How to treat trauma in therapy
Treating trauma - Counseling Today
In just the first two months of 2010, devastating earthquakes rocked Haiti and Chile, a University of Alabama in Huntsville professor stood accused of gunning down colleagues at a faculty meeting and a reportedly disgruntled pilot flew his private airplane into an Internal Revenue Service building in Austin, Texas. These tragedies ranged in scope and affected people in different states and countries, but one common denominator was the trauma they no doubt left in their wake.
Natural disasters, ongoing wars, terrorist attacks, plane crashes, school violence and abuse are among the most widely recognized causes of trauma, but one expert points out that trauma can also stem from events that don’t necessarily make the national news. “Every day, counselors work with clients who are exposed to or experience the tragedies of daily life — auto accidents, the sudden loss of family members, friends, classmates or coworkers,” says Jane Webber, associate professor at New Jersey City University and coordinator of the university’s counseling and school counseling program.
“Where we once considered traumatic events as rare, we now know that most people experience one or more such events in their lifetime.”
Carlos Zalaquett remembers working with a 64-year-old client who was referred to him for treatment for depression. “While discussing her history and intake form, she mentioned that she had felt depressed and anxious for the last four years,” says Zalaquett, coordinator of the clinical mental health counseling program and the graduate certificate in mental health counseling in the University of South Florida Department of Psychological and Social Foundations. “She didn’t have a prior history of these symptoms, but her family believed that aging and lack of a support or social network led to her current situation.”
As the two explored the woman’s strengths and therapeutic goals, the client shared with Zalaquett the goal of driving her car again. “Upon exploring the reasons for mentioning this goal, which was somewhat puzzling to me, she reported surviving a near-death car accident four years prior,” says Zalaquett, a member of the American Counseling Association. “She described living a life encompassing all of her current therapeutic goals, including driving her own car, before this traumatic crash.”
“She described living a life encompassing all of her current therapeutic goals, including driving her own car, before this traumatic crash.”
The focus of treatment rapidly shifted to addressing the client’s post-traumatic stress reaction following the accident, Zalaquett says. “We used systematic desensitization, imagery techniques and in vivo exposure to help her reduce her fear of driving and get her in the driver’s seat. Four months later, she was driving and, much to the surprise of her family, was no longer clinically depressed or anxious. She had reestablished a connection to a social network of friends and acquaintances.”
The challenges the client was facing originated from trauma, according to Zalaquett. “This original source was forgotten by her and her family due to the marked anxiety and depressive symptomology and social isolation observed, all of which were assumed to be the cause of her symptoms and not the consequences of her trauma. I saw her two years after the completion of her treatment.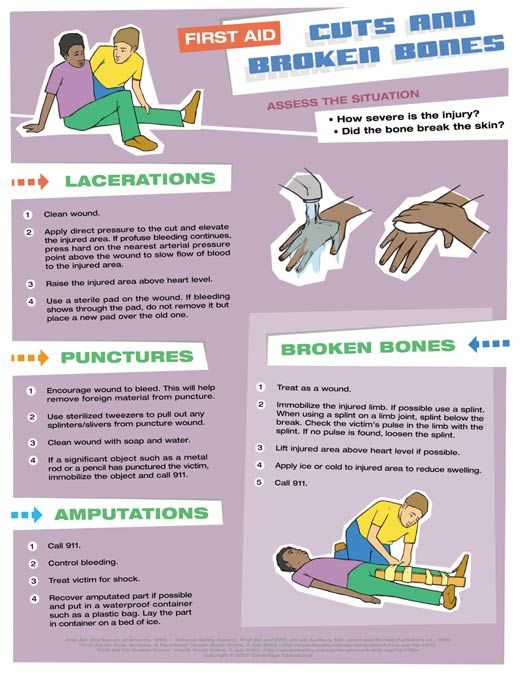 This time she was driving a close friend to therapy.”
This time she was driving a close friend to therapy.”
The root of the problem
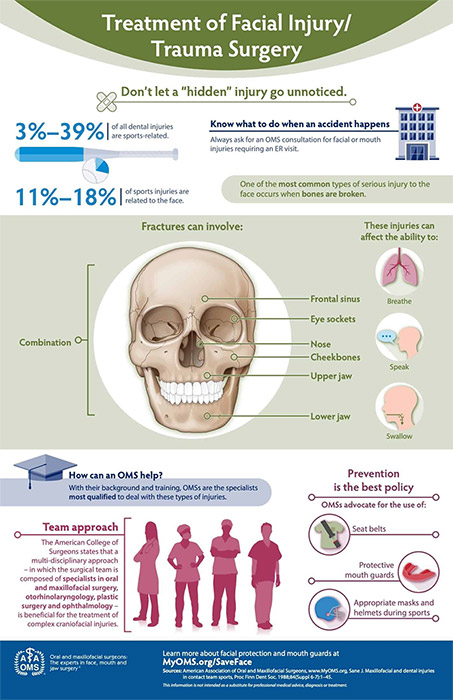
While the causes of trauma can vary widely, Zalaquett says, it is important to recognize when an event implies exposure to an extreme traumatic stressor. These events generally involve serious injury or the threat of death to the individual or witnessing an event that involves death, injury or threat of another person. Trauma can also develop when a person learns about the unexpected or violent death of, or serious harm or injury to, a family member or close associate, he adds.
“There are many traumatic events that do not meet the criterion of threatened death but are like ‘living death,'” adds Webber, who, along with J. Barry Mascari, served as editor for Terrorism, Trauma and Tragedies: A Counselor’s Guide to Preparing and Responding, the third edition of which was recently published by the ACA Foundation. Individual complex traumas such as sexual and physical abuse, domestic violence, ongoing harassment or bullying can fall into this category, Webber says.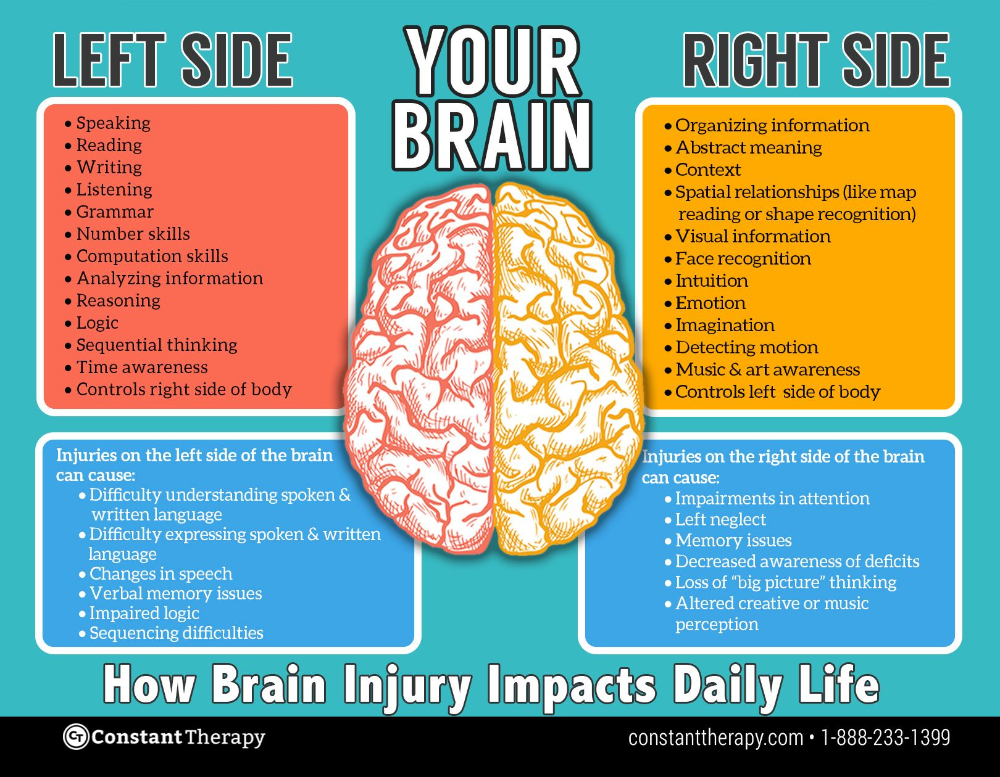
Some of the signs and symptoms associated with trauma-induced stress include sleep disturbance, emotional instability and impaired concentration, Zalaquett says. When people have become emotionally or psychologically overwhelmed, they often protect themselves through denial, disbelief and dissociation, he adds. Traumatized individuals can have difficulty performing regular duties, might experience flashbacks or nightmares and may respond to events that remind them of the trauma. “Flood victims, for example, may demonstrate very strong emotional responses to rain, storm clouds, the sound of running water or the sight or smell of mud,” he says.
Zalaquett says counselors should also be aware that clients might express their emotional distress physically, complaining of headaches, backaches, stomachaches, sudden sweating or heart palpitations, constipation or diarrhea, or susceptibility to colds and other illnesses.
But the signs of trauma aren’t always visible, Webber says, so counselors should remain patient and supportive. “I have often worked with clients who, although they have been to several therapists, have never disclosed their symptoms or their trauma history,” she says. “Being fully present in the moment with such a client helps to build a safe environment. It may be weeks or months before the client feels safe enough with the counselor to disclose even a small hint.”
“I have often worked with clients who, although they have been to several therapists, have never disclosed their symptoms or their trauma history,” she says. “Being fully present in the moment with such a client helps to build a safe environment. It may be weeks or months before the client feels safe enough with the counselor to disclose even a small hint.”
Presenting problems, intake forms and case histories can provide clues to a client’s traumatic experiences, says Webber, a past chair of the ACA Foundation who teaches disaster response, trauma and crisis counseling. “Asking solution-focused questions helps. For example, ‘When was the last time you felt good? When do you not feel this way? What are you doing when you feel differently?’ With training and supervised experience, counselors often develop an intuitive feeling about traumatized individuals — a sixth sense about the client’s fears, terror, feelings of being threatened and resulting self-protectiveness. The counselor ‘feels’ as the client feels and is alert to triggers that increase symptoms like hyperarousal, hypervigilance, dissociation, numbing, anxiety and avoidance of reminders of events. ”
”
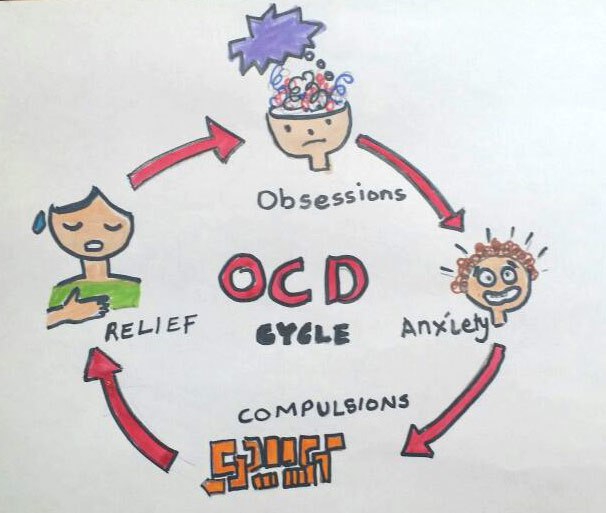
Counselors strongly emphasize the importance of helping clients understand that the feelings they are experiencing after a traumatic event are completely normal. But according to the most recent edition of the Diagnostic and Statistical Manual of Mental Disorders, when post-traumatic stress symptoms persist for at least a month, a diagnosis of post-traumatic stress disorder (PTSD) might be considered. “For individuals experiencing PTSD, many emotional and cognitive processes become more intense, while paradoxically, others are deadened,” Zalaquett says. “In a sense, individuals who have their lives suddenly and drastically changed by destructive events essentially experience more than they can integrate, and their feelings of personal control, competence, security and safety are all greatly diminished. They now view the environment — and to some extent, other people — as unsafe. On guard, they are ready for danger at all times. This state of hypervigilance also increases the likelihood of social withdrawal and isolation and decreases the likelihood these individuals will seek assistance for their distress.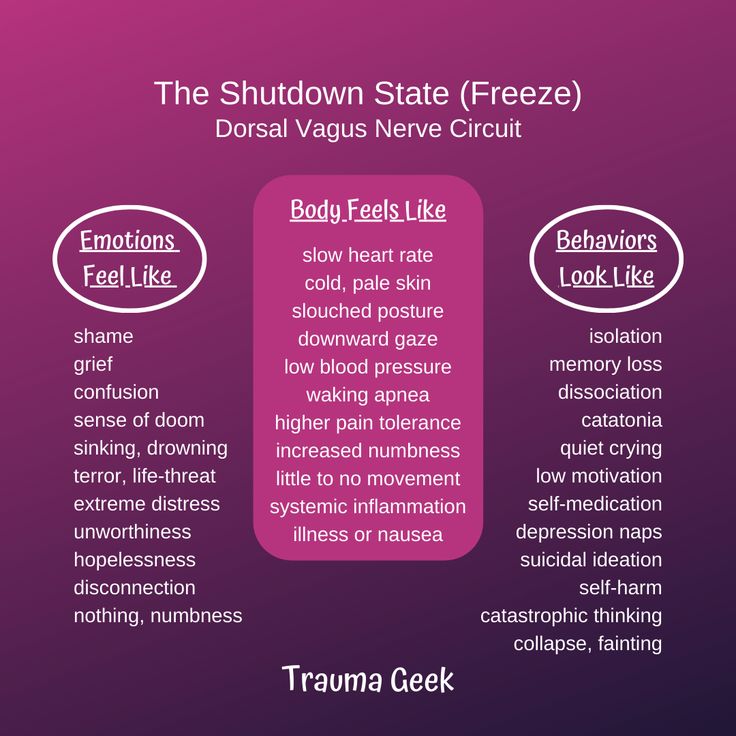 ”
”
Not everyone exposed to a traumatic event develops PTSD or other serious disorders, however. Webber notes studies have shown that the majority of people in mass disasters experience personal and spiritual growth and create new existential meaning as a result of their experience.
Certain trauma tasks are time sensitive, Webber says, such as securing an individual’s immediate physical and emotional safety, whether in the aftermath of an earthquake or in a situation of child sexual abuse. “Research shows that when survivors of mass disasters receive psychological first aid, this speeds the return to normal functioning,” she says. “Psychological first aid also provides for identification and referral for additional support for those with predisposing conditions or more serious problems.”
In disaster situations, many counselors want to begin providing counseling immediately, but doing so may have unintended negative consequences, Zalaquett advises. It is essential to conduct initial screenings of individuals to check for known symptoms or risk factors for PTSD before providing treatment, he says. “Counseling and other appropriate mental health treatments are indicated for those who are unable to overcome the trauma without assistance,” he says. “Also, early intervention for trauma survivors should emphasize helping them to connect with natural social support networks and resources available, as this has been shown to reduce the likelihood of chronic PTSD and enhance post-disaster functioning.”
“Counseling and other appropriate mental health treatments are indicated for those who are unable to overcome the trauma without assistance,” he says. “Also, early intervention for trauma survivors should emphasize helping them to connect with natural social support networks and resources available, as this has been shown to reduce the likelihood of chronic PTSD and enhance post-disaster functioning.”
Webber agrees that disasters have a different set of rules. “It is easy to confuse disaster mental health and trauma therapy,” she says. “Psychological first aid in disaster mental health is very different in purpose and use than trauma treatment. We must not only be knowledgeable about both but also know what protocol to use and when.”
Reaching out
Recognizing traumatic stress symptoms and cultural factors associated with survivors is key to developing appropriate therapeutic interventions, according to Zalaquett. Techniques vary but can include challenging irrational beliefs, correcting distorted thoughts and biases, role-playing, systematic desensitization, exposure with response prevention, relaxation training and biofeedback. But most important, he says, are the goals of counseling.
But most important, he says, are the goals of counseling.
“The primary counseling goal is to establish rapport and provide a safe and culturally respectful environment for the survivor,” Zalaquett says. “As the survivor begins to talk about whatever he or she decides, the counselor should be prepared to ask questions to elicit deeper reflection. The counseling goal is to guide the process deeper to increase understanding of the client’s feelings. As long as the client does not become overwhelmed, continue to broaden the emotional and psychological scope of the session by allowing more difficult material to surface. In general, when uncertain about what an individual wants to talk about, the best approach is to ask and trust the client’s process.”
Webber agrees that establishing safety and stability for clients, not only in the therapeutic session but also in their lives, should be first and foremost for counselors. After that, Webber recommends a variety of helpful techniques:
- Use metaphors that can be seen, heard and felt to help clients become attuned to where distress is felt in their bodies, she says.
 For example, have the client visualize the trauma as a pressure cooker with the toggle shaking and ready to blow.
For example, have the client visualize the trauma as a pressure cooker with the toggle shaking and ready to blow. - Use grounding techniques to help clients stabilize. For example, Webber says, ask clients to name five non-distressing objects they can see, five non-distressing objects they can hear and five non-distressing objects they can touch. Integrate this exercise with deep breathing.
- Try multisensory materials in sand play, play therapy, drama and art therapy. “I find that sand play integrates touch, seeing, hearing, smelling and even tasting,” she says. “Choosing miniature figures and objects that appeal to you and creating a scene in the sand is very powerful.”
- Consider eye-movement desensitization and reprocessing therapy and brainspotting. “(A counselor) must have training, but I can’t imagine trauma treatment without these brain-based power therapies that reduce flashbacks and intrusive memories quickly,” Webber says.
- Use drama. “Psychodrama offers a kinesthetic multisensory modality for clients to express their feelings and act out their sensory traumatic memories,” Webber says.
 “It provides a way to talk about trauma and one’s reactions in a symbolic way that is not as fearful as traditional talk therapy.”
“It provides a way to talk about trauma and one’s reactions in a symbolic way that is not as fearful as traditional talk therapy.” - Have the client make a scene in the sand or draw a picture of something scary and then talk about feelings. “Then do whatever you want with the picture to get rid of the feelings,” she says.
One major difference in treating trauma as opposed to other issues is that the potential for primary or secondary traumatization and compassion fatigue in counselors is very high, Webber says. “Counselors’ greatest asset is our empathy. It is also our greatest liability. Counselors may show signs of traumatization, experience fear and pain and personal distress by their exposure to the client’s trauma story.” Counselors can combat compassion fatigue and traumatization in part by developing and following through with a self-care plan and by taking time for rest and relaxation, she says.
Treating trauma can also resurrect a counselor’s own traumatic experiences, Webber says.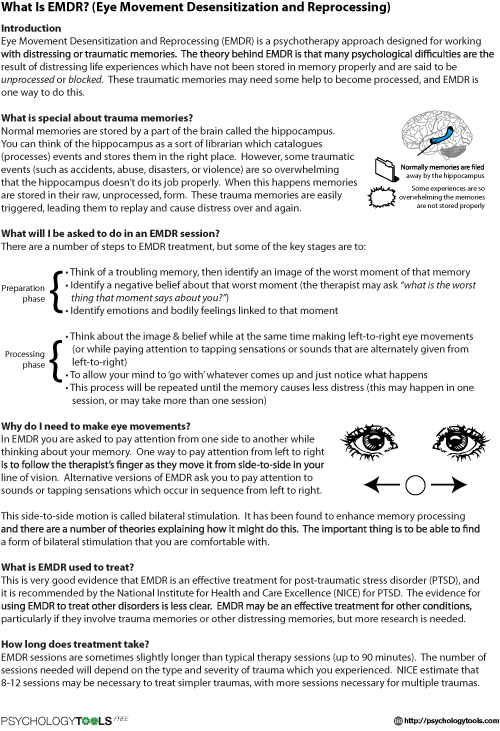 She recommends that counselors do their own trauma work with a trained therapist before working with others. If counselors are impaired or vulnerable, she adds, they should refrain from treating trauma clients.
She recommends that counselors do their own trauma work with a trained therapist before working with others. If counselors are impaired or vulnerable, she adds, they should refrain from treating trauma clients.
Those risks aside, through her years of treating trauma, Webber says her faith in humanity and in counselors’ ability to help has been strengthened. “Trauma is the ultimate existential challenge to continue living in spite of horrendous and unspeakable pain and sorrow. We are all in this world to help each other. Our greatest tool is our person, and our greatest gift is to walk with someone on his or her path to recovery.”
Helping the helpers
When it comes to the relationship between first responders and trauma, Brian Chopko says guilt plays a leading role. A counselor and assistant professor in the Department of Justice Studies at Kent State University at Stark, Chopko vividly recalls one client in her early 50s who responded to an emergency but ultimately couldn’t save the lives of two people. “She tried so hard to save them that she was almost killed herself,” says Chopko, explaining that the first responder sustained a serious injury during the rescue attempt. The woman then developed PTSD following the event.
“She tried so hard to save them that she was almost killed herself,” says Chopko, explaining that the first responder sustained a serious injury during the rescue attempt. The woman then developed PTSD following the event.
“One of her main complaints was guilt — guilt that she didn’t do enough to save these two people,” says Chopko, a former police officer and a current volunteer deputy sheriff. He asked the client to rate her guilt on a scale of 1 to 100, with 100 being the worst. “One hundred,” she responded.
Chopko used a variety of techniques, including prolonged exposure therapy, to help the first responder think differently about what had happened. What turned the tide for the client was an empty chair technique in which they addressed how the victims would feel about her rescue efforts and what they might say to her. “That was a breakthrough moment,” Chopko says. “She told me in the next session that that moment in therapy changed her life. It felt like 1,000 pounds off her shoulders.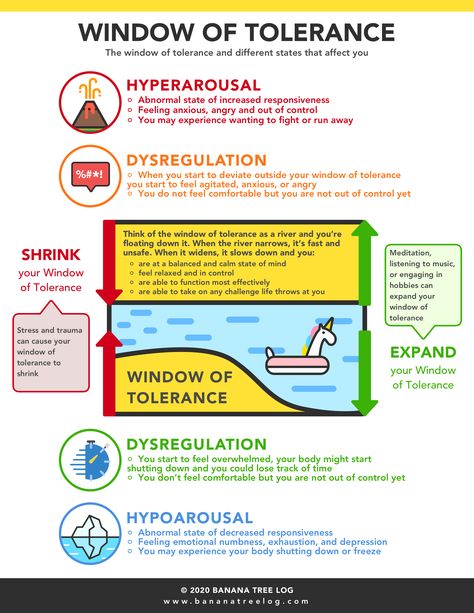 ”
”
People respond differently to trauma, Chopko says, so the crucial role of the counselor is to discover how a particular trauma has affected a particular client. People can go through the same event and have two totally different experiences, he says. After identifying the guilt from which his client was suffering, Chopko and the first responder were able to find success in treatment. After their work together, the client reported her guilt had dropped from 100 to a 2 or a 3.
While trauma affects people in different ways, Chopko says first responders undoubtedly deal with more than their fair share of it. Chopko, who teaches courses and does research on mental health issues in the criminal justice system, particularly post-traumatic stress experienced by first responders and victims of crime, recently conducted a study of 186 police officers throughout Ohio. He found that 17 percent of the officers were displaying probable PTSD symptoms. An additional 10 percent, while not meeting the criteria for PTSD, were displaying post-traumatic symptoms that were still considered significantly distressing. “More than a quarter of all police officers were currently experiencing significant or severe post-traumatic distress,” Chopko says. “Lifetime prevalence rates are much higher.”
“First responders commonly experience traumas as a routine part of their job,” Chopko says, including witnessing scenes of threatened or actual deaths or injuries from accidents, crimes, disasters, fires, suicides and hostage situations, to name a few. “In addition to viewing dead bodies and terrible injuries, first responders often have to put their hands on and handle the mangled and dead bodies,” he continues. “First responders are also often themselves put in life-threatening situations, such as the firefighters who run into a burning house to save others at great risk to themselves or the police officer who has a gun pointed at him, is involved in a shooting or is involved in a high-speed chase.”
Traumatized individuals are having a normal response to a very abnormal situation, Chopko explains. People who experience a traumatic event are expected to display post-traumatic symptoms and distress, he says. The variable is how long the symptoms and distress will last. For some, it is only a few days; for others, it may be a lifetime. First responders and others who have experienced trauma can get stuck in the fight-or-flight response, Chopko says. “This response helps you immediately survive the life-threatening event. Because the event is so overwhelming, however, the mind and body get stuck in that response. This is why people experience the hyperarousal symptoms — the mind is always waiting for that next terrible event to occur. The memories of the event never get sent into the long-term storage of memory.”
Chopko uses the analogy of a frozen computer. “If you type too many commands into a computer at once, what happens? The computer will freeze up and get stuck. The trauma is so overwhelming, the mind can’t process the horror of what occurred.”
Although survivors of trauma might not want to relive the experience and may avoid talking about it, that strategy won’t work over the long haul, according to Chopko.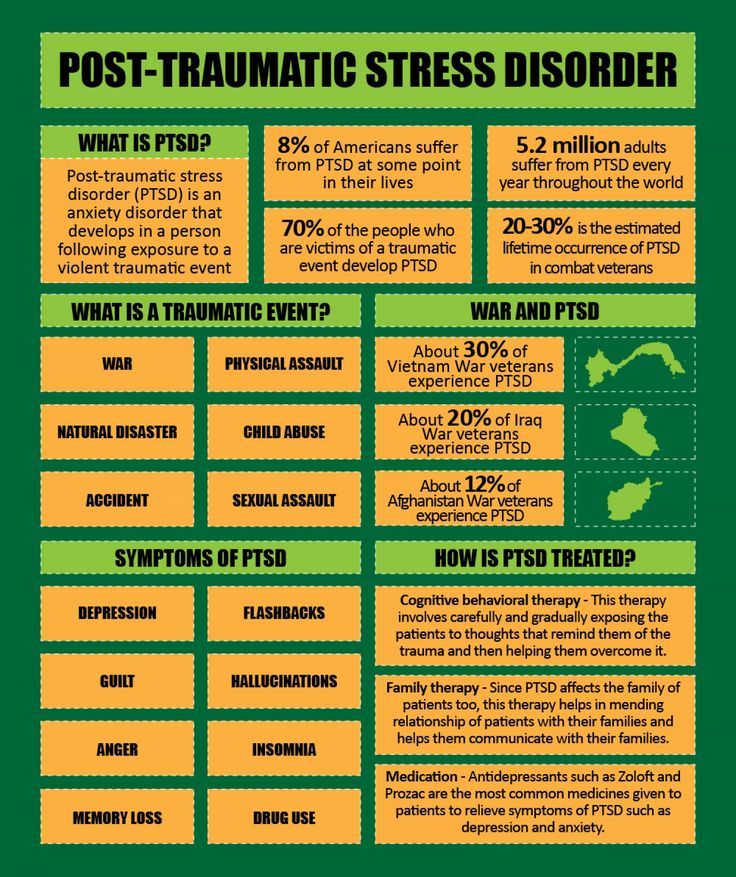 “People avoid thinking about the event because it produces more symptoms. In the short term, this strategy works by not inducing more severe symptoms. The problem is, this just reinforces your need to keep avoiding the memory to reduce symptoms, and this does not give the brain a chance to process the memory and put it into long-term storage. In the long term, avoidance has the paradoxical effect of making the symptoms worse.”
“People avoid thinking about the event because it produces more symptoms. In the short term, this strategy works by not inducing more severe symptoms. The problem is, this just reinforces your need to keep avoiding the memory to reduce symptoms, and this does not give the brain a chance to process the memory and put it into long-term storage. In the long term, avoidance has the paradoxical effect of making the symptoms worse.”
One of the biggest hurdles to helping first responders heal is the stigma attached to asking for assistance within the first responder community. “The work environment of first responders is one of a macho nature, where signs of weakness are undesirable,” Chopko says. “Many first responders feel highly uncomfortable seeking help because they don’t want to be viewed as weak by their peers and superiors and therefore suffer in silence.” The best way to address this barrier, he says, is to remind first responders of how normal their feelings are. “This is where normalizing is so important to convey that, ‘No, you are not weak or crazy. In fact, many of the other first responders are also experiencing similar reactions. They are just not talking about it.'”
In fact, many of the other first responders are also experiencing similar reactions. They are just not talking about it.'”
The good news, Chopko says, is that empirically validated treatments such as prolonged exposure therapy work well at reducing negative post-traumatic symptoms. “This type of therapy is sort of like going back and entering the commands into the computer one at a time so the computer can run smoothly without freezing.” In therapy, the client tells the story over and over again until the symptoms are reduced, resulting in the memory being processed and getting placed into long-term storage, he explains. “In this way, the opposite of avoidance is the key to recovery.”
One intervention developed specifically to help first responders is Critical Incident Stress Debriefing (CISD). With this model, all first responders involved in the traumatic event are brought together afterward to debrief. Although research has not been consistent in showing that CISD is successful in preventing future symptoms, Chopko says it offers counselors a chance to get their foot in the door with first responders.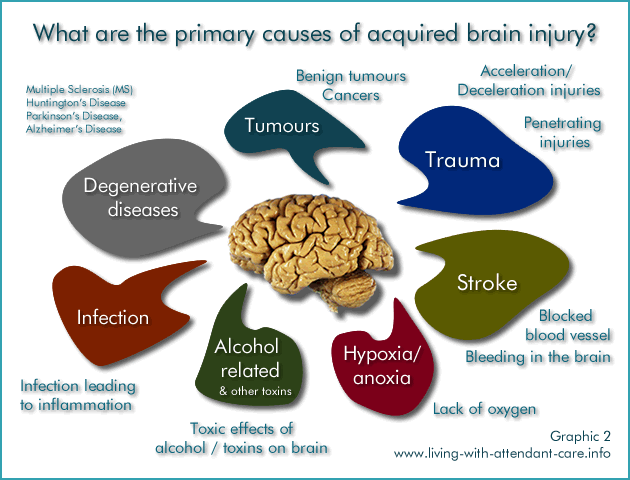 Mental health facilitators can lead the debriefings, emphasize to first responders that what they are feeling is normal and then offer them resources for additional help, he says.
Mental health facilitators can lead the debriefings, emphasize to first responders that what they are feeling is normal and then offer them resources for additional help, he says.
Another way for counselors to reach this population is to get involved in programs that train first responders in mental health issues or crisis intervention. If a counselor presents the training, he or she might be able to provide an additional training segment on post-traumatic stress, Chopko says, thus beginning the normalizing process for first responders.
Most people experience only one or two traumatic events in their lifetime. The challenge for first responders, Chopko says, is the sheer number and wide range of traumas they will experience, with a cumulative effect taking place over the years. While it is very difficult for first responders to avoid that circumstance completely, Chopko says, counselors can teach them healthy behaviors for dealing with ongoing stress, including relaxation techniques, breathing exercises and physical exercise.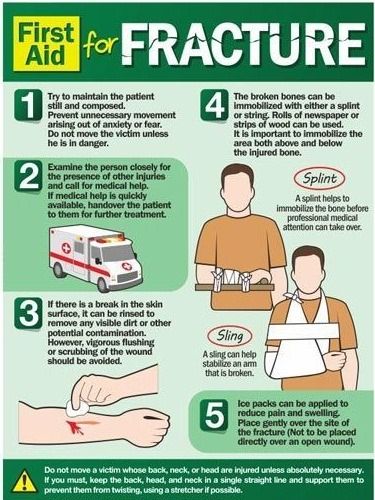 Counselors should emphasize to first responders the importance of practicing those techniques throughout their careers, not just in moments of crisis, Chopko says.
Counselors should emphasize to first responders the importance of practicing those techniques throughout their careers, not just in moments of crisis, Chopko says.
Trauma on the battlefield
With simultaneous combat zones in Afghanistan and Iraq, there is no shortage of soldiers who have endured traumatic experiences. Trauma can appear at a soldier’s every turn, says David Fenell, professor and chair of the Department of Counseling and Human Services at the University of Colorado at Colorado Springs. Among the examples are repeated exposure to life-threatening combat, witnessing the death or wounding of a comrade, an attack by an improvised explosive device or being assigned to duty in which the soldier is responsible for assisting the wounded.
A retired colonel in the U.S. Army Reserve Medical Service Corps, Fenell deployed to both Iraq and Afghanistan to provide mental health services. One of the most important tasks for counselors treating veterans is to think of the trauma as an opportunity for the client to grow and develop, says Fenell, a member of ACA. “This positive view will be very helpful to the client. I frame the symptoms as normal reaction to abnormal circumstance and avoid pathologizing the client. Too many counselors conceptualize normal stress reactions to threatening situations as PTSD. This is a mistake.”
“This positive view will be very helpful to the client. I frame the symptoms as normal reaction to abnormal circumstance and avoid pathologizing the client. Too many counselors conceptualize normal stress reactions to threatening situations as PTSD. This is a mistake.”
Fenell believes ordinary stress reactions are being misdiagnosed as PTSD among military personnel, which can have a detrimental effect. “The mainstream press has made a huge issue of the mental health concerns of returning warriors,” says Fenell, who served as chair of ACA’s Special Committee on Military and Veterans Affairs. “The military has responded and, in some ways, (that led) to the diagnosis of choice being PTSD, with traumatic brain injury a close second.” Treatment through the Department of Veterans Affairs becomes easier to obtain when the PTSD diagnosis is given, he says, but the diagnosis isn’t always a good thing. “When people are treated as if they are dysfunctional, they become dysfunctional. When people are treated as normal people in the process of getting better, they are more likely to get better. ”
”
That said, Fenell emphasizes that he does not disregard the diagnosis of PTSD. “PTSD is real and can be devastating to those who experience it and those who are close to them,” he says. “If my positive strength-based approach is not effective, I can move to more traditional approaches or refer.”
Fenell says the sooner trauma therapy can begin, the better — as long as the client is able to begin reprocessing the events and the feelings associated with them. “Again, I reassure the client that he or she is experiencing normal reactions to abnormal circumstance and that we will get through this confusing time together. It is a health-based, rather than pathology-based, way of working with the client.”
Fenell offers a few tips for working with members of the military affected by trauma:
- Establish a relationship based on trust. “My military background is invaluable in this regard with combat veterans and their families,” Fenell says.
- Normalize the symptoms.

- Engender hope. “This is crucial,” he says. “Too many civilian therapists communicate pessimism to clients nonverbally when dealing with combat trauma.”
- Ensure that the client accepts and begins to believe that he or she will improve with time and supportive therapy.
- Engage the family in treatment. “The family often begins acting differently around the traumatized client, and this typically makes the client feel worse rather than better,” Fenell says. “Get the family on board and in treatment with the client so that all are emphasizing a strength-based, ‘this will get better’ mind-set.” It’s also helpful to collaborate with the client’s military unit so that it will be positively involved as well, he says.
The greatest challenge for counselors, Fenell says, is being comfortable with the client’s tragic experiences while still expressing empathy and engendering hope. Counselors should be psychologically healthy and well grounded and able to enter the world of the client without being overwhelmed by it, he says.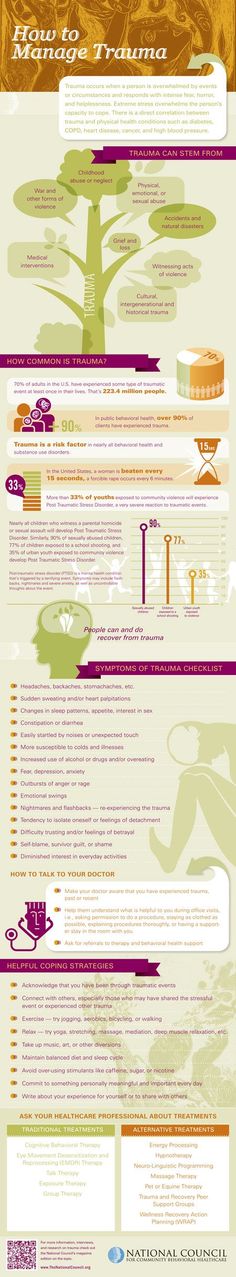 “Psychological health, personal resiliency and lots of experience help.”
“Psychological health, personal resiliency and lots of experience help.”
But, he cautions counselors, don’t become immune to your own feelings. “The counselor must be able to express accurate empathy without becoming so overinvolved that therapeutic perspective is lost. Losing perspective and feeling too much, or becoming detached and not feeling at all, can happen to some therapists when dealing with the pain associated with trauma cases over a long period of time.”
A less safe place
One of the things that makes a traumatic event such as the school shootings at Columbine or Virginia Tech so hard to handle is that violence has invaded a safe place, Webber says. “Schools are safe places, homes away from home, full of fun, football pep rallies and friends. It is unimaginable that kids and teachers could be killed in their school. More unbelievable and terrifying is that at Columbine and other schools, they were killed by students.”
In the microcosm of a K-12 school community, traumatic events can take different paths based on who is affected and how many students are affected, says J.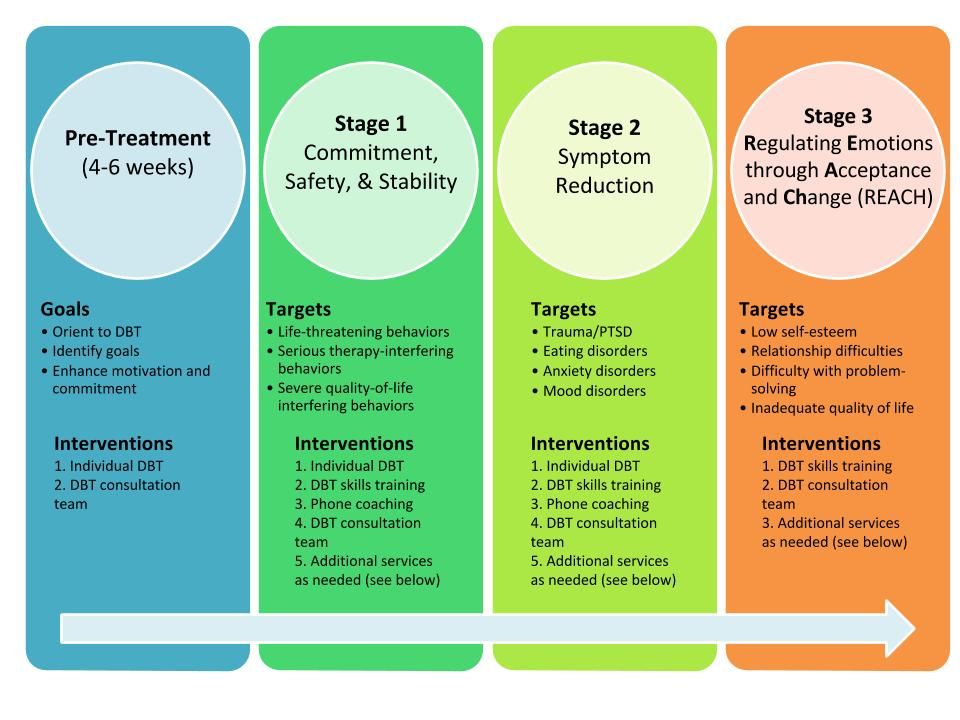 Barry Mascari, assistant professor and chair of the Counselor Education Department at Kean University in New Jersey. “Too often, schools treat everyone as if they are impacted to the same degree and inadvertently bring more students into the complex mix than is necessary,” he says.
Barry Mascari, assistant professor and chair of the Counselor Education Department at Kean University in New Jersey. “Too often, schools treat everyone as if they are impacted to the same degree and inadvertently bring more students into the complex mix than is necessary,” he says.
“Many students may not know the victim and would not have any impact but feel guilty or think they should be more upset. This needs to be normalized,” Mascari says. “The small minority that is impacted also needs some triaging, because some simply need psychological first aid to help them normalize what they are thinking and feeling. Others may need more direct follow-up because of the closeness to the event or previous trauma. School counselors are in a unique and critical position to help students weather these events and are especially critical in helping administrators manage these crises.”
Recently, federal and state governments have begun mandating response plans, and school counselors should play an important role in developing those plans, Mascari says. “When I directed the plans for a large city school district, we did everything from sharing building plans to meeting with the counselors so they understood their role in the response plan. Our school counselors played a critical role in initiating a response.”
“When I directed the plans for a large city school district, we did everything from sharing building plans to meeting with the counselors so they understood their role in the response plan. Our school counselors played a critical role in initiating a response.”
Webber says returning to routine — reopening school and restarting classes — as soon as possible is important. Sharing should be encouraged in classes rather than large assemblies, she adds, because counselors and teachers can more readily identify those who might need additional support in smaller settings.
At a university, where there is less structure and containment, it is more difficult to provide immediate support and contact from teachers and counselors, Webber says. Drop-in centers in dorm lounges, dining rooms and other areas can help to decentralize response efforts.
At schools and universities alike, Webber reminds counselors their role is also one of prevention. “National Suicide Awareness Week is one example,” she says. “After students complete brief surveys, counselors follow up with students whose survey results suggest that they may be at risk.”
“After students complete brief surveys, counselors follow up with students whose survey results suggest that they may be at risk.”
After disasters strike
From the recent earthquakes in Haiti and Chile to the 2004 Indian Ocean tsunami to the domestic devastation of Hurricane Katrina, natural disasters can strike quickly, but their impact is often enduring, altering the lives of large groups of people. While those who have lost homes and loved ones are most affected, those trying to help can be greatly impacted as well.
The most significant challenge for disaster responders is secondary traumatic stress, says Cirecie West-Olatunji, an associate professor of counselor education and coordinator of the mental health track at the University of Florida. Responders may begin to experience symptoms similar to those exhibited by the disaster survivors, she notes. “This is why self-care is an important part of disaster training,” says West-Olatunji, an ACA member who participated in a recent ACA podcast on the earthquake in Haiti. “Disaster mental health counselors who do not know their limitations and do not have a plan for resilience during service provision can become liabilities during deployment.”
“Disaster mental health counselors who do not know their limitations and do not have a plan for resilience during service provision can become liabilities during deployment.”
The second most significant challenge is cultural competence, says West-Olatunji, who represents the Association for Multicultural Counseling and Development on the ACA Governing Council. “Given the rise in disasters globally, counselors are likely to be deployed to geographic areas where the cultural mores differ from their own. Thus, they need to exemplify cultural competence that reflects responsiveness and expediency in service provision.”
In the aftermath of Hurricane Katrina, many mental health professionals were sent to the Gulf Coast to help, but some were asked to return home because of a lack of cultural competence, West-Olatunji says. “When counselors lack cultural competence when responding to disasters, they can sometimes aggravate existing symptoms. Culturally competent mental health disaster counselors are able to identify community strengths and mechanisms for healing. They are also able to incorporate community knowledge into their work and expediently apply that knowledge in their interventions.”
They are also able to incorporate community knowledge into their work and expediently apply that knowledge in their interventions.”
West-Olatunji, who lived in New Orleans for 14 years and raised her children there, recalls an experience in the aftermath of Hurricane Katrina in which her knowledge of the people and community became a lifeline. She was working with first responders from the area and their families, who were living temporarily in intact communities aboard cruise ships off the coast of New Orleans. While she was there, people were beginning to move off the ships and into trailers, but many were very resistant to the idea.
Tasked with providing communitywide intervention, West-Olatunji knew from past experience that the people of New Orleans were social. She wanted to get them more comfortable with the idea of moving into the trailers, so instead of sitting inside one of the models and waiting for people to come in and ask questions, she took a chair and sat outside. She spoke to people passing by as if she were sitting on her front porch, and then she’d invite them in. As they sat inside the trailer with her, West-Olatunji remembers, they could see it wasn’t so bad. “That’s an example of using knowledge of the community … as a vehicle to get them where I want them to be,” she says.
She spoke to people passing by as if she were sitting on her front porch, and then she’d invite them in. As they sat inside the trailer with her, West-Olatunji remembers, they could see it wasn’t so bad. “That’s an example of using knowledge of the community … as a vehicle to get them where I want them to be,” she says.
Cultural competence is also important in working through the aftermath of a disaster with clients one-on-one, she says. “It is important for counselors to honor the ways in which individuals are coping with their trauma and to acknowledge ways in which they define healing. Counselors often want to bring their own concepts of healing to trauma-affected communities, leaving out the idea that counselors can effectively co-construct solutions with their clients.”
Cultural sensitivity is especially important when it comes to religious beliefs, Zalaquett adds. “Clients’ religious interpretations of their ordeals may conflict with the counselor’s interpretation of the situation,” he says. “Nonetheless, we should not challenge clients’ deep religious beliefs. Helping victims process feelings of guilt and responsibility is one way in which we could serve them better.”
“Nonetheless, we should not challenge clients’ deep religious beliefs. Helping victims process feelings of guilt and responsibility is one way in which we could serve them better.”
Following the American Red Cross disaster mental health model means the bulk of mental health services are provided only after first responders have addressed more immediate needs, West-Olatunji says. At that point, counselors should look to the most resilient community members. “Counselors can assist by working with the less vulnerable individuals first to help stabilize the community and utilize the most resilient individuals in restoring normalcy to the community,” she says. “Further, disaster mental health counselors can serve as consultants to civil employees, educators and religious and community leaders in providing information on mental health recovery. Oftentimes, individuals will seek assistance from leaders in their own communities before approaching mental health professionals.”
Disaster counseling is very brief in nature, West-Olatunji says, with most sessions conducted in field-based settings.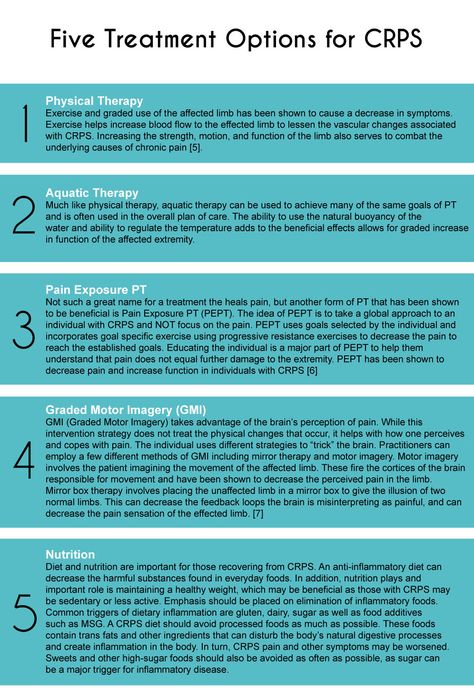 “Any individuals who require more conventional services are referred to existing services in the community,” she says. Another way for counselors to help in the aftermath of a disaster is by providing services to first responders, who are particularly vulnerable to secondary traumatic stress. Counselors from farther away can pitch in by providing assistance to counselors in the affected area, West-Olatunji says. “The most valuable support can be in the form of outreach trips with advanced counseling students, practitioners and counselor educators to provide relief, consultation and training to the affected community of counselors.”
“Any individuals who require more conventional services are referred to existing services in the community,” she says. Another way for counselors to help in the aftermath of a disaster is by providing services to first responders, who are particularly vulnerable to secondary traumatic stress. Counselors from farther away can pitch in by providing assistance to counselors in the affected area, West-Olatunji says. “The most valuable support can be in the form of outreach trips with advanced counseling students, practitioners and counselor educators to provide relief, consultation and training to the affected community of counselors.”
When one works with adults affected by a disaster, West-Olatunji says restoring regularity in their daily activities is important. “This intervention aids in the recovery process in that it reestablishes some predictability to their lives. An example would be attempting to eat meals at prescribed intervals on a daily basis or going to bed at the same time each evening.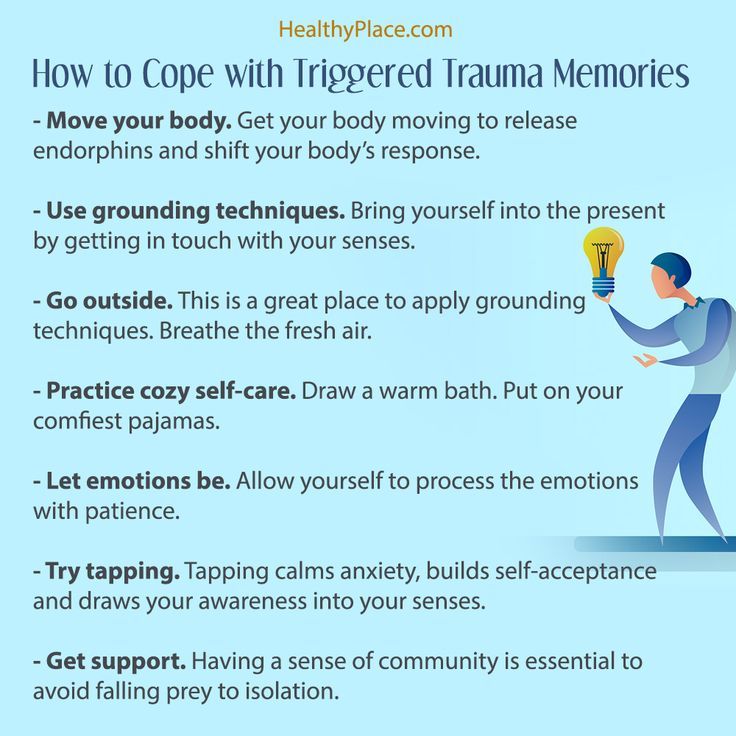 Ritualizing the daily routine is helpful in restoring a sense of safety and grounding individuals in reality.” She adds that encouraging clients to engage in reflective or meditative activities can also be helpful, as can participating in communitywide or family rituals to aid the grieving process.
Ritualizing the daily routine is helpful in restoring a sense of safety and grounding individuals in reality.” She adds that encouraging clients to engage in reflective or meditative activities can also be helpful, as can participating in communitywide or family rituals to aid the grieving process.
When it comes to children, West-Olatunji says it’s important to allow them to tell their stories about the disaster. “Some common interventions with children involve the creative arts,” she says. “Asking children to draw their stories can be a powerful tool that allows them to have a voice and also serves as a platform for therapeutic activity. Other pediatric counseling techniques include working with sand trays, dramatic play, Popsicle stick doll construction, the use of proverbs and mutual storytelling.”
While disasters bring death, destruction and heartache, West-Olatunji says the greatest lesson she has learned about trauma is an optimistic one. “People are much more resilient and psychologically hearty than I imagined. They have taught me a lot about the capacity of the human spirit.”
They have taught me a lot about the capacity of the human spirit.”
ACA Resources
- Terrorism, Trauma and Tragedies: A Counselor’s Guide to Preparing and Responding, third edition (order #72892), can be ordered directly through the ACA online bookstore at counseling.org/publications or by calling 800.422.2648 ext. 222. The cost is $29.95 for ACA members and $39.95 for nonmembers. The book, edited by Jane Webber and J. Barry Mascari, features chapters written by Webber, Mascari, Carlos Zalaquett and David Fenell, among many others.
- Disaster Mental Health and Crisis Stabilization for Children (order #78205), a live demonstration DVD presented by Jennifer Baggerly and produced by Microtraining and Multicultural Development, may also be ordered directly through ACA. The cost is $149.
- ACA also offers a Traumatology Interest Network so counselors can share experiences, ask questions and offer tips and techniques for treating trauma. For more information, contact the interest network’s facilitator, Karin Jordan, who has been working in Haiti, at kj25@uakron.
 edu, or Holly Clubb of ACA at [email protected].
edu, or Holly Clubb of ACA at [email protected].
****
Letters to the editor: [email protected]
PTSD, Childhood Trauma, and More
Trauma can affect all areas of your life — but healing is possible. Therapies optimized for trauma can be especially helpful.
Traumatic experiences can leave a deep imprint on the body and mind. The impact may show up immediately or years later, affecting your mood, relationships, and even your sense of self. But there are effective treatments to help you heal from trauma.
Around 70% of adults in the United States have experienced at least one trauma in their lives. Not everyone will have lasting effects, but 6% of U.S. adults develop post-traumatic stress disorder (PTSD).
Trauma can change your brain and nervous system, leading to dysregulation and symptoms such as depression and anxiety. As such, trauma therapies focus on soothing the nervous system, integrating traumatic memories, and supporting both mind and body healing.
There’s no one-size-fits-all when it comes to trauma treatment — the “best” type is the one that works for you. Finding the right therapy can take some time, but support is available along the way.
Trauma can come after a one-off event, such as an accident or assault, or from repeated events, like an abusive relationship or childhood neglect. Complex trauma — the kind that arises from repeated events — often stems from childhood experiences that affect your adult life.
Therapy can help you integrate traumatic event(s) and understand them — which helps you begin the healing process. Your memories of the trauma will stay, but they’ll start to have less power over you and your emotions.
“Therapy is helpful in normalizing an individual’s responses to the trauma they experienced,” explains Lisa Curtis, a licensed clinical social worker in New York. “[It] can provide them with new skills to manage their feelings and responses while also providing a context and education around the event itself. ”
”
There are many evidence-based practices (EBPs) for trauma and PTSD, which are interventions that have proven robust in working with targeted populations, though not all recommended therapies are EBPs.
Types of therapy for PTSD and trauma include:
Cognitive processing therapy (CPT) was developed by Patricia Resick, PhD, ABPP, as a treatment for PTSD. It aims to help people who feel “stuck” by their thoughts about the trauma.
In CPT, your therapist will help you learn to challenge and change unhelpful beliefs about the trauma that are keeping you “stuck.” The aim is to help you understand and think differently about the event(s), thereby relieving the negative effects.
A 2018 review concluded that, based on existing evidence, CPT is “an effective PTSD treatment with lasting benefits across a range of outcomes.”
According to the American Psychological Association (APA), this therapy is strongly recommended for PTSD.
Prolonged exposure (PE) is a behavioral treatment for PTSD that, as the name suggests, involves confronting the source of your fear to reduce anxiety around it.
Avoidance is a prominent symptom of post-traumatic stress. PE therapy aims to help you overcome avoidance that developed after your trauma.
During therapy, you’ll learn to control your breathing, talk about your trauma, and gently confront your fear in the real world. For example, someone who lived through sexual assault might go back to the location where it occurred to help them realize that the trauma is no longer happening and that they are now safe.
“The more we avoid the feelings, thoughts, sensations, memories, and images that are connected to our trauma, the worse the symptoms of trauma become,” explains Avigail Lev, PsyD, a licensed clinical behavioral therapist, author, and director of the Bay Area CBT Center in California.
“So the most important part of treating trauma is exposing individuals to the feelings, thoughts, sensations, memories, places, and images connected to their trauma [because] this aids in the process of desensitization.”
According to the APA, PE therapy is strongly recommended for PTSD.
Trauma-focused CBT (TF-CBT) therapy is a cognitive behavioral treatment mainly used for kids and teens with trauma.
TF-CBT’s goal is to help children recognize false beliefs (such as who to blame for abuse), correct unhealthy behavior patterns, and develop new ways to cope, such as self-soothing and expressing their emotions. Parents or caregivers are also involved in this approach.
A 2014 review concluded that TF-CBT could effectively reduce symptoms of PTSD in some children, and the APA strongly recommends forms of CBT for treating PTSD.
Eye Movement Desensitization and Reprocessing (EMDR) is a trauma therapy developed by psychologist Dr. Francine Shapiro in 1987. The therapy is unusual in that it doesn’t involve much talking — it aims to help you process and release traumatic memories through eye movements.
In an EMDR session, your therapist will ask you to hold a specific aspect of a traumatic event in mind while you focus on their hand moving back and forth (or, sometimes, rhythmic tapping).
The aim is to help your brain “reprocess” the memory — which wasn’t fully processed at the time due to overwhelming stress — by engaging both sides of your brain (known as bilateral stimulation).
This reprocessing aims to release the memories, ultimately relieving nightmares, flashbacks, and triggers.
For some people, EMDR may yield results faster than other forms of therapy, such as talk therapy.
A 2014 study by Shapiro found that 80% to 90% of people saw results within the first 3 sessions, while a 2017 review found it to be just as effective as cognitive behavioral therapy (CBT).
Note that EMDR appears to work best for single-event trauma, and it may not be as effective for complex trauma or complex PTSD.
According to the APA, EMDR therapy is a conditionally recommended treatment for PTSD.
Traumatic memories are held in the body as well as the mind. Somatic therapy focuses on how your emotions can physically impact the body. These emotions can resurface suddenly if you encounter a trigger or something that reminds you of a trauma.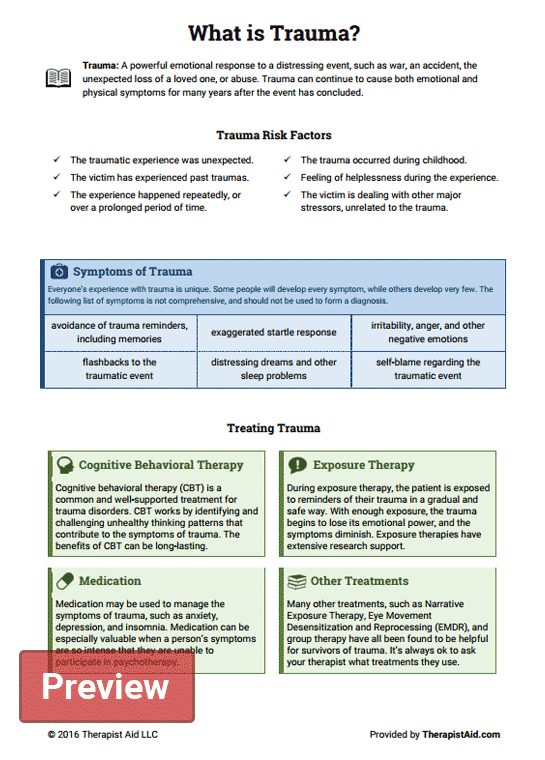
Somatic therapy aims to “release” pent-up trauma to relieve mental health symptoms and chronic pain, using methods such as developing body awareness and grounding in your body.
A 2017 study found that somatic experiencing — talking through past traumas while exploring the body’s physical responses and sensations — was an effective treatment for PTSD.
In psychodynamic therapy, your therapist will help you understand how your past has affected your current emotions, behaviors, and relationship patterns.
The aim is to help you understand the unconscious motives that drive your behavior.
Your therapist may help you understand how early childhood experiences, family dynamics, and current relationships — which may be shaped by trauma — affect your current coping methods and beliefs about the world.
According to a 2008 review, psychodynamic approaches in trauma therapy can lead to:
- improved self-esteem
- using more helpful coping methods, and fewer unhelpful coping methods
- improved relationships
- better social functioning
The authors note that psychodynamic approaches may be especially helpful in treating complex PTSD.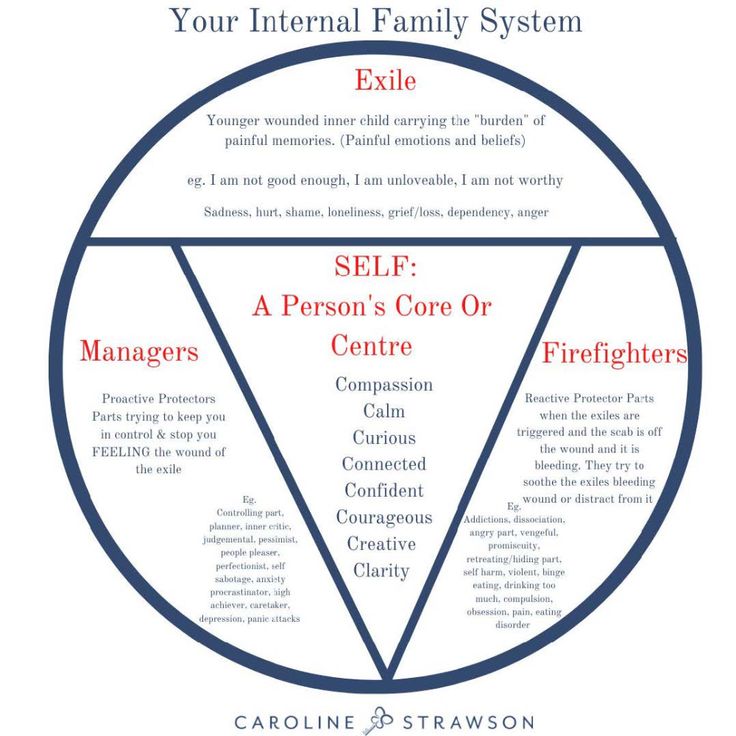
While the therapy techniques above have received the most research attention, trauma therapists may also draw on other therapeutic methods.
Additional therapies and techniques that can help you heal from trauma include:
Accelerated resolution therapy
The Substance Abuse and Mental Health Services Administration (SAMHSA) recognized accelerated resolution therapy (ART) as an evidence-based treatment for trauma-related disorders in 2015.
The technique aims to help you find relief from trauma faster than other treatments for PTSD by helping you “reprogram” how your brain stores your traumatic memories in one to three sessions. ART builds on other techniques, such as EMDR.
Hypnotherapy
Hypnotherapy is a popular alternative for people who have struggled with other therapy types, like EMDR or CPT.
In hypnotherapy, a therapist places you into a trance-like stance, where you’re awake and aware but relaxed and able to shut out distractions. Then, they work to reduce the emotion attached to the event.
“It can help release the emotional grip of trauma as it brings the subconscious fears, thoughts, and experiences to a conscious level,” explains Maria Micha, psychotherapist and clinical mental health counselor.
“Humans can’t access their subconscious mind and alter the terror that is ‘tattooed’ on that level. Techniques such as hypnotherapy can help release and replace the traumatic experience with functional thinking and mental patterns,” she adds.
A 2013 review suggests that hypnotherapy could help reduce PTSD symptoms.
Narrative therapy
Narrative therapy is a newer treatment approach in which your therapist will help you “re-author” your story to give your experiences meaning and shape how you see yourself and the world you live in.
This technique could help with various mental health issues. It can help you challenge beliefs you hold about yourself following trauma, such as feeling “broken” or powerless to change your circumstances.
For example, says Micha, “I ask my clients to rewrite their narrative of the traumatic event until the trauma has no emotional hold on them.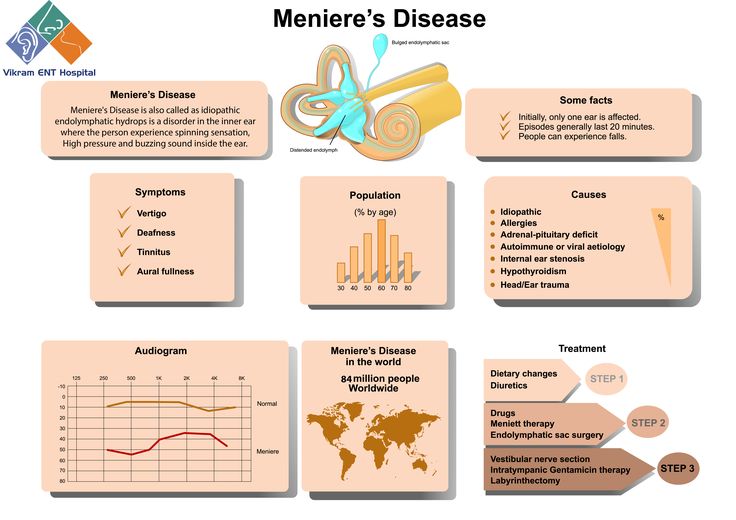 ”
”
According to the APA, narrative therapy is a conditionally recommended treatment for PTSD.
Internal family systems therapy
Internal family systems (IFS) is a type of talk therapy developed by therapist and academic Richard Schwartz, PhD.
The theory holds that your personality comprises different “parts,” each with its characteristics. All parts are held by the “Self,” or your core consciousness. So, like a family has different members, your personality has different parts, too, and all of them want what’s best for the self.
Your therapist will help you get to know your different parts during sessions. Some parts may be more affected by trauma than others. The aim is to understand why some parts are hurting and learn how to help them with compassion rather than ignore or exile them.
Art and music therapy
Art therapy can help boost mental health and support healing from trauma. It can take many forms, including dance, drama, music, writing, and creative art.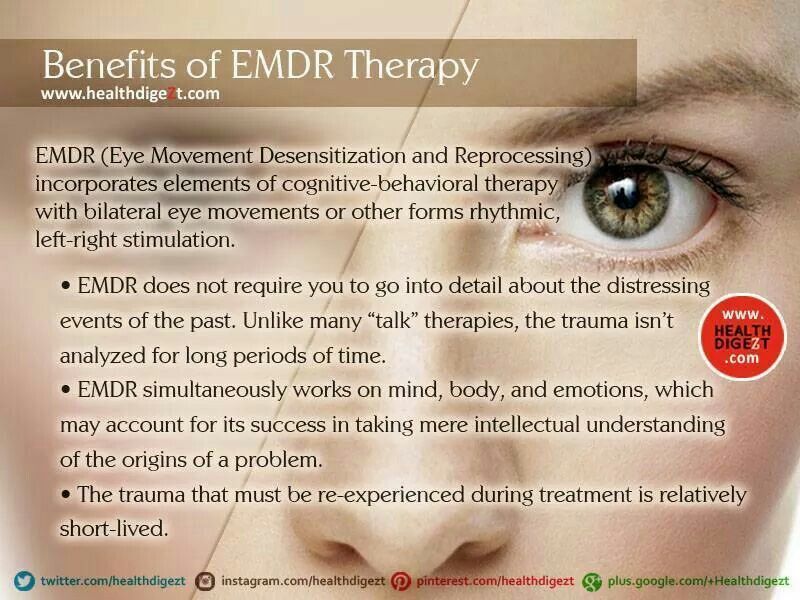
“I find art therapy very helpful in trauma therapy as the subconscious mind will often reveal the fearful patterns effortlessly,” explains Micha. “Clients are often surprised with the drawings they produce, as art will reveal suppressed subconscious emotions and fears.”
Music therapy, meanwhile, can focus on helping people ground themselves by writing songs or compositions to create affirmations and regulate their thoughts or emotions.
“Musical improvisation can help clients nonverbally explore traumatic experiences as the speech center of the brain can shut down during a traumatic flashback,” explains Kyle Fleming, a board certified music therapist and founder of a mental health practice in Illinois devoted to this type of therapy.
Inner child work
Also known as inner child healing, inner child work is a therapy that may help you heal from childhood trauma. For example, Micha usually uses it toward the end of trauma therapy with a client.
It involves “getting in touch” with your inner child to feel how you felt at various ages and working to heal your inner child’s wounds by creating the safe, secure inner and outer environments you needed as a child.
“It can help people overcome any feelings of guilt or shame they may be holding onto from childhood,” explains Jessica Pedersen, a licensed and certified clinical hypnotherapist.
Trauma systems therapy
Like trauma-focused CBT, trauma systems therapy (TST) is designed for children, adolescents, and teens.
This therapy emphasizes the person’s emotions and actions. It also considers the role that a threatening social environment or system of care can play in keeping a young person in a dysregulated state.
Most therapists will use various techniques to treat patients’ traumas rather than only one modality. And the methods they use often depend on what works for you.
“A great deal of [therapy intervention] success depends on the belief system of the clients and how ready they are for such interventions,” explains Curtis. “If a client is resistant or apprehensive about an approach, it could do more harm than good to insist on a particular technique.”
It’s also important to remember that a big part of therapy is your relationship with your therapist.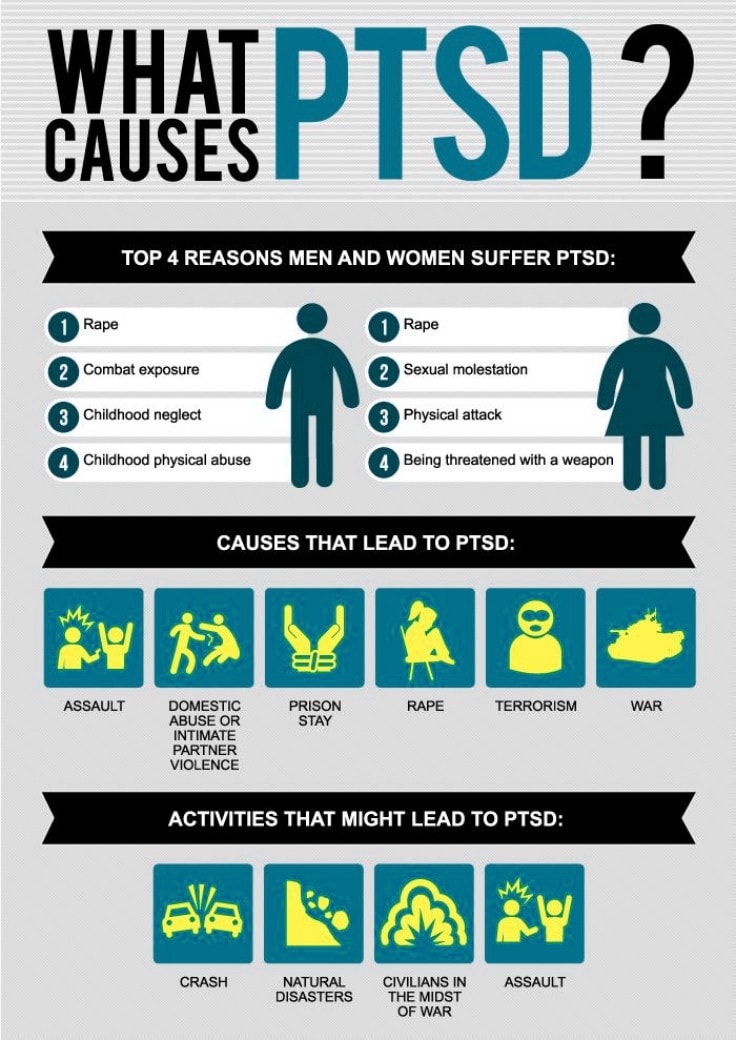 In the end, it’s essential that you feel safe with your therapist.
In the end, it’s essential that you feel safe with your therapist.
“Ask questions about the therapists’ experience, approach, and training,” Fleming recommends, “and if something feels ‘off,’ feel free to find a new therapist. It does you no good to stick with the first therapist you meet if you feel uncomfortable with them or their approach.”
There’s always another therapist who’s willing to try other techniques that feel more comfortable for you. If you need help finding one, you can check out Psych Central’s Find a Therapist resource page.
Treatment of mental trauma - how does it work?
What leads a person to psychotherapy? Most often, mental trauma, internal pain, often long for almost the entire conscious life. And a lack of understanding of what to do in order to change the situation and become happier.
The task of therapy in most cases is the treatment of psychotrauma.
What is mental trauma? It occurs when Parents often see the goal of nurturing decent behavior while ignoring the child's signals about what a unique new human being needs to come into the world.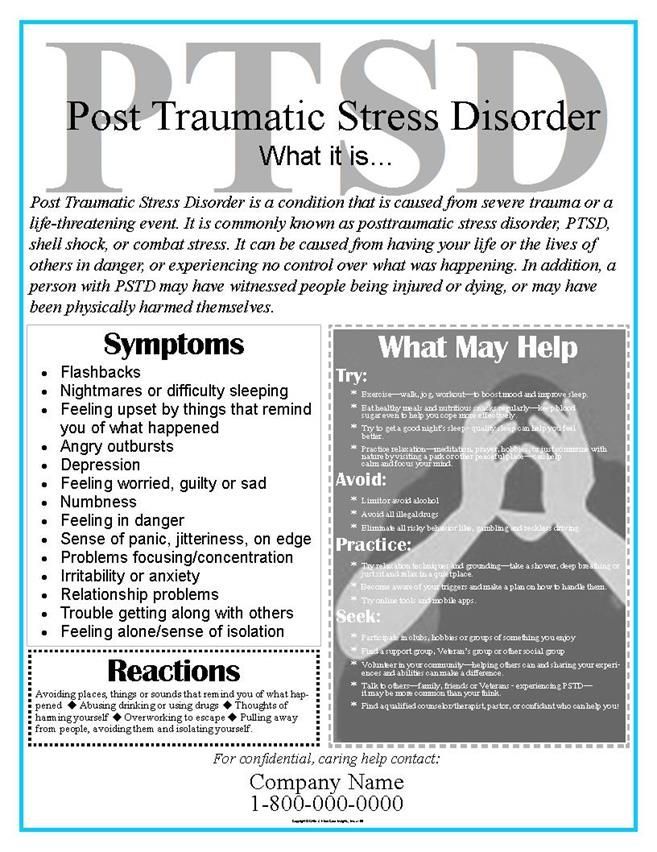 As a result, a person cannot understand himself, hear himself and respond to himself. This is especially true for people who have suffered physical violence or its threat - in order to somehow survive in a situation of violence or emotional deprivation, the child is fenced off from his emotions. nine0003
As a result, a person cannot understand himself, hear himself and respond to himself. This is especially true for people who have suffered physical violence or its threat - in order to somehow survive in a situation of violence or emotional deprivation, the child is fenced off from his emotions. nine0003
How does the treatment work? The therapist meets the person. Without criticism, reproaches, teachings. Asking him again, listening, clarifying. Involving in habitual patterns of relationships for the client. And sensitively perceiving what it is, who it is, what it is about.
The client comes to therapy primarily for himself, because for long years of his life he did not understand himself and expressed himself.
With the help of the therapist, the client learns to recognize his deep-seated feelings and the ways in which he is accustomed to interacting with people, as he interacts with the therapist now. When treating trauma, the main thing is awareness of the feelings and strategies of your Child. nine0003
nine0003
The psychotherapist touches the traumatized soul so that it stops hurting.
To do this, the therapist does what the educators and teachers did not do. Whatever happens in the therapeutic relationship, the therapist stands by the patient, listens to what is happening with the client, and understands what internal suffering and contradictions make the client behave in this way, and sometimes cause pain to others. The therapist shares with the client his suffering. It is a strong union with the therapist that allows the client to live the unhealed psychological trauma in a different way. The therapist helps the client to realize that he has - and had, the right to honor and dignity, that he has the right to feel any emotions. And that then - in his distant childhood - he had the right to care, response, love of his parents. That his state of abandonment is unnatural for human existence. nine0003
The client begins to hear himself, he hears the suffering of a small child in himself, who has been abandoned to us for many years.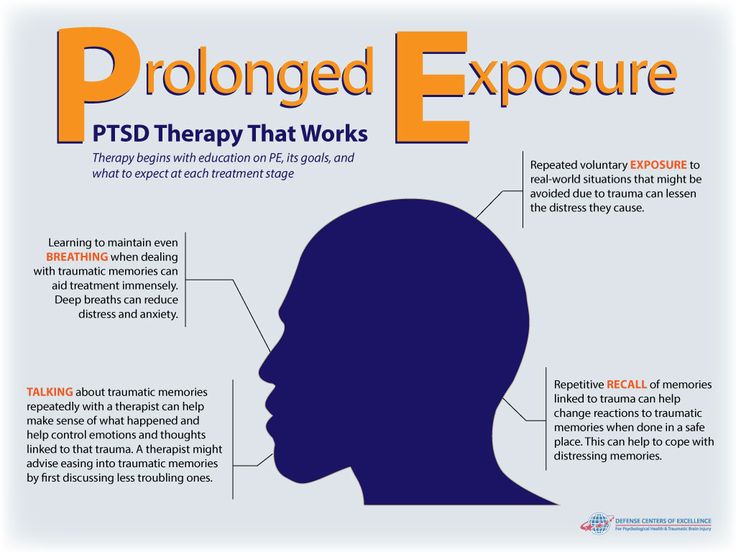
And now he can feel his pain without repressing or denying it yet. In the course of the therapeutic relationship, he learns to respond to himself.
Gradually, the client begins to realize that he is the same adult who is now next to this suffering child. And now he is responsible for his fate. nine0003
Now - 30, 40, 50 years later - next to that traumatized little child - there is a caring and sensitive adult.
Man has learned to respond to himself. And it reduces pain. The pits are overgrown with young grass. Don't believe? Get through it.
Three Psychological Techniques for Healing Childhood Trauma
Psychotherapists often talk about how important it is for the patient to get in touch with their “wounded inner child” in order to heal psychic trauma. By this child they mean all the psychological and emotional baggage left from childhood and continuing to create problems in adulthood. nine0003
The term "inner child" gained popularity thanks to self-help authors, most notably John Bradshaw and his bestselling book Coming Home.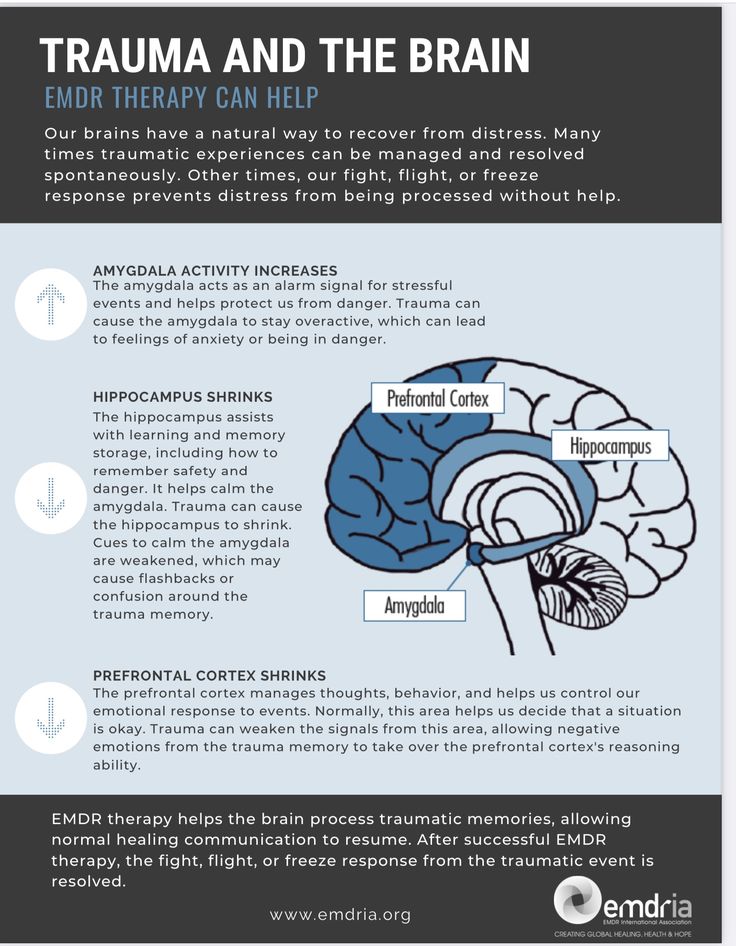
The archetype of the “wounded child” usually manifests itself in the following way: in the life of an adult, the same negative experiences and manifestations of inadequate behavior are repeated again and again, which he adopted in childhood, looking at others.
For example, if a girl in her childhood regularly observed how her father abused her mother, then in adulthood she may constantly enter into relationships with abusive men. nine0003
Addictions and mental health problems rooted in childhood are treatable. Here are a few techniques that can help you recognize negative patterns learned in childhood and re-educate your inner child.
1. Empty Chair Technique
The application of this technique is as follows: the therapist places an empty chair in front of you and asks you to imagine that a significant person for you is sitting on it - for example, one of your parents.
You "communicate" with an imaginary interlocutor, talk about your thoughts and feelings, or explain to him what you wanted, but could not get from him as a child.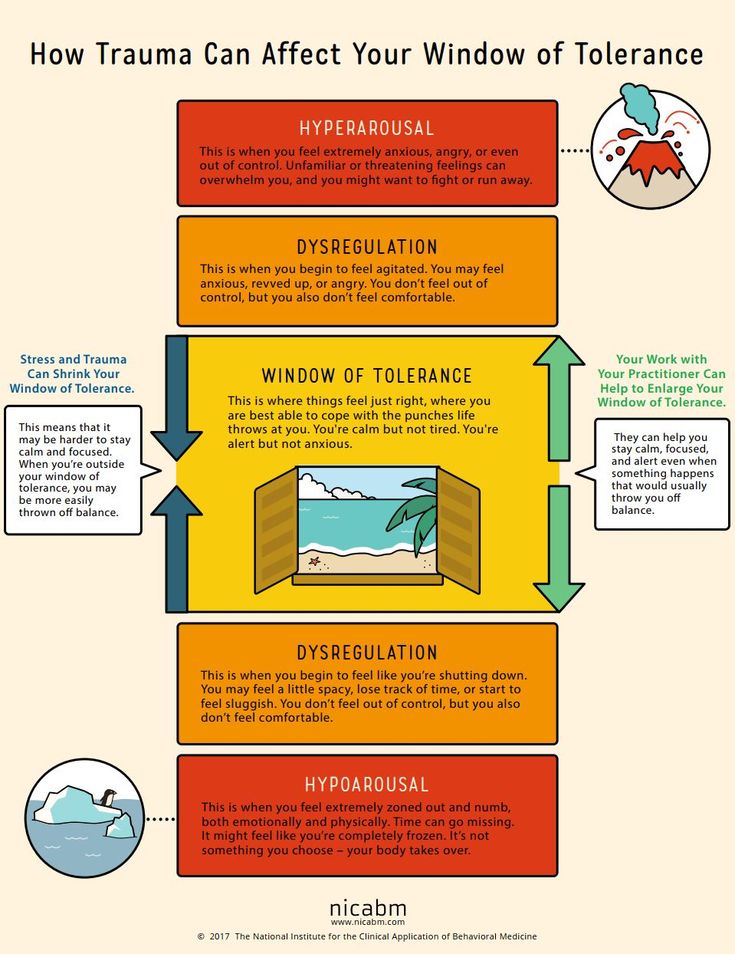 The therapist may suggest that you "reverse roles" and take the place of an imaginary interlocutor yourself. nine0003
The therapist may suggest that you "reverse roles" and take the place of an imaginary interlocutor yourself. nine0003
This work is especially helpful when people who have meant a lot to you in the past are unable or unwilling to take part in therapy. It helps you reconnect with your feelings about the past and with parts of yourself that you have tried to hide or suppress through addiction or other destructive behavior.
By getting in touch with your own feelings and memories, you can become aware of how they affect your current behavior and understand how you can change the situation. nine0003
2. Schematic Therapy
This method is suitable for patients experiencing social difficulties and those who cannot cope with the consequences of childhood trauma.
Children who grow up in a hostile or unhealthy environment often develop coping patterns, memories, emotions, ideas about themselves and others that are fraught with problems and lead to inappropriate reactions and behavior in adulthood.
During treatment, the therapist uses "re-education" techniques to help the patient's vulnerable inner child learn to meet their basic emotional needs in healthy ways. nine0003
Through various methods: dialogues, role plays, journaling, teaching important skills, schema therapy teaches the patient to look at himself and others differently and helps him overcome the desire to avoid unpleasant situations and get rid of other inappropriate reactions.
3. EMDR
Eye movement desensitization and processing (EMDR) is a technique based on information processing by the brain. It can help relieve unpleasant experiences associated with traumatic past events and manifested in the form of obsessive thoughts, sudden painful memories, anxiety, fear, panic attacks. nine0003
As the work progresses, the patient follows moving objects (eg, the therapist's fingers) with their eyes while trying to focus on internal negative images, thoughts, and feelings associated with the trauma.