How to deal with bipolar
Living With Bipolar Disorder - What is Bipolar Disorder?
Your browser is not supported
Switch to Chrome, Edge, Firefox or Safari
Main page content
With proper treatment, along with support and self-care, people with bipolar disorder can live healthy, fulfilling lives.On this page:
-
A person who has bipolar disorder also experiences changes in their energy, thinking, behavior, and sleep. During bipolar mood swings, it is difficult to carry out day-to-day tasks, work, go to school, and maintain relationships.
When a person has a manic episode, they feel overly excited, productive, and even invincible. These drastic behavior changes usually cause concern among friends and family. On the other hand, when a person has a depressive episode, they feel extremely sad, hopeless, and tired. They may avoid friends, family, and participating in their usual activities.
-
Video: Living With Bipolar Disorder
Learn about Phil's experience with bipolar disorder.
-
A severe manic or depressive episode may trigger psychotic symptoms such as delusions (false beliefs) or hallucinations (seeing or hearing things that others do not see or hear).
Tips for Living with Bipolar Disorder
Bipolar disorder is a lifelong condition that doesn’t go away on its own. While it can feel overwhelming and isolating at first, an early, accurate diagnosis is the first step toward getting better. Proper treatment, along with support and self-care, helps people with bipolar disorder live healthy, fulfilling lives.
Treatment Options
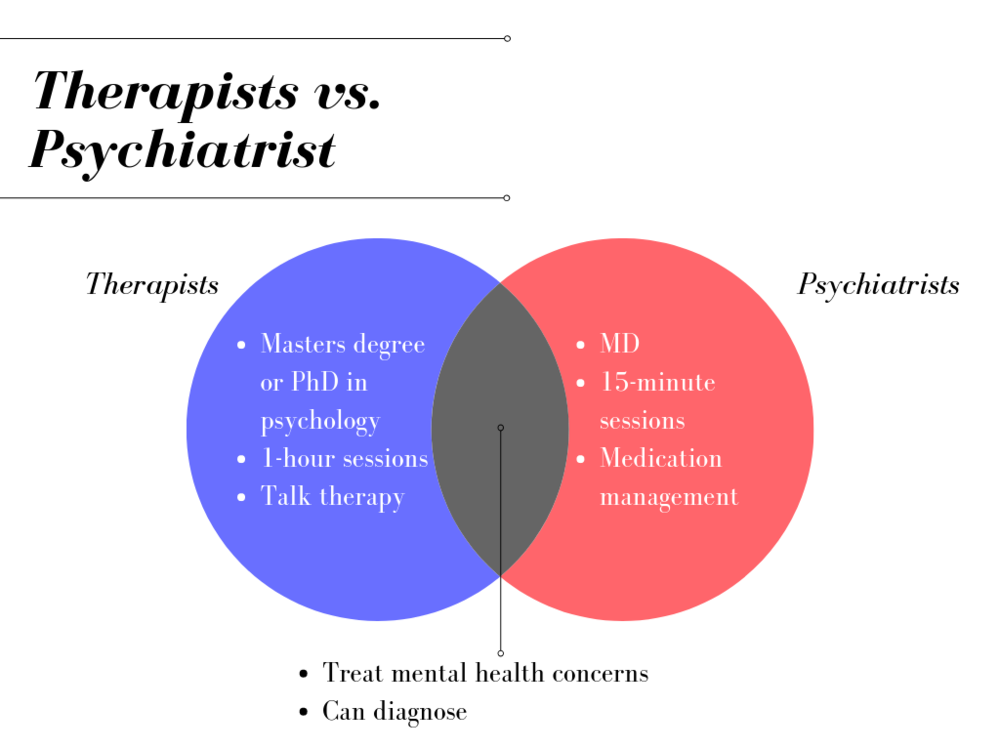
Bipolar disorder is treatable with a combination of medication and therapy.
- Medications. Mood stabilizers, antipsychotics, and antidepressants can help manage mood swings and other symptoms. It is important to understand the benefits and risks of medications. People may need to try different medications before determining which works best for them. They should never stop taking a medication without their doctor’s guidance.
- “Talk therapy” (psychotherapy). Therapy helps people accept their disorder, recognize the warning signs of a manic or depressive episode, develop coping skills for handling stress, and stick with a medication schedule. Therapy also improves communication and relationships among families.
- Long-term, continuous treatment. While there may be times between episodes where a person feels fine, a long-term, continuous treatment plan can reduce the severity and frequency of mood swings.
What You Can Do: Daily Habits Make a Difference
These healthy lifestyle habits, along with professional treatment, can help manage the symptoms of bipolar disorder:
- Stick to a consistent routine.
 Go to sleep and wake up at the same time each day. Being sleep deprived can put people at risk for manic or depressive episodes. Sleeping more than usual may be a sign of a depressive episode. Limit caffeine, which can disrupt sleep.
Go to sleep and wake up at the same time each day. Being sleep deprived can put people at risk for manic or depressive episodes. Sleeping more than usual may be a sign of a depressive episode. Limit caffeine, which can disrupt sleep. - Eat well and get regular exercise. A healthy diet will give your body proper nutrition, and exercise may help improve your mood.
- Always take your medicine as prescribed. You should do this even when your mood is stable.
- Check with your treating doctor. Always check before taking over-the-counter supplements or any medications prescribed by another doctor.
- Keep a mood journal. By tracking how you feel day-to-day, you can notice triggers, monitor how your treatment is working, and spot changes in your eating or sleeping patterns. Writing down this information can be especially helpful to your doctor if your medication needs to be adjusted.

- Keep your primary care physician updated. They are an important part of the long-term management of bipolar disorder, even if you also see a psychiatrist.
- Avoid using alcohol and illegal drugs.
- Minimize stress. Try activities like meditation or tai chi. Make changes to simplify your life when possible.
- Turn to a support network. Know which family and friends are there to help during a crisis or a tough time. Educate your loved ones about bipolar disorder so they can best support you. Ask them to help you recognize the warning signs of manic or depressive episodes.
-
References and Relevant Resources
- 2019 National Survey on Drug Use and Health | Substance Abuse and Mental Health Services Administration (SAMHSA)
- Addressing Mental Illness and Substance Use as a Young Adults | SAMHSA
- Co-Occurring Disorders: Diagnoses and Integrated Treatments | SAMHSA
- Helping Families: Resources for Mental and Substance Use Disorders | SAMHSA
- Preventing Suicide | SAMHSA
- Bipolar Disorder | National Institute of Mental Health (NIMH)
- The Diagnosis and Treatment of Bipolar Disorder: Decision-Making in Primary Care | The Primary Care Companion for CNS Disorders
- Bipolar Disorder | Mayo Clinic
- Interdepartmental Serious Mental Illness Coordinating Committee (ISMICC) | SAMHSA
- SMI Adviser | American Psychological Association (APA) and SAMHSA
- Technology Transfer Centers (TTC) Program | SAMHSA
Last Updated: 09/27/2022
Living with Bipolar Disorder - HelpGuide.
 org
orgbipolar disorder
Along with treatment, there are many things you can do to cope with bipolar disorder. These 7 tips can help you manage symptoms, prevent relapse, and take control of your life.
How to cope with bipolar disorder
No matter how down or out of control you feel, it’s important to remember that you’re not powerless when it comes to bipolar disorder. Beyond the treatment you get from your doctor or therapist, there are many things you can do for yourself to reduce your symptoms and stay on track.
Living well with bipolar disorder requires certain adjustments. Like diabetics who take insulin or recovering alcoholics who avoid drinking, if you have bipolar disorder, it's important to make healthy choices for yourself. Making these healthy choices will help you keep your symptoms under control, minimize mood episodes, and take control of your life.
Managing bipolar disorder starts with proper treatment, including medication and therapy. But there is so much more you can do to help yourself on a day-to-day basis. These tips can help you influence the course of your illness, enabling you to take greater control over your symptoms, to stay well longer, and to quickly rebound from any mood episode or relapse.
But there is so much more you can do to help yourself on a day-to-day basis. These tips can help you influence the course of your illness, enabling you to take greater control over your symptoms, to stay well longer, and to quickly rebound from any mood episode or relapse.
Living with bipolar disorder tip 1: Get involved in your treatment
Be a full and active participant in your own treatment. Learn everything you can about bipolar disorder. Become an expert on the illness. Study up on the symptoms, so you can recognize them in yourself, and research all your available treatment options. The more informed you are, the better prepared you'll be to deal with symptoms and make good choices for yourself.
Using what you've learned about bipolar disorder, collaborate with your doctor or therapist in the treatment planning process. Don't be afraid to voice your opinions or questions. The most beneficial relationships between patient and healthcare provider work as a partnership.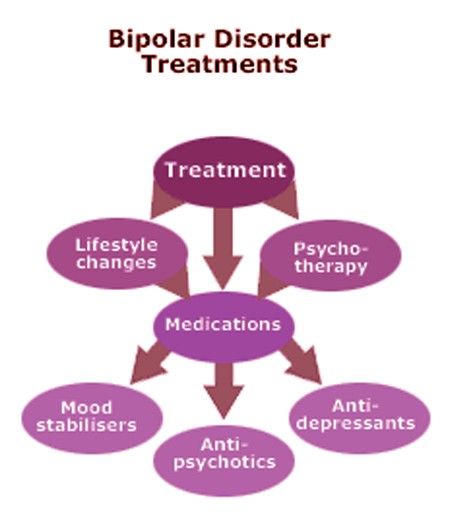 You may find it helpful to draw up a treatment contract outlining the goals you and your provider have agreed upon.
You may find it helpful to draw up a treatment contract outlining the goals you and your provider have agreed upon.
Improve your treatment by:
Being patient. Don't expect an immediate and total cure. Have patience with the treatment process. It can take time to find the right program that works for you.
Communicating with your treatment provider. Your treatment program will change over time, so keep in close contact with your doctor or therapist. Talk to your provider if your condition or needs change and be honest about your symptoms and any medication side effects.
Taking your medication as instructed. If you're taking medication, follow all instructions and take it faithfully. Don't skip or change your dose without first talking with your doctor.
Getting therapy. While medication may be able to manage some of the symptoms of bipolar disorder, therapy teaches you skills you can use in all areas of your life. Therapy can help you learn how to deal with your disorder, cope with problems, regulate your mood, change the way you think, and improve your relationships.
Therapy can help you learn how to deal with your disorder, cope with problems, regulate your mood, change the way you think, and improve your relationships.
With over 25,000 licensed counselors, BetterHelp has a therapist that fits your needs. It's easy, affordable, and convenient.
GET 20% OFF
Online-Therapy.com is a complete toolbox of support, when you need it, on your schedule. It only takes a few minutes to sign up.
GET 20% OFF
Teen Counseling is an online therapy service for teens and young adults. Connect with your counselor by video, phone, or chat.
GET 20% OFF
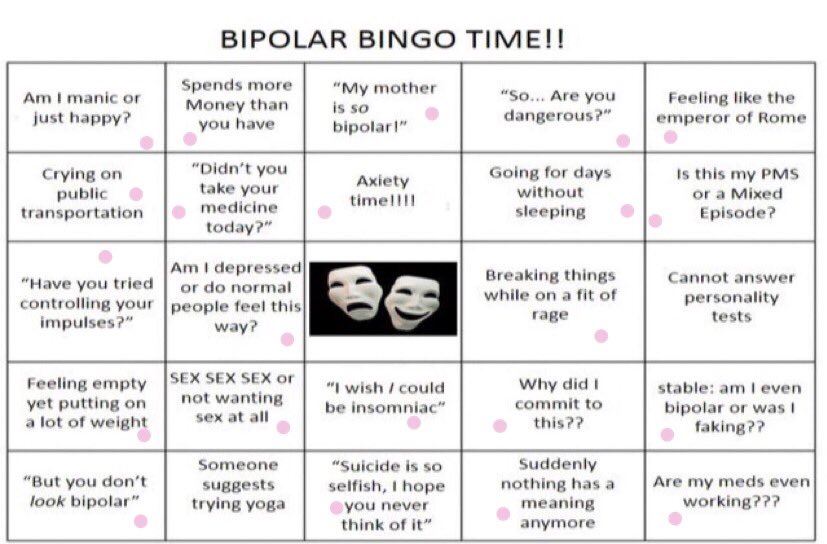
Tip 2: Monitor your symptoms and moods
In order to stay well, it's important to be closely attuned to the way you feel. By the time obvious symptoms of mania or depression appear, it is often too late to intercept the mood swing, so keep a close watch for subtle changes in your mood, sleeping patterns, energy level, and thoughts. If you catch the problem early and act swiftly, you may be able to prevent a minor mood change from turning into a full-blown episode of mania or depression.
Know your triggers and early warning signs
It's important to recognize the warning signs of an oncoming manic or depressive episode. Make a list of early symptoms that preceded your previous mood episodes. Also try to identify the triggers, or outside influences, that have led to mania or depression in the past. Common triggers include:
- stress
- financial difficulties
- arguments with your loved ones
- problems at school or work
- seasonal changes
- lack of sleep
| Common red flags for relapse |
| Warning signs of depression |
|
| Warning signs of mania or hypomania |
|
Knowing your early warning signs and triggers won't do you much good if you aren't keeping close tabs on how you're feeling. By checking in with yourself through regular mood monitoring, you can be sure that red flags don't get lost in the shuffle of your busy, daily life.
Keeping a mood chart is one way to monitor your symptoms and moods. A mood chart is a daily log of your emotional state and other symptoms you're having. It can also include information such as how many hours of sleep you're getting, your weight, medications you're taking, and any alcohol or drug use. You can use your mood chart to spot patterns and indicators of trouble ahead.
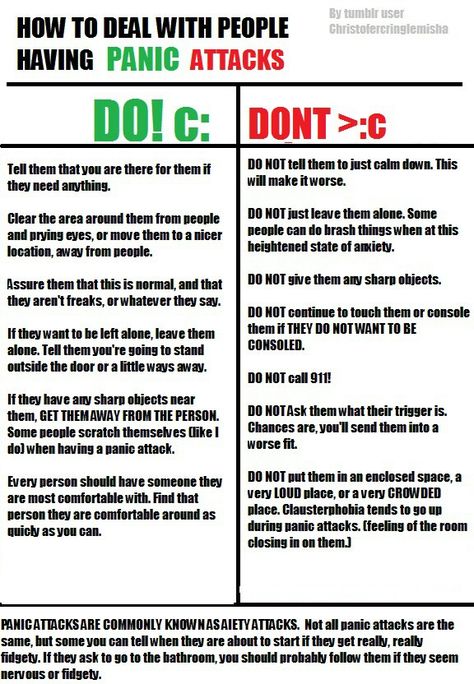
Tip 3: Act on warning signs
If you spot any warning signs of mania or depression, it's important to act swiftly. In such times, it's helpful to have a wellness toolbox to draw from. A wellness toolbox consists of coping skills and activities you can do to maintain a stable mood or to get better when you're feeling “off.”
In such times, it's helpful to have a wellness toolbox to draw from. A wellness toolbox consists of coping skills and activities you can do to maintain a stable mood or to get better when you're feeling “off.”
Develop a wellness toolbox
The coping techniques that work best will be unique to your situation, symptoms, and preferences. It takes experimentation and time to find a winning strategy. However, many people with bipolar disorder have found the following tools to be helpful in reducing symptoms and maintaining wellness:
- Talk to a supportive person.
- Get a full eight hours of sleep.
- Cut back on your activities.
- Attend a support group.
- Call your doctor or therapist.
- Do something fun or creative, or write in your journal.
- Take time for yourself to relax and unwind.
- Increase your exposure to light.
- Exercise.
- Ask for extra help from loved ones.
- Cut back on sugar, alcohol, and caffeine.

- Increase or decrease the stimulation in your environment.
Create an emergency action plan
Despite your best efforts, there may be times when you experience a relapse into full-blown mania or severe depression. In crisis situations where your safety is at stake, your loved ones or doctor may have to take charge of your care. Such times can leave you feeling helpless and out of control, but having a crisis plan in place allows you to maintain some degree of responsibility for your own treatment.
A plan of action typically includes:
A list of emergency contacts for your doctor, therapist, and close family members.
A list of all medications you are taking, including dosage information.
Symptoms that indicate you need others to take responsibility for your care, and information about any other health problems you have.
Treatment preferences such as who you want to care for you, what treatments and medications do and do not work, and who is authorized to make decisions on your behalf.
Tip 4: Reach out for face-to-face connection
Having a strong support system is essential to staying happy and healthy. Often, simply having someone to talk to face-to-face can be an enormous help in relieving bipolar depression and boosting your outlook and motivation. The people you turn to don't have to be able to “fix” you; they just have to be good listeners. The more people that you can turn to who will be available and good listeners, the more likely you are to manage your moods.
Don't isolate! Support for bipolar disorder starts close to home. It's important to have people you can count on to help you through rough times. Isolation and loneliness can cause depression, so regular contact with supportive friends and family members is therapeutic in itself. Reaching out to others is not a sign of weakness and it won't make you a burden. Support for bipolar disorder starts close to home. Your loved ones care about you and want to help. In order to manage bipolar disorder, it's essential that you have people you can count on to help you through rough times.
Join a bipolar disorder support group. Spending time with people who know what you're going through and can honestly say they've “been there” can be very therapeutic. You can also benefit from the shared experiences and advice of the group members.
Build new relationships. Isolation and loneliness make bipolar disorder worse. If you don't have a support network you can count on, take steps to develop new relationships. Try taking a class, joining a church or a civic group, volunteering, or attending events in your community.
10 tips for reaching out and building relationships
- Talk to one person about your feelings.
- Help someone else by volunteering.
- Have lunch or coffee with a friend.
- Ask a loved one to check in with you regularly.
- Accompany someone to the movies, a concert, or a small get-together.
- Call or email an old friend.
- Go for a walk with a workout buddy.
- Schedule a weekly dinner date.
- Meet new people by taking a class or joining a club.
- Confide in a counselor, therapist, or clergy member.
Tip 5: Develop an active daily routine
Your lifestyle choices, including your sleeping, eating, and exercise patterns, have a significant impact on your moods. There are many things you can do in your daily life to get your symptoms under control and to keep depression and mania at bay.
Build structure into your life. Developing and sticking to a daily schedule can help stabilize the mood swings of bipolar disorder. Include set times for sleeping, eating, socializing, exercising, working, and relaxing. Try to maintain a regular pattern of activity even through emotional ups and downs.
Exercise frequently and avoid sitting for long periods of time. Exercise has a beneficial impact on mood and may reduce the number of bipolar episodes you experience. Aerobic exercise such as running, swimming dancing, climbing or drumming – all activities that keep both arms and legs active are especially effective at treating depression. Try to incorporate at least 30 minutes of activity into your daily routine. Ten minutes here and there is just as effective as exercising for longer periods of time. Walking is a good choice for people of all fitness levels.
Try to incorporate at least 30 minutes of activity into your daily routine. Ten minutes here and there is just as effective as exercising for longer periods of time. Walking is a good choice for people of all fitness levels.
Keep a strict sleep schedule. Getting too little sleep can trigger mania, so it's important to get plenty of rest. For some people, losing even a few hours can cause problems. However, too much sleep can also worsen your mood. The best advice is to maintain a consistent sleep schedule.
Healthy sleep habits for managing bipolar disorder
- Go to bed and wake up at the same time each day.
- Avoid or minimize napping, especially if it interferes with your sleep at night.
- Instead of viewing screens or other stimulating activities before bed, try taking a bath, reading a book, or listening to relaxing music.
- Limit caffeine after lunch and alcohol at night as both interfere with sleep.
Tip 6: Keep stress to a minimum
Stress can trigger episodes of mania and depression in people with bipolar disorder, so keeping it under control is extremely important. Know your limits, both at home and at work or school. Don't take on more than you can handle and take time to yourself if you're feeling overwhelmed.
Know your limits, both at home and at work or school. Don't take on more than you can handle and take time to yourself if you're feeling overwhelmed.
Learn how to relax. Relaxation techniques such as deep breathing, meditation, yoga, and guided imagery can be very effective at reducing stress and keeping you on an even keel. A daily relaxation practice can improve your mood and keep depression at bay.
Make leisure time a priority. Do things for no other reason than that it feels good to do them. Go to a funny movie, take a walk on the beach, listen to music, read a good book, or talk to a friend. Doing things just because they are fun is no indulgence. Play is an emotional and mental health necessity.
Appeal to your senses. Stay calm and energized by appealing to your senses: sight, sound, touch, smell, and taste. Listen to music that lifts your mood, place flowers where you will see and smell them, massage your hands and feet, or sip a warm drink.
Tip 7: Watch what you put in your body
From the food you eat to the vitamins and drugs you take, the substances you put in your body have an impact on the symptoms of bipolar disorder—for better or worse.
Eat a healthy diet. There is an undeniable link between food and mood. For optimal mood, eat plenty of fresh fruits, vegetables, and whole grains and limit your fat and sugar intake. Space your meals out through the day, so your blood sugar never dips too low. High-carbohydrate diets can cause mood crashes, so they should also be avoided. Other mood-damaging foods include chocolate, caffeine, and processed foods.
Get your omega-3s. Omega-3 fatty acids may decrease mood swings in bipolar disorder. You can increase your intake of omega-3 by eating cold-water fish such as salmon, halibut, and sardines, soybeans, flaxseeds, canola oil, pumpkin seeds, and walnuts. Omega-3 is also available as a nutritional supplement.
Avoid alcohol and drugs. Drugs such as cocaine, ecstasy, and amphetamines can trigger mania, while alcohol and tranquilizers can trigger depression. Even moderate social drinking can upset your emotional balance. Substance use also interferes with sleep and may cause dangerous interactions with your medications. Attempts to self-medicate or numb your symptoms with drugs and alcohol only create more problems.
Be cautious when taking any medication. Certain prescription and over-the-counter medications can be problematic for people with bipolar disorder. Be especially careful with antidepressant drugs, which can trigger mania. Other drugs that can cause mania include over-the-counter cold medicine, appetite suppressants, caffeine, corticosteroids, and thyroid medication.
Authors: Melinda Smith, M.A., Jeanne Segal, Ph.D., and Robert Segal, M.A.
- References
Bipolar and Related Disorders.
 (2013). In Diagnostic and Statistical Manual of Mental Disorders. American Psychiatric Association. https://doi.org/10.1176/appi.books.9780890425787.x03_Bipolar_and_Related_Disorders
(2013). In Diagnostic and Statistical Manual of Mental Disorders. American Psychiatric Association. https://doi.org/10.1176/appi.books.9780890425787.x03_Bipolar_and_Related_DisordersBobo, William V. “The Diagnosis and Management of Bipolar I and II Disorders: Clinical Practice Update.” Mayo Clinic Proceedings 92, no. 10 (October 2017): 1532–51. https://doi.org/10.1016/j.mayocp.2017.06.022
Bonnín, Caterina Del Mar, María Reinares, Anabel Martínez-Arán, Esther Jiménez, Jose Sánchez-Moreno, Brisa Solé, Laura Montejo, and Eduard Vieta. “Improving Functioning, Quality of Life, and Well-Being in Patients With Bipolar Disorder.” The International Journal of Neuropsychopharmacology 22, no. 8 (August 1, 2019): 467–77. https://doi.org/10.1093/ijnp/pyz018
Hearing, CM, WC Chang, KL Szuhany, T Deckersbach, AA Nierenberg, and LG Sylvia. “Physical Exercise for Treatment of Mood Disorders: A Critical Review.” Current Behavioral Neuroscience Reports 3, no.
 4 (December 2016): 350–59. https://doi.org/10.1007/s40473-016-0089-y
4 (December 2016): 350–59. https://doi.org/10.1007/s40473-016-0089-yMelo, Matias Carvalho Aguiar, Elizabeth De Francesco Daher, Saulo Giovanni Castor Albuquerque, and Veralice Meireles Sales de Bruin. “Exercise in Bipolar Patients: A Systematic Review.” Journal of Affective Disorders 198 (July 2016): 32–38. https://doi.org/10.1016/j.jad.2016.03.004
“NIMH » Bipolar Disorder.” Accessed October 20, 2021. https://www.nimh.nih.gov/health/topics/bipolar-disorder
Qureshi, Naseem Akhtar, and Abdullah Mohammed Al-Bedah. “Mood Disorders and Complementary and Alternative Medicine: A Literature Review.” Neuropsychiatric Disease and Treatment 9 (2013): 639–58. https://doi.org/10.2147/NDT.S43419
Johnson, Lars, Ola Lundström, Anna Åberg-Wistedt, and Aleksander A Mathé. “Social Support in Bipolar Disorder: Its Relevance to Remission and Relapse.” Bipolar Disorders 5, no. 2 (2003): 129–37. https://doi.org/10.1034/j.1399-5618.2003.00021.x
Lam, Dominic H.
 , Peter Hayward, Edward R. Watkins, Kim Wright, and Pak Sham. “Relapse Prevention in Patients With Bipolar Disorder: Cognitive Therapy Outcome After 2 Years.” American Journal of Psychiatry 162, no. 2 (February 1, 2005): 324–29. https://doi.org/10.1176/appi.ajp.162.2.324
, Peter Hayward, Edward R. Watkins, Kim Wright, and Pak Sham. “Relapse Prevention in Patients With Bipolar Disorder: Cognitive Therapy Outcome After 2 Years.” American Journal of Psychiatry 162, no. 2 (February 1, 2005): 324–29. https://doi.org/10.1176/appi.ajp.162.2.324
DBSA Wellness Toolbox – Resources to help keep track of your symptoms and progress. (Depression and Bipolar Support Alliance)
Bipolar – Self-help resources. (Centre for Clinical Interventions)
Mood Charting (PDF) – Includes printable copy of the NIMH Daily Mood Chart. (CQAIMH)
Hotlines and support
In the U.S.: Call the NAMI HelpLine at 1-800-950-6264 or find DBSA Chapters/Support Groups in your area. (Depression and Bipolar Support Alliance)
UK: Call the peer support line at 0333 323 3880 and leave a message for a return call or Find a Support Group near you. (Bipolar UK)
Australia: Call the Sane Helpline at 1800 187 263 or find a local Support Group. (Bipolar Australia)
(Bipolar Australia)
Canada: Visit Finding Help for links to provincial helplines and support groups. (Mood Disorders Society of Canada)
India: Call the Helpline at 1860 2662 345 or 1800 2333 330. (Vandrevala Foundation)
Last updated: January 11, 2023
Treatment of bipolar affective disorder in St. Petersburg
- Main
- Psychotherapy
- Treatment of bipolar disorder
Usually the symptoms of bipolar disorder are attributed to personality traits or mood swings, which are logically explained. And, as a rule, even close relatives may not suspect that a person suffers from one of the most common mental disorders. nine0011
nine0011
Bipolar affective disorder is difficult to diagnose at an early stage of the disease. Therefore, we recommend that the patient himself or his relatives start keeping a diary, recording daily the features of the psycho-emotional state and key events that affect the occurrence of depressive and / or manic episodes. Such a diary will help the doctor determine the type of disease and prescribe the necessary treatment for bipolar disorder, and in the future to monitor the dynamics of the state of health. nine0011
Bipolar affective disorder is treated as an outpatient or inpatient clinic. At the peak of a depressive episode, when there is a risk of suicide, as well as to reduce the timing of the selection of pharmacotherapy, treatment of bipolar disorder should be carried out in a hospital. Bipolar personality disorder, left untreated, can progress and cause a deterioration in quality of life. Over a long distance, the disease inevitably leads to family conflicts, alcoholism or drug addiction, social degradation and, ultimately, suicide. nine0011
nine0011
With the right treatment for bipolar disorder, you can stabilize your psycho-emotional state and eventually achieve remission. Usually, it takes 15 to 20 days of hospital treatment to stabilize the psycho-emotional state. Achieving remission is possible subject to compliance with the prescribed drugs, with periodic outpatient visits to the attending physician to correct therapy.
Test: "Altman scale for self-assessment of mania"
Choose the answer that most accurately reflects your state of mind over the past week.
Bipolar disorder consultation:
+7 (812) 407-18-00
Thank you for your trust!
- Post discharge management
- Psychotherapy for couples and families
- Psychosocial personality correction
| Service | nine0044Price | |
|---|---|---|
| Outpatient treatment | ||
| Psychiatric consultation | nine00565 000 ₽ | |
| Psychotherapist appointment | 5 000 ₽ | nine0047|
Reception of the chief physician Bocharov A.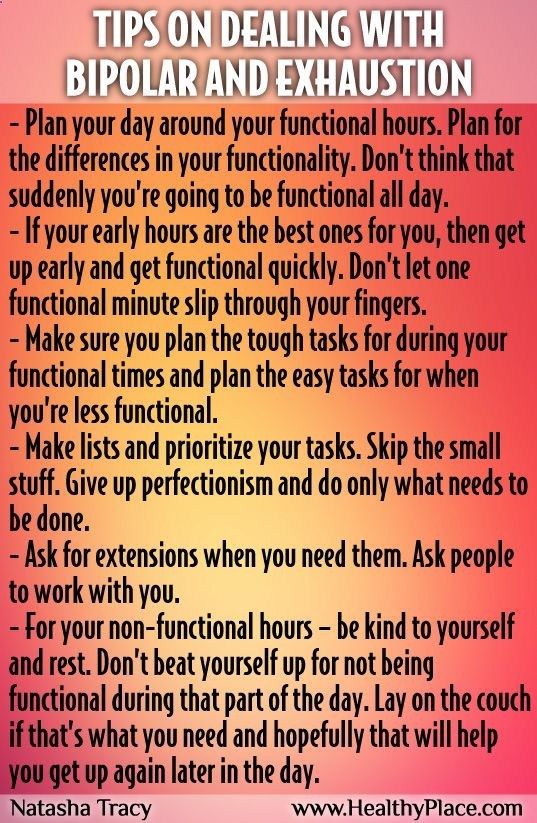 V. (Associate Professor, Ph.D.) V. (Associate Professor, Ph.D.) | 6 000 ₽ | |
| Psychiatric consultation at home | 6 000 ₽ | |
| Treatment in a hospital | ||
| Delivery to hospital | For free nine0050 | |
| Standard Chamber | 8 900 ₽ | |
| 3-bed superior room | nine0053 12 000 ₽ | |
| 2-bed superior room | 15 000 ₽ | |
| 1 local VIP room | 19 500 ₽ | |
| Doctor's appointment 2 weeks after discharge | For free | |
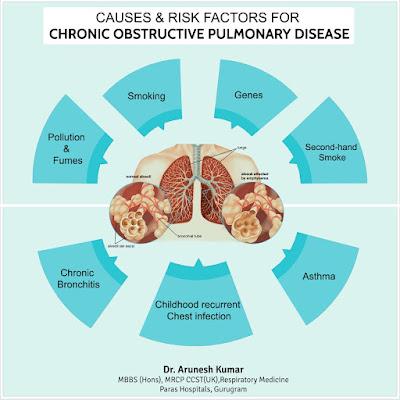
Causes of bipolar disorder
The main causes of bipolar affective disorder include genetic predisposition, disturbances in the metabolism of neurotransmitters and changes in nerve cells, and severe stress. In other words, the disease can occur in any person, regardless of age, gender and social status. nine0011
In other words, the disease can occur in any person, regardless of age, gender and social status. nine0011
Genetic causes
Genetic causes of bipolar affective disorder are a risk factor for the development of the disease. It should be emphasized that the disease itself is not inherited. However, inherited features of the regulation of neurotransmitters in the brain increase the risk of developing bipolar disorder in close relatives (for example, siblings) by 4–7 times.
Metabolic disorders in the brain
Another cause of bipolar disorder can be a metabolic disorder in the brain. An abnormal increase and decrease in the concentration of biologically active chemical compounds (mainly dopamine, serotonin and norepinephrine), which transmit nerve signals, is the cause of the manic and depressive phases. nine0011
Severe stress and the “biological defect” model
The psyche of each person has an individual threshold for resistance to stress. And the word "stress" does not necessarily mean difficult life situations - be it a dismissal, financial problems, family conflicts, divorce, or the death of a loved one. Stress factors can be an upcoming birthday, puberty, marriage or the birth of a child.
Stress factors can be an upcoming birthday, puberty, marriage or the birth of a child.
nine0011
Fig. Zubin and Spring's stress-vulnerability model.
a) Low vulnerability, BD can only develop under severe stress.
b) High vulnerability, BAD develops even under low intensity stress.
c) Individual vulnerability, corresponds to the intensity of stress.
Symptoms of bipolar disorder
Treatment of bipolar disorder in our clinic
Typically treatment of bipolar disorder is carried out in the hospital of the clinic. The conditions of the hospital allow to reduce the duration of treatment - to conduct an examination, quickly normalize the patient's psycho-emotional state, select drugs and their minimum effective dosage, conduct dynamic monitoring and adjust pharmacotherapy.
Examination
On the day of hospitalization, the patient undergoes an examination, which includes:
- psychodiagnostics;
- therapist consultation;
- neurologist consultation; nine0004
- laboratory tests;
- EEG.

Lab tests include blood tests for hormonal status (generally, thyroid problems are found in people with bipolar disorder). Pathology of the thyroid gland directly affects mood swings, therefore, when treating bipolar disorder, it is important for a doctor to know the patient's hormonal background, for example: to prescribe drugs that normalize the thyroid gland, or to exclude lithium, which inhibits its work. nine0011
Drug treatment
Based on the results, the doctor will prescribe a treatment for bipolar disorder - select drugs that relieve autonomic symptoms and normalize the psycho-emotional state (normotimics, antidepressants). Usually, the first signs of improvement in mental health are observed on the fifth day after the start of drug treatment for bipolar disorder. However, the final correction of psychopharmacotherapy can take up to 10 days.
Psychotherapeutic assistance
After stabilization of the psycho-emotional state, the patient begins attending group psychotherapy sessions. Group sessions with psychotherapists and psychologists of our clinic are held daily. Under the guidance of experienced facilitators, the patient will have the opportunity to work through their experiences and fears, get rid of pathological patterns, and receive professional help from psychologists and psychotherapists with clinical experience.
Group sessions with psychotherapists and psychologists of our clinic are held daily. Under the guidance of experienced facilitators, the patient will have the opportunity to work through their experiences and fears, get rid of pathological patterns, and receive professional help from psychologists and psychotherapists with clinical experience.
Post-discharge management
Discharge is usually done after remission, 14-21 days treatment for bipolar disorder . Then the patient continues to take the prescribed drugs and visit the attending physician once every 1-3 months for 1 year. Subject to the achievement of stable remission, after 1 year, in some cases, it is possible to completely abandon the drug treatment of bipolar disorder.
Treatment of bipolar disorder in St. Petersburg is carried out at: st. Marata, 78. We take on complex cases, including the treatment of adolescent patients and patients with drug resistance. nine0011
Treatment of bipolar comorbidities
Psychotherapeutic treatment of bipolar disorder
Psychotherapeutic treatment of bipolar affective disorder, as an adjunct to pharmacotherapy, allows a faster deep remission. Such treatment begins already in the hospital and can be continued after discharge. The number of sessions, their frequency and the form of psychotherapy (individual, family or hypnotherapy) you can choose together with the doctor. nine0011
Such treatment begins already in the hospital and can be continued after discharge. The number of sessions, their frequency and the form of psychotherapy (individual, family or hypnotherapy) you can choose together with the doctor. nine0011
In addition to individual psychotherapy sessions that correct the patient's personality, family consultations are possible. At family therapy sessions, relatives can better understand the nature of the disease and learn the right behavior that contributes to a speedy recovery. In addition, studies show that psychotherapeutic care reduces the number of hospitalizations for relapses.
Cognitive Behavioral Therapy
Cognitive Behavioral Therapy corrects abnormal behavior and thinking patterns that occur in patients with bipolar affective disorder. In addition, during psychotherapy sessions, the patient will be able to learn to recognize relapses of the disease, cope with them on their own or seek help in time, preventing a full-blown episode. nine0011
nine0011
Family Therapy
If bipolar disorder has caused a deterioration in relationships with those closest to you, we recommend that you seek the help of a family therapist. The doctor will help relatives understand the features of the disease, resolve interpersonal conflicts and restore harmony in the family.
Individual sessions of psychotherapy help overcome mood swings during the formation of stable remission. By learning to control the psycho-emotional state, as well as working through pathological patterns, it becomes easier for the patient to cope with exacerbations of the condition, which may occur for some time after undergoing treatment in the hospital. nine0011
Consequences of not getting help
To describe what bipolar disorder is in simple terms, it is necessary to understand the specifics of the condition in which people with this disease find themselves. Living with bipolar affective disorder is not easy. People learn to live with bipolar disorder over the years, experiencing rapid ups and downs in both career and family life. Imagine that you are walking on a zebra - now you are full of strength and enthusiasm, and the next minute you stop in a stupor and everything falls out of your hands: life loses its meaning, achievements no longer seem so significant, you want to escape from everyday life, hide from your eyes relatives, change their place of residence and work. nine0011
Imagine that you are walking on a zebra - now you are full of strength and enthusiasm, and the next minute you stop in a stupor and everything falls out of your hands: life loses its meaning, achievements no longer seem so significant, you want to escape from everyday life, hide from your eyes relatives, change their place of residence and work. nine0011
Add to this state of misunderstanding on the part of relatives and friends, who begin to consider you frivolous and incapable of finishing what you started to the end. At some point, you quarrel with relatives and, it would seem, nothing keeps you in this familiar and gray life. You can stay in this state for months, and then everything starts all over again. You are full of strength and enthusiasm - set yourself bold tasks, hardly sleep, call friends and want to hug strangers (just like that, because you are full of boundless love). nine0011
However, few "lucky people" with bipolar disorder manage to experience a depressive episode on their own from year to year.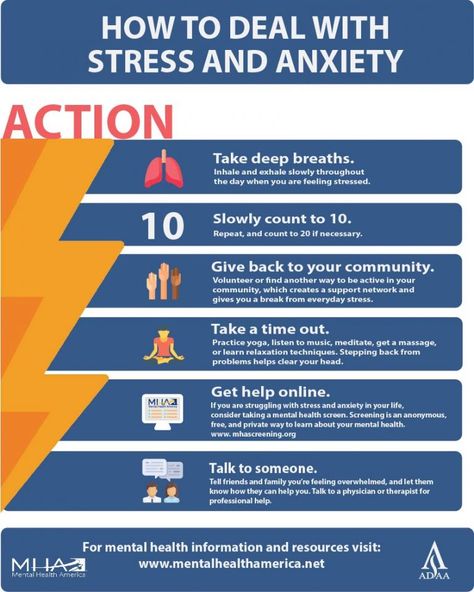 Moreover, the depressive state distorts reality no less than the euphoria of the manic stage. It can take years or decades to learn how to "live" with bipolar disorder. But many do not succeed in doing this - and the lives of these people cannot be envied. Unfortunately, some of them are socially degraded or commit suicide.
Moreover, the depressive state distorts reality no less than the euphoria of the manic stage. It can take years or decades to learn how to "live" with bipolar disorder. But many do not succeed in doing this - and the lives of these people cannot be envied. Unfortunately, some of them are socially degraded or commit suicide.
Bipolar disorder in women
If you do not seek help in time, bipolar disorder in women can lead to family conflicts, divorce, promiscuity, and the development of borderline mental disorders. To a lesser extent, women with bipolar disorder are prone to alcoholism and drug addiction, although this scenario cannot be completely excluded.
Bipolar disorder in men
The development of bipolar disorder in men causes deterioration of relationships at work (possibly dismissal), family quarrels, seeking relationships on the side, addiction to alcohol and / or gambling (gambling, Internet surfing). Ultimately, domestic violence is not ruled out against the backdrop of a depressive episode. nine0011
nine0011
Remember, mental disorders, like somatic diseases, require treatment. When you find yourself in a difficult situation, when your loved one suffers from bipolar disorder, it is necessary to remain calm and show compassion. As a rule, patients themselves cannot adequately assess their condition, so it is often the relatives who need to take the first step to start treatment and sign up for a consultation with a psychiatrist.
Sources
Bipolar disorder, focus on depression — https://psychiatr.ru
Treatments for bipolar disorder - https://www.webmd.com
Social cognitive deficits in patients with bipolar disorder in remission - https://pubmed.ncbi.nlm.nih.gov
Psychiatric disorders - https:/ /www.who.int
Update date: 01/20/2023
- Bipolar disorder
- Panic attacks
Make an appointment
Date and time: (not set)
Make an appointment with a psychotherapist
Make an appointment with a psychotherapist
Select the date and time of your appointment
Today
January 25
Tomorrow
January 26
Friday
January 27
Saturday
January 28
Sunday
January 29
Monday
January 30
Tuesday
January 31
Wednesday
February 01
Thursday
February 02
Friday
February 03
Saturday
February 04
Sunday
05 February
Monday
February 06
Tuesday
February 07
Wednesday
February 08
Thursday
09 February
Friday
February 10
Saturday
February 11
Sunday
February 12
Monday
February 13
Tuesday
February 14
Wednesday
February 15
Thursday
February 16
Friday
February 17
Saturday
February 18
Sunday
February 19
Monday
February 20
Tuesday
February 21
Wednesday
February 22
Thursday
February 23
Friday
February 24
Saturday
February 25
Sunday
February 26
Monday
February 27
Tuesday
February 28
Bipolar disorder treated
Gorkov Alexander
Ivanovich
Psychotherapist, psychologist
Top category
Experience 49 years
Psychotherapist, psychologist
Experience 49 years
Sinenchenko Andrey
Georgievich
Psychiatrist, psychotherapist
PhD
Work experience 23 years
Psychiatrist, psychotherapist, narcologist
Work experience 23 years
Bocharov Alexey
Viktorovich
Psychiatrist, psychotherapist
Head physician of clinic
Experience 42 years
Psychiatrist, psychotherapist, sexologist, child psychiatrist
Work experience 42 years
Dobromyslov Vitaly
Germanovich
Psychotherapist, hypnotherapist
Top category
Experience 28 years
Psychotherapist, hypnotherapist, narcologist
Work experience 28 years
Chuban Olga
Ivanovna
Psychiatrist, psychotherapist
First category
Work experience 14 years
Psychiatrist, psychotherapist, psychologist
Work experience 14 years
Zaripov Airat
Akhmadullovich
Psychotherapist, psychologist
Top category
Experience 26 years
Psychotherapist, psychologist
Work experience 26 years
nine0010 Suslennikova ElenaViktorovna
Psychiatrist, psychotherapist
First category
Experience 26 years
Psychiatrist, psychotherapist
Work experience 26 years
Nazarova Tamara
Kimovna
Psychotherapist, narcologist
Top category
Experience 39 years
Psychotherapist, psychologist, narcologist
Experience 39 years
Prokhorchev Konstantin
Sergeevich
Psychiatrist, psychotherapist
First category
Work experience 13 years
Psychiatrist, psychotherapist
Work experience 13 years
Miroshnikova Natalia
Valentinovna
Top category
Experience 37 years
Psychotherapist, psychologist
Work experience 37 years
Zhelobetskaya Maria
Sergeevna
Psychiatrist, psychotherapist
Top category
Work experience 23 years
Psychiatrist, psychotherapist
Work experience 23 years
Stetsiv Lyudmila
Gennadievna
Psychiatrist, psychotherapist
PhD
Experience 32 years
Psychiatrist, psychotherapist
Work experience 32 years
Endrzheevskaya Diana
Vadimovna
Psychiatrist, psychotherapist
Second category
Work experience 15 years
Psychiatrist, child psychiatrist, psychotherapist
Work experience 15 years
Usov Grigory
Mikhailovich
Psychiatrist, psychotherapist
MD
Work experience 25 years
Psychiatrist, psychotherapist
Experience 25 years
Sannikova Elena
Georgievna
Psychologist, psychotherapist
Experience 20 years
Psychologist, psychotherapist, sexologist
Experience 20 years
Zun Sergey
Andreevich
Psychiatrist, narcologist
PhD
Experience 34 years
Psychiatrist, narcologist, psychotherapist
Work experience 34 years
Leave a request for a call:
+7 (812) 407-18-00
Bipolar Disorder | Symptoms, complications, diagnosis and treatment
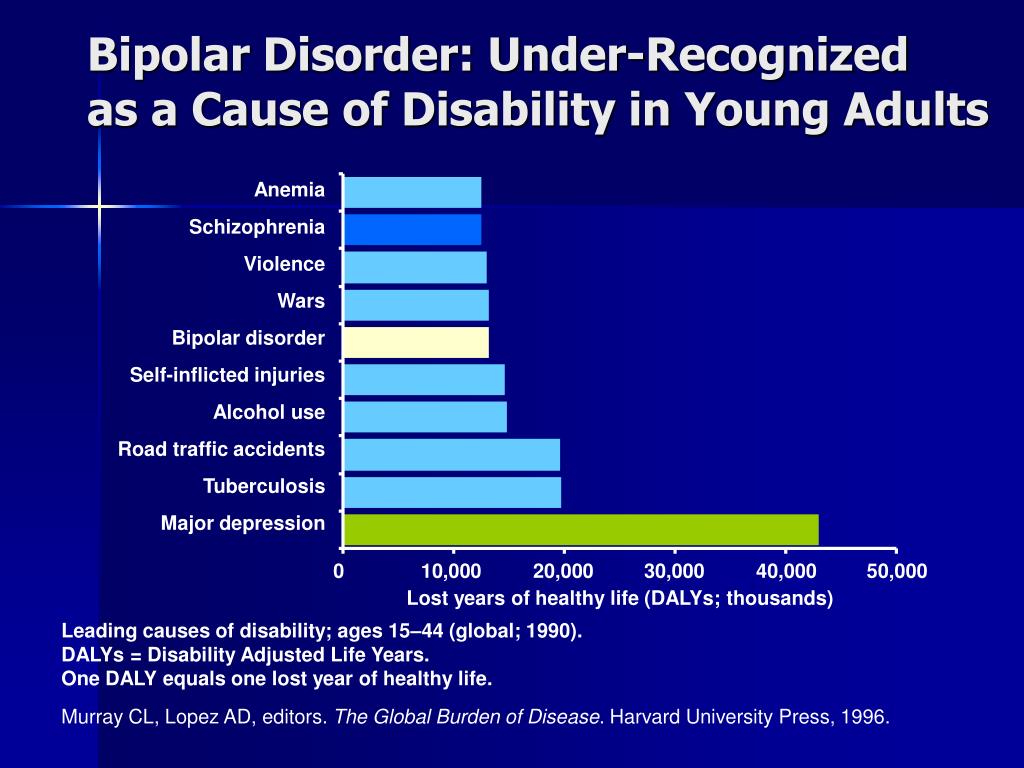
Bipolar disorder, formerly called manic depression, is a mental health condition that causes extreme mood swings that include emotional highs (mania or hypomania) and lows (depression).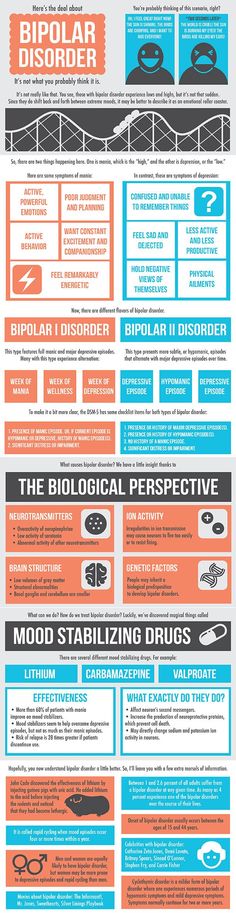 Episodes of mood swings may occur infrequently or several times a year. nine0011
Episodes of mood swings may occur infrequently or several times a year. nine0011
When you become depressed, you may feel sad or hopeless and lose interest or pleasure in most activities. When the mood shifts to mania or hypomania (less extreme than mania), you may feel euphoric, full of energy or unusually irritable. These mood swings can affect sleep, energy, alertness, judgment, behavior, and the ability to think clearly.
Although bipolar disorder is a lifelong condition, you can manage your mood swings and other symptoms by following a treatment plan. In most cases, bipolar disorder is treated with medication and psychological counseling (psychotherapy). nine0011
Symptoms
There are several types of bipolar and related disorders. These may include mania, hypomania, and depression. The symptoms can lead to unpredictable changes in mood and behavior, leading to significant stress and difficulty in life.
- Bipolar disorder I.
 You have had at least one manic episode, which may be preceded or accompanied by hypomanic or major depressive episodes. In some cases, mania can cause a break with reality (psychosis). nine0004
You have had at least one manic episode, which may be preceded or accompanied by hypomanic or major depressive episodes. In some cases, mania can cause a break with reality (psychosis). nine0004 - Bipolar disorder II. You have had at least one major depressive episode and at least one hypomanic episode, but never had a manic episode.
- Cyclothymic disorder. You have had at least two years - or one year in children and adolescents - many periods of hypomanic symptoms and periods of depressive symptoms (though less severe than major depression).
- Other types. nine0178 These include, for example, bipolar and related disorders caused by certain drugs or alcohol or due to health conditions such as Cushing's disease, multiple sclerosis or stroke.
Bipolar II is not a milder form of Bipolar I but is a separate diagnosis. Although bipolar I manic episodes can be severe and dangerous, people with bipolar II can be depressed for longer periods of time, which can cause significant impairment. nine0011
nine0011
Although bipolar disorder can occur at any age, it is usually diagnosed in adolescence or early twenties. Symptoms can vary from person to person, and symptoms can change over time.
Mania and hypomania
Mania and hypomania are two different types of episodes, but they share the same symptoms. Mania is more pronounced than hypomania and causes more noticeable problems at work, school, and social activities, as well as relationship difficulties. Mania can also cause a break with reality (psychosis) and require hospitalization. nine0011
Both a manic and a hypomanic episode include three or more of these symptoms:
- Abnormally optimistic or nervous
- Increased activity, energy or excitement
- Exaggerated sense of well-being and self-confidence (euphoria)
- Reduced need for sleep
- Unusual talkativeness
- Distractibility
- Poor decision-making, such as speculation, sexual intercourse, or irrational investment
Major depressive episode
Major depressive episode includes symptoms that are severe enough to cause noticeable difficulty in daily activities such as work, school, social activities, or relationships.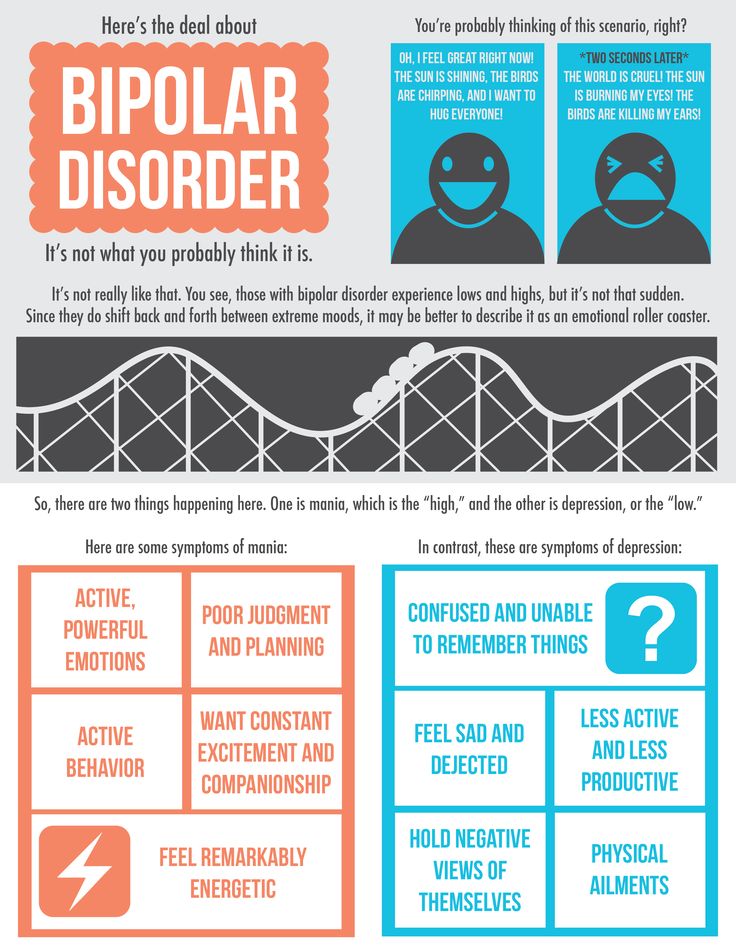 An episode includes five or more of these symptoms:
An episode includes five or more of these symptoms:
- Depressed mood, such as feeling sad, empty, hopeless, or tearful (in children and adolescents, depressed mood may manifest as irritability)
- Marked loss of interest or feeling of displeasure in all (or nearly all) activities
- Significant weight loss with no diet, weight gain, or decreased or increased appetite (in children, failure to gain weight as expected may be a sign of depression)
- Either insomnia or sleeping too much
- Either anxiety or slow behavior
- Fatigue or loss of energy nine0031 Feelings of worthlessness or excessive or inappropriate guilt
- Decreased ability to think or concentrate, or indecisiveness
- Thinking, planning or attempting suicide
Other features of bipolar disorder
Signs and symptoms of bipolar I and bipolar II disorder may include other signs such as anxiety disorder, melancholia, psychosis, or others.