Dissociative identity disorder depression
The Link Between Dissociative Identity Disorder and Depression
Many people with DID experience depression. We spoke with experts for professional and personal insights into what it’s like to live with both conditions.
Childhood trauma can increase the risk for numerous mental health conditions, including major depressive disorder, schizophrenia, and post-traumatic stress disorder (PTSD).
Perhaps one of the most direct responses to childhood trauma is dissociative identity disorder (DID). The disorder usually arises in response to severe trauma.
In fact, the American Psychiatric Association reports that about 90% of people with DID report having experienced at least one form of childhood abuse and neglect.
The majority of people with DID also live with depression, which can complicate and exacerbate both disorders.
There are three major dissociative disorders listed in the Diagnostic and Statistical Manual of Mental Disorders, 5th edition, text revision (DSM-5-TR):
- dissociative amnesia
- depersonalization-derealization disorder
- dissociative identity disorder
DID — previously known as multiple personality disorder — is the most severe form of these disorders. It’s a complex condition characterized by the presence of two or more distinct personality states (alters) in one body.
These alters may appear when the brain is unable to process and integrate traumatic experiences, memories, and feelings. In other words, DID is an extreme self-protective response to childhood trauma.
Although DID is listed in the DSM-5-TR it is still a highly controversial diagnosis, and there are many differential diagnoses for this disorder.
DID occurs in about 1.5% of the global population according to limited research, while depression is more common, affecting about 5% of adults worldwide.
However, in the DID population, depression is extremely common. A 2019 study reports that over 80% of people with DID have experienced major depressive episodes.
Still, depression may not be particularly easy to detect in people with DID.
“Just like it is hard to sometimes identify depression generally, it may be even harder to identify [it] in someone with DID,” says Stephanie Rickey, PsyD, program director of the Hill Center at McLean Hospital in Belmont, Massachusetts.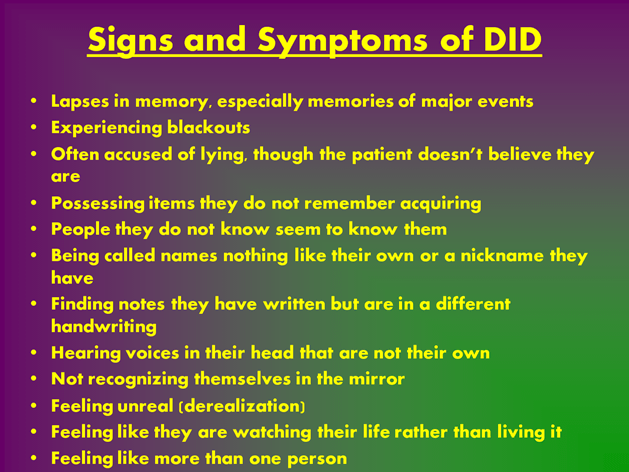
“Alterations in experience and the inherent ability to compartmentalize emotional and physical experiences may make it more challenging for the individual and others to identify [depression].”
In addition, Rickey notes that it can be difficult to determine whether certain symptoms are coming from depression or DID. For instance, a loss of energy, having trouble making decisions, or feelings of hopelessness or guilt can be seen in both disorders, making a diagnosis more complicated.
“Depression may also exacerbate the symptoms of DID or lead to more discomfort or confusion that may, in turn, lead to an increase in dissociative periods,” says Rickey.
“I think DID and depression go hand-in-hand,” says Crystalie Matulewicz who lives with both DID and depression.
Matulewicz was diagnosed with DID in 2015 but had already been diagnosed with several types of depression long before that. Her most recent diagnosis is persistent depressive disorder (PDD).
“While I do have periods of severe depression, especially around trauma anniversaries when I dissociate more, my general affect is just melancholic,” she says.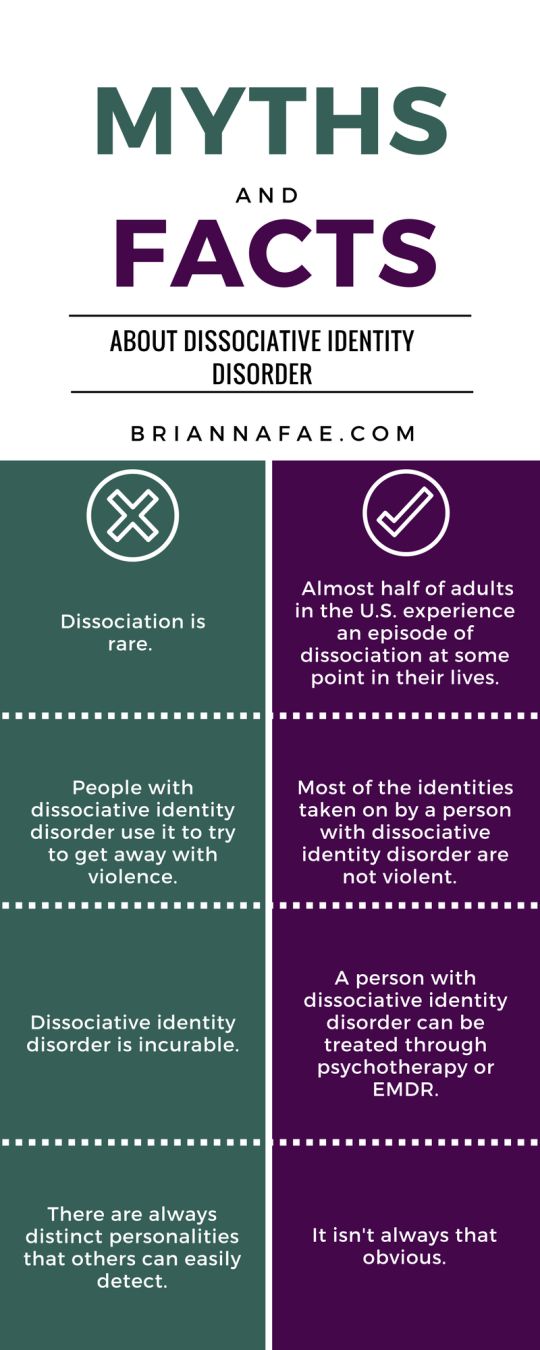
Like many people with dissociative depression, Matulewicz’s depression has not responded to medication.
“I spent many years, worked with several doctors, took part in several (very good) programs to try to find a medication that would help with the depression. But after trying more medications than I could count on my fingers and toes, we realized that my depression was treatment resistant.”
Matulewicz tries to work through her depression by staying busy.
“I work as much as I can — probably too much. Part of that is to avoid my issues, but part of that is also to avoid the depression. I can’t focus on how bad I’m feeling if I’m too busy focusing on work.”
Matulewitz also adds that a lot of her depression and dissociation triggers are date-related, so she tries to plan ahead.
“If I know a bad date is coming up, I’ll map out a plan. Do I need to work that day to distract myself? Do I need to take the day off to take care of myself?”
“I’ll plan out the day.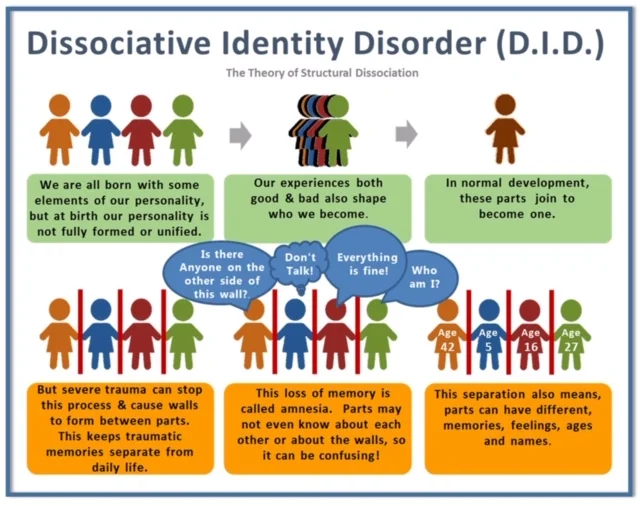 Going to the movies is a big one for me. I can do it myself, other parts can enjoy it as well, it’s entertaining, and it takes up a good chunk of time out of the day,” she says.
Going to the movies is a big one for me. I can do it myself, other parts can enjoy it as well, it’s entertaining, and it takes up a good chunk of time out of the day,” she says.
DID and depression can complicate and exacerbate one another.
Dissociative depression seems to be its own complex form of depression — and it’s often treatment-resistant. In fact, some experts suggest that dissociation in itself could be a reliable marker that a person has treatment-resistant depression.
“Having DID and depression adds extra complexity to treatment,” Matulewicz says. “While depression is commonly treated with talk therapy, medication, or a combination of the two, these treatments don’t always work so easily when DID is involved.”
“Depression in DID is often rooted in trauma, so medication isn’t as effective because it’s more than just a chemical imbalance involved.”
“Therapy for DID is long and focused on working through trauma, using coping skills and the like, so that treating depression often gets put on the back burner until other issues are addressed.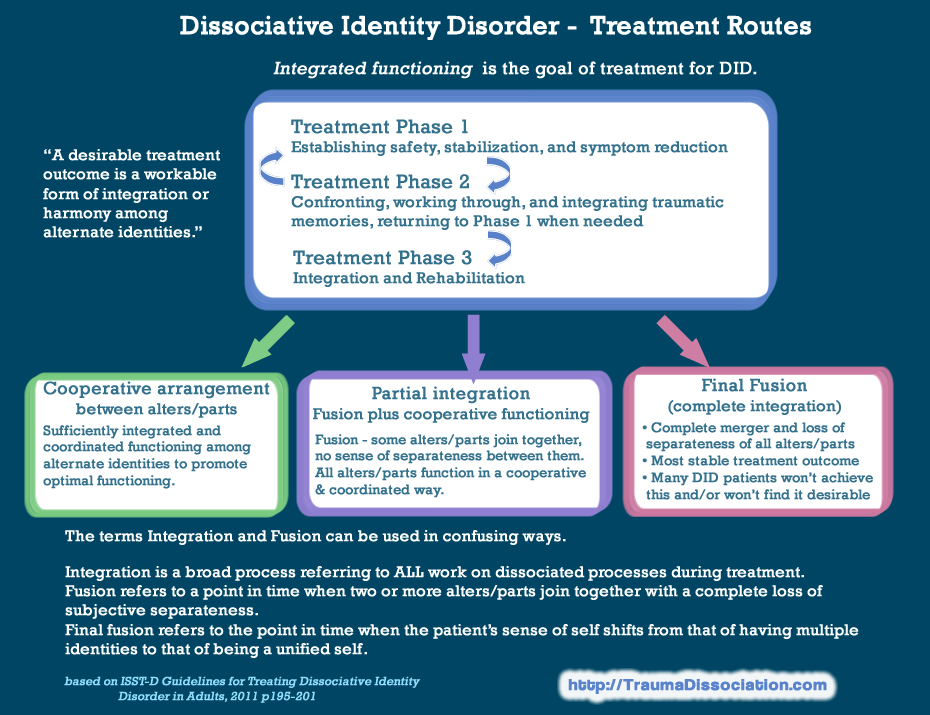 ”
”
“Then throw in the reality that multiple parts of you can have depression. Not only that, but each part’s depression can have a different cause, different triggers, and different symptoms. So then it becomes more than just treating one person’s depression — you’re treating multiple forms of depression for multiple people all within the same body,” says Matulewicz.
Does depression affect each alter differently?
“Depression is experienced by the full person. It is not possible for one alter to have major depression while another does not,” says Rickey.
Still, it’s important to note that individuals with DID may experience a sense of separation or unawareness of emotions and thoughts between alters.
“As a result, it is possible that this compartmentalization may lead to a subjective sense of one alter having depression while another does not,” says Rickey.
Matulewicz explains that alters can experience any mental health disorder, including depression, in varying severities.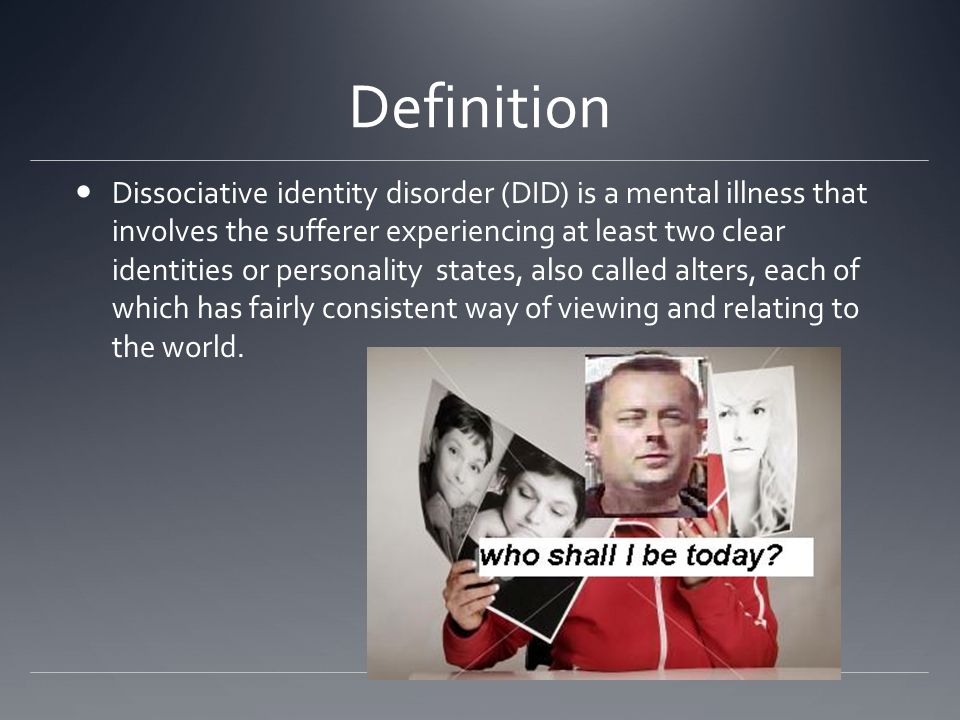
“For me, some of my parts are severely depressed to the point of being suicidal,” she says. “These parts have emerged from specific traumas and aren’t present very often, but can come out around trauma anniversaries or when triggered in a certain way.”
She notes that her other alters are “functionally depressed.” This means “they feel the typical symptoms of depression like anyone else with depression would, but focus more on what their purpose is.”
Matulewicz also shares that some of her other parts don’t experience depression at all. “They are completely closed off from any trauma we’ve experienced and don’t suffer many negative emotions at all,” she says.
If you’re experiencing suicidal thoughts, help is available
You can access free support right away with these resources:
- 988 Suicide and Crisis Lifeline.Call the Lifeline at 988 for English or Spanish, 24 hours a day, 7 days a week.
- The Crisis Text Line.
 Text HOME to the Crisis Text Line at 741741.
Text HOME to the Crisis Text Line at 741741. - The Trevor Project. LGBTQIA+ and under 25 years old? Call 866-488-7386, text “START” to 678678, or chat online 24/7.
- Veterans Crisis Line.Call 988 and press 1, text 838255, or chat online 24/7.
- Deaf Crisis Line.Call 321-800-3323, text “HAND” to 839863, or visit their website.
- Befrienders Worldwide.This international crisis helpline network can help you find a local helpline.
Was this helpful?
Depression is very common in people with DID, with more than 80% having experienced major depressive episodes. When both disorders occur together, it makes things more complicated, but treatment can still be effective.
If you are experiencing dissociation and depression, you’re not alone. Consider reaching out to a trusted healthcare professional today. Getting started on the right treatment can make a significant difference in your well-being and quality of life.
Getting started on the right treatment can make a significant difference in your well-being and quality of life.
Want to learn more about starting therapy? Psych Central’s How to Find Mental Health Support resource can help.
The Link Between Dissociative Identity Disorder and Depression
Many people with DID experience depression. We spoke with experts for professional and personal insights into what it’s like to live with both conditions.
Childhood trauma can increase the risk for numerous mental health conditions, including major depressive disorder, schizophrenia, and post-traumatic stress disorder (PTSD).
Perhaps one of the most direct responses to childhood trauma is dissociative identity disorder (DID). The disorder usually arises in response to severe trauma.
In fact, the American Psychiatric Association reports that about 90% of people with DID report having experienced at least one form of childhood abuse and neglect.
The majority of people with DID also live with depression, which can complicate and exacerbate both disorders.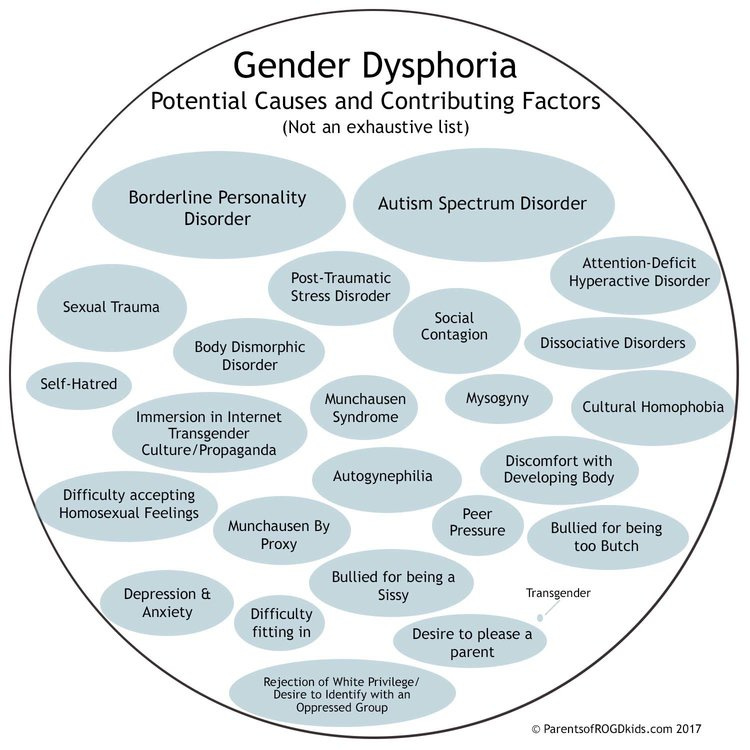
There are three major dissociative disorders listed in the Diagnostic and Statistical Manual of Mental Disorders, 5th edition, text revision (DSM-5-TR):
- dissociative amnesia
- depersonalization-derealization disorder
- dissociative identity disorder
DID — previously known as multiple personality disorder — is the most severe form of these disorders. It’s a complex condition characterized by the presence of two or more distinct personality states (alters) in one body.
These alters may appear when the brain is unable to process and integrate traumatic experiences, memories, and feelings. In other words, DID is an extreme self-protective response to childhood trauma.
Although DID is listed in the DSM-5-TR it is still a highly controversial diagnosis, and there are many differential diagnoses for this disorder.
DID occurs in about 1.5% of the global population according to limited research, while depression is more common, affecting about 5% of adults worldwide.
However, in the DID population, depression is extremely common. A 2019 study reports that over 80% of people with DID have experienced major depressive episodes.
Still, depression may not be particularly easy to detect in people with DID.
“Just like it is hard to sometimes identify depression generally, it may be even harder to identify [it] in someone with DID,” says Stephanie Rickey, PsyD, program director of the Hill Center at McLean Hospital in Belmont, Massachusetts.
“Alterations in experience and the inherent ability to compartmentalize emotional and physical experiences may make it more challenging for the individual and others to identify [depression].”
In addition, Rickey notes that it can be difficult to determine whether certain symptoms are coming from depression or DID. For instance, a loss of energy, having trouble making decisions, or feelings of hopelessness or guilt can be seen in both disorders, making a diagnosis more complicated.
“Depression may also exacerbate the symptoms of DID or lead to more discomfort or confusion that may, in turn, lead to an increase in dissociative periods,” says Rickey.
“I think DID and depression go hand-in-hand,” says Crystalie Matulewicz who lives with both DID and depression.
Matulewicz was diagnosed with DID in 2015 but had already been diagnosed with several types of depression long before that. Her most recent diagnosis is persistent depressive disorder (PDD).
“While I do have periods of severe depression, especially around trauma anniversaries when I dissociate more, my general affect is just melancholic,” she says.
Like many people with dissociative depression, Matulewicz’s depression has not responded to medication.
“I spent many years, worked with several doctors, took part in several (very good) programs to try to find a medication that would help with the depression. But after trying more medications than I could count on my fingers and toes, we realized that my depression was treatment resistant.”
Matulewicz tries to work through her depression by staying busy.
“I work as much as I can — probably too much. Part of that is to avoid my issues, but part of that is also to avoid the depression. I can’t focus on how bad I’m feeling if I’m too busy focusing on work.”
Matulewitz also adds that a lot of her depression and dissociation triggers are date-related, so she tries to plan ahead.
“If I know a bad date is coming up, I’ll map out a plan. Do I need to work that day to distract myself? Do I need to take the day off to take care of myself?”
“I’ll plan out the day. Going to the movies is a big one for me. I can do it myself, other parts can enjoy it as well, it’s entertaining, and it takes up a good chunk of time out of the day,” she says.
DID and depression can complicate and exacerbate one another.
Dissociative depression seems to be its own complex form of depression — and it’s often treatment-resistant. In fact, some experts suggest that dissociation in itself could be a reliable marker that a person has treatment-resistant depression.
“Having DID and depression adds extra complexity to treatment,” Matulewicz says. “While depression is commonly treated with talk therapy, medication, or a combination of the two, these treatments don’t always work so easily when DID is involved.”
“Depression in DID is often rooted in trauma, so medication isn’t as effective because it’s more than just a chemical imbalance involved.”
“Therapy for DID is long and focused on working through trauma, using coping skills and the like, so that treating depression often gets put on the back burner until other issues are addressed.”
“Then throw in the reality that multiple parts of you can have depression. Not only that, but each part’s depression can have a different cause, different triggers, and different symptoms. So then it becomes more than just treating one person’s depression — you’re treating multiple forms of depression for multiple people all within the same body,” says Matulewicz.
Does depression affect each alter differently?
“Depression is experienced by the full person. It is not possible for one alter to have major depression while another does not,” says Rickey.
Still, it’s important to note that individuals with DID may experience a sense of separation or unawareness of emotions and thoughts between alters.
“As a result, it is possible that this compartmentalization may lead to a subjective sense of one alter having depression while another does not,” says Rickey.
Matulewicz explains that alters can experience any mental health disorder, including depression, in varying severities.
“For me, some of my parts are severely depressed to the point of being suicidal,” she says. “These parts have emerged from specific traumas and aren’t present very often, but can come out around trauma anniversaries or when triggered in a certain way.”
She notes that her other alters are “functionally depressed.” This means “they feel the typical symptoms of depression like anyone else with depression would, but focus more on what their purpose is.”
Matulewicz also shares that some of her other parts don’t experience depression at all. “They are completely closed off from any trauma we’ve experienced and don’t suffer many negative emotions at all,” she says.
If you’re experiencing suicidal thoughts, help is available
You can access free support right away with these resources:
- 988 Suicide and Crisis Lifeline.Call the Lifeline at 988 for English or Spanish, 24 hours a day, 7 days a week.
- The Crisis Text Line.Text HOME to the Crisis Text Line at 741741.
- The Trevor Project. LGBTQIA+ and under 25 years old? Call 866-488-7386, text “START” to 678678, or chat online 24/7.
- Veterans Crisis Line.Call 988 and press 1, text 838255, or chat online 24/7.
- Deaf Crisis Line.Call 321-800-3323, text “HAND” to 839863, or visit their website.
- Befrienders Worldwide.This international crisis helpline network can help you find a local helpline.
Was this helpful?
Depression is very common in people with DID, with more than 80% having experienced major depressive episodes. When both disorders occur together, it makes things more complicated, but treatment can still be effective.
If you are experiencing dissociation and depression, you’re not alone. Consider reaching out to a trusted healthcare professional today. Getting started on the right treatment can make a significant difference in your well-being and quality of life.
Want to learn more about starting therapy? Psych Central’s How to Find Mental Health Support resource can help.
What is Dissociative Identity Disorder?
Dissociative Identity Disorder is a mental disorder characterized by either having two or more personalities, or a state of disconnection from the outside world, one's identity, and an inability to recall certain daily life events and important personal information. This disorder is often mistaken for depression, anxiety, or psychosis. Long before our days, this condition was called possession, and it was treated with exorcism. In the 19th century, this disorder was called hysteria, and in the 20th century it was called multiple personality disorder or multiple personality disorder.
Types of dissociative personality disorder
There are several types of dissociative disorders, which are characterized by different symptoms and manifestations. One of them is dissociative fugue, a disorder in which a person can find himself in a completely unfamiliar place and not remember how he got there. In this case, a person may forget some important information about himself and not even remember his name. At the same time, memory for some information, such as literature, science, and other things, can be preserved. In a state of fugue, a person assumes a different personality and identity with a different character, mannerisms and behavior. While in this identity, a person can lead an outwardly normal life. A dissociative fugue can last for hours or years. After that, a person may find himself in a completely unfamiliar place and at the same time not remember anything that happened to him in a state of fugue.
A person who has a dissociative disorder is actually suffering a lot from their condition.
Another type of dissociative disorder is the presence of several personalities in which a person finds himself in turn or simultaneously. At such moments, he disconnects from himself and stops feeling his own body, and also cannot see himself from the outside. Personalities within a person can have different ages, genders, nationalities, mental abilities, temperaments, and behave in completely different ways. Often these personalities can even have different physiological manifestations. For example, while in one personality, a person can see poorly and wear glasses, and in another, have excellent vision and walk without glasses or lenses (or think that he sees perfectly and does without glasses). Just as in the case of dissociative fugue, when switching, one person cannot remember what happened to the person during immersion in another.
Manifestations of dissociative identity disorder
This disease affects both children (adolescents) and adults and presents with similar symptoms. However, dissociative disorder with multiple personalities in adolescents is quite rare. In old age, dissociation practically does not develop. When a specialist suspects a person of dissociative identity disorder, he usually asks if it happened that the person suddenly found himself in some place and did not understand how he got there. Also, the patient may suddenly speak in a completely different voice, he may have a different handwriting. For example, a person who has one of his personalities as a child may suddenly begin to write in a child's handwriting. Such phenomenal manifestations can be evoked in a patient suffering from dissociative personality disorder, and in a state of hypnosis. That is why the French psychiatrist Jean-Martin Charcot at one time mistakenly believed that hypnosis is a pathological condition that causes hysteria and the manifestation of multiple personalities. However, later it turned out that hypnosis is only superficially similar to dissociative personality disorder, but does not cause it, and the disease itself develops without any connection with hypnosis.
See also
Myths about hypnosis
A person who has a dissociative disorder is, in fact, suffering greatly from his condition. He sees the negative or dismissive attitude of those around him: they look at him strangely, they reject him, no one finds a common language with him, because of him the family can collapse, and so on. At the moment of a dissociative state, a person does not have the opportunity to critically look at himself and his own behavior. That is, in a situation where one of the alternative personalities appears, he is in an inadequate state.
The main theory about the origin of this disease is based on the fact that in childhood such people experienced a traumatic situation, usually bullying or violence.
Dissociation is one of three conditions in which the patient is exempt from criminal liability, along with psychosis and mental retardation. There were cases when people in a dissociative state committed murder and rape. In such situations, even taking into account the severity of the crimes, patients are not sent to prison, but are sent to a psychiatric hospital or, in extreme cases, to a special ward of the psychiatric department of the prison.
Causes of dissociative identity disorder
Scientists have not yet found the genetic causes of dissociative identity disorder. The main theory about the origin of this disease is based on the fact that in childhood such people experienced a traumatic situation, usually bullying or violence. However, even this theory does not explain all 100% of cases of dissociative states. There are patients who, without an overt or identified traumatic situation in childhood, suffer from dissociative personality disorder. With regard to the physiological manifestations of this disorder, there is an assumption that in such patients certain areas of the brain stop working and others turn on. However, none of the theories suggesting physiological causes of dissociation currently explains all cases of the disease.
Diagnosis of dissociative identity disorder
Diagnosis of dissociative identity disorder is made through clinical interviews with several specialists. Sometimes the diagnosis requires not one, but several meetings with psychologists and psychiatrists, so that they have the opportunity to identify different aspects of the disorder, look at the patient's condition from several points of view and assemble a consultation. However, the specialist who identifies this disorder must have a great deal of experience and qualifications, since this disease can often be confused with others. In its manifestations, it can be similar to depression, anxiety or psychosis. It is also common for patients with dissociative identity disorder to be diagnosed with schizophrenia. Dissociation is a rare disorder and not every mental health professional can diagnose this disorder.
Medications do not cure dissociative identity disorder, but only relieve some of the symptoms.
See also
Mental norm and pathology
A separate task for a specialist in the process of diagnosing dissociation in a child is to distinguish diseases from the presence of imaginary friends in a child, which very often appear in perfectly healthy children at a certain age. To do this, a specialist must be highly qualified in the field of developmental psychology and clearly be able to recognize a dissociative disorder not only in adults, but also in children.
Treatment of dissociative identity disorder
The main treatment for dissociative personality disorder is hypnosis. Sometimes specialists connect methods of psychoanalysis or cognitive-behavioral psychotherapy to treatment. Also, in some cases, medication is used to relieve symptoms. Drugs are prescribed if the disorder is accompanied by depression, panic attacks, drug or alcohol addiction. Medications do not cure dissociative identity disorder, but only relieve some of the symptoms. If a child suffers from this disease, then specialists carry out separate work with his parents, provide them with methods of proper communication with the child to improve the results of his treatment.
If you do not treat dissociative personality disorder, but let the disease take its course, then in the case of multiple personalities, a person in an inadequate state can commit some extremely negative actions in relation to others, for example, violent ones. In the case of a dissociative fugue, a person may get lost and never return home - it will simply be impossible to find him.
- Diseases and disorders
Share:
Treatment of dissociative identity disorder in St.
- Main
- Psychiatry
- Treatment of dissociative disorder
Dissociative identity disorder is a rather rare disease in our country. However, interest in this personality disorder is reflected not only in the Western European community of psychiatrists and psychotherapists, but also in modern cinema (for example, in the film Split, which was released in domestic cinemas in 2016). The disease itself is not associated with schizophrenia, as many still mistakenly believe, and the diagnosis (F44.8 according to ICD-10, 6B64 according to ICD-11) as such appeared in the International Classification of Diseases already in the 80s of the last century.
Since 1984, psychiatrists and psychotherapists have begun to form associations for the study of dissociative personality disorder. By 1995, more than 40,000 patients were diagnosed with this disease, previously defined as a subspecies of hysterical neurosis. To date, the treatment of dissociative personality disorder has been successfully carried out with the help of pharmacotherapy and psychotherapeutic treatment.
Dissociative identity disorder is one of the psychological defense mechanisms that occurs after a trauma suffered in childhood. The mechanism helps to cope with stress and, in most cases, represses memories of psychological or sexual abuse. The presence of any factors that contribute to the emergence of painful memories activates the alter ego (“other self”). Depending on the case, there may be several “other selves”. At the same time, the person himself does not know and does not remember what these “other selves” said and did after he comes to his senses.
In childhood, dissociative identity disorder may look like a kind of game and, as a rule, goes unnoticed not only by parents, but also by peers (for example, at school). However, entering adulthood, a person with a dissociative disorder begins to experience difficulties in communicating with other people and in family life. However, today there are examples of happy families with many children, where one of the spouses is diagnosed with a dissociative disorder.
Doctor's consultation on treatment of dissociative disorder:
+7 (812) 407-18-00
Thank you for your trust!
- Psychosocial personality correction
- Anonymous treatment without registration
- Help for family and relatives
| Service | Price | |
|---|---|---|
| Outpatient treatment | ||
| Psychiatric consultation | 5 000 ₽ | |
| Psychotherapist appointment | 5 000 ₽ | |
| Reception of the chief physician Bocharov A. | 6 000 ₽ | |
| Psychiatric consultation at home | 6 000 ₽ | |
| Treatment in a hospital | ||
| Delivery to hospital | For free | |
| Standard chamber | 8 900 ₽ | |
| 3-bed superior room | 12 000 ₽ | |
| 2-bed superior room | 15 000 ₽ | |
| 1 local VIP room | 19 500 ₽ | |
| Doctor's appointment 2 weeks after discharge | For free | |
Features of dissociative personality disorder
Treatment of dissociative identity disorder
Help for family and relatives
Sources
Expert Q&A: dissociative disorders — https://psychiatry. org
Clinical handling of patients with dissociative disorders — https://pubmed.ncbi.nlm.nih.gov
Dissociative identity disorder (multiple personality disorder) — https://www.webmd.com
Update date: 10/12/2022
- Depersonalization and Derealization
- Suicidal behavior
- Anxiety disorder
Make an appointment
Date and time: (not set)
Make an appointment with a psychiatrist
Make an appointment with a psychiatrist
Select the date and time of your appointment
Tomorrow
April 17
Tuesday
April 18
Wednesday
April 19
Thursday
April 20
Friday
April 21
Saturday
April 22
Sunday
April 23
Monday
April 24
Tuesday
April 25
Wednesday
April 26
Thursday
April 27
Friday
April 28
Saturday
April 29
Sunday
April 30
Treatment for dissociative disorder
Bocharov Alexey
Viktorovich
Psychiatrist, psychotherapist
Head physician of clinic
Work experience 42 years
Psychiatrist, psychotherapist, sexologist, child psychiatrist
Work experience 42 years
Sinenchenko Andrey
Georgievich
Psychiatrist, psychotherapist
PhD
Work experience 23 years
Psychiatrist, psychotherapist, narcologist
Work experience 23 years
Zun Sergey
Andreevich
Psychiatrist, narcologist
PhD
Work experience 34 years
Psychiatrist, narcologist, psychotherapist
Work experience 34 years
Lisitsyna Elena
Alekseevna
Psychiatrist
Top category
Work experience 34 years
Psychiatrist
Work experience 34 years
Buchelnikova Victoria
Viktorovna
Psychiatrist
Head of amb.