How to get someone help for depression
SAMHSA’s National Helpline | SAMHSA
Your browser is not supported
Switch to Chrome, Edge, Firefox or Safari
Main page content
-
SAMHSA’s National Helpline is a free, confidential, 24/7, 365-day-a-year treatment referral and information service (in English and Spanish) for individuals and families facing mental and/or substance use disorders.
Also visit the online treatment locator.
SAMHSA’s National Helpline, 1-800-662-HELP (4357) (also known as the Treatment Referral Routing Service), or TTY: 1-800-487-4889 is a confidential, free, 24-hour-a-day, 365-day-a-year, information service, in English and Spanish, for individuals and family members facing mental and/or substance use disorders.
This service provides referrals to local treatment facilities, support groups, and community-based organizations.
Also visit the online treatment locator, or send your zip code via text message: 435748 (HELP4U) to find help near you. Read more about the HELP4U text messaging service.
The service is open 24/7, 365 days a year.
English and Spanish are available if you select the option to speak with a national representative. Currently, the 435748 (HELP4U) text messaging service is only available in English.
In 2020, the Helpline received 833,598 calls. This is a 27 percent increase from 2019, when the Helpline received a total of 656,953 calls for the year.
The referral service is free of charge. If you have no insurance or are underinsured, we will refer you to your state office, which is responsible for state-funded treatment programs. In addition, we can often refer you to facilities that charge on a sliding fee scale or accept Medicare or Medicaid. If you have health insurance, you are encouraged to contact your insurer for a list of participating health care providers and facilities.
If you have health insurance, you are encouraged to contact your insurer for a list of participating health care providers and facilities.
The service is confidential. We will not ask you for any personal information. We may ask for your zip code or other pertinent geographic information in order to track calls being routed to other offices or to accurately identify the local resources appropriate to your needs.
No, we do not provide counseling. Trained information specialists answer calls, transfer callers to state services or other appropriate intake centers in their states, and connect them with local assistance and support.
-
Suggested Resources
What Is Substance Abuse Treatment? A Booklet for Families
Created for family members of people with alcohol abuse or drug abuse problems. Answers questions about substance abuse, its symptoms, different types of treatment, and recovery. Addresses concerns of children of parents with substance use/abuse problems.
Addresses concerns of children of parents with substance use/abuse problems.It's Not Your Fault (NACoA) (PDF | 12 KB)
Assures teens with parents who abuse alcohol or drugs that, "It's not your fault!" and that they are not alone. Encourages teens to seek emotional support from other adults, school counselors, and youth support groups such as Alateen, and provides a resource list.After an Attempt: A Guide for Taking Care of Your Family Member After Treatment in the Emergency Department
Aids family members in coping with the aftermath of a relative's suicide attempt. Describes the emergency department treatment process, lists questions to ask about follow-up treatment, and describes how to reduce risk and ensure safety at home.Family Therapy Can Help: For People in Recovery From Mental Illness or Addiction
Explores the role of family therapy in recovery from mental illness or substance abuse. Explains how family therapy sessions are run and who conducts them, describes a typical session, and provides information on its effectiveness in recovery.
For additional resources, please visit the SAMHSA Store.
Last Updated: 08/30/2022
Helping Someone with Depression - HelpGuide.org
depression
Your support and encouragement can play an important role in your loved one's recovery. Here's how to make a difference.
How can I help someone with depression?
Depression is a serious but treatable disorder that affects millions of people, from young to old and from all walks of life. It gets in the way of everyday life, causing tremendous pain, hurting not just those suffering from it but also impacting everyone around them.
If someone you love is depressed, you may be experiencing any number of difficult emotions, including helplessness, frustration, anger, fear, guilt, and sadness. These feelings are all normal. It’s not easy dealing with a friend or family member’s depression. And if you neglect your own health, it can become overwhelming.
That said, your companionship and support can be crucial to your loved one’s recovery. You can help them to cope with depression symptoms, overcome negative thoughts, and regain their energy, optimism, and enjoyment of life. Start by learning all you can about depression and how to best talk about it with your friend or family member. But as you reach out, don’t forget to look after your own emotional health—you’ll need it to provide the full support your loved one needs.
You can help them to cope with depression symptoms, overcome negative thoughts, and regain their energy, optimism, and enjoyment of life. Start by learning all you can about depression and how to best talk about it with your friend or family member. But as you reach out, don’t forget to look after your own emotional health—you’ll need it to provide the full support your loved one needs.
Recognizing depression symptoms in a loved one
Family and friends are often the first line of defense in the fight against depression. That's why it's important to understand the signs and symptoms of depression. You may notice the problem in a depressed loved one before they do, and your influence and concern can motivate them to seek help.
Be concerned if your loved one:
Doesn't seem to care about anything anymore. Has lost interest in work, sex, hobbies, and other pleasurable activities. Has withdrawn from friends, family, and other social activities.
Expresses a bleak or negative outlook on life.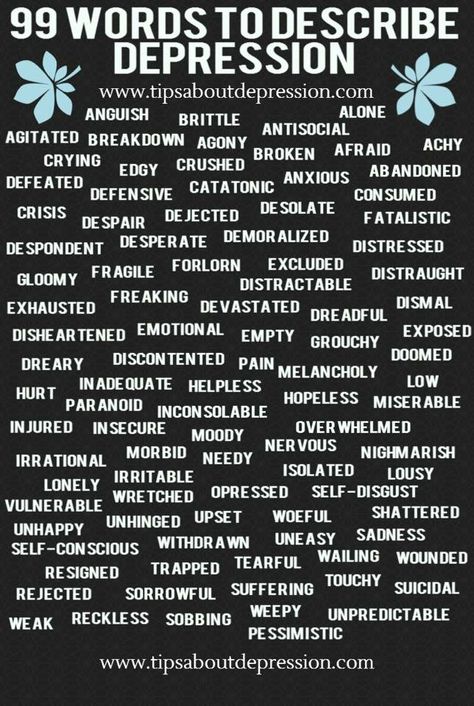 Is uncharacteristically sad, irritable, short-tempered, critical, or moody; talks about feeling “helpless” or “hopeless.”
Is uncharacteristically sad, irritable, short-tempered, critical, or moody; talks about feeling “helpless” or “hopeless.”
Frequently complains of aches and pains such as headaches, stomach problems, and back pain. Or complains of feeling tired and drained all the time.
Sleeps less than usual or oversleeps. Has become indecisive, forgetful, disorganized, and “out of it.”
Eats more or less than usual, and has recently gained or lost weight.
Drinks more or abuses drugs, including prescription sleeping pills and painkillers, as a way to self-medicate how they're feeling.
Affordable private online therapy. Get instant help, on any device, wherever you are in the world. Start feeling better today!
GET 20% OFF
With over 25,000 licensed counselors, BetterHelp has a therapist that fits your needs. Sign up today and get matched.
GET 20% OFF
Get professional online counseling for relationship or marital issues. It’s confidential, convenient, and easy to get started.
It’s confidential, convenient, and easy to get started.
GET 20% OFF
How to talk to someone about depression
Sometimes it is hard to know what to say when speaking to someone about depression. You might fear that if you bring up your worries the person will get angry, feel insulted, or ignore your concerns. You may be unsure what questions to ask or how to be supportive.
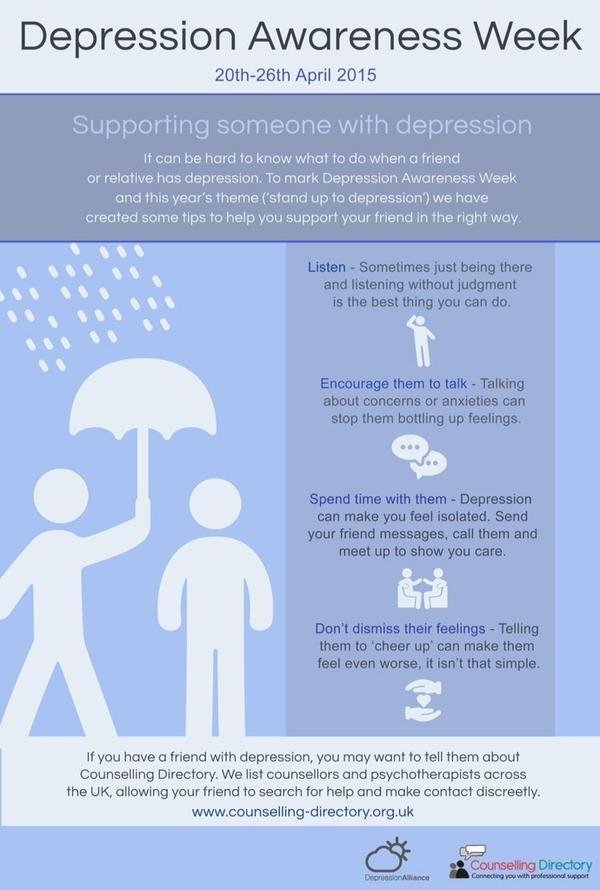
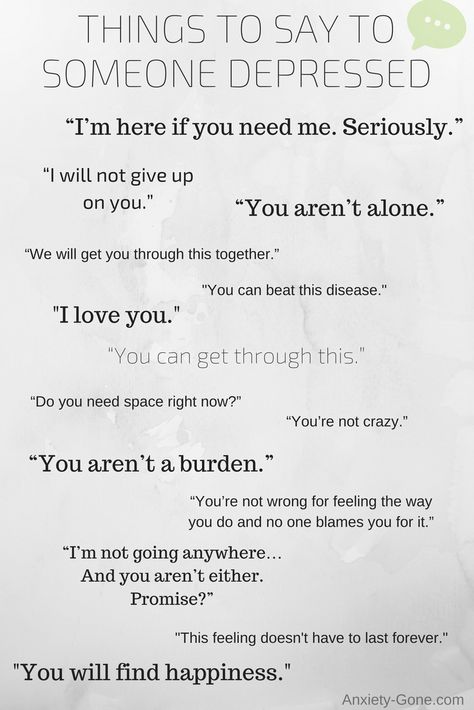
If you don't know where to start, the following suggestions may help. But remember that being a compassionate listener is much more important than giving advice. You don't have to try to “fix” your friend or family member; you just have to be a good listener. Often, the simple act of talking face to face can be an enormous help to someone suffering from depression. Encourage the depressed person to talk about their feelings, and be willing to listen without judgment.
Don't expect a single conversation to be the end of it. Depressed people tend to withdraw from others and isolate themselves. You may need to express your concern and willingness to listen over and over again. Be gentle, yet persistent.
You may need to express your concern and willingness to listen over and over again. Be gentle, yet persistent.
ADVERTISEMENT
Starting the conversation
Finding a way to start a conversation about depression with your loved one is always the hardest part. You could try saying:
- “I have been feeling concerned about you lately.”
- “Recently, I have noticed some differences in you and wondered how you are doing.”
- “I wanted to check in with you because you have seemed pretty down lately.”
Once you're talking, you can ask questions such as:
- “When did you begin feeling like this?”
- “Did something happen that made you start feeling this way?”
- “How can I best support you right now?”
- “Have you thought about getting help?”
Remember, being supportive involves offering encouragement and hope. Very often, this is a matter of talking to the person in language that they will understand and can respond to while in a depressed state of mind.
| Tips for Talking about Depression |
| What you CAN say that helps: |
|
| What you should AVOID saying: |
|
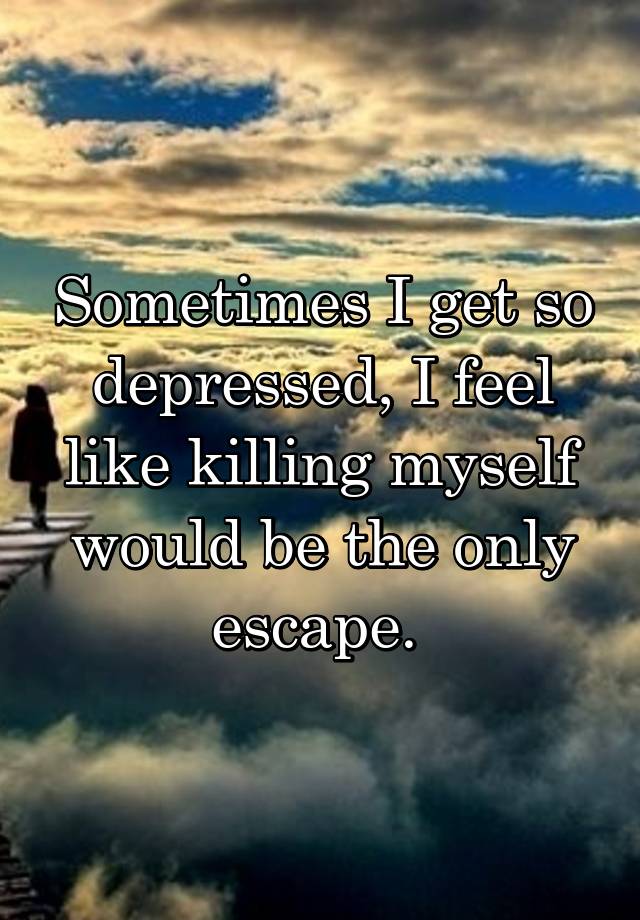
The risk of suicide is real
What to do in a crisis situation
If you believe your loved one is at an immediate risk for suicide, do NOT leave them alone.
In the U.S., dial 911 or call the 988 Suicide and Crisis Lifeline at 988.
In other countries, call your country's emergency services number or visit IASP to find a suicide prevention helpline.
It may be hard to believe that the person you know and love would ever consider something as drastic as suicide, but a depressed person may not see any other way out. Depression clouds judgment and distorts thinking, causing a normally rational person to believe that death is the only way to end the pain they're feeling.
Since suicide is a very real danger when someone is depressed, it's important to know the warning signs:
- Talking about suicide, dying, or harming oneself; a preoccupation with death
- Expressing feelings of hopelessness or self-hate
- Acting in dangerous or self-destructive ways
- Getting affairs in order and saying goodbye
- Seeking out pills, weapons, or other lethal objects
- A sudden sense of calm after depression
If you think a friend or family member might be considering suicide, don't wait, talk to them about your concerns.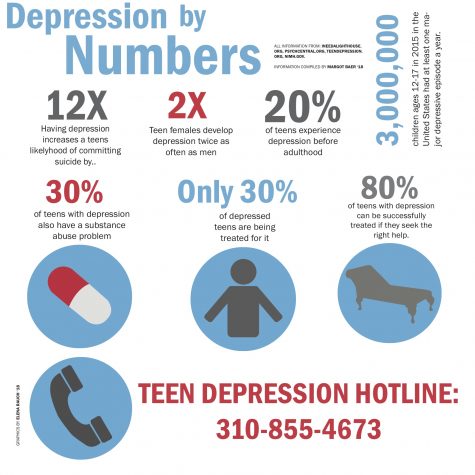 Many people feel uncomfortable bringing up the topic but it is one of the best things you can do for someone who is thinking about suicide. Talking openly about suicidal thoughts and feelings can save a person's life, so speak up if you're concerned and seek professional help immediately!
Many people feel uncomfortable bringing up the topic but it is one of the best things you can do for someone who is thinking about suicide. Talking openly about suicidal thoughts and feelings can save a person's life, so speak up if you're concerned and seek professional help immediately!
Encouraging the person to get help
While you can't control someone else's recovery from depression, you can start by encouraging the depressed person to seek help. Getting a depressed person into treatment can be difficult. Depression saps energy and motivation, so even the act of making an appointment or finding a doctor can seem daunting to your loved one. Depression also involves negative ways of thinking. The depressed person may believe that the situation is hopeless and treatment pointless.
Because of these obstacles, getting your loved one to admit to the problem—and helping them see that it can be solved—is an essential step in depression recovery.
If your friend or family member resists getting help:
Suggest a general check-up with a physician. Your loved one may be less anxious about seeing a family doctor than a mental health professional. A regular doctor's visit is actually a great option, since the doctor can rule out medical causes of depression. If the doctor diagnoses depression, they can refer your loved one to a psychiatrist or psychologist. Sometimes, this “professional” opinion makes all the difference.
Your loved one may be less anxious about seeing a family doctor than a mental health professional. A regular doctor's visit is actually a great option, since the doctor can rule out medical causes of depression. If the doctor diagnoses depression, they can refer your loved one to a psychiatrist or psychologist. Sometimes, this “professional” opinion makes all the difference.
Offer to help the depressed person find a doctor or therapist and go with them on the first visit. Finding the right treatment provider can be difficult, and is often a trial-and-error process. For a depressed person already low on energy, it is a huge help to have assistance making calls and looking into the options.
Encourage your loved one to make a thorough list of symptoms and ailments to discuss with the doctor. You can even bring up things that you have noticed as an outside observer, such as, “You seem to feel much worse in the mornings,” or “You always get stomach pains before work. ”
”
Supporting your loved one's treatment
One of the most important things you can do to help a friend or relative with depression is to give your unconditional love and support throughout the treatment process. This involves being compassionate and patient, which is not always easy when dealing with the negativity, hostility, and moodiness that go hand in hand with depression.
Provide whatever assistance the person needs (and is willing to accept). Help your loved one make and keep appointments, research treatment options, and stay on schedule with any treatment prescribed.
Have realistic expectations. It can be frustrating to watch a depressed friend or family member struggle, especially if progress is slow or stalled. Having patience is important. Even with optimal treatment, recovery from depression doesn't happen overnight.
Lead by example. Encourage the person to lead a healthier, mood-boosting lifestyle by doing it yourself: maintain a positive outlook, eat better, avoid alcohol and drugs, exercise, and lean on others for support.
Encourage activity. Invite your loved one to join you in uplifting activities, like going to a funny movie or having dinner at a favorite restaurant. Exercise is especially helpful, so try to get your depressed loved one moving. Going on walks together is one of the easiest options. Be gently and lovingly persistent—don't get discouraged or stop asking.
Pitch in when possible. Seemingly small tasks can be very hard for someone with depression to manage. Offer to help out with household responsibilities or chores, but only do what you can without getting burned out yourself!
Taking care of yourself
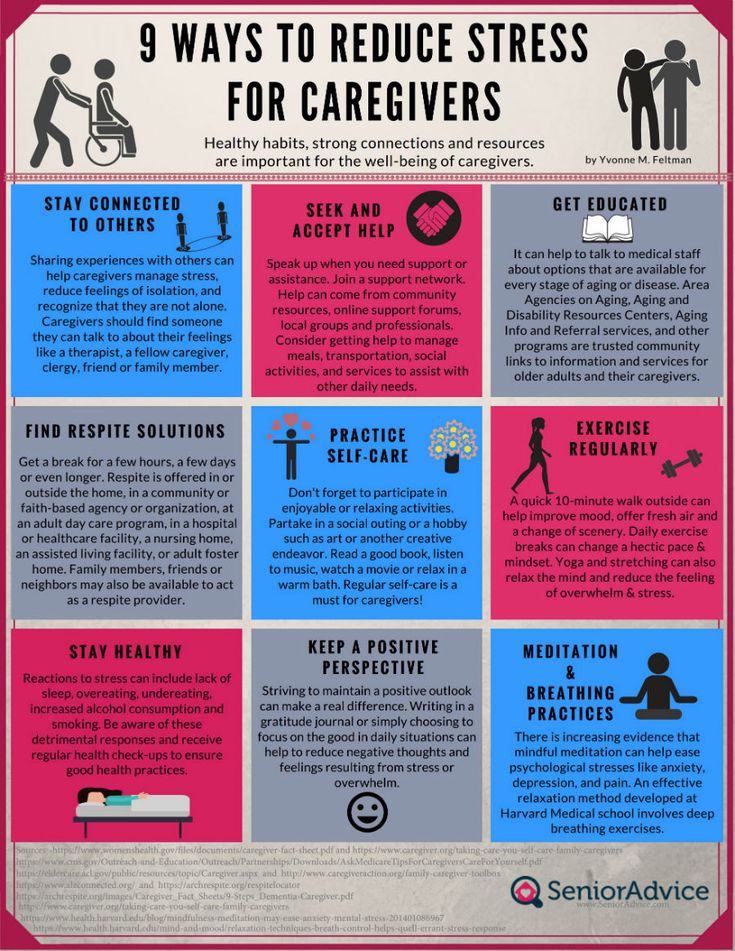
There's a natural impulse to want to fix the problems of people we care about, but you can't control someone else's depression. You can, however, control how well you take care of yourself. It's just as important for you to stay healthy as it is for the depressed person to get treatment, so make your own well-being a priority.
Remember the advice of airline flight attendants: put on your own oxygen mask before you assist anyone else.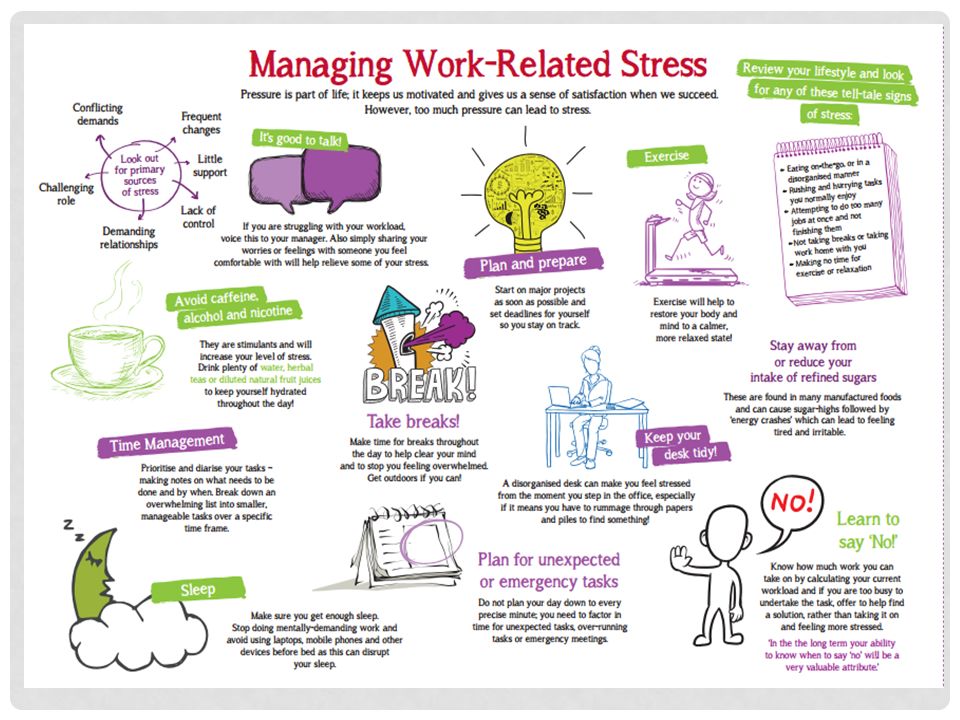 In other words, make sure your own health and happiness are solid before you try to help someone who is depressed. You won't do your friend or family member any good if you collapse under the pressure of trying to help. When your own needs are taken care of, you'll have the energy you need to lend a helping hand.
In other words, make sure your own health and happiness are solid before you try to help someone who is depressed. You won't do your friend or family member any good if you collapse under the pressure of trying to help. When your own needs are taken care of, you'll have the energy you need to lend a helping hand.
Speak up for yourself. You may be hesitant to speak out when the depressed person in your life upsets you or lets you down. However, honest communication will actually help the relationship in the long run. If you're suffering in silence and letting resentment build, your loved one will pick up on these negative emotions and feel even worse. Gently talk about how you're feeling before pent-up emotions make it too hard to communicate with sensitivity.
Set boundaries. Of course you want to help, but you can only do so much. Your own health will suffer if you let your life be controlled by your loved one's depression. You can't be a caretaker round the clock without paying a psychological price. To avoid burnout and resentment, set clear limits on what you are willing and able to do. You are not your loved one's therapist, so don't take on that responsibility.
To avoid burnout and resentment, set clear limits on what you are willing and able to do. You are not your loved one's therapist, so don't take on that responsibility.
Stay on track with your own life. While some changes in your daily routine may be unavoidable while caring for your friend or relative, do your best to keep appointments and plans with friends. If your depressed loved one is unable to go on an outing or trip you had planned, ask a friend to join you instead.
Seek support. You are NOT betraying your depressed relative or friend by turning to others for support. Joining a support group, talking to a counselor or clergyman, or confiding in a trusted friend will help you get through this tough time. You don't need to go into detail about your loved one's depression or betray confidences; instead focus on your emotions and what you are feeling. Make sure you can be totally honest with the person you turn to—choose someone who will listen without interruption and without judging you.
Authors: Melinda Smith, M.A., Lawrence Robinson, and Jeanne Segal, Ph.D.
- References
How to help in an emotional crisis. (n.d.). https://www.apa.org. Retrieved July 23, 2021, from https://www.apa.org/topics/mental-health/help-emotional-crisis
Gariépy, G., Honkaniemi, H., & Quesnel-Vallée, A. (2016). Social support and protection from depression: Systematic review of current findings in Western countries. The British Journal of Psychiatry, 209(4), 284–293. https://doi.org/10.1192/bjp.bp.115.169094
Belmaker, R. H., & Agam, G. (2008). Major Depressive Disorder. New England Journal of Medicine, 358(1), 55–68. https://doi.org/10.1056/NEJMra073096
Lee, S. L., Pearce, E., Ajnakina, O., Johnson, S., Lewis, G., Mann, F., Pitman, A., Solmi, F., Sommerlad, A., Steptoe, A., Tymoszuk, U., & Lewis, G. (2021). The association between loneliness and depressive symptoms among adults aged 50 years and older: A 12-year population-based cohort study.
 The Lancet Psychiatry, 8(1), 48–57. https://doi.org/10.1016/S2215-0366(20)30383-7
The Lancet Psychiatry, 8(1), 48–57. https://doi.org/10.1016/S2215-0366(20)30383-7Elmer, T., & Stadtfeld, C. (2020). Depressive symptoms are associated with social isolation in face-to-face interaction networks. Scientific Reports, 10(1), 1444. https://doi.org/10.1038/s41598-020-58297-9
Depressive Disorders. (2013). In Diagnostic and Statistical Manual of Mental Disorders. American Psychiatric Association. https://doi.org/10.1176/appi.books.9780890425787.x04_Depressive_Disorders
Helping Someone Receive Treatment – What to do (and not to do) when trying to help a loved one get help for depression. (Families for Depression Awareness)
Helping a Friend or Family Member with Depression or Bipolar Disorder – Downloadable brochure with tips for helping your loved one while also taking care of yourself. (Depression and Bipolar Support Alliance)
What is the role of the family caregiver? – Tips on how families can work together to manage depression treatment. (Families for Depression Awareness)
(Families for Depression Awareness)
How to Help Someone in Crisis – Advice on how to deal with a depression crisis, including situations where hospitalization is necessary. (Depression and Bipolar Support Alliance)
Around the web
Last updated: October 21, 2022
How to Help a Depressed Person - Such Things
Every week, Such Things answer questions from readers. Today we will talk about depression, or rather, how to be a good friend for a person who finds himself in this state.
***
Approximately one in four has experienced depression at least once in their life. Although sometimes we, wringing our hands, call depression just an attack of bad mood. It is necessary to distinguish between blues, a mild depressive state (minor depression, subdepression) and a real clinical depression, which can drag on for several months.
Clinical depression is characterized by three main symptoms:
- Bad mood. But not the kind that usually happens after a hard day or week.
 With depression, a person loses the ability to rejoice, does not enjoy the usual things - food, communication with friends, sex, music, films. This condition is called anhedonia.
With depression, a person loses the ability to rejoice, does not enjoy the usual things - food, communication with friends, sex, music, films. This condition is called anhedonia. - Violation of thinking. It is difficult for a depressed person to think, it seems that thoughts are “like jelly”. Work is slower.
- Motor retardation. Depression is always accompanied by a constant feeling of fatigue. Forcing yourself to go somewhere in this state is extremely difficult.
If these symptoms are observed for more than a month, then this is a reason to see a doctor, but you can cope with mild depression on your own, with the help of relatives and psychotherapy. But relatives should remember a few simple rules - what to do, and what should never be said. That's what psychologists recommend.
Let the person experience this state
Let's say your loved one experienced a failure, his expectations were not fulfilled, his plans were not realized. He is very upset, he is not happy with what he usually loves. Don't rush him. Say phrases: “Yes, stop thinking about it!” or “We need to move forward!” - it is forbidden. The state of sadness is not so bad for a person. Sadness allows you to relax a little after the race that was before, to come to your senses, to rethink, so that after that you can smoothly get out of this state.
He is very upset, he is not happy with what he usually loves. Don't rush him. Say phrases: “Yes, stop thinking about it!” or “We need to move forward!” - it is forbidden. The state of sadness is not so bad for a person. Sadness allows you to relax a little after the race that was before, to come to your senses, to rethink, so that after that you can smoothly get out of this state.
Be honest
“Yes, you failed to achieve the goal, but let's take a break and try again if you want, no - then try yourself in something else.”
Do not discount failure
Phrases: “Forget it”, “Stop it”, “Your failures mean nothing” will only make things worse. A person can and should learn from his failures a lesson. It just takes time.
Recognize the importance of this situation
“Yes, you tried, it didn't work, but it's important that you did it! The feelings you are experiencing right now are very important. Sadness, loss of strength - all this is natural, but I am there and will help you.
Sadness, loss of strength - all this is natural, but I am there and will help you.
Be careful with jokes
Do not joke rudely, scoff, ironically over the situation. Of course, it’s hard when a person close to you is in a bad mood, you want him to smile, and not go gloomy. It may seem that if you joke and make fun of the situation, then he will immediately cheer up and everything will immediately go smoothly. But it will most likely only get worse. Any rude intrusion, criticism will prevent you from getting out of a depressive state.
Do not force
It is strictly forbidden to forcefully drag a person to parties and walks in a depressed state. The mistake is that when we see a depressed person, we want to give him the energy of life. We say: "Look how great it all is!" But a person is simply not physically able to appreciate it. When he sees how people enjoy life, this only worsens his condition, he begins to wonder: "Why can't I do that?"
No aggression
Seeing that a person closes even more, in no case should one speak aggressively: “Why are you still in anguish?”, “Why are you sitting and being sad?”, “Pull yourself together, rag!” Such phrases are forbidden even as a joke.
Be patient
Do not do anything excessive, be more restrained and calm. But if the condition of a person close to you does not improve within a month, this is a reason to contact a psychotherapist or psychiatrist. Perhaps we are talking about clinical depression, which must be treated with medication.
Help get rid of the fear of specialists
Many patients with clinical depression are afraid to go to a psychotherapist or psychiatrist. They think: “What if this is something worse than just depression, what if I’m going crazy” or “I can handle it myself”. Close people at this point should gently and carefully explain: “You know, it seems to be depression, and I read that it is completely curable. We will find a way out. Let's go to the specialist together. It seems to me that this will help you get out of this state.
Stay close
Stay close or nearby so your friend always knows that if they need help they will have someone to turn to.
Do you want us to send you the best texts of "Such cases" to your e-mail? Subscribe to our weekly newsletter!
How to help a person with the development of a depressive state?
Depression: concept, mechanism of occurrence
Depression can be described as a mental disorder in which a person a period of time, bad mood persists and the loss of the ability to experience pleasure from any positive events in life.
A person suffering from a depressive disorder is characterized by such conditions as: depression, anxiety, melancholy and depressed mood.
According to official data published by the World Health Organization (WHO), this disease affects nearly 350 million people worldwide. Treat depression only 50% of this number. In other cases, the absence vital energy and interest are attributed to the blues, laziness or bad character.
What happens in the body of a person suffering from depression?
The limbic system is responsible for sleep, memory, emotions and other processes in the human body. It is a combination of various structures of the brain.
It is a combination of various structures of the brain.
In a healthy person, the components of the limbic system work according to the following principle:
- Prefrontal cortex - responsible for processing information, prevents excessive activity of the tonsils. Stimulates a person's motivation for something, influences decision-making and behavior.
- Hippocampus - responsible for emotions (both positive and negative), provides a transition of short-term long-term memory, helps to keep attention and concentration on something.
- Amygdala - activated at the time of the appearance of fear in a person and feelings of anxiety. This structure forms memories associated with experienced emotions.
With depression, a number of changes occur in the functioning of the limbic system. There is a lack of neurotransmitters in the body (chemicals that provide contacts between nerve cells).
As a result of this failure, all other structures begin to work incorrectly:
- The prefrontal cortex does not process information correctly, stops inhibiting the activity of the amygdala.
 This results in symptoms such as: a change in a person’s mood, the appearance of a feeling of anxiety, loss of motivation to do something.
This results in symptoms such as: a change in a person’s mood, the appearance of a feeling of anxiety, loss of motivation to do something. - The volume of the hippocampus decreases, as a result of which a person's memory deteriorates, he becomes distracted and cannot concentrate.
- As a result of a change in the size of the amygdala, a person develops fear, anxiety, mental disorder.
It has been established that during depression in the human body there is a lack of such neurotransmitters as: dopamine, serotonin and norepinephrine. In some cases, there is also a decrease in endorphins.
Main symptoms of depression
To better understand what depression is in a person, it is necessary to consider the main symptoms of this condition:
- Decreased self-esteem - a person ceases to adequately evaluate himself, it seems to him that that he is the worst and does not deserve anything good in life.
- Thinking errors - a person has attitudes in his head: "no one needs me", “no one understands me”, “everything around is very bad”. He feels alienated and alone.
- Loss of interest in what is happening around - the patient becomes indifferent to his life, former aspirations, interests and hobbies. Sometimes even food loses its former bright taste.
- Lack of desire to do anything - ordinary things (cleaning, washing or cooking) for a person with depression is difficult. He has to do his best.
- Sleep and appetite disorder - interest in food may be lost, due to which a person begins to lose weight rapidly. The reverse situation is also possible - constant uncontrolled overeating. In this way, the patient tries relieve tension. Also, depressive disorders are often accompanied by insomnia or constant drowsiness.
- Mental and motor retardation - such symptoms are characteristic of depression, which has turned into a severe form.
 The sharpness of the mind disappears, thoughts are confused, it is very difficult for a person to concentrate on anything.
The sharpness of the mind disappears, thoughts are confused, it is very difficult for a person to concentrate on anything. - Increased vulnerability - such people are much easier to hurt and offend. Moreover, such a reaction can occur even on the most harmless things or words.
- In advanced cases, persistent apathy can eventually lead to suicidal thoughts. Many cases are known when people with depression commit suicide.
- Depression is often accompanied by deterioration in physical condition. For example, you may receive: permanent headaches pain, indigestion, a feeling of heaviness in the chest, pain in the heart, etc.
Depending on the nature of the course of the disease and the degree of neglect, certain symptoms may manifest themselves more or lesser degree. Some of them are completely absent, but the problem still exists and needs to be addressed.
How is the disease progressing?
In most cases, depression develops gradually from small to large.
The first faint signals appear first. For example, sleep problems may appear, a person becomes irritable, unwilling to perform his usual duties.
As the disease progresses, the symptoms intensify and after one to two months all typical signs of depression.
The course of this disease is uneven. Some people experience periodic worsening of the condition. Wherein the rest of the time they are completely normal.
On average, a depressive disorder can last 6 to 8 months. If apathy dragged on for more long period, then we are talking about chronic depression (2 or more years).
Causes and factors that provoke the development of depression
Depressive disorder can develop for a variety of reasons. The main of them include the following situations: high position in society, etc. In this case, a person may develop reactive depression, as a reaction to the events taking place around.
 As a result, the endless pursuit of perfection leads to burnout and loss of interest.
As a result, the endless pursuit of perfection leads to burnout and loss of interest. People with low self-esteem are also prone to depression. They believe that they are not worthy of a good life and cannot earn the recognition of others.
 For example, it occurs in 50% of people with hypothyroidism. (a malfunction of the thyroid gland, as a result of which the production of hormones by it decreases).
For example, it occurs in 50% of people with hypothyroidism. (a malfunction of the thyroid gland, as a result of which the production of hormones by it decreases). In addition to direct causes, there are also many additional factors that provoke the appearance of depressive disorders. These include: pregnancy, psychological trauma suffered in childhood, somatics, etc.
Classification of depressive states
Today there are many different approaches to the classification of depressive disorders. Some of them are already outdated, others have not yet been fully proven.
We will single out several officially confirmed forms of depression that are included in the ICD-10 (international classifier of diseases).
Depending on the nature of the course of the disease, depression is divided into three types:
- mild - has no pronounced symptoms, so it is often confused with short-term melancholy and sadness.
- medium - clinical signs begin to appear more clearly. The man still has strength be a full member of society
- severe - this form has pronounced symptoms. The person practically loses the ability to normally function in society, delusions appear, and sometimes hallucinations.
Depressive disorders are divided into several groups depending on the cause of development. Main forms of depression:
- endogenous - the disease develops for no apparent reason,
- reactive or psychogenic - characterized as a reaction of the human psyche to difficult events, happening around (death of a loved one, bankruptcy, etc.),
- seasonal - occurs periodically, usually it is associated with a lack of heat and bright sunlight,
- pharmacogenic - is a side effect of taking certain types of drugs. For example, the use of neuroleptics can lead to the development of neuroleptic depression,
- somatogenic - appears as a result of somatic diseases (for example, against the background of atherosclerosis, head trauma, etc.
 ),
), - postpartum - 12-16% of women experience it in the first months after the birth of a child.
In addition to the above classifications, many other types of depression are known. For example, depending on predominant symptoms, it may be anxious, melancholy, lethargic and undifferentiated.
According to the nature of the course, depression is divided into:
- unipolar (stable condition during the entire period of illness),
- bipolar (symptoms of depression may change into a phase of mania),
- dysthymia (preservation of apathy for 2 or more years without pronounced symptoms),
- cyclothymia (regular changes in mood from an excited state to apathy and vice versa).
Features of the manifestation of depressive states
Depressive disorder can be different for each person. Gender plays an important role here. the patient's affiliation and age.
Women's, men's and children's depression have been found to have their own characteristics. Let's look at them in more detail.
Among women
Women are more prone to depression. Of all the cases, two-thirds are female.
For example, the famous German psychologist W. Nuber associates this pattern with a high level of stress women's load (as opposed to men's).
The main causes of depression in women include:
- hormonal changes occurring in the body (as a result of a change in the menstrual cycle (PMS), pregnancy, miscarriage, menopause, etc.),
- premenstrual dystrophic disorder (PMDD) is considered a more severe form of PMS. In this case, before the onset of menstruation, a woman begins to have a pronounced depression,
- postpartum period - against the background of a radical restructuring of the body as a result of the birth of a child, many women develop depression.
 Often it is the result of an exacerbation of mental disorders, who were present before pregnancy,
Often it is the result of an exacerbation of mental disorders, who were present before pregnancy, - emotional burnout - this especially often happens to mothers in the first year of a baby's life, when he needs in especially careful care. Constant lack of sleep, lack of time for yourself, poor nutrition - all of these factors can result in a depressive disorder.
Regardless of the cause of the appearance, it is very important to notice the first signs of the disease in time and contact for qualified medical care. It is much easier to solve the problem at the initial stage than to fight with severe consequences of a neglected form of depression.
In men
Men are less likely to develop depression than women, but they are also susceptible to this disease.
The main factors provoking the onset of depression in a man are most often:
- stressful work,
- problems in personal life,
- lack of any significant achievements,
- unsuccessful marriage, etc.

During depression, men may exhibit the following behaviors: maximum immersion in work or any other activity, alcohol abuse, aggression and irritability, etc. may appear.
In children
It may seem strange to some, but not only adults are subject to depression. Often there are cases when this disease develops in children and adolescents.
It has been found that depression occurs in almost 5% of children and adolescents aged 10-16 years. This disease often leads to an increase in morbidity, disability and an increase in the frequency of suicide.
Causes of depression in children and adolescents:
- difficult relationship with parents (use of physical and emotional pressure),
- difficulties with social adaptation in the team (lack of friends, ridicule of classmates, etc.),
- suffering from excessive parental care or vice versa indifference,
- unhappy love in adolescence, etc.

Depression or temporary blues: how to recognize?
Depression is often confused with the usual apathy that every person experiences from time to time. Indeed, at the initial stage, these two states are quite easy to confuse. However, as the disease progresses, the typical signs of depression begin to appear more clearly.
Let's look at a few key differences between depression and temporary blues:
- Prolonged depression - simple apathy usually does not last more than a couple of days. If a bad mood persists for a long period (from several weeks or more), then this is a reason to think. There is a high probability that depression is approaching you.
- Lack of response to positive events - probably many of us have experienced a situation that when a bad mood immediately changed after receiving positive news.
In the case of depression, everything is much more complicated. Here, even pleasant events cannot affect the depressed human condition.
- The appearance of additional symptoms - depression is often accompanied by fatigue and weakness, inability to concentrate one's attention, loss of working capacity, irritability, fasting or vice versa overeating, etc.
With the development of a depressive state, it is very important to make an early diagnosis, since to treat such a disease Much easier in the beginning. Without proper attention, it can progress very quickly and lead to to disastrous consequences (severe mental disorders, the development of other diseases against the background of complete loss of strength, suicidal thoughts, etc.).
Signs of seasonal depression
Often people begin to feel depressed with the arrival of the cold season (autumn, winter). This is quite logical: daylight hours are shortening, there is no bright sunlight, and the air temperature is dropping. All these factors cause drowsiness, lack of desire to do anything and a general deterioration in mood.
However, the usual autumn blues should not be confused with depression. In medicine, she was given the name - seasonal affective disorder (SAD).
A distinctive feature of this disease is that the symptoms of depression are exacerbated mainly in the autumn-winter period. At the same time, this condition is associated with a lack of sunlight.
From a medical point of view, the following main causes of SAD development can be named:
- increased production of melatonin,
- insufficient amount of serotonin,
- failures of circadian rhythms of illumination,
- increased response of cortisol and prolactin to serotonin.
With the arrival of spring and then summer, the symptoms of seasonal depression disappear completely.
When asked about what to do with seasonal depression, doctors recommend spending more time outdoors during the day to get the amount of sunlight the body needs (you can walk or even just sit by the window).
Development of depression due to trauma
Sometimes depression can be caused by a traumatic brain injury (TBI). For example, as a result of a fall from a height, a strong blow, an accident, etc.
There are the following three types of depression that can develop against the background of TBI:
- Sad - appears with a slight or moderate contusion of the temporal region of the right hemisphere. Distinctive features of sad depression: the appearance of a feeling of longing in the patient, slow pronunciation of words, slow motor reaction, memory failures, distracted attention and asthenia (weakness and increased fatigue).
- Anxious - is the result of a slight or moderate bruise of the left temple. This condition is more common in people of mature age, writing with the right hand (right-handers).
Typical symptoms: constant feeling of anxiety, the patient is restless, tossing about, taking deep breaths and looks around.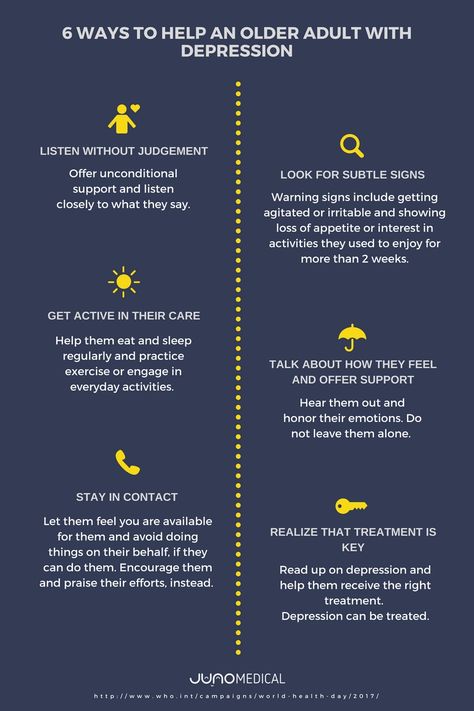 Also, this behavior is often accompanied by the utterance of disturbing speeches.
Also, this behavior is often accompanied by the utterance of disturbing speeches. - Apathetic - occurs with TBI of the anterior part of the brain. The main distinguishing feature: a person becomes everything indifferent and sad. Such patients are lethargic and have no interest in anything, including themselves.
It has been established that in almost 68% of people who are in the acute period after TBI, depressive states described above develop.
Diagnostic methods
In the treatment of depression, the timely diagnosis of this disease is of great importance. The sooner it is detected, the easier it will be to stop the symptoms.
Depressive disorders are usually diagnosed by a psychotherapist. A clinical psychologist is also often involved.
As a rule, the diagnosis is made in the course of a conversation with the patient. The profile doctor asks in detail about the condition, manifesting symptoms, periods of deterioration or a sharp improvement in the condition. During the diagnostics, the following main tasks:
During the diagnostics, the following main tasks:
- accurate determination of the presence of depression in a person,
- overall assessment of depression,
- measurement of certain symptoms resulting from depression (eg, anxiety, suicidal thoughts, etc.).
In addition to the conversation, special tests and questionnaires are used to diagnose depressive disorder.
Diagnostic sets of criteria are also used to make an accurate diagnosis, based on which assessment of the patient's condition. The most famous include ICD-10 (according to this model, all symptoms of depression are divided into into typical and additional) and DSM-IV-TR (depression is diagnosed if within 2 weeks marked at least 5 out of 9established symptoms).
In addition, patients with mood disorders are also advised to take some surveys. This is necessary in order to exclude the somatic origin of depression. For example, thyroid ultrasound is often prescribed.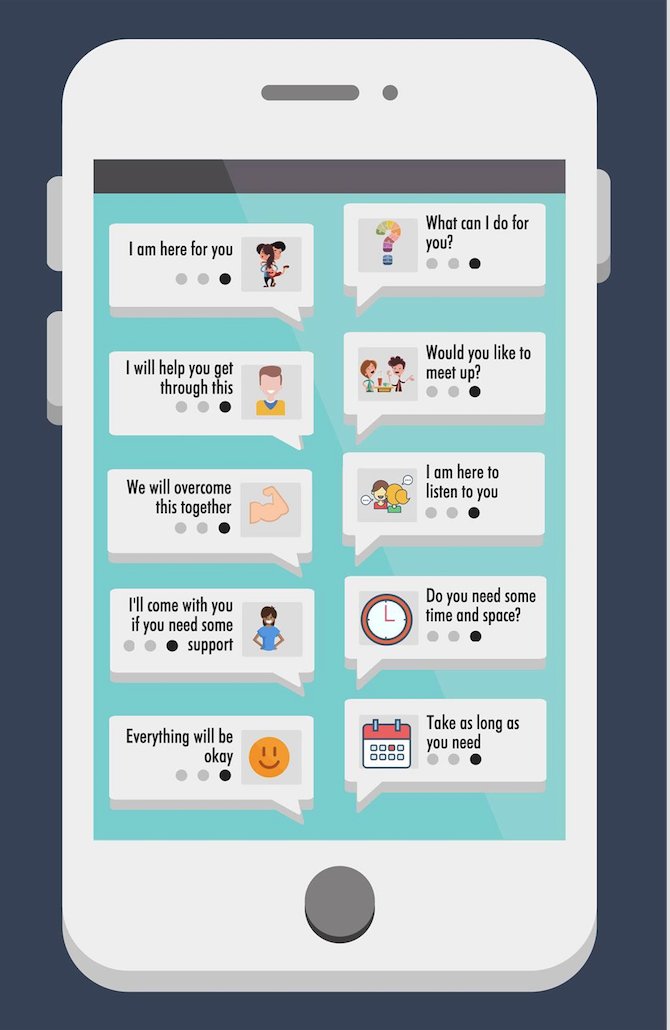 This diagnostic method will reveal hypo- or hyperthyroidism. It is known that such pathologies often provoke the development of depressive disorders.
This diagnostic method will reveal hypo- or hyperthyroidism. It is known that such pathologies often provoke the development of depressive disorders.
Today, the detection of depression is greatly hampered by the patient's attempts to remain silent about his condition. The reasons for this behavior may be different: someone is afraid of antidepressant treatment, another part of patients they are afraid of condemnation from friends and acquaintances, there are also those who associate their condition with a bad character, laziness, etc.
Treatment for depressive disorder
After making an accurate diagnosis, the next question arises - how to help yourself with depression?
In modern medicine, there are many different methods of dealing with this condition that have proven their effectiveness.
Consider the main ones:
- Drug therapy - the mainstay of treatment is taking antidepressants (stimulant, sedative or balanced action).
 For mild or moderate depression, drugs based on herbal ingredients.
For mild or moderate depression, drugs based on herbal ingredients. - Psychotherapy - in this case, the means of mental influence on a person suffering from depression are used. Known methods of psychotherapy: behavioral (aimed at increasing the patient's activity, developing self-control), interpersonal (teaching social skills), family, etc. Psychotherapy can be used as an independent treatment for depression, or in combination with taking antidepressants.
- Physical activity - sometimes a person suffering from depression is assigned a set of exercises. To get the effect, sports should be regular (2-3 times a week). Support from family and friends is welcome.
The main condition for this method of treatment is the patient's desire to engage in physical activity. - Electroconvulsive Therapy - With the help of an electric current, controlled convulsions are induced in the patient. As a result of this effect on the brain, substances that improve mood begin to be released.
 This method of treatment is usually prescribed for patients suffering from prolonged and persistent depression.
This method of treatment is usually prescribed for patients suffering from prolonged and persistent depression. - Other therapies - this may include light therapy (used for seasonal depression), sleep deprivation (minimization or lack of sleep), music therapy, etc.
With the development of depressive disorders, it is strongly not recommended to self-medicate. First of all, this concerns the use of antidepressants. Not all of them are suitable for a particular case. It all depends on the degree of neglect of the disease, the severity of symptoms and many other factors. If the antidepressant is chosen incorrectly, the patient's condition will only worsen.
Depression in a loved one: how to help?
Lack of understanding and consideration from relatives and friends is one of the most common problems experienced by people who are depressed.
Very often people around regard such a state as laziness, bad character, gaps in education, etc. Ultimately, the lack of attention to a person with depression leads to quite serious consequences.
Ultimately, the lack of attention to a person with depression leads to quite serious consequences.
If you have noticed the first symptoms of depression in someone close to you, then these tips will help alleviate the condition of a loved one:
- Create a comfortable and peaceful environment in your home - this can be a change in something in the interior, buying some kind of accent item, rearranging furniture, unloading space, etc.
People with depression are often unable to relax and feel safe, so it is important to create nice atmosphere around.
It is also necessary to ensure the flow of clean fresh air into the room. To do this, set breather. This is a compact supply ventilation system that will get rid of high concentrations that depress the immune system, carbon dioxide. - Don't underestimate the difficulties your loved one has experienced. Even if at first glance they seem insignificant, in fact, everything can be much more complicated.
Also in this case, such on-duty phrases as: “Do not invent”, “Nothing terrible is happening”, "Do something", etc.
A person must be listened to and allowed to express all the feelings that he experiences. - A person with depression should be advised carefully. Depression is primarily a disease which cannot be cured with valerian or sports. This is where professional help is needed. Therefore it is better to advise to descend or go to the psychologist or the psychotherapist. Even better would be to go with him.
- Help in solving everyday issues - a person in depression any ordinary affairs are given with great difficulty, require a lot of work, so try to provide all possible assistance.
- Do not leave your loved one even if he resists. Very often during depression people become more irritable, may be aggressive. In this case, you should try to find an alternative approach to the patient. The main thing is not to leave him alone with his difficult condition.

Learn more
 ”
”