Lexapro and erectile dysfunction
Antidepressants and Erectile Dysfunction | hims
Medically reviewed by Kristin Hall, FNP
Written by Our Editorial Team
Last updated 2/2/2021
If you’ve been diagnosed with major depression or an anxiety disorder, your healthcare provider may prescribe an antidepressant to improve your mood and provide relief from your symptoms.
Antidepressants are some of the most commonly used prescription medications. In fact, almost 13 percent of all people aged 12 and up in the United States took antidepressants on a monthly basis at some point between 2011 and 2014.
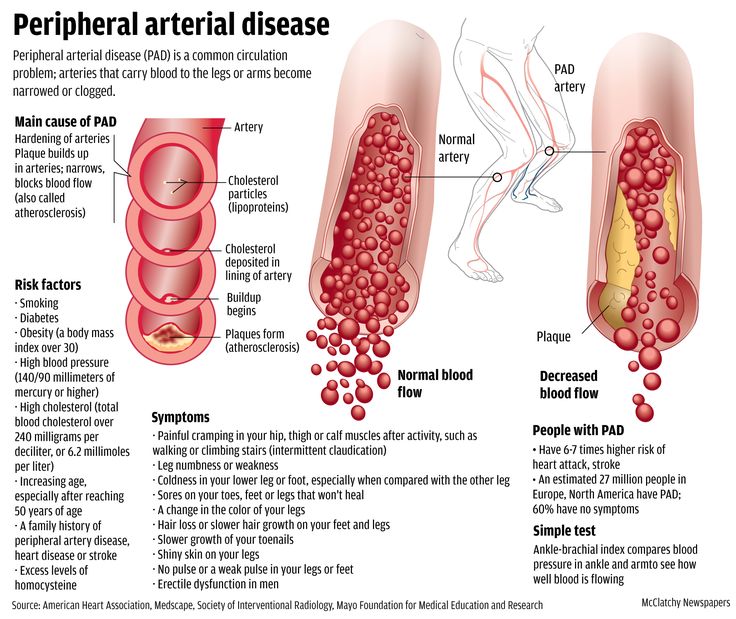
In our guide to the biggest risk factors for erectile dysfunction (ED), we listed a variety of widely used medications.
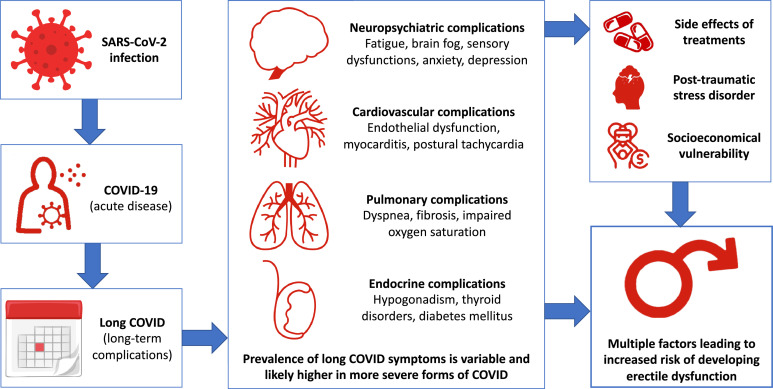
Unfortunately, antidepressants were part of the list. As it happens, antidepressants and erectile dysfunction actually have a very close link that most men might not even think about prior to or during treatment.
In fact, antidepressants are one of the types of medication most closely associated with sexual dysfunction in men.
Below, we’ve explained what antidepressants are, as well as how certain antidepressants can lead to sexual performance issues such as erectile dysfunction.
We’ve also shared the treatment options that are available if you’ve recently started to take an antidepressant and need help dealing with ED.
What Are Antidepressants?
Antidepressants are medications used to treat depression and anxiety. They work by changing the levels of certain natural chemicals, called neurotransmitters, in your brain and body.
Neurotransmitters are involved in regulating many aspects of your thoughts, feelings and bodily functions. For example, the neurotransmitter serotonin -- a common target of antidepressants -- is involved in regulating mood, happiness and anxiety.
By increasing your levels of certain neurotransmitters, antidepressant medication can stabilize your moods and reduce the severity of depression and certain forms of anxiety.
Several different types of antidepressants are used today. Your healthcare provider may suggest using one of the following classes of antidepressants:
Your healthcare provider may suggest using one of the following classes of antidepressants:
Selective serotonin reuptake inhibitors (SSRIs). These are the most widely used and common antidepressants. They work by increasing serotonin levels. SSRIs are typically used as first-line treatments for major depression and other depressive disorders.
Serotonin-norepinephrine reuptake inhibitors (SNRIs). These antidepressants work by increasing serotonin and norepinephrine levels. They’re often used when SSRIs are ineffective at controlling depression symptoms.
Tricyclic antidepressants (TCAs). These older antidepressants work by targeting five different neurotransmitter pathways. They’re equally as effective as SSRIs, but have a higher risk of causing adverse effects and generally aren’t prescribed as often.
Monoamine oxidase inhibitors (MAOIs). These antidepressants were first launched in the 1950s. Because of their high risk of side effects and drug interactions, they’re rarely used except when other medications aren’t effective.
Other antidepressants. Not all antidepressants fit into a distinct category. Some drugs used to treat depression, such as bupropion (Wellbutrin®), are commonly referred to as atypical antidepressants due to their different mechanisms of action and effects.
Our full list of antidepressants goes into more detail about these medications, how they work as treatments for depression and their potential risks and side effects.
Can Antidepressants Cause Erectile Dysfunction (ED)?
Not-so-fun-fact: Many antidepressants cause sexual dysfunction as a side effect. In men, this is most commonly manifested as a reduction in sex drive (decreased libido) and difficulties with developing and maintaining an erection.
In addition to reducing sexual desire and affecting your erectile health, certain antidepressants can also cause orgasmic dysfunction (difficulty reaching orgasm and ejaculating). For example, Lexapro may cause delayed ejaculation.
Sexual side effects such as erectile dysfunction are known to occur with many antidepressants, including the following common medications:
Citalopram (Celexa®)
Sertraline (Zoloft®)
Fluoxetine (Prozac®)
Paroxetine (Paxil®)
Duloxetine (Cymbalta®)
Escitalopram (Lexapro®)
These sexual side effects are often referred to as antidepressant-induced sexual dysfunction, or SSRI-induced sexual dysfunction.
Although not everyone develops sexual side effects from antidepressants, many people do. In a review published in the Annals of Pharmacotherapy, researchers noted that between 30 and 60 percent of people prescribed SSRIs experience some negative sexual effects.
So in short, yes, antidepressants can and often do cause ED. If you’re prescribed one of these medications and notice weaker erections or a dulled sexual response, there’s a good chance it could be a side effect of your antidepressant treatment.
Viagra online
Genuine Viagra® makes it possible
How & Why Antidepressants Cause Erectile Dysfunction
Although experts aren’t aware of exactly why some antidepressants cause erectile dysfunction, there are several theories about the sexual side effects of antidepressants.
One is that antidepressants cause sexual issues as a byproduct of their effect on serotonin. By inhibiting the reuptake of serotonin, antidepressants such as SSRIs and SNRIs increase levels of serotonin in the body and reduce the severity of depression and anxiety symptoms.
Researchers believe that this may affect other hormones and neurotransmitters, including some that are involved in sexual excitement and function.
For example, increased levels of serotonin are believed to affect testosterone, an important sex hormone responsible for libido and sexual function, and dopamine, a “feel good” chemical that’s involved in achieving orgasm and ejaculation.
Some antidepressants, including escitalopram and sertraline, are also linked to increased levels of prolactin -- a hormone that can cause low libido and orgasm dysfunction in men.
It’s important to point out that not all sexual dysfunction that occurs with antidepressants can be attributed directly to antidepressants.
Sexual performance issues are known depressive symptoms, meaning they develop in people with depression. In women, a common symptom of depression is vaginal dryness. In men, ED and delayed orgasm are both common issues.
If You Get ED, Should You Stop Taking Your Antidepressant?
If you’ve recently started to take an antidepressant and notice that you’re beginning to develop erectile dysfunction or another sexual side effect, you may have considered stopping treatment to prevent the issue from getting worse.
This isn’t a good idea for several reasons. The first is that stopping treatment might cause your depression to either come back or worsen. The second is that abruptly giving up treatment with antidepressants can cause withdrawal symptoms.
Referred to as antidepressant discontinuation syndrome, these symptoms can include nausea, flu-like issues, insomnia, dizziness, sensory disturbances and mood changes, such as agitation and irritability.
These symptoms often develop within a few days of stopping your medication and can continue for several weeks at a time.
Generic for Viagra (sildenafil)
The more affordable FDA-approved medication that treats Erectile Dysfunction at a quarter of the cost. 🙌
Generic for Cialis (tadalafil)
Affordable and helps get the job done. Generic Cialis helps you get and maintain your erections through a simple, daily dosage.
Viagra®
The OG Little Blue Pill that made its name as the first prescription Erectile Dysfunction treatment.
Cialis®
Cialis helps you get and keep stronger erections with a daily or as-needed pill.
What to Do if You Get Antidepressant-Induced ED
If you have bothersome erectile dysfunction or other side effects from an antidepressant, don’t abruptly stop taking it.
Instead, it’s best to talk with your healthcare provider about your symptoms. They may suggest one or several of the following approaches to deal with your side effects and treat your erectile dysfunction:
They may suggest one or several of the following approaches to deal with your side effects and treat your erectile dysfunction:
Switching to a different antidepressant. Some antidepressants have a lower risk of causing sexual issues than others. For example, research suggests that sexual issues are significantly more common with SSRIs than with drugs such as bupropion.If you’re prescribed an antidepressant that’s known for causing sexual health problems, your healthcare provider may suggest switching to a different medication.
Adjusting your dosage. Sometimes, it’s the dosage rather than the drug that results in side effects. Instead of changing your medication, your healthcare provider might adjust your dosage to reduce your risk of experiencing issues that affect your sex life.
Going on a drug holiday. In some cases, your healthcare provider may suggest going on a “drug holiday” by not taking your antidepressant or reducing your dosage on days when you plan to have sex.
 Drug holidays are considered a “high-risk” treatment option. Your healthcare provider may ask you to keep them informed about any side effects or symptoms of depression that occur on medication-free days.
Drug holidays are considered a “high-risk” treatment option. Your healthcare provider may ask you to keep them informed about any side effects or symptoms of depression that occur on medication-free days. Waiting for the issues to disappear. If you’re only prescribed antidepressants for the short term, your healthcare provider might simply suggest waiting until you’re done with treatment to regularly have sex.In some cases, antidepressant side effects improve over time. Your healthcare provider may suggest a “wait and see” approach to see if your sexual performance improves on its own as your body gets used to the effects of your medication.
Using ED medication. If you need to keep using your antidepressant, your healthcare provider may recommend taking ED medication such as sildenafil (the active ingredient in Viagra®) at the same time. Research has found that oral sildenafil helps to improve erections and other aspects of sexual function for many men who use antidepressants.
Can You Take Viagra With Antidepressants?
Put simply, yes. Both brand name Viagra, generic sildenafil and other ED medications are often used to treat erectile dysfunction that’s caused by antidepressants.
Other medications for ED include tadalafil (the active ingredient in Cialis®), vardenafil (Levitra®) and avanafil (Stendra®).
These medications, which are called PDE5 inhibitors, work by making it easier for blood to flow to your penis. They typically start working in 30 to 60 minutes and can be taken shortly before sex to improve your erectile function and prevent ED.
Several studies have found that PDE5 inhibitors work well at treating antidepressant-associated sexual dysfunction such as ED. In one small study of 14 people, even a mild 25mg dose of sildenafil taken prior to sex produced measurable improvements for men prescribed SSRIs.
Our guide to the most common erectile dysfunction treatments explains how these medications work, their potential side effects, how to use them and more.
Sildenafil citrate
Get hard for 95% cheaper than Viagra
Take Action to Treat Antidepressant-Induced ED
Antidepressants are highly effective for the treatment of depression and other mental illnesses, but they often cause side effects.
Unfortunately, for many men, these can include sexual health and performance issues such as erectile dysfunction.
If you take antidepressants and develop ED, it’s always best to talk to your healthcare provider about your options. They may recommend adjusting your dosage, switching antidepressants or making other changes to reduce the severity of your side effects.
Another option is to use ED medication. We offer several FDA-approved ED medications online, which are available after a consultation with a licensed healthcare provider who will determine if a prescription is appropriate.
Interested in learning more about successfully treating ED? Our guide to the causes of erectile dysfunction goes into more detail about how erectile dysfunction develops, as well as the steps that you can take to get rid of it for good.
19 Sources
Hims & Hers has strict sourcing guidelines to ensure our content is accurate and current. We rely on peer-reviewed studies, academic research institutions, and medical associations. We strive to use primary sources and refrain from using tertiary references.
- Pratt, L.A., Brody, D.J. & Gu, Q. (2017, August). Antidepressant Use Among Persons Aged 12 and Over: United States, 2011–2014. Retrieved from https://www.cdc.gov/nchs/products/databriefs/db283.htm
- Sheffler, Z.M. & Abdijadid, S. (2021, November 14). Antidepressants. StatPearls. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK538182/
- What is Serotonin? (2018, December). Retrieved from https://www.hormone.org/your-health-and-hormones/glands-and-hormones-a-to-z/hormones/serotonin
- Depression. (2018, February). Retrieved from https://www.nimh.nih.gov/health/topics/depression
- Anxiety Disorders.
 (2018, July). Retrieved from https://www.nimh.nih.gov/health/topics/anxiety-disorders
(2018, July). Retrieved from https://www.nimh.nih.gov/health/topics/anxiety-disorders - Chu, A. & Wadhwa, R. (2021, May 10). Selective Serotonin Reuptake Inhibitors. StatPearls. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK554406/
- Kendrick, T., Taylor, D. & Johnson, C.F. (2019, March). Which first-line antidepressant? British Journal of General Practice. 69 (680), 114–115. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6400617/
- Moraczewski, J. & Aedma, K.K. (2021, November 30). Tricyclic Antidepressants. StatPearls. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK557791/
- Sub Laban, T. & Saadabadi, A. (2021, August 6). Monoamine Oxidase Inhibitors (MAOI). StatPearls. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK539848/
- Gregorian, R.S., et al. (2002, October). Antidepressant-induced sexual dysfunction. Annals of Pharmacotherapy. 36 (10), 1577-89.
 Retrieved from https://pubmed.ncbi.nlm.nih.gov/12243609/
Retrieved from https://pubmed.ncbi.nlm.nih.gov/12243609/ - Jing, E. & Straw-Wilson, K. (2016, July). Sexual dysfunction in selective serotonin reuptake inhibitors (SSRIs) and potential solutions: A narrative literature review. The Mental Health Clinician. 6 (4), 191–196. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6007725/
- Park, Y.-M. (2017, May). Serum Prolactin Levels in Patients with Major Depressive Disorder Receiving Selective Serotonin-Reuptake Inhibitor Monotherapy for 3 Months: A Prospective Study. Psychiatry Investigation. 14 (3), 368–371. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5440440/
- What is hyperprolactinemia and how does it affect male sexual health? (n.d.). Retrieved from https://www.issm.info/sexual-health-qa/what-is-hyperprolactinemia-and-how-does-it-affect-male-sexual-health
- Kennedy, S.H. & Rizvi, S. (2009, April). Sexual dysfunction, depression, and the impact of antidepressants.
 Journal of Clinical Psychopharmacology. 29 (2), 157-64. Retrieved from https://pubmed.ncbi.nlm.nih.gov/19512977/
Journal of Clinical Psychopharmacology. 29 (2), 157-64. Retrieved from https://pubmed.ncbi.nlm.nih.gov/19512977/ - Gabriel, M. & Sharma, V. (2017, May 29). Antidepressant discontinuation syndrome. Canadian Medical Association Journal. 189 (21), E747. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5449237/
- Higgins, A., Nash, M. & Lynch, A.M. (2010). Antidepressant-associated sexual dysfunction: impact, effects, and treatment. Drug, Healthcare and Patient Safety. 2, 141–150. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3108697/
- Nuremberg, H.G., et al. (2003). Treatment of Antidepressant-Associated Sexual Dysfunction With Sildenafil A Randomized Controlled Trial. The Journal of the American Medical Association. 289 (1), 56-64. Retrieved from https://jamanetwork.com/journals/jama/fullarticle/195700
- Dhaliwal, A. & Gupta, M. (2021, June 25). PDE5 Inhibitors. StatPearls.
 Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK549843/
Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK549843/ - Damis, M., Patel, Y. & Simpson, G.M. (1999, December). Sildenafil in the Treatment of SSRI-Induced Sexual Dysfunction: A Pilot Study. The Primary Care Companion to the Journal of Clinical Psychiatry. 1 (6), 184–187. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC181091/
This article is for informational purposes only and does not constitute medical advice. The information contained herein is not a substitute for and should never be relied upon for professional medical advice. Always talk to your doctor about the risks and benefits of any treatment. Learn more about our editorial standards here.
When an SSRI medication impacts your sex life
The popular medications known as selective serotonin reuptake inhibitors or SSRIs (see box) can help lift people out from under a dark cloud of depression. But there are some side effects from antidepressants, including those that can affect your sex life. In addition to reducing interest in sex, SSRI medications can make it difficult to become aroused, sustain arousal, and reach orgasm. Some people taking SSRIs aren't able to have an orgasm at all. These symptoms tend to become more common with age.
In addition to reducing interest in sex, SSRI medications can make it difficult to become aroused, sustain arousal, and reach orgasm. Some people taking SSRIs aren't able to have an orgasm at all. These symptoms tend to become more common with age.
SSRI medications include
|
If you experience any sexual problems while taking an SSRI medication, talk with your doctor or therapist. About 35% to 50% of people with untreated major depression experience some type of sexual dysfunction prior to treatment. So, in some cases, sexual difficulties may stem not from the SSRI, but rather from the underlying depression.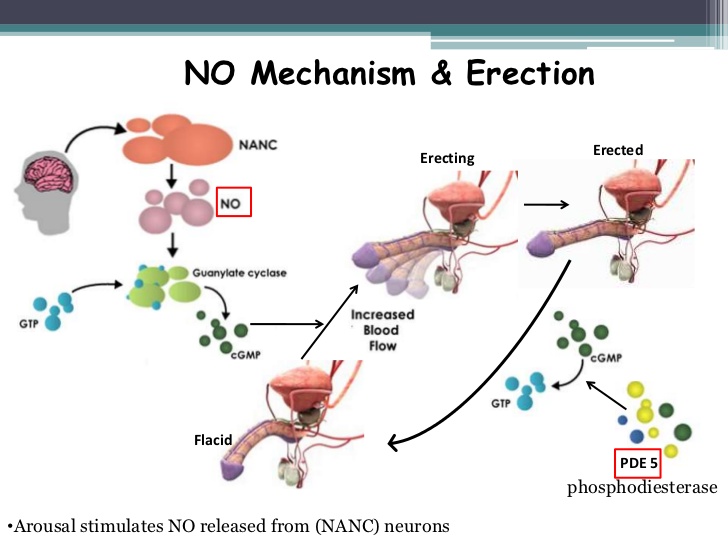 If medication is the problem, sexual side effects sometimes subside with time, so it's worth waiting a while to see if problems diminish. This is a particularly good strategy if the medication is easing your depression significantly. But if side effects from antidepressants persist, your doctor or therapist may suggest one of the following strategies, as found in the Harvard Special Health Report Understanding Depression:
If medication is the problem, sexual side effects sometimes subside with time, so it's worth waiting a while to see if problems diminish. This is a particularly good strategy if the medication is easing your depression significantly. But if side effects from antidepressants persist, your doctor or therapist may suggest one of the following strategies, as found in the Harvard Special Health Report Understanding Depression:
Lowering the dose. Sexual side effects may subside at a lower, although still therapeutic, dose.
Scheduling sex. Your medication may produce more pronounced side effects at particular times of the day, for example, within a few hours of taking it. If so, you can try scheduling sexual activity for the time when side effects are least bothersome—or take the drug at a different time.
Taking a drug holiday. Depending on how long the drug usually remains in your body, you might stop taking it for a few days—for example, before a weekend, if that's when you hope to have sex. This isn't spontaneous, but it can work if you carefully follow your doctor's directions about how to stop and resume your medication. However, there is always a chance that this might cause a relapse, especially if it is one of the drugs that leaves your system relatively rapidly.
This isn't spontaneous, but it can work if you carefully follow your doctor's directions about how to stop and resume your medication. However, there is always a chance that this might cause a relapse, especially if it is one of the drugs that leaves your system relatively rapidly.
Switching to a different drug. Certain antidepressants, such as bupropion (Wellbutrin), and mirtazapine (Remeron) are less likely to cause sexual problems. Bupropion, which affects both norepinephrine and dopamine, can sometimes improve sexual response.
Adding a drug. For some men, taking sildenafil (Viagra) or tadalafil (Cialis) can alleviate SSRI-induced erectile dysfunction. Both men and women may benefit from adding bupropion to their treatment. This medication has been found to counter SSRI-induced sexual dysfunction, boost sexual drive and arousal, and increase the intensity or duration of an orgasm. In some people, the anti-anxiety drug buspirone (BuSpar) may help increase libido and restore the ability to have an orgasm.
Meeting with a therapist. Even when physical issues or medication are at the root of sexual problems, psychological issues often become interwoven. For example, a few episodes of erectile dysfunction may cause a man to withdraw from sex and his partner to feel rejected. These issues can lead the couple to retreat further from intimacy. Working with a sex therapist or general therapist can help couples explore their sexual concerns, learn to better communicate, and expand their repertoire of sexual activities.
– By Julie Corliss
Executive Editor, Harvard Heart Letter
Sexual dysfunction during treatment with second-generation antidepressants in patients with major depressive disorders
PUBLICATIONS
Introduction.
Sexual dysfunction (sexual disorders of desire (decreased libido), sexual arousal disorder (erectile dysfunction), orgasmic disorders and sexual pain disorders (dyspareunia, vaginismus) is one of the symptoms of major depressive disorder (MDD) and is also often associated with the use of antidepressants Second generation Sexual dysfunction is sometimes a serious side effect of therapy and can lead to discontinuation of treatment and deterioration in the quality of life of patients. 0009 [1]
0009 [1]
Purpose of the study.
To assess the risk of sexual dysfunction in patients with major depressive disorder treated with second-generation antidepressants.
Materials and methods.
The analysis included English-language articles found in the PubMed, EMBASE, Cochrane Library, PsycINFO and International Pharmaceutical Abstracts search databases from 1980 to October 2012, which described the results of randomized controlled trials of antidepressants conducted for at least 6 weeks and the results observational studies with at least 1,000 participants. nine0003
The authors of the study assessed the risk of developing sexual dysfunction during the use of second-generation antidepressants.
Results.
The analysis included 63 studies (58 randomized clinical trials and 5 observational studies) with a total of 26,00 participants.
The results of a systematic review and meta-analysis demonstrated that treatment with bupropion is associated with the lowest risk of developing sexual dysfunction, while the use of paroxetine and Escilatoprama is associated with a statistically significant increase in the risk of developing sexual dysfunction compared with other members of this class of drugs. nine0003
nine0003
Conclusion.
A systematic review and meta-analysis showed that the use of paroxetine and escilatoprama was associated with the development of sexual dysfunction in patients with major depressive disorder.
Discussion. [2]
Bupropion (aplenzin, wellbutrin, wellbutrin SR, wellbutrin XL) is a selective neuronal reuptake inhibitor of catecholamines (norepinephrine and dopamine) with minimal effect on the uptake of indolamines (serotonin) and no inhibition of MAO. The drug is used to treat MDD and prevent recurrence of depressive episodes. nine0003
Paroxetine (Paxil, Pexeva) is a selective inhibitor of the reuptake of serotonin (5-hydroxytryptamine, 5-HT) by neurons in the brain. The drug has a low affinity for m-cholinergic receptors (has a weak anticholinergic effect), α1-, α2- and β-adrenergic receptors, as well as dopamine (D2), 5HT1-like, 5HT2-like and histamine h2 receptors. The drug is used to treat: MDD, obsessive-compulsive disorders, panic disorders, incl. with agoraphobia, social anxiety disorders/social phobias, generalized anxiety disorders. nine0003
with agoraphobia, social anxiety disorders/social phobias, generalized anxiety disorders. nine0003
Using the FAERS database (from 11/01/1997 to 12/31/2012) 35,358 serious side effects were recorded during the use of paroxetine (Paxil, Pexev), which led to 1,666 deaths of patients.
The most commonly reported adverse drug reactions were withdrawal, dizziness and maternal drug exposure during pregnancy. In 1,281 cases, the development of various types of sexual dysfunction was recorded. nine0003
Escilatopram (Lexapro) is a selective serotonin reuptake inhibitor. The drug increases the concentration of the neurotransmitter in the synaptic cleft, enhances and prolongs the action of serotonin on postsynaptic receptors. Escitalopram practically does not bind to serotonin (5-HT), dopamine (D1 and D2) receptors, α-adrenergic, m-cholinergic receptors, as well as benzodiazepine and opioid receptors. Indications for its use are: major depressive disorders, generalized anxiety disorders, panic disorders (including those with agoraphobia). nine0003
nine0003
Using the FAERS database (from 11/01/1997 to 12/31/2012) 6,408 serious side effects were detected during the use of escilatopram (Lexapro), which led to 2,095 hospitalizations and 604 deaths.
The most frequently diagnosed adverse drug reactions were suicidal ideation, anxiety and nausea. In 112 cases, the development of various types of sexual dysfunction was recorded.
Literature. nine0006
-
Ursula Reichenpfader, Gerald Gartlehner, Laura C. Morgan, Amy Greenblatt, Barbara Nussbaumer, Richard A. Hansen, Megan Van Noord, Linda Lux, Bradley N. Gaynes. Sexual Dysfunction associated with Second-Generation Antidepressants in Patients with Major Depressive Disorder: Results from a Systematic Review with Network Meta-Analysis. drug safety. January 2014, Volume 37, Issue 1, pp 19-31.
-
The Adverse Events Research Team. Analysis Determines Levels of Sexual Dysfunction in Second Generation Antidepressants.
 January 7, 2014.
January 7, 2014.
Antidepressants and potency. What men need to know.
How antidepressant drug side effects affect men's sexual health: 6 things for antidepressant drinkers.
In this article
- Good antidepressants and side effects.
- The simplest solution is to change the dose
- Some antidepressants are more dangerous than others
- Sedatives, if you take them, can play a role
- Changing or adding drugs can bring relief
- Sexual problems may persist after discontinuation of medication
Good antidepressants and side effects
Antidepressants are powerful in treating anxiety disorders and depression . But men often fear that the use of these drugs may jeopardize their sex life. These drugs do often have sexual side effects - they can cause problems with ejaculation (with delayed or inability to do so) and weakening of libido .
In fact, most men can get rid of the sexual dysfunction caused by antidepressants by continuing to take the medication. This is usually a solvable problem.
Patients often go to an Internet search engine, enter "sexual dysfunction" and immediately draw conclusions about their problem. In fact, there are many psychosomatic causes of sexual dysfunction, such as anxiety , anxiety disorders, depression or substance abuse . In our practice, we often see patients whose sexual function improves when undergoing psychotherapy with antidepressants, apparently because the impairment of their function was due in part to their restlessness, anxiety, apathy or depression. The conclusion is justified: men can take antidepressants without harming their sex life.
The simplest solution is to change the dose
Talk to your psychiatrist or psychotherapist and try to figure this out. Do not stop treatment and do not make changes yourself, this can lead to big problems. It may also not be correct to prescribe antidepressants by non-specialist doctors (neurologists, therapists ...) due to other specifics of their preparation, the complexity of the scheme for the effect of drugs on the human psyche and, in general, the validity of the use of one or another antidepressant in a particular situation or need other psychotherapeutic methods .
Do not stop treatment and do not make changes yourself, this can lead to big problems. It may also not be correct to prescribe antidepressants by non-specialist doctors (neurologists, therapists ...) due to other specifics of their preparation, the complexity of the scheme for the effect of drugs on the human psyche and, in general, the validity of the use of one or another antidepressant in a particular situation or need other psychotherapeutic methods .
Sometimes sexual function improves on its own with time as the body adjusts to antidepressants. And one of the easiest things to do is to adjust the dose of the medication [under the guidance of a doctor] – lower it, skip a dose, or take it later in the day.
Some antidepressants are more dangerous than others
Two classes of antidepressants are associated with the highest levels of sexual dysfunction.
The first group are selective serotonin reuptake inhibitors (SSRIs) - citalopram (Celexa), escitalopram (Lexapro), fluoxetine (Prozac), fluvoxamine (Luvox), paroxetine (Paxil) and sertraline (Zoloft). Paxil is considered the most problematic. In fact, it is considered a drug prescribed for premature ejaculation to increase the time to orgasm (ejaculation).
Paxil is considered the most problematic. In fact, it is considered a drug prescribed for premature ejaculation to increase the time to orgasm (ejaculation).
Second group - serotonin and norepinephrine reuptake inhibitors (SNRIs) - desvenlafaxine (Khedezla, Pristiq), duloxetine (Cymbalta), levomilnacipran (Fetzima), and venlafaxine (Effexor). nine0003
The newer antidepressants vilazodone (Viibryd) and vortioxetine (Trintellix) have been shown to have lower rates of sexual dysfunction than traditional SSRIs and SNRIs. Bupropion (Wellbutrin) and mirtazapine (Remeron) also have lower rates of sexual dysfunction.
If you are taking sedatives, this can play a role
Psychiatrists and psychotherapists have long known about sexual dysfunction when taking benzodiazepines used to treat anxiety, but to date there is no official data on how many men suffer from this disorder of sexual function or what is the probability of its occurrence. The most common side effect is erectile dysfunction .
The most common side effect is erectile dysfunction .
However, these drugs are only indicated for short-term use of 2-4 weeks, which reduces the chance of long-term sexual dysfunction.
Switching or adding drugs may have the desired effect
One option is to switch to another drug. An entire class of SSRIs can cause sexual dysfunction, and none of them has a very low risk. But Lexapro and Prozac seem to have the lowest risk among SSRIs.
The least problematic antidepressant is Wellbutrin. It does not affect the level of serotonin, does not cause sexual dysfunction. So taking the drug itself is not associated with the risk of sexual dysfunction. However, for some patients, this may simply not work for their anxiety, depression, or anxiety. nine0003
Sexual problems may persist after stopping medication
Some men may continue to have sexual problems after stopping antidepressants, and some may even experience problems such as premature ejaculation .