Itching and depression
Why It Happens and What to Do
You’re anxious, and your skin keeps itching. Are these symptoms related?
Though you might not think it, your skin can reveal some of your deepest emotions. Just think about the last time you blushed from embarrassment or felt goosebumps while listening to inspiring music.
Anxiety, in particular, has several ways of showing itself in the physical body: It can cause shaking hands, sweating, butterflies in your stomach, or a lump in your throat.
And for some people, anxiety can cause itchy skin. Feeling itchy from anxiety is called “psychogenic itching.” While this isn’t extremely common, it’s also not rare.
Unlike many other organs in the body, your skin has an immediate reaction to mental stress. Some researchers call it the “brain-skin connection.”
Psychogenic itching, or psychogenic pruritus, occurs when psychological factors trigger or worsen itchy skin.
So, how does this happen?
Research into anxiety and itching says that the brain plays a critical role in the sensation of itching. The brain’s sensory, motor, and emotion-related areas are activated when we’re feeling itchy, and even when we just think about scratching. The central nervous system (CNS), which is responsible for regulating anxiety, is particularly involved.
More research is needed to identify the specific mechanisms behind why anxiety and itching go together. But researchers do know that when the body’s “fight, flight, or freeze” response is activated under stress, it releases a flood of hormones and other chemicals, such as cortisol and adrenaline.
Stress also activates the immune system to release histamine, a compound known to play a role in signaling itch sensations.
In short-term stress, cortisol acts as an anti-inflammatory and helps balance out the histamine levels. However, during chronic stress, the body becomes less sensitive to cortisol, allowing for more inflammation and itching.
When you reduce anxiety, you might find that your itching goes away. In fact, there’s evidence that anti-anxiety medications and psychosocial treatments for anxiety — including cognitive behavioral therapy (CBT) — can have anti-itch effects.
Anxiety and itching can result in a continuous itch-anxiety cycle. Anxiety leads to itching, which in turn leads to more anxiety, and so on.
Psychogenic itching, as well as other types of chronic itching, can significantly affect a person’s mental health and well-being. Many people with chronic itch report that psychological stress is a factor that aggravates their itching.
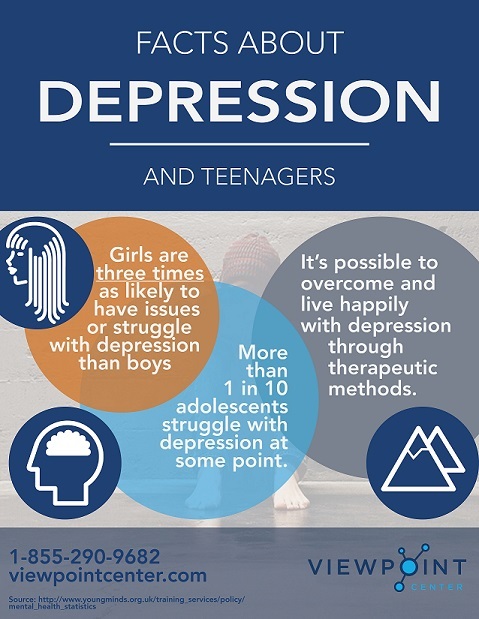
Research has also shown a link between itching and symptoms of depression. People who report severe depression also report higher itch intensity, compared to people who report low symptoms of depression.
One study found that when people with a chronic itch condition viewed stressful images — such as a snake preparing to strike or a person being pulled from a burning building — their itch severity increased.
In another study, healthy women with no chronic itch conditions reported greater itching sensations due to histamine reactions when they experienced negative emotions from distressing film clips.
You might also have experienced the “contagious itch” phenomenon.
If you see your friend scratching, or you’re reading about itching or watching a movie with a person scratching, it can make you feel itchy too! Everyone can experience this at some level, but it tends to happen to a greater degree among people with neurotic personalities.
Does anxiety make you more itchy at night?
Some people with anxiety-related itching report that their itching is worse at night. Itchy skin at night is also called nocturnal pruritus. While researchers don’t know exactly why this happens, there are a few theories.
First, your body increases blood flow to the skin at night, and your skin tends to retain less moisture — both of which could potentially worsen itchy sensations.
In addition, the body releases fewer anti-inflammatory corticosteroids at night, while releasing higher levels of certain itch-related hormones.
Also, unlike during the day when we have plenty of distractions, lying in bed at night can draw our attention to the sensations in our body, including itchy skin, making it feel more itchy.
Can anxiety cause an itchy scalp?
Some people seem to get an itchy scalp when they have anxiety. Scientists aren’t exactly sure why this happens, but we do know that anxiety increases cortisol levels, which are directly linked to hair follicles.
Internal stressors may also be linked to the growth of bacteria and fungi on the scalp, which can cause it to get dry and flaky, leading to itchiness.
To find out the cause of your itching, your physician or dermatologist will likely take your medical history, give you a dermatological exam, and request any lab tests or biopsies as needed.
If no medical source for the itching is found, your healthcare professional will work with you to explore other causes, which may include psychiatric reasons like anxiety.
According to the International Forum for the Study of Itch (IFSI), psychogenic itching falls into one of six itch categories:
- dermatological, caused by a skin condition
- systemic, caused by an organ problem
- neurological, arising from nerve problems
- psychogenic or psychosomatic, linked with psychiatric or psychosomatic conditions
- mixed
- other
To date, clinical trials haven’t explored the treatments for psychogenic itching. However, experts suggest that the following medications might be useful for relieving psychogenic itch, depending on the symptoms:
However, experts suggest that the following medications might be useful for relieving psychogenic itch, depending on the symptoms:
- hydroxyzine (antihistamine)
- tricyclic antidepressants (mainly doxepin)
- selective serotonin reuptake inhibitors (SSRIs)
- in some cases, antipsychotics and antiepileptics
You might also want to try some home remedies for itch, such as cool packs, wet wrap therapy, and applying moisturizer.
Keeping your anxiety levels to a minimum may also help relieve the itch. Try out some anxiety-reducing activities, like:
- CBT methods
- deep breathing
- meditation
- exercise
- acupuncture
- yoga
If you experience chronic itching, you may benefit from talking with a healthcare professional. Seeing a dermatologist first can rule out skin-related causes.
If you believe anxiety is causing your itching, consider trying some anxiety-reducing activities, such as meditation or yoga.
What You Can Do When They Happen Together
If you have anxiety and itchy skin, it’s possible that you’re dealing with two distinct issues. It’s also possible that these conditions are closely linked.
Anxiety disorders can cause some people to experience itchy skin and itchy skin conditions can lead to anxiety. One can exacerbate the other.
Each can be effectively treated, but it’s important to determine whether the anxiety and itching are connected. Itching due to anxiety is no less real than itching from other causes, but it may take a different approach to treatment.
According to the Anxiety and Depression Association of America, anxiety disorders affect 40 million adults in the United States every year. More than 1 in 5 people experience chronic itch at some point in their lifetime.
It’s difficult to know how many people have anxiety-related itching, or psychogenic itch.
Continue reading to learn more about the association between anxiety and itching, and what you can expect of treatment.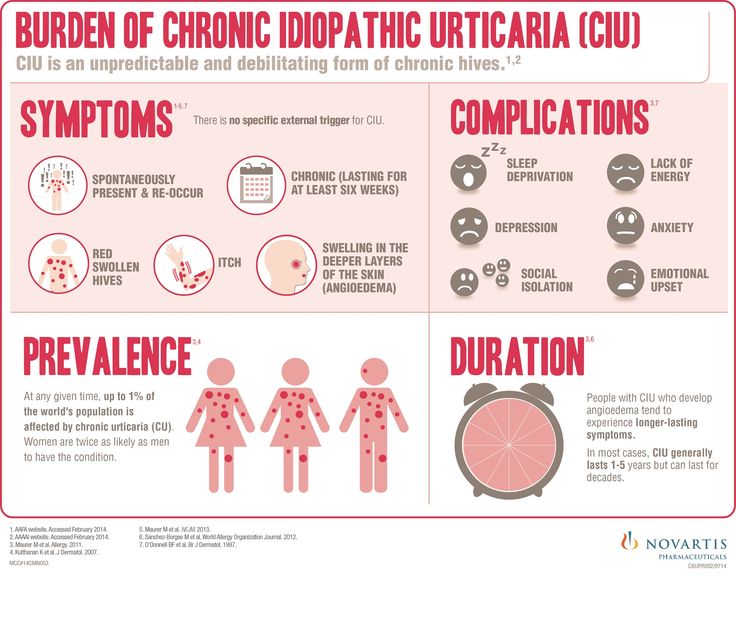
Anxiety, especially if it’s chronic, can affect your health in many ways. Anxiety is related to a number of skin problems. Just think about how a brief moment of embarrassment can cause you to blush or how being nervous can make some people break out in hives.
The weight of mental or emotional stress can also lead to some serious itching.
Your brain is always communicating with nerve endings in your skin. When anxiety kicks in, your body’s stress response can go into overdrive. This can affect your nervous system and cause sensory symptoms like burning or itching of the skin, with or without visible signs.
You can experience this sensation anywhere on your skin, including your arms, legs, face, and scalp. You might feel it only intermittently or it could be quite persistent. The itch can happen at the same time as symptoms of anxiety or it can occur separately.
Even if the cause of your itching is anxiety, serious skin problems can develop if you scratch too much or too vigorously. This can leave you with irritated, broken, or bleeding skin. It can also lead to infection. Not only that, but the scratching probably won’t do much to relieve the itch.
This can leave you with irritated, broken, or bleeding skin. It can also lead to infection. Not only that, but the scratching probably won’t do much to relieve the itch.
On the other hand, the skin condition and relentless itching may have come first, prompting the anxiety.
You may indeed have two unrelated problems — anxiety plus an itch caused by something else entirely. Depending on your specific symptoms, your doctor may want to investigate some other causes of itchy skin, such as:
- allergic reaction
- dry skin
- eczema
- insect bites and stings
- psoriasis
- scabies
- shingles
Most of these conditions can be identified upon physical examination. Itchy skin can also be a symptom of less visible conditions such as:
- anemia
- cancers such as lymphoma and multiple myeloma
- diabetes
- kidney failure
- liver disease
- multiple sclerosis
- thyroid problems
That’s why it’s so important to talk to your doctor about:
- your medical history, including pre-existing conditions, allergies, and medications
- symptoms of anxiety or depression
- any other physical symptoms you may have, even if they seem unrelated
This information will help guide the diagnosis.
Treatment depends on the specific causes of anxiety and itching. No matter the cause, unrelenting itching can have a negative impact on your overall quality of life. So, it’s worth seeking treatment.
Aside from your primary care physician, you might benefit from seeing a specialist or perhaps two. A mental health professional can help you learn to manage anxiety, which can alleviate that aggravating itch.
If your skin is seriously affected, you might also need to see a dermatologist.
Psychologists can also help with dermatological problems related to anxiety. This field is called psychodermatology.
Treatment for the itch may include:
- corticosteroids or other soothing creams or ointments
- oral selective serotonin reuptake inhibitors, a type of antidepressant that may ease chronic itching in some people
- light therapy sessions may help get itching under control
Here are some things you can do on your own to help relieve itching:
- Use hypoallergenic, fragrance-free moisturizer every day.
- Run a humidifier to help keep your skin moist.
- Avoid rough clothing, hot baths, harsh sunlight, or anything else that contributes to itchiness.
- Try over-the-counter products such as corticosteroid cream, calamine lotion, or topical anesthetics.
- When itching is impossible to ignore, put on some gloves or cover your skin to prevent yourself from scratching.
- Keep your fingernails trimmed so that if you do scratch, you’re less likely to break the skin.
Since stress can aggravate the itch, you’ll also need to take steps to lower your stress levels. Here are a few things you can try:
- acupuncture
- deep breathing exercises
- meditation
- yoga
A therapist can provide behavior modification therapy and other strategies to lessen anxiety. It’s also important to maintain a healthy diet, get plenty of sleep every night, and exercise regularly.
Any underlying medical conditions should also be addressed.
Anxiety and itching are both things that can come and go. If they’re fleeting and not causing any major problems, you may not need to see a doctor. If that’s the case, it’s still a good idea to mention it at your next appointment.
If anxiety and itching are interfering with your ability to function or causing visible skin damage or infection, see your primary care doctor as soon as possible. If necessary, you can get a referral to the appropriate specialist.
Untreated, the cycle of anxiety and itching can repeat over and over, ratcheting up your anxiety level. Frequent scratching can also lead to serious skin issues.
Anxiety and itching can be effectively treated, though. It may take some time, but with professional guidance, you can learn to manage anxiety, ultimately resolving the itch.
Regardless of which came first, anxiety and itching can be connected. With a combination of anxiety management and a good skincare routine, you can break the cycle and potentially rid yourself of persistent itch.
Itching: the current state of the problem | Bobko S.I., Tsykin A.A.
Introduction
The relevance of the phenomenon of itching is determined by its high prevalence and the associated socio-economic losses. Currently, the mechanisms of the pathogenesis of itching are not fully understood, there are difficulties in diagnosis. In addition, the number of therapeutic and prophylactic agents, the effectiveness of which has been confirmed in clinical trials, is limited. The first definition of itching as an unpleasant sensation, accompanied by a desire to scratch the skin, was proposed by S. Hafenreffer in 1660. Currently, the interpretation of itching has acquired additional features.
Epidemiology of pruritus
Itching is one of the most common subjective symptoms in dermatology, second in prevalence only to complaints of cosmetic defects. According to a number of authors, the prevalence of pruritus in the general population at the time of examination ranges from 8. 8 to 13.9% [1-3]. According to the clinical and epidemiological data of H. Alexander [4], 35% of outpatient skin clinic patients suffer from itching caused by dermatological diseases such as nodular pruritus, lichen planus, atopic dermatitis, eczema, xerosis, etc. With psoriasis, up to 87% of patients complain of itching [5, 6], and patients with atopic dermatitis and urticaria - in 100% of cases [7]. In other studies, the prevalence of pruritus in atopic dermatitis ranged from 81 to 87%, in psoriasis - from 41 to 96% [8–10].
8 to 13.9% [1-3]. According to the clinical and epidemiological data of H. Alexander [4], 35% of outpatient skin clinic patients suffer from itching caused by dermatological diseases such as nodular pruritus, lichen planus, atopic dermatitis, eczema, xerosis, etc. With psoriasis, up to 87% of patients complain of itching [5, 6], and patients with atopic dermatitis and urticaria - in 100% of cases [7]. In other studies, the prevalence of pruritus in atopic dermatitis ranged from 81 to 87%, in psoriasis - from 41 to 96% [8–10].
Itching for 6 weeks. and more, according to the conclusion of the International Forum for Study of Itch (IFSI), are classified as chronic. Itching can occur in various nosologies, presenting significant difficulties for diagnosis and treatment, and significantly affect the quality of life of patients (Table 1).
The incidence of chronic pruritus in the general population ranges from 8.4% in a cohort study of 40,000 adults in Norway [11] to 13.9% in a small pilot study in Germany involving 200 adults [12], according to other sources, up to 18. 7% [13], 20–30% [1]. According to B. Yalcin and E. Tramer [14], itching was the cause of hospitalizations in elderly patients in 11.5% of cases. In a study by R.A. Norman [15], itching was present in 2/3 of cases in elderly patients, according to H. Van Os-Medendorp [10] - in 29% of patients older than 50 years. In a study of patients in a dermatological outpatient clinic, itching was observed in 60% of cases [16].
7% [13], 20–30% [1]. According to B. Yalcin and E. Tramer [14], itching was the cause of hospitalizations in elderly patients in 11.5% of cases. In a study by R.A. Norman [15], itching was present in 2/3 of cases in elderly patients, according to H. Van Os-Medendorp [10] - in 29% of patients older than 50 years. In a study of patients in a dermatological outpatient clinic, itching was observed in 60% of cases [16].
In some patients, chronification and amplification of itching on the background of stress are noted. Chronic itching often reveals comorbid relationships with depression, anxiety, obsessive-compulsive disorders [17-19].
Itching classification
Itching performs a vital protective function in the body along with pain, being a signal for the effective removal of damaging substances from the skin. Normally, itching is a component of a protective reflex aimed at removing potentially dangerous irritating substances/objects that have fallen on the surface or deep into the skin. Under the conditions of the pathological process, itching can act as: 1) a symptom of the disease, becoming part of the clinical picture in a particular nosology; 2) symptom complex - a syndrome observed in various nosologies; 3) a monosymptom that actually corresponds to an independent dermatological diagnosis of "pruritus" - L.29in ICD-10. In the third case, itching is the most difficult diagnostic and therapeutic problem, since it is assumed that all possible objective dermatological and somatic/neurological causes of its occurrence are excluded. According to J. Rechenberger (1976), itching can be provoked not only by mechanical, electrical or chemical stimuli, but also by emotional stimuli.
Under the conditions of the pathological process, itching can act as: 1) a symptom of the disease, becoming part of the clinical picture in a particular nosology; 2) symptom complex - a syndrome observed in various nosologies; 3) a monosymptom that actually corresponds to an independent dermatological diagnosis of "pruritus" - L.29in ICD-10. In the third case, itching is the most difficult diagnostic and therapeutic problem, since it is assumed that all possible objective dermatological and somatic/neurological causes of its occurrence are excluded. According to J. Rechenberger (1976), itching can be provoked not only by mechanical, electrical or chemical stimuli, but also by emotional stimuli.
In modern studies, the classification of pruritus has been adopted depending on the mechanisms of occurrence: pruritic pruritus [30] (in skin diseases - atopic dermatitis, psoriasis, etc.), systemic (in the pathology of internal organs - primary biliary cirrhosis, chronic renal failure, Hodgkin's disease, etc. ). .), neurological/neuropathic (with compression, injury of the nerve trunks), psychogenic [31], functional [32], idiopathic [33, 34], somatoform [35] (with mental disorders) and multifactorial (with a combination of two or more of the above reasons) [30, 36, 37]. In addition, there are other classifications of itching (Table 2).
). .), neurological/neuropathic (with compression, injury of the nerve trunks), psychogenic [31], functional [32], idiopathic [33, 34], somatoform [35] (with mental disorders) and multifactorial (with a combination of two or more of the above reasons) [30, 36, 37]. In addition, there are other classifications of itching (Table 2).
Pruritus pathogenesis
The mechanisms of pathogenesis of pruritus are currently not well understood. At the present stage of scientific development, there is evidence of the existence of central neuronal pathways that are not associated with nociceptive analyzers, as well as itch-specific receptors [38, 39] and mediators that mediate the perception of itch. When examining the skin of patients with atopic dermatitis, an increase in neurogenic growth factor was noted [40]. In addition, the role of interleukin-31 and its increase in patients with atopic dermatitis, who often complain of itching, are currently being actively discussed [41, 42]. The use of antibodies to interleukin-31 in a mouse model of atopic dermatitis significantly reduced the level of pruritus [43]. Currently, the role of mediators such as vasoactive intestinal peptide (VIP), substance P, and endothelin-1 is actively discussed in the pathogenesis of pruritus.
The use of antibodies to interleukin-31 in a mouse model of atopic dermatitis significantly reduced the level of pruritus [43]. Currently, the role of mediators such as vasoactive intestinal peptide (VIP), substance P, and endothelin-1 is actively discussed in the pathogenesis of pruritus.
An imbalance in the mu-(μ) and kappa-(k) opioid receptor systems in the skin or in the central nervous system is currently suspected as one of the causes of chronic pruritus. Studies have demonstrated the positive effect of systemic kappa-opioid receptor agonists in the treatment of nodular pruritus, paraneoplastic, uremic and cholestatic pruritus [44, 45].
In the brain, sensory, motor, and affective regions are activated at the same time that itching occurs [46].
Therefore, the definition of pruritus can be formulated as follows: a feeling that is accompanied by contralateral activation of the anterior cortex and predominantly unilateral activation of additional motor areas and the lower parietal lobe and which causes scratching of the corresponding skin areas [47] – reflecting the fact that “it is not the skin that itches, and itching occurs in the brain” (Fig. 1) [48].
1) [48].
The involvement of the brain in the pathogenesis of pruritus is obvious if we assume that a psychological component may be present in each case of pruritus and that a specific psychogenic pruritus is possible, i.e. itching may be psychogenic induced. Opioids and other neurotransmitters such as acetylcholine are involved in this phenomenon (Table 3).
Patients with functional or other pruritus constantly scratch the skin, causing hyperplasia and more intense itching. Scratching temporarily suppresses the sensation of itching; then peripheral and central sensitization occurs [44]. The release of inflammatory mediators during scratching increases the sensitivity of itch receptors (peripheral sensitization), while chronic skin inflammation promotes the process of itching signals in the spinal cord and brain, which leads, respectively, to the sensation of itching of the skin (central sensitization) [30].
At the molecular level, the two-way relationship between the central nervous system and the peripheral pruritic process, caused by stress, has been widely studied [49]. For example, dermal neuropeptides are found in myelinated A-fibers and small unmyelinated C-fibers, including sensory and autonomic fibers. The skin is innervated not only by primary afferent sensory nerves, but also by postganglionic cholinergic, and parasympathetic, and adrenergic, and cholinergic sympathetic nerves. The latter serve not only to conduct stimuli from the skin to the central nervous system, but also participate in efferent "neurosecretion". Thus, emotional stress-induced release of neuropeptides may be pruritic and act on the immune system through humoral factors such as cytokines and antibodies, which regulates neuroendocrine function. Neuropeptides also exert their multiple effects on central regulatory centers that alternately regulate autonomic and behavioral responses.
For example, dermal neuropeptides are found in myelinated A-fibers and small unmyelinated C-fibers, including sensory and autonomic fibers. The skin is innervated not only by primary afferent sensory nerves, but also by postganglionic cholinergic, and parasympathetic, and adrenergic, and cholinergic sympathetic nerves. The latter serve not only to conduct stimuli from the skin to the central nervous system, but also participate in efferent "neurosecretion". Thus, emotional stress-induced release of neuropeptides may be pruritic and act on the immune system through humoral factors such as cytokines and antibodies, which regulates neuroendocrine function. Neuropeptides also exert their multiple effects on central regulatory centers that alternately regulate autonomic and behavioral responses.
In this regard, it is worth mentioning the vicious circle, or the cycle of "itching - scratching - itching." Damage to the skin barrier and subsequent inflammation lead to the development of itching. In the skin, inflammatory cells activate sensory nerves, mast cells, fibroblasts, macrophages (all of which express kappa-opioid receptors). These cells release itch mediators, which further increase inflammation. Along with the activation of sensory fibers, the itch signal is transmitted to the brain; nerves release neuropeptides that increase inflammation (called neurogenic inflammation). The itch signal is transmitted to the brain, causing the scratch reflex. Scratching leads to damage to the skin barrier (excoriations), which further increases inflammation. T-lymphocytes and eosinophils migrate into the skin, releasing pruritogen mediators. Ultimately, sensitization of sensitive nerve fibers and a decrease in the activation threshold occur. Growth factors released by eosinophils lead to the proliferation of nerve fibers. These changes increase the sensitivity of the skin, which becomes even more vulnerable to endo- and exogenous factors. This cycle is difficult to break. The cycle of “itching – scratching – itching” leads to sleep disorders, concentration of attention and perception processes, and interferes with labor activity [30] (Tables 3–5).
In the skin, inflammatory cells activate sensory nerves, mast cells, fibroblasts, macrophages (all of which express kappa-opioid receptors). These cells release itch mediators, which further increase inflammation. Along with the activation of sensory fibers, the itch signal is transmitted to the brain; nerves release neuropeptides that increase inflammation (called neurogenic inflammation). The itch signal is transmitted to the brain, causing the scratch reflex. Scratching leads to damage to the skin barrier (excoriations), which further increases inflammation. T-lymphocytes and eosinophils migrate into the skin, releasing pruritogen mediators. Ultimately, sensitization of sensitive nerve fibers and a decrease in the activation threshold occur. Growth factors released by eosinophils lead to the proliferation of nerve fibers. These changes increase the sensitivity of the skin, which becomes even more vulnerable to endo- and exogenous factors. This cycle is difficult to break. The cycle of “itching – scratching – itching” leads to sleep disorders, concentration of attention and perception processes, and interferes with labor activity [30] (Tables 3–5).
In relation to psychopathology, a depressive clinical state, which has been shown to be associated with elevated corticotropin-releasing hormone levels, has been suggested to amplify (amplify) the perception of pruritus due to an increase in central neurogenic endogenous opioid levels [19]. This theory is given the main place in the latest study of psychoneuroimmunological connections. For example, acute immobilization stress initiates mast cell degranulation via corticotropin-releasing factor, neurotensin, and substance P in rats [50]. Thus, a common mediator of pruritus, in particular corticotropin-releasing factor, may be involved in stress and depression.
Itching therapy
In the diagnostic and therapeutic guidelines for chronic pruritus of the German Dermatological Society, published in 2006 [51], the following drugs are distinguished to reduce the intensity of pruritus: antihistamines, mast cell inhibitors, systemic glucocorticosteroids, opioid receptor agonists, gabapentin, antidepressants, serotonin receptor antagonists , cyclosporine A. Local agents include local anesthetics, topical glucocorticosteroids, capsaicin, cannabinoid receptor antagonists, tacrolimus and pimecrolimus, acetylsalicylic acid, doxepin, zinc, menthol and camphor, mast cell inhibitors.
Local agents include local anesthetics, topical glucocorticosteroids, capsaicin, cannabinoid receptor antagonists, tacrolimus and pimecrolimus, acetylsalicylic acid, doxepin, zinc, menthol and camphor, mast cell inhibitors.
To date, a number of works have been published on the study of modern experimental drugs that have a central antipruritic effect (antagonists and selective agonists of kappa-opioid receptors, selective serotonin reuptake inhibitors (SSRIs)) [52-55] and local antipruritic effects (agonists of vanilloid, cannabinoid receptors, protease inhibitors, and proteinase-activating receptor antagonists) [56, 57]. In particular, palmitoylethanolamine is a selective cannabinoid type 2 receptor agonist and is available in the form of some drugs that are used in the treatment of atopic dermatitis, pruritus of unknown origin, and prurigo. According to research by S. Ständer et. al. [58, 59], there was a reduction in itching up to 60% according to the visual analogue scale. However, complete relief of itching was not achieved.
At the same time, there are reports of regression of psychogenic itching after 2 weeks. against the background of taking antidepressants from the SSRI group, in particular, paroxetine at a dose of 20 mg [60].
According to the literature, the use of selective opioid receptor agonists or SSRIs can achieve a significant (more than 50%) reduction in pruritus in only 32–55% and complete elimination of it in approximately 20% of patients [55]. The study showed a slight difference in the effectiveness of the treatment of chronic itching with antidepressants of the SSRI group (paroxetine, fluvoxamine) in 2 groups of patients, regardless of the presence of mental pathology. Group 1 included patients without mental disorders (n=37), group 2 included patients with various mental pathologies (n=35): depressive disorders, adjustment disorders, anxiety, neurotic, somatoform and dissociative disorders. In the group of patients with mental disorders, the effect of treatment in the form of regression of itching was observed in 71. 4% of cases, in the group of patients without mental disorders - in 64.9%. The differences were not statistically significant, and there was no statistically significant difference between the treatment effects of fluvoxamine and paroxetine in the treatment groups (p=0.206). The mean duration of treatment with paroxetine was 26.3 weeks and with fluvoxamine 21.5 weeks. [55].
4% of cases, in the group of patients without mental disorders - in 64.9%. The differences were not statistically significant, and there was no statistically significant difference between the treatment effects of fluvoxamine and paroxetine in the treatment groups (p=0.206). The mean duration of treatment with paroxetine was 26.3 weeks and with fluvoxamine 21.5 weeks. [55].
Capsaicin, the pungent component of red pepper, is seen as an effective treatment for a variety of pruritic conditions: activation of afferent C-fibers and subsequent reduction of neuropeptides (such as substance P) lowers the threshold for pruritic stimulation [61] – this has been demonstrated in relation to notalgia paresthetica [62, 63] brachioradial pruritus [64, 65] and prurigo nodosum [66]. Cream with local anesthetics (lidocaine, prilocaine) can play an auxiliary role along with other local agents in the treatment of pruritus. G. Yosipovitch [67] demonstrated that the preliminary use of an ointment with local anesthetics (lidocaine, prilocaine) significantly reduced the side effects of capsaicin, such as burning and hyperalgia.
Many non-specific therapeutic agents are used in addition to specific treatments. In all cases of itching, the fundamental importance of supportive care in the form of cold compresses with abundant moisture (topical moisturizing therapy with urea) cannot be ignored. This supportive therapy softens, provides hydration, facilitates the processing of crusts and reduces xerosis, which helps to reduce itching. Menthol products are also useful for relieving itching. If there is a secondary bacterial infection, additional treatment with antibacterial drugs is necessary. Occlusive dressings are recommended to help reduce excoriations. Itchy eruptions, such as prurigo due to chronic itching, can be removed with a laser, cryotherapy, injections of triamcinolone locally into the area of \u200b\u200bthe lesions. Means that play an important role in the treatment of pruritus include phototherapy, ultraviolet radiation - UVB and PUVA therapy (Fig. 2).
The traditional therapeutic approach to the treatment of pruritus is the use of antihistamines, both systemic and local. According to the EAACI (European Academy of Allergology and Clinical Immunology) classification, antihistamines of the 1st generation with sedative action (diphenhydramine, clemastine, chloropyramine, hifenadine) and 2nd generation (non-sedative) antihistamines are distinguished, among which there are metabolized (loratadine, ebastine) and active metabolites - drugs, which enter the body immediately in the form of an active substance (cetirizine, levocetirizine, desloratadine, fexofenadine). There is an opinion that in antihistamines of the 1st generation, the sedative side effect has a positive effect in the treatment of pruritic dermatosis in patients with sleep disorders, however, sedatives (except doxylamine) inhibit the REM sleep phase (rapid eye movement - the phase of rapid eye movements), which leads to to an increase in the duration and intensity of this phase, as a result, sleep becomes intermittent. Antihistamines of the first generation can cause headache, weakness, atropine-like effects: urinary retention, dry mouth, impaired vision and gastrointestinal function.
According to the EAACI (European Academy of Allergology and Clinical Immunology) classification, antihistamines of the 1st generation with sedative action (diphenhydramine, clemastine, chloropyramine, hifenadine) and 2nd generation (non-sedative) antihistamines are distinguished, among which there are metabolized (loratadine, ebastine) and active metabolites - drugs, which enter the body immediately in the form of an active substance (cetirizine, levocetirizine, desloratadine, fexofenadine). There is an opinion that in antihistamines of the 1st generation, the sedative side effect has a positive effect in the treatment of pruritic dermatosis in patients with sleep disorders, however, sedatives (except doxylamine) inhibit the REM sleep phase (rapid eye movement - the phase of rapid eye movements), which leads to to an increase in the duration and intensity of this phase, as a result, sleep becomes intermittent. Antihistamines of the first generation can cause headache, weakness, atropine-like effects: urinary retention, dry mouth, impaired vision and gastrointestinal function. Despite these shortcomings, I generation antihistamines have an advantage in the form of injectable forms. In addition, a number of drugs (for example, hydroxyzine) have anti-anxiety effects. Chloropyramine has an additional anticholinergic effect, which is taken into account in the complex treatment of atopic dermatitis. Cyproheptadine and clemastine also have antiserotonin activity. The question of the lower cost of first generation antihistamines is controversial due to the fact that they act for a short time [68].
Despite these shortcomings, I generation antihistamines have an advantage in the form of injectable forms. In addition, a number of drugs (for example, hydroxyzine) have anti-anxiety effects. Chloropyramine has an additional anticholinergic effect, which is taken into account in the complex treatment of atopic dermatitis. Cyproheptadine and clemastine also have antiserotonin activity. The question of the lower cost of first generation antihistamines is controversial due to the fact that they act for a short time [68].
Antihistamines of the second generation (non-sedative) have a higher affinity for h2-receptors and high specificity, rapid onset of action and duration of effect up to 24 hours, high selectivity of action. Due to the fact that these drugs do not penetrate the blood-brain barrier, they do not cause drowsiness.
Clinical observation
A 42-year-old patient complained of high-intensity itching on the skin of the trunk, which appeared after the use of a combined drug tolperisone containing vitamins of group B. For treatment for 2 days without effect, he independently used antihistamines, topical glucocorticosteroids. A similar episode was observed in a patient six months ago after eating red fish. Heredity is not burdened. Allergy testing has not been done before. Among the concomitant diseases - chronic gastritis, chronic pancreatitis. The skin process is represented by numerous linear excoriations, erythema on the skin of the back, severe skin itching, leading to sleep disturbances. Dermographism red (Fig. 3).
For treatment for 2 days without effect, he independently used antihistamines, topical glucocorticosteroids. A similar episode was observed in a patient six months ago after eating red fish. Heredity is not burdened. Allergy testing has not been done before. Among the concomitant diseases - chronic gastritis, chronic pancreatitis. The skin process is represented by numerous linear excoriations, erythema on the skin of the back, severe skin itching, leading to sleep disturbances. Dermographism red (Fig. 3).
According to laboratory tests, blood counts are within normal limits, total IgE is 9.3 IU/ml. In terms of differential diagnosis, the diagnoses of acute urticaria and toxicoderma for vitamins of group B were discussed. After consulting an allergist, the patient was recommended therapy with enterosorbents, antihistamines, 3 injections of dexamethasone were performed (8 mg intramuscularly on the 1st day, 2nd and 3rd days - 4 mg), which stopped the severity of the skin process. To clarify the sensitization, an allergic examination was carried out with the identification of food allergies.
To clarify the sensitization, an allergic examination was carried out with the identification of food allergies.
Among the products that most often cause the development of urticaria and angioedema, it is important to note nuts, fish, seafood, eggs, milk, and soy products. Acute urticaria can also be a manifestation of fruit-latex syndrome (this is a cross-food allergy to some fruits - bananas, pineapples, strawberries, kiwi, mangoes, passion fruit, etc. with sensitization to latex). Latex proteins are similar in structure to many other plant proteins, so a cross-reaction develops. Acute urticaria can also manifest itself as a cross-food allergy with hay fever. Among the drugs that contribute to the development of urticaria and angioedema, there are antibacterial, protein drugs, acetylsalicylic acid, nonsteroidal anti-inflammatory drugs, muscle relaxants (the patient used a centrally acting muscle relaxant), narcotic analgesics, radiopaque substances, plasma substitutes, angiotensin-converting enzyme inhibitors.
Thus, skin diseases and itching are interrelated, but only a qualified dermatologist can establish a causal relationship between itching and skin disease.
The doctor told about the unexpected causes of skin itching - Moscow 24, 07/27/2022
July 27, 08:00
Society
Photo: depositphotos/Milkos
Skin itching can warn of depression and hypothyroidism, hypothyroidism. Tatyana Romanenko, a therapist of the highest category, told Moscow 24 about this.
According to the expert, one of the causes of skin itching may be a lack of fat-soluble vitamins A and E. "These are the vitamins that are involved in the regeneration of the skin. Thanks to them, it becomes elastic," the therapist specified.
When you have a deficiency - hypovitaminosis of vitamins A and E, then not only the skin suffers, but also other skin appendages, such as hair. They can become brittle and dull, nails begin to exfoliate, and general weakness is generally characteristic. The skin becomes hypersensitive. Itching can occur almost anywhere.
The skin becomes hypersensitive. Itching can occur almost anywhere.
Tatyana Romanenko
physician of the highest category
To get rid of skin itching in this case, it is necessary to balance the diet. It should contain vegetables, fruits, animal products, recommends Romanenko.
"Another cause of skin itching or changes in the skin is a malfunction of the thyroid gland. A decrease in the production of thyroid hormones worsens the energy supply throughout the body," the therapist said in an interview with the Doctor 24 program.
In addition to skin itching, you begin to complain of drowsiness, decreased performance, weight gain, and constipation. Such skin itching, of course, cannot be ignored, you need to urgently consult a doctor, take a blood test for thyroid hormones.
Tatyana Romanenko
physician of the highest category
Itching can also be caused by depression, the doctor warns.
"What is depression? Violation of the production of neurotransmitters - dopamine and serotonin. They are responsible for our mood, performance. When the production of these neurotransmitters is disrupted, people begin to suffer, their nervous system suffers, the transmission of nerve impulses is disrupted. And one of the signs of depression is skin itching," says Romanenko.
They are responsible for our mood, performance. When the production of these neurotransmitters is disrupted, people begin to suffer, their nervous system suffers, the transmission of nerve impulses is disrupted. And one of the signs of depression is skin itching," says Romanenko.
And itching can occur in different places, she continues. In this case, it is useless to take biological supplements, you need the help of a specialist. Another cause of unpleasant symptoms on the skin can be too frequent and improper bathing.
When we bathe frequently and use hygiene products that may not be very gentle and suitable for your skin, we break the outer protective layer of the skin. The skin starts to itch.
Tatyana Romanenko
doctor of the highest category
In addition, you should not bathe in too hot water, as this can provoke excessive production of sebum. “If the skin becomes so oily, it will be a good breeding ground for various bacteria.