Detachment from people
Why You May Experience Emotional Detachment and What to Do About It
Emotional detachment is an inability or unwillingness to connect with other people on an emotional level. Being emotionally detached helps protect some people from unwanted drama, anxiety, or stress.
For others, detachment isn’t always voluntary. Instead, it’s the result of events that make the person unable to be open and honest about their emotions.
Below you’ll read about the different types of emotional detachment and learn when it’s a good thing and when it might be worrisome.
Emotional detachment describes when you or others disengage or disconnect from other people’s emotions. It may stem from an unwillingness or an inability to connect with others.
There are two general types. In some cases, you may develop emotional detachment as a response to a difficult or stressful situation. In other cases, it may result from an underlying psychological condition.
Emotional detachment can be helpful if you use it purposefully, such as by setting boundaries with certain people or groups. Boundaries can help you maintain a healthy distance from people who demand much of your emotional attention.
But emotional detachment can also be harmful when you can’t control it. You may feel “numbed” or “muted.” This is known as emotional blunting, and it’s typically a symptom or issue that you should consider working with a mental health professional to address.
Learn more about emotional blunting here.
People who are emotionally detached or removed may experience symptoms such as:
- difficulty creating or maintaining personal relationships
- a lack of attention, or appearing preoccupied when around others
- difficulty being loving or affectionate with a family member
- avoiding people, activities, or places because they’re associated with past trauma
- reduced ability to express emotion
- difficulty empathizing with another person’s feelings
- not easily sharing emotions or feelings
- difficulty committing to another person or a relationship
- not making another person a priority when they should be
Emotional detachment can slowly build over time, or it may occur more rapidly in response to an acute situation. Though everyone is different, some signs and symptoms to watch for include:
Though everyone is different, some signs and symptoms to watch for include:
- inability to feel emotions or feeling empty
- losing interest in enjoyable activities
- becoming less involved in relationships
- showing little or no empathy toward others
- being harsh or unkind to others
If you suspect you may be developing emotional detachment, you should consider talking with your doctor. They can help identify your symptoms and recommend potential treatment options.
Emotional detachment may develop due to a variety of potential causes, which can include:
- constant exposure to bad or unpleasant news
- traumatic experience
- abuse
- side effects of certain medications
- conditioning as a child due to parental or cultural expectations
Emotional detachment may be voluntary. Some people can choose to remain emotionally removed from a person or situation.
Other times, emotional detachment results from trauma, abuse, or a previous encounter. In these cases, previous events may make it difficult to be open and honest with a friend, loved one, or significant other.
In these cases, previous events may make it difficult to be open and honest with a friend, loved one, or significant other.
By choice
Some people choose to proactively remove themselves from an emotional situation.
This might be an option if you have a family member or a colleague that you know upsets you greatly. You can choose not to engage with the person or persons. This will help you remain cool and keep calm when dealing with them.
In situations like this, emotional detachment is a bit like a protective measure. It helps you prepare for situations that may trigger a negative emotional response.
As a result of abuse
Sometimes, emotional detachment may result from traumatic events, such as childhood abuse or neglect. Children who live through abuse or neglect may develop emotional detachment as a means of survival.
Children require a lot of emotional connection from their parents or caregivers. If it’s not forthcoming, the children may stop expecting it. When that happens, they may begin to turn off their emotional receptors, as in the case of reactive attachment disorder (RAD). RAD is a condition in which children cannot form bonds with their parents or caregivers.
When that happens, they may begin to turn off their emotional receptors, as in the case of reactive attachment disorder (RAD). RAD is a condition in which children cannot form bonds with their parents or caregivers.
That can lead to depressed mood, inability to show or share emotions, and behavior problems.
Other conditions
Emotional detachment or “numbing” is frequently a symptom of other conditions. You may feel distant from your emotions at times if you have:
- post-traumatic stress disorder
- bipolar disorder
- major depressive disorder
- personality disorders
Medication
Selective serotonin reuptake inhibitors (SSRIs) are a type of antidepressant. Some people who take this type of drug may experience emotional blunting or a switched-off emotional center, particularly at higher doses.
This period of emotional detachment may last as long as you take these medications. Doctors can help you find another alternative or help to find the right dosage if the medication affects you in this way.
Emotional detachment isn’t an official condition like bipolar disorder or depression. Instead, it’s often considered one element of a larger medical condition.
Conditions might include personality disorders or attachment disorders.
Emotional detachment could also be the result of acute trauma or abuse.
A healthcare professional may be able to see when you’re not emotionally available to others. They may also talk with you, a family member, or a significant other about your behaviors.
Understanding how you feel and act can help a provider recognize a pattern that could suggest this emotional issue.
Asperger’s and emotional detachment
Contrary to popular belief, people living with Asperger’s, which forms part of the Autism spectrum disorder, are not cut off from their emotions or the emotions of others.
In fact, experts indicate they may feel others’ emotions more intensely even if they do not show typical outward signs of emotional involvement, such as changes in affect or facial expressions. This can lead to them taking additional steps to avoid hurting others, even at their own expense.
This can lead to them taking additional steps to avoid hurting others, even at their own expense.
Treatment for emotional detachment depends on the reason it’s occurring.
If your healthcare professional believes you’re experiencing problems with emotional attachment because of another condition, they may suggest treating that first.
These conditions might include depression, PTSD, or borderline personality disorder. Medication and therapy are often helpful for these conditions.
If the emotional detachment symptoms result from trauma, your doctor may recommend psychotherapy, also known as talk therapy. This treatment can help you learn to overcome the impacts of the abuse. You may also learn new ways to process experiences and anxieties that previously upset you and led to emotional detachment.
For some people, however, emotional distance isn’t problematic. In that case, you may not need to seek any treatment.
However, if problems with feeling or expressing emotions have caused issues in your personal life, you may want to seek out treatment or other support. A therapist or other mental health provider can provide treatment, though you may find that talking first to your primary care provider can help connect you with those who can help.
A therapist or other mental health provider can provide treatment, though you may find that talking first to your primary care provider can help connect you with those who can help.
For some people, emotional detachment is a way of coping with overwhelming people or activities. You choose when to be involved and when to step away.
In other cases, however, numbing yourself to emotions and feelings may not be healthy. Indeed, frequently “turning off” your emotions may lead to unhealthy behaviors, such as an inability to show empathy or a fear of commitment.
People that live through trauma or abuse may find it difficult to express emotions. This may cause people to seek other, negative outlets for those feelings, such as drug or alcohol misuse, higher risk sexual behaviors, or other behaviors that can lead to involvement with law enforcement.
Emotional detachment occurs when people willingly or unwillingly turn off their connection with their emotions. This may be intentional, such as a defensive mechanism on emotionally draining people, or unintentional due to an underlying condition or medication side effect.
If you have difficulty processing emotions or you live with someone who does, you may want to consider seeking help from a mental health provider. They can offer support and treatment to help you understand how you process emotions and respond to others and activities.
Emotional Detachment: What It Means, 10 Signs + How To Heal
If these situations sound familiar, you may be experiencing emotional detachment.
What is emotional detachment?
Emotional detachment is a form of dissociation and disconnection from the self and others, describes Katie Ziskind, LMFT, a licensed marriage and family therapist and owner of Wisdom Within Counseling. Even though you may physically be in the room, you're mentally detached from people and their emotions.
Emotional detachment can be a normal, voluntary strategy to set clear boundaries. Like most things in life, balance and moderation are key. However, it can evolve into a negative response if the continual disengagement prevents you from being able to meaningfully share space and connect with others.
If you struggle with emotional detachment, it's likely you have difficulty maintaining relationships in your life. Being unable to openly express empathy and the full context of your emotions may prove to be an ongoing theme in your life. Ziskind notes people with emotional detachment often blame themselves for their inability to authentically connect with others, but it's often not their fault. When used in unhealthy ways, emotional detachment is at its core a coping mechanism designed to keep people at a distance so you feel safe—even at the cost of being numb.
Advertisement
This ad is displayed using third party content and we do not control its accessibility features.
What causes it?
According to Ziskind, emotional detachment may manifest itself as a survival mechanism to protect yourself from potential stress, overwhelm, and anxiety. If you grew up in an environment where showing the true breadth of your emotions was threatening or shameful in some way (such as a toxic family dynamic), over time you might have learned how to shut off your feelings until it became an automatic, unconscious reflex.
"I see this often in clients with a history of trauma and neglect," trauma therapist and licensed clinical social worker Canh Tran, LICSW, tells mbg. "You learn to dissociate or disconnect from your feelings and bodies to survive these adverse and traumatic experiences—because it would have been too painful to experience them."
In the face of ongoing neglect, stress, or abuse, emotional detachment can correspond to attachment disorders, post-traumatic stress disorder (PTSD), complex post-traumatic stress disorder (CPTSD), or past instances of trauma. Although it's not listed in the DSM, emotional detachment can also reveal itself as a symptom of a mental health condition or from the use of certain medications like antidepressants.
Common signs of emotional detachment.
Here are a few examples of emotional detachment and how it may show up in your life, according to Tran and Ziskind:
Advertisement
This ad is displayed using third party content and we do not control its accessibility features.
1.
People don't see you as empathetic.
Your friends and family may share deeply personal stories about what they're going through. You can feel what they're going through, but you're unable to summon the appropriate response to meet them in a heart-opening place. Since you find it hard to be affectionate and listen to their emotions, they may perceive you as being rude or uncaring.
2.
You disconnect in the face of conflict or social situations.
When people are crying, you may find yourself reaching for your phone. It's hard for you to keep up with friends and a bustling social calendar because you think people want too much from you that you're unsure you can give. Another tell is you might find yourself laughing at painful stories and experiences, says Tran.
Advertisement
This ad is displayed using third party content and we do not control its accessibility features.
3.
In general, you lack relationship skills.
Forming significant bonds with people means you have to show you care. Because you're not able or willing to connect with all of your emotions, let alone other people's emotions, it can come across like you're neutral toward your loved ones—or worse, like you're stonewalling them. For some, being around your loved ones may not feel enjoyable sometimes because you believe you're not a good communicator in certain situations or because you just don't want to go in too deep with them.
Because you're not able or willing to connect with all of your emotions, let alone other people's emotions, it can come across like you're neutral toward your loved ones—or worse, like you're stonewalling them. For some, being around your loved ones may not feel enjoyable sometimes because you believe you're not a good communicator in certain situations or because you just don't want to go in too deep with them.
4.
You have difficulty identifying feelings.
When you're in a situation where you have to label your own feelings, it may not be easy to parse through what's happening internally. You only know your emotions feel unpleasant and uncomfortable. You're not able to differentiate between your emotions as they come up and properly sort them into categories like grief, anger, or fear.
Advertisement
This ad is displayed using third party content and we do not control its accessibility features.
5.
It's not easy to share what you're going through.

When your loved ones want to hear about your struggles, you resort to emotional suppression and downplaying what you're going through—even the good experiences. Even when you're alone, you're still emotionally unavailable to yourself. You would rather distract, intellectualize, and stay clear of them.
6.
Not feeling real is a common occurrence.
Depersonalization is when there's a persistent feeling that you or your surroundings aren't real. People, events, and things may seem foggy and removed. It doesn't seem like you really feel anything at all. Because you are so detached from what's happening, you feel disconnected from your thoughts, feelings, and emotions.
7.
You have difficulty naming your needs and wants.
When your partner asks you about your needs and wants in the relationship, your mind is a total blank. It's not so simple for you to understand what you're feeling in the moment, much less reveal things that could open you up to shame or hurt you later on. Because you blunt out emotions so much, it's hard to communicate your expectations and yearnings because you're too busy evading them.
Because you blunt out emotions so much, it's hard to communicate your expectations and yearnings because you're too busy evading them.
8.
Boundary-setting is hard.
If you strive to be a people-pleaser instead of setting boundaries, Ziskind says the inability to practice good self-care could, in fact, be a sign of emotional detachment. Not being able to advocate for yourself means you're often denying your own needs and, subsequently, your own emotional desires.
9.
You're critical toward yourself.
Ziskind says emotional detachment can contribute toward a large inner critic and a lack of motivation to complete tasks. Being hypercritical leads to perfectionistic tendencies and a distorted belief that you are not good enough.
10.
You don't like taking compliments and praise.
Being able to sincerely receive praise from others means you're able to accept the positives in yourself. But for people who experience emotional detachment, you might feel awkward or tense expressing happiness with the compliment. Instead, it may be easier to sidestep the comment and deflect.
Instead, it may be easier to sidestep the comment and deflect.
Overcoming emotional detachment.
Overcoming emotional detachment can't happen until you can identify your emotions. Tran advises to start off slow. It'll be a gradual process to embrace emotions previously seen as intolerable. "Just as trauma and neglect changes us, we can also change and grow from adverse experiences," he says. "Learn to identify sensations in the body when feelings arise, find words to feelings, learn healthy boundaries like how to say no, and [allow yourself] to be witnessed by someone who can offer validation when feeling a wide range of emotions."
Ziskind recommends working on self-care activities and self-love skills, which can help address emotional detachment and rebuild a strong relationship where it matters the most: with yourself. This can happen with yoga, painting, art therapy, and animal therapy. Leaning on these practices helps facilitate a connection to your sense of self and helps you grow conscious of the triggers that cause detachment in the first place. For insight into your emotional detachment, understanding these pain points is crucial so you can choose a healthier response that serves you better and increases vulnerability.
For insight into your emotional detachment, understanding these pain points is crucial so you can choose a healthier response that serves you better and increases vulnerability.
Once you're able to let in your emotions, Ziskind says the next step is to do a grounding technique to bring your mind and body back to the present moment. This can come in the form of positive affirmations such as I am safe in this moment. "Retraining your body and brain to feel safe in the world is a key part in healing trauma and becoming more emotionally connected to the world," she says.
Lastly, if you suffer from emotional detachment, you don't have to do it alone—after all, isolation is a hallmark of this behavior. Ziskind and Tran emphasize the importance of sharing your feelings with the people you trust such as your partner, family, friends, or a trauma-informed therapist. It'll help co-create fulfilling relationships where you both feel seen, heard, and understood.
The takeaway.
Emotional detachment prevents you from getting closer to people, but it doesn't have to continue to be a psychological barrier. Acknowledging your feelings and all of your beautiful complexities can be the beginning of re-meeting yourself and others entirely with unconditional love and grace.
Take it from Tran: "Consistency, practice, patience, and compassion are all necessary on the journey of healing. While healing oftentimes can be painful and uncomfortable because it requires confronting what we've been avoiding, on the other side can be joy, freedom, peace, and more connection to ourselves and others we care about."
What is depersonalization and how to live with it? look like symptoms of depersonalization disorder, which is often confused with schizophrenia. Afisha Daily publishes three stories of people with this terrible diagnosis.
Tatyana, 28 years old: “For the first time I encountered a feeling of unreality of what was happening when I was 22 years old. One day, I just stopped feeling any emotions; my relatives suddenly became strangers, I didn’t want to communicate with anyone, go out anywhere. I didn’t feel like myself - the personality was erased, and I became a different person: the feeling that there was no more soul, only one shell. This was accompanied by constant anxiety, soul-searching, headaches, and a sense of hopelessness. This is a terrible state when suicide seems to be the only way to stop everything. nine0003
One day, I just stopped feeling any emotions; my relatives suddenly became strangers, I didn’t want to communicate with anyone, go out anywhere. I didn’t feel like myself - the personality was erased, and I became a different person: the feeling that there was no more soul, only one shell. This was accompanied by constant anxiety, soul-searching, headaches, and a sense of hopelessness. This is a terrible state when suicide seems to be the only way to stop everything. nine0003
I was very frightened and urgently called my mother, because I myself could not even go to the doctor. The neurologist at the hospital said that I was depressed and prescribed a cocktail of antidepressants and neuroleptics. Surprisingly, almost from the first days of taking the pills, I returned to life: the symptoms disappeared, my mood improved, my ability to work increased, I became sociable and open. A month later, I stopped taking these drugs and did not go to the doctor again (although I was warned not to give up the drugs). For four years, I forgot about the problems. nine0003
For four years, I forgot about the problems. nine0003
The symptoms returned when a relative offered me a new job. There were rather high requirements for employees - a mandatory driver's license, specialized education in the field of shipping and fluent English. I was given six months to prepare. The relative paid for all the courses, the university - and then the stress began. I felt that it was covering me, so I arbitrarily returned to the pills. It got a little easier for a while. I tried my last strength not to lose face, to get this job, not to let down the person who believed in me and also spent money. But I got worse and worse, and I failed the job interview. It was a very difficult period. nine0003
After that, I began to sit on forums, google articles about mental disorders with similar symptoms. There were thoughts that I had schizophrenia and I was finally going crazy. I started running around psychiatrists, but all of them refuted my suspicions. Depression was re-diagnosed, antidepressants were prescribed - anxiety subsided a little, but emotions and feelings never returned.
Once on some website I saw a description of a diagnosis that exactly matched my symptoms. Then my acquaintance with depersonalization-derealization disorder began. I went to doctors, but they basically didn't know what it was and how to treat it. Sometimes they simply did not want to listen to me - they immediately prescribed medicines and sent me home. One professor said that I "read on the Internet." I found my salvation in online consultations with a doctor who dealt with dereal: according to his scheme, I started taking antidepressants and antiepileptic drugs. nine0003
The reason for my depersonalization is neurosis, which is accompanied by anxiety: under stress, the body defends itself and the brain seems to turn off, isolation from the outside world occurs. This happens to impressionable people who worry about anything, take everything to heart. I am one of those.
My experience is 2.5 years. I know that there may be deterioration, but there is a way out. Now I have reached the stage when a new job is a joy, I feel like myself again, mental abilities, emotions and feelings are the same as before the illness. And, although I'm still on the pills, it's better than suffering again. I hope someday I can cancel them. It sounds strange, but this illness has changed me for the better. Thanks to her, I truly began to appreciate life and loved ones. Became more patient. I am glad that I can live a normal life again, feel, love, enjoy communication with people and from my favorite activities. nine0003
And, although I'm still on the pills, it's better than suffering again. I hope someday I can cancel them. It sounds strange, but this illness has changed me for the better. Thanks to her, I truly began to appreciate life and loved ones. Became more patient. I am glad that I can live a normal life again, feel, love, enjoy communication with people and from my favorite activities. nine0003
Our society is very contemptuous of those in need of psychological help. If they find out that a person has been to a psychiatrist, they immediately label him a psycho and avoid him. Nevertheless, you should not be afraid to seek qualified help, the main thing in this matter is to find a really good doctor. And there are very few of them."
Nikolai, 27 years old: “I have been neurotic since childhood: stuttering, obsessive-compulsive disorder (obsessive thoughts syndrome). In August 2014, I went to a psychiatrist with depression and impaired perception of reality, I was then 25 years old. It all started with rare panic attacks, which were replaced by bouts of severe derealization. The world turned upside down, and I had to lie down on the floor and close my eyes, this helped to come to my senses. After another such attack, I developed anxiety. nine0003
It all started with rare panic attacks, which were replaced by bouts of severe derealization. The world turned upside down, and I had to lie down on the floor and close my eyes, this helped to come to my senses. After another such attack, I developed anxiety. nine0003
Exactly 6 months I thrashed around looking for and inventing physical illnesses to justify my condition. Admitting to yourself that you are a little "cuckoo" is difficult, and this is how hypochondria appears. The catalyst for hypochondria is still such an unpleasant reality as unskilled medicine. The inertia coming from the USSR still persists - doctors sculpt a diagnosis of VVD (which has long been absent from the world classification of diseases), say that everything is in order, prescribe vitamins and send them home. Therefore, I had to engage in self-diagnosis and be terribly afraid of what was really happening to me. Unfortunately, I made the diagnosis of "depersonalization disorder" myself, once again surfing the Internet.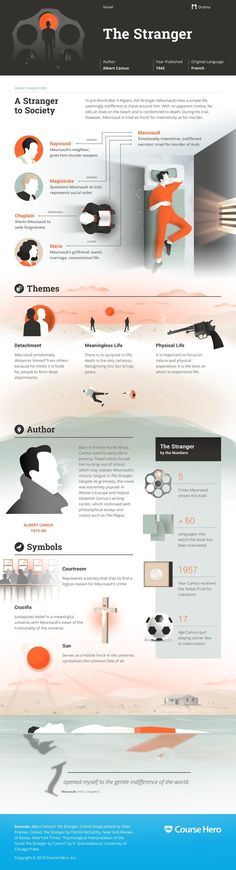 Through acquaintances, I managed to go to a psycho-neurological dispensary. There I was pumped with the same Soviet drugs, put on droppers, there was even a massage and a circular shower. At discharge, there were no significant results: it became easier to sleep, but the condition remained the same painful. nine0003
Through acquaintances, I managed to go to a psycho-neurological dispensary. There I was pumped with the same Soviet drugs, put on droppers, there was even a massage and a circular shower. At discharge, there were no significant results: it became easier to sleep, but the condition remained the same painful. nine0003
At last, miraculously, I managed to get to a good psychiatrist. Properly selected drugs have built a solid foundation for my recovery. Now pharmacology has reached such a level that drugs work reliably with a minimum of side effects and consequences for the body. Of course, they do not eliminate psychological problems, but they provide a runway for climbing to the height where these problems could be eliminated. The antidepressant began to noticeably act somewhere in 3-4 weeks after the start of the reception. The mood improved, strength appeared, life began to bring pleasure. Then slowly: communication with friends began to recover, I began to go out, my libido and the desire to do something woke up. I recovered at work: when getting to the toilet is a huge test, work becomes something unbearable. nine0003
I recovered at work: when getting to the toilet is a huge test, work becomes something unbearable. nine0003
Depersonalization is, in the usual sense, the loss of oneself; when you can't understand what kind of person you are. Recovery after this leads to a rethinking of life attitudes. For example, in the past, I limited myself, tried to conform to the ideas dictated by society. He lived according to the principle “as it should be”, and not “as I want”. During this period, the understanding of one's person is lost: who are you? why are you? who are you supposed to be? You are depersonalizing. At the turning point of frustration, you understand that you need to live for yourself, and not for others, you stop constantly looking for flaws and correcting them in order to become someone. I accepted myself." nine0003
Anastasia, 20 years old: “At school, I was often bullied because of my excess weight, no one took me seriously at home, there were constant screams and scandals because of my father’s alcohol addiction. At the age of 15, I decided to try drugs and, not knowing the “correct dosages”, I took too much at one time. After that, my health deteriorated sharply: short-term panic attacks began, heart palpitations, unsteadiness of gait, dizziness appeared. At first I thought that I had something with my heart or blood vessels; over time, this developed into a fear of a heart attack, stroke, or sudden death. Then there was an examination of the whole body, but nothing concrete was found out: the doctors either did not find anything, or made a diagnosis of "vegetovascular dystonia". One doctor advised me to get tested for cancer. nine0003
At the age of 15, I decided to try drugs and, not knowing the “correct dosages”, I took too much at one time. After that, my health deteriorated sharply: short-term panic attacks began, heart palpitations, unsteadiness of gait, dizziness appeared. At first I thought that I had something with my heart or blood vessels; over time, this developed into a fear of a heart attack, stroke, or sudden death. Then there was an examination of the whole body, but nothing concrete was found out: the doctors either did not find anything, or made a diagnosis of "vegetovascular dystonia". One doctor advised me to get tested for cancer. nine0003
Over time, the situation progressed. There was a terrible feeling inside, like anxiety: I couldn’t sleep normally, it seemed that I would die any minute. One day I realized that I did not feel my body. There was a feeling of lightness and weightlessness at the same time, and then I began to catch myself thinking that it was as if I were not there. The sensations in my hands became not mine, the reflection in the mirror was not the same. Then I realized that I was in danger not of a heart attack, but of schizophrenia. I completely surrendered to this fear: the physical symptoms disappeared, there was an indescribable horror that now I would lose touch with reality and control over myself. I began to hide the handle from the balcony so that in a fit of unconsciousness the window would not suddenly jump out. The world as I knew it was shattered. Going out into the street, I understood that there was a big barrier between me and reality. The world behind the glass seemed flat, colorless, dead. I couldn't figure out if this was a dream or reality, or maybe I had died altogether. Time just stopped, it didn't exist, it didn't exist for me. And in the soul there is emptiness, silence and no emotions. nine0003
Then I realized that I was in danger not of a heart attack, but of schizophrenia. I completely surrendered to this fear: the physical symptoms disappeared, there was an indescribable horror that now I would lose touch with reality and control over myself. I began to hide the handle from the balcony so that in a fit of unconsciousness the window would not suddenly jump out. The world as I knew it was shattered. Going out into the street, I understood that there was a big barrier between me and reality. The world behind the glass seemed flat, colorless, dead. I couldn't figure out if this was a dream or reality, or maybe I had died altogether. Time just stopped, it didn't exist, it didn't exist for me. And in the soul there is emptiness, silence and no emotions. nine0003
I found out that this is not schizophrenia on a site about dissociative disorder. Thus began a new phase. On VKontakte, I found a group about dereal, where there were hundreds of people like me. For about a week I sat in the community, reading information, personal stories and recommendations, until I fully understood that this was it - depersonalization-derealization disorder.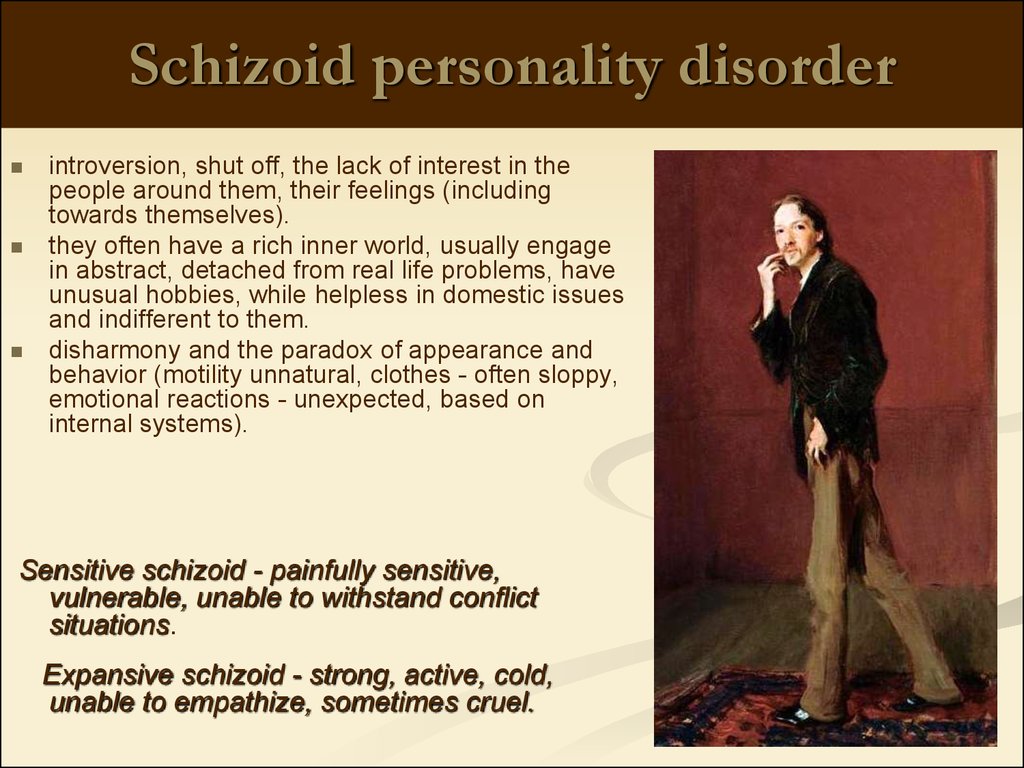
In the 11th grade, everything got to the point that I was taken from the exam in an ambulance. When I went to the doctor, he started asking something, and I was silent: I was so tired of this shit that I could not say a word. My parents found out that I have serious mental problems. It seemed to me that my mother did not understand me. I was again taken to the doctors, but we failed to find an intelligent specialist. In Soviet-era hospitals, doctors are not at all familiar with depersonalization: in one of these, I was prescribed 12 dubious pills a day, and glycine was also completely useless for my symptoms. There were doctors who were more interested in my outlook on life than my health. nine0003
As a result, I found my psychiatrist, with whom we still keep in touch, through my mother's friend. If we talk about treatment, then you can’t do without antidepressants. They help to return to the previous mode and significantly improve the condition. Now I'm 20, and I'm still on pills: I decided that it's better to feel good with them than to think about suicide every day.
“The basis of the depersonalization-derealization syndrome is an attempt of the psyche to adapt to stress in conditions of its high intensity, for example, during fear or panic. This syndrome as a separate disorder is included in the international classification of diseases (ICD-10), but often occurs as a secondary syndrome with severe anxiety, depression and other acute conditions. Depersonalization and derealization, although combined into one term due to their similarity and general nature, represent two independent symptoms that can manifest themselves separately from each other. During depersonalization, the patient's own face, figure, smile, speech seem unfamiliar, as if you are watching yourself as an outsider. Derealization, on the other hand, concerns the perception of the environment: place, time, circumstances, etc. Sometimes a feeling of “drunkenness”, “unreality” and “floating picture” is added. nine0003
The main cause of DP/DR lies in the activation of opiate receptors - there is an assumption that in this way the human body tries to reduce severe anxiety. Stress can become a reason if it was intense and caused a vegetative crisis (like a panic attack).
Feelings during depersonalization-derealization frighten with their unusualness. It seems to the patient that he has lost control of his own body, and this in itself provokes even more intense fear. It differs from schizophrenia primarily in the absence of symptoms of psychosis (hallucinations, delusions, catatonia, etc.). Also, the DP / DR syndrome can be observed in acute psychotic episodes, but then there must be appropriate mandatory symptoms of a severe mental illness. nine0003
Despite its prevalence, this diagnosis is not fully understood in terms of mechanisms and origin, which leads to difficulties in therapy. In the US, the disorder is treated primarily with antidepressants and lamotrigine. In Russia, there is no clear standard and recommendations: in DP / DR, they often look for the “main disorder”, hoping that the syndrome will recede on its own. It is not uncommon for depersonalization or derealization to resolve quickly if it occurs in the context of a panic or other anxiety disorder, but it can take years to treat these disorders in depression and bipolar affective disorder. nine0003
nine0003
tell your friends
tags
mental illnesspsychiatry depersonalization
Detachment Detachment | What is Detachment Detachment
Ironic detachment is the only way not to get upset.
Bel Kaufman. Up the stairs leading down
Detachment as a quality of personality is the ability for inner life, for building relationships with oneself, for distancing in interpersonal relationships, achieving an internal state of calmness and staying away from manifestations of bias, tendentiousness and emotionality. nine0073
Success in interpersonal relationships depends on mutual respect, which involves the ability to keep and maintain a certain distance from the other person. Nothing good will come of it if you go to extremes, allowing your surroundings familiarity and familiarity. As the poet wrote: “You cannot see a face face to face. Big things are seen from a distance. Relationships built from positions of arrogance, coldness and alienation are also doomed to break.
Relationships built from positions of arrogance, coldness and alienation are also doomed to break.
Relationships become wonderful when a golden mean is found between extremes and excesses, allowing you to feel respect from another person, to feel a certain freedom and psychological comfort. The golden mean is alien to indifference, isolation and indifference. People in their family desire close relationships. But close relationships just imply respect for each other, the realization of the fact that a loved one is a unique, inimitable world. No matter how close we are, everyone has their own individual worldview and understanding of the world. Everyone has the right to be different, and others have the same right to be different. nine0003
Intimacy is impossible without detachment. To respect the other means to respect his right to live an inner life, to understand that the other person achieves harmony only when he has learned to get along with himself and with the outside world. If you hang on your husband’s ears all day, he will not only “go into the cave” for a while, but in a panic will run away from his sticky wife.
If you hang on your husband’s ears all day, he will not only “go into the cave” for a while, but in a panic will run away from his sticky wife.
Overexertion is contraindicated for a man. He must fulfill his duties, but, nevertheless, the family for him should be a place of rest, a place where he is charged and inspired by female energy to build relationships with the outside world. If a woman thinks that loading her husband with work saves her from bad thoughts, she is deeply mistaken. What is the best way to relax? Guessed. Overload, overstrain - a direct road to treason and drunkenness. nine0003
When spouses build a relationship at a French kiss distance, they begin to exchange bad karma. It is well known that close people hurt each other more. If a stranger said something offensive, rude, this, as a rule, does not cause an emotional storm. But if the husband, son, father said - a completely different calico. An excessively short distance in a relationship, an excessively annoying rapprochement leads to tension in the relationship. Too high positive expectations bind us with a loved one. When it doesn't live up to our expectations, burnout occurs. nine0003
Too high positive expectations bind us with a loved one. When it doesn't live up to our expectations, burnout occurs. nine0003
When a person enters a state of detachment, he gradually accumulates self-control, inner strength and the ability to behave in any difficult circumstances in a balanced, calm and prudent manner. A detached person is not in a hurry and does things in a state of extreme concentration and attentiveness. Thus, he ensures the successful result of his actions.
Detachment is often associated with humor. Don Juan constantly laughed at the seriousness and arrogance of his student Carlos. Whenever Carlos became serious or upset, don Juan burst into laughter. This laugh came from a sense of detachment. Don Juan said to Carlos: “As long as it seems to you that there is nothing more important than you in this world, you will not be able to feel the world around you. You are like a blinkered horse, you see only yourself, apart from everything else.” nine0003
Detachment can come from the realization that one person cannot control all the bad things that happen on the planet. He thinks in terms of the well-known saying: "The murder of one person is a tragedy, the death of millions is a statistic." It creates the appearance of soullessness and indifference. Therefore, a compassionate decent person can receive the insulting label of a misanthrope. Albert Szent-Györgyi, in the context of this thought, writes: “I am strongly impressed by the suffering of one person, and I am ready to risk my life for him. But I can speak quite detachedly about the infection of our big cities with hundreds of millions of dead. I am not capable of multiplying the suffering of one in a hundred million.” nine0003
He thinks in terms of the well-known saying: "The murder of one person is a tragedy, the death of millions is a statistic." It creates the appearance of soullessness and indifference. Therefore, a compassionate decent person can receive the insulting label of a misanthrope. Albert Szent-Györgyi, in the context of this thought, writes: “I am strongly impressed by the suffering of one person, and I am ready to risk my life for him. But I can speak quite detachedly about the infection of our big cities with hundreds of millions of dead. I am not capable of multiplying the suffering of one in a hundred million.” nine0003
Detachment - the ability to live an inner life at a certain distance from others. Detachment waits for happiness from within itself and, when it comes, gives it to loved ones and others. O. G. Torsunov states: “You understand what an interesting paradox is. On the one hand, a person must be completely removed from wanting happiness from others, and on the other hand, he must resolutely give happiness himself to other people, and only then can he be steadily happy in life. Detachment from others is achieved through the inner life. Inner life means a relationship with yourself ... If you move away from a person, and he starts to get angry, angry and destroy everything, this means that you have no respect in your family. Respect must be developed in every family, so the person must be given the opportunity to step back. If, for example, you move away, he starts to get mad, then you need to move away further, even further, even further. You can go to your mother for a while until respect arises. Because the further you withdraw, the more likely it is to arise, withdrawal develops respect. Withdrawal because it causes attachment, the person begins to wait, he begins to feel that he is losing, and therefore respect wakes up again. And you need to be able to choose the right distance. When people properly distance themselves from each other, in accordance with their ability to be together, they save the family and more than that, harmony and love are gradually restored in their family.
Detachment from others is achieved through the inner life. Inner life means a relationship with yourself ... If you move away from a person, and he starts to get angry, angry and destroy everything, this means that you have no respect in your family. Respect must be developed in every family, so the person must be given the opportunity to step back. If, for example, you move away, he starts to get mad, then you need to move away further, even further, even further. You can go to your mother for a while until respect arises. Because the further you withdraw, the more likely it is to arise, withdrawal develops respect. Withdrawal because it causes attachment, the person begins to wait, he begins to feel that he is losing, and therefore respect wakes up again. And you need to be able to choose the right distance. When people properly distance themselves from each other, in accordance with their ability to be together, they save the family and more than that, harmony and love are gradually restored in their family. ” nine0003
” nine0003
Through detachment, a person tries to find a way out in the question of how to deal with attachments to his relatives, friends, material wealth. The Indian philosopher Jiddu Krishnamurti wrote in The Book of Life: “In order to avoid suffering, we cultivate detachment. Attachment and foresight will sooner or later bring grief, we want to become detached. Attachment is satisfying, but when we get hurt from attachment, we want to get satisfaction in another way, through detachment. Detachment is the same as attachment as long as it bears the fruits of pleasure. Therefore, we are really looking for it - it is pleasure and reward; we crave satisfaction by any means. We are dependent or attached to something because it brings us pleasure, security, strength, a sense of well-being, albeit with sorrow and fear. We seek detachment as much as we seek pleasure, so as not to get hurt, not to be wounded inside. All our aspirations are aimed at pleasure, receiving rewards. Without condemning or justifying ourselves, we must try to understand this process, because if we do not understand, then there is and cannot be any way out of the confusion and contradictions that have been created.