Dsm 5 diagnostic criteria for depression
Depression and Depressive Disorders I Psych Central
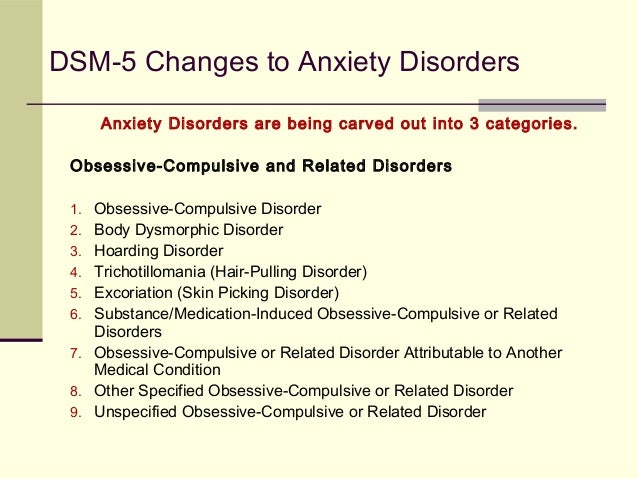
Healthcare professionals rely on the DSM-5 to determine mental health diagnoses. The manual has updated its classifications of depressive disorders with critical new guidelines.
The Diagnostic and Statistical Manual of Mental Disorders, 5th edition (DSM-5), is a reference guide used by healthcare and mental health professionals to more accurately identify and diagnose mental health conditions.
The American Psychiatric Association (APA) created the tool to be the go-to guide for mental health conditions in the United States.
Important updates and changes have been made to depressive disorders, including major depression — aka depression, major depression, or clinical depression.
These changes allow healthcare and mental health professionals to determine the most accurate diagnosis and treatment plan for these conditions.
In 1952, the APA published the first edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM) to classify mental health conditions and outline their associated diagnosing criteria.
Healthcare and mental health professionals often use the DSM as a reference guide for diagnosing mental health conditions.
With its latest revision released in 2013, the DSM is now in its 5th edition (DMS-5).
Many experts in the mental health field used evidence-based research, literature reviews, and other credible diverse sources of information to revise the DSM.
You can find symptoms, criteria, contributing factors, and much more for more than 20 mental health classifications, and even some new conditions were identified and added.
Specifiers for each condition listed are added extensions that provide medical professionals with clarifying information to ensure a more accurate diagnosis.
When making a diagnosis, all the answers may not be found in this manual, but it’s a great place to start.
The DSM-4 was published in 1994. Due to advancements in neuroscience since that time, clinical and public health experts found problems with the previous DSM-4 classification system and its criteria, according to a 2013 article.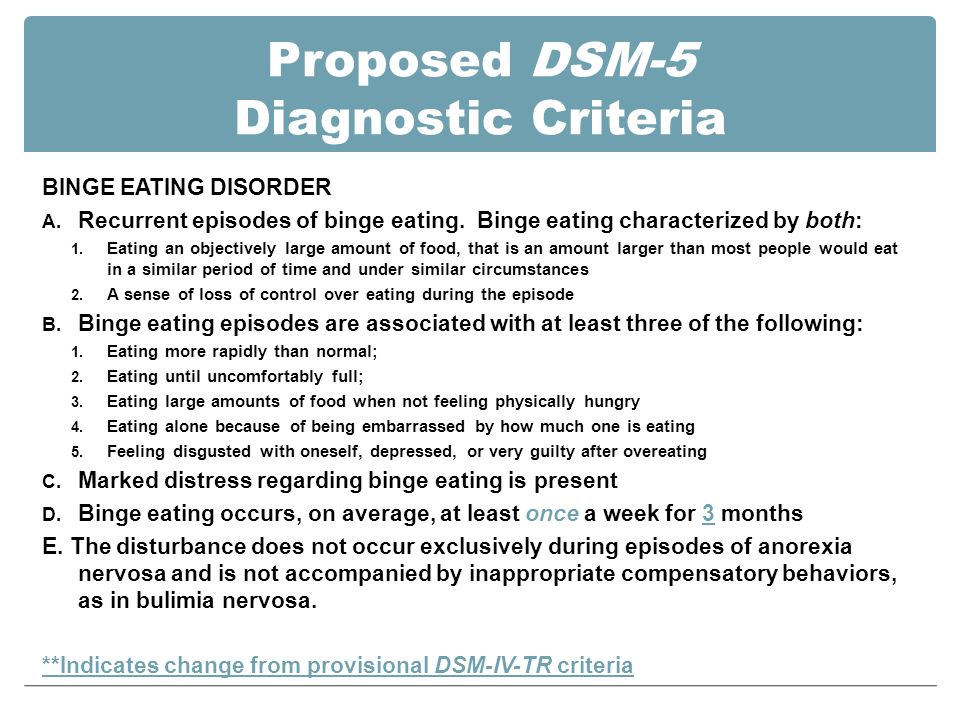
While the overall impact on the manual was small, the depressive disorders classifications saw significant changes.
Mental health and science constantly evolve as new modalities, treatments, and technologies are updated, discovered, or refuted by research and scientific breakthroughs.
The DSM changes with each new edition as the medical community learns more about mental health, and it will continue to do so.
The updated DSM-5 added two new disorders to depressive disorders:
- disruptive mood dysregulation disorder (DMDD)
- premenstrual dysphoric disorder (PMDD)
It also updated previous conditions with new criteria, exclusions, and specifiers.
What’s new for depressive disorders in the DSM-5?
| DSM-4 | DSM-5 |
|---|---|
| Bereavement excluded as criteria for major depressive disorder | Bereavement no longer excluded and is discussed as possibly contributing to major depressive disorder |
| Major depressive disorder | No changes (see added specifiers) |
| Substance and medication induced depressive disorder | No changes |
| Depressive disorder due to another medical condition | No changes |
| Other specified depressive disorder | No changes |
| Chronic major depressive disorder and dysthymic disorder | Merged and renamed to persistent depressive disorder |
| Added premenstrual dysphoric disorder | |
| Added disruptive mood dysregulation disorder (DMDD) | |
| Added “mixed features” specifier for bipolar and depressive disorders | |
| Added “anxious distress” specifier |
Let’s dive into these changes further to better understand their impact.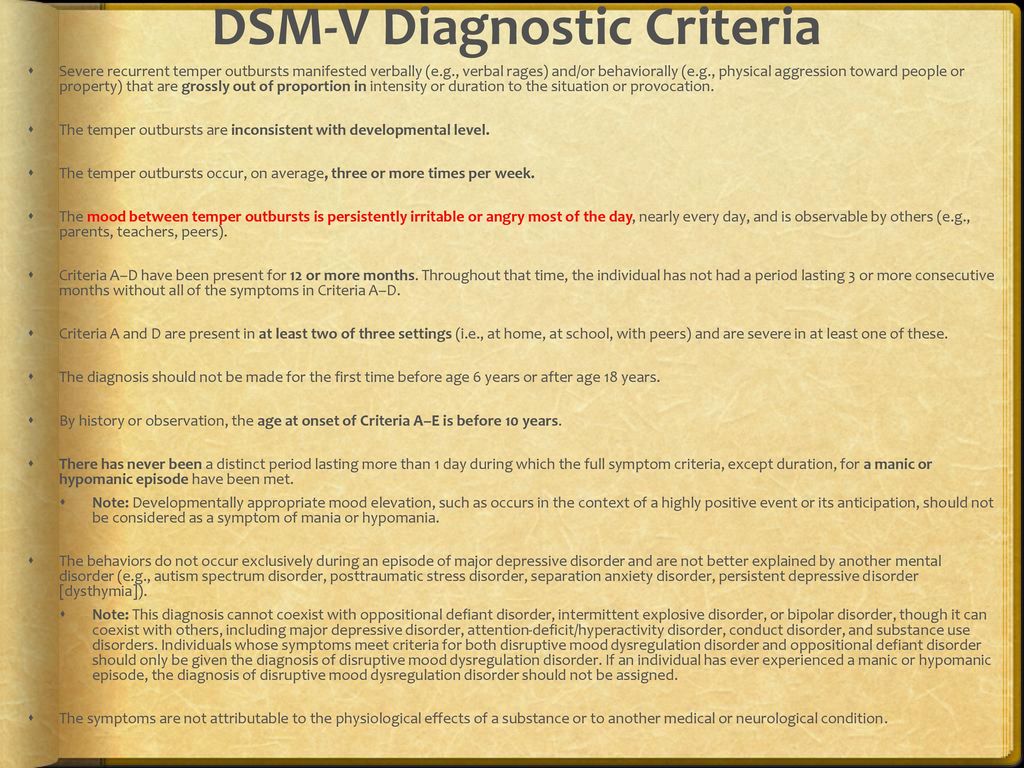
Disruptive mood dysregulation disorder (DMDD)
Disruptive mood dysregulation disorder (DMDD) is a new condition introduced in the DSM-5 to address symptoms once diagnosed and treated as childhood bipolar disorder. It can be diagnosed in children ages 6 to 18 years of age who exhibit persistent irritability and frequent episodes of extreme out-of-control behavior.
Children living with DMDD show symptoms usually before the age of 10, according to the National Institutes of Mental Health (NIMH).
Some of these symptoms can include the following:
- aggressive behavior
- severe tantrums several times a week for at least one year
- chronic irritability
- difficulty functioning due to their heightened irritability
- reacting out of proportion to the situation
DMDD may be a newly classified disorder, but treatment is available.
Treatment often centers around what has worked for similar disorders such as attention deficit hyperactivity disorder (ADHD) and anxiety.
A combination of medication and psychotherapy treatments, such as parent training, is often recommended.
Premenstrual dysphoric disorder (PMDD)
Premenstrual dysphoric disorder (PMDD) is now an official diagnosis in the DSM-5. It differs from other depressive disorders because of its connection to menstruation.
In most menstrual cycles during a year:
- at least 5 (or more) of the following symptoms must be present in the week before menstruation
- symptoms must start to improve within a few days after the onset of menstruation
- symptoms must resolve or become minimal in the week following menstruation
To be diagnosed with premenstrual dysphoric disorder, at least one more of these symptoms must also be present:
- affective lability: shifts in mood, sudden sadness or crying, increased sensitivity to rejection
- irritability: anger or increased interpersonal conflicts
- depression: depressed mood, feelings of hopelessness, or self-deprecating thoughts
- anxiety: feelings of anxiousness, tension, or being “keyed up” or “on edge”
In addition, at least five of the symptoms below must be present:
- lack of or decreased interest in usual activities
- difficulty concentrating
- fatigue or lack of energy
- change in appetite, overeating, or specific food cravings
- hypersomnia or insomnia
- sense of being overwhelmed or out of control
- other physical symptoms such as:
- breast tenderness or swelling
- joint or muscle pain
- bloating
- weight gain
For a diagnosis of PMDD, these symptoms must cause significant distress or interfere with your ability to function in daily life.
Persistent depressive disorder (dysthymia)
The DSM-5 also updated persistent depressive disorder, also known as dysthymia. The condition is classified as having a lower level of depression that’s less severe than major depressive disorder but with chronic (long-term) symptoms.
This new condition is a combination of chronic major depressive disorder and dysthymic disorder.
For this diagnosis, a person must experience the symptoms for at least 2 years.
Overall, the diagnosis of this condition is rare. Of the estimated 17% of U.S. adults diagnosed with a major depressive disorder, only 3% have been diagnosed with persistent depressive disorder.
The symptoms of this disorder are similar to other forms of depression. A thorough assessment is required to rule out other diagnoses such as bipolar disorder and major depressive disorder.
Major depressive disorder (MDD)
Clinical depression, formerly known as major depressive disorder in the DSM, is commonly diagnosed. Changes to its diagnostic criteria were limited.
Changes to its diagnostic criteria were limited.
The core criteria of symptoms for MDD weren’t changed, nor was the requisite 2-week time period needed before it can be diagnosed.
Some of the criteria for this diagnosis include:
- persistent feelings of sadness, emptiness, or hopelessness most of the day, nearly every day
- decreased pleasure and interest in most of your regular activities
- a sense of worthlessness or excessive or inappropriate feelings of guilt
- energy loss and fatigue
- noticeable physical restlessness or slowed movements
- difficulty concentrating or making decisions
- changes in appetite and weight
- sleeping more or less than usual
- regular thoughts of death or suicide, with or without a plan for suicide
In addition to either the first or second criteria being present for at least 2 weeks, at least 4 more symptoms must also be present for a diagnosis of MDD. Most symptoms should be present nearly every day.
Bereavement exclusion
There’s been much discussion about removing the “bereavement exclusion” from the diagnosis of major depression, but not much will change for most clinicians.
This exclusion is applied only if a person presents with major depressive symptoms within the first 2 months after the death of a loved one.
This exclusion was omitted in the DSM-5 for several reasons, including:
- removing the idea that bereavement lasts only 2 months
- acknowledging that bereavement can lead to a major depressive episode and generally begin soon after a loss
- bereavement-related major depression may more likely occur in people with a history of major depressive episodes
- the depressive symptoms associated with bereavement can be treated with the same therapy and medication options as depression that’s not related to bereavement
When MDD occurs in the context of bereavement, in addition to depressive symptoms, a person might also experience:
- feelings of worthlessness
- poor physical (somatic) health
- inability to function in daily life, including at home, work, or with friends
- increased chance for persistent complex bereavement disorder
- suicidal ideation
A detailed footnote is included in the criteria for MDD to help mental health professionals determine whether a person is experiencing bereavement-related major depressive disorder.
Specifiers for depressive disorders
There are a few new specifiers added:
- mixed symptoms: this new specifier has been added across the bipolar and depressive disorders to allow for the possibility of manic features in people with unipolar depression
- anxious distress: this specifier allows for the ability to rate the severity of anxious distress in people with bipolar or depressive disorders
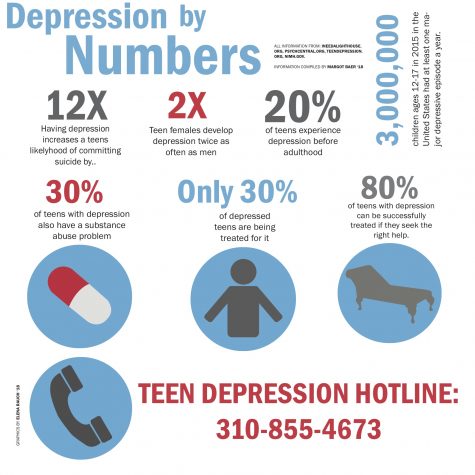
Major depressive disorder impacts the lives of many people in the United States. The National Institutes of Health (NIH) estimates that nearly 21 million adults in the United States had at least 1 major depressive episode in 2020.
Mental health professionals rely on the DSM-5 to provide an accurate and consistent diagnosis.
With the implementation of the DSM-5, depressive disorders saw some new classifications added with current conditions updated to reflect new research and scientific breakthroughs in mental health.
What Should I Know About DSM V Depression?
Updated October 6, 2022 by BetterHelp Editorial Team
DSM and depression are associated with one another, but they’re two very different things. Depression is a serious medical condition, while the DSM is a handbook that serves as an authoritative guide for diagnosing mental health disorders.
Managing Depression Starts With Small Steps
Begin Your Healing Journey With Therapy
Diagnostic Criteria For Depression According To the DSM-5Depression is a mental health disorder that may also be called a major depressive disorder or clinical depression. While depression is a mental health disorder, it can also cause physical symptoms like chronic pain or digestive issues. Depression manifests a bit differently in everyone, even though many of their symptoms may be the same. In some people, depression is fairly mild, and in others, it can be quite serious. Depending on the circumstances that brought the depression on, it can be temporary, or it can be persistent.
What Is The DSM?
DSM is an acronym for The Diagnostic and Statistical Manual of Mental Disorders (DSM), which is published by the American Psychiatric Association (APA). Healthcare providers in the United States, and somewhat in the world, rely on the DSM as an authoritative guide on diagnosing mental health disorders. Clinicians will find descriptions of mental health disorders, along with symptoms and other criteria to assist them in making qualified diagnoses. The other benefit to the DSM is that it uses common language for clinicians to use with their patients and with other clinicians, which provides consistency in diagnostics and research. Using a common language also helps pharmaceutical companies in the development of medications and other interventions.
I’m Struggling With Sadness, Do I Have Depression?
Everyone goes through periods of sadness for various lengths of time. If you consider that the main symptom of depression is sadness, it can be difficult to differentiate the difference between normal periods of sadness and depression that requires some type of clinical intervention.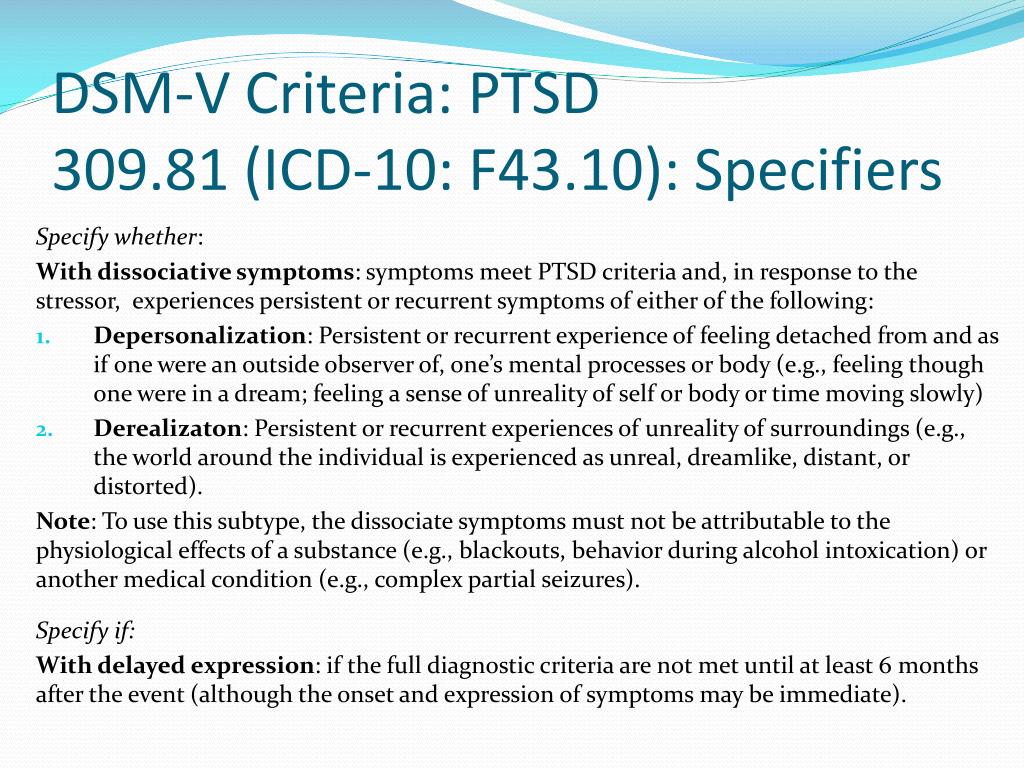
Sadness is a healthy emotion that all people experience at one time or another. It’s common to feel sadness as a result of a situation, event, or person. When you lose a job, end a relationship, get a diagnosis of serious physical disease or ailment, or hear of a loved one’s passing, you’re bound to be sad for some time.
When we contrast normal periods of sadness with depression, there’s no situation, event, or person that triggers depression. You should be able to feel happiness and joy when good things are happening in your life. You might feel frustrated, upset, or disappointed at times, but you should still be able to enjoy watching television, playing video games, reading, or doing other favorite activities. Normal periods of sadness won’t usually keep you up at night. It won’t prevent you from going to work in the morning. You’ll probably still feel like eating. In your interactions with friends, family, or coworkers, you might feel regret your words or actions, and you might wish you could have a “do-over,” but it won’t cause you to feel major guilt or worthlessness.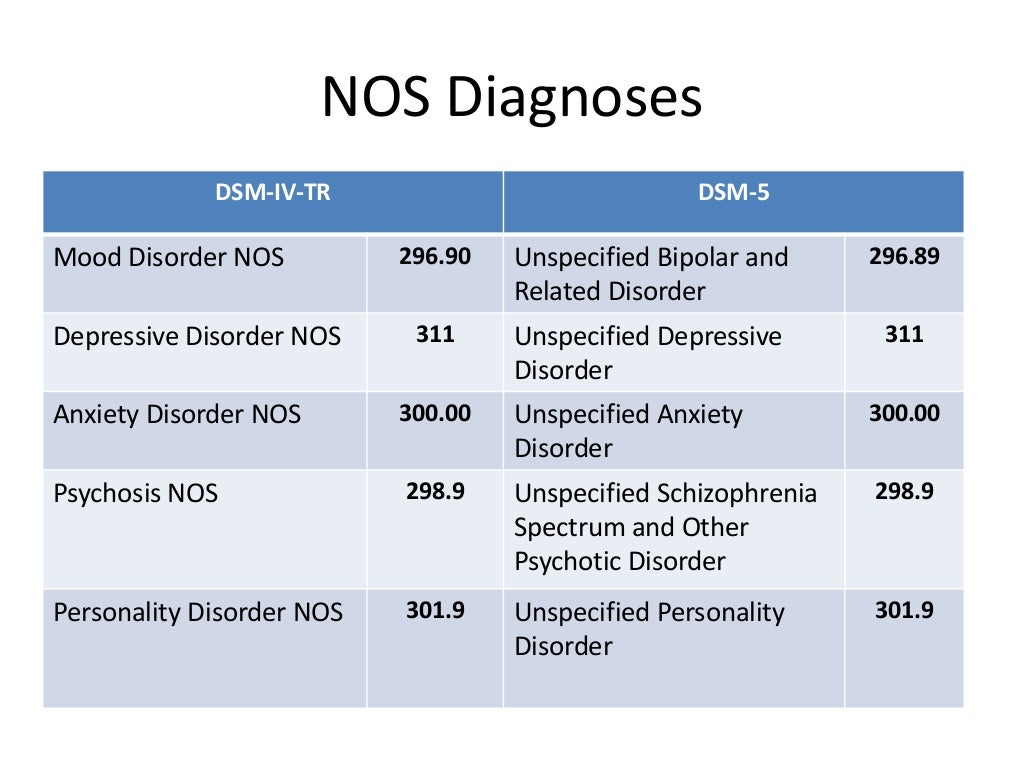
If you’re feeling sad and hopeless about everything, even when you can’t attribute it to anything specific, you may have a depressive disorder. If you have a major depressive disorder, you lose interest in the activities that you used to enjoy. You may not feel like eating, and you might be sleeping too much or too little. A depressive disorder may cause you to have negative thought patterns about yourself and everyone else.
Depression isn’t just a strong degree of sadness. It has to do with a combination of factors that relate to the duration of negative feelings, the impact they have on your body, other symptoms, and the effect that depressive symptoms have on your ability to manage normal, everyday functions. One of the most important differences between general sadness and a depressive disorder is that people with a major depressive disorder may have suicidal ideations or feelings about harming themselves or others that are difficult for them to shake off.
Diagnosing A Major Depressive Disorder During Times Of Loss Or Hardship
Diagnosing a depressive disorder becomes even more complicated when someone experiences a significant loss in addition to have persistent feelings of sadness.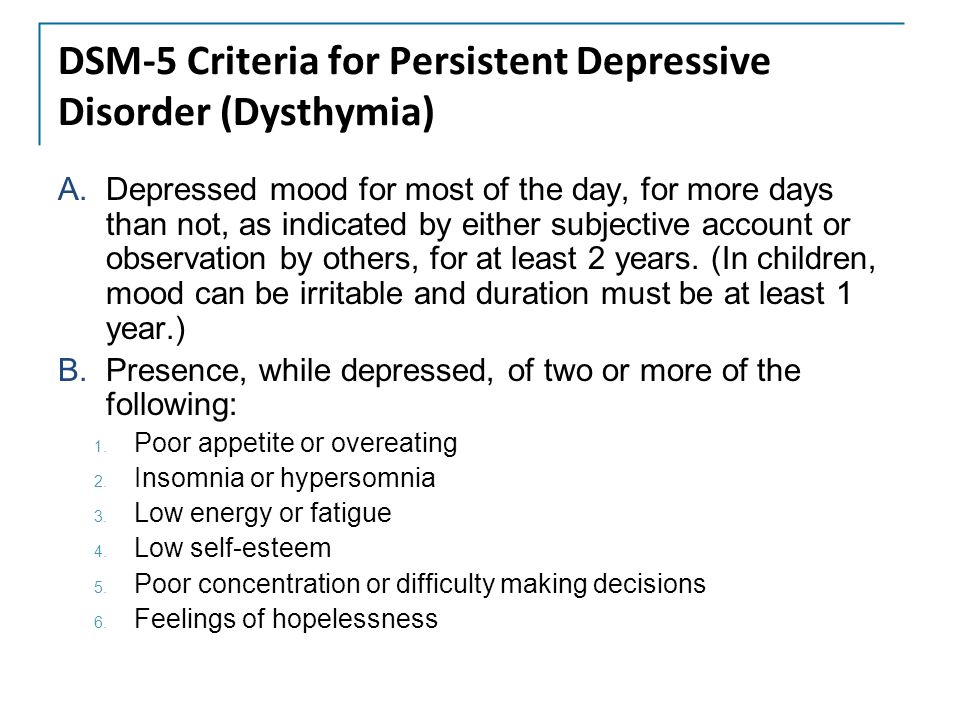 If this sounds like you or someone that you know, don’t try to make a diagnosis on your own and don’t ignore it. This type of situation calls for getting the opinion of a licensed clinician or other mental health professional.
If this sounds like you or someone that you know, don’t try to make a diagnosis on your own and don’t ignore it. This type of situation calls for getting the opinion of a licensed clinician or other mental health professional.
When you visit a mental health professional, they take a medical and mental health history from you. They will ask you a lot of questions, and they may ask you to fill out one or more questionnaires. Once they’ve done their due diligence in information gathering, they’ll compare the information with the criteria for major depressive disorder as provided by the American Psychiatric Association in the Diagnostic and Statistical Manual of Mental Disorders before making a diagnosis of a depressive disorder or something else.
The DSM-5 is the latest version of the Diagnostic and Statistical Manual of Mental Disorders. According to this guide, individuals must experience five or more of the following symptoms during the same two-week period, and the symptoms should either be related to a depressed mood or loss of interest or pleasure:
- Experiencing a depressed mood almost every day for most of the day.
- Having a noticeable decreased interest or pleasure in all or almost all activities that you formerly enjoyed almost every day.
- Having a significant weight gain or loss when not consciously trying to lose or gain weight or having a noticeable decrease or increase in appetite.
- Feeling like your thoughts are sluggish and having slower physical movements.
- Feeling fatigued or loss of energy almost every day.
- Having feelings of worthlessness, excessive guilt, or misdirected guilt almost every day.
- Difficulty being able to think, concentrate or focus almost every day.
- Having recurrent thoughts of death, having recurrent suicidal ideations, having a plan for committing suicide, or attempting suicide.
If you or someone that you know is experiencing the symptoms as described in the final bullet point, it’s important to seek emergency help. The National Suicide Prevention Lifeline 1-800-273-8255 and is available 24 hours a day, 7 days a week.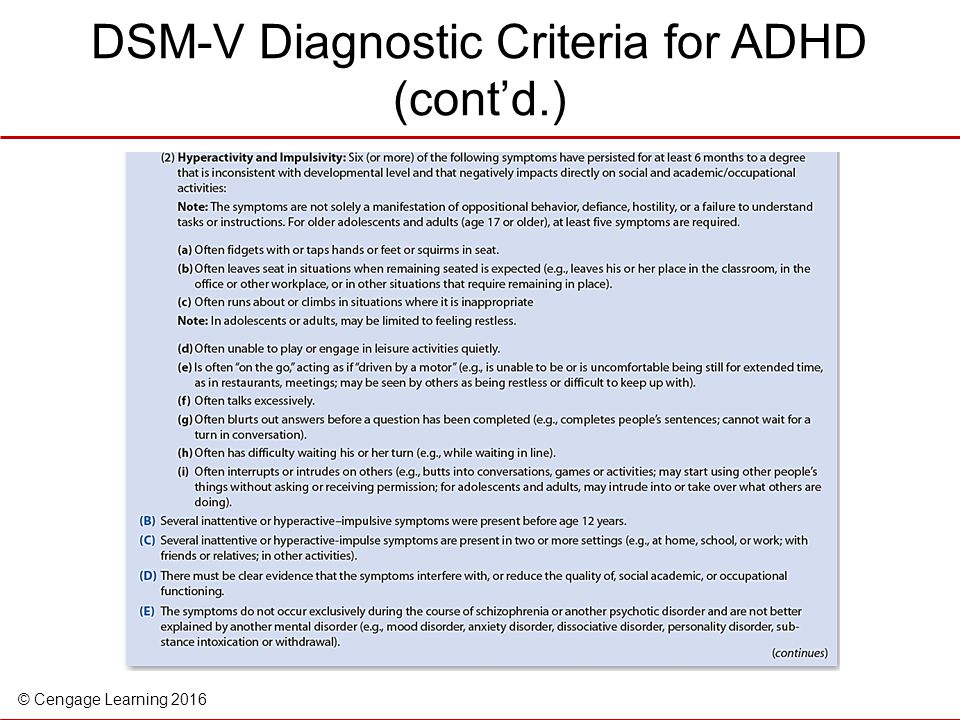
In the latest version of the DSM-5, the APA added two more specifications to help further classify diagnoses.
- Depression With Mixed Features. This means that for patients that don’t meet the full criteria for a manic episode, clinicians can allow for the presence of manic symptoms as part of their diagnosis for depression.
- Depression With Anxious Stress. Clinicians should perform an assessment of anxious distress as part of their assessment for depression and determine whether it warrants any changes in their prognosis, treatment options, or patient’s response to them.
What Are the Signs And Symptoms Of Clinical Depression?
No one is immune to the symptoms of clinical depression. It can strike anyone at any time, across genders, ethnicities, socioeconomic statuses, and other demographics.
For a clinician to accurately diagnose clinical depression, the symptoms of depression must be severe enough to cause disruption in their work, school, social life, or daily activities, and they shouldn’t be caused by substance abuse or some other medical condition.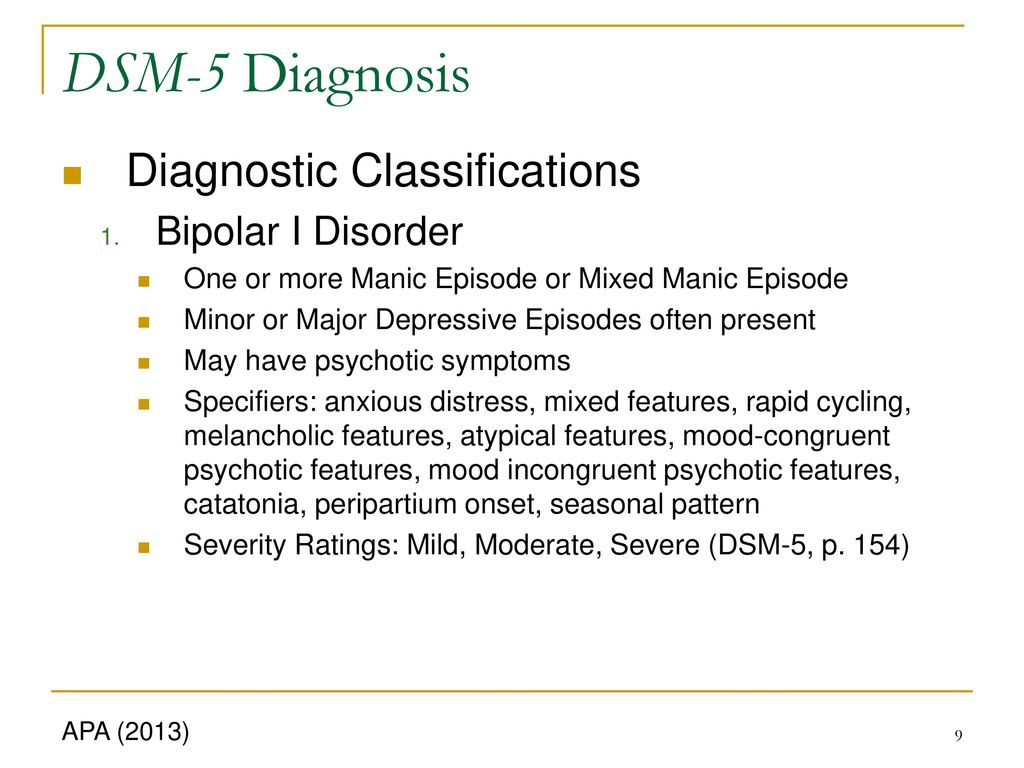
Managing Depression Starts With Small Steps
Begin Your Healing Journey With Therapy
Here are some of the questions a licensed clinician may ask to determine a diagnosis of clinical depression. Some of these are also listed under the criteria for the DSM-5.
- Feeling sad, teary-eyed, empty or hopeless
- Having angry outbursts, or expressing irritability or frustration over little things
- Losing interest or pleasure in most or all normal activities like sex, sports, or hobbies
- Sleeping far too much or far too little
- Being tired, lacking energy
- Extreme weight loss or weight gain or big changes in appetite
- Feeling anxious, agitated, or restless
- Experiencing slowed speech or body movements
- Feeling guilty, worthless, or fixating on past failures
- Having difficulty thinking, concentrating and making decisions
- Frequent or consistent thoughts of suicide or death
- Physical problems like back pain or headaches that can’t be explained
Suicide Associated With Major Depression
According to the U.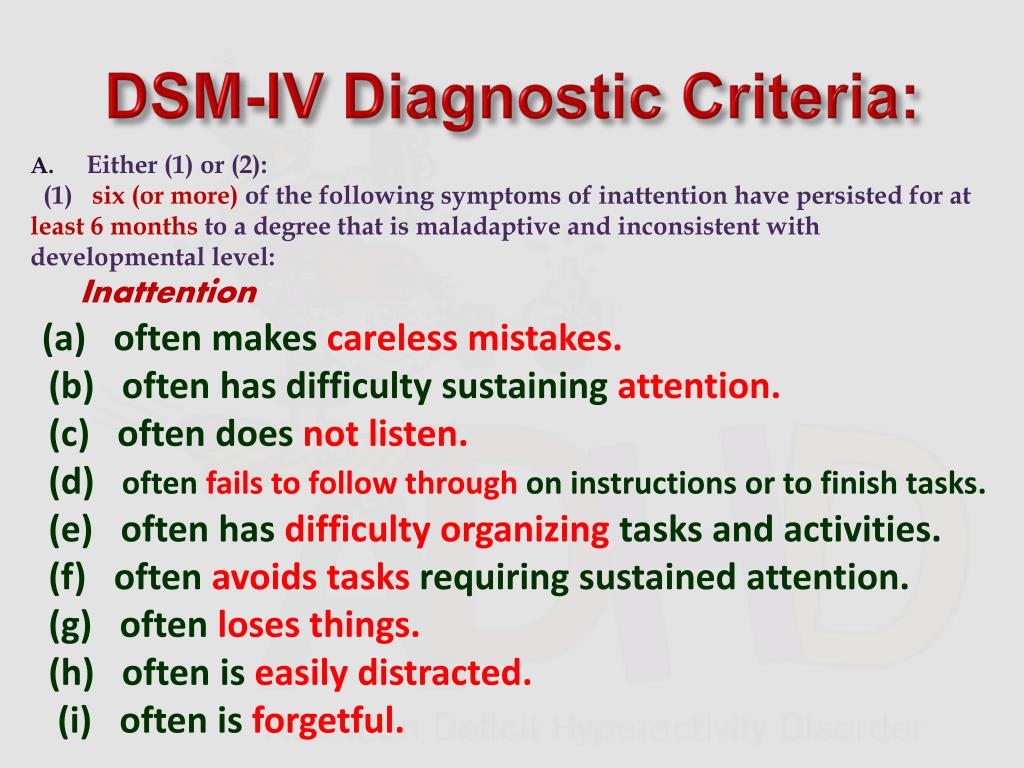 S. Department of Health and Human Services (HHS), the majority of people that have depression die due to a cause other than suicide. While that’s good news, people that have a diagnosis of depression have an increased risk of suicide when compared with people that don’t live with depression. In some cases, the risk of death by suicide may be related to the severity of the depression.
S. Department of Health and Human Services (HHS), the majority of people that have depression die due to a cause other than suicide. While that’s good news, people that have a diagnosis of depression have an increased risk of suicide when compared with people that don’t live with depression. In some cases, the risk of death by suicide may be related to the severity of the depression.
The rate for people living with depression that have been treated in an inpatient hospital setting is higher at 4%. Patients that were treated for depression on an in-patient basis following incidents of having suicidal ideations or suicide attempts are three times more likely (6%) to die by suicide as those who were treated in outpatient settings.
HHS also reports that there are significant differences in the risk of suicide connected with depression based on differences in gender. The rate for men with a lifetime history of depression that die by suicide is 7% as compared with only 1% of women that have a lifetime history of depression that die due to suicide.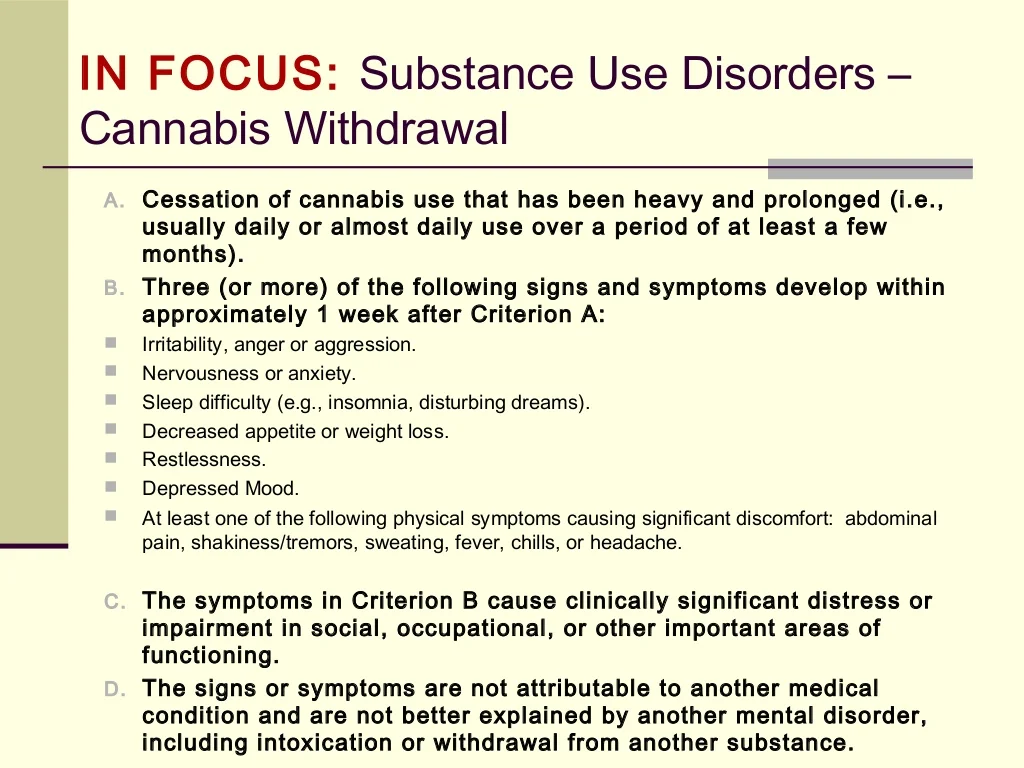
As mentioned above, if you or someone you know are suicidal, you should seek immediate help. The National Suicide Prevention Lifeline is available at 1-800-273-8255 and is reachable 24 hours a day, 7 days a week.
Clinical depression is a serious medical condition. If you suspect that you or someone that you care about has uncontrolled depression, it helps to schedule an appointment with a licensed therapist. Treatments for depression are usually quite effective. The sooner you seek help, the sooner you can begin to enjoy life again. Remember that no matter what you’re experiencing, with the right tools, you can move forward in healthy ways.
Other Commonly Asked Questions
Does the DSM-5 include depression?
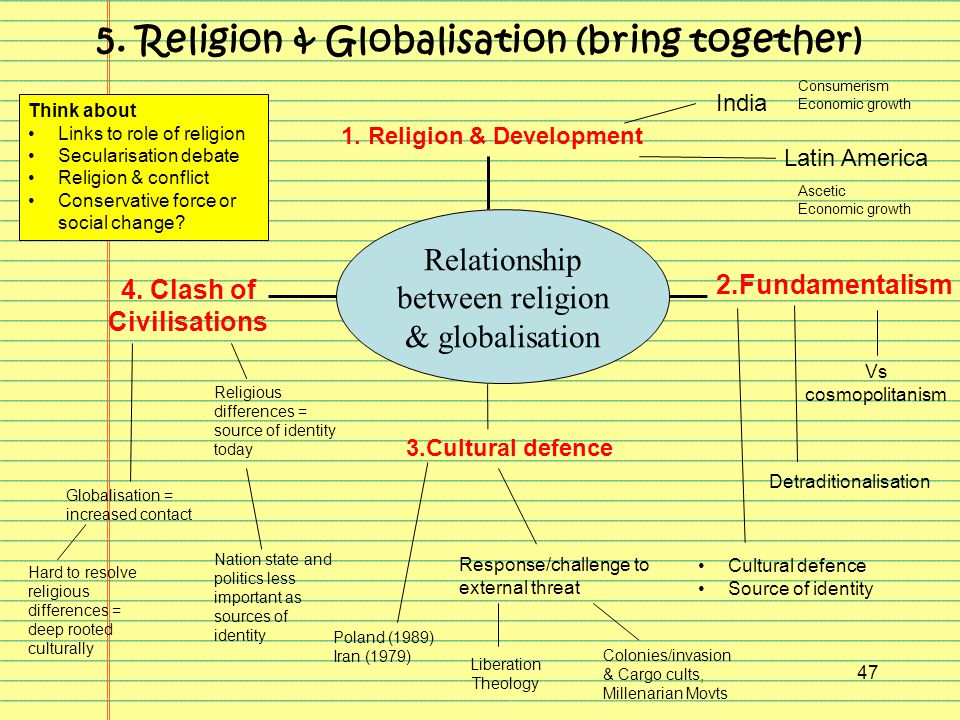
The DSM-5 includes various depressive disorders. These include but aren’t limited to premenstrual dysphoric disorder (PMDD), major depressive disorder (MDD), disruptive mood dysregulation disorder (DMDD), and persistent depressive disorder (PDD).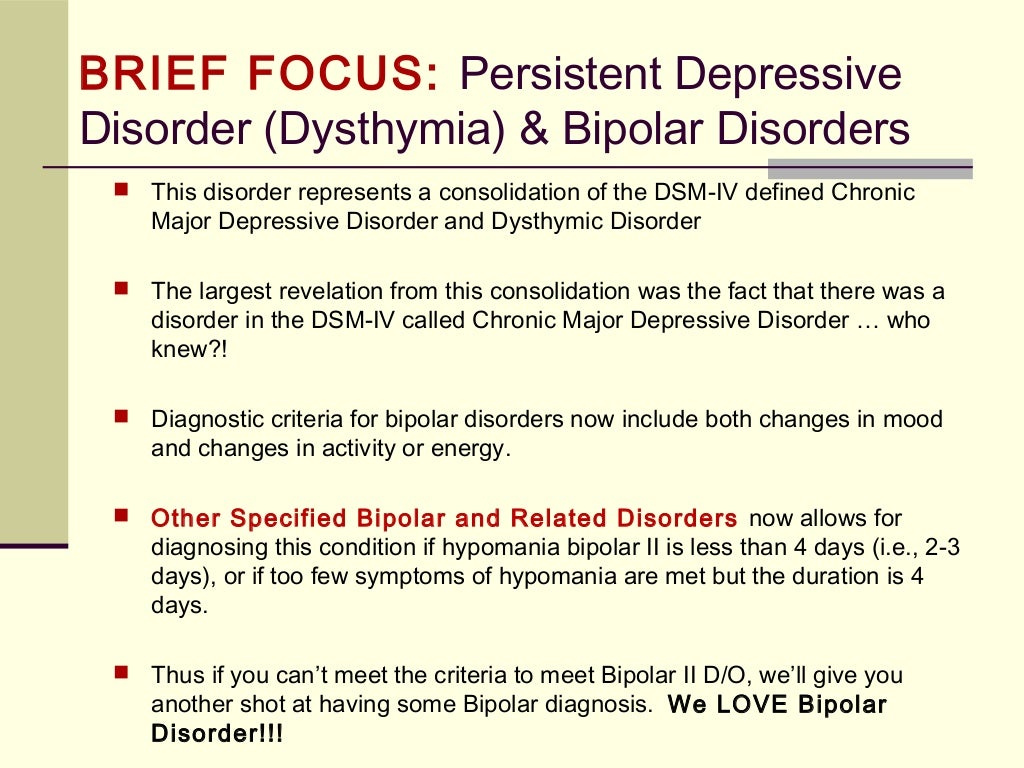 Bipolar disorder is a separate diagnosis from depressive disorders and is included under the category bipolar and related disorders. However, it is relevant to discuss because those with bipolar disorder experience alternating periods of depression and at least one manic episode or hypomanic episode. Clinical judgment will be used in the diagnostic process if other concerns (e.g. psychotic symptoms or symptoms of mania) may impact the final diagnosis a person receives. There are a variety of different potential risk factors that can increase the likelihood of a depression diagnosis. Depression risk factors include but are not restricted to the existence of another medical illness, family history, and adverse life experiences.
Bipolar disorder is a separate diagnosis from depressive disorders and is included under the category bipolar and related disorders. However, it is relevant to discuss because those with bipolar disorder experience alternating periods of depression and at least one manic episode or hypomanic episode. Clinical judgment will be used in the diagnostic process if other concerns (e.g. psychotic symptoms or symptoms of mania) may impact the final diagnosis a person receives. There are a variety of different potential risk factors that can increase the likelihood of a depression diagnosis. Depression risk factors include but are not restricted to the existence of another medical illness, family history, and adverse life experiences.
What is used to diagnose depression?
The criteria in the dsm 5 is what’s currently used to diagnose depressive disorders and other conditions, such as schizophrenia spectrum and other psychotic disorders (e.g., schizoaffective disorder, delusional disorder), anxiety disorders, and bipolar and related disorders.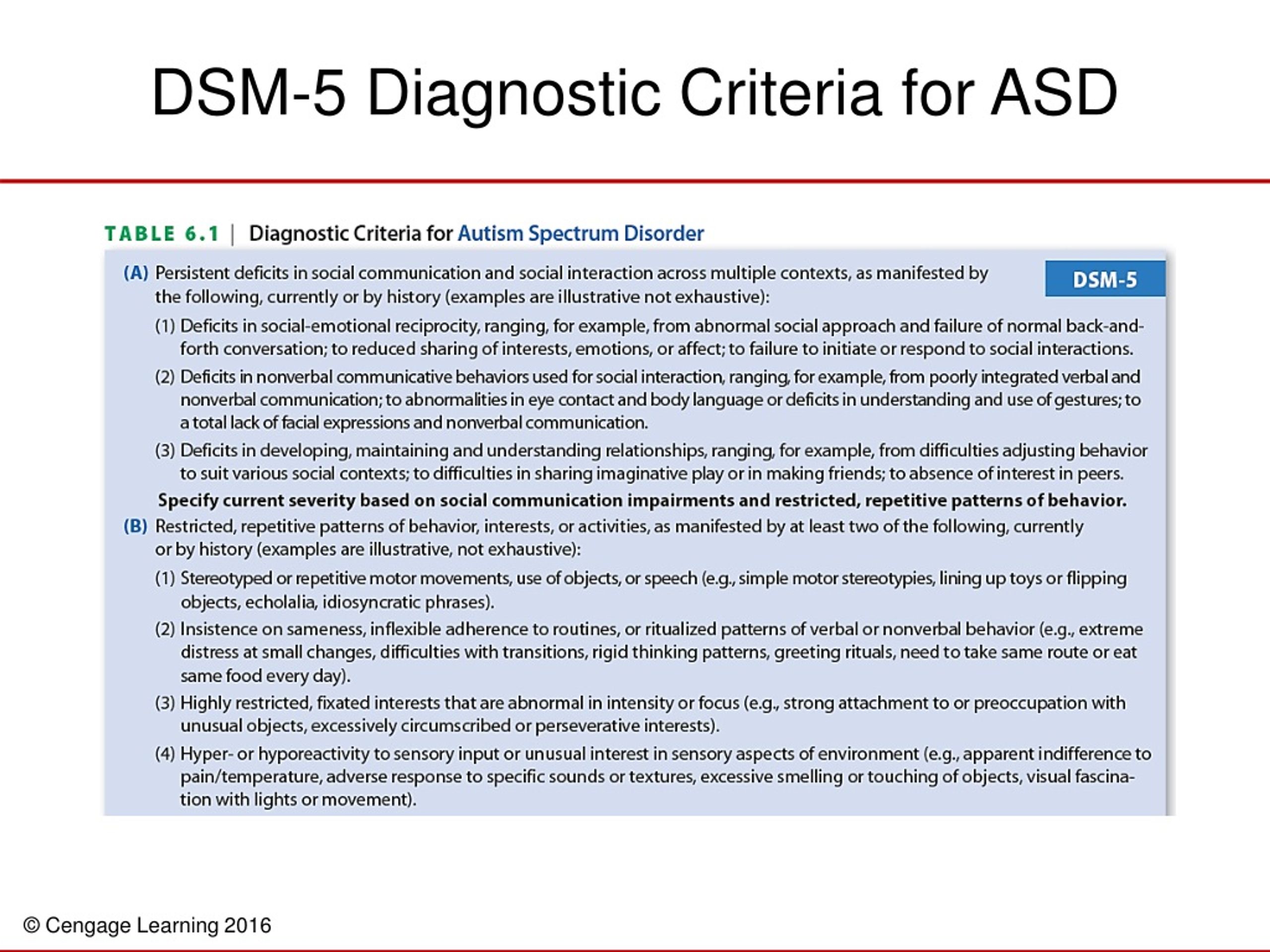 One of the significant changes made from the dsm iv tr to the dsm 5 is that the dsm 5 includes several additional depressive disorders, including disruptive mood dysregulation disorder (DMDD) and premenstrual dysphoric disorder (PMDD). The National Institutes of Health or NIH website indicates that in 2020, 71% of adults who experienced severe depression had received treatment in the past year. Depression is a very common mental health concern, and it is important that people reach out for support if they need it. The right care for depression, which may include therapy and other methods, can lead to symptom reduction. Psychotherapy can help you find not just emotional support but also coping skills and other tools that you can use to reduce or manage symptoms.
One of the significant changes made from the dsm iv tr to the dsm 5 is that the dsm 5 includes several additional depressive disorders, including disruptive mood dysregulation disorder (DMDD) and premenstrual dysphoric disorder (PMDD). The National Institutes of Health or NIH website indicates that in 2020, 71% of adults who experienced severe depression had received treatment in the past year. Depression is a very common mental health concern, and it is important that people reach out for support if they need it. The right care for depression, which may include therapy and other methods, can lead to symptom reduction. Psychotherapy can help you find not just emotional support but also coping skills and other tools that you can use to reduce or manage symptoms.
What are the requirements to be diagnosed with depression?
A major depressive episode is marked by five or more symptoms out of the nine possible symptoms listed below:
- A down, low, or depressed mood
- Low energy or fatigue
- Loss of interest in activities
- Changes in appetite or significant weight loss or gain
- A diminished ability to focus, think, or concentrate
- Insomnia or hypersomnia
- Recurring thoughts of death, suicidal ideation, or suicide attempt*
- A sense of worthlessness or disproportionate guilt
- Psychomotor changes significant enough that others notice
Symptoms need to last at least two weeks or more (exclude symptoms changes in appetite or significant weight loss or gain and suicidal ideation, recurring thoughts of death, or suicide attempt) and will cause clinically significant distress or an impairment in functioning and daily life activities such as work or school to mark a major depressive episode/episode of major depression.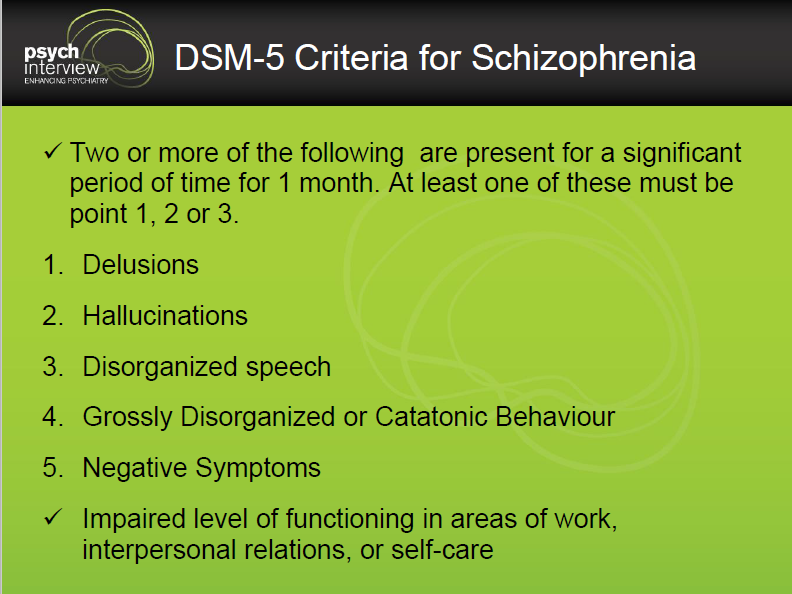 Additionally, these symptoms must not be directly substance induced or attributed to drug abuse**. Some people also experience concerns such as self harm. If you experience symptoms that cause individual clinically significant distress or impacts daily life activities, it is vital to reach out to a medical or mental healthcare professional who can help, such as a primary care physician, therapist, or psychiatrist.
Additionally, these symptoms must not be directly substance induced or attributed to drug abuse**. Some people also experience concerns such as self harm. If you experience symptoms that cause individual clinically significant distress or impacts daily life activities, it is vital to reach out to a medical or mental healthcare professional who can help, such as a primary care physician, therapist, or psychiatrist.
*If you or someone else you know is experiencing suicidal thoughts or ideation, please contact the Suicide and Crisis Lifeline at 988 or 1-800-273-8255.
**If you or someone you know experiences concerns related to substance abuse or substance use disorders, please contact the Substance Abuse and Mental Health Services Administration (SAMHSA) National Helpline at 1-800-662-HELP (4357).
Frequently Asked Questions (FAQs)
What is the DSM 5 definition of depression?
Under the DSM 5 definition of depression, you must have five of the following depression symptoms for a two-week period, and at least one of those symptoms must be item one or number two.
- Depressed mood most of the day nearly every day
- Markedly diminished interest or pleasure in all, or almost all, activities most of the day, nearly every day
- Significant weight loss when not dieting or weight gain, or decrease or increase in appetite nearly every day
- A slowing down of thought and a reduction of physical movement (observable by others, not merely subjective feelings of restlessness or being slowed down)
- Fatigue or loss of energy nearly every day
- Feelings of worthlessness or excessive or inappropriate guilt nearly every day
- Diminished ability to think or concentrate, or indecisiveness, nearly every day
- Recurrent thoughts of death, recurrent suicidal ideation without a specific plan, or a suicide attempt or a specific plan for committing suicide
If you are in crisis or significant distress, you can reach out now to the National Suicide Prevention Lifeline: 800-273-8255. The National Suicide Prevention Lifeline is available 24 hours a day, seven days a week, and is confidential. Loved ones of those in distress can also contact the National Suicide Prevention Lifeline. Their website includes links to other helps resources, such as other another national center or institute.
If you recognize depression symptoms in yourself or are otherwise concerned about your mental health and the ways it has significant distress or impairment on important areas of functioning in your life, such as impairment in social occupational or other important realms, you should reach out to a mental health professional or national center.
You can read on mental disorders DSM or on national center website, but only a mental health professional can diagnose you and recommend you treatment resources.
If you have depression, you are also at a higher risk for substance abuse, persistent depressive disorder, postpartum depression (and fathers can have postpartum depression too), eating disorders, and bipolar disorder. Depression is a common mental health condition, so reach out if you need help, particularly if you have severe depression. Your doctor will connect you with treatment, perhaps through a national center. More information on bipolar disorder can be found below.
What is the difference between DSM IV and DSM 5?
The DSM 5 is intended to allow practitioners to better identify and treat conditions. Some of the important areas of change include:
- The inclusion of Autism Spectrum Disorder as a new umbrella term.
- Clarification on ADHD.
- A new diagnosis of disruptive mood dysregulation disorder, which is relevant to children and adolescents
- Binge eating is a mental disorder
- Gender identity disorder has been removed and replaced with gender dysphoria
- Information on how to distinguish between grieving and major depression
- Hoarding has been added as disorder
- Excoriation was added as new version of obsessive-compulsive disorder
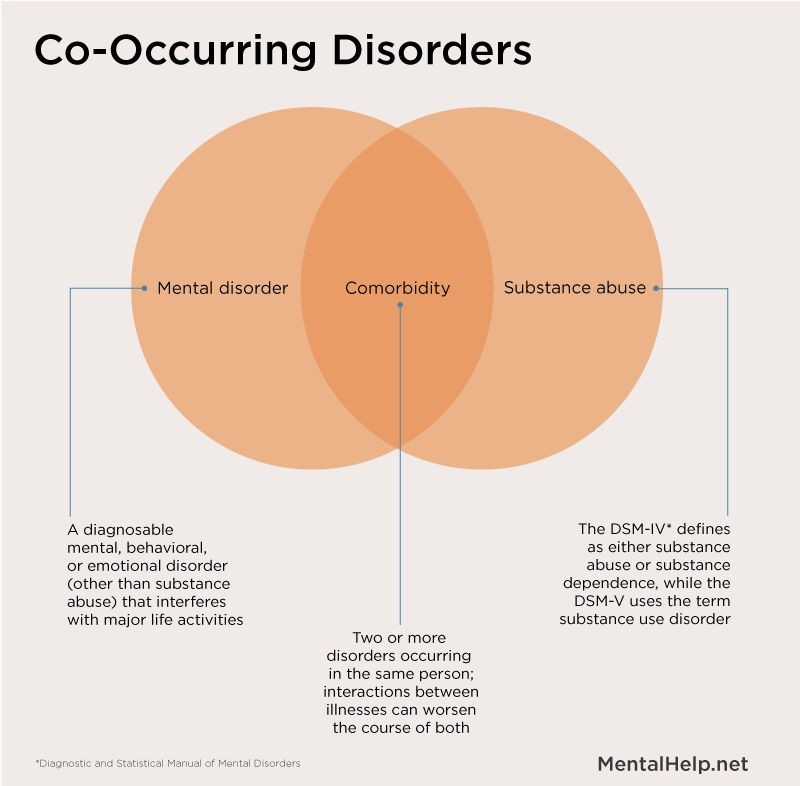
- Substance abuse and substance dependence were combined under substance abuse disorder
- Internet gaming disorder is a condition that needs more information
You can find out more about the new edition here.
Substance abuse is a common co-occurring condition with a mental health disorder, so if you have a mental illness, be careful to drink responsibly and not partake in drug abuse. If you believe you have a substance abuse or drug abuse problem, reach out to a mental health professional. Because depression is a common condition to have with a substance abuse or drug abuse issue, many places will treat both substance abuse and a mental illness at the same time. It is important to remember that substance abuse and drug abuse cannot and will not treat the root cause of a mental illness even if it brings temporary relief. A national center may have additional resources for you.
You can find more information about the changes to substance abuse classification in the DSM 5 here. One of the changes to substance abuse disorder is that criterion of legal problems from the DSM-IV was dropped in favor of cravings or a strong desire or urge to use a substance in the DSM-5.
What is the DSM 5 criteria for bipolar disorder?
To be diagnosed as having bipolar disorder, an individual must have experienced one episode of mania or hypomania. During the period of mania or hypomania, the person must have had three of the following symptoms and they should be a change from usual behavior:
- Inflated self-esteem or grandiosity
- Decreased need for sleep
- Increased talkativeness
- Racing thoughts
- Distracted easily
- Increase in goal-directed activity or psychomotor agitation
- Engaging in activities that hold the potential for painful consequences, e.g., unrestrained buying sprees
To have a depressive episode, a person must have five or more of the following depression symptoms for a two-week period.
- Depressed mood most of the day nearly every day
- Loss of interest or pleasure in all, or almost all, activities
- Significant weight loss or decrease or increase in appetite
- Engaging in purposeless movements, such as pacing the room
- Fatigue or loss of energy
- Feelings of worthlessness or guilt
- Diminished ability to think or concentrate, or indecisiveness
- Recurrent thoughts of death, recurrent suicidal ideation without a specific plan, or a suicide attempt
Remember that depression is a common mental health disorder, so you should seek a mental health professional if you have depression symptoms.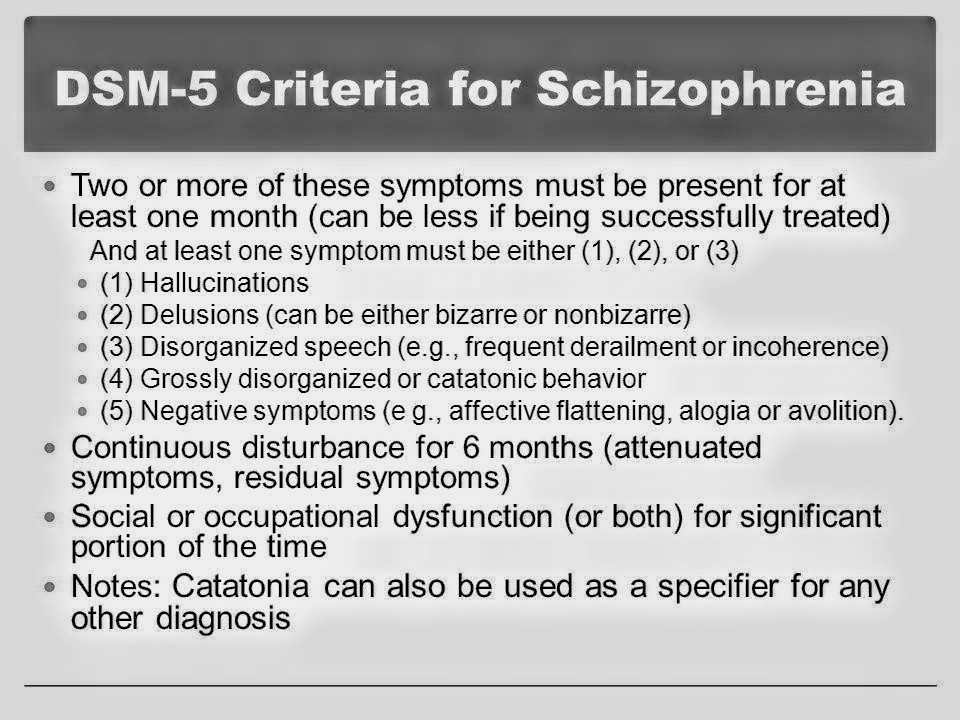 They can let you know if you have bipolar disorder or depression, and help you treat bipolar disorder or depression as necessary, such as recommending resources like from a national center.
They can let you know if you have bipolar disorder or depression, and help you treat bipolar disorder or depression as necessary, such as recommending resources like from a national center.
Is DSM IV still used?
The DSM 5 came out in 2013 and is the standard used by mental health professionals in the United States.
Why is DSM 5 criticized?
Some common criticisms of the DSM 5 include a propensity to over-diagnosis behaviors, the possible stigma than can come with the label of a diagnosis, over recommending pharmaceuticals, and general discussion with any version of the DSM about the accuracy and subjectivity.
What are DSM 5 V codes?
V codes are factors that may influence the diagnosis or treatment of a mental health disorder and should be noted by the mental health professional but are not mental health disorders on their own. Some examples are relational problems, educational and occupational problems, or housing and economic problems.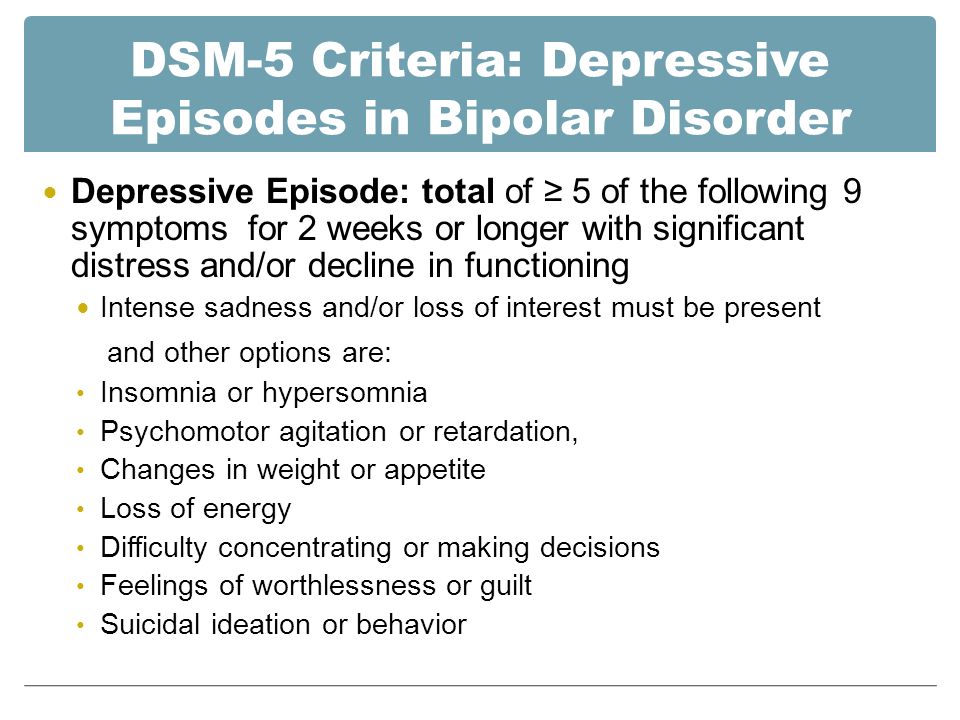
What is Axis V in mental health?
Axis V was a part of DSM-IV that provided a numeric score to describe how well a person was functioning in their life and how much the symptoms of their mental illness impact their day-to-day life.
Get Help & Support With Depression Today
Medicine, Pharmacy and Health News
Pharmacy and health medicine news | Remedium.ruPopular
- Mikhail Murashko spoke at the joint board of the Ministries of Health of the Russian Federation and the Republic of Belarus
- Timely diagnosis and treatment of orphan diseases requires new systemic solutions
- The first presentation of the Vladimir Ivanovich Kulakov Prize “Towards Life” took place in Moscow
- Obesity care for adults
- Online sales of prescription drugs
Portal map
- Media - News
- Press Releases
- Pharmacists
- Doctors
- Obstetrics and gynecology
- Allergology
- Gastroenterology
- Hepatology
- Dermatology
- Dietetics
- Infectious diseases
- Research and development
- Cardiology
- Neurology
- Oncology
- Otorhinolaryngology
- Pediatrics
- Psychiatry
- Psychology
- Pulmonology
- Rheumatology
- Dentistry
- Therapy
- Traumatology
- Urology
- Surgery
- Endocrinology
- Health professionals
- Pharmaceutical market
- Industry
- Pharmaceutical industry
- Medical equipment +
- Legal Chronicle
- Analytics
- Legislation
- Documents for pharmacies
- Health records
- Miscellaneous documents
- Medical publications
- Magazines
- Books
- Activities
- About
- About project
- Advertising
- Contacts
- Search
- English
| Login: | |
| Password: | |
| Remember me | |
| Registration | |
| Forgot your password? | |
Subscription Online
Books Magazines
News
December 12, 2022
It is now possible to transport Russian medicines through Belarus
The Council of Ministers of Belarus has allowed the transit of medicines registered in Russia through the country.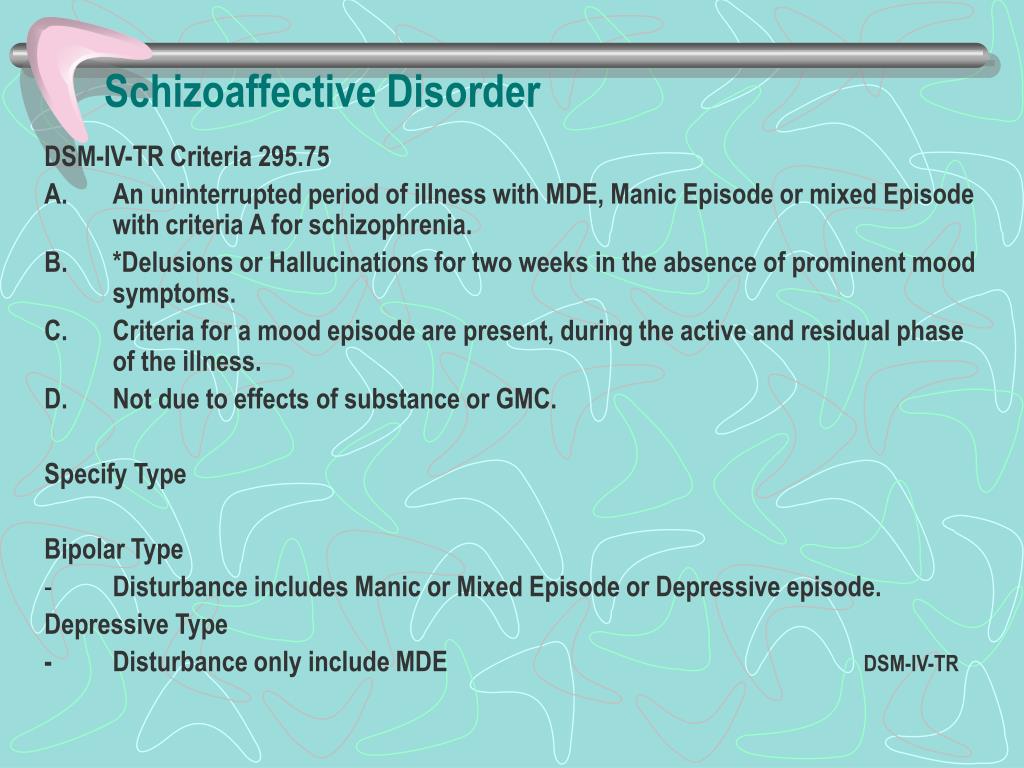
More
December 12, 2022
Novartis Announces Second Successful Phase III Trial of Targeted Factor B Inhibitor Iptacopan
December 12, 2022
It became easier to apply for the import of unregistered drugs and biomaterials
/upload/medialibrary/605/kr_cogn_gl_3.pdf
Doctors
December 6, 2022
Characteristics of the personality profile and adherence to therapy as predictors of compensation for type 1 diabetes mellitus in adolescents
I.L. Nikitina, A.O. Plaksina, A.S. Pirozhkova, I.A. Kelmanson ; National.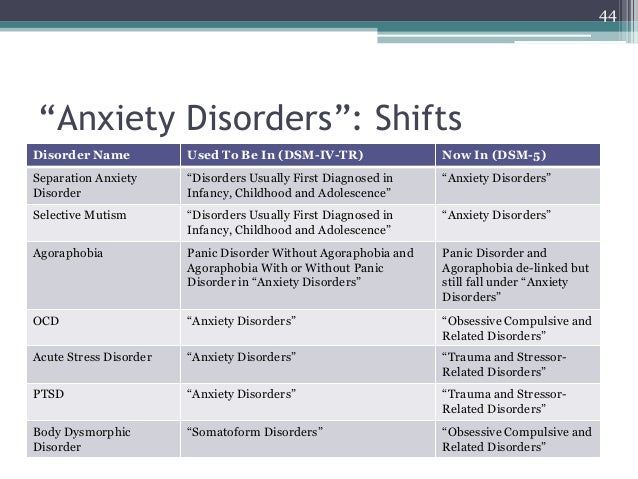 ..
..
More
December 2, 2022
Topical antibiotic therapy for perforated otitis in the COVID-19 pandemic
December 1, 2022
Lecture: Non-respiratory complications of COVID in children
Pharmacists
December 12, 2022
Lecture: Modern pharmacy. Fine tuning of the gastrointestinal tract
We present to your attention a lecture for pharmacists and pharmacists “Modern Pharmacy. Thin...
More
December 12, 2022
Lecture: Modern Pharmacy
October 24, 2022
Discovery of competitors near the pharmacy organization
Search
Partition not found.
Partition not found.
Medicine, Pharmacy and Health News
Pharmacy and health medicine news | Remedium.ruPopular
- Mikhail Murashko spoke at the joint board of the Ministries of Health of the Russian Federation and the Republic of Belarus
- Timely diagnosis and treatment of orphan diseases requires new systemic solutions
- The first presentation of the Vladimir Ivanovich Kulakov Prize "Towards Life" took place in Moscow
- Obesity care for adults
- Online sales of prescription drugs
Portal Map
- Media - News
- Press Releases
- Pharmacists
- Doctors
- Obstetrics and gynecology
- Allergology
- Gastroenterology
- Hepatology
- Dermatology
- Dietetics
- Infectious diseases
- Research and development
- Cardiology
- Neurology
- Oncology
- Otorhinolaryngology
- Pediatrics
- Psychiatry
- Psychology
- Pulmonology
- Rheumatology
- Dentistry
- Therapy
- Traumatology
- Urology
- Surgery
- Endocrinology
- Health professionals
- Pharmaceutical market
- Industry
- Pharmaceutical industry
- Medical equipment +
- Legal Chronicle
- Analytics
- Legislation
- Documents for pharmacies
- Health records
- Miscellaneous documents
- Medical publications
- Magazines
- Books
- Activities
- About
- About project
- Advertising
- Contacts
- Search
- English
| Login: | |
| Password: | |
| Remember me | |
| Registration | |
| Forgot your password? | |
Subscription Online
Books Magazines
News
December 12, 2022
It is now possible to transport Russian medicines through Belarus
The Council of Ministers of Belarus has allowed the transit of medicines registered in Russia through the country.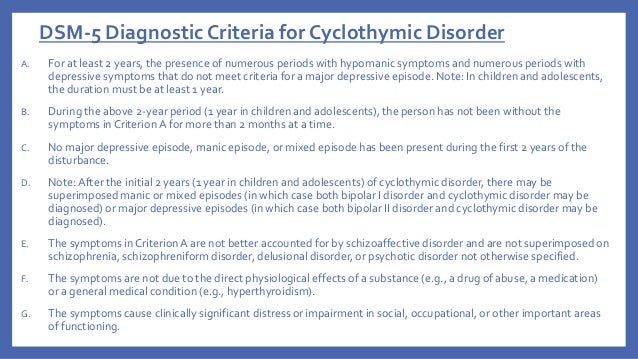
More
December 12, 2022
Novartis Announces Second Successful Phase III Trial of Targeted Factor B Inhibitor Iptacopan
December 12, 2022
It became easier to apply for the import of unregistered drugs and biomaterials
/upload/iblock/90b/parkinson%2520s%2520disease.pdf
Doctors
December 6, 2022
Characteristics of the personality profile and adherence to therapy as predictors of compensation for type 1 diabetes mellitus in adolescents
I.L. Nikitina, A.O. Plaksina, A.S. Pirozhkova, I.A. Kelmanson ; National.