Do mood stabilizers help with depression
Mood Stabilizing Medications | CAMH
Overview
Mood stabilizers are medications used in the treatment of bipolar disorder, where a person’s mood changes from a depressed feeling to a high “manic” feeling or vice versa. These drugs can help reduce mood swings and prevent manic and depressive episodes.
Mood stabilizers can take up to several weeks to reach their full effect. Because of this, other psychiatric medications such as antipsychotics; are often used in the early stages of treatment to treat acute mania.
Depression in bipolar disorder can be hard to distinguish from other forms of depression. Antidepressant medications can be effective; however, they must never be used alone with bipolar disorder as they can also cause a person who is depressed to switch into mania. Antidepressants may also lead to more frequent mood episodes, known as rapid cycling. This risk is lessened if the person is also taking a mood stabilizer.
Do I need this treatment?
The term “bipolar” refers to the two extremes of mood: mania and depression. People with bipolar disorder usually experience these extremes at different times, although the two mood states can occur together (known as a mixed state). With bipolar disorder, people can also have periods where their mood is balanced. Mood stabilizers can help to keep the mood of a person with bipolar disorder within this balanced range.
Treatment with mood stabilizers can reduce symptoms of bipolar disorder and increase people’s ability to pursue their interests and participate more fully in their relationships.
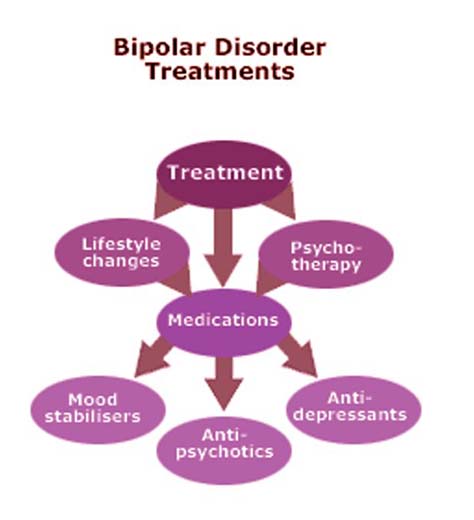
Medication is generally considered to be the cornerstone of treatment for bipolar disorder; however, combining medication with other types of therapy and support can help you to get and stay well. Forms of talk therapy that have been shown to help with bipolar disorder are interpersonal and social rhythm therapy, cognitive-behavioural therapy and family-focused education about bipolar disorder. Other aids can include peer support, school and job counselling, and housing and employment support. Eating a nutritious diet, exercising regularly and getting enough sleep are also important, as are minimizing your use of alcohol and caffeine and avoiding street drugs.
Eating a nutritious diet, exercising regularly and getting enough sleep are also important, as are minimizing your use of alcohol and caffeine and avoiding street drugs.
What does Mood Stabilizing Medication do?
How mood stabilizers work is not fully understood. It is thought that the drugs work in different ways to bring stability and calm to areas of the brain that have become overstimulated and overactive, or to prevent this state from developing.
Side effects of Mood Stabilizing Medication
The side-effects of mood stabilizers vary depending on the type of medication. With some medications, side-effects are kept to a minimum through regular monitoring of the level of the drug in the blood. Some people experience no side-effects. Others may find the side-effects distressing. Side-effects usually lessen as treatment continues.
Check the information given to you by your doctor or pharmacist on the specific effects of any drug you have been prescribed. If side-effects are not mild and tolerable, let your doctor know as soon as possible. Your doctor may:
If side-effects are not mild and tolerable, let your doctor know as soon as possible. Your doctor may:
- adjust your dose
- suggest you take the medication at a different time of day
- suggest you take your medication with food
- prescribe other medications to help control side-effects
- change your medication.
More information on side-effects is included for each type of mood stabilizer.
Getting the right doseWith lithium, carbamazepine and divalproex, the dose is based on how much of the drug is in your blood and how you respond to treatment. This means that the dose differs for everyone who takes it. Blood samples are taken regularly to make sure that the dose is neither too high nor too low. Taking less may not be effective, and taking more can make you physically sick.
The right dose is within a range, rather than a precise point. It may change over time, depending on whether the medication is being used to treat active symptoms of mania or depression or to help prevent symptoms from returning.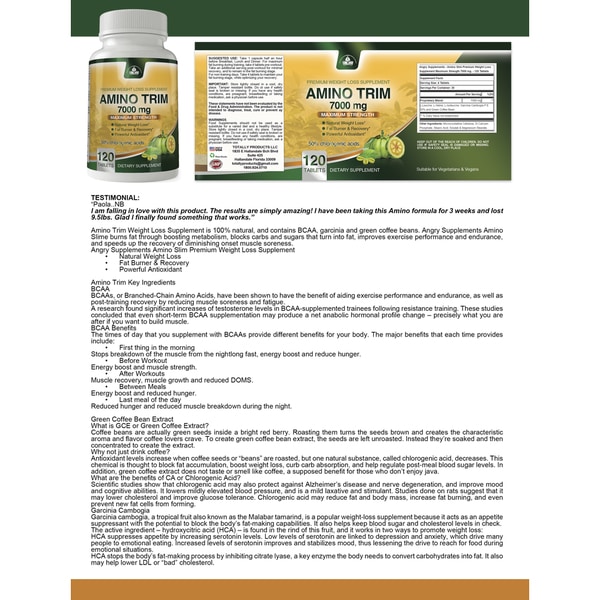 On days that you are scheduled to have your blood level tested, wait until after the test to take your morning dose to avoid inaccurate results.
On days that you are scheduled to have your blood level tested, wait until after the test to take your morning dose to avoid inaccurate results.
If you are taking carbamazepine, avoid grapefruit juice as it can raise the level of this drug in your body.
Controlling side-effects- Mood stabilizers can increase your sensitivity to the sun: wear sunscreen when outdoors to prevent burning.
- To reduce stomach upset, take your dose with food or milk.
- If your medication makes you feel drowsy, check with your doctor to see if you can take it at bedtime.
- Taking mood stabilizers can cause weight gain. Getting regular exercise and eating a low-fat, low-sugar, high-fibre diet (e.g., bran, fruits and vegetables) can help prevent weight gain.
- If side-effects are troublesome or severe, you may do better on a lower dose. Talk to your doctor.
Types of Mood Stabilizing Medication
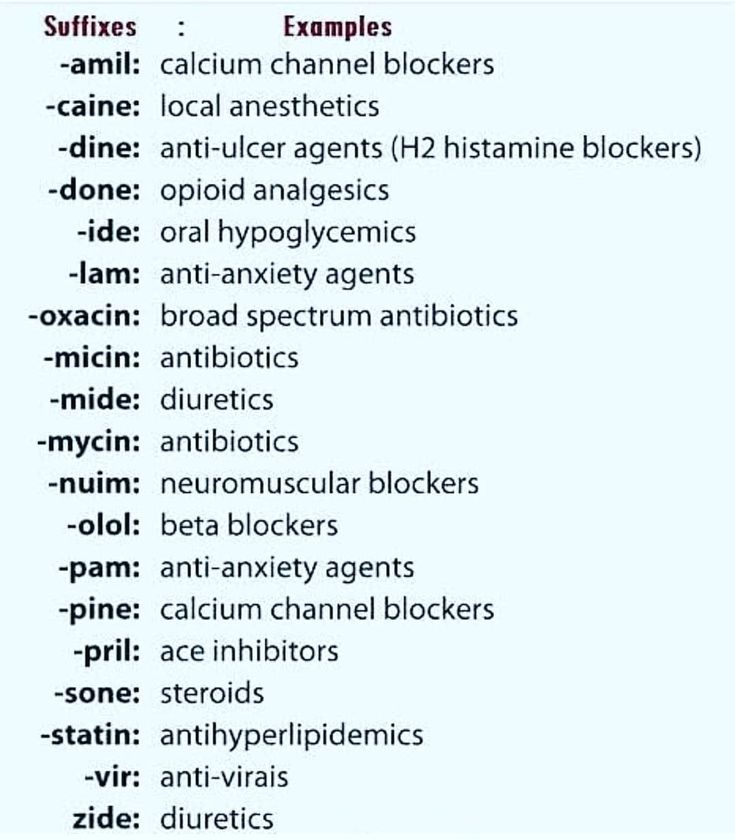
The oldest and most studied of mood stabilizers is lithium. However, many drugs that were first developed as anticonvulsants to treat epilepsy also act as mood stabilizers. These include carbamazepine, divalproex and lamotrigine. Gabapentin and topiramate are also anticonvulsants that may act as mood stabilizers, but they are usually given in addition to other medications.
However, many drugs that were first developed as anticonvulsants to treat epilepsy also act as mood stabilizers. These include carbamazepine, divalproex and lamotrigine. Gabapentin and topiramate are also anticonvulsants that may act as mood stabilizers, but they are usually given in addition to other medications.
Lithium (Carbolith, Duralith, Lithane) is found in nature in some mineral waters and is also present in small amounts in the human body.
Lithium is used to treat mania and to prevent further episodes of mania and depression.
Common side-effects of lithium include increased thirst and urination, nausea, weight gain and a fine trembling of the hands. Less common side-effects can include tiredness, vomiting and diarrhea, blurred vision, impaired memory, difficulty concentrating, skin changes (e.g., dry skin, acne) and slight muscle weakness. These effects are generally mild and fade as treatment continues. If, however, any of these effects are severe, they should be reported to your doctor immediately. Thyroid and kidney function can be affected by lithium in some people and must be monitored regularly by your doctor.
If, however, any of these effects are severe, they should be reported to your doctor immediately. Thyroid and kidney function can be affected by lithium in some people and must be monitored regularly by your doctor.
Signs of lithium overdose: Lithium blood levels can increase to dangerous levels when a person becomes severely dehydrated. Remember to drink eight to 12 cups of fluid per day, especially when it’s hot or when you’re exercising. Severe vomiting, diarrhea or a fever can also cause dehydration. If you have these symptoms, stop taking lithium and see your doctor as soon as possible.
Changing the amount of salt you use can also affect lithium levels: avoid switching to low- or no-salt diets.
Signs that the amount of lithium in the body is higher than it should be include severe nausea, vomiting and diarrhea, shaking and twitching, loss of balance, slurred speech, double vision and weakness.
If you experience any of these effects, see your doctor as soon as possible.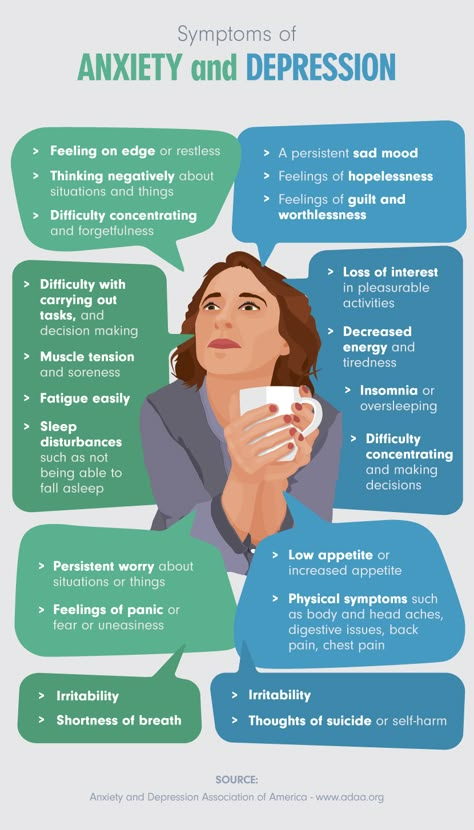 In the meantime, stop taking lithium and drink plenty of fluids. If you cannot reach your doctor and the symptoms do not clear up, go to the nearest hospital emergency department.
In the meantime, stop taking lithium and drink plenty of fluids. If you cannot reach your doctor and the symptoms do not clear up, go to the nearest hospital emergency department.
The differing names for this anticonvulsant medication reflect the various ways it is formulated. Divalproex (and its various forms) is used for acute manic episodes. Brand names include Depakene and Epival.
Common side-effects of divalproex include drowsiness, dizziness, nausea and blurred vision. Less common side-effects are vomiting or mild cramps, muscle tremor, mild hair loss, weight gain, bruising or bleeding, liver problems and, for women, changes in the menstrual cycle.
CarbamazepineCarbamazepine (Tegretol) is another anticonvulsant. It is used for mania and mixed states that do not respond to lithium or when the person is irritable or aggressive.
Common side-effects of carbamazepine include dizziness, drowsiness, blurred vision, confusion, muscle tremor, nausea, vomiting or mild cramps, increased sensitivity to sun, skin sensitivity and rashes, and poor co-ordination.
A rare but dangerous side-effect of carbamazepine is reduced blood cell counts. People who take this drug should have their blood monitored regularly for this effect. Soreness of the mouth, gums or throat, mouth ulcers or sores, and fever or flu-like symptoms can be a sign of this effect and should be reported immediately to your doctor. If carbamazepine is the cause of these symptoms, they will go away when the medication is stopped.
Oxcarbazepine (Trileptal), a closely related drug, may have less side-effects and drug interactions than carbamazepine, but is not as well studied for bipolar disorder.
LamotrigineLamotrigine (Lamictal) may be the most effective mood stabilizer for depression in bipolar disorder, but is not as helpful for mania.
The starting dose of lamotrigine should be very low and increased very slowly over four weeks or more. This approach decreases the risk of a severe rash—a potentially dangerous side-effect of this drug.
Common side-effects of lamotrigine include fever, dizziness, drowsiness, blurred vision, nausea, vomiting or mild cramps, headache and skin rash. Although it is rare, a severe skin rash can occur with lamotrigine. Any rashes that begin in the first few weeks of treatment should be reported to your doctor.
* Medications are referred to in two ways: by their generic name and by their brand or trade names. Brand names available in Canada appear here in brackets.
Frequently Asked Questions
How long should I take mood stabilizers? When you start taking mood stabilizers, it may be two weeks or more before you notice their effect and four to six weeks before they reach their full effect. It’s important to give them time to work. Once your symptoms are under control, you will be encouraged to continue to take mood stabilizers for at least six months and probably longer. How much longer varies from person to person.
Mood stabilizers can help prevent further episodes of mania or depression. In other words, staying on these medications for the long term can help to keep you well. Going off mood stabilizers, on the other hand, can greatly increase your chances of having another episode.
Once you have been taking mood stabilizers for a while and you are feeling well, you may do fine on a lower “maintenance” dose. Talk to your doctor if you would like to try this.
Are mood stabilizers addictive?Drugs that are addictive produce a feeling of euphoria, a strong desire to continue using the drug, and a need to increase the amount used to achieve the same effect. Mood stabilizers do not have these effects.
While mood stabilizers are not addictive, when you take them (or any drug) over months or years, your body adjusts to the presence of the drug. If you then stop using the drug, especially if you stop suddenly, the absence of the drug may result in withdrawal effects or in return of symptoms. With mood stabilizers, the withdrawal effects are generally mild; the greatest risk with stopping these drugs is the return of symptoms.
With mood stabilizers, the withdrawal effects are generally mild; the greatest risk with stopping these drugs is the return of symptoms.
Whether you want to cut down your dose or stop taking a medication, the same rule applies: go slowly. Sudden changes in your dose can greatly increase your risk of having another mood episode.
The first step is to ask yourself if this is the right time. Are you feeling well? Is the level of stress in your life manageable? Do you feel supported by your family and friends?
If you think you’re ready, talk to your doctor. If your doctor doesn’t agree, find out why. If you are not satisfied with his or her reasons, you may want to see another doctor for a second opinion.
If your doctor does agree, he or she will advise you not to skip doses but to reduce your dose gradually over a four to six week period. This process of cutting back will take several months.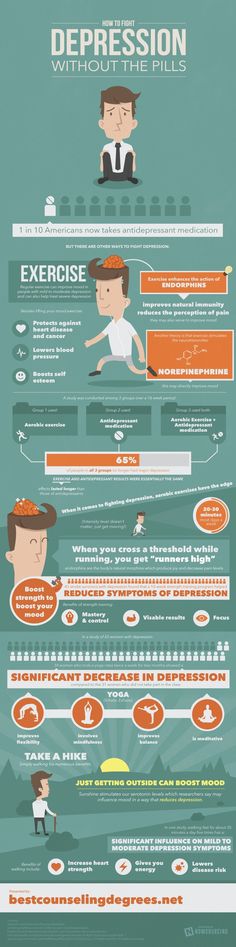
If you want to stop taking more than one medication, your doctor will usually suggest that you lower the dose of one drug at a time.
As you cut down, if you start to feel unwell, let your doctor know. You may want to go back up with your dose. Find the dose that works best for you.
Will mood stabilizers interact with other medications?Some medications can affect the blood levels of mood stabilizers, meaning your dose of mood stabilizer may have to be adjusted while you are taking the other medication. Mood stabilizers, especially carbamazepine, may also reduce the effectiveness of some other drugs. Always make sure your doctor or dentist knows about any drugs you are taking when he or she prescribes another medication. It’s also important to check with your pharmacist before using any over-the-counter medication, including pain medications, herbal remedies, cold or allergy tablets, or cough syrups.
What if I drink coffee or alcohol while taking mood stabilizers? Drinking coffee or other beverages that contain caffeine can lower lithium levels and increase tremor. If you want to dramatically change how much caffeine you have in a day (e.g., cutting back from four cups to one cup of coffee a day), check with your doctor or pharmacist first to see if your mood stabilizer dose should be adjusted.
If you want to dramatically change how much caffeine you have in a day (e.g., cutting back from four cups to one cup of coffee a day), check with your doctor or pharmacist first to see if your mood stabilizer dose should be adjusted.
People with bipolar disorder are generally advised to avoid alcohol. This is recommended because:
- Drinking alcohol can worsen depressive episodes and further impair judgment in mania.
- Many people with bipolar disorder develop addiction problems with alcohol and other drugs, especially when they use these substances to “take the edge off” their symptoms or to offset the effects of medication.
- Combining mood stabilizers with alcohol tends to enhance the negative effects of both drugs, such as drowsiness, nausea and poor co-ordination.
While avoiding alcohol is the best choice for many people with bipolar disorder, having a drink or two on occasion should be okay for those who are stable, feeling well and who have not had a substance use problem.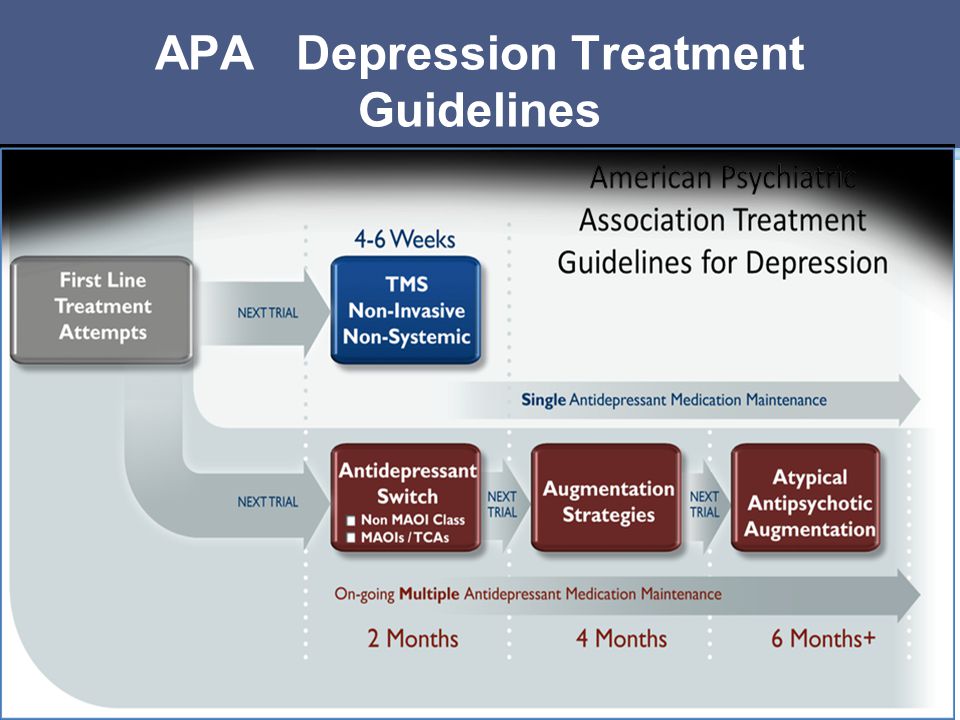
Street drugs can complicate your situation and create problems. Cocaine and amphetamines, for example, can trigger an episode of mania or depression. Marijuana could lift you up or it could bring you down; its effects on mood can be unpredictable, especially when combined with bipolar disorder. Using any street drugs (or alcohol) regularly to modify your mood increases your risk of addiction.
Will mood stabilizers affect my ability to drive safely?Mood stabilizers, especially early in treatment, may delay your reaction time. This effect could impair your ability to drive a car or operate other machinery. Avoid these activities until you adjust to the medication or if you feel slowed down.
Will mood stabilizers affect my sex drive and function? Taking lithium may reduce your interest in sex. This can be a good thing for some people and not so good for others. If you feel your interest in sex is too low, talk to your doctor about it. Sometimes an adjustment in dose can help.
If you feel your interest in sex is too low, talk to your doctor about it. Sometimes an adjustment in dose can help.
Although not common, some men who take lithium report a decreased ability to maintain an erection or to ejaculate. With bipolar disorder, many complex factors other than medication may contribute to sexual difficulties.
In women, mood stabilizers may cause changes in the menstrual cycle. Carbamazepine and other anticonvulsants may reduce the effectiveness of birth control pills.
Is it safe to take mood stabilizers while pregnant or breastfeeding? Each woman’s situation is unique and should be discussed with her doctor. For any pregnant woman with a history of bipolar disorder, the question of taking mood stabilizers during pregnancy usually comes down to a risk-benefit analysis. All mood stabilizers carry some risk—some more than others; however, episodes of depression or mania can affect prenatal care and a mother’s ability to parent her newborn child. When treatment with a mood stabilizer helps to avoid a relapse or to reduce distress, the benefits may outweigh the risks.
When treatment with a mood stabilizer helps to avoid a relapse or to reduce distress, the benefits may outweigh the risks.
Taking lithium during the first trimester in pregnancy is believed to slightly increase the risk of a heart defect in the baby. This risk has been shown to be .05-.1 per cent (i.e., one in 2,000). Newborns must be monitored for possible toxic effects of lithium; these effects usually resolve within one to two weeks.
Divalproex increases the risk of spinal defects in the developing baby by approximately five to nine per cent. Divalproex is also related to developmental delays and cognitive problems in children. Carbamazepine increases the risk of spinal defects by approximately one per cent. Lamotrigine is associated with a potential increased risk for cleft palate.
Lithium can be passed to the baby through breast milk; however, the amount varies greatly from woman to woman. Some women may be able to breastfeed with close monitoring of lithium levels in the mother’s milk and the baby’s blood.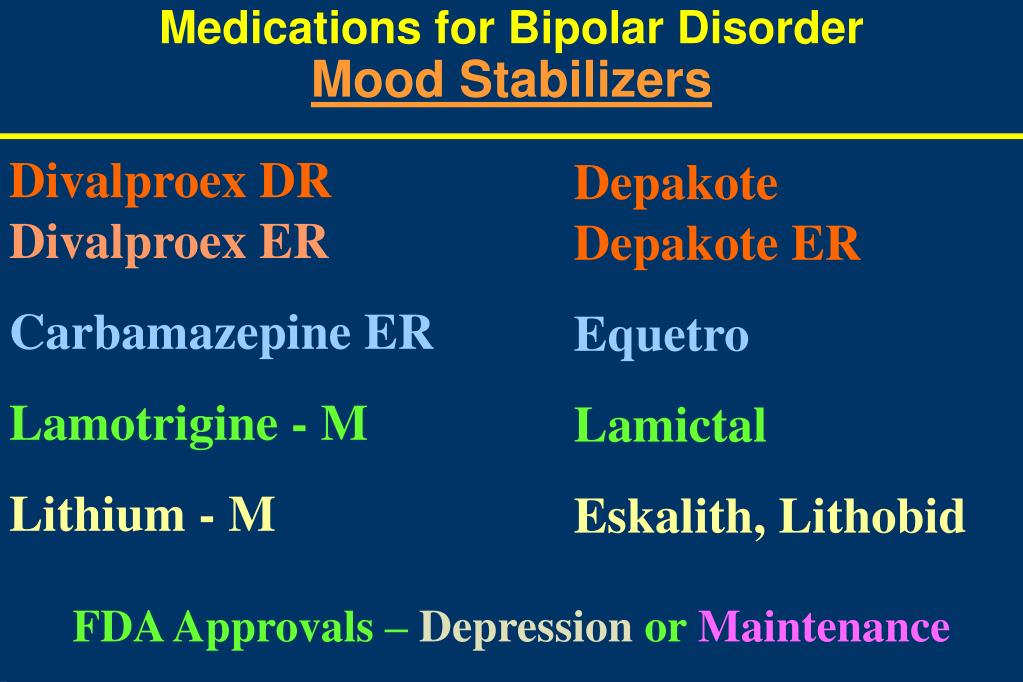
The amount of anticonvulsant mood stabilizers passed through breast milk is very small and is not considered to be a risk to the baby, especially when weighed against the benefits of breastfeeding.
If you decide to stop taking medications during pregnancy or while breastfeeding, it is a good idea to see your doctor more often to help you monitor for a return of symptoms.
Can children and teens use mood stabilizers?The first signs of bipolar disorder can appear in childhood, usually as depression or behaviour problems. Early substance use problems or petty crime can also be signs. When bipolar disorder in childhood is misdiagnosed as attention-deficit/hyperactivity disorder or unipolar depression, treatment with stimulants or antidepressants can worsen symptoms.
Mood stabilizers were developed and tested on adults. While most of these drugs are not officially approved for use by children and teens, professional guidelines direct their use in this age group.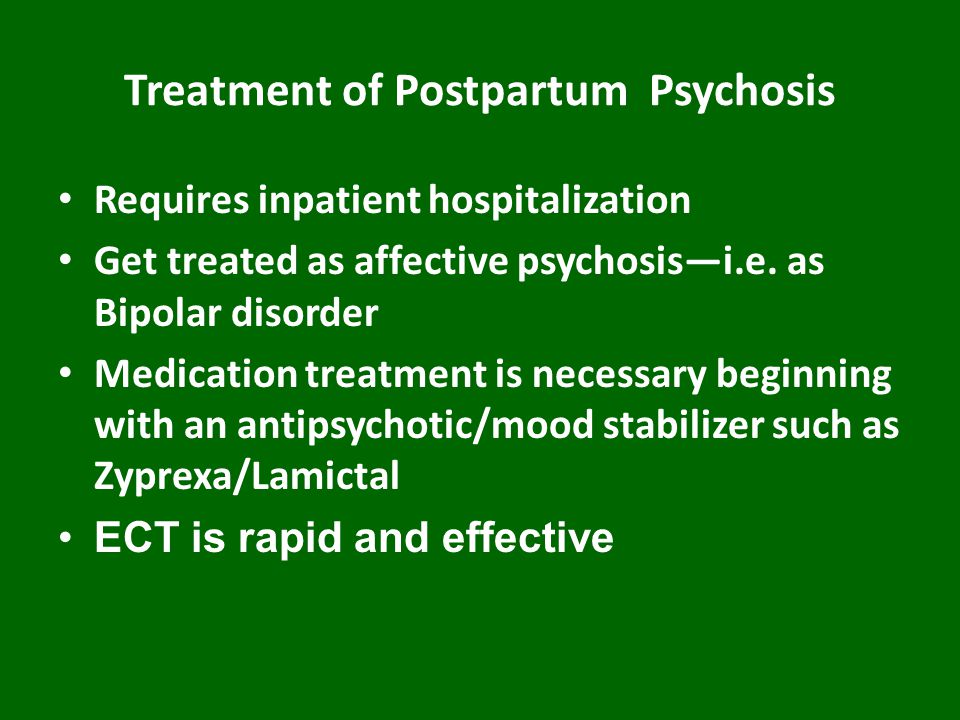 Lithium is approved for treating manic symptoms in children aged 12 and older.
Lithium is approved for treating manic symptoms in children aged 12 and older.
Children and teens may be more prone to the side-effects of these drugs and should be monitored by their doctor regularly for side-effects.
Can older adults use mood stabilizers?As people age into their 60s and older, their bodies become less able to eliminate medications. This means that older people who take mood stabilizers need to have the drug levels in their blood measured more often than younger people. Those taking lithium also need to have their kidney and thyroid function and heart rate monitored more frequently.
As people get older, they also become more sensitive to medications and may require a lower dose. Mood stabilizers can increase the risk of falls, especially when taken with other drugs.
Copyright © 2009, 2012 Centre for Addiction and Mental Health
Related Programs & Services
- Treatment at CAMH: Access CAMH
- Help for families from CAMH
- ConnexOntario
- For information on using medications while pregnant or breastfeeding, contact MotherRisk at 416 813-6780 or visit www.
 motherisk.org.
motherisk.org.
Additional Resources
- When a parent has bipolar disorder - What kids want to know
- Bipolar Disorder: An Information Guide (PDF)
- A free tutorial on bipolar disorder is available on the Mental Health 101 page.
SAMHSA’s National Helpline | SAMHSA
Your browser is not supported
Switch to Chrome, Edge, Firefox or Safari
Main page content
-
SAMHSA’s National Helpline is a free, confidential, 24/7, 365-day-a-year treatment referral and information service (in English and Spanish) for individuals and families facing mental and/or substance use disorders.
Also visit the online treatment locator.
SAMHSA’s National Helpline, 1-800-662-HELP (4357) (also known as the Treatment Referral Routing Service), or TTY: 1-800-487-4889 is a confidential, free, 24-hour-a-day, 365-day-a-year, information service, in English and Spanish, for individuals and family members facing mental and/or substance use disorders.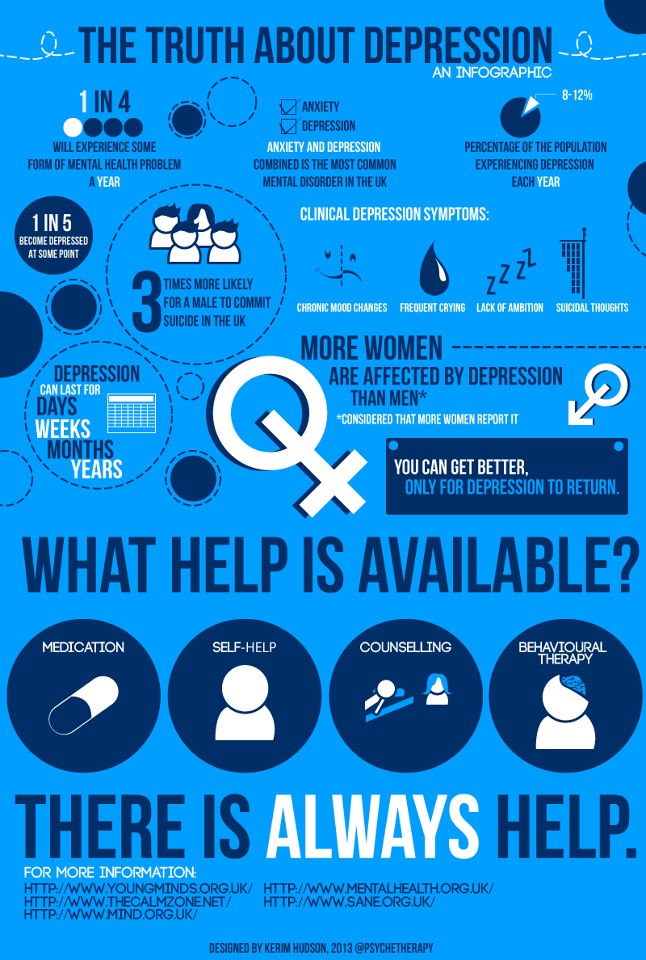 This service provides referrals to local treatment facilities, support groups, and community-based organizations.
This service provides referrals to local treatment facilities, support groups, and community-based organizations.
Also visit the online treatment locator, or send your zip code via text message: 435748 (HELP4U) to find help near you. Read more about the HELP4U text messaging service.
The service is open 24/7, 365 days a year.
English and Spanish are available if you select the option to speak with a national representative. Currently, the 435748 (HELP4U) text messaging service is only available in English.
In 2020, the Helpline received 833,598 calls. This is a 27 percent increase from 2019, when the Helpline received a total of 656,953 calls for the year.
The referral service is free of charge. If you have no insurance or are underinsured, we will refer you to your state office, which is responsible for state-funded treatment programs. In addition, we can often refer you to facilities that charge on a sliding fee scale or accept Medicare or Medicaid.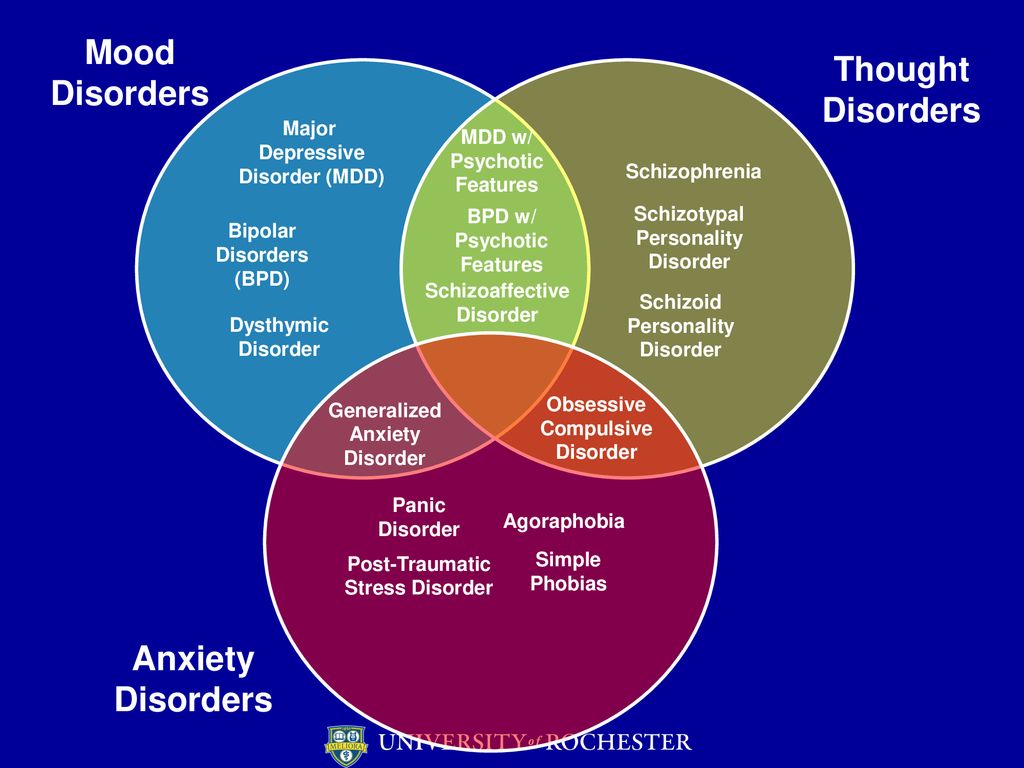 If you have health insurance, you are encouraged to contact your insurer for a list of participating health care providers and facilities.
If you have health insurance, you are encouraged to contact your insurer for a list of participating health care providers and facilities.
The service is confidential. We will not ask you for any personal information. We may ask for your zip code or other pertinent geographic information in order to track calls being routed to other offices or to accurately identify the local resources appropriate to your needs.
No, we do not provide counseling. Trained information specialists answer calls, transfer callers to state services or other appropriate intake centers in their states, and connect them with local assistance and support.
-
Suggested Resources
What Is Substance Abuse Treatment? A Booklet for Families
Created for family members of people with alcohol abuse or drug abuse problems. Answers questions about substance abuse, its symptoms, different types of treatment, and recovery. Addresses concerns of children of parents with substance use/abuse problems.
Addresses concerns of children of parents with substance use/abuse problems.It's Not Your Fault (NACoA) (PDF | 12 KB)
Assures teens with parents who abuse alcohol or drugs that, "It's not your fault!" and that they are not alone. Encourages teens to seek emotional support from other adults, school counselors, and youth support groups such as Alateen, and provides a resource list.After an Attempt: A Guide for Taking Care of Your Family Member After Treatment in the Emergency Department
Aids family members in coping with the aftermath of a relative's suicide attempt. Describes the emergency department treatment process, lists questions to ask about follow-up treatment, and describes how to reduce risk and ensure safety at home.Family Therapy Can Help: For People in Recovery From Mental Illness or Addiction
Explores the role of family therapy in recovery from mental illness or substance abuse. Explains how family therapy sessions are run and who conducts them, describes a typical session, and provides information on its effectiveness in recovery.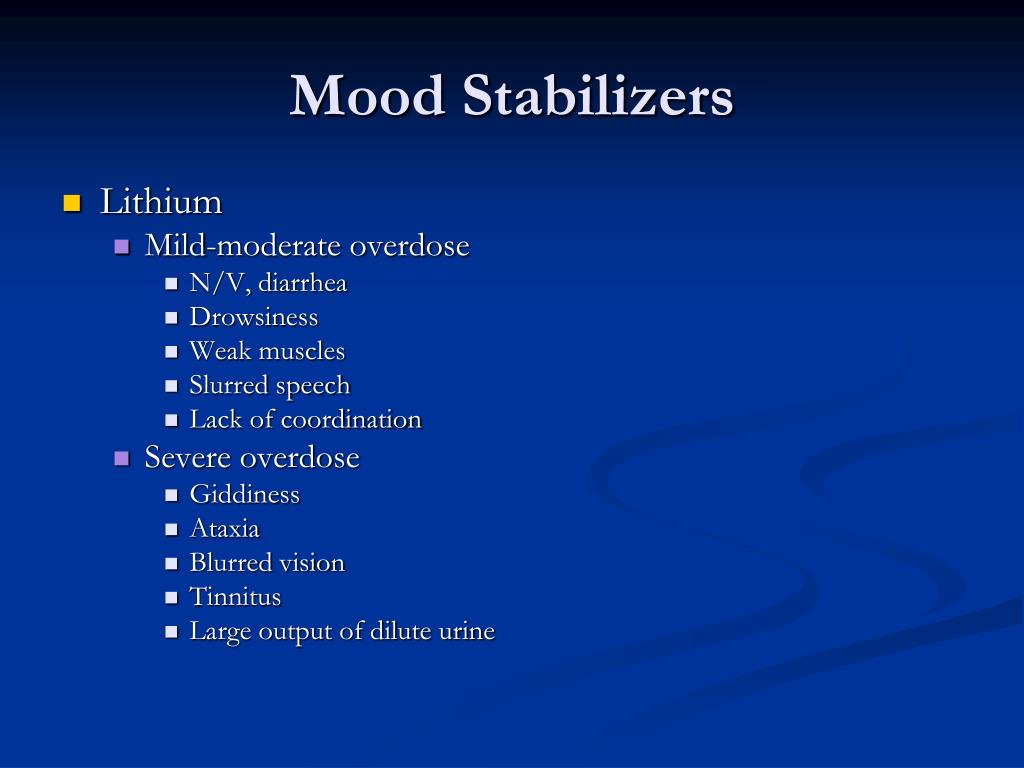
For additional resources, please visit the SAMHSA Store.
Last Updated: 08/30/2022
Fighting depression: 10 modern drugs
{{if type === 'partner-stocks'}}
{{/if}}
{{/if}} {{each list}}${this} {{if isGorzdrav}}
Delete
{{/if}}
{{/each}} {{/if}} Search by drug, disease, substance: DERMAKOSMETIKA, SOLGAR, NaturAge, Voltaren, KagocelHome
Articles
Fighting depression: 10 modern drugs
Depression is an urgent problem, the number of visits to doctors is growing every year. It can be solved by contacting a psychotherapist and taking antidepressants . These are drugs that regulate the production of hormones and biochemical processes in the body. It is strictly forbidden to prescribe them to oneself , as these are complex drugs with certain restrictions, side effects effects . The doctor must authorize their appointment and control the intake. We will tell you which of them are the most effective and common in medicine, how many they have pluses and minuses.
It can be solved by contacting a psychotherapist and taking antidepressants . These are drugs that regulate the production of hormones and biochemical processes in the body. It is strictly forbidden to prescribe them to oneself , as these are complex drugs with certain restrictions, side effects effects . The doctor must authorize their appointment and control the intake. We will tell you which of them are the most effective and common in medicine, how many they have pluses and minuses.
What is meant by
depression Doctors have known it since ancient Greece and Egypt. Hippocrates described it as melancholy - a condition that is accompanied by anxiety, despondency, insomnia, refusal of food, irritability. Most often, the cause is childhood trauma or severe, frequent stress in adulthood. There are many provoking factors: the death of a loved one, deterioration of living conditions, alcoholism, brain diseases. Such cases are referred to as psychogenic depression.
Such cases are referred to as psychogenic depression.
The second type is endogenous. The problem appears not from large external shocks, but because of internal causes. A person is constantly dissatisfied with himself, subjecting himself to criticism. Many patients have panic attacks , haunted by a feeling of fear, anxiety.
How long the period of depression lasts
Many people mistake ordinary periods of low mood for depression. If they do not last long and are quickly replaced by periods of recovery, then we are not talking about a depressive state. The problem is obvious when the symptoms persist for months and dramatically change a person's life. Then you need to see a doctor.
What happens to the body
The most common theory is that there is a malfunction of neurotransmitters located in the brain. These substances transmit signals from neuron to neuron and are responsible for a person's mood. Dysfunction leads to a slowdown in the rate of this transmission and a decrease in the number of neurotransmitters themselves. Serotonin, which is called the "hormone of happiness", suffers the most. For clarity, this biochemical process can be compared, for example, with a drop in blood sugar levels in diabetes mellitus.
Dysfunction leads to a slowdown in the rate of this transmission and a decrease in the number of neurotransmitters themselves. Serotonin, which is called the "hormone of happiness", suffers the most. For clarity, this biochemical process can be compared, for example, with a drop in blood sugar levels in diabetes mellitus.
How is
treated depressionDepression has been treated in different ways. In the ancient world - emetics and laxatives. In the Renaissance - wine and sunbathing. In the Age of Enlightenment - external stimuli, for example, insects. The 19th century brought new recipes - in particular, a solution of camphor in tartaric acid. The treatment also included the use of drugs, which are now no longer allowed for sale, and some are recognized as narcotic.
Obviously, all these drugs had no effect on increasing the amount of serotonin. And the treatment is precisely to normalize its production. This was done after creating modern antidepressants , which have a minimum of side effects, are safe for the body and are not addictive.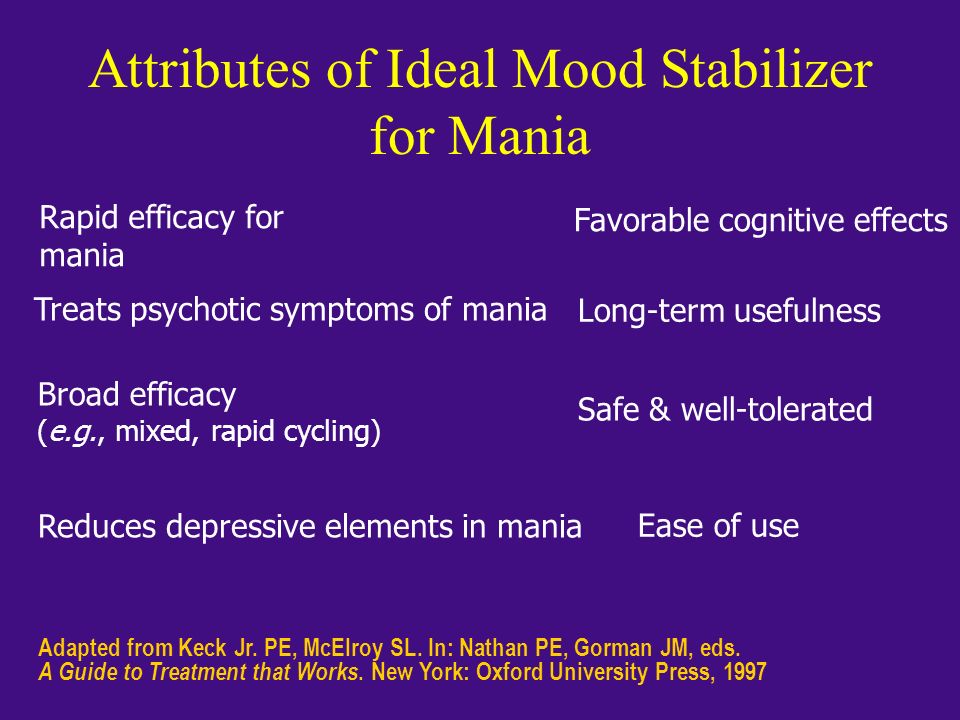 These are medicines, whose action is aimed specifically at balancing the disturbed balance of neurotransmitters: serotonin, norepinephrine, dopamine.
These are medicines, whose action is aimed specifically at balancing the disturbed balance of neurotransmitters: serotonin, norepinephrine, dopamine.
Prescription
If a healthy person takes antidepressants , there will be no effect . For a depressed patient, taking them will help:
- improve psychological state;
- get rid of irritability;
- panic fear;
- increase mental and physical activity;
- overcome the dreary mood.
Psychiatrists prescribe antidepressants for chronic back pain, headaches. And also with irritable bowel syndrome, incontinence and other cases when the body stops producing its own painkillers. Medication helps restore pain suppression mechanisms.
These drugs can only be taken with a doctor's prescription, as many of them are strong stimulants.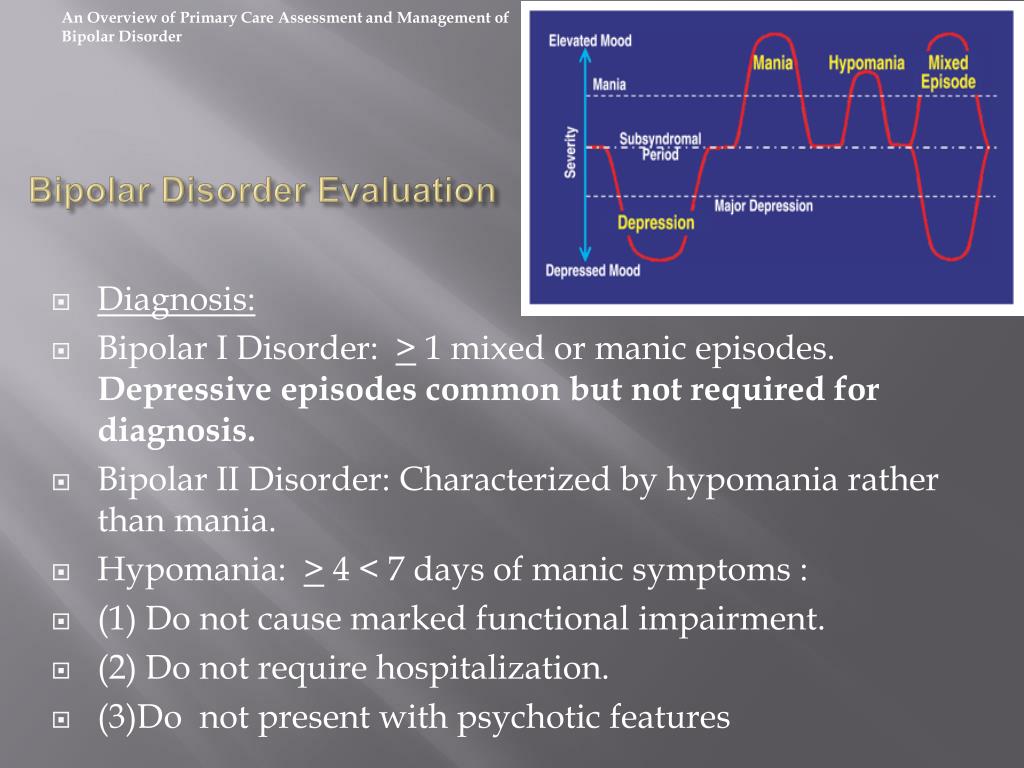 Self-administration may cost dearly - the condition may worsen. Only a doctor will correctly calculate how many medicines to take per day. In parallel with the treatment by a psychiatrist, a neurologist, a consultation of a psychotherapist is required.
Self-administration may cost dearly - the condition may worsen. Only a doctor will correctly calculate how many medicines to take per day. In parallel with the treatment by a psychiatrist, a neurologist, a consultation of a psychotherapist is required.
Precautions
- Prescribed drug start drinking from a small dose - the first couple of days they take a quarter of a tablet. Gradually increase the dose to normal. So the body adapts better. Finish the course by reducing the dose.
- The first effect of appears only 2 weeks after the start of administration. Sustained action - after six months. All this time, you need to take remedy, without making passes, breaks.
-
Products are not combined with melatonin, St. John's wort, products and dietary supplements based on sibutramine, 5-HTP. Their combination can raise serotonin to dangerous levels.
 Also, you can not combine them with monoamine oxidase inhibitors, for example, Cipralex. When writing a prescription, the doctor takes these points into account.
Also, you can not combine them with monoamine oxidase inhibitors, for example, Cipralex. When writing a prescription, the doctor takes these points into account. - Drinking antidepressants is better in parallel with visits to a psychotherapist. If the drugs normalize the biochemical processes in the body, then this doctor will help normalize the psychological state after depression.
The best antidepressants
In medicine, they have long argued that some drugs give only a placebo effect. The purpose of the study was to find out which of them are the most effective and valid . The project involved 116 thousand patients, and its results were published by the authoritative edition of the Lancet. We offer a list of the best.
1. Agomelatine
New generation drug. Agomelatine is used for severe depressive disorders, high levels of anxiety. Enhances the release of dopamine and norepinephrine, stimulates melatonin receptors. The standard therapeutic dose is 25-50 mg 1 time / day. Helps to restore the normal structure of sleep, get rid of anxiety and panic attacks attacks
The standard therapeutic dose is 25-50 mg 1 time / day. Helps to restore the normal structure of sleep, get rid of anxiety and panic attacks attacks
Pros
+ Does not adversely affect attention and memory.
+ No lethargy during the day.
+ No sexual deviations.
+ No relation to blood pressure.
+ Do not reduce dosage upon discontinuation.
Cons
— In 1-10% of cases, increased sweating, diarrhea, constipation.
- Possible increased fatigue, drowsiness.
- There are no evidence-based safety studies in people with renal or hepatic insufficiency, therefore, such patients are advised to refrain from taking drugs with active ingredient agomelatine.
2. Amitriptyline
Tricyclic antidepressant. Moreover, the World Health Organization considers Amitriptyline the most reliable in this group. The standard dose is 200-250 mg / day. The action is to block the reuptake of neurotransmitters.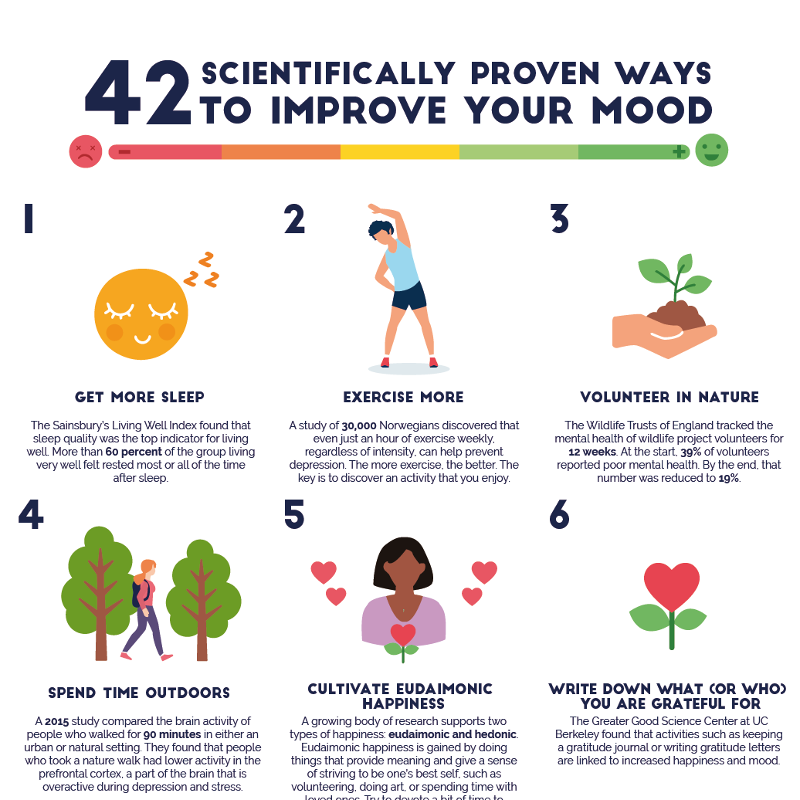 A good remedy for moderate to severe disorders of the endogenous type. Additionally, it has a sedative and hypnotic effect. Effective in the treatment of neuropathic pain, for the prevention of migraine.
A good remedy for moderate to severe disorders of the endogenous type. Additionally, it has a sedative and hypnotic effect. Effective in the treatment of neuropathic pain, for the prevention of migraine.
Pluses
+ Preparations with active ingredient amitriptyline are inexpensive.
+ High reliability, minimum side effects.
+ Relatively safe during breastfeeding.
Cons
- Possible side effect in the form of blurred vision, dry mouth.
- Lowering blood pressure.
- Some patients experience constipation.
- Drowsiness.
3. Escitalopram
It belongs to the group of modern serotonin reuptake inhibitors (SSRIs). Most often, it is recommended to take for anxiety, panic attacks. It is taken once, the standard dose is 10 mg per day. Escitalopram has a milder effect and is prescribed to patients for whom tricyclic drugs are contraindicated.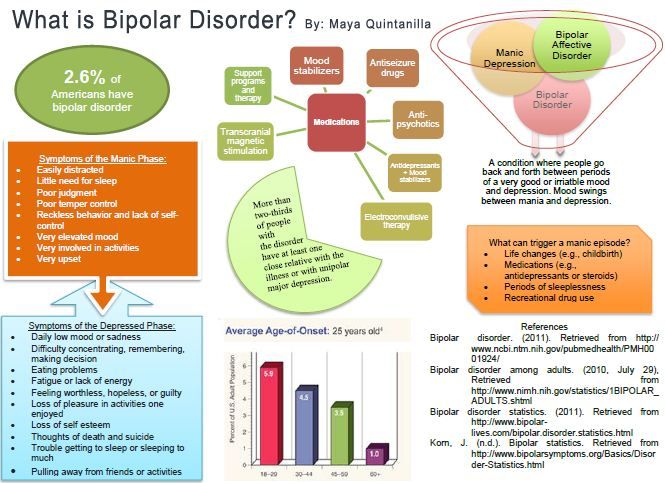
Pluses
+ Lasting effect comes after 3 months.
+ Indicated for patients with disorders of the cardiovascular system.
+ Soft action.
Cons
- In some patients, the functions of the gastrointestinal tract are disturbed, which is most often expressed in diarrhea.
- Anxiety may increase during the first 2 weeks, therefore it is recommended to start treatment with low doses and gradually increase them.
- Contraindicated in pregnancy and lactation.
4. Mirtazapine
A drug of the tetracyclic group. Mirtazapine - good stimulant for anxious depressions, has a moderate sedative effect. The average amount is 30 mg / day, it must be consumed once. Usually it is prescribed to patients who lose interest in life, cease to experience joy, pleasure. Effective in the correction of sleep, in particular, early awakenings.
Pros
+ Earlier onset of action than SSRIs (1 week).
+ Works well with most general medicines.
+ Full effect in 4 weeks.
+ Does not affect sexual function.
Cons
- The active substance mirtazapine is contraindicated in diabetes mellitus, arterial hypotension, increased intraocular pressure.
— During the appointment, you must drive carefully and engage in potentially hazardous types of work.
- 18% of patients experience drowsiness, 15% dry mouth, 5% weight loss. Other side effects occur in 1-3% of cases.
5. Paroxetine
Belongs to the SSRI group, is used most often for severe anxiety, panic, social phobia, nightmares, stress after trauma. Paroxetine can resolve the problems of anxious depression, anxiety-phobic disorders. Take once a day at a dose of 20 mg.
Pros
+ The most powerful stimulant among SSRIs.
+ Anxiety and insomnia pass quickly.
+ Minimal side effects in the form of vomiting, diarrhea.
+ Suitable for patients with cardiovascular problems.
Cons
— Not suitable for patients with severe motor, mental inhibition.
- Reduces libido.
- Harmful to the fetus when taken during pregnancy.
6. Fluoxetine
One of the most commonly used antidepressants in the SSRI group. Known as Prozac. Fluoxetine is also known as a good mood stimulant. Patients have a feeling of fear, tension, anxiety, gloomy dislike for others. Depending on the indications, the average daily dose is 20-60 mg.
Pluses
+ There is practically no effect on the work of the heart.
+ Does not cause sedation.
+ Effective for patients with motor retardation and excessive daytime sleepiness.
Cons
- May cause weight loss.
— Hypoglycemia is possible in diabetes mellitus.
- Contraindicated in severe renal impairment.
7. Fluvoxamine
Another SSRI drug. Fluvoxamine is similar to Prozac Fluoxetine but is fast acting and may cost cheaper. The effect is in a more active slowing down of the reuptake of serotonin by neurons. It is indicated for depression of various origins, as well as obsessive-compulsive disorders. The average daily dose is 100 mg.
Fluvoxamine is similar to Prozac Fluoxetine but is fast acting and may cost cheaper. The effect is in a more active slowing down of the reuptake of serotonin by neurons. It is indicated for depression of various origins, as well as obsessive-compulsive disorders. The average daily dose is 100 mg.
Pros
+ Lower price than traditional Prozac.
+ Faster action than him.
+ Relatively minor side effects (diarrhea, dry mouth, drowsiness).
Cons
- Contraindicated in diabetes.
- Pregnant women - with caution, lactation - prohibited.
- Causes nausea in some patients.
8. Sertraline
One of the widely used and universal drugs of the SSRI group. They treat almost any depressive condition, panic disorder, social phobia. However, in severe clinical cases, sertraline may not be effective enough. The standard dose is 50 mg/day.
Pros
+ No cardiotoxicity.
+ The patient's psychomotor activity does not change.
+ Does not increase body weight.
+ Combines well with other groups of antidepressants.
Cons
— In the first 2 weeks there may be problems with sleep, diarrhea.
- Side effects of a sexual nature.
- Contraindicated in pregnant women.
9. Escitalopram
The drug is classified as an SSRI. Its difference is in its effectiveness in depression, which is accompanied by involuntary movements (tic, tremor, chewing, smacking). Escitalopram is prescribed to patients with panic, anxiety, phobias, obsessive thoughts or actions. The daily dose is 20 mg.
Pluses
+ Effective in tardive dyskinesia.
+ One of the most powerful SSRIs.
+ More pronounced thymoleptic effect (improvement of mood) compared to many antidepressants of the same group.
Cons
- In some patients, anxiety increases within 2 weeks after starting treatment.
— Gastrointestinal disorders, insomnia, agitation are possible.
— Use during pregnancy only in extreme cases, incompatible with feeding.
10. Venlafaxine
Belongs to the SNRI group. In addition to blocking the reuptake of serotonin, venlafaxine has a similar effect on another neurotransmitter, norepinephrine. The medicine is prescribed for depressive conditions of various origins, social phobias, anxiety, panic. Usually take 150 mg per day.
Pros
+ Better tolerated by patients than most tricyclics.
+ More pronounced effect than classic SSRIs.
+ Fewer contraindications.
Cons
- Traditional side effects of most antidepressants: nausea, drowsiness, dry mouth, diarrhea or constipation.
- May increase eye pressure.
- The most severe withdrawal syndrome among antidepressant drugs.
This list is not to be used as a recommendation. In any case, consult your doctor before purchasing. Be healthy!
Mood stabilizers - The Pinel Case
Mood stabilizers are a class of psychotropic drugs that are commonly used to treat bipolar affective disorder (BAD). In addition, indications of normotimics are usually used to reduce aggression and irritability, to enhance the effect of antidepressants when they are insufficient. This explains the use of mood stabilizers in patients without a diagnosis of bipolar disorder: in patients with depression, personality disorders, schizoaffective disorder, or organic brain damage. Normotimics do not always mean BAD, and BAD, in turn, is not always treated with normotimics. Antipsychotics are sometimes used in combination with antidepressants to treat this mental illness. Below we will talk about four mood stabilizers: lithium salts, carbamazepine, valproic acid and lamotrigine.
In addition, indications of normotimics are usually used to reduce aggression and irritability, to enhance the effect of antidepressants when they are insufficient. This explains the use of mood stabilizers in patients without a diagnosis of bipolar disorder: in patients with depression, personality disorders, schizoaffective disorder, or organic brain damage. Normotimics do not always mean BAD, and BAD, in turn, is not always treated with normotimics. Antipsychotics are sometimes used in combination with antidepressants to treat this mental illness. Below we will talk about four mood stabilizers: lithium salts, carbamazepine, valproic acid and lamotrigine.
Lithium carbonate
In Russia, lithium carbonate is the only representative of lithium salts. In the USA, lithium citrate is still used, but in Russia it is not used. Lithium carbonate is used in bipolar and schizoaffective disorder for the relief of manic episodes and as an agent for maintenance therapy. It may also be useful in reducing irritability in patients with psychiatric disorders. The addition of lithium carbonate to antidepressant therapy can enhance their effect, although other methods are currently being used by doctors to overcome the insufficient effect of antidepressants. Another strength of lithium salts is that, according to some data, they can reduce the risk of suicide in patients with depression.
It may also be useful in reducing irritability in patients with psychiatric disorders. The addition of lithium carbonate to antidepressant therapy can enhance their effect, although other methods are currently being used by doctors to overcome the insufficient effect of antidepressants. Another strength of lithium salts is that, according to some data, they can reduce the risk of suicide in patients with depression.
To evaluate the effectiveness and safety of lithium salt therapy abroad, it is customary to evaluate the concentration of lithium ions in the blood. Such an analysis is also available in our country, but it is carried out by private laboratories and at the expense of the patient or his relatives.
Common side effects of lithium preparations are:
- hand tremor;
- lethargy, memory loss;
- skin rash, acne or hair loss;
- impaired renal function.
The drug is widely used in the practice of psychiatrists due to its strong and relatively rapidly developing action.
Unlike lithium salts, other mood stabilizers are classified as anticonvulsants, drugs used to treat epilepsy. Examples include valproic acid, carbamazepine and lamotrigine.
Valproic acid
Valproic acid is usually taken in the form of sodium salts - sodium valproate. This compound itself is unique in psychiatry in that it does not contain a cyclic part of carbon and other atoms. Valproic acid is widely used in various types of epilepsy, but it also found a place in psychiatry. The main indication is BAR. Valproic acid and its salts are used to treat the manic phase of bipolar disorder and for maintenance therapy in this disease. A number of researchers believe that valproic acid may be particularly effective in rapid phase changes and in mixed states within the framework of bipolar disorder.
A separate area of use of valproic acid is the suppression and prevention of aggression, emotional instability, impulsivity and self-harm, which can be useful in borderline personality disorder. Valproic acid is also used to enhance the effect of antipsychotics.
Valproic acid is also used to enhance the effect of antipsychotics.
The main side effects of valproic acid that usually lead to discontinuation of the drug are
- weight gain;
- digestive problems (nausea, vomiting, diarrhea and cramps) - these adverse events are usually dose-dependent: the higher the dose of the drug taken, the greater the severity of side effects;
- drowsiness and lethargy;
- liver damage.
Recently, there has been a lot of discussion among doctors about the harm of valproic acid to the fetus if the mother takes valproic acid during pregnancy. It must be said that other mood stabilizers do not have any advantage in this respect over valproic acid.
Carbamazepine
Carbamazepine is widely loved by neurologists, psychiatrists and narcologists. Various neuralgia, bipolar disorder, mood disorders due to damage to the central nervous system, alcohol dependence and withdrawal syndrome, and so on and so forth. Carbamazepine is dear to the hearts of many specialists and is prescribed for a variety of conditions. It should be taken into account that carbamazepine reduces the concentration of antipsychotics (neuroleptics) and antidepressants in the patient's blood, which can lead to a deterioration in the condition when carbamazepine is added. Like other mood stabilizers, carbamazepine is prescribed for aggression and impulsivity, if they occur with a mental disorder.
Carbamazepine is dear to the hearts of many specialists and is prescribed for a variety of conditions. It should be taken into account that carbamazepine reduces the concentration of antipsychotics (neuroleptics) and antidepressants in the patient's blood, which can lead to a deterioration in the condition when carbamazepine is added. Like other mood stabilizers, carbamazepine is prescribed for aggression and impulsivity, if they occur with a mental disorder.
Side effects of carbamazepine:
- weakness, lethargy;
- nausea;
- dizziness;
- skin rash;
- decrease in the number of leukocytes in the blood (especially at the beginning of therapy).
Lamotrigine
This drug is used in different phases of bipolar disorder and for maintenance therapy in this disease. Lamotrigine may be used to boost antidepressant therapy for resistant depression (depression that is resistant to an adequate course of antidepressant therapy).