Dissociative identity disorder types
Causes, Symptoms, Types & Treatment
Overview
What are dissociative disorders?
Dissociative disorders are mental health conditions that involve feelings of being detached from reality, being outside of your own body or experiencing memory loss (amnesia).
The word “dissociation” means to be disconnected from others, from the world around you or from yourself.
Dissociative disorders typically develop after short-term or long-term trauma.
Types of dissociative disorders
The three types of dissociative disorders include:
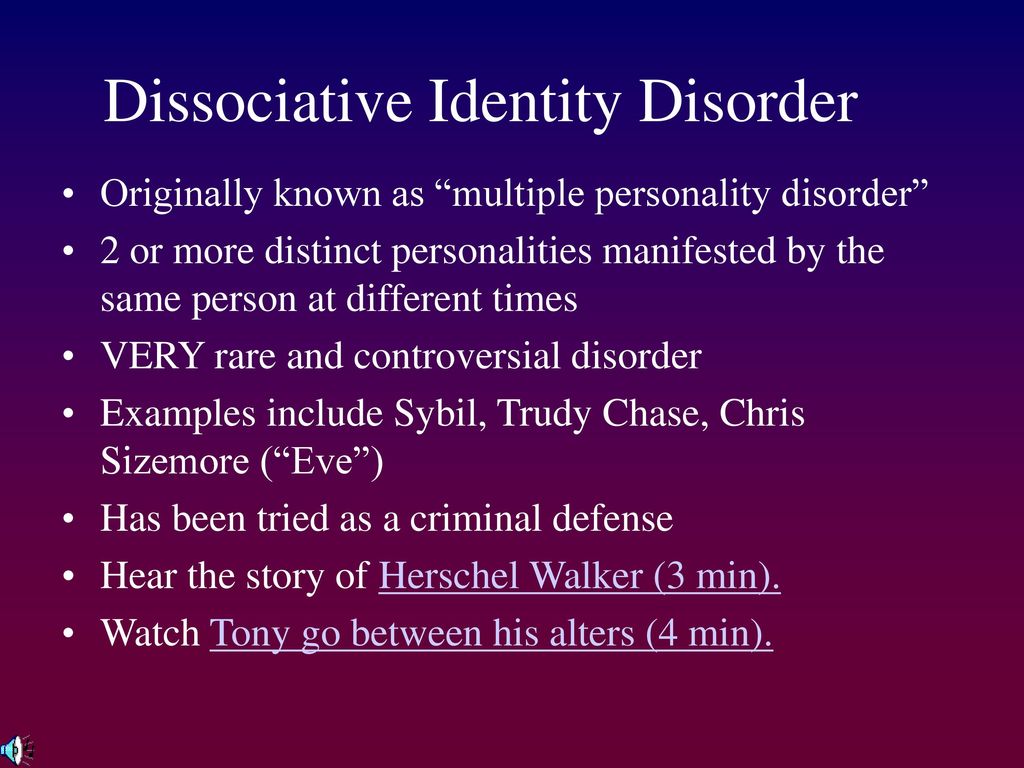
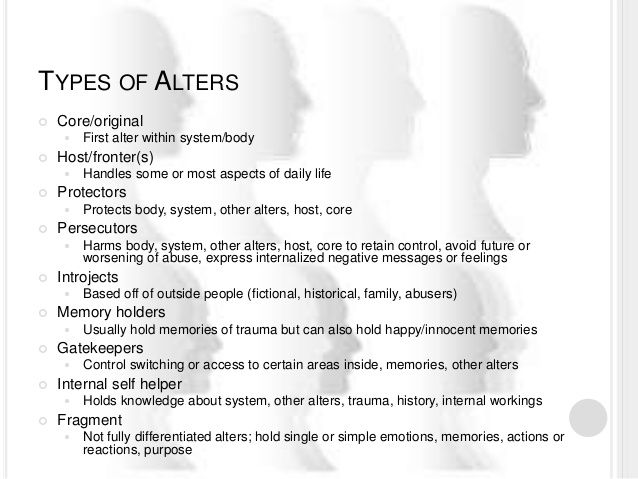
- Dissociative identity disorder (DID): People with DID have two or more separate identities. These identities (called “alters”) control their behavior at various times. Each alter has its own personal history, traits, likes and dislikes.
- Dissociative amnesia: This condition happens when you can’t remember essential information about your life. The forgetting may be limited to specific aspects of your life or may include much of your life history and/or identity.
- Depersonalization/derealization disorder: This is a condition in which you feel detached from your thoughts, feelings and body (depersonalization), and/or disconnected from your environment (derealization).
There’s also a symptom called dissociative fugue. It’s a temporary mental state in which a person has memory loss and ends up in an unexpected place.
Because dissociative disorders appear on the trauma spectrum, many people with a dissociative disorder may have co-occurring trauma-related mental health conditions, such as:
- Post-traumatic stress disorder (PTSD).
- Borderline personality disorder (BPD).
- Substance use disorders.
- Depression.
- Anxiety disorders.
Who do dissociative disorders affect?
People of all ages and racial, ethnic and socioeconomic backgrounds can develop a dissociative disorder. Women and people assigned female at birth are more likely to have a diagnosis.
People who experienced physical and/or sexual abuse in childhood have the greatest risk of developing dissociative identity disorder (DID). About 90% of people who have DID in the United States, Canada and Europe experienced childhood abuse and neglect.
How common are dissociative disorders?
Dissociative disorders are rare. About 2% of people in the United States have them.
Symptoms and Causes
What are the symptoms of dissociative disorders?
The symptoms of dissociative disorders depend on the type. Symptoms usually first develop after a traumatic event.
Stressful situations can worsen symptoms and cause issues with daily functioning.
Symptoms of dissociative identity disorder (DID)
A person with DID has two or more distinct identities. The “core” identity is the person’s usual personality. “Alters” are the person’s alternate personalities. The core is the identity you had before developing DID and alters.
Each alter has a particular set of behaviors, attitudes, preferences, memories and ways of thinking. Other people may be able to tell the difference between the alters, as well as the person with DID. Shifting from one alter to another is involuntary and sudden.
Other people may be able to tell the difference between the alters, as well as the person with DID. Shifting from one alter to another is involuntary and sudden.
Another symptom of DID is ongoing gaps in memory about everyday events, personal information and/or past traumatic events.
These symptoms can range widely in severity. For some people, the condition minimally interferes with their life. For others, it causes significant issues.
Symptoms of dissociative amnesia
In dissociative amnesia, the main symptom is an episode of amnesia (memory loss) that comes on suddenly. It can last months or years.
There are three types of amnesia:
- Localized: You can’t remember an event or period of time (the most common form of amnesia).
- Selective: You can’t remember certain details of events within a given period of time.
- Generalized: You can’t remember anything about your identity and life history (the rarest form).

You may not be aware of your memory loss or have only a little awareness. But loved ones usually recognize the memory loss.
Symptoms of depersonalization/derealization disorder
The symptoms of depersonalization/derealization disorder include experiencing one or both of the following episodes in a recurring pattern over a lengthy period of time:
- Depersonalization: This involves feelings of unreality or of being detached from your mind, body or self. It feels as if you’re observing your life and the events from afar rather than being an active participant.
- Derealization: This involves feelings of unreality or of being detached from your surroundings. People and things may not seem real.
During these episodes, you’re aware of your surroundings and know that what you’re experiencing isn’t normal.
These symptoms may start as early as childhood. The average age of the first episode is 16. Fewer than 20% of people with this condition will have their first episode after age 20.
What causes dissociative disorders?
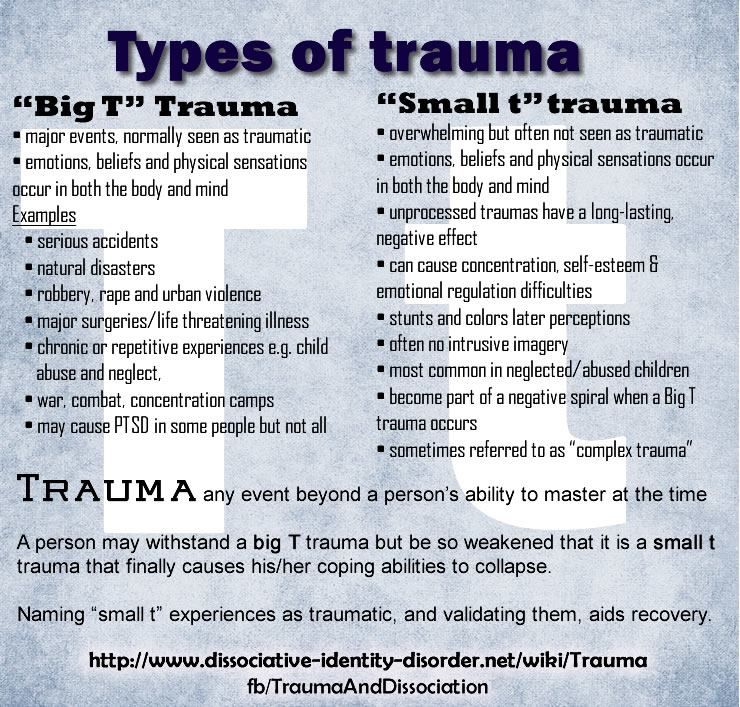
Dissociative disorders often develop as a way to deal with a catastrophic event or with long-term stress, abuse or trauma.
This is particularly true if such events take place early in childhood. At this time of life, there are limitations to your ability to fully understand what’s happening. In addition, your coping mechanisms aren’t fully developed and getting support and resources depends on the presence of caring and knowledgeable adults.
Mentally removing yourself from a traumatic situation can be a coping mechanism that helps you escape pain in the short term. This coping mechanism can become an issue if it continues to separate you from reality and removes memories of entire periods of time.
Traumatic situations may include:
- Repeated physical, mental or sexual abuse.
- An accident.
- A natural disaster.
- Military combat.
- Being a victim of a crime.
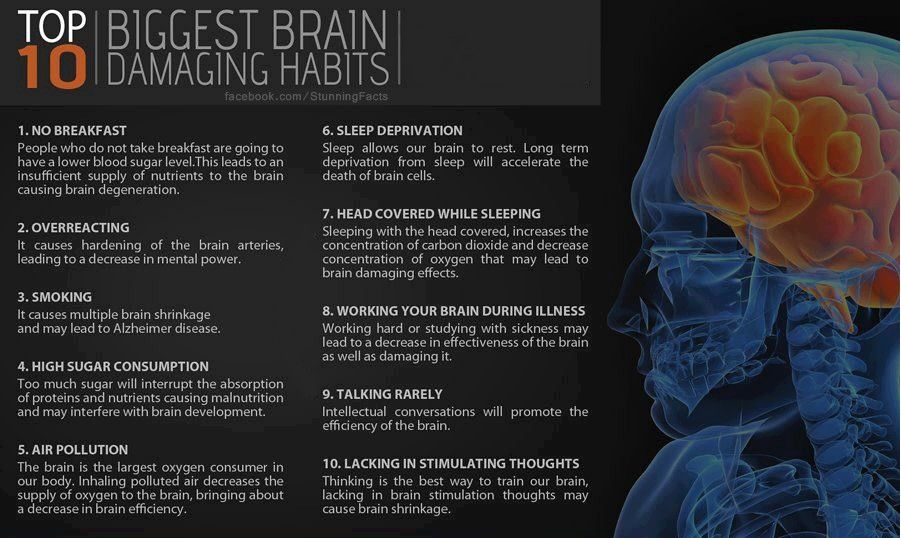
Scientists have recently been studying specific brain structures and functions that are related to dissociation. So far, they’ve found that during dissociation, structures in the memory regions deep in your brain show rhythmic activity but seem disconnected from other regions responsible for thought and planning.
So far, they’ve found that during dissociation, structures in the memory regions deep in your brain show rhythmic activity but seem disconnected from other regions responsible for thought and planning.
Diagnosis and Tests
How are dissociative disorders diagnosed?
Healthcare providers diagnose dissociative disorders by assessing your symptoms and personal history.
Your provider may order tests to rule out possible medical conditions that can cause similar symptoms (such as memory loss), including:
- Head injury.
- Brain tumors.
- Sleep deprivation.
- Substance and/or alcohol use.
Once they rule out possible causes, they’ll likely refer you to a mental health specialist, such as a psychologist, to make a diagnosis through clinical interview and observations.
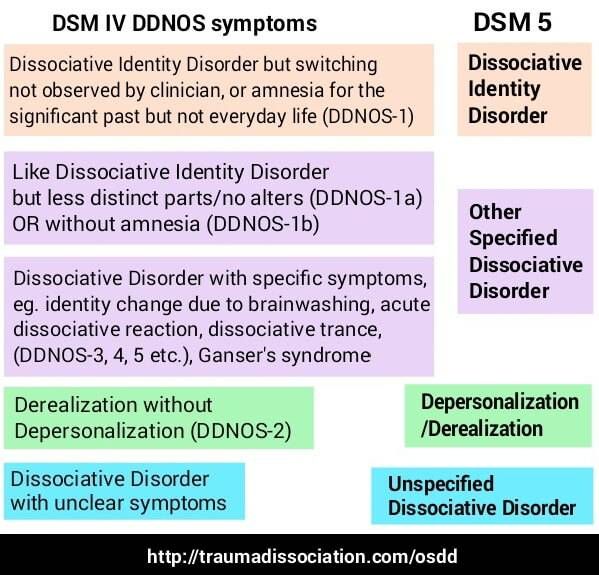
Mental health professionals use criteria in the American Psychiatric Association’s Diagnostic and Statistical Manual of Mental Disorders to diagnose specific dissociative disorders.
Management and Treatment
How are dissociative disorders treated?
Treatment of dissociative disorders usually consists of psychotherapy (talk therapy) to help you gain control over the dissociative process and symptoms.
Psychotherapy takes place with a trained, licensed mental health professional, such as a psychologist or psychiatrist. It can provide support, education and guidance to you and/or your family to help you function better and increase your well-being.
Specific types of psychotherapy commonly used for dissociative disorders include:
- Cognitive behavioral therapy (CBT): This is a structured, goal-oriented type of psychotherapy. Your therapist or psychologist helps you take a close look at your thoughts and emotions. Through CBT, you can unlearn negative thoughts and behaviors and learn to adopt healthier thinking patterns and habits.
- Dialectical behavior therapy (DBT): DBT is specially adapted for people who experience emotions very intensely.
 The main goal is to strike a balance between validation (acceptance) of who you are and your challenges and the benefits of change. Your therapist will help you learn new skills to improve emotion regulation.
The main goal is to strike a balance between validation (acceptance) of who you are and your challenges and the benefits of change. Your therapist will help you learn new skills to improve emotion regulation.
Therapy can be difficult, as it involves remembering and learning to deal with past trauma. But it can significantly help your symptoms in the long term.
Other therapies that can help include:
- Hypnosis: Hypnosis (hypnotherapy) is a state of deep relaxation and focused concentration. When you’re under hypnosis, this intense level of concentration and focus allows you to ignore ordinary distractions and be more open to guided suggestions to make changes to improve your health.
- EMDR therapy: Eye movement desensitization and reprocessing (EMDR) therapy involves moving your eyes a specific way while you process traumatic memories. EMDR’s goal is to help you heal from trauma or other distressing life experiences. Compared to other therapy methods, EMDR is relatively new.
No specific medications treat dissociative disorders. But your provider may recommend certain medications, such as antidepressants, to treat co-occurring mental health conditions.
Outlook / Prognosis
What is the prognosis for dissociative disorders?
The prognosis (outlook) for dissociative disorders varies.
With professional treatment (usually psychotherapy), many people with a dissociative disorder can address the major symptoms of the condition and improve their daily functioning.
For some people, the dissociative disorder, especially dissociative identity disorder (DID), severely impacts their life.
Suicide attempts and self-harm are common in people with DID. More than 70% of people with DID attempt suicide.
If you or a loved one are thinking about suicide, dial 988 on your phone to reach the Suicide and Crisis Lifeline. Someone will be available to help you 24/7.
Living With
When should I see my healthcare provider?
If you’re experiencing symptoms of a dissociative disorder, talk to a healthcare provider or mental health professional.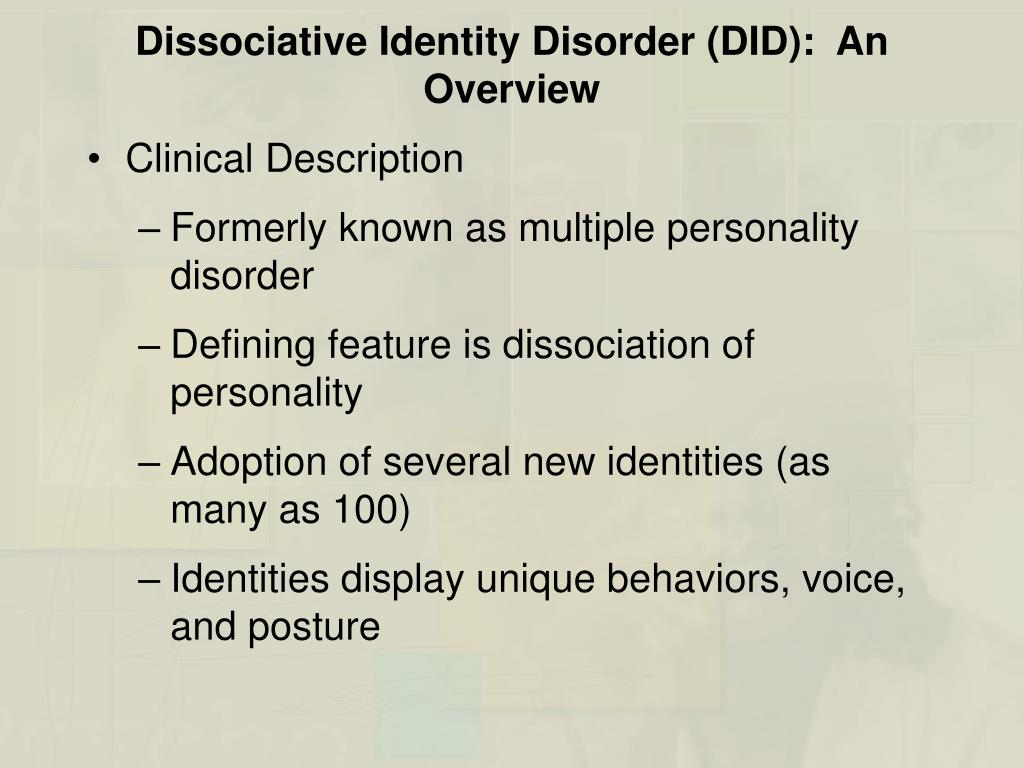
A note from Cleveland Clinic
As with all mental health conditions, seeking help as soon as symptoms appear can help decrease the disruptions to your life. Talk to a healthcare provider if you’re experiencing symptoms of dissociation. Mental health professionals can offer treatment plans that can help you manage your condition.
Causes, Symptoms, Types & Treatment
Overview
What are dissociative disorders?
Dissociative disorders are mental health conditions that involve feelings of being detached from reality, being outside of your own body or experiencing memory loss (amnesia).
The word “dissociation” means to be disconnected from others, from the world around you or from yourself.
Dissociative disorders typically develop after short-term or long-term trauma.
Types of dissociative disorders
The three types of dissociative disorders include:
- Dissociative identity disorder (DID): People with DID have two or more separate identities.
 These identities (called “alters”) control their behavior at various times. Each alter has its own personal history, traits, likes and dislikes.
These identities (called “alters”) control their behavior at various times. Each alter has its own personal history, traits, likes and dislikes. - Dissociative amnesia: This condition happens when you can’t remember essential information about your life. The forgetting may be limited to specific aspects of your life or may include much of your life history and/or identity.
- Depersonalization/derealization disorder: This is a condition in which you feel detached from your thoughts, feelings and body (depersonalization), and/or disconnected from your environment (derealization).
There’s also a symptom called dissociative fugue. It’s a temporary mental state in which a person has memory loss and ends up in an unexpected place.
Because dissociative disorders appear on the trauma spectrum, many people with a dissociative disorder may have co-occurring trauma-related mental health conditions, such as:
- Post-traumatic stress disorder (PTSD).
- Borderline personality disorder (BPD).
- Substance use disorders.
- Depression.
- Anxiety disorders.
Who do dissociative disorders affect?
People of all ages and racial, ethnic and socioeconomic backgrounds can develop a dissociative disorder. Women and people assigned female at birth are more likely to have a diagnosis.
People who experienced physical and/or sexual abuse in childhood have the greatest risk of developing dissociative identity disorder (DID). About 90% of people who have DID in the United States, Canada and Europe experienced childhood abuse and neglect.
How common are dissociative disorders?
Dissociative disorders are rare. About 2% of people in the United States have them.
Symptoms and Causes
What are the symptoms of dissociative disorders?
The symptoms of dissociative disorders depend on the type. Symptoms usually first develop after a traumatic event.
Stressful situations can worsen symptoms and cause issues with daily functioning.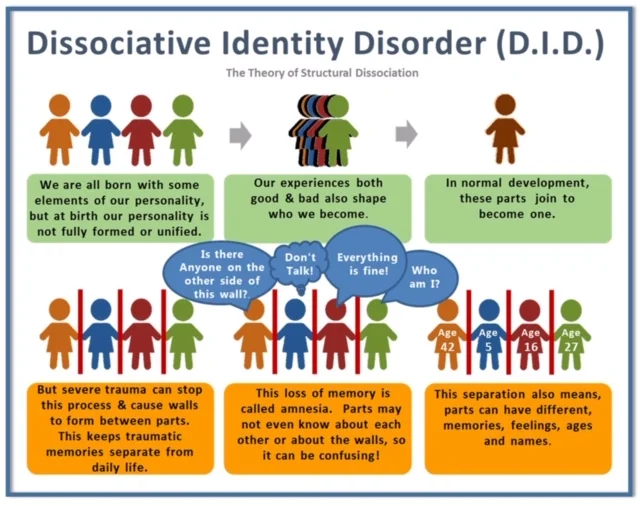
Symptoms of dissociative identity disorder (DID)
A person with DID has two or more distinct identities. The “core” identity is the person’s usual personality. “Alters” are the person’s alternate personalities. The core is the identity you had before developing DID and alters.
Each alter has a particular set of behaviors, attitudes, preferences, memories and ways of thinking. Other people may be able to tell the difference between the alters, as well as the person with DID. Shifting from one alter to another is involuntary and sudden.
Another symptom of DID is ongoing gaps in memory about everyday events, personal information and/or past traumatic events.
These symptoms can range widely in severity. For some people, the condition minimally interferes with their life. For others, it causes significant issues.
Symptoms of dissociative amnesia
In dissociative amnesia, the main symptom is an episode of amnesia (memory loss) that comes on suddenly.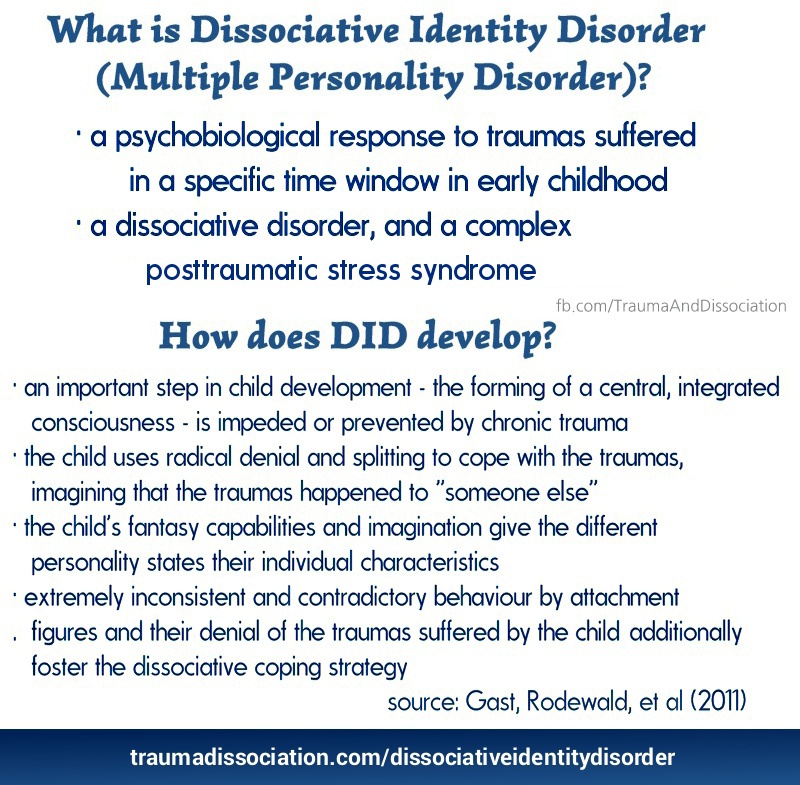 It can last months or years.
It can last months or years.
There are three types of amnesia:
- Localized: You can’t remember an event or period of time (the most common form of amnesia).
- Selective: You can’t remember certain details of events within a given period of time.
- Generalized: You can’t remember anything about your identity and life history (the rarest form).
You may not be aware of your memory loss or have only a little awareness. But loved ones usually recognize the memory loss.
Symptoms of depersonalization/derealization disorder
The symptoms of depersonalization/derealization disorder include experiencing one or both of the following episodes in a recurring pattern over a lengthy period of time:
- Depersonalization: This involves feelings of unreality or of being detached from your mind, body or self. It feels as if you’re observing your life and the events from afar rather than being an active participant.
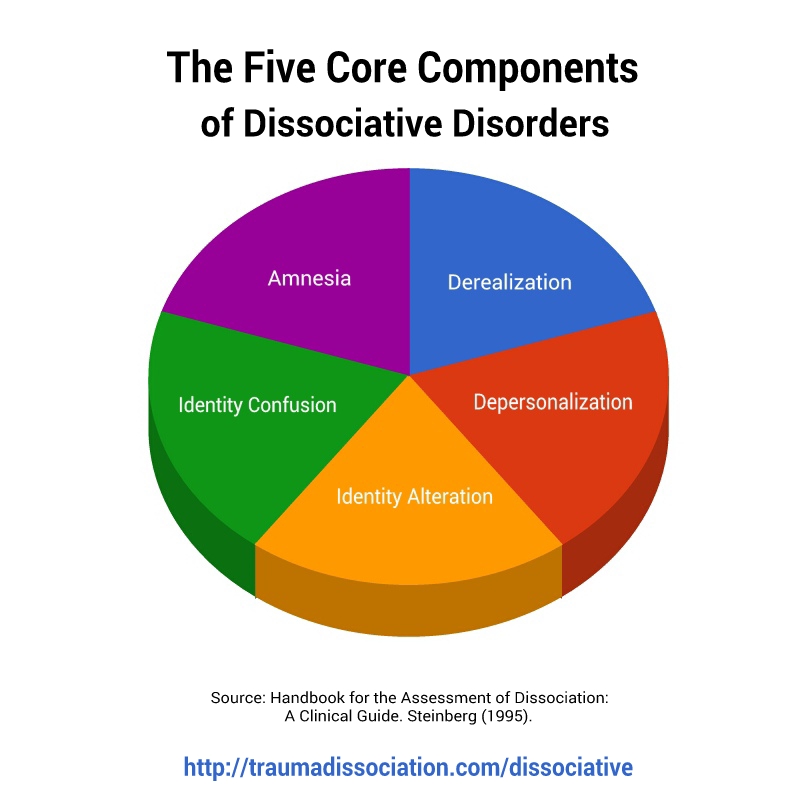
- Derealization: This involves feelings of unreality or of being detached from your surroundings. People and things may not seem real.
During these episodes, you’re aware of your surroundings and know that what you’re experiencing isn’t normal.
These symptoms may start as early as childhood. The average age of the first episode is 16. Fewer than 20% of people with this condition will have their first episode after age 20.
What causes dissociative disorders?
Dissociative disorders often develop as a way to deal with a catastrophic event or with long-term stress, abuse or trauma.
This is particularly true if such events take place early in childhood. At this time of life, there are limitations to your ability to fully understand what’s happening. In addition, your coping mechanisms aren’t fully developed and getting support and resources depends on the presence of caring and knowledgeable adults.
Mentally removing yourself from a traumatic situation can be a coping mechanism that helps you escape pain in the short term. This coping mechanism can become an issue if it continues to separate you from reality and removes memories of entire periods of time.
This coping mechanism can become an issue if it continues to separate you from reality and removes memories of entire periods of time.
Traumatic situations may include:
- Repeated physical, mental or sexual abuse.
- An accident.
- A natural disaster.
- Military combat.
- Being a victim of a crime.
Scientists have recently been studying specific brain structures and functions that are related to dissociation. So far, they’ve found that during dissociation, structures in the memory regions deep in your brain show rhythmic activity but seem disconnected from other regions responsible for thought and planning.
Diagnosis and Tests
How are dissociative disorders diagnosed?
Healthcare providers diagnose dissociative disorders by assessing your symptoms and personal history.
Your provider may order tests to rule out possible medical conditions that can cause similar symptoms (such as memory loss), including:
- Head injury.
- Brain tumors.
- Sleep deprivation.
- Substance and/or alcohol use.
Once they rule out possible causes, they’ll likely refer you to a mental health specialist, such as a psychologist, to make a diagnosis through clinical interview and observations.
Mental health professionals use criteria in the American Psychiatric Association’s Diagnostic and Statistical Manual of Mental Disorders to diagnose specific dissociative disorders.
Management and Treatment
How are dissociative disorders treated?
Treatment of dissociative disorders usually consists of psychotherapy (talk therapy) to help you gain control over the dissociative process and symptoms.
Psychotherapy takes place with a trained, licensed mental health professional, such as a psychologist or psychiatrist. It can provide support, education and guidance to you and/or your family to help you function better and increase your well-being.
Specific types of psychotherapy commonly used for dissociative disorders include:
- Cognitive behavioral therapy (CBT): This is a structured, goal-oriented type of psychotherapy.
 Your therapist or psychologist helps you take a close look at your thoughts and emotions. Through CBT, you can unlearn negative thoughts and behaviors and learn to adopt healthier thinking patterns and habits.
Your therapist or psychologist helps you take a close look at your thoughts and emotions. Through CBT, you can unlearn negative thoughts and behaviors and learn to adopt healthier thinking patterns and habits. - Dialectical behavior therapy (DBT): DBT is specially adapted for people who experience emotions very intensely. The main goal is to strike a balance between validation (acceptance) of who you are and your challenges and the benefits of change. Your therapist will help you learn new skills to improve emotion regulation.
Therapy can be difficult, as it involves remembering and learning to deal with past trauma. But it can significantly help your symptoms in the long term.
Other therapies that can help include:
- Hypnosis: Hypnosis (hypnotherapy) is a state of deep relaxation and focused concentration. When you’re under hypnosis, this intense level of concentration and focus allows you to ignore ordinary distractions and be more open to guided suggestions to make changes to improve your health.
- EMDR therapy: Eye movement desensitization and reprocessing (EMDR) therapy involves moving your eyes a specific way while you process traumatic memories. EMDR’s goal is to help you heal from trauma or other distressing life experiences. Compared to other therapy methods, EMDR is relatively new.
No specific medications treat dissociative disorders. But your provider may recommend certain medications, such as antidepressants, to treat co-occurring mental health conditions.
Outlook / Prognosis
What is the prognosis for dissociative disorders?
The prognosis (outlook) for dissociative disorders varies.
With professional treatment (usually psychotherapy), many people with a dissociative disorder can address the major symptoms of the condition and improve their daily functioning.
For some people, the dissociative disorder, especially dissociative identity disorder (DID), severely impacts their life.
Suicide attempts and self-harm are common in people with DID. More than 70% of people with DID attempt suicide.
More than 70% of people with DID attempt suicide.
If you or a loved one are thinking about suicide, dial 988 on your phone to reach the Suicide and Crisis Lifeline. Someone will be available to help you 24/7.
Living With
When should I see my healthcare provider?
If you’re experiencing symptoms of a dissociative disorder, talk to a healthcare provider or mental health professional.
A note from Cleveland Clinic
As with all mental health conditions, seeking help as soon as symptoms appear can help decrease the disruptions to your life. Talk to a healthcare provider if you’re experiencing symptoms of dissociation. Mental health professionals can offer treatment plans that can help you manage your condition.
What is Dissociative Identity Disorder?
Dissociative Identity Disorder is a mental disorder characterized by either having two or more personalities, or a state of disconnection from the outside world, one's identity, and an inability to recall certain daily life events and important personal information. This disorder is often mistaken for depression, anxiety, or psychosis. Long before our days, this condition was called possession, and it was treated with exorcism. In the 19th century, this disorder was called hysteria, and in the 20th century it was called multiple personality disorder or multiple personality disorder.
This disorder is often mistaken for depression, anxiety, or psychosis. Long before our days, this condition was called possession, and it was treated with exorcism. In the 19th century, this disorder was called hysteria, and in the 20th century it was called multiple personality disorder or multiple personality disorder.
Types of dissociative personality disorder
There are several types of dissociative disorders, which are characterized by different symptoms and manifestations. One of them is dissociative fugue, a disorder in which a person can find himself in a completely unfamiliar place and not remember how he got there. In this case, a person may forget some important information about himself and not even remember his name. At the same time, memory for some information, such as literature, science, and other things, can be preserved. In a state of fugue, a person assumes a different personality and identity with a different character, mannerisms and behavior. While in this identity, a person can lead an outwardly normal life. A dissociative fugue can last for hours or years. After that, a person may find himself in a completely unfamiliar place and at the same time not remember anything that happened to him in a state of fugue.
A person who has a dissociative disorder is actually suffering a lot from their condition.
Another type of dissociative disorder is the presence of several personalities in which a person finds himself in turn or simultaneously. At such moments, he disconnects from himself and stops feeling his own body, and also cannot see himself from the outside. Personalities within a person can have different ages, genders, nationalities, mental abilities, temperaments, and behave in completely different ways. Often these personalities can even have different physiological manifestations. For example, while in one personality, a person can see poorly and wear glasses, and in another, have excellent vision and walk without glasses or lenses (or think that he sees perfectly and does without glasses). Just as in the case of dissociative fugue, when switching, one person cannot remember what happened to the person during immersion in another.
Just as in the case of dissociative fugue, when switching, one person cannot remember what happened to the person during immersion in another.
Manifestations of dissociative identity disorder
This disease affects both children (adolescents) and adults and presents with similar symptoms. However, dissociative disorder with multiple personalities in adolescents is quite rare. In old age, dissociation practically does not develop. When a specialist suspects a person of dissociative identity disorder, he usually asks if it happened that the person suddenly found himself in some place and did not understand how he got there. Also, the patient may suddenly speak in a completely different voice, he may have a different handwriting. For example, a person who has one of his personalities as a child may suddenly begin to write in a child's handwriting. Such phenomenal manifestations can be evoked in a patient suffering from dissociative personality disorder, and in a state of hypnosis. That is why the French psychiatrist Jean-Martin Charcot at one time mistakenly believed that hypnosis is a pathological condition that causes hysteria and the manifestation of multiple personalities. However, later it turned out that hypnosis is only superficially similar to dissociative personality disorder, but does not cause it, and the disease itself develops without any connection with hypnosis.
That is why the French psychiatrist Jean-Martin Charcot at one time mistakenly believed that hypnosis is a pathological condition that causes hysteria and the manifestation of multiple personalities. However, later it turned out that hypnosis is only superficially similar to dissociative personality disorder, but does not cause it, and the disease itself develops without any connection with hypnosis.
See also
Myths about hypnosis
A person who has a dissociative disorder is, in fact, suffering greatly from his condition. He sees the negative or dismissive attitude of those around him: they look at him strangely, they reject him, no one finds a common language with him, because of him the family can collapse, and so on. At the moment of a dissociative state, a person does not have the opportunity to critically look at himself and his own behavior. That is, in a situation where one of the alternative personalities appears, he is in an inadequate state.
The main theory about the origin of this disease is based on the fact that in childhood such people experienced a traumatic situation, usually bullying or violence.
Dissociation is one of three conditions in which the patient is exempt from criminal liability, along with psychosis and mental retardation. There were cases when people in a dissociative state committed murder and rape. In such situations, even taking into account the severity of the crimes, patients are not sent to prison, but are sent to a psychiatric hospital or, in extreme cases, to a special ward of the psychiatric department of the prison.
Causes of dissociative identity disorder
Scientists have not yet found the genetic causes of dissociative identity disorder. The main theory about the origin of this disease is based on the fact that in childhood such people experienced a traumatic situation, usually bullying or violence. However, even this theory does not explain all 100% of cases of dissociative states. There are patients who, without an overt or identified traumatic situation in childhood, suffer from dissociative personality disorder. With regard to the physiological manifestations of this disorder, there is an assumption that in such patients certain areas of the brain stop working and others turn on. However, none of the theories suggesting physiological causes of dissociation currently explains all cases of the disease.
There are patients who, without an overt or identified traumatic situation in childhood, suffer from dissociative personality disorder. With regard to the physiological manifestations of this disorder, there is an assumption that in such patients certain areas of the brain stop working and others turn on. However, none of the theories suggesting physiological causes of dissociation currently explains all cases of the disease.
Diagnosis of dissociative identity disorder
Diagnosis of dissociative identity disorder is made through clinical interviews with several specialists. Sometimes the diagnosis requires not one, but several meetings with psychologists and psychiatrists, so that they have the opportunity to identify different aspects of the disorder, look at the patient's condition from several points of view and assemble a consultation. However, the specialist who identifies this disorder must have a great deal of experience and qualifications, since this disease can often be confused with others. In its manifestations, it can be similar to depression, anxiety or psychosis. It is also common for patients with dissociative identity disorder to be diagnosed with schizophrenia. Dissociation is a rare disorder and not every mental health professional can diagnose this disorder.
In its manifestations, it can be similar to depression, anxiety or psychosis. It is also common for patients with dissociative identity disorder to be diagnosed with schizophrenia. Dissociation is a rare disorder and not every mental health professional can diagnose this disorder.
Medications do not cure dissociative identity disorder, but only relieve some of the symptoms.
See also
Mental norm and pathology
A separate task for a specialist in the process of diagnosing dissociation in a child is to distinguish diseases from the presence of imaginary friends in a child, which very often appear in perfectly healthy children at a certain age. To do this, a specialist must be highly qualified in the field of developmental psychology and clearly be able to recognize a dissociative disorder not only in adults, but also in children.
Treatment of dissociative identity disorder
The main treatment for dissociative personality disorder is hypnosis. Sometimes specialists connect methods of psychoanalysis or cognitive-behavioral psychotherapy to treatment. Also, in some cases, medication is used to relieve symptoms. Drugs are prescribed if the disorder is accompanied by depression, panic attacks, drug or alcohol addiction. Medications do not cure dissociative identity disorder, but only relieve some of the symptoms. If a child suffers from this disease, then specialists carry out separate work with his parents, provide them with methods of proper communication with the child to improve the results of his treatment.
Sometimes specialists connect methods of psychoanalysis or cognitive-behavioral psychotherapy to treatment. Also, in some cases, medication is used to relieve symptoms. Drugs are prescribed if the disorder is accompanied by depression, panic attacks, drug or alcohol addiction. Medications do not cure dissociative identity disorder, but only relieve some of the symptoms. If a child suffers from this disease, then specialists carry out separate work with his parents, provide them with methods of proper communication with the child to improve the results of his treatment.
If you do not treat dissociative personality disorder, but let the disease take its course, then in the case of multiple personalities, a person in an inadequate state can commit some extremely negative actions in relation to others, for example, violent ones. In the case of a dissociative fugue, a person may get lost and never return home - it will simply be impossible to find him.
- Diseases and disorders
Share:
Treatment of dissociative identity disorder in St.
 Petersburg
Petersburg - Main
- Psychiatry
- Treatment of dissociative disorder
Dissociative identity disorder is a rather rare disease in our country. However, interest in this personality disorder is reflected not only in the Western European community of psychiatrists and psychotherapists, but also in modern cinema (for example, in the film Split, which was released in domestic cinemas in 2016). The disease itself is not associated with schizophrenia, as many still mistakenly believe, and the diagnosis (F44.8 according to ICD-10, 6B64 according to ICD-11) as such appeared in the International Classification of Diseases already in the 80s of the last century.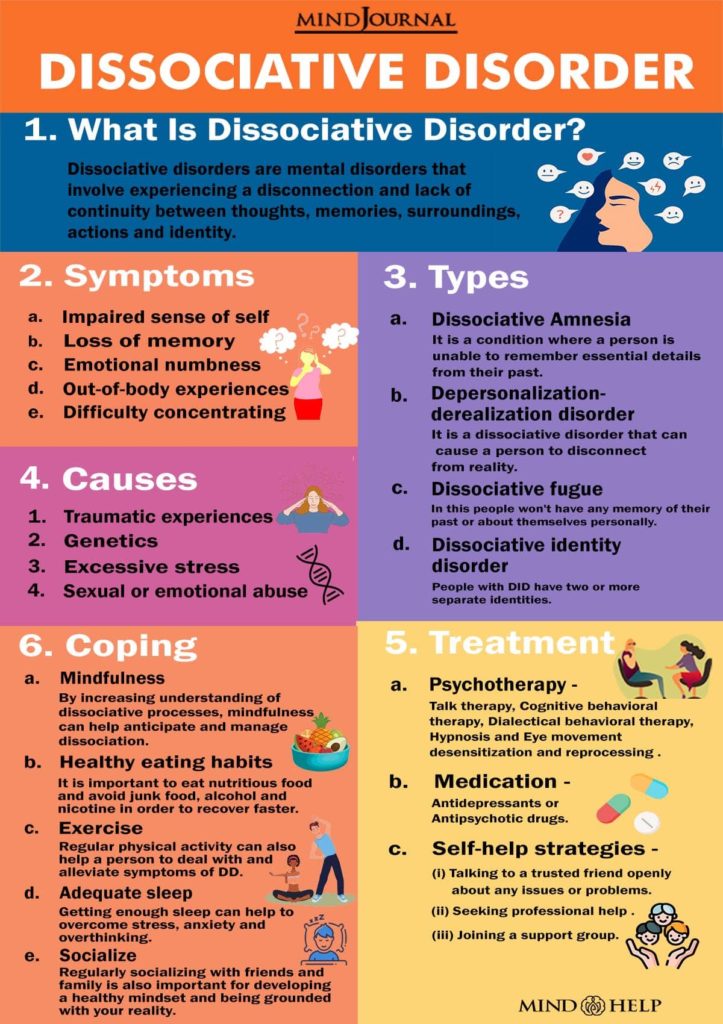
Since 1984, psychiatrists and psychotherapists have begun to form associations for the study of dissociative personality disorder. By 1995, more than 40,000 patients were diagnosed with this disease, previously defined as a subspecies of hysterical neurosis. To date, the treatment of dissociative personality disorder has been successfully carried out with the help of pharmacotherapy and psychotherapeutic treatment.
Dissociative identity disorder is one of the psychological defense mechanisms that occurs after a trauma suffered in childhood. The mechanism helps to cope with stress and, in most cases, represses memories of psychological or sexual abuse. The presence of any factors that contribute to the emergence of painful memories activates the alter ego (“other self”). Depending on the case, there may be several “other selves”. At the same time, the person himself does not know and does not remember what these “other selves” said and did after he comes to his senses.
In childhood, dissociative identity disorder may look like a kind of game and, as a rule, goes unnoticed not only by parents, but also by peers (for example, at school). However, entering adulthood, a person with a dissociative disorder begins to experience difficulties in communicating with other people and in family life. However, today there are examples of happy families with many children, where one of the spouses is diagnosed with a dissociative disorder.
Doctor's consultation on treatment of dissociative disorder:
+7 (812) 407-18-00
Thank you for your trust!
- Psychosocial personality correction
- Anonymous treatment without registration
- Help for family and relatives
| Service | Price | |
|---|---|---|
| Outpatient treatment | ||
| Psychiatric consultation | 5 000 ₽ | |
| Psychotherapist appointment | 5 000 ₽ | |
Reception of the chief physician Bocharov A.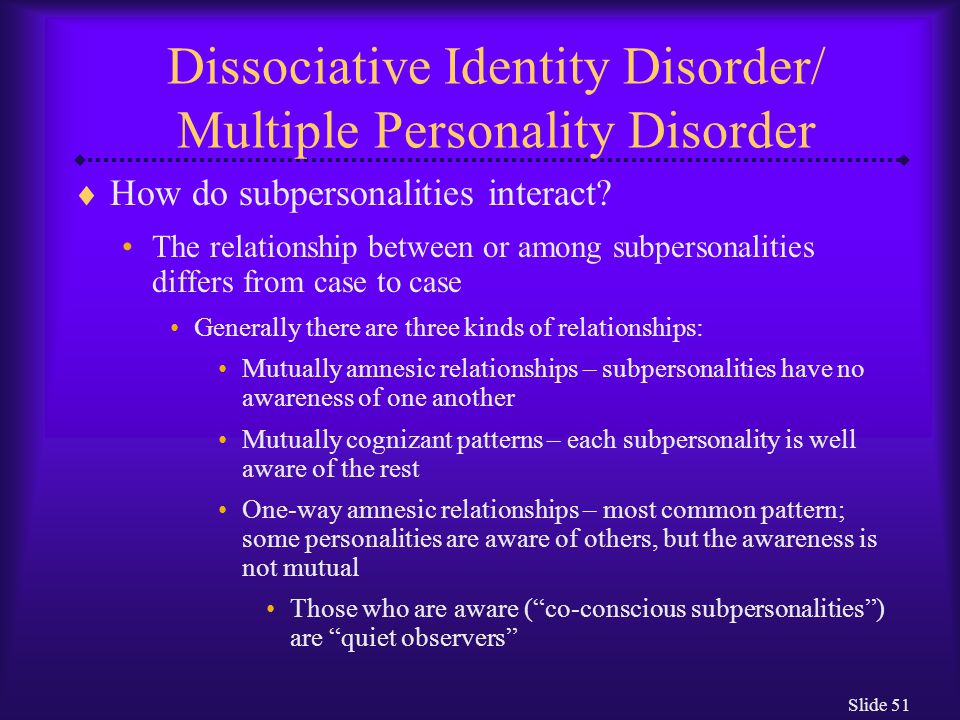 V. (Associate Professor, PhD) V. (Associate Professor, PhD) | 6 000 ₽ | |
| Psychiatric consultation at home | 6 000 ₽ | |
| Treatment in a hospital | ||
| Delivery to hospital | Is free | |
| Standard chamber | 8 900 ₽ | |
| 3-bed superior room | 12 000 ₽ | |
| 2-bed superior room | 15 000 ₽ | |
| 1 local VIP room | 19 500 ₽ | |
| Doctor's appointment 2 weeks after discharge | Is free | |
Features of dissociative personality disorder
Treatment of dissociative identity disorder
Help for family and relatives
Sources
Expert Q&A: dissociative disorders — https://psychiatry. org
org
Clinical handling of patients with dissociative disorders — https://pubmed.ncbi.nlm.nih.gov
Dissociative identity disorder (multiple personality disorder) — https://www.webmd.com
Update date: 10/12/2022
- Depersonalization and Derealization
- Suicidal behavior
- Anxiety disorder
Make an appointment
Date and time: (not set)
Make an appointment with a psychiatrist
Make an appointment with a psychiatrist
Select the date and time of your appointment
Today
November 06
Tomorrow
November 07
Tuesday
November 08
Wednesday
November 09
Thursday
November 10
Friday
November 11
Saturday
November 12
Sunday
November 13
Monday
November 14
Tuesday
November 15
Wednesday
November 16
Thursday
November 17
Friday
November 18
Saturday
November 19
Sunday
November 20
Monday
November 21
Tuesday
November 22
Wednesday
November 23
Thursday
November 24
Friday
November 25
Saturday
November 26
Sunday
November 27
Monday
November 28
Tuesday
November 29
Wednesday
November 30
Treatment for dissociative disorder on
Bocharov Alexey
Viktorovich
Psychiatrist, psychotherapist
Head physician of clinic
Experience 41 years
Psychiatrist, psychotherapist, sexologist, child psychiatrist
Work experience 41 years
Sinenchenko Andrey
Georgievich
Psychiatrist, psychotherapist
PhD
Work experience 22 years
Psychiatrist, psychotherapist, narcologist
Work experience 22 years
Zun Sergey
Andreevich
Psychiatrist, narcologist
PhD
Experience 33 years
Psychiatrist, narcologist, psychotherapist
Work experience 33 years
Lisitsyna Elena
Alekseevna
Psychiatrist
Top category
Experience 33 years
Psychiatrist
Work experience 33 years
Buchelnikova Victoria
Viktorovna
Psychiatrist
Head of amb.