Living with ocpd husband
Does Your Partner Have OCPD?
Your partner is meticulous, careful, conscientious, and driven. On the outside, they are the best partner, employee, father, or mother. But behind closed doors, you are suffering from their rigidity, demanding nature, perfectionism, and the need to be so exact and meticulous about every inconsequential matter.
If your partner is obsessively preoccupied with perfection and order, is highly critical, or if you feel pressured by your partner's high standards and obsession with perfection, you may be with someone who is struggling with obsessive-compulsive personality disorder (OCPD).
What Is OCPD?
The American Psychiatric Association (APA, 2000) defines OCPD as "pervasive pattern of preoccupation with orderliness, perfectionism, and mental and interpersonal control, at the expense of flexibility, openness, and efficiency." Underneath OCPD is usually a fear of experiencing painful feelings and the helplessness of not being able to control anything.
However much they suffer, however, someone with OCPD may not see the need to change.
According to the International OCD Foundation (OCDF), men are twice as likely to have OCPD than women. About 1 in 100 people in the United States is estimated to have OCPD. It is estimated that 3 to 8 percent of the general population may suffer from OCPD. It is the most common personality disorder.
OCPD Is Not OCD
Obsessive-compulsive disorder (OCD) is an anxiety disorder. It is characterized by compulsive actions and a series of unwanted thoughts that feed their obsession. People with OCD are usually fully aware of the irrationality and oddness of their actions but cannot help themselves. The day-to-day anxiety is overwhelming to them and forces them to come up with ways to cope.
Obsessive-compulsive personality disorder, on the other hand, is a personality disorder. It pervasively affects every aspect of their lives—not just work but also family life and friendships, and the pattern usually starts from a relatively young age. It is problematic, persistent, and pervasive.
It is problematic, persistent, and pervasive.
OCPD and OCD are not the same, even they sometimes overlap. Symptoms that overlap may include paranoia, excessive caution, inability to compromise on set rules or routines, perfectionism and the inability to trust others.
In general, a person with OCD is usually much more aware of their dysfunctional patterns. They are aware of the irrationality embedded in their obsessive fear of germs, for example, but are not able to stop due to consuming anxiety. They may feel guilty about how those around them are affected. The person with OCPD, in contrast, may have little or no insight into the obsessive nature of their behaviours and their interpersonal consequences. In fact, they may have "secondary gains" (e.g. work performance, academic achievements, recognition from employers) from their perfectionism and thus see nothing wrong with their standards. Thus, even they too suffer deeply, and it usually takes people with OCPDs a much longer time to seek help.
Do You Recognize These Signs?
If your partner has OCPD, you may consistently find them challenging to live with and impossible to please. Their high standards and fixation on perfection take away playfulness and spontaneity in a romantic relationship. Here are some of the behaviors of a person with an obsessive-compulsive personality disorder.
- They are constantly making lists and doing things.
- Everything needs to be planned, which gives little possibility for spontaneous fun and joy.
- They spend an excessive amount of time trying to perfect every detail and lose sight of the need for leisure and relaxation.
- They suffer from workaholism, even sacrificing their own healths and their relationships.
- They are frugal about money or spending on necessary items.
- They have strict moral codes, and sometimes they judge you based on them.
- They have difficulties delegating, as they believe no one will be able to meet their standards.

- They rarely express their love, which makes you feel alone and emotionally deprived as a partner.
- They hardly compromise their stance of right or wrong.
- They have a hard time making friends or sustaining relationships because of their need to always be in control.
- They get extremely frustrated and angry when things do not go as expected.
- They are highly critical and judgemental of anyone and anything that doesn’t meet their standards.
- They are unable to be efficient because of their excessive focus on perfecting the process.
- They may suffer from bouts of depressive episodes and become disengaged in a relationship.
Understanding Your Loved One with OCPD
For someone with OCPD, rules, details, doing things, and keeping order help them feel safe. Their difficulties in relinquishing control may have stemmed from early trauma, in which they felt complete existential helplessness that has scarred them for life. It is not that they want to be this way, but they feel trapped in their predicament.
It is not that they want to be this way, but they feel trapped in their predicament.
OCPD is caused by both nature and nurture. Indeed, genetic factors and natural temperament play a significant role. Research has found that if an individual's close relative or family member has OCPD, there is a heightened risk of developing the same disorder.
At the same time, where there is childhood abuse, neglects, and emotional deprivation, a person’s risk of developing OCPD increases. The excessive need for control can result from being over-controlled or overprotected by anxious parents, or it can be a response to childhood neglect and parentification (role-reversal with the parents, needing to bring oneself up). All children want to please their parents by doing everything they can; when they see that being over-controlled satisfies the parent, rigidity in thinking and functioning sets in, and may persist as they mature into adults. Furthermore, a highly regulated family environment may inadvertently contribute to the development of OCPD. If emotional expressions and playfulness are not modeled for a child, they will have a hard time learning to be vulnerable and expressive.
If emotional expressions and playfulness are not modeled for a child, they will have a hard time learning to be vulnerable and expressive.
Their OCPD tendencies constitute a coping mechanism. Deep inside, they are fearful of helplessness and vulnerabilities that had once traumatized them, and they vow to never let themselves be in that position again.
Overcoming the Challenges
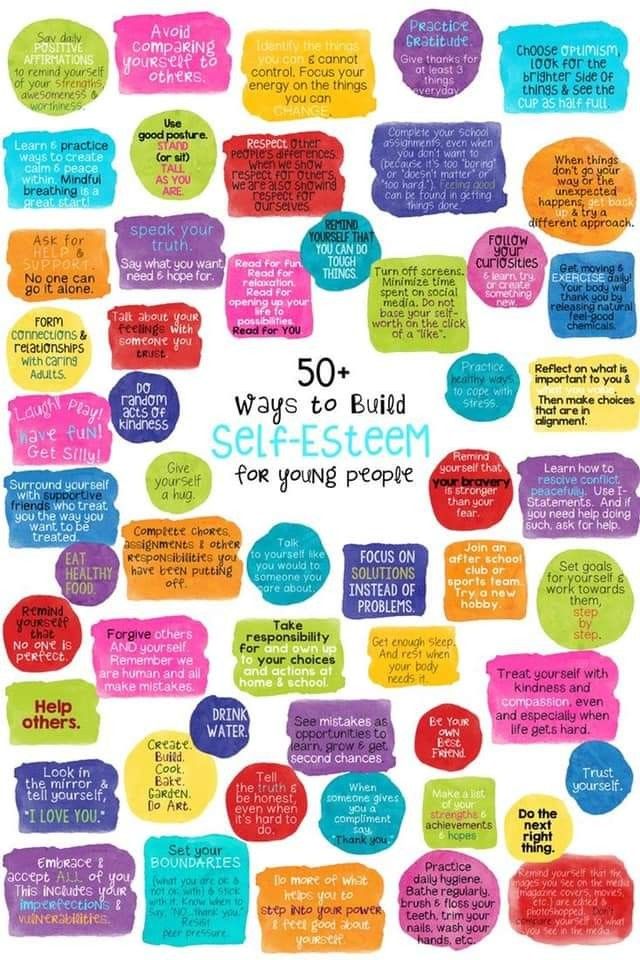
Being in a relationship with someone with OCPD may lead you to have eroded self-esteem, feeling mentally exhausted and frustrated. Every day, you have to deal with your partner's nit-picking, rigidity, and the standards they impose on you. Sadly, they are unaware of their behaviors and how they affect those around them.
Understanding the pain underneath their symptoms may help you have more empathy for their struggles, but that does not mean you allow yourself to be abused or chronically mistreated. It is easy to fall into the trap of feeling like you need to meet your partner’s impossible standards. In the process of doing so, you may lose self-confidence and become increasingly doubtful of yourself.
In the process of doing so, you may lose self-confidence and become increasingly doubtful of yourself.
Without communication, they may not have the capacity to see how their behaviors affect you and have little insight or motivation to change. Therefore, if appropriate, you may learn ways to communicate your needs and feelings in a no-confrontational, no-critical manner. Know that you deserve space in the relationship and to have your needs heard. Failing that, couples' or family therapy may be a valuable avenue to explore.
Both you and your partner deserve love, understanding, and having your emotional needs met. With insight and help, having a healthy and fulfilling relationship with someone with OCPD is possible.
How to Get Along with a Partner with OCPD (compulsive personality)
A partner with OCPD (obsessive compulsive personality disorder), can be really difficult to live with. They usually aren’t aware how extreme their rigidity has become and are often convinced that they’re right all the time. Their perfectionistic, controlling and workaholic tendencies can leave you feeling criticized, run-down, and abandoned.
Their perfectionistic, controlling and workaholic tendencies can leave you feeling criticized, run-down, and abandoned.
But with intention on their part and support from others, people with compulsive tendencies can change and become great partners—loyal, hard-working, dependable, and conscientious.
I’ll suggest seven steps to help you and your partner deal with the challenge. But first here are two key ideas to keep in mind as you consider all these steps:
- Appeal to the part of your partner that really wants to do the right thing. That’s at the core of the compulsive personality, however skewed it might have become. Their rules were originally meant to protect people, but they’ve put the cart before the horse. Once they recognize that nurturing their relationship is also the “right thing” to do, they can channel their energy into the project. This appeals to those with compulsive personality, and can help them move to the healthier end of the spectrum.
- Still, you’ll need to sort out what is and is not within your control.
 In very severe cases of OCPD there may be little you can do to help them change other than urge them to get professional help. And you should not tolerate abuse of any sort. But in all cases you’ll need to focus on what you can do to improve not only your relationship, but also your own life, rather than waiting for your partner to change. As we’ll see below, this can actually help your partner change.
In very severe cases of OCPD there may be little you can do to help them change other than urge them to get professional help. And you should not tolerate abuse of any sort. But in all cases you’ll need to focus on what you can do to improve not only your relationship, but also your own life, rather than waiting for your partner to change. As we’ll see below, this can actually help your partner change.
Contents
1. Foster Communication With Your Partner with OCPD
Compulsives don’t always communicate well. They’re often too busy to bother saying what they feel, and their behavior implies that they feel indifferent or critical. Worse, since they’ve spent much of their life “doing” rather than feeling, they may know little about what they feel. None of this means they don’t care; it means that they’re consumed with getting things done—ironically, maybe even getting things done for you.
None of this justifies bad behavior, but don’t assume that they don’t care or that they can read your mind. If you do, it will make matters worse. You can break this cycle by starting with curiosity: “Do you know how that makes me feel? Did you mean to make me feel bad?”
If you do, it will make matters worse. You can break this cycle by starting with curiosity: “Do you know how that makes me feel? Did you mean to make me feel bad?”
Strike while the iron is cold. If your partner is reactive or over-sensitive, it’s best not to try to have a discussion when they’re upset. Their rigidity and perfectionism probably get worse when they’re under pressure. Tell them you want to work it out with them when they feel calmer. Find a time when they’re less upset to engage. There will never be a perfect time, but if they’re overwhelmed with fear or anger, they may not be able to communicate well. If you can ask them about their intentions when they’re calm, you might be able to enter into a constructive dialogue.
2. See the Intentions Beneath the Surface
Extreme compulsiveness is the way some people who are naturally driven try to cope with their anxiety. When they’re upset their energy and good intentions get hijacked by their fear that they won’t meet expectations and that they will feel shame. Even when they look like they have it all together, underneath they’re probably feeling very vulnerable. It may be hard to imagine how disturbing this is for them. If you can keep this in mind, rather than taking their behavior personally, it will be easier to break the cycle and to find creative solutions to your disagreements.
Even when they look like they have it all together, underneath they’re probably feeling very vulnerable. It may be hard to imagine how disturbing this is for them. If you can keep this in mind, rather than taking their behavior personally, it will be easier to break the cycle and to find creative solutions to your disagreements.
3. Appreciate the Good
Perspective determines the quality of all relationships to some extent. You can choose whether to focus on your partner’s shortcomings or their strengths. If you can remember the good things they bring to the table, it will help you immensely.
It will also be helpful–to both of you–to tell your partner you appreciate it when they do something that feels good to you. If they do let go of control, spend time with you, say something nice, or slow down and listen, tell them that you noticed it and that you value it. That makes it more likely to happen again.
I find it helpful to understand people with OCPD as “driven,” which is far less pathologizing and can help them be more receptive to feedback.
4. Encourage Your Partner with OCPD to Get Help
People who have OCPD usually don’t think that they have a problem and resist getting help. It can be hard to get them to go to counselling or therapy, but here are some suggestions for framing it in a way that may appeal to them.
•Explain that the reason to get help is not a matter of their under-functioning, but of their habitual over-functioning. This is not a matter of weakness, but of excessive strength. They need someone professional to interrupt that pattern.
• Convey that you know they want to do the right thing.
• Recommend other articles on this blog to help them see their strengths and challenges so they might feel less criticized and more open to change.
• Help them understand the impact they have on others.
• Point out the impact their lifestyle has on their own physical and mental well-being. They may be oblivious to how they’re treating themselves, and that they could be happier than they are.
• Point out how their control actually gets in the way of their goals.
And now let’s focus a bit more on you.
5. Avoid the Division of Labor
Be wary of the division of labor in which one person is serious and demanding while the other is easy going and accepting. One brings responsibility, self-restraint and reason, the other brings joy, emotion and spontaneity. If you expect your partner to do all the organizing, providing, and limit-setting, don’t be surprised if they get very grumpy.
Imagine a spectrum from extreme compulsivity to extreme casualness. Imagine that the further one person in a couple goes toward either end, the other person automatically moves toward the opposite end. Now imagine that one person moves toward the center. The other will usually also move toward the center.
It’s also not fair to you to be cast into a limited role; your own psychological well-being is compromised if you’re supposed to stay in the less driven end of the spectrum. Are they living out your ambition for you? Is it possible that you feel uncomfortable with your own strength and anger and you have them express it for you? Or, on the other hand, are you expressing all the anger for them?
Are they living out your ambition for you? Is it possible that you feel uncomfortable with your own strength and anger and you have them express it for you? Or, on the other hand, are you expressing all the anger for them?
You might find it rewarding to allow yourself some ambition and pursue your own accomplishments. And you might find it empowering to own your own anger in a constructive way. If you can resist the division of labor, it can help the compulsive to move more toward the center of the spectrum.
Another danger is that you could take a victim role in response to their hostility, control, or over-working. Ask yourself honestly if there is anything you get out of the situation. Has it been safer or more comfortable to have someone else making all the plans and decisions and taking all the risk? It may have allowed you to avoid responsibility that you’d rather not have to deal with. Also, for some people, tolerating egregious or hostile behavior may feel like a virtue, when it doesn’t really help either of you.
Still, it will be important for you to value what you bring to the relationship: don’t forget the good things you do offer that are very different from what they offer. Their demeanor may lead you to underestimate what you mean to them.
6. Set Boundaries
But even after communicating, understanding and appreciating, it will still be important to set boundaries. If your partner has been diagnosed with OCPD, that should not be used as an excuse for offensive or oppressive behavior. If they want to be perfectionistic, workaholic or controlling that’s their choice, but they should not impose their standards on you. Seek compromise that takes into account what’s hard for both of you. Try not to give in to unrealistic demands.
Don’t let their condition become the focus of your life. It could become a distraction from your own challenges and happiness. If you find yourself talking and thinking about them all the time, set an intention to focus on what is within your control: change either the situation or your attitude toward it.
7. Create Your Own Support System
Having friends, a therapist, or a support group is particularly important if the compulsive person in your life is demanding. A support network can help you to keep track of what’s reasonable. Ask your friends for true reality checks. If you simply want to be validated, it won’t be much help. But asking trusted friends for honest feedback about what your partner can reasonably expect of you can help keep you grounded.
* * *
Being close to someone who is compulsive has its challenges and rewards. Appealing to their deeper, positive inclinations, and keeping the focus on what is within your control, may help you enjoy more of the rewards.
________________
For much more information on OCPD, check out my new book on Amazon or Barnes and Noble. If you think it would be helpful to others, please leave a review.
And, if you’d like to get all of my posts when they come out, click that subscribe button below or on the right side.
symptoms, how to get rid of and treat
Olya Selivanova
struggles with obsessive-compulsive disorder
Author profile
Since childhood, I have suffered from obsessive thoughts.
When I was nine years old, I was reading a book, when suddenly the thought occurred to me: “If you don’t finish reading today, your mother will die.” The thought frightened me, I put down the book and cried, but I had to return to reading so that my mother would not die.
From that moment on, the frightening thoughts were different. I could suddenly change the route, because the thought came to my mind: “It is not safe to go further. Get around." There were thoughts to harm loved ones: push, hit, pour over. At such moments, I thought that an evil force had entered into me, and I began to count to myself, imagined how the numbers increased in order in size and knocked bad thoughts out of my head. nine0003
By the time I was twelve, it all came to naught, and as a teenager, I decided that it was just childish oddities. But seven years later, the obsessive thoughts returned, and the doctor at the neuropsychiatric dispensary diagnosed me with Obsessive-Compulsive Disorder. I'll tell you how I was treated and how I live now.
But seven years later, the obsessive thoughts returned, and the doctor at the neuropsychiatric dispensary diagnosed me with Obsessive-Compulsive Disorder. I'll tell you how I was treated and how I live now.
Go see a doctor
Our articles are written with love for evidence-based medicine. We refer to authoritative sources and go to doctors with a good reputation for comments. But remember: the responsibility for your health lies with you and your doctor. We don't write prescriptions, we make recommendations. Relying on our point of view or not is up to you. nine0003
What is obsessive-compulsive disorder
Obsessive-compulsive disorder is a mental illness in which a person has obsessive thoughts and compulsive actions.
What is Obsessive-Compulsive Disorder - Mayo Clinic
Obsessive thoughts - obsessions - usually revolve around certain topics: fear of harming yourself and others, fear of germs and toxic substances, the need to organize everything. They appear suddenly or are provoked by external circumstances, such as a sharp object or the word "last". nine0003
They appear suddenly or are provoked by external circumstances, such as a sharp object or the word "last". nine0003
Intrusive thoughts cannot be ignored, they cause anxiety or disgust. In response to them, a person has compulsions - a strong desire to perform certain actions that, according to his feelings, will get rid of such thoughts. Compulsions are difficult to resist: the anxiety will grow until the person gives up.
For example, the obsessive thought that a person will become infected after touching a doorknob will provoke compulsive actions - repeated washing of hands, sometimes for several hours in a row. nine0003
/shizofreniya/
How much does it cost to support a relative with a mental disorder
I try not to touch doorknobs in public places and always make sure the door is closed. Do I have OCD?
Sergey Divisenko
psychotherapist
If a person's condition does not interfere with himself or others, then everything is in order, if it interferes, a disorder can be suspected. In the case of checking the door, one can say that checking if the door is closed once is not a problem, rechecking the door several times in a row and doing it systematically is already a problem. nine0003
In the case of checking the door, one can say that checking if the door is closed once is not a problem, rechecking the door several times in a row and doing it systematically is already a problem. nine0003
To understand whether or not there is OCD, the doctor pays attention to how often the patient has obsessive thoughts and compulsive actions and how they affect his life. If symptoms occur more frequently in two weeks than in seven days and interfere with daily activities, it is probably OCD.
In this case, the symptoms should have the following characteristics:
- The person should evaluate them as his own thoughts and desires.
- There must be at least one thought or action that the person unsuccessfully resists. nine0050
- The thought of a person performing a compulsive action should not in itself be pleasurable. The fact that an action will help reduce anxiety is not considered pleasant in this sense.
- Thoughts or actions must be repeated.

How obsessive-compulsive disorder is treated
OCD is considered a lifelong disorder, but with treatment it is possible to achieve remission: to get rid of obsessive thoughts and compulsive actions for a long time or to reduce their number. nine0003
Medical treatment. The main drugs for the treatment of OCD are antidepressants of the SSRI group. They increase serotonin levels in the brain, making OCD symptoms less likely to occur.
Treatment options for OCD - NHS
Depending on the course of the disease and symptoms, along with antidepressants, the doctor may prescribe other drugs: tranquilizers, neuroleptics or mood stabilizers.
Cognitive behavioral therapy. This is a type of psychotherapy during which a person learns to control their emotional response to intrusive thoughts. As a result of therapy, obsessive thoughts cease to cause anxiety and compulsive actions. nine0003
Cognitive Behavioral Therapy - NHS
Order of the Ministry of Health of the Russian Federation of September 16, 2003 No. 438 "On Psychotherapeutic Care"
438 "On Psychotherapeutic Care"
OCD in Russia is treated by psychiatrists, psychotherapists and psychologists. Psychiatrists prescribe prescription drugs. Psychotherapists and psychologists conduct psychotherapy sessions.
How I was diagnosed
At the age of 19, the development of the disease took a new turn. I was washing the kitchen knife and I had an obsessive thought that I was losing control and could cut myself and the guy who was nearby at that moment. So I began to avoid sharp objects, there was an irresistible desire to hide or throw them away. nine0003
Obsessive thoughts revolved around the topic of death: drinking nail polish remover, bleach, vinegar, throwing yourself under a vehicle or jumping out of a window. Because of this, I removed all dangerous liquids from the house and stayed away from open windows, highways and train station platforms. I didn’t sleep well at night, suffered from anxiety, considered myself crazy and dangerous, and began to move away from everyone.
I also doubted everything. Even if I just performed an action, it seemed to me that it was not completed. I opened the door to make sure that it had been closed before, closed it again, pulled the handle, asked those around me if the door was exactly closed. I could wake up at night and see if the stove was turned on, although before going to bed I went up to it and stared without blinking - so that it would crash into my memory that it was definitely turned off. My young man, seeing all this, insisted that we try to see a psychologist. nine0003
In Irkutsk, where I live, psychiatric care can be obtained free of charge at the regional psycho-neurological dispensary. I turned to the psychotherapeutic department of the dispensary for a consultation with a psychologist. At the reception, they brought me a card and said that there was no appointment with a psychologist for the next few days, but I could get to a psychiatrist: there are fewer people who want to see him.
/spravka/
How to get a certificate from the PND
At the appointment with the psychiatrist, I told about what was happening to me. The doctor was not surprised and said that it was an obsessive-compulsive disorder. It was the first time I heard my diagnosis, but I didn't believe it. On the Internet, I came across information that OCD is only pedantry, handwashing, fear of germs and perfectionism, and not the creepy things that come to my mind. The psychiatrist said that OCD was treated with antidepressants and offered to write a prescription, but I refused treatment because I thought they were serious drugs that would do more harm than help. nine0003
The doctor was not surprised and said that it was an obsessive-compulsive disorder. It was the first time I heard my diagnosis, but I didn't believe it. On the Internet, I came across information that OCD is only pedantry, handwashing, fear of germs and perfectionism, and not the creepy things that come to my mind. The psychiatrist said that OCD was treated with antidepressants and offered to write a prescription, but I refused treatment because I thought they were serious drugs that would do more harm than help. nine0003
How a visit to a neuropsychiatric dispensary with OCD will affect later life
Sergey Divisenko
psychotherapist
The patient could move freely, drive a car, use weapons and work.
With an OCD diagnosis, you can still work in any job, there are no legal barriers to this. With regard to cars and weapons, the situation has changed. In 2014 and 2015, government decrees appeared, according to which OCD became a contraindication for driving and owning weapons. nine0003
nine0003
However, from a psychiatrist's point of view, a person diagnosed with OCD can drive a car and use a weapon. Doctors of the psycho-neurological dispensary still give a certificate about this, but they do it through a medical commission.
Treatment
First hospitalizationMy condition worsened, I tried to ignore obsessive thoughts. But the more I resisted them, the stronger they became. In addition, anger, irritability and constant fatigue appeared. nine0003
With new symptoms, I decided to see an endocrinologist, because I heard that this happens with problems with the thyroid gland. According to the results of ultrasound and hormone tests, the thyroid gland was in order. Then I made an appointment with a neurologist, but he also said that this was not his profile. Both doctors suggested that my constant fatigue, anger and irritability were symptoms of depression and advised me to seek psychiatric help.
Symptoms of clinical depression - NHS
I researched information about depression and realized that antidepressants could help, all I had to do was get a prescription. I came to the psychotherapeutic department again, but there was already another psychiatrist there. Since my condition worsened, instead of a prescription, he wrote out a referral for hospitalization in a day hospital. I had prejudices about a psychiatric hospital, so I did not want to visit the hospital. But there was no strength to argue with the psychiatrist.
I came to the psychotherapeutic department again, but there was already another psychiatrist there. Since my condition worsened, instead of a prescription, he wrote out a referral for hospitalization in a day hospital. I had prejudices about a psychiatric hospital, so I did not want to visit the hospital. But there was no strength to argue with the psychiatrist.
The next day I was already in the hospital. During the registration, the psychiatrist on duty asked what I was complaining about, measured the pressure and examined whether there were injuries on the body. It turned out to be difficult for me to talk about the symptoms: there was a feeling that they would not believe me, or vice versa, they would believe me so much that they would put me in a round-the-clock hospital. But everything was fine, the psychiatrist wrote down the data on the card, gave it to the orderly, and together with him sent me to the head.
The manager looked at the card, confirmed the diagnosis of OCD and depression, and prescribed treatment: an antidepressant, an antipsychotic, a mood stabilizer, tranquilizer tablets, and injections of B vitamins.
/guide/vitamins/
Vitamins: what foods contain and how to take supplements
The routine in the hospital was as follows: I arrived at eight in the morning, had breakfast and took the prescribed pills, took injections, dined and went home. Tablets were issued immediately for one day, but they could also be issued for two days, for example, before the weekend. Once after the injection, I went to an appointment with a clinical psychologist, he gave various tests and questionnaires that tested logic and intelligence.
It was possible to move freely and receive visitors in the day hospital. The only limitation that distinguished the hospital from a regular hospital was that there were no forks and knives in the dining room. Part of the drugs used to treat psychiatric diseases cause drowsiness. Therefore, in the hospital there are wards where you can sleep. For example, after drip
Part of the drugs used to treat psychiatric diseases cause drowsiness. Therefore, in the hospital there are wards where you can sleep. For example, after drip About three times a week I went to see a psychiatrist in the same hospital. I told her about my condition and asked questions. I thought that as soon as I start taking medication, my mood will rise and my anxiety will go away. But this did not happen, so it seemed that everything was in vain and the treatment had to be abandoned. The psychiatrist explained to me that not all drugs begin to act instantly, she assured me that we were on the right track and we had to wait. These conversations made it easier. In my case, antidepressants began to work only on the third month of admission, when I no longer visited the day hospital. nine0003
Treatment at the day hospital lasted a month. All medications, medical consultations and meals were free. I spent money only on the road to the hospital and back - 600 R by public transport for the whole time.
/bye-depression/
“It reminded me of a strict regime sanatorium”: how much I spent on treating depression
After treatment, the symptoms of depression remained, but obsessive thoughts began to bother me less often: I stopped being afraid of open windows and was able to ride the escalator. Treatment had to be continued on an outpatient basis. Before I was discharged, the psychiatrist said that she would transfer my data to the psychiatric department. Now I will need to come to the local psychiatrist for prescriptions for medicines, and turn to him if the condition worsens or questions arise. nine0003 During the treatment in the hospital, I doubted everything. Even in being sick. Not only the psychiatrist, but also relatives helped to cope. They noticed the changes, but my young man did not let me stop the treatment
Treatment
Visiting a local psychiatrist After I was discharged from the hospital, I came to the registration office of the psychiatric department with a passport and I was immediately sent to the district police officer. The doctor did not change the treatment and wrote out a prescription for the same medicines that were given in the day hospital. In the future, a referral to the district police officer was also not required. I just came to the appointment when I needed to update the prescription. nine0003
The doctor did not change the treatment and wrote out a prescription for the same medicines that were given in the day hospital. In the future, a referral to the district police officer was also not required. I just came to the appointment when I needed to update the prescription. nine0003
Government Decree of July 30, 1994 No. 890 with a list of categories of beneficiaries who are entitled to free medicines
District psychiatrists were different: some were polite, some were rude and rude. Using the brute force method, I found two normal specialists - when I made an appointment at the reception, I began to ask to be directed to them. Usually the registrar complied with my request.
Spent in six months of outpatient treatment — 8895 Р
| Preparation | Spending |
|---|---|
| Antidepressants | 5988 R |
| Normotimics | 2384 P |
| Antipsychotics | 419 P |
| Tranquilizers | 104 Р |
Antidepressants
5988 R
Normotimics
2384 R
neuroleptics
419 R
Transquilizers
104 R
Free medicines for the treatment of OCD are provided to certain privileged categories of people. I’m not a beneficiary, so I bought everything with my own money. Pharmacies don’t require a passport, but they put the date of issue of the medicine on the back and don’t sell more than prescribed by prescription. For example, according to a prescription for three months, I was given only three packs of an antidepressant. When I wanted to buy one more to have a supply, the pharmacist refused
I’m not a beneficiary, so I bought everything with my own money. Pharmacies don’t require a passport, but they put the date of issue of the medicine on the back and don’t sell more than prescribed by prescription. For example, according to a prescription for three months, I was given only three packs of an antidepressant. When I wanted to buy one more to have a supply, the pharmacist refused Treatment
Second hospitalization and psychotherapyAfter six months of outpatient treatment, the district psychiatrist recommended to be treated again in the hospital. Antidepressants helped: my mood improved, I got energy and I wanted to live, but I felt a side effect from antipsychotics. I was terribly sleepy, my handwriting changed, it was difficult to write in class and generally follow the train of thought of the teacher. In addition, there were more intrusive thoughts. nine0003
In the day hospital, I was treated by the same psychiatrist as the first time. She adjusted the drug treatment so that I was not bothered by intrusive thoughts. She also said that a psychotherapist had appeared in the hospital and referred me to her for a consultation.
She also said that a psychotherapist had appeared in the hospital and referred me to her for a consultation.
Unlike the psychiatrist's consultations during the first hospitalization, we did not discuss drugs and their effects with the psychotherapist. We talked about what is happening to me and what other methods can be used to combat this, in addition to drugs. At the first appointment, I briefly talked about my lifestyle, obsessive thoughts, compulsive actions, and how I tried to resist them even before the treatment. Then the doctor explained to me what obsessive-compulsive disorder is and how it manifests itself, why my struggle only worsened the condition and led to depression. nine0003
/psychotherapy-search/
How to choose a psychotherapist
We agreed that I would try to keep the number of compulsive acts to a minimum, and I would cope with anxiety from intrusive thoughts with the help of techniques.
Speak key phrases. Thoughts in themselves mean nothing, they can come to mind automatically. We agreed that when I had an obsessive thought, I would simply tell myself that it was a manifestation of OCD. Here are the two phrases that I used: “This is just my thought that…”, “I know that this thought is a manifestation of OCD…” So gradually I stopped identifying myself with my thoughts and realized that thinking about the bad is does not mean to be a bad person. nine0003
Thoughts in themselves mean nothing, they can come to mind automatically. We agreed that when I had an obsessive thought, I would simply tell myself that it was a manifestation of OCD. Here are the two phrases that I used: “This is just my thought that…”, “I know that this thought is a manifestation of OCD…” So gradually I stopped identifying myself with my thoughts and realized that thinking about the bad is does not mean to be a bad person. nine0003
Separately, we discussed the issue of the materialization of thoughts. When terrible things are spinning in your head, and you hear from everywhere that thoughts are material, you get very worried. We discussed the fact that thoughts are intangible and you can’t invite trouble with them. This made it easier and the degree of emotions decreased.
Observe how the body reacts to anxiety. Every time I had anxiety from obsessive thoughts, I did not run away from it, but watched my body. I was shaking, my heartbeat increased, my breathing quickened, but I continued to live it. The psychotherapist said that I would not die from this. Yes, it is unpleasant and scary, but when you live emotions, you gradually learn to cope with them. nine0003
The psychotherapist said that I would not die from this. Yes, it is unpleasant and scary, but when you live emotions, you gradually learn to cope with them. nine0003
Keep a diary. In the course of the sessions, I became convinced that I cannot control the thoughts themselves - it is impossible, but I can control the reaction to them. So I started keeping a diary.
/psychotherapy/
How psychotherapy works
It was necessary to take notes according to the formula: A - situation, B - my thoughts, C - my emotions. Using such records, it is easier to track the thoughts that cause negative emotions and work them out. For example, when I could not fall asleep for a long time, I began to think that something was going wrong, and this caused anxiety. Then I wrote down the whole situation in a diary and instead of negative thoughts I formulated new ones: "My sleep does not depend on my will, and this is normal." It helped to get rid of anxiety, stop trying to sleep and go about your business. About half an hour later I went to bed and fell asleep peacefully. nine0003 I filled out the diary for a week, and then the psychotherapist and I analyzed the notes
About half an hour later I went to bed and fell asleep peacefully. nine0003 I filled out the diary for a week, and then the psychotherapist and I analyzed the notes
| I also kept a mood diary. Before treatment, there was no point in monitoring the mood: it always turned out to be bad or indifferent | On antidepressants, I began to make entries in a diary every day and could track what affects my mood |
I also kept a mood diary. Before treatment, there was no point in monitoring the mood: it always turned out to be bad or indifferent. On antidepressants, I began to make entries in a diary every day and could track what affects my mood
In the day hospital, I was treated for a month and a half, during which time I had only five sessions with a psychotherapist. All sessions, meals and drugs, as in the first hospitalization, were free. The only thing I had to spend money on was the road to the hospital and back, as well as the original antidepressant instead of the analogue provided in the dispensary. The doctor recommended the original, it suited me better. nine0003
All sessions, meals and drugs, as in the first hospitalization, were free. The only thing I had to spend money on was the road to the hospital and back, as well as the original antidepressant instead of the analogue provided in the dispensary. The doctor recommended the original, it suited me better. nine0003
3202 Р
spent on medicines and transport for a month and a half of treatment in the hospital
When I was discharged, the doctor told me that I was in a stable condition, the treatment helped me. I myself felt it: the mood was consistently good, and I quickly coped with obsessive thoughts. I was canceled all the drugs, except for antidepressants, then I had to continue taking them, be observed by the district psychiatrist and monitor my condition.
Spent one and a half months of treatment in a hospital — 3202 Р
| Expenditures | Spending |
|---|---|
| Antidepressants | 2422 P |
| Transport | 780 Р |
Antidepressants
2422 R
Transport
780 R
How do I feel after treatment
I stopped taking antidepressants a year and a month after discharge I spent another 14,640 R on them. Sometimes I have obsessive thoughts and compulsive actions, but I do not scold myself for this. I know that if I get upset, the symptoms will become more frequent. The psychiatrist warned me that OCD symptoms may appear periodically, but this is normal. nine0003
Sometimes I have obsessive thoughts and compulsive actions, but I do not scold myself for this. I know that if I get upset, the symptoms will become more frequent. The psychiatrist warned me that OCD symptoms may appear periodically, but this is normal. nine0003
14,640 Р
spent on antidepressants for a year and one month
Coronavirus last spring was a test of strength for me. The condition worsened, compulsive actions resumed, I stopped leaving the house, I began to choke on the street, obsessive thoughts about death appeared. But I managed it on my own with the help of techniques taught to me by the therapist. I kept in my head the idea that if it worked then, it will work now.
Before treatment, it was difficult for me to talk about my disorder. And now I openly talk about it and I can even joke about random manifestations of OCD. Almost everyone in my circle knows that I was being treated for OCD and depression. They help me notice compulsive actions and stop in time, treat me with understanding when I ask obvious things just in case - for example, did I close the door.
How often do people with OCD need to take drugs for life
Sergey Divisenko
psychotherapist
With the help of treatment, you can achieve remission - for a long time to get rid of the symptoms of OCD or reduce their number. Remission can occur both against the background of taking medications, and without them, against the background of psychotherapy.
Approximately 80% of patients with OCD stop taking medication sooner or later.
How much does OCD treatment cost?
In total, I treated OCD for one year and nine months. Of these, she was treated in a day hospital for two and a half months, and for a year and seven months - on an outpatient basis. nine0003
In the hospital, I only spent money on transport to and from the dispensary. Even during the second hospitalization, on the recommendation of the doctor, she bought antidepressants at the pharmacy and took them instead of those given in the hospital. The rest of the drugs, consultations and meals were free.
6 useful services for finding a psychotherapist
Most of the expenses are medicines during outpatient treatment.
Spent on OCD treatment for 1 year and 9 months — 27,337 R
| Expenditures | Spending |
|---|---|
| Antidepressants | 23 050 Р |
| Normotimics | 2384 P |
| Antipsychotics | 419 P |
| Tranquilizers | 104 Р |
| Transport during hospitalization | 1380 Р |
Save
- Obsessive Compulsive Disorder or OCD is a mental illness in which a person experiences obsessive thoughts and compulsive actions.
- OCD is considered a lifelong disorder, but remission can be achieved with the help of psychotherapy and drugs.
- OCD is treated in Russia by psychiatrists, psychotherapists and psychologists. Psychiatrists prescribe prescription drugs.
 Psychotherapists and psychologists conduct psychotherapy sessions.
Psychotherapists and psychologists conduct psychotherapy sessions. - A visit to a neuropsychiatric dispensary will not prevent people with OCD from moving freely, driving a car, using weapons, or getting a job. nine0050
- Patients with OCD can receive care free of charge in state neuropsychiatric dispensaries or at their own expense in private clinics.
Did you also have an illness that affected your lifestyle or attitude? Share your story.
Tell
The cause of OCD is unhealthy relationships in the family
76,434
Know yourself A man among peopleHealth and beauty diagnosis. The baton was picked up by Leonardo DiCaprio in The Aviator. Remember the scene in the toilet when the main character couldn't get out for fear of touching the door handle? Why is there so much focus on OCD now? Have there been more cases? nine0003
“Today there is a growing understanding and acceptance of the problems of mental disorders in society. For example, about panic and depression now we can talk quite freely. And even 10 years ago, people were afraid of the reaction of others, - explains clinical psychologist Yakov Kochetkov. - At the same time, OCD is a less clear story even for specialists, which is still in the shadows. It is more difficult for people to talk about it, they experience burning shame. At the same time, OCD is less common than depression: from 1 to 2% of people suffer from its clinical forms. Therefore, we can calculate that in our country at least 3 million people suffer consistently from obsessive-compulsive disorder and quite rarely receive help.” nine0003
For example, about panic and depression now we can talk quite freely. And even 10 years ago, people were afraid of the reaction of others, - explains clinical psychologist Yakov Kochetkov. - At the same time, OCD is a less clear story even for specialists, which is still in the shadows. It is more difficult for people to talk about it, they experience burning shame. At the same time, OCD is less common than depression: from 1 to 2% of people suffer from its clinical forms. Therefore, we can calculate that in our country at least 3 million people suffer consistently from obsessive-compulsive disorder and quite rarely receive help.” nine0003
Contrasting obsession
In the philistine mind, in movies, in magazines, the disorder is presented through the simplest, most understandable things - the fear of contamination when people wash their hands many times, or the desire to arrange things symmetrically. But this is only part of the possible options. Approximately half of people with OCD actually fear pollution. As far as symmetry is concerned, this is a rather small part.
As far as symmetry is concerned, this is a rather small part.
Two other types of OCD sufferers are often overlooked. The first one is more or less known: these are people who constantly check whether the gas is turned off, whether the lights are off, whether the door is closed correctly. We all do it sometimes, but it's a matter of balance, the balance between healthy security controls and an obsessive state. nine0003
“If you test your gas in such a way that you don't believe your own test, then it's worth considering. People with OCD may experience the reality of their actions dozens or hundreds of times. They cannot leave the house for hours. They are late for work, disrupt meetings. Communications are broken. Often their social life is complicated.”
The main problem is that people try to fight obsessive thoughts, but the more they fight them, the worse they get. Obsessive thoughts exist in contrast with the true beliefs of a person, they come to the head "by themselves", and they do not like the "owner" of the head.We all have strange thoughts from time to time, but we do not pay attention to them and send them to "spam". But people with OCD give too much importance to their thoughts. nine0003
“An ordinary young mother, only very anxious and responsible, suddenly watched a TV show about a woman who killed her children. And then she asks herself, am I not like that? She begins to have images in which her child is bloody, murdered. She begins to be frightened of her thoughts, tries to suppress them, to do something so that they do not climb into her head. But the more she does it, the more they come. And gradually the situation comes to the fact that the woman winds herself up and develops a plan on how not to stay near the child, hides knives and everything that can “kill” him, asks others to watch her, because she considers herself abnormal. It is important to understand that such a woman will never harm her child and her "danger" exists only in her head. nine0003
A believer comes to church and finds blasphemous thoughts in his head.
He tries to drive them away, but fails. “Or a person suddenly begins to think that he is gay, while it is very important for him to be a person of traditional orientation,” explains Yakov Kochetkov. “And he constantly checks himself to see if he is attracted to members of the same sex.” The main problem is that people try to fight intrusive thoughts, but the more they fight them, the worse they get. nine0003
Message from the family
But why does an ordinary person suddenly have such peculiarities? “There is evolutionary conditioning. We have genes for repetition and cleanliness. They were useful to our ancestors. If you are clean and clean up after yourself, do not live near excrement, then you are much less likely to get sick with something. Our ancestors checked everything related to safety a lot: whether the entrance to the cave was closed, whether they covered their tracks well. Scientists say that genetic predisposition explains 30% of the appearance of OCD in humans, and 70% is the influence of environmental conditions.
nine0003
What are these conditions that make a person very anxious and arouse excessive obsession in him? Education plays a huge role. In some families, the fear of infection is instilled from childhood, which means that increased hygiene is necessary. In many families, the message is broadcast: the world is dangerous and unpredictable - check everything many times.
Relationship patterns in the family also have an influence. “We have a very common symbiotic relationship between mother and children, especially sons. And often this also contributes to obsessive-compulsive disorder, says Yakov Kochetkov. Every second call to our center is not from patients, but from their parents, who say that their “boy is sick”. And when we ask how old the boy is, it turns out that he is 20 and 30 and 40.” nine0003
It is very difficult for a person in a symbiotic relationship to trust himself, to be responsible for his actions and even thoughts. Parents patronize with the best of intentions - they just do not know how to behave properly: for example, to allow a teenager to gradually separate.
Understand that he needs a separate room, his own secrets, his own thoughts - good or bad. In symbiotic families, parents usually actively intervene in the treatment process. And psychologists have to conduct therapy not only with patients, but also with parents, so that gradually they give their grown children more independence. nine0003
Features of national thinking
Ordinary people control their actions. A person with OCD also tries to control their thoughts. For him, thought is identical to action. We very often get angry on the road when someone cuts us off. Who in their hearts did not wish all the misfortunes on the head of the offender? The OCD patient believes that his words will materialize, and he is a bad person, which means, as a result, shame and guilt, and again torment and self-abasement.
The prevalence of this disorder also depends on cultural characteristics and traditions. “OCD responds very subtly to the cultural situation. For example, now people have begun to passionately rush into pseudo-religiousness, and there are much more cases associated with the fear of “bad”, blasphemous thoughts.
A man comes and says that he is a believer. We begin to understand: it turns out that he does not quite correctly interpret the basic religious postulates. “God will punish me because I have bad thoughts in my head. I have to get rid of them." But this is more about superstition than real religion, the expert believes. nine0003
Self-help methods are unlikely to help here - this is too complex a disorder“I recently gave a talk in Germany on the cultural characteristics of Russian OCD. We have a very widespread so-called magical thinking - more than in Western Europe, - says Yakov Kochetkov, - and it is strongly supported by the media. Faith flourishes in the omnipotence of otherworldly forces, in the fact that it is possible to act with energy on some objects. If I burn a neighbor's hair, then the neighbor will burn or die. And this leads to the fact that in Russia a person with OCD finds support for his fear with thoughts of harming someone.
If I thought now that my mother has cancer, then she can really get sick, because thoughts are material. I have to do many, many rituals to prevent this, present a bright positive image or knock on wood. How can OCD not arise here? Perhaps this is due to the fact that in Russia there are regions where magical thinking has become part of the national culture for centuries - for example, Altai, the Far North, Mari El. nine0003
How can a specialist help?
Self-help methods are unlikely to work here - this is too complex a disorder. And how can specialists - psychotherapists, clinical psychologists help? “We do two central things that have been proven to work in research around the world. First: exposure. The term means moving towards your fear. Is the client afraid of pollution? For example, after careful preparation, we agree with the client that he will try to touch things that he considers dirty. After that, he will not wash his hands, but in our presence he will wait until the anxiety itself begins to decrease.
People with OCD feel like this hell will never end. Our task is to show him that even with dirty hands he will soon calm down, that his anxiety is finite.” nine0003
The second important focus of the psychologist's attention is dealing with thinking errors. The client is shown that thought is not equal to action, thought is not equal to reality. If the client believes that his thoughts can harm other people, he is invited to conduct a series of behavioral experiments: can he force the flower in the therapist's office to wither with his mind or can he guess the number conceived by the psychologist. Experiments show that no matter how hard the client tries, his thoughts do not affect either the psychologist or those around him. Gradually, psychotherapy helps to get to the most “terrible” thoughts of the client and make sure that his relatives or friends do not get sick or die from the fact that a person thinks badly of them. nine0003
About the expert
Yakov Kochetkov — director of the Center for Cognitive Therapy, candidate of biological sciences, clinical psychologist.
Learn more