Drug that erases memory
Caution! These 10 Drugs Can Cause Memory Loss
7. Hypertension drugs (Beta-blockers)
Why they are prescribed: Beta-blockers slow the heart rate and lower blood pressure and typically are prescribed for high blood pressure, congestive heart failure and abnormal heart rhythms. They're also used to treat chest pain (angina), migraines, tremors and, in eyedrop form, certain types of glaucoma.
Examples: Atenolol (Tenormin), carvedilol (Coreg), metoprolol (Lopressor, Toprol), propranolol (Inderal), sotalol (Betapace), timolol (Timoptic) and some other drugs whose chemical names end with "-olol."
How they can cause memory loss: Beta-blockers are thought to cause memory problems by interfering with ("blocking") the action of key chemical messengers in the brain, including norepinephrine and epinephrine.
Alternatives: For older people, benzothiazepine calcium channel blockers, another type of blood pressure medication, are often safer and more effective than beta-blockers. If the beta-blocker is being used to treat glaucoma, I recommend talking with your health care professional about potentially using a carbonic anhydrase inhibitor, such as dorzolamide (Trusopt), instead.
8. Sleeping aids (Nonbenzodiazepine sedative-hypnotics)
Why they are prescribed: Sometimes called the "Z" drugs, these medications are used to treat insomnia and other sleep problems. They also are prescribed for mild anxiety.
Examples: Eszopiclone (Lunesta), zaleplon (Sonata) and zolpidem (Ambien).
How they can cause memory loss: Although these are molecularly distinct from benzodiazepines (see No. 1 above), they act on many of the same brain pathways and chemical messengers, producing similar side effects and problems with addiction and withdrawal.
The "Z" drugs also can cause amnesia and sometimes trigger dangerous or strange behaviors, such as cooking a meal or driving a car — with no recollection of the event upon awakening.
Alternatives: There are alternative drug and nondrug treatments for insomnia and anxiety, so talk with your health care professional about options. Melatonin, in doses from 3 to 10 mg before bedtime, for instance, sometimes helps to reestablish healthy sleep patterns.
Melatonin, in doses from 3 to 10 mg before bedtime, for instance, sometimes helps to reestablish healthy sleep patterns.
Before stopping or reducing the dosage of these sleeping aids, be sure to consult your health care professional. Sudden withdrawal can cause serious side effects, so a health professional should always monitor the process.
9. Incontinence drugs (Anticholinergics)
Why they are prescribed: These medications are used to relieve symptoms of overactive bladder and reduce episodes of urge incontinence, an urge to urinate so sudden and strong that you often can't get to a bathroom in time.
Examples: Darifenacin (Enablex), oxybutynin (Ditropan XL, Gelnique, Oxytrol), solifenacin (Vesicare), tolterodine (Detrol) and trospium (Sanctura). Another oxybutynin product, Oxytrol for Women, is sold over the counter.
How they can cause memory loss: These drugs block the action of acetylcholine, a chemical messenger that mediates all sorts of functions in the body. In the bladder, anticholinergics prevent involuntary contractions of the muscles that control urine flow. In the brain, they inhibit activity in the memory and learning centers. The risk of memory loss is heightened when the drugs are taken for more than a short time or used with other anticholinergic drugs.
In the bladder, anticholinergics prevent involuntary contractions of the muscles that control urine flow. In the brain, they inhibit activity in the memory and learning centers. The risk of memory loss is heightened when the drugs are taken for more than a short time or used with other anticholinergic drugs.
A 2006 study of oxybutynin ER, for example, found its effect on memory to be comparable to about 10 years of cognitive aging. ("In other words," as the study's lead author put it, "we transformed these people from functioning like 67-year-olds to 77-year-olds.")
Older people are particularly vulnerable to the other adverse effects of anticholinergic drugs, including constipation (which, in turn, can cause urinary incontinence), blurred vision, dizziness, anxiety, depression and hallucinations.
Alternatives: As a first step, it's important to make sure that you have been properly diagnosed. Check with your doctor or other health professional to see if your urinary incontinence symptoms might stem from another condition (such as a bladder infection or another form of incontinence) or a medication (such as a blood pressure drug, diuretic or muscle relaxant).
Once these are ruled out, I'd recommend trying some simple lifestyle changes, such as cutting back on caffeinated and alcoholic beverages, drinking less before bedtime, and doing Kegel exercises to strengthen the pelvic muscles that help control urination.
If these approaches don't work out, consider trying adult diapers, pads or panty liners, which can be purchased just about anywhere. They can be worn comfortably (and invisibly) under everyday clothing and virtually eliminate the risk of embarrassing accidents. In my experience, many patients are reluctant to try this approach, but once over the initial hurdle, come to prefer it for security and peace of mind.
Correction: An earlier version of this article mistakenly implied that mirabegron (Myrbetriq), which the FDA approved last year for the treatment of overactive bladder, is an anticholinergic drug; in fact, it is in a new class of medications called beta-3 adrenergic agonists and is not expected to cause memory loss seen with anticholinergic medications. There currently are no data describing the effect of Myrbetriq on cognition.
There currently are no data describing the effect of Myrbetriq on cognition.
Ask the Pharmacist
Information contained in the Ask the Pharmacist column by Dr. Armon B. Neel Jr. is intended to help individuals and their families become more informed about medication usage and interactions, and be better health care consumers. Any advice or information provided should not be followed in lieu of a personal consultation with a trained medical professional.
10. Antihistamines (First-generation)
Why they are prescribed: These medications are used to relieve or prevent allergy symptoms or those of the common cold. Some antihistamines are also used to prevent motion sickness, nausea, vomiting and dizziness, and to treat anxiety or insomnia.
Examples: Brompheniramine (Dimetane), carbinoxamine (Clistin), chlorpheniramine (Chlor-Trimeton), clemastine (Tavist), diphenhydramine (Benadryl) and hydroxyzine (Vistaril).
How they can cause memory loss: These medications (prescription and over-the-counter) inhibit the action of acetylcholine, a chemical messenger that mediates a wide range of functions in the body. In the brain, they inhibit activity in the memory and learning centers, which can lead to memory loss.
In the brain, they inhibit activity in the memory and learning centers, which can lead to memory loss.
Alternatives: Newer-generation antihistamines such as loratadine (Claritin) and cetirizine (Zyrtec) are better tolerated by older patients and do not present the same risks to memory and cognition.
The Forgetting Pill Erases Painful Memories Forever
Jonah Lehrer
New research shows that memories are formed and then actually rebuilt — and soon scientists may be able to target and erase specific memories altogether.
Photo: Dwight Eschliman
Jeffrey Mitchell, a volunteer firefighter in the suburbs of Baltimore, came across the accident by chance: A car had smashed into a pickup truck loaded with metal pipes. Mitchell tried to help, but he saw at once that he was too late.
The car had rear-ended the truck at high speed, sending a pipe through the windshield and into the chest of the passenger—a young bride returning home from her wedding. There was blood everywhere, staining her white dress crimson.
Mitchell couldn't get the dead woman out of his mind; the tableau was stuck before his eyes. He tried to tough it out, but after months of suffering, he couldn't take it anymore. He finally told his brother, a fellow firefighter, about it.
Pushing to remember a traumatic event soon after it occurs doesn’t unburden us—it reinforces the fear and stress.
Miraculously, that worked. No more trauma; Mitchell felt free. This dramatic recovery, along with the experiences of fellow first responders, led Mitchell to do some research into recovery from trauma. He eventually concluded that he had stumbled upon a powerful treatment. In 1983, nearly a decade after the car accident, Mitchell wrote an influential paper in the Journal of Emergency Medical Services that transformed his experience into a seven-step practice, which he called critical incident stress debriefing, or CISD.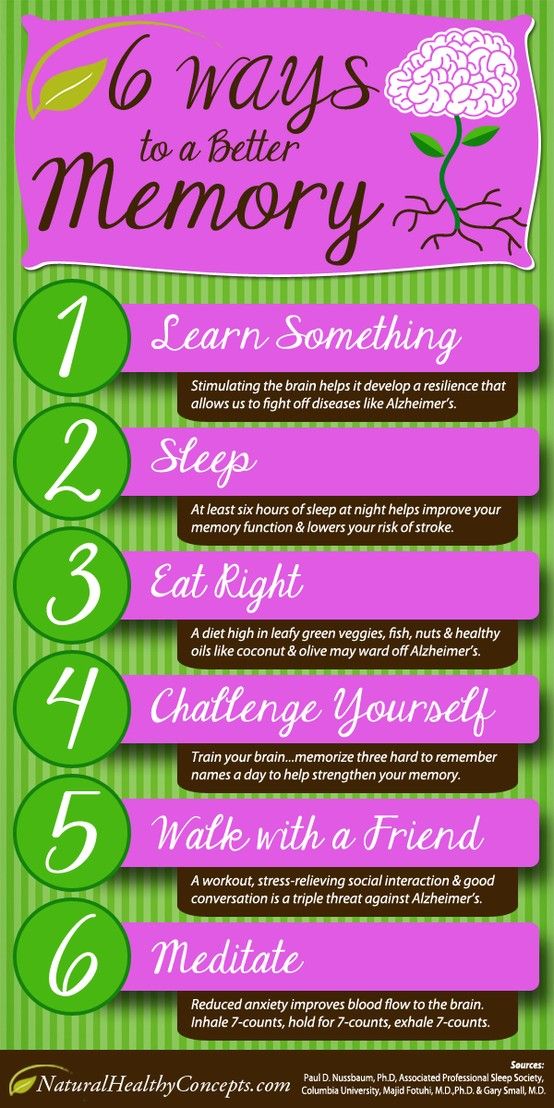 The central idea: People who survive a painful event should express their feelings soon after so the memory isn't "sealed over" and repressed, which could lead to post-traumatic stress disorder.
The central idea: People who survive a painful event should express their feelings soon after so the memory isn't "sealed over" and repressed, which could lead to post-traumatic stress disorder.
In recent years, CISD has become exceedingly popular, used by the US Department of Defense, the Federal Emergency Management Agency, the Israeli army, the United Nations, and the American Red Cross. Each year, more than 30,000 people are trained in the technique. (After the September 11 attacks, 2,000 facilitators descended on New York City.)
Even though PTSD is triggered by a stressful incident, it is really a disease of memory. The problem isn't the trauma—it's that the trauma can't be forgotten. Most memories, and their associated emotions, fade with time. But PTSD memories remain horribly intense, bleeding into the present and ruining the future. So, in theory, the act of sharing those memories is an act of forgetting them.
A typical CISD session lasts about three hours and involves a trained facilitator who encourages people involved to describe the event from their perspective in as much detail as possible. Facilitators are trained to probe deeply and directly, asking questions such as, what was the worst part of the incident for you personally? The underlying assumption is that a way to ease a traumatic memory is to express it.
Facilitators are trained to probe deeply and directly, asking questions such as, what was the worst part of the incident for you personally? The underlying assumption is that a way to ease a traumatic memory is to express it.
The problem is, CISD rarely helps—and recent studies show it often makes things worse. In one, burn victims were randomly assigned to receive either CISD or no treatment at all. A year later, those who went through a debriefing were more anxious and depressed and nearly three times as likely to suffer from PTSD. Another trial showed CISD was ineffective at preventing post-traumatic stress in victims of violent crime, and a US Army study of 952 Kosovo peacekeepers found that debriefing did not hasten recovery and led to more alcohol abuse. Psychologists have begun to recommend that the practice be discontinued for disaster survivors. (Mitchell now says that he doesn't think CISD necessarily helps post-traumatic stress at all, but his early papers on the subject seem clear on the link.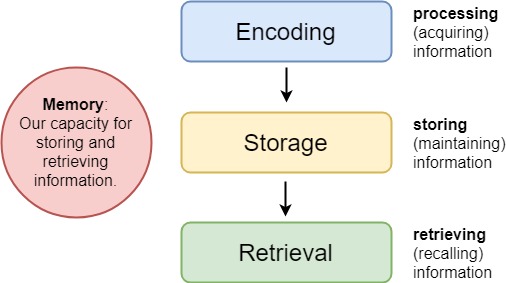 )
)
Most Popular
Mitchell was right about one thing, though. Traumatic, persistent memories are indeed a case of recall gone awry. But as a treatment, CISD misapprehends how memory works. It suggests that the way to get rid of a bad memory, or at a minimum denude it of its negative emotional connotations, is to talk it out. That's where Mitchell went wrong. It wasn't his fault, really; this mistaken notion has been around for thousands of years. Since the time of the ancient Greeks, people have imagined memories to be a stable form of information that persists reliably. The metaphors for this persistence have changed over time—Plato compared our recollections to impressions in a wax tablet, and the idea of a biological hard drive is popular today—but the basic model has not. Once a memory is formed, we assume that it will stay the same. This, in fact, is why we trust our recollections. They feel like indelible portraits of the past.
None of this is true. In the past decade, scientists have come to realize that our memories are not inert packets of data and they don't remain constant. Even though every memory feels like an honest representation, that sense of authenticity is the biggest lie of all.
When CISD fails, it fails because, as scientists have recently learned, the very act of remembering changes the memory itself. New research is showing that every time we recall an event, the structure of that memory in the brain is altered in light of the present moment, warped by our current feelings and knowledge. That's why pushing to remember a traumatic event so soon after it occurs doesn't unburden us; it reinforces the fear and stress that are part of the recollection.
This new model of memory isn't just a theory—neuroscientists actually have a molecular explanation of how and why memories change. In fact, their definition of memory has broadened to encompass not only the cliché cinematic scenes from childhood but also the persisting mental loops of illnesses like PTSD and addiction—and even pain disorders like neuropathy. Unlike most brain research, the field of memory has actually developed simpler explanations. Whenever the brain wants to retain something, it relies on just a handful of chemicals. Even more startling, an equally small family of compounds could turn out to be a universal eraser of history, a pill that we could take whenever we wanted to forget anything.
Unlike most brain research, the field of memory has actually developed simpler explanations. Whenever the brain wants to retain something, it relies on just a handful of chemicals. Even more startling, an equally small family of compounds could turn out to be a universal eraser of history, a pill that we could take whenever we wanted to forget anything.
And researchers have found one of these compounds.
In the very near future, the act of remembering will become a choice.
Photo illustration: Curtis Mann; Photo: Owen Franken/Corbis
Most Popular
Every memory begins as a changed set of connections among cells in the brain. If you happen to remember this moment—the content of this sentence—it's because a network of neurons has been altered, woven more tightly together within a vast electrical fabric. This linkage is literal: For a memory to exist, these scattered cells must become more sensitive to the activity of the others, so that if one cell fires, the rest of the circuit lights up as well. Scientists refer to this process as long-term potentiation, and it involves an intricate cascade of gene activations and protein synthesis that makes it easier for these neurons to pass along their electrical excitement. Sometimes this requires the addition of new receptors at the dendritic end of a neuron, or an increase in the release of the chemical neurotransmitters that nerve cells use to communicate. Neurons will actually sprout new ion channels along their length, allowing them to generate more voltage. Collectively this creation of long-term potentiation is called the consolidation phase, when the circuit of cells representing a memory is first linked together. Regardless of the molecular details, it's clear that even minor memories require major work. The past has to be wired into your hardware.
Scientists refer to this process as long-term potentiation, and it involves an intricate cascade of gene activations and protein synthesis that makes it easier for these neurons to pass along their electrical excitement. Sometimes this requires the addition of new receptors at the dendritic end of a neuron, or an increase in the release of the chemical neurotransmitters that nerve cells use to communicate. Neurons will actually sprout new ion channels along their length, allowing them to generate more voltage. Collectively this creation of long-term potentiation is called the consolidation phase, when the circuit of cells representing a memory is first linked together. Regardless of the molecular details, it's clear that even minor memories require major work. The past has to be wired into your hardware.
That understanding of how memories are created emerged in the 1970s. But what happens after a memory is formed, when we attempt to access it, was much less well understood. In the late 1990s, Karim Nader, a young neuroscientist studying emotional response at New York University, realized that no one knew.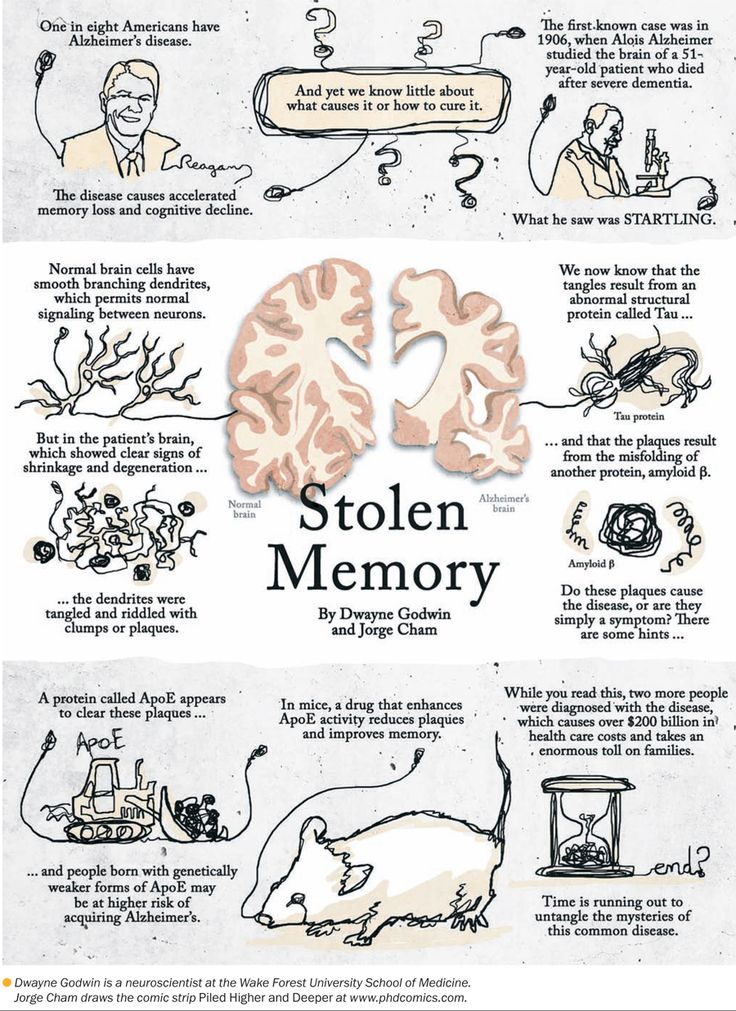 "My big advantage was that I wasn't trained in memory," Nader says. "I was very naive about the subject. Even though the field wasn't that interested in the mechanisms of recall, it struck me as a mystery worth pursuing."
"My big advantage was that I wasn't trained in memory," Nader says. "I was very naive about the subject. Even though the field wasn't that interested in the mechanisms of recall, it struck me as a mystery worth pursuing."
He began with the simplest question he could think of. While it was clear that new proteins were needed for the making of memories—proteins are cellular bricks and mortar, the basis of any new biological construction—were additional proteins made when those memories were recalled? Nader hypothesized that they were, and he realized that he could test his notion by temporarily blocking protein synthesis in a brain and looking to see if that altered recall. "This is the kind of question you ask when you don't know how else to approach the subject," Nader says. "But I had to do something, so why not this?"
His boss, the famed neuroscientist Joseph LeDoux, couldn't have been more discouraging. "I told Karim he was wasting his time," LeDoux says. "I didn't think the experiment would work. " To LeDoux, the reason was obvious: Even if Nader blocked protein synthesis during recall, the original circuitry would still be intact, so the memory should be too. If Nader could induce amnesia, it would be temporary. Once the block was removed, the recall would return as strong as ever. And so LeDoux and Nader made a bet: If Nader failed to permanently erase a set of fear memories in four lab animals, he had to buy LeDoux a bottle of tequila. If it worked, drinks were on LeDoux. "I honestly assumed I'd be spending a bunch of money on alcohol," Nader says. "Everyone else knew a lot more about the neuroscience of memory. And they all told me it would never work."
" To LeDoux, the reason was obvious: Even if Nader blocked protein synthesis during recall, the original circuitry would still be intact, so the memory should be too. If Nader could induce amnesia, it would be temporary. Once the block was removed, the recall would return as strong as ever. And so LeDoux and Nader made a bet: If Nader failed to permanently erase a set of fear memories in four lab animals, he had to buy LeDoux a bottle of tequila. If it worked, drinks were on LeDoux. "I honestly assumed I'd be spending a bunch of money on alcohol," Nader says. "Everyone else knew a lot more about the neuroscience of memory. And they all told me it would never work."
Most Popular
He taught several dozen rats to associate a loud noise with a mild but painful electric shock. It terrified them—whenever the sound played, the rats froze in fear, anticipating the shock. After reinforcing this memory for several weeks, Nader hit the rats with the noise once again, but this time he then injected their brains with a chemical that inhibited protein synthesis. Then he played the sound again. "I couldn't believe what happened," Nader says. "The fear memory was gone. The rats had forgotten everything." The absence of fear persisted even after the injection wore off.
Then he played the sound again. "I couldn't believe what happened," Nader says. "The fear memory was gone. The rats had forgotten everything." The absence of fear persisted even after the injection wore off.
The secret was the timing: If new proteins couldn't be created during the act of remembering, then the original memory ceased to exist. The erasure was also exceedingly specific. The rats could still learn new associations, and they remained scared of other sounds associated with a shock but that hadn't been played during the protein block. They forgot only what they'd been forced to remember while under the influence of the protein inhibitor.
The disappearance of the fear memory suggested that every time we think about the past we are delicately transforming its cellular representation in the brain, changing its underlying neural circuitry. It was a stunning discovery: Memories are not formed and then pristinely maintained, as neuroscientists thought; they are formed and then rebuilt every time they're accessed. "The brain isn't interested in having a perfect set of memories about the past," LeDoux says. "Instead, memory comes with a natural updating mechanism, which is how we make sure that the information taking up valuable space inside our head is still useful. That might make our memories less accurate, but it probably also makes them more relevant to the future."
"The brain isn't interested in having a perfect set of memories about the past," LeDoux says. "Instead, memory comes with a natural updating mechanism, which is how we make sure that the information taking up valuable space inside our head is still useful. That might make our memories less accurate, but it probably also makes them more relevant to the future."
After collecting his tequila, Nader hit the library in an attempt to make sense of his bizarre observations. "I couldn't believe that no one had ever done this experiment before," he says. "I thought, there's no way I'm this lucky." Nader was right. He had unknowingly replicated a 44-year-old experiment performed by a Rutgers psychologist named Donald Lewis, in which rats had been trained to be afraid of a sound—associating it, again, with an electric shock—and then had those memories erased by a separate electroconvulsive shock. Lewis had discovered what came to be called memory reconsolidation, the brain's practice of re-creating memories over and over again.
But by the mid-1970s, neuroscientists had largely stopped investigating reconsolidation. Other researchers failed to replicate several of Lewis' original experiments, so the phenomenon was dismissed as an experimental error. "These guys had discovered it all way before me," Nader says. "But they had been left out of all the textbooks."
Nader was convinced that Lewis' work had been rejected unjustly. But no one wanted to hear it. "Man, it was brutal," Nader says. "I couldn't get published anywhere." He was shunned at conferences and accused in journal articles of "forgetting the lessons of the past." By 2001, just a few years after his experimental triumph, he was on the verge of leaving the field. He thought of Thomas Kuhn, the philosopher of science who famously observed that overturning paradigms is always a fearsome task. "Why put up with this shit?" Nader says. "I finally understood what Kuhn was talking about. I'd run straight into a very stubborn paradigm."
Most Popular
But Nader was so angry at his scientific opponents that he refused to let them win, and by 2005 other researchers had started to take his side. Multiple papers demonstrated that the act of recall required some kind of protein synthesis—that it was, at the molecular level, nearly identical to the initial creation of a long-term recollection.
Multiple papers demonstrated that the act of recall required some kind of protein synthesis—that it was, at the molecular level, nearly identical to the initial creation of a long-term recollection.
To be more specific: I can recall vividly the party for my eighth birthday. I can almost taste the Baskin-Robbins ice cream cake and summon the thrill of tearing wrapping paper off boxes of Legos. This memory is embedded deep in my brain as a circuit of connected cells that I will likely have forever. Yet the science of reconsolidation suggests that the memory is less stable and trustworthy than it appears. Whenever I remember the party, I re-create the memory and alter its map of neural connections. Some details are reinforced—my current hunger makes me focus on the ice cream—while others get erased, like the face of a friend whose name I can no longer conjure. The memory is less like a movie, a permanent emulsion of chemicals on celluloid, and more like a play—subtly different each time it's performed.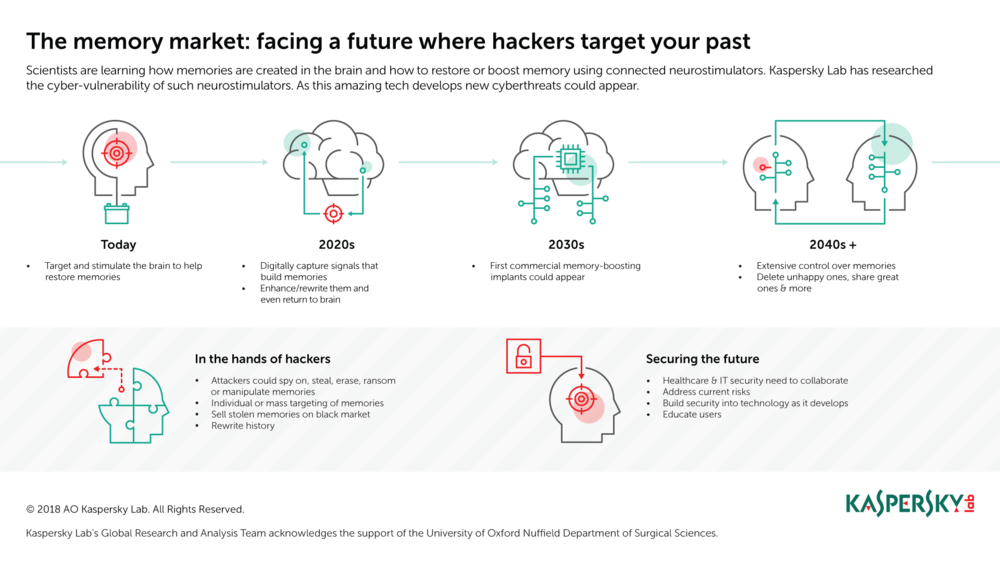 In my brain, a network of cells is constantly being reconsolidated, rewritten, remade. That two-letter prefix changes everything.
In my brain, a network of cells is constantly being reconsolidated, rewritten, remade. That two-letter prefix changes everything.
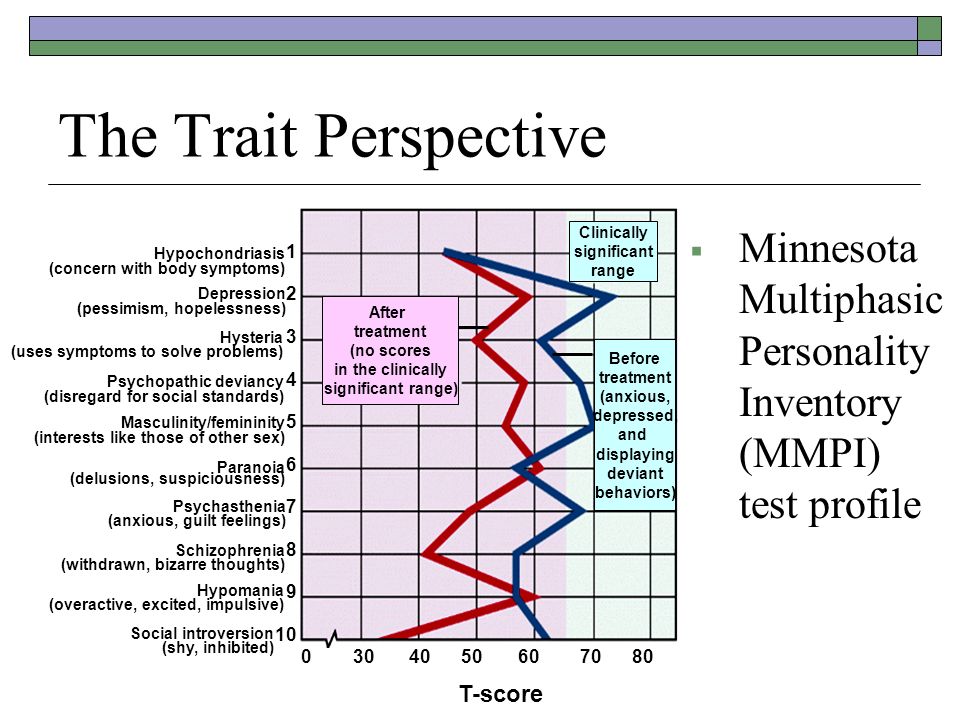
Memory Erasure: How It Works
For years scientists have been able to change the emotional tone of a memory by administering certain drugs just before asking people to recall the event in detail. New research suggests that they'll be able to target and erase specific memories altogether. Here's how.
1/ Pick a memory.
It has to be something deeply implanted in the brain, a long-term memory that has undergone a process called consolidation—a restructuring of neural connections.
2/ Recall requires neural connections by protein synthesis.
To remember something, your brain synthesizes new proteins to stabilize circuits of neural connections. To date, researchers have identified one such protein, called PKMzeta. Before trying to erase the targeted memory, researchers would ensure that it was ensconced by having the patient write down an account of the event or retell it aloud several times.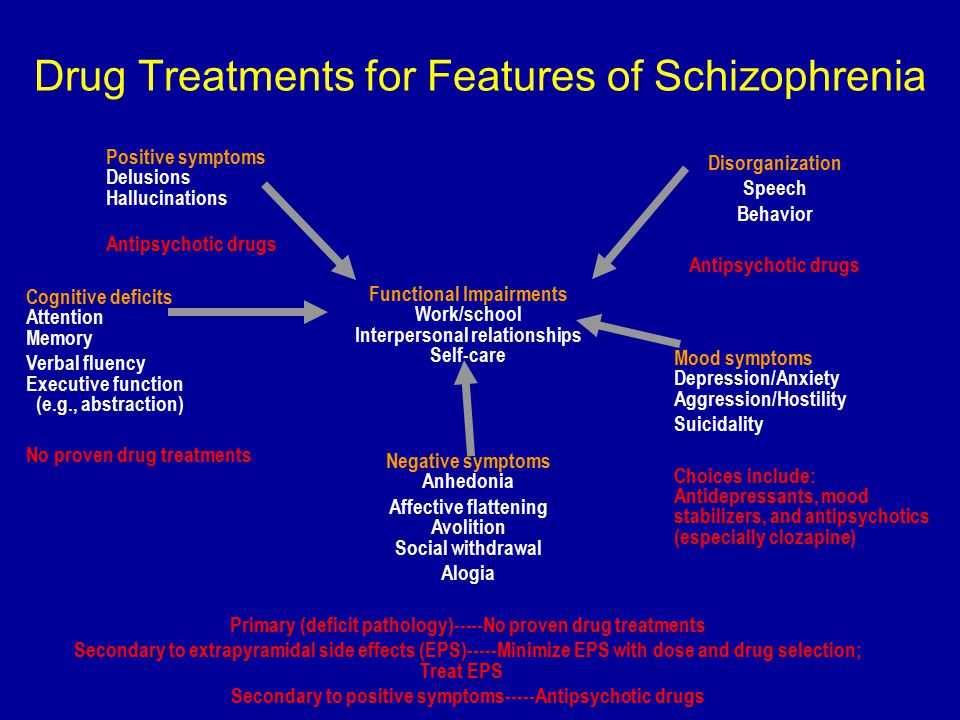
3/ Nuke the memory.
To delete the memory, researchers would administer a drug that blocks PKMzeta and then ask the patient to recall the event again. Because the protein required to reconsolidate the memory will be absent, the memory will cease to exist. Neuroscientists think they'll be able to target the specific memory by using drugs that bind selectively to receptors found only in the correct area of the brain.
4/ Everything else is fine.
If the drug is selective enough and the memory precise enough, everything else in the brain should be unaffected and remain as correct—or incorrect—as ever.
Illustration: Teagan White
Once you start questioning the reality of memory, things fall apart pretty quickly. So many of our assumptions about the human mind—what it is, why it breaks, and how it can be healed—are rooted in a mistaken belief about how experience is stored in the brain. (According to a recent survey, 63 percent of Americans believe that human memory "works like a video camera, accurately recording the events we see and hear so that we can review and inspect them later. ") We want the past to persist, because the past gives us permanence. It tells us who we are and where we belong. But what if your most cherished recollections are also the most ephemeral thing in your head?
") We want the past to persist, because the past gives us permanence. It tells us who we are and where we belong. But what if your most cherished recollections are also the most ephemeral thing in your head?
Most Popular
Consider the study of flashbulb memories, extremely vivid, detailed recollections. Shortly after the September 11 attacks, a team of psychologists led by William Hirst and Elizabeth Phelps surveyed several hundred subjects about their memories of that awful day. The scientists then repeated the surveys, tracking how the stories steadily decayed. At one year out, 37 percent of the details had changed. By 2004 that number was approaching 50 percent. Some changes were innocuous—the stories got tighter and the narratives more coherent—but other adjustments involved a wholesale retrofit. Some people even altered where they were when the towers fell. Over and over, the act of repeating the narrative seemed to corrupt its content.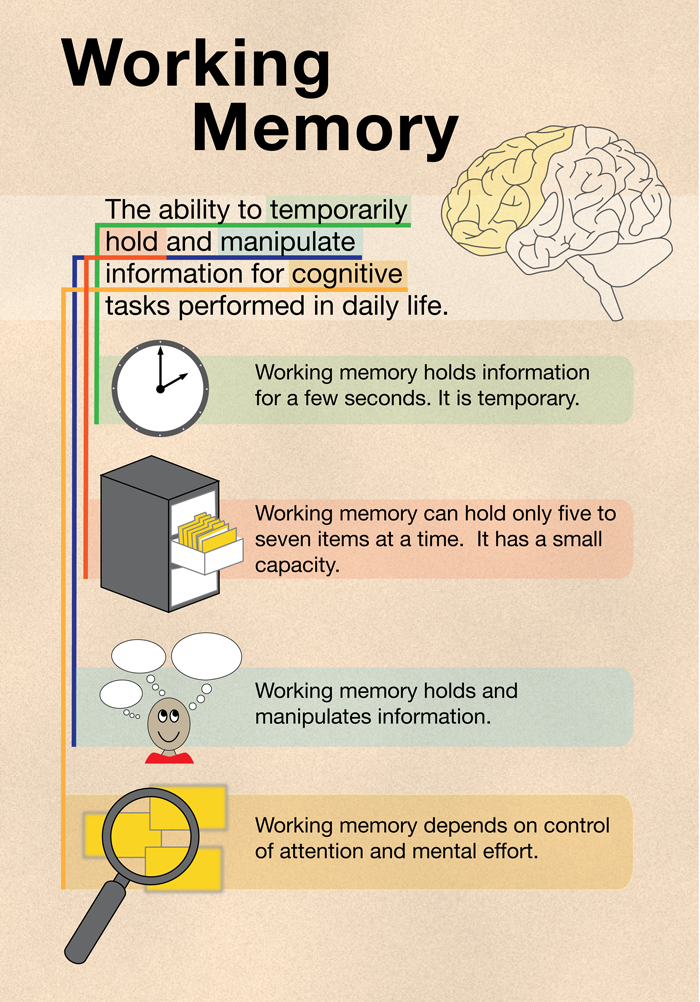 The scientists aren't sure about this mechanism, and they have yet to analyze the data from the entire 10-year survey. But Phelps expects it to reveal that many details will be make-believe. "What's most troubling, of course, is that these people have no idea their memories have changed this much," she says. "The strength of the emotion makes them convinced it's all true, even when it's clearly not."
The scientists aren't sure about this mechanism, and they have yet to analyze the data from the entire 10-year survey. But Phelps expects it to reveal that many details will be make-believe. "What's most troubling, of course, is that these people have no idea their memories have changed this much," she says. "The strength of the emotion makes them convinced it's all true, even when it's clearly not."
Reconsolidation provides a mechanistic explanation for these errors. It's why eyewitness testimony shouldn't be trusted (even though it's central to our justice system), why every memoir should be classified as fiction, and why it's so disturbingly easy to implant false recollections. (The psychologist Elizabeth Loftus has repeatedly demonstrated that nearly a third of subjects can be tricked into claiming a made-up memory as their own. It takes only a single exposure to a new fiction for it to be reconsolidated as fact.)
And this returns us to critical incident stress debriefing. When we experience a traumatic event, it gets remembered in two separate ways. The first memory is the event itself, that cinematic scene we can replay at will. The second memory, however, consists entirely of the emotion, the negative feelings triggered by what happened. Every memory is actually kept in many different parts of the brain. Memories of negative emotions, for instance, are stored in the amygdala, an almond-shaped area in the center of the brain. (Patients who have suffered damage to the amygdala are incapable of remembering fear.) By contrast, all the relevant details that comprise the scene are kept in various sensory areas—visual elements in the visual cortex, auditory elements in the auditory cortex, and so on. That filing system means that different aspects can be influenced independently by reconsolidation.
When we experience a traumatic event, it gets remembered in two separate ways. The first memory is the event itself, that cinematic scene we can replay at will. The second memory, however, consists entirely of the emotion, the negative feelings triggered by what happened. Every memory is actually kept in many different parts of the brain. Memories of negative emotions, for instance, are stored in the amygdala, an almond-shaped area in the center of the brain. (Patients who have suffered damage to the amygdala are incapable of remembering fear.) By contrast, all the relevant details that comprise the scene are kept in various sensory areas—visual elements in the visual cortex, auditory elements in the auditory cortex, and so on. That filing system means that different aspects can be influenced independently by reconsolidation.
The larger lesson is that because our memories are formed by the act of remembering them, controlling the conditions under which they are recalled can actually change their content. The problem with CISD is that the worst time to recall a traumatic event is when people are flush with terror and grief. They'll still have all the bodily symptoms of fear—racing pulse, clammy hands, tremors—so the intense emotional memory is reinforced. It's the opposite of catharsis. But when people wait a few weeks before discussing an event—as Mitchell, the inventor of CISD, did himself—they give their negative feelings a chance to fade. The volume of trauma is dialed down; the body returns to baseline. As a result, the emotion is no longer reconsolidated in such a stressed state. Subjects will still remember the terrible event, but the feelings of pain associated with it will be rewritten in light of what they feel now.
The problem with CISD is that the worst time to recall a traumatic event is when people are flush with terror and grief. They'll still have all the bodily symptoms of fear—racing pulse, clammy hands, tremors—so the intense emotional memory is reinforced. It's the opposite of catharsis. But when people wait a few weeks before discussing an event—as Mitchell, the inventor of CISD, did himself—they give their negative feelings a chance to fade. The volume of trauma is dialed down; the body returns to baseline. As a result, the emotion is no longer reconsolidated in such a stressed state. Subjects will still remember the terrible event, but the feelings of pain associated with it will be rewritten in light of what they feel now.
Most Popular
LeDoux insists that these same principles have been used by good therapists for decades. "When therapy heals, when it helps reduce the impact of negative memories, it's really because of reconsolidation," he says. "Therapy allows people to rewrite their own memories while in a safe space, guided by trained professionals. The difference is that we finally understand the neural mechanism."
"Therapy allows people to rewrite their own memories while in a safe space, guided by trained professionals. The difference is that we finally understand the neural mechanism."
But competent talk therapy is not the only way to get at those mechanisms. One intriguing approach to treating PTSD that emerged recently involves administering certain drugs and then asking patients to recall their bad memories. In one 2010 clinical trial, subjects suffering from PTSD were given MDMA (street name: ecstasy) while undergoing talk therapy. Because the drug triggers a rush of positive emotion, the patients recalled their trauma without feeling overwhelmed. As a result, the remembered event was associated with the positive feelings triggered by the pill. According to the researchers, 83 percent of their patients showed a dramatic decrease in symptoms within two months. That makes ecstasy one of the most effective PTSD treatments ever devised.
Other scientists have achieved impressive results with less extreme drugs.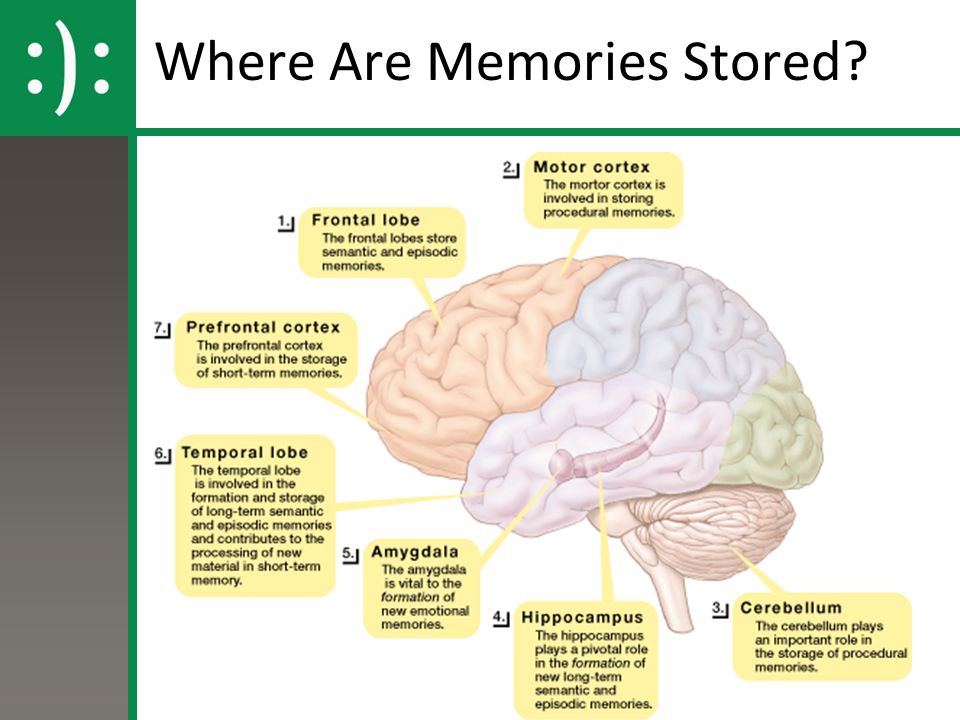 In 2008, Alain Brunet, a clinical psychologist at McGill University, identified 19 patients who had been suffering for several years from serious stress and anxiety disorders such as PTSD. (Their traumas included sexual assaults, car crashes, and violent muggings.) People in the treatment group were given the drug propranolol, a beta-blocker that has long been used for conditions like high blood pressure and performance anxiety; it inhibits norepinephrine, a neurotransmitter involved in the production of strong emotions. Brunet asked subjects to write a detailed description of their traumatic experiences and then gave them a dose of propranolol. While the subjects were remembering the awful event, the drug suppressed the visceral aspects of their fear response, ensuring that the negative feeling was somewhat contained.
In 2008, Alain Brunet, a clinical psychologist at McGill University, identified 19 patients who had been suffering for several years from serious stress and anxiety disorders such as PTSD. (Their traumas included sexual assaults, car crashes, and violent muggings.) People in the treatment group were given the drug propranolol, a beta-blocker that has long been used for conditions like high blood pressure and performance anxiety; it inhibits norepinephrine, a neurotransmitter involved in the production of strong emotions. Brunet asked subjects to write a detailed description of their traumatic experiences and then gave them a dose of propranolol. While the subjects were remembering the awful event, the drug suppressed the visceral aspects of their fear response, ensuring that the negative feeling was somewhat contained.
One week later, all the patients returned to the lab and were exposed once again to a description of the traumatic event. Here's where things got interesting: Subjects who got the placebo demonstrated levels of arousal consistent with PTSD (for example, their heart rate spiked suddenly), but those given propranolol showed significantly lower stress responses. Although they could still remember the event in vivid detail, the emotional memory located in the amygdala had been modified. The fear wasn't gone, but it no longer seemed crippling. "The results we get sometimes leave me in awe," Brunet says. "These are people who are unable to lead normal lives, and yet after just a few sessions they become healthy again."
Although they could still remember the event in vivid detail, the emotional memory located in the amygdala had been modified. The fear wasn't gone, but it no longer seemed crippling. "The results we get sometimes leave me in awe," Brunet says. "These are people who are unable to lead normal lives, and yet after just a few sessions they become healthy again."
Photo illustration: Curtis Mann; Photo: Ed Andrieski/AP
Most Popular
Recoveries are possible, but they aren't necessarily neat. One of Brunet's patients was Lois, a retired member of the Canadian military living in Kingston, Ontario. (She asked that I not use her last name.) When Lois describes the tragic arc of her life, she sounds like a cursed character in the Old Testament. Sexually molested as a child, she married an abusive man, who would later hang himself at home. Years after that, her teenage daughter was hit by a truck and died. "I'd been holding it together my entire life," she says.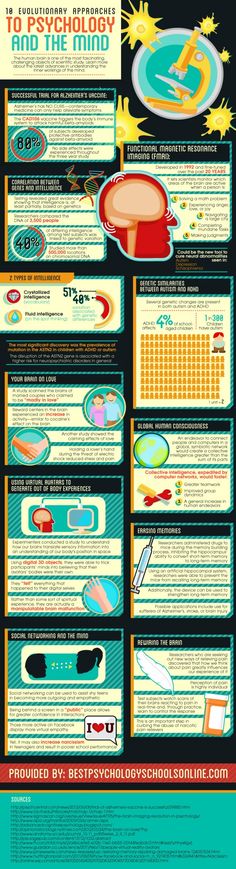 "But when I heard my child was gone I just started sobbing and couldn't stop. I felt this pain that I thought was going to kill me."
"But when I heard my child was gone I just started sobbing and couldn't stop. I felt this pain that I thought was going to kill me."
Lois coped by drinking. She would start around noon and keep going until she went to bed. "I lost four years to alcohol," she says. "But if I wasn't drunk then I was crying. I knew I was killing myself, but I didn't know what else to do."
“Psychiatry never cures anything—all we do is treat the worst symptoms. But this new treatment could be the first psychiatric cure ever.”
In early 2011, Lois learned about the experimental trials being conducted by Brunet. She immediately wrote him an email, begging for help. "I'd spent a lot of my life in standard talk therapy," she says. "It just didn't do it for me. But this seemed like it might actually work." Last spring Lois began reconsolidation treatment at Brunet's hospital, driving to Montreal once a week. The routine was always the same: A nurse would give her propranolol, wait for the drug to take effect, and then have her read her life story out loud. The first few weeks were excruciating. "I was a mess for days afterward," she says. "I couldn't believe I'd signed up for this." But then, after five weeks of therapy, Lois felt herself slowly improve. She would still cry when describing the death of her daughter—Lois cried during our interview—but now she could stop crying. "That was the difference," she says. "I still remembered everything that happened, and it still hurt so much, but now I felt like I could live with it. The feelings were just less intense. The therapy let me breathe."
The first few weeks were excruciating. "I was a mess for days afterward," she says. "I couldn't believe I'd signed up for this." But then, after five weeks of therapy, Lois felt herself slowly improve. She would still cry when describing the death of her daughter—Lois cried during our interview—but now she could stop crying. "That was the difference," she says. "I still remembered everything that happened, and it still hurt so much, but now I felt like I could live with it. The feelings were just less intense. The therapy let me breathe."
Such improvements, small though they may seem, are almost unheard of in psychiatry. "We never cure anything," Brunet says. "All we do is try to treat the worst symptoms. But I think this treatment has the potential to be the first psychiatric cure ever. For many people, the PTSD really is gone."
Propranolol, of course, is an imperfect drug, a vintage tool commandeered for a new purpose. Despite Brunet's optimistic assessment, many of his patients remain traumatized, albeit perhaps less so. While he is currently conducting a larger-scale, randomized PTSD trial with the beta-blocker, future therapies will rely on more targeted compounds. "These norepinephrine inhibitors are just what's available right now," LeDoux says. "They work OK, but their effect is indirect." What reconsolidation therapy really needs is a drug that can target the fear memory itself. "The perfect drug wouldn't just tamp down the traumatic feeling," he says. "It would erase the actual representation of the trauma in the brain."
While he is currently conducting a larger-scale, randomized PTSD trial with the beta-blocker, future therapies will rely on more targeted compounds. "These norepinephrine inhibitors are just what's available right now," LeDoux says. "They work OK, but their effect is indirect." What reconsolidation therapy really needs is a drug that can target the fear memory itself. "The perfect drug wouldn't just tamp down the traumatic feeling," he says. "It would erase the actual representation of the trauma in the brain."
Most Popular
Here's the amazing part: The perfect drug may have already been found.
The chemistry of the brain is in constant flux, with the typical neural protein lasting anywhere from two weeks to a few months before it breaks down or gets reabsorbed. How then do some of our memories seem to last forever? It's as if they are sturdier than the mind itself. Scientists have narrowed down the list of molecules that seem essential to the creation of long-term memory—sea slugs and mice without these compounds are total amnesiacs—but until recently nobody knew how they worked.
In the 1980s, a Columbia University neurologist named Todd Sacktor became obsessed with this mental mystery. His breakthrough came from an unlikely source. "My dad was a biochemist," Sacktor says. "He was the one who said I should look into this molecule, because it seems to have some neat properties." Sacktor's father had suggested a molecule called protein kinase C, an enzyme turned on by surges of calcium ions in the brain. "This enzyme seemed to have a bunch of properties necessary to be a regulator of long-term potentiation," Sacktor says. "But so did a bunch of other molecules. It took me a few years to figure out if my dad was right."
In fact, it took Sacktor more than a decade. (He spent three years just trying to purify the molecule.) What he discovered is that a form of protein kinase C called PKMzeta hangs around synapses, the junctions where neurons connect, for an unusually long time. And without it, stable recollections start to disappear. While scientists like Nader had erased memories using chemicals that inhibited all protein synthesis, Sacktor was the first to target a single memory protein so specifically. The trick was finding a chemical that inhibited PKMzeta activity. "It turned out to be remarkably easy," Sacktor says. "All we had to do was order this inhibitor compound from the chemical catalog and then give it to the animals. You could watch them forget."
The trick was finding a chemical that inhibited PKMzeta activity. "It turned out to be remarkably easy," Sacktor says. "All we had to do was order this inhibitor compound from the chemical catalog and then give it to the animals. You could watch them forget."
What does PKMzeta do? The molecule's crucial trick is that it increases the density of a particular type of sensor called an AMPA receptor on the outside of a neuron. It's an ion channel, a gateway to the interior of a cell that, when opened, makes it easier for adjacent cells to excite one another. (While neurons are normally shy strangers, struggling to interact, PKMzeta turns them into intimate friends, happy to exchange all sorts of incidental information.) This process requires constant upkeep—every long-term memory is always on the verge of vanishing. As a result, even a brief interruption of PKMzeta activity can dismantle the function of a steadfast circuit.
If the genetic expression of PKMzeta is amped up—by, say, genetically engineering rats to overproduce the stuff—they become mnemonic freaks, able to convert even the most mundane events into long-term memory. (Their performance on a standard test of recall is nearly double that of normal animals.) Furthermore, once neurons begin producing PKMzeta, the protein tends to linger, marking the neural connection as a memory. "The molecules themselves are always changing, but the high level of PKMzeta stays constant," Sacktor says. "That's what makes the endurance of the memory possible."
(Their performance on a standard test of recall is nearly double that of normal animals.) Furthermore, once neurons begin producing PKMzeta, the protein tends to linger, marking the neural connection as a memory. "The molecules themselves are always changing, but the high level of PKMzeta stays constant," Sacktor says. "That's what makes the endurance of the memory possible."
Most Popular
For example, in a recent experiment, Sacktor and scientists at the Weizmann Institute of Science trained rats to associate the taste of saccharin with nausea (thanks to an injection of lithium). After just a few trials, the rats began studiously avoiding the artificial sweetener. All it took was a single injection of a PKMzeta inhibitor called zeta-interacting protein, or ZIP, before the rats forgot all about their aversion. The rats went back to guzzling down the stuff.
Photo illustration: Curtis Mann; Photo: Doug Kanter/Getty
By coupling these amnesia cocktails to the memory reconsolidation process, it's possible to get even more specific. Nader, LeDoux, and a neuroscientist named Jacek Debiec taught rats elaborate sequences of association, so that a series of sounds predicted the arrival of a painful shock to the foot. Nader calls this a "chain of memories"—the sounds lead to fear, and the animals freeze up. "We wanted to know if making you remember that painful event would also lead to the disruption of related memories," Nader says. "Or could we alter just that one association?" The answer was clear. By injecting a protein synthesis inhibitor before the rats were exposed to only one of the sounds—and therefore before they underwent memory reconsolidation—the rats could be "trained" to forget the fear associated with that particular tone. "Only the first link was gone," Nader says. The other associations remained perfectly intact. This is a profound result. While scientists have long wondered how to target specific memories in the brain, it turns out to be remarkably easy: All you have to do is ask people to remember them.
Nader, LeDoux, and a neuroscientist named Jacek Debiec taught rats elaborate sequences of association, so that a series of sounds predicted the arrival of a painful shock to the foot. Nader calls this a "chain of memories"—the sounds lead to fear, and the animals freeze up. "We wanted to know if making you remember that painful event would also lead to the disruption of related memories," Nader says. "Or could we alter just that one association?" The answer was clear. By injecting a protein synthesis inhibitor before the rats were exposed to only one of the sounds—and therefore before they underwent memory reconsolidation—the rats could be "trained" to forget the fear associated with that particular tone. "Only the first link was gone," Nader says. The other associations remained perfectly intact. This is a profound result. While scientists have long wondered how to target specific memories in the brain, it turns out to be remarkably easy: All you have to do is ask people to remember them.
This isn't Eternal Sunshine of the Spotless Mind-style mindwiping. In some ways it's potentially even more effective and more precise. Because of the compartmentalization of memory in the brain—the storage of different aspects of a memory in different areas—the careful application of PKMzeta synthesis inhibitors and other chemicals that interfere with reconsolidation should allow scientists to selectively delete aspects of a memory. Right now, researchers have to inject their obliviating potions directly into the rodent brain. Future treatments, however, will involve targeted inhibitors, like an advanced version of ZIP, that become active only in particular parts of the cortex and only at the precise time a memory is being recalled. The end result will be a menu of pills capable of erasing different kinds of memories—the scent of a former lover or the awful heartbreak of a failed relationship. These thoughts and feelings can be made to vanish, even as the rest of the memory remains perfectly intact. "Reconsolidation research has shown that we can get very specific about which associations we go after," LeDoux says. "And that's a very good thing. Nobody actually wants a totally spotless mind."
"Reconsolidation research has shown that we can get very specific about which associations we go after," LeDoux says. "And that's a very good thing. Nobody actually wants a totally spotless mind."
Most Popular
The astonishing power of PKMzeta forces us to redefine human memory. While we typically think of memories as those facts and events from the past that stick in the brain, Sacktor's research suggests that memory is actually much bigger and stranger than that. In fact, PTSD isn't the only disease that's driven by a broken set of memories—other nasty afflictions, including chronic pain, obsessive-compulsive disorder, and drug addiction, are also fueled by memories that can't be forgotten.
Sacktor is convinced that the first therapeutic use of PKMzeta inhibitors will involve making people forget not an event but physical pain. For reasons that remain mysterious, some sensory nerves never recover from bodily injury; even after a wound heals, the hurt persists.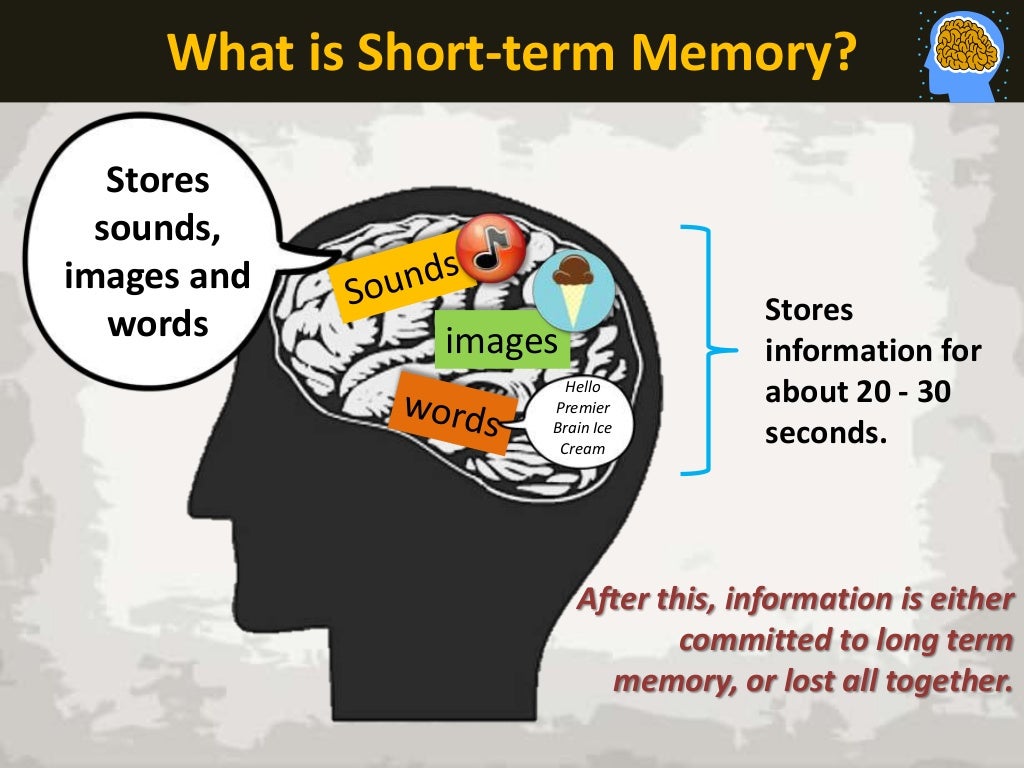 The body remembers. Because these memories are made of the exact same stuff as every other kind of memory, injecting an inhibitor near the spinal cord—where, presumably, the sensation of pain is being stored—and then somehow inducing or focusing on the pain could instantly erase the long-term suffering, as if the nerves themselves were reset. "It's hard to argue against this form of memory alteration," Sacktor says. "It might be the only way to treat neuropathic pain." PTSD is the emotional version of this problem. Instead of the pain coming from the spinal cord, it comes from the amygdala, where a trauma is encoded and just won't let go. For many reconsolidation researchers, there is little difference among categories of hurt. It doesn't matter if the tragedy is physical or psychic: The treatment is the same.
The body remembers. Because these memories are made of the exact same stuff as every other kind of memory, injecting an inhibitor near the spinal cord—where, presumably, the sensation of pain is being stored—and then somehow inducing or focusing on the pain could instantly erase the long-term suffering, as if the nerves themselves were reset. "It's hard to argue against this form of memory alteration," Sacktor says. "It might be the only way to treat neuropathic pain." PTSD is the emotional version of this problem. Instead of the pain coming from the spinal cord, it comes from the amygdala, where a trauma is encoded and just won't let go. For many reconsolidation researchers, there is little difference among categories of hurt. It doesn't matter if the tragedy is physical or psychic: The treatment is the same.
There is perhaps no societal plague more expensive than drug addiction. In the US, the overall cost of substance abuse exceeds $600 billion a year. Previous attempts to treat drug addiction with drugs have largely failed; methadone is among the best, and it's not that good. But addiction is driven by memory—associating the high with a crack pipe, or the buzz of nicotine with the smell of smoke—which means that reconsolidation therapy offers some hope. Studies of morphine-addled rats have found that a few doses of a PKMzeta inhibitor can eliminate their cravings. Nader, meanwhile, has just begun a trial in which cocaine addicts are given propranolol and then shown a drug-related cue, such as a video of people shooting up. Because the blood-pressure medicine dials down their basic emotional response to the world—it reduces symptoms of stress but also inhibits expressions of pleasure—Nader believes it can slowly diminish the desire for illicit substances. "The craving is a learned association," he says. "We're hoping to weaken that association over time."
But addiction is driven by memory—associating the high with a crack pipe, or the buzz of nicotine with the smell of smoke—which means that reconsolidation therapy offers some hope. Studies of morphine-addled rats have found that a few doses of a PKMzeta inhibitor can eliminate their cravings. Nader, meanwhile, has just begun a trial in which cocaine addicts are given propranolol and then shown a drug-related cue, such as a video of people shooting up. Because the blood-pressure medicine dials down their basic emotional response to the world—it reduces symptoms of stress but also inhibits expressions of pleasure—Nader believes it can slowly diminish the desire for illicit substances. "The craving is a learned association," he says. "We're hoping to weaken that association over time."
Being able to control memory doesn't simply give us admin access to our brains. It gives us the power to shape nearly every aspect of our lives. There's something terrifying about this. Long ago, humans accepted the uncontrollable nature of memory; we can't choose what to remember or forget. But now it appears that we'll soon gain the ability to alter our sense of the past.
But now it appears that we'll soon gain the ability to alter our sense of the past.
The problem with eliminating pain, of course, is that pain is often educational. We learn from our regrets and mistakes; wisdom is not free. If our past becomes a playlist—a collection of tracks we can edit with ease—then how will we resist the temptation to erase the unpleasant ones? Even more troubling, it's easy to imagine a world where people don't get to decide the fate of their own memories. "My worst nightmare is that some evil dictator gets ahold of this," Sacktor says. "There are all sorts of dystopian things one could do with these drugs." While tyrants have often rewritten history books, modern science might one day allow them to rewrite us, wiping away genocides and atrocities with a cocktail of pills.
Most Popular
Those scenarios aside, the fact is we already tweak our memories—we just do it badly. Reconsolidation constantly alters our recollections, as we rehearse nostalgias and suppress pain. We repeat stories until they're stale, rewrite history in favor of the winners, and tamp down our sorrows with whiskey. "Once people realize how memory actually works, a lot of these beliefs that memory shouldn't be changed will seem a little ridiculous," Nader says. "Anything can change memory. This technology isn't new. It's just a better version of an existing biological process."
We repeat stories until they're stale, rewrite history in favor of the winners, and tamp down our sorrows with whiskey. "Once people realize how memory actually works, a lot of these beliefs that memory shouldn't be changed will seem a little ridiculous," Nader says. "Anything can change memory. This technology isn't new. It's just a better version of an existing biological process."
It's a pretty notion—hey, this memory-alteration stuff is totally natural, man—but some ethicists and clinicians dispute whether this kind of therapy is acceptable. Researchers in the field counter that not treating suffering is cruel, regardless of the type of pain involved. We have a duty, they say, to take psychological pain seriously. We can no longer ignore people like Lois. "If you're in a car accident and you break your leg, everyone agrees we need to give you treatment and painkillers," Nader says. "But if something terrible happens and your mind breaks, people conclude that treatment is a dangerous idea, at least if it's effective. But what's the difference?" Just think of all the poor souls in therapy, trying to talk themselves into a better place. These scientists point out that memory tweaks will one day be used in the same way—except that unlike CISD or Jungian analysis or selective serotonin reuptake inhibitors, these therapies could put permanent recovery just one pill away.
But what's the difference?" Just think of all the poor souls in therapy, trying to talk themselves into a better place. These scientists point out that memory tweaks will one day be used in the same way—except that unlike CISD or Jungian analysis or selective serotonin reuptake inhibitors, these therapies could put permanent recovery just one pill away.
At the moment, of course, such treatments remain entirely hypothetical, an avant-garde limited to the lab. PKMzeta inhibitors can zap rodent memories, but we can't ask the rats how they feel afterward. Maybe they feel terrible. Maybe they miss their fear. Maybe they miss their morphine. Or maybe all they know is that they miss something. They just can't remember what.
Contributing editor Jonah Lehrer ([email protected]) is the author of the new book Imagine: How Creativity Works, out in March.
Topics20.03featuresmedicinememoryNeuroscience
More from WIREDDrugs that reduce memory. Five groups of drugs that affect memory
Memory loss is most commonly reported as a sign of aging, a consequence of substance use, or a symptom of diseases such as Alzheimer's disease.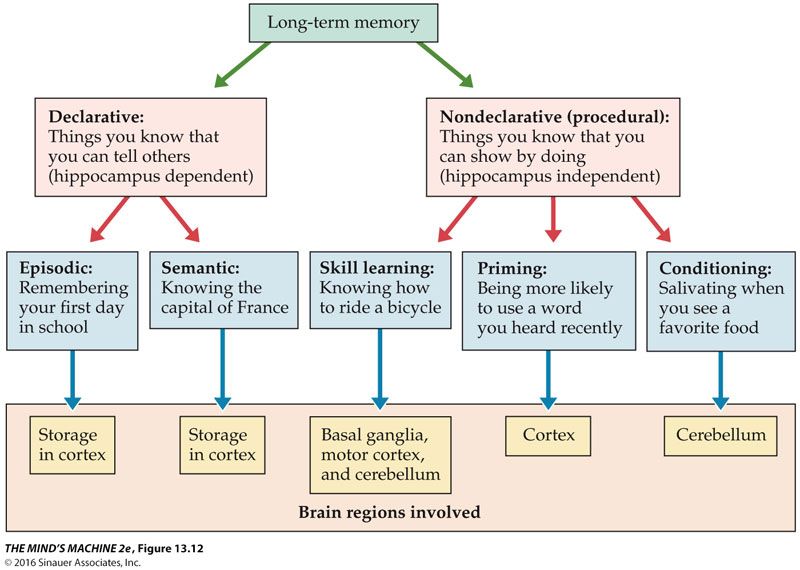 Many people do not know that episodes of forgetfulness can occur as a side effect of certain medications.
Many people do not know that episodes of forgetfulness can occur as a side effect of certain medications.
“Scientists now know that memory decline with aging is not at all inevitable,” writes Dr. Armon B. Neel, geriatric pharmacist, “In fact, the brain is capable of growing new nerve cells and rewiring connections between neurons throughout life. nine0003
In order to educate patients about the unknown side effects of certain medications, Dr. Neil has compiled a list of medications that can cause forgetfulness.
Is memory loss interfering with your life? The "culprit" may be one of these drugs.
Anti-anxiety drugs (benzodiazepines)
Representatives of : alprazolam (Xanax), chlordiazepoxide (Librium), clonazepam (Klonopin), diazepam (Valium), flurazepam (Dalmane), lorazepam (Ativan). nine0003
These medicines are usually prescribed for anxiety, agitation, muscle spasms, delirium. They suppress the activity of certain areas of the brain, due to which they can disrupt the transfer of data from short-term to long-term memory. This is why benzodiazepines are so commonly used by anesthesiologists.
This is why benzodiazepines are so commonly used by anesthesiologists.
To avoid these side effects, pharmacists recommend taking benzodiazepines in short courses. If you suffer from complications associated with increased anxiety, such as insomnia, then it is better to opt for alternative treatments. nine0003
Cholesterol-lowering drugs (statins)
Representatives of : atorvastatin (Lipitor), fluvastatin (Lescol), lovastatin (Mevacor), pravastatin (Pravachol), rosuvastatin (Crestor), and simvastatin (Zocor).
Statins lower blood cholesterol, but can also lower cholesterol levels in the brain where it is needed. If this happens, the connections between nerve cells are disrupted.
If you are on a statin for a slight increase in blood cholesterol levels, but you do not have a diagnosis of coronary disease, a vitamin shake is a better choice. nine0003
“Talk to your doctor about this. You may be given a combination of sublingual (under the tongue) vitamin B12 (1,000 micrograms per day), folic acid (800 micrograms per day), and vitamin B6 (200 mg per day),” recommends Dr. Neil.
Neil.
Antidepressants (tricyclic antidepressants)
Representatives of : amitriptyline (Elavil), clomipramine (Anafranil), desipramine (Norpramin), doxepin (Sinequan), imipramine (Tofranil).
These drugs are prescribed for patients suffering from depression, as well as eating disorders, chronic pain, and obsessive-compulsive disorders. More than a third of adults taking these drugs complain of memory impairment and about half of problems with concentration. nine0003
To avoid these side effects, it is worth talking to your doctor about the possibility of using non-drug treatments. Venlafaxine (Effexor) is also a good alternative because it has minimal negative effects on memory.
Hypertension medicines (beta-blockers)
Representatives of : atenolol (Tenormin), carvedilol (Coreg), metoprolol (Lopressor, Toprol), propranolol (anaprilin), sotalol (Betapace), timolol (Timoptic) . nine0003
Beta-blockers are used to slow the heart rate and lower blood pressure. At the same time, they can block the effects of important substances such as adrenaline and norepinephrine, leading to memory problems.
At the same time, they can block the effects of important substances such as adrenaline and norepinephrine, leading to memory problems.
Calcium channel blockers, which are derivatives of benzothiazepine, are safer in this respect. In addition, they are often more efficient.
Hypnotics (non-benzodiazepine hypnotics and sedatives)
Representatives : eszopiclone (Lunesta), zaleplon (Sonata), and zolpidem (Ambien).
These drugs help you sleep. But just like the aforementioned sedatives, they can interfere with the link between short-term and long-term memory.
“There are alternative drugs and non-drug treatments for insomnia. Talk to your doctor about them. For example, melatonin at night at a dose of 3 to 10 mg helps restore healthy sleep. However, be aware that abrupt withdrawal of sleeping pills can lead to side effects, so any changes in the course of treatment should be carried out by the attending physician, ”says Dr. Neil. nine0003
nine0003
Always consult your doctor before making any changes to your medication.
Forget everything: scientists have found a way to get rid of negative memories | Articles
The NRC "Kurchatov Institute" is engaged in research that should help get rid of painful memories. They can be erased with the help of special pharmacological preparations, the most effective of which turned out to be protein synthesis inhibitors. This is evidenced by the results of experiments conducted on mice. In the future, the development of Russian scientists can help people suffering from post-traumatic syndrome. nine0003
“Afghan Syndrome”
Post-traumatic stress disorder (PTSD), also known as “Vietnamese” or “Afghan” syndrome, is a severe mental condition that occurs as a result of a single or repeated traumatic situation, such as participation in combat actions, severe physical injury, sexual assault, or life threatening. In PTSD, a group of characteristic symptoms — such as high levels of anxiety, nightmares, and depression — persist for at least a month after the event.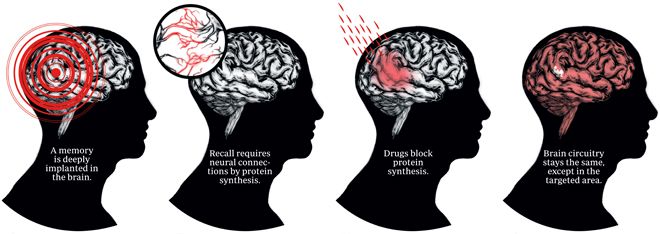 And in some cases, the trauma experienced makes itself felt throughout life. nine0003
And in some cases, the trauma experienced makes itself felt throughout life. nine0003
Currently, PTSD is treated in two ways: medication (antidepressants, tranquilizers and other drugs) and psychotherapy. Often, treatment is ineffective, and a person may need constant supervision by a specialist, which takes time and large financial costs.
Employees of the laboratory of neurosciences of the Kurchatov complex of NBICS-nature-like technologies found out how to get rid of negative memories. Researchers conducted a series of experiments on mice to either completely erase or change memories of a traumatic situation. To influence memory, protein synthesis inhibitors were used - they inhibit the synthesis of proteins in brain cells. In particular, cycloheximide has shown its effectiveness in mice. nine0003
Electric cell
— People with this syndrome always remember the traumatic experience. Such a memory becomes obsessive - in his thoughts a person constantly reproduces negative events that caused him suffering in the past, - Olga Ivashkina, a junior researcher at the laboratory of neuroscience at the Kurchatov Institute, explained to Izvestia. - A standard example: a person who participated in hostilities hears, for example, the roar of a car engine. This loud and sudden sound evokes in him the memory of the shooting. As a result, all negative memories are activated, panic and intense fear arise, the person is in a depressed mental state. These traumatic memories must be removed. To find ways to get rid of them, we modeled such an injury in mice. nine0003
- A standard example: a person who participated in hostilities hears, for example, the roar of a car engine. This loud and sudden sound evokes in him the memory of the shooting. As a result, all negative memories are activated, panic and intense fear arise, the person is in a depressed mental state. These traumatic memories must be removed. To find ways to get rid of them, we modeled such an injury in mice. nine0003
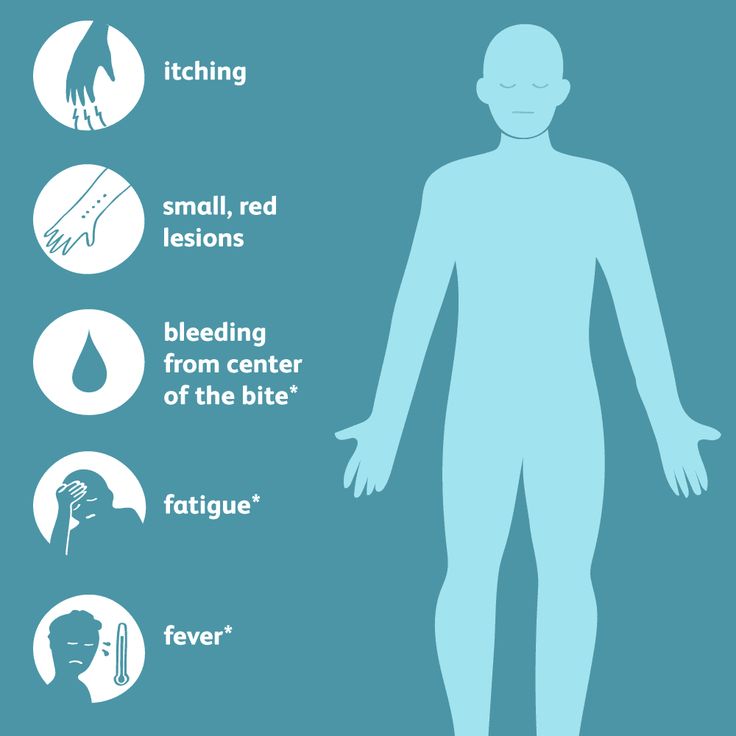
Rodents were placed in a new environment for them (experimental cage, through which a current was applied) - such an effect frightened the animals. As a result, when the mice were placed in a similar environment again, the past traumatic experience made them feel fear, as before. Researchers conducted a series of experiments to either completely erase or change memories of a traumatic situation. So far, protein synthesis inhibitors have been shown to be highly effective against traumatic memories. nine0003
- Such drugs disrupt all protein synthesis in the brain, which allows you to affect the memory, which is in a labile state, that is, available for change. In other words, the mice learned something, then we asked them to remember this situation,” Olga Ivashkina said. When they remember, the memory becomes active. If at this moment we introduce an inhibitor of protein synthesis, we can break it.
In other words, the mice learned something, then we asked them to remember this situation,” Olga Ivashkina said. When they remember, the memory becomes active. If at this moment we introduce an inhibitor of protein synthesis, we can break it.
The mechanism of memory erasure is associated with a disruption in the formation of new proteins necessary to enhance synaptic contacts between neurons in various areas of the brain, Ksenia Toropova, a junior researcher at the neuroscience laboratory at the Kurchatov Institute, noted in an interview with Izvestia. nine0003
- Both in the process of learning and under stress, the active expression of a number of genes begins in the brain, as a result, the proteins necessary for the formation of neural networks associated with memory are synthesized. With the introduction of protein synthesis inhibitors, these processes are disrupted and the memory of a new event cannot form, she explained.
From theory to practice
As Izvestia was told at the Kurchatov Institute, research with protein synthesis inhibitors will be continued in the near future.