Mania is most likely to be characterized by feelings of
Bipolar disorder - Symptoms and causes
Overview
Bipolar disorder, formerly called manic depression, is a mental health condition that causes extreme mood swings that include emotional highs (mania or hypomania) and lows (depression).
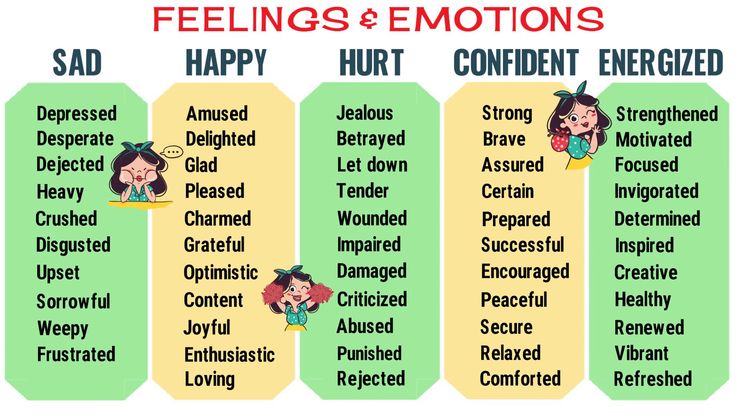
When you become depressed, you may feel sad or hopeless and lose interest or pleasure in most activities. When your mood shifts to mania or hypomania (less extreme than mania), you may feel euphoric, full of energy or unusually irritable. These mood swings can affect sleep, energy, activity, judgment, behavior and the ability to think clearly.
Episodes of mood swings may occur rarely or multiple times a year. While most people will experience some emotional symptoms between episodes, some may not experience any.
Although bipolar disorder is a lifelong condition, you can manage your mood swings and other symptoms by following a treatment plan. In most cases, bipolar disorder is treated with medications and psychological counseling (psychotherapy).
Bipolar disorder care at Mayo Clinic
Products & Services
- Book: Mayo Clinic Family Health Book, 5th Edition
- Newsletter: Mayo Clinic Health Letter — Digital Edition
Symptoms
There are several types of bipolar and related disorders. They may include mania or hypomania and depression. Symptoms can cause unpredictable changes in mood and behavior, resulting in significant distress and difficulty in life.
- Bipolar I disorder. You've had at least one manic episode that may be preceded or followed by hypomanic or major depressive episodes. In some cases, mania may trigger a break from reality (psychosis).
- Bipolar II disorder. You've had at least one major depressive episode and at least one hypomanic episode, but you've never had a manic episode.
- Cyclothymic disorder. You've had at least two years — or one year in children and teenagers — of many periods of hypomania symptoms and periods of depressive symptoms (though less severe than major depression).
- Other types. These include, for example, bipolar and related disorders induced by certain drugs or alcohol or due to a medical condition, such as Cushing's disease, multiple sclerosis or stroke.
Bipolar II disorder is not a milder form of bipolar I disorder, but a separate diagnosis. While the manic episodes of bipolar I disorder can be severe and dangerous, individuals with bipolar II disorder can be depressed for longer periods, which can cause significant impairment.
Although bipolar disorder can occur at any age, typically it's diagnosed in the teenage years or early 20s. Symptoms can vary from person to person, and symptoms may vary over time.
Mania and hypomania
Mania and hypomania are two distinct types of episodes, but they have the same symptoms. Mania is more severe than hypomania and causes more noticeable problems at work, school and social activities, as well as relationship difficulties. Mania may also trigger a break from reality (psychosis) and require hospitalization.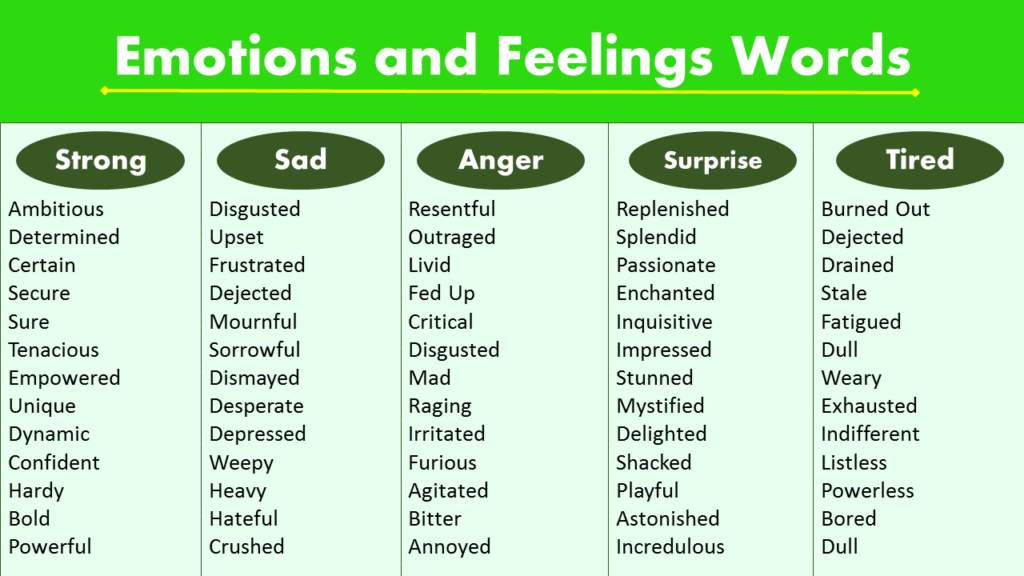
Both a manic and a hypomanic episode include three or more of these symptoms:
- Abnormally upbeat, jumpy or wired
- Increased activity, energy or agitation
- Exaggerated sense of well-being and self-confidence (euphoria)
- Decreased need for sleep
- Unusual talkativeness
- Racing thoughts
- Distractibility
- Poor decision-making — for example, going on buying sprees, taking sexual risks or making foolish investments
Major depressive episode
A major depressive episode includes symptoms that are severe enough to cause noticeable difficulty in day-to-day activities, such as work, school, social activities or relationships. An episode includes five or more of these symptoms:
- Depressed mood, such as feeling sad, empty, hopeless or tearful (in children and teens, depressed mood can appear as irritability)
- Marked loss of interest or feeling no pleasure in all — or almost all — activities
- Significant weight loss when not dieting, weight gain, or decrease or increase in appetite (in children, failure to gain weight as expected can be a sign of depression)
- Either insomnia or sleeping too much
- Either restlessness or slowed behavior
- Fatigue or loss of energy
- Feelings of worthlessness or excessive or inappropriate guilt
- Decreased ability to think or concentrate, or indecisiveness
- Thinking about, planning or attempting suicide
Other features of bipolar disorder
Signs and symptoms of bipolar I and bipolar II disorders may include other features, such as anxious distress, melancholy, psychosis or others. The timing of symptoms may include diagnostic labels such as mixed or rapid cycling. In addition, bipolar symptoms may occur during pregnancy or change with the seasons.
The timing of symptoms may include diagnostic labels such as mixed or rapid cycling. In addition, bipolar symptoms may occur during pregnancy or change with the seasons.
Symptoms in children and teens
Symptoms of bipolar disorder can be difficult to identify in children and teens. It's often hard to tell whether these are normal ups and downs, the results of stress or trauma, or signs of a mental health problem other than bipolar disorder.
Children and teens may have distinct major depressive or manic or hypomanic episodes, but the pattern can vary from that of adults with bipolar disorder. And moods can rapidly shift during episodes. Some children may have periods without mood symptoms between episodes.
The most prominent signs of bipolar disorder in children and teenagers may include severe mood swings that are different from their usual mood swings.
When to see a doctor
Despite the mood extremes, people with bipolar disorder often don't recognize how much their emotional instability disrupts their lives and the lives of their loved ones and don't get the treatment they need.
And if you're like some people with bipolar disorder, you may enjoy the feelings of euphoria and cycles of being more productive. However, this euphoria is always followed by an emotional crash that can leave you depressed, worn out — and perhaps in financial, legal or relationship trouble.
If you have any symptoms of depression or mania, see your doctor or mental health professional. Bipolar disorder doesn't get better on its own. Getting treatment from a mental health professional with experience in bipolar disorder can help you get your symptoms under control.
When to get emergency help
Suicidal thoughts and behavior are common among people with bipolar disorder. If you have thoughts of hurting yourself, call 911 or your local emergency number immediately, go to an emergency room, or confide in a trusted relative or friend. Or contact a suicide hotline. In the U.S., call or text 988 to reach the 988 Suicide & Crisis Lifeline, available 24 hours a day, seven days a week. Or use the Lifeline Chat. Services are free and confidential.
Or use the Lifeline Chat. Services are free and confidential.
If you have a loved one who is in danger of suicide or has made a suicide attempt, make sure someone stays with that person. Call 911 or your local emergency number immediately. Or, if you think you can do so safely, take the person to the nearest hospital emergency room.
Request an Appointment at Mayo Clinic
From Mayo Clinic to your inbox
Sign up for free, and stay up to date on research advancements, health tips and current health topics, like COVID-19, plus expertise on managing health.
To provide you with the most relevant and helpful information, and understand which
information is beneficial, we may combine your email and website usage information with
other information we have about you. If you are a Mayo Clinic patient, this could
include protected health information. If we combine this information with your protected
health information, we will treat all of that information as protected health
information and will only use or disclose that information as set forth in our notice of
privacy practices. You may opt-out of email communications at any time by clicking on
the unsubscribe link in the e-mail.
If we combine this information with your protected
health information, we will treat all of that information as protected health
information and will only use or disclose that information as set forth in our notice of
privacy practices. You may opt-out of email communications at any time by clicking on
the unsubscribe link in the e-mail.
Causes
The exact cause of bipolar disorder is unknown, but several factors may be involved, such as:
- Biological differences. People with bipolar disorder appear to have physical changes in their brains. The significance of these changes is still uncertain but may eventually help pinpoint causes.
- Genetics. Bipolar disorder is more common in people who have a first-degree relative, such as a sibling or parent, with the condition.
 Researchers are trying to find genes that may be involved in causing bipolar disorder.
Researchers are trying to find genes that may be involved in causing bipolar disorder.
Risk factors
Factors that may increase the risk of developing bipolar disorder or act as a trigger for the first episode include:
- Having a first-degree relative, such as a parent or sibling, with bipolar disorder
- Periods of high stress, such as the death of a loved one or other traumatic event
- Drug or alcohol abuse
Complications
Left untreated, bipolar disorder can result in serious problems that affect every area of your life, such as:
- Problems related to drug and alcohol use
- Suicide or suicide attempts
- Legal or financial problems
- Damaged relationships
- Poor work or school performance
Co-occurring conditions
If you have bipolar disorder, you may also have another health condition that needs to be treated along with bipolar disorder. Some conditions can worsen bipolar disorder symptoms or make treatment less successful. Examples include:
Examples include:
- Anxiety disorders
- Eating disorders
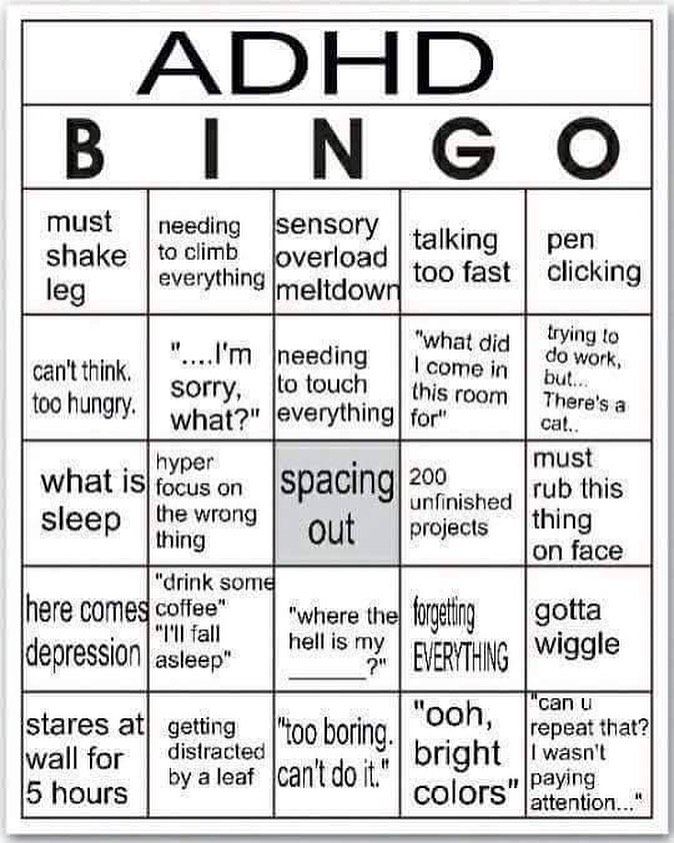
- Attention-deficit/hyperactivity disorder (ADHD)
- Alcohol or drug problems
- Physical health problems, such as heart disease, thyroid problems, headaches or obesity
More Information
- Bipolar disorder care at Mayo Clinic
- Bipolar disorder and alcoholism: Are they related?
Prevention
There's no sure way to prevent bipolar disorder. However, getting treatment at the earliest sign of a mental health disorder can help prevent bipolar disorder or other mental health conditions from worsening.
If you've been diagnosed with bipolar disorder, some strategies can help prevent minor symptoms from becoming full-blown episodes of mania or depression:
- Pay attention to warning signs. Addressing symptoms early on can prevent episodes from getting worse. You may have identified a pattern to your bipolar episodes and what triggers them.
 Call your doctor if you feel you're falling into an episode of depression or mania. Involve family members or friends in watching for warning signs.
Call your doctor if you feel you're falling into an episode of depression or mania. Involve family members or friends in watching for warning signs. - Avoid drugs and alcohol. Using alcohol or recreational drugs can worsen your symptoms and make them more likely to come back.
- Take your medications exactly as directed. You may be tempted to stop treatment — but don't. Stopping your medication or reducing your dose on your own may cause withdrawal effects or your symptoms may worsen or return.
By Mayo Clinic Staff
Related
Associated Procedures
Products & Services
Bipolar Disorder (Manic Depression): Symptoms & Treatment
Overview
What is bipolar disorder?
Bipolar disorder (formerly known as manic-depressive illness or manic depression) is a lifelong mood disorder and mental health condition that causes intense shifts in mood, energy levels, thinking patterns and behavior. These shifts can last for hours, days, weeks or months and interrupt your ability to carry out day-to-day tasks.
These shifts can last for hours, days, weeks or months and interrupt your ability to carry out day-to-day tasks.
There are a few types of bipolar disorder, which involve experiencing significant fluctuations in mood referred to as hypomanic/manic and depressive episodes. However, people with bipolar disorder aren’t always in a hypomanic/manic or depressive state. They also experience periods of normal mood, known as euthymia.
Manic episodes
A key feature of bipolar I disorder is manic episodes. To meet the criteria for bipolar I disorder, you must have had at least one manic episode in your life for at least a week with or without ever experiencing a depressive episode.
Mania is a condition in which you have a period of abnormally elevated or irritable mood, as well as extreme changes in emotions, thoughts, energy, talkativeness and activity level. This highly energized level of physical and mental activity and behavior is a change from your usual self and is noticeable by others.
People who are in manic states may indulge in activities that cause them physical, social or financial harm, such as suddenly spending or gambling extreme amounts of money or driving recklessly. They also occasionally develop psychotic symptoms, such as delusions and hallucinations, which can cause difficulties in distinguishing bipolar disorder from other disorders such as schizophrenia or schizoaffective disorder.
People with certain types of bipolar such as bipolar II disorder experience hypomania, which is a less severe form of mania. It doesn’t last as long as manic episodes and it doesn’t interfere with daily functioning as much.
Depressive episodes
During a depressive episode, you experience a low or depressed mood and/or loss of interest in most activities, as well as many other symptoms of depression, such as:
- Tiredness.
- Changes in appetite.
- Feelings of worthlessness and hopelessness.
Why is bipolar disorder no longer called manic-depressive illness?
In the last few decades, the medical world, especially the field of psychiatry, has intentionally made a shift from using “manic-depressive illness” or “manic depression” to describe bipolar disorder.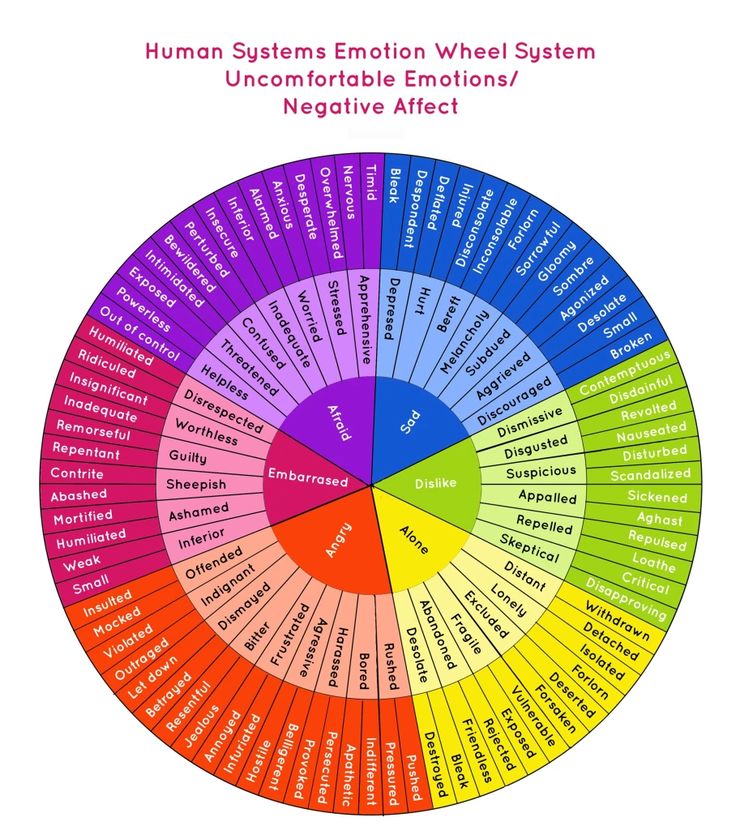 There are several reasons for this shift, including:
There are several reasons for this shift, including:
- Healthcare providers used to use “manic depression” to describe a wide range of mental health conditions. As mental health condition classification systems, including the Diagnostic and Statistical Manual of Mental Disorders (DSM), have become more sophisticated, the new term “bipolar disorder” allows for more clarity in diagnosis.
- There’s a lot of stigma and negativity associated with the terms “manic” and “mania,” especially due to the use of “maniac.” Similarly, people use the term “depression” casually to describe periods of sadness that don’t qualify as clinical depression. Using “bipolar disorder” takes the focus away from these two words. “Bipolar disorder” is more of a clinical, medical term and less emotionally loaded than “manic depression.”
- The term “manic depression” excludes the cyclothymic or hypomanic (bipolar II disorder) versions of the condition.
What are the types of bipolar disorder?
There are four types of bipolar disorder, including:
- Bipolar I disorder: People with bipolar I disorder have experienced one or more episodes of mania.
 Most people with bipolar I will have episodes of both mania and depression, but an episode of depression isn’t necessary for a diagnosis. The depressive episodes usually last at least two weeks. To be diagnosed with bipolar I, your manic episodes must last at least seven days or be so severe that you need hospitalization. People with bipolar I can also experience mixed states (episodes of both manic and depressive symptoms).
Most people with bipolar I will have episodes of both mania and depression, but an episode of depression isn’t necessary for a diagnosis. The depressive episodes usually last at least two weeks. To be diagnosed with bipolar I, your manic episodes must last at least seven days or be so severe that you need hospitalization. People with bipolar I can also experience mixed states (episodes of both manic and depressive symptoms). - Bipolar II disorder: People with bipolar II experience depressive episodes and hypomanic episodes. But they never experience a full manic episode that’s characteristic of bipolar I disorder. While hypomania is less impairing than mania, bipolar II disorder is often more debilitating than bipolar I disorder due to chronic depression being more common in bipolar II.
- Cyclothymic disorder (cyclothymia): People with cyclothymic disorder have a chronically unstable mood state. They experience hypomania and mild depression for at least two years.
 People with cyclothymia may have brief periods of normal mood (euthymia), but these periods last fewer than eight weeks.
People with cyclothymia may have brief periods of normal mood (euthymia), but these periods last fewer than eight weeks. - Other specified and unspecified bipolar and related disorders: If a person doesn’t meet the diagnostic criteria for bipolar I, II or cyclothymia but has still experienced periods of clinically significant abnormal mood elevation, it’s considered other specified or unspecified bipolar disorder.
What’s the difference between borderline personality disorder and bipolar disorder?
While borderline personality disorder (BPD) and bipolar disorder have similar symptoms and are often confused for each other, they’re distinct conditions.
BPD involves a longstanding pattern of abrupt, moment-to-moment swings in moods, behavior and self-image that are often triggered by conflicts in interactions with other people. Nonsuicidal self-injury is also common in BPD but not in bipolar disorder.
Bipolar disorder is different from BPD because it involves distinct, longer-lasting episodes of mania/hypomania and/or depression. Several things can trigger manic or depressive episodes, such as sleep changes, stress, medications and substance use.
Several things can trigger manic or depressive episodes, such as sleep changes, stress, medications and substance use.
Who does bipolar disorder affect?
Bipolar disorder can affect anyone. The average age of onset is 25 years, but, more rarely, it can start as early as early childhood or as late as in your 40s or 50s.
Although bipolar disorder affects people assigned female at birth (AFAB) and people assigned male at birth (AMAB) in equal numbers, the condition tends to affect them differently.
People AFAB with bipolar disorder may switch moods more quickly. When people with bipolar disorder experience four or more manic or depressive episodes in a year, this is called “rapid cycling.” Varying levels of sex hormones and thyroid hormones, together with the tendency for people AFAB to be prescribed antidepressants, may contribute to the more rapid cycling in this population.
People AFAB with bipolar disorder may also experience more periods of depression than people AMAB.
How common is bipolar disorder?
Bipolar disorder affects approximately 5.7 million adult Americans or about 2.6% of the U.S. population.
Symptoms and Causes
What are the signs and symptoms of bipolar disorder?
The defining sign of bipolar I disorder is a manic episode that lasts at least one week, while people with bipolar II disorder or cyclothymia experience hypomanic episodes.
But many people with bipolar disorder experience both hypomanic/manic and depressive episodes. These changing mood states don’t always follow a set pattern, and depression doesn’t always follow manic phases. A person may also experience the same mood state several times — with periods of euthymia in between — before experiencing the opposite mood.
Mood changes in bipolar disorder can happen over a period of weeks, months and sometimes even years.
An important aspect of the mood changes is that they’re a departure from your regular self and that the mood change is sustained for a long time. It may be many days or weeks in the case of mania and many weeks or months in the case of depression.
It may be many days or weeks in the case of mania and many weeks or months in the case of depression.
The severity of the depressive and manic phases can differ from person to person and in the same person at different times.
Signs and symptoms of manic episodes
Some people with bipolar disorder will have episodes of mania or hypomania many times throughout their life; others may experience them only rarely.
Signs and symptoms of a manic episode include:
- Excessive happiness, hopefulness and excitement.
- Sudden and severe changes in mood, such as going from being joyful to being angry and hostile.
- Restlessness.
- Rapid speech and racing thoughts.
- Increased energy and less need for sleep.
- Increased impulsivity and poor judgment, such as suddenly quitting your job.
- Making grand and unattainable plans.
- Reckless and risk-taking behavior, such as drug and alcohol misuse and having unsafe or unprotected sex.
- Feeling like you’re unusually important, talented or powerful.
- Psychosis — experiencing hallucinations and delusions (in the most severe manic episodes).
Most of the time, people experiencing a manic episode are unaware of the negative consequences of their actions. With bipolar disorder, suicide is an ever-present danger — some people become suicidal in manic episodes, not just depressive episodes.
If a person is having an intense manic episode, especially if they’re experiencing hallucinations and delusions, they may need to be hospitalized to protect themselves and others from possible harm.
Signs and symptoms of hypomania
Some people with bipolar disorder have milder manic-like symptoms. This is called hypomania. With hypomania, you may feel very good and find that you can get a lot done. People with hypomania can often function well in social situations or at work.
You may not feel like anything is wrong during a hypomanic episode.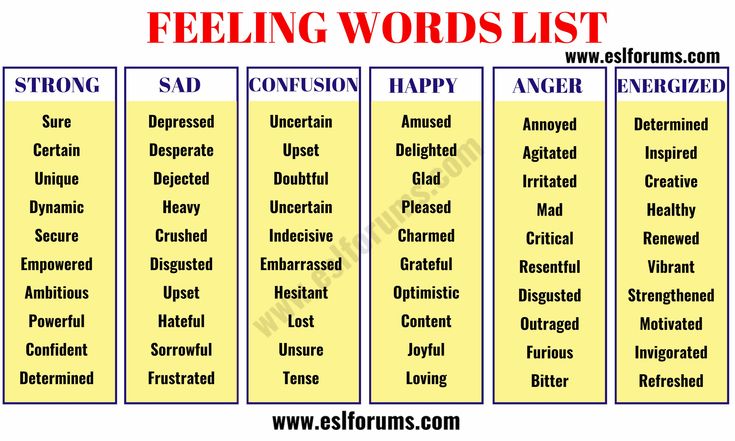 But your family and friends may notice your mood swings and activity level changes and think that they’re unusual for you. After hypomania, you might experience severe depression.
But your family and friends may notice your mood swings and activity level changes and think that they’re unusual for you. After hypomania, you might experience severe depression.
Signs and symptoms of depressive episodes
The symptoms of depressive episodes in bipolar disorder are the same as those of major depression. They include:
- Overwhelming sadness.
- Low energy and fatigue.
- Lack of motivation.
- Feelings of hopelessness or worthlessness.
- Loss of enjoyment of things that were once pleasurable for you.
- Difficulty concentrating and making decisions.
- Uncontrollable crying.
- Irritability.
- Increased need for sleep.
- Insomnia or excessive sleep.
- A change in appetite, causing weight loss or gain.
- Thoughts of death or suicide (suicidal ideation).
If you’re experiencing suicidal ideation (thoughts of suicide), it’s important to seek immediate care. Call 911 or the National Suicide Prevention Lifeline at 1.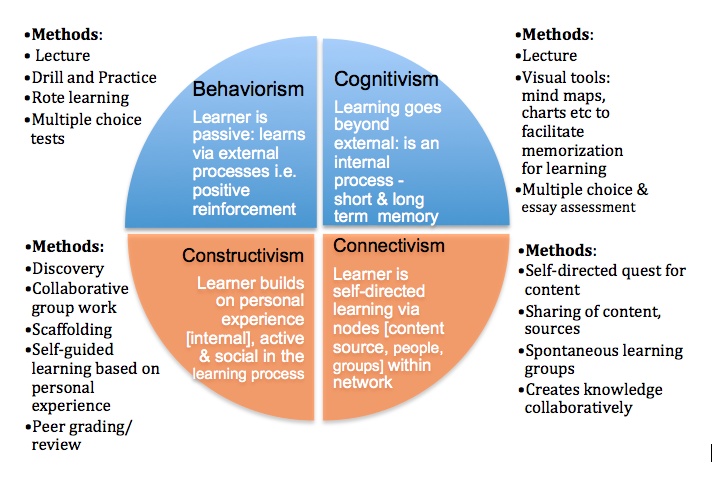 800.273.8255. Someone will be available to talk with you 24 hours a day, seven days a week.
800.273.8255. Someone will be available to talk with you 24 hours a day, seven days a week.
Signs and symptoms of a mixed episode
The symptoms of a mixed episode include both manic and depressive symptoms together. During a mixed episode, you have the negative feelings and thoughts that come with depression but also feel agitated, restless and high energy.
People who experience mixed episodes often describe it as the worst part of bipolar disorder.
What causes bipolar disorder?
Scientists don’t yet know the exact cause of bipolar disorder.
But they do believe there’s a strong genetic (inherited) component. Bipolar disorder is considered one of the most heritable psychiatric conditions — more than two-thirds of people with bipolar disorder have at least one close biological relative with the condition. However, just because you have a biological relative with bipolar disorder, doesn’t necessarily mean you’ll also develop it.
Other factors that scientists think contribute to the development of bipolar disorder include:
- Changes in your brain: Researchers have identified subtle differences in the average size or activation of some brain structures in people with bipolar disorder.
 However, brain scans can’t diagnose the condition.
However, brain scans can’t diagnose the condition. - Environmental factors like trauma and stress: A stressful event, such as the death of a loved one, a serious illness, divorce or financial problems can trigger a manic or depressive episode. Because of this, stress and trauma may also play a role in the development of bipolar disorder.
Scientists are currently performing research to determine the relationship that these factors have in bipolar disorder, how they may help prevent its onset and what role they may play in its treatment.
Diagnosis and Tests
How is bipolar disorder diagnosed?
To diagnose bipolar disorder, your healthcare provider may use many tools, including:
- A physical exam.
- A thorough medical history, which will include asking about your symptoms, lifetime history, experiences and family history.
- Medical tests, such as blood tests, to rule out other conditions that could be causing your symptoms, such as hyperthyroidism.
- A mental health evaluation. Your healthcare provider may perform the evaluation, or they may refer you to a mental health specialist, such as a psychologist or psychiatrist.
To be diagnosed with bipolar disorder, you must have experienced at least one episode of mania or hypomania. Mental health providers use the Diagnostic and Statistical Manual of Mental Disorders (DSM) to diagnose the type of bipolar disorder a person may be experiencing.
To determine what type of bipolar disorder you may have, your mental health provider assesses the pattern of symptoms and how much they affect your life during the most severe episodes.
People with bipolar disorder are more likely to also have the following mental health conditions:
- Anxiety.
- Attention-deficit /hyperactivity disorder (ADHD).
- Post-traumatic stress disorder (PTSD).
- Substance use disorders/dual diagnosis.
Because of this, as well as the fact that memory is often impaired during mania so people can’t remember experiencing it, it can be difficult for healthcare providers to properly diagnose people with bipolar disorder.
People with bipolar disorder who are experiencing a severe manic episode with hallucinations may be incorrectly diagnosed with schizophrenia. Bipolar disorder can also be misdiagnosed as borderline personality disorder (BPD).
Because of this, it’s important to be honest and thorough when explaining all of your symptoms and experiences when talking with your healthcare provider. It can also be helpful to include a loved one who may be able to provide additional details about your mental health history in your discussions with your provider.
Management and Treatment
How is bipolar disorder treated?
Treatment can help many people, including those with the most severe forms of bipolar disorder. An effective treatment plan usually includes a combination of the following therapies:
- Psychotherapy (talk therapy).
- Medications.
- Self-management strategies, like education and identifying the early symptoms of an episode or possible triggers of episodes.

- Helpful lifestyle habits, such as exercise, yoga and meditation. These can support, but not replace, treatment.
- Other therapies, such as electroconvulsive therapy (ECT) in cases that are poorly responsive to medication or where rapid control of symptoms is necessary to prevent harm.
Bipolar disorder is a lifelong condition, so treatment is a lifelong commitment. It can sometimes take several months to years before you and your healthcare provider find a comprehensive treatment plan that works best for you. Although this can be discouraging, it’s important to continue treatment.
Episodes of mania and depression typically come back over time. Between episodes, many people with bipolar disorder don’t have mood changes, but some people may have lingering symptoms. Long-term, continuous treatment can help manage these symptoms.
If you have other mental health conditions in addition to bipolar disorder, such as anxiety or ADHD, it can be more difficult to treat the conditions. For example, the antidepressants healthcare providers prescribe to treat obsessive-compulsive disorder (OCD) and the stimulants they prescribe to treat ADHD may worsen symptoms of bipolar disorder and may even trigger a manic episode.
For example, the antidepressants healthcare providers prescribe to treat obsessive-compulsive disorder (OCD) and the stimulants they prescribe to treat ADHD may worsen symptoms of bipolar disorder and may even trigger a manic episode.
Again, even though it may be difficult to treat these conditions, it’s not impossible. Be sure to stay committed to finding a treatment plan that works for you.
What types of therapy are used to treat bipolar disorder?
Psychotherapy, also called “talk therapy,” can be an effective part of the treatment plan for people with bipolar disorder.
Psychotherapy is a term for a variety of treatment techniques that aim to help you identify and change troubling emotions, thoughts and behaviors. Working with a mental health professional, such as a psychologist or psychiatrist, can provide support, education and guidance to you and your family.
Different types of therapy for bipolar disorder include:
- Psychoeducation: Psychoeducation is the way mental health professionals teach people about their mental health conditions.
 As bipolar disorder is a complex condition, learning about the condition and how it can affect your life can help you and your loved ones manage and cope with it better.
As bipolar disorder is a complex condition, learning about the condition and how it can affect your life can help you and your loved ones manage and cope with it better. - Interpersonal and social rhythm therapy (IPSRT): This therapy is designed to help you improve your moods by understanding and working with your biological and social rhythms. IPSRT is an effective therapy for people with mood disorders, including bipolar disorder. It emphasizes techniques to improve medication adherence (taking your medication regularly), manage stressful life events and reduce disruptions in social rhythms (day-to-day differences in habitual behaviors). IPSRT teaches you skills that let you protect yourself against the development of future manic or depressive episodes.
- Family-focused therapy: This therapy is for adults and children with bipolar disorder and their caregivers. During this treatment, your loved ones will join you in therapy sessions of psychoeducation regarding bipolar disorder, communication improvement training and problem-solving skills training.
- Cognitive behavioral therapy (CBT): This is a structured, goal-oriented type of therapy. Your therapist or psychologist helps you take a close look at your thoughts and emotions. You’ll come to understand how your thoughts affect your actions. Through CBT, you can unlearn negative thoughts and behaviors and learn to adopt healthier thinking patterns and habits.
What medications are used to treat bipolar disorder?
Certain medications can help manage symptoms of bipolar disorder. You may need to try several different medications, with guidance from your healthcare provider, before finding what works best.
Medications healthcare providers generally prescribe to treat bipolar disorder include:
- Mood stabilizers.
- Second-generation (“atypical”) neuroleptics (also called antipsychotics).
- Antidepressants.
If you’re taking medication for bipolar disorder, you should:
- Talk with your healthcare provider to understand the risks, side effects and benefits of the medication.
- Tell your healthcare provider about any prescription drugs, over-the-counter medications or supplements you’re already taking.
- Tell your healthcare provider right away if you’re experiencing concerning side effects. They may need to change your dose or try a different medication.
- Remember that medication for bipolar disorder must be taken consistently, as prescribed.
Mood stabilizers for bipolar disorder
People with bipolar disorder typically need mood-stabilizing medication to manage manic or hypomanic episodes.
Types of mood stabilizers and their brand names include:
- Lithium (Eskalith®, Lithobid®, Lithonate®).
- Valproic acid (Depakene®).
- Divalproex sodium (Depakote®).
- Carbamazepine (Tegretol®, Equetro®).
- Lamotrigine (Lamictal®).
Lithium is one of the most widely prescribed and studied medications for treating bipolar disorder. Lithium is a natural salt and will reduce symptoms of mania within two weeks of starting therapy, but it may take weeks to months before the manic symptoms are fully managed. Because of this, healthcare providers often prescribe other drugs like antipsychotic drugs or antidepressant drugs to help manage symptoms.
Because of this, healthcare providers often prescribe other drugs like antipsychotic drugs or antidepressant drugs to help manage symptoms.
Thyroid gland and kidney problems can sometimes develop when taking lithium, so your healthcare provider will monitor the function of your thyroid and kidneys, as well as monitor the levels of lithium in your blood, as levels can easily become too high.
Anything that lowers the level of sodium in your body, such as switching to a low-sodium diet, heavy sweating, fever, vomiting or diarrhea may cause a toxic buildup of lithium in your body. Be aware of these conditions and alert your doctor if you’re on lithium and experience them.
The following are signs of lithium toxicity (lithium overdose). Call your healthcare provider immediately or go to the nearest emergency room if you experience:
- Blurred vision or double vision.
- Irregular pulse.
- Extremely fast or slow heartbeat.
- Difficulty breathing.
- Confusion and dizziness.
- Severe trembling or convulsions.
- Passing large amounts of pee.
- Uncontrolled eye movements.
- Unusual bruising or bleeding.
Neuroleptic medications for bipolar disorder
Healthcare providers often prescribe second-generation or atypical neuroleptics (antipsychotics) in combination with a mood stabilizer for people with bipolar disorder. These medications help with both manic and depressive episodes.
Only four of these drugs are U.S. Food and Drug Administration (FDA)-approved to help treat bipolar depression, including:
- Cariprazine (Vraylar®).
- Lurasidone (Latuda®).
- Olanzapine-fluoxetine combination (Symbyax®).
- Quetiapine (Seroquel®).
However, other medications, such as olanzapine (Zyprexa®), risperidone (Risperdal®) and aripiprazole (Abilify®), are commonly prescribed as well.
Antidepressants for bipolar disorder
Healthcare providers sometimes prescribe antidepressant medication to treat depressive episodes in bipolar disorder, combining the antidepressant with a mood stabilizer to prevent triggering a manic episode.
Antidepressants are never used as the only medication to treat bipolar disorder because only taking an antidepressant drug can trigger a manic episode.
What are the side effects of bipolar disorder medications?
Side effects of bipolar disorder medications are common and vary by medication. It’s important to talk with your healthcare provider about what you can expect when taking certain medications. It’s also important to tell them if you’re experiencing side effects.
Never stop taking your medication unless your healthcare provider tells you to do so. Abruptly stopping medication can cause severe side effects and trigger severe episodes.
The most common side effects of bipolar disorder medications include:
- Weight gain.
- Metabolic dysregulation, including abnormal lipid levels (dyslipidemia), high blood pressure (hypertension) and high blood sugar (hyperglycemia).
- Drowsiness.
- Akathisia — feelings of restlessness and agitation with a compelling need to move, rock or pace.
What other medical treatments are used for bipolar disorder?
Other treatment options your healthcare provider may consider for treating bipolar disorder include:
- Electroconvulsive therapy (ECT): This is a procedure in which a brief application of an electric current to your brain, through your scalp, induces a seizure. It’s most often used to treat people with severe depression. ECT is very safe and highly effective for medication-resistant depression or acute life-threatening mania. It’s the best treatment for mania in people who are pregnant. ECT is uses general anesthesia, so you’ll be asleep during the procedure and won’t feel any pain.
- Transcranial magnetic stimulation (TMS): This therapy involves a short electromagnetic coil that passes an electric current into your brain. Healthcare providers sometimes use it to treat medication-resistant depression. It’s an alternative to ECT. TMS isn’t painful and doesn’t require general anesthesia.

- Thyroid medications: These medications can sometimes act as mood stabilizers. Studies have shown positive results in reducing symptoms in people AFAB with hard-to-treat, rapid-cycling bipolar disorder.
- Ketamine treatment: Ketamine, an anesthetic, given at low doses through an IV, has been proven to provide short-term antidepressant and antisuicidal effects for people with bipolar disorder.
- Hospitalization: This is considered an emergency option in bipolar disorder care. It becomes necessary when someone is experiencing a severe depressive or manic episode and they’re an immediate threat to themselves or others.
What lifestyle changes can help with bipolar disorder?
Your healthcare team will likely recommend making lifestyle changes to stop patterns of behavior that worsen the symptoms of bipolar disorder. Some of these lifestyle changes include:
- Quit drinking alcohol and/or using recreational drugs and tobacco: It’s essential to quit drinking and using drugs, including tobacco, since they can interfere with medications you may take.
 They can also worsen bipolar disorder and trigger a mood episode.
They can also worsen bipolar disorder and trigger a mood episode. - Keep a daily diary or mood chart: Keeping track of your daily thoughts, feelings and behaviors can help you be aware of how well your treatment is working and/or help you identify potential triggers of manic or depressive episodes.
- Maintain a healthy sleep schedule: Bipolar disorder can greatly affect your sleep patterns, and changes in your frequency of sleep can even trigger an episode. Prioritize a routine sleeping schedule, including going to sleep and getting up at the same times every day.
- Exercise: Exercise has been proven to improve mood and mental health in general, so it may help manage your symptoms related to bipolar disorder. Since weight gain is a common side effect of bipolar disorder medications, exercise may also help with weight management.
- Meditation: Meditation has been shown to be effective in improving the depression that’s part of bipolar disorder.
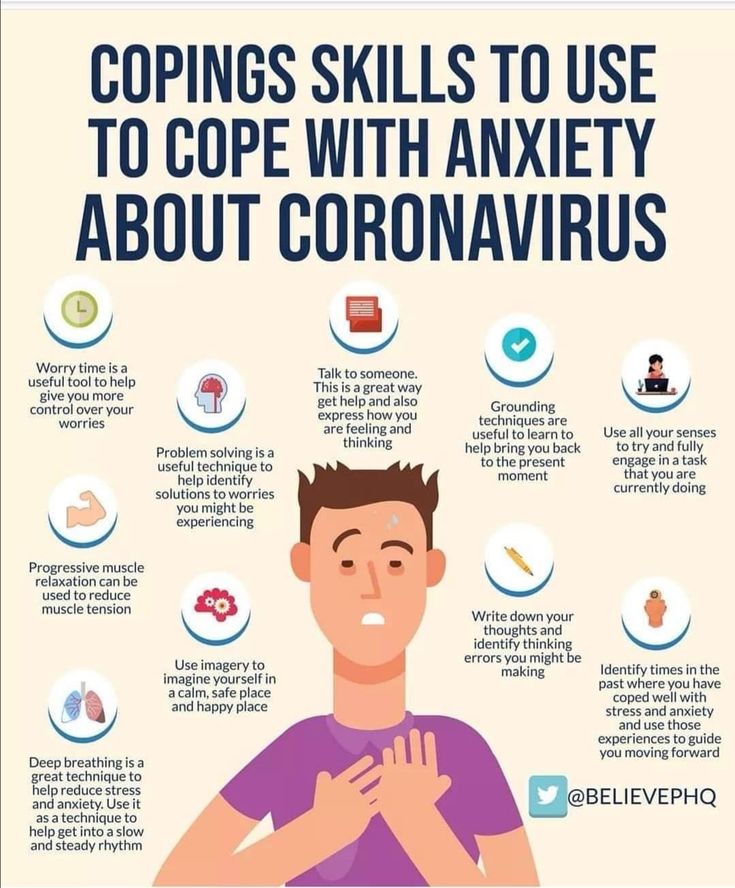
- Manage stress and maintain healthy relationships: Stress and anxiety can worsen mood symptoms in many people with bipolar disorder. It’s important to manage your stress in a healthy way and to try to eliminate stressors when you can. A big part of this is maintaining healthy relationships with friends and family who support you, and letting go of toxic relationships with people who add stress to your life.
Prevention
Can bipolar disorder be prevented?
Unfortunately, there’s no known way to prevent bipolar disorder because scientists don’t know its exact cause.
But it’s important to know the signs and symptoms of bipolar disorder and to seek early intervention.
Outlook / Prognosis
What is the outlook (prognosis) of bipolar disorder?
The prognosis for bipolar disorder is often poor unless it’s properly treated. Many people with bipolar disorder who receive appropriate treatment can live fulfilling and productive lives.
Bipolar disorder results in approximately nine years reduction in expected life span, and as many as1 in 5 people with bipolar disorder commit suicide. An estimated 60% of all people with bipolar disorder have drug or alcohol dependence.
This is why it’s essential to seek medical care and stay committed to treatment for bipolar disorder.
Regular and continued use of medication can help reduce episodes of mania and depression. By knowing how to recognize the symptoms and triggers of these episodes, there’s a better chance for effective treatment and finding coping methods that may prevent long periods of illness, extended hospital stays and suicide.
Living With
When should I see my healthcare provider about bipolar disorder?
If you’ve been diagnosed with bipolar disorder, you’ll need to see your healthcare team regularly throughout your life to make sure your treatment is working well for you. This team may include your:
- Primary healthcare provider.
- Psychiatrist.
- Psychologist or therapist.
- Neurologist.
When should I go to the emergency room (ER) for bipolar disorder?
If you’re experiencing any of these situations, it’s essential to call 911 or get to the nearest emergency room:
- Thoughts of death or suicide.
- Thoughts or plans of hurting yourself or others.
- Experiencing hallucinations and delusions.
- Symptoms of lithium toxicity (overdose), such as severe nausea and vomiting, severe hand tremors, confusion and vision changes.
A note from Cleveland Clinic
Bipolar disorder is a lifelong illness. But long-term, ongoing treatment, such as medication and talk therapy, can help manage your symptoms and enable you to live a healthy, purposeful life. It’s important to see your healthcare team regularly to monitor your treatment plan and symptoms. Know that your healthcare providers and loved ones are there to support you.
Mania of persecution - causes of occurrence, in what diseases it occurs, diagnosis and methods of treatment
I confirm More
- INVITRO
- Library
- Symptoms
- Persecution mania
Stroke
nine0016 19819 20 AugustIMPORTANT!
The information in this section should not be used for self-diagnosis or self-treatment. In case of pain or other exacerbation of the disease, only the attending physician should prescribe diagnostic tests. For diagnosis and proper treatment, you should contact your doctor.
For a correct assessment of the results of your analyzes in dynamics, it is preferable to do studies in the same laboratory, since different laboratories may use different research methods and units of measurement to perform the same analyzes. nine0003
Mania of persecution: causes of occurrence, in which diseases it occurs, diagnosis and methods of treatment.
Definition
Mania of persecution (delusion of persecution) is a mental disorder, which is expressed in a person's obsession about a threat to his own safety, about the presence of surveillance of him. No protection (isolation, relocation) saves such patients from delusional ideas.
Varieties of persecution mania
Psychiatric disorders that manifest as delusions can vary greatly depending on the underlying disorder. Often, by the type and structure of delusions, one can draw a conclusion about the cause of its occurrence. Delirium can be systematized , logical , well linked to the environment. In these cases, it can be identified only by the obsession of the state. Such nonsense accompanies the formation of a new "I" in schizophrenia. Sometimes delirium is fragmentary, unsystematized and can be supplemented with illusory perception, pseudo-hallucinations ("pseudo" - because the patient understands that they are unreal) of certain "enemies", "spies" or "murderers", which is characteristic of acute alcoholic psychosis. Delirium may be accompanied by sensory sensations . So, for example, with an obsessive idea of the penetration of harmful creatures into the body, the patient feels their physical passage through the skin, mouth. With a combination of diseases that affect the patient's psyche, n application of delusional ideas. This is the case, for example, with alcoholic psychosis that occurs in patients with schizophrenia.
In these cases, it can be identified only by the obsession of the state. Such nonsense accompanies the formation of a new "I" in schizophrenia. Sometimes delirium is fragmentary, unsystematized and can be supplemented with illusory perception, pseudo-hallucinations ("pseudo" - because the patient understands that they are unreal) of certain "enemies", "spies" or "murderers", which is characteristic of acute alcoholic psychosis. Delirium may be accompanied by sensory sensations . So, for example, with an obsessive idea of the penetration of harmful creatures into the body, the patient feels their physical passage through the skin, mouth. With a combination of diseases that affect the patient's psyche, n application of delusional ideas. This is the case, for example, with alcoholic psychosis that occurs in patients with schizophrenia.
Diseases in which delusions appear, or persecution mania
Organic vascular disease , which is accompanied by sclerotic changes, encephalopathy, stroke, quite often causes a change in the patient's personality. The clinical picture of such changes may be accompanied by the emergence of various psychoses and delusions. In addition, mental disorders are aggravated by age-related changes. Since the disorder is based on compensation and decompensation of brain nutrition, the clinical picture of the disease is periodic. nine0003
The clinical picture of such changes may be accompanied by the emergence of various psychoses and delusions. In addition, mental disorders are aggravated by age-related changes. Since the disorder is based on compensation and decompensation of brain nutrition, the clinical picture of the disease is periodic. nine0003
In the case of the habitual stereotype of life under standard loads, the patient copes with the situation, but with any deviations from the norm or the presentation of new requirements, psychosis may occur.
Along with depression, anxiety, they often coexist with delusional states: paranoia, auditory hallucinations. Psychoses are aggravated in the evening and at night and are accompanied by neurological disorders. Syndromes that develop against the background of vascular disorders may include manic, anxious, depressive components. It is possible to attach delusional ideas of persecution, especially if the patients' ability to analyze and abstract is sharply reduced. Therefore, the delirium of such persons is characterized by a rough structure and lack of logic. Most often they develop delusions of jealousy, poisoning and persecution mania. nine0003
Therefore, the delirium of such persons is characterized by a rough structure and lack of logic. Most often they develop delusions of jealousy, poisoning and persecution mania. nine0003
With schizophrenia persecutory delusions are considered the most common. As a rule, this condition is observed in paranoid schizophrenia. In the analysis of delirium, its logic and good linkage with external circumstances are noted. Often delusions are supplemented by sensory sensations, especially if there is an obsession with poisoning. Patients feel a suspicious taste, burning, smell, which, in their opinion, indicate poisoning. Thus, the picture of delirium is characterized by complexity, the inclusion of various emotional components in the plot - “hints”, “insults”, “ridicule”. This developed "decoration" of persecution mania distinguishes the delirium in schizophrenia from the intoxication lesion in alcoholism. Intelligence in patients with schizophrenia does not suffer, which is also a characteristic feature of the disease. nine0003
nine0003
Often, the development of persecution mania is preceded by the appearance of an unmotivated fear of people and social phobia.
Such fear makes you avoid others, be afraid of people walking behind.
Persecution mania can develop in bipolar affective disorder - a mental illness, the symptom of which is the alternation of depression and manic episodes. Moreover, in women, the disease often begins with periods of depression, in men - with the development of mania. The period of depression is accompanied by tearfulness, despondency, complaints of lack of strength. Such patients are characterized by a violation of concentration, memory, and a decrease in cognitive abilities. After a while, depression is replaced by a manic syndrome. Despondency turns into excessive gaiety, talkativeness. A person makes many plans that remain unrealized. Self-control of one's condition in these two phases of the disease changes significantly. During depression, patients tend to be aware that there is no reason for such a condition and seek medical help, while during a manic period, self-criticism decreases, and any advice to visit a doctor is perceived extremely negatively. Psychotic symptoms are a characteristic feature of bipolar disorder. During the depressive phase, delusions of guilt or hypochondriacal delusions (confidence in the violation of the state of one's body) may form. During the manic phase, inflated self-esteem leads to the formation of delusions of grandeur, and lack of criticality and suspicion develop into delusions of persecution. nine0003
During depression, patients tend to be aware that there is no reason for such a condition and seek medical help, while during a manic period, self-criticism decreases, and any advice to visit a doctor is perceived extremely negatively. Psychotic symptoms are a characteristic feature of bipolar disorder. During the depressive phase, delusions of guilt or hypochondriacal delusions (confidence in the violation of the state of one's body) may form. During the manic phase, inflated self-esteem leads to the formation of delusions of grandeur, and lack of criticality and suspicion develop into delusions of persecution. nine0003
Epilepsy that develops in children can also be accompanied by persecution mania. The clinical picture of the disease is characterized not only by the occurrence of repeated spontaneous seizures, but also by various neurological and mental personality changes. Patients with epilepsy are characterized, on the one hand, by a tendency to the viscosity of thinking, and on the other, impulsiveness.
Epileptics often show egocentrism, obsession with their needs, excessive attention to their health, cruelty and aggressiveness, and are in a depressed mood. nine0003
Mental disorders also include sensory, psychosensory and speech disorders, fears, sleep disturbance and disorientation. Among the delusional syndromes in children with epilepsy, there may be paranoid delirium with plots of persecution, excessive attention to one's health. Sometimes it can be mania, including hallucinations or ideas of fantastic events.
Delusions of persecution may be a manifestation of disease Bourneville-Pringle disease (tuberous sclerosis) - a genetically determined disease in which proliferation of the skin and blood vessels, damage to the nervous system and the growth of benign tumors in various organs are noted. Clinical signs of the disease appear either from birth or in the first year of life. nine0003
A characteristic skin symptom is hypomelanotic spots (discolored areas of the skin or a spot in the form of a leaf of a tree), which are observed in all patients in the second year of life.
Neurological symptoms include convulsive paroxysms. They cannot be controlled with anticonvulsant therapy and tend to be the main cause of disability. In the future, mental retardation and behavioral changes are detected.
The earlier epileptic seizures occur, the more severe mental retardation is. If the development of the nervous system is ahead of the pathological process, then various psychoses (fear, persecution mania, intrusive behavior) are more pronounced in patients. nine0003
Acute paranoid, which is manifested by delusions of persecution and hallucinations, occurs with alcohol and drug intoxication . In the subacute period of the disease, hallucinations are absent in patients, and the structure of mania becomes more ordered and logical. As a rule, against the background of isolation and suspiciousness, inexplicable attacks of fear and aggression occur in patients with alcoholism.
Which doctors to contact in case of persecution mania
It is very difficult to induce a patient who imagines surveillance or persecution to see a doctor.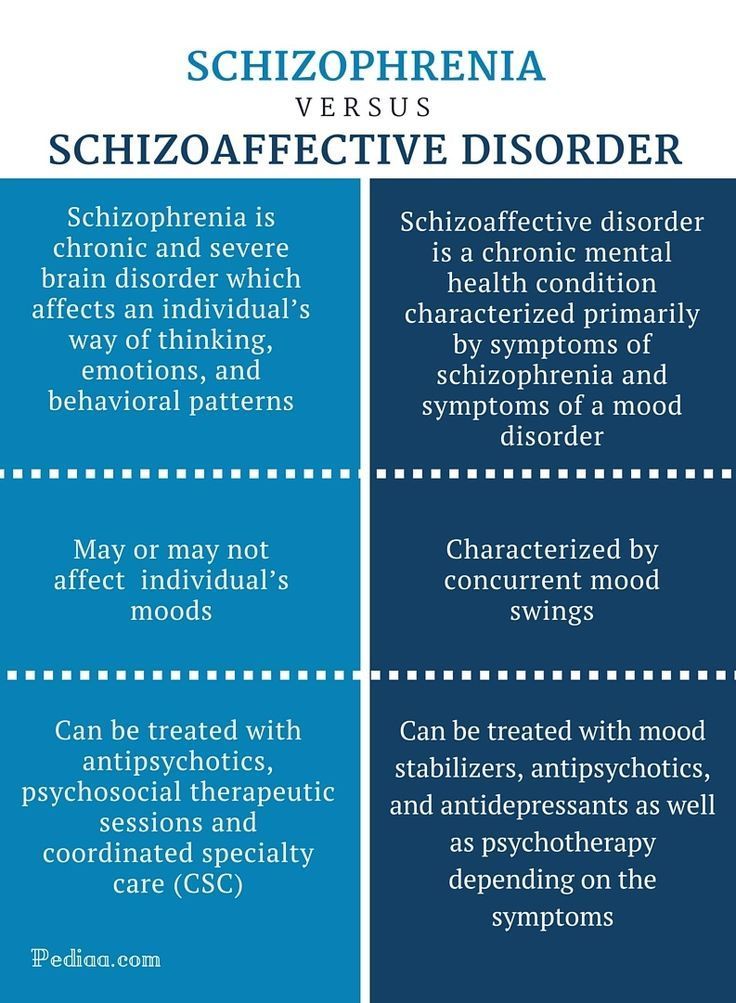 However, this must be done using a variety of reasons. If you can't overcome your fear of seeing a therapist or neurologist, you need to contact therapist or a pediatrician who can make a preliminary diagnosis. In some cases, consultation with a dermatologist and ophthalmologist may be required. nine0003
However, this must be done using a variety of reasons. If you can't overcome your fear of seeing a therapist or neurologist, you need to contact therapist or a pediatrician who can make a preliminary diagnosis. In some cases, consultation with a dermatologist and ophthalmologist may be required. nine0003
Diagnosis and examination of persecutory mania
Only a thorough examination of persons with persecutory obsession can help to make a correct diagnosis. The results of CT and MRI of the brain testify to vascular pathologies that can contribute to the development of delusions of persecution.
CT scan of the brain and skull
Scanning of the brain, skull and surrounding tissues, which allows diagnosing various pathologies. nine0003
RUB 4,590 Sign up
MRI of the brain
Safe and informative scanning of brain structures for the diagnosis of its pathologies.
RUB 5,140 Sign up
The presence of foci of excitation in epilepsy is confirmed by echoencephalography. In addition, x-rays of the skull, CT and MRI of the brain are performed. nine0021 Diagnosis of Bourneville-Pringle disease includes x-rays of the chest, skull, hands and feet, electroencephalography, CT, MRI, and urinalysis.
Electroencephalography (EEG)
EEG is a safe and painless method for studying the functional state of the brain.
RUB 2,840 Sign up
Skull x-ray
X-ray examination of the skull to detect violations of the structure and integrity of the bones of the skull of various nature.
RUB 2,090 Sign up
CT scan of the brain and skull
Scanning of the brain, skull and surrounding tissues, which allows diagnosing various pathologies.
RUB 4,590 Sign up nine0003
MRI of the brain
Safe and informative scanning of brain structures for diagnosing its pathologies.
RUB 5,140 Sign up
X-ray of the thoracic spine
X-ray examination to assess the condition and structural integrity of the vertebrae.
RUB 2,440 Sign up nine0003
X-ray of the skull
X-ray examination of the skull to detect violations of the structure and integrity of the bones of the skull of various nature.
RUB 2,090 Sign up
X-ray of the bones of the hand
X-ray examination of the bones of the hand is intended for the diagnosis of traumatic injuries, pathological changes, as well as the assessment of bone development . ..
..
RUB 2,340 Sign up
X-ray of the bones of the foot
X-ray examination of the foot in two projections allows diagnosing injuries and other pathological changes, including flat feet.
RUB 2,340 Sign up nine0003
General urinalysis (Urine analysis with sediment microscopy)
Method of determination Determination of physical and chemical parameters is carried out on an automatic analyzer using the "dry chemistry" method. Hardware microscope...
Up to 1 business day
Available with home visit
410 RUB nine0003
In garbage
Diagnosis of schizophrenia and alcoholic paranoid requires a careful medical history taking from the physician.
What to do in case of persecution mania
The main principle to be followed when detecting persecution mania is psychiatric alertness.
Communicating with such people should be as friendly as possible in order to prevent suicidal attempts and not provoke aggression. nine0003
Advice to visit a doctor can be justified by the presence of other diseases.
Treatment of persecutory mania
When treating patients with delusions of persecution, a systematic approach is necessary, since delusions are only one of the symptoms of an organic lesion of the central nervous system. Acute mental disorders require urgent medical attention, as they can provoke suicidal events. To stop the excitation, antipsychotics-antipsychotics are used. For patients with vascular lesions, the doctor may also prescribe drugs that improve blood circulation and brain nutrition. nine0003
Sources:
- The World Federation of Societies for Biological Psychiatry (WFSBP) Guidelines for the Biological Therapy of Schizophrenia / A.
 Hasan, P. Falkai, T. Wobrok et al. // Contemporary Therapy of Mental Disorders: Thematic issue. – № 2, 2014.
Hasan, P. Falkai, T. Wobrok et al. // Contemporary Therapy of Mental Disorders: Thematic issue. – № 2, 2014. - Studenikin V.M. Epilepsy in childhood // The attending physician. No. 5, 2015.
- Pringle-Bourneville disease: diagnostics at the intersection of disciplines / Kuklin I.A., Kenikfest Yu.V., Volkova N.V., Tolstaya A.I., Bochkarev Yu.M., Glazkova L.K., Rimar O. G., Krupina N.E. // Modern problems of dermatovenereology, immunology and medical cosmetology. No. 4, 2010. – P. 51–58. nine0006
IMPORTANT!
The information in this section should not be used for self-diagnosis or self-treatment. In case of pain or other exacerbation of the disease, only the attending physician should prescribe diagnostic tests. For diagnosis and proper treatment, you should contact your doctor.
For a correct assessment of the results of your analyzes in dynamics, it is preferable to do studies in the same laboratory, since different laboratories may use different research methods and units of measurement to perform the same analyzes. nine0003
nine0003
Recommendations
-
Cholesterol plaques
6824 November 18th
-
Hepatic colic
4509 09 November
- nine0002 Laryngeal edema
3958 07 November
Show more
Stroke
Diabetes mellitus
Facial numbness
Numbness of the face: causes of occurrence, in which diseases it occurs, diagnosis and methods of treatment.
More
Toxicosis of pregnancy
Pylorospasm
Pyloric stenosis
nine0002 Intestinal obstructionVomiting
Hypokalemia
Anemia
Shock
nine0002 SepsisPeritonitis
Acute heart failure
Thyrotoxicosis
Stroke
nine0002 Liver failureHyperventilation
Alkalosis
Alkalosis: causes of occurrence, in what diseases it occurs, diagnosis and methods of treatment.
More
Motion sickness
nine0002 WormsAngina
Mumps
Stroke
cerebral palsy
Epilepsy
Hyperthyroidism
Increased salivation
Increased salivation: causes, in which diseases it occurs, diagnosis and methods of treatment.
More
Rheumatism
nine0002 StrokeArthritis
Iron deficiency
Ulcer
Thrombocytosis
Thrombocytosis: causes of occurrence, in what diseases it occurs, diagnosis and methods of treatment.
More nine0003
Stroke
Angina
Parkinson's disease
Esophageal dyskinesia
Tumor
nine0002 DiverticulumDysphagia
Impairment of the act of swallowing, or dysphagia, is caused by the impossibility of passing the food bolus formed in the oral cavity through the oropharyngeal or pharyngeal-esophageal part into the stomach.