Is lithium a controlled substance
Lithium: Side Effects, Uses, Dosage, and More
If you have bipolar disorder, your medical professional may prescribe a drug called lithium.
Lithium is used for the following purposes in adults and some children:
- acute (short-term) treatment of manic and mixed episodes related to bipolar I disorder
- maintenance (long-term) treatment of bipolar I disorder
We explain more about bipolar disorder and how lithium helps treat it in the “How is lithium used for bipolar I disorder?” section below.
Lithium details
Lithium’s classification (the group of drugs it belongs to) is a mood stabilizer. It’s a generic medication.
Comparing lithium’s forms
Lithium comes in several forms, all of which you take by mouth:
- extended-release (ER) tablets, which are long-acting
- immediate-release (IR) tablets, which are short-acting
- capsules
- liquid solution
We cover only the capsule, liquid solution, and IR tablet forms of lithium in this article. These forms of lithium aren’t available as brand-name drugs.
If you’d like to learn about lithium ER tablets, your medical professional or pharmacist can tell you more.
Most medications, including lithium, may cause side effects that can be serious or mild. To give you an idea of what might occur with lithium, we’ve listed some of the medication’s more common side effects below. It’s important to note that we haven’t included all the potential side effects.
For more complete information about possible side effects of lithium, you can talk with your medical professional or pharmacist. They may also be able to recommend tips on how to help prevent and ease side effects.
Note: Certain factors may affect a medication’s side effects. These factors can include other health conditions you may have, other drugs you may be taking, and your age.
Mild side effects
Some of the mild side effects that lithium may cause are listed below. For information about other mild side effects of the drug, we suggest that you talk with your medical professional or pharmacist. It may also be helpful to refer to the medication guide for lithium.
It may also be helpful to refer to the medication guide for lithium.
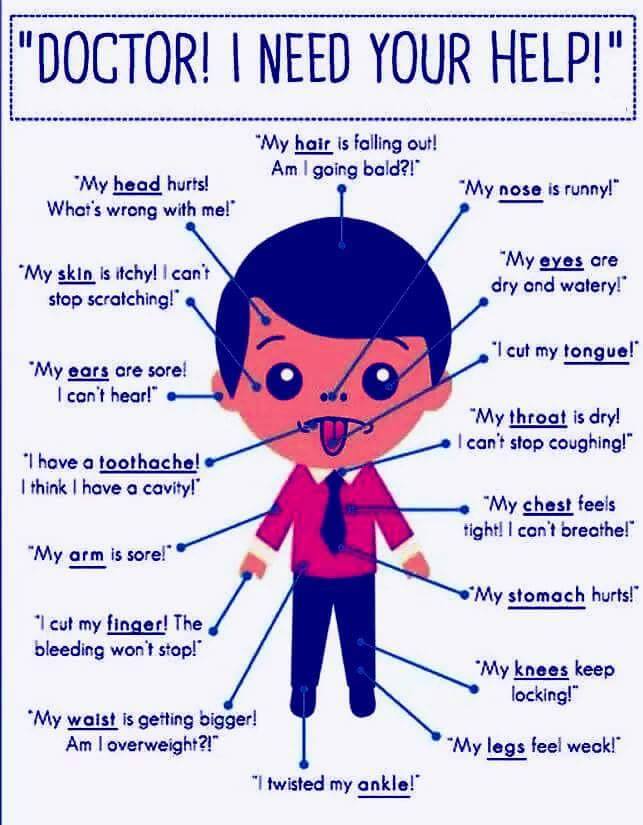
Mild side effects of lithium that have been reported in studies include:
- weight gain or weight loss*
- rash*
- hair loss
- headache
- blurry vision
- dizziness
- feelings of general discomfort, such as feeling ill
- increased thirst
- loss of appetite
- nausea or vomiting
- trouble coordinating muscle movements, which can lead to problems walking or keeping your balance
Mild side effects of many drugs tend to lessen in a couple of days or a few weeks. But if you find that the side effects bother you, we encourage you to talk with your medical professional or pharmacist.
* For details about this side effect, you can see “Side effects: A closer look” below.
Serious side effects
Lithium may cause serious side effects, but this isn’t common. If you do develop serious side effects while taking lithium, be sure to call your medical professional immediately. If you feel as if you’re having a medical emergency, call 911 or your local emergency number right away.
If you feel as if you’re having a medical emergency, call 911 or your local emergency number right away.
Serious side effects of lithium that have been reported in studies include the following:
- tremors (shaking you can’t control)*
- allergic reaction*
- thyroid problems, such as hypothyroidism (low thyroid hormone levels) or hyperthyroidism (high thyroid hormone levels)
- low level of sodium in your blood
- heart problems, such as Brugada syndrome (a condition that causes an abnormal heart rhythm)
- hyperparathyroidism (an overactive parathyroid gland, which can lead to a high level of calcium in your blood)
- increased pressure around your brain, which can lead to vision problems
- kidney problems, such as chronic kidney disease
- nerve problems, such as neuroleptic malignant syndrome (a rare reaction that can occur after taking certain drugs)
- serotonin syndrome (a condition caused by the buildup of the chemical serotonin in your body)
- urinating larger amounts than usual
- lithium toxicity† (boxed warning)
* For details about this side effect, you can see “Side effects: A closer look” below.
† See the “What is lithium toxicity?” section below for more information.
Long-term side effects
It’s possible that lithium may cause long-term side effects. But the length of time lithium’s side effects last tends to vary from person to person.
For example, some side effects like hypothyroidism (low thyroid hormone levels) and kidney problems may cause effects that last for months or years. Lithium toxicity (high levels of lithium in your blood) may also cause certain long-term problems.
To help monitor for these side effects, your medical professional may give you thyroid or kidney function tests periodically during treatment. They’ll also check your lithium levels frequently with a blood test.
For more details about what to expect with lithium treatment, you can talk with your medical professional.
Side effects: A closer look
This section provides a close-up look at key side effects of lithium.
Weight gain or weight loss
Weight gain or weight loss may occur with lithium. But weight changes were a rare side effect in studies of the drug.
But weight changes were a rare side effect in studies of the drug.
Changes in weight are a common symptom of depressive episodes related to bipolar disorder. And lithium is used to treat bipolar I disorder. So you may gain or lose weight while you’re taking lithium because your symptoms are improving. Weight changes may not be a side effect of the drug itself.
Tips for managing
If you’re concerned about weight changes while taking lithium, we encourage you to talk with your medical professional. They can suggest ways to help you maintain a weight that’s healthy for you.
Tremors
Tremors (shaking you can’t control) may occur with lithium. This was a common side effect in studies of the drug.
You may have different types of tremors with lithium. Some may be mild, such as shaky hands. But others can be a symptom of more serious conditions.
For example, tremors that affect your arms, legs, or whole body may be more severe. This type of tremor can be a symptom of serious conditions such as:
This type of tremor can be a symptom of serious conditions such as:
- lithium toxicity*
- serotonin syndrome (a condition caused by the buildup of the chemical serotonin in your body)
- nerve problems, such as neuroleptic malignant syndrome
* Lithium has a boxed warning from the Food and Drug Administration (FDA) about lithium toxicity. For details, you can see the “What is lithium toxicity?” section above.
Tips for managing
If you have tremors while taking lithium, it’s recommended that you tell your medical professional right away. They can help figure out if the side effect is a symptom of a more serious condition.
Rash
A rash may occur with lithium. This side effect was more common in children than in adults during studies of the drug.
You may have other symptoms along with rash. These include:
- itchy skin
- dry skin
- skin redness or darkened skin color
- swelling
Tips for managing
If you have a rash while taking lithium, we suggest you tell your medical professional right away. A rash can be a sign of a serious allergic reaction. Your doctor can recommend ways to treat this side effect.
A rash can be a sign of a serious allergic reaction. Your doctor can recommend ways to treat this side effect.
Allergic reaction
Many drugs, including lithium, can cause an allergic reaction. Even though allergic reaction wasn’t reported in studies of lithium, it can still happen.
Symptoms that can occur with a mild allergic reaction may include:
- itchiness
- skin rash
- flushing (temporary warmth, redness, or deepening of skin color)
A more severe allergic reaction may also occur, but this is rare. Symptoms of a severe allergic reaction may include swelling of your mouth, tongue, or throat, which may cause trouble breathing. You may also experience swelling under your skin, often in your lips, eyelids, hands, or feet.
Tips for managing
If you have symptoms of an allergic reaction to lithium, be sure to call your medical professional immediately. If you feel as if you’re having a medical emergency, call 911 or your local emergency number right away.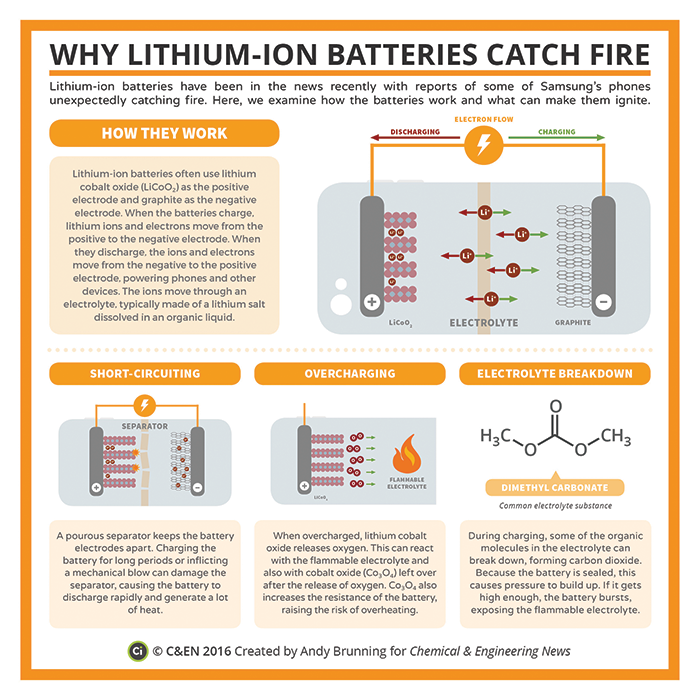
Lithium has a boxed warning about lithium toxicity. A boxed warning is a serious warning from the Food and Drug Administration (FDA). This warning appears on the drug’s label and alerts you to possible serious risks.
Lithium toxicity refers to a high level of lithium in your blood, which may cause serious side effects.
Your risk for lithium toxicity may be higher if you:
- were recently ill
- have heart problems
- have kidney problems
- have changes in your sodium levels or potassium levels
- are dehydrated
- take other medications that cause the level of lithium in your blood to increase
To lessen your risk for lithium toxicity, your medical professional will check your lithium levels frequently with a blood test.
Symptoms of lithium toxicity
Lithium toxicity can cause the following mild or moderate symptoms:
- blurry vision
- drowsiness
- lightheadedness
- loss of coordination
- nausea, vomiting, or diarrhea
- ringing in your ears
- slurred speech
- tremors (shaking you can’t control)
- weakness
More serious symptoms of lithium toxicity include coma, seizures, and death. You may also have heart problems (such as an abnormal heart rhythm) or kidney problems (such as kidney failure).
You may also have heart problems (such as an abnormal heart rhythm) or kidney problems (such as kidney failure).
If you have any symptoms of lithium toxicity, it’s important to tell your medical professional right away. They’ll likely lower your lithium dosage. Or they may switch you to a different treatment for your condition.
If you have bipolar I disorder, your medical professional may prescribe lithium for you.
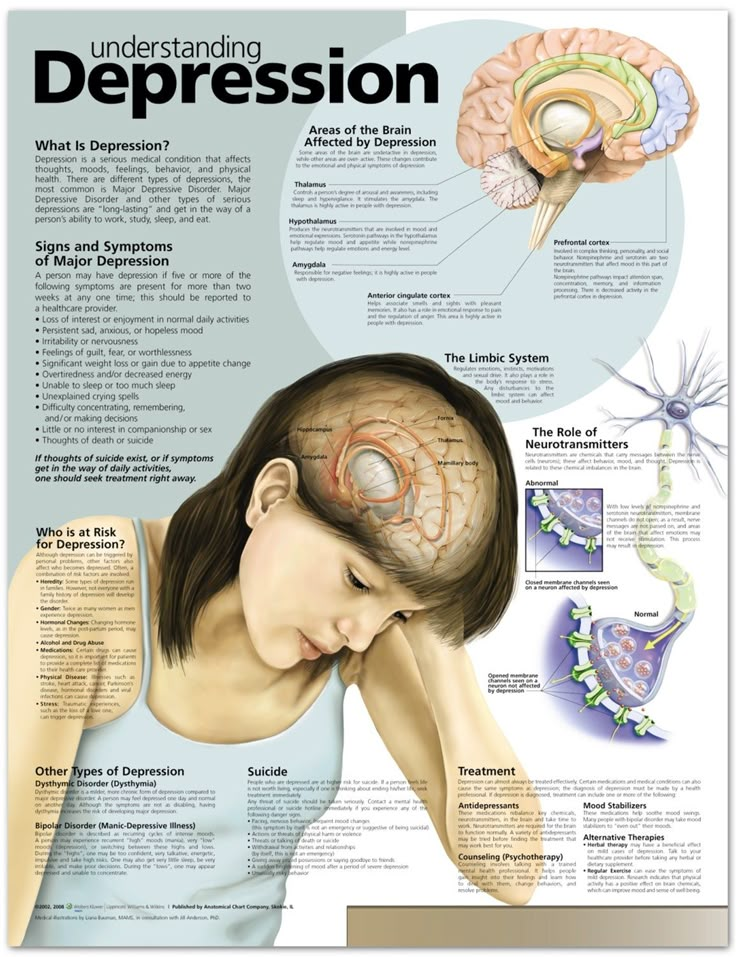
Bipolar disorder causes extreme mood shifts that may last for several days. Generally, these moods alternate between manic episodes and depressive episodes. Manic episodes are periods of very high energy and excitement. Depressive episodes are periods in which you have depression symptoms.
You may also have mixed episodes with bipolar disorder. Mixed episodes (also called mixed features) may describe either:
- periods of mania that occur with symptoms of depression, or
- periods of depression that occur with symptoms of mania
Lithium is specifically used for acute (short-term) treatment of manic and mixed episodes related to bipolar I disorder. Lithium can also be used as a maintenance (long-term) treatment for bipolar I disorder. Lithium is used for these purposes in adults and children ages 7 years and older.
Lithium can also be used as a maintenance (long-term) treatment for bipolar I disorder. Lithium is used for these purposes in adults and children ages 7 years and older.
How lithium makes you feel
Lithium is a mood stabilizer. This means it can help stabilize the mood changes that bipolar disorder causes. The effects of lithium can vary from person to person. The way the drug works in your body isn’t exactly known.
If you have questions about how lithium might make you feel, you can talk with your medical professional or pharmacist.
Below we share answers to some commonly asked questions about lithium.
Is lithium approved to treat depression?
Lithium isn’t approved to treat depression. But it may be prescribed off-label to treat certain types of depression. Off-label means using a drug for a condition it hasn’t been approved to treat.
Lithium is approved to treat manic and mixed episodes related to bipolar I disorder. It’s also sometimes used off-label to treat depressive episodes caused by bipolar I disorder.
If you’d like to learn more about using lithium for depression and what this dosage would be, you can talk with your medical professional or pharmacist.
How does lithium work? And what is its half-life?
Lithium is a mood stabilizer. This means it can help stabilize the mood changes that bipolar disorder causes. But the way lithium works* to treat this condition isn’t known for sure.
The half-life of lithium is 18 to 36 hours. (A drug’s half-life is the amount of time it takes for half of a dose to leave your system.) So it takes about 18 to 36 hours for your body to get rid of half of a dose of lithium.
* The way a drug works in your body is called its “mechanism of action.”
Can lithium be used for schizophrenia or anxiety?
Although lithium isn’t approved to treat schizophrenia or anxiety, it may be prescribed off-label to treat these conditions. Off-label means using a drug for a condition it hasn’t been approved to treat.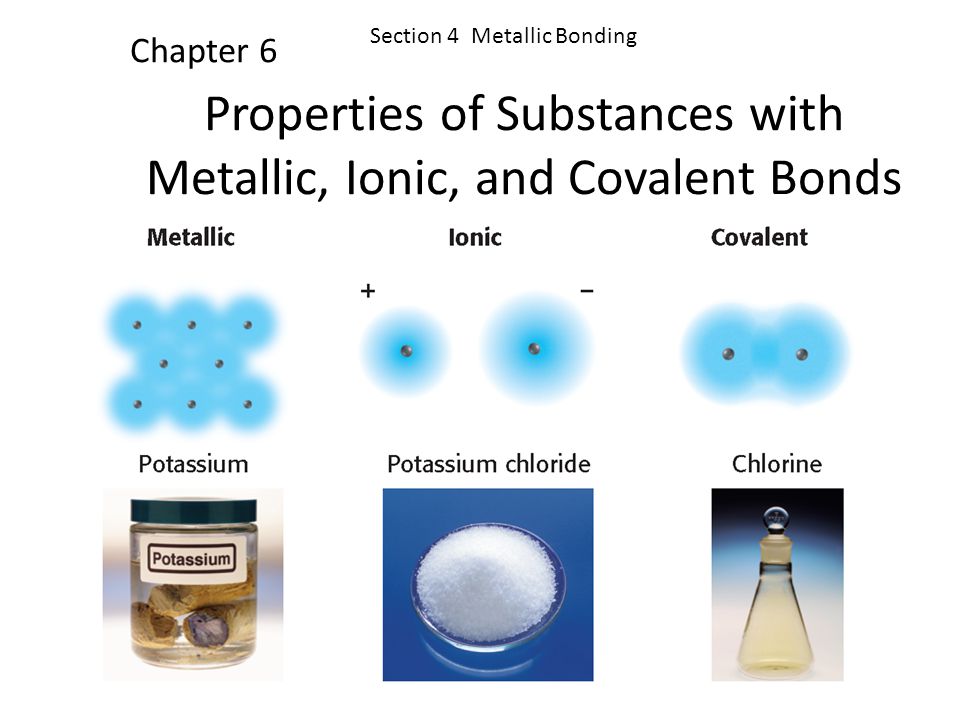
When used for these purposes, lithium is usually taken along with other drugs that treat schizophrenia or anxiety. If you’d like to learn more about lithium treatment for these conditions, you can talk with your medical professional.
Is Lamictal an alternative to lithium?
Yes, lamotrigine (Lamictal) is a possible alternative to lithium. Both lithium and Lamictal are mood stabilizers. Both drugs can be used as maintenance (long-term) treatments for bipolar disorder.
However, Lamictal may cause serious skin reactions such as Stevens-Johnson syndrome. For this reason, your medical professional may recommend that you try lithium before Lamictal.
To learn more about how lithium and Lamictal are alike and different, we suggest talking with your medical professional or pharmacist.
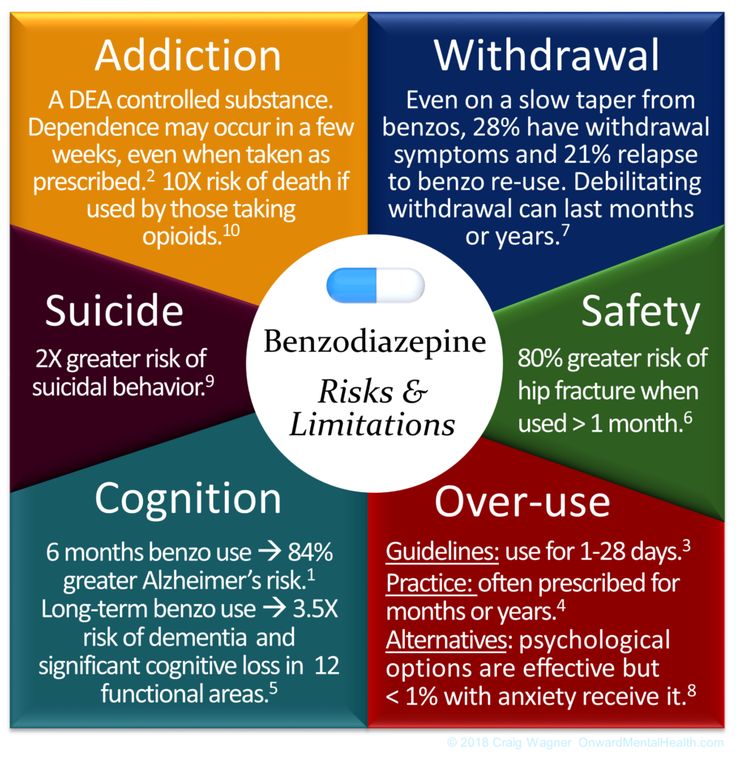
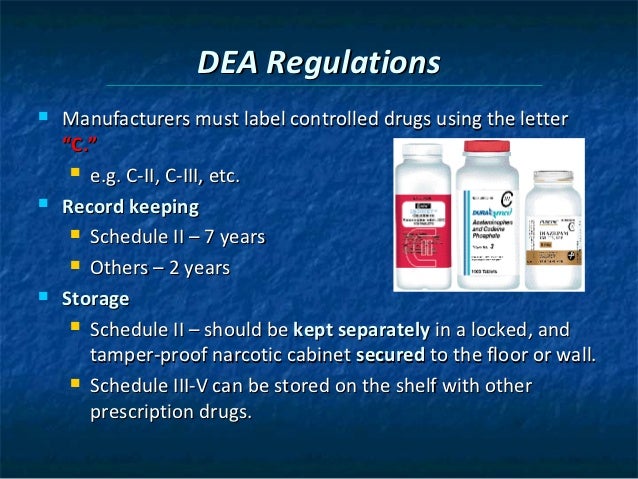
Is lithium a controlled substance?
No, lithium isn’t a controlled substance.
Controlled substances are medications that have a high potential for addiction or misuse. (Addiction refers to the continued use of a drug even if it’s causing you harm. Misuse refers to taking a drug differently than the way it was prescribed.) But lithium isn’t known to be addictive or to have a high potential for being misused.
(Addiction refers to the continued use of a drug even if it’s causing you harm. Misuse refers to taking a drug differently than the way it was prescribed.) But lithium isn’t known to be addictive or to have a high potential for being misused.
Your medical professional can provide more information if you have more questions about lithium and controlled substances.
Before taking lithium, we encourage you to talk with your medical professional. You can tell them about any medical conditions you have. You can also tell them about your overall health and other medications you’re taking.
We provide more details about these considerations below.
Interactions
Taking certain drugs, foods, vaccines, and other substances with a medication may affect how that medication works. These effects are known as interactions.
Before you take lithium, it’s important to tell your medical professional about any other drugs you take. This includes prescription and over-the-counter medication. It’s also important to mention any herbs, supplements, and vitamins you take. They or your pharmacist can tell you about possible interactions these substances may have with lithium.
It’s also important to mention any herbs, supplements, and vitamins you take. They or your pharmacist can tell you about possible interactions these substances may have with lithium.
Interactions with drugs or supplements
Lithium can interact with several types of drugs. These drugs include:
- drugs that increase the level of a chemical in your body called serotonin, such as:
- certain antidepressants, including:
- serotonin-norepinephrine reuptake inhibitors (SNRIs)
- selective serotonin reuptake inhibitors (SSRIs)
- monoamine oxidase inhibitors (MAOIs)
- certain antidepressants, including:
- certain antipsychotic drugs, such as quetiapine (Seroquel) or risperidone (Risperdal)
- nonsteroidal anti-inflammatory drugs (NSAIDs), such as:
- ibuprofen (Advil)
- aspirin
- certain blood pressure or heart failure drugs, including:
- angiotensin-converting enzyme (ACE) inhibitors, such as lisinopril (Zestril)
- angiotensin II receptor blockers (ARBs), such as valsartan (Diovan)
- calcium channel blockers, such as diltiazem (Cardizem CD, Cartia XT)
- methyldopa
- certain seizure drugs, such as:
- carbamazepine (Carbatrol, Tegretol)
- phenytoin (Dilantin)
- the asthma drug theophylline
- the antibiotic metronidazole (Flagyl)
- the dietary supplement potassium iodide
- the altitude sickness drug acetazolamide
- caffeine
- diuretic drugs
- sodium bicarbonate
It’s important to note that we haven’t listed all types of drugs that may interact with lithium.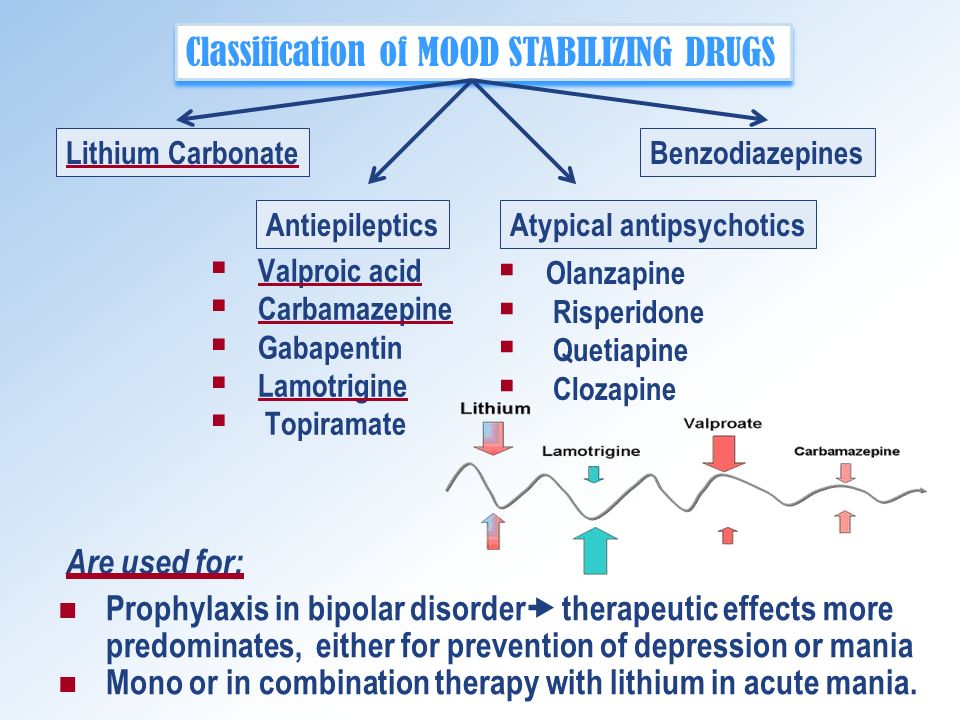 Your medical professional or pharmacist can provide more details as well as information about other possible interactions.
Your medical professional or pharmacist can provide more details as well as information about other possible interactions.
FDA boxed warning
Lithium has a boxed warning from the Food and Drug Administration (FDA) about lithium toxicity. This is a high level of lithium in your blood. The boxed warning appears on the drug’s label and alerts you to possible serious risks.
For details, you can see the “What is lithium toxicity?” section above.
Other warnings
If you have certain medical conditions or other factors that affect your health, lithium may not be the right choice for you. Before you take lithium, it’s important to discuss your health history with your medical professional. The list below includes some factors to consider.
- Heart problems. If you have heart problems, be sure to tell your medical professional before starting lithium. Lithium may reveal a condition called Brugada syndrome (a type of abnormal heart rhythm) in people who have heart problems.
 Your medical professional may check for symptoms of this condition during treatment.
Your medical professional may check for symptoms of this condition during treatment. - Kidney problems. It’s very important to tell your medical professional if you have any kidney problems before starting lithium. Kidney problems increase your risk for lithium toxicity. If you have kidney problems, your medical professional may lower your lithium dosage or prescribe a different drug for you.
- Thyroid problems. Lithium may cause thyroid problems. These can include hypothyroidism (low thyroid hormone levels) and hyperthyroidism (high thyroid hormone levels). Your risk for this side effect may be higher if you have thyroid problems before starting lithium. We suggest you tell your medical professional if you have a thyroid problem before you start lithium. They’ll likely watch your thyroid function closely while you take the drug.
- Allergic reaction. If you’ve had an allergic reaction to lithium or any of its ingredients, you should not take lithium.
 Your medical professional can recommend other treatments that might be better choices for you.
Your medical professional can recommend other treatments that might be better choices for you. - Use of antipsychotic drugs. It’s important to tell your medical professional if you’re taking any antipsychotic drugs before starting lithium. These drugs can increase your risk for nerve problems while taking lithium, such as neuroleptic malignant syndrome. If you take these drugs, your medical professional can advise whether lithium is right for treating your condition.
Lithium and alcohol
It’s recommended that you avoid drinking alcohol while taking lithium.
Drinking alcohol with lithium can raise your risk for lithium toxicity, which can cause serious side effects. If you drink alcohol, it’s important to talk with your medical professional about whether it’s safe to drink while you’re taking lithium.
Lithium treatment while pregnant or breastfeeding
It may not be safe to take lithium while pregnant or breastfeeding. Your medical professional can advise you about taking lithium during these times.
Your medical professional can advise you on how much lithium to take and how often. It’s important to follow the instructions they provide. Commonly used dosages are mentioned below, but always take the dosage your medical professional recommends.
Forms and strengths
Lithium comes in several forms that you take by mouth:
- extended-release (ER) tablets, which are long-acting
- immediate-release (IR) tablets, which are short-acting
- IR capsules
- IR liquid solution
We cover only the IR tablet, capsule, and liquid solution forms of lithium in this article. The table below shows the available strengths of each of these forms of lithium.
| Form | Strength |
| IR tablet | 300 milligrams (mg) |
| capsule | 150 mg, 300 mg, and 600 mg |
| liquid solution | 8 milliequivalents (mEq) of lithium per 5 milliliters (mL) of solution |
If you’d like to learn about lithium ER tablets, your medical professional or pharmacist can tell you more.
Dosage for bipolar I disorder
Typically, your medical professional will start by prescribing a low dosage of lithium. Then they’ll slowly increase your dosage over time until the symptoms of your condition have been reduced.
Lithium can be used in adults and children ages 7 years and older. Below are the recommended starting dosages of lithium for bipolar I disorder.
| Tablet or capsule starting dosage | Liquid solution starting dosage | |
| Adults and children who weigh 31 kilograms (kg)* (66 pounds [lbs.]) or more) | 300 mg 3 times per day | 8 mEq (5 mL) 3 times per day |
| Children who weigh 20 kg to 30 kg (44 lbs. to 65 lbs.) | 300 mg 2 times per day | 8 mEq (5 mL) 2 times per day |
If your child weighs less than 20 kg, their medical professional will recommend whether lithium is right for them, and what their dosage would be.
Your medical professional may adjust your lithium dosage depending on factors such as:
- your age
- your weight
- other medications you take
- other health conditions you have
- the level of lithium in your blood
If you have questions about the dosage that’s right for you, we recommend that you talk with your medical professional.
* One kg equals about 2.2 lb.
Normal range of lithium
To lessen your risk for side effects from lithium, your medical professional may regularly check your lithium levels with blood tests.
Your doctor will start by prescribing a low dose of lithium. Then they’ll check your lithium blood levels 3 days later. Your medical professional may increase your dosage every few days until your lithium blood level is 0.8 mEq/mL to 1.2 mEq/mL. This is considered a normal range for lithium levels.
Your medical professional may continue to check your lithium blood levels frequently until your condition is stable.
Lithium is a generic prescription drug. The costs of prescription medications may depend on several factors, such as your insurance coverage and the pharmacy you use.
If you’re wondering how to pay for lithium, we suggest that you talk with your medical professional or pharmacist. You may also want to visit Medicine Assistance Tool or NeedyMeds to see if support options are available.
It’s possible. Withdrawal symptoms weren’t reported in studies of lithium. However, some people have reported withdrawal symptoms after suddenly stopping lithium.
Withdrawal symptoms
Possible withdrawal symptoms with lithium can include:
- anxiety
- irritability
- trouble sleeping
It’s also possible that after stopping lithium, your bipolar disorder symptoms may start to come back.
It’s important that you do not stop taking lithium unless your medical professional says it’s safe to do so. They may lower your dosage slowly over time when it’s safe for you to stop lithium treatment. This can lessen your risk of side effects after stopping the drug.
This can lessen your risk of side effects after stopping the drug.
It’s important that you don’t take more lithium than your medical professional recommends. Taking more than the recommended dosage can lead to severe side effects, including lithium toxicity. This is a high level of lithium in the blood, which can cause serious side effects.
In fact, lithium has a boxed warning from the Food and Drug Administration (FDA) about lithium toxicity. The boxed warning appears on the drug’s label and alerts you to possible serious risks. For details about lithium toxicity, including its symptoms, you can see the “What is lithium toxicity?” section above.
Symptoms of overdose
Symptoms caused by an overdose can include:
- seizures
- irreversible brain damage
- coma
What to do in case you take too much lithium
If you believe you’ve taken too much lithium, call your medical professional right away. You can also call 800-222-1222 to reach the American Association of Poison Control Centers, or use its online resource.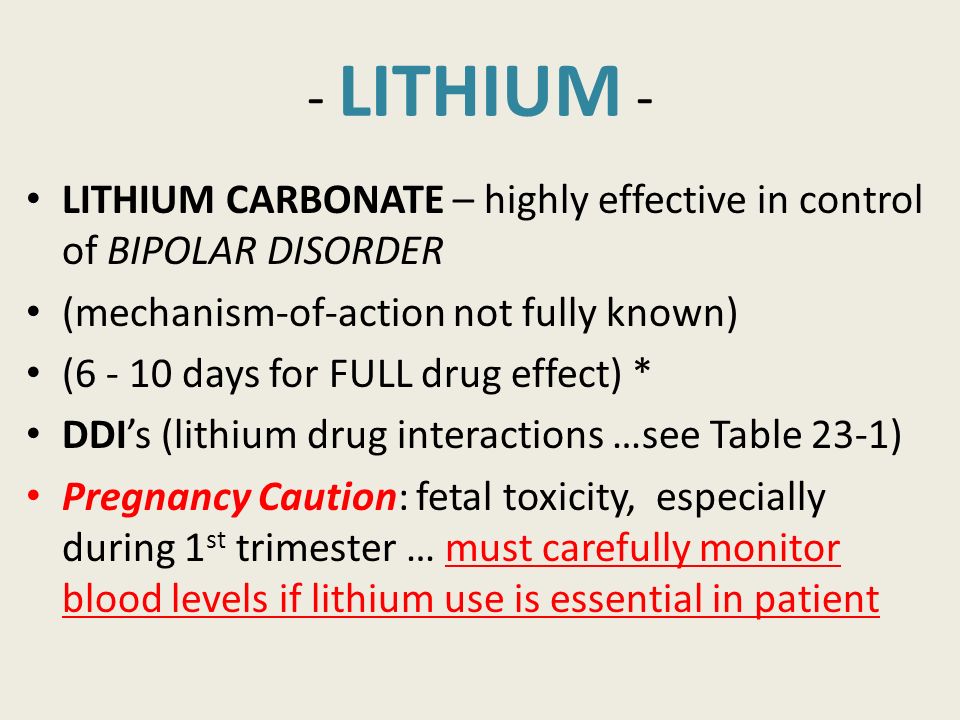 But if your symptoms are severe, immediately call 911 (or your local emergency number) or go to the closest emergency room.
But if your symptoms are severe, immediately call 911 (or your local emergency number) or go to the closest emergency room.
Your medical professional can give you instructions on how to take lithium. They can also explain how much to take and how often. It’s important to follow the instructions they provide.
Lithium comes in several forms that you take by mouth:
- extended-release (ER) tablets, which are long-acting
- immediate-release (IR) tablets, which are short-acting
- capsules
- liquid solution
We cover only the IR tablet, capsule, and liquid solution forms of lithium in this article. If you’d like to learn about lithium ER tablets, your medical professional or pharmacist can tell you more.
Tips for taking lithium
You’ll likely take lithium two to three times a day.
It’s important to avoid becoming dehydrated or overheated while taking lithium. You can stay hydrated and keep your body temperature low by drinking plenty of liquids. This is especially important while in hot weather or while exercising.
This is especially important while in hot weather or while exercising.
It’s also important to eat a consistent amount of salt while taking lithium. Changing your salt intake could affect your lithium blood levels. Lower lithium blood levels could make the drug less effective. But higher lithium blood levels could raise your risk for lithium toxicity.*
Your medical professional can help determine the right amount of liquid and salt for you while taking lithium.
* Lithium has a boxed warning from the Food and Drug Administration (FDA) about lithium toxicity. For details, you can see the “What is lithium toxicity?” section above.
When to take
It’s recommended that you take lithium doses around the same times each day. This helps keep a steady level of lithium in your system, which may help prevent withdrawal symptoms. (To learn more about withdrawal, you can see the “Can lithium cause withdrawal if you stop taking it?” section above.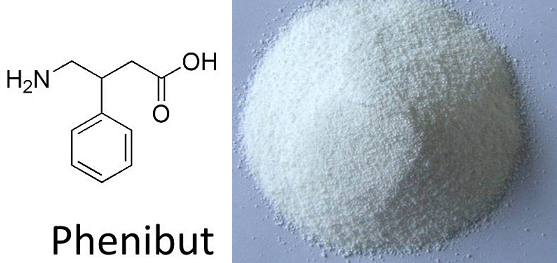 )
)
Taking lithium with food may help reduce some side effects of the drug.
Taking lithium with other drugs
Your medical professional may prescribe lithium by itself to treat your condition. But depending on the severity of your symptoms, they may prescribe lithium along with other drugs.
For example, your medical professional may prescribe lithium along with certain antipsychotics. Examples include:
- olanzapine (Zyprexa)
- quetiapine (Seroquel)
- risperidone (Risperdal)
- ziprasidone (Geodon)
Before starting lithium, it’s important to tell your medical professional about any other drugs you take. This is because certain drugs, including antipsychotics in some cases, may increase your risk for side effects from lithium. Or they may affect how lithium works.
For more information about possible interactions with lithium, you can see the “What should you know before taking lithium?” section above.
Frequently asked questions about taking lithium
Below we share answers to some questions you may have about lithium treatment.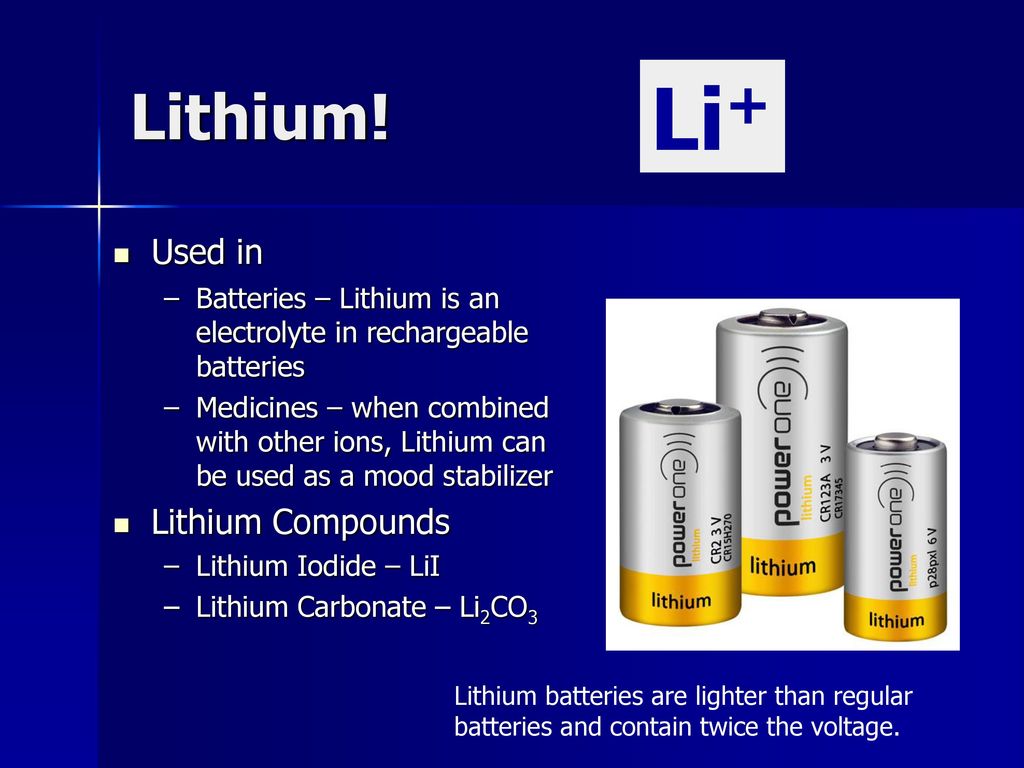
- How long does lithium take to work? You may not notice lithium starting to reduce your symptoms until you’ve taken the drug for about a week. It typically takes several weeks for your symptoms to be reduced completely. We recommend talking with your medical professional about when you can expect to notice lithium working.
- What should I do if I miss a dose of lithium? It’s recommended that you take a missed dose of lithium as soon as you remember. But if it’s almost time for your next dose, you can skip your missed dose and take your next dose at its regular time. It’s important that you do not take two doses of lithium to make up for a missed dose. An extra dose can raise your risk for side effects from the drug. If you aren’t sure whether to take a missed dose or skip it, we suggest you talk with your medical professional or pharmacist.
- Is lithium meant for long-term use? Your medical professional may prescribe lithium for short-term or long-term use.
 If the drug is working for you and isn’t causing bothersome effects, you may take lithium long term.
If the drug is working for you and isn’t causing bothersome effects, you may take lithium long term. - Can you chew, split, or crush lithium? The manufacturer of lithium hasn’t stated if the drug can be chewed, split, or crushed. You should not chew split or crush lithium tablets or capsules without first talking with your medical professional or pharmacist. They can help you if you’re not able to swallow the tablets or capsules whole.
- Should you take lithium with food? You can take lithium with food or without it. But taking lithium with food can help reduce certain side effects of the drug, such as nausea.
What should you ask your medical professional?It’s common to have questions about your treatment plan for lithium. Your medical professional is there to work with you and help address any concerns you have.
To help guide your discussion, here are some suggestions:
- You can write down questions you have before your visit.
For example, “How will taking lithium affect my mood, body, and lifestyle?”
- You can think about asking a loved one or friend to come with you to your appointment. Having in-person support may help you feel more at ease.
- You can ask your medical professional to explain something that you find unclear.
Working with your healthcare team may help you stay on track with your treatment. If you find that you’re not getting answers to your questions or receiving the care you deserve, consider seeking a second opinion.
If you still have questions about lithium after reading this article, talking with your medical professional may be helpful. Together you can decide if lithium might be a good choice for you.
You can also discuss other treatments, forms of support, and resources that may benefit you. We’ve listed some suggestions below.
Additional treatment options
While you take lithium, additional treatments or remedies may help you better manage your condition. These can include:
These can include:
- having a daily routine
- joining a support group
- keeping a mood journal
- participating in psychotherapy
Finding support
Whether you’re looking for a therapist, support group, or information about how to afford therapy, these resources may help:
- how to find a therapist
- online counseling search through BetterHelp
- online support groups
- how to afford therapy
Other resources
To receive weekly information about mental health, you may want to sign up for the Psych Central newsletter. You’ll find stories directly from other people about their mental health journey as well as the latest information about treatments.
Q:
I’ve heard that lithium can cause thyroid problems. Will I need to take medications for my thyroid while taking lithium?
Anonymous
A:
Lithium can cause thyroid problems in some people.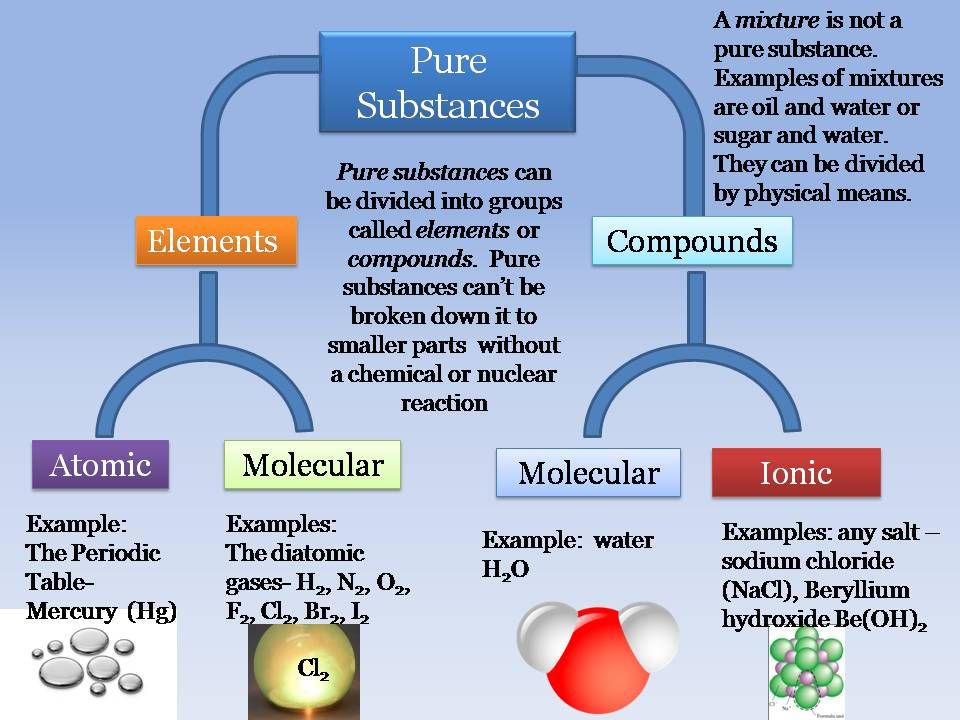 Your doctor will monitor your thyroid function while you’re taking lithium. If your thyroid isn’t functioning properly, you may be prescribed medication to help with this, such as levothyroxine (Synthroid). Your doctor will determine whether you need to take thyroid medication during your lithium treatment.
Your doctor will monitor your thyroid function while you’re taking lithium. If your thyroid isn’t functioning properly, you may be prescribed medication to help with this, such as levothyroxine (Synthroid). Your doctor will determine whether you need to take thyroid medication during your lithium treatment.
Neal Patel, PharmDAnswers represent the opinions of our medical experts. All content is strictly informational and should not be considered medical advice.
Disclaimer: Psych Central has made every effort to make certain that all information is factually correct, comprehensive, and up to date. However, this article should not be used as a substitute for the knowledge and expertise of a licensed healthcare professional. You should always consult your doctor or another healthcare professional before taking any medication. The drug information contained herein is subject to change and is not intended to cover all possible uses, directions, precautions, warnings, drug interactions, allergic reactions, or adverse effects.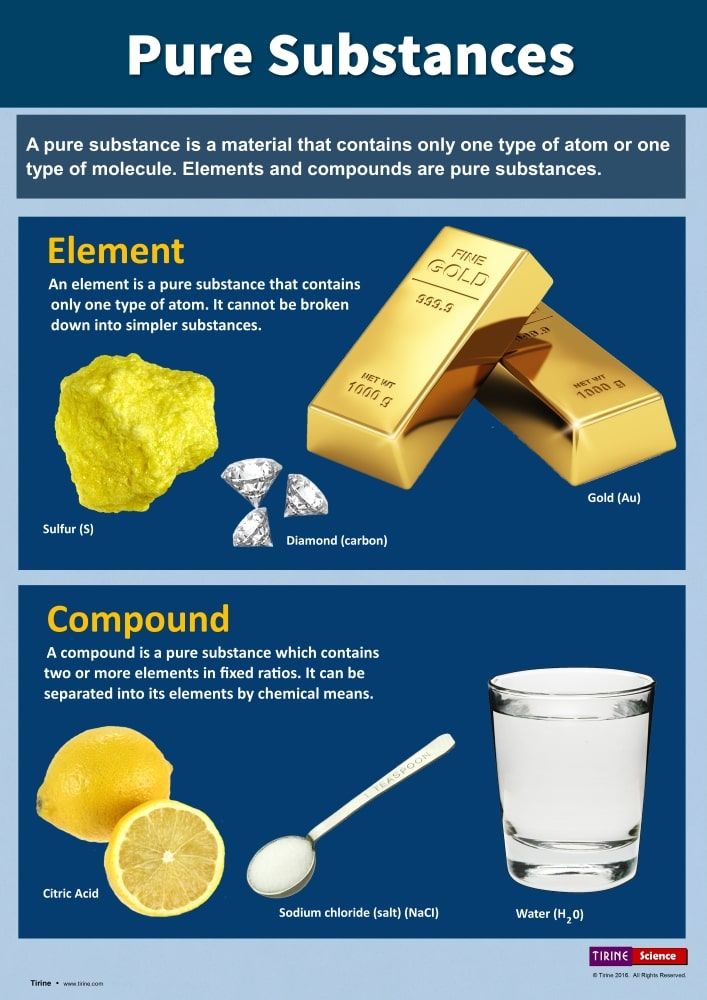 The absence of warnings or other information for a given drug does not indicate that the drug or drug combination is safe, effective, or appropriate for all patients or all specific uses.
The absence of warnings or other information for a given drug does not indicate that the drug or drug combination is safe, effective, or appropriate for all patients or all specific uses.
Lithium - StatPearls - NCBI Bookshelf
Krutika Chokhawala; Sarah Lee; Abdolreza Saadabadi.
Author Information
Last Update: July 11, 2022.
Continuing Education Activity
Despite the availability of newer mood stabilizers, lithium continues to be a first-line treatment for bipolar disorder. It is often underutilized because of the potential for side effects, and perhaps because it is an older drug. This activity outlines the indications and contraindications for lithium use, provides instructions for administration and monitoring, and reviews lithium toxicity. This activity highlights the role of the interprofessional team in caring for patients who are undergoing, or who may undergo lithium therapy.
Objectives:
Identify the indications for lithium therapy.

Describe the potential adverse effects of lithium therapy.
Explain the need for monitoring lithium levels.
Review the importance of a well-coordinated interprofessional team in caring for patients undergoing lithium therapy.
Access free multiple choice questions on this topic.
Indications
Lithium was the first mood stabilizer and is still the first-line treatment option, but is underutilized because it is an older drug. Lithium is a commonly prescribed drug for a manic episode in bipolar disorder as well as maintenance therapy of bipolar disorder in a patient with a history of a manic episode. The primary target symptoms of lithium are mania and unstable mood.[1]
Lithium is also prescribed for major depressive disorder as an adjunct therapy, bipolar disorder without a history of mania, treatment of vascular headaches, and neutropenia. These are off-label uses, meaning they are not FDA-approved. Patients with rapid cycling and mixed state types of bipolar disorder generally do less well on lithium.
Patients with rapid cycling and mixed state types of bipolar disorder generally do less well on lithium.
Mechanism of Action
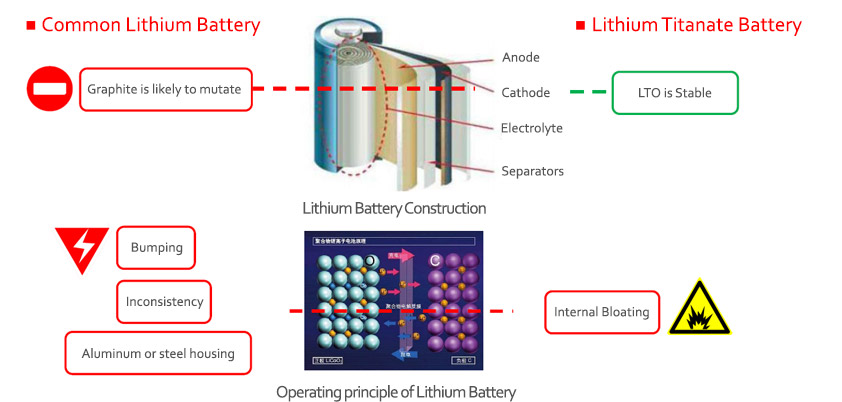
The mechanism of action of lithium is not known. It is rapidly absorbed, has a small volume of distribution, and is excreted in the urine unchanged (there is no metabolism of lithium).
Lithium modifies sodium transport in nerve and muscle cells. It alters the metabolism of neurotransmitters, specifically catecholamines and serotonin.[2] It may alter intracellular signaling via second messenger systems by inhibition of inositol monophosphate. This inhibition, in turn, affects neurotransmission through the phosphatidylinositol secondary messenger system. Lithium also decreases protein kinase C activity, which alters genomic expression associated with neurotransmission. Lithium appears to increase cytoprotective proteins and possibly activates neurogenesis and increases gray matter volume.[3]
The half-life of lithium is 18 to 30 hours. It has lower absorption on an empty stomach.
Administration
Lithium is administered orally in pill form, capsule, or liquid. The tablet is available in a controlled release 450 mg tablet or a slow-release formulation in a 300 mg tablet. Capsules are available in 150 mg, 300 mg, and 600 mg strength. The liquid formulation is available as 8 mEq/5 mL strength. The dosage usually starts at 300 mg twice or three times a day.[4]
It takes about 1 to 3 weeks for lithium to show the effects and remission of symptoms. Many patients show only a partial reduction of symptoms, and some may be nonresponders. In cases where the patient does not display an adequate response, consider monitoring plasma levels, and titrating the dose. A single nighttime dose may be a consideration to minimize side effects in stabilized patients. Lower doses and lower serum levels of lithium are preferable in elderly patients. If patients do not show an adequate response, the clinician should consider augmentation. The preferred agents are valproate, lamotrigine, and atypical antipsychotics like risperidone, olanzapine, quetiapine, ziprasidone, and aripiprazole.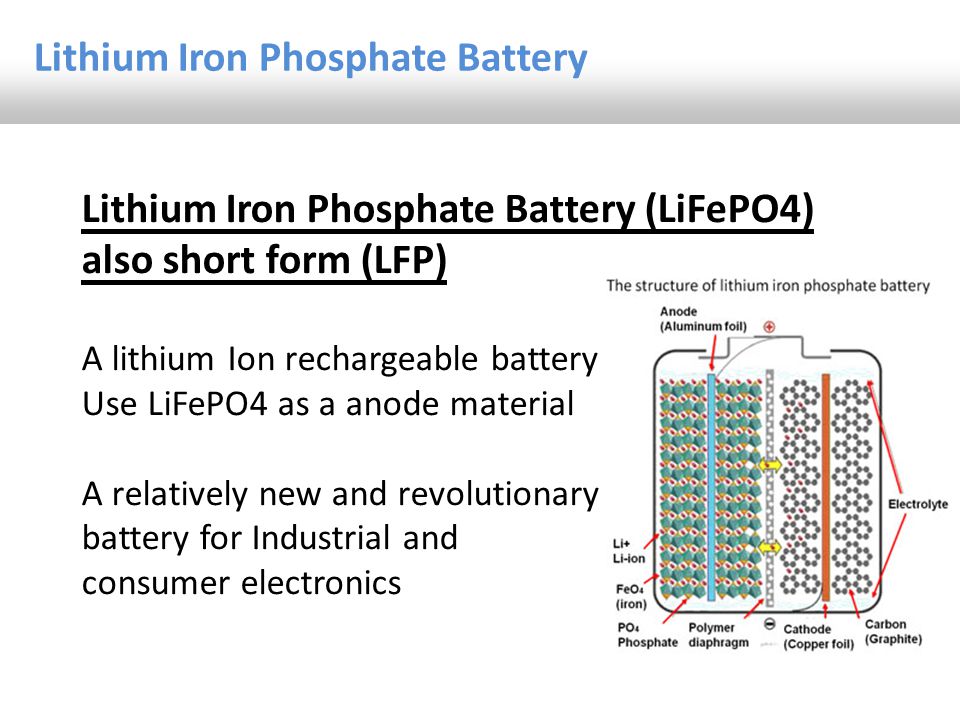
Lithium should be tapered gradually over three months. Rapid discontinuation increases the risk of relapse. Certain medications increase serum lithium levels, including diuretics (especially thiazides), non-steroidal anti-inflammatory drugs like ibuprofen and COX-2 inhibitors, and angiotensin-converting enzyme inhibitors. Metronidazole raises lithium levels by decreasing its renal clearance. Carbamazepine, phenytoin, and methyldopa may increase the toxicity of lithium.
Adverse Effects
Lithium can cause several adverse effects. Typically the side effects are dose-related. Notable side effects include:
Cardiac: Bradycardia, flattened or inverted T waves, heart block, and sick sinus syndrome.
CNS: Confusion, memory problems, new or worsening tremor, hyperreflexia, clonus, slurred speech, ataxia, stupor, delirium, coma, and seizures (rarely). These effects are theoretically due to excess action on the same sites that mediate therapeutic action.
 [5]
[5] Renal: Nephrogenic diabetes insipidus with polyuria and polydipsia. These side effects are due to lithium's action on ion transport.[6]
Hematologic: Leukocytosis and aplastic anemia
Gastroenterologic: Diarrhea and nausea
Endocrinal: Euthyroid goiter or hypothyroid goiter
Other: Acne, rash, and weight gain. Lithium-induced weight gain is more common in women than in men.
Some patients on haloperidol and lithium may develop an encephalopathic syndrome similar to neuroleptic malignant syndrome.
Contraindications
Lithium is not recommended in patients with renal impairment. It is also not recommended in patients with cardiovascular disease. Lithium causes reversible T wave changes and can unmask Brugada syndrome. A cardiology consult is necessary if a patient experiences unexplained palpitations and syncope. It is also not advisable to consider lithium for treatment in children under 12 years of age.
Lithium is not considered for treatment during pregnancy due to a 2 to 3 fold increase of significant congenital disabilities. Ebstein's anomaly is a cardiac defect in infants associated with lithium treatment during pregnancy. It is crucial to weigh the risks versus benefits of continuing a pregnant patient on lithium.[7] If a patient remains on lithium, monitoring should be done every four weeks until 36 weeks, and then every week after that. If a mother receives lithium during delivery, it is essential to monitor the infant for hypotonia and floppy baby syndrome for at least 48 hours. Breastfeeding is not advisable; if a lactating mother is on lithium therapy, breast milk will contain lithium.
Monitoring
Before starting treatment with lithium, it is essential to get kidney function tests and thyroid function tests. In patients above 50 years of age, an electrocardiogram is also necessary. Repeat these tests once or twice a year in patients on lithium therapy. Because lithium is associated with weight gain, it is important to weigh a patient before starting treatment. It is also beneficial to determine if the patient has prediabetes, diabetes, or dyslipidemia.
It is also beneficial to determine if the patient has prediabetes, diabetes, or dyslipidemia.
Monitoring of therapeutic levels includes trough plasma levels drawn 8 to 12 hours after the last dose. The therapeutic range is 1.0 to 1.5 mEq/L for acute treatment and 0.6 to 1.2 mEq/L for chronic therapy. Monitoring should be done every 1 to 2 weeks until reaching the desired therapeutic levels. Then, check lithium levels every 2 to 3 months for six months. It is also important to monitor patients for dehydration and lower the dose when there are signs of infection, excessive sweating, or diarrhea. Toxic levels are when the drug level is more than 2 mEq/L.
Toxicity
Lithium has a very narrow therapeutic index, and toxic levels are when the drug is above 2 mEq/L, which is very close to its therapeutic range. Lithium toxicity can cause interstitial nephritis, arrhythmia, sick sinus syndrome, hypotension, T wave abnormalities, and bradycardia. Rarely, toxicity can cause pseudotumor cerebri and seizures.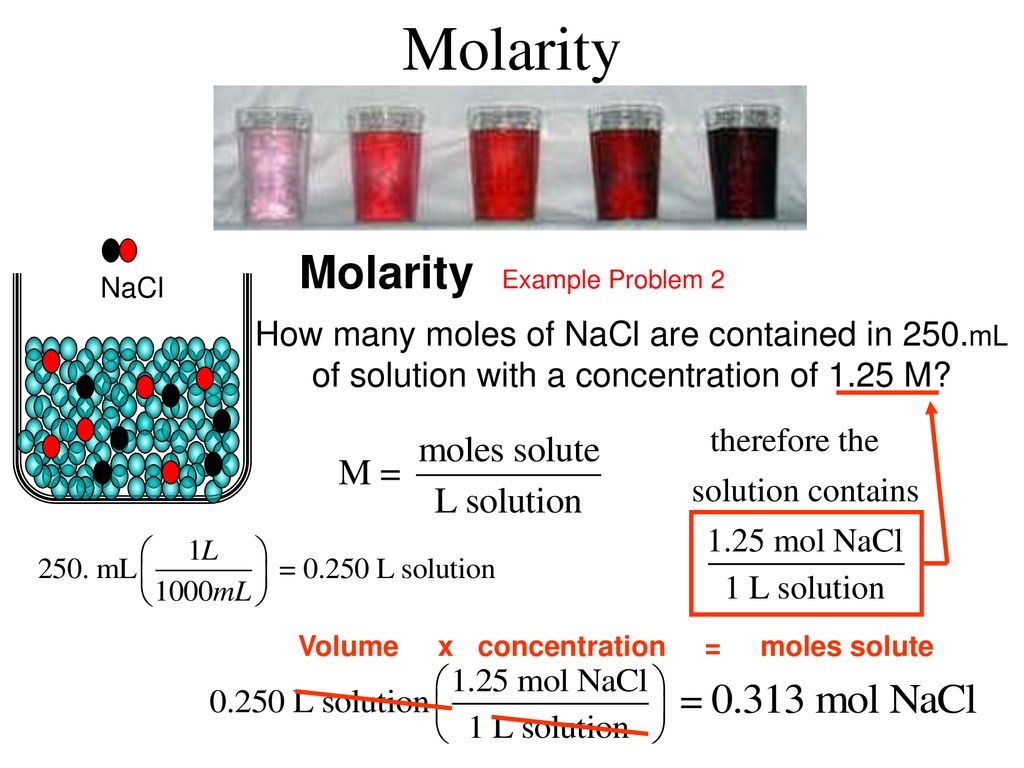 Lithium toxicity has no antidote. Treatment for lithium toxicity is primarily hydration and to stop the drug. Give hydration with normal saline, which will also enhance lithium excretion. Avoid all diuretics. If the patient has severe renal dysfunction or failure, or severely altered mental status, then start with hemodialysis. 20 to 30 mg of propranolol given 2 to 3 times per day may help reduce tremors.
Lithium toxicity has no antidote. Treatment for lithium toxicity is primarily hydration and to stop the drug. Give hydration with normal saline, which will also enhance lithium excretion. Avoid all diuretics. If the patient has severe renal dysfunction or failure, or severely altered mental status, then start with hemodialysis. 20 to 30 mg of propranolol given 2 to 3 times per day may help reduce tremors.
Enhancing Healthcare Team Outcomes
The psychiatrist generally prescribes lithium, but the drug levels are often monitored by the primary care provider, mental health nurse, pharmacist, and the internist, functioning as an interprofessional team. Lithium continues to be a first-line treatment option for mood stabilization. When prescribed, the pharmacist should carefully inspect the dosing and perform medication reconciliation, so avoid any issues with dosing and subsequent serum levels. Mental health nurses should be alert to the signs and symptoms of lithium toxicity and report such to the prescriber immediately if these are present.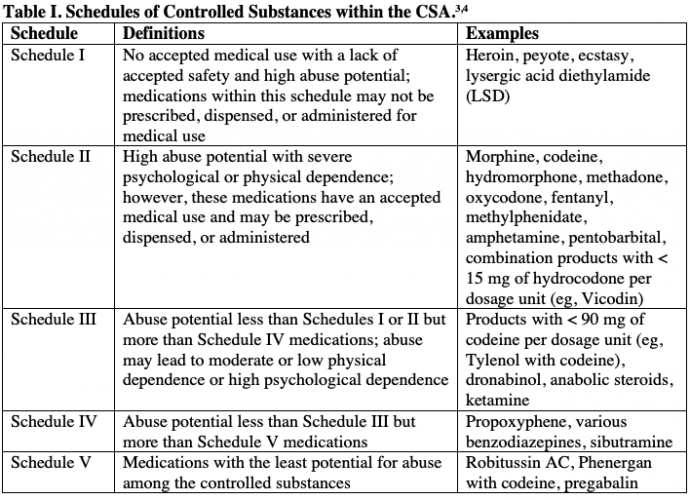 It is essential to maintain coordination of care in patients on /lithium therapy owing to its narrow therapeutic index and potential adverse effects and toxicity.[8]
It is essential to maintain coordination of care in patients on /lithium therapy owing to its narrow therapeutic index and potential adverse effects and toxicity.[8]
Every patient on lithium needs close monitoring; if the patient is unlikely to comply with followup, clinicians should not prescribe them the drug; this is where the interprofessional team paradigm is most effective. [Level 5]
Review Questions
Access free multiple choice questions on this topic.
Comment on this article.
References
- 1.
Hayes JF, Pitman A, Marston L, Walters K, Geddes JR, King M, Osborn DP. Self-harm, Unintentional Injury, and Suicide in Bipolar Disorder During Maintenance Mood Stabilizer Treatment: A UK Population-Based Electronic Health Records Study. JAMA Psychiatry. 2016 Jun 01;73(6):630-7. [PubMed: 27167638]
- 2.
Perveen T, Haider S, Mumtaz W, Razi F, Tabassum S, Haleem DJ. Attenuation of stress-induced behavioral deficits by lithium administration via serotonin metabolism.
 Pharmacol Rep. 2013;65(2):336-42. [PubMed: 23744417]
Pharmacol Rep. 2013;65(2):336-42. [PubMed: 23744417]- 3.
Sheng R, Zhang LS, Han R, Gao B, Liu XQ, Qin ZH. Combined prostaglandin E1 and lithium exert potent neuroprotection in a rat model of cerebral ischemia. Acta Pharmacol Sin. 2011 Mar;32(3):303-10. [PMC free article: PMC4002767] [PubMed: 21258357]
- 4.
Sajatovic M. Treatment of bipolar disorder in older adults. Int J Geriatr Psychiatry. 2002 Sep;17(9):865-73. [PubMed: 12221662]
- 5.
Rybakowski JK. Effect of Lithium on Neurocognitive Functioning. Curr Alzheimer Res. 2016;13(8):887-93. [PubMed: 27087441]
- 6.
Tabibzadeh N, Vrtovsnik F, Serrano F, Vidal-Petiot E, Flamant M. [Chronic metabolic and renal disorders related to lithium salts treatment]. Rev Med Interne. 2019 Sep;40(9):599-608. [PubMed: 30827493]
- 7.
Poels EMP, Bijma HH, Galbally M, Bergink V. Lithium during pregnancy and after delivery: a review. Int J Bipolar Disord.
 2018 Dec 02;6(1):26. [PMC free article: PMC6274637] [PubMed: 30506447]
2018 Dec 02;6(1):26. [PMC free article: PMC6274637] [PubMed: 30506447]- 8.
Cipriani A, Hawton K, Stockton S, Geddes JR. Lithium in the prevention of suicide in mood disorders: updated systematic review and meta-analysis. BMJ. 2013 Jun 27;346:f3646. [PubMed: 23814104]
How we are treated: Normotim - Indicator
What is bipolar affective disorder, why is it so difficult to diagnose mania and hypomania, why taking lithium salts requires constant blood tests and what is the main difference between dietary supplements and a drug with a similar composition, read in the new issue of the column "How we are being treated" on Indicator.Ru.
Lithium enters the bipolar disorder - and the doctor tells them ... This could be the beginning of a joke about a new drug with salts of this metal, which is offered in pharmacies as a Russian alternative to drugs for bipolar affective disorder. Only psychiatrists are not laughing. Let's figure out what's the matter.
Two sides of the same coin
Lithium salt preparations may be prescribed for bipolar affective disorder (BAD), episodes of mania and hypomania, and less often for major depressive disorder (although this indication is not approved by the Food and Drug Administration and medicines in the United States, it has been prescribed worldwide since the 1980s and confirmed by clinical studies). What is a BAR, against which preparations with lithium salts turned out to be the first line of defense? Bipolar disorder is called because the patient often has two "poles" of behavior: the depressive stage and the manic stage.
Everyone has heard about depression, and many are sure that they have experienced it more than once, even if we are talking about a short mood swing - no longer than a week or two. In reality, depression manifests itself not just as an attack of sadness and depression, but is also accompanied by apathy, loss of interest in all matters and pleasures, and lasts at least a month.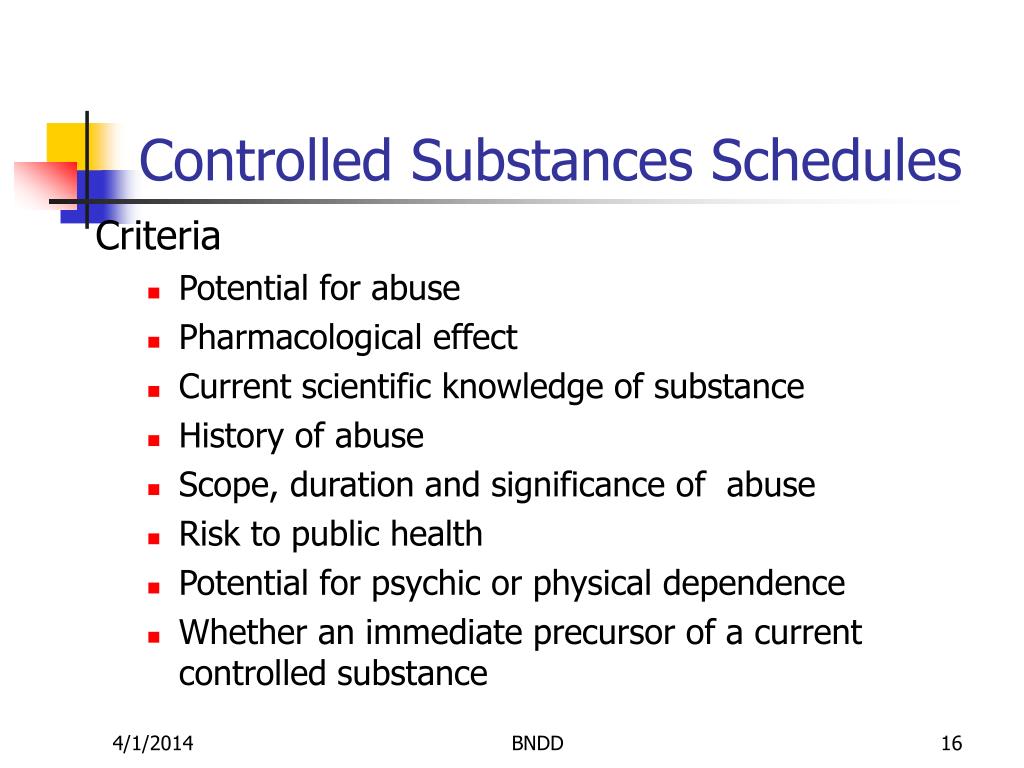 With mania, the situation is even more fun - both literally and figuratively. Almost everyone, having heard this word, imagines a maniac or a patient from anecdotes who imagines himself to be Napoleon (the notorious megalomania). In reality, psychiatrists understand this term as an enthusiastic, excited state, constant euphoria and a very high spirits for no reason. The thoughts of a person in the stage of mania randomly race with emotions, he gushes with ideas and can work to the limit, be unexpectedly assertive, unpredictable and irritable, often distracted. A similar mood can also occur in a healthy person, but the fuse will last only a few days. People with mania can stay in this state for months.
With mania, the situation is even more fun - both literally and figuratively. Almost everyone, having heard this word, imagines a maniac or a patient from anecdotes who imagines himself to be Napoleon (the notorious megalomania). In reality, psychiatrists understand this term as an enthusiastic, excited state, constant euphoria and a very high spirits for no reason. The thoughts of a person in the stage of mania randomly race with emotions, he gushes with ideas and can work to the limit, be unexpectedly assertive, unpredictable and irritable, often distracted. A similar mood can also occur in a healthy person, but the fuse will last only a few days. People with mania can stay in this state for months.
The manic patient feels joyful, active and productive, his self-esteem may be inflated if he does not reach exhaustion or suffer from impulsive actions. A weaker version of this condition is called hypomania, and a person may perceive it as the norm, complaining only of periodic depression, and others may confuse it with an active extrovert.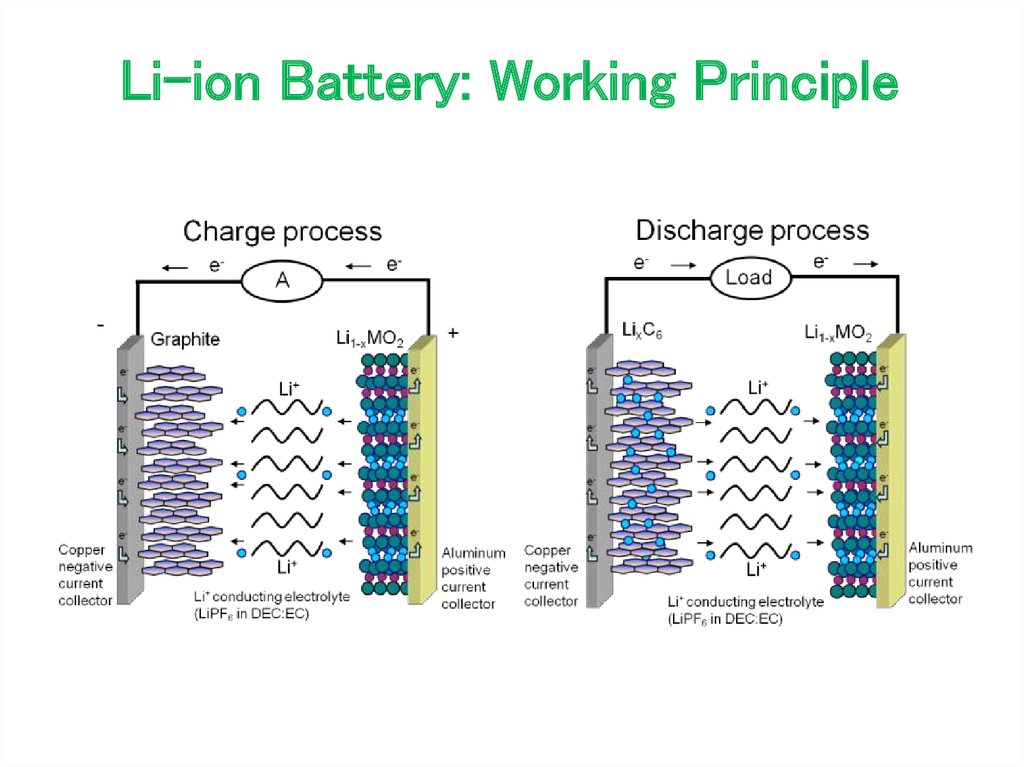 It is not surprising that even a psychiatrist finds it difficult to diagnose BAD immediately and distinguish it from unipolar depression (that is, without another “pole”), because not every patient analyzes and remembers his mood in sequence and in different months of life. And even more so, it never occurs to anyone to complain if the mood is upbeat and inspired. In the first type of BAD, depressive episodes (which are usually three times longer) alternate with manic episodes, in the second, periods of rise look like hypomania, but there are other varieties. One of the saddest can be called a mixed type, when increased energy is pricked by a depressed mood. Unless there is no mania without depression in BAD: perhaps the body cannot withstand constant life “on the rise” and lack of sleep.
It is not surprising that even a psychiatrist finds it difficult to diagnose BAD immediately and distinguish it from unipolar depression (that is, without another “pole”), because not every patient analyzes and remembers his mood in sequence and in different months of life. And even more so, it never occurs to anyone to complain if the mood is upbeat and inspired. In the first type of BAD, depressive episodes (which are usually three times longer) alternate with manic episodes, in the second, periods of rise look like hypomania, but there are other varieties. One of the saddest can be called a mixed type, when increased energy is pricked by a depressed mood. Unless there is no mania without depression in BAD: perhaps the body cannot withstand constant life “on the rise” and lack of sleep.
You can learn how to understand medicines on your own in the author's online course "How we are treated" by the editor of Indicator.Ru Ekaterina Mishchenko: https://clck.ru/Pnmtk
Lithium has become one of the oldest drug components in the field of symptom control BAR. The use of salts of this metal against the symptoms of mental disorders began in the late 1940s in Australia (and even earlier they tried to treat gout, cancer and epilepsy, but did not succeed very much). All these years, he confidently holds positions, not leaving the list of drugs recommended by the World Health Organization as the most effective, safe and cost-effective for use. In the acute stage of mania, according to clinical studies, lithium may be inferior to drugs from the antipsychotic group in terms of tolerability and effectiveness. But in recommendations for bipolar disorder, he is even ahead of antidepressants, because the latter can provoke the transformation of depression into mania or a rapid change in episodes of both stages.
The use of salts of this metal against the symptoms of mental disorders began in the late 1940s in Australia (and even earlier they tried to treat gout, cancer and epilepsy, but did not succeed very much). All these years, he confidently holds positions, not leaving the list of drugs recommended by the World Health Organization as the most effective, safe and cost-effective for use. In the acute stage of mania, according to clinical studies, lithium may be inferior to drugs from the antipsychotic group in terms of tolerability and effectiveness. But in recommendations for bipolar disorder, he is even ahead of antidepressants, because the latter can provoke the transformation of depression into mania or a rapid change in episodes of both stages.
What, what
What are lithium-based drugs and how do they work? Lithium is an alkali metal, which means that it tends to chemical reactions very strongly (as a reducing agent). If a piece of iron can be put on the table and left, then metallic lithium is even stored in kerosene, otherwise it is immediately covered with a film of oxide and carbonate. Upon contact with wet skin and mucous membranes, it leaves chemical burns, as it begins to turn into alkali, taking oxygen and hydrogen from the water (the remaining hydrogen is released). Few people would think of swallowing such a medicine. Not surprisingly, lithium is used in the form of salts in medicine. Most often (and in Russia - without options) it is lithium carbonate - Li 2 CO 3 .
Upon contact with wet skin and mucous membranes, it leaves chemical burns, as it begins to turn into alkali, taking oxygen and hydrogen from the water (the remaining hydrogen is released). Few people would think of swallowing such a medicine. Not surprisingly, lithium is used in the form of salts in medicine. Most often (and in Russia - without options) it is lithium carbonate - Li 2 CO 3 .
But recently an alternative has appeared, which (to the indignation of psychiatrists) has begun to be offered in pharmacies instead of the traditional Sedalit. This drug is Normotim (the name directly refers to the drug group of mood stabilizers, or mood stabilizers), which, in addition to lithium in the form of ascorbate (salt of ascorbic acid, that is, in combination with vitamin C), also contains vitamins B1 and B2. Indeed, the lack of these vitamins can cause neurological disorders (for example, Wernicke-Korsakoff syndrome). However, vitamins must be distinguished from medicines: if they “cure” something, then only their own lack.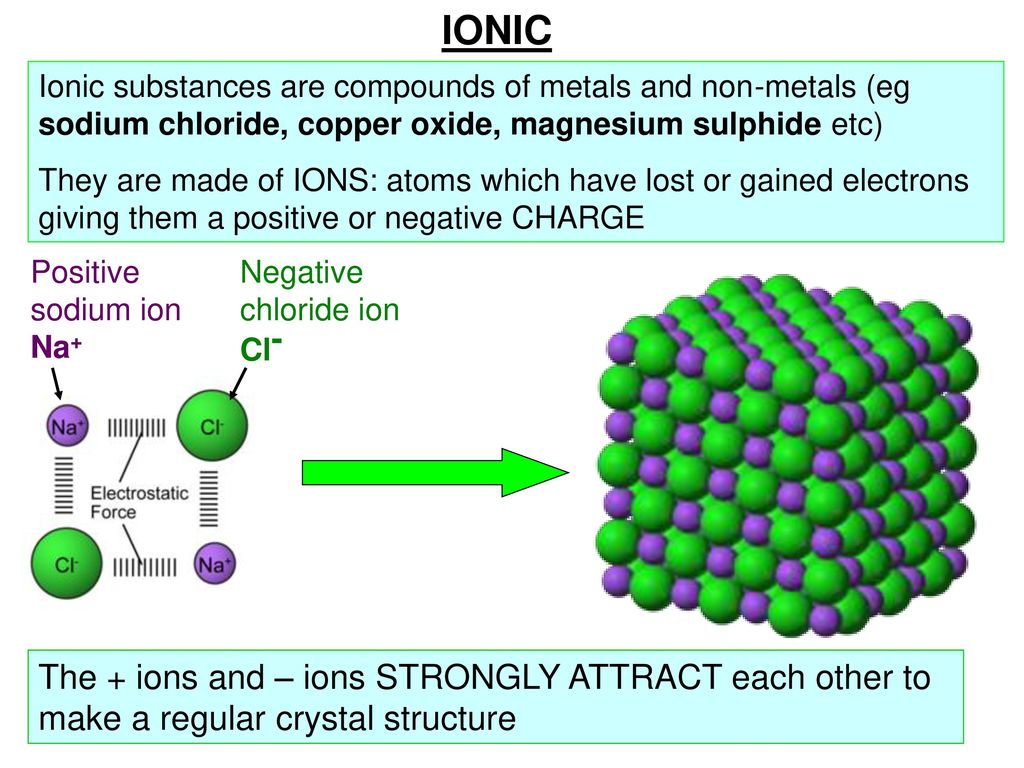 On the other hand, the preparation contains approximately the daily norm of both vitamins for an adult male (1, 2), which is too little for a serious overdose, so they cannot harm.
On the other hand, the preparation contains approximately the daily norm of both vitamins for an adult male (1, 2), which is too little for a serious overdose, so they cannot harm.
Lithium salts can still be toxic to humans. Side effects include reduced thyroid hormone production (hypothyroidism, which, somewhat paradoxically, increases the likelihood of depression), diabetes insipidus (increased thirst and increased urine output due to impaired thirst control in the hypothalamus, subsequent kidney failure), poisoning . And this is not counting the frequent (more than 10% of patients), but less dangerous cases, when patients develop muscle weakness, dry mouth, nausea, their hands tremble and ECG values change. Acne appears a little less often, hair deteriorates.
But that's not all. Toxic amounts of lithium are close to the dosages prescribed to patients. Therefore, when prescribing such drugs, each doctor is obliged to individually select the dosage, monitoring the safe content of lithium salts in the blood. In blood plasma, the threshold of safe concentrations for adults is 1.2 mmol / l, and for children - 0.5-1 mmol / l.
In blood plasma, the threshold of safe concentrations for adults is 1.2 mmol / l, and for children - 0.5-1 mmol / l.
Lithium at work
Since lithium salts have been used in the treatment of mental disorders since the middle of the last century, their effect on people has been well studied. The mechanism of action of lithium is not well understood. He probably replaces sodium, his "neighbor" in the column in the periodic table of chemical elements. In healthy people, it does not cause euphoria, unlike many other drugs in psychiatry, the sale of which often has to be severely limited. Lithium increases the production of serotonin, which is mistakenly called the “hormone of happiness” (but for all the variety of its roles with depression, it can really be associated). It can also interfere with other signaling agents (such as nitric oxide NO) and activate a pathway called mTOR. But how this affects the mood is not known for certain.
On the other hand, this did not prevent physicians from conducting many clinical trials of drugs with lithium salts and learning about its effectiveness in various areas. So, in acute mania (according to the Cochrane Collaboration review, which reviewed studies involving a total of more than four thousand patients), lithium was more effective than placebo and topiramate (drugs for epilepsy) and, most likely, was in no way inferior to other mood stabilizers and drugs from the antipsychotic group ( except olanzapine and risperidone, but this is not certain).
So, in acute mania (according to the Cochrane Collaboration review, which reviewed studies involving a total of more than four thousand patients), lithium was more effective than placebo and topiramate (drugs for epilepsy) and, most likely, was in no way inferior to other mood stabilizers and drugs from the antipsychotic group ( except olanzapine and risperidone, but this is not certain).
The Cochrane Library is a database of the Cochrane Collaboration, an international non-profit organization involved in the development of World Health Organization guidelines. The name of the organization comes from the name of its founder, the 20th-century Scottish medical scientist Archibald Cochrane, who championed the need for evidence-based medicine and the conduct of competent clinical trials and wrote the book Efficiency and Efficiency: Random Reflections on Public Health. Medical scientists and pharmacists consider the Cochrane Database one of the most authoritative sources of such information: the publications included in it have been selected according to the standards of evidence-based medicine and report the results of randomized, double-blind, placebo-controlled clinical trials.
Indicator.Ru
Help
In general, lithium is recognized as an effective and safe remedy for long-term use against bipolar disorder (although there is clearly less data on the unipolar variant of the disorder). It was also not entirely clear to the reviewers (published in 2001) how well it helps prevent suicide and whether it is better than antidepressants. Another review attempted to answer the question about antidepressants (for unipolar disorder), but could only conclude that both groups of drugs are effective, but there were too few qualitative comparisons.
Against schizoaffective disorders, lithium can also help, but the evidence for this is 22 clinical trials with a high risk of biased interpretation, so no hasty conclusions should be drawn.
The lists (not) appeared
And now about lithium ascorbate. There is no drug Normotim in the state register of approved clinical trials. What's the matter? And the fact is that this is not a medicine, but a dietary supplement.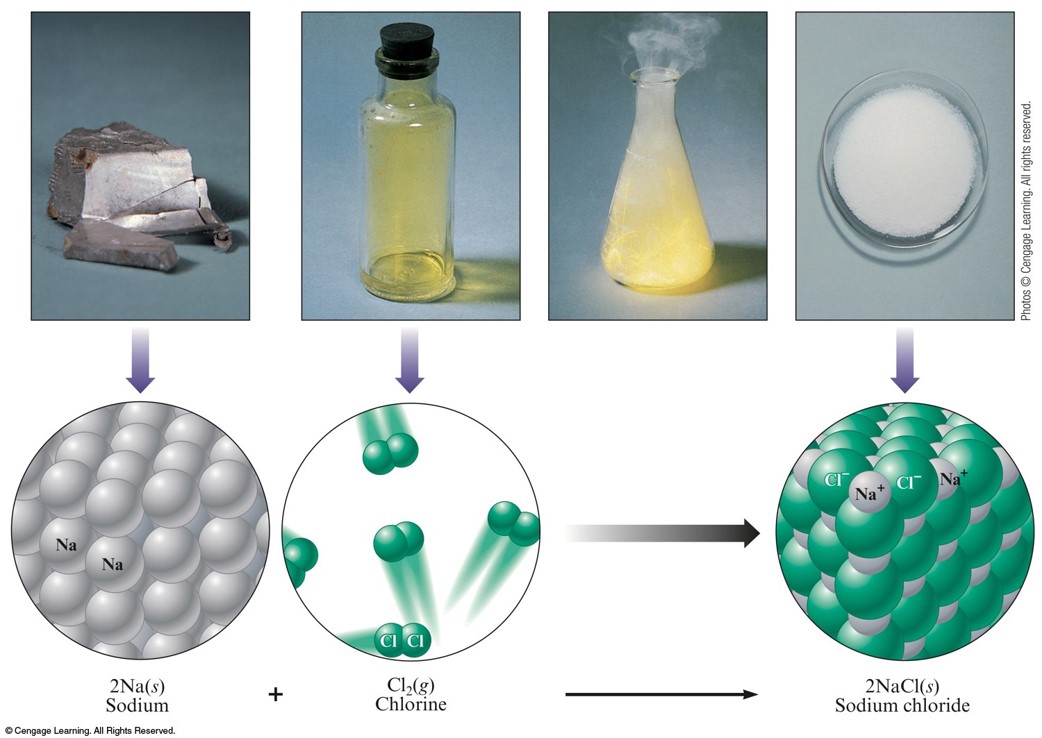 Moreover, it was registered recently, because it cannot be found in the database of the Federal Service for Supervision of Consumer Rights Protection and Human Welfare, which has not been updated for a year.
Moreover, it was registered recently, because it cannot be found in the database of the Federal Service for Supervision of Consumer Rights Protection and Human Welfare, which has not been updated for a year.
Double-blind, randomized, placebo-controlled method is a method of clinical drug research in which the subjects are not privy to important details of the study being conducted. “Double-blind” means that neither the subjects nor the experimenters know who is being treated with what, “randomized” means that the distribution into groups is random, and placebo is used to show that the effect of the drug is not based on autosuggestion and that this medicine helps better than a tablet without active substance. This method prevents subjective distortion of the results. Sometimes the control group is given another drug with already proven efficacy, rather than a placebo, to show that the drug not only treats better than nothing, but also outperforms analogues.
Indicator.Ru
Help
One Normotim tablet contains 6.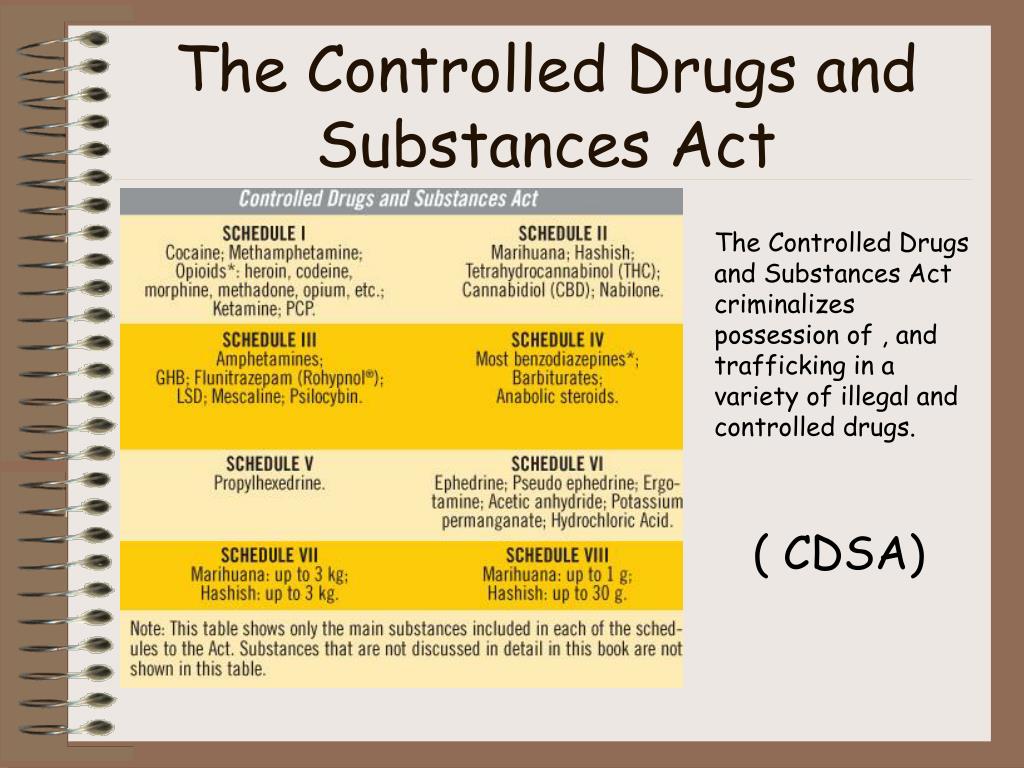 36 mg of lithium ascorbate. Analogue tablets - a popular drug with lithium carbonate - contain 300 mg of the active substance, which is almost 47 times more. Even if you start recalculating the content of lithium separately, without the carbonate or ascorbate part, this ratio does not change in favor of Normotim: lithium alone in a dose of Sedalite will be about 56 mg. It is not surprising that on the site at the very bottom we will see a warning: "is not a drug." And if it is not, then what is the demand from it?
36 mg of lithium ascorbate. Analogue tablets - a popular drug with lithium carbonate - contain 300 mg of the active substance, which is almost 47 times more. Even if you start recalculating the content of lithium separately, without the carbonate or ascorbate part, this ratio does not change in favor of Normotim: lithium alone in a dose of Sedalite will be about 56 mg. It is not surprising that on the site at the very bottom we will see a warning: "is not a drug." And if it is not, then what is the demand from it?
Despite this, the authors of the study on the Normotim website claim that the supplement creates therapeutic concentrations of lithium in the blood (they explain this by the increased bioavailability of ascorbate compared to carbonate and other compounds). True, in this study there is absolutely no control group, there are many diagnoses (and the condition with them, as we found out above, can itself change cyclically), and there are only 54 patients. In addition, the authors state that toxicity tests were carried out on rodents, and in another Normotim's work was also credited with fighting obesity and depression (defined as "an unstable emotional background"). But neither in the Russian-language databases of scientific articles ("KiberLeninka"), nor in the English-language (PubMed) scientific articles on clinical trials of lithium ascorbate simply do not exist. This means that they were either not carried out, or they were not successful (few people want to publish negative results).
But neither in the Russian-language databases of scientific articles ("KiberLeninka"), nor in the English-language (PubMed) scientific articles on clinical trials of lithium ascorbate simply do not exist. This means that they were either not carried out, or they were not successful (few people want to publish negative results).
Indicator.Ru recommends: give preference to a medicine, not dietary supplements
Do not forget that a single dose for a patient can reach a couple of grams of the active substance. Yes, they do not prescribe it immediately, but select it, focusing on the desired concentration of lithium, which is judged by blood tests. Normotim tablets for the required dosage would have to be swallowed by the hundreds. The manufacturer's statement on therapeutic values in the blood is published only in a study on the drug's website. On the one hand, it has not been proven, but even if it is true, it only says that Normotim is dangerous, because it will be difficult to calculate a harmless dose. In order for the lithium preparation not to harm, it is necessary to investigate the effect of a particular salt. This has not been done for ascorbate.
In order for the lithium preparation not to harm, it is necessary to investigate the effect of a particular salt. This has not been done for ascorbate.
“This is a harmless vitamin at best, and no one has tested its safety in people with electrolyte and endocrine disorders. Lithium is not a harmless substance after all. But the main thing is that this Skolkovo development is not a cure for bipolar disorder, ”writes Maria Gantman, a psychiatrist and former researcher at the Scientific Center for Mental Health of the Russian Academy of Medical Sciences.
Normotim also contains vitamins, but mental disorders are not beriberi. It is worth treating the drug exactly as a dietary supplement. Therefore, if you are going to really be treated, then Normotim will not help with this. It is better to turn to real medicines, for example, based on lithium carbonate, and with an adequate dosage. Yes, they will have to be used under the supervision of doctors and with measurements of their concentration in the blood.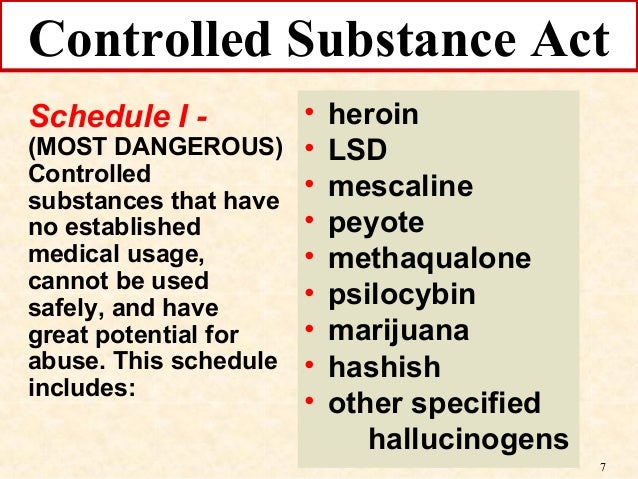 But they work and are even included in international recommendations.
But they work and are even included in international recommendations.
Our advice cannot be compared to a doctor's prescription. Before you start taking this or that drug, be sure to consult a specialist.
Like the material? Add Indicator.Ru to "My Sources" of Yandex.News and read us more often.
Press releases about scientific research, information about the latest published scientific articles and announcements of conferences, as well as data on grants and awards won, please send to [email protected].
Modern therapy of the depressive phase in bipolar affective disorder (review)
Diagnosis of bipolar affective disorder (BAD) in general and the depression that develops in this case - bipolar depression (BD) in particular is a complex problem. The differential diagnosis of bipolar disorder should be made with recurrent depression, schizophrenia, personality disorders, substance abuse, and affective disorders with somatic or neurological causes.
Based on a study by R. Hirschfeld et al. [59], 69% of patients before the diagnosis of bipolar disorder was observed with other diagnoses: unipolar depression (60%), anxiety disorder (26%), schizophrenia (18%), borderline or antisocial personality disorder (17%), alcohol abuse or other substances (16%) and schizoaffective disorder (11%). The greatest difficulty is the differential diagnosis of BAD type II and recurrent depressive disorder [74]. In 50% of cases, BAD manifests precisely with manifestations of depression. Despite the descriptions by P. Mitchel et al. [70], the clinical features of bipolar depression (high level of psychomotor retardation, heaviness in the body, lability of emotions, hyperphagia with weight gain, hypersomnia), the absence of verified episodes of elevated mood in the anamnesis leads to frequent diagnostic errors. In this case, hypomania, as a rule, does not fall into the field of view of the doctor and most often remains undiagnosed [9].5].
Several independent diagnostic studies have shown that up to 50% of young patients diagnosed with recurrent depression subsequently develop a bipolar course, i.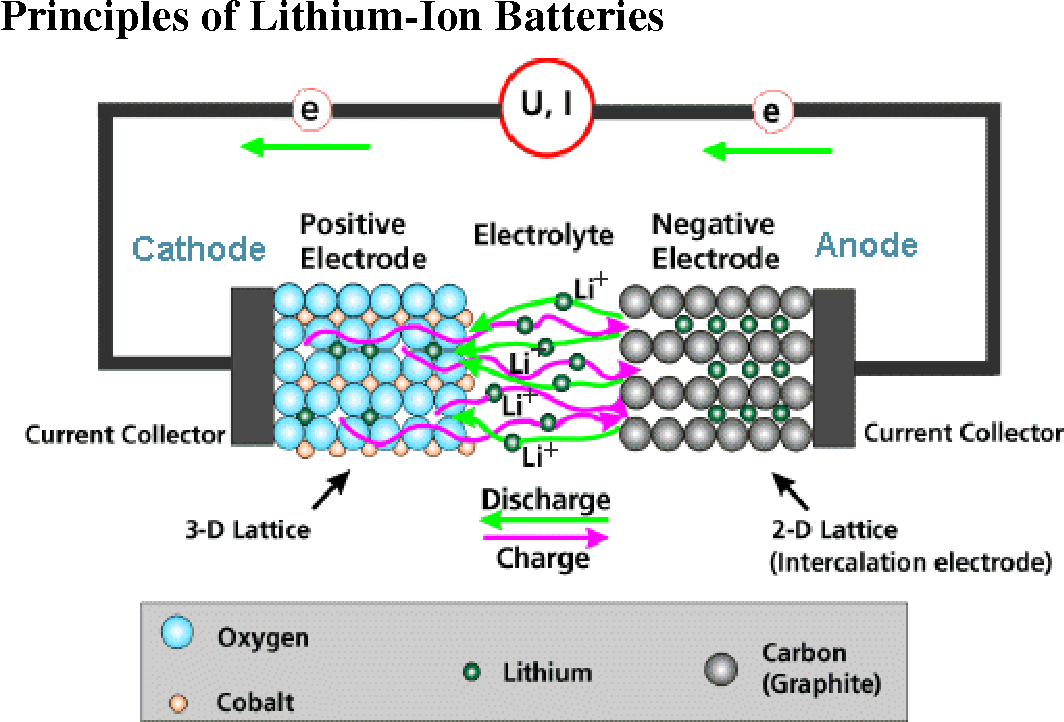 e. they endure at least one episode of hypomania or mania [53]. The correct diagnosis of BAD, on average, is established only 10 years after the onset of the disease [8]. As a result, a significant proportion of patients with bipolar disorder are observed for a long time with an erroneous diagnosis, and they do not receive adequate therapy [25].
e. they endure at least one episode of hypomania or mania [53]. The correct diagnosis of BAD, on average, is established only 10 years after the onset of the disease [8]. As a result, a significant proportion of patients with bipolar disorder are observed for a long time with an erroneous diagnosis, and they do not receive adequate therapy [25].
According to G. Sachs [86], such errors are associated primarily with the imperfection of the diagnostic system. When diagnosing an affective episode, the features of clinical symptoms are not taken into account, and such important factors as the age of manifestation, heredity and the course of the disease are not included in the criteria for affective disorders.
Meanwhile, timely diagnosis of bipolar disorder, detection of signs of this disease at the time of the development of depression in a patient, and administration of mood stabilizer therapy reduces the risk of complications and increases the chances of establishing a stable remission [8].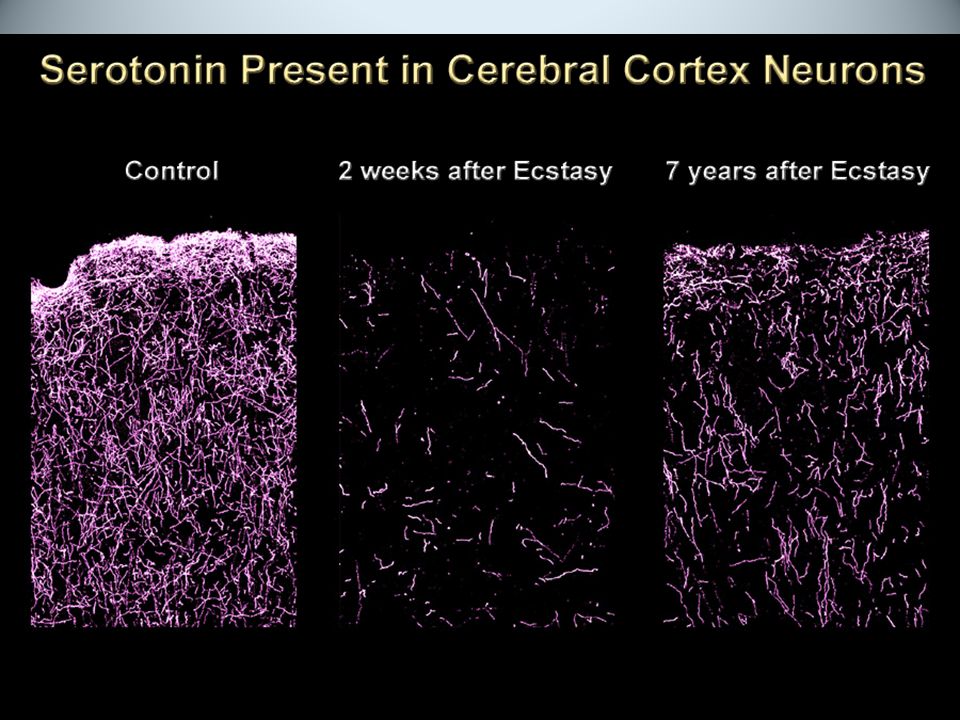 Features of the course of the disease, allowing to differentiate BD with recurrent (unipolar) depression, are given in tab. 1.
Features of the course of the disease, allowing to differentiate BD with recurrent (unipolar) depression, are given in tab. 1.
There are other clinical signs that are more characteristic of BD compared to unipolar depression: a high level of psychomotor retardation, a feeling of heaviness in the body (“lead paralysis”), psychotic inclusions. The database often has features of confusion, i.e. in the structure of the symptom complex there are elements of manic symptoms. G. Parker et al. [75] showed that DSM-IV atypical features (high levels of anxiety, emotional lability, sensitivity to frustration situations, hyperphagia with weight gain, hypersomnia) are also associated with the diagnosis of bipolar disorder. One of the characteristic symptoms, especially in adolescents and the elderly, is irritability [70]. In addition, BD patients are characterized by a higher frequency and shorter duration of affective episodes [16].
It should be noted that there are significant shortcomings of the ICD-10 clinical classification adopted in Russia, which make it difficult to diagnose bipolar disorder in cases where manic symptoms are limited to episodes of hypomania. In accordance with the ICD-10, the diagnosis of bipolar disorder is established in the presence of at least one manic or mixed and depressive episode during the course of the disease. Unlike the American DSM-IV classification, in ICD-10 type II BAD is included only in the subsection "Other bipolar affective disorders" (F31.8) along with recurrent manic episodes. The DSM-IV defines the division into type I and type II bipolar disorder. BAD type II implies the presence of at least one full-blown depressive and at least one hypomanic episode (but not full-blown mania or a mixed state). Studies of the phenomenology, heredity, and course of this type of BAD define it as an independent disease with an extremely low probability of transformation into type I BAD [35].
In accordance with the ICD-10, the diagnosis of bipolar disorder is established in the presence of at least one manic or mixed and depressive episode during the course of the disease. Unlike the American DSM-IV classification, in ICD-10 type II BAD is included only in the subsection "Other bipolar affective disorders" (F31.8) along with recurrent manic episodes. The DSM-IV defines the division into type I and type II bipolar disorder. BAD type II implies the presence of at least one full-blown depressive and at least one hypomanic episode (but not full-blown mania or a mixed state). Studies of the phenomenology, heredity, and course of this type of BAD define it as an independent disease with an extremely low probability of transformation into type I BAD [35].
Modern large-scale studies consistently confirm the high prevalence of bipolar disorder, as well as the existence of a wide range of bipolar disorders. According to this concept, bipolar spectrum disorders account for up to 50% of all mood disorders [7, 15, 22, 30, 56], which contradicts existing ideas that at least 80% of these diseases belong to recurrent depression and dysthymia.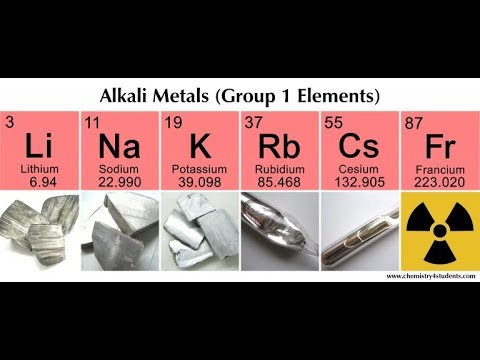 .
.
Some authors consider resistance to antidepressants in depressed patients as a predictor of BAD [82, 111]. Recently, this opinion was confirmed by the results of a large cohort study [64]. At the same time, the results of a meta-analysis of 10 studies, including 863 patients with BD and 2226 with unipolar depression, did not reveal a significant difference in the therapeutic effect of antidepressants depending on the diagnosis [103].
Pharmacotherapy BD
It is known that patients with bipolar disorder spend about half of their lives in a painful state, with depression occupying the largest share [60]. Depressive phases prevail in the picture of the disease in terms of frequency and duration. The damage from BD exceeds the damage from manias, since depression causes more disruption in the professional and social life of patients and increases the risk of suicide during and after an episode of depression [92, 107]. The frequency of parasuicides in mixed and depressive episodes reaches 25-50%, so the relief of depressive phases is one of the main goals of therapy for bipolar disorder.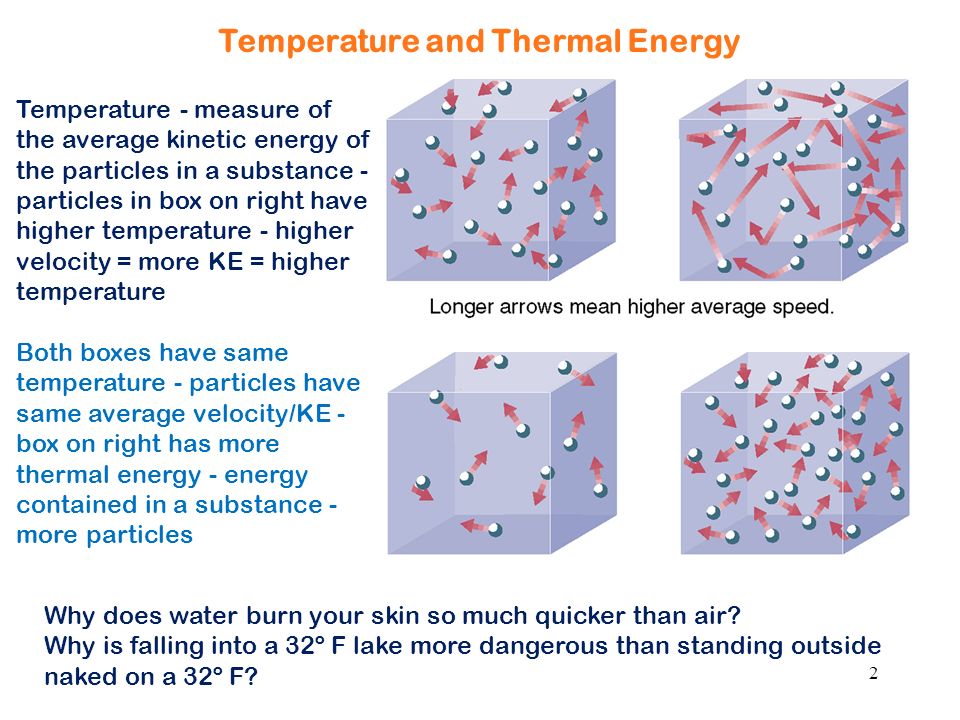
Depression is only one of the manifestations of BD, and the disease itself requires complex therapy, so the treatment strategy for BD should be based on its impact on the course of the underlying disease. For the treatment of BD, drugs of various pharmacological groups are used, the characteristics of which are presented below.
Antidepressants
In recent years, clinical guidelines for the treatment of BD have been published in various countries, but there is no complete consensus. In particular, there is no consensus among researchers regarding the use of antidepressants, since their use is associated with the risk of developing phase inversion, which is considered an unfavorable factor that aggravates the overall course of bipolar disorder and increases the risk of subsequent exacerbations [2, 38, 76]. Moreover, in approximately 25% of patients with bipolar disorder, uncontrolled use of antidepressants can lead to an increase in phase formation and the formation of a fast-cyclic and continual course [49, 97, 105].
In real psychiatric practice, antidepressants are often prescribed for BD, including as monotherapy [39], while the risk of phase inversion and the effect of such inversion on the prognosis of the further course of the disease are practically not taken into account [20].
Despite the widespread practical use of antidepressants in the treatment of AD, the number of studies of their efficacy and safety that meet the requirements of evidence-based medicine is very limited (Table 2) .
Tricyclic antidepressants (TCAs) have been used to treat bipolar disorder since their introduction into medical practice in the 1950s. In a retrospective analysis that included 1755 patients with recurrent and 277 with bipolar depression who received TCAs at the Psychiatric Clinic of the University of Munich in 1980-1992. [71], there were no significant differences between the groups in terms of the length of stay in the clinic and the dynamics of psychometric scales, which is an indirect confirmation of the effectiveness of TCA in BD.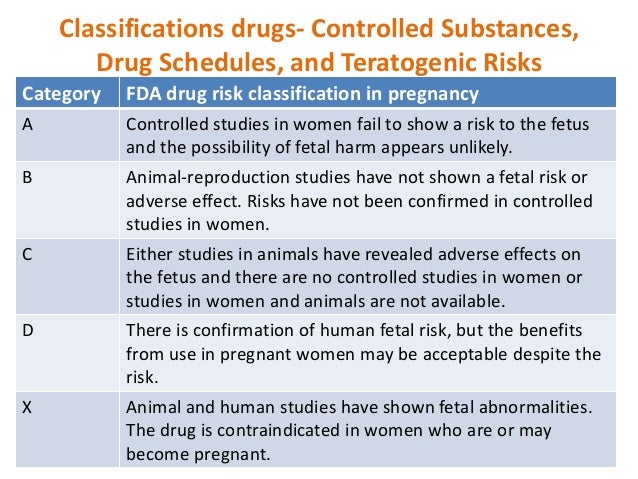 Another analysis of hospitalizations since 1920 to 1982, conducted in Switzerland [14], did not reveal an increase in the number of phase changes after the start of the use of TCAs. This conclusion, however, was refuted by controlled studies conducted in subsequent years to evaluate the effectiveness of TCAs (amitriptyline, clomipramine, desipramine and four studies using imipramine) in BD (see Table 2) .
Another analysis of hospitalizations since 1920 to 1982, conducted in Switzerland [14], did not reveal an increase in the number of phase changes after the start of the use of TCAs. This conclusion, however, was refuted by controlled studies conducted in subsequent years to evaluate the effectiveness of TCAs (amitriptyline, clomipramine, desipramine and four studies using imipramine) in BD (see Table 2) .
Meta-analysis of 12 randomized clinical trials by H. Gijsman et al. [47], included 1089 patients. It was based on both placebo-controlled and comparative studies with another antidepressant or drugs from other groups (normotimics, atypical antipsychotics). A meta-analysis showed that the risk of phase inversion with TCAs is significantly higher than with selective serotonin reuptake inhibitors (SSRIs) or MAO inhibitors (10% vs 3.2%). In addition, TCAs were slightly less effective than other antidepressants in AD, but the differences were not statistically significant.
Similar results were obtained in a meta-analysis conducted by S. Montgomery [72], which showed that the frequency of affect inversions with SSRIs was 2-3% compared with 11% with TCAs. According to another analysis of antidepressant studies, TCAs provoke phase inversion in bipolar disorder in 11-38% of cases [79]. The results of several open studies indicate even higher rates of phase inversion - 31-74% with BD TCA monotherapy [48]. The frequency of inversions is dose-dependent and the higher the higher the doses used [50].
In a double-blind, placebo-controlled trial of paroxetine adjunct to lithium therapy, no efficacy advantage of paroxetine over either lithium alone or lithium/imipramine combination was found, although the incidence of phase reversal in the paroxetine group was significantly lower than in the imipramine group [62].
Fluoxetine, compared with other SSRIs, caused a phase inversion somewhat more often, which may be due to its long half-life (T ½ of the active metabolite of norfluoxetine - 7-10 days), so it is undesirable to use it in patients with a history of mania induced by antidepressants [9].
In a prospective, double-blind study, when bupropion or desipramine was added to baseline mood stabilizer therapy, both drugs were equally effective. However, phase inversion was observed in 5 of 10 patients in the desipramine group and only in 1 of 9 patients treated with bupropion [83]. In a comparative study of bupropion, sertraline, and venlafaxine, used on the background of mood stabilizer therapy in 174 patients with type I and type II BD, in all groups there was an approximately equal number of responders (49-53%) and the number of patients who achieved remission (34-41%) [77]. At the same time, phase inversion was significantly more common in patients treated with venlafaxine.
In an open-label study of 83 patients with type II BD, venlafaxine monotherapy was superior to lithium monotherapy (responder rates 58.1% vs. 20.0%, patients in remission 44.2 vs. 7.5 %, respectively) [12]. In this study, there was no increase in phase inversion with venlafaxine.
Another study showed that the risk of phase inversion depends on the type of disease - in patients with BAD type II, inversion was significantly less common than in patients with BAD type I (12 and 2%, respectively) [10].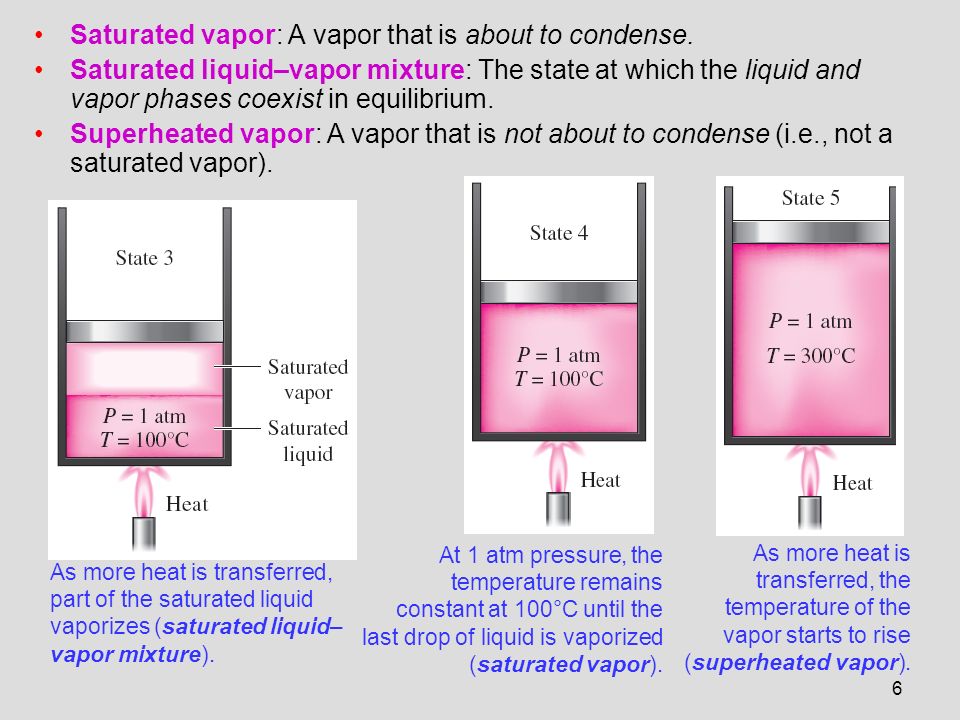 According to A.A. Aleksandrova [1], in the treatment of patients with BAD type I TCA, the frequency of phase inversion reaches 70%, and in patients with BAD type II - only 5-10%.
According to A.A. Aleksandrova [1], in the treatment of patients with BAD type I TCA, the frequency of phase inversion reaches 70%, and in patients with BAD type II - only 5-10%.
There are data on the development of tachyphylaxis to the effect of antidepressants during long-term therapy and during their repeated prescriptions to patients with bipolar disorder [13, 89]. According to L. Altshuler et al. [9], with BD monotherapy with antidepressants, a complete remission (total score when assessed on the Hamilton scale no more than 7) was observed only in 15-20% of patients. Moreover, relapse within 4 months was observed in 20-25% of patients, even with a good outcome, regardless of whether the antidepressant was continued or stopped [11].
There is evidence of insufficient efficacy of antidepressants in the treatment of BD [88]. In the STEP-BD study [87], the addition of paroxetine and bupropion to mood stabilizer therapy was not superior to placebo. In another double-blind, placebo-controlled comparative study, paroxetine was not superior to placebo in efficacy and was significantly inferior to the atypical antipsychotic quetiapine in reducing depressive symptoms on the MADRS scale [66].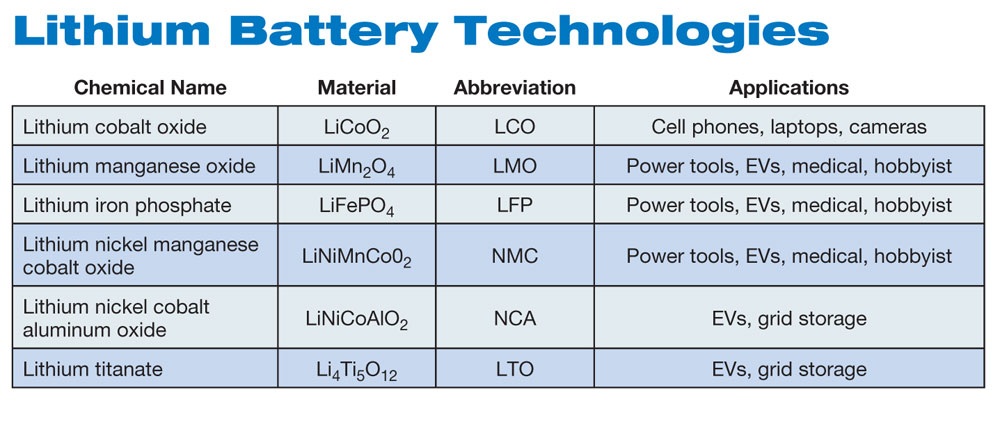 In a recent meta-analysis by M. Sidor and G. Macqueen [90] showed no superiority of antidepressants compared to placebo. At the same time, there was also no significant increase in the risk of phase inversion under their influence.
In a recent meta-analysis by M. Sidor and G. Macqueen [90] showed no superiority of antidepressants compared to placebo. At the same time, there was also no significant increase in the risk of phase inversion under their influence.
Thus, the available results of studies on the effectiveness of antidepressants in AD are highly controversial. In part, this may be due to the well-known fact that in patients with BD on the background of the appointment of an antidepressant, an improvement in the condition can be observed, which neither clinicians nor researchers can confidently explain by the action of the drug, and not by the spontaneous end of the depressive phase. In addition, an analysis conducted in the United States by the Federal Drug Administration (FDA) [101] showed the bias in the publication of clinical studies on the effectiveness of antidepressants: most of the studies with negative results were not published or were presented as studies with positive results (for example, phase inversion was regarded as an effective treatment).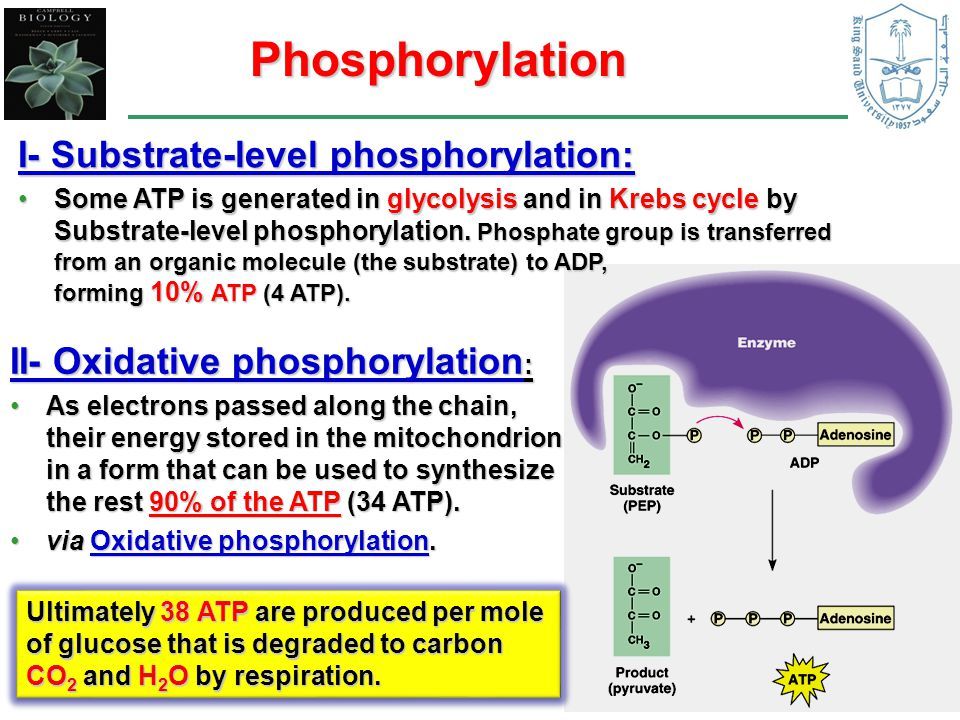 With an adequate assessment, only 51% (instead of 93%) of clinical studies on the effectiveness of antidepressants could be assessed as positive, and 49% as studies with a negative result. In general, antidepressants in BD are recommended to be used for the shortest possible time and, already at the first stage, to be combined with normothymic drugs that prevent phase inversion.
With an adequate assessment, only 51% (instead of 93%) of clinical studies on the effectiveness of antidepressants could be assessed as positive, and 49% as studies with a negative result. In general, antidepressants in BD are recommended to be used for the shortest possible time and, already at the first stage, to be combined with normothymic drugs that prevent phase inversion.
In a meta-analysis by S. Ghaemi et al. [46] with long-term use of antidepressants for the prevention of BD, the risk of phase inversion was 72% higher than with monotherapy with mood stabilizers, although the former showed greater effectiveness in preventing depressive phases. During the period of antidepressant withdrawal, in order to identify both depressive and manic symptoms, careful monitoring of the patient's condition is necessary [41, 42].
The question of the use of antidepressants in BD remains debatable. In most clinical guidelines, antidepressants retain their role in the treatment of OD, but they are recommended to be prescribed in combination with mood stabilizers [49, 108].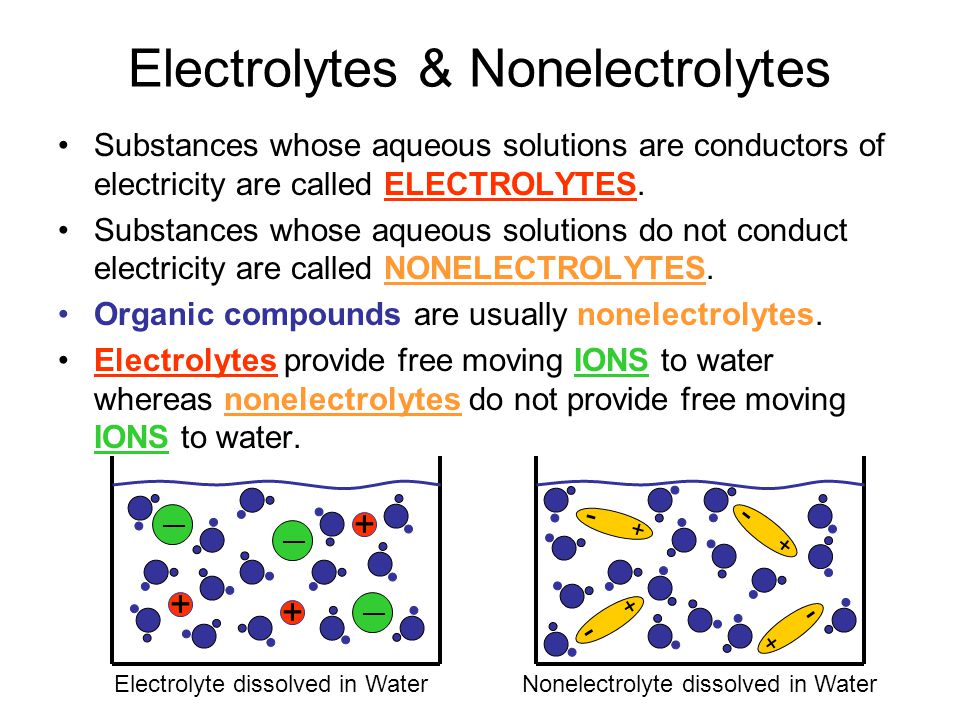
Normotimics
According to modern concepts, mood stabilizers are the drugs of first choice in the treatment of both mania and OD. This group includes 4 main drugs with a proven normothymic effect: lithium carbonate, sodium valproate, carbamazepine and lamotrigine. All drugs in this group have a more or less pronounced antidepressant effect. The main advantage of normotimics is a preventive effect, which allows prolonging the euthymic period. They also prevent the development of phase inversion caused by the additional prescription of antidepressants, often inevitable during periods of depressive states. Normotimics should be prescribed from the moment the disease is diagnosed, followed by continuous use throughout life [2].
Lithium salts have occupied leading positions among mood stabilizers for many years. The use of lithium in bipolar disorder was based on almost half a century of empirical experience and only later supported by the results of randomized clinical trials [104]. Some current guidelines for the treatment of BD recommend lithium as the first drug to start treatment of the bipolar phase of any polarity [17, 49, 108]. It is assumed that lithium has specific anti-suicidal properties [6, 33]. In a double-blind, placebo-controlled study [48], lithium monotherapy was found to be effective in 79% of patients with BD and 36% with recurrent depression. In a review [106] of 9 different placebo-controlled studies of lithium in BD, including a total of 149 patients, the drug showed a clear antidepressant effect in 36% of cases, and positive dynamics was noted in another 79% of patients.
Some current guidelines for the treatment of BD recommend lithium as the first drug to start treatment of the bipolar phase of any polarity [17, 49, 108]. It is assumed that lithium has specific anti-suicidal properties [6, 33]. In a double-blind, placebo-controlled study [48], lithium monotherapy was found to be effective in 79% of patients with BD and 36% with recurrent depression. In a review [106] of 9 different placebo-controlled studies of lithium in BD, including a total of 149 patients, the drug showed a clear antidepressant effect in 36% of cases, and positive dynamics was noted in another 79% of patients.
The dependence of the antidepressant activity of lithium on its blood concentration was shown in a double-blind, randomized, placebo-controlled comparative study, which studied the effectiveness of adding imipramine and paroxetine to lithium in patients with BD [73]. Although the purpose of this study was not to study the effectiveness of lithium itself, patients in the control group received only lithium.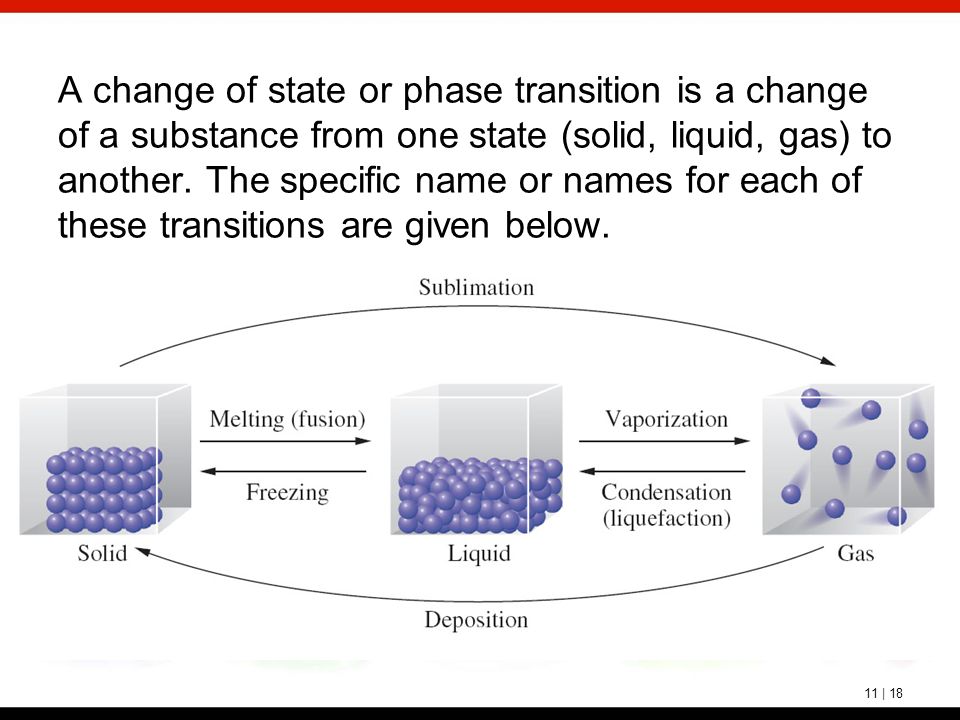 When prescribing paroxetine or imipramine to patients with high serum lithium concentrations (0.8 mmol/l), the same therapeutic effect was observed as with lithium monotherapy, which allowed the authors to conclude that lithium monotherapy in BD is a fairly effective method. treatment, and the drug has its own thymoanaleptic effect. However, in a recent study of lithium versus quetiapine [110], lithium was not superior to placebo in reducing depressive symptoms.
When prescribing paroxetine or imipramine to patients with high serum lithium concentrations (0.8 mmol/l), the same therapeutic effect was observed as with lithium monotherapy, which allowed the authors to conclude that lithium monotherapy in BD is a fairly effective method. treatment, and the drug has its own thymoanaleptic effect. However, in a recent study of lithium versus quetiapine [110], lithium was not superior to placebo in reducing depressive symptoms.
The disadvantage of the antidepressant effect of lithium is its slow development. When prescribing lithium salts during the depressive phase, it takes an average of 6-8 weeks to achieve a clear clinical effect, so monotherapy in the acute period of the depressive phase is in most cases insufficient.
In recent years, a lot of data has been accumulated on the significant disadvantages of lithium salts in terms of safety and tolerability, especially when used in high doses. Common side effects of lithium preparations include weight gain, tremors, gastrointestinal disturbances, and drowsiness. The concentration of lithium in the blood plasma to achieve an antidepressant effect should be maintained at a level of 0.6-0.8 mmol/l, however, this increases the risk of side effects [45, 78]. Antidepressants, valproate or lamotrigine may be used to increase the effectiveness of lithium therapy [102, 109].
The concentration of lithium in the blood plasma to achieve an antidepressant effect should be maintained at a level of 0.6-0.8 mmol/l, however, this increases the risk of side effects [45, 78]. Antidepressants, valproate or lamotrigine may be used to increase the effectiveness of lithium therapy [102, 109].
In connection with the above disadvantages of lithium, a number of modern guidelines favor valproate among mood stabilizers [55], which has moderate antidepressant properties [65], has a more favorable side effect profile compared to lithium salts, and is better tolerated by patients [104]. Some experts believe that valproate can be considered as a drug with anti-suicidal properties, since it can improve cognition and mood [61, 67]. The efficacy of valproate in BD has been studied in a number of studies. Thus, in an open study [106], the effectiveness of valproate in the treatment of depression in patients with BAD type II was 63% in general, and 82% in the subgroup of patients who had not previously received antidepressants. However, in a double-blind, randomized study [63] including patients with type I and type II bipolar disorder, by the end of week 8, there was no significant difference between the proportions of patients meeting the criteria for recovery in the valproate (43%) and placebo (27%) groups. . At the end of the study, valproate did not outperform placebo when assessed on the Hamilton scale, although at 2, 4 and 5 weeks this indicator was significantly better in the group receiving the active drug. It is believed that statistical differences between the effects of valproate and placebo were not obtained in this study due to undersampling [84].
However, in a double-blind, randomized study [63] including patients with type I and type II bipolar disorder, by the end of week 8, there was no significant difference between the proportions of patients meeting the criteria for recovery in the valproate (43%) and placebo (27%) groups. . At the end of the study, valproate did not outperform placebo when assessed on the Hamilton scale, although at 2, 4 and 5 weeks this indicator was significantly better in the group receiving the active drug. It is believed that statistical differences between the effects of valproate and placebo were not obtained in this study due to undersampling [84].
In an 8-week, double-blind, randomized study [36], 25 outpatients reported positive results with valproate in patients with type I bipolar disorder. It was significantly superior to placebo in reducing symptoms of depression and anxiety. In a meta-analysis by L. Smith et al. [94], valproate was also significantly superior to placebo in reducing depressive symptoms. There is evidence that valproate is more effective in treating depression in patients with rapid cycling or type II bipolar disorder compared to type I bipolar disorder [62].
There is evidence that valproate is more effective in treating depression in patients with rapid cycling or type II bipolar disorder compared to type I bipolar disorder [62].
The number of studies on the use of carbamazepine in BD is limited, and they cover a small number of patients. According to the results of a meta-analysis [76] of studies with different design, including patients with recurrent depression and BD, the response to carbamazepine therapy was observed in 56 and 44% of patients in open-label and controlled studies, respectively. Moderate efficacy of carbamazepine in BD was shown in one placebo-controlled study [21], but these results were not confirmed in other studies [93]. In total, 8 open-label and 4 small-scale controlled studies of the use of carbamazepine in BD were found in the literature, including 244 patients, of which 55% responded to therapy. At the same time, ⅓ of these, a pronounced effect or an effect that determines clinical recovery was observed [4].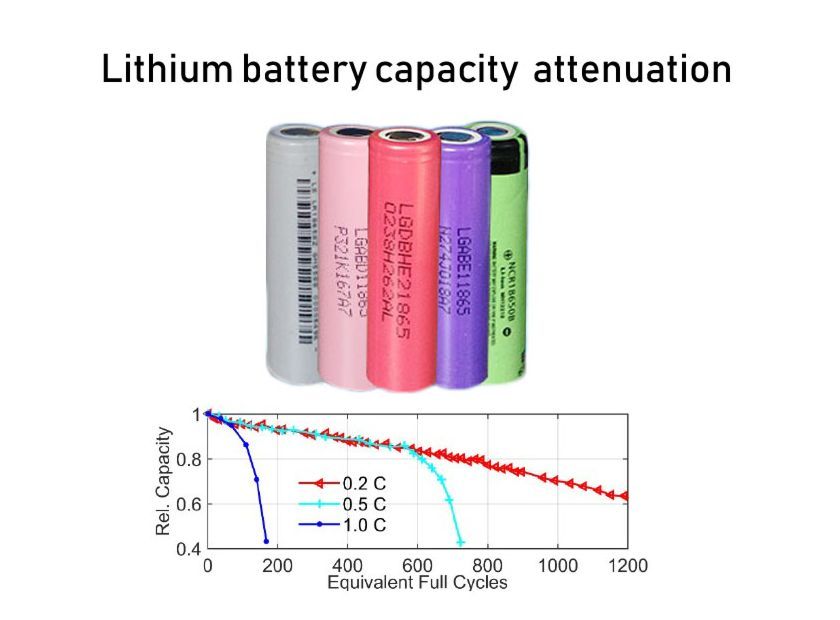 Obviously, to confirm the antidepressant effect of carbamazepine in BD, additional placebo-controlled studies are needed. Current guidelines consider this drug as a second/third line therapy for OBD [54, 108].
Obviously, to confirm the antidepressant effect of carbamazepine in BD, additional placebo-controlled studies are needed. Current guidelines consider this drug as a second/third line therapy for OBD [54, 108].
Lamotrigine occupies a special place among anticonvulsants in the treatment of BD. This drug showed significant antidepressant activity when used alone in a multicentre, double-blind, randomized, placebo-controlled study [27], which included 195 patients with moderate depression in type I bipolar disorder. Two groups of patients received fixed doses of lamotrigine 200 and 50 mg per day for 7 weeks, and patients in the third group received placebo. Patients in the lamotrigine groups experienced a significant reduction in depressive symptoms compared with the placebo group. The most significant antidepressant effect of lamotrigine was at a dose of 200 mg per day. A "significant improvement" score on the overall clinical impression scale was achieved in 51% and 41% of patients treated with lamotrigine 200 and 50 mg, respectively, compared with 26% in the placebo group.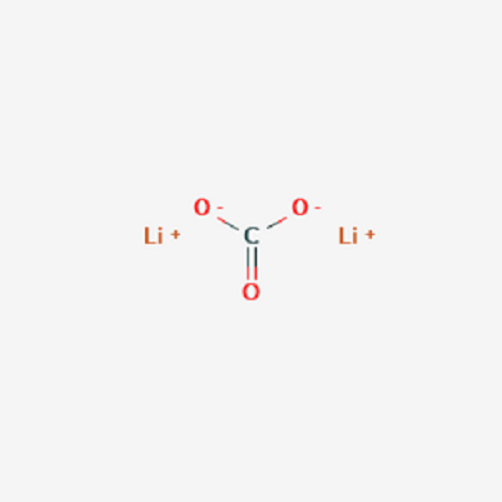
Data on the efficacy of lamotrigine were confirmed by the results of a large multicenter, double-blind, placebo-controlled study that included 200 patients with BD in bipolar I and type II [24]. Lamotrigine at all doses (100–400 mg daily) was superior to placebo, with a greater response to lamotrigine in patients with type I BD. However, in other controlled trials [29], lamotrigine in BD did not show any benefit compared to placebo. However, one meta-analysis [44] showed superiority of lamotrigine over placebo, especially in patients with severe depression.
Lamotrigine is safe and well tolerated by patients. Its most common side effect is headache, and the frequency of affect reversal is comparable to that of placebo. With a rapid increase in doses of the drug, a rash developed in 0.3% of patients, with a slow titration of doses, its frequency decreased to 0.01%. In most guidelines, lamotrigine, like lithium and valproate, are considered first-line drugs for AD.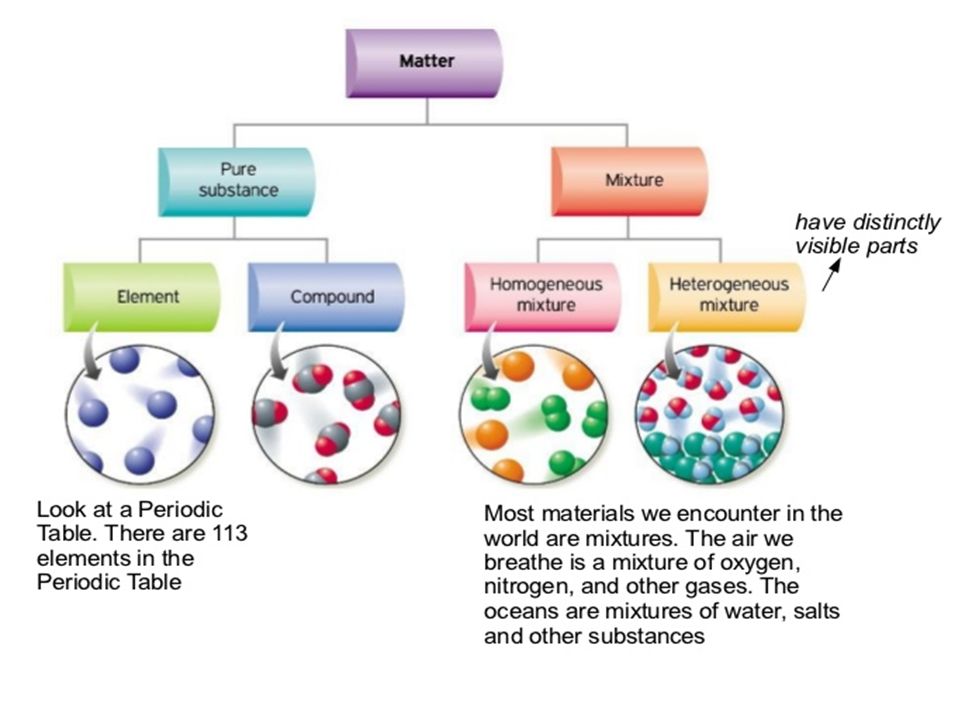
At the same time, analysis of data from large double-blind randomized controlled trials [96] showed that lamotrigine was inferior in efficacy to two FDA-approved drugs for the treatment of OBD (quetiapine and olanzapine plus fluoxetine), but superior to them in tolerability. This led the authors to suggest that lamotrigine is more likely to be indicated in patients with mild episodes of AD who are prone to sedation and weight gain.
Another anticonvulsant, topiramate, is also attracting attention for its potential efficacy in OBD. In a small randomized blind study in 36 outpatients with BD, when the anticonvulsant topiramate or the antidepressant bupropion was added to normothymic therapy with valproate or lithium, an equal efficacy of therapy with a significant reduction in depressive symptoms after 2 weeks of treatment was found [67]. Topiramate is safe and well tolerated; its most common side effect is weight loss (average 5.8 kg over 8 weeks). However, further studies are required to confirm its effectiveness in AD.
Another anticonvulsant, gabapentin, has been studied in only one double-blind, placebo-controlled, cross-over study compared with lamotrigine [41]. At the same time, the effectiveness of therapy in the gabapentin group did not significantly differ from placebo and was lower than that of lamotrigine (26%, 19% and 45%, respectively).
Antipsychotics
In the last decade, the appearance of atypical antipsychotics in the arsenal of drugs has significantly expanded the possibilities of treating bipolar disorder, including its depressive phase. Considering that 50% of patients with bipolar disorder have psychotic symptoms at different stages of the disease, the appointment of antipsychotics becomes almost inevitable. Meanwhile, the use of classical antipsychotics in patients with bipolar disorder is limited by a number of factors. It has been shown that patients with bipolar disorder are more at risk of developing extrapyramidal symptoms and tardive dyskinesia compared with patients of other diagnostic groups [5, 51].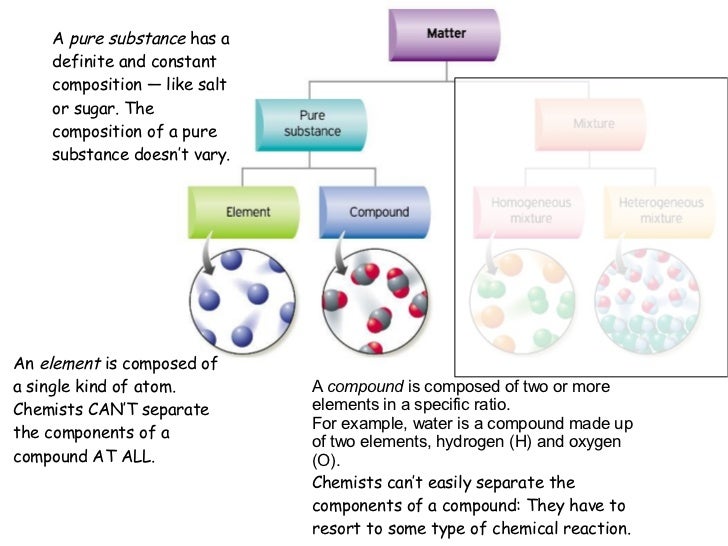 In addition, the depressogenic effect of classical antipsychotics is well known [3].
In addition, the depressogenic effect of classical antipsychotics is well known [3].
A meta-analysis that included 21 randomized and 13 non-randomized trials demonstrated a significant superiority of atypical antipsychotics over classical antipsychotics in BD [43].
Studies of olanzapine and quetiapine have demonstrated an antidepressant effect in addition to the reduction of psychotic symptoms and good tolerability. Thus, in a randomized 8-week study [100], which included 833 patients with moderate depression in type I bipolar disorder, both olanzapine monotherapy (10 mg per day) and its combination with fluoxetine were significantly superior to placebo in terms of antidepressant effect (response rate - 56, 1, 390 and 30.4%, remission rate - 48.8, 32.8 and 24.5%, respectively). Olanzapine was well tolerated by BD patients, with the most common side effects being drowsiness, increased appetite, weight gain, and dry mouth [100]. The combination of olanzapine with fluoxetine has been shown to be superior to lamotrigine in reducing depressive symptoms and the risk of self-injurious behavior.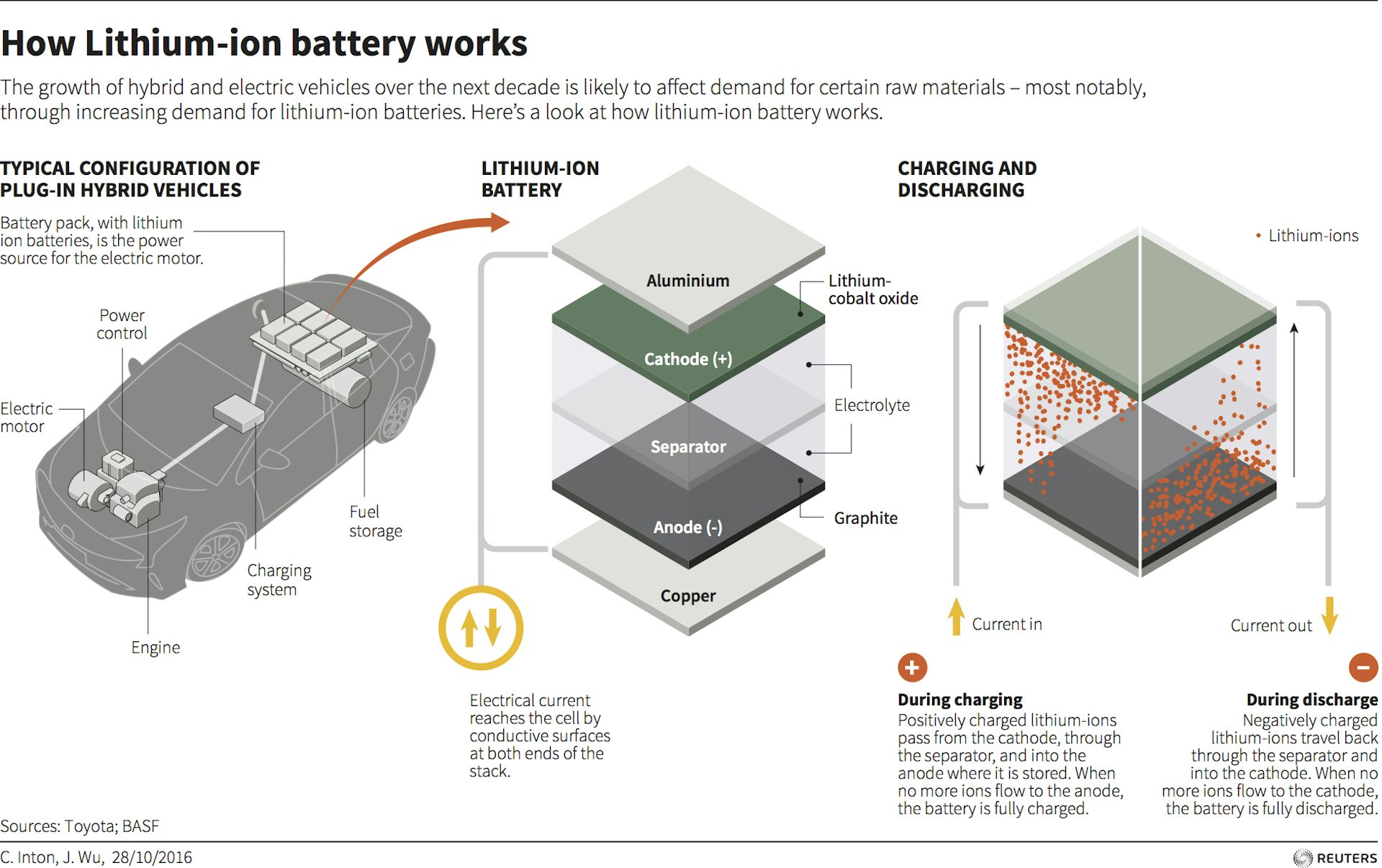 However, metabolic side effects were more frequently observed with its use [26].
However, metabolic side effects were more frequently observed with its use [26].
The effectiveness of quetiapine in BD was also confirmed by the results of a meta-analysis of 7 randomized controlled trials [32]. In an 8-week, randomized, placebo-controlled study [28] of quetiapine (300 and 600 mg daily) in the treatment of 542 patients with depression in BAD types I and II, the drug at both doses was significantly superior to placebo in the ability to reduce the main symptoms of depression, including suicidality. thoughts. In another study, quetiapine was also significantly superior to placebo and lithium in reducing depressive symptoms on the Montgomery-Asberg scale [110]. These data were confirmed in subsequent studies. Thus, in the EMBOLDEN II study [66], quetiapine demonstrated superiority in reducing depressive symptoms over both placebo and active therapy with paroxetine. The antidepressant/quetiapine combination was also statistically significantly more effective than the antidepressant/lithium combination both in terms of the number of patients who responded to treatment (88 and 50%, respectively) and the number of patients who achieved remission (88 and 38%) [54]. Quetiapine and the combination of olanzapine with fluoxetine are officially registered for the relief of BD.
Quetiapine and the combination of olanzapine with fluoxetine are officially registered for the relief of BD.
The antidepressant effect of risperidone has not been demonstrated in small, double-blind studies [69], although in an open study in patients with resistant recurrent depression, its addition to citalopram led to an increase in the effect of the antidepressant [81]. In double-blind, placebo-controlled studies, amisulpride has also been shown to have an antidepressant effect when used at low doses. However, these studies included patients with depressive states in diagnostic categories other than bipolar disorder [31]. The effectiveness of amisulpride as a treatment for BD requires further study.
Aripiprazole, according to the results of a meta-analysis of randomized placebo-controlled trials, is effective in patients with both mania and depression, but its use may be limited by side effects - akathisia, insomnia, anxiety and nausea [18]. Another meta-analysis [40] showed that a significant difference from placebo in the treatment of patients with an acute episode of BD was noted only after 8 weeks of aripiprazole use, while the effect of the drug did not differ significantly from placebo.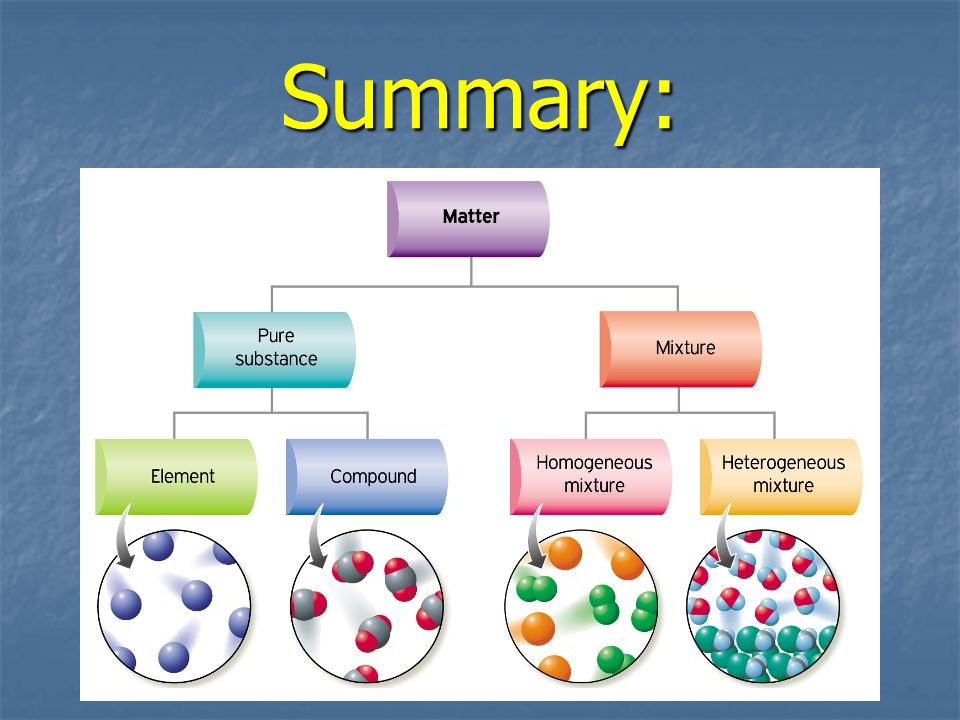 In addition, long-term outcomes of BD treatment with aripiprazole remain unexplored.
In addition, long-term outcomes of BD treatment with aripiprazole remain unexplored.
Therapeutic tactics for the relief of BD
Treatment for mild, moderate and severe depression without psychotic symptoms in type I and type II bipolar disorder is identical.
In patients not receiving normotimic, BD therapy should be started with a drug of this group. If the patient is already receiving a mood stabilizer, an attempt to increase its dose, the addition of quetiapine or the use of combination therapy with olanzapine and fluoxetine, or the addition of a second mood stabilizer and the addition of psychotherapy, is recommended. If these therapeutic measures are ineffective, it is possible to use combined therapy with a mood stabilizer and an antidepressant (mainly SSRIs), which is prescribed for the shortest possible time. When using combination therapy, it is necessary to take into account possible drug interactions of drugs.
If the second course of therapy is ineffective, it is possible to change the normotimic and / or antidepressant, or, in the case of protracted conditions, increasing social disadaptation, the issue of using electroconvulsive therapy (ECT) [80]. When ECT fails, anti-resistance measures are taken, similar to those used for resistant depression in recurrent depressive disorder.
When ECT fails, anti-resistance measures are taken, similar to those used for resistant depression in recurrent depressive disorder.
In severe OD, as well as in the presence of suicidal thoughts, already at the first stage of treatment, combined therapy with a mood stabilizer and an antidepressant is recommended [99] or the use of quetiapine, or a combination of olanzapine with fluoxetine. If the first course is ineffective, an attempt to change the antidepressant is first recommended, then a mood stabilizer, or the use of ECT.
Thus, at present, there is no drug that, in monotherapy, could provide all the effects necessary for BD, namely, the rapid relief of depressive and psychotic symptoms, the prevention of suicide and the prevention of phases of both poles. Some drugs appear to be very promising, but the number of well-designed studies in this area remains very limited. There has not been a single consensus among experts regarding the stages of BD therapy. Approaches to diagnosing BD also require improvement.