Bipolar disorder care plan
6 Bipolar Disorders Nursing Care Plans
Home » Nursing Care Plans » 6 Bipolar Disorders Nursing Care Plans
Updated on
By Paul Martin, BSN, R.N.
ADVERTISEMENTS
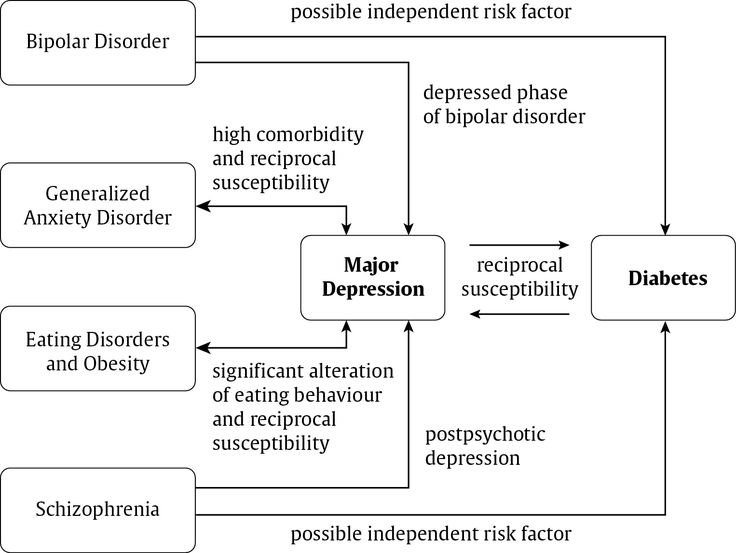
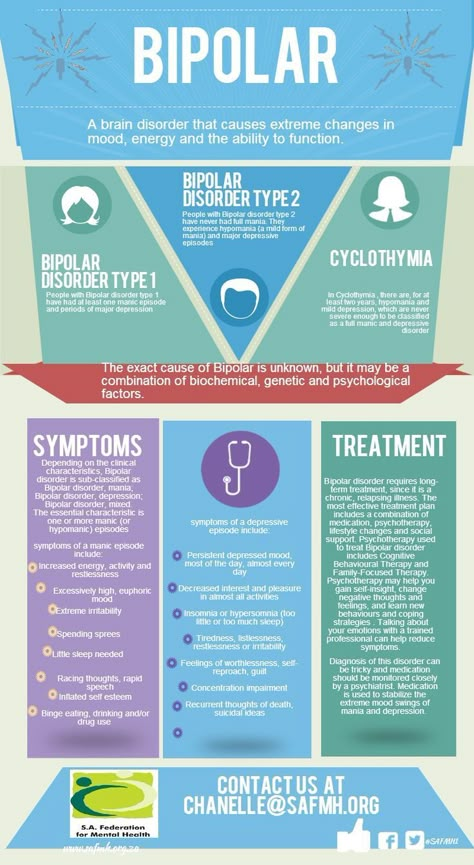
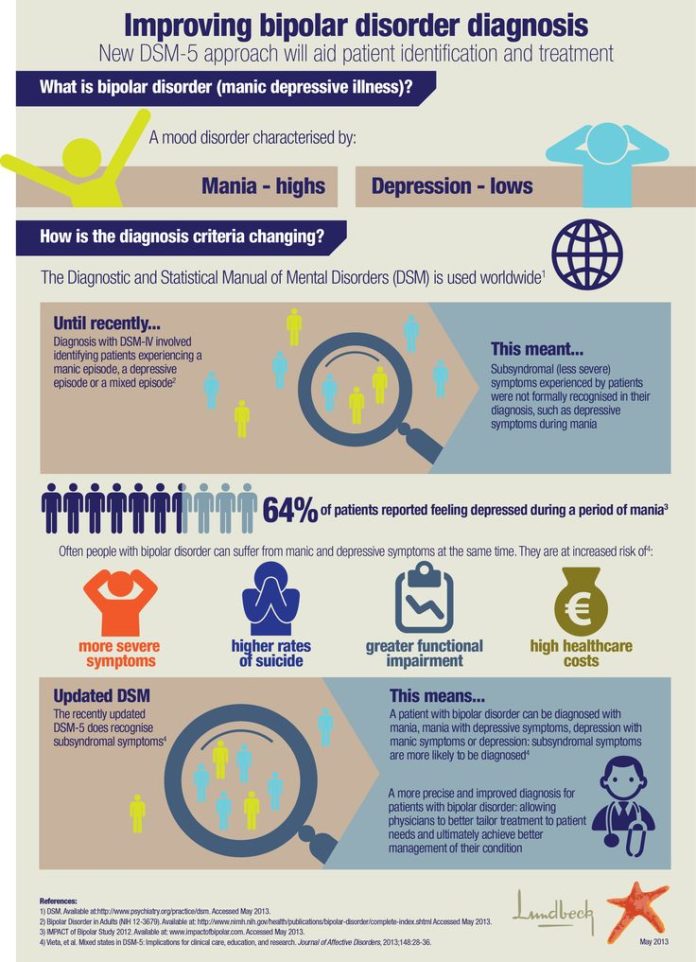
Bipolar disorders are mood disorders that comprise of one or more manic or hypomanic episode and usually one or more depressive episodes with periods of relatively normal functioning in between. They are said to be linked to biochemical imbalances in the brain and it is said that the disease is genetically transferred.
Nursing Care PlansClients with bipolar disorders are at a high risk for suicide. Although clients in the manic phase are briefly agitated, energized and elated, their underlying depression makes them likely to inflict self-injury.
Essential responsibilities of nurses are to provide a safe environment, to improve the self-esteem, to meet the physiologic needs and to guide patients toward socially appropriate behavior.
Here are six nursing care plans and nursing diagnosis for bipolar disorders:
ADVERTISEMENTS
- Risk For Injury
- Risk For Violence: Self-Directed or Other Directed
- Impaired Social Interaction
- Ineffective Individual Coping
- Interrupted Family Processes
- Total Self-Care Deficit
ADVERTISEMENTS
Risk For InjuryNursing Diagnosis
- Risk for Injury
Risk factors
- Affective, cognitive, and psychomotor factors.
- Biochemical/neurologic imbalances.
- Exhaustion and dehydration.
- Extreme hyperactivity/physical agitation.
- Rage reaction.
Possibly evidenced by
- Abrasions, bruises, cuts from running/falling into objects.
- Extreme hyperactivity.
- Impaired judgment (reality-testing, risk behavior).
- Lack of fluid ingestion.
- Lack of control over purposeless and potentially injurious movements.

Desired Outcomes
- Patient will respond to the medication within the therapeutic levels.
- Patient will sustain optimum health through medication management and therapeutic regimen.
- Patient will have stable cardiac status while in the hospital.
- Patient will drink 8 oz of fluid every hour throughout the day while on acutely manic stage.
- Patient will remain free from falls and abrasions every day while in the hospital.
- Patient will be free of dangerous levels of hyperactive motor behavior with the aid of medications and nursing interventions within the first 24 hours.
- Patient will spend time with the nurse in a quiet environment three to four times a day between 7 am and 11 pm with the aid of nursing guidance.
- Patient will take short voluntary rest periods during the day.
- Patient will be free of excessive physical agitation and purposeless motor activity within 2 weeks.
- Patient will be free of injury within 2 to 3 weeks:
- Stable cardiac status.
- Skin free of abrasions and scrapes.
- Well dehydrated.
- Stable cardiac status.
| Nursing Interventions | Rationale |
|---|---|
| Provide structured solitary activities with the assistance of a nurse or aide. | Structure provides focus and security. |
| Provide frequent rest periods. | Prevents exhaustion. |
| Provide frequent high-calorie fluids (e.g., fruit shake, milk). | Prevents the risk of serious dehydration. |
| Maintain a low level of stimuli in client’s environment (e.g., loud noises, bright light, low-temperature ventilation). | Helps minimize escalation of anxiety. |
| Acute mania might warrant the use of phenothiazines and seclusions to decrease any physical harm. | Exhaustion and death result from dehydration, lack of sleep, and constant physical activity. |
Observe for signs of lithium toxicity (e.g., nausea, vomiting, diarrhea, drowsiness, muscle weakness, tremor, lack of coordination, blurred vision, or ringing in your ears).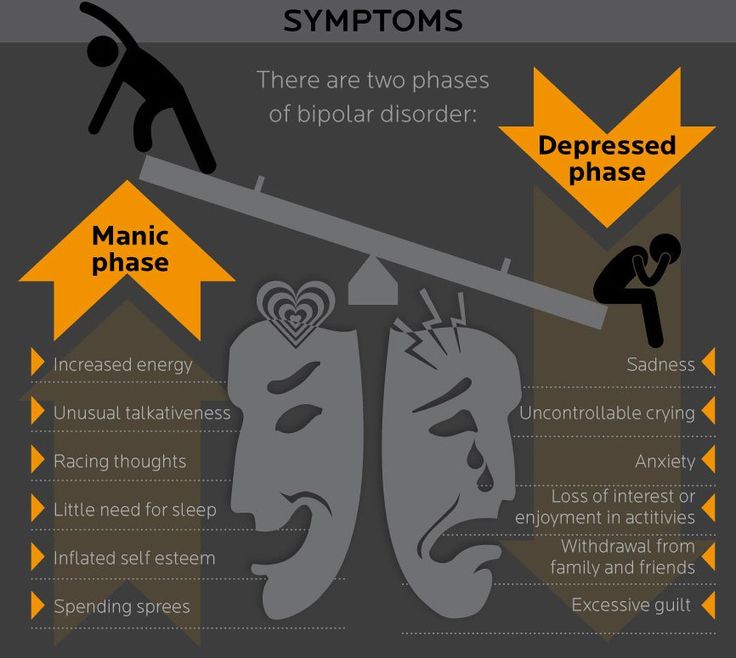 | There is a small margin of safety between therapeutic and toxic doses. |
| Protect client from giving away money and possessions. Hold valuables in a hospital safe until rational judgment returns. | Client’s “generosity” is a manic defense that is consistent with irrational, grandiose thinking. |
| Redirect violent behavior. | Physical exercise can decrease tension and provide focus. |
ADVERTISEMENTS
Recommended ResourcesRecommended nursing diagnosis and nursing care plan books and resources.
Disclosure: Included below are affiliate links from Amazon at no additional cost from you. We may earn a small commission from your purchase. For more information, check out our privacy policy.
- Nursing Care Plans: Nursing Diagnosis and Intervention (10th Edition)
This an awesome book to help you create and customize effective nursing care plans.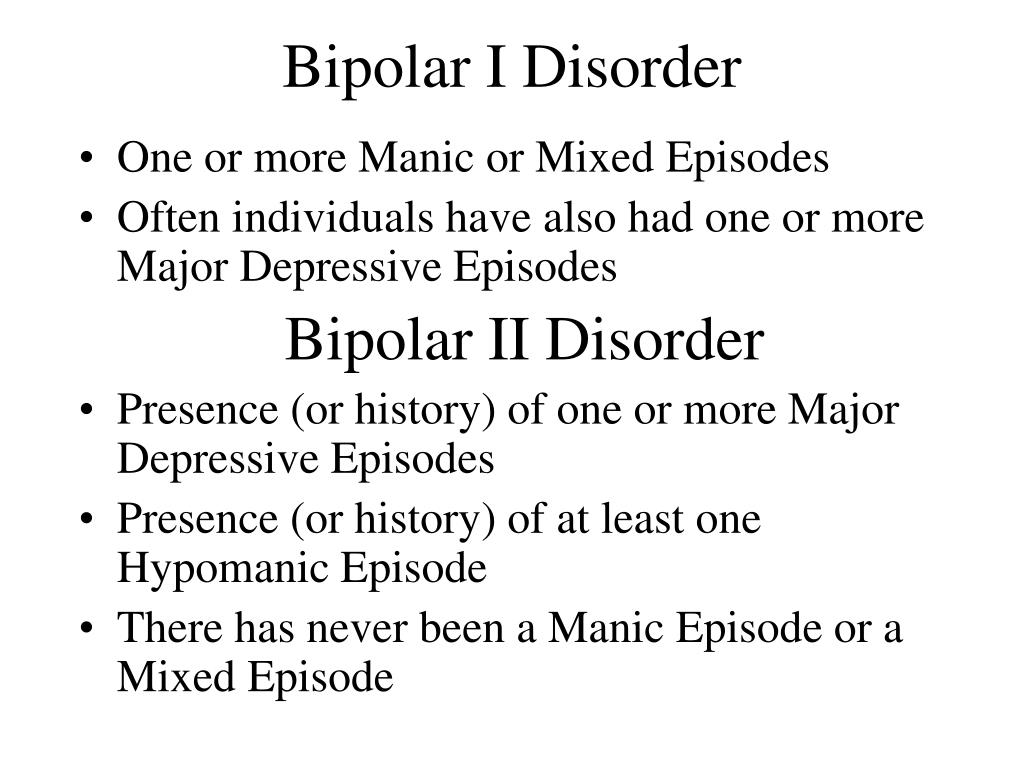 We highly recommend this book for its completeness and ease of use.
We highly recommend this book for its completeness and ease of use. - Nurse’s Pocket Guide: Diagnoses, Prioritized Interventions and Rationales
A quick-reference tool to easily select the appropriate nursing diagnosis to plan your patient’s care effectively. - NANDA International Nursing Diagnoses: Definitions & Classification, 2021-2023 (12th Edition)
The official and definitive guide to nursing diagnoses as reviewed and approved by the NANDA-I. This book focuses on the nursing diagnostic labels, their defining characteristics, and risk factors – this does not include nursing interventions and rationales. - Nursing Diagnosis Handbook, 12th Edition Revised Reprint with 2021-2023 NANDA-I® Updates
Another great nursing care plan resource that is updated to include the recent NANDA-I updates. - Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5(TM))
Useful for creating nursing care plans related to mental health and psychiatric nursing.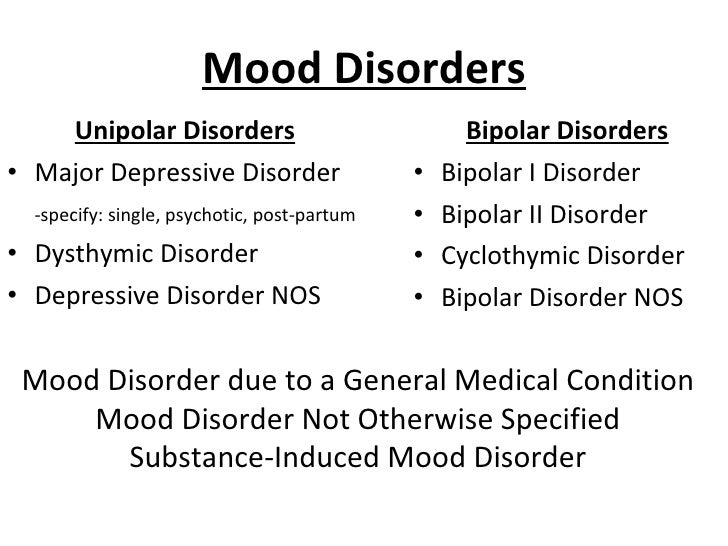
- Ulrich & Canale’s Nursing Care Planning Guides, 8th Edition
Claims to have the most in-depth care plans of any nursing care planning book. Includes 31 detailed nursing diagnosis care plans and 63 disease/disorder care plans. - Maternal Newborn Nursing Care Plans (3rd Edition)
If you’re looking for specific care plans related to maternal and newborn nursing care, this book is for you. - Nursing Diagnosis Manual: Planning, Individualizing, and Documenting Client Care (7th Edition)
An easy-to-use nursing care plan book that is updated with the latest diagnosis from NANDA-I 2021-2023. - All-in-One Nursing Care Planning Resource: Medical-Surgical, Pediatric, Maternity, and Psychiatric-Mental Health (5th Edition)
Definitely an all-in-one resource for nursing care planning. It has over 100 care plans for different nursing topics.
Other recommended site resources for this nursing care plan:
- Nursing Care Plans (NCP): Ultimate Guide and Database MUST READ!
Over 150+ nursing care plans for different diseases and conditions.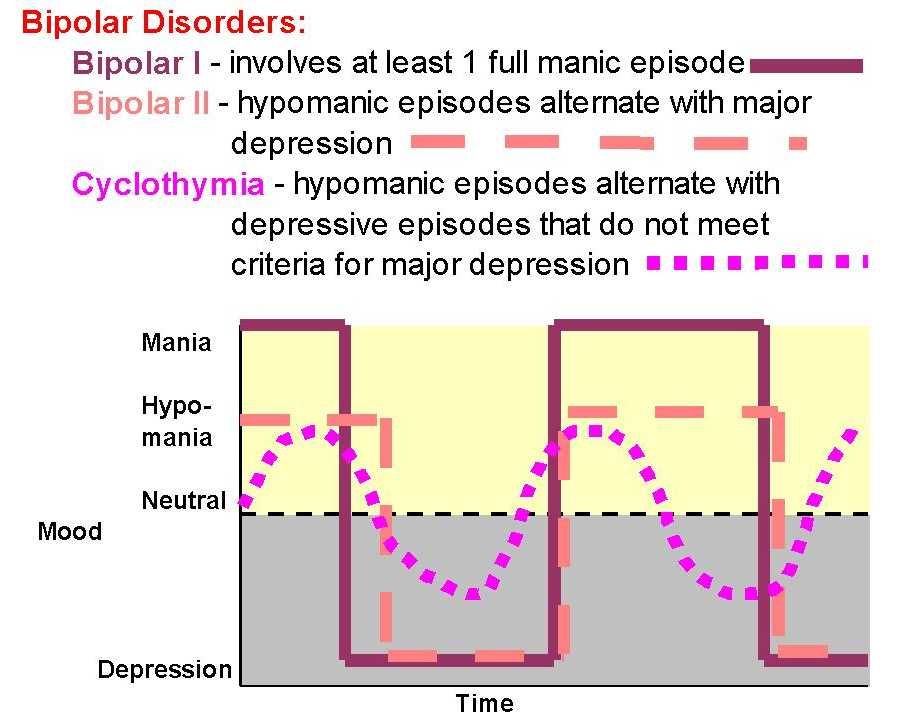 Includes our easy-to-follow guide on how to create nursing care plans from scratch.
Includes our easy-to-follow guide on how to create nursing care plans from scratch. - Nursing Diagnosis Guide and List: All You Need to Know to Master Diagnosing
Our comprehensive guide on how to create and write diagnostic labels. Includes detailed nursing care plan guides for common nursing diagnostic labels.
Other care plans for mental health and psychiatric nursing:
- Alcohol Withdrawal | 5 Care Plans
- Anxiety and Panic Disorders | 7 Care Plans
- Bipolar Disorders | 6 Care Plans
- Major Depression | 9 Care Plans
- Personality Disorders | 4 Care Plans
- Schizophrenia | 6 Care Plans
- Sexual Assault | 1 Care Plan
- Substance Dependence and Abuse | 8 Care Plans
- Suicide Behaviors | 3 Care Plans
ADVERTISEMENTS
Categories Mental Health and Psychiatric Care Plans, Nursing Care Plans Tags Impaired Social Interaction, ineffective coping, Ineffective Individual Coping, Interrupted Family Processes, risk for injury, Risk For Violence: Self-Directed or Other Directed, self-care deficit, Total Self-Care Deficit
Paul Martin, BSN, R.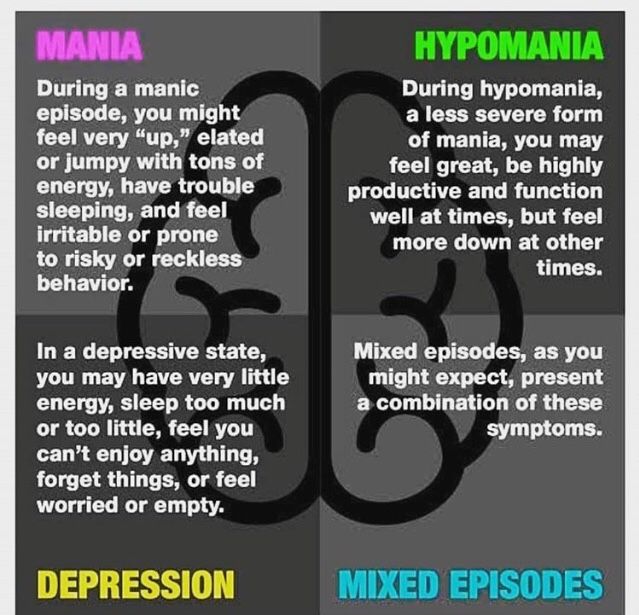 N.
N.
Paul Martin is a registered nurse with a bachelor of science in nursing since 2007. Having worked as a medical-surgical nurse for five years, he handled different kinds of patients and learned how to provide individualized care to them. Now, his experiences working in the hospital is carried over to his writings to help aspiring students achieve their goals. He is currently working as a nursing instructor and have a particular interest in nursing management, emergency care, critical care, infection control, and public health. As a writer at Nurseslabs, his goal is to impart his clinical knowledge and skills to students and nurses helping them become the best version of themselves and ultimately make an impact in uplifting the nursing profession.
© 2023 Nurseslabs | Ut in Omnibus Glorificetur Deus!
Bipolar Disorder Nursing Care Management Guide
Updated on
By Marianne Belleza, R. N.
N.
ADVERTISEMENTS
Bipolar disorders are mood disorders characterized by mood swings from profound depression to extreme euphoria (mania), with intervening periods of normalcy. Learn about the nursing management, assessment, diagnosis, and care planning for bipolar disorder in this study guide.
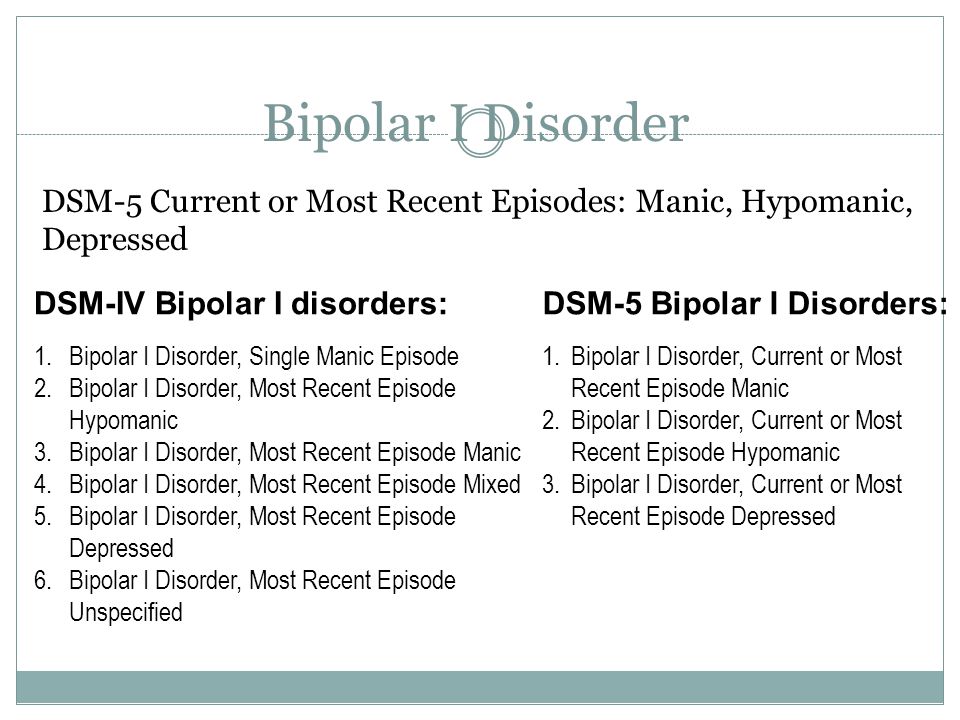
Types of Bipolar Disorder- Bipolar I disorder is the diagnosis given to an individual who is experiencing, or has experienced, a full syndrome of of manic or mixed symptoms; the client may also have experienced periods of depression.
- Bipolar II disorder. Bipolar II disorder is characterized by recurrent bouts of major depression with the episodic occurrence of hypomania; this individual has never experienced a full syndrome of manic or mixed symptoms.
- Cyclothymic disorder. The essential feature is a chronic mood disturbance of at least 2 years’ duration, involving numerous periods of depression and hypomania, but not of sufficient severity and duration to meet the criteria for either bipolar I or bipolar II disorder.
- Bipolar disorder due to general medical condition. This disorder is characterized by a prominent and persistent disturbance in mood (bipolar symptomatology) that is judged to be the direct result of the physiological effects of a general medical condition (APA, 2000).
- Substance-induced bipolar disorder. The bipolar symptoms associated with this disorder are considered to be the direct result of the physiological effects of a substance (e.g., use or abuse of a drug or a medication, or toxin exposure).
The pathophysiology of bipolar disorder, or manic-depressive illness (MDI), has not been determined, and no objective biologic markers correspond definitively with the disease state.
- The genetics component of bipolar disorder appears to be complex; the condition is likely to be caused by multiple different common disease alleles, each of which contributes a relatively low degree risk on its own.
- Many loci are now known to be associated with the development of bipolar disorder.
- These loci are grouped as major affective disorder (MAFD) loci and numbered in the order of their discovery.
Globally, the life-long prevalence rate of bipolar disorder is 0.3 to 1.5%.
- The life-long prevalence of bipolar disorder in the United States has been noted to range from 0.9 to 2.1%.
- For both bipolar I and bipolar II, the age range is from childhood to 50 years, with a mean age of approximately 21 years.
- BPI occurs equally in both sexes; however, rapid-cycling bipolar disorder is more common in women than in men.
Predisposing factors to bipolar disorder include:
- Biological. Twin studies have indicated a concordance rate for bipolar disorder among monozygotic twins at 60% to 80% compared to 10% to 20% in dizygotic twins.
- Biochemical. Just as there is an indication of lowered levels of norepinephrine and dopamine during an episode of depression, the opposite appears to be true of an individual experiencing a manic episode.
- Physiological. Right-sided lesions in the limbic system, temporobasal areas, basal ganglia, and thalamus have been shown to induce secondary mania.
- Medication side effects. Certain medications used to treat somatic illnesses have been known to trigger a manic response; the most common of these are the steroids frequently used to treat chronic illnesses such as multiple sclerosis and systemic lupus erythematosus.
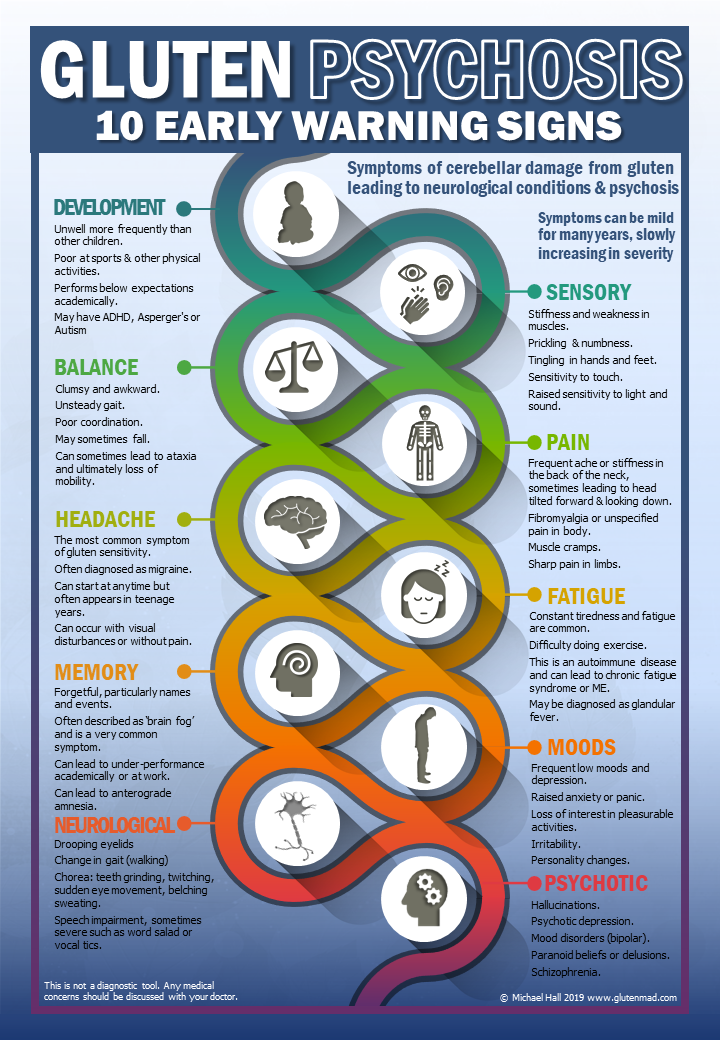
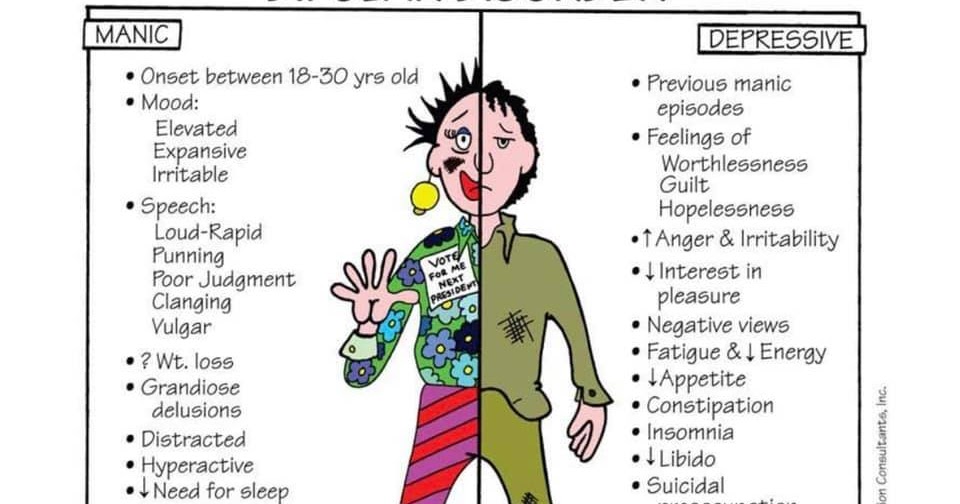
These are the symptoms of bipolar disorder:
- Heightened, grandiose, or agitated mood. The affect of a manic individual is one of elation and euphoria- a continuous “high”.
- Exaggerated self-esteem.
 Usual inhibitions are discarded in favor of sexual and behavioral indiscretions.
Usual inhibitions are discarded in favor of sexual and behavioral indiscretions. - Sleeplessness. Sleep patterns are disturbed; client becomes oblivious to feelings of fatigue, and rest and sleep are abandoned for days or weeks.
- Pressured speech. Loquaciousness, or pressured speech, is so forceful and strong that it is difficult to interrupt maladaptive thought processes.
- Flight of ideas. There is a continuous, rapid shift from one topic to another.
- Reduced ability to filter out extraneous stimuli; easily distractible. There is inability to concentrate because of a limited attention span; the individual is easily distracted by even the slightest stimulus in the environment.
- Increased number of activities with increased energy. Motor activity is constant; the individual is literally moving at all times.
- Multiple, grandiose, high risk activities, using poor judgement; with severe consequences.
A number of reasons exist for obtaining selected laboratory studies in patients with bipolar disorder; an extensive range of tests is indicated, because bipolar disorder encompasses both depression and mania and because a significant number of medical causes for each state exist.
- Complete blood count. A complete blood count with differential is used to rule out anemia as a cause of depression in bipolar disorder.
- Erythrocyte sedimentation rate. The erythrocyte sedimentation rate (ESR) is determined to look for underlying disease process such as lupus or an infection; an elevated ESR often indicates an underlying disease process.
- Fasting glucose. In some cases, a fasting glucose level is indicates to rule out diabetes.
- Electrolytes. Serum electrolyte concentrations are measured to help diagnose electrolyte problems, especially with sodium, that are related to depression.
- Proteins. Low serum protein levels found in patients who are depressed may be a result of not eating.
- Thyroid hormones. Thyroid tests are performed to rule out hyperthyroidism (mania) and hypothyroidism (depression).
- Creatinine and blood urea nitrogen. Kidney failure can present as depression; treatment with lithium can affect urinary clearances, and serum creatinine and blood urea nitrogen (BUN) levels can increase.
- Substance and alcohol screening. Alcohol abuse and abuse of a wide variety of drugs can present as either mania or depression.
- MRI. The total value of performing MRI in a patient with bipolar disorder remains unclear; however a couple of reasons do exist for performing an imaging study.
- Electrocardiography. Many of the anti depressants, especially the tricyclic agents and some of the antipsychotics can affect the heart and cause conduction problems.
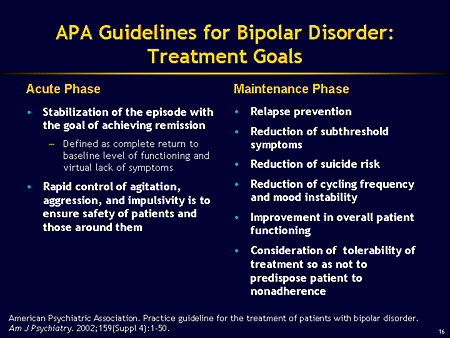
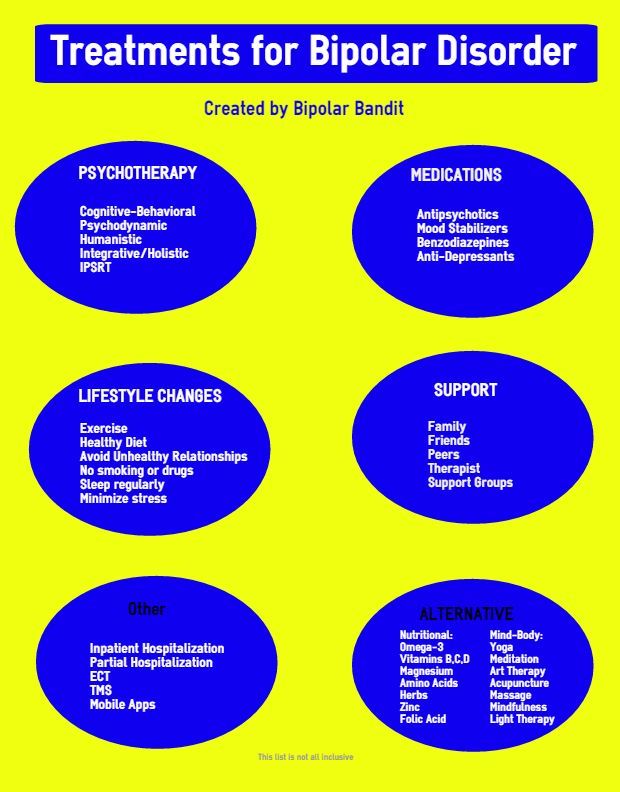
The treatment of bipolar disorder is directly related to the phase of the episode (i.e. depression or mania) and the severity of that phase.
- Psychotherapy. Psychotherapy helps patients with bipolar disorder but does not cure the disorder itself; when Schottle and colleagues looked at psychotherapy for patients, family, and caregivers, they found that although results were heterogeneous, most studies demonstrated relevant positive results in regard to decreased relapse rates, improved quality of life, increased functioning, or more favorable symptom improvement.
- Electroconvulsive therapy. Electroconvulsive therapy (ECT) is useful in a number of instances in patients with bipolar disorder, such as when rapid, definitive medical/psychiatric treatment is needed; when the risks of ECT are less than that of other treatments; when the bipolar disorder is refractory to an adequate trial with other treatment strategies; and when the patient prefers this treatment modality.
- Diet. Patients should be advised not to make significant changes in their salt intake, because increased salt intake may lead to reduced serum lithium levels and reduced efficacy, and reduced intake may lead to increased levels and toxicity.
- Activity. Patients in the depressed state are encouraged to exercise; these individuals should try to develop a regular daily schedule of major activities, especially times of going to bed and waking up.
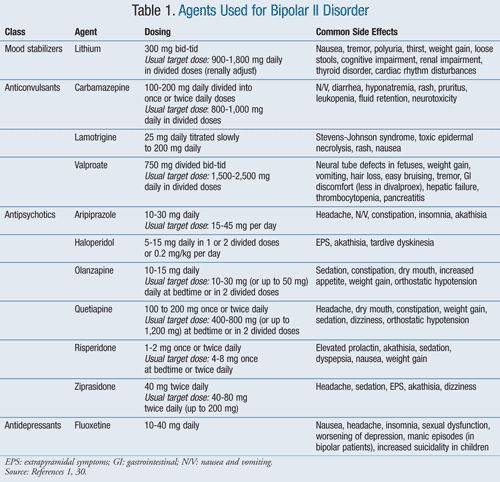
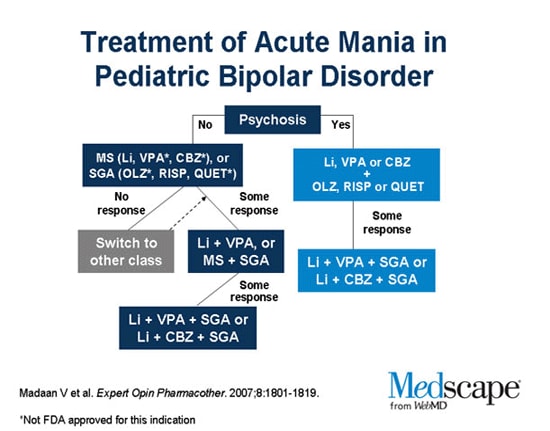
Appropriate medication for managing bipolar disorder depends on the stage the patient is experiencing.
- Anxiolytics, benzodiazepines. By binding to specific receptor sites, benzodiazepines appear to potentiate the effects of gamma-aminobutyric acid (GABA) and facilitate inhibitory GABA neurotransmission and the action of other inhibitory neurotransmitters.
- Mood stabilizers. Lithium is the drug commonly used for prophylaxis and treatment of manic episodes.
- Anticonvulsants. Anticonvulsants have been effective in preventing mood swings associated with bipolar disorder, especially in those patients known as rapid cyclers.
- Antipsychotics, 2nd generation. Second generation, or atypical, antipsychotics are increasingly being used for treatment of both acute mania and mood stabilization in patients with bipolar I disease.
- Antipsychotics, 1st generation. First-generation antipsychotics, also known as conventional or typical antipsychotics, are efficacious in treating both psychotic and nonpsychotic manic and mixed episodes, as well as hypomania.
- Antipsychotics, phenothiazine. Phenothiazine antipsychotics, which are classified as first-generation antipsychotics, are efficacious in treating both psychotic and nonpsychotic manic and mixed episodes, as well as hypomania.
- Antiparkinsons agents, dopamine agonists. Dopamine agonists are non-errgot agents that bind to D2 and D3 dopamine receptors in the striatum and substantia nigra.
Nursing management of a patient with bipolar disorder include the following:
Nursing AssessmentAssessment of a patient with bipolar disorder include:
- History. Taking a history with a client in a manic phase often proves difficult; obtaining data in several short sessions, as well as talking to family members, may be necessary.
- General appearance and motor behavior. Client with mania experience psychomotor agitation and seem to be in perpetual motion; sitting still is difficult; this continual movement has many ramifications; clients can be exhausted or injure themselves.
- Mood and affect. Mania is reflected in periods of euphoria, exuberant activity, grandiosity, and false sense of well being.
- Thought process and content. Cognitive ability or thinking is confused and jumbled with thoughts racing one after another, which is often referred to as flight of ideas; clients cannot connect concepts, and they jump from one subject to another.
Nursing diagnoses commonly established for clients in the manic phase are as follows:
- Risk for other-directed violence related to manic excitement, suspicion of others, paranoid ideation.
- Risk for injury related to extreme hyperactivity, destructive behaviors.
- Imbalanced nutrition: less than body requirements related to refusal or inability to sit still long enough to eat meals.
- Disturbed thought processes related to psychotic process.
- Disturbed sensory perception related to sleep deprivation, psychotic process.
Main Article: 6 Bipolar Disorders Nursing Care Plans
Nursing care planning goals for bipolar disorders are:
- Client will no longer exhibit potentially injurious movements after 24 hours with administration with administration of tranquilizing medications.
- Client will experience no physical injury.
- Client’s agitation will be maintained at manageable level with the administration of tranquilizing medications during first week of treatment.
- Client will not harm self or others.
- Client will consume sufficient finger foods and between-meal snacks to meet recommended daily allowances of nutrients.
- Within one week, client will be able to recognize and verbalize when thinking is non-reality based.
- Client will be able to recognize and verbalize when he or she is interpreting the environment inaccurately.
Nursing interventions for bipolar disorder client are:
- Providing for safety. A primary nursing responsibility is to provide a safe environment for client and others; for clients who feel out of control, the nurse must establish external controls emphatically and nonjudgementally.
- Meeting physiologic needs.
 Decreasing environmental stimulation may assist client to relax; the nurse must provide a quiet environment without noise, television, and other distractions; finger foods or things client can eat while moving around are the best options to improve nutrition.
Decreasing environmental stimulation may assist client to relax; the nurse must provide a quiet environment without noise, television, and other distractions; finger foods or things client can eat while moving around are the best options to improve nutrition. - Providing therapeutic communication. Clients with mania have short attention spans, so the nurse uses simple, clear sentences when communicating; they may not be able to handle a lot of information at once, so the nurse breaks information into many small segments.
- Promoting appropriate behavior. The nurse can direct their need for movement into socially acceptable, large motor activities such as arranging chairs for a community meeting or walking.
- Managing medications. Periodic serum lithium levels are used to monitor the client’s safety and to ensure that the dose given has increased the serum lithium level to a treatment level or reduced it to a maintenance level.
The goals are met as evidenced by:
- Client is able to differentiate between reality and unrealistic events or situations.
- Client is able to recognize thoughts that are not based in reality and intervene to stop their progression.
- Client has gained or maintained weight during hospitalization.
- There is no evidence of violent behavior to self and others.
- Client is no longer exhibiting signs of physical agitation.
Documentation in a patient with bipolar disorder include:
- Individual findings, including factors affecting, interactions, nature of social exchanges, specifics of individual behavior.
- Cultural and religious beliefs, and expectations.
- Plan of care.
- Teaching plan.
- Responses to interventions, teaching, and actions performed.
- Attainment or progress toward the desired outcome.
Quiz time about bipolar disorder from our nursing test bank! Please visit our nursing test bank page for more NCLEX practice questions.
ADVERTISEMENTS
1. Ralph is admitted at Nurseslabs Medical Center with the diagnosis of bipolar disorder, single manic episode. Which of the following behaviors would the nurse expect to assess?
A. Apathy, poor insight, and poverty of ideas.
B. Anxiety, somatic complaints, and insomnia.
C. Elation, hyperactivity, and impaired judgment.
D. Social isolation, delusional thinking, and clang associations.
1. Answer: C. Elation, hyperactivity, and impaired judgment.
- Option C: A client with bipolar disorder, manic episode, would demonstrate flight of ideas and hyperactivity as part of the increased psychomotor activity. The mood is one of elation, and the feeling is that one is invincible; therefore, judgment may be quite impaired.

- Option A: The symptoms in option A would be more characteristic of an individual with long-term schizophrenia.
- Option B: The symptoms in option B would be more characteristic of someone with an anxiety disorder, although a manic individual may also not sleep because of excessive energy.
- Option D: The symptoms in option D are more characteristic of schizophrenia.
2. In a day treatment program, a manic client is creating considerable chaos, behaving in a dominating and manipulative way. Which nursing intervention is most appropriate?
A. Allow the peer group to intervene.
B. Describe acceptable behavior and set realistic limits with the client.
C. Recommend that the client is hospitalized for treatment.
D. Tell the client that his behavior is inappropriate.
2. Answer: B. Describe acceptable behavior and set realistic limits with the client.
- Option B: In this situation, it would be appropriate for the nurse to suggest alternative behaviors in place of unacceptable ones to help the client gain self-control.

- Option A: The peer group is not responsible for monitoring the client’s behavior.
- Option C: The client’s behavior does not warrant hospitalization.
- Option D: The client is told only what is unacceptable and is not given any alternatives.
3. Nurse Nadine is assessing James who is diagnosed with bipolar disorder. The nurse would expect to find a history of:
A. A depressive episode followed by prolonged sadness.
B. A series of depressive episodes that recur periodically.
C. Symptoms of mania that may or may not be followed by depression.
D. Symptoms of mania that include delusional thoughts.
3. Answer: C. Symptoms of mania that may or may not be followed by depression.
- Option C: The definition of bipolar disorder is a mood disturbance in which the symptoms of mania have occurred at least one time. Depression may or may not occur as a separate episode in bipolar disorder.
- Options A, B, D: None of the other options indicate a correct understanding of bipolar disorder.
4. The nurse is planning activities for a client who has bipolar disorder with aggressive social behavior. Which of the following activities would be most appropriate for this client?
A. Ping pong.
B. Writing.
C. Chess.
D. Basketball.
4. Answer: B. Writing.
- Option B: Solitary activities that require a short attention span with mild physical exertion are the most appropriate activities for a client who is exhibiting aggressive behavior. Writing, walks with staff, and finger painting are activities that minimize stimuli and provide a constructive release for tension.
- Options A, C, D: Competitive games can stimulate aggression and increase psychomotor activity.
5. The nurse assesses a client with the admitting diagnosis of bipolar affective disorder, mania.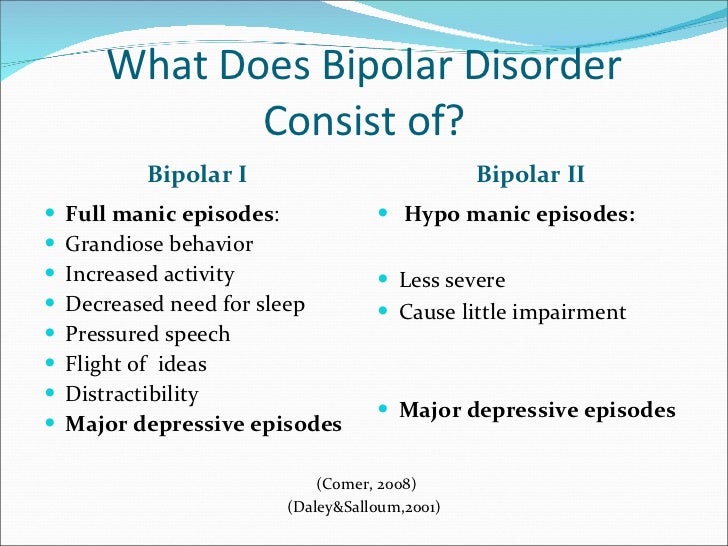 The symptom presented by the client that requires the nurse’s immediate intervention is the client’s:
The symptom presented by the client that requires the nurse’s immediate intervention is the client’s:
A. Outlandish behaviors and inappropriate dress.
B. Grandiose delusions of being a royal descendant of King Arthur.
C. Nonstop physical activity and poor nutritional intake.
D. Constant, incessant talking that includes sexual innuendoes and teasing the staff.
5. Answer: C. Nonstop physical activity and poor nutritional intake.
- Option C: Mania is a mood characterized by excitement, euphoria, hyperactivity, excessive energy, decreased need for sleep, and impaired ability to concentrate or complete a single train of thought. Mania is a period when the mood is predominately elevated, expansive, or irritable. All options reflect a client’s possible symptomatology. Option C, however, clearly presents a problem that compromises one’s physiological integrity and needs to be addressed immediately.
Interesting resources for further reading about bipolar disorder:
- Bartels, S.
 J., Mueser, K. T., & Miles, K. M. (1997). A comparative study of elderly patients with schizophrenia and bipolar disorder in nursing homes and the community. Schizophrenia Research, 27(2-3), 181-190. [Link]
J., Mueser, K. T., & Miles, K. M. (1997). A comparative study of elderly patients with schizophrenia and bipolar disorder in nursing homes and the community. Schizophrenia Research, 27(2-3), 181-190. [Link] - Black, J. M., & Hawks, J. H. (2005). Medical-surgical nursing. Elsevier Saunders,.
- Boyd, M. A. (Ed.). (2008). Psychiatric nursing: Contemporary practice. lippincott Williams & wilkins.
- Keltner, N. L. (2013). Psychiatric nursing. Elsevier Health Sciences.
- Videbeck, S. L. (2010). Psychiatric-mental health nursing. Lippincott Williams & Wilkins.
ADVERTISEMENTS
Categories Psychiatric Nursing Tags anticonvulsants, Antipsychotics, anxiolytics, benzodiazepines, Bipolar, bipolar disorder, Bipolar I Disorder, Complete Blood Count (CBC), diet, Electrocardiography, Electroconvulsive Therapy (ECT), Erythrocyte Sedimentation Rate (ESR), psychotherapeutic drugs
Marianne Belleza, R.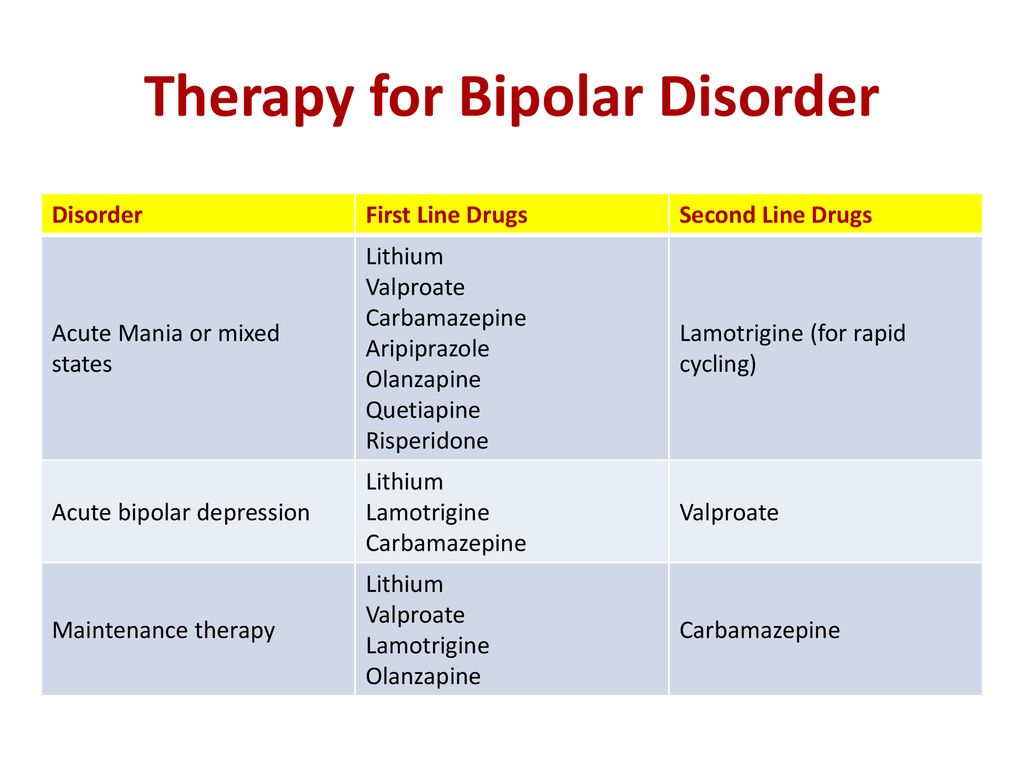 N.
N.
Marianne is a staff nurse during the day and a Nurseslabs writer at night. She is a registered nurse since 2015 and is currently working in a regional tertiary hospital and is finishing her Master's in Nursing this June. As an outpatient department nurse, she is a seasoned nurse in providing health teachings to her patients making her also an excellent study guide writer for student nurses. Marianne is also a mom of a toddler going through the terrible twos and her free time is spent on reading books!
© 2023 Nurseslabs | Ut in Omnibus Glorificetur Deus!
Treatment of bipolar disorder: what methods and drugs do doctors use?
Modern psychiatry is represented by new generation drugs, innovative approaches in psychotherapy. They are used in bipolar disorders. Patients should not be treated as if they were depression or schizophrenia - the drug regimen is selected depending on the phase and condition of the patient. If we are talking about depression, antidepressants are selected, if about mania, they are contraindicated, anxiolytics and sedatives are prescribed.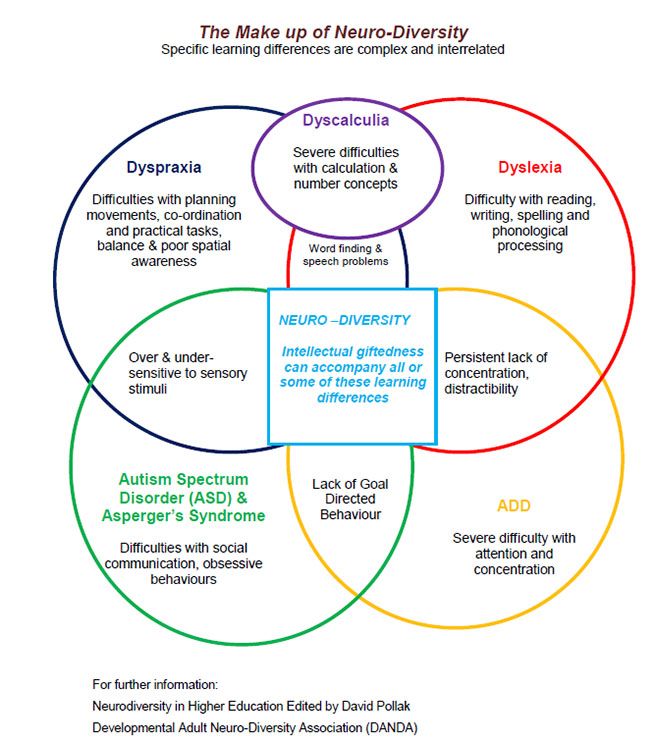 nine0003
nine0003
Submit an application for diagnosis and treatment
I confirm that I accept the terms of consent to the processing of personal data.
Bipolar personality disorder is quite complex in terms of the treatment of the disease. Building a therapy strategy can only be entrusted to an experienced psychiatrist. In no case should patients self-medicate, as this may lead to a worsening of the condition. Treatment is primarily medical, but psychotherapy and lifestyle changes are also recommended. The treatment regimen is selected by the doctor individually, depending on the characteristics of the course of the disease and the psychotype of the patient. Abuse of antidepressants or refusal to take medications with a temporary improvement in well-being can lead to complications, so the patient should be constantly under the supervision of the attending physician. nine0003
Treatment of bipolar disorder: what methods and drugs do doctors use?
If you or someone close to you suffers from bipolar disorder, do not delay seeking qualified help. The sooner you start treatment, the higher your chances of success. Timely and effective treatment of bipolar disorder relieves its symptoms, reduces the frequency and intensity of mood swings, and helps to live a normal life. In a previous article on bipolar disorder, I have already looked at the general aspects of this disorder. Today's post is entirely dedicated to the treatment of bipolar disorder. In this regard, before you start reading, I will answer the most common question: Can bipolar disorder be cured on its own? The short and simple answer is NO! You can greatly help the treatment, make the process easier and more effective, but nothing more. For non-believers, I'll explain why. If the fact of the disease is established, then it manifested itself through the symptoms. Symptoms are what we see. Therefore, the disease takes over the mind, since we see its manifestations. If a person could suppress the manifestation of symptoms by willpower, then no one would ever know about any disease, that is, it would not exist.
Any person experiences different emotions from time to time, but as long as he can control them, he is mentally healthy. If emotions take over and control the consciousness of a person, he is sick. How can a sick person fight on his own with what he cannot control? - No way! In this case, it is impossible to do without outside help. nine0003
Overview of bipolar disorder and its treatment
Bipolar disorder is a lifelong condition. Its manifestations are always unpredictable, so "ups" and "downs" alternate without any apparent pattern. If treatment is delayed, these ups and downs can be devastating. The recurring episodes of manic and depressive phases that characterize the disease make it difficult to lead a normal, stable, and productive life. In a manic phase, you may be hyperactive and irresponsible; in a depressive phase, it may be difficult for you to do anything at all. Early diagnosis and treatment will undoubtedly help to avoid these problems. The success of treatment for bipolar disorder depends on a number of factors. Medications alone are not enough. In order to get the most out of your treatment, it is very important to educate yourself and educate yourself about your illness, communicate with doctors and psychologists, and provide yourself with a strong support system to lead a healthy lifestyle and stick to your treatment plan. The healing process for bipolar disorder is long and will not happen overnight. Like the mood swings of bipolar disorder, treatment too will have its ups and downs. Finding the right treatment will take time, and failures happen along the way. But with proper attention to the disease, as well as a consistent commitment to the desire to improve your condition, you can take control of the symptoms of bipolar disorder and live life to the fullest. What can you do to feel better? Know the difference between the symptoms of the disease and the characteristics of your psyche. The professionals you turn to for help can help separate your personality traits from the symptoms of the disease, which will allow you to recognize in which cases changes in your behavior are caused by the disease and which are not.
To do this, you must be open and honest about your behavior, because you will have to monitor it in order to improve the recognition of episodes of bipolar disorder. · Educate your family members and involve them in the process of fighting the disease. Your loved ones can help identify symptoms and monitor your behavior. They will also motivate and support you, which will certainly allow you to deal with future crises much more effectively. · Live a healthy life. A normal and healthy lifestyle, including regular sleep, a healthy diet, the absence of alcohol, drugs and risky behavior is one of the main conditions for recovery. Develop an individualized treatment plan. Talk to your doctor about your medications, especially side effects that may be bothering you. There are many options for drug exposure and there is always plenty to choose from. It is very important to consult with specialists before making any changes in the treatment process, from the set of medications used, the schedule for taking them, and ending with the daily routine.
nine0003
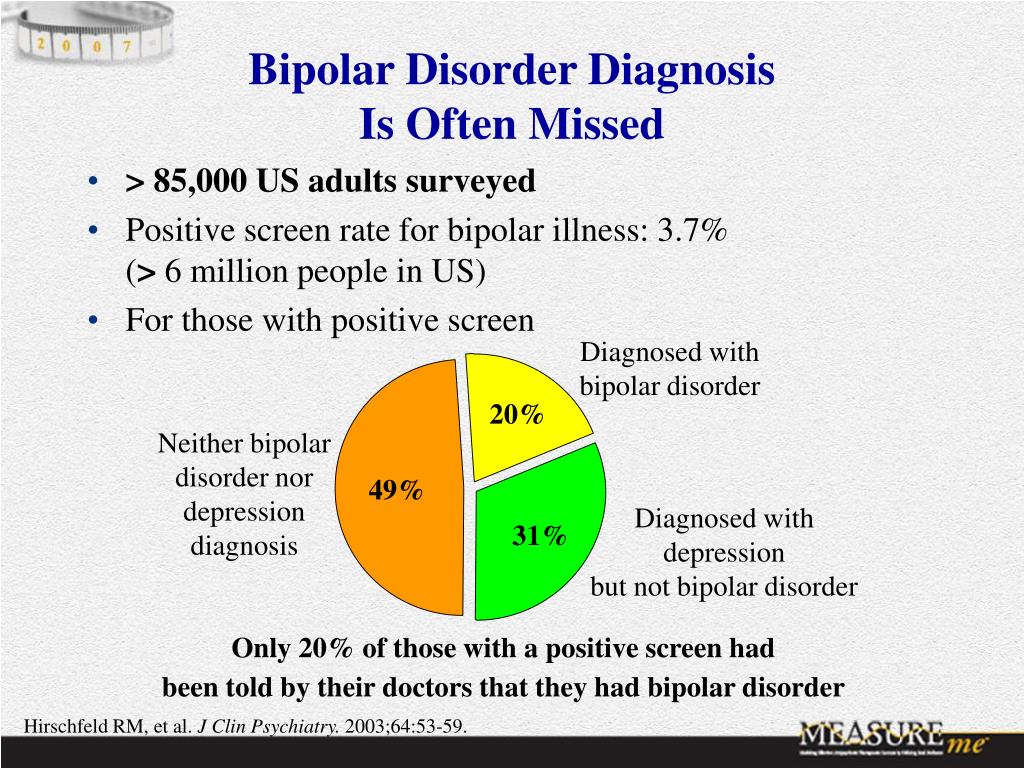
Accurate diagnosis of bipolar disorder
Obtaining an accurate diagnosis is the first step in the successful treatment of bipolar disorder. This is not always easy to do. The mood swings of bipolar disorder can be difficult to distinguish from other mental health problems such as depression, ADHD (attention deficit hyperactivity disorder), or borderline personality disorder. For many people with bipolar disorder, it takes years and multiple visits to the doctor before the problem is identified and properly diagnosed. Correctly diagnosing bipolar disorder can be difficult even for qualified professionals, so it is better to consult a psychiatrist with experience in the treatment of bipolar disorder, and not just a psychotherapist in an outpatient clinic or a local doctor. An experienced psychiatrist who specializes in the treatment of bipolar disorder is likely to be much better informed about the latest research in the field and advanced treatments. He also probably maintains contact with other specialists, which will make your treatment more effective. What to expect from the diagnosis? A diagnostic evaluation for bipolar disorder typically consists of the following: · Psychiatric evaluation - a complete psychiatric history (data collection and medical history) will be taken by a medical specialist. You will answer questions about your symptoms, tell your history of concerns, any treatment you may have received in the past, and your family history of mood disorders. · Physical Examination and Investigations – There are no specific laboratory tests to detect bipolar disorder. But the doctor must take a medical history and conduct a series of tests to rule out diseases or medications that may be causing your symptoms. For example, screening for thyroid disorders is especially important, as thyroid problems can cause mood swings that mimic the symptoms of bipolar disorder. In addition to a psychiatric evaluation and physical exam, your doctor may talk to family and friends about your mood and behavior.
Very often, people around you can give a more accurate and objective picture of your symptoms. Diseases and drugs that can mimic symptoms of bipolar disorder Thyroid disorders Corticosteroids Antidepressants Adrenal disorders (eg, Addison's disease, Cushing's syndrome) Anxiety drugs Drugs for Parkinson's disease Vitamin B12 deficiency Neurological disorders (e.g. epilepsy, multiple sclerosis)
Types of Bipolar Disorder
I have already covered the types of this disorder in the article Bipolar Disorder, which you can read if some of the terms are not clear to you. But in order not to refer those who know what is at stake to another publication, I will once again remind you of the types of bipolar disorder, only in more detail. Each type of bipolar disorder is defined by the nature of the episodes of mania and depression. Treatment may differ depending on the type of bipolar disorder you have been diagnosed with. · Bipolar I disorder (mania and depression) - Bipolar I disorder is the classic form of the disease and also the most typical type of bipolar disorder. It is characterized by at least one episode of mania or a mixed episode. The vast majority of people with bipolar I disorder also have at least one episode of depression, although this is not necessary for a diagnosis. · Bipolar II disorder (hypomania and depression) - full-blown mania does not appear here. Instead, the illness involves recurring episodes of depression and hypomania (a mild form of mania). In order to be diagnosed with Bipolar II, you must have had at least one episode of hypomania and one major depressive episode. If you have had a manic episode at least once in your life, your diagnosis will be changed to Bipolar I disorder. · Cyclothymia (hypomania and mild depression) - Cyclothymia is a mild form of bipolar disorder. Like any bipolar disorder, cyclothymia is made up of cyclical mood swings. However, the highs and lows are not severe enough to unambiguously qualify as mania or depression. For a diagnosis of cyclothymia, you must experience multiple episodes of hypomania and mild depression over at least a two year period.
Since people with cyclothymia are at an increased risk of developing full-blown bipolar disorder, this form of the disease needs to be carefully screened for accurate and timely diagnosis. nine0003
Bipolar disorder or depression?
Bipolar disorder is often misdiagnosed as depression. One reason for this is that most people with bipolar disorder seek help when they are in the depressive phase of the illness. If a person is going through a manic phase, he rarely sees a doctor because he doesn't acknowledge that there is a problem. In addition, in people with bipolar disorder, a significantly greater percentage of the time is spent in depressive phases than in manic or hypomanic phases. Misdiagnosed, bipolar disorder is a potentially dangerous problem because the treatment for bipolar depression is different from that for regular depression. In fact, antidepressants used to treat regular depression can significantly worsen bipolar disorder. Therefore, it is very important to contact a specialist in a timely manner, who will help you understand what is really happening. Signs that your depression is really bipolar disorder: · Episodes of depression are recurring. · You had your first episode of depression before the age of 25. · You have a relative with bipolar I disorder. · When you are not depressed, your mood and energy levels are higher than those of most other people. · When you are depressed, you sleep a lot and overeat. Episodes of depression are short (less than 3 months). You lose touch with reality when you are depressed. · You have had a case of postpartum depression. · You have had episodes of mania or hypomania while taking antidepressants. · Your antidepressants stopped working a few months after you started taking them. · You have tried 3 or more antidepressants without success, but nothing worked for you. nine0003
Treatment options for bipolar disorder
If your doctor determines that you have bipolar disorder, they will offer treatment options and possibly prescribe medication. You may also be referred to other specialists for advice and development of an individual treatment plan.
Comprehensive treatment for bipolar disorder
Comprehensive treatment plan for bipolar disorder aims to: Relieve symptoms Restore the ability to act and solve problems both at home and at work Reduce the chance of relapses A complete treatment plan includes: Medications - Medications are the backbone of the bipolar disorder treatment process. By taking stabilizing drugs, you minimize the "ups" and "downs" and retain the ability to manage the situation. · Psycho1therapy - necessary to deal with bipolar disorder and the problems that the disease has caused in your life. Working with a doctor, you will learn about how to deal with difficult or unpleasant emotions, reconnect with others, deal with stress, and learn how to manage your mood. · Education - Managing symptoms and preventing complications begins with an in-depth understanding of one's illness. Education is a key component of treatment. The more you and your loved ones know about bipolar disorder, the easier it will be to avoid problems and deal with setbacks. · Lifestyle changes – By carefully following a healthy lifestyle, you can minimize the impact of bipolar disorder symptoms. This includes maintaining a regular sleep pattern, avoiding alcohol and drugs, a consistent exercise program, avoiding conflict, avoiding stressful situations, and maintaining a positive mindset at all times. · Support – Life with bipolar disorder can be challenging, so having a strong support system can help change your outlook and increase positive motivation. Participation in a bipolar disorder support group will give you the opportunity to share your experiences and learn from those who have already gone through the stages that you are just going through now. The support of friends and family is also invaluable. nine0003
The role of medication in treating bipolar disorder
Most people with bipolar disorder need medication to keep their symptoms under control. Long-term drug treatment can reduce the frequency and severity of episodes of the disease, and sometimes prevent them completely. If you have been diagnosed with bipolar disorder, you and your doctor will work together to find the right drug or drug combination that is best for you. Because everyone reacts differently to medications, you may try a wide variety of medications before you find one (or group of medications) that relieves symptoms. Do not take it into your head to "get" medicines and take them - the consequences can be not just bad, but terrible · Visit your doctor regularly. It is important to have regular blood tests to ensure that the blood level of the drug is in the therapeutic range (sufficient for a therapeutic effect, but not so high as to aggravate the situation). Determining the exact dose of medication you need is a constant balancing act between too little and too much, so regular monitoring will help keep you from showing symptoms and keep you healthy. · Continue taking your medicines even if your mood is stable. Do not stop taking your medicines as soon as you start to feel better. Most people need to take medication on a regular basis to avoid relapses.
· Don't expect medicines to solve all your problems. For bipolar disorder, medications can help reduce symptoms of mania and depression, but in order to feel better, it's important to lead a lifestyle that supports good health. This includes the support of others, therapeutic treatment and proper rest. · Be extremely careful with antidepressants. Studies show that antidepressants are not particularly effective in treating bipolar depression. In addition, they can cause mania or sudden and frequent jumps between depression and mania. nine0003
Psychotherapy as an important part of treatment
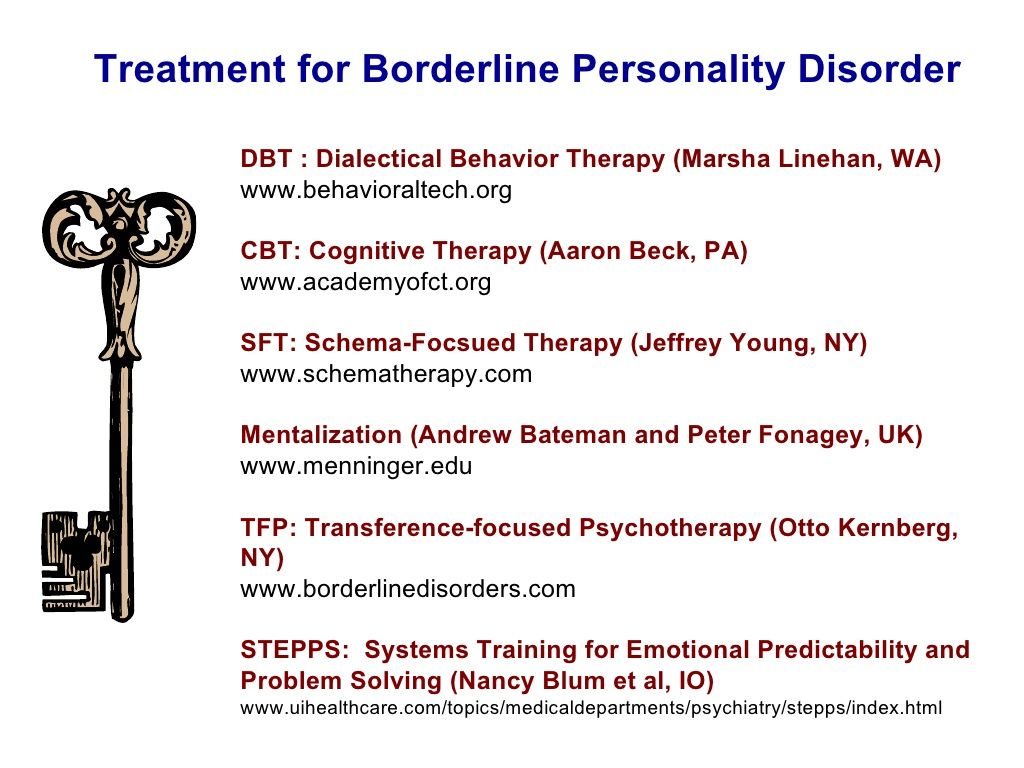
People who take drugs to treat bipolar disorder are much more likely to be cured if they also receive medical treatment. In therapy, you will learn how to deal with issues that cause symptoms of bipolar disorder, such as relationship issues and self-esteem. Therapy sessions will address other issues you struggle with, such as substance abuse or anxiety. Particularly useful in the treatment of bipolar disorder are the following three therapies: Cognitive Behavioral Therapy Interpersonal and Social Rhythm Therapy Family Therapy
Cognitive Behavioral Therapy
In Cognitive Behavioral Therapy sessions, you will learn about how your thoughts affect your emotions, and you will learn to change negative thought patterns into more positive ways of responding. In the treatment of bipolar disorder, the emphasis is on managing symptoms, avoiding relapse triggers, and dealing with problems that arise.
Interpersonal and social rhythm therapy
Interpersonal Therapy addresses the most pressing relationship issues to help you connect better with those around you. This type of treatment aims to reduce stress levels, and since stress is a trigger for bipolar disorder, interpersonal and social rhythmic therapy will help reduce mood swings, making them less frequent and less severe. In the treatment of bipolar disorder, interpersonal therapy is often combined with social rhythm therapy. It has been proven that people with bipolar disorder have an increased sensitivity to biological rhythms. In turn, biological rhythms can be easily disturbed by a mismatch between biorhythms and social rhythms. Social rhythm therapy focuses on stabilizing social rhythms such as sleeping, eating, working hours. When these rhythms are stabilized, the biological rhythms that control mood also remain stable. nine0003
Family therapy
Living with a person who suffers from bipolar disorder is very difficult, which leads to tension in family relationships. Family therapy is focused on solving these problems and is aimed at restoring a healthy and supportive home environment. Informing family members about the disease and teaching them how to deal with its symptoms is a major component of family therapy.
Alternative treatments for bipolar disorder
Most alternative treatments for bipolar disorder are actually complementary treatments, meaning they must be used in conjunction with medication, therapy, and lifestyle changes. Here are some useful additions: Day and Night Therapy — Like Social Rhythm Therapy, Day and Night Therapy focuses on the biological rhythms of people with bipolar disorder. This therapy offers assistance in organizing biorhythms by properly adjusting lighting at different times of the day to provide darkness when nighttime rest is needed and light when wakefulness is needed. One of the main components of this therapy is the restriction of daylight or artificial light for ten hours each night. · Focus and Meditation - Research has shown that focus based cognitive therapy and meditation help fight and prevent depression, anger, anxiety, and anxiety. Meditation, yoga, breathing exercises and focusing on one's own mind help break down negative thinking patterns. · Acupuncture — Acupuncture is currently being studied as an additional treatment for bipolar disorder. Some researchers believe that it may help people with bipolar disorder by modulating their response to stress. Research on acupuncture in the treatment of bipolar depression has already shown a reduction in symptoms, and every year there is more and more evidence that acupuncture can relieve the symptoms of not only depression, but also mania. nine0003
Treatment of bipolar affective disorder in St. Petersburg
- Home
- Psychotherapy
- Treatment of bipolar disorder
Usually the symptoms of bipolar disorder are attributed to personality traits or mood swings, which are logically explained. And, as a rule, even close relatives may not suspect that a person suffers from one of the most common mental disorders. nine0003
Bipolar affective disorder is difficult to diagnose at an early stage of the disease. Therefore, we recommend that the patient himself or his relatives start keeping a diary, recording daily the features of the psycho-emotional state and key events that affect the occurrence of depressive and / or manic episodes. Such a diary will help the doctor determine the type of disease and prescribe the necessary treatment for bipolar disorder, and in the future to monitor the dynamics of the state of health. nine0003
Bipolar affective disorder is treated as an outpatient or inpatient clinic. At the peak of a depressive episode, when there is a risk of suicide, as well as to reduce the timing of the selection of pharmacotherapy, treatment of bipolar disorder should be carried out in a hospital. Bipolar personality disorder, left untreated, can progress and cause a deterioration in quality of life. Over a long distance, the disease inevitably leads to family conflicts, alcoholism or drug addiction, social degradation and, ultimately, suicide. nine0003
With the right treatment for bipolar disorder, you can stabilize your psycho-emotional state and eventually achieve remission. Usually, it takes 15 to 20 days of hospital treatment to stabilize the psycho-emotional state. Achieving remission is possible subject to compliance with the prescribed drugs, with periodic outpatient visits to the attending physician to correct therapy.
Test: "Altman scale for self-assessment of mania"
Choose the answer that most accurately reflects your state of mind over the past week.
Bipolar disorder doctor's consultation:
+7 (812) 407-18-00
Thank you for your trust!
- Post discharge management
- Psychotherapy for couples and families
- Psychosocial personality correction
| Service | nine0112Price | |
|---|---|---|
| Outpatient treatment | ||
| Psychiatric consultation | nine01245 000 ₽ | |
| Psychotherapist appointment | 5 000 ₽ | nine0115|
| Reception of the chief physician Bocharov A. | 6 000 ₽ | |
| Psychiatric consultation at home | 6 000 ₽ | |
| Treatment in a hospital | ||
| Delivery to hospital | For free nine0118 | |
| Standard chamber | 8 900 ₽ | |
| 3-bed superior room | nine0121 12 000 ₽ | |
| 2-bed superior room | 15 000 ₽ | |
| 1 local VIP room | 19 500 ₽ | |
| Doctor's appointment 2 weeks after discharge | For free | |
Causes of bipolar disorder
The main causes of bipolar affective disorder include genetic predisposition, disturbances in the metabolism of neurotransmitters and changes in nerve cells, and severe stress. In other words, the disease can occur in any person, regardless of age, gender and social status. nine0003
Genetic causes
Genetic causes of bipolar disorder are a risk factor for the development of the disease. It should be emphasized that the disease itself is not inherited. However, inherited features of the regulation of neurotransmitters in the brain increase the risk of developing bipolar disorder in close relatives (for example, siblings) by 4–7 times.
Metabolic disorders in the brain
Another cause of bipolar disorder may be a metabolic disorder in the brain. An abnormal increase and decrease in the concentration of biologically active chemical compounds (mainly dopamine, serotonin and norepinephrine), which transmit nerve signals, is the cause of the manic and depressive phases. nine0003
Severe stress and the “biological defect” model
The psyche of each person has an individual threshold for resistance to stress. And the word "stress" does not necessarily mean difficult life situations - be it a dismissal, financial problems, family conflicts, divorce, or the death of a loved one. Stress factors can be an upcoming birthday, puberty, marriage or the birth of a child.
nine0003
Fig. Zubin and Spring's stress-vulnerability model.
a) Low vulnerability, BD can only develop under severe stress.
b) High vulnerability, BAD develops even under low intensity stress.
c) Individual vulnerability, corresponds to the intensity of stress.
Symptoms of bipolar disorder
Treatment of bipolar disorder in our clinic
Typically treatment of bipolar disorder is carried out in the hospital of the clinic. The conditions of the hospital allow to reduce the duration of treatment - to conduct an examination, quickly normalize the patient's psycho-emotional state, select drugs and their minimum effective dosage, conduct dynamic monitoring and adjust pharmacotherapy.
Examination
On the day of hospitalization, the patient undergoes an examination, which includes:
- psychodiagnostics;
- consultation of a therapist;
- consultation with a neurologist;
- laboratory tests;
- EEG.
Lab tests include blood tests for hormonal status (generally, thyroid problems are found in people with bipolar disorder). Pathology of the thyroid gland directly affects mood swings, therefore, when treating bipolar disorder, it is important for a doctor to know the patient's hormonal background, for example: to prescribe drugs that normalize the thyroid gland, or to exclude lithium, which inhibits its work. nine0003
Drug treatment
Based on the results obtained, the doctor will prescribe a treatment for bipolar disorder - he will select drugs that relieve autonomic symptoms and normalize the psycho-emotional state (normotimics, antidepressants). Usually, the first signs of improvement in mental health are observed on the fifth day after the start of drug treatment for bipolar disorder. However, the final correction of psychopharmacotherapy can take up to 10 days.
Psychotherapeutic assistance
After stabilization of the psycho-emotional state, the patient begins attending group psychotherapy sessions. Group sessions with psychotherapists and psychologists of our clinic are held daily. Under the guidance of experienced facilitators, the patient will have the opportunity to work through their experiences and fears, get rid of pathological patterns, and receive professional help from psychologists and psychotherapists with clinical experience.
Post-discharge management
Discharge is usually done after remission, 14-21 days treatment for bipolar disorder . Then the patient continues to take the prescribed drugs and visit the attending physician once every 1-3 months for 1 year. Subject to the achievement of stable remission, after 1 year, in some cases, it is possible to completely abandon the drug treatment of bipolar disorder.
Treatment of bipolar disorder in St. Petersburg is carried out at: st. Marata, 78. We take on complex cases, including the treatment of adolescent patients and patients with drug resistance. nine0003
Treatment of bipolar comorbidities
Psychotherapeutic treatment of bipolar disorder
Psychotherapeutic treatment of bipolar affective disorder, as an adjunct to pharmacotherapy, allows a faster deep remission. Such treatment begins already in the hospital and can be continued after discharge. The number of sessions, their frequency and the form of psychotherapy (individual, family or hypnotherapy) you can choose together with the doctor. nine0003
In addition to individual psychotherapy sessions that correct the patient's personality, family consultations are possible. At family therapy sessions, relatives can better understand the nature of the disease and learn the right behavior that contributes to a speedy recovery. In addition, studies show that psychotherapeutic care reduces the number of hospitalizations for relapses.
Cognitive Behavioral Therapy
Cognitive Behavioral Therapy corrects the pathological patterns of behavior and thinking that occur in patients with bipolar affective disorder. In addition, during psychotherapy sessions, the patient will be able to learn to recognize relapses of the disease, cope with them on their own or seek help in time, preventing a full-blown episode. nine0003
Family Therapy
If bipolar disorder has caused a deterioration in relationships with those closest to you, we recommend that you seek the help of a family therapist. The doctor will help relatives understand the features of the disease, resolve interpersonal conflicts and restore harmony in the family.
Individual sessions of psychotherapy help overcome mood swings during the formation of stable remission. By learning to control the psycho-emotional state, as well as working through pathological patterns, it becomes easier for the patient to cope with exacerbations of the condition, which may occur for some time after undergoing treatment in the hospital. nine0003
Consequences of not getting help
To describe what bipolar disorder is in simple terms, it is necessary to understand the specifics of the condition in which people with this disease find themselves. Living with bipolar affective disorder is not easy. People learn to live with bipolar disorder over the years, experiencing rapid ups and downs in both career and family life. Imagine that you are walking on a zebra - now you are full of strength and enthusiasm, and the next minute you stop in a stupor and everything falls out of your hands: life loses its meaning, achievements no longer seem so significant, you want to escape from everyday life, hide from your eyes relatives, change their place of residence and work. nine0003
Add to this state of misunderstanding on the part of relatives and friends, who begin to consider you frivolous and incapable of finishing what you started to the end. At some point, you quarrel with relatives and, it would seem, nothing keeps you in this familiar and gray life. You can stay in this state for months, and then everything starts all over again. You are full of strength and enthusiasm - set yourself bold tasks, hardly sleep, call friends and want to hug strangers (just like that, because you are full of boundless love). nine0003
However, few "lucky ones" with bipolar disorder manage to experience a depressive episode on their own from year to year. Moreover, the depressive state distorts reality no less than the euphoria of the manic stage. It can take years or decades to learn how to "live" with bipolar disorder. But many do not succeed in doing this - and the lives of these people cannot be envied. Unfortunately, some of them are socially degraded or commit suicide.
Bipolar disorder in women
If you do not seek help in time, bipolar disorder in women can lead to family conflicts, divorce, promiscuity, and the development of borderline mental disorders. To a lesser extent, women with bipolar disorder are prone to alcoholism and drug addiction, although this scenario cannot be completely excluded.
Bipolar disorder in men
The development of bipolar disorder in men causes deterioration of relationships at work (possibly dismissal), family quarrels, looking for relationships on the side, addiction to alcohol and / or gambling (gambling, Internet surfing). Ultimately, domestic violence is not ruled out against the backdrop of a depressive episode.