Am i having a depression relapse
Signs of Depression Relapse
1 / 13
When Depression Comes Back
Some people with major depression have symptoms only once in their life. Others have them again and again. Once you get treatment, it's important to pay attention to your feelings. That will help you catch possible signs of a relapse. Seek help quickly and you may be able to prevent a full-blown episode. Don't stop a treatment that works for you unless the doctor says it's OK.
Swipe to advance
2 / 13
More Than "Blue"
How can you tell depression from simple sadness? Are you down because of a specific event, like losing a job or a bad breakup? That could be normal, short-term sadness. But if you feel hopeless, teary, or "empty" every day for more than 2 weeks -- and it gets in the way of your daily life -- it may be clinical depression.
Swipe to advance
3 / 13
Isolation and Withdrawal
Do you avoid leaving the house? Does the shortest conversation feel like too much effort? Do you retreat to your room when family members try to draw you out? A strong social network is important. A loss of pleasure in activities can point to depression. Look for a support group. It can help to talk to other people who know what you're going through.
Swipe to advance
4 / 13
Sleep Changes
A shift in your habits like insomnia -- trouble falling or staying asleep -- could be a warning sign. A lack of shuteye can cause or worsen other symptoms linked to depression, like fatigue. Do you lie awake at night while your mind races? Or do you sleep too much because you don't want to get out of bed? Discuss it with your doctor. If your troubles are a symptom of depression relapse, medication and talk therapy may help.
If your troubles are a symptom of depression relapse, medication and talk therapy may help.
Swipe to advance
5 / 13
Irritability
Do little things flip you out? Do you fuss and fight with friends and family? Did your laid-back manner give way to fits of fury? Depression can show itself in irritability and anger. It makes it tough to handle everyday stresses. Men are more likely than women to behave recklessly and, sometimes, violently when depressed.
Swipe to advance
6 / 13
Can't Enjoy Sex, Fun, or Friends
This is a biggie. Activities you used to enjoy may now feel like a burden. If you've been depressed in the past and notice that you've lost feelings for your spouse or children, aren't interested in work, hobbies, or other favorite activities for more than 2 weeks, you might be relapsing.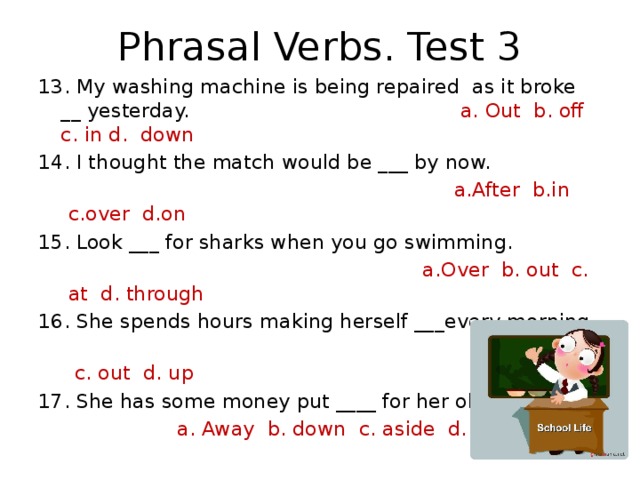 It's more likely if your symptoms come back within 6 months of an episode. Ask your doctor for help.
It's more likely if your symptoms come back within 6 months of an episode. Ask your doctor for help.
Swipe to advance
7 / 13
Feeling Worthless
Old feelings of self-loathing and guilt may creep back in. Or maybe you can't turn off the inner critic that wants to focus on your failures. You may feel you're to blame for events that are out of your control. Psychotherapy can help lift your low self-esteem and build up your strengths.
Swipe to advance
8 / 13
Chronic Aches and Pains
Do you have back pain even though you haven’t strained your back? Or how about chronic headaches and stomachaches? Unexplained chest pain or achy legs and arms? Depression can have physical symptoms, too. If your aches and pains don't get better with treatment, ask your doctor if depression could be to blame.
Swipe to advance
9 / 13
Sudden Weight Gain or Loss
Depression can change your relationship with food. You may forget it's time to eat. You might have to force yourself to have a meal. You could overeat or binge eat. If you've had depression, pay attention to strong changes in your appetite and weight.
Swipe to advance
10 / 13
Fatigue
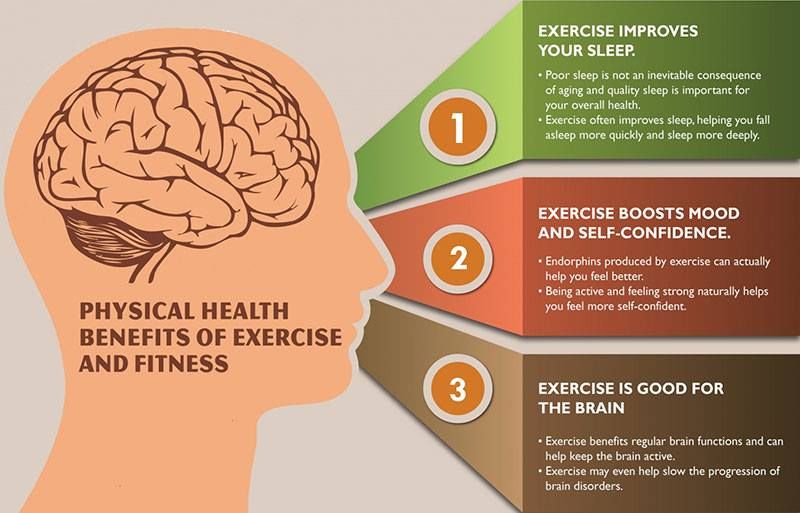
Do you have to drag yourself through the day? Depression can make you feel too tired or weak to wash the dishes -- or even get dressed. Not eating, or eating unhealthy food, can add to your fatigue. Good nutrition, exercise, and sleep can help you fight it.
Swipe to advance
11 / 13
Slowed-Down Thinking
Is your brain sluggish? Do you lose focus easily? Find it hard to concentrate? Have trouble remembering things? You might have problems making decisions -- as minor as what to wear in the morning or as major as problem-solving at work.
Swipe to advance
12 / 13
Suicidal Thoughts
This is a serious sign. It could mean you have severe depression. Some people think about suicide often. Others plan how to harm themselves. You're more likely to reach this point if you feel hopeless and you've lost interest in the things you once enjoyed. If you or someone you know has suicidal thoughts or talks about suicide, seek immediate help from a psychiatrist or other mental health professional.
Swipe to advance
13 / 13
What You Can Do
No two people with depression feel the same. If you have any of these warning signs or symptoms that concern you, talk to your regular doctor or a psychiatrist. They may suggest therapy or more medication to prevent a relapse. Cut your stress and do something every day that makes you feel good. You might need long-term treatment if you've had three or more depression episodes.
Swipe to advance
Up Next
Next Slideshow Title
Skip Ad
1 / 13
Skip Ad
Sources | Medically Reviewed on 12/17/2020 Reviewed by Smitha Bhandari, MD on December 17, 2020
IMAGES PROVIDED BY:
(1) Bass_nroll / Flikr
(2) Fuse
(3) Andy Ryan / Photonica
(4) Rosebud Pictures / Riser
(5) Rosebud Pictures / Riser
(6) Fuse
(7) DreamPictures / Photodisc
{8) Paul Bradbury / OJO Images
(9) STOCK4B
(10) Hill Street Studios / Workbook Stock
(11) Fat Chance Productions / Iconica
(12) Mike Powell / Digital Vision
(13) Ariel Skelley / The Image Bank
REFERENCES:
WebMD Medical Reference: "Depression Recovery: An Overview," "Sleep and Depression," "What Is Depression?" "Depression in Women," "Depression: Recognizing the Emotional Symptoms," "Depression in Men."
Centre for Addiction and Mental Health: "Recovery and Relapse Prevention."
Mayo Clinic: "Mental health: What's normal, what's not."
MedicineNet: "Sleep Disorders: Sleep and Depression," "Depression Symptoms in Men," "Depression," "Definition of Depression."
National Institute of Mental Health: "Symptoms of Depression and Mania."
American Academy of Family Physicians: "Depression in Women."
American Family Physician: "Depression and Sex Drive."
American College of Physicians.
Psychology Today: "Aches and Pains."
WebMD Health News: "Body Aches May Signal Depression."
Surgeon General: "Mental Health: A Report of the Surgeon General."
Debbara Dingman, PhD, clinical psychologist in private practice; adjunct faculty, Georgia State University; faculty, Pine River Psychotherapy Institute, Atlanta.
American Association of Suicidology: "Some Facts About Suicide and Depression."
American Congress of Obstetricians and Gynecologists: "Depression."
Journal of Clinical Psychiatry, 2007; vol 9: pp 214-223.
Centre for Addiction and Mental Health: "Understanding Depression."
Reviewed by Smitha Bhandari, MD on December 17, 2020
This tool does not provide medical advice. See additional information.
THIS TOOL DOES NOT PROVIDE MEDICAL ADVICE. It is intended for general informational purposes only and does not address individual circumstances. It is not a substitute for professional medical advice, diagnosis or treatment and should not be relied on to make decisions about your health. Never ignore professional medical advice in seeking treatment because of something you have read on the WebMD Site. If you think you may have a medical emergency, immediately call your doctor or dial 911.
SAMHSA’s National Helpline | SAMHSA
Your browser is not supported
Switch to Chrome, Edge, Firefox or Safari
Main page content
-
SAMHSA’s National Helpline is a free, confidential, 24/7, 365-day-a-year treatment referral and information service (in English and Spanish) for individuals and families facing mental and/or substance use disorders.
Also visit the online treatment locator.
SAMHSA’s National Helpline, 1-800-662-HELP (4357) (also known as the Treatment Referral Routing Service), or TTY: 1-800-487-4889 is a confidential, free, 24-hour-a-day, 365-day-a-year, information service, in English and Spanish, for individuals and family members facing mental and/or substance use disorders. This service provides referrals to local treatment facilities, support groups, and community-based organizations.
Also visit the online treatment locator, or send your zip code via text message: 435748 (HELP4U) to find help near you. Read more about the HELP4U text messaging service.
The service is open 24/7, 365 days a year.
English and Spanish are available if you select the option to speak with a national representative. Currently, the 435748 (HELP4U) text messaging service is only available in English.
Currently, the 435748 (HELP4U) text messaging service is only available in English.
In 2020, the Helpline received 833,598 calls. This is a 27 percent increase from 2019, when the Helpline received a total of 656,953 calls for the year.
The referral service is free of charge. If you have no insurance or are underinsured, we will refer you to your state office, which is responsible for state-funded treatment programs. In addition, we can often refer you to facilities that charge on a sliding fee scale or accept Medicare or Medicaid. If you have health insurance, you are encouraged to contact your insurer for a list of participating health care providers and facilities.
The service is confidential. We will not ask you for any personal information. We may ask for your zip code or other pertinent geographic information in order to track calls being routed to other offices or to accurately identify the local resources appropriate to your needs.
No, we do not provide counseling. Trained information specialists answer calls, transfer callers to state services or other appropriate intake centers in their states, and connect them with local assistance and support.
-
Suggested Resources
What Is Substance Abuse Treatment? A Booklet for Families
Created for family members of people with alcohol abuse or drug abuse problems. Answers questions about substance abuse, its symptoms, different types of treatment, and recovery. Addresses concerns of children of parents with substance use/abuse problems.It's Not Your Fault (NACoA) (PDF | 12 KB)
Assures teens with parents who abuse alcohol or drugs that, "It's not your fault!" and that they are not alone. Encourages teens to seek emotional support from other adults, school counselors, and youth support groups such as Alateen, and provides a resource list.After an Attempt: A Guide for Taking Care of Your Family Member After Treatment in the Emergency Department
Aids family members in coping with the aftermath of a relative's suicide attempt. Describes the emergency department treatment process, lists questions to ask about follow-up treatment, and describes how to reduce risk and ensure safety at home.
Describes the emergency department treatment process, lists questions to ask about follow-up treatment, and describes how to reduce risk and ensure safety at home.Family Therapy Can Help: For People in Recovery From Mental Illness or Addiction
Explores the role of family therapy in recovery from mental illness or substance abuse. Explains how family therapy sessions are run and who conducts them, describes a typical session, and provides information on its effectiveness in recovery.For additional resources, please visit the SAMHSA Store.
Last Updated: 08/30/2022
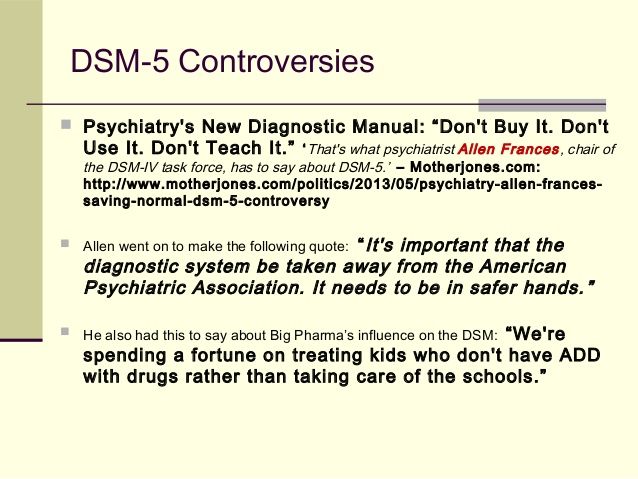
And again the same agony: 11 signs of the return of depression - Psychology
Personality
Trouble does not come alone! Mental problems are difficult to determine on your own, but everything is easier with depression - look for symptoms in our material unsplash.com
Depression is a widespread mental health problem that affects a person's ability to function in daily life. If you have experienced depression in the past, it is possible that the same condition will recur. Although treatment for depression, such as therapy with a psychologist or medication, works well, studies have also shown that about a third of people who stop treatment experience depression again within one year. nine0003
If you have experienced depression in the past, it is possible that the same condition will recur. Although treatment for depression, such as therapy with a psychologist or medication, works well, studies have also shown that about a third of people who stop treatment experience depression again within one year. nine0003
What is a relapse?
Relapse of depression refers to the recurrence of symptoms after achieving remission, a period of return to baseline functioning, usually lasting 16-20 weeks. While it is possible that those who relapse will experience the same symptoms as during their first depressive episode, it is also possible that the symptoms they experience will be completely different next time.
Signs of depression recurrence
For this reason, it is important to be aware of the various potential signs or symptoms of depression relapse. The following is a complete list of potential signs to look out for, and the following sections provide a detailed description of these signs and symptoms to help you determine if they are affecting you.
Bad mood
Irritability
Loss of interest or pleasure
Brain fog
Sleep changes
Social isolation
Feelings of worthlessness
Weight gain or loss
Tiredness
Pain
Suicidal thoughts
if your bad mood has no obvious cause, lasts more than 2 weeks and is present every day, you may be experiencing a relapse of depression
unsplash.com
Valid in Russia hotline of the center for emergency psychological assistance of the Ministry of Emergency Situations of Russia by phone - 8 (495) 989-50-50 (free of charge in Moscow). Call it if you feel mentally unstable or your loved one needs support, and you are afraid of harm. Also find out about other options: during the quarantine in Moscow, there is a volunteer psychological help line at 8 (800) 700-88-05. Additionally, you can get free consultations at a school, university, or get a referral from work - feel free to ask. Now back to the symptoms. nine0003
Bad mood
Feeling depressed, sad or in a bad mood is one of the hallmarks of depression and its relapse. Typical symptoms are tears, feelings of hopelessness, emptiness. These feelings are a normal reaction to obvious causes, such as the loss of a job, the loss of a loved one, a broken relationship, or a divorce. However, if your low mood has no apparent cause, lasts more than 2 weeks, and is present every day, you may be experiencing a relapse of depression. This is especially true if your bad mood or feelings of sadness are interfering with your daily life. For example, you may find it difficult to go to work because of bouts of crying, or you may feel that life will never get better. These are signs that a bad mood may indicate a relapse of depression. nine0003
Typical symptoms are tears, feelings of hopelessness, emptiness. These feelings are a normal reaction to obvious causes, such as the loss of a job, the loss of a loved one, a broken relationship, or a divorce. However, if your low mood has no apparent cause, lasts more than 2 weeks, and is present every day, you may be experiencing a relapse of depression. This is especially true if your bad mood or feelings of sadness are interfering with your daily life. For example, you may find it difficult to go to work because of bouts of crying, or you may feel that life will never get better. These are signs that a bad mood may indicate a relapse of depression. nine0003
Irritability
Do you find yourself getting irritated more easily than before? Yell at people or find yourself ready to even fight? If so, you may be experiencing irritability as a symptom of a relapse of depression. Most likely, you do not tolerate stressful situations well. This means that you tend to react with irritation or anger when faced with minor inconveniences. In other words, everything around you can annoy you and make you argue with others. nine0003
In other words, everything around you can annoy you and make you argue with others. nine0003
Loss of interest or pleasure
Another hallmark of a relapse of depression is a loss of interest in things you used to enjoy. It can be attraction to a partner, sex with him, hobbies, meeting friends, or anything that you used to enjoy.
Brain fog
Most people with depression experience something known as brain fog. Brain fog means slow thinking and loss of concentration. You may have trouble getting work done or even having a conversation. nine0003
Sleep changes
Sleep is another aspect of your health that can be easily affected during a relapse of depression. If you notice changes in your sleep, such as trouble falling asleep, waking up at night, not getting enough rest, or sleeping too much, then you may be experiencing a relapse of depression. Some people with depression find that as soon as their head hits the pillow, they begin to reflect on their day and what went wrong or stressed them out. This, in turn, can make it difficult to sleep and lead to insomnia. It can also increase fatigue and make it difficult to get out of bed in the morning. nine0003
This, in turn, can make it difficult to sleep and lead to insomnia. It can also increase fatigue and make it difficult to get out of bed in the morning. nine0003
Social isolation
If you avoid social situations or feel isolated or alone during social gatherings, you may be experiencing a relapse of depression. Social isolation can take a toll on your relationships, which in turn can make your depression worse. If striking up a conversation seems like too much effort, leaving the house is an impossible feat, or you're just hanging out in your room much more than is considered acceptable behavior, then you may have social problems. This sign may be associated with a loss of pleasure, as you do not experience any pleasure from interacting with other people. nine0003
Feelings of worthlessness
If you feel that you have low self-esteem, that you do not deserve or deserve better things in life, or that you are generally overly critical of yourself, then feeling worthless may indicate a relapse of depression. This problem can also be associated with feelings of guilt, focusing on one's shortcomings or failures instead of positive achievements, and excessive internal criticism. If you constantly blame yourself for something bad, your inner critic and self-hatred may be a sign of a larger problem, including a relapse of depression. nine0003
This problem can also be associated with feelings of guilt, focusing on one's shortcomings or failures instead of positive achievements, and excessive internal criticism. If you constantly blame yourself for something bad, your inner critic and self-hatred may be a sign of a larger problem, including a relapse of depression. nine0003
Weight gain or loss
Sudden changes in weight, such as weight loss or weight gain, may indicate a relapse of depression. Other signs may be a loss of interest in foods you once loved, or a lack of effort for healthy eating or regular exercise. People who struggle with weight gain or weight loss due to a relapse of depression may also overeat or overeat with other eating disorders. If you notice that your eating habits or weight have changed, this may be a sign that depression is returning. nine0003
Tired
Are you tired of just thinking about getting out of bed, doing the dishes or paying the bills? When you feel tired, you may feel like things are getting a lot more difficult. For example, a chore such as folding clothes becomes an overwhelming task that you simply cannot complete quickly. If you notice yourself being lazy all day, fatigue may be a sign that depression is returning.
For example, a chore such as folding clothes becomes an overwhelming task that you simply cannot complete quickly. If you notice yourself being lazy all day, fatigue may be a sign that depression is returning.
Pain
Depression is experienced not only in the mind. Some people also notice that their aches and pains increase when they show signs of depression. These pains can take many forms and travel throughout the body. The following are some of the types of pain that can occur with a relapse of depression:
Muscle pain
Headaches
Stomach pain
Chest pain
Back pain
Pain in limbs (such as in the legs or arms)
Social isolation can be negatively affected on your relationship, which in turn can exacerbate your depression
unsplash.com
Suicidal thoughts
Finally, suicidal thoughts are a sure sign that you have severe depression. If so, then your depression has returned. In the case of severe depression, you have probably also lost interest in things you used to enjoy. You may also feel hopeless about your position in the world. All this indicates a relapse of depression.
In the case of severe depression, you have probably also lost interest in things you used to enjoy. You may also feel hopeless about your position in the world. All this indicates a relapse of depression.
Causes of Depression Recurrence
If you are experiencing a depression relapse, you may be wondering why your depression returned. It is true that depression can return at any time, even if you are on medication or in treatment. She may also return without any obvious external triggers or stressors. However, sometimes a relapse of depression follows an external event. The following are some possible triggers or causes for depression relapse. nine0003
Experiencing the death of a loved one or other significant loss
Experiencing a stressful life event (e.g., being fired from a job, divorce, having your first child, preparing for final school exams)
Hormonal changes related to a stage in your life (e.g., puberty, pregnancy, menopause)
Failure to use or discontinuing coping strategies (eg, journaling, regular exercise, managing negative thoughts)
Changes in medications you are taking
Sleep disturbances (eg starting a new job that requires a change in sleep pattern)
Seek medical attention if you have more than three symptoms. Please don't let this disease run its course. Subscribe to our Yandex.Zen channel0003
Please don't let this disease run its course. Subscribe to our Yandex.Zen channel0003
Vasilisa Volodina: “The hottest week of the month is ahead”
A popular astrologer made a forecast from January 16 to 22, 2023
Ani Lorak showed a video with a new man
Philip Kirkorov “blessed” the couple in a bold bikini: “The breast implant sticks out”
The artist enjoys her vacation in Dubai
10 phrases that betray self-doubt
Actor Semyon Yakubov advises you to pay attention to whether these expressions are in your vocabulary
Focus on positive: how to stop winding yourself up
WomanHit.ru will tell you several ways that will disperse negative thoughts
Okhlobystin said that Smolyaninov * severely beat his ex-wife Artur
Who is the last one: what disorders do residents of a big city most often face
What price do we pay for professional success
4 “bells” that you are on the verge of a nervous breakdown
Our psyche can bring an unpleasant surprise
Artistry and emancipation: how to develop these qualities in a child
Singer Alex Anokhin will share his advice on how a child can learn to overcome excitement, be liberated on stage and show artistry, singer Alex Anokhin will share with the parents of future artists
Passed away actor from "Molodezhka" and "Method" Dmitry Sidorov
Celebrity was 52 years old
How to captivate a child with music (and why this should be done)
Theater and film actor Semyon Yakubov, who also teaches acting at a children's creative studio, gave practical advice from personal experience world of show business - in a new video review WomanHit. ru
ru
How dental infections imperceptibly destroy our teeth
Dentist Vladimir Losev, Candidate of Medical Sciences, tells how to understand that you need specialist help
Beauty trends 2023: what procedures you should pay attention to in the new year
Face harmonization will remain one of the main trends in the field of care. was pregnant
The last photo of the traveler, which she took on board the plane, has been preserved
Prints, total bow and quilted furniture: studying the trendy interior of the coming year
Designer and architect Alexander Osipov — about which trends are becoming obsolete this year and will be considered completely obsolete in 2023
how to recognize and how to cope with a depressive disorder
06/25/2021
During the period of remission, when treatment is left behind, patients with cancer diagnosis, as well as their loved ones, may experience depression. Clinical psychologist Svetlana Malysheva told Profilaktika Media about why a depressive state occurs at a time when the disease has receded, and how to help a loved one cope with it. nine0003
Clinical psychologist Svetlana Malysheva told Profilaktika Media about why a depressive state occurs at a time when the disease has receded, and how to help a loved one cope with it. nine0003
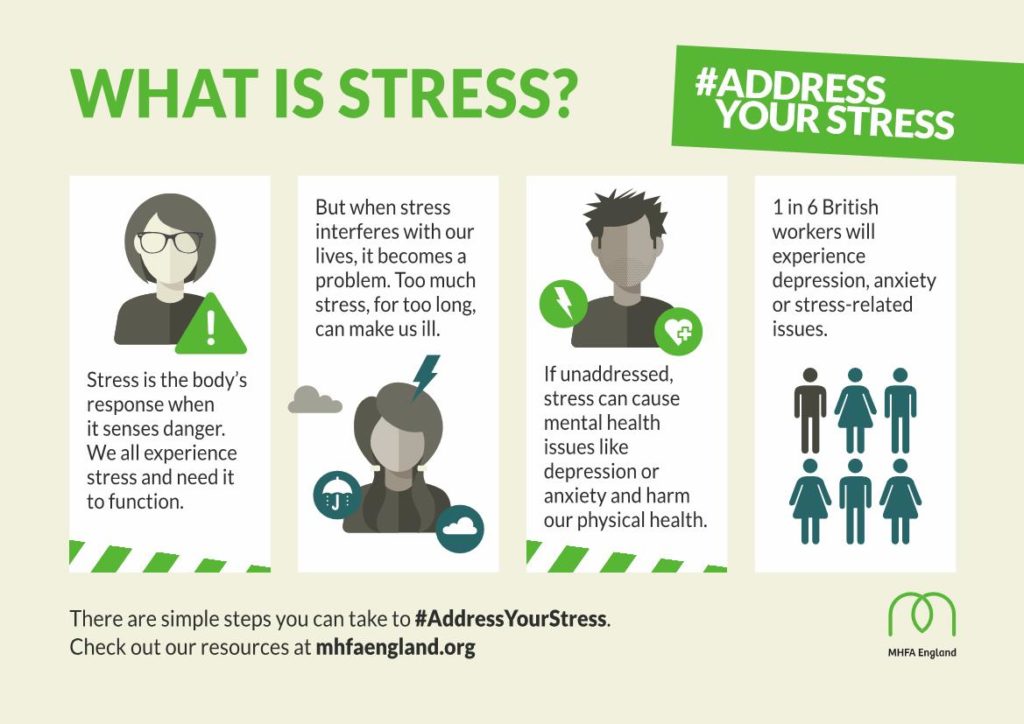
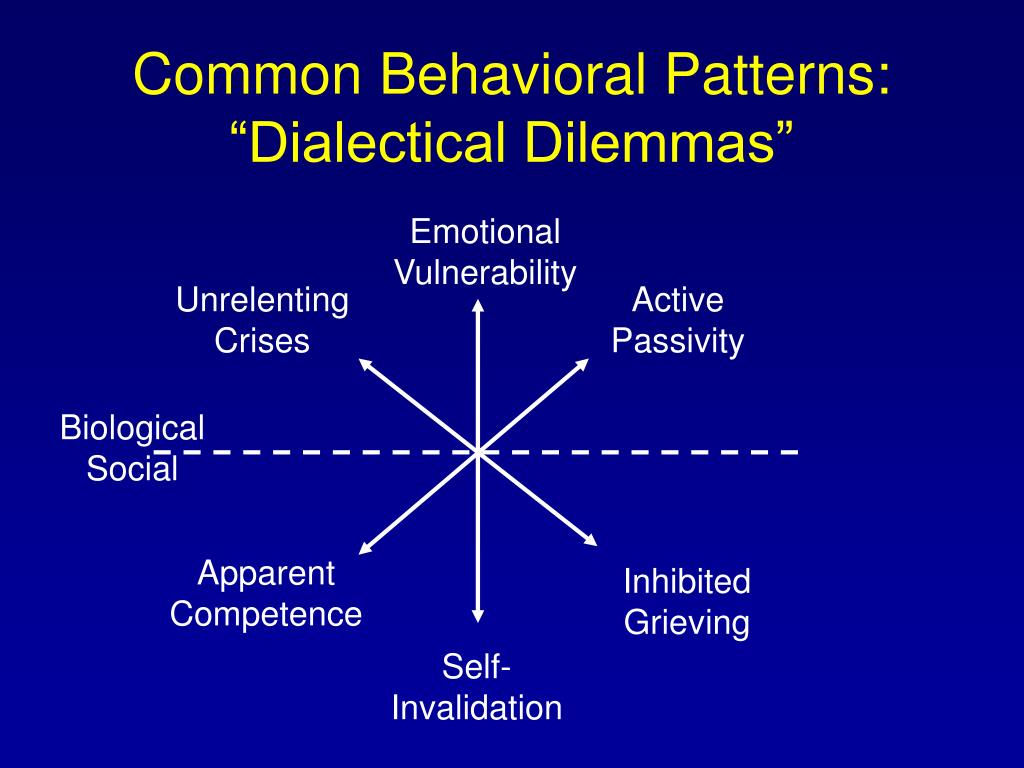
SYMPTOMS AND CAUSES OF DEPRESSION
What symptoms are red flags and signs of depression in patients in remission?
Depression is the most common disorder in the modern world, it has many nuances and many faces. However, signs of depression are universal and do not directly relate to a cancer diagnosis. We usually evaluate a person's emotional state according to two important criteria: the first is the duration of the symptoms and the second is how strong they are. It is very important - how long, and how hard. We can talk about symptoms of depression if a person has a reduced mood background for more than two weeks (regardless of the time of day or events), when appetite decreases or increases, sleep patterns change, when a person suddenly loses interest in things that used to bring him pleasure. We can also observe mental retardation, when a person is not able to concentrate on anything, it is difficult to remember information, he builds phrases poorly, he exhibits motor retardation or, conversely, hyperexcitability. Such patients often feel worthless, level the significance of themselves and their past experience, feel the futility of the future and powerlessness to do anything about it. Another very important point - the expression of suicidal thoughts - can also mean that a person has experienced a depressive disorder. nine0003
We can also observe mental retardation, when a person is not able to concentrate on anything, it is difficult to remember information, he builds phrases poorly, he exhibits motor retardation or, conversely, hyperexcitability. Such patients often feel worthless, level the significance of themselves and their past experience, feel the futility of the future and powerlessness to do anything about it. Another very important point - the expression of suicidal thoughts - can also mean that a person has experienced a depressive disorder. nine0003
What are the main causes of depression in patients in remission?
There are several options. The first is that the person had depression before the illness. If a person had a depressive episode before a cancer diagnosis, then such a traumatic event as an oncological diagnosis, a crisis stage in life, significantly increases the likelihood of depression. Another option is post-traumatic stress disorder: a person has completed treatment, but he is unable to return to normal life. This is not a well-developed stress reaction at the moment when experiences come with a delay in time - even after the end of treatment, a person travels around the oncology center for a kilometer, he has dreams, it seems to him that he smells either chemistry or some drugs, and the person begins to literally shake. All this can also lead to depressive symptoms. nine0003
This is not a well-developed stress reaction at the moment when experiences come with a delay in time - even after the end of treatment, a person travels around the oncology center for a kilometer, he has dreams, it seems to him that he smells either chemistry or some drugs, and the person begins to literally shake. All this can also lead to depressive symptoms. nine0003
Why does a person in remission get depressed? Most often at first it is a manifestation of anxiety disorders: almost all patients who have completed treatment live with the fear of relapse. Constant anxiety about the future, fear of uncertainty, a feeling of being unable to control one’s life, fixation on any symptoms are exhausting, take strength and energy, and eventually turn into a lowered mood background, which also affects somatics. In such patients, the head, back, and neck may actually hurt. A person thinks that this is a disease, and something urgently needs to be done, he cannot relax. However, it turns out that this is a masked depression, and in fact there is simply no organic reason to confirm that the disease has returned.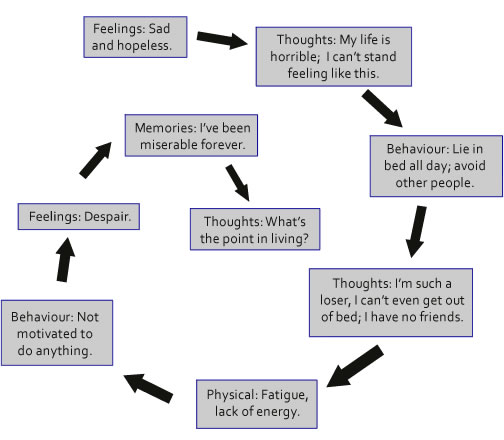 nine0003
nine0003
In addition, after completing treatment, a person is faced with the "Gulliver's syndrome": he lived through a serious crisis, but loved ones can be very far from him emotionally. “How can they understand me, they weren’t near death on the edge?!”, the man thinks. And all the past values that existed before the illness seem irrelevant to him. And what is relevant, a person no longer knows, and this also provokes apathy. It seems that the person has been treated, but the quality of life is declining, and he cannot get ready. nine0003
It is important to remember that depression is a disease that needs to be treated. There are only 2-3% of endogenous depressions caused by a “breakdown” inside the body. All other depressions are the result of stress.
What is the danger of depression during remission?
The biggest risk is suicidal. Between 40 and 60% of suicide attempts in the world are committed by people diagnosed with depression. A person with depression is 35 times more likely to commit suicide than anyone else. Every 6th person with depression in the world commits suicide. These are very high risks! nine0003
Every 6th person with depression in the world commits suicide. These are very high risks! nine0003
Clinical psychologist Svetlana Malysheva
WAYS TO GET OUT OF THE SITUATION
Where can a depressed person look for sources of positive emotions? Are there specific methods, tips, recommendations?
I very often hear even from healthy people the phrase - “Something I'm depressed!”. Unfortunately, the idea that we should not experience unpleasant emotions, we should not be sad, suffer, worry, worry, and should not be afraid has taken root in our society. Rejoice and think positive! Unfortunately, this is very neurotic. Feeling positive emotions all the time is not normal! This is a different diagnosis! A person who has gone through a cancer diagnosis is really scared, and we cannot discount such emotions. However, society's intolerance to difficult emotions creates an atmosphere in which "you have to be peppy." Often this does not happen because loved ones are impatient with the person's condition - they are also scared, they do not know how to cope with it and do not leave the person who has gone through the diagnosis with space to respond.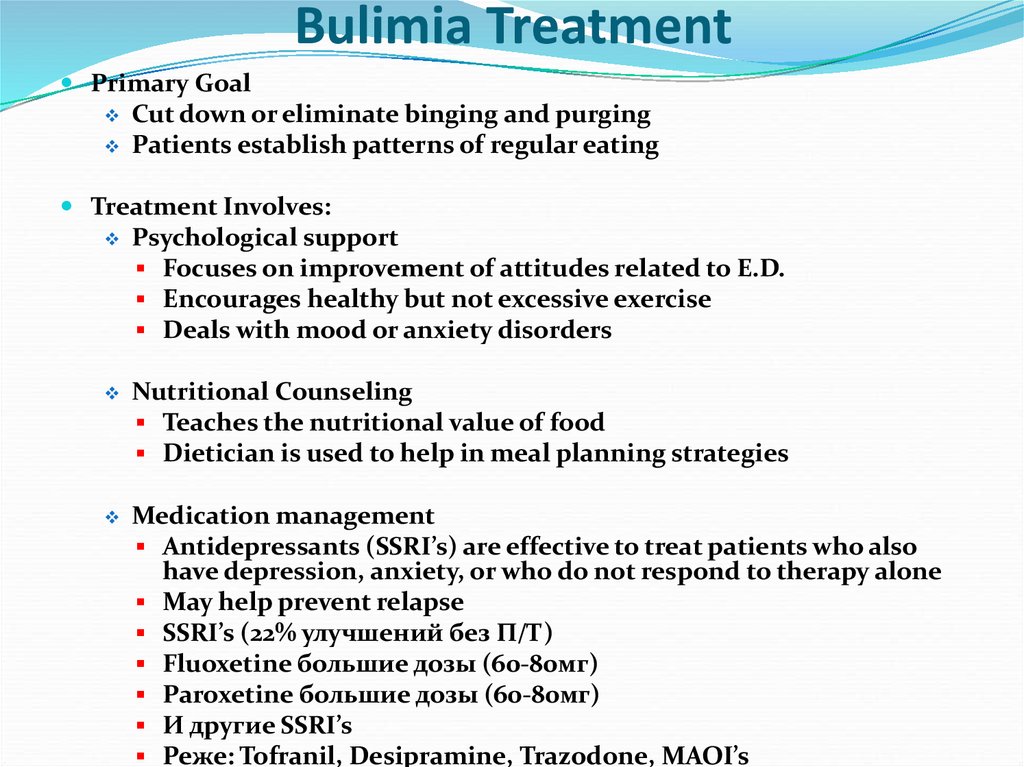 However, sometimes people are in a hurry to identify depression in themselves, because there is a certain requirement for themselves and society - to think positively, to experience only background joy. This is a distorted understanding of reality. It is worth training tolerance for different emotions in your life, recognizing - "I can be afraid, anxious, sad, I should not be joyful all the time, because it's strange." Then, even in the case of an abnormal decrease in mood, a person will have a clearer understanding that something is wrong, that he lacks strength - neither physical nor moral, nothing pleases him, and he needs to seek help, recognizing that depression - it's a disease! Not a weakness, not a “lack of pumping”, not a lack of personal growth, as coaches like to say. Depression is about a disease! nine0003
However, sometimes people are in a hurry to identify depression in themselves, because there is a certain requirement for themselves and society - to think positively, to experience only background joy. This is a distorted understanding of reality. It is worth training tolerance for different emotions in your life, recognizing - "I can be afraid, anxious, sad, I should not be joyful all the time, because it's strange." Then, even in the case of an abnormal decrease in mood, a person will have a clearer understanding that something is wrong, that he lacks strength - neither physical nor moral, nothing pleases him, and he needs to seek help, recognizing that depression - it's a disease! Not a weakness, not a “lack of pumping”, not a lack of personal growth, as coaches like to say. Depression is about a disease! nine0003
How should relatives and friends behave? How to help a person in remission cope with depression?
The diagnosis comes to a family that has already lived somehow before, and there are already some family relationships.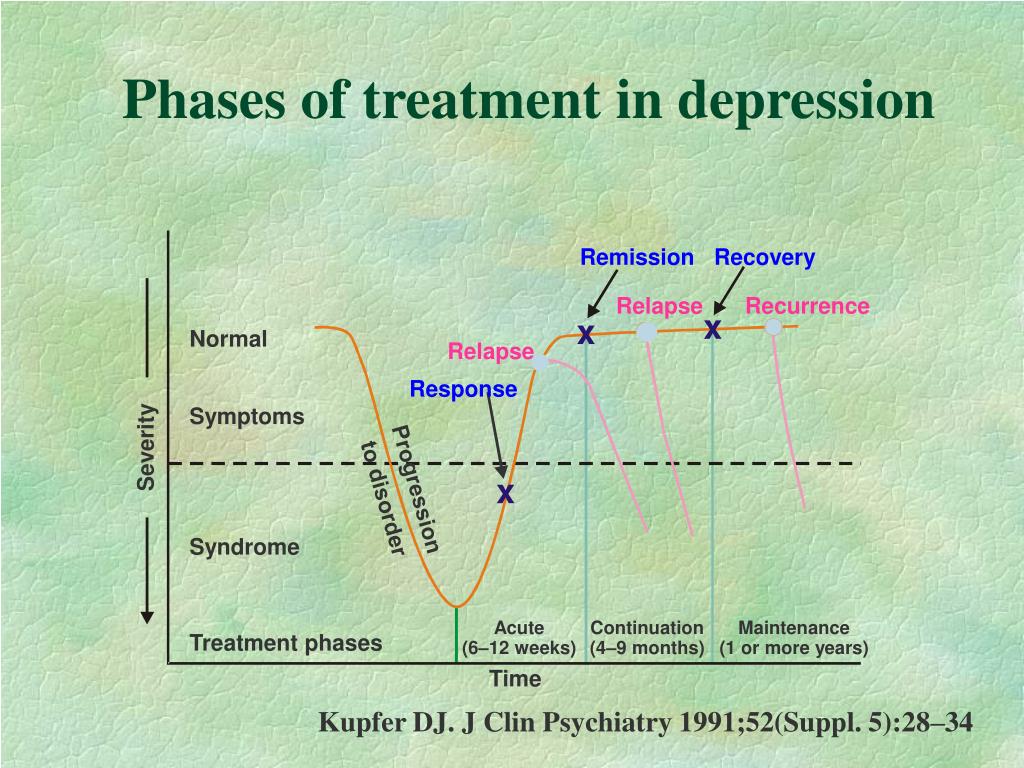 It's great if they are close - then it will be easier for the patient's relative to find the words, and the loved one will hear them sooner.
It's great if they are close - then it will be easier for the patient's relative to find the words, and the loved one will hear them sooner.
Often relatives, of course, do not notice that what is happening to their loved one is a pathology, and they can explain this by fatigue, a change in character due to treatment, and they can also get tired themselves. Therefore, the rehabilitation of the family where there is a cancer patient is very important, even if he has completed treatment and is going to recover. Planned rehabilitation is needed, because not only the person himself, but the whole family has passed this diagnosis. At the same time, close people may simply not be ready to talk about these things, but this does not mean that they cannot help. We can listen and give space to a person to react when we do not try to slow him down with the words “hold on, fight, everything will pass, live, look at others!”. In fact, even if you are just listening, you are already helping, and this is a hundred times better than the words “fight, pull yourself together, move forward” said out of inner fear.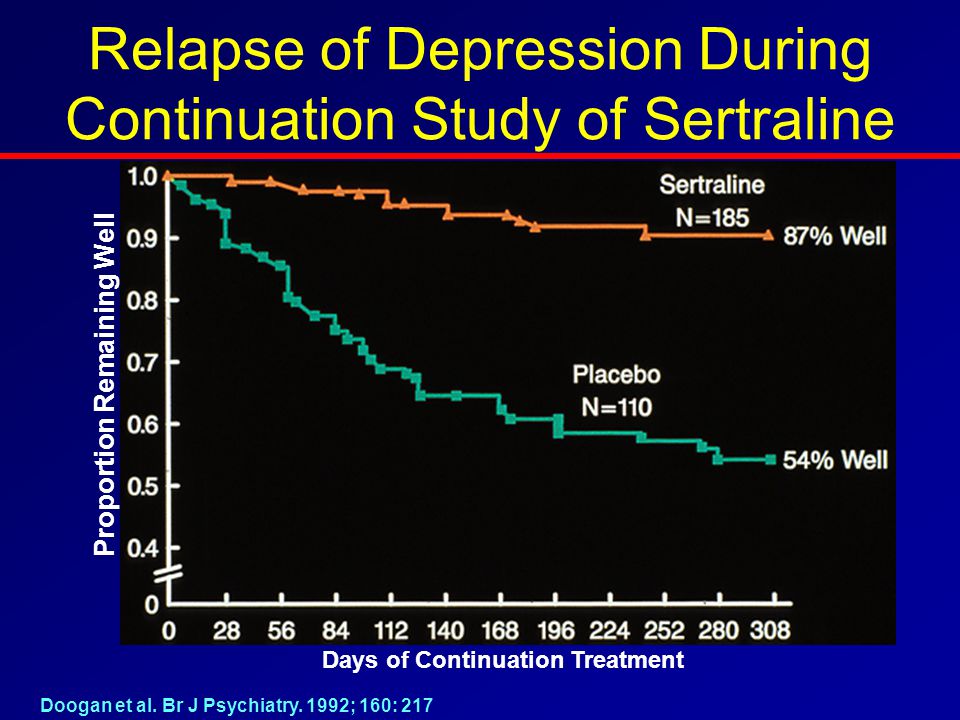 In my experience, people don't like to be told "hold on!". It is more correct to say: “I am, I am here, I will be there. I can just sit and be silent. Sometimes it is very appreciated when a person can just be there. This is already a lot! When he does not devalue the emotions of a loved one, but simply shares them. nine0003
In my experience, people don't like to be told "hold on!". It is more correct to say: “I am, I am here, I will be there. I can just sit and be silent. Sometimes it is very appreciated when a person can just be there. This is already a lot! When he does not devalue the emotions of a loved one, but simply shares them. nine0003
How to act if the person himself is not aware of the problem and believes that he is only in a bad mood?
It is always very significant for me when close people are not indifferent, but we cannot always catch up and help - a person must want this himself. A person can suffer, experience certain difficult emotions, but this does not mean that he is ready to do something with this suffering. Sometimes the fears of relatives manifest themselves in certain expectations of how their loved one should behave: “I’m so worried about you, suddenly something is wrong with you, or I don’t finish something and feel bad, and then it seems to me that you have to live somehow differently so that I can be calm. This means that a person is not indifferent and takes care of his loved ones, but these are our expectations. If a relative feels that something is wrong with his loved one in remission or at the stage of undergoing treatment, it is worth asking for help from a clinical psychologist, first of all, the relative himself, and not the patient! This may be an indication that a relative is not coping, and this is normal, because he cannot take care of himself now. “How can I take care of myself when my loved one is sick?! Am I an egoist?” the man thinks. Even when relatives ask to work with their loved one, we always start with the relative. And then it turns out that a dialogue is built between relatives, and immediately the process goes on for the family, in general, much more efficiently. nine0003
This means that a person is not indifferent and takes care of his loved ones, but these are our expectations. If a relative feels that something is wrong with his loved one in remission or at the stage of undergoing treatment, it is worth asking for help from a clinical psychologist, first of all, the relative himself, and not the patient! This may be an indication that a relative is not coping, and this is normal, because he cannot take care of himself now. “How can I take care of myself when my loved one is sick?! Am I an egoist?” the man thinks. Even when relatives ask to work with their loved one, we always start with the relative. And then it turns out that a dialogue is built between relatives, and immediately the process goes on for the family, in general, much more efficiently. nine0003
The helper also needs help, because psychological defenses protect the sick person himself: it is his plane that has lost control, and we, relatives, are watching this plane. Our psychological defense does not work like that, and we are more prone to secondary traumatization. For relatives of the patient, this is exactly the same psychotrauma as for a person with an oncological diagnosis. This is a family problem, this is a crisis and extreme situation (how to get into a flood) with a threat to life, with uncertainty, at the limit of human capabilities. nine0003
For relatives of the patient, this is exactly the same psychotrauma as for a person with an oncological diagnosis. This is a family problem, this is a crisis and extreme situation (how to get into a flood) with a threat to life, with uncertainty, at the limit of human capabilities. nine0003
WHERE TO GET HELP
How to find a specialist who works with such patients? How to understand that this is your specialist, and how to formulate a request?
First of all, it must be a certified specialist. Do not be afraid to ask if he has a basic psychological education, what training he has undergone, whether he understands how the brain works, in what approach, what problems he can work with. It is important! If you feel that your loved one has or suspects a depressive disorder, you need a specialist who has a basic psychological education. It is best if this is a psychotherapist who is trained in working with depressive episodes. You can request qualifications, documents. Coming to a specialist, a person himself understands what he does not like, and he begins to speak as it is - no additional preparation is needed here. And already to form a specific request with which you need to work, and to find out the criteria is the task of a specialist. For example, if these are tension headaches, then we will work with anxiety, we will scale it, we will agree that our target is anxiety. How do we know it's working? There will be many criteria, and a person will notice changes both in sensations and in real life. It does not matter in which paradigm the specialist works. The most important thing is a psychotherapeutic contact, when you can say everything that worries you right during therapy, even if some of this is directed to the specialist himself. Talk about everything, even if it's "I don't think therapy is working" or "You're pushing me." This is very important information for a psychotherapist! nine0003
Coming to a specialist, a person himself understands what he does not like, and he begins to speak as it is - no additional preparation is needed here. And already to form a specific request with which you need to work, and to find out the criteria is the task of a specialist. For example, if these are tension headaches, then we will work with anxiety, we will scale it, we will agree that our target is anxiety. How do we know it's working? There will be many criteria, and a person will notice changes both in sensations and in real life. It does not matter in which paradigm the specialist works. The most important thing is a psychotherapeutic contact, when you can say everything that worries you right during therapy, even if some of this is directed to the specialist himself. Talk about everything, even if it's "I don't think therapy is working" or "You're pushing me." This is very important information for a psychotherapist! nine0003
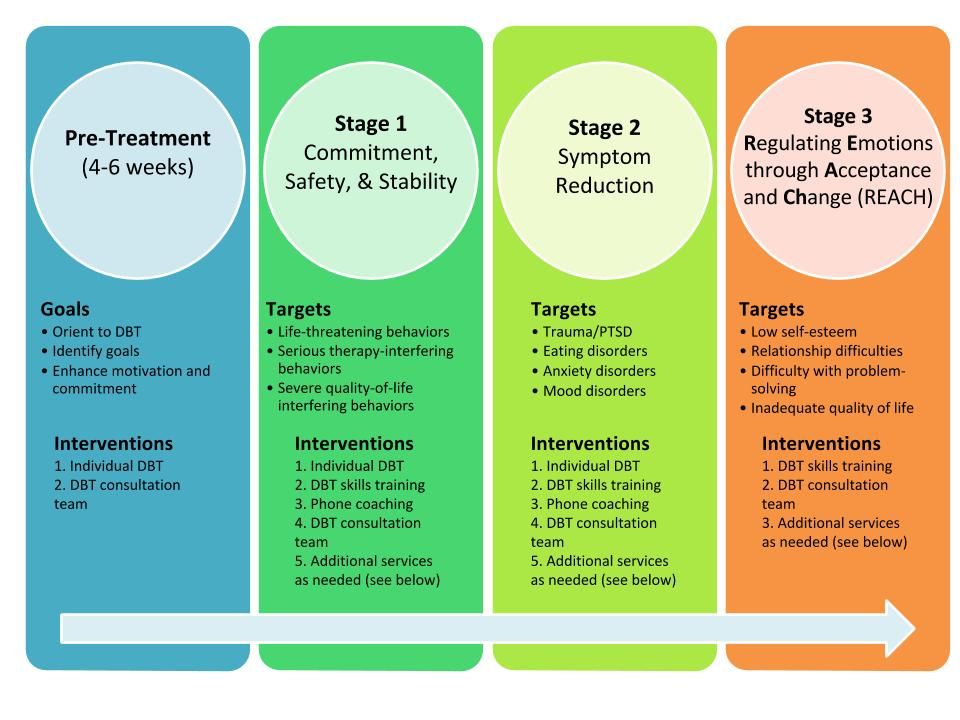
In which cases of depression is it necessary to include drug therapy?
With mild to moderate depression, we can cope with psychotherapeutic methods. In a severe course of a depressive disorder, with a suicidal risk, of course, it is worth connecting drug therapy. It is very important to contact competent specialists! With depression, a person's activity is reduced, he thinks about the meaninglessness of life, engages in self-flagellation, self-accusation, and drugs prescribed for depressive disorders create a physical feeling that strength and energy have returned. Energy appears, but emotionally a person is still extremely vulnerable, and the largest percentage of suicides occurs at this very moment. Here we need a very precise work of a psychiatrist, a psychotherapist. Cognitive-behavioral therapy has shown the world's best results in working with depression - no worse than medication. However, I often refer patients for consultation with a psychotherapist or psychiatrist. And either the psychotherapist leads the patient himself, or he draws up his conclusion, prescribes drugs, and the patient and I continue to work with psychotherapeutic methods.
In a severe course of a depressive disorder, with a suicidal risk, of course, it is worth connecting drug therapy. It is very important to contact competent specialists! With depression, a person's activity is reduced, he thinks about the meaninglessness of life, engages in self-flagellation, self-accusation, and drugs prescribed for depressive disorders create a physical feeling that strength and energy have returned. Energy appears, but emotionally a person is still extremely vulnerable, and the largest percentage of suicides occurs at this very moment. Here we need a very precise work of a psychiatrist, a psychotherapist. Cognitive-behavioral therapy has shown the world's best results in working with depression - no worse than medication. However, I often refer patients for consultation with a psychotherapist or psychiatrist. And either the psychotherapist leads the patient himself, or he draws up his conclusion, prescribes drugs, and the patient and I continue to work with psychotherapeutic methods.