Is schizophrenia really that bad
Schizophrenia Myths and Facts
Written by Stephanie Watson
There's a lot of incorrect info out there about schizophrenia. Some of it is spread by movies or TV shows. Or sometimes, people use stereotypes when talking about this mental illness.
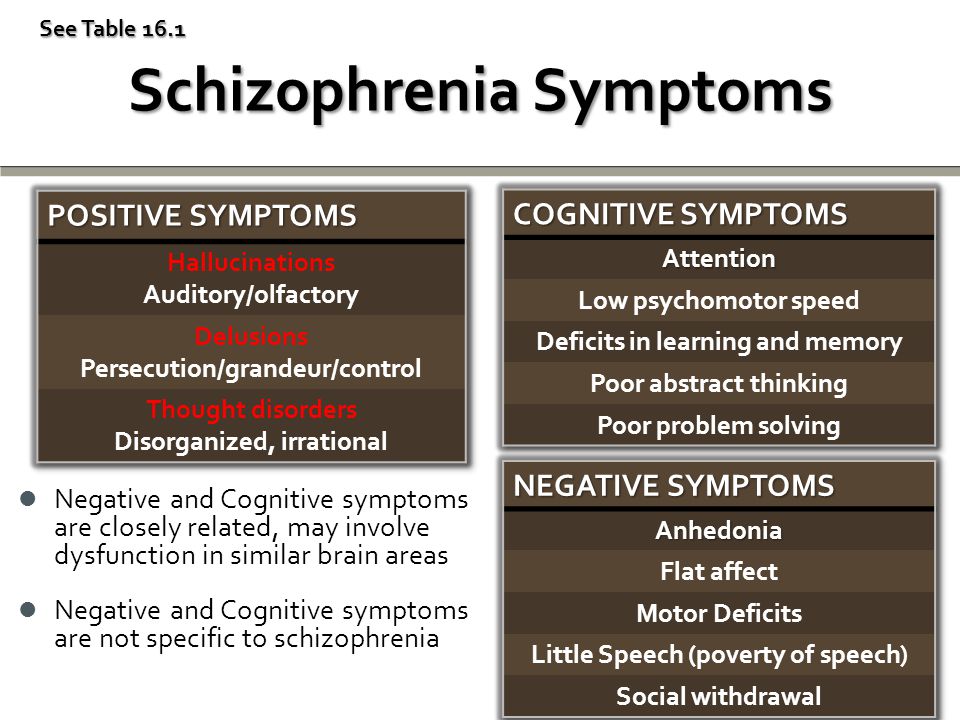
Schizophrenia is a serious mental disorder that affects your ability to think and act clearly. When you have schizophrenia, your brain often tells you you’re seeing things or hearing voices that aren’t there. This makes it hard to tell what’s real and what isn’t. It also affects how well you think, make decisions, and manage your emotions.
Around 1% of people in the U.S. have schizophrenia. It affects men and women equally. Women tend to get schizophrenia in their 20s or 30s. Men tend to get it in their late teens to early 20s. It’s rare in kids younger than 12. And it usually doesn’t appear for the first time in adults over 40.
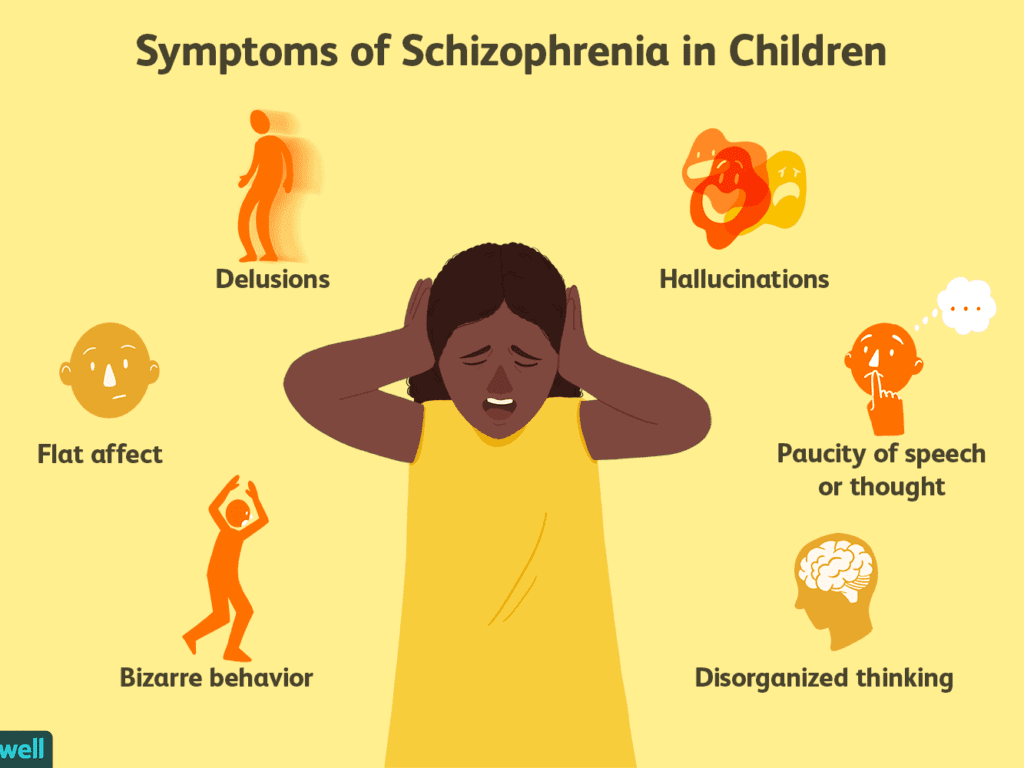
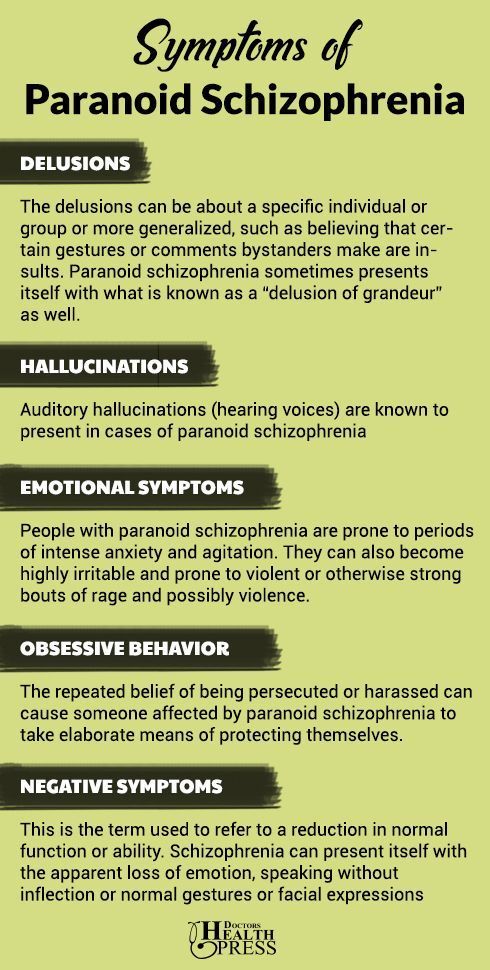
If you get schizophrenia, you might have:
- Delusions, or false beliefs that don’t change, even when you’re given new ideas and facts
- A hard time remembering things
- Disordered thoughts
- Hallucinations, or hearing voices, seeing things, or smelling things others can’t
- Lack of emotion in your face or voice
- Problems focusing
- Trouble understanding information and making decisions
Commonly, people with schizophrenia don’t know they have it, which can make treatment much more challenging.
Get the real story behind some common myths.
Myth No. 1: It means you have multiple personalities. This is one of the biggest misunderstandings about schizophrenia. One poll found that 64% of Americans believe the condition involves a split personality, which means someone acts like they're two separate people.
Some of the most common symptoms of schizophrenia are hallucinations and delusions, which include hearing voices in your head and acting on false beliefs. This isn’t the same as multiple personality disorder, or, more accurately, dissociative identity disorder (DID).
A person with schizophrenia doesn't have two different personalities. Instead, they have false ideas or have lost touch with reality. Multiple personality disorder is unrelated.
Myth No. 2: Most people with schizophrenia are violent or dangerous. In movies and TV shows, who is the crazed killer? Often it's the character with this condition. That's not the case in real life.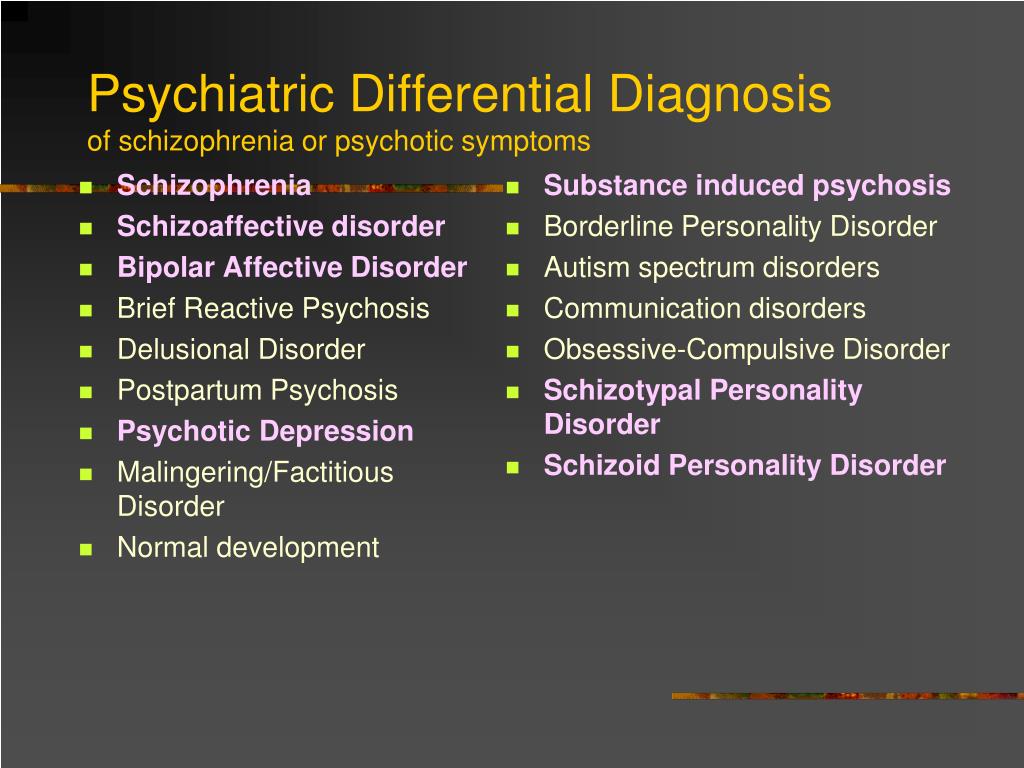
Even though people with schizophrenia can act unpredictably at times, most aren't violent, especially if they're getting treated. People with schizophrenia are more likely to be victims of violence. They’re also more likely to harm themselves than others -- suicide rates among people with schizophrenia are high.
When people with this brain disorder do commit violent acts, they usually have another condition, like childhood conduct problems or substance abuse. But the disorder alone doesn’t make you physically aggressive.
Myth No. 3: Bad parenting is the cause. Mothers, in particular, often get blamed.
But schizophrenia is a mental illness. It has many causes, including genes, trauma, and drug abuse. Mistakes you've made as a parent won't give your child this condition.
Myth No. 4: If a parent has schizophrenia, you'll get it, too. Genes do play a role. But just because one of your parents has this mental illness doesn't mean you're destined to get it. You might have a slightly higher risk, but scientists don’t think genes are the only cause. Certain viruses, not getting enough nutrition before you’re born, and other things play a role in turning on the genes.
You might have a slightly higher risk, but scientists don’t think genes are the only cause. Certain viruses, not getting enough nutrition before you’re born, and other things play a role in turning on the genes.
If one parent has schizophrenia, your risk of getting the condition is about 10%. Having more than one family member with it raises your risk.
Myth No. 5: People with schizophrenia aren’t smart. Some studies have found that people with the condition have more trouble on tests of mental skills such as attention, learning, and memory. But that doesn't mean they're not intelligent.
Many creative and smart people throughout history have had schizophrenia, such as Russian ballet dancer Vaslav Nijinsky and Nobel Prize-winning mathematician John Nash. Scientists are even looking into links between genes that may be related to both psychosis and creativity.
Myth No. 6: If you have schizophrenia, you belong in a mental hospital. There was a time when people with mental illnesses were sent to asylums or even prisons. But now that experts know more about this disease, fewer people need to be placed in long-term mental health facilities.
But now that experts know more about this disease, fewer people need to be placed in long-term mental health facilities.
The level of care you need depends on how severe your symptoms are. Most people with schizophrenia live independently with family or in supportive housing in the community. It’s important to be in close contact with your doctor, and to have support in place to help you continue your treatment as needed.
Myth No. 7: You can't hold a job if you have it. Schizophrenia can make it harder for you to land a job and go to work every day. But with the right treatment, many people can find a position that fits their skills and abilities.
Myth No. 8: Schizophrenia makes people lazy. The illness can make it harder for someone to take care of their daily needs, such as dressing and bathing. This doesn’t mean they're "lazy." They just need some help with their daily routine.
Myth No. 9: It comes on with a sudden psychotic break.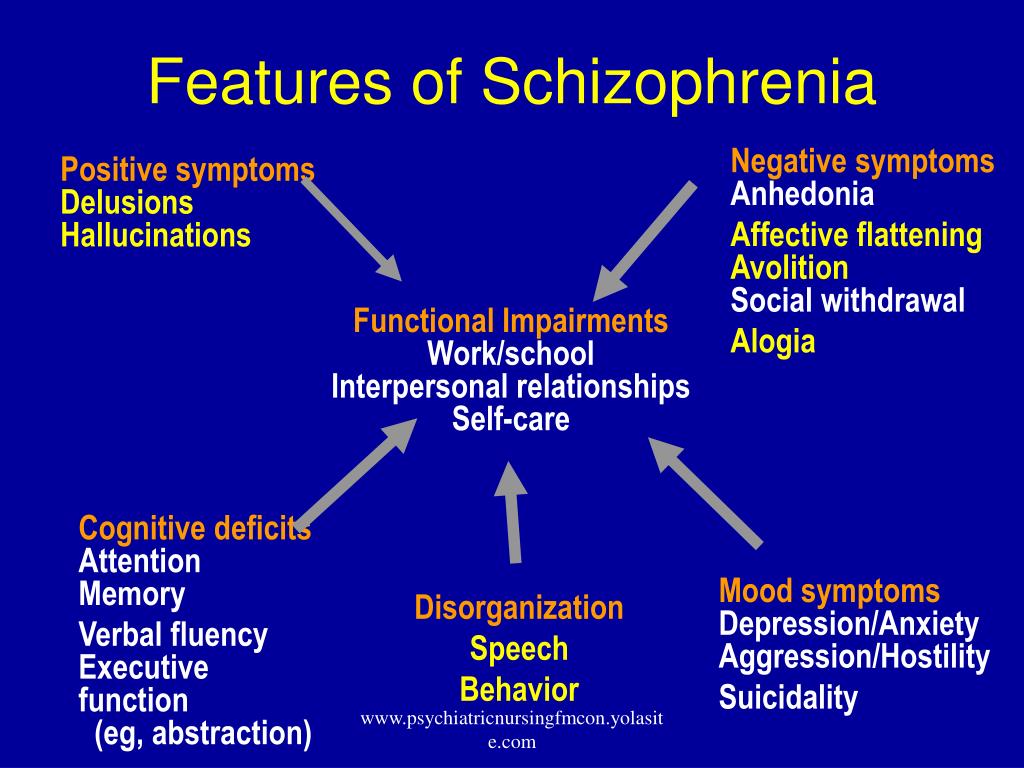
Fact: Some people have a big mental event that leads to a schizophrenia diagnosis. But symptoms can appear over time and are hard to notice. If you have early symptoms of schizophrenia, you might:
- Be less social
- Show less interest in normal activities
- Withdraw from everyday life
Other symptoms, like acting out delusions and hallucinating, can show up later.
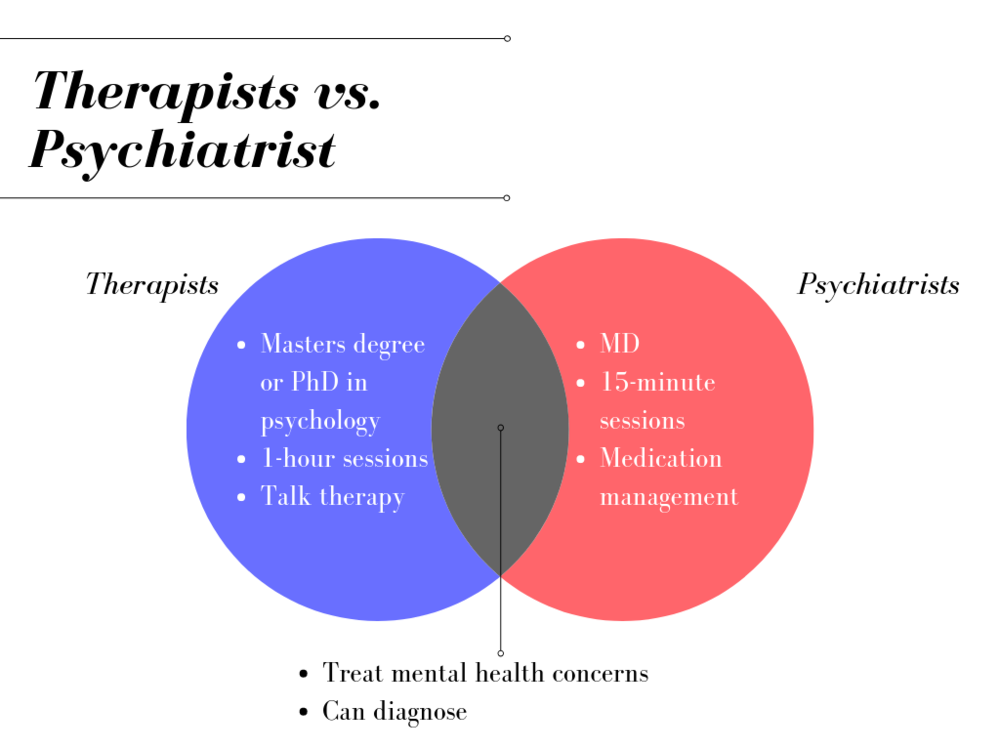
Myth No. 10: You can never recover from it. Schizophrenia can be hard to treat, but it's not impossible. Antipsychotic medications help stabilize you, and lower the risk of future symptoms. Talk therapy and cognitive behavioral therapy are also helpful tools that can show you how to handle stress better and live well.
With the right medicine and therapy, about 25% of people with this disease will recover completely. Another 50% will see some improvement in their symptoms. Many people with the condition can live full, productive lives.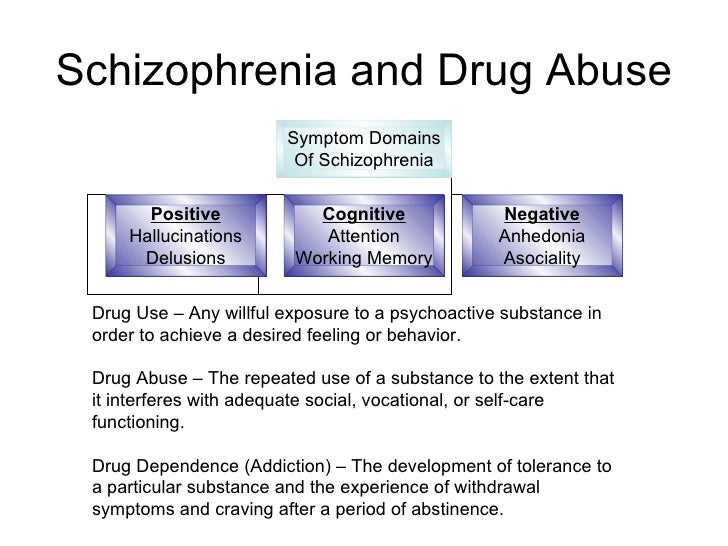
Six Common Myths and Misconceptions About Schizophrenia
Split personality. Violent behavior. Never being able to hold onto a job or have a career. Myths abound about schizophrenia, a serious and complex mental disorder currently affecting about 1 percent of American adults.
Patients diagnosed with schizophrenia do not present with a split personality, nor is it common for someone with the disorder to be violent, says Simon Rego, PsyD, chief psychologist at Montefiore Medical Center and Associate Professor of Psychiatry and Behavioral Sciences at Albert Einstein College of Medicine in New York City. And many individuals with schizophrenia are able to work.
Here, experts dispel some of the more common myths about schizophrenia.
#1 Myth: Schizophrenia means you have a split personality.
Reality: “This is a classic myth,” Dr. Rego says. A split personality, also called a Dissociative Identity Disorder or a Multiple Personality Disorder, is extraordinarily rare, he explains. It is quite distinct from schizophrenia, he says. “Schizophrenia is a thought disorder,” he explains, “The myth likely stems from the fact that in schizophrenia there is a breakdown, or split, between thoughts, emotions, and behavior.”
It is quite distinct from schizophrenia, he says. “Schizophrenia is a thought disorder,” he explains, “The myth likely stems from the fact that in schizophrenia there is a breakdown, or split, between thoughts, emotions, and behavior.”
This split results in the person confusing reality and fantasy, Dr. Rego explains. “The person may experience delusions and hallucinations, and emotions may become blunted or inappropriate,” he explains. When most people think of schizophrenia, they think of someone who is seeing things and hearing voices, Dr. Rego points out. “These are what are called positive symptoms, but people with schizophrenia have negative symptoms, too,” he says. Among the common negative symptoms are low motivation, difficulty forming social connections, and a flat, blunted affect, Dr. Rego says. A lack of pleasure in everyday activities, rarely speaking, and difficulty paying attention are also symptoms, according to the American Psychological Association.
#2 Myth: Violence is common among individuals with schizophrenia.
Reality: It’s actually rare for someone with schizophrenia to be violent, says Dr. Rego. An individual with schizophrenia is much more likely to be the victim of violence rather than the perpetrator, he says. “They tend to struggle more to have the social benefits that most of us have,” Dr. Rego explains. “They may be homeless or staying in a shelter, where they may be singled out and assaulted.”
Some individuals with psychiatric disorders like schizophrenia do become aggressive, says Scott Ira Krakower, DO, assistant unit chief of psychiatry at Zucker Hillside Hospital in Glen Oaks, New York. “However, it is a myth that this is always the case,” he says. “A person can be aggressive and have an anger problem and not have schizophrenia,” he explains. Both medication and counseling can help with any signs of violent behavior, he says.
#3 Myth: People with schizophrenia can’t ever hold down a job.
Reality: Actually, some individuals, when stable, are able to function quite well, Dr. Rego says. “When they are being compliant with their medication and are engaged in some sort of psychosocial treatment, they are often quite functional,” he says. The National Alliance on Mental Illness estimates that as many as half of the two million Americans with schizophrenia can improve significantly or even recover completely if they get treatment. Dr. Rego refers to the “recovery model” of treatment for schizophrenia, and an article in the Current Opinion in Psychiatry.
Rego says. “When they are being compliant with their medication and are engaged in some sort of psychosocial treatment, they are often quite functional,” he says. The National Alliance on Mental Illness estimates that as many as half of the two million Americans with schizophrenia can improve significantly or even recover completely if they get treatment. Dr. Rego refers to the “recovery model” of treatment for schizophrenia, and an article in the Current Opinion in Psychiatry.
“Working appears to help people recover from schizophrenia, and recent advances in vocational rehabilitation have been shown to be effective in countries with differing economies and labor markets. A growing body of research supports the concept that empowerment is an important component of the recovery process,” the authors write.
About a quarter of young people with the disorder recover when treated within six months to two years, reports the American Psychological Association, and another 35 to 40% percent are improved enough after longer-term treatment to live fairly normal lives with only minor symptoms. What makes this possible is psychosocial support—psychotherapy, family education, and self-help groups that can help people with schizophrenia cope and regain their lives. Job training and vocational counseling also can be useful. Still, cautions Dr. Krakower, some patients have difficulty holding down a job. “And it’s okay for them to get additional treatment,” he says. “Sometimes they may need to be on disability, and that’s okay, too.”
What makes this possible is psychosocial support—psychotherapy, family education, and self-help groups that can help people with schizophrenia cope and regain their lives. Job training and vocational counseling also can be useful. Still, cautions Dr. Krakower, some patients have difficulty holding down a job. “And it’s okay for them to get additional treatment,” he says. “Sometimes they may need to be on disability, and that’s okay, too.”
#4 Myth: A person with schizophrenia can seem perfectly normal one moment and change into a different person the next.
Reality: A sudden dramatic change of character in individuals with schizophrenia is not the usual scenario, Dr. Rego says. In fact, it’s common for the signs and symptoms of this mental disorder to surface over time. “There are often soft signs that the illness is going to take root,” Dr. Rego says. In the typical progression of the illness, a person may first become flat, isolate more frequently, and decrease their participation in activities. Then a psychotic break could occur—from a stressor such as starting college, Dr. Rego says. “So it is more of a slow progression, with a waxing and waning course that occurs over months and years,” he explains.
Then a psychotic break could occur—from a stressor such as starting college, Dr. Rego says. “So it is more of a slow progression, with a waxing and waning course that occurs over months and years,” he explains.
#5. Myth: People with schizophrenia usually require long-term hospitalization.
Reality: Appropriate treatment today may include a combination of out-patient care, acute hospitalization, and longer-term hospitalization when needed, Dr. Krakower says. And, even when family support and financial resources are available, many patients still need inpatient treatment, he adds.
“But the treatment model for schizophrenia is moving away from longer-term hospitalization and toward outpatient treatment,” he says. “At times, individuals may benefit from going to a day program or a partial day hospital, where they can receive daily treatment. Therapy may vary from individual to group therapy and the medication of choice is usually second-generation antipsychotic agents (i.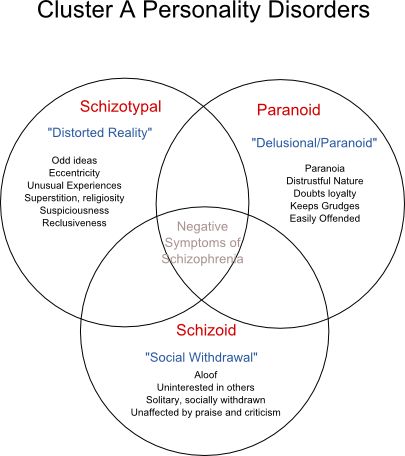 e. aripiprazole, clozapine, and risperidone).”
e. aripiprazole, clozapine, and risperidone).”
In a longer-care setting, the time can vary from weeks to months and depends on how the patient is progressing, Dr. Krakower says.
Long-term hospitalization may also be an indication that the person isn't getting enough support. “In some cases, society has failed them,” says Stephen Ferrando, MD, Director of Psychiatry at Westchester Medical Center Health Network (WMCHealth). “We are not providing enough services for them to succeed.”
#6. Myth: Bad parenting is what causes schizophrenia.
Years ago, it was believed that the mother or both parents were responsible if the child developed schizophrenia, Dr. Rego explains. While there is a genetic susceptibility—the disorder tends to run in families—there is absolutely no evidence that it is caused by how a person is parented, he says.
“Plus, even if your parent has schizophrenia your chances of getting it are less than 25 percent,” Dr. Ferrando explains.
So what does cause it? Rather than a single gene for schizophrenia, it’s likely that various genes, as well as environmental factors, are responsible, according to the American Psychological Association.
Environmental factors that may trigger the onset of schizophrenia can range from extreme academic stress to substance abuse. Dr. Ferrando says. “We know that extreme environmental stress like these situations can trigger the onset of schizophrenia,” he says.
If you or a loved one has been diagnosed with schizophrenia, it may feel scary. Understanding the reality of the disorder not only helps to erase the stigma surrounding the condition but also frees you up to focus on an effective treatment plan.
- “Have you got the wrong impression about schizophrenia?” 18 September 2017. BBC. http://www.bbc.com/news/health-41282282
- “Schizophrenia.” National Institute of Mental Health. Last updated November, 2017. https://www.nimh.nih.gov/health/statistics/schizophrenia.shtml
- "Schizophrenia Attitudes and Awareness." National Alliance on Mental Health. https://www.nami.org/About-NAMI/Publications-Reports/Survey-
- "Recovery from schizophrenia and the recovery model.
" Current Opinion in Psychiatry. https://www.ncbi.nlm.nih.gov/pubmed/19417668
- “Schizophrenia treatment.” American Psychological Association. http://www.apa.org/topics/schiz/treatment.aspx
- “Recognizing the signs of schizophrenia.” American Psychological Association. http://www.apa.org/helpcenter/recognizing-schizophrenia.aspx
Notes: This article was originally published March 5, 2018 and most recently updated October 2, 2020.
Rosemary Black
Rosemary Black is a veteran journalist who has written about food, health, fitness, and parenting for more than 25 years. A former senior editor at Everyday Health, she was food editor for the New York Daily News and Parade's Dash magazine. Rosemary, the author of four cookbooks, has written for QualityHealth.com and various other websites and magazines. The mom of 7 lives with her family in Westchester County, New York.
Schizophrenia is not a disease
Home > News > Schizophrenia is not a disease
| Psychiatrist Jim van Os is changing the way people think about schizophrenia. An article by Professor Van Os of the Maastricht University Medical Center with two colleagues was published at the beginning of November 2010 in the journal Nature . This work is a research-based perspective on schizophrenia. The title of the article is The environment and schizophrenia. It argues that the onset and development of schizophrenia still remain misunderstood, despite all the discovered genes involved in this disorder. Scientists are looking at genetic influences combined with environmental factors such as childhood abuse and trauma, cannabis use, social exclusion of minorities, and urban living. For studies have shown that the four environmental factors mentioned increase the likelihood of schizophrenia. Even in people without an increased genetic predisposition to develop schizophrenia. nine0003 According to the prevailing paradigm, approximately 15% of the population is genetically vulnerable to schizophrenia. Isn't it time to abandon this paradigm? According to Van Os, many researchers are not yet ready to accept this. They "dive deep" into DNA in search of an analogue of "dark matter". But more and more scientists doubt the existence of such "dark" genetic material. ""In recent years, environmental studies have brought more results, but attention to genes has noticeably decreased. It has already been clearly established that under adverse conditions in childhood and in an unfavorable living environment, schizophrenia can develop without a genetic predisposition. But genetic sensitivity, nevertheless, increases the risk of the disorder "". In an article published in a special issue of Nature on schizophrenia, Van Os writes about the interaction of genetic and environmental factors. nine0003 - Where does the idea that schizophrenia is primarily a hereditary disease come from? Van Os: ""Including from classic twin studies: with identical and dizygotic couples. With the advent of gene technology, researchers began to study all diseases with a high hereditary factor. To find matching genes as quickly as possible. They have indeed been found, but so far they explain only a very small part of the previously discovered hereditary factor. Real geneticists say: studies that mapped all DNA variants in a specific group of patients did not give the expected results, that is, there is another genetic explanation. Now they say that every schizophrenic patient has one or the other mutation: instead of a limited number of general variants that cannot explain schizophrenia, they now offer something special. The editors of Nature asked us and two other critics of the genetic approach to write down our thoughts on schizophrenia precisely because of the lack of progress in biological research in psychiatry. Every week you can read in the newspapers about a new discovery that will change everything radically. The reader does not understand that the fiftieth gene for schizophrenia has already been discovered, or that one part of the brain in a patient with schizophrenia has already been abnormally lit. Neuroscanning as a whole has also yielded little. "Bio-optimism" has dried up, and a different approach is required. nine0003 As far as we are concerned, we are trying to explain how a genetically determined disease can also be a socially determined disease. - And how is research going in this direction? Van Os: ""It is very common for patients to report psychic trauma or the use of cannabis products. This needs to be given more attention. Gene researchers don't hear these stories from patients because only a tube of blood comes into the lab, and that's it. Such researchers always say, "I don't believe in gene-environment interactions." According to my observations, there is a linear relationship between such statements and the number of patients they see with their own eyes. And in the old twin studies, social factors were almost never known. nine0003 - Why has there been so little research on the role of environmental factors in the past? Van Os: ""The methodology for studying environmental factors was not perfect enough. It's an observational study where you're looking for characteristics that appear at the same time, such as an increase in smoking and an increase in lung cancer. Such studies always raise some suspicions. - How can the methodology be improved? Van Os: ""In modern observational research, you conduct research in completely different environments, using the maximum number of different research schemes. If even then, under certain conditions of research, you again and again show a connection between the indicator of the environment and psychosis, then this is really something real. - Can you give a specific example? Van Os: ""Take the use of cannabis products and psychosis. Studies on the use of cannabis products show that the most common people can develop subtle and mild symptoms of psychosis. Large cohort studies show that users of cannabis products have higher rates of psychosis. In addition, there are, for example, experimental studies during which people smoked cigarettes with marijuana or placebo by lot. There is now also evidence of risks for residents of large cities, for people belonging to national minorities who feel disadvantaged and socially excluded, and for people who suffered childhood abuse or other mental trauma. Now we are planning to analyze the genetic component in such studies. - How are these studies organized? Van Os: ""A group of European schizophrenia researchers, all of whom used to work at the London Institute of Psychiatry, received 12 million euros from the European Union to study the effects of genes and environment. - How do you find such people? Van Os: "" Through surveys using questionnaires. Approximately 15% of the general population say they have had hallucinations or thoughts at least once in their lives that a computer is interfering with their brain. But in reality, a mental disorder is not only the number and severity of symptoms, but also the degree of subjective suffering of a person in connection with these symptoms. Some people hear voices and function perfectly, and some, after hearing them a couple of times, panic and run to a psychiatrist. So everything is relative. nine0003 - You deviate from the existing classification and conduct research, the essence of which is not whether a person suffers from a disorder or not, but to what extent this occurs. Van Os: ""When such reasoning is applied to depression or anxiety, it causes much less skepticism. Because every few days can be depressed. If this period lasts 2 weeks, and a person does not get out of it, then this is called depression. nine0003 There is strong evidence for a similar continuum for psychosis. This is a continuum of experiences that can be measured in society, including paranoid ideas, transient hallucinations, motivational disorders, and subtle changes in thinking. Just like in schizophrenia, only much more subtle, because the population has its own gradient. There is much more evidence here than the molecular genetics of schizophrenia provides. It's time for a paradigm shift, and that's why we can now write about this topic in Nature"". nine0003 - What are the benefits of such research for doctors and patients? Do we already know that some environmental factors can be dangerous, especially for children and young adults? Van Os: ""It's important for prevention. - What kind of lifestyle can prevent schizophrenia? Van Os: "You can teach people who are sensitive to psychosis to get up in the morning with the thought 'I have a lot of opportunity'." You can also get up with the thought that you are again entering the same circular track, that your life is determined by others, and you yourself cannot control your environment in any way. Naturally, such a thought may come, because it may be your reality. For example, you work in the secretariat and your job is to do what others throw at your desk. You should refuse this. But often we drive ourselves mentally into a negative spiral, forgetting that contacts and a social network can cause positive feelings and generate optimism. For this purpose, special forms of psychotherapy have been developed, and recent studies show that this is very good for your health. nine0003 - Leaving aside getting up in the morning, don't you think the danger is a bit more serious? Van Os: ""There is some confusion about schizophrenia. At the same time, the entire diagnostic system is based on the use of dichotomous categories: you either have something or not, one disorder or another. At the same time, in clinical practice there may be confusion with labels - with the same symptoms, one psychiatrist will put "schizophrenia" and another - "depression", so it's not about labels, but about whether a particular person needs in help. nine0003 In the modern sense, schizophrenia is a disorder in which four groups of symptoms converge, which in ordinary life occur very often - in a mild form and separately from each other - in 10-20% of the population. It seems to me that it is more correct to consider this disorder multidimensionally (dimentional), i.e. assessing the severity of each group of symptoms. In the DSM-IV, symptoms of varying severity and from different groups are referred to as various illnesses. - Why are there so many diagnoses in DSM - IV ? Van Os: "" DSM-IV was published in 1994 after a very complex process. DSM is an initiative of an American professional organization that brings together psychiatrists - the American Psychiatric Association (APA). First of all, American psychiatrists needed a clear illness, a very severe one, in which psychotherapy does not help. Just as neurologists have well-defined brain diseases, so psychiatrists wanted something that could be treated with pills. Well, and to separate from the rising psychology, because psychologists do not have the right to prescribe drugs. Then the criteria for schizophrenia were so narrowed that only the most seriously ill patients fell under them. - You are a member of the DSM - V Working Group on Psychosis and Schizophrenia. How did you get into this group with your different from the American ""European"" way of thinking? Van Os: ""APA wanted to update the DSM-V with the latest science. I was invited because of my publications about these four groups of symptoms, because I considered this disorder multidimensionally. In addition to me, the psychosis working group includes ten Americans, one German and one British. After three years of working together, we have learned to reach agreement. nine0003 - And what is the result? Van Os: "We are going to submit a proposal to the APA for the term 'psychotic syndromes'. - So, you want the name "schizophrenia" out of use. Last year you suggested calling schizophrenia in the future " salience syndrome "". Van Os: ""No, this name has a lot of drawbacks. The word Salience is very difficult to translate. It means something like "importance of meaning". We suggest that the APA work with the WHO to look for a new name for this disorder. ""Schizophrenia"" means that you are suffering from a serious illness with a real Greek name, in which little depends on the patient himself. If you in the company say that you have depression, then everyone will immediately understand that we are talking about an increase or decrease in mood. If you say that you have schizophrenia, then people will not have the slightest idea what is wrong with you "". nine0003 - If it's not "" salience syndrome "", then what? Van Os: ""The new name will not appear until about ten years later. Although in Asia things are moving very fast. Since 2002, schizophrenia has been called integration dysregulation syndrome in Japan. The name was also changed in Hong Kong - to thought-perception dysregulation syndrome ("syndrome of dysregulation of thinking and perception""). Help : Johannes Jacobus (Jim) van Os was born in 1960; studied medicine in Amsterdam and psychiatry in London. After that, he worked in psychiatric clinics in Jakarta, Casablanca, Bordeaux and London. Van Os is Professor of Psychiatric Epidemiology at the University of Maastricht and "Guest Lecturer" at the Institute of Psychiatry in London. Together with colleagues, he develops the latest forms of assistance to psychiatric patients. He and his research team have identified various new risk factors for psychosis, anxiety and depression. In 2010, for the fourth year in a row, he was named the best psychiatrist in the country by the Dutch medical community. Van Os is also a member of the DSM-V Psychotic Disorders Section Working Group. Source: Schizofrenie is geen ziekte. – NRC Handelsblad, 11/13/10, Sect. Wetenschap, p. 4-5. Source: mniip.org
|
ISSN 2588-0519 (Print)
ISSN 2618-8473 (Online)
Schizophrenia
Schizophrenia- Health »
- A
- B
- C
- Г
- Д
- Е
- Ё
- Ж
- З
- И
- К
- Л
- М
- Н
- О
- П
- Р
- С
- Т
- У
- Ф
- Х
- Ц
- Ч
- Ш
- Щ
- Ъ
- Ы
- Ь
- Э
- Ю
- Я
- Popular Topics
- Air pollution nine1 М
- Н
- О
- П
- Р
- С
- Т
- У
- Ф
- Х
- Ц
- Ч
- Ш
- Щ
- Ъ
- Ы
- L
- E
- J
- R
- WHO in countries »
- Reporting
- Regions »
- Africa
- America
- Southeast Asia nine0192
- Europe
- Eastern Mediterranean
- Western Pacific
- Media Center
- Press releases
- Statements
- Media messages
- Comments
- Reporting
- Online Q&A
- Developments
- Photo reports
- Questions and answers
- Update
- Emergencies "
- News "
- Disease Outbreak News
- WHO data »
- Dashboards »
- COVID-19 Monitoring Dashboard
- Highlights "
- About WHO »
- General director
- About WHO
- WHO activities nine0192
- Where does WHO work?
- Governing Bodies »
- World Health Assembly
- Executive committee
- Main page/
- Media Center/
- Newsletters/
- Read more/
- Schizophrenia
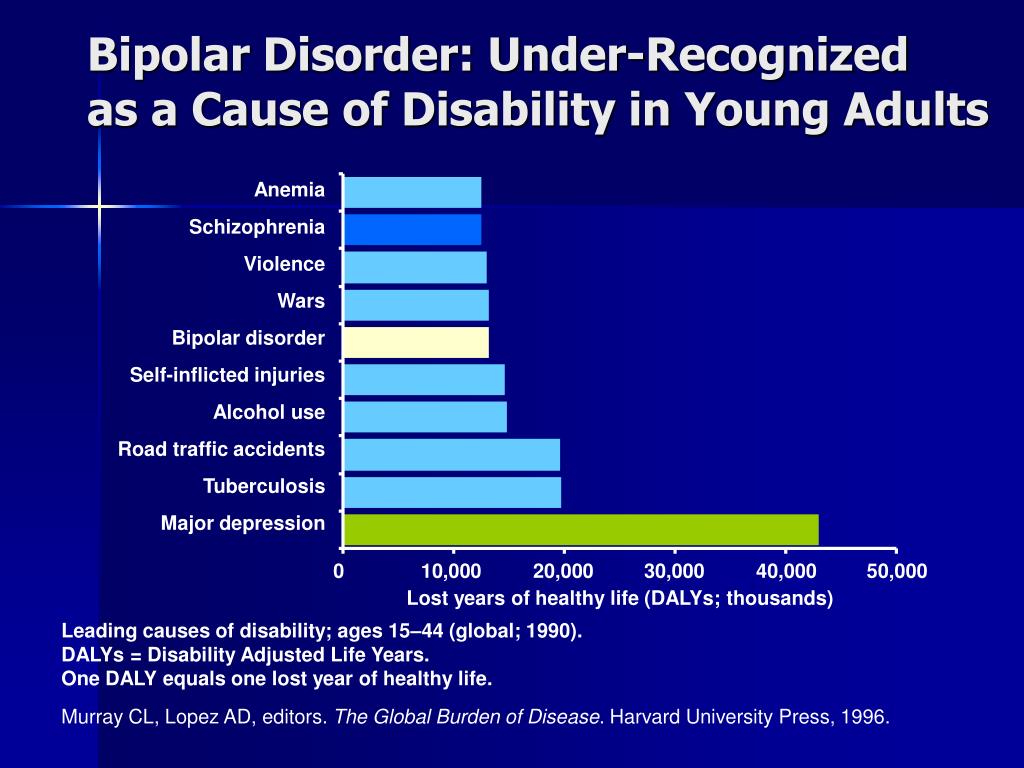
Basic Facts- Schizophrenia is a severe mental disorder that affects approximately 24 million people, or 1 in 300 people worldwide.
 nine0167
nine0167 - Schizophrenia causes psychosis, is associated with severe disability, and can negatively affect all areas of life, including personal, family, social, academic and work life.
- People with schizophrenia are often subject to stigma, discrimination and human rights violations.
- Worldwide, more than two thirds of people with psychosis do not receive specialized mental health care.
- There are a number of effective options for helping patients with schizophrenia, which can lead to a complete recovery of at least one in three patients.
Symptoms
Schizophrenia is characterized by significant disturbances in the perception of reality and behavioral changes, such as: nine0192
- persistent hallucinations: the patient hears, sees, touches non-existent things and smells non-existent smells;
- sensation of external influence, control or passivity: the presence in the patient of the sensation that his feelings, impulses, actions or thoughts are dictated from outside, put in or disappear from consciousness by someone else's will, or that his thoughts are broadcast to others;
- disorganized thinking, often expressed in incoherent or pointless speech;
- significant disorganization of behavior, such as the patient doing things that may seem strange or meaningless, or an unpredictable or inappropriate emotional response that prevents the patient from organization of their behavior; nine0192
- "negative symptoms" such as extreme poverty of speech, smoothness of emotional reactions, inability to feel interest or pleasure, social autism; and/or
- extreme arousal or, conversely, slowness of movement, freezing in unusual positions.
People with schizophrenia often also experience persistent cognitive or thinking problems that affect memory, attention, or problem-solving skills.
At least one third of patients with schizophrenia experience complete remission of symptoms (1). In some, periods of remission and exacerbation of symptoms follow each other throughout life, in others there is a gradual increase in symptoms. nine0003
Magnitude of the problem and impact
Schizophrenia affects approximately 24 million people, or 1 in 300 people (0.32%) worldwide. Among adults, the rate is 1 in 222 (0.45%) (2). Schizophrenia is less common than many other mental disorders. Onset is most common in late adolescence and between the ages of 20 and 30; while women tend to have a later onset of the disease. nine0003
Schizophrenia is often accompanied by significant stress and difficulties in personal relationships, family life, social contacts, studies, work or other important areas of life.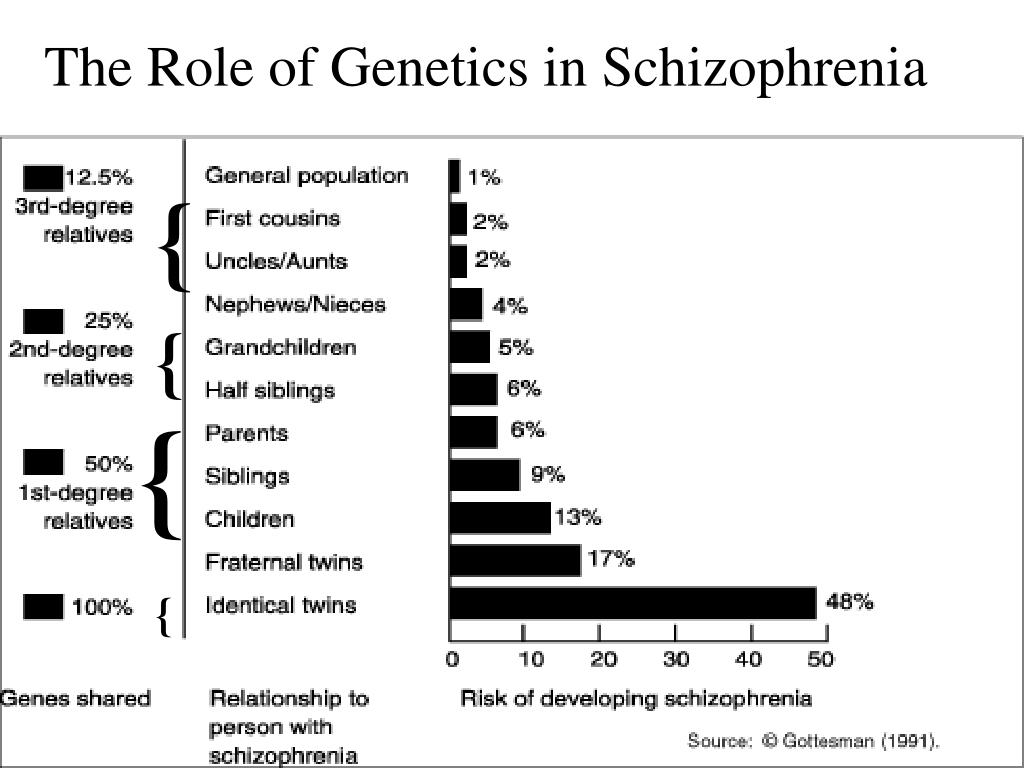
Individuals with schizophrenia are 2-3 times more likely to die early than the population average (2). It is often associated with physical illnesses such as cardiovascular disease, metabolic disease, and infectious disease.
Patients with schizophrenia often become the object of human rights violations both within the walls of psychiatric institutions and in everyday life. Significant stigmatization of people with this disease is a widespread phenomenon that leads to their social isolation and has a negative impact on their relationships with others, including family and friends. This creates grounds for discrimination, which in turn limits access to health services in general, education, housing and employment. nine0003
Humanitarian emergencies and health crises can cause intense stress and fear, disrupt social support mechanisms, cause isolation and disrupt health services and supply of medicines. All these shocks can have a negative impact on the lives of people with schizophrenia, in particular by exacerbating existing symptoms of the disease.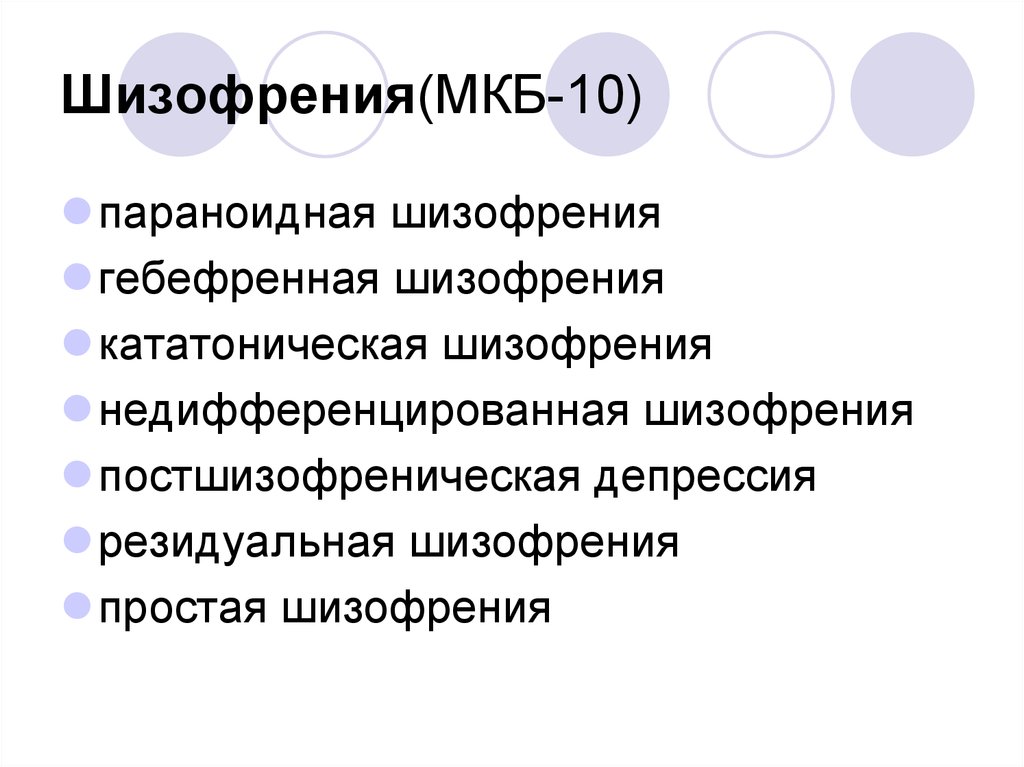 People with schizophrenia are more vulnerable during emergencies to various human rights violations and, in particular, face neglect, abandonment, homelessness, abuse and social exclusion. nine0003
People with schizophrenia are more vulnerable during emergencies to various human rights violations and, in particular, face neglect, abandonment, homelessness, abuse and social exclusion. nine0003
Causes of schizophrenia
Science has not established any one cause of the disease. It is believed that schizophrenia may be the result of the interaction of a number of genetic and environmental factors. Psychosocial factors may also influence the onset and course of schizophrenia. In particular, heavy marijuana abuse is associated with an increased risk of this mental disorder.
Assistance services
At present, the vast majority of people with schizophrenia do not receive mental health care worldwide. Approximately 50% of patients in psychiatric hospitals are diagnosed with schizophrenia (4). Only 31.3% of people with psychosis get specialized mental health care (5). Much of the resources allocated to mental health services are inefficiently spent on the care of patients admitted to psychiatric hospitals.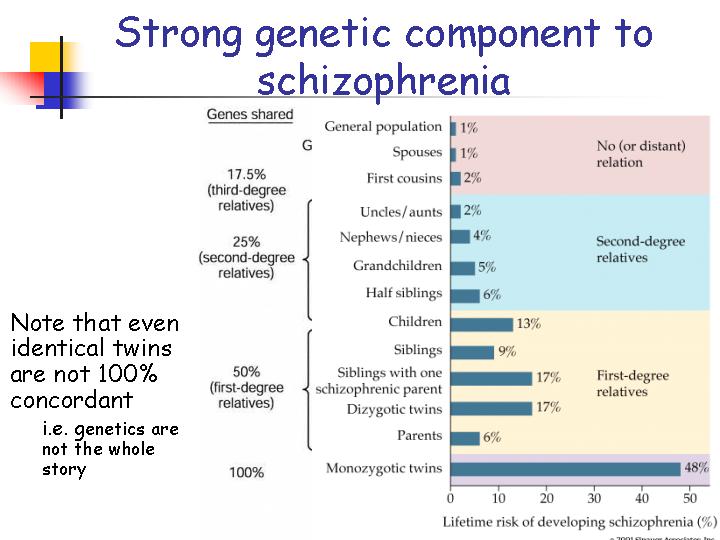
Available scientific evidence clearly indicates that hospitalization in psychiatric hospitals is not an effective way of providing care for mental disorders and is regularly associated with the violation of the basic rights of patients with schizophrenia. Therefore, it is necessary to ensure the expansion and acceleration of work on the transfer of functions in the field of mental health care from psychiatric institutions to the level of local communities. Such work should begin with the organization of the provision a wide range of quality community-based mental health services. Options for community-based mental health care include integrating this type of care into primary health care and hospital care. general care, setting up community mental health centres, outpatient care centres, social housing with nursing care and social home care services. Involvement in the care process is important the patient with schizophrenia, his family members and members of local communities.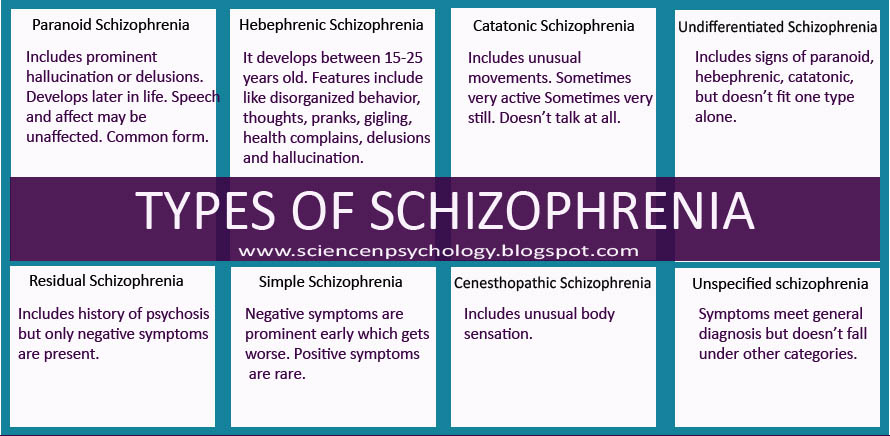 nine0003
nine0003
Schizophrenia management and care
There are a number of effective approaches to treating people with schizophrenia, including medication, psychoeducation, family therapy, cognitive behavioral therapy, and psychosocial rehabilitation (eg, life skills education). The most important interventions for helping people with schizophrenia are assisted living, special housing and employment assistance. It is extremely important for people with schizophrenia and their families and/or caregivers to a recovery-centered approach that empowers people to participate in decisions about their care. nine0003
WHO activities
steps are in place to ensure that appropriate services are provided to people with mental disorders, including schizophrenia. One of the key recommendations The action plan is to transfer the function of providing assistance from institutions to local communities. WHO Special Mental Health Initiative aims to further progress towards the goals of the Comprehensive Plan mental health action 2013–2030 by ensuring that 100 million more people have access to quality and affordable mental health care. nine0003
nine0003
The WHO Mental Health Gap Action Program (mhGAP) is developing evidence-based technical guidelines, tools and training packages to scale up services in countries, especially in low-resource settings. The program focuses on a priority list of mental health disorders, including psychosis, and aims to strengthen the capacity of non-specialized health workers in as part of an integrated approach to mental health care at all levels of care. To date, the mhGAP Program has been implemented in more than 100 WHO Member States. nine0003
The WHO QualityRights project aims to improve the quality of care and better protect human rights in mental health and social care settings and to expand opportunities of various organizations and associations to defend the rights of persons with mental disorders and psychosocial disabilities.
The WHO guidelines on community mental health services and human rights-based approaches provide information for all stakeholders who intend to develop or transform mental health systems and services.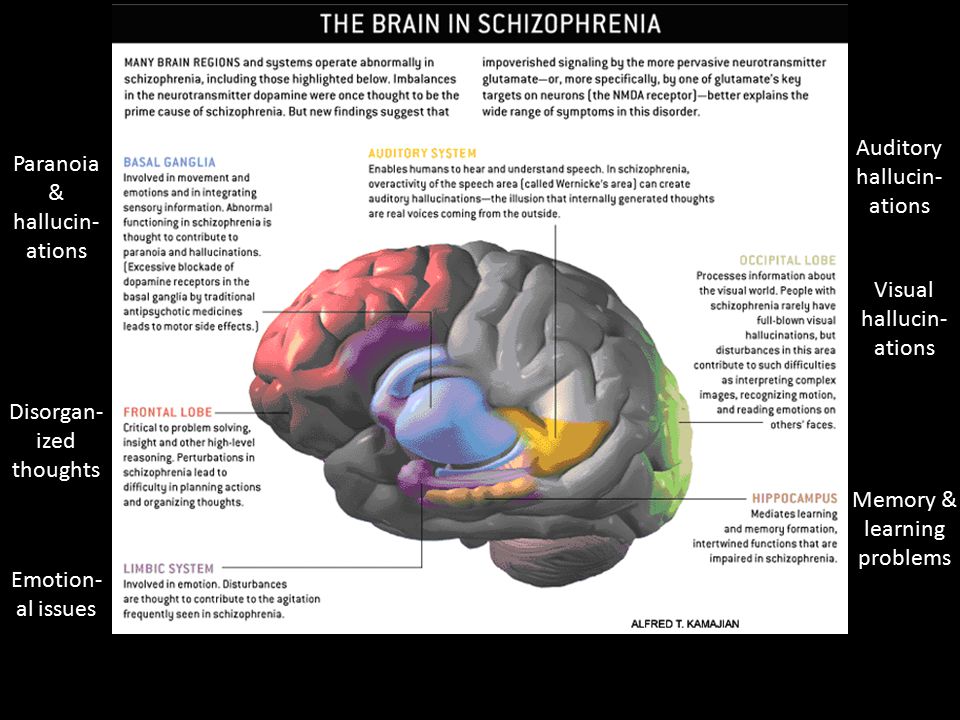
 The participants in this study were both patients and people vulnerable to schizophrenia, i.e. first-degree relatives of patients with schizophrenia. They also study the reactions of brain tissue to cannabis. One thing is present in all these studies: people who consume more cannabis products are more likely to have psychosis and schizophrenia. What is the cause and what is the effect has not yet been proven, but the connection itself is present. nine0003
The participants in this study were both patients and people vulnerable to schizophrenia, i.e. first-degree relatives of patients with schizophrenia. They also study the reactions of brain tissue to cannabis. One thing is present in all these studies: people who consume more cannabis products are more likely to have psychosis and schizophrenia. What is the cause and what is the effect has not yet been proven, but the connection itself is present. nine0003  At the same time, we study genes, lifestyle and life circumstances in patients and healthy people. We also study people with familial vulnerability (ground) or psychometric vulnerability, which means that they have more psychotic experiences." nine0003
At the same time, we study genes, lifestyle and life circumstances in patients and healthy people. We also study people with familial vulnerability (ground) or psychometric vulnerability, which means that they have more psychotic experiences." nine0003  In the picture of such a continuum, each will have its own indicator. Will we all be patients as a result?
In the picture of such a continuum, each will have its own indicator. Will we all be patients as a result? 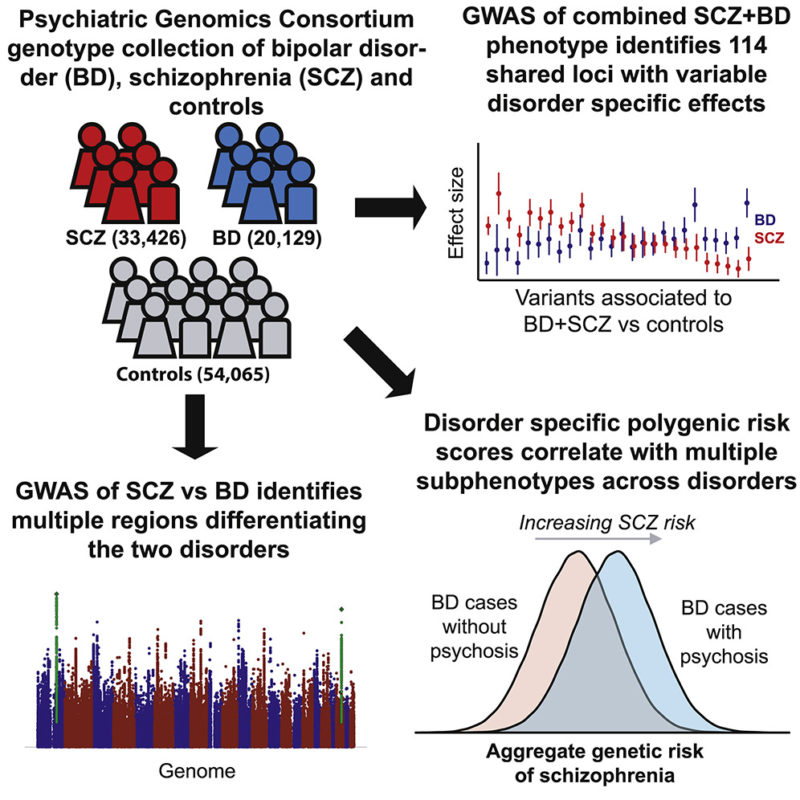 We see that for schizophrenia, lifestyle is no less important than for diseases of the heart and blood vessels.
We see that for schizophrenia, lifestyle is no less important than for diseases of the heart and blood vessels. 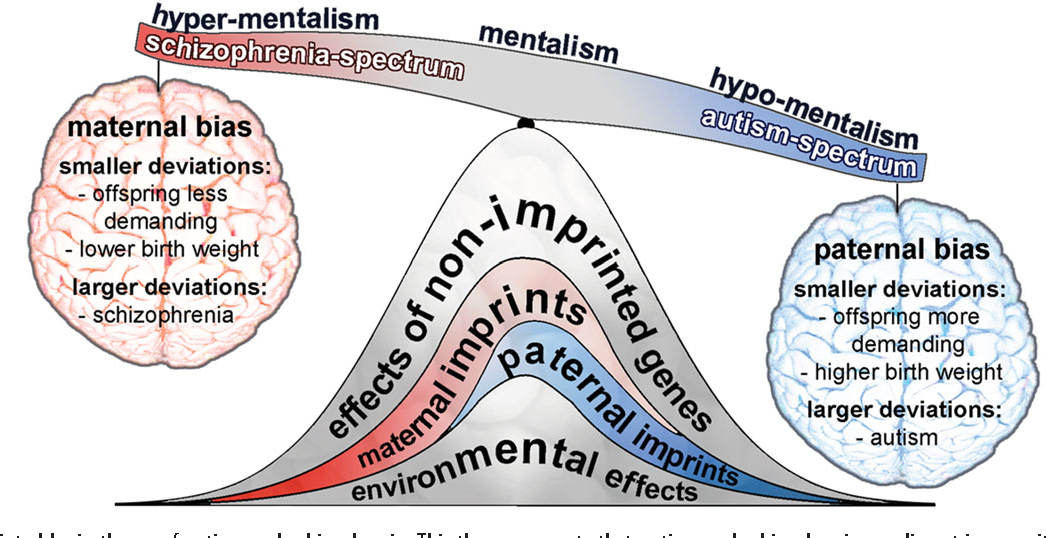 The current version of the American DSM-IV defines schizophrenia, based on the duration and severity of the illness, as the most severe form of the entire spectrum of "schizoid" disorders.
The current version of the American DSM-IV defines schizophrenia, based on the duration and severity of the illness, as the most severe form of the entire spectrum of "schizoid" disorders.  In addition to the diagnosis of schizophrenia, there are about 25 different psychotic diagnoses in the psychosis and schizophrenia section of the DSM-IV. This is too much. Overall, I think that categorizing disorders has done more harm than good. nine0003
In addition to the diagnosis of schizophrenia, there are about 25 different psychotic diagnoses in the psychosis and schizophrenia section of the DSM-IV. This is too much. Overall, I think that categorizing disorders has done more harm than good. nine0003 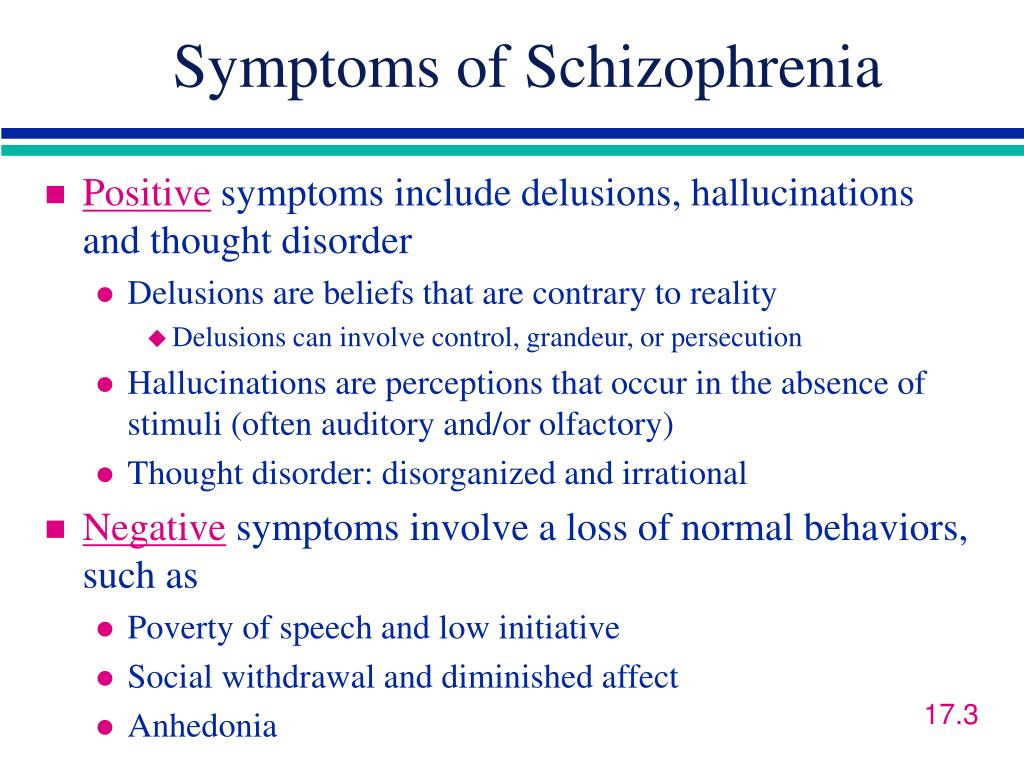 For less severe psychotic syndromes, other diagnostic categories have been created. Social scientists are now working on the reconstruction of this story, and this is important, because then we will see how we in the Western world look at "" madness "". nine0003
For less severe psychotic syndromes, other diagnostic categories have been created. Social scientists are now working on the reconstruction of this story, and this is important, because then we will see how we in the Western world look at "" madness "". nine0003  " Instead of the disease "schizophrenia" there will be a schizophrenic syndrome. Schizophrenia is not a disease. This is the essence of the change. In addition, it will be possible to determine the severity of symptoms within the framework of the schizophrenic syndrome. Thus, the doctor will be able to make a diagnosis, and at the same time clarify the symptoms and their severity. But whoever wants to can continue to use many of the old diagnoses. Giving them up right away is too big a step. It should not be forgotten that journals were written on the basis of DSM-IV diagnoses and departments at universities were named, health insurance systems and the pharmaceutical industry worked. It is my hope that in the coming years the notion that schizophrenia is a well-defined illness with known causes, treatments and course will disappear. It is declared, but in fact it is not true"". nine0003
" Instead of the disease "schizophrenia" there will be a schizophrenic syndrome. Schizophrenia is not a disease. This is the essence of the change. In addition, it will be possible to determine the severity of symptoms within the framework of the schizophrenic syndrome. Thus, the doctor will be able to make a diagnosis, and at the same time clarify the symptoms and their severity. But whoever wants to can continue to use many of the old diagnoses. Giving them up right away is too big a step. It should not be forgotten that journals were written on the basis of DSM-IV diagnoses and departments at universities were named, health insurance systems and the pharmaceutical industry worked. It is my hope that in the coming years the notion that schizophrenia is a well-defined illness with known causes, treatments and course will disappear. It is declared, but in fact it is not true"". nine0003  What's up with this name?
What's up with this name?  South Korea will follow. There the name is of great importance, because "schizophrenia" carries a connotation of mystification. Anyone who in Asian culture - especially in Japan - receives this label, in reality receives an order to commit suicide "". nine0003
South Korea will follow. There the name is of great importance, because "schizophrenia" carries a connotation of mystification. Anyone who in Asian culture - especially in Japan - receives this label, in reality receives an order to commit suicide "". nine0003  nine0003
nine0003