Kyleena mood swings
What They are and How to Get Rid – Even
Since the development of the birth control pill in 1960, women have had a growing number of options for hormonal contraception. One of the more recent innovations is the development of intrauterine devices, or IUDs, which are designed to offer women long term control over their fertility.
Instead of having to remember to take a pill each day, remember to buy and use condoms, or regularly replace patches or rings, women can choose to have an IUD placed in their uterus and receive contraceptive protection that is more than 99 percent effective.
Hormonal IUDs like Kyleena can effectively prevent pregnancy for up to five years, but they may also cause unpleasant side effects that can be difficult to manage. Fortunately, it may be possible to avoid the side effects of Kyleena or get rid of them entirely.
What is Kyleena?
Kyleena is a brand name IUD that releases a type of progestin hormone called levonorgestrel. Similar to other IUDs, Kyleena is shaped like a T and is a small, flexible device that can be placed inside the uterus for the prevention of pregnancy.
The U.S. Food and Drug Administration (FDA) approved Kyleena for use in the United States in 2000, and it has grown in popularity over the past two decades.
Kyleena is put in place by a trained medical professional during an office visit, and no surgery is required for placement. Kyleena can prevent pregnancy for up to five years, but there are other reasons why women use Kyleena.
Why do women use Kyleena?
Although Kyleena is first and foremost a type of hormonal contraceptive, there are other reasons why women use Kyleena. Kyleena can be used for the long term prevention of pregnancy (up to five years), but it can also help women with heavy periods reduce the flow and pain associated with menstruation.
Some women who use Kyleena eventually stop having periods at all during the time that the IUD is in place. Kyleena is one of the most effective forms of birth control; like other IUDs, it is more than 99 percent effective at preventing pregnancy.
Kyleena is one of the most effective forms of birth control; like other IUDs, it is more than 99 percent effective at preventing pregnancy.
Kyleena does not function as an emergency contraceptive and cannot prevent against infection of sexually transmitted diseases, including HIV.
How does Kyleena work?
Kyleena is a hormonal IUD that works by releasing small amounts of levonorgestrel, a type of progestin hormone, into the uterus. Unlike combination birth control, which includes both progestin and estrogen hormones, Kyleena does not contain any form of estrogen.
While the device releases progestin locally with the intent of impacting the female reproductive system, the effects on the body are systemic. This is because the hormones released by Kyleena interact with estrogen, androgen, glucocorticoid, and mineralocorticoid receptors in the brain.
Each of these receptors plays an important role in a number of processes occurring within the body, including mood, immune function, and cognition. It is because of the impact of these hormones on the body’s processes that long term use of hormonal contraceptives is linked to an increased risk of breast cancer and cardiovascular disease.
It is because of the impact of these hormones on the body’s processes that long term use of hormonal contraceptives is linked to an increased risk of breast cancer and cardiovascular disease.
Devices like Kyleena are believed to work in three ways to prevent pregnancy:
- Inhibits sperm from reaching or fertilizing the egg
- Thickens cervical mucus to prevent sperm from entering the uterus
- Thins the uterine lining to prevent implantation
Kyleena is more than 99 percent effective at preventing pregnancy, and for some women, it can also help to reduce the flow of heavy menstrual periods by thinning the lining of the uterus.
However, while there are many benefits to taking Kyleena, some women experience unpleasant symptoms while using the device. The hormones contained in Kyleena impact the hypothalamic-pituitary-adrenal (HPA) axis, which plays an important role in the body’s response to stressful life events.
When the HPA axis becomes dysregulated, women are more likely to experience immune system disorders, memory impairment, obesity, and cardiometabolic disorders.
What side effects are associated with Kyleena?
Hormonal IUDs like Kyleena do have some side effects, including both common and serious side effects. Some women may find certain side effects, such as reduced pain during menstrual periods, beneficial depending on how their body responds to the medication, while others do not.
Common side effects associated with Kyleena include:
- Yeast infection of the vagina and vulva
- Bacterial vaginosis, an infection of the vagina
- Vomiting
- Acne
- Nausea
- Vulvovaginitis, an inflammation or infection of the vagina or vulva
- Abnormally long or heavy periods (can be severe)
- Bleeding not related to menstrual period (can be severe)
- Absence of menstrual periods (can be prolonged)
Other side effects are experienced less frequently and may require medical attention, depending on their severity and the length of time for which they are experienced:
- Decrease in the frequency of menstruation
- Change in libido
- Backache
- Hormone-induced hot flashes
- Headache
- Inflammation of the cervix
- Itching
- Nervousness
- Pelvic pain
- Weight gain
- Eczema, a skin condition associated with itching and redness
- Ovarian cysts
- Breast pain or tenderness
- Hair loss
- Hair growth on parts of the body that normally do not have hair
- Intense abdominal pain
- Mood changes
- Pain with menstruation
- Vaginal discharge
- Skin rash
- Depression
- Anemia
- Enlargement of the ovaries
- Swelling of the abdomen
- Uterine cramps
- Visible water retention
- Decrease in the production of breast milk
- Hives
- Darkening of the skin
- Pain with sexual intercourse
Other side effects of Kyleena are more serious and require immediate medical attention. If you experience any of the following issues, seek medical attention right away:
If you experience any of the following issues, seek medical attention right away:
- Blood clot in an artery
- Blood clot in the lung
- Stroke
- Angioedema, a type of allergic reaction
- Pelvic Inflammatory Disease, an infection of the female reproductive organs
- Blood clot in a deep vein of the extremities
- Expulsion of the IUD
- Pregnancy occurring outside of the womb
- Blood infection of Group A streptococcus bacteria
- Migraine headache
- Sepsis caused by a bacterial infection
- Infection by actinomyces bacteria
- Blood clot in the veins
- Breast cancer
- High blood pressure
- Puncture of the uterus by the IUD
How can you get rid of the side effects associated with Kyleena?
While some women using Kyleena will experience very few side effects, others may experience a variety of unpleasant symptoms that make the device nearly intolerable.
It is believed that hormonal forms of contraception like the Kyleena IUD cause certain side effects because of interactions between the hormones and nutrients in the body, which cause a shift in biochemistry.
As nutrients are depleted, women experience imbalances in the body and undesirable symptoms. The World Health Organization (WHO) has established that hormonal contraceptives like Kyleena can cause depletions of vitamins and minerals like folic acid, vitamins B2, B6, B12, C, and E, as well as magnesium, selenium, and zinc.
Fortunately, it is possible to avoid certain side effects of Kyleena with nutrient support. Managing your unique biochemistry is a balancing act, and women have different nutritional needs while using hormonal contraceptives like Kyleena.
When provided with therapeutic doses of certain vitamins, minerals, and mitochondrial antioxidants, side effects including low sex drive, weight gain, mood swings, headaches, and fatigue are less likely to occur.
Dietary supplements that address these unique needs, such as Even, can provide nutritional support and minimize the potential side effects associated with Kyleena.
Sources
https://www.kyleena-us.com/safety/
https://www.drugs.com/mtm/kyleena.html
https://www.webmd.com/drugs/2/drug-172655/kyleena-intrauterine/details/list-sideeffects
https://www.plannedparenthood.org/learn/birth-control/iud
https://pubmed.ncbi.nlm.nih.gov/23852908/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5815295/
https://www.theatlantic.com/health/archive/2012/01/how-progestin-a-synthetic-female-hormone-could-affect-the-brain/251299/
Kyleena - Uses, Side Effects, Interactions
How does this medication work? What will it do for me?
This is an intrauterine device (IUD): a soft, flexible T-shaped contraceptive (birth control) device that is placed inside the uterus. It releases the medication levonorgestrel continuously over a period of 5 years to prevent pregnancy.
Levonorgestrel is a progestin, which is a hormone produced by the ovaries. This medication prevents the lining of the uterus (endometrium) from building up, which makes it very difficult for an egg to be implanted. It also changes the cervical mucus, making it harder for sperm to swim through the cervix.
Levonorgestrel IUD starts to work as soon as it is inserted. However, it is advised to wait 24 to 48 hours before having sexual intercourse.
This medication may be available under multiple brand names and/or in several different forms. Any specific brand name of this medication may not be available in all of the forms or approved for all of the conditions discussed here. As well, some forms of this medication may not be used for all of the conditions discussed here.
Your doctor may have suggested this medication for conditions other than those listed in these drug information articles. If you have not discussed this with your doctor or are not sure why you are taking this medication, speak to your doctor. Do not stop taking this medication without consulting your doctor.
Do not stop taking this medication without consulting your doctor.
Do not give this medication to anyone else, even if they have the same symptoms as you do. It can be harmful for people to take this medication if their doctor has not prescribed it.
What form(s) does this medication come in?
Kyleena® consists of a small, white, T-shaped body made from soft, flexible plastic. The vertical and horizontal arms of the T-body are about 3 cm long. The vertical arm is surrounded by a narrow, cylindrical drug reservoir that contains levonorgestrel. Nonmedicinal ingredients: barium sulphate, copper phthalocyanine, polydimethylsiloxane elastomer, polyethylene, polypropylene, silica colloidal anhydrous, and silver. Two fine blue plastic threads are attached to the tip of the vertical arm. In addition, the vertical stem contains a silver ring located close to the horizontal arms, which is visible under ultrasound.
How should I use this medication?
This device is placed inside the uterus by your doctor within 7 days after the start of your period. Your doctor will most likely perform a gynecological examination before the device is inserted to examine your uterus for correct placement and to rule out pregnancy or other gynecological conditions that would make using levonorgestrel undesirable.
Your doctor will most likely perform a gynecological examination before the device is inserted to examine your uterus for correct placement and to rule out pregnancy or other gynecological conditions that would make using levonorgestrel undesirable.
The device is inserted during a routine office visit with your doctor and only takes a few minutes. You may have to go back to your doctor's office about 4 to 12 weeks after the device is inserted to ensure it is in the right position, and then once a year thereafter or as directed by your doctor. The device can be left in place for up to 5 years, after which you must decide whether to replace the device with a new one or simply to remove the old device.
It is important this medication be used exactly as recommended by your doctor. If you miss an appointment to have a new levonorgestrel-releasing intrauterine device removed or inserted, contact your doctor as soon as possible to reschedule your appointment. After 5 years, this device may not prevent pregnancy.
Do not dispose of medications in wastewater (e.g. down the sink or in the toilet) or in household garbage. Ask your pharmacist how to dispose of medications that are no longer needed or have expired.
Who should NOT take this medication?
Do not take this medication if you:
- are allergic to levonorgestrel or any ingredients or components of the device
- are or may be pregnant
- have a bacterial infection of the heart valves (endocarditis)
- have a previously inserted intrauterine device that has not been removed
- have an infection of the genital tract
- have abnormal cells in the cervix
- have abnormalities of the uterus (e.g., fibroids) that distort the shape of the uterus
- have acute liver disease or a liver tumour
- have cancer that responds to progestins (i.e., uterine, cervical, or breast cancer)
- have current or recurrent pelvic inflammatory disease or a condition that increases the risk of pelvic inflammatory disease
- have had an abortion complicated by an infection within the past 3 months
- have inflammation of the cervix
- have inflammation of the endometrium (lining of the uterus) after pregnancy within the past 3 months
- have recently had an abnormal growth of cells inside the uterus
- have a tumour related to pregnancy
- have unexplained bleeding of the uterus
What side effects are possible with this medication?
Many medications can cause side effects. A side effect is an unwanted response to a medication when it is taken in normal doses. Side effects can be mild or severe, temporary or permanent.
A side effect is an unwanted response to a medication when it is taken in normal doses. Side effects can be mild or severe, temporary or permanent.
The side effects listed below are not experienced by everyone who takes this medication. If you are concerned about side effects, discuss the risks and benefits of this medication with your doctor.
The following side effects have been reported by at least 1% of people taking this medication. Many of these side effects can be managed, and some may go away on their own over time.
Contact your doctor if you experience these side effects and they are severe or bothersome. Your pharmacist may be able to advise you on managing side effects.
- abdominal or pelvic pain
- acne
- breast tenderness or pain
- decreased or absent menstrual bleeding
- headache
- hair growth on the face, chest, stomach, or legs
- hair loss
- infrequent menstrual periods
- nausea
- oily skin
- painful menstrual periods
- spotting between periods
- symptoms of ovarian cysts (e.
 g., pelvic pain, pain with intercourse, abdominal bloating, swelling, pain with bowel movements)
g., pelvic pain, pain with intercourse, abdominal bloating, swelling, pain with bowel movements) - vaginal discharge
Although most of the side effects listed below don't happen very often, they could lead to serious problems if you do not seek medical attention.
Check with your doctor as soon as possible if any of the following side effects occur:
- expulsion of the device (e.g., increased vaginal bleeding)
- increased blood pressure
- migraine
- perforation of the uterus (e.g., severe lower abdominal pain, bleeding)
- signs of a blood clot in the arm or leg (tenderness, pain, swelling, warmth, or redness in the arm or leg) or lungs (difficulty breathing, sharp chest pain that is worst when breathing in, coughing, coughing up blood, sweating, or passing out)
- signs of depression (e.g., poor concentration, changes in weight, changes in sleep, decreased interest in activities, thoughts of suicide)
- symptoms of a pelvic infection (e.
 g., constant pain in the lower stomach, fever, unusual vaginal discharge)
g., constant pain in the lower stomach, fever, unusual vaginal discharge)
Stop taking the medication and seek immediate medical attention if any of the following occur:
- signs of a serious allergic reaction (e.g., abdominal cramps, difficulty breathing, nausea and vomiting, or swelling of the face and throat)
- signs of stroke (e.g., sudden or severe headache; sudden loss of coordination; vision changes; sudden slurring of speech; or unexplained weakness, numbness, or pain in arm or leg)
- symptoms of intrauterine pregnancy, ectopic pregnancy, or miscarriage (e.g., constant pain in lower stomach, nausea, breast tenderness, vaginal bleeding)
Some people may experience side effects other than those listed. Check with your doctor if you notice any symptom that worries you while you are taking this medication.
Are there any other precautions or warnings for this medication?
Before you begin using a medication, be sure to inform your doctor of any medical conditions or allergies you may have, any medications you are taking, whether you are pregnant or breast-feeding, and any other significant facts about your health. These factors may affect how you should use this medication.
These factors may affect how you should use this medication.
Blood clots: This medication may increase the chance of blood clot formation, causing reduction of blood flow to organs or the extremities.
If you have a history of clotting you may be at increased risk of experiencing blood clot-related problems such as heart attack, stroke, or clots in the deep veins of your leg. Discuss with your doctor how this medication may affect your medical condition, how your medical condition may affect the dosing and effectiveness of this medication, and whether any special monitoring is needed.
If you experience symptoms such as sharp pain and swelling in the leg, difficulty breathing, chest pain, blurred vision, or difficulty speaking, contact your doctor immediately.
Blood pressure: Levonorgestrel can cause an increase in blood pressure. If you have high blood pressure, discuss with your doctor how this medication may affect your medical condition, how your medical condition may affect the dosing and effectiveness of this medication, and whether any special monitoring is needed.
If you experience an increase in your blood pressure after having this device inserted, contact your doctor.
Depression: Hormones, such as progestins, are known to contribute to mood swings and symptoms of depression. If you have depression or a history of depression, discuss with your doctor how this medication may affect your medical condition, how your medical condition may affect the dosing and effectiveness of this medication, and whether any special monitoring is needed.
If you experience symptoms of depression such as poor concentration, changes in weight, changes in sleep, or decreased interest in activities, or notice them in a family member who is taking this medication, contact your doctor as soon as possible.
Diabetes: While low-dose contraceptives, such as this device, often have very little effect on blood sugar control, women with diabetes or those with a family history of diabetes should monitor their blood sugar closely to detect any worsening of blood sugar control.
Ectopic pregnancy: If you have a history of ectopic pregnancy (when a fertilized egg implants itself outside of the uterus), have had surgery on the fallopian tubes, or have had a pelvic infection, you should speak to your doctor or pharmacist before using this device. If you experience lower abdominal pain along with a missed period or unexpected bleeding while using this medication, contact your doctor.
Expulsion of device: Bleeding or pain may indicate that the device has either moved out of position or been expelled from the uterine cavity. A device that is out of position is less effective and should be removed and replaced by a new device.
Eye problems: Some women may experience a change in vision or contact lens tolerance. If this occurs, contact your eye doctor.
Headache: Levonorgestrel, like other hormones, may cause severe headache or migraine. If you have a history of migraine, discuss with your doctor how this medication may affect your medical condition, how your medical condition may affect the dosing and effectiveness of this medication, and whether any special monitoring is needed.
If you notice increasing numbers or severity of headaches after the device has been inserted, contact your doctor as soon as possible.
Heart disease: Levonorgestrel may increase the risk of developing blood clots, causing reduced blood flow to organs or the extremities. If you have a history of clotting, you may be at increased risk of experiencing blood-clot-related problems such as heart attack, stroke, or clots in the deep veins of your leg. Cigarette smoking increases the risk of serious adverse effects on the heart and blood vessels. Discuss with your doctor how this medication may affect your medical condition, how your medical condition may affect the dosing and effectiveness of this medication, and whether any special monitoring is needed.
If you experience symptoms such as sharp pain and swelling in the leg, difficulty breathing, chest pain, blurred vision, or difficulty speaking, contact your doctor immediately.
Heart valve disorders: This medication can increase your risk of getting an infection in your heart valves if you were born with or have acquired a heart valve defect. You may need to take antibiotics before the insertion and removal of this medication to prevent the infection.
You may need to take antibiotics before the insertion and removal of this medication to prevent the infection.
Infections: In the first few weeks after this device is inserted, you may be at an increased risk of a serious infection known as pelvic inflammatory disease (PID). This infection can cause the development of pregnancy outside the uterus (ectopic pregnancy) or ongoing pelvic pain. If you experience heavy bleeding, unusual vaginal discharge, pain in the lower stomach area, pain during sexual activity, chills, or fever, contact your doctor as soon as possible.
Liver function: Women who have a history of liver problems, particularly during pregnancy, may also be at an increased risk of developing liver problems when using this device. Your doctor may want to test your liver function regularly with blood tests while you are taking this medication.
If you experience symptoms of liver problems such as fatigue, feeling unwell, loss of appetite, nausea, yellowing of the skin or whites of the eyes, dark urine, pale stools, abdominal pain or swelling, and itchy skin, contact your doctor immediately.
Menstrual bleeding: Some women may experience pain and bleeding when the device is inserted or removed. Irregular menstrual bleeding is common for the first few months after the device is inserted. Over time, menstrual bleeding decreases and may stop completely while the device is inserted.
If you develop unusual or unexpected menstrual bleeding after using this medication for some time, contact your doctor.
Ovarian cysts: This medication can cause the development of ovarian cysts. Most of these don't have any symptoms and disappear on their own within 2 to 3 months. However, if you experience pain in the pelvic area, contact your doctor.
Perforation: The chance of the device puncturing the cervix or uterus is very rare (between 1 in 1,000 and 1 in 10,000). If it were to occur, it would most likely be when the device is being inserted. If this happens, the device should be removed as soon as possible.
Removal of the device: If you experience any of the following, check with your doctor to see if you should have your device removed:
- confirmed or suspected breast or endometrial cancer
- migraines or severe headaches
- recurrent inflammation of the lining of the uterus
- recurrent pelvic infections
- significantly elevated blood pressure
- stroke or heart attack
Sexually transmitted infections (STIs): This device does not protect against STIs, including HIV/AIDS. For protection against STIs, use latex condoms.
For protection against STIs, use latex condoms.
Pregnancy: This device should not be used during pregnancy. If you become pregnant, have this device removed as soon as possible. The effects of levonorgestrel on a developing infant are not well known, and the risk of harm to the baby cannot be completely ruled out. Removal of this device or probing of the uterus may result in spontaneous abortion, but an intrauterine system that is left in place during pregnancy increases chances of having a miscarriage or premature delivery. Talk to your doctor about the risks to you and your unborn child.
Breast-feeding: Hormonal birth control, such as this device, is not the first choice of birth control for women who are breast-feeding. This medication passes into breast milk. If you are a breast-feeding mother and are using levonorgestrel, it may affect your baby. Some women using this medication have reported decreased milk production. Talk to your doctor about whether you should continue breast-feeding.
Children: The levonorgestrel-releasing intrauterine system is not intended to be used by girls who have not had their first menstrual period. The safety and effectiveness of using this medication have not been established for adolescents less than 18 years old.
What other drugs could interact with this medication?
There may be an interaction between levonorgestrel intrauterine system and any of the following:
- acitretin
- anticoagulants (e.g., apixaban, dabigatran, rivaroxaban)
- aprepitant
- bosentan
- cladribine
- corticosteroids (e.g., dexamethasone, hydrocortisone, prednisone)
- cyclosporine
- dabrafenib
- diabetes medications (e.g., canagliflozin, glyburide, insulin, linagliptin, lixisenatide, metformin, rosiglitazone)
- elagolix
- flibanserin
- heparin
- HIV non-nucleoside reverse transcriptase inhibitors (NNRTIs; e.g., efavirenz, etravirine, nevirapine)
- HIV protease inhibitors (e.
 g., atazanavir, indinavir, lopinavir, saquinavir, tipranavir)
g., atazanavir, indinavir, lopinavir, saquinavir, tipranavir) - low-molecular-weight heparins (e.g., dalteparin, enoxaparin, tinzaparin)
- lumacaftor and ivacaftor
- mifepristone
- modafinil
- mycophenolate
- octreotide
- pomalidomide
- retinoic acid medications (e.g., etretinate, isotretinoin)
- rifampin
- St. John 's wort
- seizure medications (e.g., carbamazepine, gabapentin, levetiracetam, phenytoin, rufinamide, topiramate)
- selegiline
- thalidomide
- tranexamic acid
- triazolam
- ulipristal
- warfarin
If you are taking any of these medications, speak with your doctor or pharmacist. Depending on your specific circumstances, your doctor may want you to:
- stop taking one of the medications,
- change one of the medications to another,
- change how you are taking one or both of the medications, or
- leave everything as is.

An interaction between two medications does not always mean that you must stop taking one of them. Speak to your doctor about how any drug interactions are being managed or should be managed.
Medications other than those listed above may interact with this medication. Tell your doctor or prescriber about all prescription, over-the-counter (non-prescription), and herbal medications you are taking. Also tell them about any supplements you take. Since caffeine, alcohol, the nicotine from cigarettes, or street drugs can affect the action of many medications, you should let your prescriber know if you use them.
All material copyright MediResource Inc. 1996 – 2022. Terms and conditions of use. The contents herein are for informational purposes only. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Source: www.medbroadcast.com/drug/getdrug/Kyleena
Mood swings: reasons, how to deal with
The pandemic seemed like the best time for us to launch a rubric, the idea of which we had been nurturing for a long time. In "Question to a Psychologist" we will ask questions that concern many experts, and they, in turn, will share their knowledge that can help you - and simply increase your mental health literacy.
In "Question to a Psychologist" we will ask questions that concern many experts, and they, in turn, will share their knowledge that can help you - and simply increase your mental health literacy.
This time we decided to talk about the problem of mood swings that each of us faced during quarantine. How not to become a hostage of your own emotions, how to sound the alarm, suspecting you have a bipolar disorder, and what can be done to “return to the shores” and balance the internal state shattered by self-isolation and depressive news reports? Practicing psychologist, transactional analyst and family systems psychotherapist Anastasia Polyakova answers.
Julia Samoshkina
Tags:
health
psychology
psyche
What happens when we sit on an emotional swing?
1) First of all, let's agree that emotions are normal . And the fact that they are very diverse both in intensity and color is also the norm. We will not get away from them: emotions were, are and will always be with us. This is a natural part of life. Another question is how we will deal with it. If anger has attacked you, you don’t need to immediately run to a psychiatrist with the question “What is wrong with me?”.
And the fact that they are very diverse both in intensity and color is also the norm. We will not get away from them: emotions were, are and will always be with us. This is a natural part of life. Another question is how we will deal with it. If anger has attacked you, you don’t need to immediately run to a psychiatrist with the question “What is wrong with me?”.
2) Each of us always has a complete emotional kit with us. Our brain and psyche are arranged in such a way that all of us, without exception, can experience anger, sadness, joy, excitement associated with future plans - in a word, a full emotional spectrum. It’s just that some emotions are our “favorites”, and some we strongly suppress. And when these suppressed emotions wake up, then we begin to literally tear to pieces. For example, your parents told you as a child that “it’s not good to be angry, you are a well-mannered boy,” and in this case, instead of anger, you now fall into despondency every time. If in quarantine you suddenly discovered with amazement that you are capable of anger, find a peculiar benefit in this - after all, you have discovered something completely new in yourself. At first, it may even frighten you: in this case, the secondary emotion of fear is mixed in. Do not worry and do not let yourself get confused: as we remember from the first point, it is completely normal to experience completely different emotions.
If in quarantine you suddenly discovered with amazement that you are capable of anger, find a peculiar benefit in this - after all, you have discovered something completely new in yourself. At first, it may even frighten you: in this case, the secondary emotion of fear is mixed in. Do not worry and do not let yourself get confused: as we remember from the first point, it is completely normal to experience completely different emotions.
3) We subconsciously strive to be consistent . But our world is not black and white, and neither is our attitude towards it. Each event has several facets.
This is most evident in personal relationships. I can be angry with my partner, but at the same time be glad that he is next to me. Come closer to me, move away. You can read more about this in the book by Gerold Kreisman “I hate you, just don’t leave me. Borderline Personalities and How to Understand Them. In life, ambiguous events often occur. And the reaction to them is logically also very ambiguous. This is a fairly common story, which, nevertheless, can become a source of misunderstanding not only from your loved ones, but also for yourself. Indeed, in such cases, we most often cannot fully realize what is happening to us. For example, yesterday I was upset that my partner did not support my ideas. And today it infuriates me unbearably that he climbs with his smart recommendations. And it’s not clear what to do: ask for advice or deal with it yourself?
And the reaction to them is logically also very ambiguous. This is a fairly common story, which, nevertheless, can become a source of misunderstanding not only from your loved ones, but also for yourself. Indeed, in such cases, we most often cannot fully realize what is happening to us. For example, yesterday I was upset that my partner did not support my ideas. And today it infuriates me unbearably that he climbs with his smart recommendations. And it’s not clear what to do: ask for advice or deal with it yourself?
First, let's understand that it's okay to be sad about something first and then get angry. First, be glad that you don’t have to go to work, and then miss it locked up. Yes, this ambiguity can confuse our thoughts. But you can work with this.
Take any item, such as a laptop. You may like something about it, but something will annoy. For example, you like its color, the fact that it is cold when you touch it, but you will be annoyed by the fingerprint on the screen. I can be glad that I bought this laptop, but I can be upset that when I went to the store, my partner was not with me and I was alone. That is, I can look at this subject from different angles. And accordingly, at the same time, I will experience different emotions.
I can be glad that I bought this laptop, but I can be upset that when I went to the store, my partner was not with me and I was alone. That is, I can look at this subject from different angles. And accordingly, at the same time, I will experience different emotions.
First of all, ask yourself: “What exactly makes me angry? What exactly is frustrating?" Find a more precise reason for your emotions. For example, instead of the generic and vague phrase “I am depressed because of the coronavirus,” choose a more narrow and specific wording such as “I am sad because my usual rhythm of life has been forced to change” or “I am upset because I I can be as free to move as before.” Or “What am I mad at? Because household members violate my boundaries. Or “I lose my temper when I’m working and I want to concentrate, and at this time a child runs into the room.”
This way it will become clearer what exactly irritates you, what upsets you, and what brings positive emotions. In fact, this way you will better understand what and how affects your condition. If we isolate this specificity and understand that many different aspects can be concentrated around one event, internal integrity will appear - and, as a result, a more integral attitude to the situation, phenomenon and manifestation of emotions.
In fact, this way you will better understand what and how affects your condition. If we isolate this specificity and understand that many different aspects can be concentrated around one event, internal integrity will appear - and, as a result, a more integral attitude to the situation, phenomenon and manifestation of emotions.
4) It is important to know about the existence of such concepts as "lability" and "rigidity" . All people are different. Each of us has different settings that determine how this or that emotional process will proceed. For a clearer understanding, you can conditionally imagine a certain scale. At one end there will be a point of the easiest switching from one emotion to another, at the other - a complete lack of this flexibility. We are all on this scale in one way or another. Labile people switch between emotions more easily. Rigid people have a hard time with this. People with a labile psyche can be compared to sparklers - they quickly flare up, sparkle, but also quickly fade. A person with a rigid psyche is like a candle that burns with an even flame until all the wax is melted. It is important to determine what type you are. People who are prone to sudden emotional swings are like sparklers - they are labile. Those with a rigid psyche demonstrate greater constancy. For example, if they are upset in the morning, then they will walk around in a depressed state all day.
A person with a rigid psyche is like a candle that burns with an even flame until all the wax is melted. It is important to determine what type you are. People who are prone to sudden emotional swings are like sparklers - they are labile. Those with a rigid psyche demonstrate greater constancy. For example, if they are upset in the morning, then they will walk around in a depressed state all day.
5) Emotions are closely related to stress and in most cases serve as a response to a stressful situation. "I got stepped on my foot - I got angry."
We have four basic responses to stress that work without our awareness:
- beat;
- run;
- freeze;
- play dead.
The first two strategies can be classified as conditionally active. The second two are passive.
"Bey" can manifest itself as "Get business training and save the economy with your achievements. " This reaction is most often manifested through anger.
" This reaction is most often manifested through anger.
"Run" is realized through fear and makes us move and move away from danger.
The following two reactions can be compared to freezing. "Freeze" means "Lie on the couch and stick to the ceiling."
“Play dead” is a more radical version: “If I am already dead, what is the demand on me? I don't have to fight or deal with anything." In essence, the play-dead strategy is a depressive state.
We all have preferred strategies, but they can change.
6) Under the influence of any stress (it doesn't matter if it's a pandemic or a small everyday situation when you forgot your keys at home) all emotional reactions are intensified . This is due to the fact that the function of any emotion is to solve problem situations.
- Sadness and sadness are needed in order to live through losses, which have become in abundance in the current realities.
— Anger is evolutionarily needed to protect one's boundaries. None of us have ever spent so much time at home side by side with loved ones. At the same time, each of us has a need for personal space, our own rituals. During self-isolation, the problem of personal territory is especially acute, as anger signals.
- Fear protected our ancestors from danger - and now we need it in order not to risk our health by arranging barbecue in a noisy company.
- Joy is needed for rapprochement and a more productive coexistence. It is obvious that it is difficult for one now. We need to come together to get through difficult times. Robinson Crusoe first talked to a cabbage fork before he met Friday. If there is no person nearby, we start to invent him.
Considering that the stress level is going through the roof right now, it is logical that our emotions are many times stronger. However, if you think of emotions as something that has its own function and clear purpose, then it will be much easier to cope with them. For example, “What does this fear want to warn me about? Perhaps about me buying myself more protective masks and once again not leaving the house without a reason.
For example, “What does this fear want to warn me about? Perhaps about me buying myself more protective masks and once again not leaving the house without a reason.
7) We used to call strong emotions "bipolar" - we are talking about bipolar affective disorder. However, do not rush to make such a serious diagnosis for yourself : this disease has very specific symptoms and criteria.
Bipolar disorder is a mental illness characterized by alternating affective states (depression and mania). The dangerous thing is that a person ceases to control behavior and loses criticism of what is happening.
During mania, people spend money, take out loans, give away property, make grandiose plans, and never finish anything.
In depression, all motivation is lost, a person can lie in bed for weeks, he is not able to go to work and take care of loved ones.
Symptoms of mania:
- Hyperactivity.

- Excessive talkativeness.
- Many different confused thoughts.
- Irritability.
- Little need for sleep.
- Increased self-esteem.
- Risk behavior: overspending, drinking, drug use, impulsive decisions and actions, risky and exalted sexual behavior.
Symptoms of depression:
- Sadness.
- Uncontrollable attacks of fear.
- Feeling worthless and hopeless.
- Excessive feeling of guilt.
- Fatigue.
- Alarm.
- Sleep disturbance.
- Fencing off from relatives and friends.
- Changes in eating habits (increase or decrease in appetite).
Check these lists first, and if you find confirmation of your suspicions, seek authoritative help from a psychiatrist or psychotherapist. Typically, bipolar disorder is treated with a combination of medication and psychotherapy.
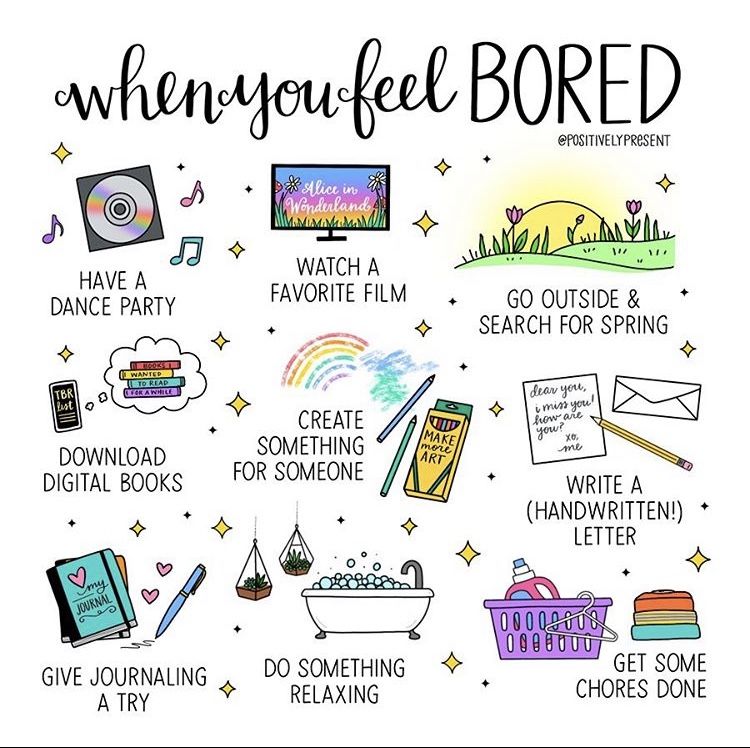
What to do with emotional swings? How to help yourself?
1) It is important to describe in words what is happening to you and give your condition a name. Sometimes it is difficult for us to understand what kind of emotion we are experiencing. To do this, you can resort to this technique. Search Google for pictures of faces that depict a variety of emotions and have a clear description of which emotion is illustrated. Go to the mirror and match your face with this or that image. This will help you realize what kind of emotion is imprinted on your face at this particular moment in time.
Sometimes it is difficult for us to understand what kind of emotion we are experiencing. To do this, you can resort to this technique. Search Google for pictures of faces that depict a variety of emotions and have a clear description of which emotion is illustrated. Go to the mirror and match your face with this or that image. This will help you realize what kind of emotion is imprinted on your face at this particular moment in time.
2) Determine the emotion function. Why did she come? What is this anger trying to tell me? What is this sadness about? How can I build relationships using joy?
3) Think about how to respond to emotions in order to smooth them out. This item will not only be useful as self-help, but will also be useful to those who are close to a hyper-emotional person.
- If you witness anger, show it to be serious. This will help reduce its intensity.

- If you are faced with fear, you need to provide physical and psychological protection and safety. "Are you afraid to go outside? Let's create all the necessary conditions for a full and comfortable life at home."
- Sadness — it is important to share it with someone and not be alone with this negative emotion. In order to be “effectively” sad, it is important for us to speak out the reason for sadness - and to do this in a certain sense selfishly, without thinking about the feelings of others. It is important that someone share the pain, experiences with us and mourn with us. Not only have Zoom parties with your friends, but also discuss together what we all have lost due to the outbreak of the pandemic. Consistency is especially important here so as not to get stuck in sadness.
- Joy - to respond vitally, that is, to be alive and involved. When a joyful child brings a drawing to his mother, it is necessary that she respond with a lively smile and say “Wow!”.
 The formal "Well done, go draw some more" is not suitable. React as vividly as possible to the joy of the other person. The energy of joy, the ability to experience it constructively, feeling included, is the right scenario. The same applies to yourself. When we think that it is worse for someone now than me, and in general it is a sin to rejoice, we extinguish the positive in ourselves. Such a strategy is not very useful for a harmonious sense of self.
The formal "Well done, go draw some more" is not suitable. React as vividly as possible to the joy of the other person. The energy of joy, the ability to experience it constructively, feeling included, is the right scenario. The same applies to yourself. When we think that it is worse for someone now than me, and in general it is a sin to rejoice, we extinguish the positive in ourselves. Such a strategy is not very useful for a harmonious sense of self.
4) Learn to smooth out the amplitude of emotional reactions. If we draw a graph of our emotional state, we get a curve with its peaks and valleys. In order for the amplitude to be smaller, you need to look for minuses in a conditionally positive state and pluses in a conditionally negative one. We are talking about the so-called secondary benefits. “What do I get in this state? How does it benefit me and what is fraught with?” Such an analysis will help to even out sharp changes in emotional reactions and significantly reduce the amplitude of their fluctuations.
How does the IUD work? - September 8, 2020
Sep 08, 2020
How does the IUD work? – September 8, 2020
Posted at 2:14 AM in Pregnancy Prevention, Women's Health to Andrew Thorne
The IUD is not a new method of birth control, but it has become more popular in recent years. Demand for IUDs has skyrocketed since 2016, according to Planned Parenthood statistics. A common question we get from our patients at One Community Health is, "How does the IUD work?" Read on to learn more about this popular contraceptive.
What is an IUD?
IUD stands for intrauterine device. It is a long-term, highly effective contraceptive option. The device itself is a small "T" shaped piece of plastic that is placed in the uterus. Depending on the specific device, IUDs last from 3 to 12 years if they have not been removed before.
How does the IUD work?
As we mentioned above, there are different types of IUDs, and each one works a little differently. Some are copper coated and some are hormone coated. Copper is toxic to spermatozoa, and if it enters the uterus, it acts as a spermicide, preventing fertilization.
Some are copper coated and some are hormone coated. Copper is toxic to spermatozoa, and if it enters the uterus, it acts as a spermicide, preventing fertilization.
IUDs coated with the hormone progestin thicken cervical mucus so sperm cannot reach the egg. In some cases, it stops ovulation - the release of an egg during a woman's monthly menstrual cycle. If the egg is not released, pregnancy is not dangerous.
How effective are IUDs?
IUDs are 99% effective in preventing pregnancy, making them one of the most effective forms of birth control available today. One of the reasons why they are so effective is that they are practically reliable, which means you cannot forget to take them or misuse them, as is possible with pills and condoms.
IUD benefits
- Comfortable
- 99% efficient
- Can be removed at any time if you want to get pregnant
- Hormonal IUDs can relieve heavy periods
- Non-hormonal option available for people who prefer (copper IUDs)
- Copper IUDs can serve as emergency contraception if inserted within 5 days of unprotected intercourse.

Reverse
Some people experience minor side effects, including:
- Irregular bleeding in the first few months
- More heavy periods and more severe cramps (copper IUD)
- Menses lighter/shorter or no menses (some progestin IUDs)
- PMS-like symptoms such as mood swings, headaches, acne, nausea, and breast tenderness (progestin IUDs)
In rare cases, there may be more serious side effects. Another disadvantage of IUDs is that they do not protect against STDs.
Different types of IUDs
Four types of hormonal IUDs are available. They all work in the same way, but last for a different amount of time.
- Mirena - lasts up to 7 years
- Kailina - lasts up to 5 years
- Liletta - lasts up to 7 years
- Skyla - lasts up to 3 years
The only non-hormonal or copper IUD available in the US is the Paragard.