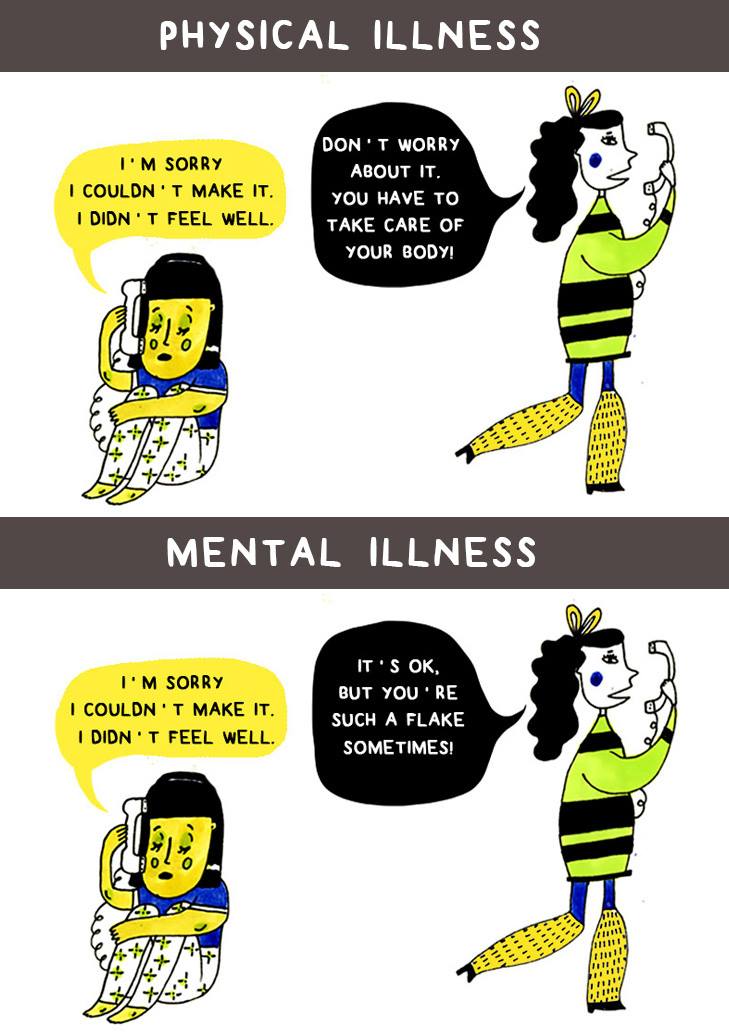
Many people have mental health concerns from time to time. But a mental health concern becomes a mental illness when ongoing signs and symptoms cause frequent stress and affect your ability to function.
A mental illness can make you miserable and can cause problems in your daily life, such as at school or work or in relationships. In most cases, symptoms can be managed with a combination of medications and talk therapy (psychotherapy).
Products & Services
- Book: Mayo Clinic Family Health Book, 5th Edition
- Newsletter: Mayo Clinic Health Letter — Digital Edition
Symptoms
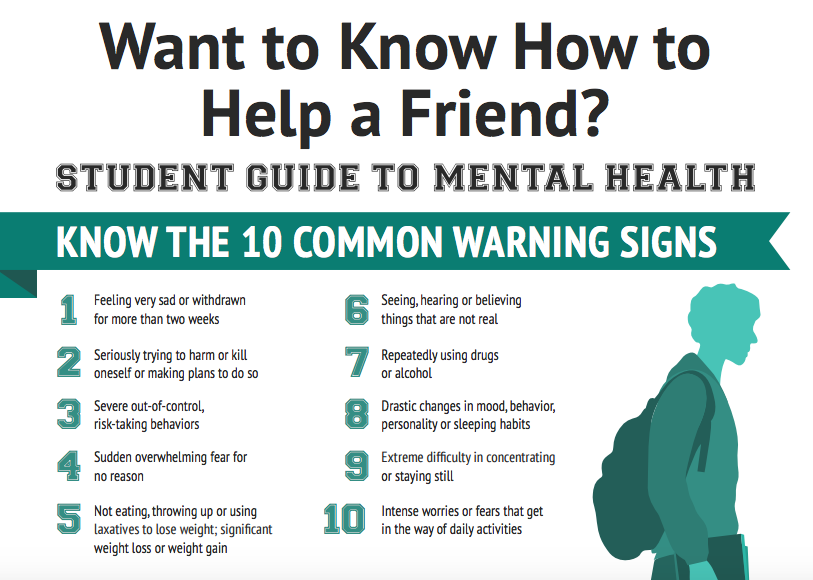
Signs and symptoms of mental illness can vary, depending on the disorder, circumstances and other factors. Mental illness symptoms can affect emotions, thoughts and behaviors.
Examples of signs and symptoms include:
- Feeling sad or down
- Confused thinking or reduced ability to concentrate
- Excessive fears or worries, or extreme feelings of guilt
- Extreme mood changes of highs and lows
- Withdrawal from friends and activities
- Significant tiredness, low energy or problems sleeping
- Detachment from reality (delusions), paranoia or hallucinations
- Inability to cope with daily problems or stress
- Trouble understanding and relating to situations and to people
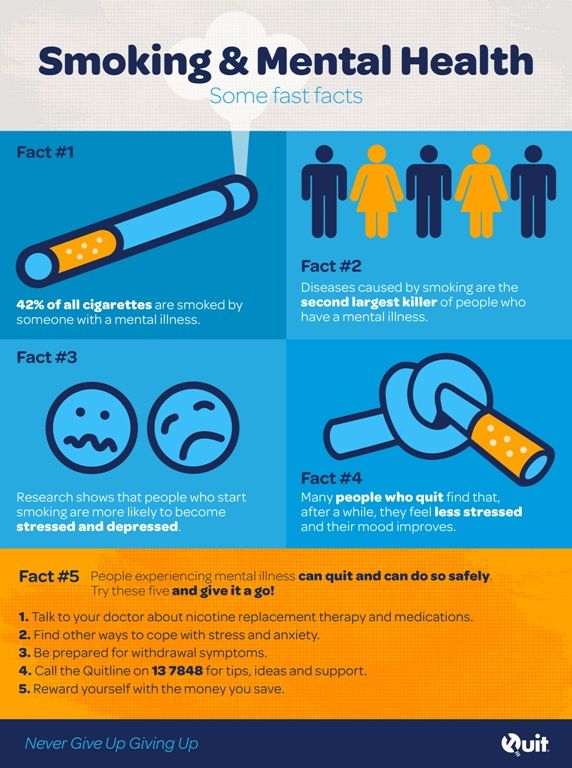
- Problems with alcohol or drug use
- Major changes in eating habits
- Sex drive changes
- Excessive anger, hostility or violence
- Suicidal thinking
Sometimes symptoms of a mental health disorder appear as physical problems, such as stomach pain, back pain, headaches, or other unexplained aches and pains.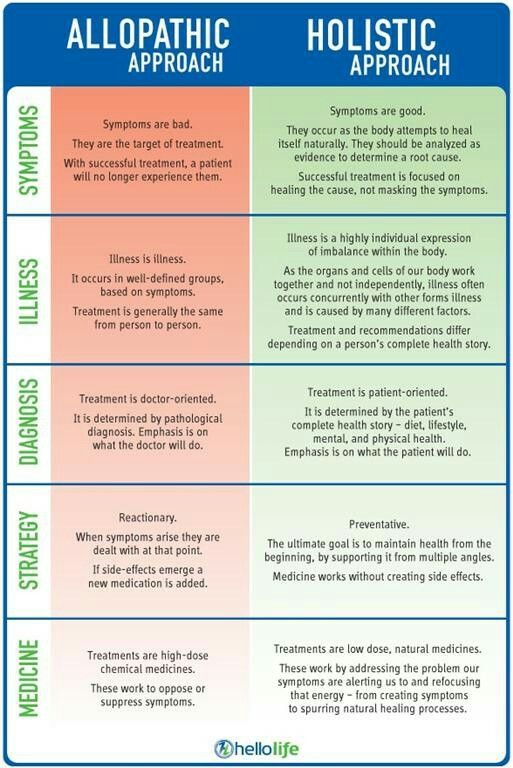
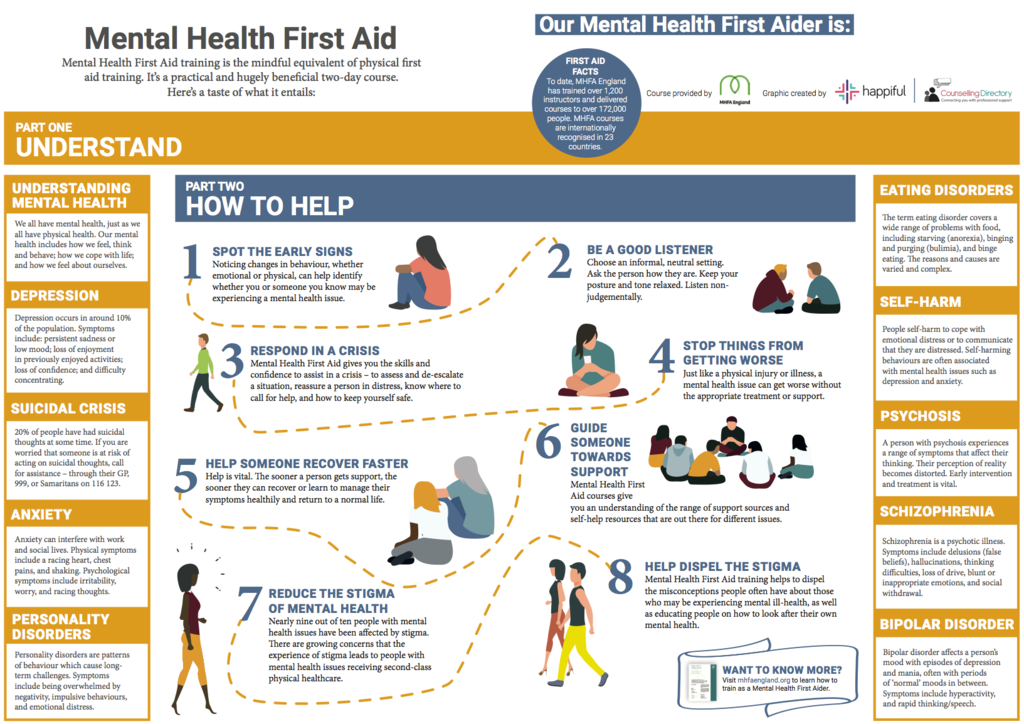
When to see a doctor
If you have any signs or symptoms of a mental illness, see your primary care provider or a mental health professional. Most mental illnesses don't improve on their own, and if untreated, a mental illness may get worse over time and cause serious problems.
If you have suicidal thoughts
Suicidal thoughts and behavior are common with some mental illnesses. If you think you may hurt yourself or attempt suicide, get help right away:
- Call 911 or your local emergency number immediately.
- Call your mental health specialist.
- Contact a suicide hotline. In the U.S., call or text 988 to reach the 988 Suicide & Crisis Lifeline, available 24 hours a day, seven days a week. Or use the Lifeline Chat. Services are free and confidential.
- Seek help from your primary care provider.
- Reach out to a close friend or loved one.
- Contact a minister, spiritual leader or someone else in your faith community.
Suicidal thinking doesn't get better on its own — so get help.
Helping a loved one
If your loved one shows signs of mental illness, have an open and honest discussion with him or her about your concerns. You may not be able to force someone to get professional care, but you can offer encouragement and support. You can also help your loved one find a qualified mental health professional and make an appointment. You may even be able to go along to the appointment.
If your loved one has done self-harm or is considering doing so, take the person to the hospital or call for emergency help.
Request an appointment
From Mayo Clinic to your inbox
Sign up for free, and stay up to date on research advancements, health tips and current health topics, like COVID-19, plus expertise on managing health. Click here for an email preview.
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you.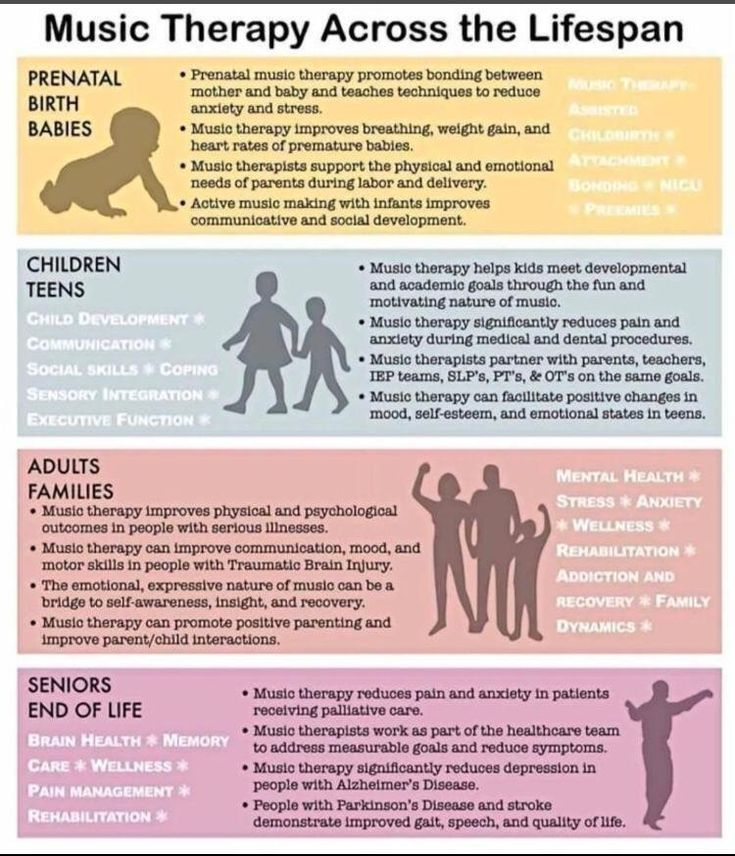 If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
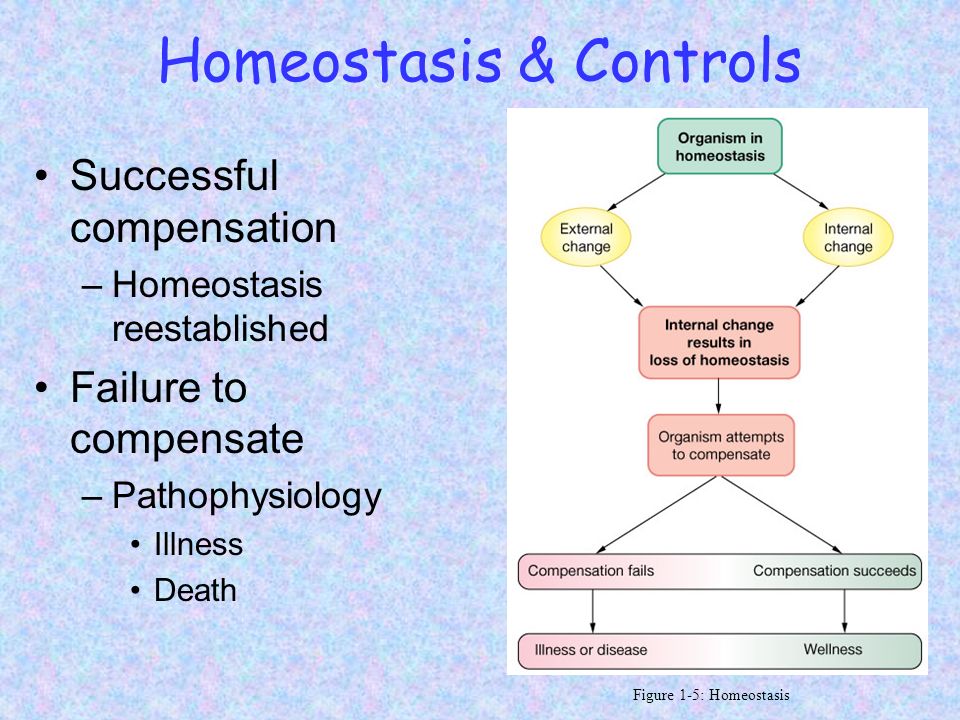
Causes
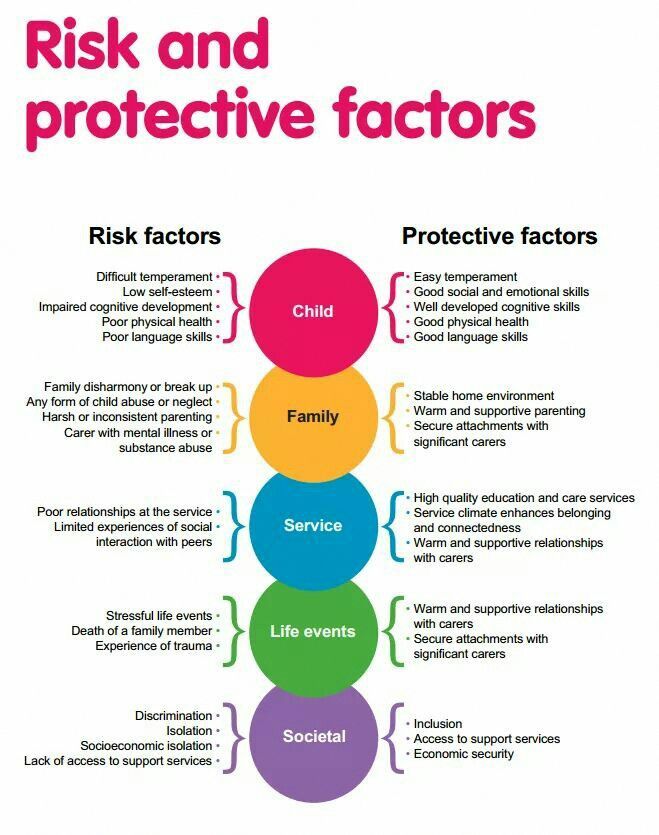
Mental illnesses, in general, are thought to be caused by a variety of genetic and environmental factors:
- Inherited traits. Mental illness is more common in people whose blood relatives also have a mental illness. Certain genes may increase your risk of developing a mental illness, and your life situation may trigger it.
- Environmental exposures before birth.
 Exposure to environmental stressors, inflammatory conditions, toxins, alcohol or drugs while in the womb can sometimes be linked to mental illness.
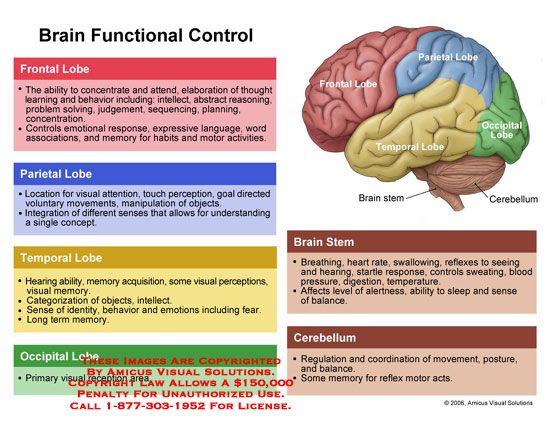
Exposure to environmental stressors, inflammatory conditions, toxins, alcohol or drugs while in the womb can sometimes be linked to mental illness. - Brain chemistry. Neurotransmitters are naturally occurring brain chemicals that carry signals to other parts of your brain and body. When the neural networks involving these chemicals are impaired, the function of nerve receptors and nerve systems change, leading to depression and other emotional disorders.
Risk factors
Certain factors may increase your risk of developing a mental illness, including:
- A history of mental illness in a blood relative, such as a parent or sibling
- Stressful life situations, such as financial problems, a loved one's death or a divorce
- An ongoing (chronic) medical condition, such as diabetes
- Brain damage as a result of a serious injury (traumatic brain injury), such as a violent blow to the head
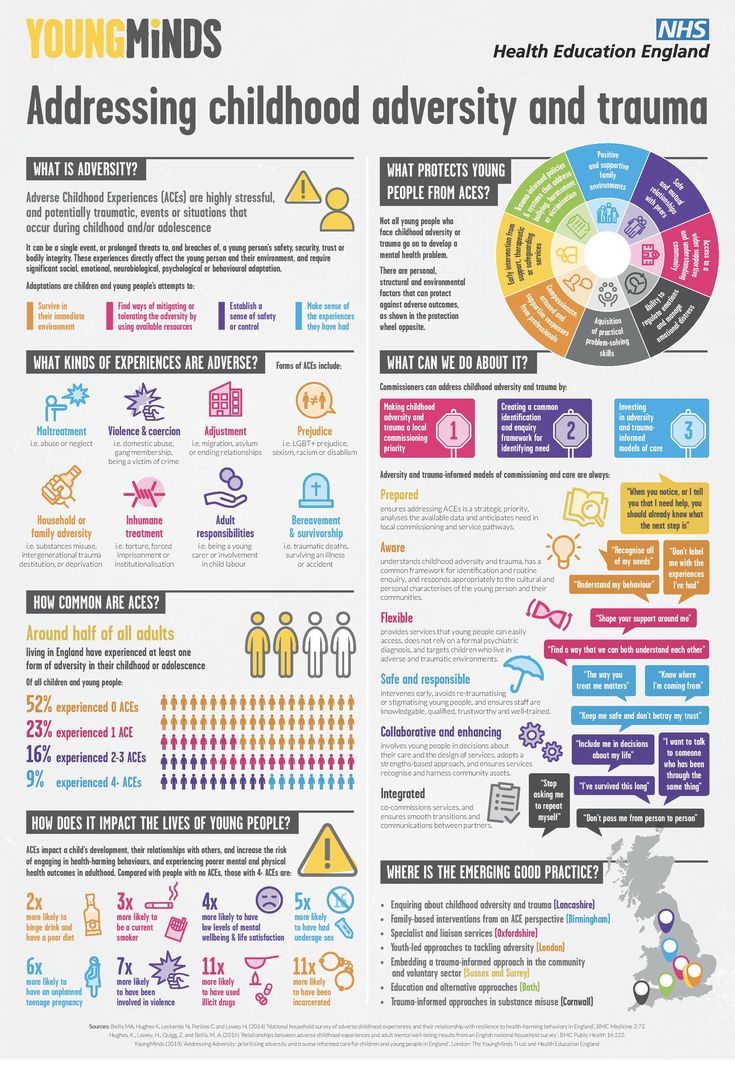
- Traumatic experiences, such as military combat or assault
- Use of alcohol or recreational drugs
- A childhood history of abuse or neglect
- Few friends or few healthy relationships
- A previous mental illness
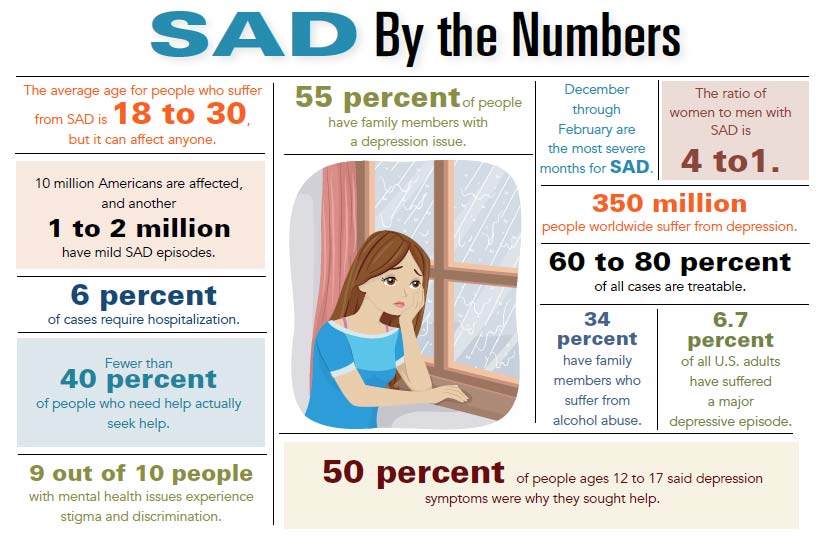
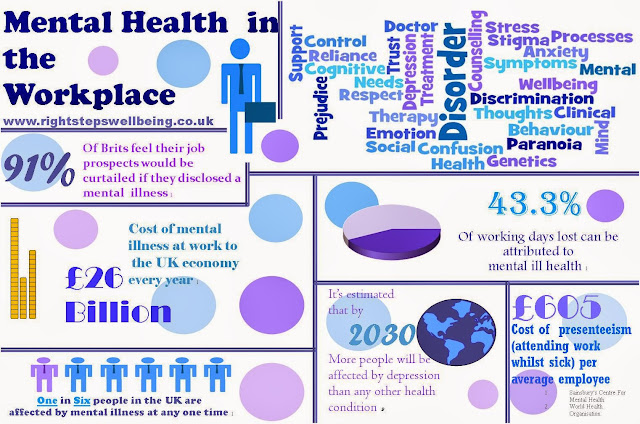
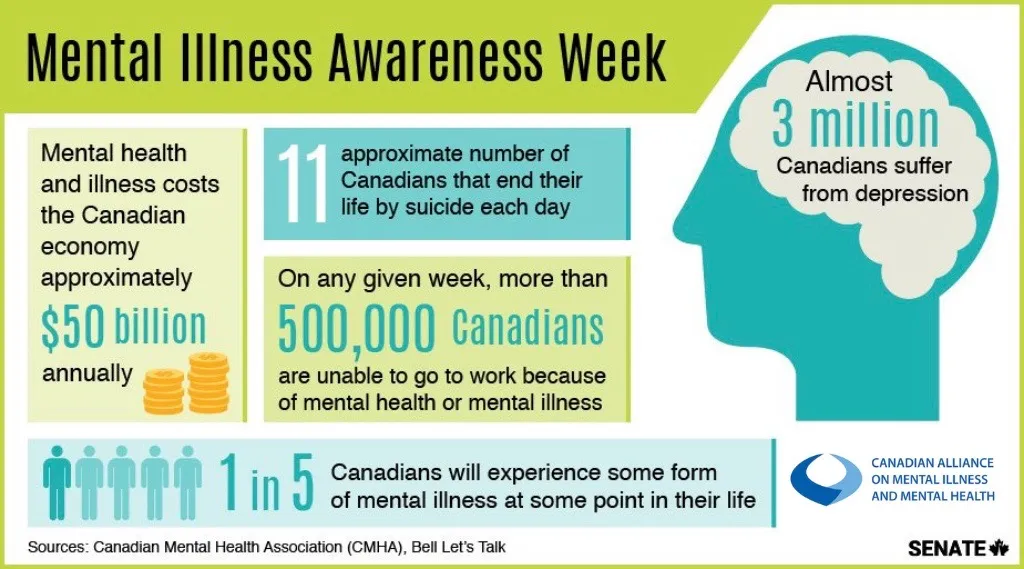
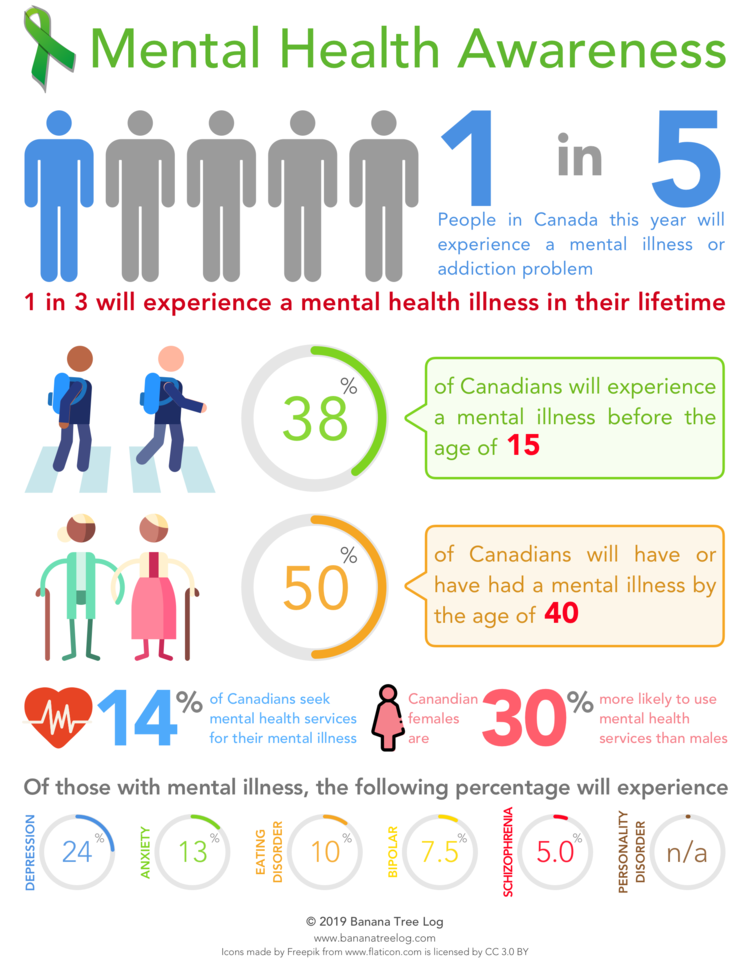
Mental illness is common.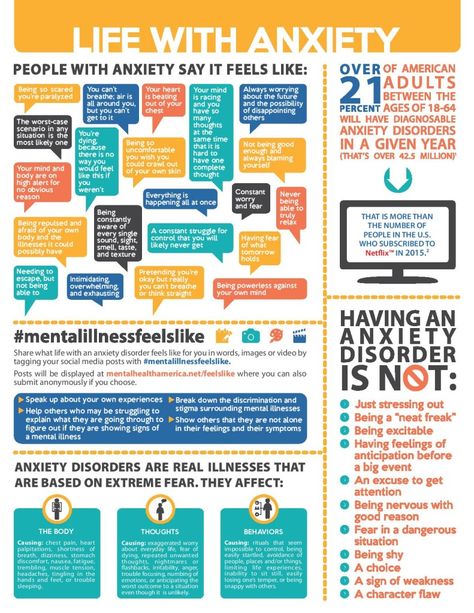 About 1 in 5 adults has a mental illness in any given year. Mental illness can begin at any age, from childhood through later adult years, but most cases begin earlier in life.
About 1 in 5 adults has a mental illness in any given year. Mental illness can begin at any age, from childhood through later adult years, but most cases begin earlier in life.
The effects of mental illness can be temporary or long lasting. You also can have more than one mental health disorder at the same time. For example, you may have depression and a substance use disorder.
Complications
Mental illness is a leading cause of disability. Untreated mental illness can cause severe emotional, behavioral and physical health problems. Complications sometimes linked to mental illness include:
- Unhappiness and decreased enjoyment of life
- Family conflicts
- Relationship difficulties
- Social isolation
- Problems with tobacco, alcohol and other drugs
- Missed work or school, or other problems related to work or school
- Legal and financial problems
- Poverty and homelessness
- Self-harm and harm to others, including suicide or homicide
- Weakened immune system, so your body has a hard time resisting infections
- Heart disease and other medical conditions
Prevention
There's no sure way to prevent mental illness. However, if you have a mental illness, taking steps to control stress, to increase your resilience and to boost low self-esteem may help keep your symptoms under control. Follow these steps:
However, if you have a mental illness, taking steps to control stress, to increase your resilience and to boost low self-esteem may help keep your symptoms under control. Follow these steps:
- Pay attention to warning signs. Work with your doctor or therapist to learn what might trigger your symptoms. Make a plan so that you know what to do if symptoms return. Contact your doctor or therapist if you notice any changes in symptoms or how you feel. Consider involving family members or friends to watch for warning signs.
- Get routine medical care. Don't neglect checkups or skip visits to your primary care provider, especially if you aren't feeling well. You may have a new health problem that needs to be treated, or you may be experiencing side effects of medication.
- Get help when you need it. Mental health conditions can be harder to treat if you wait until symptoms get bad. Long-term maintenance treatment also may help prevent a relapse of symptoms.
- Take good care of yourself. Sufficient sleep, healthy eating and regular physical activity are important. Try to maintain a regular schedule. Talk to your primary care provider if you have trouble sleeping or if you have questions about diet and physical activity.
By Mayo Clinic Staff
Related
Associated Procedures
News from Mayo Clinic
Products & Services
Mental illness - Diagnosis and treatment
Diagnosis
To determine a diagnosis and check for related complications, you may have:
- A physical exam. Your doctor will try to rule out physical problems that could cause your symptoms.
- Lab tests. These may include, for example, a check of your thyroid function or a screening for alcohol and drugs.
- A psychological evaluation. A doctor or mental health professional talks to you about your symptoms, thoughts, feelings and behavior patterns.
 You may be asked to fill out a questionnaire to help answer these questions.
You may be asked to fill out a questionnaire to help answer these questions.
Determining which mental illness you have
Sometimes it's difficult to find out which mental illness may be causing your symptoms. But taking the time and effort to get an accurate diagnosis will help determine the appropriate treatment. The more information you have, the more you will be prepared to work with your mental health professional in understanding what your symptoms may represent.
The defining symptoms for each mental illness are detailed in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), published by the American Psychiatric Association. This manual is used by mental health professionals to diagnose mental conditions and by insurance companies to reimburse for treatment.
Classes of mental illness
The main classes of mental illness are:
- Neurodevelopmental disorders. This class covers a wide range of problems that usually begin in infancy or childhood, often before the child begins grade school.
 Examples include autism spectrum disorder, attention-deficit/hyperactivity disorder (ADHD) and learning disorders.
Examples include autism spectrum disorder, attention-deficit/hyperactivity disorder (ADHD) and learning disorders. - Schizophrenia spectrum and other psychotic disorders. Psychotic disorders cause detachment from reality — such as delusions, hallucinations, and disorganized thinking and speech. The most notable example is schizophrenia, although other classes of disorders can be associated with detachment from reality at times.
- Bipolar and related disorders. This class includes disorders with alternating episodes of mania — periods of excessive activity, energy and excitement — and depression.
- Depressive disorders. These include disorders that affect how you feel emotionally, such as the level of sadness and happiness, and they can disrupt your ability to function. Examples include major depressive disorder and premenstrual dysphoric disorder.
- Anxiety disorders. Anxiety is an emotion characterized by the anticipation of future danger or misfortune, along with excessive worrying.
 It can include behavior aimed at avoiding situations that cause anxiety. This class includes generalized anxiety disorder, panic disorder and phobias.
It can include behavior aimed at avoiding situations that cause anxiety. This class includes generalized anxiety disorder, panic disorder and phobias. - Obsessive-compulsive and related disorders. These disorders involve preoccupations or obsessions and repetitive thoughts and actions. Examples include obsessive-compulsive disorder, hoarding disorder and hair-pulling disorder (trichotillomania).
- Trauma- and stressor-related disorders. These are adjustment disorders in which a person has trouble coping during or after a stressful life event. Examples include post-traumatic stress disorder (PTSD) and acute stress disorder.
- Dissociative disorders. These are disorders in which your sense of self is disrupted, such as with dissociative identity disorder and dissociative amnesia.
- Somatic symptom and related disorders. A person with one of these disorders may have physical symptoms that cause major emotional distress and problems functioning.
 There may or may not be another diagnosed medical condition associated with these symptoms, but the reaction to the symptoms is not normal. The disorders include somatic symptom disorder, illness anxiety disorder and factitious disorder.
There may or may not be another diagnosed medical condition associated with these symptoms, but the reaction to the symptoms is not normal. The disorders include somatic symptom disorder, illness anxiety disorder and factitious disorder. - Feeding and eating disorders. These disorders include disturbances related to eating that impact nutrition and health, such as anorexia nervosa and binge-eating disorder.
- Elimination disorders. These disorders relate to the inappropriate elimination of urine or stool by accident or on purpose. Bed-wetting (enuresis) is an example.
- Sleep-wake disorders. These are disorders of sleep severe enough to require clinical attention, such as insomnia, sleep apnea and restless legs syndrome.
- Sexual dysfunctions. These include disorders of sexual response, such as premature ejaculation and female orgasmic disorder.
- Gender dysphoria.
 This refers to the distress that accompanies a person's stated desire to be another gender.
This refers to the distress that accompanies a person's stated desire to be another gender. - Disruptive, impulse-control and conduct disorders. These disorders include problems with emotional and behavioral self-control, such as kleptomania or intermittent explosive disorder.
- Substance-related and addictive disorders. These include problems associated with the excessive use of alcohol, caffeine, tobacco and drugs. This class also includes gambling disorder.
- Neurocognitive disorders. Neurocognitive disorders affect your ability to think and reason. These acquired (rather than developmental) cognitive problems include delirium, as well as neurocognitive disorders due to conditions or diseases such as traumatic brain injury or Alzheimer's disease.
- Personality disorders. A personality disorder involves a lasting pattern of emotional instability and unhealthy behavior that causes problems in your life and relationships.
 Examples include borderline, antisocial and narcissistic personality disorders.
Examples include borderline, antisocial and narcissistic personality disorders. - Paraphilic disorders. These disorders include sexual interest that causes personal distress or impairment or causes potential or actual harm to another person. Examples are sexual sadism disorder, voyeuristic disorder and pedophilic disorder.
- Other mental disorders. This class includes mental disorders that are due to other medical conditions or that don't meet the full criteria for one of the above disorders.
Treatment
Your treatment depends on the type of mental illness you have, its severity and what works best for you. In many cases, a combination of treatments works best.
If you have a mild mental illness with well-controlled symptoms, treatment from your primary care provider may be sufficient. However, often a team approach is appropriate to make sure all your psychiatric, medical and social needs are met. This is especially important for severe mental illnesses, such as schizophrenia.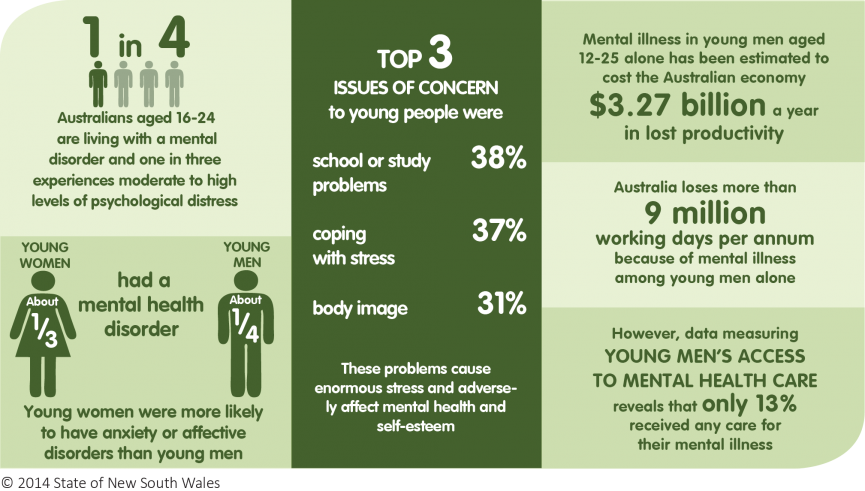
Your treatment team
Your treatment team may include your:
- Family or primary care doctor
- Nurse practitioner
- Physician assistant
- Psychiatrist, a medical doctor who diagnoses and treats mental illnesses
- Psychotherapist, such as a psychologist or a licensed counselor
- Pharmacist
- Social worker
- Family members
Medications
Although psychiatric medications don't cure mental illness, they can often significantly improve symptoms. Psychiatric medications can also help make other treatments, such as psychotherapy, more effective. The best medications for you will depend on your particular situation and how your body responds to the medication.
Some of the most commonly used classes of prescription psychiatric medications include:
- Antidepressants. Antidepressants are used to treat depression, anxiety and sometimes other conditions.
 They can help improve symptoms such as sadness, hopelessness, lack of energy, difficulty concentrating and lack of interest in activities. Antidepressants are not addictive and do not cause dependency.
They can help improve symptoms such as sadness, hopelessness, lack of energy, difficulty concentrating and lack of interest in activities. Antidepressants are not addictive and do not cause dependency. - Anti-anxiety medications. These drugs are used to treat anxiety disorders, such as generalized anxiety disorder or panic disorder. They may also help reduce agitation and insomnia. Long-term anti-anxiety drugs typically are antidepressants that also work for anxiety. Fast-acting anti-anxiety drugs help with short-term relief, but they also have the potential to cause dependency, so ideally they'd be used short term.
- Mood-stabilizing medications. Mood stabilizers are most commonly used to treat bipolar disorders, which involves alternating episodes of mania and depression. Sometimes mood stabilizers are used with antidepressants to treat depression.
- Antipsychotic medications. Antipsychotic drugs are typically used to treat psychotic disorders, such as schizophrenia.
 Antipsychotic medications may also be used to treat bipolar disorders or used with antidepressants to treat depression.
Antipsychotic medications may also be used to treat bipolar disorders or used with antidepressants to treat depression.
Psychotherapy
Psychotherapy, also called talk therapy, involves talking about your condition and related issues with a mental health professional. During psychotherapy, you learn about your condition and your moods, feelings, thoughts and behavior. With the insights and knowledge you gain, you can learn coping and stress management skills.
There are many types of psychotherapy, each with its own approach to improving your mental well-being. Psychotherapy often can be successfully completed in a few months, but in some cases, long-term treatment may be needed. It can take place one-on-one, in a group or with family members.
When choosing a therapist, you should feel comfortable and be confident that he or she is capable of listening and hearing what you have to say. Also, it's important that your therapist understands the life journey that has helped shape who you are and how you live in the world.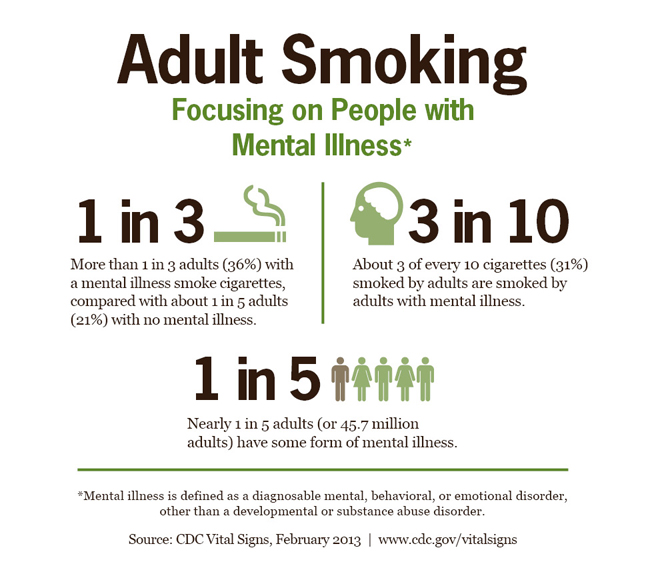
Brain-stimulation treatments
Brain-stimulation treatments are sometimes used for depression and other mental health disorders. They're generally reserved for situations in which medications and psychotherapy haven't worked. They include electroconvulsive therapy, repetitive transcranial magnetic stimulation, deep brain stimulation and vagus nerve stimulation.
Make sure you understand all the risks and benefits of any recommended treatment.
Hospital and residential treatment programs
Sometimes mental illness becomes so severe that you need care in a psychiatric hospital. This is generally recommended when you can't care for yourself properly or when you're in immediate danger of harming yourself or someone else.
Options include 24-hour inpatient care, partial or day hospitalization, or residential treatment, which offers a temporary supportive place to live. Another option may be intensive outpatient treatment.
Substance misuse treatment
Problems with substance use commonly occur along with mental illness. Often it interferes with treatment and worsens mental illness. If you can't stop using drugs or alcohol on your own, you need treatment. Talk to your doctor about treatment options.
Often it interferes with treatment and worsens mental illness. If you can't stop using drugs or alcohol on your own, you need treatment. Talk to your doctor about treatment options.
Participating in your own care
Working together, you and your primary care provider or mental health professional can decide which treatment may be best, depending on your symptoms and their severity, your personal preferences, medication side effects, and other factors. In some cases, a mental illness may be so severe that a doctor or loved one may need to guide your care until you're well enough to participate in decision-making.
More Information
- Mental health providers: Tips on finding one
- Deep brain stimulation
- Electroconvulsive therapy (ECT)
- Psychotherapy
- Transcranial magnetic stimulation
- Vagus nerve stimulation
Request an appointment
From Mayo Clinic to your inbox
Sign up for free, and stay up to date on research advancements, health tips and current health topics, like COVID-19, plus expertise on managing health.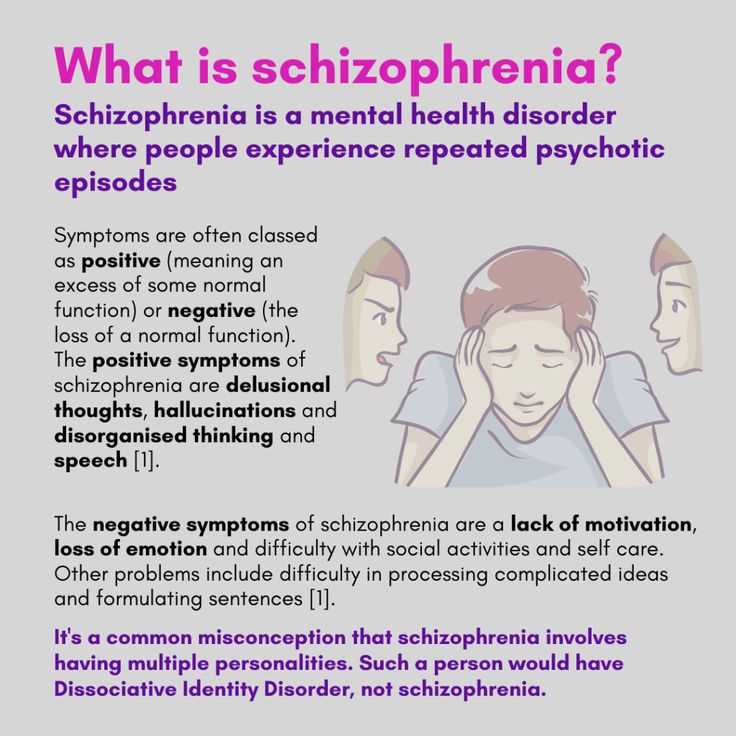 Click here for an email preview.
Click here for an email preview.
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Lifestyle and home remedies
In most cases, a mental illness won't get better if you try to treat it on your own without professional care. But you can do some things for yourself that will build on your treatment plan:
But you can do some things for yourself that will build on your treatment plan:
- Stick to your treatment plan. Don't skip therapy sessions. Even if you're feeling better, don't skip your medications. If you stop, symptoms may come back. And you could have withdrawal-like symptoms if you stop a medication too suddenly. If you have bothersome drug side effects or other problems with treatment, talk to your doctor before making changes.
- Avoid alcohol and drug use. Using alcohol or recreational drugs can make it difficult to treat a mental illness. If you're addicted, quitting can be a real challenge. If you can't quit on your own, see your doctor or find a support group to help you.
- Stay active. Exercise can help you manage symptoms of depression, stress and anxiety. Physical activity can also counteract the effects of some psychiatric medications that may cause weight gain. Consider walking, swimming, gardening or any form of physical activity that you enjoy.
 Even light physical activity can make a difference.
Even light physical activity can make a difference. - Make healthy choices. Maintaining a regular schedule that includes sufficient sleep, healthy eating and regular physical activity are important to your mental health.
- Don't make important decisions when your symptoms are severe. Avoid decision-making when you're in the depth of mental illness symptoms, since you may not be thinking clearly.
- Determine priorities. You may reduce the impact of your mental illness by managing time and energy. Cut back on obligations when necessary and set reasonable goals. Give yourself permission to do less when symptoms are worse. You may find it helpful to make a list of daily tasks or use a planner to structure your time and stay organized.
- Learn to adopt a positive attitude. Focusing on the positive things in your life can make your life better and may even improve your health. Try to accept changes when they occur, and keep problems in perspective.
 Stress management techniques, including relaxation methods, may help.
Stress management techniques, including relaxation methods, may help.
Coping and support
Coping with a mental illness is challenging. Talk to your doctor or therapist about improving your coping skills, and consider these tips:
- Learn about your mental illness. Your doctor or therapist can provide you with information or may recommend classes, books or websites. Include your family, too — this can help the people who care about you understand what you're going through and learn how they can help.
- Join a support group. Connecting with others facing similar challenges may help you cope. Support groups for mental illness are available in many communities and online. One good place to start is the National Alliance on Mental Illness.
- Stay connected with friends and family. Try to participate in social activities, and get together with family or friends regularly. Ask for help when you need it, and be upfront with your loved ones about how you're doing.
- Keep a journal. Or jot down brief thoughts or record symptoms on a smartphone app. Keeping track of your personal life and sharing information with your therapist can help you identify what triggers or improves your symptoms. It's also a healthy way to explore and express pain, anger, fear and other emotions.
Preparing for your appointment
Whether you schedule an appointment with your primary care provider to talk about mental health concerns or you're referred to a mental health professional, such as a psychiatrist or psychologist, take steps to prepare for your appointment.
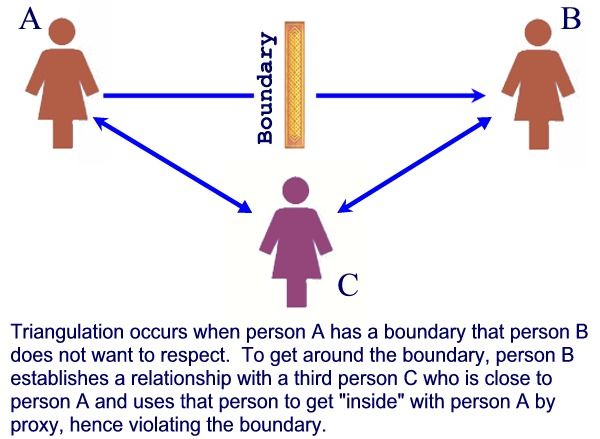
If possible, take a family member or friend along. Someone who has known you for a long time may be able to share important information, with your permission.
What you can do
Before your appointment, make a list of:
- Any symptoms you or people close to you have noticed, and for how long
- Key personal information, including traumatic events in your past and any current, major stressors
- Your medical information, including other physical or mental health conditions
- Any medications, vitamins, herbal products or other supplements you take, and their dosages
- Questions to ask your doctor or mental health professional
Questions to ask may include:
- What type of mental illness might I have?
- Why can't I get over mental illness on my own?
- How do you treat my type of mental illness?
- Will talk therapy help?
- Are there medications that might help?
- How long will treatment take?
- What can I do to help myself?
- Do you have any brochures or other printed material that I can have?
- What websites do you recommend?
Don't hesitate to ask any other questions during your appointment.
What to expect from your doctor
During your appointment, your doctor or mental health professional is likely to ask you questions about your mood, thoughts and behavior, such as:
- When did you first notice symptoms?
- How is your daily life affected by your symptoms?
- What treatment, if any, have you had for mental illness?
- What have you tried on your own to feel better or control your symptoms?
- What things make you feel worse?
- Have family members or friends commented on your mood or behavior?
- Do you have blood relatives with a mental illness?
- What do you hope to gain from treatment?
- What medications or over-the-counter herbs and supplements do you take?
- Do you drink alcohol or use recreational drugs?
Your doctor or mental health professional will ask additional questions based on your responses, symptoms and needs. Preparing and anticipating questions will help you make the most of your time with the doctor.
By Mayo Clinic Staff
Related
Associated Procedures
News from Mayo Clinic
Products & Services
SIGNS OF MENTAL DISORDERS (WHEN TO SEE A DOCTOR)
Signs of mental disorders, and also the frequency of their occurrence is a common question, exciting people in recent years. This is especially true in connection with the fact that the pace of life is steadily growing, and the resources of human nervous system remain unchanged. Very often mental violations develop gradually, stepwise, introducing features into the psyche a person who was previously not peculiar to him, respectively, there are good chances to notice them in time and provide proper medical care.
According to the latest data, mental disorders are detected in 25-30% of the population, that is, one in four in the world. However, it is noteworthy that while 75-80% are sick non-psychotic, mild mental disorders. serious mental illnesses such as schizophrenia occur in 6-17% cases. Alcoholism - in 60%.
Alcoholism - in 60%.
It must be remembered that mental disorder is not a sentence, because with sufficient and timely treatment by a specialist, as well as a responsible attitude and attention to their condition, the symptoms of mental disorders can be stopped, (and often the disorder itself can be completely cured), which will help to maintain the former social, professional status and quality of life.
SIGNS
Asthenic syndrome.
This condition may accompany any mental disorders and many of the somatic diseases. Asthenia expressed in weakness, low performance, mood swings, increased sensitivity. A person starts crying easily, instantly gets irritated and loses his temper. Often asthenia is accompanied sleep disturbances, feeling of weakness, increased fatigue, inability to cope with the usual workload, study.
Obsessive states.
A wide range of obsessions includes many manifestations: from constant doubts, unpleasant thoughts, "stuck, spinning in the head", fears with which a person does not able to cope, to an irresistible desire for purity or performing certain unusual actions. Under the control of the obsessive state, a person can return home several times in order to check whether he turned off the iron, gas, water, whether he closed the door with a key. An obsessive fear of an accident can force the patient to perform some rituals that, according to the sufferer, can avert trouble. If you notice that your friend or relative washes his hands for hours, became overly squeamish and is always afraid of getting infected with something - this also obsession. The desire not to step on cracks in the asphalt, joints tiles, avoidance of certain modes of transport or people in clothing a certain color or type is also an obsessive state.
Under the control of the obsessive state, a person can return home several times in order to check whether he turned off the iron, gas, water, whether he closed the door with a key. An obsessive fear of an accident can force the patient to perform some rituals that, according to the sufferer, can avert trouble. If you notice that your friend or relative washes his hands for hours, became overly squeamish and is always afraid of getting infected with something - this also obsession. The desire not to step on cracks in the asphalt, joints tiles, avoidance of certain modes of transport or people in clothing a certain color or type is also an obsessive state.
Mood changes.
It is especially important to pay attention not to how much for short-term changes under the influence of momentary factors, how much for mood changes that were not previously characteristic a person, long-term, from 2 weeks or more.
- Longing, depression, longing for self-accusations, talk about their own worthlessness, sinfulness, about death, lack of future, hope for the best, etc.
- Unnatural frivolity, carelessness.
- Foolishness, not characteristic of age and character.
- Euphoric state, optimism without any basis.
- Apathy, painful feeling of lack of emotions.
- Fussiness, talkativeness, inability to concentrate, confused thinking.
- Irritability, anger, aggressiveness
- Inability to control emotions, tearfulness, slight breakdowns in conversation natural bashfulness, inability to restrain sexual desires or vice versa, the disappearance of libido, the absence of a morning erection in men
Unusual sensations in the body.
Stinging, burning in the skin, sensations burning, “twisting” pressure in the body, stirring “something inside”, "rustling in the head", the presence of foreign objects in the body - can signal disturbances in the nervous system.
Hypochondria.
Expressed in an obsessive, obsessive search for themselves of serious illnesses and disorders, painful "listening" to the slightest change in the state of your body. At the same time, the patient often does not trust doctors, requires repeated and deeper research, completely focused on finding difficult diseases, requires to be treated as a patient.
At the same time, the patient often does not trust doctors, requires repeated and deeper research, completely focused on finding difficult diseases, requires to be treated as a patient.
Appetite disorders.
It is important to note how sudden increased appetite - "wolfish appetite", and its sharp decrease and perversion of taste preferences. The reason may be as in the disease gastrointestinal tract, and in the general depression of the state, or painful conviction of excessive fullness in its absence. Also it is important if previously tasty food has lost its taste, has become bland, tasteless, "like cardboard."
Illusions
Do not confuse illusions with hallucinations. Illusions force a person to perceive real objects and phenomena in distorted form, while in hallucinations a person feels something that in reality does not exist.
Examples of illusions:
- the pattern on the wallpaper seems to be an interweaving of snakes or worms;
- sizes of objects are perceived in a distorted form;
- the sound of raindrops on the windowsill seems to be the careful steps of someone terrible;
- the shadows of the trees turn into terrible creatures crawling up with frightening intentions, etc.

Hallucinations not guess, then susceptibility to hallucinations can manifest itself more noticeable. Hallucinations can affect all the senses, that is be visual and auditory, tactile and gustatory, olfactory and common, as well as combined in any combination. To the sick all he is sees, hears and feels, seems completely real. He may not believe that all this is not felt, not heard, not seen by others. Their he can perceive bewilderment as a conspiracy, deceit, mockery, get irritated at not being understood.
- Auditory hallucinations human hears various kinds of noise, fragments of words or coherent phrases. Voices can give commands or comment on every action of the patient, laugh at him or discuss his thoughts.
- Taste and olfactory hallucinations often cause a sensation of an unpleasant quality: a disgusting taste or smell.
- For tactile hallucinations, the patient it seems that someone is biting him, touching him, strangling him, that they are crawling on him insects that some creatures are introduced into his body and there move or eat the body from the inside.
- Outwardly subject to hallucinations expressed in conversations with an invisible interlocutor, sudden laughter or constant intense listening to something. The patient can always to shake off something, to cry out, to examine oneself with preoccupied look or ask others if they see something on his body or in the surrounding space.
Changes in thinking
Previously uncharacteristic overestimation own abilities or abilities, confidence in one's own exclusivity, passion for esotericism, magic, suddenly appeared belief in the supernatural. The rate at which thoughts flow in the head can also change, or become uncomfortably slow, or so fast that sometimes it is very difficult to concentrate on one thought.
Delusional thoughts.
Delusional states often accompany psychoses. Delusion is based on erroneous judgments, and the patient stubbornly maintains its false belief, even if there are obvious contradictions with reality.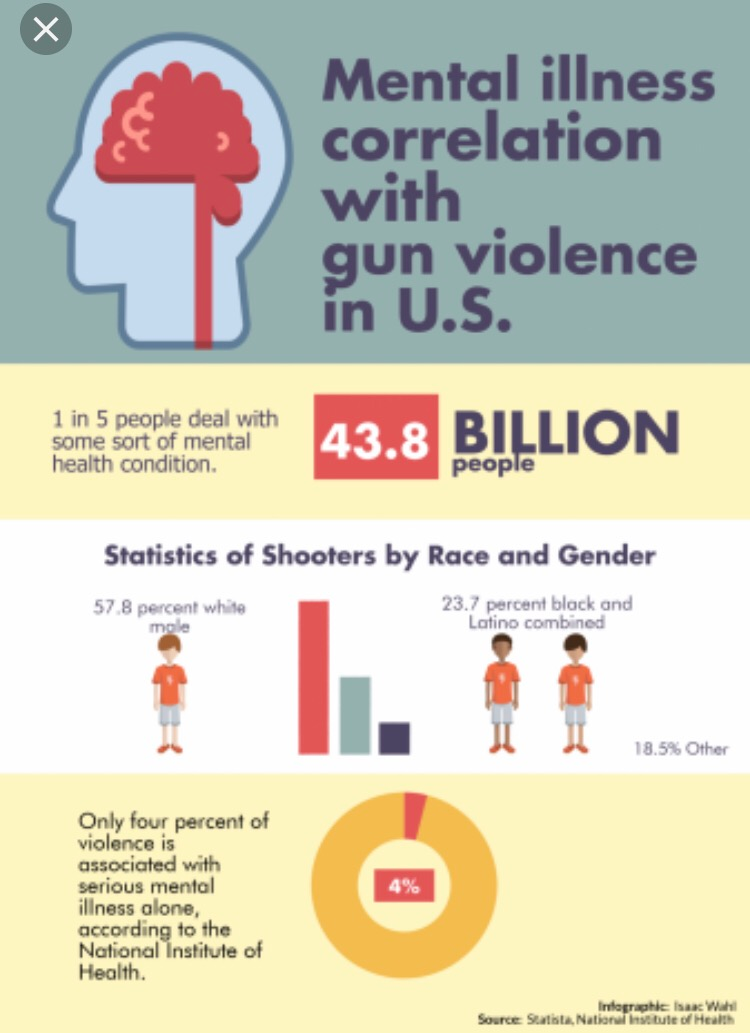 Crazy ideas acquire significance that determines everything behavior. Delusional disorders can be expressed in an erotic form, or in the conviction of one's great mission, in descent from a noble kind or aliens. It may seem to the patient that someone is trying to kill or poison, rob or kidnap. Sometimes the development of delusional state is preceded by a feeling of unreality of the surrounding world or own personality.
Crazy ideas acquire significance that determines everything behavior. Delusional disorders can be expressed in an erotic form, or in the conviction of one's great mission, in descent from a noble kind or aliens. It may seem to the patient that someone is trying to kill or poison, rob or kidnap. Sometimes the development of delusional state is preceded by a feeling of unreality of the surrounding world or own personality.
Desocialization.
There are people who are unsociable and unsociable in strength of his character. This is normal and should not arouse suspicion. mental disorders. But if a born merry fellow, the soul company, a family man and a good friend suddenly begins to destroy social connections, becomes unsociable, shows coldness towards those who have recently was dear to him - this is a reason to worry about his mental health. A person becomes sloppy, stops taking care of himself, maybe quit your job for no good reason, abandon your career, former goals and interests, in society can begin to behave shockingly - commit acts that are considered indecent and unacceptable.
Gathering or excessive generosity
Yes, any collector can be suspicion. Especially in cases where the gathering becomes obsession, subjugates the whole life of a person. It may expressed in the desire to drag into the house things found in the garbage, hoarding products without paying attention to expiration dates, or pick up stray animals in numbers that exceed the ability provide them with proper care and maintenance.
Desire to distribute all one's property, excessive spending can also be regarded as suspicious symptom. Especially in the case when a person was not different before generosity or altruism. Particular attention should be paid to this a condition, especially when a person begins to unexpectedly actively attend banks and make loans.
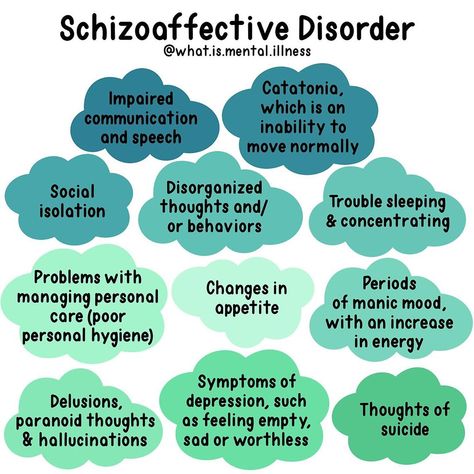
Schizophrenia
Schizophrenia- Health »
- A
- B
- C
- Г
- Д
- Е
- Ё
- Ж
- З
- И
- К
- Л
- М
- Н
- О
- П
- Р
- С
- Т
- In
- f
- x
- c h
- Sh
- K.
- B
- U
- Air pollution
- Н
- О
- П
- Р
- С
- Т
- У
- Ф
- Х
- Ц
- Ч
- Ш
- Щ
- Ъ
- Ы
- Ь
- E
- Yu
- I
- WHO in countries »
- Reporting
- Regions »
- Africa
- America
- Southeast Asia
- Europe
- Eastern Mediterranean
- Western Pacific
- Media Center
- Press releases
- Statements
- Media messages
- Comments
- Reporting
- Online Q&A
- Events
- Photo reports
- case studies
- Questions and answers
- Speeches
- Latest information
- Emergencies "
- News "
- Disease Outbreak News
- WHO data »
- Dashboards »
- COVID-19 Monitoring Dashboard
- Basic moments "
- About WHO »
- CEO
- About WHO
- WHO activities
- Where does WHO work?
- Governing Bodies »
- World Health Assembly
- Executive committee
- Main page/
- Media Center/
- Newsletters/
- Read more/
- Schizophrenia
- Schizophrenia is a severe mental disorder that affects approximately 24 million people, or 1 in 300 people worldwide.
- Schizophrenia causes psychosis, is associated with severe disability, and can negatively affect all areas of life, including personal, family, social, academic and work life.
- People with schizophrenia are often subject to stigma, discrimination and human rights violations.
- Worldwide, more than two thirds of people with psychosis do not receive specialized mental health care.
- There are a number of effective options for helping patients with schizophrenia, which can lead to a complete recovery of at least one in three patients.
- persistent delusions: the patient has a persistent belief in the truth of certain things, despite evidence to the contrary;
- persistent hallucinations: the patient hears, sees, touches non-existent things and smells non-existent smells;
- sensation of external influence, control or passivity: the presence in the patient of the sensation that his feelings, impulses, actions or thoughts are dictated from outside, put in or disappear from consciousness by someone else's will, or that his thoughts are broadcast to others;
- disorganized thinking, often expressed in incoherent or pointless speech;
- Significant disorganization of behavior, which manifests itself, for example, in the performance by the patient of actions that may seem strange or meaningless, or in an unpredictable or inappropriate emotional reaction that does not give the patient the opportunity to organization of their behavior;
- "negative symptoms" such as extreme poverty of speech, smoothness of emotional reactions, inability to feel interest or pleasure, social autism; and/or
- extreme excitement or, on the contrary, slowness of movements, freezing in unusual postures.
- 9003 9003 9003 9003 900 9003 900 9003 Popular Topics
Basic facts
Symptoms
Schizophrenia is characterized by significant disturbances in perception of reality and behavioral changes such as:
People with schizophrenia often also experience persistent cognitive or thinking problems that affect memory, attention, or problem-solving skills.
At least one third of patients with schizophrenia experience complete remission of symptoms (1). In some, periods of remission and exacerbation of symptoms follow each other throughout life, in others there is a gradual increase in symptoms.
Scope and impact
Schizophrenia affects approximately 24 million people, or 1 in 300 people (0.32%) worldwide. Among adults, the rate is 1 in 222 (0.45%) (2). Schizophrenia is less common than many other mental disorders. Onset is most common in late adolescence and between the ages of 20 and 30; while women tend to have a later onset of the disease.
Schizophrenia is often accompanied by significant stress and difficulties in personal relationships, family life, social contacts, studies, work or other important areas of life.
Individuals with schizophrenia are 2-3 times more likely to die early than the population average (2). It is often associated with physical illnesses such as cardiovascular disease, metabolic disease, and infectious disease.
It is often associated with physical illnesses such as cardiovascular disease, metabolic disease, and infectious disease.
Patients with schizophrenia often become the object of human rights violations both within the walls of psychiatric institutions and in everyday life. Significant stigmatization of people with this disease is a widespread phenomenon that leads to their social isolation and has a negative impact on their relationships with others, including family and friends. This creates grounds for discrimination, which in turn limits access to health services in general, education, housing and employment.
Humanitarian emergencies and health crises can cause intense stress and fear, disrupt social support mechanisms, cause isolation and disrupt health services and supply of medicines. All these shocks can have a negative impact on the lives of people with schizophrenia, in particular by exacerbating existing symptoms of the disease. People with schizophrenia are more vulnerable during emergencies to various human rights violations and, in particular, face neglect, abandonment, homelessness, abuse and social exclusion.
Causes of schizophrenia
Science has not established any one cause of the disease. It is believed that schizophrenia may be the result of the interaction of a number of genetic and environmental factors. Psychosocial factors may also influence the onset and course of schizophrenia. In particular, heavy marijuana abuse is associated with an increased risk of this mental disorder.
Assistance services
At present, the vast majority of people with schizophrenia do not receive mental health care worldwide. Approximately 50% of patients in psychiatric hospitals are diagnosed with schizophrenia (4). Only 31.3% of people with psychosis get specialized mental health care (5). Much of the resources allocated to mental health services are inefficiently spent on the care of patients admitted to psychiatric hospitals.
Available scientific evidence clearly indicates that hospitalization in psychiatric hospitals is not an effective way of providing care for mental disorders and is regularly associated with the violation of the basic rights of patients with schizophrenia.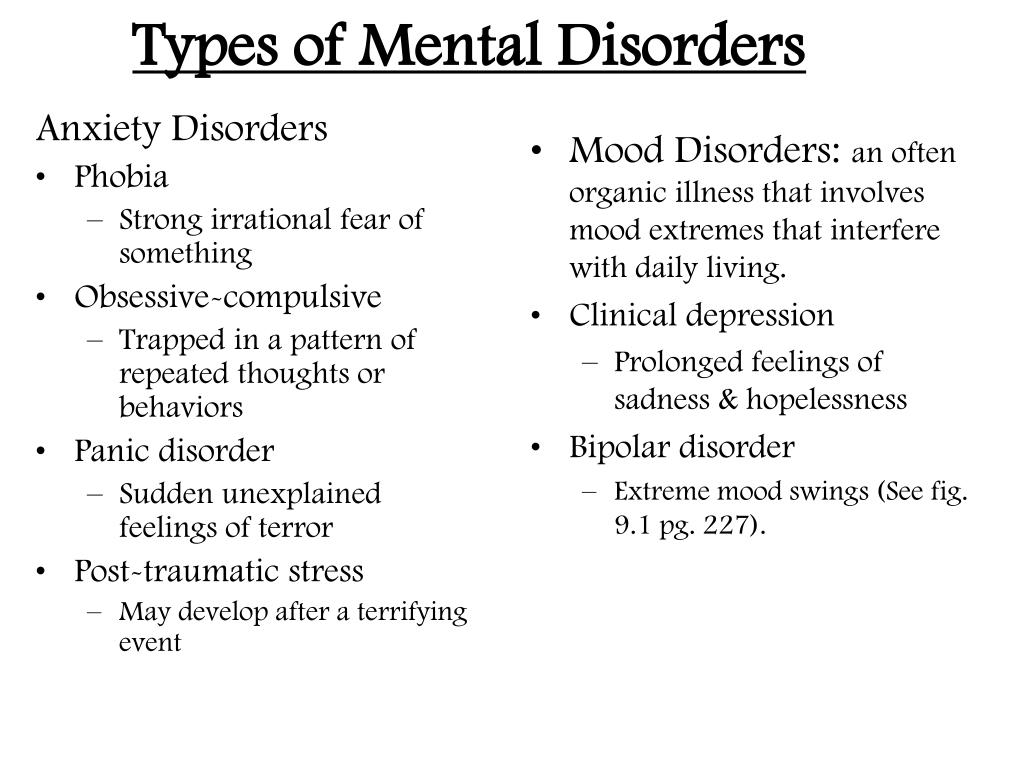 Therefore, it is necessary to ensure the expansion and acceleration of work on the transfer of functions in the field of mental health care from psychiatric institutions to the level of local communities. Such work should begin with the organization of the provision a wide range of quality community-based mental health services. Options for community-based mental health care include integrating this type of care into primary health care and hospital care. general care, setting up community mental health centres, outpatient care centres, social housing with nursing care and social home care services. Involvement in the care process is essential the patient with schizophrenia, his family members and members of local communities.
Therefore, it is necessary to ensure the expansion and acceleration of work on the transfer of functions in the field of mental health care from psychiatric institutions to the level of local communities. Such work should begin with the organization of the provision a wide range of quality community-based mental health services. Options for community-based mental health care include integrating this type of care into primary health care and hospital care. general care, setting up community mental health centres, outpatient care centres, social housing with nursing care and social home care services. Involvement in the care process is essential the patient with schizophrenia, his family members and members of local communities.
Schizophrenia management and care
There are a number of effective approaches to treating people with schizophrenia, including medication, psychoeducation, family therapy, cognitive behavioral therapy, and psychosocial rehabilitation (eg, life skills education). The most important interventions for helping people with schizophrenia are assisted living, special housing and employment assistance. It is extremely important for people with schizophrenia and their families and/or caregivers to a recovery-centered approach that empowers people to participate in decisions about their care.
The most important interventions for helping people with schizophrenia are assisted living, special housing and employment assistance. It is extremely important for people with schizophrenia and their families and/or caregivers to a recovery-centered approach that empowers people to participate in decisions about their care.
WHO activities
steps are in place to ensure that appropriate services are provided to people with mental disorders, including schizophrenia. One of the key recommendations The action plan is to transfer the function of providing assistance from institutions to local communities. WHO Special Mental Health Initiative aims to further progress towards the goals of the Comprehensive Plan mental health action 2013–2030 by ensuring that 100 million more people have access to quality and affordable mental health care.
The WHO Mental Health Gap Action Program (mhGAP) is developing evidence-based technical guidelines, tools and training packages to scale up services in countries, especially in low-resource settings.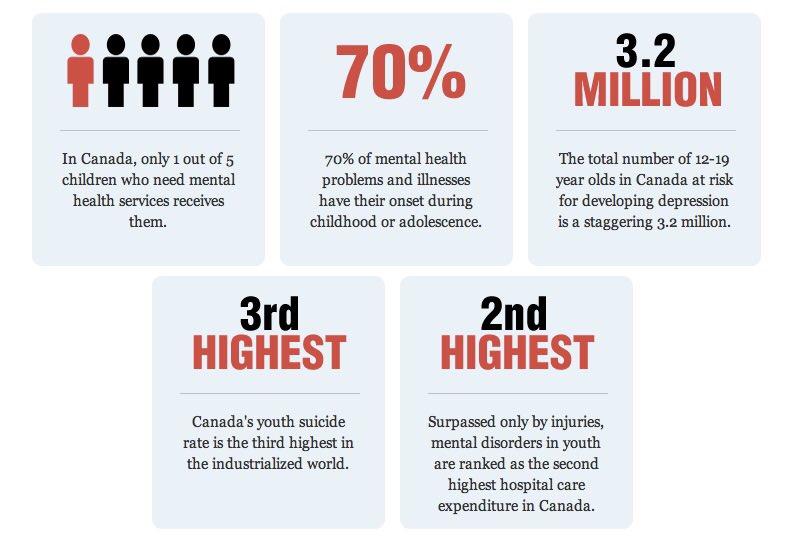 The program focuses on a priority list of mental health disorders, including psychosis, and aims to strengthen the capacity of non-specialized health workers in as part of an integrated approach to mental health care at all levels of care. To date, the mhGAP Program has been implemented in more than 100 WHO Member States.
The program focuses on a priority list of mental health disorders, including psychosis, and aims to strengthen the capacity of non-specialized health workers in as part of an integrated approach to mental health care at all levels of care. To date, the mhGAP Program has been implemented in more than 100 WHO Member States.
The WHO QualityRights project aims to improve the quality of care and better protect human rights in mental health and social care settings and to expand opportunities of various organizations and associations to defend the rights of persons with mental disorders and psychosocial disabilities.
The WHO guidelines on community mental health services and human rights-based approaches provide information for all stakeholders who intend to develop or transform mental health systems and services. health in accordance with international human rights standards, including the UN Convention on the Rights of Persons with Disabilities.
Bibliography
(1) Harrison G, Hopper K, Craig T, Laska E, Siegel C, Wanderling J.