Do antidepressants cause drowsiness
Side effects - Antidepressants - NHS
The side effects of antidepressants can cause problems at first, but they generally improve with time.
It's important to continue treatment, even if you're affected by side effects, as it will take several weeks before you begin to benefit from treatment. With time, you should find that the benefits of treatment outweigh any problems from side effects.
During the first few months of treatment, you'll usually see your doctor or a specialist nurse at least once every 2 to 4 weeks to see how well the medicine is working.
For more information about your specific medicine, see the patient information leaflet that comes with it.
SSRIs and SNRIs
Common side effects of selective serotonin reuptake inhibitors (SSRIs) and serotonin-noradrenaline reuptake inhibitors (SNRIs) can include:
- feeling agitated, shaky or anxious
- feeling and being sick
- indigestion and stomach aches
- diarrhoea or constipation
- loss of appetite
- dizziness
- not sleeping well (insomnia), or feeling very sleepy
- headaches
- loss of libido (reduced sex drive)
- difficulties achieving orgasm during sex or masturbation
- difficulties obtaining or maintaining an erection (erectile dysfunction)
These side effects should improve within a few weeks, although some can occasionally persist.
Tricyclic antidepressants (TCAs)
Common side effects of TCAs can include:
- dry mouth
- slight blurring of vision
- constipation
- problems passing urine
- drowsiness
- dizziness
- weight gain
- excessive sweating (especially at night)
- heart rhythm problems (arrhythmia), such as noticeable palpitations or a fast heartbeat (tachycardia)
The side effects should ease after a couple of weeks as your body begins to get used to the medicine.
Potential health risks
Serotonin syndrome
Serotonin syndrome is an uncommon, but potentially serious, set of side effects linked to SSRIs and SNRIs.
Serotonin syndrome occurs when the levels of a chemical called serotonin in your brain become too high. It's usually triggered when you take an SSRI or SNRI in combination with another medicine (or substance) that also raises serotonin levels, such as another antidepressant or St John's wort.
Symptoms of serotonin syndrome can include:
- confusion
- agitation
- muscle twitching
- sweating
- shivering
- diarrhoea
If you experience these symptoms, you should stop taking the medicine and get immediate advice from your GP or specialist. If this is not possible, call NHS 111.
Symptoms of severe serotonin syndrome include:
- seizures (fits)
- irregular heartbeat (arrhythmia)
- unconsciousness
If you experience symptoms of severe serotonin syndrome, get emergency medical help immediately by dialling 999 to ask for an ambulance.
Hyponatraemia
Elderly people who take antidepressants, particularly those who take SSRIs, may experience a severe fall in sodium (salt) levels, known as hyponatraemia. This may lead to a build-up of fluid inside the cells of the body, which can be potentially dangerous.
This can happen because SSRIs can block the effects of a hormone that regulates levels of sodium and fluid in the body. Elderly people are vulnerable because fluid levels become more difficult for the body to regulate as people age.
Mild hyponatraemia can cause symptoms similar to depression or side effects of antidepressants, such as:
- feeling sick
- headache
- muscle pain
- reduced appetite
- confusion
More severe hyponatraemia can cause:
- feeling listless and tired
- disorientation
- agitation
- psychosis
- seizures (fits)
The most serious cases of hyponatraemia can cause you to stop breathing or enter a coma.
If you suspect mild hyponatraemia, you should call your GP for advice and stop taking SSRIs for the time being.
If you suspect severe hyponatraemia, call 999 and ask for an ambulance.
Hyponatraemia can be treated by feeding a sodium solution into the body through an intravenous drip.
Diabetes
Long-term use of SSRIs and TCAs has been linked to an increased risk of developing type 2 diabetes, although it's not clear if the use of these antidepressants directly causes diabetes to develop.
It may be that the weight gain some people using antidepressants experience increases the risk of them developing type 2 diabetes.
Suicidal thoughts
In rare cases, some people experience suicidal thoughts and a desire to self-harm when they first take antidepressants. Young people under 25 seem particularly at risk.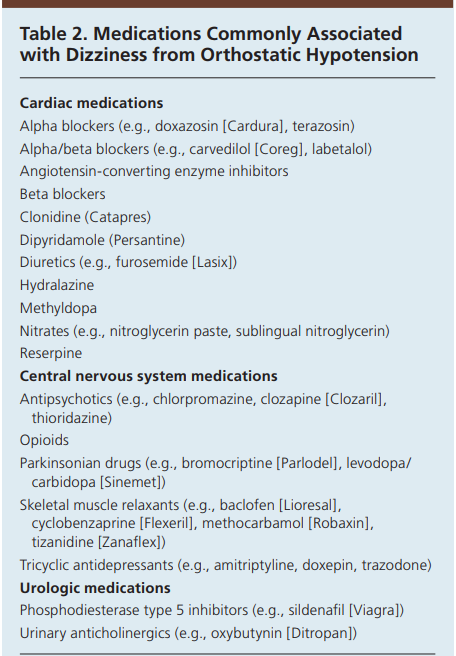
Contact your GP, or go to A&E immediately, if you have thoughts of killing or harming yourself at any time while taking antidepressants.
It may be useful to tell a relative or close friend if you've started taking antidepressants and ask them to read the leaflet that comes with your medicines. You should then ask them to tell you if they think your symptoms are getting worse, or if they're worried about changes in your behaviour.
Page last reviewed: 4 November 2021
Next review due: 4 November 2024
Effects of Antidepressants on Sleep
Papers of Particular Interest, Published Recently, Have Been Highlighted as: • Of importance •• Of major importance
1. Moussavi S, Chatterji S, Verdes E, Tandon A, Patel V, Ustun B. Depression, chronic diseases, and decrements in health: results from the world health surveys. Lancet. 2007;370:851–858. doi: 10. 1016/S0140-6736(07)61415-9. [PubMed] [CrossRef] [Google Scholar]
1016/S0140-6736(07)61415-9. [PubMed] [CrossRef] [Google Scholar]
2. Greden JF. Unmet need: what justifies the search for a new antidepressant? J Clin Psychiatry. 2002;63(Suppl 2):3–7. [PubMed] [Google Scholar]
3. Wichniak A, Wierzbicka A, Jernajczyk W. Sleep and antidepressant treatment. Curr Pharm Des. 2012;18:5802–5817. doi: 10.2174/138161212803523608. [PubMed] [CrossRef] [Google Scholar]
4. Le Bon O. Contribution of sleep research to the development of new antidepressants. Dialogues Clin Neurosci. 2005;7:305–313. [PMC free article] [PubMed] [Google Scholar]
5. Mendlewicz J. Sleep disturbances: core symptoms of major depressive disorder rather than associated or comorbid disorders. World J Biol Psychiatry. 2009;10:269–275. doi: 10.3109/15622970802503086. [PubMed] [CrossRef] [Google Scholar]
6. Wilson S, Argyropoulos S. Antidepressants and sleep: a qualitative review of the literature. Drugs. 2005;65:927–947. doi: 10.2165/00003495-200565070-00003. [PubMed] [CrossRef] [Google Scholar]
7. Gursky JT, Krahn LE. The effects of antidepressants on sleep: a review. Harv Rev Psychiatry. 2000;8:298–306. doi: 10.1080/hrp.8.6.298. [PubMed] [CrossRef] [Google Scholar]
Gursky JT, Krahn LE. The effects of antidepressants on sleep: a review. Harv Rev Psychiatry. 2000;8:298–306. doi: 10.1080/hrp.8.6.298. [PubMed] [CrossRef] [Google Scholar]
8. Thase ME. Depression, sleep, and antidepressants. J Clin Psychiatry. 1998;59(Suppl 4):55–65. [PubMed] [Google Scholar]
9. Wichniak A, Wierzbicka A, Jernajczyk W. Sleep as a biomarker for depression. Int Rev Psychiatry. 2013;25:632–645. doi: 10.3109/09540261.2013.812067. [PubMed] [CrossRef] [Google Scholar]
10. Baglioni C, Nanovska S, Regen W, Spiegelhalder K, Feige B, Nissen C, Reynolds CF, Riemann D. Sleep and mental disorders: a meta-analysis of polysomnographic research. Psychol Bull. 2016;142:969–990. doi: 10.1037/bul0000053. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
11. Abad VC, Guilleminault C. Sleep and psychiatry. Dialogues Clin Neurosci. 2005;7:291–303. [PMC free article] [PubMed] [Google Scholar]
12. Kaplan KA, Harvey AG. Hypersomnia across mood disorders: a review and synthesis. Sleep Med Rev. 2009;13:275–285. doi: 10.1016/j.smrv.2008.09.001. [PubMed] [CrossRef] [Google Scholar]
Sleep Med Rev. 2009;13:275–285. doi: 10.1016/j.smrv.2008.09.001. [PubMed] [CrossRef] [Google Scholar]
13. McClintock SM, Husain MM, Wisniewski SR, Nierenberg AA, Stewart JW, Trivedi MH, Cook I, Morris D, Warden D, Rush AJ. Residual symptoms in depressed outpatients who respond by 50% but do not remit to antidepressant medication. J Clin Psychopharmacol. 2011;31:180–186. doi: 10.1097/JCP.0b013e31820ebd2c. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
14. Kay DB, Dombrovski AY, Buysse DJ, Reynolds CF, Begley A, Szanto K. Insomnia is associated with suicide attempt in middle-aged and older adults with depression. Int Psychogeriatr. 2016;28:613–619. doi: 10.1017/S104161021500174X. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
15. Schmid DA, Wichniak A, Uhr M, Ising M, Brunner H, Held K, Weikel JC, Sonntag A, Steiger A. Changes of sleep architecture, spectral composition of sleep EEG, the nocturnal secretion of cortisol, ACTH, GH, prolactin, melatonin, ghrelin, and leptin, and the DEX-CRH test in depressed patients during treatment with mirtazapine. Neuropsychopharmacology. 2006;31:832–844. doi: 10.1038/sj.npp.1300923. [PubMed] [CrossRef] [Google Scholar]
Neuropsychopharmacology. 2006;31:832–844. doi: 10.1038/sj.npp.1300923. [PubMed] [CrossRef] [Google Scholar]
16. Thompson C. Onset of action of antidepressants: results of different analyses. Hum Psychopharmacol. 2002;17(Suppl 1):S27–S32. doi: 10.1002/hup.386. [PubMed] [CrossRef] [Google Scholar]
17. Doghramji K, Jangro WC. Adverse effects of psychotropic medications on sleep. Psychiatr Clin North Am. 2016;39:487–502. doi: 10.1016/j.psc.2016.04.009. [PubMed] [CrossRef] [Google Scholar]
18. Fava M. Daytime sleepiness and insomnia as correlates of depression. J Clin Psychiatry. 2004;65(Suppl 16):27–32. [PubMed] [Google Scholar]
19. Jindal RD, Thase ME. Treatment of insomnia associated with clinical depression. Sleep Med Rev. 2004;8:19–30. doi: 10.1016/S1087-0792(03)00025-X. [PubMed] [CrossRef] [Google Scholar]
20. Hashimoto T, Shiina A, Hasegawa T, Kimura H, Oda Y, Niitsu T, Ishikawa M, Tachibana M, Muneoka K, Matsuki S, Nakazato M, Iyo M. Effect of mirtazapine versus selective serotonin reuptake inhibitors on benzodiazepine use in patients with major depressive disorder: a pragmatic, multicenter, open-label, randomized, active-controlled, 24-week trial. Ann General Psychiatry. 2016;15:27. doi: 10.1186/s12991-016-0115-1. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
Ann General Psychiatry. 2016;15:27. doi: 10.1186/s12991-016-0115-1. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
21. Jindal RD, Friedman ES, Berman SR, Fasiczka AL, Howland RH, Thase ME. Effects of sertraline on sleep architecture in patients with depression. J Clin Psychopharmacol. 2003;23:540–548. doi: 10.1097/01.jcp.0000095345.32154.9a. [PubMed] [CrossRef] [Google Scholar]
22. Furukawa TA, Streiner DL, Young LT. Antidepressant and benzodiazepine for major depression. Cochrane Database Syst Rev. 2002; CD001026. [PubMed]
23. Serretti A, Mandelli L. Antidepressants and body weight: a comprehensive review and meta-analysis. J Clin Psychiatry. 2010;71:1259–1272. doi: 10.4088/JCP.09r05346blu. [PubMed] [CrossRef] [Google Scholar]
24. Hickie IB, Rogers NL. Novel melatonin-based therapies: potential advances in the treatment of major depression. Lancet. 2011;378:621–631. doi: 10.1016/S0140-6736(11)60095-0. [PubMed] [CrossRef] [Google Scholar]
25. Quera-Salva MA, Hajak G, Philip P, Montplaisir J, Keufer-Le GS, Laredo J, Guilleminault C. Comparison of agomelatine and escitalopram on nighttime sleep and daytime condition and efficacy in major depressive disorder patients. Int Clin Psychopharmacol. 2011;26:252–262. doi: 10.1097/YIC.0b013e328349b117. [PubMed] [CrossRef] [Google Scholar]
Comparison of agomelatine and escitalopram on nighttime sleep and daytime condition and efficacy in major depressive disorder patients. Int Clin Psychopharmacol. 2011;26:252–262. doi: 10.1097/YIC.0b013e328349b117. [PubMed] [CrossRef] [Google Scholar]
26. Quera-Salva MA, Lemoine P, Guilleminault C. Impact of the novel antidepressant agomelatine on disturbed sleep-wake cycles in depressed patients. Hum Psychopharmacol. 2010;25:222–229. doi: 10.1002/hup.1112. [PubMed] [CrossRef] [Google Scholar]
27. Sowa-Kucma M, Panczyszyn-Trzewik P, Misztak P, Jaeschke RR, Sendek K, Styczen K, Datka W, Koperny M. Vortioxetine: a review of the pharmacology and clinical profile of the novel antidepressant. Pharmacol Rep. 2017;69:595–601. doi: 10.1016/j.pharep.2017.01.030. [PubMed] [CrossRef] [Google Scholar]
28. Wilson S, Hojer AM, Buchberg J, Areberg J, Nutt DJ. Differentiated effects of the multimodal antidepressant vortioxetine on sleep architecture: part 1, a pharmacokinetic/pharmacodynamic comparison with paroxetine in healthy men. J Psychopharmacol. 2015;29:1085–1091. doi: 10.1177/0269881115599387. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
J Psychopharmacol. 2015;29:1085–1091. doi: 10.1177/0269881115599387. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
29. Rottach KG, Schaner BM, Kirch MH, Zivotofsky AZ, Teufel LM, Gallwitz T, Messer T. Restless legs syndrome as side effect of second generation antidepressants. J Psychiatr Res. 2008;43:70–75. doi: 10.1016/j.jpsychires.2008.02.006. [PubMed] [CrossRef] [Google Scholar]
30. Narowska D, Bozek M, Krysiak K, Antczak J, Holka-Pokorska J, Jernajczyk W, Wichniak A. Frequent difficulties in the treatment of restless legs syndrome—case report and literature review. Psychiatr Pol. 2015;49:921–930. doi: 10.12740/PP/35395. [PubMed] [CrossRef] [Google Scholar]
31. Buschkamp JA, Frohn C, Juckel G. Mirtazapine induces nightmares in depressed patients. Pharmacopsychiatry. 2017. [PubMed]
32. Szaulińska K, Pływaczewski R, Sikorska O, Holka-Pokorska J, Wierzbicka A, Wichniak A, Sliwinski P. Obstructive sleep apnea in severe mental disorders. Psychiatr Pol. 2015;49:883–895.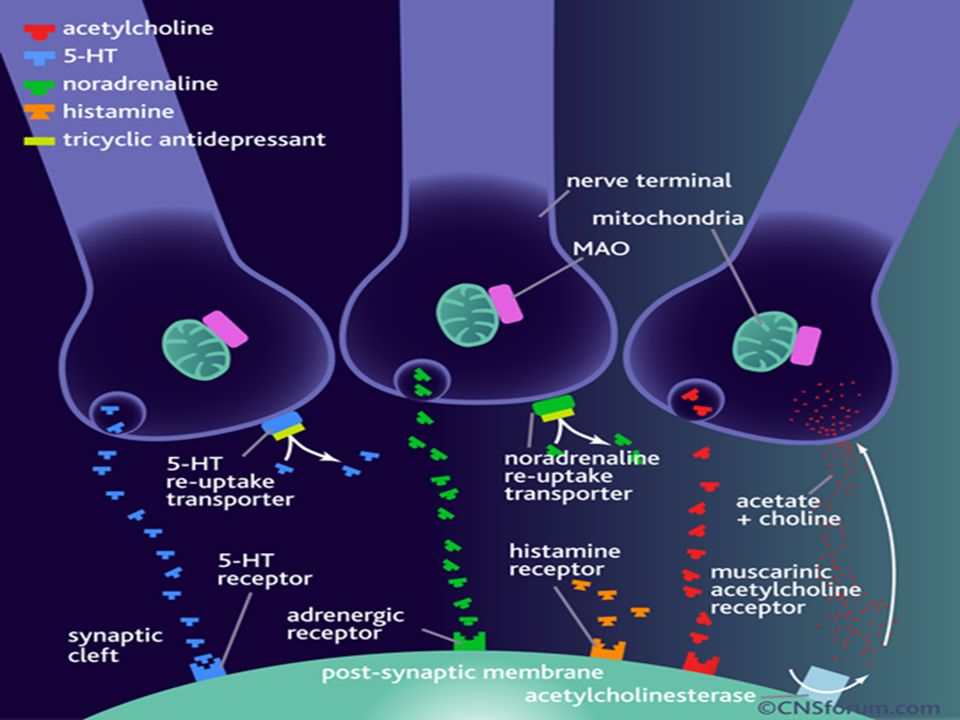 doi: 10.12740/PP/32566. [PubMed] [CrossRef] [Google Scholar]
doi: 10.12740/PP/32566. [PubMed] [CrossRef] [Google Scholar]
33. Wittchen HU, Jacobi F, Rehm J, Gustavsson A, Svensson M, Jonsson B, Olesen J, Allgulander C, Alonso J, Faravelli C, Fratiglioni L, Jennum P, Lieb R, Maercker A, van OJ PM, Salvador-Carulla L, Simon R, Steinhausen HC. The size and burden of mental disorders and other disorders of the brain in Europe 2010. Eur Neuropsychopharmacol. 2011;21:655–679. doi: 10.1016/j.euroneuro.2011.07.018. [PubMed] [CrossRef] [Google Scholar]
34. Ohayon MM. Epidemiology of insomnia: what we know and what we still need to learn. Sleep Med Rev. 2002;6:97–111. doi: 10.1053/smrv.2002.0186. [PubMed] [CrossRef] [Google Scholar]
35. Nowicki Z, Grabowski K, Cubala WJ, Nowicka-Sauer K, Zdrojewski T, Rutkowski M, Bandosz P. Prevalence of self-reported insomnia in general population of Poland. Psychiatr Pol. 2016;50:165–173. doi: 10.12740/PP/58771. [PubMed] [CrossRef] [Google Scholar]
36. Qaseem A, Kansagara D, Forciea MA, Cooke M, Denberg TD. Management of chronic insomnia disorder in adults: a clinical practice guideline from the American College of Physicians. Ann Intern Med. 2016;165:125–133. doi: 10.7326/M15-2175. [PubMed] [CrossRef] [Google Scholar]
Management of chronic insomnia disorder in adults: a clinical practice guideline from the American College of Physicians. Ann Intern Med. 2016;165:125–133. doi: 10.7326/M15-2175. [PubMed] [CrossRef] [Google Scholar]
37. Sateia MJ, Buysse DJ, Krystal AD, Neubauer DN, Heald JL. Clinical practice guideline for the pharmacologic treatment of chronic insomnia in adults: an American Academy of sleep medicine clinical practice guideline. J Clin Sleep Med. 2017;13:307–349. doi: 10.5664/jcsm.6470. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
38. Bonnet MH, Arand DL. Hyperarousal and insomnia: state of the science. Sleep Med Rev. 2010;14:9–15. doi: 10.1016/j.smrv.2009.05.002. [PubMed] [CrossRef] [Google Scholar]
39. Riemann D, Spiegelhalder K, Feige B, Voderholzer U, Berger M, Perlis M, Nissen C. The hyperarousal model of insomnia: a review of the concept and its evidence. Sleep Med Rev. 2010;14:19–31. doi: 10.1016/j.smrv.2009.04.002. [PubMed] [CrossRef] [Google Scholar]
40. Mendelson WB, Roth T, Cassella J, Roehrs T, Walsh JK, Woods JH, Buysse DJ, Meyer RE. The treatment of chronic insomnia: drug indications, chronic use and abuse liability. Summary of a 2001 new clinical drug evaluation unit meeting symposium. Sleep Med Rev. 2004;8:7–17. doi: 10.1016/S1087-0792(03)00042-X. [PubMed] [CrossRef] [Google Scholar]
Mendelson WB, Roth T, Cassella J, Roehrs T, Walsh JK, Woods JH, Buysse DJ, Meyer RE. The treatment of chronic insomnia: drug indications, chronic use and abuse liability. Summary of a 2001 new clinical drug evaluation unit meeting symposium. Sleep Med Rev. 2004;8:7–17. doi: 10.1016/S1087-0792(03)00042-X. [PubMed] [CrossRef] [Google Scholar]
41. Wiegand MH. Antidepressants for the treatment of insomnia : a suitable approach? Drugs. 2008;68:2411–2417. doi: 10.2165/0003495-200868170-00001. [PubMed] [CrossRef] [Google Scholar]
42. Wilson SJ, Nutt DJ, Alford C, Argyropoulos SV, Baldwin DS, Bateson A, Britton T, Crowe C, Dijk DJ, Espie C, Gringras P, Hajak G, Idzikowski C, Krystal A, Nash JR, Selsick H, Sharpley AL, Wade AG. British Association for Psychopharmacology consensus statement on evidence-based treatment of insomnia, parasomnias and circadian rhythm disorders. J Psychopharmacol. 2010;24:1577–1601. doi: 10.1177/0269881110379307. [PubMed] [CrossRef] [Google Scholar]
43. Liu Y, Xu X, Dong M, Jia S, Wei Y. Treatment of insomnia with tricyclic antidepressants: a meta-analysis of polysomnographic randomized controlled trials. Sleep Med. 2017;34:126–133. doi: 10.1016/j.sleep.2017.03.007. [PubMed] [CrossRef] [Google Scholar]
Liu Y, Xu X, Dong M, Jia S, Wei Y. Treatment of insomnia with tricyclic antidepressants: a meta-analysis of polysomnographic randomized controlled trials. Sleep Med. 2017;34:126–133. doi: 10.1016/j.sleep.2017.03.007. [PubMed] [CrossRef] [Google Scholar]
44. Thompson W, Quay TA, Rojas-Fernandez C, Farrell B, Bjerre LM. Atypical antipsychotics for insomnia: a systematic review. Sleep Med. 2016;22:13–17. doi: 10.1016/j.sleep.2016.04.003. [PubMed] [CrossRef] [Google Scholar]
45. Wichniak A, Jarkiewicz M, Okruszek L, Wierzbicka A, Holka-Pokorska J, Rybakowski JK. Low risk for switch to mania during treatment with sleep promoting antidepressants. Pharmacopsychiatry. 2015;48:83–88. doi: 10.1055/s-0034-1396802. [PubMed] [CrossRef] [Google Scholar]
46. Jernajczyk W, Sobańska A, Wierzbicka A, Wichniak A, Szatkowska E. The therapy of primary insomnia with citalopram. J Sleep Res. 2006;15(Suppl. 1):154. [Google Scholar]
SIDE EFFECTS OF ANTIDEPRESSANTS (SSRIs) | Clinical Center "Psychiatry - Narcology"
Currently, the most commonly prescribed antidepressants are drugs from the group of selective serotonin reuptake inhibitors (SSRIs).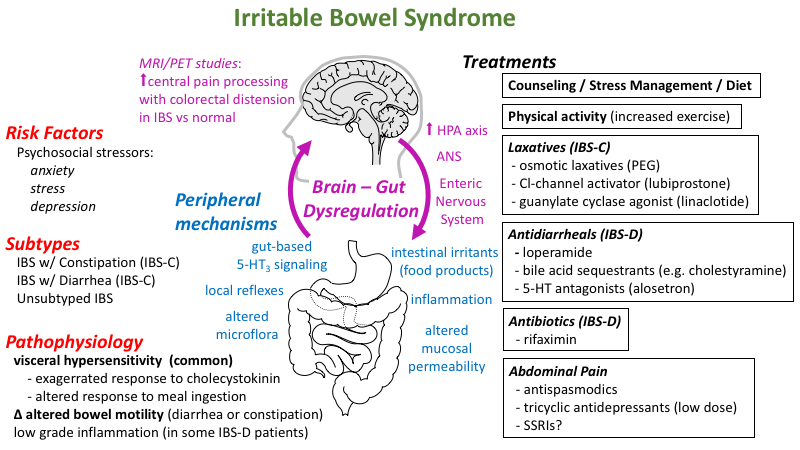 For most, these medicines are safe and effective, but like all medicines, they can cause side effects. According to statistics, about 40% of patients taking antidepressants also experience side effects, in about 25% of cases they are quite unpleasant. Two of the most common side effects (sexual dysfunction and weight gain) are often the reason people stop taking these medications. nine0003
For most, these medicines are safe and effective, but like all medicines, they can cause side effects. According to statistics, about 40% of patients taking antidepressants also experience side effects, in about 25% of cases they are quite unpleasant. Two of the most common side effects (sexual dysfunction and weight gain) are often the reason people stop taking these medications. nine0003
Listed below are the 7 most common side effects of antidepressants that patients should be aware of:
1. SOMATIC SYMPTOMS.
When medications are first prescribed to treat depression, the most common physical symptoms are headache, nausea, joint and muscle pain, rash, and diarrhea. These symptoms are usually mild and temporary. The results of clinical studies have shown that nausea and headache are the most common. As a rule, these symptoms are adaptive in nature, as a rule, they pass on their own, without requiring discontinuation of the drug. nine0003
2. SLEEP DISTURBANCE.
SLEEP DISTURBANCE.
Many patients, when first prescribed antidepressants, report problems with sleep: difficulty falling asleep or light sleep with frequent awakenings. Also, against the background of taking SSRIs, nightmares and sleepwalking can be observed. Studies have shown that about 22% of people taking antidepressants experience sleep problems.
3. DAY SLEEPNESS .
Sleepiness during the day may be the result of a poor night's sleep, or the direct sedative effect of the antidepressant. In the case when it is a sedative effect, the problem can be solved by transferring the drug to the evening. nine0003
4. MIGRAINES
Due to the fact that people who are prone to depression also often suffer from migraines, you need to be careful when taking medications in combination. Medicines; used to treat migraines, triptans, like SSRIs, increase serotonin levels in the brain. If these drugs are used together, it can lead to the development of serotonin syndrome, which manifests itself in the form of headache, heart palpitations, hot flashes. Be sure to discuss with your doctor how to avoid the development of serotonin syndrome if you are prescribed medications of both groups. nine0003
Be sure to discuss with your doctor how to avoid the development of serotonin syndrome if you are prescribed medications of both groups. nine0003
5. WEIGHT SET.
Weight gain is one of the late side effects of antidepressants and is one of the most common reasons for refusing to continue taking or changing the drug. A good prevention of this side effect is moderate physical activity (for example, a 30-minute workout every other day). The likelihood of weight gain also depends on the drug that is prescribed. According to clinical trials, while taking paroxetine, about 25% of patients gain 7% of their weight. nine0003
6. SUICIDE .
The risk of suicide while taking antidepressants is currently under extensive investigation. According to most studies, compared with placebo, taking SSRIs or other antidepressants doubles the likelihood of suicidal thoughts. The overall risk of this side effect when taking antidepressants in adolescents and adults is 2 to 4 percent.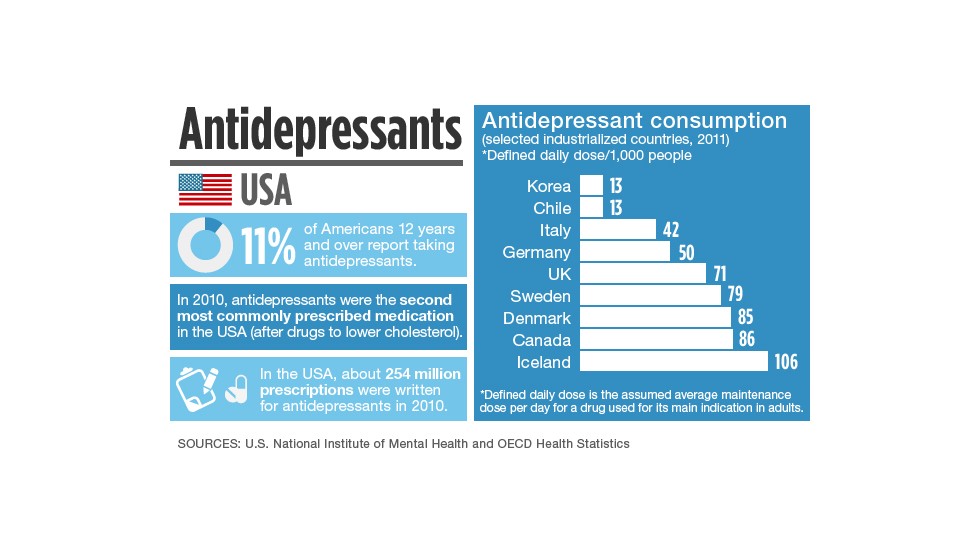 One of the reasons for suicide while taking antidepressants is that medications increase activity, giving energy for the implementation of a suicidal plan. Regular follow-up by a doctor can reduce the risk of this side effect. nine0003
One of the reasons for suicide while taking antidepressants is that medications increase activity, giving energy for the implementation of a suicidal plan. Regular follow-up by a doctor can reduce the risk of this side effect. nine0003
7. SEXUAL DYSFUNCTION.
Sexual dysfunction is one of the most common long-term side effects of SSRIs. These include decreased sexual desire, delayed ejaculation in men, and inability to achieve orgasm in women. Up to 60% of people taking SSRIs experience one of these side effects. And these are the side effects that patients are not ready to endure.
If you are concerned about any side effects, discuss them with your doctor. As a rule, you can find a solution for any of them. It is not recommended to stop taking medications on your own. nine0003
whether they help, treat or relieve symptoms, cause addiction, make them gain weight
Daniil Davydov
medical journalist
Author profile
million people.
At the same time, the cures for this disease are surrounded by many myths. Antidepressants are accused of ineffectiveness and severe side effects, but often the problem is not with the drugs themselves, but with their misuse. nine0003
We collected 8 myths about antidepressants and found out how close they are to the truth.
Go see a doctor
Our articles are written with love for evidence-based medicine. We refer to authoritative sources and go to doctors with a good reputation for comments. But remember: the responsibility for your health lies with you and your doctor. We don't write prescriptions, we make recommendations. Relying on our point of view or not is up to you.
Myth 1
Antidepressants almost never help nine0065 Most likely, this myth arose due to the fact that antidepressants do not work in all patients - so even some doctors and scientists doubt their effectiveness. However, antidepressants cannot be called ineffective, there are just important nuances in the use of these drugs.
Antidepressants are a class of drugs that normalize the level of neurotransmitters, that is, chemicals that help nerve cells in the brain exchange information.
What are Antidepressants - International Drug Database RxLis
What Medications Help Clinical Depression in Adults - International Primer for Physicians UpToDate
How Antidepressants Help Pain - Mayo Clinic Bulletin
All Antidepressants Used to Treat Depression in Adults , work - The Lancet
Who Antidepressants Help and Who Don't - Clinical Guidelines for British PhysiciansPDF, 141 KB
These medicines help people whose problems are due to a deficiency or excess of neurotransmitters. Antidepressants reduce symptoms of depression, obsessive-compulsive disorder, generalized anxiety disorder, post-traumatic stress disorder, and bipolar affective disorder.
There is evidence that antidepressants are effective for chronic pain. Antidepressants increase the amount of neurotransmitters in the spinal cord, which reduces pain signals. nine0003
nine0003
Most specialists have no doubts that antidepressants work. For example, according to the British Royal College of Psychiatry, 50-65% of people with depression who take antidepressants feel better - compared with 25-30% of those who take a placebo.
However, there are situations where the benefit of antidepressants is questionable. For example, antidepressants are good for treating moderate to severe depression, but do not work well for people with mild depression - psychotherapy is more suitable for them. nine0003
And there are situations when these medicines were prescribed by mistake. Then antidepressants really won't help.
When antidepressants don't help
Sergey Divisenko
psychotherapist
There are three cases when antidepressants most often cause problems.
The antidepressant didn't work because the doctor prescribed the wrong dose. Minimum doses of these drugs do not help in half of the cases. Then competent doctors increase the doses to those recommended in clinical guidelines, while illiterate ones refuse them. nine0003
nine0003
Sometimes, in order for antidepressants to work, they need to be augmented—i.e., enhanced—with other classes of drugs. For example, second-generation antipsychotics, or normothymics, that is, drugs that stabilize mood. If this is not done, the person taking antidepressants will not feel relief.
The antidepressant didn't work because the doctor misdiagnosed and was trying to treat a condition that these drugs don't work for. To help a person, one had to either use other drugs or use non-drug methods of treatment: for example, psychotherapy, transcranial stimulation, or electroconvulsive therapy. nine0003
For example, in bipolar disorder, symptoms can be very similar to depression or anxiety. But with bipolar disorder, antidepressants help only if they are used together with other drugs - mood stabilizers. By themselves, they will either work for a short time, or they will not work, or they can cause a phase inversion - that is, a person will switch from a depressive phase to a manic one.
The patient was not helped by a particular antidepressant, but another might. nine0008 Antidepressants differ in the principle of action - on this basis they are divided into classes. It happens that one antidepressant does not work, but another from the same or another class helps. If the treatment does not work, you should not stop drug therapy, but continue to look for a drug that will help this particular patient.
Myth 2
Antidepressants only relieve symptoms, but do not eliminate the cause of the disorderIn most cases, this is not a myth. However, in some situations, antidepressants act on the cause of the disorder. nine0003
Depression is a heterogeneous disease. Experts identify a different number of subtypes of depression - from 4 to 12. But for our purposes, depression can be divided into two large subtypes.
American Criteria for Depressive Disorders - A Handbook for Psychiatrists DSM-5PDF, 32 MB
What Depression Is - An International Primer for Physicians UpToDate
associated with depression. Disorders that can be attributed to this group are more common. nine0003
Disorders that can be attributed to this group are more common. nine0003
If these causes affect a person long enough and he does not understand how to deal with them, depression may develop. In this situation, antidepressants act as drugs that alleviate the symptoms of the disease. To influence the cause of the problem, psychotherapy is needed.
Depression provoked by internal causes. Approximately 7% of people with depression have the correct way of thinking, there are no internal conflicts and injuries, and there are no serious illnesses. In this situation, the cause of depression is the lack of neurotransmitters: serotonin, norepinephrine and dopamine in the synapses of brain nerve cells. In such people, the antidepressant acts precisely on the cause of the disease, that is, it corrects the production of serotonin in neuronal synapses. nine0003
Myth 3
As soon as it gets better, you can stop taking the antidepressant This is also not exactly a myth - it would be more correct to call it a belief that is true only for some, but not for all patients with depression.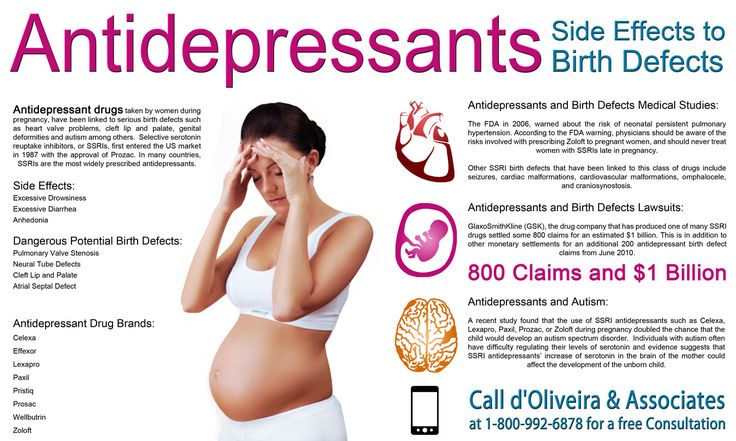
It is generally advised to continue taking antidepressants for at least six months after remission. If the duration of the disease is short, that is, the person was ill for about two weeks, then for the onset of remission, one or two months usually need to take medication. If the duration of the disease is long, from several months or years, then more time is required for the onset of remission. It’s impossible to say exactly how much: different people with depression have different recovery times. nine0003
Some people have recurrent depression. In this case, the period during which you need to take the medicine depends on how many bouts of depression have already been during your life. If more than three, it is recommended to take antidepressants for several years or for life.
Myth 4
Antidepressants cause addiction Perhaps the roots of this myth are that some people need to take depression medication for life. And at the beginning of treatment, some patients have to increase the dose.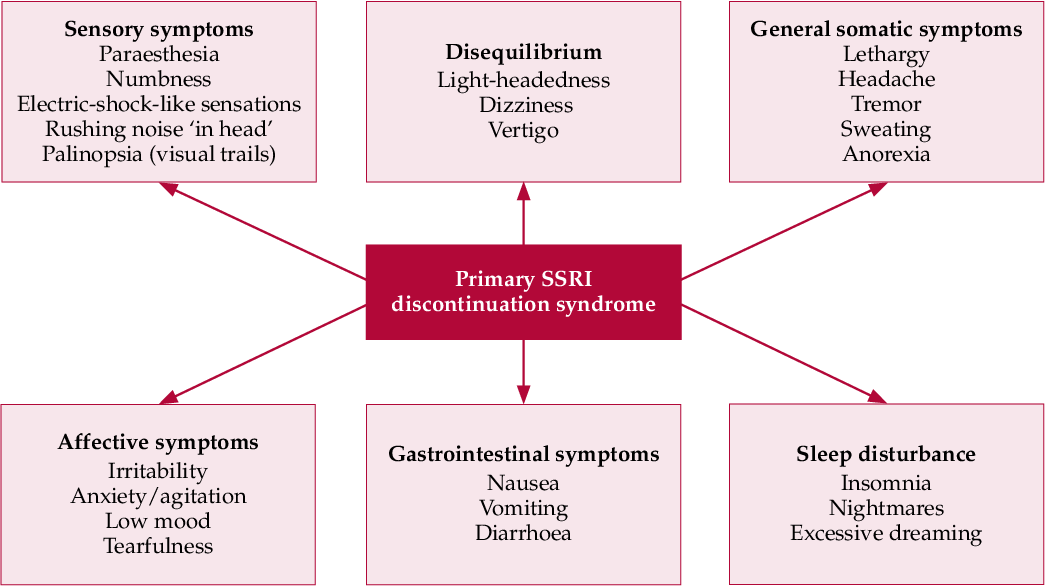 But in fact, antidepressants do not cause either true physical or drug dependence. nine0003
But in fact, antidepressants do not cause either true physical or drug dependence. nine0003
True physical dependence on a drug is a situation where a person becomes so addicted to a drug that when it is withdrawn, the symptoms of the disease sharply increase. People who are dependent on the drug have to increase the dosage, otherwise the drug stops helping.
What is True Drug Addiction—Bulletin of the National Institute for the Study of Drug AbusePDF, 7 MB
What is Drug Addiction—Bulletin of the American Psychiatric Association
Drug dependence may include physical dependence on a drug. But this addiction has a unique feature. Dependence can also develop in a healthy person who used the drug not to recover, but to enjoy it. But when he tries to quit the drug, he still experiences physical suffering, which is called the withdrawal syndrome. As a result, a person is forced to look for a new dose of a drug.
Although a person who takes antidepressants to treat depression gets better, the drugs themselves are neither pleasurable nor addictive.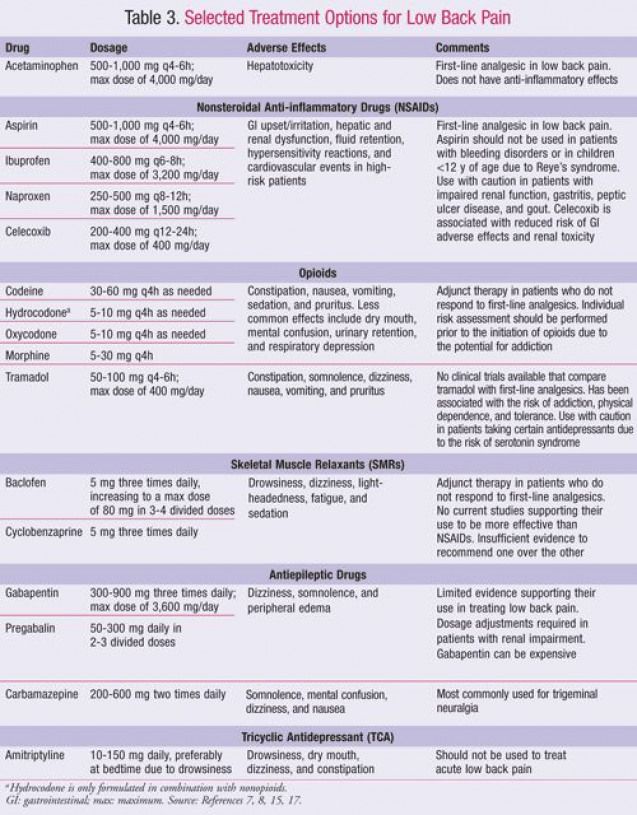 Taking them as drugs is useless.
Taking them as drugs is useless.
Of all the drugs that are used in psychiatry, true physical dependence can only be caused by psychostimulants that activate mental activity and anti-anxiety, that is, benzodiazepine tranquilizers. Antidepressants are not included in this list, because there is no need to increase the dosage of correctly selected drugs from this group. nine0003
However, some people who stop taking antidepressants early sometimes experience withdrawal symptoms such as nausea, hand tremors, and some feel “shocks” in the head, similar to the sensations of an electric shock. Depressive symptoms return to patients who need to take the medicine for a very long time.
Antidepressants are sometimes abused, but they cannot cause addiction - Journal of Modern Psychiatry
To avoid unpleasant consequences, stop taking antidepressants only if the attending physician says that they are no longer needed. But even in this situation, it is necessary to cancel antidepressants slowly, that is, gradually reducing the dose.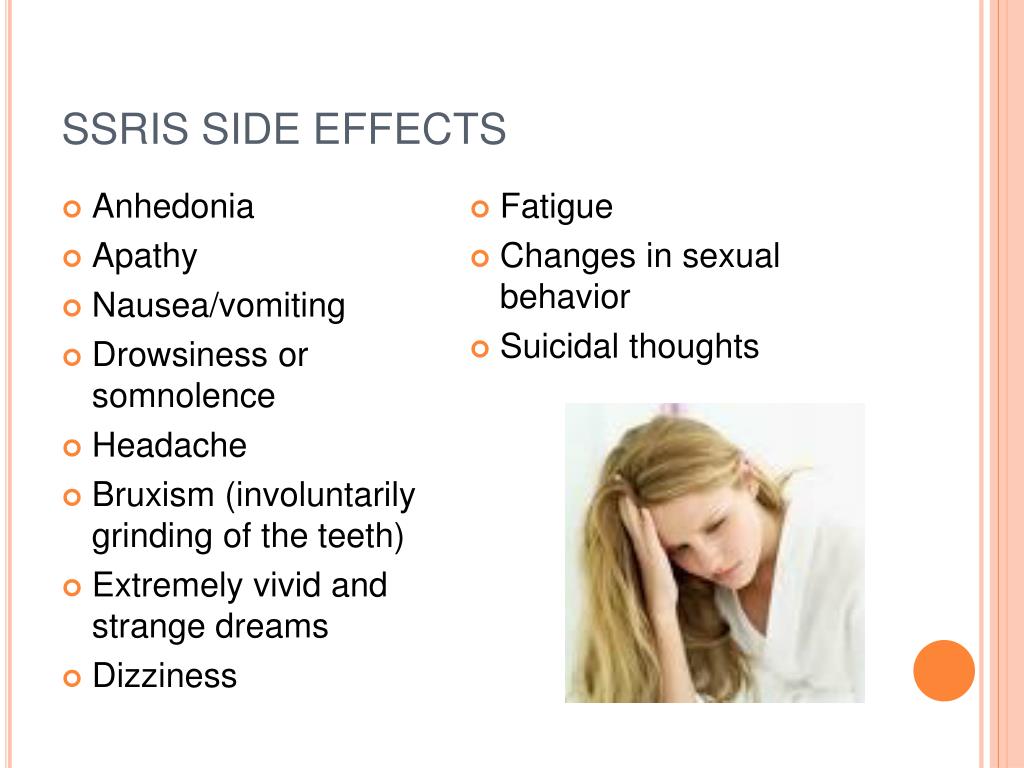 This will help avoid unpleasant side effects. nine0003
This will help avoid unpleasant side effects. nine0003
Myth 5
A person on antidepressants becomes lethargic and loses interest in lifeThis popular myth is based on real but outdated data.
These mental changes are seen in patients taking first-generation tricyclic antidepressants such as amitriptyline. It has a sedative, that is, a sedative effect. A person who takes high doses of amitriptyline can indeed become sleepy and indifferent to the outside world. nine0003
Amitriptyline - Sedative - Drugs.com International Drug Database
SSRIs do not sedate - Drugs.com International Drug Database
Current second-generation antidepressants that are recommended to start treatment with, such as selective serotonin reuptake inhibitors, or SSRIs almost never cause drowsiness and apathy.
On the contrary, in most people with depression they return interest in life. nine0003
Sometimes SSRIs do cause drowsiness, but this has not yet been proven
Sergey Divisenko
psychotherapist
It is believed that in rare cases, modern antidepressants can provoke SSRI-induced apathy. But this condition is extremely rare.
But this condition is extremely rare.
And even then psychiatrists still doubt that the cause is precisely in the drugs, and not in the patient's condition. After all, some people during the time of taking antidepressants may develop other adverse mental states in which apathy occurs: for example, schizotypal disorder, which was not noticed before. nine0003
Myth 6
Antidepressants have many side effectsThis is partly true: both SSRIs and antidepressants from other groups have side effects. But it is quite possible to deal with them.
At the beginning of treatment, when people first start taking antidepressants, many complain of increased anxiety, dry mouth, nausea, and trouble sleeping. But after a few days or weeks after the start of the course of treatment, these symptoms usually disappear. If the side effects do not stop, it makes sense to consult a doctor - he will replace the antidepressant. nine0003
Dealing with antidepressant side effects - tips from the Mayo Clinic staff
Here's what to do before the side effects go away:
- take your antidepressant with meals, unless the instructions say otherwise, so the antidepressant will be less annoying stomach;
- put a bottle of clean water on the desktop - if your mouth is dry, you can take a sip.
 Unsweetened lollipops and chewing gum also help with dry mouth; nine0216
Unsweetened lollipops and chewing gum also help with dry mouth; nine0216 - take a walk for at least half an hour before going to bed - this will make it easier to fall asleep. If you can’t sleep at all, you can ask your doctor to pick up sleeping pills.
The second most common side effect is increased anxiety at the start of antidepressant use. To avoid this problem, psychiatrists resort to two effective methods:
- titrate the dose - that is, start with the minimum dose of the antidepressant and then gradually increase it;
- at the beginning of the reception, sedatives - tranquilizers are prescribed together with the antidepressant. nine0216
The third common side effect of SSRIs, especially sertraline, known as Zoloft, and escitalopram, better known as Cipralex, is decreased libido. Approximately 20-30% of people taking antidepressants from this group experience a decrease in sexual desire to one degree or another. At the same time, it is difficult to say how much the drugs are to blame, because approximately 35-50% of people with depression have already experienced sexual dysfunction.
Many people with depression experience sexual dysfunction before starting antidepressants - Harvard Medical School Bulletin
Switching to another antidepressant usually helps, but many people prefer to wait until the medication can be stopped. In some cases, psychiatrists prescribe antidepressants from other groups in addition to the libido-lowering antidepressant. Sometimes it helps to regain interest in sex.
Myth 7
Weight gain due to antidepressantsThis is not a myth, but a half-truth. There are both antidepressants that contribute to weight gain, and those that do not have a similar effect. nine0003
The most common complaint about weight gain during treatment is people taking the tetracyclic antidepressant mirtazapine, which actually increases appetite. Another weight gaining antidepressant is paroxetine, better known by the trade name Paxil. But "Zoloft" and "Cipralex" do not contribute to weight gain.
If a patient feels that an antidepressant is causing them to overeat, it is wise to consult a doctor and discuss a change of drug. nine0003
nine0003
Myth 8
Antidepressants are expensiveTrue, but not for all patients. Most people can cure depression and not go broke.
Antidepressants from different groups vary greatly in price. There are both very expensive drugs and relatively low-cost drugs among them. At the same time, both of them work equally well. However, there are situations when a cheap antidepressant cannot be dispensed with.
On the left - inexpensive "Zoloft" for 327 R, a drug based on sertraline, on the right - the most expensive antidepressant "Ixel" based on milnacipran for 2453 R For example, there is a good antidepressant venlafaxine. The maximum dose of venlafaxine can reach up to 375 mg per day. If these are inexpensive tablets of a domestic manufacturer, then a course of treatment for a month costs about 2000 R. But sometimes inexpensive tablets are not very well tolerated: they cause headache, nausea, sweating, tachycardia, that is, rapid heartbeat. In such cases, you need to switch to a prolonged form of venlafaxine - "Venlafaxine Retard", or "Velaxin XR".