Mental health and the military
Veterans & Active Duty | NAMI: National Alliance on Mental Illness
Nearly 1 in 4 active duty members showed signs of a mental health condition, according to a 2014 study in JAMA Psychiatry. On this page we focus on questions that military personnel often ask, concerning treatment resources, disclosure and staying healthy during the transition to civilian life. If you are having thoughts of suicide, the Veterans Crisis Line is available 24/7 by dialing 1-800-273-8255 and pressing 1.
NAMI offers information, support and education specifically for veterans, service members and their families. To learn more, visit NAMI Homefront.
Mental Health Concerns
There are three primary mental health concerns that you may encounter serving in the military.
- Postraumtic Stress Disorder (PTSD). Traumatic events, such as military combat, assault, disasters or sexual assault can have long-lasting negative effects such as trouble sleeping, anger, nightmares, being jumpy and alcohol and drug abuse.
When these troubles don't go away, it could be PTSD. The 2014 JAMA Psychiatry study found the rate of PTSD to be 15 times higher than civilians.
- Depression. More than just experiencing sadness, depression doesn't mean you are weak, nor is it something that you can simply "just get over." Depression interferes with daily life and normal functioning and may require treatment. The 2014 JAMA Psychiatry study found the rate of depression to be five times higher than civilians.
- Traumatic Brain Injury (TBI). A traumatic brain injury is usually the result of significant blow to the head or body. Symptoms can include headaches, fatigue or drowsiness, memory problems and mood changes and mood swings.
In the Mental Health Conditions section of our site we discuss these conditions and others and how to recognize the symptoms of mental illness in yourself or someone else.
Who Should I Tell?
Service men and women owe it to their fellow service members to stay in good mental as well as physical health. If you’re concerned about a possible mental health condition—or if you enter the armed forces with a past or present mental health condition—know that the armed forces do not require service members to disclose mental health problems to their chain of command. The responsibility for deciding whether to disclose your condition does fall on the medical officers and care providers you consult. They receive training on military policies concerning the confidentiality of protected health information (PHI). Here are some people to consider speaking with.
If you’re concerned about a possible mental health condition—or if you enter the armed forces with a past or present mental health condition—know that the armed forces do not require service members to disclose mental health problems to their chain of command. The responsibility for deciding whether to disclose your condition does fall on the medical officers and care providers you consult. They receive training on military policies concerning the confidentiality of protected health information (PHI). Here are some people to consider speaking with.
- Confidential counselors are available for service members and their families through Military One Source at 1-800-342-9647. If you’re unsure whether to seek treatment or if you someone you know might need treatment, they are an excellent first stop for information and advice.
- Primary care providers can be helpful for discussing concerns and treatment options.
- Behavioral health care providers working at primary care clinics are available on many military bases so you can seek a specialist’s advice without leaving base.
 And at some bases, you can find convenient Embedded Behavioral Health teams—clinics separate from traditional medical facilities.
And at some bases, you can find convenient Embedded Behavioral Health teams—clinics separate from traditional medical facilities.
If you or someone you know is struggling or in crisis, help is available. Call or text 988 or chat 988lifeline.org to reach the 988 Suicide & Crisis Lifeline.
How Will Asking for Mental Health Treatment Affect My Career?
Military personnel have always taken care of their physical health, but in today’s armed forces, mental health is equally essential to mission success. The military has changed many of its policies in recent years to encourage better mental health. The Department of Defense acknowledges that untreated mental health conditions pose a greater safety threat than mental health conditions for which you’re seeking treatment.
Under 2014 rules, talking to a doctor about your concerns, asking if you need a diagnosis, or seeking treatment does not affect your career. If your doctor needs to disclose your condition, your career is not at risk from this disclosure.
In addition, with changes to security clearance procedures, you no longer risk losing clearance by consulting a doctor. If you seek help for combat-related issues or receive marital counseling, you do not have to worry about “question 21” regarding treatment for mental or emotional conditions.
The Dangers of Not Disclosing
Untreated mental illness can, however, damage your career. If the symptoms are severe, your commanding officer may require duty limitations or recommend separation from the military for medical reasons.
Military records show that talking to a doctor is a good career move. According to a 2006 study in Military Medicine, 97% of personnel who sought mental health treatment did not experience any negative career impact. The same study showed that it’s risky to ignore a mental health condition. If it worsens, a commanding officer can require a mental health evaluation, which is much more damaging to your career. Among people who had command-directed evaluations, 39% had negative career impact.
Military Policy and Your Privacy
When you seek mental health care, your care provider will inform you that the Department of Defense follows the privacy guidelines set down by HIPAA and the Privacy Act. These guidelines ensure the privacy of your mental health records in most situations. If your care provider discovers that your mental health condition may endanger yourself, others or the mission, however, they are obligated to disclose this information to the chain of command.
Military policy states that care providers can only share certain information and only in those situations involving safety. The precise definition of those circumstances is different for each of the branches of the armed forces.
In the Army, for example, PHI policy states that information can only be released in situations involving an acute threat of harm to self, others or mission; upon admission or discharge from inpatient hospitalization; when entering formal substance abuse treatment; and when enrolling in personnel reliability programs.
If a medical officer or military care provider observes that your health condition poses a danger, the officer will share your medical profile with commanding officers. The information they are allowed to share includes your diagnosis and the medically recommended duty limitations. Unit commanders will decide what duties to assign you until your condition improves.
You can avoid situations requiring disclosure by discussing your concerns with providers when they first arise. Ignoring symptoms may allow them to worsen. A mental health condition may affect only you at first, but if your condition doesn’t improve, your ability to perform your duties may suffer.
If commanders or supervisors observe behaviors that appear to compromise safety or job performance, they can request a command-directed behavioral health evaluation. A command-directed evaluation doesn’t guarantee as much confidentiality as a medical consultation you seek yourself.
How Can I Help a Fellow Warrior?
Strengthening our fighting forces is a group effort. If you’re concerned about a friend or colleague, the most important thing you can do is to ask how they’re doing and to listen without judgment. The symptoms of a mental health condition can sometimes make individuals forget that mission success relies on staying healthy in mind as well as body. They might not realize that their worries are symptoms of mental illness. Listen patiently, offer encouragement and remind them that anyone can develop these symptoms, from privates to generals.
If you’re concerned about a friend or colleague, the most important thing you can do is to ask how they’re doing and to listen without judgment. The symptoms of a mental health condition can sometimes make individuals forget that mission success relies on staying healthy in mind as well as body. They might not realize that their worries are symptoms of mental illness. Listen patiently, offer encouragement and remind them that anyone can develop these symptoms, from privates to generals.
Remind your fellow warrior that the central mission of the armed forces is to maintain a strong fighting force. Share the information here with him or her. Emphasize that talking to a counselor or medical officer won’t hurt career or security clearance, and that every service member has a duty to build resilience by seeking advice and treatment when it’s indicated.
If someone you know tells you about a mental health concern, don’t laugh it off or promise it will get better on its own, even if you want to comfort the person. The stresses of deployment and military life put soldiers at risk for mental illness and make treating them more complicated. The military medical system can’t succeed in its mission to “restore the fighting force” without the help of all personnel to encourage treating mental health conditions swiftly before they can worsen.
The stresses of deployment and military life put soldiers at risk for mental illness and make treating them more complicated. The military medical system can’t succeed in its mission to “restore the fighting force” without the help of all personnel to encourage treating mental health conditions swiftly before they can worsen.
For more advice, recommend that your friend call the completely confidential counselors at Military One Source (1-800-342-9647).
Making a Strong Transition to Civilian Life
Returning to civilian life can be a time of joy, but also a time of emotional upheaval. Your experiences in the service may have changed the way you look at life. You may have new abilities, new friendships or new concerns.
If you were in combat or similarly stressful situations, it’s possible some of the habits that helped you stay strong during traumatic events will be less useful in civilian life. Keeping strong in civilian life might require developing new habits. You may also be at increased risk of PTSD and other symptoms that your brain is recovering from trauma.
Some veterans find they miss the structure that the military life provides. Some miss feeling a sense of purpose in their daily work. Others may feel isolated because civilians don’t understand the experience of serving. The memories of your experiences also may take time to deal with.
Remember that readjusting takes time. Give yourself opportunities to maintain your physical and mental health during the transition. At NAMI, we understand the questions facing many service members when they return to civilian life. We're here to help. Check out your local NAMI Affiliate to see if it offers a support program for returning vets.
Maintaining a Strong Body and Mind
Here are some important tips and suggestions for maintaining a strong body and mind:
- Reach out to other veterans or veterans’ groups. It's much easier to make the transition when you're not alone. Social support from non-veterans helps as well. Locate a spiritual or religious advisor you enjoy talking to, or a mental health professional.

- Talk to family and friends about your experiences. Even if they don't fully understand what you're going through, it helps them to understand why you may have trouble interacting at times.
- Recognize that others might not understand your military service or your views. If you talk about your experiences and get a negative response, let it go.
- Prepare ahead of time for insensitive questions or topics of conversation. You don’t need to tell anyone about your experiences unless you want to. Practice how to respond or respectfully decline to answer.
- Search the web for information on mental health and transitioning. Identify strategies ahead of time to support your transition. Real Warriors is a great site for all soldiers, whether they be active duty, National Guard or Reserve, or veterans and their families. The information and tools there can help with everything from budgeting and work to insomnia, PTSD and depression.
- Take care of your body and your mind by proactively finding veteran-friendly health services in your area.
 You can obtain information on local services through My HealtheVet, the VA’s online personal health record. This site for veterans, active duty service members, and their families provides access to health records, a personal health journal, online VA prescription refill information and details regarding federal and VA benefits and resources.
You can obtain information on local services through My HealtheVet, the VA’s online personal health record. This site for veterans, active duty service members, and their families provides access to health records, a personal health journal, online VA prescription refill information and details regarding federal and VA benefits and resources. - Take your time reconnecting with family and friends. When you were serving, your role in the family was “distant service member.” Now you and your family are developing a new role for you. Since time has passed, your new role might not be identical to your role before serving. You and your family will adjust and be stronger than before, but don’t expect the adjustments to happen immediately.
- Try to be patient with your civilian coworkers and the civilian work schedule. At times you may feel frustrated that employees in civilian life leave when the work day officially ends, regardless of whether the “mission” for the day is complete.
 They may appear less committed than you're used to, and less interested in team work. You may also find that you and your civilian coworkers have different modes of speech at the office. Military jargon is a complex language and you might feel like you’re having to translate yourself into “civilian English.”
They may appear less committed than you're used to, and less interested in team work. You may also find that you and your civilian coworkers have different modes of speech at the office. Military jargon is a complex language and you might feel like you’re having to translate yourself into “civilian English.” - Recognize that you will feel frustrated sometimes while returning to civilian life, but frustration is normal during this transition. In fact, frustration is a sign that you’re adjusting and growing stronger.
- If you find yourself growing more frustrated or isolated over time, talk to a health professional about whether mental health care can help you increase your resilience. The Department of Defense sponsors coaching and support at In Transition (1-800-424-7877). Medical professionals can help you come out of this transition stronger than before.
The important thing to remember is that you’re not alone. There are many people who want to support you. You can start preparing now, by looking at the VA’s list of common challenges and solutions, or the MilitaryOneSource database of websites offering assistance with the transition to civilian life.
You can start preparing now, by looking at the VA’s list of common challenges and solutions, or the MilitaryOneSource database of websites offering assistance with the transition to civilian life.
Veteran and Military Mental Health Issues
Book
Catarina Inoue 1 , Evan Shawler 2 , Christopher H. Jordan 3 , Christopher A. Jackson 4
In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan.
.
Affiliations
Affiliations
- 1 1st Special Operations Medical Group
- 2 Uniformed Services University of the Health Sciences
- 3 Hurlburt Field Air Force Base
- 4 University of Texas Health Science Center at San Antonio
- PMID: 34283458
- Bookshelf ID: NBK572092
Free Books & Documents
Book
Catarina Inoue et al.
Free Books & Documents
In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan.
.
Authors
Catarina Inoue 1 , Evan Shawler 2 , Christopher H. Jordan 3 , Christopher A. Jackson 4
Affiliations
- 1 1st Special Operations Medical Group
- 2 Uniformed Services University of the Health Sciences
- 3 Hurlburt Field Air Force Base
- 4 University of Texas Health Science Center at San Antonio
- PMID: 34283458
- Bookshelf ID: NBK572092
Excerpt
As the United States faces two decades of continuous war, media and individuals with personal military connections have elevated public and professional concerns for the mental health of veterans and service members. The most publicized mental health challenges facing veterans service members are PTSD and depression. Some research has suggested that approximately 14% to 16% of U.S. service members deployed to Afghanistan and Iraq have PTSD or depression. Although these mental health concerns are highlighted, other issues like suicide, traumatic brain injury (TBI), substance abuse, and interpersonal violence can be equally harmful in this population. The effects of these issues can be wide-reaching and substantially impacts service members and their families. While combat and deployments are linked to increased risks for these mental health conditions, general military service can also lead to difficulties. There is no specified timeline for the presentation of these mental health concerns. Still, there are particularly stressful times for individuals and families, such as in close proximity to combat or when separating from active military service.
The most publicized mental health challenges facing veterans service members are PTSD and depression. Some research has suggested that approximately 14% to 16% of U.S. service members deployed to Afghanistan and Iraq have PTSD or depression. Although these mental health concerns are highlighted, other issues like suicide, traumatic brain injury (TBI), substance abuse, and interpersonal violence can be equally harmful in this population. The effects of these issues can be wide-reaching and substantially impacts service members and their families. While combat and deployments are linked to increased risks for these mental health conditions, general military service can also lead to difficulties. There is no specified timeline for the presentation of these mental health concerns. Still, there are particularly stressful times for individuals and families, such as in close proximity to combat or when separating from active military service.
Current U.S. Census reports estimate roughly 18 million veterans and 2.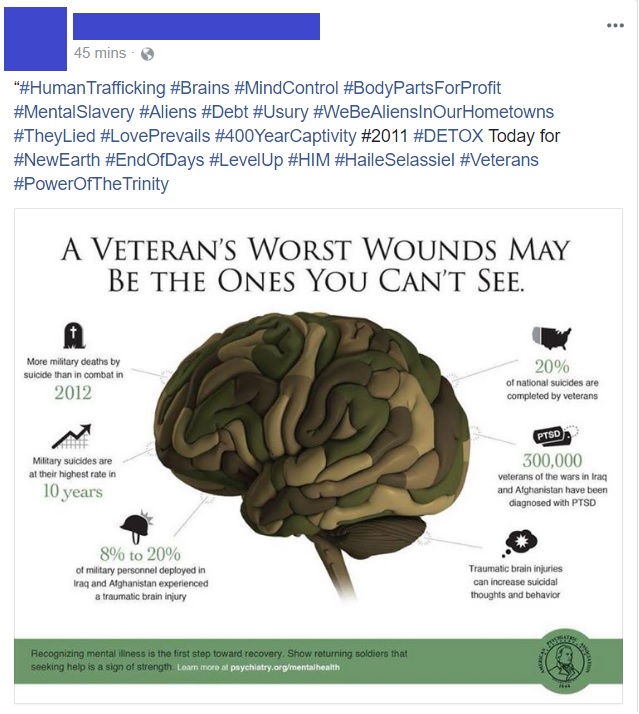 1 million active-duty and reserve service members (https://www.census.gov/newsroom/press-releases/2020/veterans-report.html). Since September 11, 2001, there have been 2.8 million active-duty American military personnel deployed to Iraq, Afghanistan, and beyond, leading to increasing numbers of combat veterans amongst the population. More than 6% of the U.S. population have served or are serving in the military. However, this statistic fails to capture the even greater number of family members affected by military service. Understanding military service and its relation to a patient’s physical and mental health can help providers improve their quality of care and potentially help save a patient’s life.
1 million active-duty and reserve service members (https://www.census.gov/newsroom/press-releases/2020/veterans-report.html). Since September 11, 2001, there have been 2.8 million active-duty American military personnel deployed to Iraq, Afghanistan, and beyond, leading to increasing numbers of combat veterans amongst the population. More than 6% of the U.S. population have served or are serving in the military. However, this statistic fails to capture the even greater number of family members affected by military service. Understanding military service and its relation to a patient’s physical and mental health can help providers improve their quality of care and potentially help save a patient’s life.
Post-Traumatic Stress Disorder (PTSD)
Post-traumatic stress disorder (PTSD) was first codified in the Diagnostic and Statistical Manual of Mental Disorders (DSM) 3 in 1980, driven in part by sociopolitical aftereffects of the Vietnam War.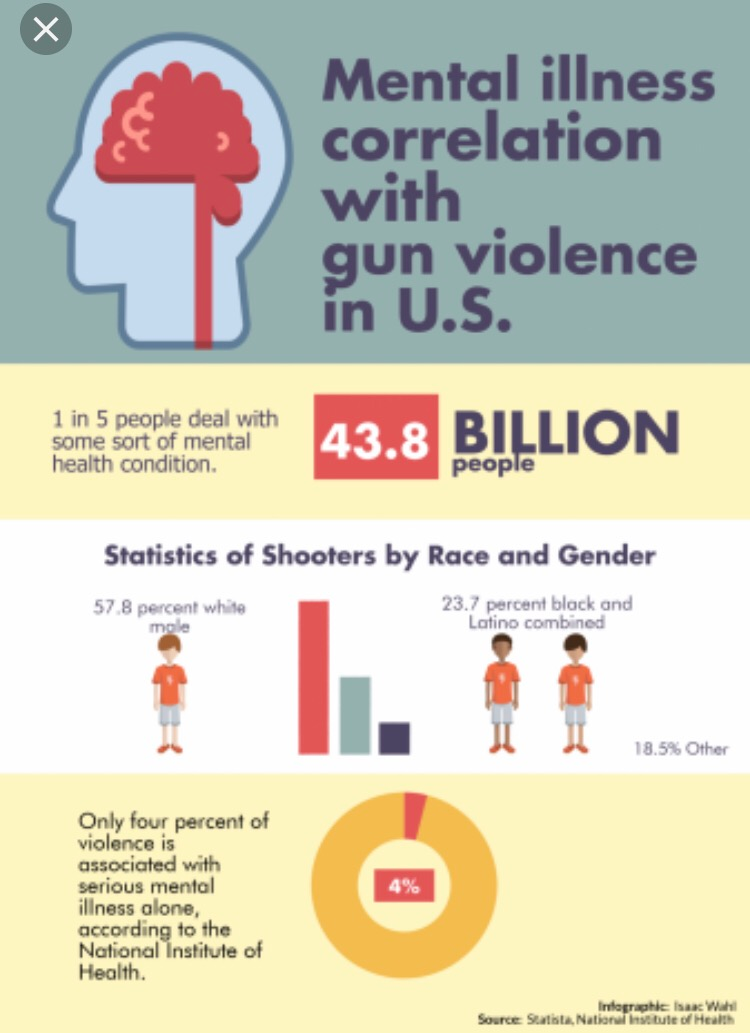 It has been alluded to in different forms throughout history, from “soldier’s heart” at the time of the Civil War, “shell shock” in the First World War, or “combat fatigue” around the Vietnam War. DSM criteria remained largely unchanged until the most recent update in 2013, although its classification continues to be debated. It is a complex and evolving biological, psychological, and social entity, making it challenging to study and diagnose. PTSD is often researched in war and disaster survivors but can affect anybody, including children. It is usually seen in survivors of violent events such as assault, disasters, terror attacks, and war, although it is also possible to experience PTSD from secondhand exposure, such as learning that a close friend or family member experienced a violent threat or accident. Many individuals exposed to trauma have transient numbness or heightened emotions, nightmares, anxiety, and hypervigilance but usually overcome symptoms within one month. In roughly 10 to 20% of cases, symptoms become persistent and debilitating.
It has been alluded to in different forms throughout history, from “soldier’s heart” at the time of the Civil War, “shell shock” in the First World War, or “combat fatigue” around the Vietnam War. DSM criteria remained largely unchanged until the most recent update in 2013, although its classification continues to be debated. It is a complex and evolving biological, psychological, and social entity, making it challenging to study and diagnose. PTSD is often researched in war and disaster survivors but can affect anybody, including children. It is usually seen in survivors of violent events such as assault, disasters, terror attacks, and war, although it is also possible to experience PTSD from secondhand exposure, such as learning that a close friend or family member experienced a violent threat or accident. Many individuals exposed to trauma have transient numbness or heightened emotions, nightmares, anxiety, and hypervigilance but usually overcome symptoms within one month. In roughly 10 to 20% of cases, symptoms become persistent and debilitating.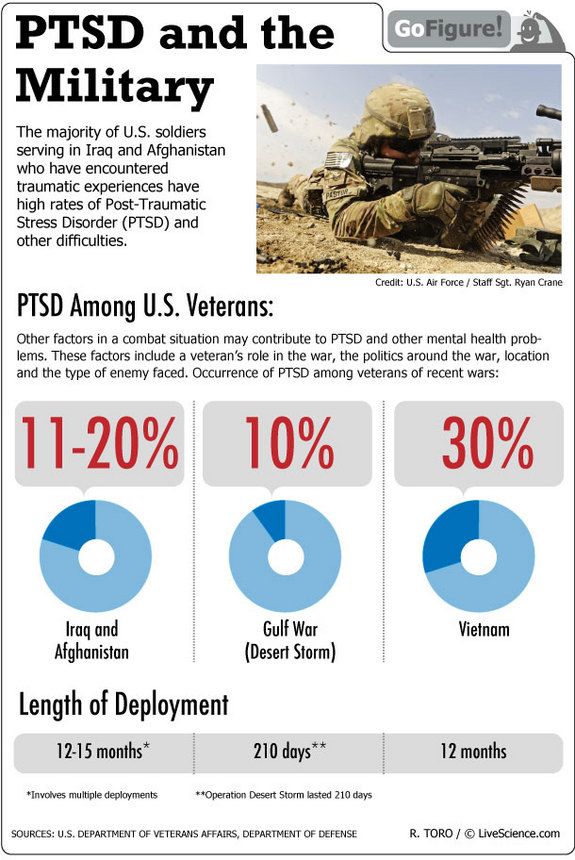 PTSD features intrusive thoughts, flashbacks, and nightmares regarding the past trauma, causing avoidance of reminders, hypervigilance, and sleep difficulties. Often, reliving the event can feel as threatening as inciting trauma. Symptoms can interfere with interpersonal and occupational function and manifest in psychological, emotional, physical, behavioral, and cognitive manners. Military personnel can be exposed to an array of potentially traumatizing experiences. Wartime deployments can result in witnessing severe injuries or violent death, sometimes occurring suddenly and not always on expected targets. Apart from the austere environment of deployment, active duty military members are at risk of experiencing non-military-related traumas such as interpersonal violence, physical or sexual abuse. Symptoms related to these traumas can sometimes be exacerbated in the deployed environment.
PTSD features intrusive thoughts, flashbacks, and nightmares regarding the past trauma, causing avoidance of reminders, hypervigilance, and sleep difficulties. Often, reliving the event can feel as threatening as inciting trauma. Symptoms can interfere with interpersonal and occupational function and manifest in psychological, emotional, physical, behavioral, and cognitive manners. Military personnel can be exposed to an array of potentially traumatizing experiences. Wartime deployments can result in witnessing severe injuries or violent death, sometimes occurring suddenly and not always on expected targets. Apart from the austere environment of deployment, active duty military members are at risk of experiencing non-military-related traumas such as interpersonal violence, physical or sexual abuse. Symptoms related to these traumas can sometimes be exacerbated in the deployed environment.
Depression
After two decades of continuous war in Afghanistan, a growing population of veterans with combat and deployment experience is presenting for mental health care.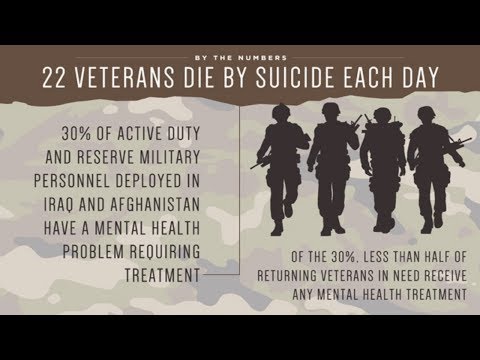 Providers must take into account not only the physical wounds these veterans may have sustained but also the less visible ones such as PTSD, acute stress disorder, and depression. Although the condition does not garner the same attention as PTSD, depression remains one of the leading mental health conditions in the military. In fact, studies show that up to 9% of all appointments in the ambulatory military health network are related to depression. The military environment can act as a catalyst for the development and progression of depression. For example, separation from loved ones and support systems, stressors of combat, and seeing oneself and others in harm’s way are all elements that increase the risk of depression in active duty and veteran populations. Military medical facilities saw an increase from a baseline of 11.4% of members diagnosed with depression to a rate of 15% after deployments to Iraq or Afghanistan. With such a high prevalence, providers must be responsible for identifying active duty and veteran patients who may be suffering from depression.
Providers must take into account not only the physical wounds these veterans may have sustained but also the less visible ones such as PTSD, acute stress disorder, and depression. Although the condition does not garner the same attention as PTSD, depression remains one of the leading mental health conditions in the military. In fact, studies show that up to 9% of all appointments in the ambulatory military health network are related to depression. The military environment can act as a catalyst for the development and progression of depression. For example, separation from loved ones and support systems, stressors of combat, and seeing oneself and others in harm’s way are all elements that increase the risk of depression in active duty and veteran populations. Military medical facilities saw an increase from a baseline of 11.4% of members diagnosed with depression to a rate of 15% after deployments to Iraq or Afghanistan. With such a high prevalence, providers must be responsible for identifying active duty and veteran patients who may be suffering from depression.
Major depression manifests through many symptoms, including depressed mood, loss of interest in activities, insomnia, weight loss or gain, psychomotor retardation, fatigue, decreased ability to concentrate, thoughts of worthlessness, and thoughts of suicide. These symptoms coalesce to significantly impact patients’ abilities to function fully. While the complement of symptoms is readily apparent on paper, a patient’s actual presentation can often be ambiguous. One out of every two depressed patients is not appropriately diagnosed by their general practitioner. Therefore, it is paramount to correctly screen for, identity, and follow through with appropriate treatments, especially in the active duty and veteran military population.
Suicide
Veteran suicide rates are at the highest level in recorded history, with annual deaths by suicide at over 6,000 veterans per year. Overall suicide rates within the United States have increased by 30% between 1999 and 2016. A study involving 27 states estimated 17.8% of these recorded suicides were by veterans. The U.S. Department of Veterans Affairs (VA) published data in 2016 that indicated veteran suicide rates were 1.5 times greater than non-veterans. Research has shown that veterans are at significantly increased risk of suicide during their first year outside of the military. In 2018, a Presidential Executive Order was signed to improve suicide prevention services for veterans during their transition to civilian life. Additionally, the Department of Defense (DoD) and VA have made suicide prevention a major priority because of observed increases in fatal and non-fatal suicide attempts throughout the wars in Iraq and Afghanistan. Within the U.S. Armed Forces, suicide rates doubled between 2000 and 2012, but since 2012 there have been no appreciable changes in the annual rate, with approximately 19.74 deaths per 100,000 service members.
A study involving 27 states estimated 17.8% of these recorded suicides were by veterans. The U.S. Department of Veterans Affairs (VA) published data in 2016 that indicated veteran suicide rates were 1.5 times greater than non-veterans. Research has shown that veterans are at significantly increased risk of suicide during their first year outside of the military. In 2018, a Presidential Executive Order was signed to improve suicide prevention services for veterans during their transition to civilian life. Additionally, the Department of Defense (DoD) and VA have made suicide prevention a major priority because of observed increases in fatal and non-fatal suicide attempts throughout the wars in Iraq and Afghanistan. Within the U.S. Armed Forces, suicide rates doubled between 2000 and 2012, but since 2012 there have been no appreciable changes in the annual rate, with approximately 19.74 deaths per 100,000 service members.
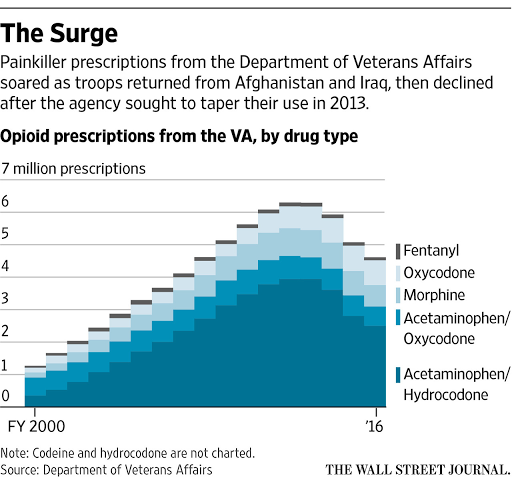
Substance Use Disorders
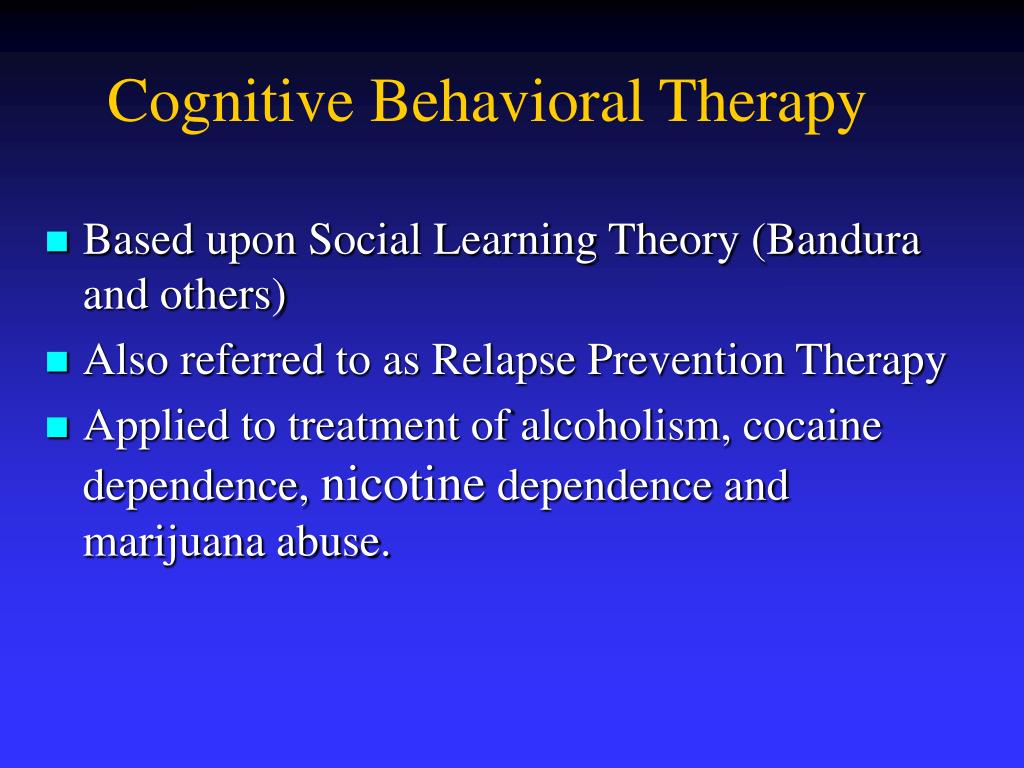
Despite public attention over recent decades, SUDs, including alcohol use, remains a problem among veterans and military members. In these populations, alcohol use is common and is often used for stress relief and socializing. SUDs are associated with significant adverse medical, psychiatric, interpersonal, and occupational outcomes. One study on military personnel found that approximately 30% of completed suicides and around 20% of deaths due to high-risk behavior were attributable to alcohol or drug use. In the general U.S. population, alcohol is the fourth leading cause of preventable death, and 31% of driving-related fatalities involve alcohol intoxication. The DSM-5 defines SUD as a cluster of behaviors surrounding compulsive drug-seeking. This includes impaired control of, dysfunctional social functioning due to, and physiologic changes caused by drug use. Addiction is the most severe stage, characterized by loss of self-control leading to compulsive drug-seeking despite a desire to quit. Substances include legal drugs such as caffeine, nicotine, and alcohol; prescription medications such as opioids, sedative/hypnotics, and stimulants; and illicit drugs such as marijuana, cocaine, methamphetamines, heroin, hallucinogens, and inhalants.
In these populations, alcohol use is common and is often used for stress relief and socializing. SUDs are associated with significant adverse medical, psychiatric, interpersonal, and occupational outcomes. One study on military personnel found that approximately 30% of completed suicides and around 20% of deaths due to high-risk behavior were attributable to alcohol or drug use. In the general U.S. population, alcohol is the fourth leading cause of preventable death, and 31% of driving-related fatalities involve alcohol intoxication. The DSM-5 defines SUD as a cluster of behaviors surrounding compulsive drug-seeking. This includes impaired control of, dysfunctional social functioning due to, and physiologic changes caused by drug use. Addiction is the most severe stage, characterized by loss of self-control leading to compulsive drug-seeking despite a desire to quit. Substances include legal drugs such as caffeine, nicotine, and alcohol; prescription medications such as opioids, sedative/hypnotics, and stimulants; and illicit drugs such as marijuana, cocaine, methamphetamines, heroin, hallucinogens, and inhalants.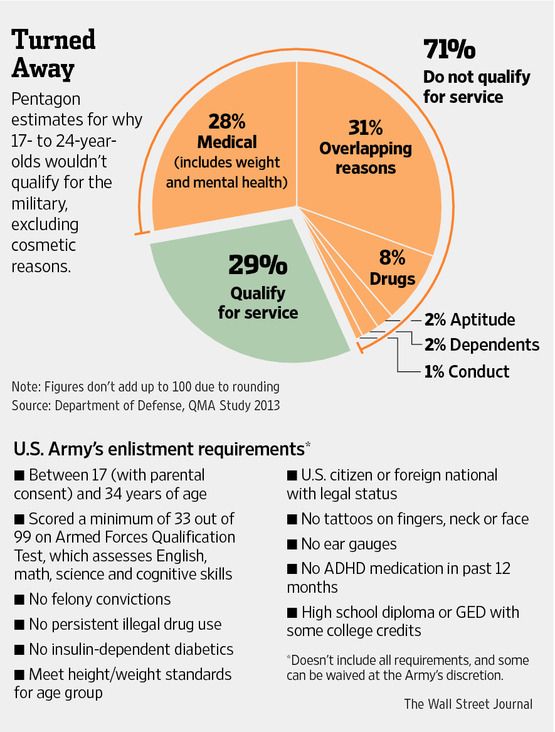
Copyright © 2022, StatPearls Publishing LLC.
Sections
- Continuing Education Activity
- Introduction
- Etiology
- Epidemiology
- History and Physical
- Evaluation
- Treatment / Management
- Differential Diagnosis
- Prognosis
- Complications
- Consultations
- Deterrence and Patient Education
- Enhancing Healthcare Team Outcomes
- Review Questions
- References
Similar articles
-
Suicidal Ideation.

Harmer B, Lee S, Duong TVH, Saadabadi A. Harmer B, et al. 2022 May 18. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan–. 2022 May 18. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan–. PMID: 33351435 Free Books & Documents.
-
Prescription of Controlled Substances: Benefits and Risks.
Preuss CV, Kalava A, King KC. Preuss CV, et al. 2022 Sep 21. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan–. 2022 Sep 21. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan–. PMID: 30726003 Free Books & Documents.
-
NP Safe Prescribing Of Controlled Substances While Avoiding Drug Diversion.

Dydyk AM, Sizemore DC, Haddad LM, Lindsay L, Porter BR. Dydyk AM, et al. 2022 Oct 9. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan–. 2022 Oct 9. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan–. PMID: 33232099 Free Books & Documents.
-
Florida Controlled Substance Prescribing.
Dydyk AM, Sizemore DC, Fariba KA, Sanghavi D, Porter BR. Dydyk AM, et al. 2022 Oct 9. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan–. 2022 Oct 9. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan–. PMID: 33428370 Free Books & Documents.
-
Combat duty in Iraq and Afghanistan, mental health problems and barriers to care.

Hoge CW, Castro CA, Messer SC, McGurk D, Cotting DI, Koffman RL. Hoge CW, et al. US Army Med Dep J. 2008 Jul-Sep:7-17. US Army Med Dep J. 2008. PMID: 20088060
See all similar articles
References
-
- Deahl MP, Klein S, Alexander DA. The costs of conflict: meeting the mental health needs of serving personnel and service veterans. Int Rev Psychiatry. 2011 Apr;23(2):201-9. - PubMed
-
- Gates MA, Holowka DW, Vasterling JJ, Keane TM, Marx BP, Rosen RC. Posttraumatic stress disorder in veterans and military personnel: epidemiology, screening, and case recognition.
 Psychol Serv. 2012 Nov;9(4):361-82. - PubMed
Psychol Serv. 2012 Nov;9(4):361-82. - PubMed
- Gates MA, Holowka DW, Vasterling JJ, Keane TM, Marx BP, Rosen RC. Posttraumatic stress disorder in veterans and military personnel: epidemiology, screening, and case recognition.
-
- Liu Y, Collins C, Wang K, Xie X, Bie R. The prevalence and trend of depression among veterans in the United States. J Affect Disord. 2019 Feb 15;245:724-727. - PubMed
-
- Sullivan RM, Cozza SJ, Dougherty JG. Children of Military Families. Child Adolesc Psychiatr Clin N Am. 2019 Jul;28(3):337-348. - PubMed
-
- Ravindran C, Morley SW, Stephens BM, Stanley IH, Reger MA.
 Association of Suicide Risk With Transition to Civilian Life Among US Military Service Members. JAMA Netw Open. 2020 Sep 01;3(9):e2016261. - PMC - PubMed
Association of Suicide Risk With Transition to Civilian Life Among US Military Service Members. JAMA Netw Open. 2020 Sep 01;3(9):e2016261. - PMC - PubMed
- Ravindran C, Morley SW, Stephens BM, Stanley IH, Reger MA.
Publication types
who is supposed to and how to get it
Precisely because of the popularity of this method of release, it is difficult for those conscripts who are actually diagnosed with mental illness to pass the military medical commission.
Today we will talk about both sides of this problem. We suggest that you familiarize yourself with the list of diagnoses that are not called up for service, whether it is possible to mow down in this way, and how the disease will affect the life of a young person.
Content of article
- What diseases are not recruited for?
- How to get out of service?
- What awaits conscripts who mow down from the psychiatric service?
- How mental illness release works in practice
- What are the consequences of psychiatric release
What illnesses are not recruited for?
The list of mental illnesses that are ineligible for compulsory military service is in a document called the Schedule of Diseases. A more detailed list can be found in the fifth chapter of the document.
Recall that thanks to this documentation, representatives and members of the military medical commission determine the eligibility category for a recruit in the process of passing recruiting events.
Let us examine in more detail, in the presence of which mental disorders conscripts are not sent to military service:
- if the conscript is diagnosed with organic mental disorders, which are characterized by clearly noticeable disorders of asthenic, affective, dissociative and cognitive types;
- if a young person is diagnosed with schizophrenia, has mood disorders, psychoses of the endogenous type;
- if there are other mental disorders that were provoked by the presence of an infection or past illnesses;
- if the conscript is diagnosed with neurosis, post-traumatic disorders, depressive states and depressive reactions;
- if there are personality disorders, habit disorders, gender identity or sexual orientation disorders;
- in case of psychosis on the background of alcoholism, in case of chronic alcohol dependence;
- if the conscript has been diagnosed with substance abuse or drug addiction;
- if the conscript has a mental retardation or is diagnosed with autism.

It is not superfluous to note that the above diagnoses have different symptoms. In this regard, in the process of restoring the shelf life category, these categories may differ.
Should you join the army with mental illness?
Take the test and find out right now
Take the test ~ 1 minute
In the event that a conscript has been diagnosed with severe diagnoses, or a psychotic state persists for a long time, by law he must receive an exemption from the army for psychiatry. Also, such a person is completely removed from the register at the military commissariat.
In such situations, the military commission is obliged to put the category "D" on the ticket. After the recruiting events are completed, the young man must be registered with the psycho-neurological dispensary.
If the conscript's illness is less severe or less severe, he must be placed in the reserve. At the same time, the conscript is assigned a category of fitness "B".
A certain list of mental illnesses or disorders are treatable. If a conscript is diagnosed with a disease from this list, according to the rules, the commission at the military registration and enlistment office is obliged to grant the young man a delay of 6 months.
— Alina Petrova, Director of Agenda. No
During this deferral, the conscript must undergo medical treatment. In the event that, after a delay in the process of the next draft board, the person is healthy, he will be sent to military service. In this case, the category of validity "B" is established.
According to the regulations, only the category of validity, according to which the conscript was accepted, should be indicated in the military ID. The ticket should not contain information regarding the disease or the article of the Disease Schedule document, according to which the category was set.
How to get out of service?
In order to be legally exempt from military service for health reasons, you should contact our company.
We will help recruits to pass all the commissions, additional examinations, we will help to get a military ID in psychiatry. Contact us by phone numbers listed on the site, and our managers will answer all your questions.
What awaits conscripts who mow down from the psychiatric service?
If a conscript tries to get out of the army due to mental illness, it will be considered a violation of the law. Such a violation entails criminal liability.
However, as a rule, it is impossible to do this: a psychiatrist works as part of the military medical commission. A professional will definitely be able to distinguish whether a conscript is feigning, or actually has an appropriate diagnosis.
We will answer all your questions
We will help you understand whether you personally should serve
In the event that the psychiatrist has doubts, the conscript is sent for an additional examination to the neuropsychiatric dispensary. As a rule, for examination, a conscript is obliged to become a day hospital and undergo appropriate activities within 1-3 weeks.
During this time, the young person is observed and his behavior is monitored by doctors. Sometimes the military commissariat may send a conscript for additional examination in a psychiatric hospital.
In the event that this happens, the young person receives the appropriate documentation, which must be provided at work for release. Also, such documents are issued for study. In a psychiatric hospital, a conscript undergoes an outpatient examination.
If a conscript really has a number of deviations that correspond to one or another mental disorder, the doctors of the specialized clinic will understand this. Otherwise, an attempt to simulate a disease will be established.
In order to be diagnosed with a disorder, a person must undergo tests or consult with a psychiatrist. In the process of such a conversation, specialists carefully monitor gestures, repeat a series of questions in order to find out if the conscript is lying.
— Alina Petrova, Director of Subpoenas.No
How mental illness exemptions work in practice
Mental illness is a significant reason for a conscript to be transferred to the reserve. However, sometimes it happens that the military commissariat does not perceive the seriousness of the diagnosis of the conscript, or they ignore the problem. In such cases, even a large person can be called into service.
Let's talk about one of the situations in our practice. The young man turned to our company at the very moment he received the summons to send.
The conscript claimed that during the commission a doctor from the military commissariat forced him to rewrite the passed mental test. After that, the category "B" was approved by the doctor. In connection with this category, the conscript became fit, and the military registration and enlistment office issued him a summons to be sent to military service.
After we filed a complaint with a higher military registration and enlistment office, the conscript managed to avoid a decision on conscription. As soon as the decision was canceled, our specialists helped the young man to confirm the diagnosis: he went through the events at the military commissariat again and received a military ID.
As soon as the decision was canceled, our specialists helped the young man to confirm the diagnosis: he went through the events at the military commissariat again and received a military ID.
What are the consequences of a psychiatric release?
It is widely believed that if a conscript has received a psychiatric qualification, he will have restrictions in later life, or a number of responsibilities.
As a rule, young people with diagnoses are required to register with a psychoneurological dispensary, they must attend consultations with a psychiatrist without fail. In addition, such people cannot drive a vehicle, it is difficult for them to get a job or obtain a gun license.
— Alina Petrova, Director of Subpoenas. No
In the event that a conscript has been diagnosed with a severe diagnosis, for example, schizophrenia, such restrictions are in place. Nevertheless, there is a list of diseases, according to which you can get rid of the army and avoid changes in life.
These diseases include all kinds of neuroses, stress disorders, and other pathologies. It is not necessary that the presence of such a disease should affect the future life of the conscript.
Legal company Agenda.Net®
We have been protecting the rights and interests of conscripts since 2015.
Services for conscripts ›
whether people with depression and other mental disorders are subject to conscription, how to confirm the diagnosis for the commission
I am 24 years old and I have been diagnosed with recurrent depressive disorder, as Russian doctors call it. Now I take antidepressants. Can I be mobilized?
Daniil Davydov
medical journalist
Author profile
Recurrent depressive disorder, or major depressive disorder, as this disease is called abroad, is a chronic mental disorder. People with such a diagnosis receive category B in peacetime and do not serve in the army. But, according to the psychiatrist with whom we talked, if a person does not submit medical documents confirming the diagnosis to the military registration and enlistment office and does not complain about health, during partial mobilization, a person with depression can still be called up.
At the same time, there are other categories of people with mental illness who are not called up even during mobilization.
Go see a doctor
Our articles are written with love for evidence-based medicine. We refer to authoritative sources and go to doctors with a good reputation for comments. But remember: the responsibility for your health lies with you and your doctor. We don't write prescriptions, we make recommendations. Relying on our point of view or not is up to you.
What mental illnesses serve as grounds for deferment or cancellation of conscription
For all chronic mental disorders, due to which a person does not lose his ability to work, the medical commission assigns fitness category B. These are, for example:
- anxiety disorders;
- affective disorders such as recurrent depression or bipolar affective disorder;
- consequences of early organic brain damage.

Outside of the declared mobilization, a person with category B is not involved in military service. But the problem is that Decree No. 647 does not specify which specific categories of citizens are subject to partial mobilization, so people with category B can still be called up.
Decree of the President of the Russian Federation dated September 21, 2022 No. 647
One way or another, in order to receive category B, you should contact the dispensary department of the state round-the-clock psychiatric hospital at the place of registration or actual residence and receive a referral for hospitalization in a psychiatric hospital. The survey lasts 10 days. They will carry out diagnostics, and then an examination, after which the doctors will send the conclusion directly to the military registration and enlistment office.
But it is important to keep in mind that during partial mobilization, the military enlistment office conducts a medical examination, but not a commission. If a person mobilized during a medical examination complains about his health, doctors have the right to send him for an additional examination to a medical institution.
If a person mobilized during a medical examination complains about his health, doctors have the right to send him for an additional examination to a medical institution.
In case of partial mobilization, a medical examination is carried out in a unit or on the basis of the military registration and enlistment office - “Explain-rf”
Under no circumstances are people with mental disorders taken into the army, due to which a person lost his ability to work and received a disability of the first or second group. Such people belong to category D. The list, for example, includes:
- schizophrenia;
- schizoaffective disorder;
- persistent effects of brain injury;
- severe epilepsy.
Community 11/23/21
What is depression?
Documents needed to avoid being drafted
Right now, the only sure way to not be drafted due to a mental illness is to have a Group 1 or 2 disability associated with it. If a person with a disability still receives a summons, he will need to submit two documents to the military registration and enlistment office:
If a person with a disability still receives a summons, he will need to submit two documents to the military registration and enlistment office:
- Certificate of the first or second disability group.
- Discharge summary from the outpatient card of the neuropsychiatric dispensary.
So what? 09/26/22
Students and graduate students were given a deferment from mobilization: who has the right to it
A diagnosis that allows assigning a category C or D to a serviceman must be made by a medical commission - a team of psychiatrists.
Order of the Ministry of Health dated June 30, 2022 No. 451n “On approval of the procedure for conducting a medical psychiatric examination”, according to which any medical organization licensed for this activity can conduct a psychiatric examination, will enter into force only next year. Until then, it is more reliable to obtain the conclusion of a psychiatric commission after an examination in a psychiatric hospital based on state institutions - any state psychiatric hospital.