Depressive and anxiety disorders
Mental Health Conditions: Depression and Anxiety | Overviews of Diseases/Conditions | Tips From Former Smokers
Español (Spanish)
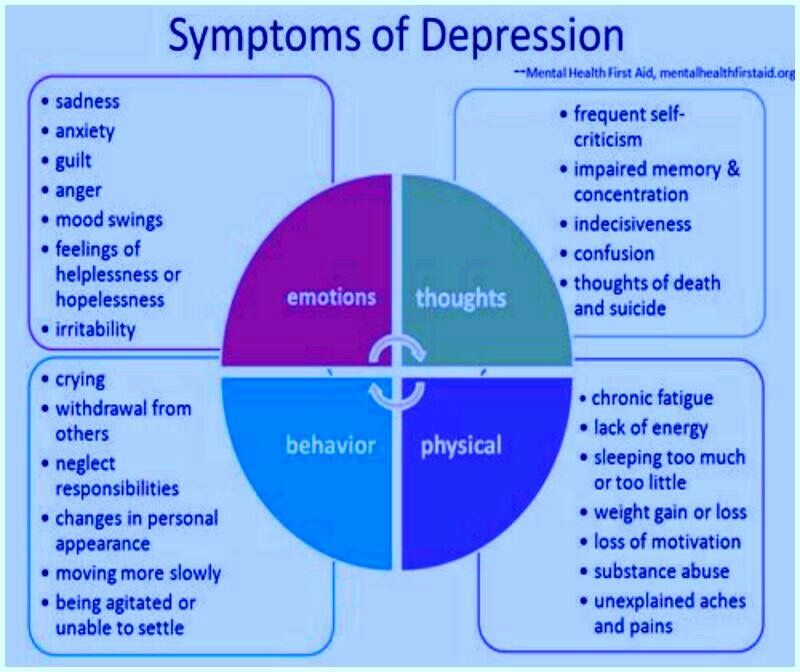
Depression is more than just feeling down or having a bad day. When a sad mood lasts for a long time and interferes with normal, everyday functioning, you may be depressed. Symptoms of depression include:1
- Feeling sad or anxious often or all the time
- Not wanting to do activities that used to be fun
- Feeling irritable‚ easily frustrated‚ or restless
- Having trouble falling asleep or staying asleep
- Waking up too early or sleeping too much
- Eating more or less than usual or having no appetite
- Experiencing aches, pains, headaches, or stomach problems that do not improve with treatment
- Having trouble concentrating, remembering details, or making decisions
- Feeling tired‚ even after sleeping well
- Feeling guilty, worthless, or helpless
- Thinking about suicide or hurting yourself
The following information is not intended to provide a medical diagnosis of major depression and cannot take the place of seeing a mental health professional. If you think you are depressed‚ talk with your doctor or a mental health professional immediately. This is especially important if your symptoms are getting worse or affecting your daily activities.
Top of Page
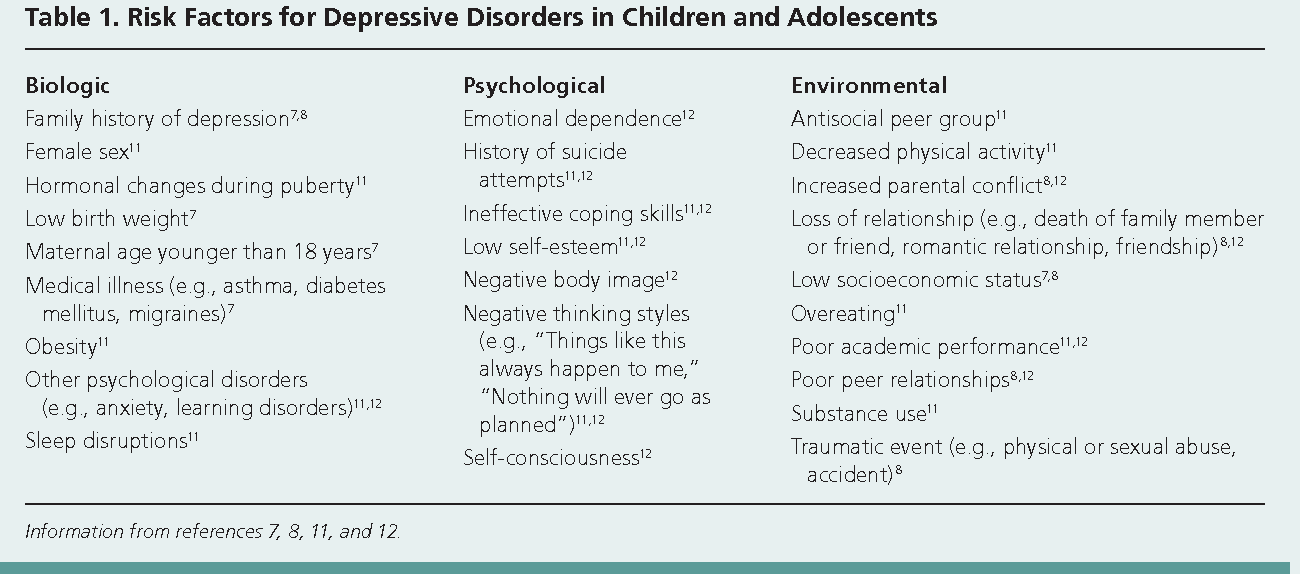
The exact cause of depression is unknown. It may be caused by a combination of genetic, biological, environmental, and psychological factors.2 Everyone is different‚ but the following factors may increase a person’s chances of becoming depressed:1
- Having blood relatives who have had depression
- Experiencing traumatic or stressful events, such as physical or sexual abuse, the death of a loved one, or financial problems
- Going through a major life change‚ even if it was planned
- Having a medical problem, such as cancer, stroke, or chronic pain
- Taking certain medications. Talk to your doctor if you have questions about whether your medications might be making you feel depressed.
- Using alcohol or drugs
Top of Page
In general‚ about 1 out of every 6 adults will have depression at some time in their life. 3 Depression affects about 16 million American adults every year.4 Anyone can get depressed, and depression can happen at any age and in any type of person.
3 Depression affects about 16 million American adults every year.4 Anyone can get depressed, and depression can happen at any age and in any type of person.
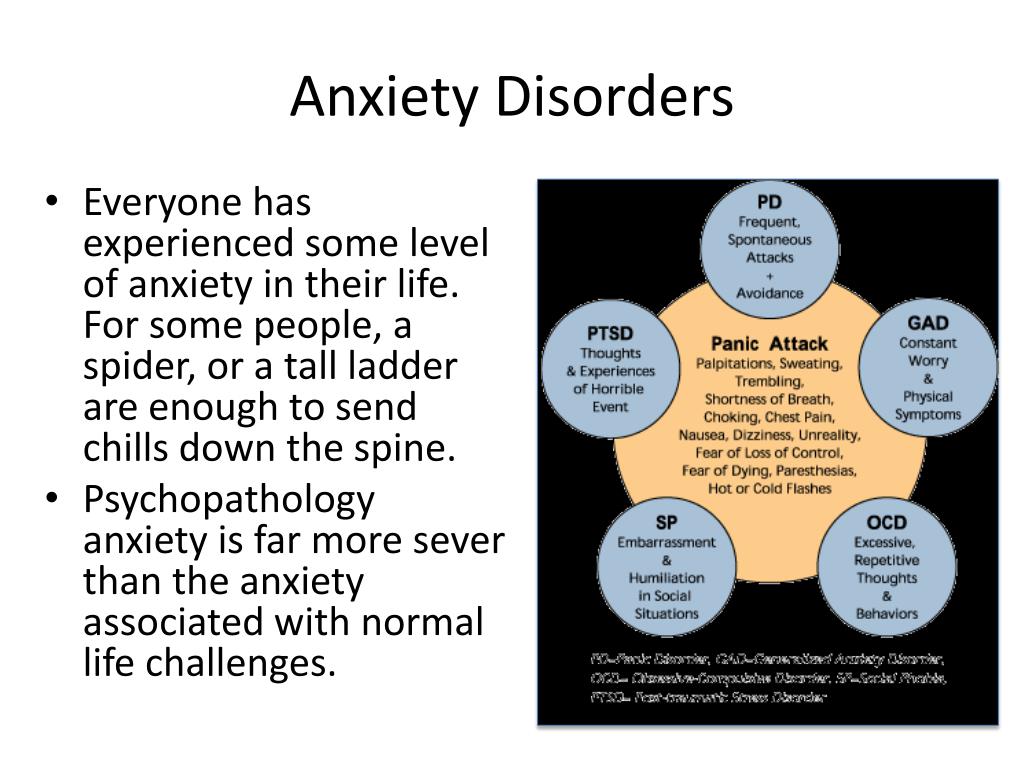
Many people who experience depression also have other mental health conditions.1,5 Anxiety disorders often go hand in hand with depression. People who have anxiety disorders struggle with intense and uncontrollable feelings of anxiety, fear, worry, and/or panic.1 These feelings can interfere with daily activities and may last for a long time.
Top of Page
Smoking is much more common among adults with mental health conditions, such as depression and anxiety, than in the general population.6 About 3 out of every 10 cigarettes smoked by adults in the United States are smoked by persons with mental health conditions.
6 Why smokers are more likely than nonsmokers to experience depression, anxiety, and other mental health conditions is uncertain. More research is needed to determine this.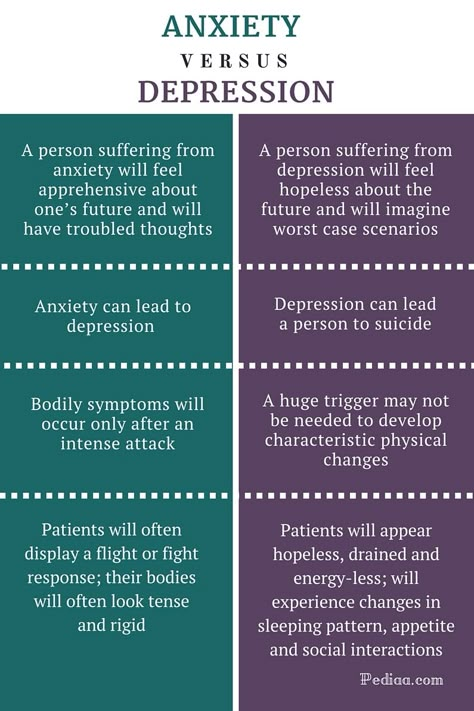 No matter the cause‚ smoking is not a treatment for depression or anxiety. Getting help for your depression and anxiety and quitting smoking is the best way to feel better.
No matter the cause‚ smoking is not a treatment for depression or anxiety. Getting help for your depression and anxiety and quitting smoking is the best way to feel better.
Top of Page
Many helpful treatments for depression are available. Treatment for depression can help reduce symptoms and shorten how long the depression lasts. Treatment can include getting therapy and/or taking medications. Your doctor or a qualified mental health professional can help you determine what treatment is best for you.
- What Is Depression?
- What Causes Depression?
- Who Gets Depression?
- What Is the Link Between Smoking and Mental Health Conditions?
- What Are the Treatments for Depression?
- Depression and Suicide: Getting Help in a Crisis
- Additional Resources
- References
Web
- Quit Smoking
- Smokefree.govexternal icon
Smartphone Apps/Text
- Text QUITNOW to 333888—Message and data rates may apply
- quitSTART appexternal icon—tips, information, and challenges to help you quit
Telephone
- 1-800-QUIT-NOW
- 1-855-DÉJELO-YA (Español [Spanish])
- Asian Smokers’ Quitlineexternal icon
- 1-800-838-8917 (中文 (Chinese) [Cantonese & Mandarin])
- 1-800-556-5564 (한국어 [Korean])
- 1-800-778-8440 (Tiếng Việt [Vietnamese])
Rebecca M.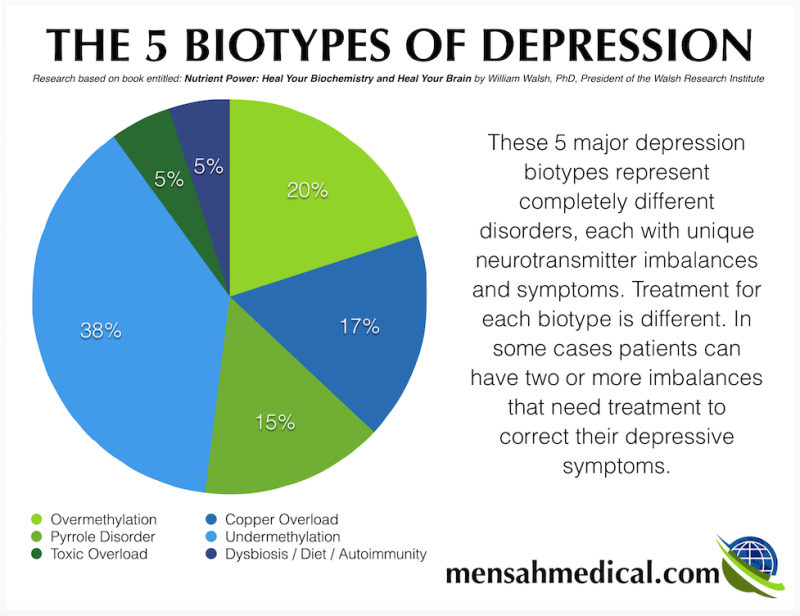 , age 57, struggled with depression and had a few wake-up calls as a smoker. She felt depressed and smoked cigarettes to help her cope with her feelings. The more Rebecca smoked, the harder it seemed to quit. Rebecca finally quit smoking after getting care for her depression and realizing that she had to take care of her own health. She now leads a new, smokefree life.
, age 57, struggled with depression and had a few wake-up calls as a smoker. She felt depressed and smoked cigarettes to help her cope with her feelings. The more Rebecca smoked, the harder it seemed to quit. Rebecca finally quit smoking after getting care for her depression and realizing that she had to take care of her own health. She now leads a new, smokefree life.
“I quit smoking and I got care for my depression.”
- Therapy. Many people benefit from psychotherapy—also called therapy or counseling.7,8 Most therapy lasts for a short time and focuses on thoughts‚ feelings‚ and issues that are happening in your life now. In some cases‚ understanding your past can help‚ but finding ways to address what is happening in your life now can help you cope and prepare you for challenges in the future.With therapy, you’ll work with your therapist to learn skills to help you cope with life, change behaviors that are causing problems‚ and find solutions.
 Do not feel shy or embarrassed about talking openly and honestly about your feelings and concerns. This is an important part of getting better.Some common goals of therapy include:
Do not feel shy or embarrassed about talking openly and honestly about your feelings and concerns. This is an important part of getting better.Some common goals of therapy include: - Getting healthier
- Quitting smoking and stopping drug and alcohol use
- Overcoming fears or insecurities
- Coping with stress
- Making sense of past painful events
- Identifying things that worsen your depression
- Having better relationships with family and friends
- Understanding why something bothers you and creating a plan to deal with it
- Medication. Many people with depression find that taking prescribed medications called antidepressants can help improve their mood and coping skills. Talk to your doctor about whether they are right for you. If your doctor writes you a prescription for an antidepressant‚ ask exactly how you should take the medication. If you are already using nicotine replacement therapy or another medication to help you quit smoking, be sure to let your doctor know.
 Several antidepressant medications are available‚ so you and your doctor have options to choose from. Sometimes it takes several tries to find the best medication and the right dose for you, so be patient. Also be aware of the following important information:
Several antidepressant medications are available‚ so you and your doctor have options to choose from. Sometimes it takes several tries to find the best medication and the right dose for you, so be patient. Also be aware of the following important information: - When taking these medications‚ it is important to follow the instructions on how much to take. Some people start to feel better a few days after starting the medication‚ but it can take up to 4 weeks to feel the most benefit. Antidepressants work well and are safe for most people‚ but it is still important to talk with your doctor if you have side effects. Side effects usually do not get in the way of daily life‚ and they often go away as your body adjusts to the medication.
- Don’t stop taking an antidepressant without first talking to your doctor. Stopping your medicine suddenly can cause symptoms or worsen depression. Work with your doctor to safely adjust how much you take.
- Some antidepressants may cause risks during pregnancy.
 Talk with your doctor if you are pregnant or might be pregnant, or if you are planning to become pregnant.
Talk with your doctor if you are pregnant or might be pregnant, or if you are planning to become pregnant. - Antidepressants cannot solve all of your problems. If you notice that your mood is getting worse or if you have thoughts about hurting yourself‚ it is important to call your doctor right away.
Quitting smoking will not interfere with your mental health treatment or make your depression worse. In fact, research shows that quitting smoking can actually improve your mental health in the long run.9,10,11
Top of Page
Some people who are depressed may think about hurting themselves or committing suicide (taking their own life). If you or someone you know is having thoughts about hurting themselves or committing suicide‚ please seek immediate help. The following resources can help:
- Call or text the National Suicide Prevention Lifeline at 988, available 24 hours a day, 7 days a week.
- Call 911 or go to the nearest hospital emergency department for emergency medical treatment.
- Call your mental health provider.
- Get help from your primary doctor or other health care provider.
- Reach out to a close friend or loved one.
- Contact a minister, spiritual leader, or someone else in your faith community.
Top of Page
Web
- Quit Smoking
- Smokefree.govexternal icon
Smartphone Apps/Text
- Text QUITNOW to 333888—Message and data rates may apply
- quitSTART appexternal icon—tips, information, and challenges to help you quit
Telephone
- 1-800-QUIT-NOW
- 1-855-DÉJELO-YA (Español [Spanish])
- Asian Smokers’ Quitlineexternal icon
- 1-800-838-8917 (中文 (Chinese) [Cantonese & Mandarin])
- 1-800-556-5564 (한국어 [Korean])
- 1-800-778-8440 (Tiếng Việt [Vietnamese])
Rebecca M., age 57, struggled with depression and had a few wake-up calls as a smoker. She felt depressed and smoked cigarettes to help her cope with her feelings.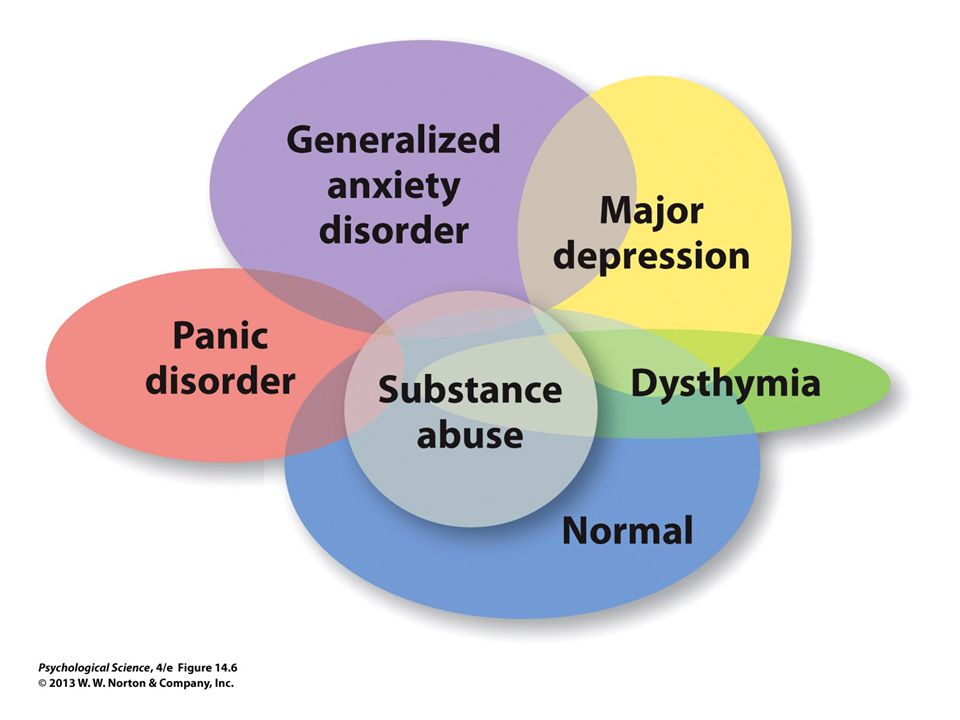 The more Rebecca smoked, the harder it seemed to quit. Rebecca finally quit smoking after getting care for her depression and realizing that she had to take care of her own health. She now leads a new, smokefree life.
The more Rebecca smoked, the harder it seemed to quit. Rebecca finally quit smoking after getting care for her depression and realizing that she had to take care of her own health. She now leads a new, smokefree life.
“I quit smoking and I got care for my depression.”
If you are a smoker and dealing with depression or anxiety, consider the following resources:
- Depression
- MentalHealth.gov
- National Alliance on Mental Illness (NAMI)
- National Institute of Mental Health
- What Is Depression?
- What Are Anxiety Disorders?
- Anxiety and Depression Association of America
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition. Arlington, VA: American Psychiatric Publishing, 2013 [accessed 2018 Mar 22].
- Belmaker RH, Agam G. Major Depressive Disorder. New England Journal of Medicine 2008;358:355–68 [accessed 2018 Mar 22].
- Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE.
 Lifetime Prevalence and Age-of-Onset Distributions of DSM-IV Disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry 2005;62(6):593-602 [accessed 2018 Mar 22].
Lifetime Prevalence and Age-of-Onset Distributions of DSM-IV Disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry 2005;62(6):593-602 [accessed 2018 Mar 22]. - Substance Abuse and Mental Health Services Administration. Results from the 2013 National Survey on Drug Use and Health: Mental Health Findings [PDF – 2.37MB]. Rockville, MD: Department of Health and Human Services, Substance Abuse and Mental Health Services Administration, Center for Behavioral Health Statistics and Quality, 2014 [accessed 2018 Mar 22].
- Kessler RC, Birnbaum HG, Shahly V, Bromet E, Hwang I, McLaughlin KA, Sampson N, Andrade LH, de Girolamo G, Demyttenaere K, Haro JM, Karam AN, Kostyuchenko S, Kovess V, Lara C, Levinson D, Matschinger H, Nakane Y, Browne MO, Ormel J, Posada-Villa J, Sagar R, Stein DJ. Age Differences in the Prevalence and Co-Morbidity of DSM-IV Major Depressive Episodes: Results From the WHO World Mental Health Survey Initiative. Depression and Anxiety 2010;27(4):351–64 [accessed 2018 Mar 22].

- Centers for Disease Control and Prevention. Vital Signs: Current Cigarette Smoking Among Adults Aged ≥ 18 Years with Mental Illness—United States, 2009–2011. Morbidity and Mortality Weekly Report 2013;62(05):81–7 [accessed 2018 Mar 22].
- American Psychiatric Association. Practice Guidelines for the Treatment of Patients With Major Depressive Disorder, Third Edition [PDF – 1.64MB]. Arlington, VA: American Psychiatric Publishing, 2010 [accessed 2018 Mar 22].
- Davidson JRT. Major Depressive Disorder Treatment Guidelines in America and Europe. Journal of Clinical Psychiatry 2010;71(Suppl E1):e04 [accessed 2018 Mar 22].
- Tidey JW, Miller ME. Smoking Cessation and Reduction in People With Chronic Mental Illness. BMJ 2015; doi:http://dx.doi.org/10.1136/bmj.h5065 [accessed 2018 Mar 22].
- Evins AE, Cather C, Laffer A. Treatment of Tobacco Use Disorders in Smokers With Serious Mental Illness: Toward Clinical Best Practices. Harvard Review of Psychiatry 2015;23(2):90–8 [accessed 2018 Mar 22].
- Hitsman B, Moss TG, Montoya ID, George TP. Treatment of Tobacco Dependence in Mental Health and Addictive Disorders. Canadian Journal of Psychiatry 2009;54(6):368–78 [accessed 2018 Mar 22].
Top of Page
What is Depression? | Anxiety and Depression Association of America, ADAA
264 million people worldwide live with depression.* Our World Data
In 2017, around 17.3 million adults age 18 or older in the U.S. had experienced at least one major depressive episode in the last year (6.7% of adults in the U.S.).* (National Institute of Mental Health)
- Types of Depression
- ADAA Resources
- Additional Resources
Losing a loved one, getting fired from a job, going through a divorce, and other difficult situations can lead a person to feel sad, lonely and scared. These feelings are normal reactions to life's stressors. Most people feel low and sad at times. However, in the case of individuals who are diagnosed with depression as a psychiatric disorder, the manifestations of the low mood are much more severe and they tend to persist.
Depression occurs more often in women than men. Some differences in the manner in which the depressed mood manifests have been found based on sex and age. In men it manifests often as tiredness, irritability and anger. They may show more reckless behavior and abuse drugs and alcohol. They also tend to not recognize that they are depressed and fail to seek help. In women depression tends to manifest as sadness, worthlessness, and guilt. In younger children depression is more likely to manifest as school refusal, anxiety when separated from parents, and worry about parents dying. Depressed teenagers tend to be irritable, sulky, and get into trouble in school. They also frequently have co-morbid anxiety, eating disorders, or substance abuse. In older adults depression may manifest more subtly as they tend to be less likely to admit to feelings of sadness or grief and medical illnesses which are more common in this population also contributes or causes the depression.
- Download a brochure
- Depression symptoms
- Depression treatment and management
- Screen yourself or a loved one for depression
- Bipolar disorder
- Additional Resources
- MoodNetwork
Types of Depression
There are different types of depressive disorders, and while there are many similarities among them, each depressive disorder has its own unique set of symptoms.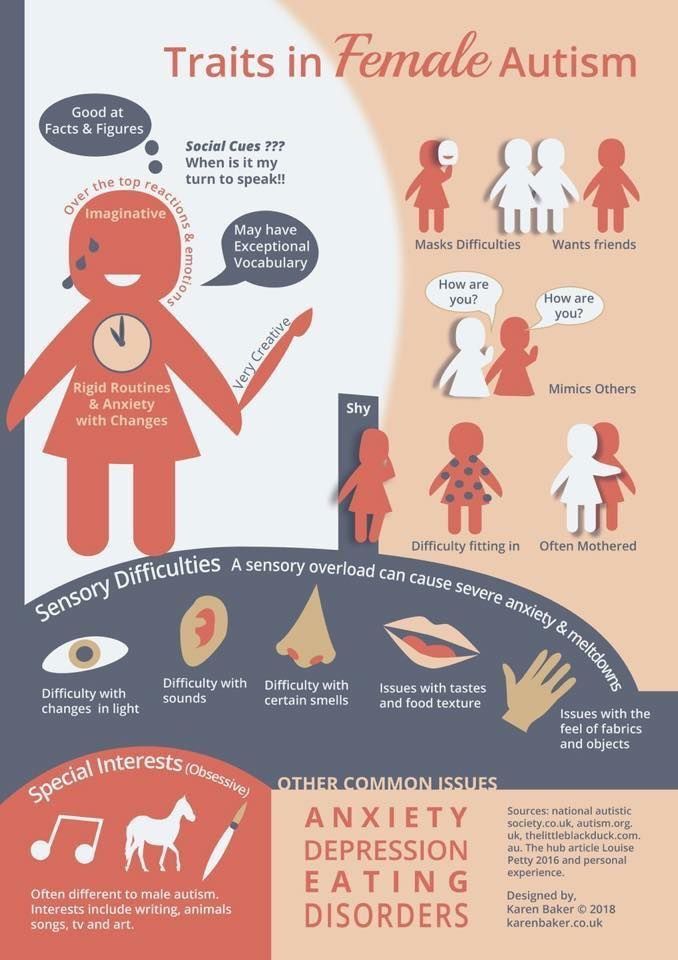
The most commonly diagnosed form of depression is Major Depressive Disorder. In 2017, around 17.3 million aged 18 years or older in the U.S. had experienced at least one major depressive episode in the last year, which represented 6.7 percent of all American adults. Depression is the leading cause of disability in the United States among people ages 15-44. View the SAMSHA website for statistics from the 2017 National Survey on Drug Use and Health.
Major depression is characterized by having at least five nine common symptoms. One of the symptoms must be either an overwhelming feeling of sadness or a loss of interest and pleasure in most usual activities. The other symptoms that are associated with major depression include decrease or increase in appetite, insomnia or hypersomnia, psychomotor agitation or retardation, constant fatigue, feelings of worthlessness or excessive and inappropriate guilt, recurrent thoughts of death and suicidal ideation with or without specific plans for committing suicide, and cognitive difficulties, such as, diminished ability to think, concentrate and take decisions. The symptoms must persist for two weeks or longer and represent a significant change from previous functioning. Social, occupational, educational, or other important functioning are impacted by major depressive disorder. For instance, the person may start missing work or school, or stop going to classes or their usual social activities.
The symptoms must persist for two weeks or longer and represent a significant change from previous functioning. Social, occupational, educational, or other important functioning are impacted by major depressive disorder. For instance, the person may start missing work or school, or stop going to classes or their usual social activities.
Another type of depression is called Persistent depressive disorder (dysthymia). The essential feature of this mood disorder is a low, dark or sad mood that is persistently present for most of the day and on most days, for at least 2 years (children and adolescents may experience predominantly irritability and the mood persist for at least 1 year). For the individual to receive the diagnosis of persistent depressive disorder they should also have two of the diagnostic symptoms which include poor appetite or overeating, insomnia or hypersomnia, low energy or fatigue, low self-esteem, poor concentration, difficulty making decisions, or feelings of hopelessness.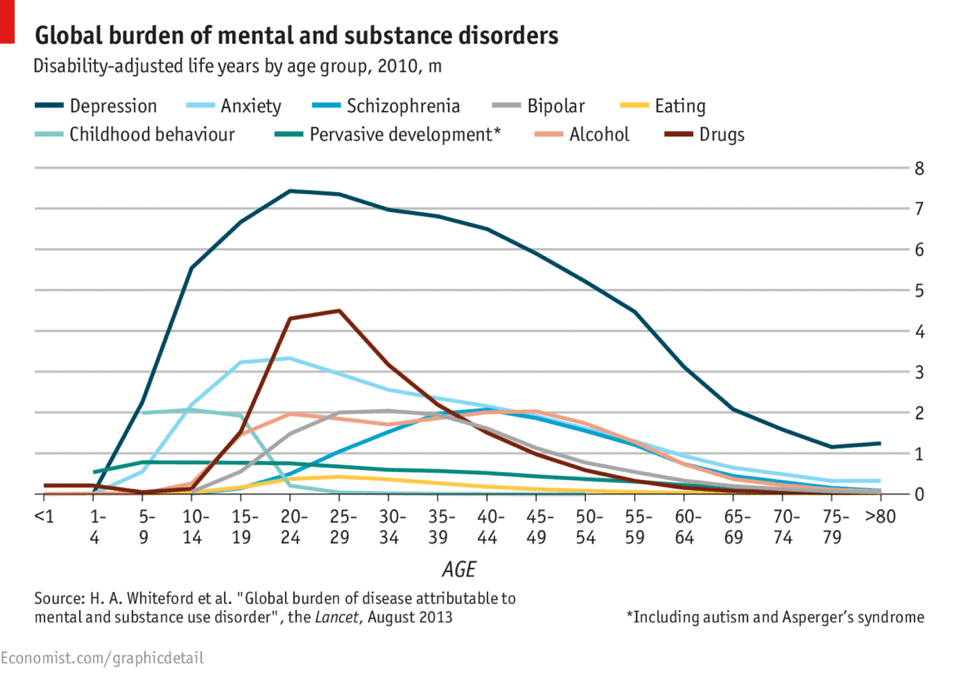 During this period, any symptom-free intervals last no longer than two months. The symptoms are not as severe as with major depression. Major depression may precede persistent depressive disorder, and major depressive episodes may also occur during persistent depressive disorder.
During this period, any symptom-free intervals last no longer than two months. The symptoms are not as severe as with major depression. Major depression may precede persistent depressive disorder, and major depressive episodes may also occur during persistent depressive disorder.
Premenstrual dysphoric disorder is another manifestation of depression which is a severe and sometimes disabling extension of premenstrual syndrome (PMS). Although regular PMS and Premenstrual dysphoric disorder (PMDD) both have physical and emotional symptoms, the mood changes in PMDD are much more severe and can disrupt social, occupational, and other important areas of functioning. In both PMDD and PMS, symptoms usually begin seven to 10 days before the start of a menstrual period and continue for the first few days of the period. Both PMDD and PMS may also cause breast tenderness, bloating, fatigue, and changes in sleep and eating habits. PMDD is characterized by emotional and behavioral symptoms that are more severe, such as sadness or hopelessness, anxiety or tension, extreme moodiness, irritability or anger.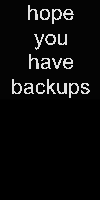
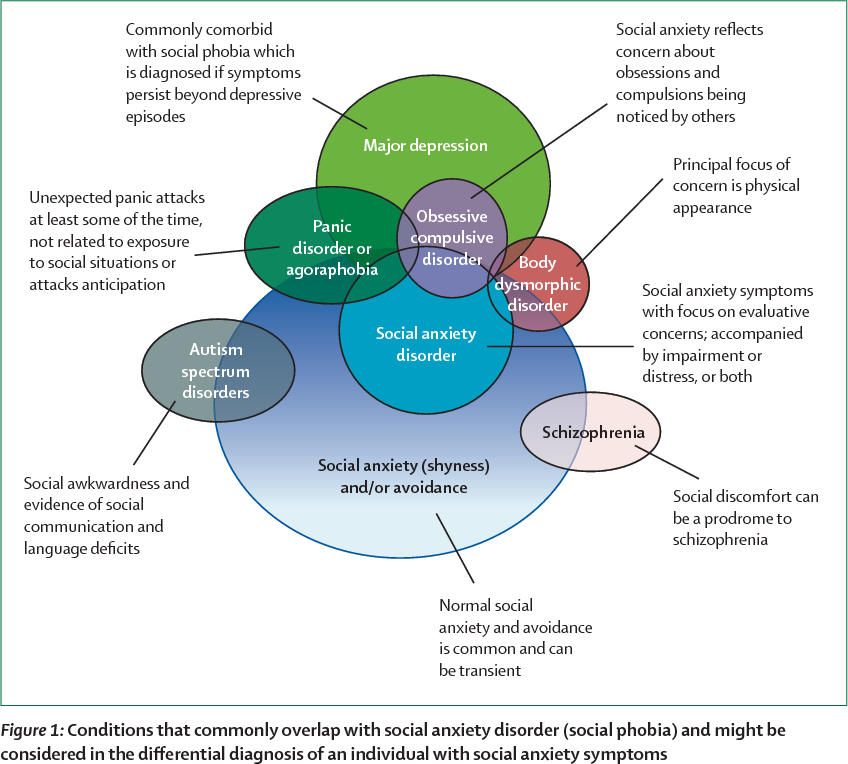
Some medical conditions can trigger depressive symptoms in individuals. This is called depressive disorder due to another medical condition. Endocrine and reproductive system disorders are commonly associated with depressive symptoms. For example, people with low levels of the thyroid hormone (hypothyroidism) often experience fatigue, weight gain, irritability, memory loss, and low mood. When the hypothyroidism is treated it usually reduces the depression. Cushing's syndrome is another hormonal disorder caused by high levels of the hormone cortisol which can also cause depressive symptoms. Other conditions that have been found to cause depression include conditions such as HIV/AIDS, diabetes, strokes, Parkinson’s disease etc.
Adjustment Disorder with Depressed Mood is diagnosed when symptoms of depression are triggered within 3 months of onset of a stressor. The stressor usually involves a change of some kind in the life of the individual which he/she finds stressful.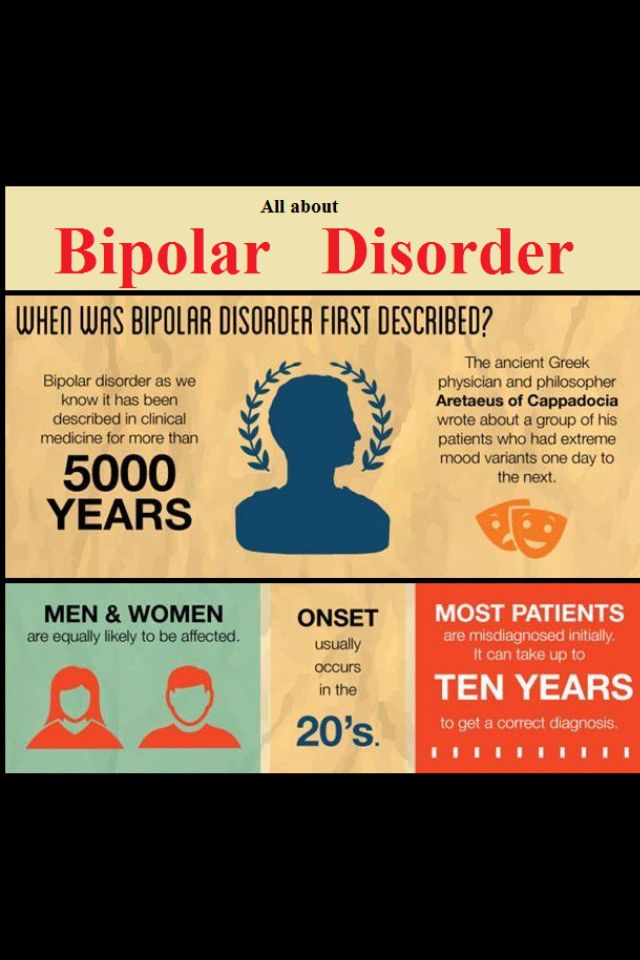 Sometimes the stressor can even be a positive event such as a new job, marriage, or baby which is nevertheless stressful for the individual. The distress is typically out of proportion to the expected reaction and the symptoms cause significant distress and impairment in functioning. The symptoms typically resolve within 6 months when the person begins to cope and adapt to the stressor, or when the stressor is removed. Treatment tends to be time limited and relatively simple since some additional support during the stressful period helps the person recover and adapt.
Sometimes the stressor can even be a positive event such as a new job, marriage, or baby which is nevertheless stressful for the individual. The distress is typically out of proportion to the expected reaction and the symptoms cause significant distress and impairment in functioning. The symptoms typically resolve within 6 months when the person begins to cope and adapt to the stressor, or when the stressor is removed. Treatment tends to be time limited and relatively simple since some additional support during the stressful period helps the person recover and adapt.
Another type of depression is related to changes in the length of days or seasonality. This type of depression is called Seasonal affective disorder (SAD). People with SAD suffer the symptoms of a Major Depressive Disorder only during a specific time of year, usually winter. This appears to be related to the shorter days of winter, and the lack of sunlight in many parts of the country.
Depression and Anxiety Disorders: Not the Same
Depression and anxiety disorders are different, but people with depression often experience symptoms similar to those of an anxiety disorder, such as nervousness, irritability, and problems sleeping and concentrating. But each disorder has its own causes and its own emotional and behavioral symptoms.
But each disorder has its own causes and its own emotional and behavioral symptoms.
Many people who develop depression have a history of an anxiety disorder earlier in life. There is no evidence one disorder causes the other, but there is clear evidence that many people suffer from both disorders.
Sleep and Anxiety and Depression
- Anxiety, Stress, Depression and Sleep
- Sleep Disorders
Sources:
1. NIMH: Depression Basics
2. View the NIMH website for statistics from the 2017 National Survey on Drug Use and Health
3. American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Arlington, VA: American Psychiatric Publishing.
4. Sadock, B. J., Sadock, V. A., & Ruiz, P. (2009). Comprehensive Textbook of Psychiatry (Ninth edition.) Philadelphia: Wolters Kluwer.
ADAA Resources: Webinars, Blog Posts and Brochures
Depression Brochure - 2022
Webinars
- Depression: How to Recognize it and How to Treat it
- Can Yoga Help with Depression? What Does the Research Say?
- Depresión y ansiedad en niños/Anxiety and Depression in Children - Spanish psychoeducational video
- Depresión/Depression
- Depression Among College Students
- Depression and Heart Disease: Chicken and the Egg, and What You Can Do
- For My Anxiety or Depression: Should I Use Medication or Therapy?
- How to Help Depressed and Suicidal Teenagers
- Asking Your Pharmacist About Medications for Anxiety and Depression
- Anxiety, Depression, and the LGBTQ Community: Thriving Through the Challenges
- Exercise Against Anxiety and Depression
- Our Kids: Anxiety and Depression
- Treatments for Anxious and Depressed Kids and Teens
- Bullying, Anxiety, and Depression
- What Is Cognitive-Behavioral Therapy and How Is It Used to Treat Anxiety and Depression?
- Depression: What You Need to Know About Medications
- Genetics of Depression and Anxiety: What Do Clinicians Need to Know? - ADAA professional webinar
- Mindfulness Over Matter: Integrating Mindfulness Into the Treatment of Depression - Presented in Partnership with The Child Mind Institute - ADAA professional webinar
- Management of Treatment Resistant Depression - ADAA professional webinar
- Introduction to the Magic of CBT for Anxiety, OCD, and Depression - ADAA professional webinar
- Psychotherapy for GAD and Comorbid Major Depression - ADAA professional webinar
Blog Posts
- Depression Across the Lifespan: Depression—and its Treatments—are Different for Each Life Stage
- What is Depression? How Can We Overcome It?
- Is My Child Depressed?
- Childhood Depression
- Watch, Ask and Listen: How to Tell if Your Child or Teen is Anxious or Depressed
- How Do You Talk to Your Loved One Suffering With Depression?
- Revolutionizing Depression Treatment with Digital Therapeutics
- Dealing with Valentine's Day Depression
- Criticism: Depression and Anxiety
- Can CBD Help with My Anxiety and Depression
- Influences of Cultural Differences in the Diagnosis and Treatment of Anxiety and Depression
- Revolutionizing Depression Treatment with Digital Therapeutics
- Heart Disease and Depression Often Go Hand in Hand: WomenHeart Can Help -
- Depression Among College Students
- Anxiety and Depression in Sexual and Gender Minority Individuals
- Dr.
 Chris’s Techniques For Lessening Anxiety And Depression
Chris’s Techniques For Lessening Anxiety And Depression - Seniors Coping with Anxiety and Depression
- Depression and Daily Life
- Alleviating Anxiety, Stress and Depression with the Pet Effect
- What is Depression and How Do I Know If I Have It?
- Depression Treatment – It Works
- Understanding Anxiety and Depression for LGBTQ People
Additional Resources
- What Is Major Depressive Disorder?, HealthCentral, ADAA President Charles Nemeroff, MD, PhD
- Tips for How to Explain Depression So Other People Understand, Healthline, ADAA Member David Rosmarin, PhD, ABPP
- Faster and Easier Approaches for Improving Patients' Depression Treatment Outcomes, CareForYourMind.org, ADAA Member Michael Thase, MD
- What to Expect From Therapy for Depression—and How to Start the Process, Self Magazine
- Some of the best books about depression in 2021, Medical News Today
- BlueCross BlueShield
- Child Mind Institute
- Depression and Bipolar Support Alliance
- Depression Stories on The Mighty
- Disability Benefits
- HeadsUpGuys
- Hope for Depression Research Foundation
- I Had a Black Dog, His Name Was Depression
- Major Depression: The Impact on Overall Health
- National Institute of Mental Health
- World Health Organization
Anxiety, depression and insomnia - the unity or autonomy of functional disorders
It is known that patients with so-called "functional" disorders constitute a significant proportion of patients in the daily practice of doctors of various profiles. Such disorders include insomnia, anxiety and depression, which are common in the practice of neurologists, and which pose the need to resolve the issue of their connection and cause-and-effect relationships.
Such disorders include insomnia, anxiety and depression, which are common in the practice of neurologists, and which pose the need to resolve the issue of their connection and cause-and-effect relationships.
In practice, we are talking about considering two possibilities: 1) as isolated independent conditions caused by factors specific to each of them, and, accordingly, having features of therapy; 2) as mutually potentiating states that can act as "masks" and continuations of each other and require a unified approach when choosing therapy.
In addition, there is another important aspect of the problem - the differentiation of organic and functional disorders of the CNS. It is generally accepted that organic diseases are based on structural disorders, i.e. an anatomical substrate. The terms "functional diseases" or "functional disorders of the nervous system" are used to refer to diseases and syndromes that do not have an anatomical substrate. It should be noted that over time, ideas about the nature of organic brain disorders have changed significantly.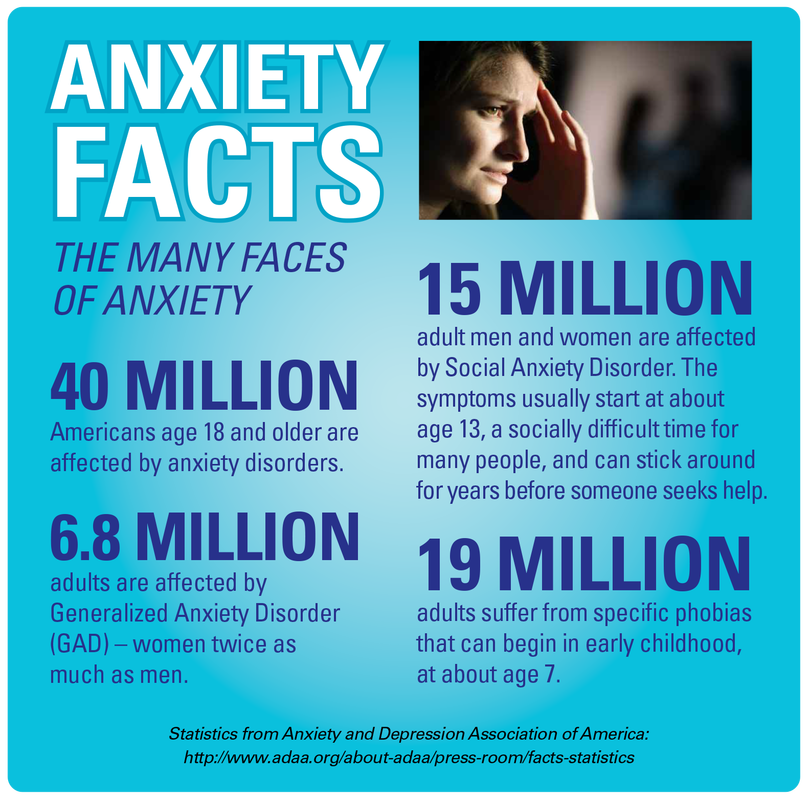 These now include not only gross anatomical pathology, but also biochemical disorders (impaired metabolism of biologically active substances, etc.), which can change the interaction of the functional systems of the brain. However, in clinical medicine, organic and functional diseases and syndromes are distinguished. At the same time, the latter include those disorders in which organic disorders are minimal and cannot be determined without the use of special research methods. In the practice of a neurologist, these include, among others, anxiety disorders, depression, and insomnia.
These now include not only gross anatomical pathology, but also biochemical disorders (impaired metabolism of biologically active substances, etc.), which can change the interaction of the functional systems of the brain. However, in clinical medicine, organic and functional diseases and syndromes are distinguished. At the same time, the latter include those disorders in which organic disorders are minimal and cannot be determined without the use of special research methods. In the practice of a neurologist, these include, among others, anxiety disorders, depression, and insomnia.
This review is devoted to the consideration of these disorders in terms of the prevalence of these forms of pathology, the frequency and combination of features of their pathogenesis.
Insomnia
Insomnia is defined as a clinical syndrome characterized, on the one hand, by the presence of sleep disorders in the form of disturbances in its onset (difficulty falling asleep), consolidation (frequent nocturnal awakenings and long periods of wakefulness) or quality (dissatisfaction with the depth of sleep, lack of refreshing effect of night sleep), provided that these disorders occur when there is sufficient time for sleep and have consequences in the form of disturbances in daytime activities of various kinds.
Existing studies [1-7] show a high prevalence of sleep disorders among the population of different countries. Thus, according to a population study [1], conducted in the United States with the involvement of 3,000 respondents among the adult population, sleep disorders were detected in 35% of the respondents. Among the European population, the prevalence of insomnia is characterized by indicators ranging from 10 to 30% [2]. Canadian researchers [3], who analyzed data on 2000 healthy people over the age of 18, identified at least one symptom of insomnia in 40% of them. In Pakistan, during a survey of 1488 adult urban residents, sleep disorders were noted in 31.3% [4], in India - in 18.6%. In Japan, the frequency of sleep disorders was 20.3% [5].
In Russian neurology, epidemiologically, the work of A.V. Wayne [6], conducted in 1989 in Moscow, which summarized the data obtained on a sample of 5,500 respondents over 14 years of age: more than 45% had dissatisfaction with sleep. One of the latest works in this direction is the study of sleep disorders in residents of Chuvashia [7], in which sleep disorders were studied in 2004 residents of this region of our country. Often or constantly complaining about sleep disorders turned out to be 20%.
One of the latest works in this direction is the study of sleep disorders in residents of Chuvashia [7], in which sleep disorders were studied in 2004 residents of this region of our country. Often or constantly complaining about sleep disorders turned out to be 20%.
The causes of insomnia can be a number of factors (acute and chronic stress, anxiety, comorbidities, pain, etc.), leading to a hyperactivation reaction with the mobilization of the body's adaptive resources at different levels - cerebral, sympathetic, endocrine. One of the constant manifestations of such activation is the quantitative and qualitative changes in the sleep process. With short-term exposure to stress, episodic insomnia develops (lasting up to one week), while persistence of stress is the leading factor in the chronification of insomnia. The persistence of stress with the subsequent development of a number of diseases can be facilitated by: high intensity or duration of the stress reaction, culminating in the depletion of adaptive reserves; personal or biological characteristics that determine the weakness of anti-stress protection.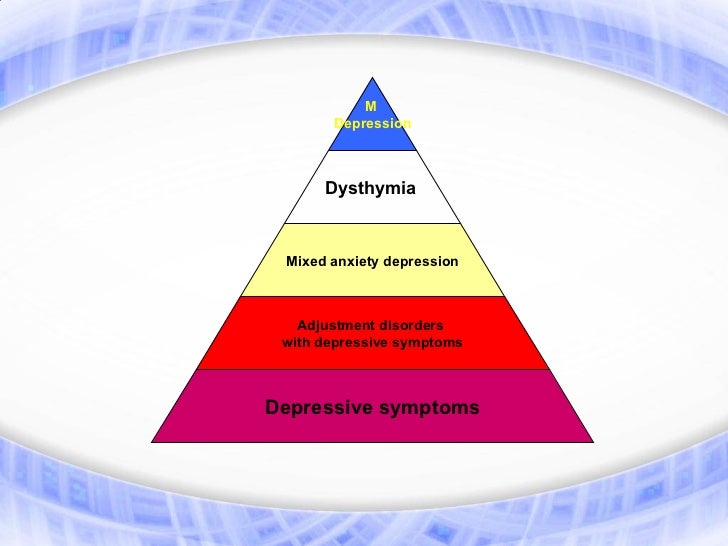
Insomnia disorders can consist both in a violation of falling asleep (presomnic nature of disorders), maintaining sleep (intrasomnic), and in difficulties with awakening, dissatisfaction with the quality of sleep, daytime manifestations (postsomnic).
Sleep disorders can be recorded by various methods, the most common of which is polysomnography. Polysomnographic curves for these disorders register an increase in sleep latency, the duration of nocturnal wakefulness, the index of awakenings and micro-awakenings, a reduction in the density of delta sleep with a compensatory increase in the representation of superficial sleep phases.
The presence of cerebral hyperactivation in insomnia was confirmed [8] by the data of functional magnetic resonance imaging (fMRI): in violation of sleep, the absence of a decrease in the level of metabolism in brain areas associated with emotional response was revealed, primarily the mesiotemporal cortex and the anterior cingulate gyrus. The presence of sympathetic activation in insomnia was confirmed [9] by the results of a study of heart rate variability, which showed an increase in the ratio between the low-frequency (sympathetic) and high-frequency (parasympathetic) components of the spectral power of heart rate variability towards increase. In patients with insomnia, this ratio turned out to be higher than in healthy people both in the state of wakefulness and at various stages of non-REM and REM sleep.
The presence of sympathetic activation in insomnia was confirmed [9] by the results of a study of heart rate variability, which showed an increase in the ratio between the low-frequency (sympathetic) and high-frequency (parasympathetic) components of the spectral power of heart rate variability towards increase. In patients with insomnia, this ratio turned out to be higher than in healthy people both in the state of wakefulness and at various stages of non-REM and REM sleep.
Particular attention is paid to the activation of the endocrine system in insomnia. It is expressed primarily in an increase in cortisol production during the day. When comparing the levels of cortisol and adrenocorticotropic hormone (ACTC) in blood plasma, it was shown that the maximum differences in these indicators in patients with insomnia and well-sleeping people are observed in the evening and at night. The presence of hyperactivation interferes with falling asleep and maintaining sleep at this level of regulation [10]. In addition, the release of "stress hormones" during insomnia is also extremely important due to the fact that there are reciprocal relationships between norepinephrine in the periphery and norepinephrine in the brain: an increase in the level of the peripheral hormone counteracts an increase in the level of norepinephrine in the brain tissues, and its deficiency in the central nervous system leads to an increase in the basal level of corticosteroids [11]. The latter (especially glucocorticoids) activate the tryptophan pyrrolase enzyme located in the liver, which converts tryptophan to the kynurenine metabolic pathway, which can lead to a decrease in serotonin synthesis. There are separate reports indicating that corticosteroids induce tyrosine transaminase, as a result of which the content of tyrosine in the blood decreases and the synthesis of norepinephrine in the brain decreases [12]. Thus, a decrease in the level of norepinephrine triggers a whole cascade of biochemical reactions.
In addition, the release of "stress hormones" during insomnia is also extremely important due to the fact that there are reciprocal relationships between norepinephrine in the periphery and norepinephrine in the brain: an increase in the level of the peripheral hormone counteracts an increase in the level of norepinephrine in the brain tissues, and its deficiency in the central nervous system leads to an increase in the basal level of corticosteroids [11]. The latter (especially glucocorticoids) activate the tryptophan pyrrolase enzyme located in the liver, which converts tryptophan to the kynurenine metabolic pathway, which can lead to a decrease in serotonin synthesis. There are separate reports indicating that corticosteroids induce tyrosine transaminase, as a result of which the content of tyrosine in the blood decreases and the synthesis of norepinephrine in the brain decreases [12]. Thus, a decrease in the level of norepinephrine triggers a whole cascade of biochemical reactions.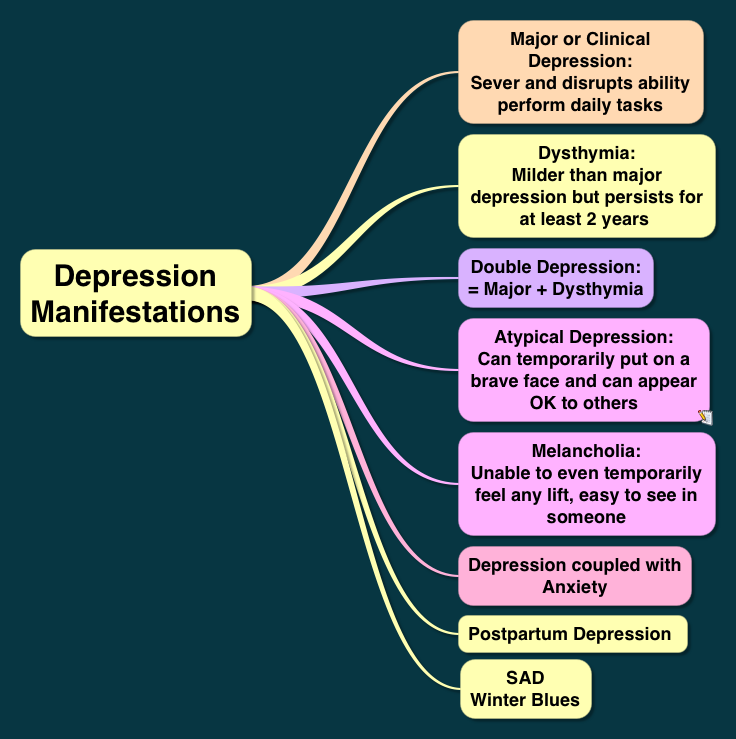
Obviously, there are other ways in which glucocorticoids and ACTH can affect the metabolism and activity of monoamines, since cortisol induces or inhibits a number of enzyme systems. But the above facts show that a positive feedback relationship (a kind of vicious circle) can be established between the increased secretion of cortisol and a deficiency of serotonin and norepinephrine in the brain: a deficiency of these monoamines leads to hypercorticism and disruption of the circadian rhythm of secretion, and an excess of cortisol disrupts synthesis, as a result what their deficiency is formed, which subsequently can become one of the mechanisms for the development of endogenous depression, according to one of the main theories of its formation - monoamine.
It can be seen from the above that the generality and universality of biological changes at the brain level play an important role in maintaining the sleep-wake cycle, and any quantitative (mainly deficient) and qualitative (metabolic disorders) changes can form complex pathological conditions that need to be carried out. differential diagnosis and choice of treatment tactics.
differential diagnosis and choice of treatment tactics.
Given the impact of insomnia on the body, it becomes clear the connection between insomnia disorders and a number of mental illnesses. So, in generalized anxiety disorder, their frequency reaches 56-75%, in bipolar affective disorder during a depressive episode - 80% [13].
Alarm
Anxiety initially reflects the normal reaction of the body, in particular the psyche, to changing environmental conditions and the effects of stress. But with their prolonged exposure or inadequate adaptive behavior, it loses its sanogenic property, turning into an anxiety disorder, often combined with depression and insomnia.
During the formation and consolidation of such a pathological reaction, anxiety is characterized by constant anxiety, often associated with a sense of impending danger, internal tension, and the expectation of unforeseen events. In general, we are talking about hypertrophied and maladaptive reactions to stress.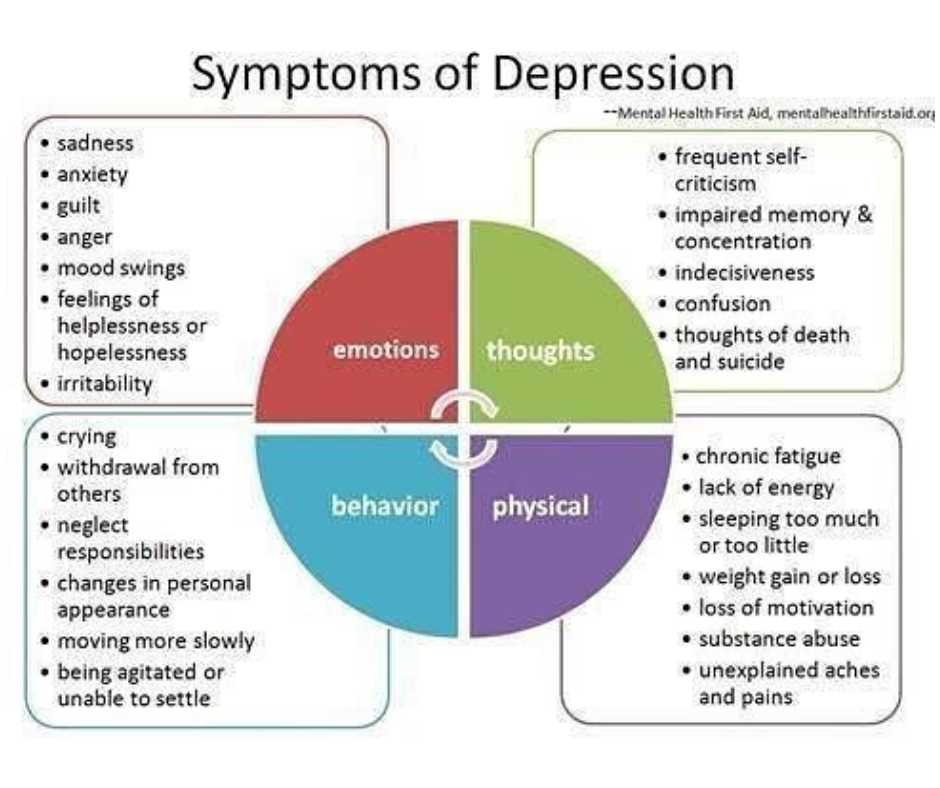
According to one of the American studies [13], the annual prevalence of anxiety disorders in the general population is 18.1%, and during the lifetime - 28.2%, which is significantly higher than the prevalence of any other mental disorder [14] . In a study conducted in Morocco [15], the prevalence of this disease during the year was higher than the above figures - 25.5%.
The frequency of the considered pathology depends on a number of cultural factors. Thus, post-traumatic stress disorder occurs in 1-2% of the population of Western Europe and in 6-9% of the inhabitants of North America and in more than 10% of the inhabitants of countries involved in religious conflicts [16].
In an international study conducted under the auspices of WHO [17], the incidence of anxiety disorders in the world at the level of primary care was determined to be 8%, while in Italy this figure was 3.8%, and in Greece - 14.8% .
In addition to the above, it can be added that in institutions of the general medical network the frequency of anxiety disorders reaches 23-78%, in outpatient services - an average of 45. 9% [eighteen].
9% [eighteen].
It is noted that the frequency of anxiety disorders depends on the presence of chronic somatic diseases, especially cardiovascular diseases. Fear of having a heart disease and associated death (cardiophobia) is diagnosed in 80% of patients in general medical practice who seek pain in the heart area [19]. In patients with coronary heart disease (CHD), anxious hypochondriacal reactions are detected in 28.2%, somatized reactions in 3%, anxiety-phobic reactions in 2.9%%; anxiety disorders are recorded in 98.6% of patients with arterial hypertension and in 89.6% of patients with chronic heart failure [20]. According to the American Psychiatric Association, the incidence of early generalized anxiety disorder (GAD) in patients with acute cerebrovascular accident reaches 27%, late (after 3 months) - 23% [21].
There are three main approaches to explaining the causes of anxiety disorders; psychological, neurobiological and genetic.
The psychoanalytic approach is based on the well-known works of S. Freud on the nature of neurotic anxiety, which they opposed to realistic anxiety. Under realistic anxiety, they consider [22] a rational and understandable reaction to danger, which performs an adaptive function. From the point of view of cognitive-behavioral therapy, pathological anxiety arises as a result of maladaptive and dysfunctional cognitions, which are either inherent in the individual from birth or arise in the process of his development. If an individual has dysfunctional beliefs, any event or stimulus can be seen as threatening life or personal freedom, which triggers an anxiety reaction. However, such anxiety does not contribute to adaptation and subsequently leads to an even stronger fixation of dysfunctional disorders.
Freud on the nature of neurotic anxiety, which they opposed to realistic anxiety. Under realistic anxiety, they consider [22] a rational and understandable reaction to danger, which performs an adaptive function. From the point of view of cognitive-behavioral therapy, pathological anxiety arises as a result of maladaptive and dysfunctional cognitions, which are either inherent in the individual from birth or arise in the process of his development. If an individual has dysfunctional beliefs, any event or stimulus can be seen as threatening life or personal freedom, which triggers an anxiety reaction. However, such anxiety does not contribute to adaptation and subsequently leads to an even stronger fixation of dysfunctional disorders.
Genetic predisposition plays a role in the occurrence and persistence of an anxiety disorder. There is evidence of a gene responsible for the risk of developing anxiety disorders. This was revealed in an Icelandic study [23] by genotyping 353 people. Information has been obtained on the association of anxiety disorder with the gene 9q31 [23]. A high level of concordance in the development of GAD in monozygotic twins was also revealed [24] - 37.9% (in contrast to the risk of developing panic disorders - 22.6%).
Information has been obtained on the association of anxiety disorder with the gene 9q31 [23]. A high level of concordance in the development of GAD in monozygotic twins was also revealed [24] - 37.9% (in contrast to the risk of developing panic disorders - 22.6%).
There are ideas that the hippocampus and amygdala play an important role in the neurobiological substrate of anxiety disorders. According to neuroimaging research methods, individuals with anxiety disorders have increased activation of the amygdala in response to threatening stimuli compared to controls [25]. If we talk about the hippocampus, then, as animal studies show, it is involved in the formation of the fear response and avoidance of danger. In the case of prolonged exposure of an animal to threatening stimuli, a decrease in the volume of the hippocampus and a change in behavior towards avoiding any new stimuli occur [26].
It is also known that anxiety realizes its function of quick response to changing environmental conditions through the activation of the hypothalamic-pituitary-adrenal system, which has an indirect effect on sleep [27]. For example, in rats under conditions of acute stress, REM sleep primarily reacts, changes in which are associated with changes in the secretion of corticotropin-releasing hormone (CRH), or corticoliberin [28]. In different models of stress in rats, an increase in the phase of REM sleep and a reduction in slow-wave sleep were noted [29]. The subjects also showed an increase in the representation of the REM phase when exposed to a stress factor [30]. At the same time, with an increase in the activity of the sympathetic nervous system and, in fact, a decrease in the number of non-REM sleep phases to 2 (NREM1, NREM2), there is an increase in periods of superficial sleep with frequent awakenings and "micro-awakenings". This is reflected in the polysomnographic picture of sleep (see figure): a characteristic “palisade of anxiety” appears on the hypnogram (frequent awakenings - falling asleep, not deeper than the 2nd stage of sleep.
For example, in rats under conditions of acute stress, REM sleep primarily reacts, changes in which are associated with changes in the secretion of corticotropin-releasing hormone (CRH), or corticoliberin [28]. In different models of stress in rats, an increase in the phase of REM sleep and a reduction in slow-wave sleep were noted [29]. The subjects also showed an increase in the representation of the REM phase when exposed to a stress factor [30]. At the same time, with an increase in the activity of the sympathetic nervous system and, in fact, a decrease in the number of non-REM sleep phases to 2 (NREM1, NREM2), there is an increase in periods of superficial sleep with frequent awakenings and "micro-awakenings". This is reflected in the polysomnographic picture of sleep (see figure): a characteristic “palisade of anxiety” appears on the hypnogram (frequent awakenings - falling asleep, not deeper than the 2nd stage of sleep.
Characteristic graphic "palisade of anxiety", detected during polysomnography in a patient with anxiety-depressive syndrome.
The presence of sleep disorders is a "core" symptom of generalized anxiety disorder - about 60-70% of patients with this diagnosis have sleep disorders [31].
Depression
In general medical practice, depression ranks second after arterial hypertension, occurring in approximately one in 10 outpatients, and the overall prevalence rate is about 50% [32]. In a large international study [33], conducted at the end of the last century, depression was detected on average in 69% (45-95%) of patients seeking medical help for somatic disorders. There is also evidence that depression is the only cause of 10-20% of visits to general practitioners [34], and their prevalence among patients with severe somatic diseases reaches 20-60% [35].
Of all the diagnostically significant manifestations of depression, two symptoms of the current depressive episode are of a somatic nature: fatigue/weakness/apathy, observed in 73% of patients, insomnia/drowsiness - in 63% [36].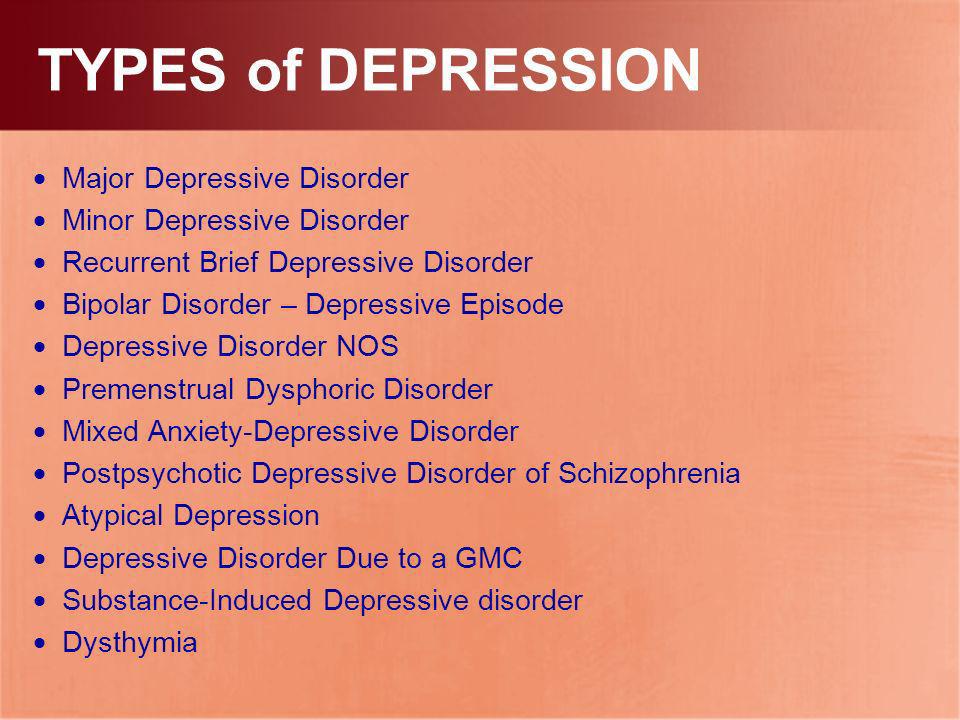
As for insomnia, in some cases it is so pronounced that patients perceive depression as a sleep disorder [37].
Polysomnographic abnormalities are detected in 40-60% of outpatients and 90% of hospitalized patients with a depressive episode, among which are sleep continuity disorders (increased sleep latency, total wake time during sleep, frequency of early morning awakenings, reduced total sleep duration). The absolute and relative (from the total sleep time) deficit of slow-wave sleep is characteristic. Quantitative and qualitative changes in REM sleep include a reduction in REM latency, an increase in the duration of the first period of REM sleep, an increase in REM activity (total number of eye movements during the night), an increase in REM density (ratio - REM activity / total REM time -sleep) and an increase in the proportion of REM sleep from total sleep time [38]. Sleep in patients with depression in remission may also remain disturbed: the duration of delta sleep is reduced, and the time to the onset of REM sleep is reduced (the latter is associated with an increased risk of relapse of depression).
Polysomnographic studies conducted in individuals at high risk of developing depression have shown that the shortened time of the onset of the REM sleep phase and the lack of slow-wave sleep are familial and polysomnographic abnormalities may precede the clinical manifestation of depression [39]. It is believed that the role of genetic factors is about 30-40%. The remaining 60-70% are attributed to behavioral factors and determined by the interaction of the genome with the environment.
Among the neurobiological theories of depression, serotonergic and noradrenergic theories dominate, which are confirmed by the fact that any agent that inhibits the reuptake of serotonin and norepinephrine (which is the basis of the effect of a number of antidepressants) leads to a clinically significant improvement in the condition of patients with depression. The role of corticoliberin and stress hormones in the formation of depressive disorders is also noted. Currently, neurotrophic GABA-, glutamate-mediated, dopaminergic theories of depression are being considered [40].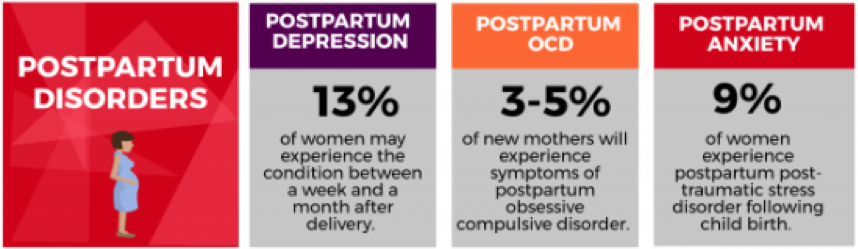
The circadian hypothesis is also widespread, according to which manifestations of abnormal circadian rhythms characteristic of depression, including diurnal fluctuations in symptoms, disturbances in sleep and other behavioral and physiological functions, are not only typical clinical manifestations of a depressive disorder, but also one of the key pathogenetic factors of depression. Since the leading role in the regulation of these rhythms belongs to melatonin, much attention is currently paid to it in the study of depression, including in the therapeutic aspect: it is believed that the correction of melatonin levels in patients with depression can be an important additional component of treatment. If we take into account the violation of the circadian rhythm, then it is also advisable to prescribe a drug such as melaxen (Unipharm).
Summarizing the above materials, we can state that such functional disorders as anxiety, depression and insomnia, often combined, are widespread in the practical work of a neurologist, and they are often comorbid somatic pathology. At the basis of their development, they have similar mechanisms, the main component of which is the hyperactivation of the sympathetic nervous system. This corresponds to general changes in the structure of sleep (an increase in the representation of the fast phase, a decrease in its latency, a reduction in slow-wave sleep), but at the same time, there are signs that characterize each of the conditions studied: "alpha-delta rhythm" in depression, which necessitates a differentiated approach to the diagnosis of these conditions and their therapy with the development of uniform standards for diagnosis and treatment.
At the basis of their development, they have similar mechanisms, the main component of which is the hyperactivation of the sympathetic nervous system. This corresponds to general changes in the structure of sleep (an increase in the representation of the fast phase, a decrease in its latency, a reduction in slow-wave sleep), but at the same time, there are signs that characterize each of the conditions studied: "alpha-delta rhythm" in depression, which necessitates a differentiated approach to the diagnosis of these conditions and their therapy with the development of uniform standards for diagnosis and treatment.
Anxiety-depressive disorder diagnosis: causes, treatment, prevention
Anxiety-depressive disorders belong to the category of neuroses, they require modern pharmacotherapy and necessarily psychotherapy. Psychologists and psychiatrists are sounding the alarm - modern society is completely unable to cope with stressful situations, which explains the high percentage of patients suffering from such diseases. It is possible to prevent anxiety and depressive disorders at first with the help of relaxation techniques, timely rest.
It is possible to prevent anxiety and depressive disorders at first with the help of relaxation techniques, timely rest.
Submit an application for diagnosis and treatment
I confirm that I accept the terms of consent to the processing of personal data.
The very name anxiety-depressive disorder implies that the patient's diagnosis has two components at once - depression and anxiety. This is a disease that accompanies the life of modern people and significantly reduces their quality of life. World Health Organization experts warn: if we do not begin to resist stressful situations, do not learn to relax and do not realize the seriousness and usefulness of mental hygiene, after 5 years, anxiety-depressive disorder will take the leading position after cardiovascular diseases in the number of years lost due to disability .
Symptoms of an anxiety-depressive disorder
Anxiety-depressive disorder (ADD) is a disease from the group of neuroses, which is characterized by a feeling of incessant anxiety. Moreover, anxiety appears in a person not as a response to a real threat, but as a kind of sense of danger that occurs against the background of a depressive component and low mood. All symptoms of anxiety-depressive disorder can be divided into two clusters - physiological manifestations and psychological manifestations. Physiological symptoms:
Moreover, anxiety appears in a person not as a response to a real threat, but as a kind of sense of danger that occurs against the background of a depressive component and low mood. All symptoms of anxiety-depressive disorder can be divided into two clusters - physiological manifestations and psychological manifestations. Physiological symptoms:
In general, the symptoms are similar to those of stress, but for a doctor to diagnose an anxiety-depressive disorder, symptoms must be observed at least for several weeks.
Causes of anxiety-depressive disorder
The prevalence of the disorder is equally marked both among patients with a low standard of living and among patients with high social conditions. Women get TDD more often than men because of their emotionality. In addition, the disease can develop in women against the background of hormonal changes during pregnancy or after childbirth, with a change in the menstrual cycle. Among the most common causes of anxiety-depressive disorder are the following:
Among the most common causes of anxiety-depressive disorder are the following:
- Change in socio-economic status (loss of job, decrease in income)
- Severe emotional upheavals (divorce, illness, death)
- Alcohol and drug abuse (anxiety-depressive disorder may develop due to the use of psychoactive substances)
- Genetic causes (if a close relative has had ADD, the likelihood of developing the disease increases dramatically)
- Age (in older people, ADD is very often diagnosed as a response to the growing up of children and grandchildren, the death of acquaintances and loneliness)
Treatment of anxiety-depressive disorder
If the diagnosis of anxiety-depressive disorder is confirmed, the doctor determines the treatment strategy depending on the severity of the case and the course of the disease. Several treatment options are possible.
- Drug treatment. Antidepressants of the modern generation are prescribed, sedatives can be additionally recommended.
 They contribute to the normalization of the emotional sphere, smooth out emotional lability, and reduce anxiety. As a result, metabolic and endocrine processes in the body are normalized. The first results of treatment can be seen a week after the start of treatment, the therapeutic effect is achieved after 3-4 weeks.
They contribute to the normalization of the emotional sphere, smooth out emotional lability, and reduce anxiety. As a result, metabolic and endocrine processes in the body are normalized. The first results of treatment can be seen a week after the start of treatment, the therapeutic effect is achieved after 3-4 weeks. - Psychotherapeutic treatment. After the examination, the doctor prescribes a course of psychotherapy, which is selected individually. It can be cognitive behavioral therapy, supportive therapy, family therapy, holistic psychotherapy, hypnotherapy. In the process of psychotherapy, the patient gets rid of the manifestations of anxiety-depressive disorder, learns to cope with emerging stressful situations and respond to them correctly. Thus, in the process of psychotherapy, not only the treatment of an anxiety-depressive disorder that has already arisen occurs, but also the prevention of the development of a psychological disease in the future.
Treatment of anxiety-depressive disorder in Israel
Complex treatment of anxiety-depressive disorder is practiced in Israel. Complexity means the combination of drug treatment, psychotherapy with additional methods of psychotherapy. Additional techniques are designed to solve various problems. For example, hippotherapy reduces anxiety, relieves psychosomatic manifestations of the disease and fears. Art therapy is designed to unleash the potential of creative people, lead to mood stabilization. Music therapy is used to relieve stress, normalize the emotional state. Sports therapy according to the method of Moshe Feldenkrais is used to improve blood circulation, "connect" the mind and body during exercise. Bibliotherapy is needed for the patient to understand the mechanisms of the development of the disease, the causes and methods of treatment. Hydrotherapy and yoga therapy are used for relaxation. All of the above methods have been used by IsraClinic for a long time and successfully. In Israel, only the most advanced and effective methods of treatment are used, which have proven themselves well. Examples are dozens of successfully cured patients.
Complexity means the combination of drug treatment, psychotherapy with additional methods of psychotherapy. Additional techniques are designed to solve various problems. For example, hippotherapy reduces anxiety, relieves psychosomatic manifestations of the disease and fears. Art therapy is designed to unleash the potential of creative people, lead to mood stabilization. Music therapy is used to relieve stress, normalize the emotional state. Sports therapy according to the method of Moshe Feldenkrais is used to improve blood circulation, "connect" the mind and body during exercise. Bibliotherapy is needed for the patient to understand the mechanisms of the development of the disease, the causes and methods of treatment. Hydrotherapy and yoga therapy are used for relaxation. All of the above methods have been used by IsraClinic for a long time and successfully. In Israel, only the most advanced and effective methods of treatment are used, which have proven themselves well. Examples are dozens of successfully cured patients.