Lexapro postpartum depression
SAMHSA’s National Helpline | SAMHSA
Your browser is not supported
Switch to Chrome, Edge, Firefox or Safari
Main page content
-
SAMHSA’s National Helpline is a free, confidential, 24/7, 365-day-a-year treatment referral and information service (in English and Spanish) for individuals and families facing mental and/or substance use disorders.
Also visit the online treatment locator.
SAMHSA’s National Helpline, 1-800-662-HELP (4357) (also known as the Treatment Referral Routing Service), or TTY: 1-800-487-4889 is a confidential, free, 24-hour-a-day, 365-day-a-year, information service, in English and Spanish, for individuals and family members facing mental and/or substance use disorders.
This service provides referrals to local treatment facilities, support groups, and community-based organizations.
Also visit the online treatment locator, or send your zip code via text message: 435748 (HELP4U) to find help near you. Read more about the HELP4U text messaging service.
The service is open 24/7, 365 days a year.
English and Spanish are available if you select the option to speak with a national representative. Currently, the 435748 (HELP4U) text messaging service is only available in English.
In 2020, the Helpline received 833,598 calls. This is a 27 percent increase from 2019, when the Helpline received a total of 656,953 calls for the year.
The referral service is free of charge. If you have no insurance or are underinsured, we will refer you to your state office, which is responsible for state-funded treatment programs. In addition, we can often refer you to facilities that charge on a sliding fee scale or accept Medicare or Medicaid. If you have health insurance, you are encouraged to contact your insurer for a list of participating health care providers and facilities.
If you have health insurance, you are encouraged to contact your insurer for a list of participating health care providers and facilities.
The service is confidential. We will not ask you for any personal information. We may ask for your zip code or other pertinent geographic information in order to track calls being routed to other offices or to accurately identify the local resources appropriate to your needs.
No, we do not provide counseling. Trained information specialists answer calls, transfer callers to state services or other appropriate intake centers in their states, and connect them with local assistance and support.
-
Suggested Resources
What Is Substance Abuse Treatment? A Booklet for Families
Created for family members of people with alcohol abuse or drug abuse problems. Answers questions about substance abuse, its symptoms, different types of treatment, and recovery. Addresses concerns of children of parents with substance use/abuse problems.
Addresses concerns of children of parents with substance use/abuse problems.It's Not Your Fault (NACoA) (PDF | 12 KB)
Assures teens with parents who abuse alcohol or drugs that, "It's not your fault!" and that they are not alone. Encourages teens to seek emotional support from other adults, school counselors, and youth support groups such as Alateen, and provides a resource list.After an Attempt: A Guide for Taking Care of Your Family Member After Treatment in the Emergency Department
Aids family members in coping with the aftermath of a relative's suicide attempt. Describes the emergency department treatment process, lists questions to ask about follow-up treatment, and describes how to reduce risk and ensure safety at home.Family Therapy Can Help: For People in Recovery From Mental Illness or Addiction
Explores the role of family therapy in recovery from mental illness or substance abuse. Explains how family therapy sessions are run and who conducts them, describes a typical session, and provides information on its effectiveness in recovery.
For additional resources, please visit the SAMHSA Store.
Last Updated: 08/30/2022
Alcohol, Tobacco, and Other Drugs
Your browser is not supported
Switch to Chrome, Edge, Firefox or Safari
Misusing alcohol, tobacco, and other drugs can have both immediate and long-term health effects.The misuse and abuse of alcohol, tobacco, illicit drugs, and prescription medications affect the health and well-being of millions of Americans. NSDUH estimates allow researchers, clinicians, policymakers, and the general public to better understand and improve the nation’s behavioral health. These reports and detailed tables present estimates from the 2021 National Survey on Drug Use and Health (NSDUH).
Alcohol
Data:
- Among the 133.1 million current alcohol users aged 12 or older in 2021, 60.0 million people (or 45.1%) were past month binge drinkers.
 The percentage of people who were past month binge drinkers was highest among young adults aged 18 to 25 (29.2% or 9.8 million people), followed by adults aged 26 or older (22.4% or 49.3 million people), then by adolescents aged 12 to 17 (3.8% or 995,000 people). (2021 NSDUH)
The percentage of people who were past month binge drinkers was highest among young adults aged 18 to 25 (29.2% or 9.8 million people), followed by adults aged 26 or older (22.4% or 49.3 million people), then by adolescents aged 12 to 17 (3.8% or 995,000 people). (2021 NSDUH) - Among people aged 12 to 20 in 2021, 15.1% (or 5.9 million people) were past month alcohol users. Estimates of binge alcohol use and heavy alcohol use in the past month among underage people were 8.3% (or 3.2 million people) and 1.6% (or 613,000 people), respectively. (2021 NSDUH)
- In 2020, 50.0% of people aged 12 or older (or 138.5 million people) used alcohol in the past month (i.e., current alcohol users) (2020 NSDUH)
- Among the 138.5 million people who were current alcohol users, 61.6 million people (or 44.4%) were classified as binge drinkers and 17.7 million people (28.8% of current binge drinkers and 12.8% of current alcohol users) were classified as heavy drinkers (2020 NSDUH)
- The percentage of people who were past month binge alcohol users was highest among young adults aged 18 to 25 (31.
 4%) compared with 22.9% of adults aged 26 or older and 4.1% of adolescents aged 12 to 17 (2020 NSDUH)
4%) compared with 22.9% of adults aged 26 or older and 4.1% of adolescents aged 12 to 17 (2020 NSDUH) - Excessive alcohol use can increase a person’s risk of stroke, liver cirrhosis, alcoholic hepatitis, cancer, and other serious health conditions
- Excessive alcohol use can also lead to risk-taking behavior, including driving while impaired. The Centers for Disease Control and Prevention reports that 29 people in the United States die in motor vehicle crashes that involve an alcohol-impaired driver daily
Programs/Initiatives:
- STOP Underage Drinking interagency portal - Interagency Coordinating Committee on the Prevention of Underage Drinking
- Interagency Coordinating Committee on the Prevention of Underage Drinking
- Talk. They Hear You.
- Underage Drinking: Myths vs. Facts
- Talking with your College-Bound Young Adult About Alcohol
Relevant links:
- National Association of State Alcohol and Drug Abuse Directors
- Department of Transportation Office of Drug & Alcohol Policy & Compliance
- Alcohol Policy Information Systems Database (APIS)
- National Institute on Alcohol Abuse and Alcoholism
Tobacco
Data:
- In 2020, 20.
 7% of people aged 12 or older (or 57.3 million people) used nicotine products (i.e., used tobacco products or vaped nicotine) in the past month (2020 NSDUH)
7% of people aged 12 or older (or 57.3 million people) used nicotine products (i.e., used tobacco products or vaped nicotine) in the past month (2020 NSDUH) - Among past month users of nicotine products, nearly two thirds of adolescents aged 12 to 17 (63.1%) vaped nicotine but did not use tobacco products. In contrast, 88.9% of past month nicotine product users aged 26 or older used only tobacco products (2020 NSDUH)
- Tobacco use is the leading cause of preventable death, often leading to lung cancer, respiratory disorders, heart disease, stroke, and other serious illnesses. The CDC reports that cigarette smoking causes more than 480,000 deaths each year in the United States
- The CDC’s Office on Smoking and Health reports that more than 16 million Americans are living with a disease caused by smoking cigarettes
Electronic cigarette (e-cigarette) use data:
- In 2021, 13.2 million people aged 12 or older (or 4.7%) used an e-cigarette or other vaping device to vape nicotine in the past month.
 The percentage of people who vaped nicotine was highest among young adults aged 18 to 25 (14.1% or 4.7 million people), followed by adolescents aged 12 to 17 (5.2% or 1.4 million people), then by adults aged 26 or older (3.2% or 7.1 million people).
The percentage of people who vaped nicotine was highest among young adults aged 18 to 25 (14.1% or 4.7 million people), followed by adolescents aged 12 to 17 (5.2% or 1.4 million people), then by adults aged 26 or older (3.2% or 7.1 million people). - Among people aged 12 to 20 in 2021, 11.0% (or 4.3 million people) used tobacco products or used an e-cigarette or other vaping device to vape nicotine in the past month. Among people in this age group, 8.1% (or 3.1 million people) vaped nicotine, 5.4% (or 2.1 million people) used tobacco products, and 3.4% (or 1.3 million people) smoked cigarettes in the past month. (2021 NSDUH)
- Data from the Centers for Disease Control and Prevention’s 2020 National Youth Tobacco Survey. Among both middle and high school students, current use of e-cigarettes declined from 2019 to 2020, reversing previous trends and returning current e-cigarette use to levels similar to those observed in 2018
- E-cigarettes are not safe for youth, young adults, or pregnant women, especially because they contain nicotine and other chemicals
Resources:
- Tips for Teens: Tobacco
- Tips for Teens: E-cigarettes
- Implementing Tobacco Cessation Programs in Substance Use Disorder Treatment Settings
- Synar Amendment Program
Links:
- Truth Initiative
- FDA Center for Tobacco Products
- CDC Office on Smoking and Health
- National Institute on Drug Abuse: Tobacco, Nicotine, and E-Cigarettes
- National Institute on Drug Abuse: E-Cigarettes
Opioids
Data:
- Among people aged 12 or older in 2021, 3.
 3% (or 9.2 million people) misused opioids (heroin or prescription pain relievers) in the past year. Among the 9.2 million people who misused opioids in the past year, 8.7 million people misused prescription pain relievers compared with 1.1 million people who used heroin. These numbers include 574,000 people who both misused prescription pain relievers and used heroin in the past year. (2021 NSDUH)
3% (or 9.2 million people) misused opioids (heroin or prescription pain relievers) in the past year. Among the 9.2 million people who misused opioids in the past year, 8.7 million people misused prescription pain relievers compared with 1.1 million people who used heroin. These numbers include 574,000 people who both misused prescription pain relievers and used heroin in the past year. (2021 NSDUH) - Among people aged 12 or older in 2020, 3.4% (or 9.5 million people) misused opioids in the past year. Among the 9.5 million people who misused opioids in the past year, 9.3 million people misused prescription pain relievers and 902,000 people used heroin (2020 NSDUH)
- According to the Centers for Disease Control and Prevention’s Understanding the Epidemic, an average of 128 Americans die every day from an opioid overdose
Resources:
- Medication-Assisted Treatment
- Opioid Overdose Prevention Toolkit
- TIP 63: Medications for Opioid Use Disorder
- Use of Medication-Assisted Treatment for Opioid Use Disorder in Criminal Justice Settings
- Opioid Use Disorder and Pregnancy
- Clinical Guidance for Treating Pregnant and Parenting Women With Opioid Use Disorder and Their Infants
- The Facts about Buprenorphine for Treatment of Opioid Addiction
- Pregnancy Planning for Women Being Treated for Opioid Use Disorder
- Tips for Teens: Opioids
- Rural Opioid Technical Assistance Grants
- Tribal Opioid Response Grants
- Provider’s Clinical Support System - Medication Assisted Treatment Grant Program
Links:
- National Institute on Drug Abuse: Opioids
- National Institute on Drug Abuse: Heroin
- HHS Prevent Opioid Abuse
- Community Anti-Drug Coalitions of America
- Addiction Technology Transfer Center (ATTC) Network
- Prevention Technology Transfer Center (PTTC) Network
Marijuana
Data:
- In 2021, marijuana was the most commonly used illicit drug, with 18.
 7% of people aged 12 or older (or 52.5 million people) using it in the past year. The percentage was highest among young adults aged 18 to 25 (35.4% or 11.8 million people), followed by adults aged 26 or older (17.2% or 37.9 million people), then by adolescents aged 12 to 17 (10.5% or 2.7 million people).
7% of people aged 12 or older (or 52.5 million people) using it in the past year. The percentage was highest among young adults aged 18 to 25 (35.4% or 11.8 million people), followed by adults aged 26 or older (17.2% or 37.9 million people), then by adolescents aged 12 to 17 (10.5% or 2.7 million people). - The percentage of people who used marijuana in the past year was highest among young adults aged 18 to 25 (34.5%) compared with 16.3% of adults aged 26 or older and 10.1% of adolescents aged 12 to 17 (2020 NSDUH)
- Marijuana can impair judgment and distort perception in the short term and can lead to memory impairment in the long term
- Marijuana can have significant health effects on youth and pregnant women.
Resources:
- Know the Risks of Marijuana
- Marijuana and Pregnancy
- Tips for Teens: Marijuana
Relevant links:
- National Institute on Drug Abuse: Marijuana
- Addiction Technology Transfer Centers on Marijuana
- CDC Marijuana and Public Health
Emerging Trends in Substance Misuse:
- Methamphetamine—In 2019, NSDUH data show that approximately 2 million people used methamphetamine in the past year.
 Approximately 1 million people had a methamphetamine use disorder, which was higher than the percentage in 2016, but similar to the percentages in 2015 and 2018. The National Institute on Drug Abuse Data shows that overdose death rates involving methamphetamine have quadrupled from 2011 to 2017. Frequent meth use is associated with mood disturbances, hallucinations, and paranoia.
Approximately 1 million people had a methamphetamine use disorder, which was higher than the percentage in 2016, but similar to the percentages in 2015 and 2018. The National Institute on Drug Abuse Data shows that overdose death rates involving methamphetamine have quadrupled from 2011 to 2017. Frequent meth use is associated with mood disturbances, hallucinations, and paranoia. - Cocaine—In 2019, NSDUH data show an estimated 5.5 million people aged 12 or older were past users of cocaine, including about 778,000 users of crack. The CDC reports that overdose deaths involving have increased by one-third from 2016 to 2017. In the short term, cocaine use can result in increased blood pressure, restlessness, and irritability. In the long term, severe medical complications of cocaine use include heart attacks, seizures, and abdominal pain.
- Kratom—In 2019, NSDUH data show that about 825,000 people had used Kratom in the past month. Kratom is a tropical plant that grows naturally in Southeast Asia with leaves that can have psychotropic effects by affecting opioid brain receptors.
 It is currently unregulated and has risk of abuse and dependence. The National Institute on Drug Abuse reports that health effects of Kratom can include nausea, itching, seizures, and hallucinations.
It is currently unregulated and has risk of abuse and dependence. The National Institute on Drug Abuse reports that health effects of Kratom can include nausea, itching, seizures, and hallucinations.
Resources:
- Tips for Teens: Methamphetamine
- Tips for Teens: Cocaine
- National Institute on Drug Abuse
More SAMHSA publications on substance use prevention and treatment.
Last Updated: 01/05/2023
Use of antidepressants for the treatment of postpartum depression
Review question
In this Cochrane review, we wanted to know how effective antidepressants work in treating women with postpartum depression.
Why is this important?
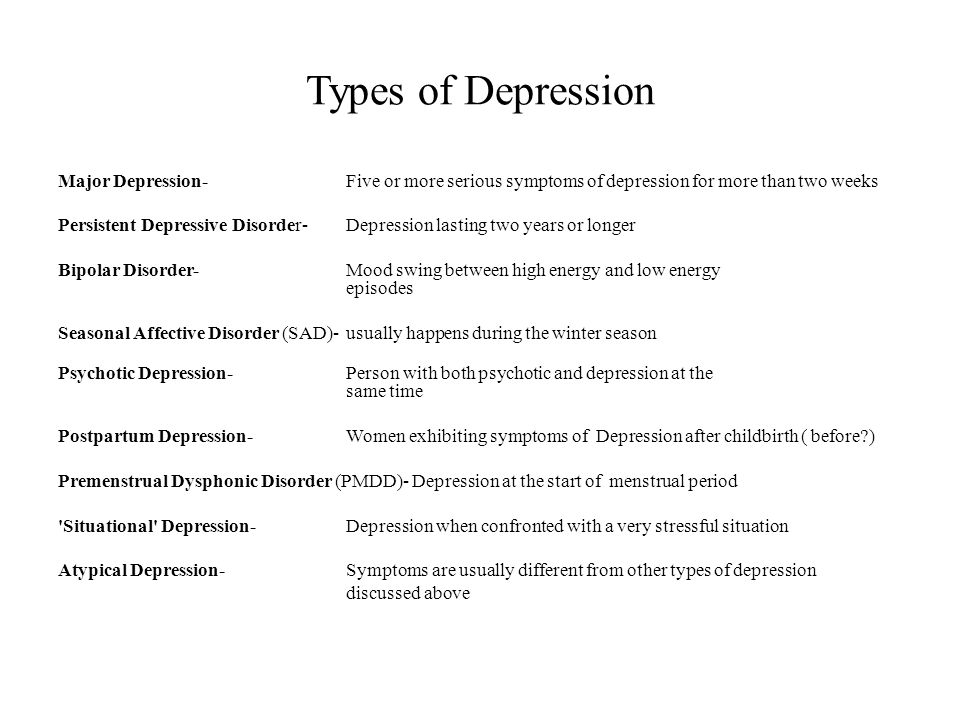
Postpartum depression is depression that begins within 12 months of the birth of a child. Postpartum depression affects many women. Postpartum depression can have serious short and long term consequences for the mother, the baby and the family as a whole.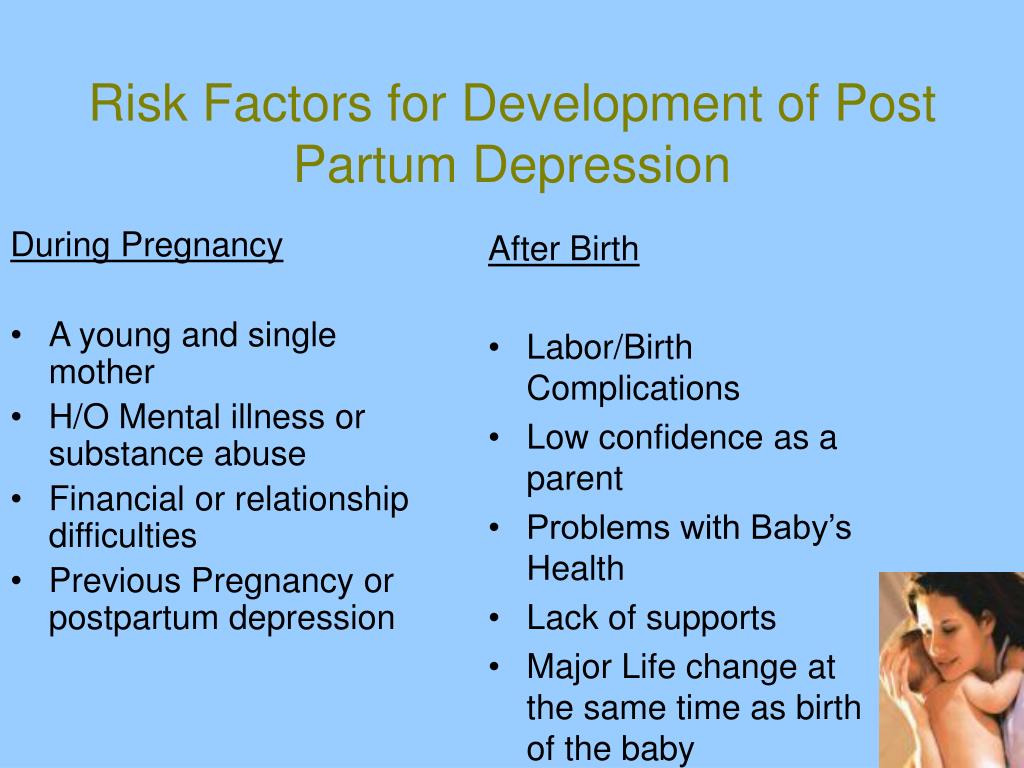
There are several ways to treat postpartum depression. Treatment for depression may include antidepressants, psychotherapy, support, or counseling. The type of treatment offered depends on the severity of the depression, other conditions, and the woman's choice. In general, pregnant women or women who are breastfeeding are often concerned about the potential adverse effects of antidepressants on their baby.
It is important to know if antidepressants can be an effective and acceptable treatment for women with postpartum depression.
What we did
In May 2020, we searched for studies on antidepressant treatment for women with postpartum depression. We looked for randomized controlled trials in which treatments were randomly assigned to participants. These studies provide the most reliable evidence.
We included 11 studies involving 1016 women. The studies compared antidepressants with placebo, conventional treatments (watch and wait, regular visits with a care coordinator), psychological interventions (therapy), psychosocial interventions (peer support or counseling), any other medication or other type of antidepressant, and complementary medicine (food supplements).
Eight of these studies were conducted in high-income English-speaking countries. The duration of treatment ranged from 4 to 24 weeks.
The outcome we focused on was the effectiveness of the treatment (how well the treatment worked). Efficacy was measured by the number of people who responded well to treatment or no longer met the criteria for depression at the end of treatment (remission). We also looked at whether women and/or their children experienced adverse effects of treatment.
What did we find?
We found that women receiving antidepressants may respond slightly better to treatment and have less postpartum depression than women receiving placebo. The number of adverse effects experienced by women was similar between the groups. There have been few studies comparing antidepressants with other treatments. The most commonly studied were antidepressants from the group "SSRIs" (selective serotonin reuptake inhibitors).
Terminals
Only a few eligible studies were identified in this review. There is some evidence that antidepressants may work better than placebo in women with postpartum depression. There is insufficient evidence to compare antidepressants with other treatments for postpartum depression. Clinicians need to consider evidence from general population studies and existing clinical guidelines, along with the woman's medical history and current symptoms, to make an individual decision about the risks and benefits of treating the woman.
Certainty of evidence
Our certainty (confidence) in the evidence is low. Some results are based on only a few studies with a small number of women in each group. Therefore, we are not sure how reliable these results are. Our conclusions may change if more research is done. Our findings that antidepressants may work better than placebo are similar to those of a large number of studies in the general population.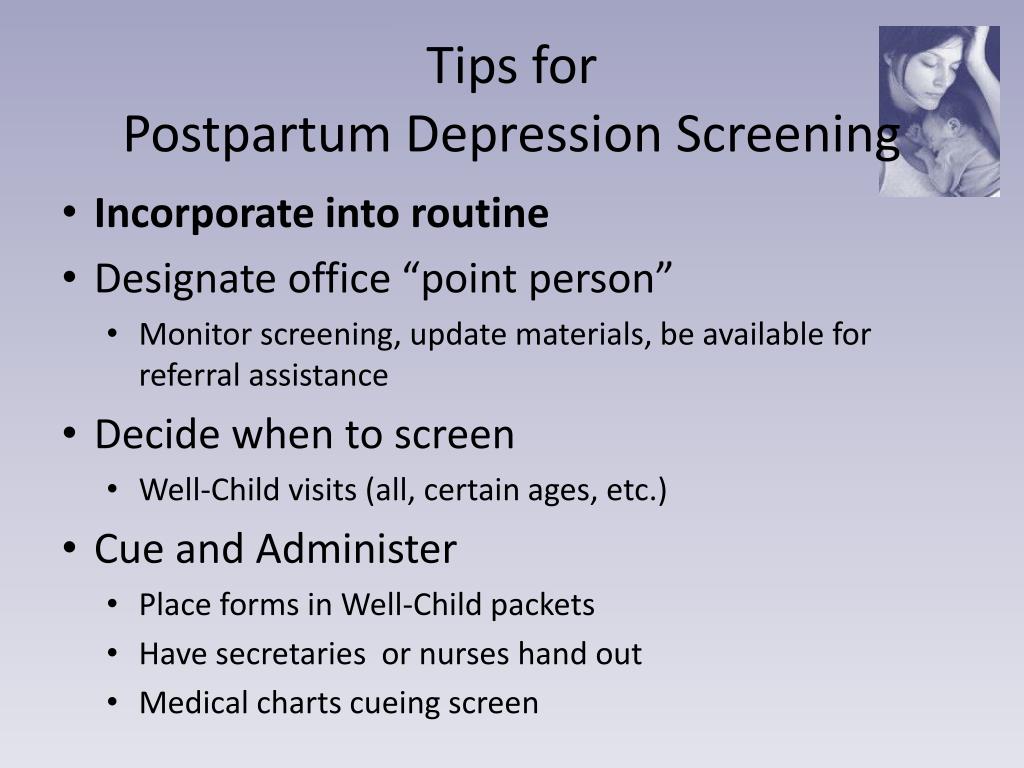
Translation notes:
Translation: Mikhailova Katerina Dmitrievna. Editing: Yudina Ekaterina Viktorovna. Russian translation project coordination: Cochrane Russia - Cochrane Russia, Cochrane Geographic Group Associated to Cochrane Nordic. For questions related to this translation, please contact us at: [email protected].
Treatment of postpartum depression and psychosis
Postpartum depression
WHAT ARE THE CAUSES AND RISK FACTORS FOR POSTPARTUM DEPRESSION?
As with other mental health disorders, there is an opinion about the genetic predisposition to the occurrence of postpartum depression.
Sudden changes in hormonal levels during pregnancy and after childbirth are considered biological factors contributing to the development of this condition. People who have experienced depression or anxiety in the past are at risk for depression during pregnancy or after childbirth. An interesting fact is that men are also subject to changes in the hormonal background during pregnancy. Also important concomitant factors are stress associated with any complications during pregnancy or childbirth and stress before caring for a child.
Also important concomitant factors are stress associated with any complications during pregnancy or childbirth and stress before caring for a child.
Additional risk factors associated with the development of postpartum depression are also low self-esteem, low socioeconomic status, lack of social support before and after childbirth, problems between spouses, including the experience of violence on behalf of a partner.
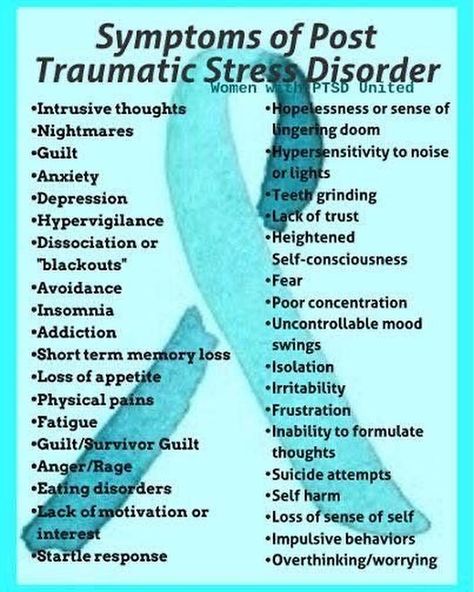
WHAT ARE THE SYMPTOMS AND SIGNS OF POSTPARTUM DEPRESSION?
Symptoms of postpartum depression appear during depression or up to four weeks after childbirth and include the following:
- Feelings of deep sadness, emptiness, emotional numbness, irritability, anger.
- Feelings of irritability and anger.
- Tendency to end relationships with family, friends, or avoiding pastimes that the patient usually enjoyed.
- Constant apathy and fatigue, sleep problems, overeating, loss of appetite.
- Strong feelings of worthlessness and inadequacy.
 Strong feelings of concern and anxiety associated with the child or lack of interest in him.
Strong feelings of concern and anxiety associated with the child or lack of interest in him. - Thoughts of suicide or fear of harming the child.
Postpartum psychosis is much less common and is a severe form of postpartum depression. Symptoms include the following:
- Brad
- Hallucinations (voices or visions that do not exist)
- Thoughts of harming a child
- Severe depressive symptoms.
HOW DO DOCTORS DIAGNOSIS POSTPARTUM DEPRESSION?
There are no tests to accurately determine postpartum depression. In this regard, medical professionals diagnose the disease by collecting a complete medical, family and psychological history of the patient. The advantage for patients is that the healthcare professional takes into account all aspects of the patient's life and environment. This includes, but is not limited to, gender, sexual orientation, cultural, religious, ethnicity, and socioeconomic status.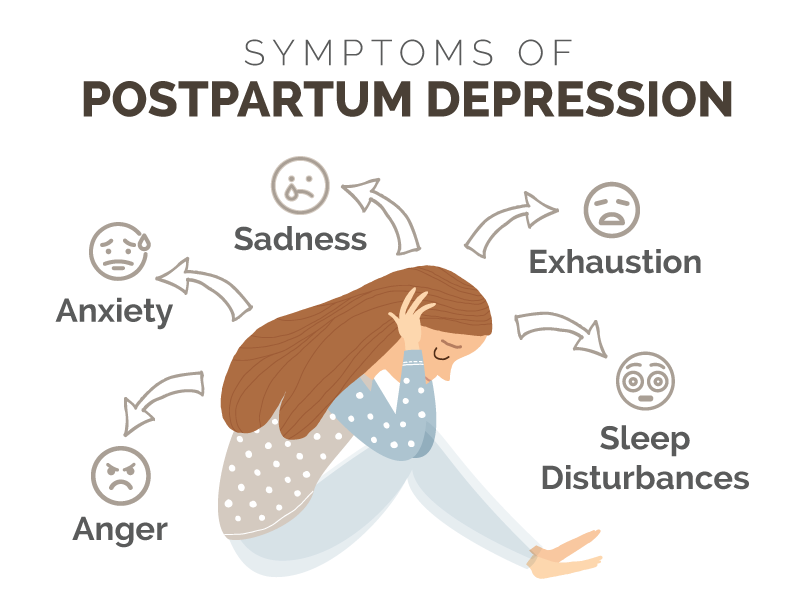 The health worker may conduct a physical examination of the patient or allow the patient's personal physician to perform such an examination. The physical examination usually includes laboratory tests to assess the patient's general health and is done to identify health conditions that affect psychological symptoms.
The health worker may conduct a physical examination of the patient or allow the patient's personal physician to perform such an examination. The physical examination usually includes laboratory tests to assess the patient's general health and is done to identify health conditions that affect psychological symptoms.
Postpartum depression is different from the so-called baby blues, a sad state after childbirth, which is observed in most recent deliveries. In baby blues, there may be minor episodes of crying, sadness, irritability, anxiety, and confusion. Unlike the symptoms of postpartum depression, the symptoms of baby blues reach their peak by the fourth day after delivery and disappear by day 10, without causing inconvenience to the woman's daily activities.
Postpartum psychosis is a psychiatric emergency that requires immediate intervention due to the possibility of suicide or child homicide. Symptoms of postpartum psychosis usually begin within two weeks of giving birth and include extremely disorganized thinking, bizarre behavior, hallucinations, and delusions. Postpartum psychosis is often a symptom of bipolar disorder, also called manic depression.
Postpartum psychosis is often a symptom of bipolar disorder, also called manic depression.
HOW IS POSTPARTUM DEPRESSION TREATED?
Training programs and support groups
Treatment for postpartum depression is the same for men and women. Parents of both sexes who received this diagnosis benefited enormously from being informed about the disease, as well as from the support of other parents who experienced such a situation.
Psychotherapy
Psychotherapy ("talk therapy") involves working with a trained therapist to identify ways to solve a problem and deal with any type of depression, including postpartum depression. It can act as a strong intervention, thereby producing positive changes in the brain. It is a particularly important alternative to drug treatment for women who are breastfeeding. In general, completion of this therapy takes from several weeks to several months. Further counseling is needed only for severe depression or other psychiatric symptoms.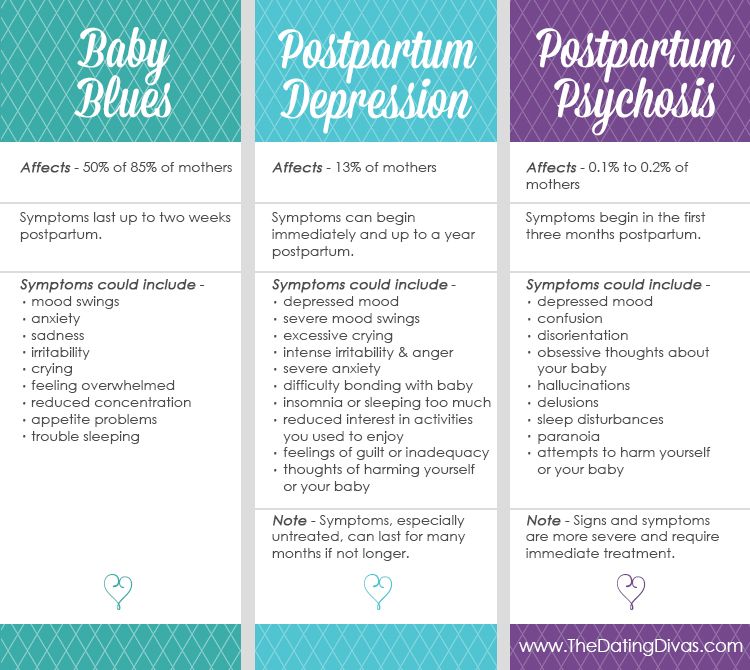
Interpersonal Therapy: Helps relieve depressive symptoms and helps the sufferer develop more effective social and interpersonal skills. Interpersonal therapy uses the following two strategies to do this.
- The first is to inform about the origin of depression. The therapist should be sure to emphasize that depression is a common condition and most patients should expect improvement from treatment.
- The second strategy is to identify specific problems (for example, the stress of caring for a child or interpersonal conflicts). Once problems are identified, the therapist is able to set realistic goals for solving those problems. Together with the participation of the patient, various treatment techniques will be applied to achieve these goals.
Cognitive Behavioral Therapy: Helps alleviate illness and reduce the risk of recurrence by changing the way the patient thinks. In cognitive behavioral therapy, the therapist uses three techniques to achieve these goals.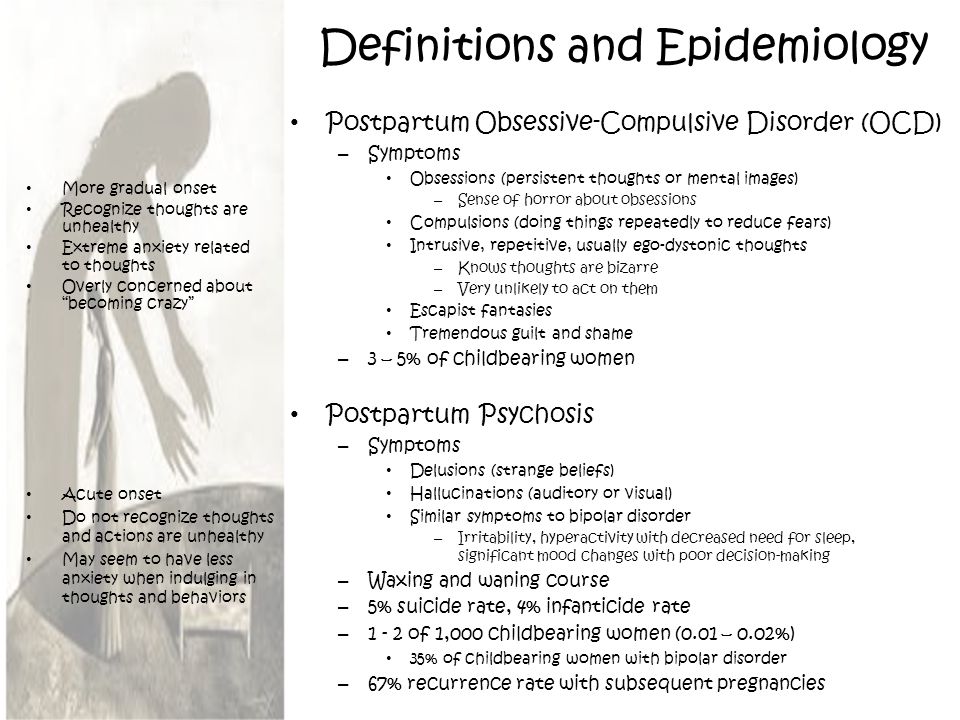
- Didactic component: This phase helps to establish positive expectations from the therapy and establish interaction.
- Cognitive component: Helps to identify thoughts and beliefs that influence behavior, especially those that predispose the patient to postpartum depression.
- Behavioral component: uses behavioral modification techniques to teach the patient more effective problem solving strategies.
Medicines
Medical treatment for postpartum depression usually consists of the use of antidepressants. The main types of antidepressants used are selective serotonin reuptake inhibitors (SSRIs), serotonin/norepinephrine/dopamine reuptake inhibitors (NSRIs), tricyclic antidepressants (TCAs), and monoamine oxidase inhibitors (monoamine). oxidase inhibitors (MAOIs).Selective serotonin reuptake inhibitors (SSRIs) affect the level of serotonin in the brain.For many clinicians, they are the first choice due to the high level of efficacy and overall safety of this group. Examples of antidepressants are given below.Special name first , with the brand name in brackets
Examples of antidepressants are given below.Special name first , with the brand name in brackets
• Fluoxetine (Prozac)
• Sertraline (Zoloft)
• Paroxetine (Paxil)
• Fluvoxamine (Luvox)
• Citalopram (Celexa)
• Escitalopram (Lexapro)
• Vilazodone (Viibryd)
• Vortioxetine (Trintellix)
SNRIs and NDRs:
• Bupropion (Wellbutrin)
• Mirtazapine (Remeron)
• Venlafaxine (Effexor)
• Duloxetine (Cymbalta)
• Desvenlafaxine (Pristiq)
• Levomilnacipran (Fetzima)
Tricyclic antidepressants (TCAs) are sometimes prescribed for severe cases of depression or when selective serotonin reuptake inhibitors (SSRIs) or serotonin/norepiphrine/dopamine reuptake inhibitors (SNRIs) are not effective. These drugs affect many chemicals in the brain (neurotransmitters), especially epinephrine and norepinephrine (adrenaline and norepinephrine, respectively). Examples include:
• amitriptyline (Elavil),
• clomipramine (Anafranil),
• desipramine (Norpramin),
• doxepin (Adapin),
• imipramine (Tofranil),
• nortriptyline (Pamelor).
Approximately two-thirds of patients who take medication recover. For a noticeable improvement in mood, it is necessary to take the prescribed dose for two to six weeks. That is why stopping the drug before a visible improvement is undesirable. Monoamine oxidase inhibitors (MAOIs) are not often prescribed due to the popularity of selective serotonin reuptake inhibitors (SSRIs). Due to potential interactions, monoamine oxidase inhibitors (MAOIs) should not be taken with other medications or foods containing tyramine (found in aged cheeses, wines, and meats). For example, the monoamine oxidase inhibitors phenelzine (Nardil) and tranylcypromine (Parnate).
The atypical use of antipsychotic drugs is commonly practiced as an adjunct to normothymic drugs in cases of postpartum psychosis. Examples of neuroleptics:
• aripiprazole (Abilify),
• olanzapine (Zyprexa),
• paliperidone (Invega),
• Quetiapine (Seroquel),
• risperidone (Risperdal),
• ziprasidone (Geodon),
• asenapine (Saphris),
• iloperidone (Fanapt),
• Lurasidone (Latuda).
Normotimics outside the group of antipsychotics are also sometimes used along with antipsychotics in the treatment of postpartum psychosis, since bipolar disorder may also be present in some patients. Examples of normotics not included in the group of antipsychotics:
• lithium (Lithium Carbonate, Lithium Citrate),
• Divalproex sodium (Depakote),
• carbamazepine (Tegretol), and
• lamotrigine (Lamictal).
© Pobedish.ru (translated from English)
(
Pobedish.ru 7 votes: 4.86 out of 5 )
Did the article help? Support the site!
Transfer funds for site
Help
Share an article:
Share
Tweet