Does pristiq affect libido
Sexual Side Effects of Depression Treatments and How to Cope
A lower libido or sex drive is one possible symptom of depression. In addition, the medications you take to treat depression may cause further issues with sexual function.
While antidepressants may cause sexual side effects, certain types of medications may notincrease your risk as much as others. Having your doctor adjust your dosages can also help.
For some people, sexual side effects from antidepressants may decrease over time. For others, these side effects may persist.
If you suspect your depression treatments are causing sexual side effects, here’s what you can do about it.
If you recently started an antidepressant and are experiencing symptoms of sexual dysfunction, you’re not alone. Loss of libido is a common problem for adults.
According to one study, researchers found that depression is associated with a 50 to 70 percent higher risk of decreased sexual desire. In addition, sexual dysfunction can increase the risk of developing depression by as much as 130 to 200 percent.
The following medications are commonly used to treat depression:
- selective serotonin reuptake inhibitors (SSRIs)
- serotonin and norepinephrine reuptake inhibitors (SNRIs)
- tricyclic medications, which are typically only used if SSRIs and SNRIs don’t help
- monoamine oxidase inhibitors (MAOIs), which are prescribed for when other antidepressants haven’t worked
In theory, if depression is causing you to have a lower sex drive, then seeking treatment could help. But some of the treatments for depression can cause sexual dysfunction.
Getting too much serotonin in the brain — a major function in treating depression — can inadvertently inhibit your sex drive.
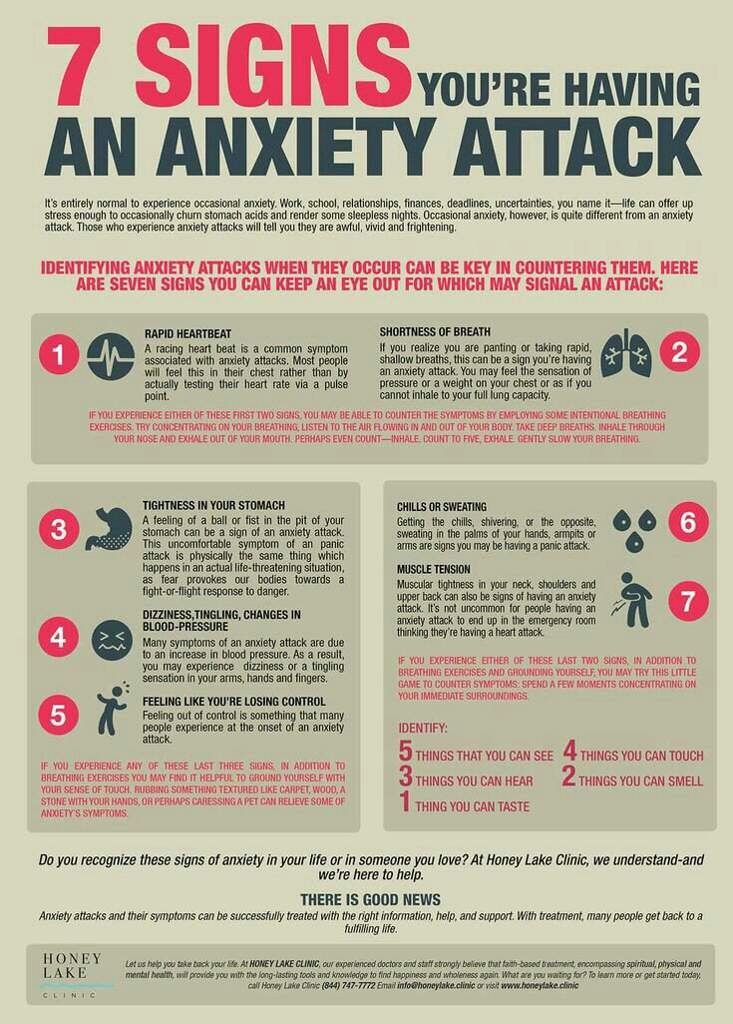
More specifically, antidepressants can cause the following side effects:
- a loss of libido, or overall desire to have sex
- decreased arousal
- erectile dysfunction in males
- vaginal dryness in females
- problems with orgasm
The exact side effects can vary between individuals, and you may not experience all possible symptoms.
The following antidepressants for major depressive disorder are known to be the least likely to cause sexual side effects:
- bupropion (Wellbutrin SR and XL), a type of antidepressant used to treat seasonal affective disorder (SAD), as well as help with smoking cessation
- mirtazapine (Remeron and Remeron SolTab)
- selegiline (Emsam), an MAOI that comes in the form of a skin patch
- vilazodone (Viibryd)
- vortioxetine (Trintellix)
On the flipside, some of the most common SSRIs are linked to sexual side effects, including:
- citalopram (Celexa)
- escitalopram (Lexapro)
- fluoxetine (Prozac)
- paroxetine (Paxil)
- paroxetine mesylate (Pexeva)
- sertraline (Zoloft)
SNRIs may also carry higher risks of sexual dysfunction, such as:
- desvenlafaxine (Pristiq)
- duloxetine (Cymbalta)
- venlafaxine (Effexor XR)
Certain MAOIs and tricyclic medications can also cause sexual side effects. This includes the following:
This includes the following:
- amitriptyline (Elavil)
- clomipramine (Anafranil)
- isocarboxazid (Marplan)
- phenelzine (Nardil)
- nortriptyline (Pamelor)
- tranylcypromine (Parnate)
One way to determine whether your antidepressant is linked to sexual side effects is to consider how you felt before taking your medication. If you had no issues with libido at that time, chances are your medication is to blame, not your depression.
Experiencing sexual side effects from antidepressants doesn’t mean you’re stuck with these symptoms for good.
In some cases, the solution may be to wait it out as your body gets used to your medication. After a while, you may experience fewer sexual side effects.
Depending on your individual experience, your symptoms may not ease with time alone. If sexual dysfunction continues to persist for several weeks, your doctor may recommend:
- adjusting your dose (never cut down on your medication without talking to your doctor first)
- switching medications
- choosing an antidepressant with the least risk for side effects
Your doctor may also recommend incorporating an additional antidepressant to your treatment plan to help counteract the side effects of your original medication.
For example, taking bupropion in addition to an SSRI has been shown to reverse sexual side effects of SSRIs in some people.
People who experience sexual side effects from their depression treatment may consider taking medications to improve function. These include sildenafil (Viagra) and tadalafil (Cialis).
There’s ongoing but limited research about the use of sildenafil to alleviate sexual side effects, but the Food and Drug Administration (FDA) hasn’t approved such usage. Adding bupropion may be more beneficial in these cases.
If you’re taking antidepressants and are experiencing sexual dysfunction, talk to your doctor about your options.
However, never reduce your dosage or stop taking your medication altogether. This may increase your risk for depression symptoms to return. Always talk to your doctor first.
You also shouldn’t allow the fear of sexual side effects stop you from seeking depression treatment. Not everyone who takes antidepressants experiences the same side effects. Your doctor can work with you to figure out the right type of medication and dosage.
Your doctor can work with you to figure out the right type of medication and dosage.
Sexual side effects are common when you first start taking medications for depression. Certain antidepressants carry more of these risks than others.
For some people, the side effects are temporary. You may also be able to manage these symptoms by switching medications or adjusting your treatment in other ways.
Talk to your doctor about any concerns you have with your depression treatment. Sexual side effects may take time to manage, so it’s important to work with your doctor rather than stopping your medication altogether.
Sex While on Antidepressants: What You Should Know
by Anne Windermere Patient Advocate
Medical Reviewer
Jerry Kennard, Ph.D.
iStock
Medical Reviewer
Jerry Kennard, Ph. D.
D.
If you have ever experienced mild, moderate or severe depression you know that it affects your entire body. Your thoughts and movements feel heavy and sluggish. Even in milder cases of depression it’s an effort to move, to concentrate or to feel enthusiasm for anything.
When it comes to sex, though, the picture isn’t that straightforward.
Depression and sex
Undertake a quick internet search and you’d be forgiven for thinking that depression kills sex lives. In fact, some people find that sex is the one thing that provides comfort and solace. Some men even report an increase in sex drive, partly driven by the same needs. So the fact that you can maintain a sex life does not mean you don’t have depression.
In most cases, however, the symptoms of depression, which include fatigue, aches and pains, and a lack of energy, mean that interest in sex diminishes or disappears entirely. Unfortunately, the most commonly prescribed antidepressants tend to be the worst offenders when it comes to low sex drive in both men and women.
Antidepressants that cause sexual side effects
The Mayo Clinic identifies the following antidepressants as the most likely to cause sexual side effects:
Citalopram (Celexa)
Desvenlafaxine (Pristiq, Khedezla)
Duloxetine (Cymbalta)
Escitalopram (Lexapro)
Fluoxetine (Prozac)
Isocarboxazid (Marplan)
Paroxetine (Paxil, Paxil CR, Pexeva)
Phenelzine (Nardil)
Sertraline (Zoloft)
Tranylcypromine (Parnate)
Venlafaxine (Effexor XR)
Antidepressants identified as least likely to cause sexual side effects are:
Bupropion (Wellbrutin XL, Wellbrutin SR, Apllenzin, Forfivo XL)
Mirtazapine (Remeron)
Selegiline (Emsam) This is used as a skin patch.
Vilazodone (Viibryd)
Vortioxetine (Trintellix)
Sexual side effects in men and women
Men may experience difficulties in achieving or maintaining an erection as well as problems in achieving orgasm. Women may experience delayed lubrication and orgasm. In both men and women, the desire to engage in sexual intercourse may be greatly lessened or non-existent.
Women may experience delayed lubrication and orgasm. In both men and women, the desire to engage in sexual intercourse may be greatly lessened or non-existent.
The causes of sexual dysfunction may partly be due to depression itself. However, where sexual dysfunction appears to result from antidepressant medication, possible reasons relate to serotonin and dopamine. Antidepressants whose action is to increase the amount of serotonin in the brain (SSRIs) is also thought to depress sexual desire. As serotonin increases so dopamine, a neurotransmitter associated with pleasure and reward, may decrease. Decreased dopamine levels could account for lower sexual arousal.
Recommendations
There is no single, approved remedy for overcoming antidepressant-induced sexual dysfunction. What follows is a general round-up of some of the suggestions I have uncovered:
Time: If you’re taking antidepressants it can take several weeks before the therapeutic effects take hold and side effects diminish. Some people find once things have settled, their sex life improves. (Consider asking your doctor about switching the time antidepressant medication is taken to see if this helps.)
Some people find once things have settled, their sex life improves. (Consider asking your doctor about switching the time antidepressant medication is taken to see if this helps.)
Viagra: The pill famous for helping men achieve and maintain an erection has been used in various trials, with both men and women, with mixed results. Fibanserin (Addyi), meanwhile, was first approved by the FDA in 2015 for use in women who experience low sexual desire. Although not approved for antidepressant-induced sexual dysfunction, the controversial “female viagra” looks destined to be prescribed for that very reason, according to this article in Scientific American.
Dosage variation: With the approval of your doctor, small variations in antidepressant medication may have some positive effects with regard to sexual function. If this is not successful, then switching to an alternate antidepressant may be considered.
Lifestyle: It may feel counter-intuitive to exercise when your mood is very low, but even a modest amount of exercise can lift the spirits and improve wellbeing. A healthy diet is another important factor to consider.
A healthy diet is another important factor to consider.
Updated by: Jerry Kennard
Meet Our Writer
Anne Windermere
These articles were written by a longtime HealthCentral community member who shared valuable insights from her experience living with multiple chronic health conditions. She used the pen name "Merely Me."
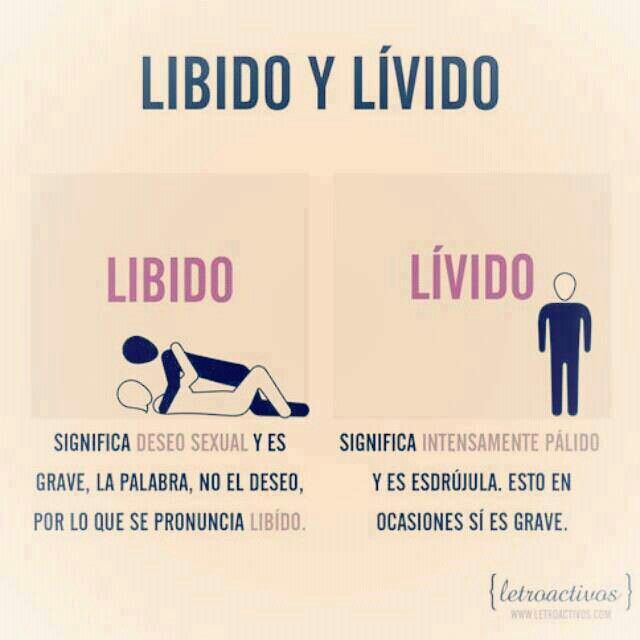
How does the libido work?
The term libido is commonly used to describe sexual desire or desire for sexual activity. Modern medicine recognizes the importance of libido as one of the key indicators of overall health and quality of life. In the article we understand how the libido works, why it is for a person and why sometimes the libido changes.
Content
- Evolution and libido
- Which hormones regulate libido in women
- What governs male libido
- Neurotransmitters: libido in the head
- Why libido increases
- Why libido can decrease
- Note
Evolution and Libido
Although the libido today is influenced by many factors, from psychological to cultural, its nature is evolutionary in origin.
Sex drive is a common trait in the reproduction of mammals and birds. The sexual activity of many species varies depending on the sexual cycle, that is, from periodically repeating changes in the body of females from one ovulation to another.
The fact is that the probability of conception is not uniform, but varies depending on the phase of the cycle. Man, for example, belongs to polyestrous animals, that is, species in which sexual cycles are repeated throughout the year. And although a person can conceive offspring on any day, the probability of fertilization is higher precisely on the days of ovulation. Libido these days is also, as a rule, increased.
Fluctuating libido is a mechanism that allows you to increase the frequency of sexual intercourse on the most favorable days for conception. Libido is an important force of natural selection, which encourages us to reproduce with maximum efficiency and pass our genetic material to the next generations, that is, to win the evolutionary lottery.
What hormones regulate libido in women
The main hormones that regulate sexual desire are sex hormones: estrogen, progesterone and testosterone. All three hormones are present in both male and female bodies. However, women have significantly less testosterone than men. Conversely, estrogen and progesterone are mostly female sex hormones.
In the first (follicular) phase of the menstrual cycle, several follicles grow and mature in the ovaries at once, the level of estrogen in the blood also increases. About a week before ovulation, a single dominant follicle is determined and continues to grow. The remaining follicles stop in their development and undergo the opposite - atresia. At the same time, the concentration of estrogen in the blood grows further, due to the production of the hormone by the dominant follicle. In the middle of the cycle, the follicle bursts, ovulation occurs - the release of the egg into the uterus through the fallopian tubes. After ovulation, estrogen levels gradually decrease.
Experiments have shown that both men and women rate photographs of women's faces taken before ovulation as more attractive than photographs of the same women after ovulation.
Women's libido is also strongest around ovulation, when estrogen is at its peak.
In addition, estrogen plays an important role in women's health, energizes and enhances attractiveness.
After ovulation comes the second (luteal) phase of the menstrual cycle. In place of the bursting follicle, a corpus luteum is formed, which releases progesterone. If fertilization does not occur, then by the end of the menstrual cycle, the corpus luteum disintegrates, and progesterone levels fall.
Low estrogen levels and high progesterone levels at the end of the cycle lead to a decrease in libido. With the onset of menstruation, sexual desire increases again.
However, due to the fact that both progesterone and estrogen levels simultaneously decrease approximately one week before the end of the cycle, PMS symptoms may occur: swelling, bloating, lethargy, mood swings.
In women who take hormonal contraceptives, hormone fluctuations are less pronounced, so changes in libido are not so noticeable.
Some women who take oral contraceptives may not notice any change in sex drive, while others report decreased libido as an unwanted side effect.
What governs male libido
The main male sex hormone is testosterone. Its fluctuations can affect the level of sexual desire. Thus, a decrease in testosterone is associated with low libido.
But if in women hormonal fluctuations are extended for a long period (about a month), then in men changes occur more often: testosterone levels are usually elevated in the morning, and decrease in the evening. Therefore, sexual desire is also often higher in the morning and lower late in the evening. In addition to daily fluctuations, testosterone levels also change throughout life, reaching a maximum in adolescence with a gradual decrease after 30 years.
Testosterone is not the only fuel that fuels the male libido.
Estradiol, the predominant form of estrogen, also affects sex drive.
In addition to testosterone, estradiol levels also affect libido. This is partly due to the fact that estradiol affects the areas of the brain that control sexual behavior, and partly due to the role of the hormone in the regulation of testosterone levels.
Sex hormones, their receptors and the aromatase enzyme are in a complex balance that regulates sexual behavior, erection, libido, as well as mood and mental state.
Neurotransmitters: libido in the head
The exact role of neurotransmitters, active brain chemicals, in sexual desire is not fully understood. But it can be noted that one of the “controlling” libido is a neurotransmitter and the hormone oxytocin. Oxytocin is called the hormone of love and affection because it is responsible for the positive emotions that a person experiences during the period of falling in love and at the peak of sexual desire. Oxytocin rises with arousal and orgasm.
Oxytocin is the hormone of love and affection. In women, nipple stimulation can cause a surge of oxytocin followed by arousal. In experiments on male rats, oxytocin has been shown to cause erection and ejaculation, and also increase sperm count.
One study showed that treating a patient with oxytocin nasal spray had a positive effect on libido, erection and orgasm. A little later, the successful experiment was repeated on 29 heterosexual couples. Participants reported that the introduction of the "love hormone" increased the intensity of orgasm and the satisfaction of partners after intercourse. In addition, participants were able to better share sexual desires and empathize with partners.
The effects were more pronounced in men. Men also noted higher levels of sexual satiety. However, the effect of treatment varied from small to moderate.
Another neurotransmitter that can influence libido is dopamine. Dopamine plays an important role in emotional behavior, attention, memory, reward and pleasure. Dopamine can affect testosterone levels, and testosterone can affect dopamine.
Dopamine can affect testosterone levels, and testosterone can affect dopamine.
The neurotransmitter dopamine also affects libido. Sex hormones create conditions for increasing the synthesis of dopamine, and its release leads to an increase in sexual desire, by activating the right areas of the brain.
In men, one of the key areas of the brain responsible for sexual behavior is the medial preoptic area. Injections of substances that mimic the effects of dopamine into such an area in rats lead to an increase in sexual activity.
An increase in libido can also occur after administration of the dopamine precursor, L-DOPA. Conversely, the introduction of molecules that block the work of dopamine leads to a decrease in libido.
Why libido increases
Hypersexuality due to various causes is diagnosed in approximately 2% of the population. An excessively high libido can be caused by:
- High levels of mood-regulating neurotransmitters such as dopamine and serotonin.

- A side effect of certain drugs (including those that affect dopamine levels).
- Damage to areas of the brain involved in sexual behavior (particularly in epilepsy).
Persistent sexual arousal that causes discomfort is a sign of hypersexual disorder.
There is a noticeable difference between high and too high libido. The cause for concern is the increase in sexual desire to a level that is out of control and interferes with daily life.
Why libido can decrease
A decrease in sexual desire is more common than an increase in it. Clinical criteria for diagnosing low libido have not been established, as there is a wide range of what is considered "low": normal sexual desire for one person may seem high or low for another. However, the following symptoms are commonly mentioned:
- Loss of desire for a partner.
- Disinterest in masturbation.
- Few or no sexual fantasies.
- Anxiety about lack of interest in sex.

Persistent reluctance to have sex may be a sign of hypoactive sexual desire disorder - anaphrodisia.
Hormonal disorders are a common cause of anaphrodisia. Libido may decrease in response to changes in estrogen, progesterone, and testosterone levels. Testosterone is the prime suspect.
In the absence of testosterone in men, libido is low, while treatment of testosterone deficiency leads to normalization of libido.
Women may also experience decreased sexual desire due to low testosterone, but decreased estrogen is more likely to be the cause. This is what happens during menopause. In a 2008 study, 27% of premenopausal women and 52% of menopausal women experienced low sex drive.
In addition to hormonal fluctuations, anaphrodisia can be caused by:
- Stress,
- Diabetes,
- High blood pressure,
- Certain medications, especially antidepressants,
- Alcohol abuse,
- Smoking,
- Underuse of drugs
In most cases, restoring libido can be achieved by making healthier lifestyle changes and reducing stress levels. Sometimes drug therapy is required to normalize hormonal balance.
Sometimes drug therapy is required to normalize hormonal balance.
Note
- Libido has an evolutionary origin. It helps mammals, including humans, maximize the chance of having offspring.
- The female libido is mainly dependent on progesterone and estrogen. In the first phase of the cycle before ovulation, there is a lot of estrogen, and little progesterone - libido is increased. In the second phase, estrogen becomes less and progesterone increases, so libido decreases.
- Taking oral contraceptives may affect a woman's libido.
- Male libido is primarily controlled by testosterone. The highest level of the hormone is in adolescence, and after 30 years it gradually decreases. Following testosterone, libido may also decrease.
- In addition to hormones, sexual desire is influenced by neurotransmitters: dopamine and oxytocin.
- Increased or decreased libido are relative concepts. There are no single indicators for determining the "normality" of a libido: what is a "normal" sexual desire for one person may seem high or low for another.
- Decreased libido - anaphrodisia - may be associated with stress, hormonal imbalance, bad habits, taking certain medications.
- Increased libido may be a symptom of a hypersexual disorder or may occur after certain drugs, brain injury or damage, or neurotransmitter imbalance.
- If the change in libido causes discomfort, you should consult a doctor.
Quality of life, high libido, good mood are in many cases indicators of good health. The Atlas Genetic Test helps you take care of yourself, understand your predisposition to multifactorial diseases, and improve your health with personalized test results.
Atlas Blog Articles about attraction:
A conversation with an expert. How to enjoy sex?
Sleep, diet and giving up your smartphone: what habits will make you happier?
- Roslan et al. The Bio-Psycho-Social Dimension in Women's Sexual Desire: 'Argumentum ad novitatem'.
 2019
2019 - Motta-Mena, Puts. Endocrinology of human female sexuality, mating, and reproductive behavior. 2016
- Roberts et al. Female facial attractiveness increases during the fertile phase of the menstrual cycle. 2004
- Rastrelli et al.Testosterone and sexual function in men.2018
- Oti et al. Systemic effects of oxytocin on male sexual activity via the spinal ejaculation generator in rats.2021
- MacDonald, Feifel. Dramatic improvement in sexual function induced by intranasal oxytocin. 2012
- Shoemaker. Male Libido, Testosterone, & Neurotransmitters. 2019
- Grazzotin. Libido: the biological scenario. 2000
- Montjero et al. Sexual side effects of antidepressant and antipsychotic drugs. 2015
- Shulster et al. The role of estradiol in male reproductive function. 2016
- Tuijl et. al. Three Diagnoses for Problematic Hypersexuality; Which Criteria Predict Help-Seeking Behavior? 2020
- West et.
 al. Prevalence of low sexual desire and hypoactive sexual desire disorder in a nationally representative sample of US women.2008
al. Prevalence of low sexual desire and hypoactive sexual desire disorder in a nationally representative sample of US women.2008 - Behnia et. al. Differential effects of intranasal oxytocin on sexual experiences and partner interactions in couples. 2014
- Dominguez, Hull. Dopamine, the medial preoptic area, and male sexual behavior.2005
"You Can Hack Your Libido Through Your Body": Researcher Sarah Hill on Hormones and Female Sexuality
Female hormones are so powerful that they can kill or revive your libido - and even "change" your orientation. How does this happen?
A couple of months ago, the publishing house "MIF" published a book by a researcher in the field of evolutionary psychology Sarah Hill - "You and your hormones." In it, Hill details exactly how hormones, both natural and in birth control pills, affect women's lives. At a meeting with a publishing house, Forbes Woman author Daria Shipacheva interviewed Sarah Hill. We publish the most interesting excerpts from it: about sexuality, gender, the difference between arousal and desire, and the effect of contraceptives on relationships.
At a meeting with a publishing house, Forbes Woman author Daria Shipacheva interviewed Sarah Hill. We publish the most interesting excerpts from it: about sexuality, gender, the difference between arousal and desire, and the effect of contraceptives on relationships.
Finished reading here
Do birth control pills kill sex?
- Many people think that oral contraceptives (OCs) can greatly reduce libido. On the other hand, I have come across this figure: only 2% of women surveyed say that their sex life has become worse after they started taking hormonal contraceptives. Can you please tell me how this compares with what your research shows?
- Indeed, many women complain of a decrease in libido under the influence of hormonal contraceptives - in particular, OK. Complain, of course, and other side effects. What is it connected with?
Complain, of course, and other side effects. What is it connected with?
When you use hormonal contraception, your body starts producing more globulins, special proteins that bind sex hormones. In this way, for example, part of the testosterone it produces is captured and made unavailable to your body. If your libido is sensitive to testosterone levels - and women can vary quite a lot in this parameter - then most likely, libido will decrease.
The second reason is directly related to how birth control generally works. This is due to the suppression of the increase in estrogen levels, which in the natural cycle occurs before ovulation - and then ovulation does not occur, and pregnancy becomes impossible. But long-term studies show that at that stage of the cycle, when estrogen levels are higher, libido is usually stronger - and women have more sex. If contraceptives suppress estrogen levels, it is understandable why this can lead to a decrease in libido. And if, in parallel with this, the available level of testosterone also decreases, the matter may end with the complete disappearance of sexual desire.
And if, in parallel with this, the available level of testosterone also decreases, the matter may end with the complete disappearance of sexual desire.
In terms of numbers, there are indeed reports of a drop in libido of 2% or so, and this is really very little. I would say that it is difficult to generalize here, because everything depends very much on the individual woman, as well as on what kind of hormonal contraception she uses. The fourth generation progestin usually has fewer side effects compared to the second and third generation progestins. More research is needed: at the current stage, it is difficult to give any unambiguous recommendations about which pills are best for a particular woman and minimize the risk of a decrease in libido.
- I know of a study where scientists concluded that pills containing more progesterone and less estrogen had less effect on libido, which sounds counterintuitive to me. From what you said above and what is written in your book, we can conclude that it is the high level of progesterone in OK that should first of all “kill” libido. How would you comment on such observations?
From what you said above and what is written in your book, we can conclude that it is the high level of progesterone in OK that should first of all “kill” libido. How would you comment on such observations?
- To be honest, I'm not familiar with the study you're talking about. I would be very curious to look at these conclusions of scientists. When choosing pills together with a doctor, you should pay attention to which progesterone is used there. The fact is that there are progestins that have a pronounced antiandrogenic effect. We know for sure about them that they are very, very harmful to the libido: not only do they suppress estrogen, they also block a woman's access to her own testosterone.
- We know that hormonal contraception is extremely effective when used correctly. At the same time, some women complain of a significant decrease in libido and therefore do not even want to think about OK, although their bad experience may be due to the fact that they used second or third generation pills. And now they are generally afraid to use hormonal contraception. This applies not only to pills, but also to hormonal implants and spirals. What advice would you give to such women?
And now they are generally afraid to use hormonal contraception. This applies not only to pills, but also to hormonal implants and spirals. What advice would you give to such women?
- I would recommend not giving up this opportunity after one bad experience. It is worth conducting different experiments - after all, hormonal contraception has almost 100 different types: different progestins are used, dosages of progesterone and estrogen, delivery methods are different. Sometimes the method of delivery of the active substance alone makes a big difference: a certain type of progesterone supplied by a spiral may not work quite the same as the same substance from a pill.
Therefore, please consult your doctor and try different options under his supervision if you are not yet ready to give up the idea of hormonal contraception completely.
It is also very important to keep a diary - in order to accurately track changes in your well-being, including libido.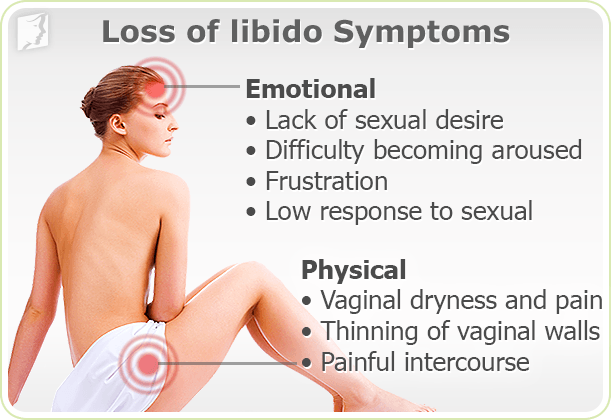 Then it will be possible to respond to specific deviations and change or cancel the drug in time.
Then it will be possible to respond to specific deviations and change or cancel the drug in time.
The physiological processes that trigger the stress response block the area of the brain that is responsible for sexual desire. It can be said that stress and libido are antagonists
Sexual "brake" and "gas" - in the head
- Since we started talking about sexual attraction: I heard the opinion that this term is generally outdated. It cannot be said about a woman that she has a strong or weak libido in general - all these are very subtle matters, very dependent on the influences of various internal and external stimuli. For example, Emily Nagoski in her book “How a Woman Wants” writes about “gas pedal” and “brake pedal” - this is her metaphor, with which she explains how female arousal and desire appear. Context is important: stress, of course, hits the “brake pedal” and kills l ibido, and a high level of intimacy, on the contrary, performs the function of a “gas pedal” and starts. How would you explain these two processes from a neurobiological point of view? [[{"fid":"364349","view_mode":"default","fields":{"format":"default","alignment":"","field_file_image_alt_text[und][0][value ]":"Sarah Hill","field_file_image_title_text[und][0][value]":false,"external_url":""},"type":"media","field_deltas":{"1":{" format":"default","alignment":"","field_file_image_alt_text[und][0][value]":"Sarah Hill","field_file_image_title_text[und][0][value]":false,"external_url" :""}},"attributes":{"alt":"Sarah Hill","class":"media-element fancyboxed file-default","data-delta":"1"}}]]
Context is important: stress, of course, hits the “brake pedal” and kills l ibido, and a high level of intimacy, on the contrary, performs the function of a “gas pedal” and starts. How would you explain these two processes from a neurobiological point of view? [[{"fid":"364349","view_mode":"default","fields":{"format":"default","alignment":"","field_file_image_alt_text[und][0][value ]":"Sarah Hill","field_file_image_title_text[und][0][value]":false,"external_url":""},"type":"media","field_deltas":{"1":{" format":"default","alignment":"","field_file_image_alt_text[und][0][value]":"Sarah Hill","field_file_image_title_text[und][0][value]":false,"external_url" :""}},"attributes":{"alt":"Sarah Hill","class":"media-element fancyboxed file-default","data-delta":"1"}}]]
- Very interesting question. What does stress look like in terms of brain function? Those physiological processes that trigger the stress response essentially "block" the area of the brain that is responsible for sexual desire. We can say that stress and libido are antagonists.
We can say that stress and libido are antagonists.
A woman's sexual desire, as you quite rightly noted, is very, very contextual. In men, this mechanism is more primitive: there is a person nearby who is sexually attractive to them - excellent, we turn on all the sexual processes in the body. And for a long time it was believed that attraction according to the male type is “correct”.
But you have to understand that the woman bears both the burden of pregnancy and all the additional risks associated with sex. That's why evolution designed our brains to turn on the sexual response only in the right situations: low stress, favorable conditions, a potential partner being tested for "worthiness" for the role of a potential father. Of course, all these things happen to us on a subconscious level - the head knows that we use various means of contraception, it's all generally unimportant, and in general, maybe it's a one-night stand, sex without penetration or with a partner of our own. gender. However, the process of arousal is triggered outside of consciousness: the female brain responds to a huge number of signals from the external and internal world, and these signals are associated with the fact that, from the point of view of evolution, should increase the chances for the survival of offspring.
gender. However, the process of arousal is triggered outside of consciousness: the female brain responds to a huge number of signals from the external and internal world, and these signals are associated with the fact that, from the point of view of evolution, should increase the chances for the survival of offspring.
— How can this program be hacked? For example, if a woman experiences a low level of arousal, but wants to increase it?
— You can come up with a lot of life hacks here. You can work, for example, directly with relationships - doing something with your partners that will generally increase the level of intimacy and trust. Because there is a linear relationship between the deepening of the spiritual connection between partners and the growth of female libido - Emily Nagoski in her book just talks about this.
Moreover, the female body, even in a state of stress and the "brake pedal" pressed, can also turn on the "gas pedal" - if a sexual context appears: touches, kisses, and so on.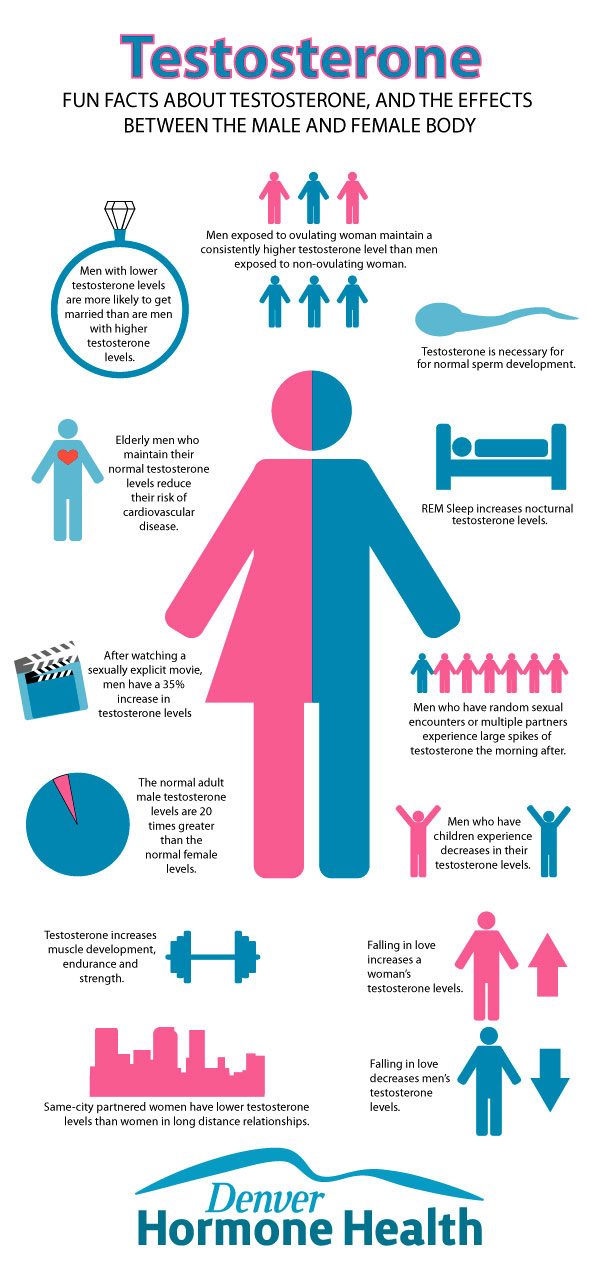 Of course, this should all be done by mutual consent. That is, you can go through physiology - even if initially the brain is not very attuned to sex, you can hack libido through the body, and then the brain will “catch up” with the body over time.
Of course, this should all be done by mutual consent. That is, you can go through physiology - even if initially the brain is not very attuned to sex, you can hack libido through the body, and then the brain will “catch up” with the body over time.
You can also try to influence testosterone. For example, winning competitive sports—and even board games—usually results in higher testosterone levels in women, and therefore increased attraction.
Desire and excitement are never synonyms. A woman may encounter a dissonance between desire and arousal - and begin to doubt herself
- Nagoski draws a distinction between desire and arousal - they say that these are different processes and they may not occur in a woman at the same time. What can you say about this in terms of neuroscience?
— Indeed, it happens that we experience arousal at moments when we do not want sex — that is, low desire can be combined with high arousal.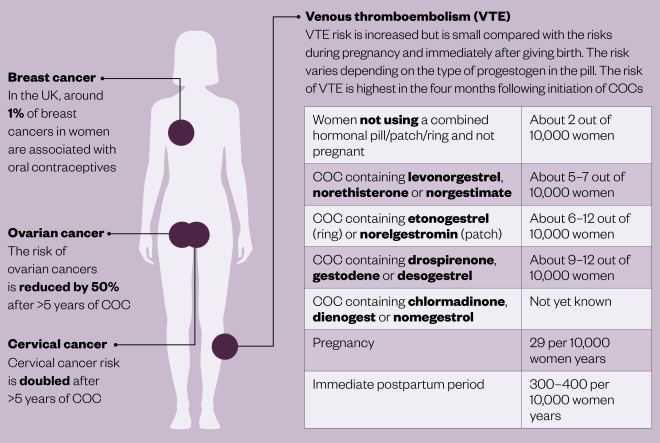 Sometimes the opposite happens: there is a strong desire for sex, but in terms of the response of the body, little happens.
Sometimes the opposite happens: there is a strong desire for sex, but in terms of the response of the body, little happens.
And here it is very important for women to learn this difference: desire and excitement are never synonyms. A woman may encounter a dissonance between desire and arousal - and begin to doubt herself. Her partner may also doubt his attractiveness to a woman. But in fact, such dissonance for female sexuality is normal, this phenomenon is called nonconcordance. Nonconcordance occurs in most women. Therefore, it seems to me that it is worth enjoying both processes - both arousal and desire - and managing them as far as possible.
- And yet, it seems, there is a difference between spontaneous desire and desire in response - and the latter is more pronounced in women. Tell us how it works?
- Spontaneous desire is directly related to estrogen. It happens like this: you hang out your underwear or vacuum there, and suddenly - “oops, it seems like you want sex”! And obviously it wasn't the vacuum cleaner that turned you on. This is a spontaneous desire: when it arises, you start thinking about sex, fantasize about it out of the blue.
It happens like this: you hang out your underwear or vacuum there, and suddenly - “oops, it seems like you want sex”! And obviously it wasn't the vacuum cleaner that turned you on. This is a spontaneous desire: when it arises, you start thinking about sex, fantasize about it out of the blue.
Men do this quite often - spontaneous thoughts about sex - and therefore it seems to them that women also "should" think about sex all the time. It seems to be "normal". But in women, this actually happens much less often - usually somewhere in the middle of the cycle, near ovulation, when the probability of becoming pregnant is high.
For a long time, excitement and desire according to the male type were considered the norm of sexuality.
Much more often women have a reciprocal desire. It's when you're hanging out your underwear, and then your partner comes up and starts touching, kissing and saying that it would be nice to have sex right now. The woman's body was set up more for washing, but in principle, desire appears in response to stimulation - why not?
It's when you're hanging out your underwear, and then your partner comes up and starts touching, kissing and saying that it would be nice to have sex right now. The woman's body was set up more for washing, but in principle, desire appears in response to stimulation - why not?
The response desire is especially active in the second half of the cycle - in the luteal phase, when the own level of estrogen sags and spontaneous desire becomes small. Men often do not understand this - it seems to them that a woman's interest in spontaneous sex should always be on the same level as theirs, but this does not work for us.
For a long time, excitement and desire according to the male type were considered the norm of sexuality. But now science has advanced, and we understand that all types of sexual response are good in their own way, none should be considered somehow less valuable than others.
- It turns out that women who take hormonal contraceptives will be more likely to experience reciprocal desire - all because of the drop in estrogen, right?
- Yes, that's right. I write about this in my book - and you just need to accept it as a kind of temporary phenomenon. There is nothing wrong with this - and it is absolutely not necessary to build self-identification around this change, God forbid, consider yourself "frigid".
- Let's talk a little about asexual people here. Some of them say that they get aroused, they just do not feel attracted to people and have no desire to have sex with them. How does asexuality work from a biological point of view?
- Great question - it's a pity that I don't have an answer to it. Asexuality seems to me a strikingly interesting phenomenon, but I do not fully understand how it works. What are my guesses?
Asexuality seems to me a strikingly interesting phenomenon, but I do not fully understand how it works. What are my guesses?
It is clear that everything related to sexual arousal and desire originates in the brain - and there is certainly a hormonal component to what happens there in asexual people. We can see this in the OC studies as well, as some women lose their sexual desire after starting birth control.
The influence of hormones on sexuality, attraction and even orientation is generally amazing. I have seen stories of women who self-identified as lesbians, but after they started taking OK, they began to consider men sexually attractive as well! And vice versa, in heterosexual women, against the background of OK, an interest in girls woke up. Yes, these are rare cases, but such exceptions give us a very interesting opportunity to trace how certain hormones can shape sexuality.
There is no doubt that hormones play a role in the development of asexuality. Another thing is that asexuality is a very subtle and complex relationship between biological and psychological, and we have not yet precisely defined the role of biology.
- I remember the story of one transgender person - this was a born woman who felt asexual and gender non-binary. She had a very low libido, she did not experience any sexual desire. Then she began to take very small doses of testosterone, her libido began to grow - and she even began to experience sexual desire. So there is no doubt that hormones are very, very powerful things.
— It certainly is. Transgender transition today can be considered such a natural experiment in the field of how the attraction of men and women to the opposite or same sex works - and what role hormones play in all this.
- D I think it can be summed up like this: if you feel like an asexual person, but it does not cause you discomfort, then that's fine, you can do nothing about it at all. And if you want your libido to grow, you can go to the doctor and try, for example, hormone therapy.
- I think this is very wise and good advice.
How hormones affect mate choice
- In your book, you talk about how hormone pills affect what kind of people we find attractive. For example, heterosexual women who start taking OCs often find less masculine men more attractive than those who do not use the pill. What other interesting observations do you have?
This is indeed a very interesting area for research. If this is how things really work, then taking hormones can have a very significant impact on your relationship.
If this is how things really work, then taking hormones can have a very significant impact on your relationship.
Research has been going on for decades that show that during the follicular phase of the menstrual cycle, when women produce a lot of estrogens, they find masculine men more attractive - a lower voice, a squarer jaw, and so on. This is for women with a natural cycle. But women who take hormonal pills find more attractive men who have less masculine features - for them, other characteristics of a potential partner come to the fore. Some research suggests that women on OK are more aroused by a man's ability to financially provide for his family, empathy, and his ability to maintain a stable relationship. That is, they want to find in a man, first of all, such a stereotypical “good father”, a safe partner.
Pills can affect which partners you choose for yourself - and this, in turn, can even affect the frequency of divorces
- So, hormonal pills can help you choose a more “correct” person for a relationship?
- It turns out that yes, the pills can affect which partners you choose - and this, in turn, can even affect the divorce rate. Actually, there are already studies showing that women who choose partners while taking hormonal pills are less likely to get divorced - because they choose not so much “males” as “fathers”. And here, of course, the effect of estrogen is easily traced.
Actually, there are already studies showing that women who choose partners while taking hormonal pills are less likely to get divorced - because they choose not so much “males” as “fathers”. And here, of course, the effect of estrogen is easily traced.
Again, there is scientific evidence showing that if you chose a partner using pills and then stopped taking OCs, you are more likely to have relationship difficulties. And vice versa: if you didn’t take pills before, but started in marriage, this can also lead to problems in a couple.
So if you've become concerned about hormonal contraception while already in a couple, it may reduce your attraction to your partner.
— And what to do then? Throw pills (or start taking them again), get divorced? Or maybe try seeing a family therapist?
- If you generally have a very good relationship with your partner, then other factors - even as strong as the influence of hormones - will be less important.