Does luvox make you gain weight
Antidepressants and Weight Gain
Many individuals have the experience of weight gain while receiving treatment with an antidepressant, and often wonder if selective serotonin reuptake inhibitors (SSRIs) are associated with weight gain. This is an excellent, complex, and clinically important question.
Depression, anxiety, appetite, and weight: There is a relationship between appetite and depression, with changes in appetite representing a core symptom of major depressive disorder. Many individuals with anxiety disorders also note appetite changes when their anxiety symptoms are not well controlled. Some individuals lose weight when they are experiencing depression or anxiety, and some notice increased appetite and weight gain. Therefore, at the time of starting an antidepressant, some individuals may be at either a lower or higher weight than they would be at in the absence of a mood or anxiety disorder.
Drugs with known weight gain: Some medications used commonly in psychiatry have well established side effects of weight changes. For example, valproic acid, some of the atypical antipsychotic medications, lithium, the antidepressant mirtazapine (Remeron), and tricyclic antidepressants are associated with weight gain. There has been little systematic long-term data regarding weight effects of SSRI antidepressants (which include fluoxetine (Prozac), sertraline (Zoloft), citalopram (Celexa), escitalopram (Lexapro), paroxetine (Paxil), and fluvoxamine (Luvox), and the SNRIs venlafaxine (Effexor) and duloxetine (Cymbalta), although some studies suggest weight gain may occur and may vary by gender, specific medication, and other patient variables. Bupropion (Wellbutrin) is usually considered weight neutral.
Whether or not a study was short- or long-term – or clinically how long a patient has been on a medication – may influence the likelihood of weight changes. A recent meta-analysis assessed studies with available data (Serretti and Mandelli, 2010). In acute studies (4-12 weeks duration), most SSRIs, SNRIs, and bupropion have been associated with weight loss. In longer term studies (longer than four months), most antidepressant medications with available data did not have significantly associated weight gain, and the most was seen with paroxetine and the older antidepressant amitriptyline (mean weight gain about 5-6 lbs). Only bupropion was associated with significant weight loss (about 4 lbs).
In longer term studies (longer than four months), most antidepressant medications with available data did not have significantly associated weight gain, and the most was seen with paroxetine and the older antidepressant amitriptyline (mean weight gain about 5-6 lbs). Only bupropion was associated with significant weight loss (about 4 lbs).
SSRIs: Data that inform risk of weight gain and how specific medications compare to each other
There have been a few studies to provide head-to-head comparisons of weight gain amongst those treated with specific SSRIs. For example, Fava and colleages (2000) completed a study in which patients with major depression were randomly assigned to either fluoxetine, sertraline, or paroxetine. Only those that completed the 26-32 week trial were included in the final analysis of weight gain. Those who received paroxetine experienced a statistically significant weight gain from baseline to end point. Those who received fluoxetine had a trend for weight loss (not statistically significant), and those who received sertraline had a trend for moderate weight gain (not statistically significant).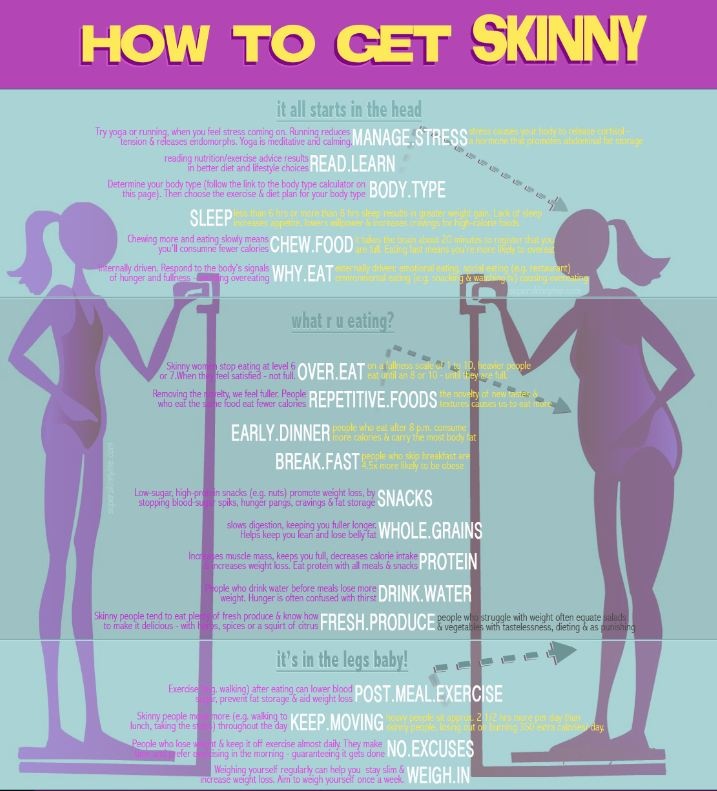
Those that received paroxetine were also significantly more likely than those who received fluoxetine or sertraline to gain >7% of their original body weight, the threshold used in many studies to indicate clinically important weight gain. Mean percent changes in weight from the beginning of the study to the end were: 0.2% weight loss with fluoxetine, 1% weight gain with sertraline, and 3.6% weight increase with paroxetine. Therefore, if the typical participant weighted 150 lbs, the weight gain would be about 5.4 lbs with paroxetine and 1.5 lbs with sertraline, and the weight loss would be less than 1 pound with fluoxetine. While these are overall modest differences from the baseline weights, they are means, so some individual patients could certainly have had very different experiences than the mean.
In another study (Maina 2004), researchers assessed patients in an anxiety disorder clinic for weight changes with the tricyclic antidepressant clomipramine or SSRIs over a 2. 5 year period. The group included 138 patients with obsessive compulsive disorder. They were not randomly assigned to medication. On average, the patients as a group gained 2.5% of their baseline weight (1.58 kg or 3.5 pounds over 2.5 years of treatment). 14.5% of the sample gained >7% of their initial body weight. For all medications except fluoxetine, which did not have significant weight gain, the others (clomipramine, citalopram, fluvoxamine, paroxetine, and sertraline) were associated with statistically significant weight gain over the 2.5 year duration of study. Clomipramine had the greatest percentile of patients who gained >7% of body weight, while fluoxetine and sertraline had the lowest. Women were more likely to gain weight than men.
5 year period. The group included 138 patients with obsessive compulsive disorder. They were not randomly assigned to medication. On average, the patients as a group gained 2.5% of their baseline weight (1.58 kg or 3.5 pounds over 2.5 years of treatment). 14.5% of the sample gained >7% of their initial body weight. For all medications except fluoxetine, which did not have significant weight gain, the others (clomipramine, citalopram, fluvoxamine, paroxetine, and sertraline) were associated with statistically significant weight gain over the 2.5 year duration of study. Clomipramine had the greatest percentile of patients who gained >7% of body weight, while fluoxetine and sertraline had the lowest. Women were more likely to gain weight than men.
Postpartum Women
Wisner and colleagues (2005) specifically looked at the weight impact of treatment with nortriptyline, sertraline, or placebo in women with histories of postpartum depression (PPD) who took medication after childbirth to prevent having PPD again. Mean weights after 17 weeks of treatment were not significantly different between the treatment groups. On average, women lost about 1.8 pounds over the course of the study. Because the study was a depression prevention study, women were not experiencing depression at the time of study entry, so the treatment of depressive symptoms would not be a driving factor for weight change.
Mean weights after 17 weeks of treatment were not significantly different between the treatment groups. On average, women lost about 1.8 pounds over the course of the study. Because the study was a depression prevention study, women were not experiencing depression at the time of study entry, so the treatment of depressive symptoms would not be a driving factor for weight change.
The Bottom Line
Antidepressant medications can potentially contribute to weight gain, and certain antidepressants may carry a higher risk. Specifically among SSRIs, from these studies data suggest paroxetine carries the highest risk of weight gain and fluoxetine the lowest risk in the class. Additionally, recovery from depression and anxiety disorders may also contribute to increased appetite and weight. Not everyone will experience the same benefits or side effects to specific drugs. If over time, weight gain occurs and it appears that the antidepressant appear to be a major contributor to weight gain, one might consider switching to another medication or non-pharmacologic treatments.
Marlene Freeman, MD
Serretti A & Mandelli L. Antidepressants and Body Weight: A Comprehensive Review and Meta-Analysis. J Clin Psychiatry 2010;71(10):1259–1272.
Wisner et al. Weight changes in postpartum women with remitted depression. J Clin Psychiatry. 2005; 66(3):291-3.
Fava M, Judge R, Hoog SL, Nilsson ME, Koke SC. Fluoxetine versus sertraline and paroxetine in major depressive disorder: changes in weight with long-term treatment. J Clin Psychiatry. 2000; 61(11):863-7.
Maina G, Albert U, Salvi V, Bogetto F. Weight gain during long-term treatment of obsessive-compulsive disorder: a prospective comparison between serotonin reuptake inhibitors. J Clin Psychiatry. 2004; 65(10):1365-71.
Related Posts
Fluvoxamine Advanced Patient Information - Drugs.com
Medically reviewed by Drugs.com. Last updated on Feb 21, 2023.
Oral route(Capsule, Extended Release;Tablet)
Antidepressants can increase the risk of suicidal thinking and behavior in children, adolescents, and young adults with major depressive disorder and other psychiatric disorders. This risk was not observed in patients older than 24 years, and the risk was reduced in patients 65 years or younger. Closely monitor patients of all ages for clinical worsening and emergence of suicidal thoughts and behaviors. . Fluvoxamine maleate tablets are not approved for use in pediatric patients except for patients with obsessive compulsive disorder .
This risk was not observed in patients older than 24 years, and the risk was reduced in patients 65 years or younger. Closely monitor patients of all ages for clinical worsening and emergence of suicidal thoughts and behaviors. . Fluvoxamine maleate tablets are not approved for use in pediatric patients except for patients with obsessive compulsive disorder .
Commonly used brand name(s)
In the U.S.
- Luvox
- Luvox CR
Available Dosage Forms:
- Capsule, Extended Release
- Tablet
Therapeutic Class: Antidepressant
Pharmacologic Class: Serotonin Reuptake Inhibitor
Uses for fluvoxamine
Fluvoxamine is used to treat obsessive compulsive disorder (OCD). It belongs to a group of medicines known as selective serotonin reuptake inhibitors (SSRIs). These medicines are thought to work by increasing the activity of a chemical called serotonin in the brain. .
Fluvoxamine is available only with your doctor's prescription.
Before using fluvoxamine
In deciding to use a medicine, the risks of taking the medicine must be weighed against the good it will do. This is a decision you and your doctor will make. For fluvoxamine, the following should be considered:
Allergies
Tell your doctor if you have ever had any unusual or allergic reaction to fluvoxamine or any other medicines. Also tell your health care professional if you have any other types of allergies, such as to foods, dyes, preservatives, or animals. For non-prescription products, read the label or package ingredients carefully.
Pediatric
Appropriate studies performed to date have not demonstrated pediatric-specific problems that would limit the usefulness of fluvoxamine tablets in children 8 to 17 years of age. Because fluvoxamine may cause weight loss or a decrease in appetite, children who will be taking fluvoxamine for a long time should have their weight and growth measured by the doctor regularly.
Appropriate studies have not been performed on the relationship of age to the effects of fluvoxamine extended-release capsules in the pediatric population. Safety and efficacy have not been established.
Geriatric
Appropriate studies performed to date have not demonstrated geriatric-specific problems that would limit the usefulness of fluvoxamine in the elderly. However, elderly patients are more likely to have hyponatremia (low sodium in the blood) and age-related liver problems, which may require an adjustment in the dose for patients receiving fluvoxamine.
Breastfeeding
There are no adequate studies in women for determining infant risk when using this medication during breastfeeding. Weigh the potential benefits against the potential risks before taking this medication while breastfeeding.
Interactions with medicines
Although certain medicines should not be used together at all, in other cases two different medicines may be used together even if an interaction might occur. In these cases, your doctor may want to change the dose, or other precautions may be necessary. When you are taking fluvoxamine, it is especially important that your healthcare professional know if you are taking any of the medicines listed below. The following interactions have been selected on the basis of their potential significance and are not necessarily all-inclusive.
In these cases, your doctor may want to change the dose, or other precautions may be necessary. When you are taking fluvoxamine, it is especially important that your healthcare professional know if you are taking any of the medicines listed below. The following interactions have been selected on the basis of their potential significance and are not necessarily all-inclusive.
Using fluvoxamine with any of the following medicines is not recommended. Your doctor may decide not to treat you with this medication or change some of the other medicines you take.
- Agomelatine
- Alosetron
- Astemizole
- Bromopride
- Cisapride
- Eliglustat
- Furazolidone
- Iproniazid
- Isocarboxazid
- Levomethadyl
- Linezolid
- Mavacamten
- Methylene Blue
- Metoclopramide
- Moclobemide
- Pargyline
- Phenelzine
- Pimozide
- Procarbazine
- Ramelteon
- Rasagiline
- Selegiline
- Terfenadine
- Thioridazine
- Tizanidine
- Tranylcypromine
Using fluvoxamine with any of the following medicines is usually not recommended, but may be required in some cases. If both medicines are prescribed together, your doctor may change the dose or how often you use one or both of the medicines.
If both medicines are prescribed together, your doctor may change the dose or how often you use one or both of the medicines.
- Abciximab
- Abrocitinib
- Acalabrutinib
- Aceclofenac
- Acemetacin
- Acenocoumarol
- Alfentanil
- Almotriptan
- Alprazolam
- Amiodarone
- Amoxapine
- Amphetamine
- Amtolmetin Guacil
- Anagrelide
- Ancrod
- Anisindione
- Antithrombin III Human
- Apixaban
- Ardeparin
- Asenapine
- Aspirin
- Avapritinib
- Belzutifan
- Bemiparin
- Bendamustine
- Benzhydrocodone
- Benzphetamine
- Bivalirudin
- Bosutinib
- Brigatinib
- Bromfenac
- Bufexamac
- Buprenorphine
- Bupropion
- Butorphanol
- Cangrelor
- Carvedilol
- Celecoxib
- Certoparin
- Choline Salicylate
- Cilostazol
- Citalopram
- Clonixin
- Clopidogrel
- Clorgyline
- Clozapine
- Codeine
- Colchicine
- Cyclobenzaprine
- Dalteparin
- Danaparoid
- Daridorexant
- Defibrotide
- Deflazacort
- Dermatan Sulfate
- Desirudin
- Desmopressin
- Desvenlafaxine
- Dexfenfluramine
- Dexibuprofen
- Dexketoprofen
- Dextroamphetamine
- Dextromethorphan
- Diclofenac
- Dicumarol
- Diflunisal
- Dihydrocodeine
- Dihydroergotamine
- Dipyridamole
- Dipyrone
- Dolasetron
- Domperidone
- Donepezil
- Doxorubicin
- Doxorubicin Hydrochloride Liposome
- Droperidol
- Droxicam
- Duloxetine
- Edoxaban
- Elacestrant
- Eletriptan
- Elexacaftor
- Encorafenib
- Enoxaparin
- Entrectinib
- Epoprostenol
- Eptifibatide
- Ergoloid Mesylates
- Ergonovine
- Ergotamine
- Escitalopram
- Etodolac
- Etofenamate
- Etoricoxib
- Felbinac
- Fenfluramine
- Fenoprofen
- Fentanyl
- Fepradinol
- Feprazone
- Fexinidazole
- Finerenone
- Floctafenine
- Flufenamic Acid
- Fluoxetine
- Flurbiprofen
- Fondaparinux
- Frovatriptan
- Granisetron
- Heparin
- Hydrocodone
- Hydromorphone
- Hydroxytryptophan
- Ibrutinib
- Ibuprofen
- Iloprost
- Indomethacin
- Infigratinib
- Iobenguane I 123
- Iobenguane I 131
- Ivacaftor
- Ivosidenib
- Ketoprofen
- Ketorolac
- Lasmiditan
- Lemborexant
- Levomilnacipran
- Levorphanol
- Lisdexamfetamine
- Lithium
- Lorcaserin
- Lornoxicam
- Loxoprofen
- Lumateperone
- Lumiracoxib
- Lurbinectedin
- Meclofenamate
- Mefenamic Acid
- Melatonin
- Meloxicam
- Meperidine
- Metaxalone
- Methadone
- Methamphetamine
- Methylergonovine
- Milnacipran
- Mirtazapine
- Mitapivat
- Mobocertinib
- Morniflumate
- Morphine
- Morphine Sulfate Liposome
- Nabumetone
- Nadroparin
- Nalbuphine
- Naproxen
- Naratriptan
- Nepafenac
- Nialamide
- Niflumic Acid
- Nimesulide
- Nimesulide Beta Cyclodextrin
- Olanzapine
- Olaparib
- Omaveloxolone
- Ondansetron
- Ospemifene
- Oxaprozin
- Oxycodone
- Oxymorphone
- Oxyphenbutazone
- Ozanimod
- Pacritinib
- Palonosetron
- Parecoxib
- Parnaparin
- Paroxetine
- Pemigatinib
- Pentazocine
- Pentosan Polysulfate Sodium
- Pexidartinib
- Phenindione
- Phenprocoumon
- Phenylbutazone
- Piketoprofen
- Piperaquine
- Pirfenidone
- Piroxicam
- Pixantrone
- Pomalidomide
- Pranoprofen
- Prasugrel
- Proglumetacin
- Propyphenazone
- Proquazone
- Remifentanil
- Reviparin
- Rimegepant
- Rivaroxaban
- Rizatriptan
- Rofecoxib
- Safinamide
- Salicylic Acid
- Salsalate
- Selexipag
- Selumetinib
- Sertraline
- Sibutramine
- Sirolimus Protein-Bound
- Sodium Salicylate
- Sonidegib
- Sparsentan
- St John's Wort
- Sufentanil
- Sulfinpyrazone
- Sulindac
- Sumatriptan
- Tacrolimus
- Tamoxifen
- Tapentadol
- Tasimelteon
- Tazemetostat
- Tenoxicam
- Tezacaftor
- Theophylline
- Tiaprofenic Acid
- Ticagrelor
- Ticlopidine
- Tinzaparin
- Tirofiban
- Tolfenamic Acid
- Tolmetin
- Toloxatone
- Tolvaptan
- Tramadol
- Treprostinil
- Triclabendazole
- Tryptophan
- Ubrogepant
- Valdecoxib
- Venetoclax
- Venlafaxine
- Vilazodone
- Voclosporin
- Vorapaxar
- Vortioxetine
- Warfarin
- Zanubrutinib
- Ziprasidone
- Zolmitriptan
Using fluvoxamine with any of the following medicines may cause an increased risk of certain side effects, but using both drugs may be the best treatment for you. If both medicines are prescribed together, your doctor may change the dose or how often you use one or both of the medicines.
If both medicines are prescribed together, your doctor may change the dose or how often you use one or both of the medicines.
- Amitriptyline
- Amlodipine
- Clomipramine
- Cyclosporine
- Diazepam
- Fosphenytoin
- Galantamine
- Ginkgo
- Haloperidol
- Imipramine
- Mexiletine
- Midazolam
- Phenytoin
- Propranolol
- Roflumilast
- Ropivacaine
- Suvorexant
- Tacrine
- Triazolam
- Zolpidem
Interactions with food/tobacco/alcohol
Certain medicines should not be used at or around the time of eating food or eating certain types of food since interactions may occur. Using alcohol or tobacco with certain medicines may also cause interactions to occur. The following interactions have been selected on the basis of their potential significance and are not necessarily all-inclusive.
Using fluvoxamine with any of the following is usually not recommended, but may be unavoidable in some cases.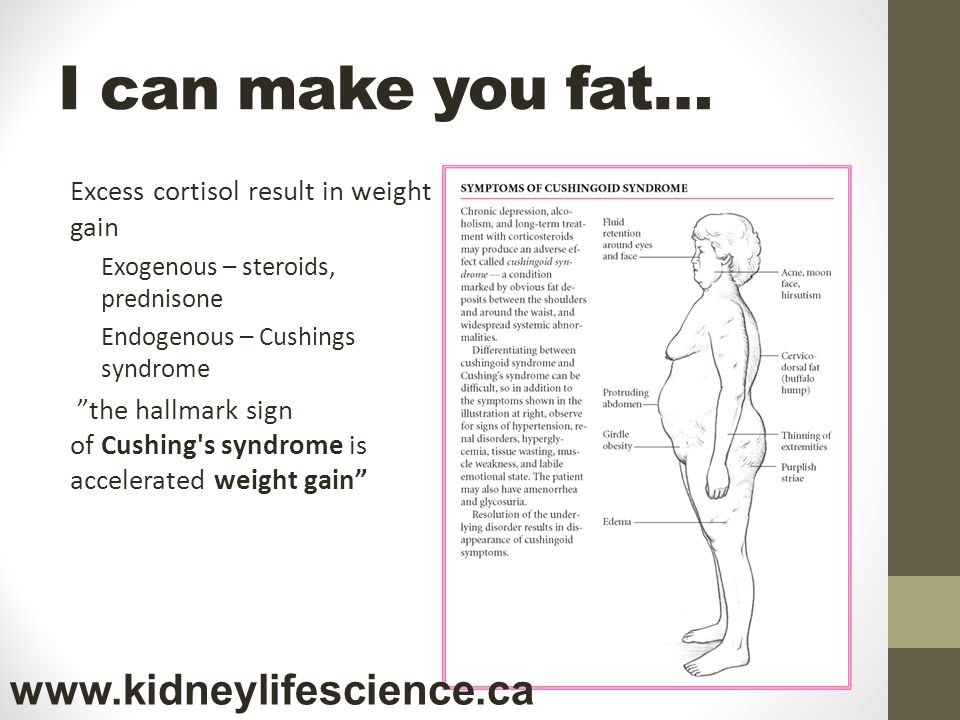 If used together, your doctor may change the dose or how often you use fluvoxamine, or give you special instructions about the use of food, alcohol, or tobacco.
If used together, your doctor may change the dose or how often you use fluvoxamine, or give you special instructions about the use of food, alcohol, or tobacco.
- Tobacco
Other medical problems
The presence of other medical problems may affect the use of fluvoxamine. Make sure you tell your doctor if you have any other medical problems, especially:
- Bipolar disorder (mental disease with mania and depression), history of or
- Bleeding problems or
- Depression, or history of or
- Glaucoma, angle-closure or
- Heart attack, recent or
- Heart disease or
- Heart rhythm problems (eg, arrhythmia, QT prolongation) or
- Hyponatremia (low sodium in the blood) or
- Mania (feeling elated), history of or
- Mental health problems, or history of or
- Seizures, or history of—Use with caution. May make these conditions worse.
- Liver disease—Use with caution. The effects may be increased because of slower removal of the medicine from the body.

Proper use of fluvoxamine
Take fluvoxamine exactly as directed by your doctor. Do not take more of it, do not take it more often, and do not take it for a longer time than your doctor ordered.
Fluvoxamine should come with a Medication Guide. Read and follow the instructions carefully. Ask your doctor if you have any questions.
Fluvoxamine may be taken with or without food. Take fluvoxamine at bedtime, unless your doctor tells you otherwise.
Swallow the extended-release capsule whole. Do not crush, break, or chew it.
You might have to take fluvoxamine for several months before you begin to feel better.
Dosing
The dose of fluvoxamine will be different for different patients. Follow your doctor's orders or the directions on the label. The following information includes only the average doses of fluvoxamine. If your dose is different, do not change it unless your doctor tells you to do so.
The amount of medicine that you take depends on the strength of the medicine.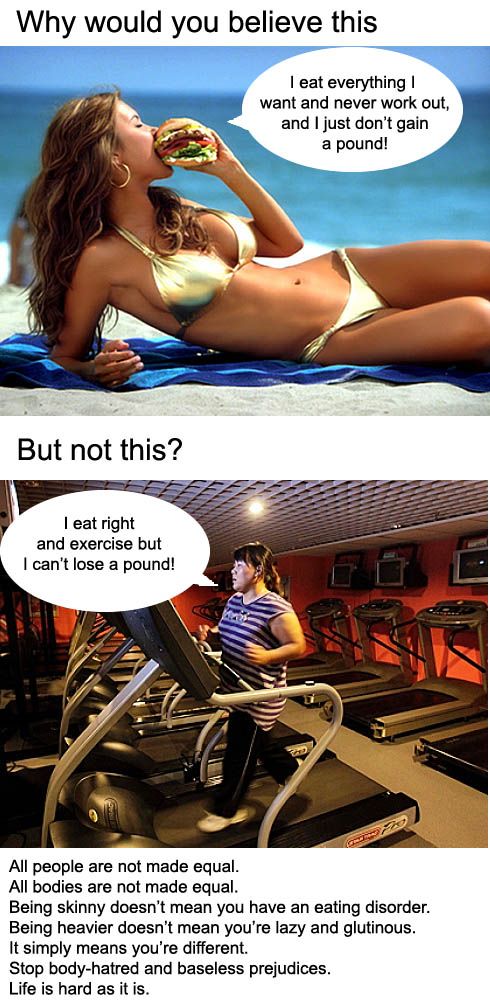 Also, the number of doses you take each day, the time allowed between doses, and the length of time you take the medicine depend on the medical problem for which you are using the medicine.
Also, the number of doses you take each day, the time allowed between doses, and the length of time you take the medicine depend on the medical problem for which you are using the medicine.
- For treatment of obsessive-compulsive disorder:
- For oral dosage form (extended-release capsules):
- Adults—At first, 100 milligrams (mg) once a day at bedtime. Your doctor may adjust your dose as needed. However, the dose is usually not more than 300 mg per day.
- Children—Use and dose must be determined by your doctor.
- For oral dosage form (tablets):
- Adults—At first, 50 milligrams (mg) once a day at bedtime. Your doctor may adjust your dose as needed. However, the dose is usually not more than 300 mg per day. If your daily dose is higher than 100 mg, your doctor may want you to take it in 2 divided doses.
- Children 8 to 17 years of age—At first, 25 mg once a day at bedtime. Your doctor may adjust your dose as needed. However, the dose is usually not more than 200 mg or 300 mg per day based on age.
 If your daily dose is higher than 50 mg, your doctor may want you to take it in 2 divided doses.
If your daily dose is higher than 50 mg, your doctor may want you to take it in 2 divided doses. - Children younger than 8 years of age—Use and dose must be determined by your doctor.
- For oral dosage form (extended-release capsules):
Missed dose
If you miss a dose of fluvoxamine, take it as soon as possible. However, if it is almost time for your next dose, skip the missed dose and go back to your regular dosing schedule. Do not double doses.
Storage
Store the medicine in a closed container at room temperature, away from heat, moisture, and direct light. Keep from freezing.
Keep out of the reach of children.
Do not keep outdated medicine or medicine no longer needed.
Ask your healthcare professional how you should dispose of any medicine you do not use.
Precautions while using fluvoxamine
It is very important that your doctor check your progress at regular visits. This will allow for changes in the dose and to help reduce any side effects. Blood tests may be needed to check for unwanted effects.
Blood tests may be needed to check for unwanted effects.
Do not take alosetron (Lotronex®), pimozide (Orap®), ramelteon (Rozerem®), thioridazine (Mellaril®), or tizanidine (Zanaflex®) while you are taking fluvoxamine. You could have more side effects than usual if you use these medicines together.
Do not take fluvoxamine with a monoamine oxidase (MAO) inhibitor (eg, isocarboxazid [Marplan®], linezolid [Zyvox®], methylene blue injection, phenelzine [Nardil®], selegiline [Eldepryl®], tranylcypromine [Parnate®]). Do not start taking fluvoxamine during the 2 weeks after you stop a MAO inhibitor and wait 2 weeks after stopping fluvoxamine before you start taking a MAO inhibitor. If you take them together or do not wait 2 weeks, you may develop confusion, agitation, restlessness, stomach or intestinal symptoms, a sudden high body temperature, an extremely high blood pressure, or severe seizures.
Fluvoxamine may cause a serious condition called serotonin syndrome if taken together with some medicines.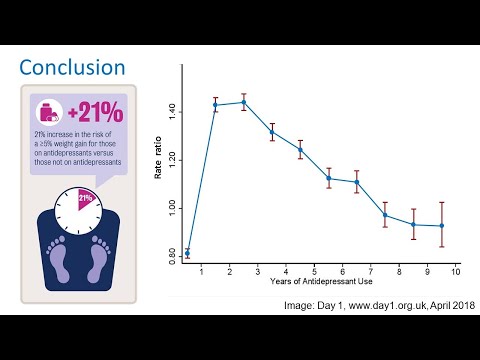 Do not use fluvoxamine with buspirone (Buspar®), fentanyl (Abstral®, Duragesic®), lithium (Eskalith®, Lithobid®), tryptophan, St. John's wort, amphetamines, or some pain or migraine medicines (eg, rizatriptan, sumatriptan, tramadol, Frova®, Imitrex®, Maxalt®, Relpax®, Ultram®, Zomig®). Check with your doctor first before taking any other medicines with fluvoxamine.
Do not use fluvoxamine with buspirone (Buspar®), fentanyl (Abstral®, Duragesic®), lithium (Eskalith®, Lithobid®), tryptophan, St. John's wort, amphetamines, or some pain or migraine medicines (eg, rizatriptan, sumatriptan, tramadol, Frova®, Imitrex®, Maxalt®, Relpax®, Ultram®, Zomig®). Check with your doctor first before taking any other medicines with fluvoxamine.
Fluvoxamine may cause some people to be agitated, irritable or display other abnormal behaviors. It may also cause some children, teenagers, and young adults to have suicidal thoughts and tendencies or to become more depressed. Some people may have trouble sleeping, get upset easily, have a big increase in energy, or start to act reckless. If you, or your caregiver notice any of these side effects, tell your doctor right away. Let the doctor know if you or anyone in your family has bipolar disorder (manic-depressive) or has tried to commit suicide.
Avoid drinking alcohol with fluvoxamine.
Fluvoxamine may cause some people to become drowsy, less able to think clearly, or to have blurred vision or poor muscle control. Make sure you know how you react to fluvoxamine before you drive, use machines, or do anything else that could be dangerous if you are not alert or able to see clearly.
Do not suddenly stop taking fluvoxamine without checking with your doctor first. Your doctor may want you to gradually reduce the amount you are taking before stopping it completely. This is to decrease the chance of having withdrawal symptoms such as agitation, confusion, headache, irritability, numbness or tingling, restlessness, trouble sleeping, or unusual drowsiness or weakness.
Fluvoxamine may increase your risk for bleeding problems. Make sure your doctor knows if you are also taking other medicines that thin the blood, including aspirin, NSAIDs (eg, diclofenac, ibuprofen, naproxen, Advil®, Aleve®, Celebrex®, Voltaren®), or warfarin (Coumadin®, Jantoven®).
Hyponatremia (low sodium in the blood) may occur with fluvoxamine. Check with your doctor right away if you have confusion, difficulty concentrating, headaches, memory problems, weakness, and unsteadiness.
Tell your doctor right away if you develop a rash or hives, swelling of the face, eyes, or mouth, or trouble breathing after taking fluvoxamine.
Check with your doctor right away if you have decreased interest in sexual intercourse, delayed or inability to have an orgasm in women, inability to have or keep an erection in men, or loss in sexual ability, desire, drive, or performance. These could be symptoms of sexual dysfunction.
Some men and women who use fluvoxamine have become infertile (unable to have children). Talk with your doctor before using fluvoxamine if you plan to have children.
Do not take other medicines unless they have been discussed with your doctor. This includes prescription or nonprescription (over-the-counter [OTC]) medicines and herbal (eg, St. John's wort) or vitamin supplements.
Fluvoxamine side effects
Along with its needed effects, a medicine may cause some unwanted effects. Although not all of these side effects may occur, if they do occur they may need medical attention.
Check with your doctor immediately if any of the following side effects occur:
More common
- Decreased interest in sexual intercourse
- inability to have or keep an erection
- loss in sexual ability, desire, drive, or performance
Less common
- Behavior, mood, or mental changes
- delayed or inability to have an orgasm
- trouble with breathing
- trouble with urinating
- twitching
Rare
- Absence of or decrease in body movements
- agitation
- blurred vision
- chills
- clumsiness or unsteadiness
- confusion
- convulsions (seizures)
- diarrhea
- fever
- inability to move the eyes
- increase in body movements
- menstrual changes
- nosebleeds
- overactive reflexes
- poor coordination
- red or irritated eyes
- redness, tenderness, itching, burning, or peeling of the skin
- restlessness
- shivering
- skin rash
- sore throat
- sweating
- talking or acting with excitement you cannot control
- trembling or shaking
- unusual bruising
- unusual, incomplete, or sudden body or facial movements
- unusual secretion of milk (in females)
- weakness
Some side effects may occur that usually do not need medical attention. These side effects may go away during treatment as your body adjusts to the medicine. Also, your health care professional may be able to tell you about ways to prevent or reduce some of these side effects. Check with your health care professional if any of the following side effects continue or are bothersome or if you have any questions about them:
More common
- Change in sexual performance or desire
- constipation
- headache
- trouble sleeping
- unusual tiredness
Less common
- Change in sense of taste
- decreased appetite
- feeling of constant movement of self or surroundings
- frequent urination
- heartburn
- increased sweating
- stomach pain
- unusual weight gain or loss
Other side effects not listed may also occur in some patients. If you notice any other effects, check with your healthcare professional.
Call your doctor for medical advice about side effects. You may report side effects to the FDA at 1-800-FDA-1088.
Frequently asked questions
- SSRI’s vs SNRI’s - What's the difference between them?
- What are some common side effects of antidepressants?
- Can the antidepressant fluvoxamine (Luvox) be used to treat COVID-19?
View more FAQ
More about fluvoxamine
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (354)
- Drug images
- Side effects
- Dosage information
- During pregnancy
- Support group
- Drug class: selective serotonin reuptake inhibitors
- Breastfeeding
- En español
Patient resources
- Drug Information
- Fluvoxamine Tablets
- Fluvoxamine Extended-Release Capsules
Other brands
Luvox, Luvox CR
Professional resources
- Prescribing Information
Related treatment guides
- Body Dysmorphic Disorder
- Anxiety and Stress
- Anorexia/Feeding Problems
- Borderline Personality Disorder
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
Medical Disclaimer
How hormones make you gain weight - 4fresh blog
Elena and Anastasia Kostyukhin
The authors of the article. Nutritionists, founders of the GetHealth healthy lifestyle project
Have you tried everything but still can't lose weight? Maybe your hormones are to blame.
Steady accumulation of fat may be the result of hormonal imbalance. In this case, conventional diets and other recommendations no longer work, because they do not address the hormonal underlying causes, such as excess cortisol, low insulin and/or leptin sensitivity, estrogen imbalance, hypothyroidism (insufficiency of hormones produced by the thyroid gland). In fact, some hormonal imbalances can make losing weight completely impossible.
In this article, you will learn why hormonal imbalances can cause you to gain weight and how to deal with it. Let's figure it out.
And what about hormones?
Hormones are special molecules that act as intermediaries between different parts of your body. When they enter the bloodstream in response to specific stimuli, they are immediately transferred to certain target cells.
Targets for each hormone differ in the presence of specific, suitable receptors. The interaction between the hormone and the receptor sets off a cascade of biochemical reactions in the target cell that ultimately alters the function or activity of the cell.
Thus, hormones regulate complex processes, including growth, energy production, blood sugar, hunger and satiety, and metabolism.
1. Insulin
When it comes to weight loss, one of the most important hormones is insulin. It is produced by the pancreas and is known to regulate blood sugar levels, inhibit lipolysis (the breakdown of fats) and stimulate lipogenesis (the formation of fat stores).
Chronically high insulin levels can lead to insulin resistance. In this state, the cells lose their sensitivity to the hormone, and the pancreas has to produce more and more insulin in order to control blood sugar levels. However, this is getting harder and harder to do.
As a result, there comes a point when the level of sugar and insulin in the blood becomes steadily high. This leads to weight gain and a high risk of type 2 diabetes.
Many factors contribute to the development of insulin resistance. One of these is thought to be elevated levels of free fatty acids in the blood.
The main cause of high free fatty acids is eating too many calories and being overweight. In fact, overeating, weight gain, and obesity are strongly associated with insulin resistance.
Other potential causes of insulin resistance include:
- Frequent use of fructose as an added sugar (not from fruits).
- Oxidative stress: a consequence of chronic stress, smoking, drinking alcohol and "artificial" foods, contact with polluted environment, overtraining.
- Sedentary lifestyle, lack of activity.
- Gut microbiota: Disruption of the bacterial environment in the gut can cause inflammation, which exacerbates insulin resistance and other metabolic problems.
What can you do?
- When you eat a lot of sugar, fast food and processed carbohydrates (cakes, pastries), insulin goes out of whack. That is why the very first reasonable step is to minimize these foods in your diet.
- Eat a whole food diet. Be sure to include healthy fats: nuts, oily fish. If there are no contraindications, try intermittent fasting, for starters - 12:12 or 10:14.
- Add any physical activity to your schedule on a regular basis: walking, running, group or personal training, dancing, swimming, etc.
Preventing insulin resistance can be one of the most powerful ways to stay lean and live a much longer, healthier life.
2. Leptin
Fat secreted leptin controls appetite and helps you feel full. In simple terms, when leptin levels are balanced, you don't overeat.
Similar to insulin, chronically high leptin levels can cause leptin resistance. When the body becomes resistant to leptin, the brain no longer recognizes the signal of the hormone and mistakenly believes that you are hungry, even if in fact the body already has enough energy stored up.
Other possible causes of leptin resistance include chronic inflammation and increased levels of free fatty acids in the bloodstream.
For most people who struggle with leptin resistance, getting themselves to overcome the hunger signal caused by this condition is VERY difficult.
What can you do?
- Avoid processed foods: Highly processed foods can compromise intestinal integrity and cause inflammation. As we have said, inflammation is closely linked to the development of leptin resistance.
- Add soluble fiber: Eating soluble fiber can improve gut health and protect against obesity.
- Add Protein: Eating plenty of protein can help you lose weight.
- Exercise: Physical activity can help reverse leptin resistance.
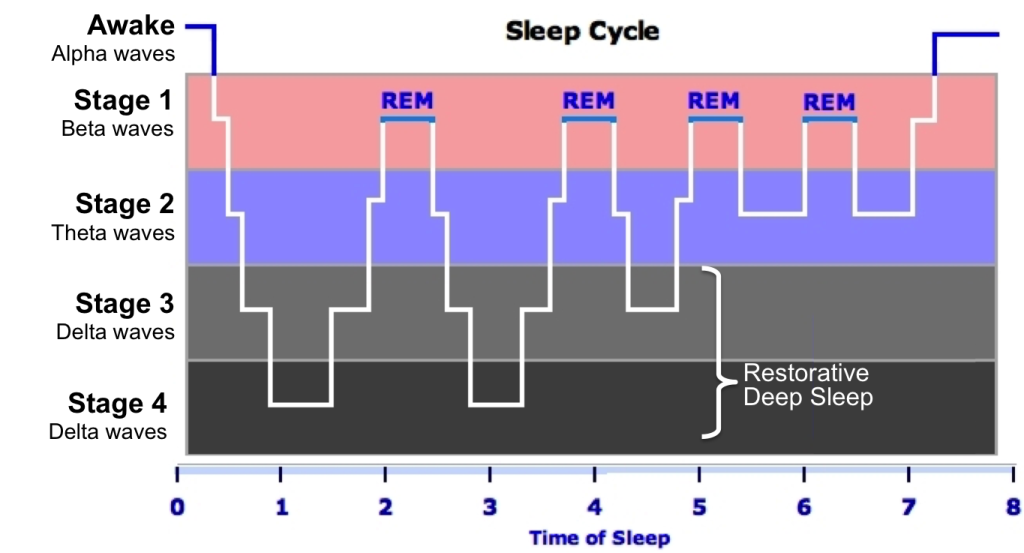
- Sleep: Lack of sleep is closely linked to the problem of disturbing normal leptin levels.
While there is no easy way to cure leptin resistance, you can make long-term lifestyle changes that will make a difference in how you feel right from the start.
3. Ghrelin
Ghrelin is a hormone produced in the intestines. It is often referred to as the hunger hormone because ghrelin's main function is to increase appetite. It is he who stimulates you to eat more and accumulate fats.
In addition, it affects your sleep/wake cycle, taste sensations, and carbohydrate metabolism.
Ghrelin is produced in the stomach and released when the stomach is empty. It enters the bloodstream and affects the part of the brain known as the hypothalamus, which regulates your hormones and appetite. The higher the level of ghrelin, the hungrier you become. That's why if you're looking to lose weight, lowering your ghrelin levels can be helpful.
Ghrelin levels usually rise before meals when your stomach is empty. It then declines shortly after the stomach is full.
No matter how much you weigh, ghrelin levels usually go up when you go on a diet. This is your body's natural reaction to trying to protect you from hunger and exhaustion.
During a strict diet, your appetite increases and levels of the "satiety hormone" leptin decrease. The metabolic rate also tends to drop significantly, especially if you restrict calories for an extended period of time.
For obvious reasons, this mechanism can make losing weight much more difficult.
What can you do?
Ghrelin seems to be a hormone that cannot be controlled. However, there are a few habits you can adopt to keep it healthy:
- Avoid extremes: both obesity and anorexia throw ghrelin out of balance.
- Get enough sleep, rest, do not allow a state of complete weakness.
- Gain muscle mass, do fitness.
- Eat more protein: Protein increases satiety and reduces hunger.
Protein Sources
- fish and seafood,
- meat and poultry,
- eggs,
- quinoa,
- nuts and seeds,
- legumes and lentils.
The best way to control ghrelin is with a sustainable healthy eating plan. Extreme diets and drastic calorie reduction can negatively impact hormone levels and interfere with normal function.
4. Cortisol
Cortisol is an important steroid hormone that belongs to a class of hormones called glucocorticoids. It is produced by the adrenal glands, located just above the kidneys.
In addition to helping with the stress response, other functions of cortisol include:
- increased blood sugar level;
- reduction of inflammation;
- suppression of the immune system;
- aid in nutrient metabolism.
Cortisol is usually released in close conjunction with your body's circadian rhythm, with 50-60% released after 30-40 minutes of being awake, and then cortisol levels drop throughout the day.
Cortisol is also released during times of stress. This prepares your body for a potentially dangerous situation. And while this reaction is normal, chronically high cortisol levels can lead to negative side effects:
What can you do?
While there can be many stressors in your life that can potentially increase your cortisol levels, there are several effective ways to manage your cortisol levels.
- Universal tip - be active and get enough sleep. Physical activity relieves tension and allows you to be more resilient to stress, while healthy sleep ensures quality recovery and hormonal balance.
- Try to eat mindfully. The Intuitive Eating concept involves total concentration on what and how you eat and how you feel while eating. The easiest way to start practicing mindful eating is to get rid of distractions* while eating. This will allow you to eat more slowly and mindfully, as well as better feel and recognize the signals of hunger and satiety.
* Examples of distractions: phone, TV, laptop, very loud music, book, conversations that distract from food, road (food on the run).
- Another potential tool for managing cortisol levels is meditation. You can start with a few minutes of measured deep breathing. While inhaling deeply, count the duration of the breath in seconds, pause at the top of the inhalation for the same number of seconds that you inhaled, and exhale for the same number of seconds. Repeat this cycle a couple of times, and if breathing allows, gradually increase the time of inhalation, retention and exhalation, maintaining a ratio of 1:1:1.
For example: inhale - mentally count to 5, hold - again count to 5, exhale - and again 5 counts. Do at least 5-7 reps.
You can also use any practice that has a relaxing effect on you: a massage, a spa, talking to a loved one, reading, listening to a favorite artist's album, or a walk in the park.
Conclusion and general recommendations
To get a complete picture of your hormonal health, we strongly recommend that you see your doctor. You will need to take a consultation and pass comprehensive tests. In addition to the indicators disclosed in the article, it will also be useful to immediately pass biochemical analysis, female profile (hormones) and thyroid profile. This will help you avoid wrong decisions about the true cause of weight gain and protect yourself from additional danger.
The general recommendations in this article may be useful as a preventative measure.
Sources
Instagram GetHealth
-
#Vitamins
-
#Health
Subscription
Useful newsletters in your mail. It remains only to subscribe
Data processing when subscribing
Read on topic
Nutrition
9 gluten-free cereals in the diet
vitamins
Skin problems: when is it time to see an endocrinologist?
Sport
Your own massager: 9 devices for home massage
Trends
Catch Zen: 5 Meditation Apps
Five Surprising Factors Affecting Your Weight
- Kersty Brewer
- BBC
Subscribe to our Newsletter “Context”
Image caption, Jackie (left) and Gillian are twins but have very different body mass indexes. Here are five unexpected factors that may be affecting your weight.
1. Gut microbiome
Gillian and Jackie are twins, but one weighs 41 kg more than the other.
Professor Tim Spector has been following their development for 25 years as part of the UK's nationwide twin program. He believes that the difference in their weight is due to tiny microorganisms - microbes that live in our intestines.
"Every time you eat something, you feed hundreds of trillions of microbes. You never eat alone," he explains.
Stool samples taken from each of the sisters revealed that the thinner Gillian had a very diverse gut flora, while Jackie had very few gut microbes.
- Kefir improves intestinal microflora. Scientific evidence
- British scientists have found a possible cause of obesity in adolescents
- Scientists: obesity contributes to the development of 11 types of cancer
could be," says Professor Spector, who bases his findings on a study of five thousand people.
Image copyright, Science Photo Library
Image caption,Human gut bacteria
To diversify your microbiome, you need to eat a healthy and varied diet rich in various types of fiber.
As the professor points out, most Britons consume only half the required amount of fiber.
Healthy fiber sources:
- bran cereal
- fruits, including berries and pears
- vegetables, such as broccoli and carrots
- beans
- pulses
- nuts
Podcast
What was that?
We quickly, simply and clearly explain what happened, why it is important and what will happen next.
episodes
The End of the Story Podcast
Why do some people follow a strict diet, exercise regularly, and still fail to lose weight, while others do very little and yet remain in good shape?
Scientists at the University of Cambridge believe that about 40-70% of our weight depends on the set of genes that we inherited from our parents.
"It's a lottery," admits Prof. Sadaf Farooqi. "It's now very clear that genes affect our weight, and if you have a defect in certain genes, that might be enough to make you fat."
These specific genes can influence appetite, portion size, and even what kind of food a person prefers. Genes also determine how we burn calories and whether our body is able to distribute fat efficiently.
There are at least 100 genes that affect weight, including the MC4R gene, which controls hunger and appetite.
Experts believe that one person in every thousand has a defective variant of the MC4R gene, which means that its owners tend to be hungrier and crave more fatty foods.
"You can't do anything about your genes, but some people will benefit from knowing that their genes increase their chances of getting fat. Knowing this, they can change their diet and exercise," says Professor Farooqi.
3.
There is some truth in the old saying, "Eat breakfast yourself, share lunch with a friend, and give dinner to an enemy", but not in the way you might think.
Obesity expert Dr. James Brown says that the later we eat, the more likely we are to gain weight. And not because we are less active at night, as many people think, but because of our internal clock.
"Our bodies are wired to handle calories most efficiently during the day when it's light, not at night when it's dark," he explains.
This is the reason why people who work shifts or work different hours may find it harder not to gain weight.
At night, our body hardly digests fats and sugars, so it is better to eat something high-calorie before seven in the evening if you want to lose weight or not gain weight.
Image copyright, Getty Images
Image caption,Eggs for breakfast are good!
Over the past ten years, the national average for dinner in the UK has moved from 5:00 pm to around 8:00 pm, and this has also contributed to more overweight people, Dr. Brown points out.
But even with today's pace of life, and no matter what hours you work, there are things you can control to be in good shape.
According to Dr. Brown's rules, you can't skip breakfast or eat just one slice of toasted bread in the morning.
For breakfast, eat something that contains protein, some fat and carbohydrates, such as eggs and a piece of wholemeal bread. This way you will feel full longer.
This should be followed by a substantial, nutritious lunch and a lighter supper.
4. How to trick your brain
Image credit: Getty Images calories.
Behavioral scientist Hugo Harper offers several ways to subconsciously change your eating habits so you don't count calories all the time.
For example, it would be more effective not to rely on your own willpower, but simply to remove something from your field of vision that whets your appetite.
Therefore, do not lay out unhealthy snacks in plain sight, rather put a bowl of fruit or something healthy there.
Do not sit in front of the TV with a pack of cookies - put as many cookies on the saucer as you are going to eat (maximum - two), and with this amount go to the living room.
Dr. Harper also advises to replace rather than cancel something completely, especially if you love it - just choose a low-calorie option.
For example, drink low-calorie carbonated drinks. Or reduce your serving size. This will be more effective than trying, for example, to completely get rid of the habit of drinking tea with chocolate chip cookies.
Image copyright, Getty Images
Image caption,Be patient, Bobik, and the donut will be yours!
"People tend not to notice the difference if their portion is reduced by 5-10%," says Harper.
In addition, people often eat automatically without even thinking about what they are eating, so if you use a smaller plate or follow the recipe on the package, this will prevent mindless absorption of calories.