How long does alcohol depression last
The Connection & Dual Treatment Near Me
Can drinking alcohol cause depression and, conversely, can depression lead to misusing alcohol? If you or someone you care about are struggling with depression and alcohol abuse, you may be interested in learning more about how alcohol can play a role in depression and vice versa, as well as the different factors that can affect alcohol, depression, and addiction.
Simultaneous treatment for alcohol use disorder and a depressive disorder can help you or your loved one take back control of your mental health, physical wellbeing, and overall happiness. Know that you’re not alone and help is available.
Ways to Get in Contact With Us
If you believe you or someone you love may be struggling with addiction, let us hear your story and help you determine a path to treatment.
There are a variety of confidential, free, and no obligation ways to get in contact with us to learn more about treatment.
- Call us at
- Verify Your Insurance Coverage for Treatment
Understanding Depression
Everyone feels blue or down from time to time, and people often say that they feel “depressed” during these temporary bouts of sadness. But clinical depression isn’t just a matter of feeling the occasional ups and downs or periodic sadness caused by issues of daily life.
Major depressive disorder, persistent depressive disorder, and other depressive disorders are treatable mental health disorders that are characterized by symptoms of sadness, emptiness, or irritable mood that affects a person’s body and mind, specifically the ability to function. Although researchers have identified several risk factors for depressive disorders, they can occur in anyone. Not everyone who experiences risk factors will develop a depressive disorder, but risk factors can play a role in its development. These risk factors include:1,2,3,4,5
- Genetics and heritability. Genes are not destiny, but a family history of depression is considered a risk factor. First-degree family members of individuals with major depressive disorder have a risk two- to four-times higher than the general population.
- Biological factors and illness.
 This includes your physical health, such as having a serious illness like cancer, diabetes, or heart disease, as well as your levels of neurotransmitters (brain chemicals), which can become imbalanced and influence depression.
This includes your physical health, such as having a serious illness like cancer, diabetes, or heart disease, as well as your levels of neurotransmitters (brain chemicals), which can become imbalanced and influence depression. - Stress, major life changes, and exposure to trauma. Any of these can be a risk factor, but particularly if you experienced them in childhood.
- Taking certain medications. Some of the side effects of medications can cause or contribute to depressive symptoms.
- Low socioeconomic status. While socioeconomic status can play a role at any point in your lifespan, it can be a particular risk factor early in life.
- Using illicit substances or alcohol. Different substances can increase your risk of developing depression.
Signs and Symptoms of Depression
To be diagnosed with major depressive disorder or another depressive disorder, people typically need to display symptoms almost every day for at least 2 weeks.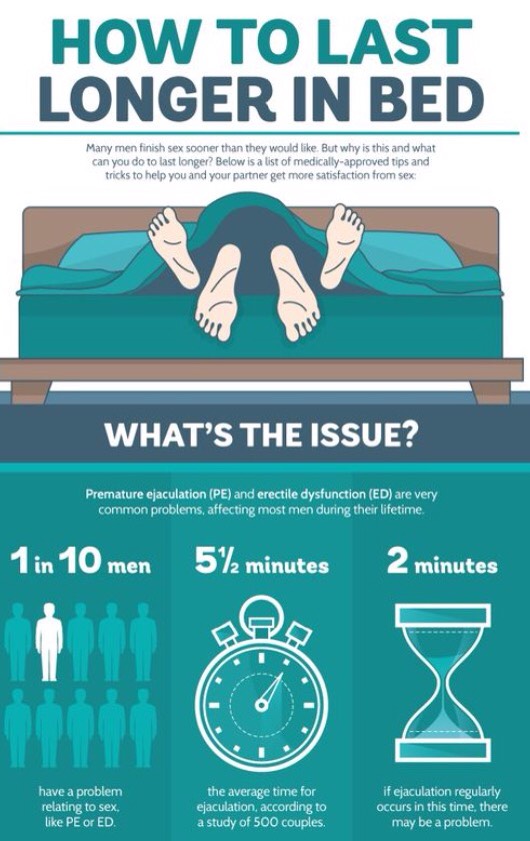 The symptoms are severe enough that they cause significant stress and impairment in social, occupational, or other important areas of functioning.5 While the specific types of depressive disorders can look a bit different, they tend to share common symptoms that include:1,5,6
The symptoms are severe enough that they cause significant stress and impairment in social, occupational, or other important areas of functioning.5 While the specific types of depressive disorders can look a bit different, they tend to share common symptoms that include:1,5,6
- A persistent low mood, feelings of sadness, and/or feeling anxious or empty.
- Feeling hopeless or pessimistic.
- Irritability, frustration, or restlessness.
- Feeling excessively or inappropriately guilty, worthless, or helpless.
- Losing interest or pleasure in activities or hobbies you once enjoyed.
- A lack of energy or fatigue.
- Moving or talking more slowly than usual.
- Difficulty thinking, remembering, or making decisions.
- Changes in sleep, such as trouble falling or staying asleep (insomnia) or sleeping more than usual (hypersomnia).
- Changes in appetite with significant weight loss or weight gain (e.g., a change of more than 5% of body weight).
- Having thoughts of self-harm, death, or suicide, or making suicidal attempts.
- Aches, pains, headaches, cramps, or digestive problems that aren’t easily explainable and do not improve with treatment.
How Alcohol Abuse Can Factor into Depression
Can alcohol cause depression or vice versa? Research has shown that there seems to be a bidirectional relationship between alcohol use disorder (AUD) and depressive disorders; both disorders can exist together, each disorder increases the risk for the other disorder, and each disorder can worsen the other.7 Regardless of the order of which came first, AUD or a depressive disorder, both issues are among the most prevalent psychiatric disorders and co-occur often.7,8,9,10
Are you in need of substance abuse and co-occurring mental health treatment? Plenty of American Addiction Centers locations across the nation offer specialized co-occurring disorder treatment. Call our admissions navigators today to discover your treatment options.
The pathways leading to the development of co-occurring AUD and a depressive disorder are complex and intertwined. Some individuals may be genetically susceptible to both. For others, symptoms of a depressive disorder can influence the development of an AUD. One possible contributor to cooccurrence is that people may alleviate symptoms of a depressive disorder with substances like alcohol. People who experience major depressive symptoms may start to rely on alcohol to ease their symptoms and feel better, but over time, this can develop into a full-blown alcohol use disorder.10 Even in instances where a person doesn’t develop an AUD, self-medication may not be helpful long-term, as it is associated with increased psychiatric comorbidity, higher stress levels, and lower health-related quality of life.3,10 Research also has associated AUD with a risk not only for the onset of depressive symptoms but also depressive disorders.
It’s important to note that the co-occurrence of AUD and depressive disorders, specifically major depressive disorder and persistent depressive disorder, is associated with greater severity and worse prognosis than either disorder alone.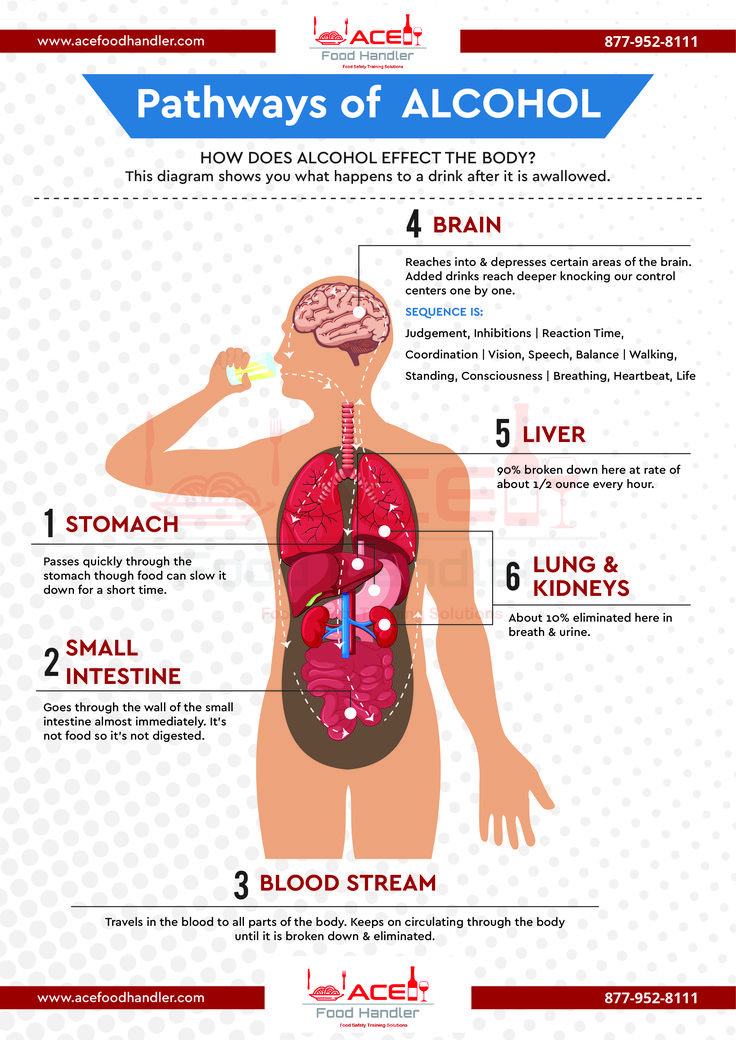 This includes a heightened risk for suicidal behavior.7
This includes a heightened risk for suicidal behavior.7
It’s a vicious pairing that can be difficult to overcome, however, treatment can be effective.
Can Alcohol Make Depression Worse?
Yes, alcohol can exacerbate depression and depressive symptoms. In addition, a clinical review in the journal, Professional Psychology: Research and Practice explains that drinking can interfere with recovery from depression. Depressed study participants who were heavy drinkers displayed worse outcomes from depression treatment; furthermore, even mild to moderate amounts of alcohol appeared to worsen depression, with depressed patients who drank low levels of alcohol (less than 1 oz per day) experiencing worse outcomes from pharmacological treatments.13
Alcohol use disorders may be more prevalent in people who also have depression than they are in the general population. The occurrence of alcohol use disorder and a depressive disorder are associated with greater severity and a worse prognosis for both disorders.
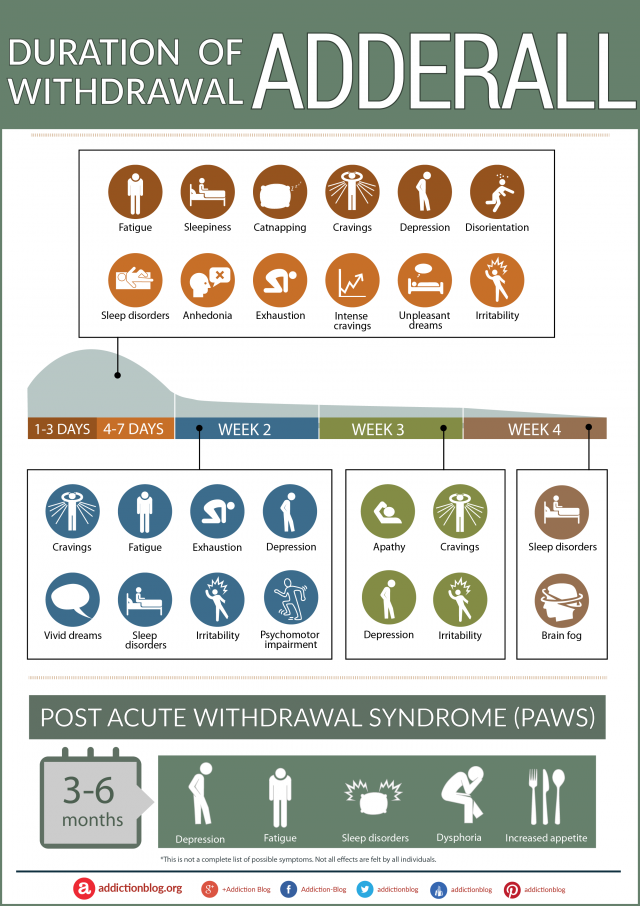
How Long Does Alcohol-Induced Depression Last?
The duration of alcohol-induced depression can vary widely. Generally speaking, depressive symptoms associated with alcohol-induced depression have been shown to improve significantly after you’ve abstained from alcohol for a certain amount of time, typically 3-4 weeks in many cases.11 However, research also suggests that substance-induced depression can turn into independent depression should symptoms of depression persist following cessation of alcohol or other substances of abuse.
Take Our “Am I an Alcoholic?” Self-Assessment
Take our free, 5-minute “Am I an Alcoholic?” self-assessment below if you think you or someone you love might be struggling with an alcohol use disorder (AUD). The evaluation consists of 11 yes or no questions that are intended to be used as an informational tool to assess the severity and probability of an AUD. The test is free, confidential, and no personal information is needed to receive the result.
Treatment for Co-Occurring Depression and Alcohol Use Disorder
Treatment often includes an integrated approach to simultaneously address both alcohol use disorder and depression..
Many treatments can help co-occurring depression and AUD. Some of these can include:14,15,16
- Detox. This is usually the first step in the recovery process followed by entry into a formal drug rehabilitation program. Detox helps you safely and comfortably withdraw from alcohol.
- Antidepressants/Medications. You may receive antidepressants, which can help treat both the depression and some symptoms of AUD. In addition, you may receive naltrexone, a medication that helps people stop drinking and reduces depressive symptoms, disulfiram, which is used as an alcohol deterrent (it causes unpleasant symptoms if you drink alcohol), or acamprosate, which is used to help maintain abstinence from alcohol.
- Behavioral therapies.
 These can include:
These can include: - Cognitive-Behavioral Therapy (CBT). This helps you learn positive coping mechanisms to replace the thought and behavioral patterns that can contribute to or worsen AUD and depression.
- Dialectical Behavior Therapy (CBT). This is mainly used to help reduce self-harm and suicidal behavior.
- Behavioral Activation. This is a type of behavioral therapy that is effective for both AUD and depression. It involves developing an understanding of how negative life experiences and behaviors influence your mood and emotions and encourages you to take an active approach to increase your positive life experiences.
- Mutual support groups, which include 12-step groups like Alcoholics Anonymous (AA) and non-12-step groups like SMART Recovery. These groups are effective both as treatment and as aftercare for both AUD and depression. You’ll benefit from the support of others who know what it’s like to be in your shoes, which can lessen feelings of isolation and help you feel connected.

Find Drug and Alcohol Treatment Centers Near You
Other Frequently Asked Questions Regarding Alcohol & Depression
References
- National Institute of Mental Health. (2018). Depression.
- Çakıcı, M., Gökçe, Ö., Babayiğit, A., Çakıcı, E., & Eş, A. (2017).
- Kaltenboeck, A. & Harmer, C. (2018). The neuroscience of depressive disorders: A brief review of the past and some considerations about the future. Brain and Neuroscience Advances, 2.
- Kwong, A., López-López, J. A., Hammerton, G., Manley, D…& Pearson, R. M. (2019). Genetic and Environmental Risk Factors Associated With Trajectories of Depression Symptoms From Adolescence to Young Adulthood. JAMANetwork Open, 2(6), e196587.
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Arlington, VA: American Psychiatric Publishing.
- Obeid, S., Akel, M., Haddad, C., Fares, K…& Hallit, S. (2020).
- McHugh, R. K., & Weiss, R. D. (2019). Alcohol Use Disorder and Depressive Disorders. Alcohol research : current reviews, 40(1), arcr.v40.1.01. https://doi.org/10.35946/arcr.v40.1.01.
- National Institute of Mental Health. (2021). Depression.
- Fergusson, D. M., Boden, J. M., & Horwood, L. J. (2009). Tests of causal links between alcohol abuse or dependence and major depression. Archives of general psychiatry, 66(3), 260–266.
- Turner, S., Mota, N., Bolton, J., & Sareen, J. (2018). Self-medication with alcohol or drugs for mood and anxiety disorders: A narrative review of the epidemiological literature. Depression and anxiety, 35(9), 851–860.
- American Society for Addiction Medicine (ASAM) Principles of Addiction Medicine, Sixth Edition (2 hard copies in our department library. Online access available—ask Scot for login credentials)
- Nunes EV, Liu X, Samet S, Matseoane K, Hasin D.
 Independent versus substance-induced major depressive disorder in substance-dependent patients: observational study of course during follow-up. J Clin Psychiatry. 2006 Oct;67(10):1561-7. doi: 10.4088/jcp.v67n1010. PMID: 17107247.
Independent versus substance-induced major depressive disorder in substance-dependent patients: observational study of course during follow-up. J Clin Psychiatry. 2006 Oct;67(10):1561-7. doi: 10.4088/jcp.v67n1010. PMID: 17107247. - Ramsey, S. E., Engler, P. A., & Stein, M. D. (2005). Alcohol Use Among Depressed Patients: The Need for Assessment and Intervention. Professional Psychology: Research and Practice, 36(2), 203–207.
- McHugh, R. K., & Weiss, R. D. (2019). Alcohol Use Disorder and Depressive Disorders. Alcohol Research: Current Reviews, 40(1), arcr.v40.1.01.
- National Institute on Drug Abuse. (2020). Common Comorbidities with Substance Use Disorders Research Report: What are the treatments for comorbid substance use disorder and mental health conditions?
- National Alliance on Mental Illness. (2020). Substance Use Disorders.
- National Institute on Alcohol Abuse and Alcoholism. (2008).
 Genetics of Alcohol Use Disorder.
Genetics of Alcohol Use Disorder. - National Alliance on Mental Illness. (2021). Medication Frequently Asked Questions.
The Effects of Alcohol on Depression
Perhaps you’ve been wondering, does alcohol cause depression? Does alcohol make depression worse? First, however, it is important to learn more about what depression is and the effects of alcohol on depression. Depression and alcohol addiction are often interlinked.
Depression Defined
It’s common for anyone to feel down or blue from to time, and individuals often say that they are feeling “depressed” during their temporary periods of sadness. However, clinical depression isn’t just undergoing periodic sadness that is caused by daily life issues or experiencing the occasional ups and downs. Many treatable mental health disorders are distinguished by the following symptoms:
- An irritable mood that affects an individual’s mind and body, particularly the ability to function
- Emptiness
- Sadness
The treatable depression disorders are:
- Persistent depressive disorder
- Major depressive disorder
- Various other depressive disorders
Does Alcohol Cause Depression?
The question that will be answered in this blog is, “Does alcohol cause depression?” Research has shown and indicated that there does seem to be a two-way relationship occurring between depression and alcohol addiction.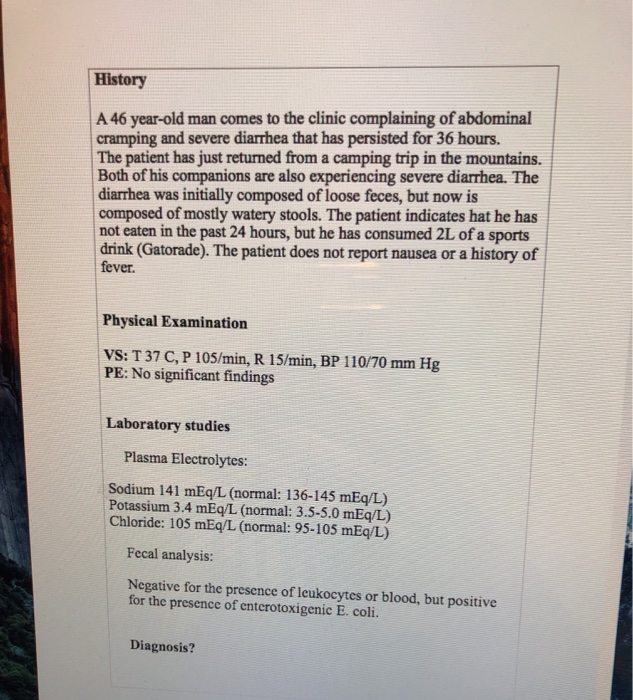 Both depressive disorders and alcohol use disorder (AUD) can exist together. Each disorder can increase the risk of the other.
Both depressive disorders and alcohol use disorder (AUD) can exist together. Each disorder can increase the risk of the other.
So, does alcohol make depression worse? The answer is yes, either disorder can worsen the other. Regardless of the actual order in which they came, depression and alcohol addiction are both issues that are among the most widespread psychiatric disorders that co-occur often.
There was a study in JAMA Psychiatry that pointed out that there could be a direct cause and effect relationship between alcohol and depression, specifically alcohol abuse and dependence, along with major depressive disorder in specific circumstances. Alcohol can worsen the depressive symptoms in individuals who have already experienced the symptoms or individuals who could be genetically vulnerable to depressive disorders.
If an individual’s depressive symptoms are caused by alcohol use, the symptoms might stop after reducing their intake significantly, or altogether stopping their alcohol use. However, it has also been suggested by research that substance-induced depression can transition more into an independent form of depression should the symptoms continue to persist following the cessation of other substances of abuse or alcohol.
However, it has also been suggested by research that substance-induced depression can transition more into an independent form of depression should the symptoms continue to persist following the cessation of other substances of abuse or alcohol.
Does Alcohol Make Depression Worse?
Does alcohol make depression worse? The answer is yes, alcohol can certainly exacerbate depressive symptoms and depression. Additionally, a clinical review in the following journal, Professional Psychology: Research and Practice thoroughly explained that drinking can interfere with an individual that is trying to recover from depression.
The depressed study participants who were considered heavy drinkers exhibited even worse outcomes from depression treatment. Furthermore, mild to moderate amounts of alcohol has appeared to worsen depression. The study indicated that the depressed patients who drank low amounts of alcohol such as less than 1 oz per day ended up experiencing even worse outcomes from pharmacological treatments.
Alcohol use disorders might be more widespread in individuals who also have depression. Depression and alcohol addiction are certainly interlinked. The actual development of depressive disorder and alcohol use disorder is related to a worse prognosis for both disorders and greater severity.
Why Might People Experience Depression After Drinking Alcohol?
There are many reasons why people might experience depression after drinking. Firstly, alcohol is known to temporarily help improve an individual’s mood or lift a person’s spirits. However, the more a person drinks, the more likely their emotional state will start plummeting. Sometimes, alcohol tends to make a person feel worse than they did before.
Alcohol affects people in various ways. The effects of alcohol on depression can be extremely severe. Some individuals never recognize depression feelings or any type of negative feelings at all after engaging in drinking moderately.
Other individuals might begin to feel anxious or depressed after simply one drink. Understanding the relationship between depression and alcohol addiction can help a person manage their depression after drinking. It may even help individuals to avoid drinking in the first place, especially if they are prone to experiencing symptoms of depression.
Understanding the relationship between depression and alcohol addiction can help a person manage their depression after drinking. It may even help individuals to avoid drinking in the first place, especially if they are prone to experiencing symptoms of depression.
If you are curious about the overall effects of alcohol on depression, it is important to learn more about how this substance and mental health disorder affect one another. Alcohol and depression can contribute to symptoms in even indirect ways. It’s important to remember that alcohol is a depressant. Drinking alcohol is known to trigger dopamine release and activate the reward system in a person’s brain. At first, alcohol is known to create a stimulant effect.
There has been research that has linked alcohol and depression with adolescents. Especially when they have engaged in regular or heavy use. Adults who have met the alcohol use disorder criteria have also had a higher risk of experiencing alcohol and depression symptoms. To summarize, even though alcohol might seem as though it improves your overall mood at the moment, it can bring you down with long-term use. There are various areas that alcohol disrupts such as the following:
To summarize, even though alcohol might seem as though it improves your overall mood at the moment, it can bring you down with long-term use. There are various areas that alcohol disrupts such as the following:
Alcohol Disrupts Sleep
Have you ever experienced a night of poor sleep where you were tossing and turning, experiencing bizarre dreams, and woke up with your heart racing? These bad dreams are pretty normal. Troubled sleep can relate to the actual changes in an individual’s brain chemistry that is related to alcohol use.
Does alcohol make you depressed? Yes, but it can also interfere with a person’s sleep-wake cycle and keep a person from receiving enough REM sleep. Drinking is known to create various physical consequences – such as dehydration and nausea which can also keep a person from receiving peaceful sleep. Poor sleep is also able to easily affect a person’s mood the next day. Lingering physical symptoms such as exhaustion can make it difficult to concentrate, overall making a person feel pretty low.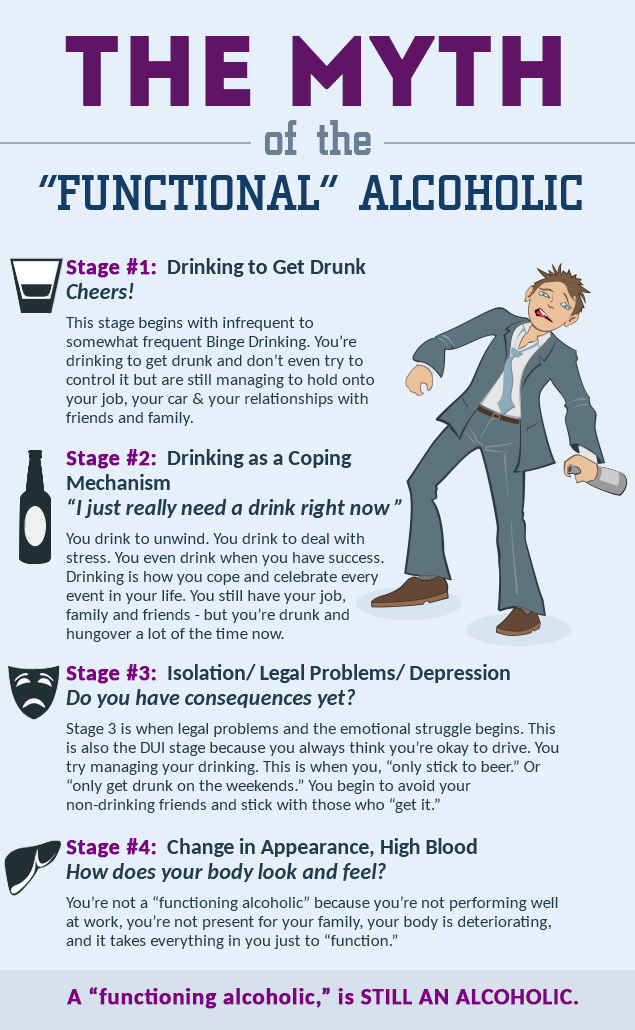
Alcohol Can Worsen Negative Emotions
Undergoing a low mood after a heavy night of drinking can make a person feel pretty awful. Especially when an individual already has depression, drinking might make them feel even worse. Alcohol can enhance the magnitude and severity of a person’s emotional state.
Alcohol can also affect the areas of a person’s brain that assist in regulating emotions. Commonly, a person might start drinking to forget what’s on their mind. Once the initial boost starts to wear off, it’s typical that the individual will start wallowing in their emotions instead.
Since alcohol can cloud an individual’s brain, it can also keep a person from being able to view helpful solutions to their problems. Alcohol also lowers an individual’s inhibitions. So if the person has been trying to keep their challenging emotions at bay, such as anger or sadness, it’s possible those feelings can come flooding in when the person drinks.
The above-mentioned scenario can lead to a difficult cycle.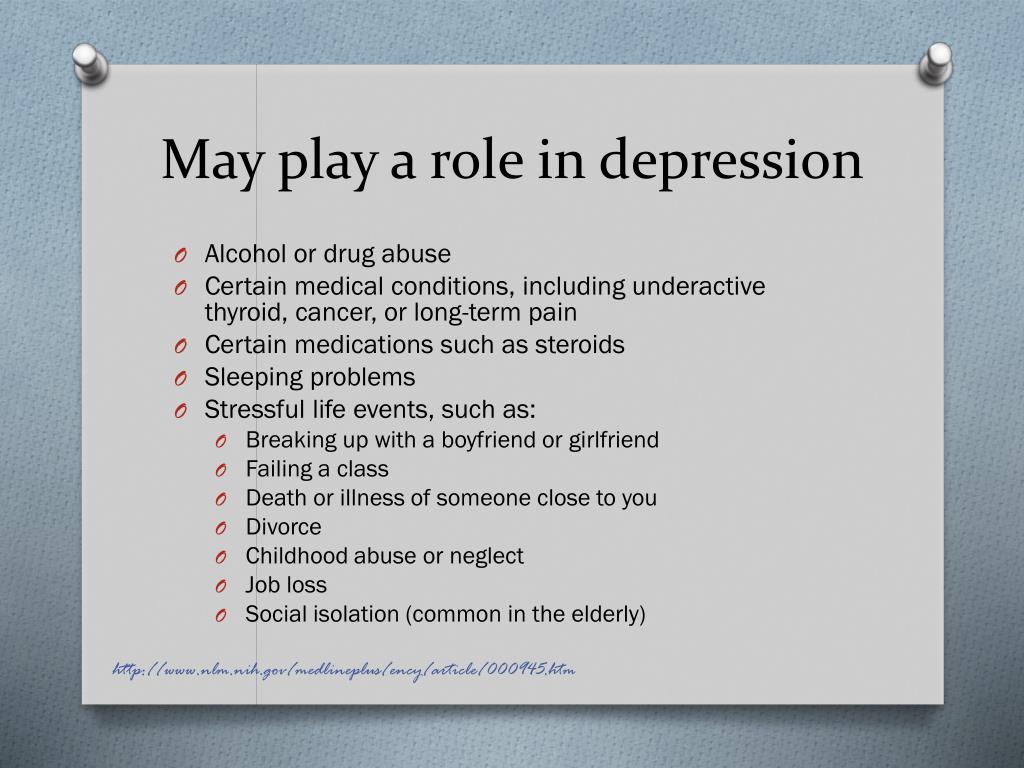 An individual might begin drinking more regularly to feel better about themselves and forget about unfavorable memories and emotions. Increased alcohol use typically doesn’t help. It is more likely to worsen a negative mood state, along with the person’s physical health.
An individual might begin drinking more regularly to feel better about themselves and forget about unfavorable memories and emotions. Increased alcohol use typically doesn’t help. It is more likely to worsen a negative mood state, along with the person’s physical health.
Drinking to Cope Can Become a Pattern
When an individual regularly turns to alcohol to manage negative feelings and challenges, they might not take any other actions that could assist them in effectively addressing those same problems. As a result of that, any troubles a person might be facing, from work stress to even relationships, could get much worse. If an individual tends to rely on alcohol to ease their anxiety in social situations, they might not ever find or be able to address the underlying causes of their discomfort.
The lowered inhibitions that are mentioned above can lead a person to make decisions that normally wouldn’t be made. When it’s combined with heightened mood states, displeasing effects can occur.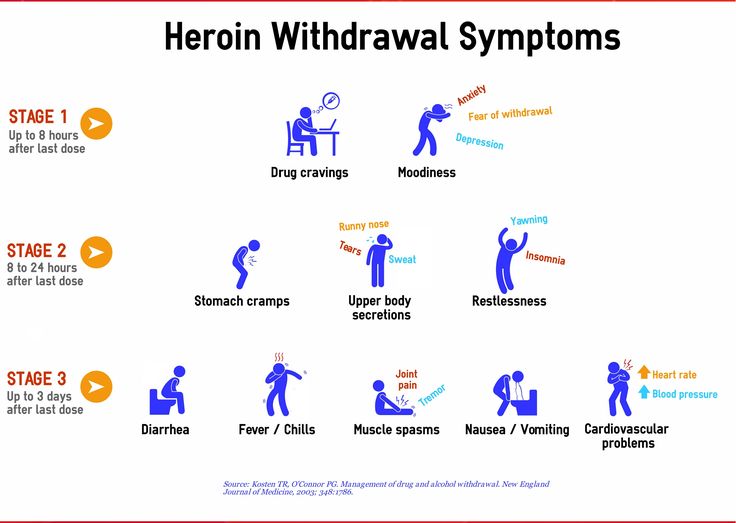 Increased anger might lead a person to pick fights with loved ones, while extreme self-loathing and sadness could result in severe depression symptoms.
Increased anger might lead a person to pick fights with loved ones, while extreme self-loathing and sadness could result in severe depression symptoms.
How Long Does Alcohol-Induced Depression Last?
The actual duration of alcohol-induced depression can greatly vary. Depressive symptoms that are associated with alcohol-induced depression have been shown to significantly improve after an individual has abstained from alcohol for a certain period. It is typically 3-4 weeks in a variety of cases. However, there has been research that has suggested that substance-related depression can turn into a more independent depression if the symptoms of depression persevere following the cessation of substance or alcohol use.
How Do Depressive Disorders and Alcoholism Co-occur?
The actual pathways leading to the overall development of the co-occurring depressive disorder and an AUD are intertwined and complex. Some individuals might present to be susceptible to both alcohol and depression. For other individuals, the actual symptoms of a depressive disorder can impact and influence AUD development.
For other individuals, the actual symptoms of a depressive disorder can impact and influence AUD development.
A possible contributor to the cooccurrence is that individuals attempt to relieve depressive disorder symptoms with various substances such as alcohol. People who undergo major depressive symptoms might start the process of relying on alcohol to feel better, and ease their symptoms. However, over time, this pattern can develop into a full-scale alcohol use disorder.
Even in circumstances where an individual doesn’t develop an AUD, self-medicating might not present to be beneficial long-term, as it is connected with higher stress levels, lower-health related qualify of life, and increased psychiatric comorbidity. Research has gone one step further to associate an AUD with risk, not only for the onset of experiencing depressive symptoms, but also depressive disorders. It’s essential to note the co-occurrence of depressive disorders and AUD, particularly persistent depressive disorder and major depressive disorder.
The above-mentioned scenario might include a more heightened suicidal behavior risk. Depression and alcohol addiction is a vicious pair that can certainly be challenging to overcome. However, treatment can be super effective in treating the effects of alcohol on depression.
What is the Best Treatment for Co-occurring Depression and Alcohol Use Disorder?
The treatment for co-occurring alcohol use disorder and depression generally includes an integrated perspective that can simultaneously address both depression and alcohol use disorder. Many treatments do help AUD and co-occurring depression and they include:
Detox
Detox is generally the first step in an individual’s recovery process and it’s followed by the person’s entry into a formal drug rehabilitation program. With detox, the person can comfortably and safely withdraw from alcohol.
Medications
An individual might receive antidepressants for some symptoms of their AUD or depression. Additionally, a person might receive other medications aimed to assist with abstinence from alcohol.
Additionally, a person might receive other medications aimed to assist with abstinence from alcohol.
Behavioral Therapies
- Cognitive-behavioral therapy (CBT)
- Dialectical behavioral therapy (DBT)
- Group therapy and support groups
- Individual therapy
- Holistic therapy
New Directions for Women Can Help Ladies Who Are Suffering From Alcoholism
If you or a woman close to you is struggling with depression, alcohol abuse, or a co-occurring disorder, we can help you. Here at New Directions for Women, we assist women in overcoming alcohol addictions. Contact us today to get started.
Don’t forget to share this post!
Alcoholic depression - symptoms, causes, diagnosis and treatment of alcoholic depression
Article reviewed by an expert:
MAKE AN APPOINTMENT
Alcoholic depression is an affective disorder that occurs in people suffering from alcoholism. Usually lasts from 2 weeks to 1 month. The maximum severity of symptoms is usually observed during the development of withdrawal symptoms. This condition often occurs after an exit from alcoholic psychosis, it can also develop during periods of binges and remissions. It is accompanied by a decrease in mood, longing, a feeling of guilt, uselessness and uselessness. Suicidal thoughts and actions are possible. The diagnosis is exposed on the basis of the anamnesis and clinical manifestations. Treatment is drug therapy combined with psychotherapy.
Usually lasts from 2 weeks to 1 month. The maximum severity of symptoms is usually observed during the development of withdrawal symptoms. This condition often occurs after an exit from alcoholic psychosis, it can also develop during periods of binges and remissions. It is accompanied by a decrease in mood, longing, a feeling of guilt, uselessness and uselessness. Suicidal thoughts and actions are possible. The diagnosis is exposed on the basis of the anamnesis and clinical manifestations. Treatment is drug therapy combined with psychotherapy.
Alcoholic depression - what is it?
Depression in alcoholism was described by Bleuler in 1920 under the name "alcoholic melancholia". Subsequent studies have confirmed both the presence of specific depressive and subdepressive conditions in alcoholics, and the complex, diverse links between alcoholism and depressive disorders. The frequency of development of the disease and the severity of symptoms directly correlates with the duration and severity of alcoholism. Middle-aged and elderly patients suffer from a depressive disorder more often than younger ones. Most of the patients are people over 40 years of age.
Middle-aged and elderly patients suffer from a depressive disorder more often than younger ones. Most of the patients are people over 40 years of age.
The average duration of post-alcoholic depression in alcoholism ranges from 2 weeks to 1 month. In severe cases, symptoms may persist for a year or more. The duration of the disease depends on the psycho-emotional characteristics, character traits, features of the constitution and the state of the body of patients. Women suffer more often than men, but in men, depression is more severe and is more often complicated by suicide attempts. The aggravation of male depression is facilitated by the fact that the representatives of the stronger sex rarely seek medical help during the development of the disease. Treatment of depression in alcoholism is carried out by specialists in the field of narcology, psychotherapy and psychiatry.
Causes of alcohol depression
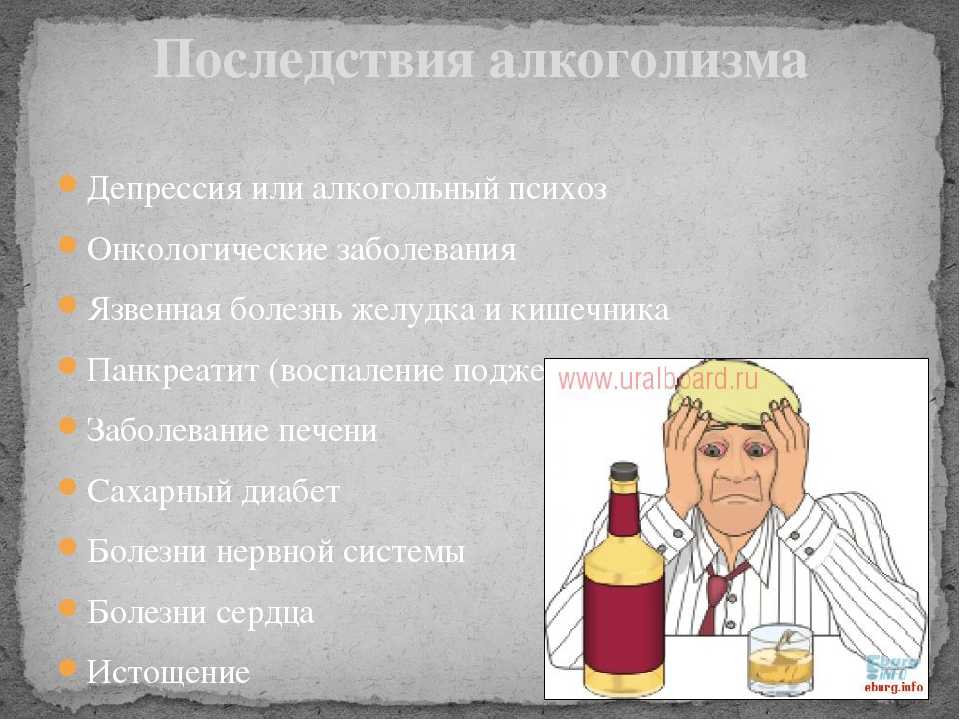
Depression in alcoholism is a multifactorial disease.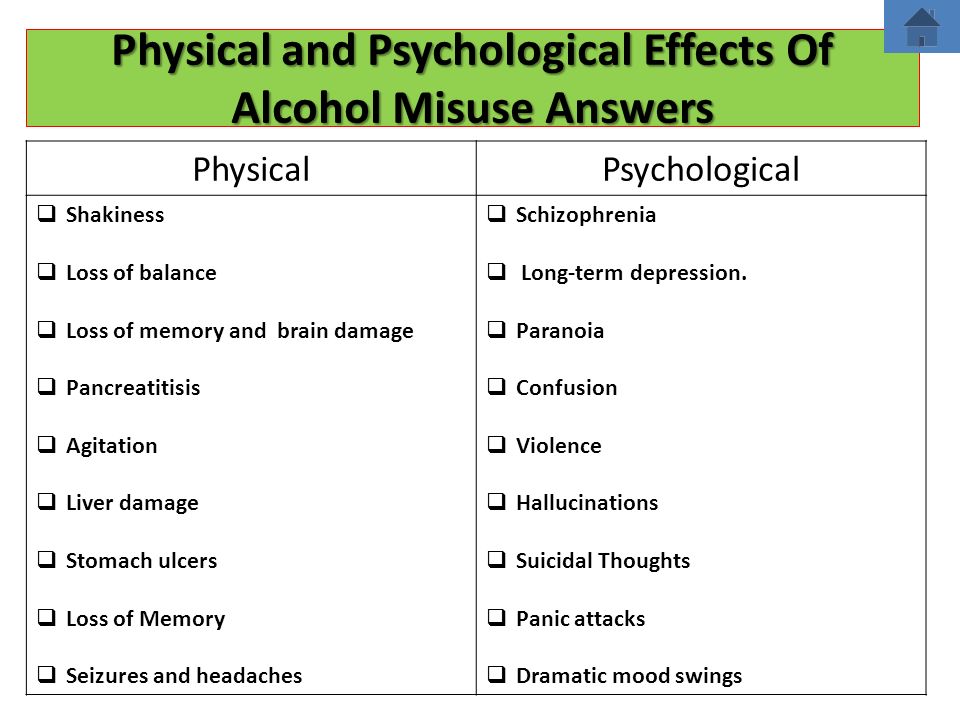 A whole range of circumstances leads to its development, including changes in general metabolism, disruption of brain receptors, personality changes, characteristic mental and somatic disorders, uncontrolled craving for alcohol, withdrawal phenomena when drinking alcohol is stopped, social and domestic problems. Narcologists constantly have to deal with alcoholic depression that develops in various clinical situations.
A whole range of circumstances leads to its development, including changes in general metabolism, disruption of brain receptors, personality changes, characteristic mental and somatic disorders, uncontrolled craving for alcohol, withdrawal phenomena when drinking alcohol is stopped, social and domestic problems. Narcologists constantly have to deal with alcoholic depression that develops in various clinical situations.
Alcoholic depression is part of the symptom complex of deprivation syndrome, acute alcohol intoxication, binge drinking and uncontrolled craving for alcohol. The most common cause of depressive mental disorder in alcoholics is withdrawal symptoms. Mental suffering of patients is provoked by severe physical and psychological discomfort and social problems, combined with a pathological need for alcohol.
Several bouts of depression occur in patients undergoing treatment for alcoholism in specialized clinics. In the initial stages of therapy, such patients develop a "sobriety phobia" - a pronounced fear of the possibility of life without alcohol. This stage is accompanied by a kind of mourning, due to the loss of alcohol. The second wave of depression is usually observed before the discharge of patients from the hospital, at the stage when the person no longer suffers from the consequences of intoxication. Longing for alcohol and psychological problems come to the fore.
This stage is accompanied by a kind of mourning, due to the loss of alcohol. The second wave of depression is usually observed before the discharge of patients from the hospital, at the stage when the person no longer suffers from the consequences of intoxication. Longing for alcohol and psychological problems come to the fore.
Sometimes depressive disorders develop against the background of remission, when a person feels lost, unable to fit in, “fallen out” of the normal rhythm of life and social environment, suffering from changes in habitual patterns of behavior, forced to solve numerous problems that arose during the period of alcoholism, without having enough external support and internal reserves. Such depressions can cause a breakdown and further alcoholization of the patient.
It should be borne in mind that the premorbid background is of some importance in the development of alcoholism. Even before the start of alcohol consumption, many patients have an increased tendency to mood swings, the development of asthenic conditions, depressive neurosis, subdepression and all kinds of borderline disorders.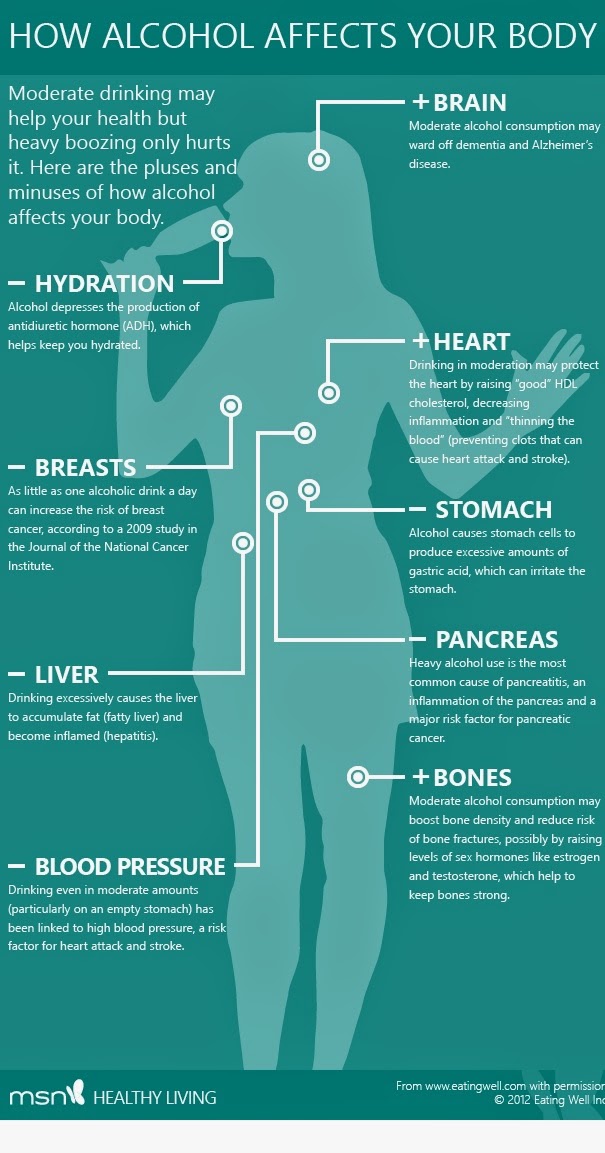 As alcoholism develops, this tendency is aggravated and aggravated due to secondary psycho-emotional and personality changes. There are also complications and neurosis after a complete rejection of alcohol.
As alcoholism develops, this tendency is aggravated and aggravated due to secondary psycho-emotional and personality changes. There are also complications and neurosis after a complete rejection of alcohol.
Symptoms and differential diagnosis of alcohol depression
Symptoms of depression in alcoholism are usually mild. Severe affective disorders are relatively rare. The mood is constantly depressed, the patient suffers from a feeling of emptiness and meaninglessness of existence. There is a feeling of loss of colors, the emotional colorlessness of the world, characteristic of depressive disorders. This perception causes depression and anxiety. Anhedonia develops - a person loses the ability to rejoice, cannot enjoy.
Psychological changes are combined with motor and intellectual retardation. Gait and movements slow down, the voice becomes quiet, monotonous. Mimic diversity disappears, the patient's face almost constantly retains a sad expression.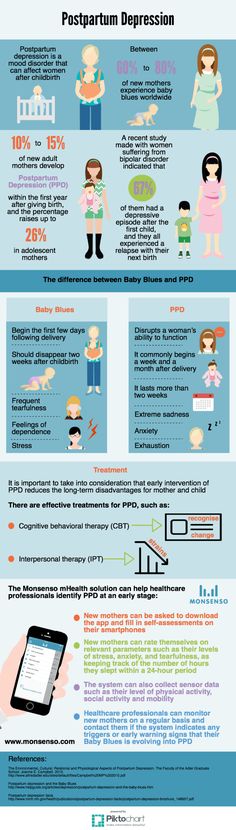 The patient is in a state of inactivity for a significant part of the time, responds to questions with a delay, has difficulty trying to understand someone else's thought or instruction. It is difficult for him to think and formulate statements.
The patient is in a state of inactivity for a significant part of the time, responds to questions with a delay, has difficulty trying to understand someone else's thought or instruction. It is difficult for him to think and formulate statements.
Hallucinations and delusions are usually absent. Often there are overvalued ideas of one's own guilt, uselessness, uselessness, fatal inadequacy and inadequacy. There is a tendency to self-abasement and self-accusation. The future looks bleak, hopeless, unpromising. Some patients consider some of their own previous actions as a serious crime. Many patients have thoughts of suicide, suicide attempts are possible. Sometimes (mainly in older patients) alcoholic depression is combined with increased anxiety.
Alcoholic depression is differentiated from other depressive disorders and conditions that include individual symptoms of depression. Unlike a depressive disorder, "drunken grief" is not accompanied by a sense of the colorlessness of the world and the loss of the ability to feel a variety of emotions. This state arises on an "emotional wave" and passes within a few hours, occasionally - several days.
This state arises on an "emotional wave" and passes within a few hours, occasionally - several days.
Separate elements of depression are often observed in withdrawal syndrome, but, unlike real alcoholic depression, they disappear after abstinence from drinking alcohol for 1-3 days. Reactive depression on the background of alcoholism in patients develops against the background of severe traumatic events (death of a relative, divorce, etc.); with alcoholic depression, there are no such events in the recent past of patients. Alcohol intake can provoke an exacerbation of other mental illnesses (psychogenic depression, depressive phase of bipolar affective disorder), therefore, when affective symptoms appear in patients with alcoholism, a thorough history taking is necessary.
Treatment and prognosis for alcoholic depression
Treatment of depression in alcoholism is carried out in a narcological hospital. In the process of treatment, drugs, psychotherapy and non-drug methods are used. Patients are prescribed antidepressants for alcoholism (usually SSRIs, tricyclic antidepressants, or MAO inhibitors). With increased anxiety and sleep disorders, short-term courses of drug therapy and treatment with the use of hypnotics and tranquilizers (diazepam, phenazepam, tazepam, etc.) are carried out. In parallel, they carry out detoxification therapy and provide psychological assistance.
Patients are prescribed antidepressants for alcoholism (usually SSRIs, tricyclic antidepressants, or MAO inhibitors). With increased anxiety and sleep disorders, short-term courses of drug therapy and treatment with the use of hypnotics and tranquilizers (diazepam, phenazepam, tazepam, etc.) are carried out. In parallel, they carry out detoxification therapy and provide psychological assistance.
With early detection and timely hospitalization, the prognosis for alcoholic depression in most cases is relatively favorable. Single depressive episodes, as a rule, quickly stop, suicidal intentions disappear, working capacity is restored (if it was not impaired due to other diseases). However, if the patient continues to drink alcohol, these conditions may recur and worsen as alcoholism develops.
Alcohol and stress | Depression after binge
Publication date: 09/20/2020 11:18
Depression with alcoholism
Alcohol and stress can cause anxiety and depression. The frequency of depression in people suffering from alcohol dependence varies according to various sources from 26 to 60%. Psychiatrist-narcologist Vladislav Sipovich, Chief Physician of the multidisciplinary Medical Center "Health Harmony", shares his knowledge on the development of a depressive symptomatic complex in patients with alcoholism at various stages of the disease and stages of its treatment.
The frequency of depression in people suffering from alcohol dependence varies according to various sources from 26 to 60%. Psychiatrist-narcologist Vladislav Sipovich, Chief Physician of the multidisciplinary Medical Center "Health Harmony", shares his knowledge on the development of a depressive symptomatic complex in patients with alcoholism at various stages of the disease and stages of its treatment.
What is primary in the occurrence of anxiety-depressive syndrome - depression or alcoholism?
In this pair of diseases it is difficult to determine what was the primary cause - depression or alcoholism. Their causal relationship is often implicit. Everything depends on the specific case. Quite often, a person in a stressful situation reaches for a glass of alcohol as a lifeline. Stress can be caused by various circumstances - conflicts at work and in the family, loss of income, death of loved ones, social problems, and even a simple quarrel in transport. The more unexpected the negative event, the stronger the stressful state caused by it.
On the other hand, it is known that chronic alcoholism causes a failure of the "stress" system, similar to depressive states with increased release of corticotropin and activation of the hypothalamic-pituitary system. It is corticotropin that is responsible for increasing the formation of cortisol in the adrenal glands, which is responsible for loss of appetite, the occurrence of subjective feelings of anxiety, immunosuppression and increased inflammatory reactions. These changes prolong depression after quitting alcohol for up to four weeks. With a combination of alcoholism and depression, the risk of their occurrence doubles, and long-term use of large doses of ethanol increases the risk of developing depression, suicide attempts and anxiety by 40%.
By the way, a huge role in the development of depressive states and alcohol dependence belongs to the common hereditary factor. It is responsible for 35-60% of these diseases.
Acupuncture treatment is an effective way to get rid of alcohol dependence in the early stages of the disease.
Can depression lead to a relapse of alcohol dependence in the process of remission of the disease?
Depressive conditions can occur at any stage of the treatment and rehabilitation of alcoholism, provoke a resumption of craving for alcohol and thus lead to a relapse of the disease. Therefore, it is important to diagnose and eliminate the cause of depression in a timely manner, otherwise the effectiveness of treatment and rehabilitation measures will be significantly reduced or practically reduced to zero.
What determines the duration of depression in alcoholism?
One of the most pressing questions - how long does depression last after drinking? First of all, it depends on the severity of depression with a hangover. In acute alcohol withdrawal syndrome, severe somatic, vegetative and neurological disorders are observed. In this state, depression is often combined with increased irritability, anxiety, and hysteria. Anxiety usually lasts 2-3 days, but depression after binge, accompanied by longing and self-blame, is more stable and lasts for 1-2 weeks.
How to treat depressive disorders in acute withdrawal syndrome?
Specific therapy is indispensable in this case. The use of benzodiazepine tranquilizers, GABA (gamma-aminobutyric acid) derivatives such as phenibut, antidepressants with sedative activity and lack of anticholinergic action, hepatoprotectors with antidepressant activity of the heptral type, as well as drugs that stabilize the autonomic system are shown.
How to get rid of depression after drinking?
After recovering from alcohol withdrawal, the main problem is becoming a stable and prolonged remission. The difficulty of solving this problem lies in the fact that over the course of many years of alcohol abuse, the patient has developed an alcoholic lifestyle and a psychological attraction to alcohol, the so-called alcohol dominant. This can lead to affective disorders during the rehabilitation process:
-
Hypochondria with numerous complaints of headache of unclear localization, pressure surges, frequent colds, skin rashes.
 This is due to the fact that prolonged alcohol consumption blurred the clinical picture of vegetative-somatic disorders and the patient seemed to be healthy. Cessation of drinking brings out all these disorders to their full extent, which is often considered to be the sick result of improper treatment. He can say that while he was drinking, he was healthy, but stopped - he began to get sick. Such conclusions can serve as an impetus for the resumption of the alcoholic status of the body, when alcohol is taken as a cure for manifested diseases. For the treatment of such patients, a combination of psychotherapy and medication is most effective.
This is due to the fact that prolonged alcohol consumption blurred the clinical picture of vegetative-somatic disorders and the patient seemed to be healthy. Cessation of drinking brings out all these disorders to their full extent, which is often considered to be the sick result of improper treatment. He can say that while he was drinking, he was healthy, but stopped - he began to get sick. Such conclusions can serve as an impetus for the resumption of the alcoholic status of the body, when alcohol is taken as a cure for manifested diseases. For the treatment of such patients, a combination of psychotherapy and medication is most effective. -
Apathy, which is often the result of the treatment of systematic household drinking without a significant decrease in social status, and is also observed in patients with high tolerance to alcohol and its uniform daily distribution. After the start of treatment, especially by the method of encoding or torpedo, active patients become sad, lethargic, lack of initiative, indifferent, avoiding contact with relatives and friends.
 Treatment of depressive-apathetic disorders is carried out with the help of positive, activating psychotherapy and stimulant antidepressants. Without medical help, apathetic manifestations can last for years and eventually lead to a relapse of the disease.
Treatment of depressive-apathetic disorders is carried out with the help of positive, activating psychotherapy and stimulant antidepressants. Without medical help, apathetic manifestations can last for years and eventually lead to a relapse of the disease. -
Asthenization, characteristic of patients with an initially weak psyche with laziness, contemplation, lethargy, avoidance of reality inherent in it. Alcohol literally transforms such patients, making them active, cheerful, with illusions of complete well-being and well-being. In this case, alcohol dependence is formed very quickly and then it is difficult to treat. Astheno-depressive disorders during remission are manifested in loss of interest in life, lethargy, weakness, unwillingness to take the initiative, to take any action. Long-term treatment with the connection of rational and family psychotherapy, biostimulants (ginseng, eleutherococcus, pantocrine, etc.), small doses of stimulating antidepressants.
-
Anxiety occurring in suspicious, indecisive, shy and anxious patients.
 Often, if necessary, to perform embarrassing actions (new acquaintances, business meetings, interviews, etc.), such people fall into pessimism, their mood deteriorates. Alcohol becomes a means of adaptation to such conditions, the absence of which during the period of remission becomes a real stress for the psyche, accustomed to solving problems with the help of alcohol intoxication. Anxious and suspicious character traits become pronounced, the mood steadily decreases, patients become gloomy, grouchy and irritable. All arising problems are exaggerated and become unsolvable. Treatment includes positive psychotherapy, mild neuroleptics, tranquilizers, and antidepressants.
Often, if necessary, to perform embarrassing actions (new acquaintances, business meetings, interviews, etc.), such people fall into pessimism, their mood deteriorates. Alcohol becomes a means of adaptation to such conditions, the absence of which during the period of remission becomes a real stress for the psyche, accustomed to solving problems with the help of alcohol intoxication. Anxious and suspicious character traits become pronounced, the mood steadily decreases, patients become gloomy, grouchy and irritable. All arising problems are exaggerated and become unsolvable. Treatment includes positive psychotherapy, mild neuroleptics, tranquilizers, and antidepressants. -
Dysphoria observed during the rehabilitation of patients with long-term alcoholism, binges with amnesia and aggression. For the first 3-6 months of rehabilitation, patients behave calmly, and then they become silent, gloomy, picky, tense, showing verbal aggression. Often there is a "dry hangover" in the morning with withdrawal symptoms.
 The appearance of such signs portends a relapse of the disease and requires the immediate connection of drug therapy.
The appearance of such signs portends a relapse of the disease and requires the immediate connection of drug therapy.
Thus, in conclusion, I can say that the treatment of depression after binge drinking, acute abstinence and other conditions of alcoholic disease, regardless of the type of depressive conditions, the stage of the disease, the stages of treatment and rehabilitation, must be carried out only under the supervision of an experienced psychiatrist-narcologist. Specialists of the Medical Center "Harmony of Health" will help you not only when the patient comes out of hard drinking, but also provide effective rehabilitation, stable remission and mild withdrawal of the patient from depression at adequate costs.
If your loved one, such as your wife or husband, suffers from alcohol addiction and depression, you can help them get started on treatment.
Cost of our services
* one bottle of solution, trace elements, vitamins, soothing.
** two bottles of solution, trace elements, various vitamins, sedatives and sleeping pills.
*** three bottles of solution, trace elements, various vitamins, sedatives and sleeping pills, protection against toxins.
**** also + heptral
Our narcologists
Sipovich Vladislav Alekseevich
psychiatrist, psychiatrist-narcologist, psychotherapist
Chief physician at the Medical Medical Center “Harmony of Health”
Education: Medical State University named after acad. I.P. Pavlova
Experience in providing narcological and psychotherapeutic assistance - 18 years, namely: home visits, outpatient and inpatient work
Andrey Vladimirovich Tkachenko
Psychiatrist-narcologist
Education :
in 2009 graduated from the medical faculty of St. Petersburg State Pediatric Medical Academy, in the specialty of the general profile.
Completed internship as a psychiatrist.
Work experience
For the last few years she has been working as a visiting psychiatrist-narcologist.