How do you know if your depressed teenager
SAMHSA’s National Helpline | SAMHSA
Your browser is not supported
Switch to Chrome, Edge, Firefox or Safari
Main page content
-
SAMHSA’s National Helpline is a free, confidential, 24/7, 365-day-a-year treatment referral and information service (in English and Spanish) for individuals and families facing mental and/or substance use disorders.
Also visit the online treatment locator.
SAMHSA’s National Helpline, 1-800-662-HELP (4357) (also known as the Treatment Referral Routing Service), or TTY: 1-800-487-4889 is a confidential, free, 24-hour-a-day, 365-day-a-year, information service, in English and Spanish, for individuals and family members facing mental and/or substance use disorders.
This service provides referrals to local treatment facilities, support groups, and community-based organizations.
Also visit the online treatment locator, or send your zip code via text message: 435748 (HELP4U) to find help near you. Read more about the HELP4U text messaging service.
The service is open 24/7, 365 days a year.
English and Spanish are available if you select the option to speak with a national representative. Currently, the 435748 (HELP4U) text messaging service is only available in English.
In 2020, the Helpline received 833,598 calls. This is a 27 percent increase from 2019, when the Helpline received a total of 656,953 calls for the year.
The referral service is free of charge. If you have no insurance or are underinsured, we will refer you to your state office, which is responsible for state-funded treatment programs. In addition, we can often refer you to facilities that charge on a sliding fee scale or accept Medicare or Medicaid. If you have health insurance, you are encouraged to contact your insurer for a list of participating health care providers and facilities.
If you have health insurance, you are encouraged to contact your insurer for a list of participating health care providers and facilities.
The service is confidential. We will not ask you for any personal information. We may ask for your zip code or other pertinent geographic information in order to track calls being routed to other offices or to accurately identify the local resources appropriate to your needs.
No, we do not provide counseling. Trained information specialists answer calls, transfer callers to state services or other appropriate intake centers in their states, and connect them with local assistance and support.
-
Suggested Resources
What Is Substance Abuse Treatment? A Booklet for Families
Created for family members of people with alcohol abuse or drug abuse problems. Answers questions about substance abuse, its symptoms, different types of treatment, and recovery. Addresses concerns of children of parents with substance use/abuse problems.
Addresses concerns of children of parents with substance use/abuse problems.It's Not Your Fault (NACoA) (PDF | 12 KB)
Assures teens with parents who abuse alcohol or drugs that, "It's not your fault!" and that they are not alone. Encourages teens to seek emotional support from other adults, school counselors, and youth support groups such as Alateen, and provides a resource list.After an Attempt: A Guide for Taking Care of Your Family Member After Treatment in the Emergency Department
Aids family members in coping with the aftermath of a relative's suicide attempt. Describes the emergency department treatment process, lists questions to ask about follow-up treatment, and describes how to reduce risk and ensure safety at home.Family Therapy Can Help: For People in Recovery From Mental Illness or Addiction
Explores the role of family therapy in recovery from mental illness or substance abuse. Explains how family therapy sessions are run and who conducts them, describes a typical session, and provides information on its effectiveness in recovery.
For additional resources, please visit the SAMHSA Store.
Last Updated: 08/30/2022
Alcohol, Tobacco, and Other Drugs
Your browser is not supported
Switch to Chrome, Edge, Firefox or Safari
Misusing alcohol, tobacco, and other drugs can have both immediate and long-term health effects.The misuse and abuse of alcohol, tobacco, illicit drugs, and prescription medications affect the health and well-being of millions of Americans. NSDUH estimates allow researchers, clinicians, policymakers, and the general public to better understand and improve the nation’s behavioral health. These reports and detailed tables present estimates from the 2021 National Survey on Drug Use and Health (NSDUH).
Alcohol
Data:
- Among the 133.1 million current alcohol users aged 12 or older in 2021, 60.0 million people (or 45.1%) were past month binge drinkers.
 The percentage of people who were past month binge drinkers was highest among young adults aged 18 to 25 (29.2% or 9.8 million people), followed by adults aged 26 or older (22.4% or 49.3 million people), then by adolescents aged 12 to 17 (3.8% or 995,000 people). (2021 NSDUH)
The percentage of people who were past month binge drinkers was highest among young adults aged 18 to 25 (29.2% or 9.8 million people), followed by adults aged 26 or older (22.4% or 49.3 million people), then by adolescents aged 12 to 17 (3.8% or 995,000 people). (2021 NSDUH) - Among people aged 12 to 20 in 2021, 15.1% (or 5.9 million people) were past month alcohol users. Estimates of binge alcohol use and heavy alcohol use in the past month among underage people were 8.3% (or 3.2 million people) and 1.6% (or 613,000 people), respectively. (2021 NSDUH)
- In 2020, 50.0% of people aged 12 or older (or 138.5 million people) used alcohol in the past month (i.e., current alcohol users) (2020 NSDUH)
- Among the 138.5 million people who were current alcohol users, 61.6 million people (or 44.4%) were classified as binge drinkers and 17.7 million people (28.8% of current binge drinkers and 12.8% of current alcohol users) were classified as heavy drinkers (2020 NSDUH)
- The percentage of people who were past month binge alcohol users was highest among young adults aged 18 to 25 (31.
 4%) compared with 22.9% of adults aged 26 or older and 4.1% of adolescents aged 12 to 17 (2020 NSDUH)
4%) compared with 22.9% of adults aged 26 or older and 4.1% of adolescents aged 12 to 17 (2020 NSDUH) - Excessive alcohol use can increase a person’s risk of stroke, liver cirrhosis, alcoholic hepatitis, cancer, and other serious health conditions
- Excessive alcohol use can also lead to risk-taking behavior, including driving while impaired. The Centers for Disease Control and Prevention reports that 29 people in the United States die in motor vehicle crashes that involve an alcohol-impaired driver daily
Programs/Initiatives:
- STOP Underage Drinking interagency portal - Interagency Coordinating Committee on the Prevention of Underage Drinking
- Interagency Coordinating Committee on the Prevention of Underage Drinking
- Talk. They Hear You.
- Underage Drinking: Myths vs. Facts
- Talking with your College-Bound Young Adult About Alcohol
Relevant links:
- National Association of State Alcohol and Drug Abuse Directors
- Department of Transportation Office of Drug & Alcohol Policy & Compliance
- Alcohol Policy Information Systems Database (APIS)
- National Institute on Alcohol Abuse and Alcoholism
Tobacco
Data:
- In 2020, 20.
 7% of people aged 12 or older (or 57.3 million people) used nicotine products (i.e., used tobacco products or vaped nicotine) in the past month (2020 NSDUH)
7% of people aged 12 or older (or 57.3 million people) used nicotine products (i.e., used tobacco products or vaped nicotine) in the past month (2020 NSDUH) - Among past month users of nicotine products, nearly two thirds of adolescents aged 12 to 17 (63.1%) vaped nicotine but did not use tobacco products. In contrast, 88.9% of past month nicotine product users aged 26 or older used only tobacco products (2020 NSDUH)
- Tobacco use is the leading cause of preventable death, often leading to lung cancer, respiratory disorders, heart disease, stroke, and other serious illnesses. The CDC reports that cigarette smoking causes more than 480,000 deaths each year in the United States
- The CDC’s Office on Smoking and Health reports that more than 16 million Americans are living with a disease caused by smoking cigarettes
Electronic cigarette (e-cigarette) use data:
- In 2021, 13.2 million people aged 12 or older (or 4.7%) used an e-cigarette or other vaping device to vape nicotine in the past month.
 The percentage of people who vaped nicotine was highest among young adults aged 18 to 25 (14.1% or 4.7 million people), followed by adolescents aged 12 to 17 (5.2% or 1.4 million people), then by adults aged 26 or older (3.2% or 7.1 million people).
The percentage of people who vaped nicotine was highest among young adults aged 18 to 25 (14.1% or 4.7 million people), followed by adolescents aged 12 to 17 (5.2% or 1.4 million people), then by adults aged 26 or older (3.2% or 7.1 million people). - Among people aged 12 to 20 in 2021, 11.0% (or 4.3 million people) used tobacco products or used an e-cigarette or other vaping device to vape nicotine in the past month. Among people in this age group, 8.1% (or 3.1 million people) vaped nicotine, 5.4% (or 2.1 million people) used tobacco products, and 3.4% (or 1.3 million people) smoked cigarettes in the past month. (2021 NSDUH)
- Data from the Centers for Disease Control and Prevention’s 2020 National Youth Tobacco Survey. Among both middle and high school students, current use of e-cigarettes declined from 2019 to 2020, reversing previous trends and returning current e-cigarette use to levels similar to those observed in 2018
- E-cigarettes are not safe for youth, young adults, or pregnant women, especially because they contain nicotine and other chemicals
Resources:
- Tips for Teens: Tobacco
- Tips for Teens: E-cigarettes
- Implementing Tobacco Cessation Programs in Substance Use Disorder Treatment Settings
- Synar Amendment Program
Links:
- Truth Initiative
- FDA Center for Tobacco Products
- CDC Office on Smoking and Health
- National Institute on Drug Abuse: Tobacco, Nicotine, and E-Cigarettes
- National Institute on Drug Abuse: E-Cigarettes
Opioids
Data:
- Among people aged 12 or older in 2021, 3.
 3% (or 9.2 million people) misused opioids (heroin or prescription pain relievers) in the past year. Among the 9.2 million people who misused opioids in the past year, 8.7 million people misused prescription pain relievers compared with 1.1 million people who used heroin. These numbers include 574,000 people who both misused prescription pain relievers and used heroin in the past year. (2021 NSDUH)
3% (or 9.2 million people) misused opioids (heroin or prescription pain relievers) in the past year. Among the 9.2 million people who misused opioids in the past year, 8.7 million people misused prescription pain relievers compared with 1.1 million people who used heroin. These numbers include 574,000 people who both misused prescription pain relievers and used heroin in the past year. (2021 NSDUH) - Among people aged 12 or older in 2020, 3.4% (or 9.5 million people) misused opioids in the past year. Among the 9.5 million people who misused opioids in the past year, 9.3 million people misused prescription pain relievers and 902,000 people used heroin (2020 NSDUH)
- According to the Centers for Disease Control and Prevention’s Understanding the Epidemic, an average of 128 Americans die every day from an opioid overdose
Resources:
- Medication-Assisted Treatment
- Opioid Overdose Prevention Toolkit
- TIP 63: Medications for Opioid Use Disorder
- Use of Medication-Assisted Treatment for Opioid Use Disorder in Criminal Justice Settings
- Opioid Use Disorder and Pregnancy
- Clinical Guidance for Treating Pregnant and Parenting Women With Opioid Use Disorder and Their Infants
- The Facts about Buprenorphine for Treatment of Opioid Addiction
- Pregnancy Planning for Women Being Treated for Opioid Use Disorder
- Tips for Teens: Opioids
- Rural Opioid Technical Assistance Grants
- Tribal Opioid Response Grants
- Provider’s Clinical Support System - Medication Assisted Treatment Grant Program
Links:
- National Institute on Drug Abuse: Opioids
- National Institute on Drug Abuse: Heroin
- HHS Prevent Opioid Abuse
- Community Anti-Drug Coalitions of America
- Addiction Technology Transfer Center (ATTC) Network
- Prevention Technology Transfer Center (PTTC) Network
Marijuana
Data:
- In 2021, marijuana was the most commonly used illicit drug, with 18.
 7% of people aged 12 or older (or 52.5 million people) using it in the past year. The percentage was highest among young adults aged 18 to 25 (35.4% or 11.8 million people), followed by adults aged 26 or older (17.2% or 37.9 million people), then by adolescents aged 12 to 17 (10.5% or 2.7 million people).
7% of people aged 12 or older (or 52.5 million people) using it in the past year. The percentage was highest among young adults aged 18 to 25 (35.4% or 11.8 million people), followed by adults aged 26 or older (17.2% or 37.9 million people), then by adolescents aged 12 to 17 (10.5% or 2.7 million people). - The percentage of people who used marijuana in the past year was highest among young adults aged 18 to 25 (34.5%) compared with 16.3% of adults aged 26 or older and 10.1% of adolescents aged 12 to 17 (2020 NSDUH)
- Marijuana can impair judgment and distort perception in the short term and can lead to memory impairment in the long term
- Marijuana can have significant health effects on youth and pregnant women.
Resources:
- Know the Risks of Marijuana
- Marijuana and Pregnancy
- Tips for Teens: Marijuana
Relevant links:
- National Institute on Drug Abuse: Marijuana
- Addiction Technology Transfer Centers on Marijuana
- CDC Marijuana and Public Health
Emerging Trends in Substance Misuse:
- Methamphetamine—In 2019, NSDUH data show that approximately 2 million people used methamphetamine in the past year.
 Approximately 1 million people had a methamphetamine use disorder, which was higher than the percentage in 2016, but similar to the percentages in 2015 and 2018. The National Institute on Drug Abuse Data shows that overdose death rates involving methamphetamine have quadrupled from 2011 to 2017. Frequent meth use is associated with mood disturbances, hallucinations, and paranoia.
Approximately 1 million people had a methamphetamine use disorder, which was higher than the percentage in 2016, but similar to the percentages in 2015 and 2018. The National Institute on Drug Abuse Data shows that overdose death rates involving methamphetamine have quadrupled from 2011 to 2017. Frequent meth use is associated with mood disturbances, hallucinations, and paranoia. - Cocaine—In 2019, NSDUH data show an estimated 5.5 million people aged 12 or older were past users of cocaine, including about 778,000 users of crack. The CDC reports that overdose deaths involving have increased by one-third from 2016 to 2017. In the short term, cocaine use can result in increased blood pressure, restlessness, and irritability. In the long term, severe medical complications of cocaine use include heart attacks, seizures, and abdominal pain.
- Kratom—In 2019, NSDUH data show that about 825,000 people had used Kratom in the past month. Kratom is a tropical plant that grows naturally in Southeast Asia with leaves that can have psychotropic effects by affecting opioid brain receptors.
 It is currently unregulated and has risk of abuse and dependence. The National Institute on Drug Abuse reports that health effects of Kratom can include nausea, itching, seizures, and hallucinations.
It is currently unregulated and has risk of abuse and dependence. The National Institute on Drug Abuse reports that health effects of Kratom can include nausea, itching, seizures, and hallucinations.
Resources:
- Tips for Teens: Methamphetamine
- Tips for Teens: Cocaine
- National Institute on Drug Abuse
More SAMHSA publications on substance use prevention and treatment.
Last Updated: 01/05/2023
HOW TO UNDERSTAND THAT YOUR TEENAGER IS DEPRESSED
14 August 2020 10:08
Views: 14737
The teenage years are often a very difficult time for children and their parents. This period is very important for mental well-being. Let's figure out what features of a teenager's behavior you should pay attention to and when to see a doctor.
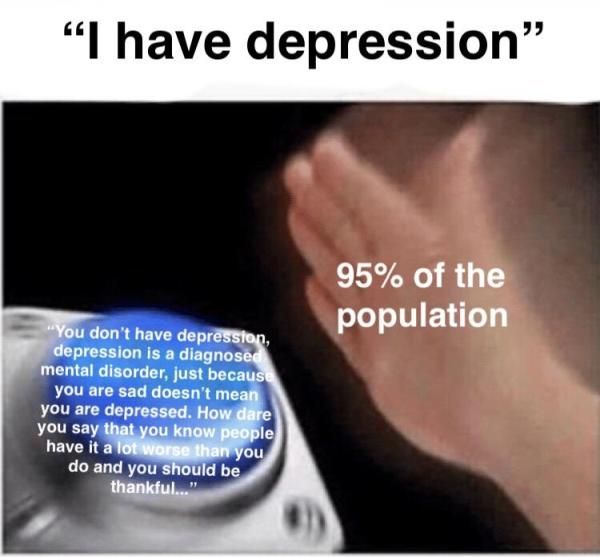
People of all ages experience sadness, irritability, or low energy from time to time. Such feelings are considered normal, but if the negative does not disappear and does not weaken for a long time, this is a reason to contact a specialist. In the case of a child, this condition can mean depression. It is treatable, but it is not always easy to recognize even a specialist.
In the case of a child, this condition can mean depression. It is treatable, but it is not always easy to recognize even a specialist.
How serious is this in general?
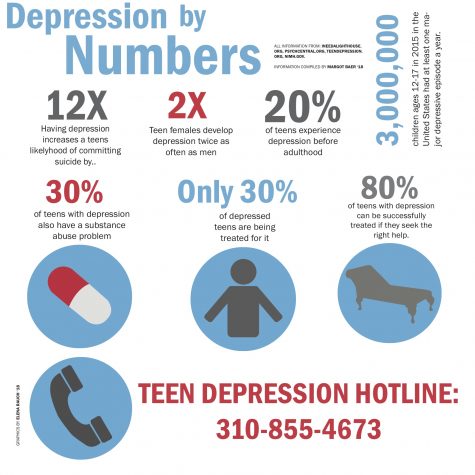
According to the World Health Organization (WHO), depression is one of the leading causes of morbidity and disability among adolescents worldwide, with about 10-20% of them experiencing mental health problems but not being diagnosed and treated.
Who is at risk?
The reasons for the development of depression in adolescents are different and are determined individually in each specific situation. A person is made vulnerable by emotional, social, as well as physical factors: violence and abuse, social status among peers, family well-being, school or university performance.
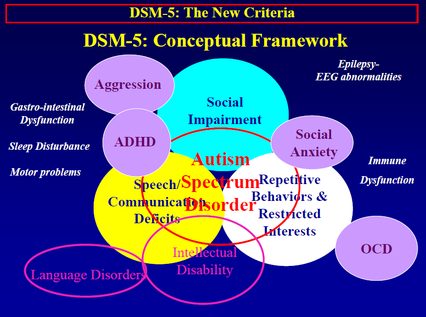
Some teenagers are at higher risk for depression. This problem concerns children with chronic diseases or other neuropsychiatric disorders, such as autism spectrum disorders. At risk are adolescents who have become parents or entered into early marriage, as well as ethnic minorities.
Maybe my child is just lazy and doesn't want to do anything? Or just upset? How to understand that he is really bad?
Depression is not a condition that can be overcome by willpower. This is a persistent lack of interest in any activity, which is accompanied by a feeling of sadness. Often, this condition can cause suicidal thoughts, sleep and wake disturbances, and even physical symptoms such as headaches and stomach pains, and a constant feeling of fatigue. It may seem that a person is lazy, does not want to do anything, in fact, he will be in a state of apathy, which is one of the symptoms of depression.
Very often, depression is disguised as mood swings, and sometimes the teenager himself does not make contact, isolates himself from family and friends and does not want to talk about his mood. Such a condition should not be ignored, because it can result in serious consequences - antisocial behavior or in the worst case, for example, a suicide attempt.
You should not immediately try on labels on a teenager, because he may be sick, which is why it is so important to be aware of the symptoms of depression and communicate with your child. Gently bring him to the conversation, position him towards you, let him know that you are on his side and you care. Start a conversation with these phrases:
1. "Let's talk to you about this, it's important to me."
2. "Let's think about how we can solve this problem."
3. "You mean a lot to me, I'm worried about your condition."
What should you pay attention to?
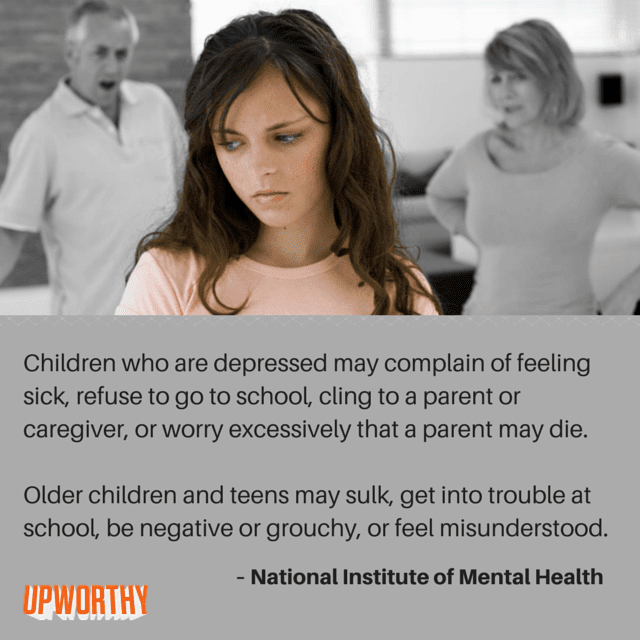
First and most importantly, depression can manifest itself in different ways in different children and it does not proceed in the same way as in adults. Adults with depressive disorder are more likely to experience sadness, children and adolescents behave angry and irritable. Also, a sharp decline in grades at school often begins, changes in normal behavior are observed. Here are some wake-up calls:
defiant, reckless behavior, abrupt changes in behavior;
· irritability and anger;
Complaints of pain in the head or abdomen;
insomnia or, conversely, too much sleep;
fatigue, lack of energy;
decrease in appetite, loss or, conversely, a set of overweight;
· anxiety;
reduced physical activity;
Difficulties in making decisions;
Lack of concentration
Feelings of guilt or worthlessness
Thoughts of death or suicide;
aloof behavior
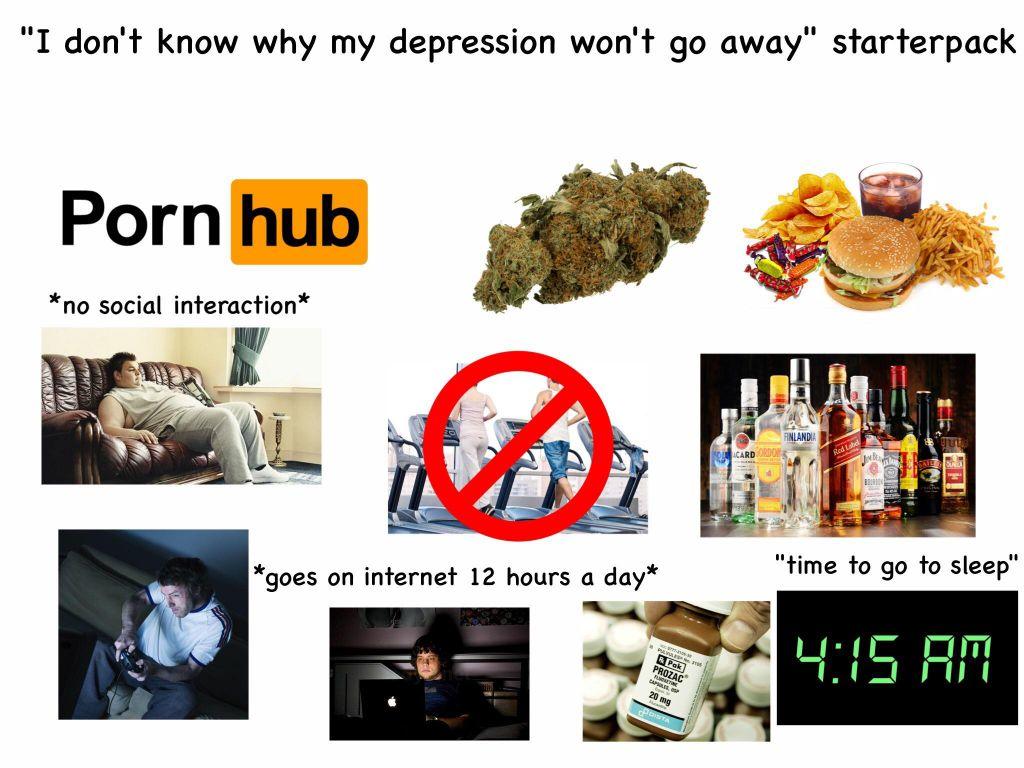
The use of psychoactive substances, alcohol;
the child cries for no reason;
increased sensitivity to criticism;
feeling of hopelessness and helplessness.
Which doctor treats depression?
Depressive disorders are dealt with by psychiatrists, psychotherapists, and sometimes psychologists. Unlike SARS, which in most cases can be dealt with on your own at home, depression requires mandatory monitoring by a doctor, since the causes of the disease are different. Hence the different treatments.
As a rule, adolescents are prescribed medication, psychotherapy, and are also given recommendations for changing their lifestyle. Normalization of sleep and wakefulness, sports, balanced nutrition - all these simple things can really do their bit in the fight against depressive disorder.
How long will the treatment last?
Overcoming depression can take time, in this regard, unfortunately, no guarantees can be made on the timing. According to this, treatment should be continued for 4-6 months after remission, as shorter periods lead to an increased risk of depression recurrence. Therefore, a teenager will need a lot of support. Remember, depressive disorders are treatable! This is not a life sentence, and a teenager will not be registered with a psychiatrist if he does not pose a threat to himself.
Next news
news
Teen Depression - Evidence-Based Medicine for All
What is Teen Depression
Teen depression is a serious medical problem and is characterized by persistent feelings of sadness and loss of interest in any activity. This affects the thoughts, feelings, and behavior of the adolescent and can cause emotional, functional, and physical problems. The course of depression in different periods of life is significantly different due to differences in the functioning of the brain, the symptoms of teenage depression are significantly different from the symptoms of adult depression.
Depression. Symptoms of increased suicidal risk
Research has found that certain behaviors such as...
Communication problems with peers, learning problems and changes in growing internal organs can cause a lot of trouble for teenagers. In some teenagers, they are not limited to short-term mood swings and turn into depression.
Teenage depression is not temporary laziness, it is not something that can be overcome by an effort of will. It should not be underestimated and attributed to the "weakness" or "bad education" of the teenager. It can have serious consequences and requires long-term treatment. For most adolescents, depression is mild and responds well to medication and psychotherapy.
Symptoms of depression in adolescents
The main symptoms of depression in adolescents are emotional and behavioral changes.
Emotional changes
- Frequent manifestation of feelings of sadness or longing, including crying for no apparent reason
- Irritability, grief or anger at the most insignificant occasions
- Loss of interest or pleasure in normal activities of an adolescent
- Loss of interest in or constant conflict with family and friends
- Feeling of worthlessness, guilt, fixation on past failures, excessive self-criticism
- Too painful reaction to failures
- Difficulties in thinking, concentrating, making decisions and remembering events
- Constant feeling that present and future life is gloomy and bleak
- Frequent thoughts of death, suicidal thoughts.
Behavioral changes
- Chronic fatigue and apathy
Teenage suicides. Analysis of the causes
Research shows that suicide in adolescence ...
- Insomnia or excess sleep
- Appetite changes: decreased appetite and weight loss, or increased appetite and rapid weight gain
- Alcohol or drug use
- Agitation or restlessness - such as restlessness, arm twisting, etc.
- Slowing of thinking, speech or body movements
- Frequent complaints of body aches and headaches, which may lead to frequent visits to the school medical office, but usually have no objective cause
- Decreased school performance or frequent absenteeism
- Untidy and slovenly appearance, e.g. grossly mismatched clothing, disheveled hair
- Provocative or risky behavior
- Self-aggression, purposeful self-infliction of minor injuries: cuts, burns, excessive piercings and tattoos.
Depression in adolescents. Pathology or physiological crisis?
It can be very difficult to distinguish between normal teenage behavior caused by a physiological crisis or objective problems and the true symptoms of teenage depression. If you suspect something is wrong - first of all, talk to your teenager. Try to determine how well he or she is handling his or her feelings.
If symptoms of depression begin to interfere with your child's life, talk to the school doctor or psychologist. You can also contact your family doctor or pediatrician.
When to see a doctor
If you suspect your child has depression, contact your doctor immediately. Don't expect depression symptoms to go away on their own - if left untreated, they can get worse or lead to other problems. Depressed teenagers are at risk of suicide, even if the symptoms do not seem severe.
Postpartum depression. Q&A
Interview with Dr. Mark Zakowski, OB/GYN and ...
If you are a teenager and suspect you are depressed, or if you have a friend with depression, don't delay seeking help. Talk to a professional (doctor or psychologist), share your concerns with a parent, close friend, spiritual leader, teacher, or someone else you trust.
Teen depression and suicidal ideation
If your child is expressing suicidal thoughts, seek help immediately. Take these conversations seriously. If you think that a teenager in the near future may harm others or himself: injure himself or attempt suicide - call an ambulance. If your psychiatrist sees the need for hospitalization, do not refuse it.
Causes of depression in adolescents
It is not known for certain what causes depression. Various factors may be involved in the development of depression, for example:
- Neurotransmitter imbalance. Neurotransmitters are natural chemicals in the brain that likely play a role in the development of depression.
When the balance of these chemicals in the brain is disturbed, symptoms of depression appear.
- Hormones. Changes in the body of a teenager associated with his maturation lead to an imbalance in hormones. This can indirectly influence the triggering or intensification of depression.
- Hereditary factors. Depression is more common in people whose biological (blood) relatives also have the condition.
- Early childhood trauma. Traumatic events in childhood, such as physical or emotional abuse, or the loss of a parent, can cause changes in the brain that make a person more susceptible to depression.
Risk factors for teen depression
Many factors increase the risk of starting or worsening teen depression, including:
Depression and its shades
Have you ever had difficult events in your life, after which you feel...
- Having problems that negatively affect the adolescent's self-esteem, such as obesity, peer problems, long-term bullying, or academic problems
- If the patient was a victim or witness of violence (both physical and sexual)
- Presence of other psychiatric disorders such as anxiety disorder, anorexia or bulimia, attention deficit/hyperactivity disorder (ADHD), or others.
- Presence of a chronic physical disease - malignancy, diabetes mellitus or asthma
- Certain personality traits such as low self-esteem, overdependence on another person, excessive self-criticism or persistent pessimism
- Alcohol, nicotine or drug abuse
- Female: Depression is more common in women than in men
- Sexual minority: if the patient is gay, lesbian, bisexual, or transgender, it is not uncommon for the patient to become socially isolated or bullied, which may increase the risk of depression
Having a family history of psychiatric disorders also increases a teenager's risk of depression:
Complications of teen depression
Untreated depression can lead to emotional, behavioral and physical problems that affect every area of your child's life. Complications associated with teen depression may include:
- Low self-esteem
- Alcohol and drug abuse
- Learning problems
- Family conflicts and communication difficulties
- Social isolation
- Dangerous and illegal behavior
- Suicide.
Preparing for a doctor's visit
First, you should contact your family doctor or pediatrician by making an appointment. You can go directly to a psychiatrist.
If possible, include your teenager in preparing for the doctor's visit. Together with him, make the following list:
How exercise protects against depression
A study published in the journal Cell investigates the mechanism. ..
- Describe any of the adolescent's symptoms, including any that seem unrelated to you
- List key personal information, including recent stresses and changes in your child's life
- List all medications, vitamins, and dietary supplements your child is taking or has recently taken
- Write down any questions you and your child want to ask the doctor.
For example, you might ask:
- Do these symptoms indicate depression in my child?
- What are other possible diagnoses?
- Will additional testing be required?
- What is the best treatment for this situation?
- Are there any side effects from the medicines you prescribe?
- How should treatment progress and effectiveness be monitored?
- My child has other medical conditions, how will this affect treatment? Could these diagnoses be related to depression?
- Are there any restrictions that the child must follow?
- How often should I visit a psychiatrist?
- Can changes in diet, exercise, or other activities alleviate depression?
- Do you have printed materials that we could study at home? What sites do you recommend we visit?
Do not hesitate to ask questions that arise during a conversation with a doctor.
Your doctor will likely ask your teenager and you the following questions:
- When did family members or friends first notice symptoms of depression?
- How long have you yourself experienced symptoms of depression? Does the depressed mood haunt you all the time, or does it happen from time to time?
- Do you have sudden mood swings? Say, when was the last time you felt overwhelmed with happiness and energy?
- Have you ever had suicidal thoughts when you were in a bad mood?
- How severe are your symptoms? Do they interfere with school, relationships with friends, or other daily activities?
- Do you have any biological (blood) relatives with depression or another mental disorder?
- Does the teenager have any other diseases?
- Did the teenager use alcohol, marijuana or street drugs?
- How much does a teenager sleep at night? Has sleep duration changed recently?
- What do you think relieves symptoms in a teenager?
- What do you think makes them worse?
- Has the child's diet, eating habits and preferences changed? Have you noticed a sharp change in the child's weight: an increase or weight loss?
Diagnosis of depression in adolescents
When a doctor suspects teenage depression, they usually do the following examinations and tests:
Examination. The doctor will do a physical exam and ask you a series of questions about your child's health to rule out physical causes of depression. In some cases, depression may be secondary, that is, caused by another disease.
Laboratory tests. Your teen's doctor may order a complete blood count or thyroid hormone test to make sure there are no other medical conditions.
Psychological assessment. This assessment consists of discussing with your teenager his/her thoughts, feelings and behaviors and may include a questionnaire. This will help to accurately determine the diagnosis and measure the risk of complications.
Diagnostic Criteria for Depression
To be diagnosed with depression, your teen must meet criteria in the Diagnostic and Statistical Manual of Mental Disorders (DSM) published by the American Psychiatric Association. This guide is used by psychiatrists to diagnose mental conditions.
The symptoms may be based on how your teenager feels or what people around him or her experience. To be diagnosed with depression, symptoms must occur most of the day, almost every day, for at least two weeks, and cause changes in the adolescent's usual behavior.
To be diagnosed with depression, an adolescent must have at least one of the following symptoms:
- Depressed mood, such as sadness, emptiness, or tearfulness (during adolescence, depressed mood may be manifested by chronic irritability)
- Decreased interest in or loss of pleasure in all or most activities that previously brought joy and pleasure.
In addition, the adolescent must have four or more of the following:
- Significant weight loss without a targeted diet, or, conversely, sudden weight gain; decrease or increase in appetite
- Insomnia or excessive sleepiness
- Anxiety or slow behavior that catches the eye of loved ones
- Chronic fatigue, weakness and lack of initiative
- Feelings of worthlessness, or excessive or causeless guilt
- Problems with decision making, with concentration
- Recurrent thoughts of death or suicide, making plans for suicide, or attempting suicide.
However:
- Symptoms must not be due to direct effects of psychotropic drugs (alcohol, drugs, drugs) or hypothyroidism
- Symptoms should not be caused by fresh grief, such as occurs at the death of a loved one.
Other types of depression
Atypical depression. In this type of depression, the key symptoms are chronic hunger, weight gain, drowsiness, heavy arms and legs, and difficulty maintaining interpersonal relationships.
Postpartum depression. This type of depression may occur in new mothers. Postpartum depression can begin immediately after childbirth or several weeks later. Its symptoms are more intense and more persistent than those of adolescent depression and make it very difficult for the mother to take care of her child and perform other daily tasks.
Psychotic depression. This is a severe depression accompanied by psychotic symptoms such as delusions or hallucinations.
Dysthymia. This is a less severe but longer term form of depression. While not causing severe symptoms of depression, this disorder can still prevent a teenager from functioning normally in daily life and reduce the quality of life.
Other disorders that can cause depressive symptoms in adolescents
There are several other disorders that cause depression, among others. It is important to clearly identify these diseases so that the adolescent receives optimal treatment. During the examination, the doctor will keep these diseases in mind in order to exclude or recognize them in time:
- Seasonal affective disorder. This is a type of depression associated with changes in the seasons and reduced exposure to sunlight.
- Adjustment disorder. This is an over-expressed emotional response to a traumatic event in an adolescent's life. This is a separate mental illness that can affect feelings, thoughts and behavior.
- Bipolar disorder. Bipolar disorder is characterized by mood swings that range from mania to depression. It can sometimes be very difficult to distinguish bipolar disorder from true depression, but this is very important because the treatment of depression is different from that of bipolar disorder.
- Cyclothymia or cyclothymic disorder. This is a mild form of bipolar disorder.
- Schizoaffective disorder. This is a condition in which a person meets the criteria for both schizophrenia and depression.
Treatment of adolescent depression
Many therapies are currently available to treat this disorder. In some cases, a doctor may prescribe medications that relieve symptoms of depression. For other teenagers, psychotherapy sessions are enough. A combination of drug therapy and psychological counseling (psychotherapy) is the most effective approach for most adolescents with depression.
If your teenager has severe depression or is at serious risk of self-harm and suicide, he/she may need to stay in a hospital or a rigorous outpatient treatment program until symptoms begin to subside.
Medications
Because studies on the effects of antidepressants in adolescence are few, physicians rely primarily on adult studies when prescribing medications. The FDA has approved two drugs for the treatment of teen depression, fluoxetine and escitalopram. However, the doctor may prescribe other drugs if the clinical situation requires it.
More information: SSRIs for depression and seizure risk
Talk to your doctor about possible side effects of drug therapy, weighing the benefits and risks.
Antidepressants and increased risk of suicide
All antidepressants are prescription drugs. These drugs are quite safe, but in some cases they can significantly increase the intensity of suicidal thoughts and intentions, especially in the first few weeks after starting them, or after changing the dose. Therefore, such patients should be closely monitored by relatives and friends, as well as medical professionals.
If your teenager has suicidal thoughts while taking antidepressants, contact your doctor immediately.
For most adolescents, the benefits of taking antidepressants far outweigh any possible risks. In the long term, antidepressants reduce the intensity of suicidal thoughts and intentions.
Monitor your teen's medications closely. To achieve the proper effect, antidepressants must be taken strictly in the prescribed doses. Due to the risk of overdose when attempting suicide in depressed adolescents, a doctor may only prescribe a small amount of antidepressants at a time.
Sometimes it takes time and trial and error to find the best drug for your child. This will require patience as some medications take eight weeks or longer to develop their full effect and also to reduce their side effects.
If you notice side effects from treatment in your teenager - you should not stop the drug right away - you should first consult a doctor. Some antidepressants can cause a withdrawal syndrome (withdrawal), so their course should not be interrupted abruptly - this can provoke a significant increase in depression. Encourage your teen not to give up, encourage and support him/her.
If antidepressant treatment is not working, your doctor may recommend a cytochrome P450 (CYP450) blood test to check for specific genes that affect the body's ability to respond to antidepressants. This will help determine which antidepressants are best for your child. However, these genetic tests have a number of limitations and should not be used routinely.
Antidepressants and pregnancy
If your teenage daughter is pregnant or breastfeeding, some antidepressants may pose an increased risk to the health of her unborn child. If your daughter is pregnant or planning to become pregnant, make sure she talks to her doctor about managing depression during pregnancy.
Psychotherapy
Psychotherapy, also called psychological counseling or "talk therapy", is a way to treat depression by discussing problems with a therapist in private. Psychotherapy can be carried out both alone and together with other members of the family or team.
During these regular meetings, your teenager can learn about the causes of depression, learn to recognize and make changes to unhealthy lifestyles or thoughts, better understand their experiences, find better ways to get along with others and solve problems, and learn to set themselves realistic goals. Psychotherapy can help your teen regain a sense of happiness and control over their life, and help relieve symptoms of depression such as feelings of hopelessness and anger. It can also help a teenager survive a crisis or other current difficulties.
Hospitalization and other treatment programs
In some adolescents, depression is so severe that they require a hospital stay, especially if the adolescent is at high risk of self-harm or is dangerous to another person. Psychiatric treatment in the hospital will help keep your teen safe until the symptoms are under control. There are also outpatient treatments such as "day hospital", where a teenager has to come to the department every day, but still spends most of the day at home.
Lifestyle changes and home remedies for teen depression
You (the parents) are your child's best advocates and helpers in dealing with depression. Here are some steps to help you and your child cope with his/her illness:
- Stick to your treatment plan. Make sure your teenager attends appointments with a doctor or therapist. Even if the teenager feels well, make sure he or she continues to take the medication as directed by the doctor. If your teen stops taking medication, the symptoms of depression may return. Abrupt withdrawal of medications can cause a withdrawal syndrome. Never stop taking a depression medication without talking to your doctor.
- Learn more about depression and share books and websites recommended by your doctor with your teen. Self-education can better motivate your teenager to stick to the treatment plan.
- Pay special attention to your communication with your teenager. Talk to him/her about worries, stress your unconditional support. Create an environment in which the child can share his problems with you and be sure that he will be listened to and understood.
- Pay attention to warning signs. Discuss with your doctor or therapist the expected trend in your symptoms and keep track of it. Make a plan so you and your child know what to do if symptoms worsen. Ask family members or friends to also watch for warning signs.
- Help your teen develop healthy habits. Even mild regular physical activity can reduce symptoms of depression. Sleep is also important for all adolescents, and is especially important for depressed adolescents. If your teen has trouble sleeping, see your doctor for advice.
- Help your teen avoid alcohol and drugs. Your teen may think that alcohol or drugs reduce the symptoms of depression, but in the long run they only make them worse, and then the depression will be much more difficult to treat.
Patient support
Show genuine interest, concern, and a desire to understand your child's feelings. Listen to your teenager without judgment and try to put yourself in his/her position. Raise your child's self-esteem by celebrating every, even small, success.
The following simple tips will help you be a strong supporter of your child:
- Encourage your teen to create and maintain healthy friendships with peers and others. Positive relationships help build your teen's trust in people. Encourage your teen to avoid relationships with people whose behavior may exacerbate depressive symptoms.
- Encourage physical activity. Participating in sports, school activities, or clubs can help your teen focus on positive things and interrupt negative feelings or behaviors.
- Teach your child to ask for help. Teenagers are reluctant to seek support when they are depressed. Encourage your teen to have sincere conversations with a family member or other trusted adult when needed.
- Have realistic expectations. Many teenagers are prone to self-flagellation if they are not able to live up to unrealistic standards they have invented - in school, in sports, and so on. Let your teen know that it's okay to be imperfect.
- Make your teen's life easier. teach him/her to choose commitments carefully and set reasonable goals. Let your teen know that it's okay to do less if the symptoms of depression are on the rise.
- Structure time. Help your teen make written plans for the day or week to stay organized and productive.
- Encourage your teen to keep a personal diary as well: it can help improve mood by allowing your child to express pain, anger, fear, or other emotions they might not otherwise be able to express.
- Connect with other teens who are struggling with depression. Connecting with other teens who are experiencing similar problems can help your child deal with depression.
Support groups for teens with depression are available in many cities, ask your doctor if he knows of such groups in your city. Similar support groups are also available on the Internet, but you should first make sure that the site is trustworthy.
- Teach your child to take care of their health. Make sure your teen is eating regularly and properly, exercising regularly, and getting enough sleep.
Prevention of teen depression
There is no reliable way to prevent depression. However, some tips can help reduce your risk.
Reward your teen:
- Follow stress control measures, such as not taking on too many obligations at once
- Increase low self-esteem by allowing yourself to enjoy even small successes
- Accept friendship and social support, especially in times of crisis
- Get treated early in problems to prevent major depression from developing
- Strictly adhere to your doctor's treatment, even after symptoms subside, to help prevent recurrence of depression.