How to stop being manic
How to Deal With Mania and Manic Episodes
Written by Charlotte Huff
In this Article
- Warning Signs
- Management
- Reducing Risk
- Prevention
If your doctor has diagnosed you with bipolar disorder, you know what a manic episode feels like. To be diagnosed, you must have had at least one episode of mania or its milder form, hypomania.
During these stretches, you may feel fabulous, with lots of energy and an "up" mood. But in the case of bipolar disorder,” those feelings are a symptom of mental illness. So it’s important to recognize the early signs that mania is developing.
Warning Signs
Just because you’re extra-energetic and in a good mood doesn’t mean you’re starting a manic episode. But be aware of patterns, such as when:
- You feel you’re on top of your life even if it’s not really going well.
- You have anxiety that can’t be explained by a stressful event, such as an upcoming exam.
- Your thoughts race and you're irritable.
- You're sleeping less and not taking good care of yourself.
- You talk too much or faster than usual.
- Your sex drive is revved up.
- You turn more often to alcohol or drugs or do other risky things like drive dangerously.
Management
Once you're in a full-blown manic state, you may not think you need help or be willing to accept it. That's why the best way to deal with mania is to address it early on.
If you think you're heading into a manic stretch, first get in touch with your doctor. They may need to change your medication dose or recommend that you try another one.
Take your medicine exactly as your doctor prescribes, even if you don’t think you need it. Tell your doctor about any supplements or herbs you’re taking. They may cause worrisome side effects.
Other things that may help:
- Review what's happening in your life and your stress level. See if you can dial back your commitments a bit.
 If you slow down now, you may avoid having to take more time off later because your symptoms got worse.
If you slow down now, you may avoid having to take more time off later because your symptoms got worse. - See a counselor or therapist. If you aren’t already in therapy, find someone who treats people with bipolar disorder. They can help you learn ways to identify and cope with troubling thoughts, emotions, or behavior.
- Look for ways to relax. When you talk with others, focus on listening. Carve out time to read, listen to your favorite music, or watch a show.
- Get enough sleep. This is not a time to skimp on your ZZZs. You need at least 6 hours a night.
- Watch out for caffeine. Steer clear not only of caffeine in beverages, like sodas and energy drinks, but in over-the-counter medications.
- Stay away from drugs and alcohol. They can affect your mood and may interact with medications you’re taking.
- Above all, don’t postpone seeking help so you can continue to ride the manic “high.” The higher your manic episode rises, the further your mood may tumble after it ends.

Reducing Risk
Talk to your doctor or therapist about what you should do when you're already in a manic state. And plan ahead. You might ask trusted friends or relatives to call your doctor if they notice signs of mania.
Here are some practical ways to protect yourself while you're in a manic episode:
- Keep up your normal routine. As much as possible, try to maintain a stable daily schedule. This includes your sleep, eating, and exercise patterns.
- Guard your finances: Limit how much cash you carry. Consider temporarily giving your credit cards to someone you trust to avoid impulse purchases.
- Delay big decisions. Don't make any major changes before you talk to someone, such as a mental health clinician or a relative. At the least, give yourself time to reflect before you take action.
- Bypass risky situations. This isn’t the right time to begin a new relationship or sort through a conflict with a friend.
Prevention
Once you feel better, keep up your healthy habits. That includes exercise, which can improve both mood and sleep. Build up your toolbox of strategies to reduce the intensity of future episodes:
That includes exercise, which can improve both mood and sleep. Build up your toolbox of strategies to reduce the intensity of future episodes:
- Look at what boosts your stress level. Lots of aspects of your life, whether it’s your job or a person you deal with, may affect your mood.
- Think about what may have been early signs of previous episodes. Was missing sleep for a few nights an early signal? Tell loved ones about those signs so they can watch out for them, too.
- Track your mood each day. When you keep a daily mood diary, you and your doctor or therapist can look for patterns. How do medication, sleep patterns, and life events affect how you feel?
- Once your mood is stable, reflect on how mania affects you in good and bad ways. Write down those thoughts. Then you can remind yourself of the downside when you're tempted to ignore the early signs of mania.
Coping with Mania: Tips, Recovery, and Prevention
What is bipolar disorder and mania?
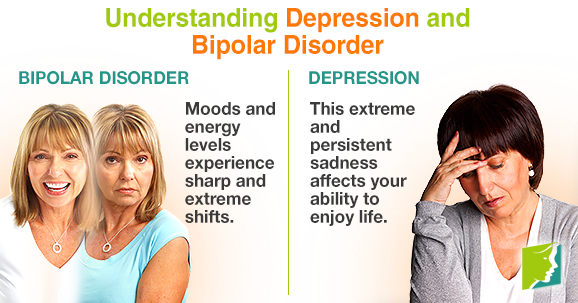
Bipolar disorder is a mental health condition that can cause you to experience episodes of extreme highs and extreme lows. These episodes are called mania and depression. The severity and frequency of these episodes will help your healthcare provider determine the type of bipolar disorder you have.
These episodes are called mania and depression. The severity and frequency of these episodes will help your healthcare provider determine the type of bipolar disorder you have.
- Bipolar 1 disorder occurs when you have at least one manic episode. You may or may not also have a major depressive episode before or after a manic episode. In addition, you may experience a hypomanic episode, which is less severe than mania.
- Bipolar 2 disorder is when you have a major depressive episode that lasts at least two weeks, and a hypomanic episode that lasts at least four days.
Read on to learn about mania and ways to help manage it.
Mania is a symptom associated with bipolar 1 disorder. You may experience the following during a manic episode:
- abnormally elevated mood
- persistently irritable mood
- unusually energetic mood
The DSM-5 is a medical reference commonly used by healthcare professionals to aid in diagnosis. According to this reference, to be considered a manic episode, your symptoms of mania must last at least a week, unless you’re hospitalized. Your symptoms may last less than a week if you’re hospitalized and successfully treated.
According to this reference, to be considered a manic episode, your symptoms of mania must last at least a week, unless you’re hospitalized. Your symptoms may last less than a week if you’re hospitalized and successfully treated.
During a manic episode, your behavior is very different from normal behavior. While some people are naturally more energetic than others, those experiencing mania have an abnormal level of energy, irritability, or even goal-directed behavior.
Some of the other symptoms you may experience during a manic episode include:
- feelings of inflated self-esteem and self-importance
- feeling like you don’t need sleep, or need very little sleep
- becoming unusually talkative
- experiencing racing thoughts
- being easily distracted
- engaging in risky behaviors, such as shopping sprees, sexual indiscretions, or making big business investments
Mania can cause you to become psychotic. This means you have lost touch with reality.
Manic episodes shouldn’t be taken lightly. They affect your ability to perform as usual in work, school, and social activities. Someone experiencing a manic episode may need to go to the hospital to keep from hurting themselves.
Manic episodes can vary from person to person. Some people can recognize they’re heading toward a manic episode, while others may deny the seriousness of their symptoms.
If you experience mania, in the heat of the moment, you probably won’t realize you’re having a manic episode. So, perhaps the best way to cope with mania is to plan ahead. Here are some steps you can take to prepare.
Reach out to your healthcare team
The first and most important thing to do if you think you have manic episodes, is to reach out to your mental health provider. This could include a psychiatrist, psychiatric nurse practitioner, counselor, social worker, or other mental health professional. If you’re worried that you’re close to the onset of a manic episode, contact your mental health provider as soon as possible to discuss your symptoms.
If you have a loved one or family member who is familiar with your illness, they may also help you receive support.
Online psychiatry services
Read our roundup of the best online psychiatry services to find the right fit for you.
Identify medications that help
Healthcare providers typically treat acute manic episodes with medications known as antipsychotics. These drugs can reduce manic symptoms more quickly than mood stabilizers. However, long-term treatment with mood stabilizers can help prevent future manic episodes.
Examples of antipsychotics include:
- olanzapine (Zyprexa)
- risperidone (Risperdal
- quetiapine (Seroquel)
Examples of mood stabilizers include:
- lithium (Eskalith)
- divalproex sodium (Depakote
- carbamazepine (Tegretol)
If you’ve taken these medications in the past and have some understanding of how they work for you, you may want to write down that information in a medication card. Or you could have it added to your medical record.
Or you could have it added to your medical record.
Avoid triggers that worsen your mania
Alcohol, illegal drugs, and mood-altering prescription drugs can all contribute to a manic episode and affect your ability to recover. Avoiding these substances can help you maintain your emotional balance. It may also help make recovery easier.
Maintain a regular eating and sleeping schedule
When you’re living with bipolar disorder, having structure in your daily life is vital. This includes following a healthy diet and avoiding caffeine and sugary foods that could affect your mood.
Getting enough regular sleep can also help you avoid manic or depressive episodes. In addition, it can help reduce the severity of any episodes that do occur.
Watch your finances
Going on spending sprees can be one of the major symptoms of mania. You can cope with this by limiting how easily you can access your finances. For example, keep enough cash to maintain your everyday lifestyle around your home, but do not have extra cash readily available.
You also may want to keep credit cards and other spending methods in places where they’re more difficult to use. Some people find it helpful to give their credit cards to a trusted friend or family member, while others avoid obtaining credit cards altogether.
Set up daily reminders
Create reminders for taking your medications and maintaining a regular bedtime. Also, consider using phone or computer notifications to help you keep your schedule.
In the recovery period, it’s time to start regaining control over your life and schedule. Discuss with your mental health provider and loved ones what you’ve learned from the episode, such as possible triggers. You can also start reestablishing a schedule for sleeping, eating, and exercising.
It’s important to think about what you can learn from this episode and how you can help yourself in the future. This will help you engage later in mania prevention.
Following a manic episode, many people gain insight into what may lead to their episodes. Examples of common mania triggers can include:
Examples of common mania triggers can include:
- drinking alcohol or abusing illegal drugs
- staying up all night and skipping sleep
- hanging out with others known to be an unhealthy influence (such as those who typically try to convince you to use alcohol or drugs)
- going off your regular diet or exercise program
- stopping or skipping your medications
- skipping therapy sessions
Keeping yourself on a routine as much as possible can help reduce manic episodes. But keep in mind that it won’t prevent them altogether.
If you or a loved one has bipolar disorder, there are certain key preparations you may wish to make.
Wellness recovery action plan
A “Wellness Recovery Action Plan” helps you account for important decisions and contact persons you may need if you get into a crisis. The National Alliance on Mental Illness recommends these plans as a means to avoid a crisis or have easy resources to reach out to. Examples of items on this plan include:
- phone numbers of key family members, friends, and/or healthcare providers
- phone numbers of local crisis lines, walk-in crisis centers and the National Suicide Prevention Lifeline at 1-800-273-TALK (8255)
- your personal address and phone number
- medications that you’re currently taking
- known triggers for mania
You can also create other plans with trusted family members or loved ones. For instance, your plan can record decisions about who will handle certain things during an episode. It might record who will take care of important tasks such as paying your bills or feeding your pets. It can also record who will manage financial details, such as finding sales receipts or making returns if spending sprees become a problem.
For instance, your plan can record decisions about who will handle certain things during an episode. It might record who will take care of important tasks such as paying your bills or feeding your pets. It can also record who will manage financial details, such as finding sales receipts or making returns if spending sprees become a problem.
Psychiatric advance directive
In addition to your Wellness Recovery Action Plan, you can create a Psychiatric Advance Directive. This legal document appoints a family member or loved one to act on your behalf while you’re experience a manic or depressive episode. Doing this can ensure that your wishes, such as where you’d like to be taken if you need to be hospitalized, are carried out if you’re in crisis.
Fire drill
You can also think about holding a “fire drill” for a future manic episode. This is a simulation where you imagine you’re going into a manic episode. You can practice who you would call, and ask them what they would do to help you.
Seeking help
While no one likes to think about manic episodes, it’s important to be aware of them and seek support in advance. Examples of organizations that can help include the National Alliance on Mental Illness (www.NAMI.org) and the Depression and Bipolar Support Alliance (DBSAlliance.org).
If you experience mania, you can take steps to decrease your risk of having episodes, such as following your treatment plan and avoiding triggers. These steps can help reduce the number and severity of your episodes.
But because you can’t prevent manic episodes entirely, it also helps to be prepared. Stay connected with your healthcare team, make decisions in advance of manic episodes, and be ready to reach out for help when you need it. Preparing for a manic episode before it happens can help you manage your condition and live more comfortably with bipolar disorder.
Manic syndrome - good mood or mania?
Inadequately elevated mood is a state that is exactly the opposite of depression. If it haunts a person for a sufficiently long time and is accompanied by other inadequate or illogical manifestations, then it is considered a mental disorder. This condition is referred to as manic and requires special treatment. Depending on the severity of the symptoms, consultation with a psychotherapist or psychiatrist may be required.
If it haunts a person for a sufficiently long time and is accompanied by other inadequate or illogical manifestations, then it is considered a mental disorder. This condition is referred to as manic and requires special treatment. Depending on the severity of the symptoms, consultation with a psychotherapist or psychiatrist may be required.
Features of the development of mania
In some cases, a tendency to mania can be a character trait, as well as a tendency to apathy. Increased activity, constant mental agitation, inappropriately high spirits, outbursts of anger or aggression are all symptoms of a manic syndrome. This is the name for a whole group of conditions that have different causes and sometimes different symptoms.
Both various life situations and incidents and uncorrected pathological character traits lead to the development of mania. A person prone to manic behavior is very often obsessed with an idea, he strives to realize it, even if it is unrealistic. Often patients are driven by theories that have political, religious or scientific justifications. Quite often, patients show a tendency to active social and social activities.
Often patients are driven by theories that have political, religious or scientific justifications. Quite often, patients show a tendency to active social and social activities.
A significant proportion of manic patients have so-called overvalued thoughts and ideas. Sometimes they can be global, sometimes they are ideas of the household level. From the outside, the behavior of patients talking about their ideas sometimes looks quite comical. If the overvalued thought is of a global nature, the patient, on the contrary, seems thoughtful and enthusiastic to those around him. Especially if he has enough education and erudition to justify his beliefs.
This condition is not always a pathology, it can be individual mental characteristics. Treatment is necessary if overvalued thoughts and ideas get out of control and absorb the entire life of the patient, in other words, they prevent him or others from living.
When do you need medical attention?
Manic syndrome is already a deviation from the norm, which is characterized by a number of symptoms that are more unpleasant for others than for the patient himself. This disease is manifested by disturbances in mental activity and the emotional sphere.
This disease is manifested by disturbances in mental activity and the emotional sphere.
Usually the behavior of a manic patient is incomprehensible to others and looks at least strange.
There are certain symptoms that indicate the need for medical attention:
- Extremely high spirits, up to constant mental excitement and euphoria.
- Inappropriate optimism, the patient does not notice real problems and is not inclined to experience a bad mood appropriate to the occasion.
- Accelerated speech, accelerated thinking, lack of concentration on objects and phenomena that the patient is not interested in. Therefore, in mania, learning is often difficult when you have to pay attention to rather boring things.
- Increased mobility, active gestures and hyperbolic facial expressions.
- Extravagance, pathological generosity. The patient can spend all the savings in a minute, not realizing the responsibility for his actions.
- Insufficient control over behavior.
 The patient does not realize that his high spirits are not appropriate everywhere.
The patient does not realize that his high spirits are not appropriate everywhere. - Hypersexuality, often with promiscuity (for example, a person who has never been prone to cheating before suddenly begins to flirt “indiscriminately”, enters into close relationships that he would never have dared to before, to the point that he starts several novels in parallel or embarks on a series of "short non-committal relationships", about which later, after the episode of mania has passed, he will repent and feel shame and even disgust, sincerely not understanding "how this could happen").
Treatment is complicated by the fact that the patient himself often does not recognize himself as ill. He considers his condition normal, subjectively pleasant and does not understand why others do not like his behavior: after all, he feels good, like never before. It is difficult to send such a patient to see a doctor and persuade him to therapy.
Our doctors
Ivanova Tatyana Semyonovna
Psychiatrist, doctor of the highest category
Experience 26 years
Make an appointment
Gravolatova Elena Nikolaevna
doctor - psychiatrist, candidate of medical sciences
Years 32 years
Sign up for an appointment
Lastovkina Valeria Valeriyevna
Psychiatrist
STARS 4 years
Sign up for an appoint Psychiatrist, candidate of medical sciences, doctor of the highest category
Experience 47 years
Make an appointment
Bogdanova Natalia Ivanovna
Psychiatrist, psychotherapist
Experience 20 years
Make an appointment
Symptoms and signs of the disease
In addition to the above signs, there are several characteristic symptoms that unite almost all manic states:
- A tendency to thoughtlessly waste money.

- Tendency to unprofitable transactions, gambling.
- Frequent violation of the law.
- Tendency to provoke fights and conflicts.
- Excessive alcohol consumption or addiction to other bad habits.
- Promiscuous sexual behavior.
- Pathological sociability - the patient often meets strange, suspicious personalities and spends time in a variety of companies.
If these signs get out of hand, seek medical attention. It is important to understand that such behavior is not promiscuity, but symptoms of a disease that needs to be treated. Appeal to common sense is useless.
In some cases, the patient has a specific mania - for example, a mania for a particular purpose. Then the patient is sincerely confident in his special mission and tries to fulfill it with all his might, despite the skepticism of those around him.
Varieties of manic states
There are several classifications according to the manifestations of mania and according to their content.
According to the content, the following types are distinguished:
- Mania of persecution - accompanied by paranoia. The patient is convinced that he is being persecuted, anyone can act as a persecutor - from relatives and friends to special services.
- Mania for a special purpose - the patient is sure that he needs to create a new religion, make a scientific discovery, save humanity.
- Megalomania - similar to the previous one. The main difference is that the patient does not have a goal, he simply considers himself the chosen one - the most intelligent, beautiful, rich.
- Mania of guilt, politeness, self-destruction, nihilistic - more rare situations. In patients prone to alcohol abuse, jealousy mania is often noted.
According to the emotional state, the manic syndrome can be:
- Joyful mania – excitation, unreasonably elevated mood.
- Angry - irascibility, a tendency to create conflict situations.
- Paranoid - manifested by paranoia of persecution, paranoia of relationships.

- Oneiroid - accompanied by hallucinations.
- Manic-depressive syndrome is characterized by alternating mania and depression.
In manic-depressive disorder, intervals may alternate at equal intervals, or one type of behavior predominates. Sometimes the next phase may not come for years.
Treatment of manic states
Diagnosed mania is a condition that requires mandatory treatment. It is customary to carry out complex therapy: pharmacological and psychotherapeutic. Pharmaceutical preparations are selected to relieve symptoms: for example, a patient with increased excitability will receive a prescription for sedatives, antipsychotics help to relieve concomitant symptoms, and to prevent the development of the next phase - normotimics.
With regard to psychotherapeutic treatment, usually work with a specialist goes in the direction of cognitive and cognitive-behavioral therapy, as well as psychoeducation (targeted informing the patient about the disease and learning to recognize early signs (“markers”) of the phase change and respond quickly to them in order to prevent the development of the next full-fledged depression or mania). In the course of psychotherapy, one can find and eliminate the cause of the disease, correct the behavior and way of thinking of the patient. On average, treatment takes about a year, but after improvement, dynamic monitoring is required, since the manic syndrome can recur.
In the course of psychotherapy, one can find and eliminate the cause of the disease, correct the behavior and way of thinking of the patient. On average, treatment takes about a year, but after improvement, dynamic monitoring is required, since the manic syndrome can recur.
If the patient is in serious condition, hospitalization is recommended. Usually it is prescribed in order to protect others and the patient himself.
Regardless of the patient's condition, it is important to start treatment as soon as symptoms appear. Psychotherapists of the CELT clinic also work with manic states. Thanks to their serious experience and high qualifications, they will help restore mental health.
Manic disorders
Classification of manic episodes according to severity includes hypomania, mania without psychotic episodes, and mania with psychotic episodes.
Under hypomania understand a mild degree of mania, in which changes in mood and behavior are long-term and pronounced, not accompanied by delusions and hallucinations. An elated mood manifests itself in the sphere of emotions as a joyful cloudlessness, irritability, in the sphere of speech - as increased talkativeness with ease and superficial judgments, increased contact. In the field of behavior, there is an increase in appetite, sexuality, distractibility, a decrease in the need for sleep, and individual actions that go beyond morality. Ease of associations, increase in working capacity and creative productivity are subjectively felt. Objectively, the number of social contacts and success increase. At the same time, there are episodes of reckless or irresponsible behavior, increased sociability or familiarity.
An elated mood manifests itself in the sphere of emotions as a joyful cloudlessness, irritability, in the sphere of speech - as increased talkativeness with ease and superficial judgments, increased contact. In the field of behavior, there is an increase in appetite, sexuality, distractibility, a decrease in the need for sleep, and individual actions that go beyond morality. Ease of associations, increase in working capacity and creative productivity are subjectively felt. Objectively, the number of social contacts and success increase. At the same time, there are episodes of reckless or irresponsible behavior, increased sociability or familiarity.
The main criterion for diagnosis is an elevated or irritable mood that is abnormal for the individual, persists for at least several days, and is accompanied by the above symptoms.
It should be noted that hypomanic episodes are possible in some somatic and psychiatric disorders. For example, with hyperthyroidism, anorexia or therapeutic starvation in the phase of food arousal; with intoxication with certain psychoactive substances - PAS (amphetamines, alcohol, marijuana, cocaine), however, there are other manifestations of somatic and mental pathology and PAS intoxication.
In a typical form , an extended manic state is manifested by the so-called manic triad: a painfully elevated mood, an accelerated flow of thoughts, and motor excitation. The leading sign of a manic state is a manic affect, manifested in an elevated mood, a feeling of happiness, contentment, well-being, an influx of pleasant memories and associations. It is characterized by an aggravation of sensations and perceptions, an increase in mechanical and some weakening of logical memory, superficial thinking, lightness and unproductiveness of judgments and conclusions, ideas of reassessment of one's own personality , up to delusional ideas of greatness, disinhibition of inclinations and weakening of higher feelings, instability, ease of switching attention.
Mania without psychotic symptoms. The main difference from hypomania is that elevated mood affects the change in the norms of social functioning, manifests itself in inadequate actions that are not controlled by the patient. The pace of the passage of time accelerates and the need for sleep is significantly reduced. Tolerance and need for alcohol increase, sexual energy and appetite increase, there is a craving for travel and adventure. Thanks to the leap of ideas, many plans arise, the implementation of which is not carried out. The patient strives for bright and flashy clothes, speaks in a loud voice, incurs a lot of debt and gives money to people he hardly knows. He easily falls in love and is sure of the love of the whole world for himself. Gathering a lot of random people, he arranges holidays on credit. There is reckless driving, a marked increase in sexual energy, or sexual promiscuity. There are no hallucinations or delusions, although there may be perceptual disturbances (eg, subjective hyperacusis, vivid color perception).
The pace of the passage of time accelerates and the need for sleep is significantly reduced. Tolerance and need for alcohol increase, sexual energy and appetite increase, there is a craving for travel and adventure. Thanks to the leap of ideas, many plans arise, the implementation of which is not carried out. The patient strives for bright and flashy clothes, speaks in a loud voice, incurs a lot of debt and gives money to people he hardly knows. He easily falls in love and is sure of the love of the whole world for himself. Gathering a lot of random people, he arranges holidays on credit. There is reckless driving, a marked increase in sexual energy, or sexual promiscuity. There are no hallucinations or delusions, although there may be perceptual disturbances (eg, subjective hyperacusis, vivid color perception).
The main symptom is an elevated, expansive, irritable (angry) or suspicious mood, which is not characteristic of this individual. The change in mood should be distinct and persist throughout the week.
Mania with psychotic symptoms. It is a pronounced mania with a bright jump of ideas and manic excitement, to which secondary crazy ideas of greatness, high origin, hypereroticity, value join. There may be hallucinatory hails confirming the significance of the person, or "voices" telling the patient about emotionally neutral things, or delusions of meaning and persecution. The greatest difficulty lies in the differential diagnosis with schizoaffective disorders, however, with these disorders, there should be symptoms characteristic of schizophrenia, and delusions with them are less consistent with mood. However, the diagnosis can be considered as the starting point for the assessment of schizoaffective disorder (first episode).
Mental disorder formerly referred to as manic-depressive psychosis (MDP). It is characterized by repeated (at least two) manic, depressive and mixed episodes that alternate without a definite sequence. A feature of this psychosis is the presence of light interphase gaps (intermissions), in which all signs of the disease disappear, a complete restoration of a critical attitude to the transferred painful condition is observed, premorbid characterological and personal properties, professional knowledge and skills are preserved.