Meditation grey matter
Brief Mindfulness Meditation Induces Gray Matter Changes in a Brain Hub
1. Tang Y. Y., Holzel B. K., Posner M. I. The neuroscience of mindfulness meditation. Nature Reviews Neuroscience. 2015;16(4):213–225. doi: 10.1038/nrn3916. [PubMed] [CrossRef] [Google Scholar]
2. Goyal M., Singh S., Sibinga E. M. S., et al. Meditation programs for psychological stress and well-being: a systematic review and meta-analysis. JAMA Internal Medicine. 2014;174(3):357–368. doi: 10.1001/jamainternmed.2013.13018. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
3. Hölzel B. K., Lazar S. W., Gard T., Schuman-Olivier Z., Vago D. R., Ott U. How does mindfulness meditation work? Proposing mechanisms of action from a conceptual and neural perspective. Perspectives on Psychological Science . 2011;6(6):537–559. doi: 10.1177/1745691611419671. [PubMed] [CrossRef] [Google Scholar]
4. Tang Y. Y. The Neuroscience of Mindfulness Meditation: How the Body and Mind Work Together to Change our Behavior? London: Springer Nature; 2017. [CrossRef] [Google Scholar]
5. Fox K. C. R., Nijeboer S., Dixon M. L., et al. Is meditation associated with altered brain structure? A systematic review and meta-analysis of morphometric neuroimaging in meditation practitioners. Neuroscience and Biobehavioral Reviews. 2014;43:48–73. doi: 10.1016/j.neubiorev.2014.03.016. [PubMed] [CrossRef] [Google Scholar]
6. Hölzel B. K., Carmody J., Vangel M., et al. Mindfulness practice leads to increases in regional brain gray matter density. Psychiatry Research: Neuroimaging. 2011;191(1):36–43. doi: 10.1016/j.pscychresns.2010.08.006. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
7. MacCoon D. G., Imel Z. E., Rosenkranz M. A., et al. The validation of an active control intervention for Mindfulness Based Stress Reduction (MBSR) Behaviour Research and Therapy. 2012;50(1):3–12. doi: 10.1016/j.brat.2011.10.011. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
8. Rosenkranz M. A., Davidson R. J., MacCoon D. G., Sheridan J. F., Kalin N. H., Lutz A. A comparison of mindfulness based stress reduction and an active control in modulation of neurogenic inflammation. Brain, Behavior, and Immunity. 2013;27(1):174–184. doi: 10.1016/j.bbi.2012.10.013. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
J., MacCoon D. G., Sheridan J. F., Kalin N. H., Lutz A. A comparison of mindfulness based stress reduction and an active control in modulation of neurogenic inflammation. Brain, Behavior, and Immunity. 2013;27(1):174–184. doi: 10.1016/j.bbi.2012.10.013. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
9. MacCoon D. G., MacLean K. A., Davidson R. J., Saron C. D., Lutz A. No sustained attention differences in a longitudinal randomized trial comparing mindfulness based stress reduction versus active control. PLoS One. 2014;9(6, article e97551) doi: 10.1371/journal.pone.0097551. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
10. Doll A., Hölzel B. K., Boucard C. C., Wohlschläger A. M., Sorg C. Mindfulness is associated with intrinsic functional connectivity between default mode and salience networks. Frontiers in Human Neuroscience. 2015;9:p. 461. doi: 10.3389/fnhum.2015.00461. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
11. Brewer J. A., Worhunsky P. D., Gray J. R., Tang Y. Y., Weber J., Kober H. Meditation experience is associated with differences in default mode network activity and connectivity. Proceedings of the National Academy of Sciences of the United States of America. 2011;108(50):20254–20259. doi: 10.1073/pnas.1112029108. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
Brewer J. A., Worhunsky P. D., Gray J. R., Tang Y. Y., Weber J., Kober H. Meditation experience is associated with differences in default mode network activity and connectivity. Proceedings of the National Academy of Sciences of the United States of America. 2011;108(50):20254–20259. doi: 10.1073/pnas.1112029108. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
12. Creswell J. D., Taren A. A., Lindsay E. K., et al. Alterations in resting-state functional connectivity link mindfulness meditation with reduced interleukin-6: a randomized controlled trial. Biological Psychiatry. 2016;80(1):53–61. doi: 10.1016/j.biopsych.2016.01.008. [PubMed] [CrossRef] [Google Scholar]
13. Wells R. E., Yeh G. Y., Kerr C. E., et al. Meditation’s impact on default mode network and hippocampus in mild cognitive impairment: a pilot study. Neuroscience Letters. 2013;556:15–19. doi: 10.1016/j.neulet.2013.10.001. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
14. Leech R., Sharp D. J. The role of the posterior cingulate cortex in cognition and disease. Brain. 2014;137(1):12–32. doi: 10.1093/brain/awt162. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
Leech R., Sharp D. J. The role of the posterior cingulate cortex in cognition and disease. Brain. 2014;137(1):12–32. doi: 10.1093/brain/awt162. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
15. Tang Y. Y., Ma Y., Wang J., et al. Short-term meditation training improves attention and self-regulation. Proceedings of the National Academy of Sciences of the United States of America. 2007;104(43):17152–17156. doi: 10.1073/pnas.0707678104. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
16. Tang Y. Y., Ma Y., Fan Y., et al. Central and autonomic nervous system interaction is altered by short-term meditation. Proceedings of the National Academy of Sciences of the United States of America. 2009;106(22):8865–8870. doi: 10.1073/pnas.0904031106. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
17. Tang Y. Y., Lu Q., Geng X., Stein E. A., Yang Y., Posner M. I. Short-term meditation induces white matter changes in the anterior cingulate.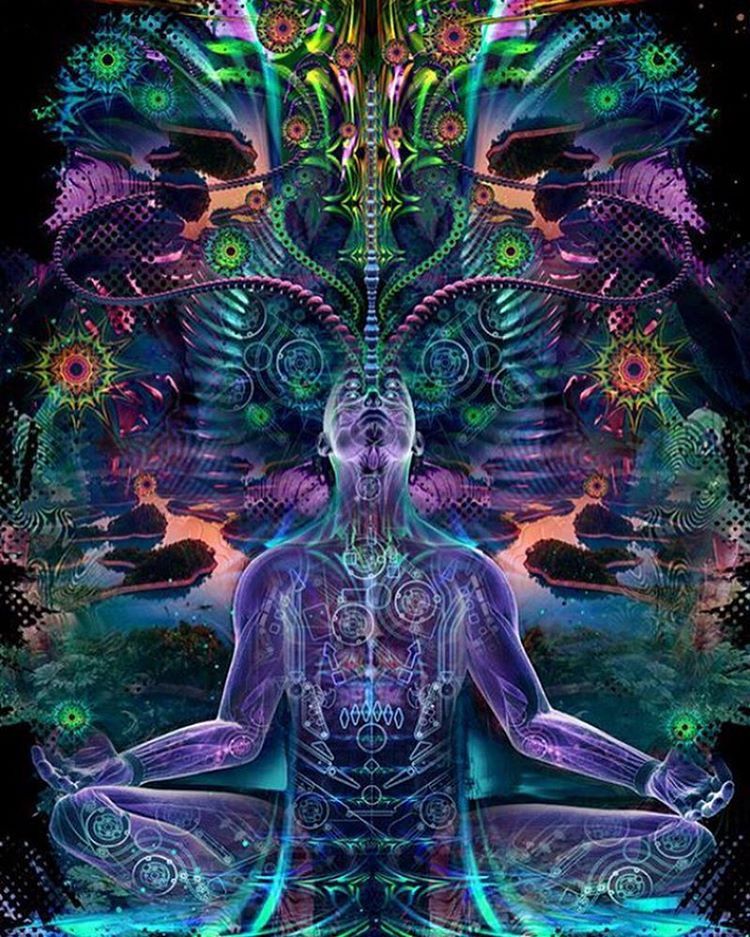 Proceedings of the National Academy of Sciences of the United States of America. 2010;107(35):15649–15652. doi: 10.1073/pnas.1011043107. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
Proceedings of the National Academy of Sciences of the United States of America. 2010;107(35):15649–15652. doi: 10.1073/pnas.1011043107. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
18. Tang Y. Y., Lu Q., Fan M., Yang Y., Posner M. I. Mechanisms of white matter changes induced by meditation. Proceedings of the National Academy of Sciences of the United States of America. 2012;109(26):10570–10574. doi: 10.1073/pnas.1207817109. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
19. Mori S., Wakana S., van Zijl P. C., et al. MRI Atlas of Human White Matter. New York: Elsevier Science; 2005. [Google Scholar]
20. Wakana S., Jiang H., Nagae-Poetscher L. M., van Zijl P. C. M., Mori S. Fiber tract-based atlas of human white matter anatomy. Radiology. 2004;230(1):77–87. doi: 10.1148/radiol.2301021640. [PubMed] [CrossRef] [Google Scholar]
21. Raichle M. E., MacLeod A. M., Snyder A. Z., Powers W. J., Gusnard D. A., Shulman G. L. A default mode of brain function. Proceedings of the National Academy of Sciences of the United States of America. 2001;98(2):676–682. doi: 10.1073/pnas.98.2.676. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
L. A default mode of brain function. Proceedings of the National Academy of Sciences of the United States of America. 2001;98(2):676–682. doi: 10.1073/pnas.98.2.676. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
22. Hagmann P., Cammoun L., Gigandet X., et al. Mapping the structural core of human cerebral cortex. PLoS Biology. 2008;6(7, article e159) doi: 10.1371/journal.pbio.0060159. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
23. Lu H., Song Y., Xu M., Wang X., Li X., Liu J. The brain structure correlates of individual differences in trait mindfulness: a voxel-based morphometry study. Neuroscience. 2014;272:21–28. doi: 10.1016/j.neuroscience.2014.04.051. [PubMed] [CrossRef] [Google Scholar]
24. Chételat G., Mézenge F., Tomadesso C., et al. Reduced age-associated brain changes in expert meditators: a multimodal neuroimaging pilot study. Scientific Reports. 2017;7(1, article 10160) doi: 10.1038/s41598-017-07764-x. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
[PMC free article] [PubMed] [CrossRef] [Google Scholar]
25. Tang Y. Y., Hölzel B. K., Posner M. I. Traits and states in mindfulness meditation. Nature Reviews Neuroscience. 2016;17(1):p. 59. doi: 10.1038/nrn.2015.7. [PubMed] [CrossRef] [Google Scholar]
26. Rothbart M. K., Ahadi S. A., Evans D. E. Temperament and personality: origins and outcomes. Journal of Personality and Social Psychology. 2000;78(1):122–135. doi: 10.1037/0022-3514.78.1.122. [PubMed] [CrossRef] [Google Scholar]
27. Evans D. E., Rothbart M. K. Developing a model for adult temperament. Journal of Research in Personality. 2007;41(4):868–888. doi: 10.1016/j.jrp.2006.11.002. [CrossRef] [Google Scholar]
28. Tang Y.-Y., Tang R., Jiang C., Posner M. I. Short-term meditation intervention improves self-regulation and academic performance. Journal of Child and Adolescent Behaviour. 2014;2(4):p. 154. doi: 10.4172/2375-4494.1000154. [CrossRef] [Google Scholar]
29. Ding X. , Tang Y. Y., Tang R., Posner M. I. Improving creativity performance by short-term meditation. Behavioral and Brain Functions. 2014;10(1):p. 9. doi: 10.1186/1744-9081-10-9. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
, Tang Y. Y., Tang R., Posner M. I. Improving creativity performance by short-term meditation. Behavioral and Brain Functions. 2014;10(1):p. 9. doi: 10.1186/1744-9081-10-9. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
30. Fan Y., Tang Y. Y., Tang R., Posner M. I. Time course of conflict processing modulated by brief meditation training. Frontiers in Psychology. 2015;6:p. 911. doi: 10.3389/fpsyg.2015.00911. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
31. Reuter M., Schmansky N. J., Rosas H. D., Fischl B. Within-subject template estimation for unbiased longitudinal image analysis. NeuroImage. 2012;61(4):1402–1418. doi: 10.1016/j.neuroimage.2012.02.084. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
32. Reuter M., Fischl B. Avoiding asymmetry-induced bias in longitudinal image processing. NeuroImage. 2011;57(1):19–21. doi: 10.1016/j.neuroimage.2011.02.076. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
33. Reuter M., Rosas H. D., Fischl B. Highly accurate inverse consistent registration: a robust approach. NeuroImage. 2010;53(4):1181–1196. doi: 10.1016/j.neuroimage.2010.07.020. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
Reuter M., Rosas H. D., Fischl B. Highly accurate inverse consistent registration: a robust approach. NeuroImage. 2010;53(4):1181–1196. doi: 10.1016/j.neuroimage.2010.07.020. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
34. Lim H. K., Jung W. S., Ahn K. J., et al. Regional cortical thickness and subcortical volume changes are associated with cognitive impairments in the drug-naive patients with late-onset depression. Neuropsychopharmacology. 2012;37(3):838–849. doi: 10.1038/npp.2011.264. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
35. Hervais-Adelman A., Moser-Mercer B., Murray M. M., Golestani N. Cortical thickness increases after simultaneous interpretation training. Neuropsychologia. 2017;98:212–219. doi: 10.1016/j.neuropsychologia.2017.01.008. [PubMed] [CrossRef] [Google Scholar]
36. Pegueroles J., Vilaplana E., Montal V., et al. Longitudinal brain structural changes in preclinical Alzheimer’s disease. Alzheimer’s & Dementia. 2017;13(5):499–509. doi: 10.1016/j.jalz.2016.08.010. [PubMed] [CrossRef] [Google Scholar]
2017;13(5):499–509. doi: 10.1016/j.jalz.2016.08.010. [PubMed] [CrossRef] [Google Scholar]
37. Bercaw E. L., Hanks R. A., Millis S. R., Gola T. J. Changes in neuropsychological performance after traumatic brain injury from inpatient rehabilitation to 1-year follow-up in predicting 2-year functional outcomes. The Clinical Neuropsychologist. 2010;25(1):72–89. doi: 10.1080/13854046.2010.532813. [PubMed] [CrossRef] [Google Scholar]
38. Nesvåg R., Bergmann Ø., Rimol L. M., et al. A 5-year follow-up study of brain cortical and subcortical abnormalities in a schizophrenia cohort. Schizophrenia Research. 2012;142(1-3):209–216. doi: 10.1016/j.schres.2012.10.004. [PubMed] [CrossRef] [Google Scholar]
39. Storsve A. B., Fjell A. M., Tamnes C. K., et al. Differential longitudinal changes in cortical thickness, surface area and volume across the adult life span: regions of accelerating and decelerating change. The Journal of Neuroscience. 2014;34(25):8488–8498. doi: 10.1523/JNEUROSCI.0391-14.2014. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
doi: 10.1523/JNEUROSCI.0391-14.2014. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
40. Greenberg J., Romero V. L., Elkin-Frankston S., Bezdek M. A., Schumacher E. H., Lazar S. W. Reduced interference in working memory following mindfulness training is associated with increases in hippocampal volume. Brain Imaging and Behavior. 2019;13(2):366–376. doi: 10.1007/s11682-018-9858-4. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
41. Destrieux C., Fischl B., Dale A., Halgren E. Automatic parcellation of human cortical gyri and sulci using standard anatomical nomenclature. NeuroImage. 2010;53(1):1–15. doi: 10.1016/j.neuroimage.2010.06.010. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
42. Tang Y. Y., Tang R., Gross J. J. Promoting psychological well-being through an evidence-based mindfulness training program. Frontiers in Human Neuroscience. 2019;13:p. 237. doi: 10.3389/fnhum.2019.00237. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
43. Lutz A., Slagter H. A., Dunne J. D., Davidson R. J. Attention regulation and monitoring in meditation. Trends in Cognitive Sciences. 2008;12(4):163–169. doi: 10.1016/j.tics.2008.01.005. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
Lutz A., Slagter H. A., Dunne J. D., Davidson R. J. Attention regulation and monitoring in meditation. Trends in Cognitive Sciences. 2008;12(4):163–169. doi: 10.1016/j.tics.2008.01.005. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
44. Hölzel B. K., Carmody J., Evans K. C., et al. Stress reduction correlates with structural changes in the amygdala. Social Cognitive and Affective Neuroscience. 2010;5(1):11–17. doi: 10.1093/scan/nsp034. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
45. Takeuchi H., Taki Y., Sassa Y., et al. Working memory training using mental calculation impacts regional gray matter of the frontal and parietal regions. PLoS One. 2011;6(8, article e23175) doi: 10.1371/journal.pone.0023175. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
46. Gotink R. A., Vernooij M. W., Ikram M. A., et al. Meditation and yoga practice are associated with smaller right amygdala volume: the Rotterdam study. Brain Imaging and Behavior. 2018;12(6):1631–1639. doi: 10.1007/s11682-018-9826-z. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
2018;12(6):1631–1639. doi: 10.1007/s11682-018-9826-z. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
47. Brodmann K. Vergleichende Lokalisationslehre der Grosshirnrinde inihren Prinzipien dargestellt auf Grund des Zellenbaues. Berlin: Barth; 1909. [Google Scholar]
48. Vann S. D., Aggleton J. P., Maguire E. A. What does the retrosplenial cortex do? Nature Reviews Neuroscience. 2009;10(11):792–802. doi: 10.1038/nrn2733. [PubMed] [CrossRef] [Google Scholar]
49. https://en.wikipedia.org/wiki/Isthmus_of_cingulate_gyrus.
50. Chrastil E. R. Heterogeneity in human retrosplenial cortex: a review of function and connectivity. Behavioral Neuroscience. 2018;132(5):317–338. doi: 10.1037/bne0000261. [PubMed] [CrossRef] [Google Scholar]
51. Corcoran K. A., Yamawaki N., Leaderbrand K., Radulovic J. Role of retrosplenial cortex in processing stress-related context memories. Behavioral Neuroscience. 2018;132(5):388–395. doi: 10. 1037/bne0000223. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
1037/bne0000223. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
52. Huang Y., Hullfish J., de Ridder D., Vanneste S. Meta-analysis of functional subdivisions within human posteromedial cortex. Brain Structure & Function. 2019;224(1):435–452. doi: 10.1007/s00429-018-1781-3. [PubMed] [CrossRef] [Google Scholar]
53. McLaren M. E., Szymkowicz S. M., O’Shea A., Woods A. J., Anton S. D., Dotson V. M. Dimensions of depressive symptoms and cingulate volumes in older adults. Translational Psychiatry. 2016;6(4, article e788) doi: 10.1038/tp.2016.49. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
54. Caetano S. C., Kaur S., Brambilla P., et al. Smaller cingulate volumes in unipolar depressed patients. Biological Psychiatry. 2006;59(8):702–706. doi: 10.1016/j.biopsych.2005.10.011. [PubMed] [CrossRef] [Google Scholar]
55. Yeh P. H., Zhu H., Nicoletti M. A., Hatch J. P., Brambilla P., Soares J. C. Structural equation modeling and principal component analysis of gray matter volumes in major depressive and bipolar disorders: differences in latent volumetric structure. Psychiatry Research. 2010;184(3):177–185. doi: 10.1016/j.pscychresns.2010.07.007. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
Psychiatry Research. 2010;184(3):177–185. doi: 10.1016/j.pscychresns.2010.07.007. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
56. Pan P., Zhu L., Yu T. T., et al. Aberrant spontaneous low-frequency brain activity in amnestic mild cognitive impairment: a meta-analysis of resting-state fMRI studies. Ageing Research Reviews. 2017;35:12–21. doi: 10.1016/j.arr.2016.12.001. [PubMed] [CrossRef] [Google Scholar]
57. Wang H., Tan L., Wang H. F., et al. Magnetic resonance spectroscopy in Alzheimer’s disease: systematic review and meta-analysis. Journal of Alzheimer’s Disease. 2015;46(4):1049–1070. doi: 10.3233/JAD-143225. [PubMed] [CrossRef] [Google Scholar]
58. Tumati S., Martens S., Aleman A. Magnetic resonance spectroscopy in mild cognitive impairment: systematic review and meta-analysis. Neuroscience and Biobehavioral Reviews. 2013;37(10):2571–2586. doi: 10.1016/j.neubiorev.2013.08.004. [PubMed] [CrossRef] [Google Scholar]
59. Reiman E. M., Caselli R. J., Chen K., Alexander G. E., Bandy D., Frost J. Declining brain activity in cognitively normal apolipoprotein E epsilon 4 heterozygotes: a foundation for using positron emission tomography to efficiently test treatments to prevent Alzheimer’s disease. Proceedings of the National Academy of Sciences of the United States of America. 2001;98(6):3334–3339. doi: 10.1073/pnas.061509598. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
Reiman E. M., Caselli R. J., Chen K., Alexander G. E., Bandy D., Frost J. Declining brain activity in cognitively normal apolipoprotein E epsilon 4 heterozygotes: a foundation for using positron emission tomography to efficiently test treatments to prevent Alzheimer’s disease. Proceedings of the National Academy of Sciences of the United States of America. 2001;98(6):3334–3339. doi: 10.1073/pnas.061509598. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
60. Reiman E. M., Chen K., Alexander G. E., et al. Functional brain abnormalities in young adults at genetic risk for late-onset Alzheimer’s dementia. Proceedings of the National Academy of Sciences of the United States of America. 2004;101(1):284–289. doi: 10.1073/pnas.2635903100. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
61. Maarouf C. L., Kokjohn T. A., Walker D. G., et al. Biochemical assessment of precuneus and posterior cingulate gyrus in the context of brain aging and Alzheimer’s disease. PLoS One. 2014;9(8, article e105784) doi: 10.1371/journal.pone.0105784. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
PLoS One. 2014;9(8, article e105784) doi: 10.1371/journal.pone.0105784. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
62. He Y., Wang L., Zang Y., et al. Regional coherence changes in the early stages of Alzheimer’s disease: a combined structural and resting-state functional MRI study. NeuroImage. 2007;35(2):488–500. doi: 10.1016/j.neuroimage.2006.11.042. [PubMed] [CrossRef] [Google Scholar]
63. Sperling R. A., LaViolette P. S., O’Keefe K., et al. Amyloid deposition is associated with impaired default network function in older persons without dementia. Neuron. 2009;63(2):178–188. doi: 10.1016/j.neuron.2009.07.003. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
64. Ries M. L., Schmitz T. W., Kawahara T. N., Torgerson B. M., Trivedi M. A., Johnson S. C. Task-dependent posterior cingulate activation in mild cognitive impairment. NeuroImage. 2006;29(2):485–492. doi: 10.1016/j.neuroimage.2005.07.030. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
65. Fjell A. M., Walhovd K. B., Reinvang I., et al. Selective increase of cortical thickness in high-performing elderly--structural indices of optimal cognitive aging. NeuroImage. 2006;29(3):984–994. doi: 10.1016/j.neuroimage.2005.08.007. [PubMed] [CrossRef] [Google Scholar]
Fjell A. M., Walhovd K. B., Reinvang I., et al. Selective increase of cortical thickness in high-performing elderly--structural indices of optimal cognitive aging. NeuroImage. 2006;29(3):984–994. doi: 10.1016/j.neuroimage.2005.08.007. [PubMed] [CrossRef] [Google Scholar]
66. Gard T., Hölzel B. K., Lazar S. W. The potential effects of meditation on age-related cognitive decline: a systematic review. Annals of the New York Academy of Sciences. 2014;1307(1):89–103. doi: 10.1111/nyas.12348. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
67. Koenigsberg H. W., Fan J., Ochsner K. N., et al. Neural correlates of using distancing to regulate emotional responses to social situations. Neuropsychologia. 2010;48(6):1813–1822. doi: 10.1016/j.neuropsychologia.2010.03.002. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
68. Morawetz C., Bode S., Derntl B., Heekeren H. R. The effect of strategies, goals and stimulus material on the neural mechanisms of emotion regulation: a meta-analysis of fMRI studies. Neuroscience and Biobehavioral Reviews. 2017;72:111–128. doi: 10.1016/j.neubiorev.2016.11.014. [PubMed] [CrossRef] [Google Scholar]
Neuroscience and Biobehavioral Reviews. 2017;72:111–128. doi: 10.1016/j.neubiorev.2016.11.014. [PubMed] [CrossRef] [Google Scholar]
69. Powers J. P., LaBar K. S. Regulating emotion through distancing: a taxonomy, neurocognitive model, and supporting meta-analysis. Neuroscience and Biobehavioral Reviews. 2019;96:155–173. doi: 10.1016/j.neubiorev.2018.04.023. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
70. Adapa R. M., Davis M. H., Stamatakis E. A., Absalom A. R., Menon D. K. Neural correlates of successful semantic processing during propofol sedation. Human Brain Mapping. 2014;35(7):2935–2949. doi: 10.1002/hbm.22375. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
71. Koch C., Massimini M., Boly M., Tononi G. Neural correlates of consciousness: progress and problems. Nature Reviews Neuroscience. 2016;17(5):307–321. doi: 10.1038/nrn.2016.22. [PubMed] [CrossRef] [Google Scholar]
72. Koch C., Massimini M., Boly M. , Tononi G. Posterior and anterior cortex – where is the difference that makes the difference? Nature Reviews Neuroscience. 2016;17(10):p. 666. doi: 10.1038/nrn.2016.105. [PubMed] [CrossRef] [Google Scholar]
, Tononi G. Posterior and anterior cortex – where is the difference that makes the difference? Nature Reviews Neuroscience. 2016;17(10):p. 666. doi: 10.1038/nrn.2016.105. [PubMed] [CrossRef] [Google Scholar]
73. Vasey M. W., Harbaugh C. N., Lonigan C. J., et al. Dimensions of temperament and depressive symptoms: replicating a three-way interaction. Journal of Research in Personality. 2013;47(6):908–921. doi: 10.1016/j.jrp.2013.09.001. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
Eight weeks to a better brain – Harvard Gazette
Health & Medicine
"Although the practice of meditation is associated with a sense of peacefulness and physical relaxation, practitioners have long claimed that meditation also provides cognitive and psychological benefits that persist throughout the day," says study senior author Sara Lazar.
Credit: pexels.com
Meditation study shows changes associated with awareness, stress
By Sue McGreevey MGH Communications
Date
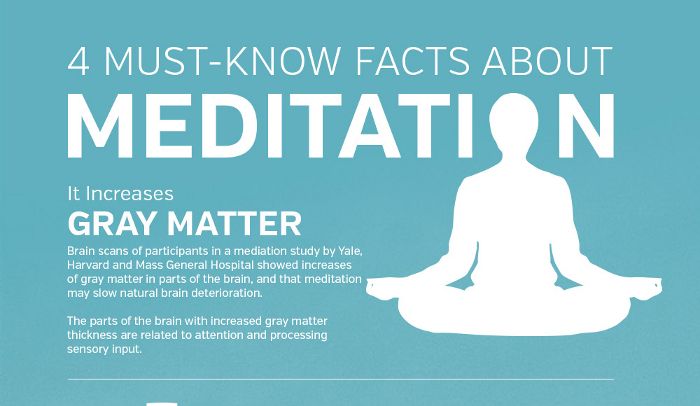
Participating in an eight-week mindfulness meditation program appears to make measurable changes in brain regions associated with memory, sense of self, empathy, and stress. In a study that will appear in the Jan. 30 issue of Psychiatry Research: Neuroimaging, a team led by Harvard-affiliated researchers at Massachusetts General Hospital (MGH) reported the results of their study, the first to document meditation-produced changes over time in the brain’s gray matter.
In a study that will appear in the Jan. 30 issue of Psychiatry Research: Neuroimaging, a team led by Harvard-affiliated researchers at Massachusetts General Hospital (MGH) reported the results of their study, the first to document meditation-produced changes over time in the brain’s gray matter.
“Although the practice of meditation is associated with a sense of peacefulness and physical relaxation, practitioners have long claimed that meditation also provides cognitive and psychological benefits that persist throughout the day,” says study senior author Sara Lazar of the MGH Psychiatric Neuroimaging Research Program and a Harvard Medical School instructor in psychology. “This study demonstrates that changes in brain structure may underlie some of these reported improvements and that people are not just feeling better because they are spending time relaxing.”
Previous studies from Lazar’s group and others found structural differences between the brains of experienced meditation practitioners and individuals with no history of meditation, observing thickening of the cerebral cortex in areas associated with attention and emotional integration. But those investigations could not document that those differences were actually produced by meditation.
But those investigations could not document that those differences were actually produced by meditation.
For the current study, magnetic resonance (MR) images were taken of the brain structure of 16 study participants two weeks before and after they took part in the eight-week Mindfulness-Based Stress Reduction (MBSR) Program at the University of Massachusetts Center for Mindfulness. In addition to weekly meetings that included practice of mindfulness meditation — which focuses on nonjudgmental awareness of sensations, feelings, and state of mind — participants received audio recordings for guided meditation practice and were asked to keep track of how much time they practiced each day. A set of MR brain images was also taken of a control group of nonmeditators over a similar time interval.
Meditation group participants reported spending an average of 27 minutes each day practicing mindfulness exercises, and their responses to a mindfulness questionnaire indicated significant improvements compared with pre-participation responses. The analysis of MR images, which focused on areas where meditation-associated differences were seen in earlier studies, found increased gray-matter density in the hippocampus, known to be important for learning and memory, and in structures associated with self-awareness, compassion, and introspection.
The analysis of MR images, which focused on areas where meditation-associated differences were seen in earlier studies, found increased gray-matter density in the hippocampus, known to be important for learning and memory, and in structures associated with self-awareness, compassion, and introspection.
Participant-reported reductions in stress also were correlated with decreased gray-matter density in the amygdala, which is known to play an important role in anxiety and stress. Although no change was seen in a self-awareness-associated structure called the insula, which had been identified in earlier studies, the authors suggest that longer-term meditation practice might be needed to produce changes in that area. None of these changes were seen in the control group, indicating that they had not resulted merely from the passage of time.
“It is fascinating to see the brain’s plasticity and that, by practicing meditation, we can play an active role in changing the brain and can increase our well-being and quality of life,” says Britta Hölzel, first author of the paper and a research fellow at MGH and Giessen University in Germany. “Other studies in different patient populations have shown that meditation can make significant improvements in a variety of symptoms, and we are now investigating the underlying mechanisms in the brain that facilitate this change.”
“Other studies in different patient populations have shown that meditation can make significant improvements in a variety of symptoms, and we are now investigating the underlying mechanisms in the brain that facilitate this change.”
Amishi Jha, a University of Miami neuroscientist who investigates mindfulness-training’s effects on individuals in high-stress situations, says, “These results shed light on the mechanisms of action of mindfulness-based training. They demonstrate that the first-person experience of stress can not only be reduced with an eight-week mindfulness training program but that this experiential change corresponds with structural changes in the amygdala, a finding that opens doors to many possibilities for further research on MBSR’s potential to protect against stress-related disorders, such as post-traumatic stress disorder.” Jha was not one of the study investigators.
James Carmody of the Center for Mindfulness at University of Massachusetts Medical School is one of the co-authors of the study, which was supported by the National Institutes of Health, the British Broadcasting Company, and the Mind and Life Institute. For more information on the work of Lazar’s team.
For more information on the work of Lazar’s team.
How Meditation Affects the Gray Matter of the Brain
Friends, there is a wonderful doctor of science and a medical practitioner in the USA who is engaged in mind and body research - David Hamilton. In his blog I found an interesting article about the relationship between meditation and brain function. I share with you the translation of this material. If you had doubts whether or not to meditate, then this article, I hope, will resolve them. So
I like to meditate. I am convinced that the feeling of calm that comes from practicing helps me overcome the problems and troubles that inevitably happen in everyone's life. Of course, it happens that 10-15 minutes of silence is an unaffordable luxury. I skip my “workouts”, but I clearly feel their absence on such days.
I don't know a single person who hasn't been affected by stress. Unfortunately, it is the cause of many diseases. According to the Centers for Disease Control and Prevention, nearly 90% of doctor visits in the United States are thought to be related to the effects of stress.
Prolonged stress leads to serious exhaustion of the body. It's a direct route to the doctor's office.
Just like aspirin is a headache pill, meditation is the antidote to anxiety. Regular practice is a significant contribution to health: it calms the nervous system, improves immunity, and evens out the heart rhythm. It has been observed that meditation promotes the production of nitric oxide, which dilates the arteries and thereby lowers blood pressure.
Researchers at the Center for Functional Integrative Neuroscience at the University of Aarhus in Denmark compared brain MRI scans of those who did not meditate and a control group that did not. The results showed that the practice causes real physical changes in the brain - an increase in gray matter volume.
A study by Giuseppe Pagoni and Milos Sekis (scientists in the Department of Psychiatry and Behavioral Sciences at Emory University in Atlanta) compared the volume of gray matter in the brains of people who do Zen meditation with those who are far from this or other ways of contemplation. As a rule, with age, the volume of gray matter in people decreases. But it turned out that in meditators it remains at the same level.
As a rule, with age, the volume of gray matter in people decreases. But it turned out that in meditators it remains at the same level.
Regular meditation saves not only the physical resources of the body, but also intellectual
Related articles:
Mindfulness against bad habits
Walking Meditation: Walking for the Benefits of Body and Soul
In 2008, the impact of practice on gene activation was discovered at Harvard University. Even for beginners who have completed an eight-week course, about 1,560 genes are affected. For long-term adherents, this figure fluctuates around 2,200 genes. The study noted that meditation triggers delayed physiological effects, one of which is to slow down the rate of aging.
We have all heard stories of people who were so shocked that their hair turned white in a matter of weeks. We know that stress accelerates the aging process. So why does it come as a surprise to many that stress management techniques can slow down fading?
Early gray hair can be caused by genetic predisposition, but more often by stressful situations
There are many types of meditation. For example, insight meditation is a technique for moving attention to the body or breath. Observations conducted at the Massachusetts General Hospital found that practice thickens the prefrontal cortex of the brain, which is responsible for attention. This effect is due to the fact that the brain is somewhat similar to muscles. When we run, swim, lift weights and squat, the muscle groups involved become larger and tighter. A similar situation occurs with the contents of the human cranium: those areas that are in tension increase. This phenomenon is called neuroplasticity, it characterizes changes in the brain throughout the life of the organism.
For example, insight meditation is a technique for moving attention to the body or breath. Observations conducted at the Massachusetts General Hospital found that practice thickens the prefrontal cortex of the brain, which is responsible for attention. This effect is due to the fact that the brain is somewhat similar to muscles. When we run, swim, lift weights and squat, the muscle groups involved become larger and tighter. A similar situation occurs with the contents of the human cranium: those areas that are in tension increase. This phenomenon is called neuroplasticity, it characterizes changes in the brain throughout the life of the organism.
At university, I was taught that the brain, like yeast dough, grows from birth to a certain age. In adolescence, this "mass" is placed in the oven and baked until cooked. Further, the bun removed from the oven retains its shape and mass (in the case of a confectionery product - until eaten, regarding a person - until death). Teachers passed on the knowledge to me and my classmates that the brain of a mature individual is static, like hardened cement.
This analogy is now abandoned. However, history knows many misconceptions: the Earth is not flat and does not stand on three pillars. The gray matter is sensitive to activity (studying, drawing, walking, running, meditating), it is dynamic until the last breath of the individual.
Don't trade cheerfulness for chronic stress!
Please enable JavaScript to view the comments powered by Disqus.
What actually happens to your brain after meditation?
It is customary to call meditation a special mental state of a person that occurs as a result of certain mental exercises. Scientists have long been interested in meditation and the effects it has on the brain. It is generally believed that meditation helps to cope with depression and stress. What's more, some research suggests that it causes structural changes in the brain. Several months of regular meditation allegedly lead to an increase in gray matter. This is especially true of several areas responsible for memory and emotions. Gray matter is made up of dendrites that receive information from neurons. The more they grow, the more plastic neural circuits become. In other words, the brain begins to work better with information and remember it better. But is it really so?
This is especially true of several areas responsible for memory and emotions. Gray matter is made up of dendrites that receive information from neurons. The more they grow, the more plastic neural circuits become. In other words, the brain begins to work better with information and remember it better. But is it really so?
According to some reports, meditation not only relieves stress, but also increases the volume of gray matter in the brain
Does the MBSR program improve the brain? time. However, other scientists questioned the results of such studies, and there were several reasons for this. The fact is that the recorded changes in the structure of the brain could have arisen for a different reason, not at all related to mediation.
It is quite possible that the increase in gray matter was due to the fact that the brain began to do something new for itself. In other words, the study lacked a control group that would provide more objective information. In addition, a small number of people took part in such studies, which also casts doubt on the results.
According to some scientists, meditation increases the plasticity of neural connections
Scientists at the University of Wisconsin decided to correct all these shortcomings in their new study. They recruited more than seventy volunteers for the experiment. All people were divided into three groups. The first group was engaged in mindfulness-based stress reduction (MBSR program). It involves mindfulness meditation. It is this kind of meditation that is said to contribute most to the increase in gray matter in the brain.
The second group was engaged in healthy eating, music therapy and exercise. The third group of volunteers did nothing at all. But they were told that they would soon begin psychic exercises.
As scientists note in an article published in Science Advances, two months later, no major changes in the brain occurred in any of the volunteers. That is, music therapy and meditation affected the gray matter no more than ordinary everyday life.
People who practiced meditation did not change the structure of the brain
Why meditation does not change the structure of the brain
Is meditation really useless? In fact this is not true. Meditation is practiced to reduce stress and depression. It is quite possible that she really copes with these tasks effectively. However, reducing depression does not require an increase in gray matter volume in the areas responsible for memory or emotions. True, we should not forget that, according to some scientists, meditation, on the contrary, can harm a person’s mental health.
Meditation is practiced to reduce stress and depression. It is quite possible that she really copes with these tasks effectively. However, reducing depression does not require an increase in gray matter volume in the areas responsible for memory or emotions. True, we should not forget that, according to some scientists, meditation, on the contrary, can harm a person’s mental health.
In addition, this study does not yet give grounds to say that meditation does not change the structure of the brain at all. So far, it can only be argued that the volume of gray matter does not increase after two months of training. It is possible that the effect will be noticeable, for example, only after two years of regular meditation. Obviously, a longer study is needed to draw definitive conclusions. Or perhaps people should meditate more diligently.
ATTENTION! We see that you have not yet subscribed to our Yandex.Zen channel. Be sure to subscribe to have access to important information that we do not publish on the site.