Does alcohol help with pain
Using Alcohol to Relieve Your Pain: What Are the Risks?
People have used alcohol to relieve pain since ancient times. Laboratory studies confirm that alcohol does indeed reduce pain in humans and in animals. Moreover, recent research suggests that as many as 28 percent of people experiencing chronic pain turn to alcohol to alleviate their suffering. Despite this, using alcohol to alleviate pain places people at risk for a number of harmful health consequences.
What are the risks?
Mixing alcohol and pain medicines can be harmful
-
Mixing alcohol and acetaminophen can cause acute liver failure
-
Mixing alcohol and aspirin increases risk for gastric bleeding
-
Alcohol increases analgesic, reinforcing, and sedative effects of opiates, elevating risk for combined misuse of alcohol and opiates as well as overdose.
If you’re taking medications to manage your pain, talk to your doctor or pharmacist about any reactions that may result from mixing them with alcohol.
Analgesic doses of alcohol exceed levels recommended in the Dietary Guidelines for Americans, 2020-2025
-
According to the Dietary Guidelines for Americans, 2020–2025, if alcohol is consumed, intake should be limited to 1 drink or less in a day for women and 2 drinks or less in a day for men. The greatest pain-reducing effects occur when alcohol is consumed at doses exceeding these guidelines.
-
Tolerance develops to alcohol’s analgesic effects so that it takes more alcohol to produce the same effects. Increasing alcohol use to stay ahead of tolerance can lead to other problems, including the development of alcohol dependence.
Chronic alcohol drinking makes pain worse
-
Withdrawal from chronic alcohol use often increases pain sensitivity which could motivate some people to continue drinking or even increase their drinking to reverse withdrawal-related increases in pain.
-
Over time, alcohol misuse generates a painful small fiber peripheral neuropathy, the most common neurologic complication associated with alcohol use disorder.

If you use alcohol to relieve your pain, it is important to learn about possible adverse health effects.
References
U.S. Department of Health and Human Services and U.S. Department of Agriculture. Dietary Guidelines for Americans, 2020–2025. 9th ed. Washington, DC: U.S. Government Printing Office, 2020, p. 29. Available at https://www.dietaryguidelines.gov/sites/default/files/2020-12/Dietary_Guidelines_for_Americans_2020-2025.pdf. Accessed January 6, 2021.
Brennan, P.L.; Schutte, K.K.; and Moos, R.H. Pain and use of alcohol to manage pain: Prevalence and 3-year outcomes among older problem and non-problem drinkers. Addiction 100:777–786, 2005.
Riley III, J.L., and King, C. Self-report of alcohol use for pain in a multi-ethnic community sample. Journal of Pain 10:944–952, 2009.
Pain Killer or Pain Causer?
All TreatmentsDrugs & Medications
Some people find that having a few drinks helps ease chronic pain.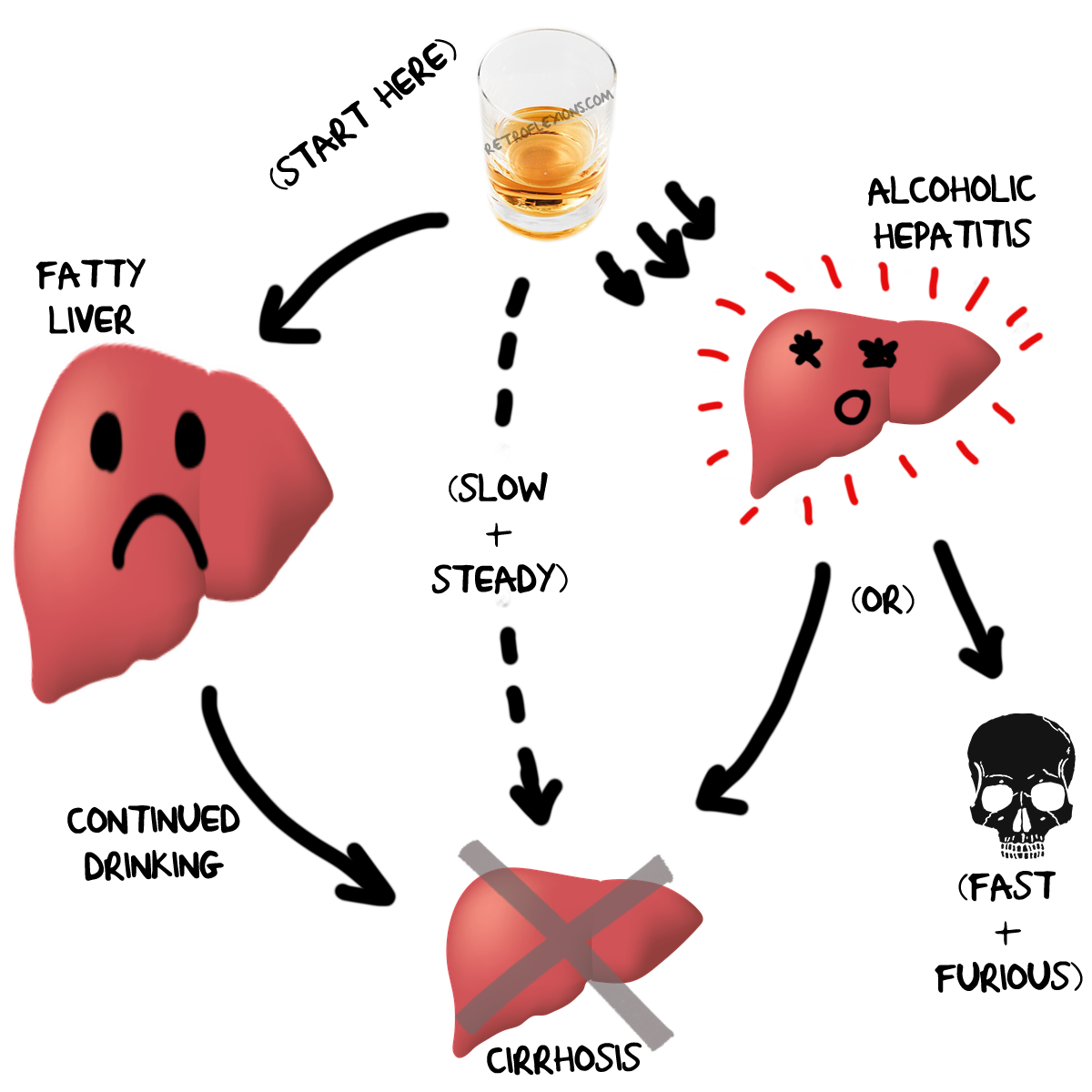 Others have good reason to abstain.
Others have good reason to abstain.
Susan McQuillan, MS, RDN, CDN
Registered Dietitian
If you have a glass of wine or a cocktail or two most nights to cope with chronic pain (eg, back pain), you may be on to something. Research studies have found that moderate use of alcohol does, in fact, relieve pain for many people, and those who routinely drink reasonable amounts of alcohol reportedly cope better with pain and disability than those who don’t drink at all. That makes sense, because alcohol is an analgesic and anesthetic and as such, can reduce the sensation of both physical and emotional pain.
Alcohol is an analgesic and anesthetic and as such, can reduce the sensation of both physical and emotional pain. Photo Source: 123RF.com.
Although research has not yet shown that alcohol reduces inflammation specifically associated with chronic pain, studies have shown that moderate drinking reduces inflammation in the body that leads to cardiovascular disease.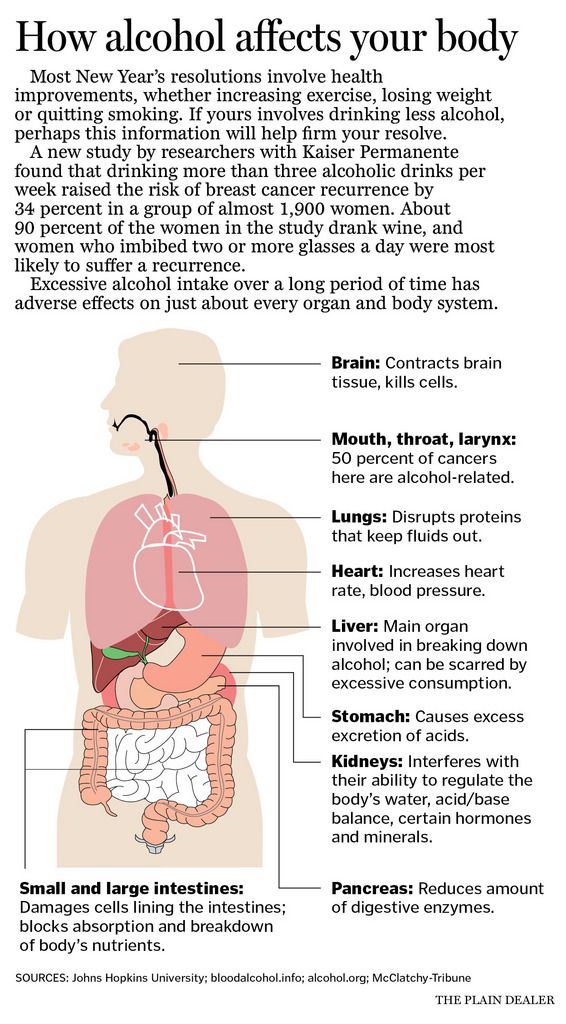 Other studies have shown that, compared to nondrinkers and heavy drinkers, those who consume light to moderate amounts of alcoholic beverages, including beer and wine, have reduced markers of inflammation throughout the body, and that this reduction may be due directly to the ethanol content of the alcoholic beverages consumed.
Other studies have shown that, compared to nondrinkers and heavy drinkers, those who consume light to moderate amounts of alcoholic beverages, including beer and wine, have reduced markers of inflammation throughout the body, and that this reduction may be due directly to the ethanol content of the alcoholic beverages consumed.
According to the Centers for Disease Control and the U.S. Dietary Guidelines, moderate drinking is defined as up to one drink a day for women and up to 2 drinks a day for men. Unfortunately, not everyone who drinks alcohol does so in moderation, and for some people, alcohol, even in small doses, carries big risks to health and well-being.
Some people who drink alcohol to cope with pain were heavy drinkers before they had a chronic condition. Others became more dependent on alcohol after developing a painful disease or disability, suggesting that chronic pain can put some people at risk of alcohol abuse and addiction. Studies have found that when people who are in recovery from alcohol addiction suffer from chronic pain, they have a significantly higher rate of relapse than those who don’t have chronic medical conditions.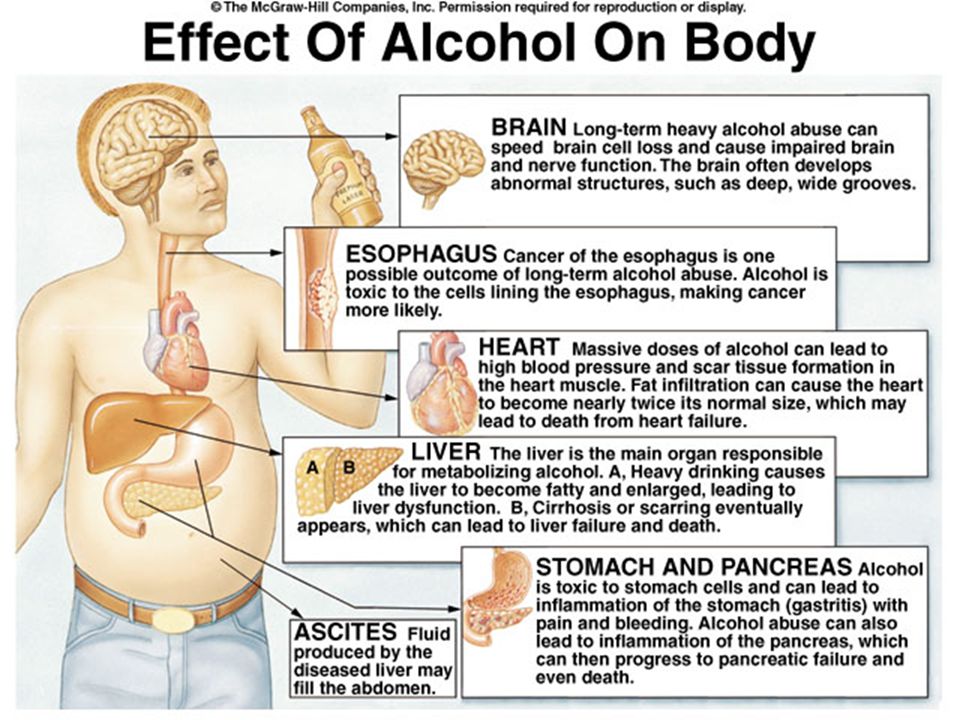
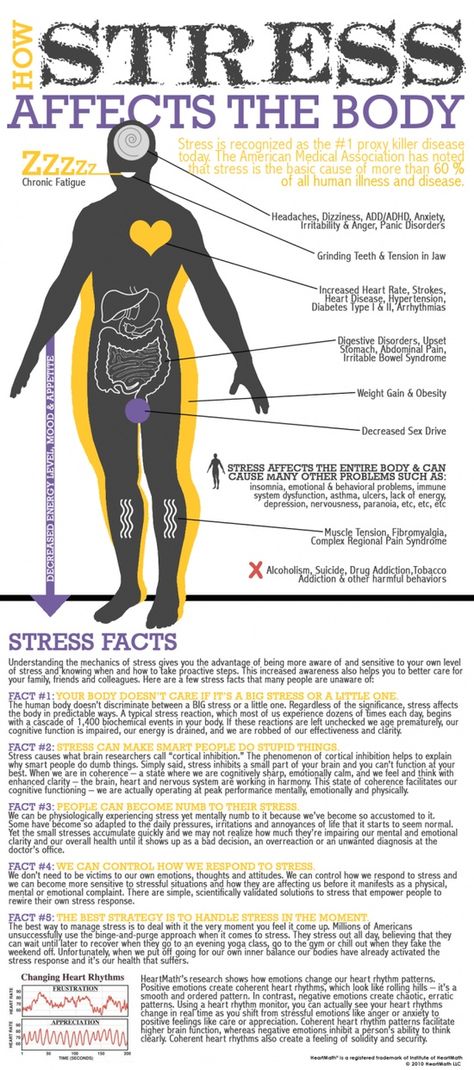
For many people, excessive drinking can lead to even more pain and other health complications. For instance, chronic alcoholism is linked to peripheral neuropathy, or damage to peripheral nerves that causes stabbing pain and numbness in your hands and feet, and interferes with your central nervous system’s ability to send signals from your brain and spinal cord to the rest of your body.
Pain can lead people to drink more alcohol than they might otherwise consume, and researchers have found the most pain relief comes from drinking amounts that are well above general guidelines for moderate use. But even if you stick to the guidelines for drinking in moderation, routine use of alcohol could still be harmful to your health, especially if you are also taking pain medication. This is as true for aspirin and other over-the-counter drugs used to treat inflammatory pain as it is for stronger prescription medications. Over time, combining alcohol with aspirin can cause bleeding in the stomach and combining alcohol with acetaminophen can cause acute liver failure.
The bottom line? Speak with your doctor if you regularly drink alcoholic beverages to relieve or cope with pain. That way you’ll be sure the amount you drink can safely be combined with any medications you take and that, overall, the benefits of drinking outweigh any risk of side effects that could cause more damage and pain in your body.
Zale EL, Maisto SA, Ditre JW. Interrelations between pain and alcohol. Clinical Psychology Review. April 2015;37:57-71. http://www.sciencedirect.com/science/article/pii/S0272735815000367 Accessed November 7, 2017.
Apkarian AV, Neugebauer V, Koob G, et al. Neural mechanism of pain and alcohol dependence. Pharmacology Biochemisry and Behavior. November 2013;112:34-41.
Witkiewitz K, Vowles KE, McCallion E, et al. Pain as a predictor of heavy drinking lapses in the COMBINE study and the UK Alcohol Treatment Trial. Addiction. August 2015;110(8):1262-1271.http://onlinelibrary.wiley.com/doi/10.1111/add.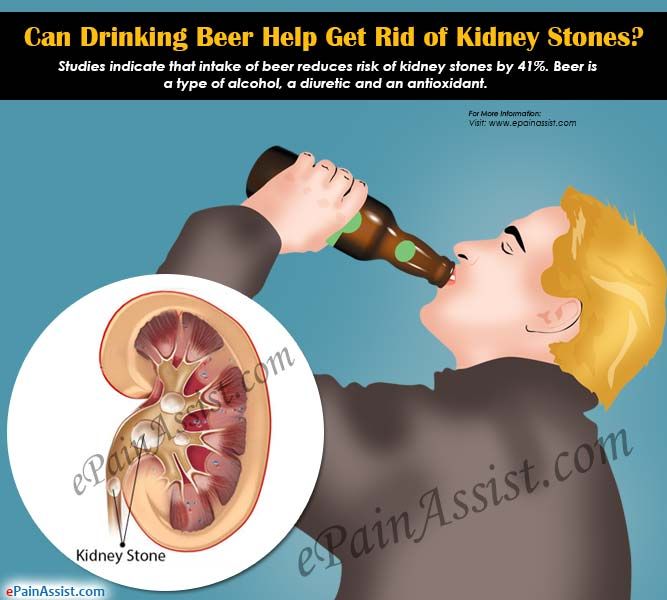 12964/full Accessed November 7, 2017.
12964/full Accessed November 7, 2017.
Imhof A, Woodward M, Doering N, et al. Overall alcohol intake, beer, wine, and systemic markers of inflammation in western Europe: results from three MONICA samples (Augsburg, Glasgow, Lille). European Heart Journal. December 2004;25(23):2092-2100.
Centers for Disease Control. Alcohol and Public Health. Updated July 25, 2017.https://www.cdc.gov/alcohol/fact-sheets/moderate-drinking.htm Accessed November 7, 2017.
NIH/National Institute on Alcohol Abuse and Alcoholism. Using alcohol to relieve your pain: What are the risks? Updated July 2013.https://pubs.niaaa.nih.gov/publications/PainFactsheet/Painalcohol.pdf Accessed November 7, 2017.
Notes: This article was originally published November 7, 2017 and most recently updated December 18, 2018.
Susan McQuillan, MS, RDN, CDN Registered Dietitian
Susan McQuillan, MS, RDN, CDN, has contributed diet, nutrition, lifestyle, and general health articles to web sites such as QualityHealth. com, PsychologyToday.com blogs, CalorieLab.com and to magazines such as Parent & Child, A&P Supermarket’s Easy Solutions, Natural Health, Santé, the Magazine for Restaurant Professionals, ADDitude, Woman’s Day, Prevention, Family Circle, Cooking Light, Fitness, McCalls, Women’s Sports & Fitness, Fit Pregnancy, Living Fit, BabyTalk, Shape Cooks and Country Cooking.
com, PsychologyToday.com blogs, CalorieLab.com and to magazines such as Parent & Child, A&P Supermarket’s Easy Solutions, Natural Health, Santé, the Magazine for Restaurant Professionals, ADDitude, Woman’s Day, Prevention, Family Circle, Cooking Light, Fitness, McCalls, Women’s Sports & Fitness, Fit Pregnancy, Living Fit, BabyTalk, Shape Cooks and Country Cooking.
Scientists told which alcohol "saves" headaches better than pills - news on UNN
News: Society
ArchiveAugust 20, 2020, 13:55 • Irina Makarenko • 293880
Kyiv. August 19. UNN. Relieve headaches with a couple of beers. This conclusion was reached by scientists from the University of Greenwich in London.
Claimed to be scientifically proven to relieve the drink. nine0003
Thus, the researchers took into account the data obtained during the 18 experiments. In total, more than 400 volunteers took part in the study - the results were very unexpected.
So, it turned out that two glasses of the mentioned drink cope with a headache more effectively than paracetamol.
READ ALSO: Brown-eyed vs blue-eyed: scientists told who is more susceptible to alcohol.
"The results suggest that alcohol is an effective pain reliever that provides clinically significant underestimations of pain intensity," the scientists said. nine0003
Earlier, scientists from Canada stated that wine can help the human body defend itself against coronavirus, and scientists from the United States came to the conclusion that red wine helps fight mental disorders.
Experts from the University of Washington Medical School, in turn, stated that wine is also able to "protect" eyesight. In all cases, we are talking exclusively about moderate consumption of the drink.
As reported in UNN, in Ukraine, the State Statistics Service recorded an increase in the popularity of domestic wine. Its Ukrainians began to buy in stores more often than imported. nine0003
Let's clarify that the 5 most famous Ukrainian wine brands today are as follows: "Koblevo", "Shabo", Koktebel, Inkerman and Oreanda.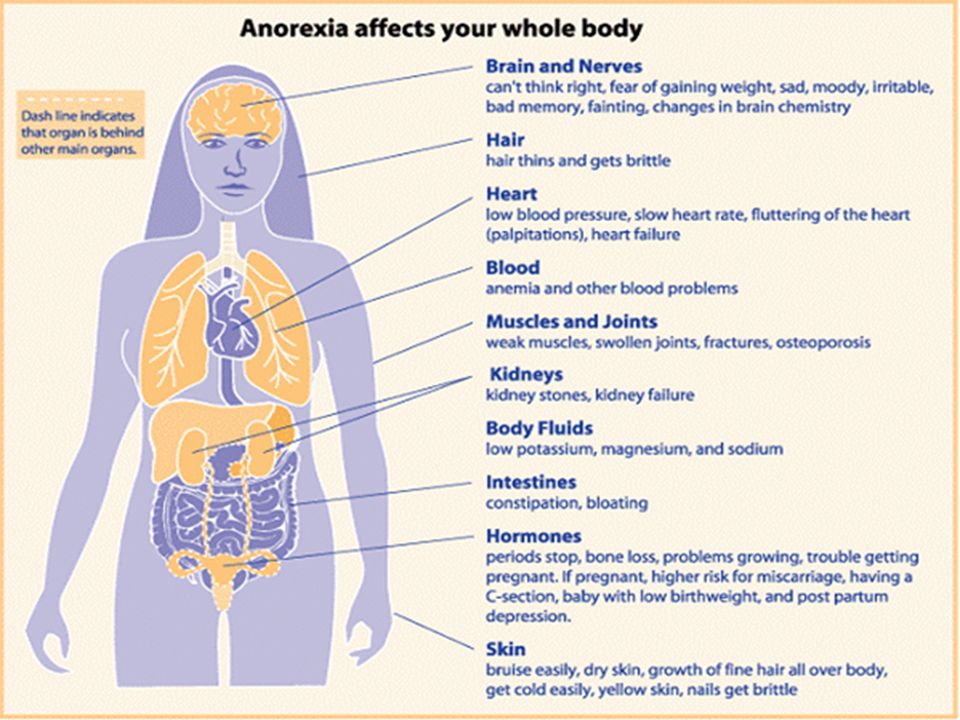
Source: UNN
Tags: pain, alcohol, research
Subscribe to the UNN news channel in Telegram
Latest news of the section
Saturday, December 17, 2022
- 17:54
The main Christmas tree of the country shone in Kyiv. While in test mode
- 17:11
Underground and on generators: National selection for Eurovision 2023 started in Ukraine
- 16:42
The woman who was released during the exchange has her sons returned. The guys were kept in the occupied territory and in the Russian Federation
- 15:40
Dictionary.com has chosen the word of the year - "woman"
- 13:52
Brovary was left without water supply and heat - mayor
Related news
Friday, August 21, 2020
- 13:52
The Armed Forces of Ukraine decided to abandon the 120-millimeter Molot mortars
- 13:35
In Donbas militants are increasing the combat effectiveness of army corps - intelligence
- 13:21
JFO: since the beginning of the day, no shelling by militants was recorded
- 13:08
"The city of the revival of shipbuilders": Zelensky came up with a "brand epithet" for Nikolaev
- 13:07
UAH 92 million allocated from the capital budget for payments on Independence Day
Alcohol and pain - Neurology — LiveJournal
?Previous Entry | Next Entry
In the mechanisms of action of alcohol (ethyl alcohol) there are several aspects that are undoubtedly reflected in the occurrence and change of pain. First of all, this is the similarity of the action of alcohol and endorphins (due to which neural networks and synapses perceive alcohol as an endorphin). Alcohol in small doses, like endorphins, has a psychostimulating effect, which is accompanied by a feeling of increased physical activity, an increase in mood with a touch of pleasure - euphoria. The psychostimulating effect of alcohol is due to complex neurophysiological changes in neurotransmitter and neuromodulatory mechanisms. The most pronounced response to alcohol intake is noted in the following neurotransmitter systems: dopamine, glutamate, GABA, endogenous opioids (endorphin and enkephalin). The last three systems are widely represented in the brain, and therefore the effect of alcohol is of a pronounced general nature. The listed neurotransmitter systems are responsible for the organization of neuronal activity, regulation of mood, attention, memory, learning, the level (quality) of cognitive processes and the threshold of pain sensitivity.
First of all, this is the similarity of the action of alcohol and endorphins (due to which neural networks and synapses perceive alcohol as an endorphin). Alcohol in small doses, like endorphins, has a psychostimulating effect, which is accompanied by a feeling of increased physical activity, an increase in mood with a touch of pleasure - euphoria. The psychostimulating effect of alcohol is due to complex neurophysiological changes in neurotransmitter and neuromodulatory mechanisms. The most pronounced response to alcohol intake is noted in the following neurotransmitter systems: dopamine, glutamate, GABA, endogenous opioids (endorphin and enkephalin). The last three systems are widely represented in the brain, and therefore the effect of alcohol is of a pronounced general nature. The listed neurotransmitter systems are responsible for the organization of neuronal activity, regulation of mood, attention, memory, learning, the level (quality) of cognitive processes and the threshold of pain sensitivity. It is important to note that the psychostimulating effect of alcohol is accompanied by an increase in the threshold of pain sensitivity. That is why, against the background of intoxication, damage to the body can be perceived as insignificant or not registered at all by the subject until the effect of alcohol passes and the basic level of pain thresholds is restored. However, more often after the removal of alcohol from the body, a decrease in pain sensitivity thresholds is observed due to depletion or feedback inhibition of the synthesis of neurotransmitters and an increase in the activity of their capture and resorption. As a result, there is a pathophysiological basis for acute pain syndromes typical of the post-alcohol period. nine0002 Today, the idea of the mechanisms of information transfer through synaptic structures has been supplemented by the idea of information transfer using the method of interneuronal interaction through extrasynaptic receptors. In some parts of the brain, the density of receptor structures outside the classical synapse can be significantly higher than in the synapse itself (70% of dopaminergic axon varicose veins are asynaptic and are capable of actively releasing the neurotransmitter).
It is important to note that the psychostimulating effect of alcohol is accompanied by an increase in the threshold of pain sensitivity. That is why, against the background of intoxication, damage to the body can be perceived as insignificant or not registered at all by the subject until the effect of alcohol passes and the basic level of pain thresholds is restored. However, more often after the removal of alcohol from the body, a decrease in pain sensitivity thresholds is observed due to depletion or feedback inhibition of the synthesis of neurotransmitters and an increase in the activity of their capture and resorption. As a result, there is a pathophysiological basis for acute pain syndromes typical of the post-alcohol period. nine0002 Today, the idea of the mechanisms of information transfer through synaptic structures has been supplemented by the idea of information transfer using the method of interneuronal interaction through extrasynaptic receptors. In some parts of the brain, the density of receptor structures outside the classical synapse can be significantly higher than in the synapse itself (70% of dopaminergic axon varicose veins are asynaptic and are capable of actively releasing the neurotransmitter).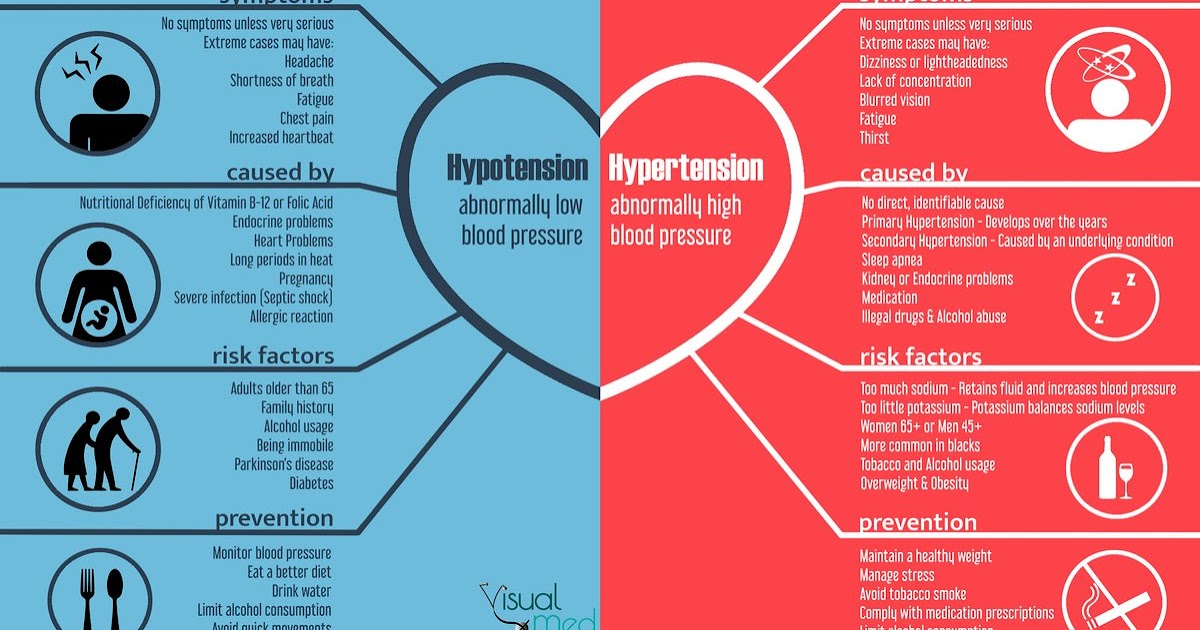 Consequently, various mediator compounds can enter the intercellular environment, which means that complex relationships between mediators arise at the extrasynaptic level, and this ensures flexible, highly plastic work of neuron patterns. The entry into the intercellular environment of alcohol, which is perceived as endorphin, and an increase or decrease in its concentration changes the relationship of the extrasynaptic level and contributes to a change in pain sensitivity thresholds and the appearance or suppression of pain. nine0003
Consequently, various mediator compounds can enter the intercellular environment, which means that complex relationships between mediators arise at the extrasynaptic level, and this ensures flexible, highly plastic work of neuron patterns. The entry into the intercellular environment of alcohol, which is perceived as endorphin, and an increase or decrease in its concentration changes the relationship of the extrasynaptic level and contributes to a change in pain sensitivity thresholds and the appearance or suppression of pain. nine0003
An independent link in the pathogenesis of pain in alcohol addicts is the effect of alcohol on the state of receptors in various structures of the nervous system. The study of the dynamics of the activity of dopamine D2 receptors using X-ray contrast methods has established that after repeated administration of alcohol, a pronounced depletion of dopamine D2 receptors is recorded. The level of exhaustion corresponds to the critical level and affects the ability to receive pleasure and reward. Undoubtedly, the depletion of dopamine receptors affects the entire cascade of neurotransmitter dynamics and pain thresholds. The ability to receive pleasure and increase pain thresholds in such depletion are restored with the introduction of alcohol or after a long period of rehabilitation and restoration of the activity of dopamine D2 receptors. nine0003
Undoubtedly, the depletion of dopamine receptors affects the entire cascade of neurotransmitter dynamics and pain thresholds. The ability to receive pleasure and increase pain thresholds in such depletion are restored with the introduction of alcohol or after a long period of rehabilitation and restoration of the activity of dopamine D2 receptors. nine0003
Glial cells are actively involved in the formation of pain. It turned out that they have their own analgesic potential. A study (Whitten L., 2008) of patients with alcohol dependence and pain syndromes found that inhibition of glial cells led to a decrease in pain intensity. Conversely, their activation increased the pain. From this, the author concluded that glia is involved in the formation of neuropathic pain, typical of alcoholic polyneuropathies. This study, extended to the use of opioids, found that increased glial activity reduced the analgesic effects of opiates. The presented data gave reason to believe that, on the one hand, glial cells are involved in the formation of tolerance to opioids, and on the other hand, these data explain the ineffectiveness of opioids in neuropathic pain.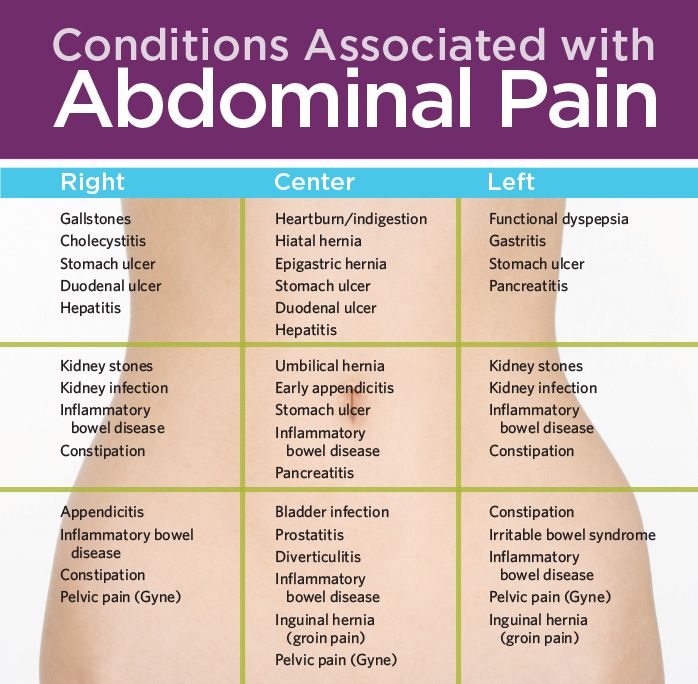 If these data are extrapolated to the effect of alcohol on glial cells, it becomes clear why in the later stages of alcoholism complicated by polyneuropathies, alcohol does not alleviate neuropathic pain. nine0003
If these data are extrapolated to the effect of alcohol on glial cells, it becomes clear why in the later stages of alcoholism complicated by polyneuropathies, alcohol does not alleviate neuropathic pain. nine0003
The effect of alcohol on pain is closely related to biorhythms. For example, for the relief of pain at night, a significantly larger amount of analgesics is required. The same dynamics of the analgesic effect is characteristic of alcohol. Diurnal fluctuations also affect the resistance to the toxic effects of alcohol, it decreases at night.
In the pathogenesis of pain in the post-alcoholic period, there is also a contribution from inflammatory processes caused by the general toxic and vascular effects of alcohol. Alcohol in the body is oxidized to acetaldehyde due to the activity of alcohol dehydrogenase and alcohol oxidase (further, acetaldehyde is oxidized by aldehyde dehydrogenase to acetate, which is then included in the citrate cycle with the formation of macroergic bonds).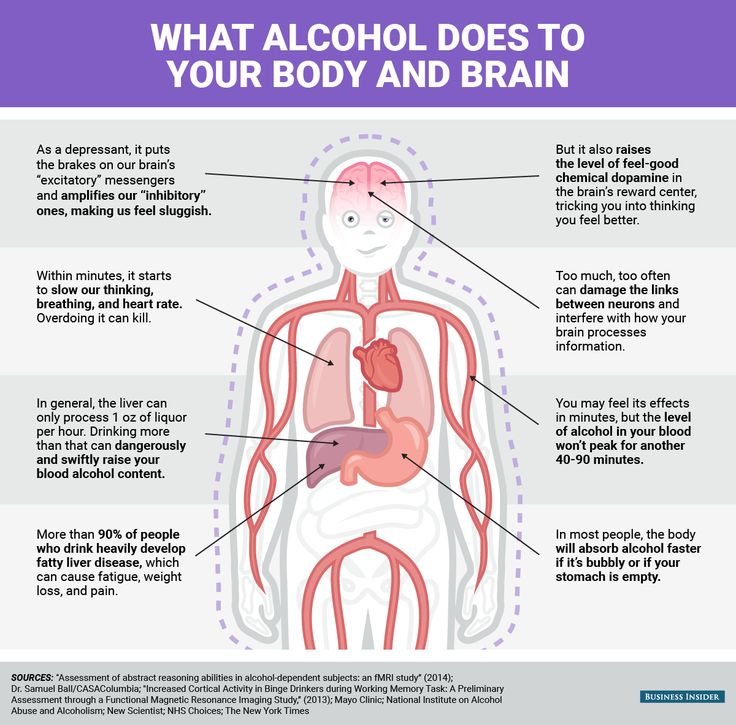 Acetaldehyde is highly toxic, as it is involved in free radical damage to cell membranes and cell microstructures, it can cause brain edema, neuronal death, and damage to the blood-brain barrier. These mechanisms are clearly reflected in the clinic of acute alcohol poisoning, which is accompanied by intense headache without a clear localization. A throbbing or pressing headache often occurs after drinking small amounts of alcohol in individuals who drink it infrequently. With the systematic use of moderate doses of alcohol, there are often complaints of diffuse dull headache, combined with a violation of the autonomic balance and general vascular symptoms. An independent complex of pain disorders occurs in patients with alcoholism in the structure of the withdrawal syndrome and in the event of somatic diseases of alcoholic origin. In such observations, a combination of acute pain syndromes and chronic pain syndromes with different localization is possible. nine0003
Acetaldehyde is highly toxic, as it is involved in free radical damage to cell membranes and cell microstructures, it can cause brain edema, neuronal death, and damage to the blood-brain barrier. These mechanisms are clearly reflected in the clinic of acute alcohol poisoning, which is accompanied by intense headache without a clear localization. A throbbing or pressing headache often occurs after drinking small amounts of alcohol in individuals who drink it infrequently. With the systematic use of moderate doses of alcohol, there are often complaints of diffuse dull headache, combined with a violation of the autonomic balance and general vascular symptoms. An independent complex of pain disorders occurs in patients with alcoholism in the structure of the withdrawal syndrome and in the event of somatic diseases of alcoholic origin. In such observations, a combination of acute pain syndromes and chronic pain syndromes with different localization is possible. nine0003
Self-contributing to the relationship between alcohol and pain are mood disorders that occur within alcohol dependence (which is replete with affective disorders such as anxiety and/or depressive disorder).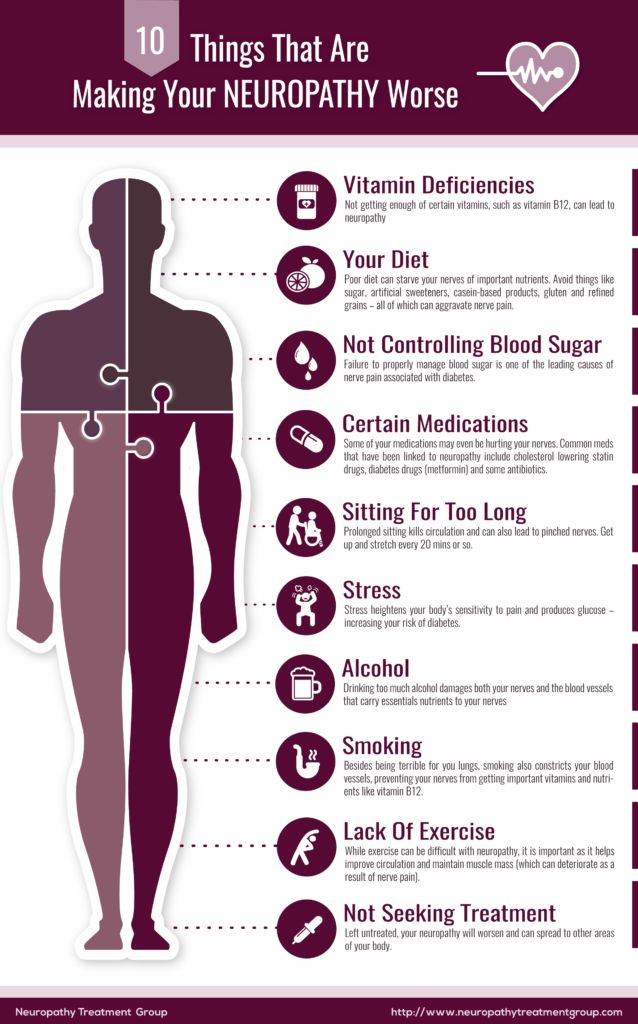 Studies of the pathogenetic mechanisms of depression and chronic pain have established the presence of common links in the pathogenesis of these conditions (this is reflected in the fact that the depression clinic is replete with various algic phenomena, and chronic pain is necessarily complicated by anxiety and depressive syndromes). The increase in the prevalence of chronic pain in depression and anxiety (and depression and anxiety in chronic pain) is associated with biochemical characteristics that have common links for all types of disorders. These include involvement of the serotonergic and noradrenergic systems and hypercortisolemia. Most often, pain disorders occur in depression caused by exhaustion and impaired noradrenergic transmission. With alcoholism, depletion of almost all neurotransmitter systems gradually develops, both due to the direct influence of chronic alcohol consumption, and due to the development of systemic disorders and secondary shifts in associated neurotransmitter systems.
Studies of the pathogenetic mechanisms of depression and chronic pain have established the presence of common links in the pathogenesis of these conditions (this is reflected in the fact that the depression clinic is replete with various algic phenomena, and chronic pain is necessarily complicated by anxiety and depressive syndromes). The increase in the prevalence of chronic pain in depression and anxiety (and depression and anxiety in chronic pain) is associated with biochemical characteristics that have common links for all types of disorders. These include involvement of the serotonergic and noradrenergic systems and hypercortisolemia. Most often, pain disorders occur in depression caused by exhaustion and impaired noradrenergic transmission. With alcoholism, depletion of almost all neurotransmitter systems gradually develops, both due to the direct influence of chronic alcohol consumption, and due to the development of systemic disorders and secondary shifts in associated neurotransmitter systems.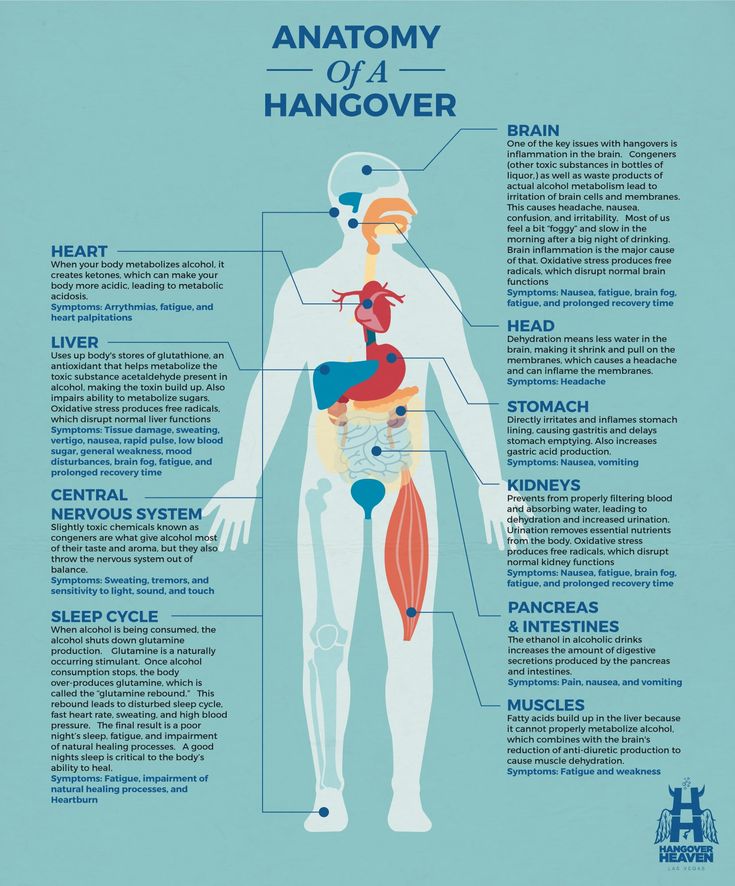 nine0003
nine0003
You can read more about the effect of alcohol on pain in the article "Alcohol and Pain" by N.P. Vanchakova, St. Petersburg State Medical University (Human Ecology magazine 2010.04) [Read]
© Laesus de Liro
TAGS:
Dear authors of scientific materials that I use in my messages! If you see this as a violation of the “Copyright Law of the Russian Federation” or wish to see the presentation of your material in a different form (or in a different context), then in this case write to me (at the postal address: [email protected]) and I will immediately I will eliminate all violations and inaccuracies. But since my blog has no commercial purpose (and basis) [for me personally], but has a purely educational purpose (and, as a rule, always has an active link to the author and his scientific work), so I would be grateful to you for the chance make some exceptions for my messages (against existing legal regulations). Sincerely, Laesus De Liro. nine0003
Sincerely, Laesus De Liro. nine0003
-
Innervation (sensory) of the knee joint
Knowledge of the innervation of the knee joint is becoming increasingly important due to the recently gaining popularity of treatment methods ...
-
Nikolaou syndrome
NEUROLOGIST'S HANDBOOK The main tool and effective means of symptomatic and pathogenetic therapy of pain syndrome are…
-
nociplastic pain
The IASP (International Association for the Study of Pain) defines pain as an unpleasant sensory and emotional experience that…
-
Coccygodynia (pain in the coccyx)
.
 .. these patients are “real sufferers” - clients of psychiatrists, hypnotherapists, psychics, healers (according to the figurative expression of G.I. Ivanichev ...
.. these patients are “real sufferers” - clients of psychiatrists, hypnotherapists, psychics, healers (according to the figurative expression of G.I. Ivanichev ... -
Neurostimulation in the treatment of pain syndromes
nine0002 ... I liked it when in winter, after severe frosts and snowfalls, a thaw came, it rained, and then frosts returned, and our ... -
stomalgia nine0122
… pain in the face or mouth is the most common complaint in dental and neurological practice.
 Stomalgia (SA) - chronically ...
Stomalgia (SA) - chronically ... -
angina pectoris nine0122
CLINICAL PHENOMENOLOGY OF ANGINA PAIN SYNDROME
-
Spinal osteomyelitis nine0122
SPONDYLITIS and SPONDYLODISCITIS [read] (or download) the article in PDF format The relevance of the problem of "spondylodiscitis" is determined by .

Learn more