Dependent personality disorder mother
How Dependent Personality Disorder Affects a Family – BrightQuest Treatment Centers
Dependent personality disorder (DPD) creates feelings of helplessness in those who have it, and their dependent behavior can have a negative impact on their loved ones as well. Without trained intervention families afflicted by DPD may disintegrate over time, but when treatment is provided it can lead to dramatic and positive changes in family dynamics—and this is especially true when family members participate directly in the recovery program.
When a person has dependent personality disorder (DPD), they rely on others to care for them and watch out for their interests. Even as they advance in adulthood they will retain their dependent characteristics, which shape their choices and act as a distorting influence in their interactions with friends, family members, and co-workers.
Adopting a veneer of normalcy, they may get married, have children, and assume many of the life responsibilities such commitments entail. But their feelings of helplessness and lack of self-confidence inevitably erect barriers that prevent them from enjoying a healthy family life.
Through their dependent actions and behavior, they subtly and subconsciously shape family dynamics to trap everyone in their orbit, which makes them feel more secure and protected.
On the surface at least, dependent personality disorder breeds passivity, resignation, and surrender. But people who have this disorder are often so frightened and desperate for attention that they wield their helplessness like a weapon, manipulating partners, parents, children, and siblings into taking care of them indefinitely.
This type of manipulation is motivated by fear of failure and abandonment and not by malicious intent. Nevertheless, it is still unhealthy for everyone involved.
Dependent Personality Disorder Characteristics
It is believed that DPD develops as a learned response to patterns of childhood conditioning and reinforcement.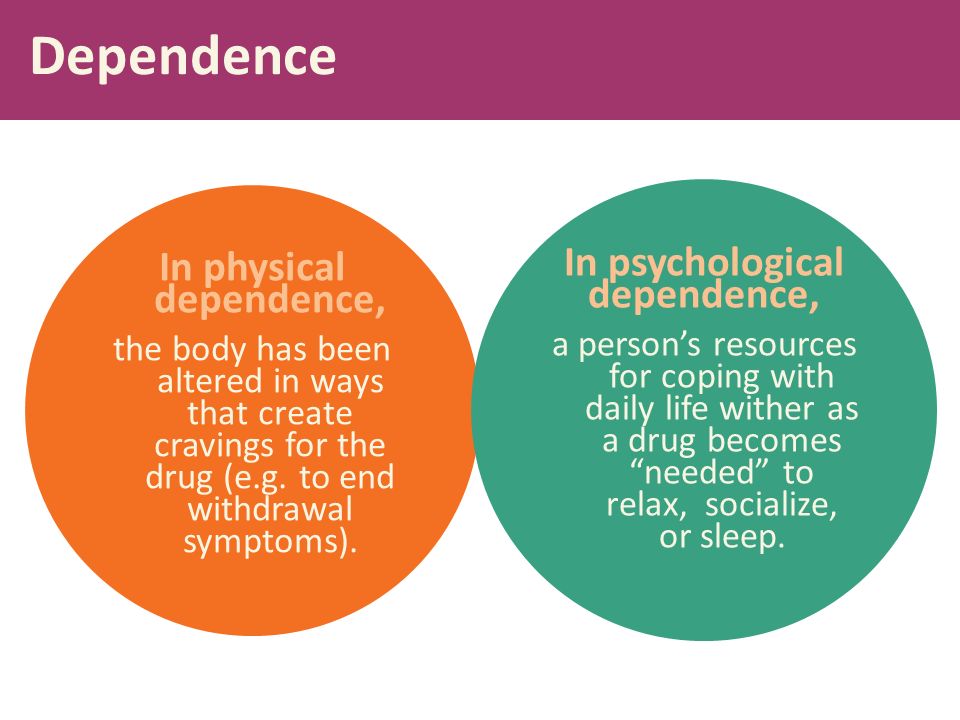 When needy or demanding behavior is rewarded by parents, and independent action is discouraged, it can set the stage for a lifelong habit of dependency.
When needy or demanding behavior is rewarded by parents, and independent action is discouraged, it can set the stage for a lifelong habit of dependency.
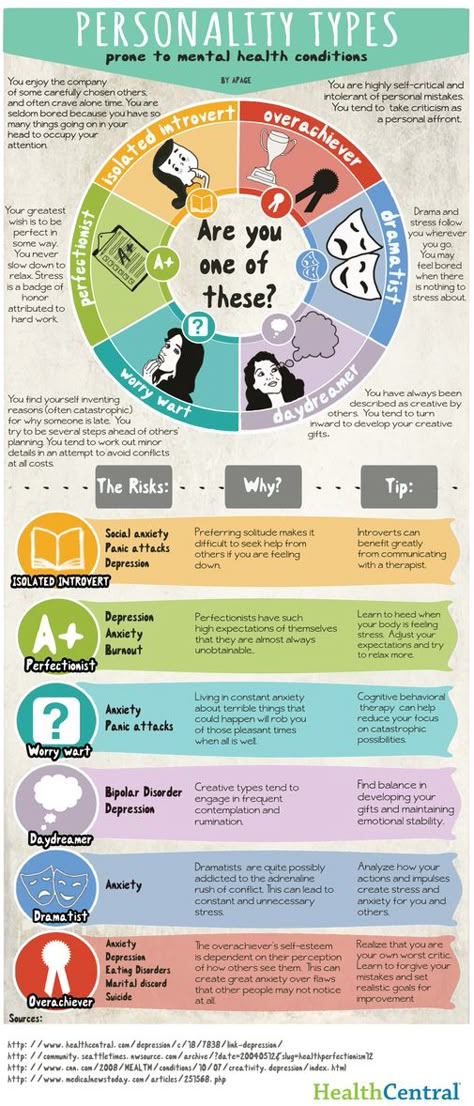
First manifesting in adolescence or early adulthood, dependent personality disorder will betray its presence through a range of emotional, psychological, and behavioral symptoms. They may include:
- Indecisiveness, an inability to make decisions or follow them through
- Reluctance to take responsibility for personal, occupational, financial, or household affairs
- A fear of being left alone, even temporarily
- Lack of self-confidence and poor self-esteem
- Self-centeredness, revealed by a tendency to constantly talk about one’s problems and concerns, with little or no acknowledgement of the needs of others
- Going to great lengths to achieve validation, attention, or support
- Passivity in the face of conflict, used as a strategy to disarm the anger or disapproval of others
- Clinginess, neediness, and other behaviors that reveal extreme dependence on certain individuals
Needless to say, dealing with such symptoms on a daily basis can be exhausting for family members, who must pick up the slack for loved ones who lack the capacity to give as much as they take. Because of their neediness, a person with DPD absorbs the time and energy of everyone around them, often making it difficult for loved ones to take care of their own needs.
Because of their neediness, a person with DPD absorbs the time and energy of everyone around them, often making it difficult for loved ones to take care of their own needs.
Dependent Personality Disorder and Relationships
When someone has dependent personality disorder, their relationships with spouses or partners can quickly become strained by the unequal status of the two parties involved. Most people enter into such relationships expecting authority and responsibility to be shared, and when undue burden is placed on one person it can leave them feeling exploited or overwhelmed, which may cause them to frequently lash out in anger or frustration.
Dependent personality disorder can also interfere with the parent-child relationship. Kids of all ages look to their moms and dads for guidance and support, but when a parent has DPD it can cause the lines of authority and responsibility to become blurred. Instead of children relying on parents, the parents may begin to lean on their children, and that reversal of roles can hinder the natural development of young people unprepared to handle such duties. In this case the caregiver becomes the cared for, and this can devolve into a subtle form of parental neglect.
In this case the caregiver becomes the cared for, and this can devolve into a subtle form of parental neglect.
Some adults with DPD fail to create their own separate families, in part because their needy and dependent behavior alienates potential partners. In these instances, they may remain reliant on their parents or siblings to help them make decisions and manage their lives: parents of adults with DPD are often called on to continue supporting their children emotionally, financially, and logistically, leading to feelings of resentment and disappointment that the adult child with DPD will inevitably feel and react to. This will only deepen their feelings of shame and embarrassment, and make it that much harder for them to find or build the self-confidence necessary to someday assert their independence.
Call For a Confidential Phone Assessment.
619-466-0547Getting Help for Dependent Personality Disorder
Dependent behavior takes a toll on everyone it affects, and when one person in the family has untreated DPD it can cause stress and misery for all.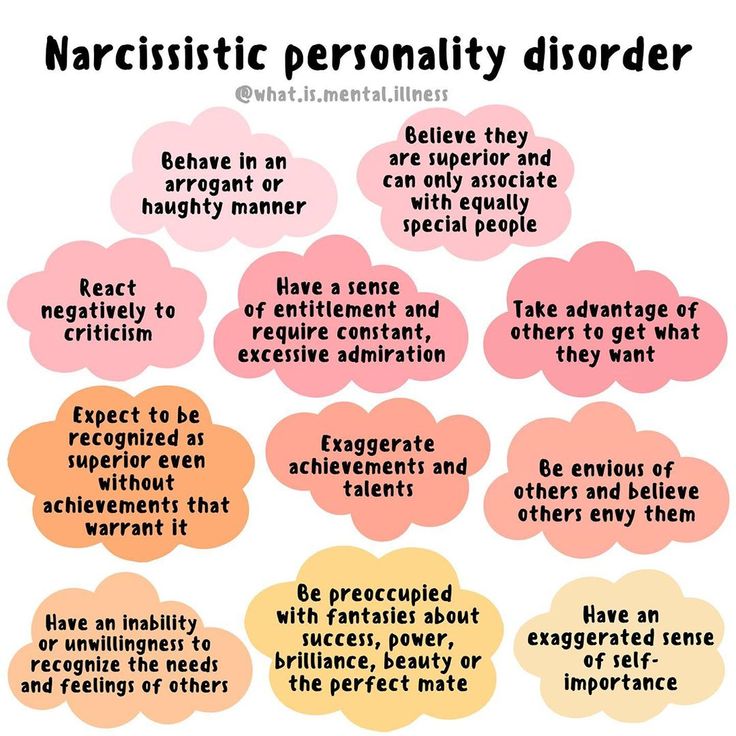
When dependent behavior is observed, the first step is to seek out the services of a mental health professional, who can diagnose DPD and recommend a course of treatment that can ameliorate the symptoms of this unpleasant condition.
Treatment plans for dependent personality disorder will include individual and group therapy, possibly medication if an additional co-occurring mental health disorder has been diagnosed (this is common with DPD), holistic techniques that promote mindfulness and stress management, and life skills and coping skills classes that can show the person with DPD how to change the way they relate to others and the world around them.
But when DPD is present, its impact on the family should not be overlooked. Most residential mental health treatment centers offer family therapy programs as a part of their recovery regimens, and this type of therapy can be highly beneficial to families that have been put under long-term duress by the high-maintenance behavior of a dependent person.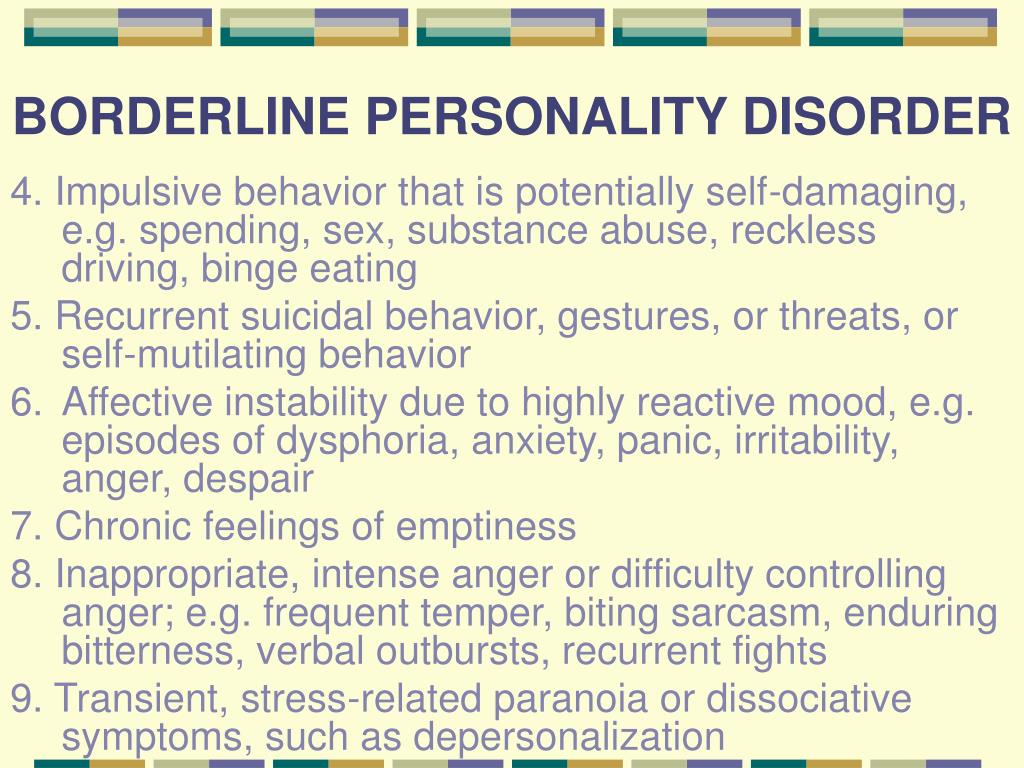 Ultimately, the person with DPD must learn to be more self-reliant, confident, and independent, and having the support of family members can give them the strength and motivation they need to pursue recovery with vigor and determination.
Ultimately, the person with DPD must learn to be more self-reliant, confident, and independent, and having the support of family members can give them the strength and motivation they need to pursue recovery with vigor and determination.
Men and women who’ve struggled with dependent personality disorder need liberation from the worst effects of this condition, but so do the ones they love, and that is most likely to happen when treatment and recovery become cooperative ventures.
Dependent Personality Disorder | Abnormal Psychology
Learning Objectives
- Describe the characteristics and diagnosis of dependent personality disorder
Dependent Personality Disorder
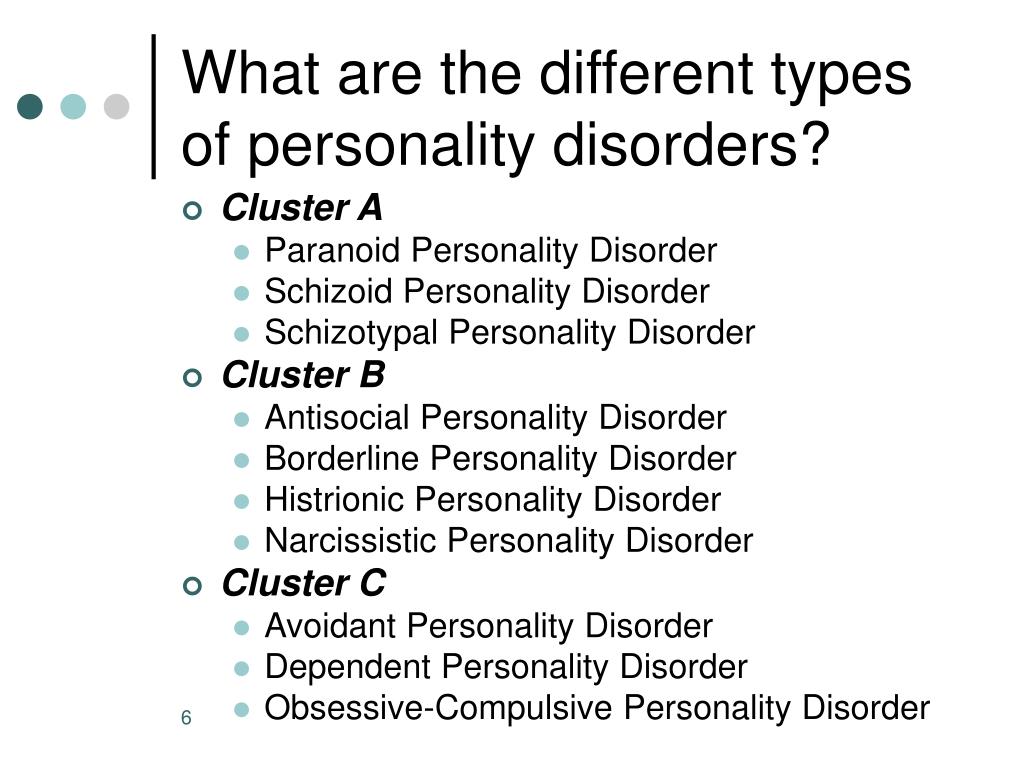
Dependent personality disorder (DPD) is a cluster C personality disorder characterized by a pervasive psychological dependence on other people.
| Avoidant | socially inhibited and oversensitive to negative evaluation; avoids occupations that involve interpersonal contact because of fears of criticism or rejection; avoids relationships with others unless guaranteed to be accepted unconditionally; feels inadequate and views self as socially inept and unappealing; unwilling to take risks or engage in new activities if they may prove embarrassing | C |
| Dependent | allows others to take over and run their life; is submissive, clingy, and fears separation; cannot make decisions without advice and reassurance from others; lacks self-confidence; cannot do things on their own; feels uncomfortable or helpless when alone | C |
| Obsessive-Compulsive | pervasive need for perfectionism that interferes with the ability to complete tasks; preoccupied with details, rules, order, and schedules; excessively devoted to work at the expense of leisure and friendships; rigid, inflexible, and stubborn; insists things be done a certain way; miserly with money | C |
Dependent personality disorder (DPD) is a long-term condition in which people depend on others to meet their emotional and physical needs, with only a minority achieving normal levels of independence. Dependent personality disorder (DPD) is characterized by excessive fear and anxiety. Dependent personality disorder (DPD) begins by early adulthood, is present in a variety of contexts, and is associated with inadequate functioning. Symptoms can include anything from extreme passivity, devastation, or helplessness when relationships end; avoidance of responsibilities; and severe submission.
Dependent personality disorder (DPD) is characterized by excessive fear and anxiety. Dependent personality disorder (DPD) begins by early adulthood, is present in a variety of contexts, and is associated with inadequate functioning. Symptoms can include anything from extreme passivity, devastation, or helplessness when relationships end; avoidance of responsibilities; and severe submission.
People who have dependent personality disorder are overdependent on other people when it comes to making decisions. They cannot make a decision on their own as they need constant approval from other people. Consequently, individuals diagnosed with DPD tend to place the needs and opinions of others above their own as they do not have the confidence to trust their decisions. This kind of behavior can explain why people with DPD tend to show passive and clingy behavior. These individuals display a fear of separation and cannot stand being alone. When alone, they experience feelings of isolation and loneliness due to their overwhelming dependence on other people.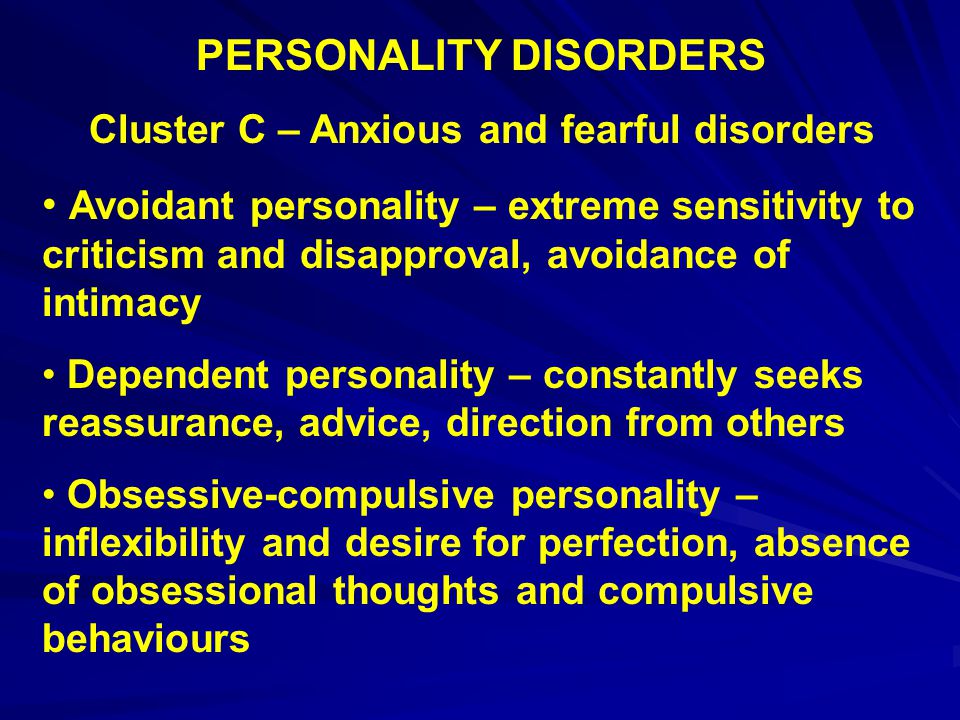
DSM-5 Criteria
DSM-5 refers to dependent personality disorder as a pervasive and excessive need to be taken care of, which leads to submissive and clinging behavior and fears of separation. This behavior begins by early adulthood and can be present in a variety of contexts.
According to the DSM-5, the disorder is indicated by at least five of the following factors:
- has difficulty making everyday decisions without an excessive amount of advice and reassurance from others.
- needs others to assume responsibility for most major areas of their life.
- has difficulty expressing disagreement with others because of fear of loss of support or approval.
- has difficulty initiating projects or doing things on their own (because of a lack of self-confidence in judgment or abilities rather than a lack of motivation or energy).
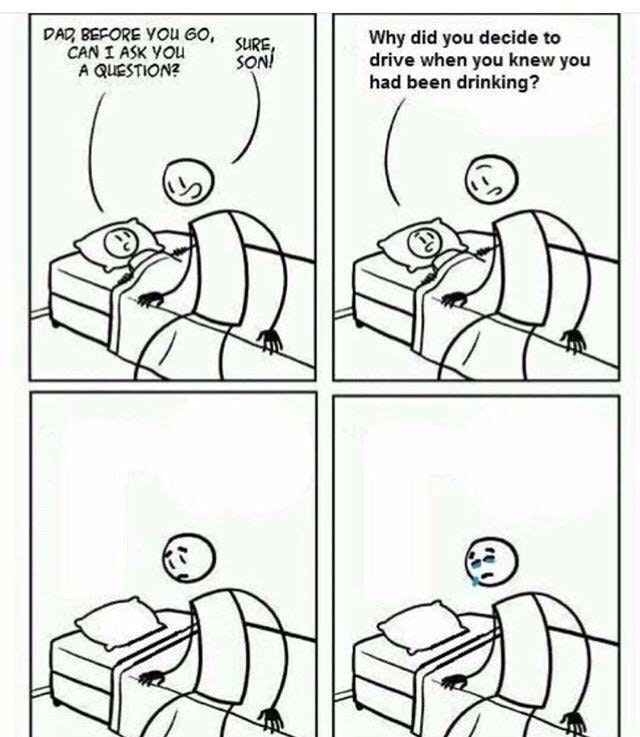
Figure 1. People with DPD can be clingy and may constantly need the approval of others.
- goes to excessive lengths to obtain nurturance and support from others, to the point of volunteering to do things that are unpleasant.
- feels uncomfortable or helpless when alone because of exaggerated fears of being unable to care for themselves.
- urgently seeks another relationship as a source of care and support when a close relationship ends.
- is unrealistically preoccupied with fears of being left to take care of themselves.
Differential Diagnosis
There are similarities between individuals with dependent personality disorder and individuals with borderline personality disorder in that they both have a fear of abandonment. Those with dependent personality disorder do not exhibit impulsive behavior, unstable affect, and poor self-image experienced by those with borderline personality disorder.
The following conditions are commonly comorbid with dependent personality disorder:
- mood disorders
- anxiety disorders
- adjustment disorder
- borderline personality disorder
- avoidant personality disorder
- histrionic personality disorder
Epidemiology
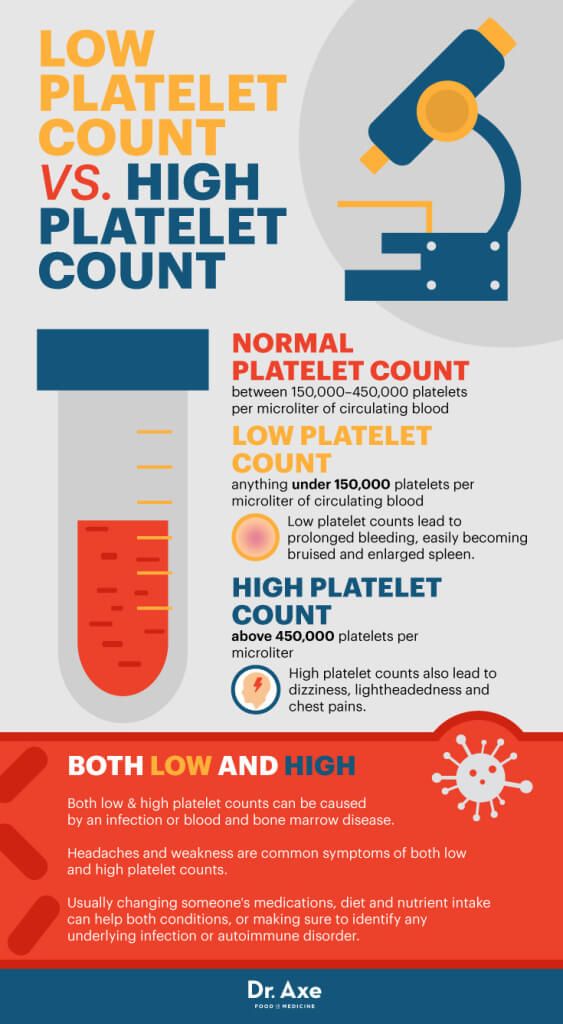
Based on a survey of 43,093 Americans, 0. 49% of adults meet diagnostic criteria for DPD (National Epidemiologic Survey on Alcohol and Related Conditions (NESARC; Grant et al., 2004). Traits related to DPD, like most personality disorders, emerge in childhood or early adulthood. DPD is more common among women compared to men as 0.6% of women have DPD compared to 0.4% of men. A 2004 twin study suggests a heritability of 0.81 for developing dependent personality disorder. Because of this, there is significant evidence that this disorder runs in families. Children and adolescents with a history of anxiety disorders and physical illnesses are more susceptible to acquiring this disorder.
49% of adults meet diagnostic criteria for DPD (National Epidemiologic Survey on Alcohol and Related Conditions (NESARC; Grant et al., 2004). Traits related to DPD, like most personality disorders, emerge in childhood or early adulthood. DPD is more common among women compared to men as 0.6% of women have DPD compared to 0.4% of men. A 2004 twin study suggests a heritability of 0.81 for developing dependent personality disorder. Because of this, there is significant evidence that this disorder runs in families. Children and adolescents with a history of anxiety disorders and physical illnesses are more susceptible to acquiring this disorder.
Etiology
Figure 2. Overprotective parenting behavior is a risk factor for DPD.
The exact cause of dependent personality disorder is unknown. A study in 2012 estimated that between 55% and 72% of the risk of the condition is inherited from one’s parents. The difference between a dependent personality and a dependent personality disorder is somewhat subjective, which makes diagnosis sensitive to cultural influences such as gender role expectations.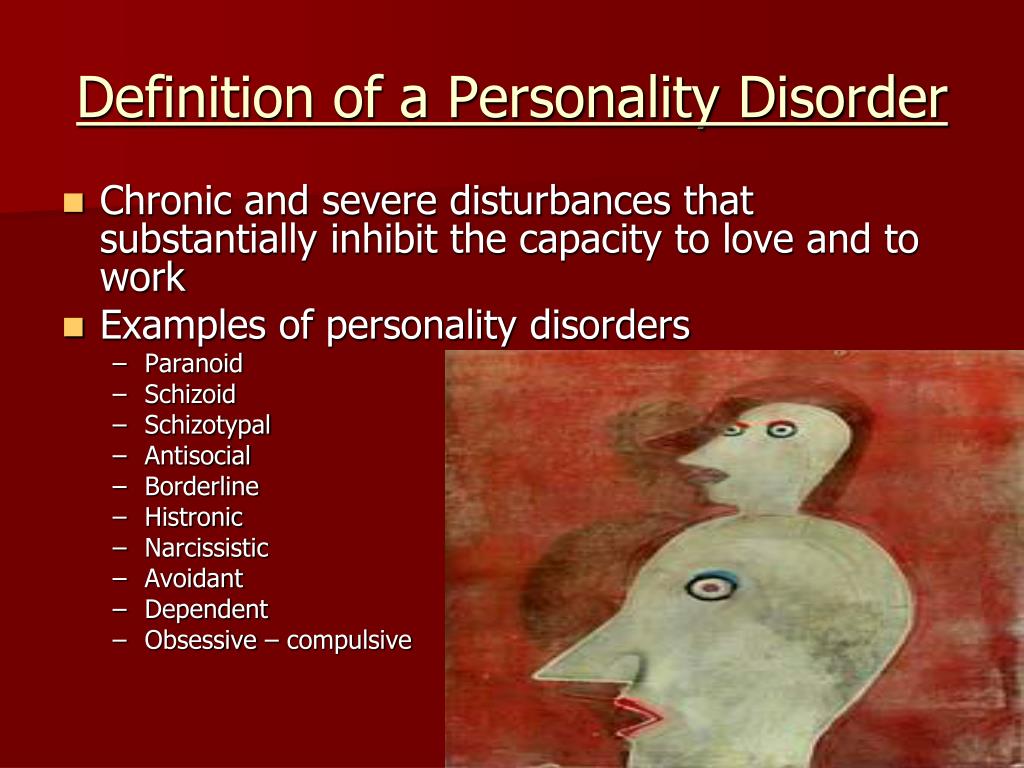 There is a higher frequency of the disorder seen in women than men.
There is a higher frequency of the disorder seen in women than men.
Dependent traits in children tended to increase with parenting behaviors and attitudes characterized by overprotectiveness and authoritarianism. Traumatic or adverse experiences early in an individual’s life, such as neglect and abuse or serious illness, can increase the likelihood of developing personality disorders, including dependent personality disorder, later on in life. This likelihood is especially prevalent for those individuals who also experience high interpersonal stress and poor social support.
Treatment
People who have DPD are generally treated with psychotherapy. The main goal of this therapy is to make the individual more independent and help them form healthy relationships with the people around them. This is done by improving their self-esteem and confidence.
Medication can be used to treat patients who suffer from depression or anxiety because of their DPD, but this does not treat the core problems caused by DPD.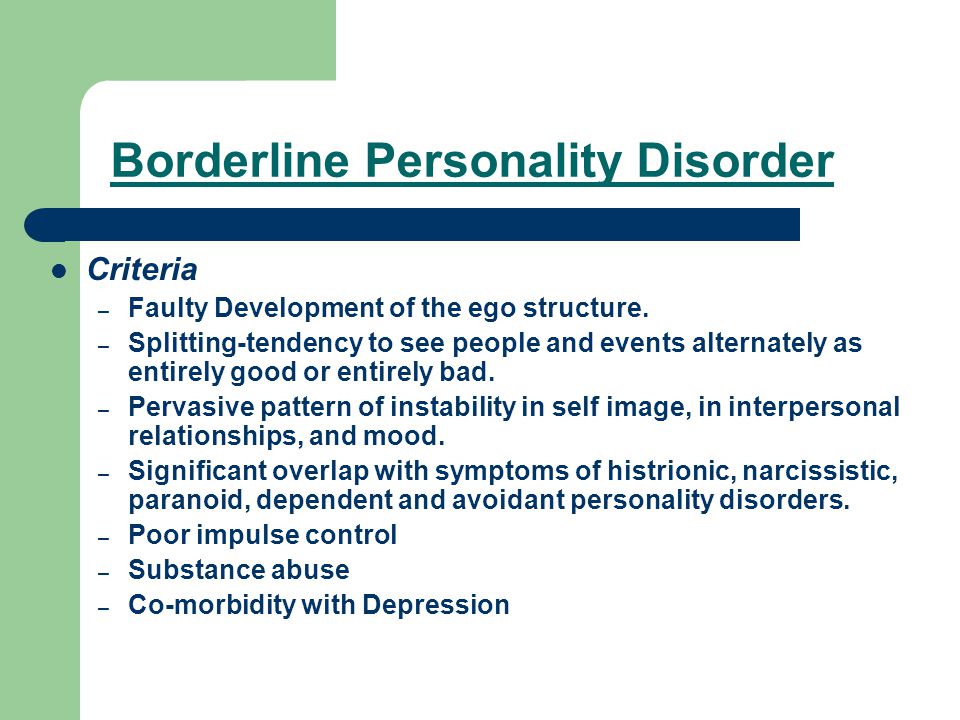
Key Takeaways: Dependent personality disorder
Case Study: DEPENDENT PERSONALITY DISORDER
This case study looks at the patient of a 27-year-old, white female named Sally. She works as an administrative assistant whose work required extensive data entry. Sally’s mother used her network to get this stable job for her daughter. Sally is consumed with pleasing her mother and even asks for her mother’s advice on what to wear to the office each day. Sally consistently worries about pleasing others and her colleagues at work, even at the expense to herself, which leads to the diagnosis of dependent personality disorder. The degree to which her self-destructive passivity and compliance at work stemmed from her early experiences within the family are unclear, but her parents’ overprotectiveness likely played some role in the etiology of her personality pathology.
Watch IT
This video describes the diagnostic criteria and treatment options for dependent personality disorder.
You can view the transcript for “What is Dependent Personality Disorder?” here (opens in new window).
Try It
Glossary
dependent personality disorder (DPD): a personality disorder characterized by a pervasive and excessive need to be taken care of, leading to a lack of independent action
Dependent Personality Disorder: 10 Signs - How to Recognize the Problem
How to Get Through Tough Times: Daily Psy Tips
7 Unrealistic Expectations for Healthy Relationships
Equivalent to 10 Cigarettes a Day: How Loneliness Kills Us - Research Findings
42,024
Man and WomanPractices how toSolitude
- Photo
- Unsplash
Natalie could not understand why her sister Amanda was not divorcing her husband. She watched for years how she tolerates his betrayals, unbearable character, desire to control every step, even cruelty. The sister constantly complained about her husband, but did not divorce him. When Natalie realized that the cause was dependent personality disorder, it became easier for her to communicate with her sister. How to understand that it is in him?
The sister constantly complained about her husband, but did not divorce him. When Natalie realized that the cause was dependent personality disorder, it became easier for her to communicate with her sister. How to understand that it is in him?
1. Strong fear of separation
Fear of separation is not the same as fear of rejection. When we fear separation, we feel rejected. When we are afraid of separation, we do not perceive ourselves as a complete person without another person.
2. Unwillingness to make decisions
Since childhood, Amanda has been afraid to make decisions. She needed a million advice from her sister in any situation, until a husband appeared in her life. Even after she had already made some decision, she repeatedly asked if she had done the right thing.
3. The need to shift responsibility to others
This can be about anything: finances, the decision to marry or divorce, the principles of raising children, and so on.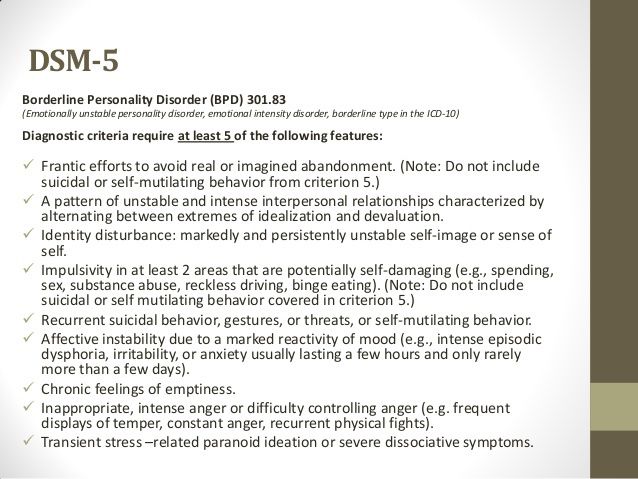 People with ADHD are usually happy to give it all to someone else. For a man who wants to control everything, such a wife becomes an ideal choice, because he does not tolerate attacks on authority in the house. However, such a "coincidence" of two people is dysfunctional.
People with ADHD are usually happy to give it all to someone else. For a man who wants to control everything, such a wife becomes an ideal choice, because he does not tolerate attacks on authority in the house. However, such a "coincidence" of two people is dysfunctional.
4. Fear of confrontation
Amanda hated conflict situations and preferred never to argue with her husband and even with Natalie herself, she was afraid of losing their sympathy and approval. Because of this, she constantly endured what she did not like at all.
5. The habit of doing things you don't really want to do
One day, after going to the church where her sister worked as a volunteer, Natalie noticed that she was very upset. Natalie asked if she liked helping out during a church service. The sister admitted that she never wanted and does not want to do this, but one of the ministers pressed on the feeling of guilt, saying that there was no one else who could not cope without her.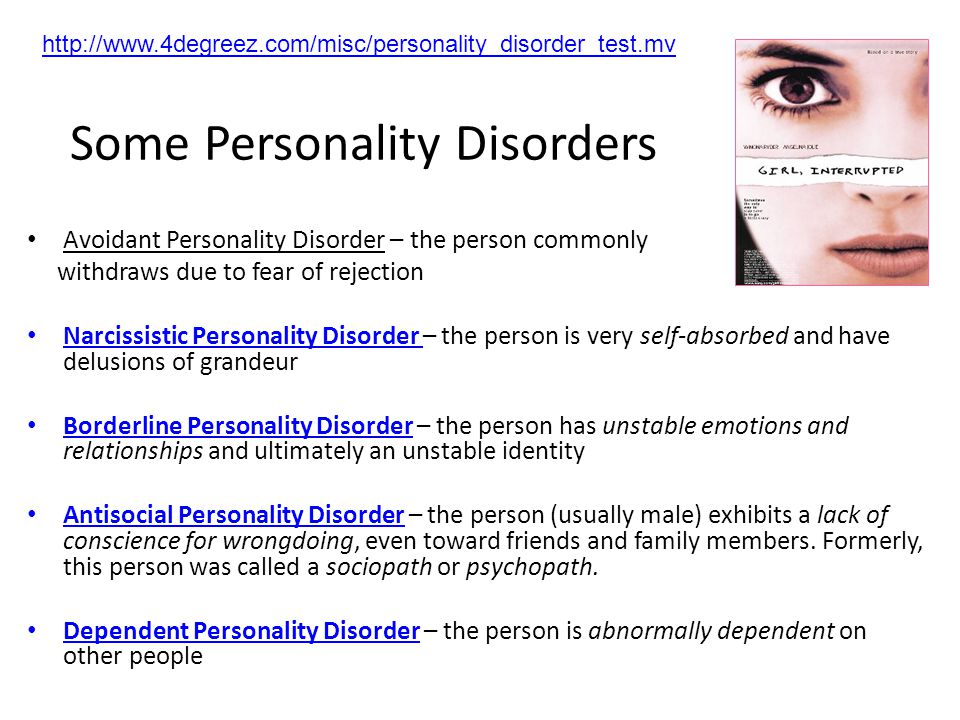
6. Belief in their own inadequacy
People with ADHD sincerely believe that they cannot take care of themselves, so they definitely need someone else who will be responsible for them. Usually they cannot be alone for a long time, without some kind of relationship. If there is a break, they fill this void with friends and relatives until a new partner appears.
7. False passivity and helplessness
One of the contradictions in Amanda's case was that she was a very successful and confident woman at work. At home, she became passive and unable to make decisions. Natalie knew that, in fact, her sister was more than capable of doing serious things and being responsible for them.
8. Hypersensitivity to criticism
Sister Natalie was comfortable with constructive criticism at work, but the slightest disapproval from loved ones became a disaster for her. Any reproach from her husband was unsettling. When her husband temporarily disappeared from life, this attitude was transferred to Natalie - her sister could not bear even a hint of disapproval of some actions.
When her husband temporarily disappeared from life, this attitude was transferred to Natalie - her sister could not bear even a hint of disapproval of some actions.
9. Tolerance to violence
One of the main characteristics of such people is the ability to ignore violence against them, to justify the abuser in all possible ways. Even if aggression is obvious, it is difficult to resist. This attitude makes them a target for controlling people.
10. Failure to respect their own needs
People with this disorder consider the needs of others more important. Especially when it comes to the person they "rely" on. They gladly satisfy other people's desires, because they consider this a manifestation of love. Unfortunately, this feature is often used for selfish purposes, putting people with ADHD in an unpleasant or even dangerous position.
Some time later, my sister still found the strength to get a divorce, and her family supported her. In less than a few months, she found herself in a new relationship.
In less than a few months, she found herself in a new relationship.
Source: growwithchristine.com
Narcissistic personality: how it is formed and expressed in relationships
Adapting the psyche to a crisis: 9 ways to survive
How to choose the right psychotherapist
“I have everything I need. But I'm still not satisfied with life.”
“I'm happy with my husband, but I constantly fall in love with my colleagues. What is wrong with me?"
Secrets of the male orgasm
Why do men not like to talk about their feelings?
Peculiarities of psychotherapeutic work with clients with a dependent personality structure
Year of publication and journal number:
2012, No. 2
The article will focus not on people dependent on various substances, but on clients with a dependent personality structure.
In classifiers of mental disorders, when describing people with a dependent personality structure, the terms “Dependent Personality Disorder” (heading “Disorders of Mature Personality and Adult Behavioral Disorders in ICD-10) and “Dependent Personality Disorder” (heading “Personality Disorders”) are used in DSM-IV).
The characteristic features of this personality disorder include: active or passive shifting to others of making most important decisions in one’s life, lack of self-control, lack of self-confidence, “gluing” to the object of addiction, lack of psychological boundaries, etc. These psychological characteristics are often accompanied by various symptoms. Among them are often found: psychosomatic diseases, alcoholism, drug addiction, deviant behavior, co-dependent and counter-dependent manifestations.
Most often, the dependent personality structure manifests itself in the form of dependent and codependent behavior. Therefore, dependence and co-dependence are different forms of manifestation of the dependent personality structure.
They have a number of personal properties in common: mental infantilism, pathological attachment to the object of dependence, with the only difference being that in the case of dependence such an object will be a substance, and in the case of co-dependence, another person.
The professional activity of a psychologist/psychotherapist often focuses on a codependent client.
Typical characteristics of a co-dependent person are involvement in the life of the Other, complete preoccupation with his problems and affairs. A co-dependent person is pathologically attached to the Other: a spouse, a child, a parent. In addition to the highlighted qualities, co-dependent people are also characterized by:
- low self-esteem;
- need for constant approval and support from others;
- uncertainty of psychological boundaries;
- the feeling of being powerless to change anything in destructive relationships, etc. [2, p. 22].
Codependent people make the members of their system dependent on them throughout their lives. At the same time, co-dependents actively intervene in the life of the addict, control him, know how best to act and what to do, disguising their control and intervention as love and care.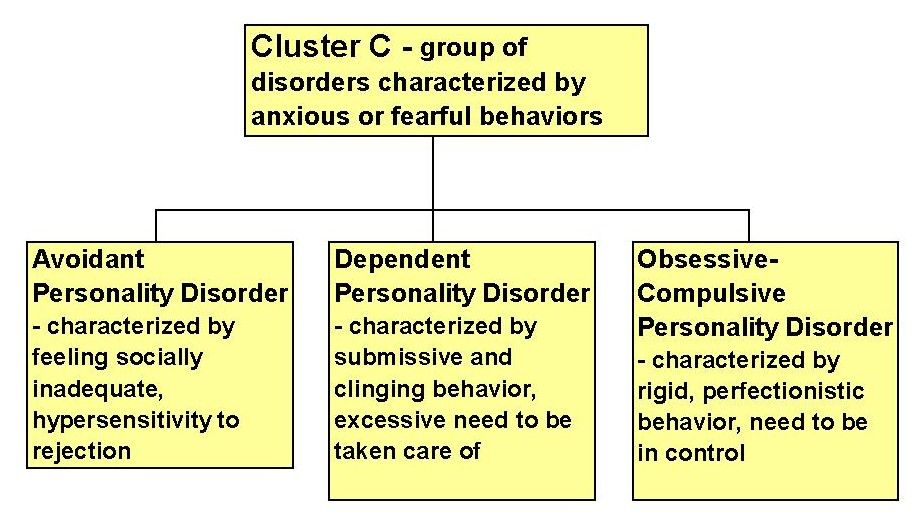 The other member of the couple - the dependent - has, accordingly, the opposite qualities: he is lack of initiative, irresponsible, incapable of self-control.
The other member of the couple - the dependent - has, accordingly, the opposite qualities: he is lack of initiative, irresponsible, incapable of self-control.
It is traditional to view addicts as some kind of social evil, and co-dependents as their victims. The behavior of codependents, as a rule, is socially approved and accepted. However, from a psychological point of view, the contribution of the codependent to such pathological relationships is no less than the dependent. The co-dependent himself no less needs the dependent - he is dependent on the dependent. This is a variant of the so-called "human" addiction.
Co-dependents themselves maintain dependency relationships, and when they escalate to a symptom, then they turn to a specialist to “cure” the addict, that is, in fact, return him to his former dependent relationship.
Any attempts by the dependent to get out of the control of the codependent cause a lot of aggression in the latter.
The partner of the co-dependent - the addict - is perceived as an object and its function in the pair of co-dependent-addict is comparable to the function of the object of the addict (alcohol, drug. ..). This function is to “plug a hole” in the identity of the co-dependent with the help of an object (in our case, a partner) in order to be able to feel whole, to find the meaning of life. It is not surprising that for a co-dependent, the dependent, despite all his shortcomings (from the point of view of the co-dependent), is so important, because he provides the most important function for him - meaning-forming. Without it, the life of a codependent loses all meaning. The dependent has its own object for this. Hence such a strong attachment of the co-dependent to the dependent.
..). This function is to “plug a hole” in the identity of the co-dependent with the help of an object (in our case, a partner) in order to be able to feel whole, to find the meaning of life. It is not surprising that for a co-dependent, the dependent, despite all his shortcomings (from the point of view of the co-dependent), is so important, because he provides the most important function for him - meaning-forming. Without it, the life of a codependent loses all meaning. The dependent has its own object for this. Hence such a strong attachment of the co-dependent to the dependent.
It is not surprising that the Other occupies such an important place in the picture of the Codependent World. But with all the importance and fixation on the Other, the attitude towards it is purely instrumental - as a function. In fact, there is simply no Other for the codependent, due to his egocentric position, as an individual person with his experiences, aspirations, desires. Yes, the Other is present in the picture of the Codependent World, even exaggeratedly, but only functionally.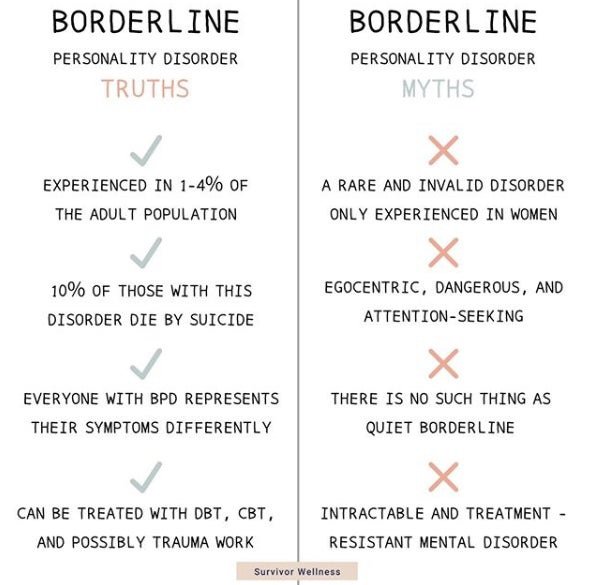
The reason for the formation of both dependent and codependent personality structure is the incompleteness of one of the most important stages of development in early childhood - the stage of establishing psychological autonomy necessary for the development of one's own "I", separate from parents. In fact, we are talking about a second birth - psychological, the birth of the Self as an autonomous entity with its own boundaries. According to G. Ammon, “... the formation of the border of the Self in symbiosis is a decisive phase in the development of the Self and identity. This emergence of the border of the Self, which contributes to the distinction between Self and non-Self in terms of identity formation, becomes possible due to the primary functions of the child's Self. In forming the boundaries of the self, the child also depends on the constant support of the environment, his primary group, especially the mother" [1, p. 65].
In M. Mahler's research, it was found that people who successfully complete this stage at the age of two or three years have a holistic inner sense of their uniqueness, a clear idea of their "I" and who they are.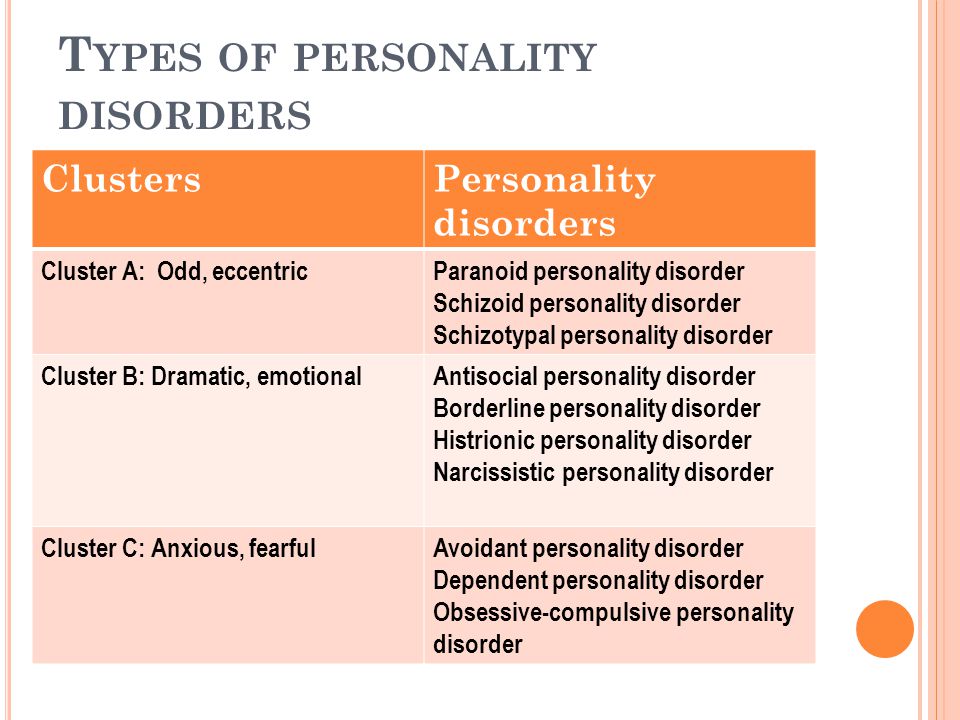 Feeling your Self allows you to declare yourself, rely on your inner strength, take responsibility for your behavior, and not expect someone to control you. Such people are able to be in intimate relationships without losing themselves. M. Mahler believed that for the successful development of a child's psychological autonomy, it is necessary that both parents have psychological autonomy [5]. The leading condition for such a birth of the I of the child is its acceptance by parental figures. In the same case, when parents, for various reasons, are not able to accept (unconditionally love) their child, he remains in a state of chronic dissatisfaction in accepting his own self and is forced all his life to unsuccessfully try to find this feeling or obsessively “cling” to another ( co-dependent), or by compensating for this feeling with chemical surrogates (dependent).
Feeling your Self allows you to declare yourself, rely on your inner strength, take responsibility for your behavior, and not expect someone to control you. Such people are able to be in intimate relationships without losing themselves. M. Mahler believed that for the successful development of a child's psychological autonomy, it is necessary that both parents have psychological autonomy [5]. The leading condition for such a birth of the I of the child is its acceptance by parental figures. In the same case, when parents, for various reasons, are not able to accept (unconditionally love) their child, he remains in a state of chronic dissatisfaction in accepting his own self and is forced all his life to unsuccessfully try to find this feeling or obsessively “cling” to another ( co-dependent), or by compensating for this feeling with chemical surrogates (dependent).
In terms of psychological development, dependent and codependent are approximately on the same level. Undoubtedly, this is the level of the borderline organization of the personality structure with its characteristic egocentrism, impulsiveness as an inability to retain affect, and low self-esteem. The dependent-codependent pair is formed according to the principle of complementarity. It is difficult to imagine a couple of a person with an autonomous self and a co-dependent.
The dependent-codependent pair is formed according to the principle of complementarity. It is difficult to imagine a couple of a person with an autonomous self and a co-dependent.
They also have a pathological attachment to the object of addiction in common. In the case of a codependent personality structure, such an object, as mentioned earlier, is a partner. In the case of an addict, a “non-human” object. The mechanism of “choosing” an object is not clear, but in both cases we are dealing with a dependent personality structure.
How do people with this personality structure get into psychotherapy? Most often, a psychologist/psychotherapist deals with two types of request:
1. The request is made by a co-dependent, and the client of the psychologist/psychotherapist becomes a dependent (the co-dependent brings or sends the dependent to therapy). In this case, we are faced with a situation that is not standard for psychotherapy: the customer is a co-dependent, and the client becomes a dependent.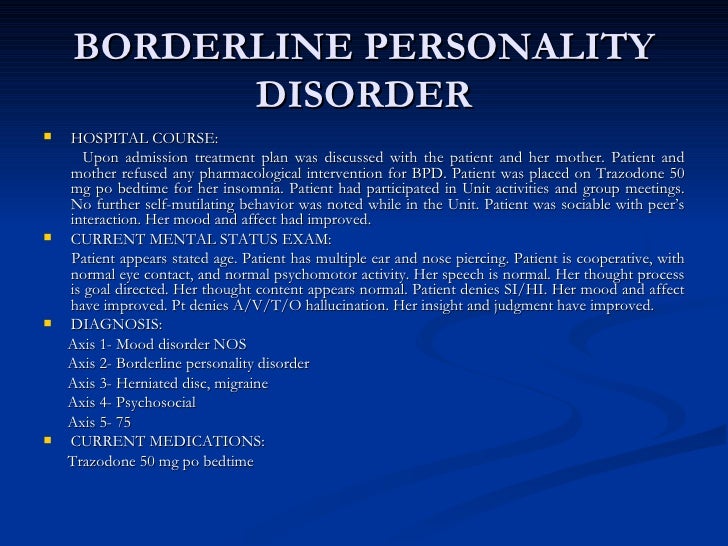 This situation seems to be prognostically unfavorable for therapy, since here we are not really dealing with the client - one of the necessary conditions for therapy is not observed - the client's recognition of his own "contribution" to the current problem situation, as well as the denial of the existence of the problem itself. As an example of the situation under consideration, we can cite cases of parents asking to “fix” the child’s problem behavior, or one of the spouses who wants to rid their partner of a pathological habit.
This situation seems to be prognostically unfavorable for therapy, since here we are not really dealing with the client - one of the necessary conditions for therapy is not observed - the client's recognition of his own "contribution" to the current problem situation, as well as the denial of the existence of the problem itself. As an example of the situation under consideration, we can cite cases of parents asking to “fix” the child’s problem behavior, or one of the spouses who wants to rid their partner of a pathological habit.
2. The codependent seeks therapy himself. This is a prognostically more promising option for therapy. Here we deal in one person with both the client and the customer. For example, parents seek professional help with a desire to sort out a problematic relationship with a child, or one of the spouses wants with the help of a psychotherapist to understand the reason for his relationship with a partner that does not suit him.
If in the first case psychotherapy is impossible in principle, then in the second case the codependent client has a chance. Despite this, such clients usually do not respond well to psychotherapy, since the range of their problems is due to a basic defect in their psyche. Lack of self-control, infantilism, limited scope of interests, “sticking” to the object of dependence are a serious challenge for a psychologist/psychotherapist.
Despite this, such clients usually do not respond well to psychotherapy, since the range of their problems is due to a basic defect in their psyche. Lack of self-control, infantilism, limited scope of interests, “sticking” to the object of dependence are a serious challenge for a psychologist/psychotherapist.
Dependent clients are easily recognized at the first contact. Most often, the initiator of the meeting is a co-dependent close relative of the addict - mother, wife ... Often, the first feeling of the client is surprise. And not by accident. After talking with the calling mother about the problems of her boy, you naturally wonder how old he is? To your surprise, you find out that the boy is 25, 30, or even more ... So you come across one of the central qualities of the addict's personality - his infantilism. The essence of mental infantilism lies in the discrepancy between the psychological age and the age of the passport. Adult men and women in their behavior demonstrate childish traits atypical for their age - touchiness, impulsiveness, irresponsibility. Such clients themselves are not aware of their problems and are not able to ask for help from the environment - usually their relatives ask for help or someone brings them to therapy literally “by the hand”. The psychotherapist will have to work with a "little child" who is not aware of his desires, needs, his separation from the environment. Dependents always remain for co-dependent children.
Such clients themselves are not aware of their problems and are not able to ask for help from the environment - usually their relatives ask for help or someone brings them to therapy literally “by the hand”. The psychotherapist will have to work with a "little child" who is not aware of his desires, needs, his separation from the environment. Dependents always remain for co-dependent children.
Working with both dependent and co-dependent clients is not limited to the therapist-client relationship, but inevitably draws the psychotherapist into the field relationship. The psychologist/therapist has to work not with one person, but with the system. He is constantly drawn into these systemic relationships. It is very important for a psychologist/therapist to be aware of this. If he is drawn into systemic relations, he loses his professional position and becomes professionally ineffective, since it is impossible to change the system while being in the system itself.
One form of "pulling" the therapist into the system is the so-called triangles.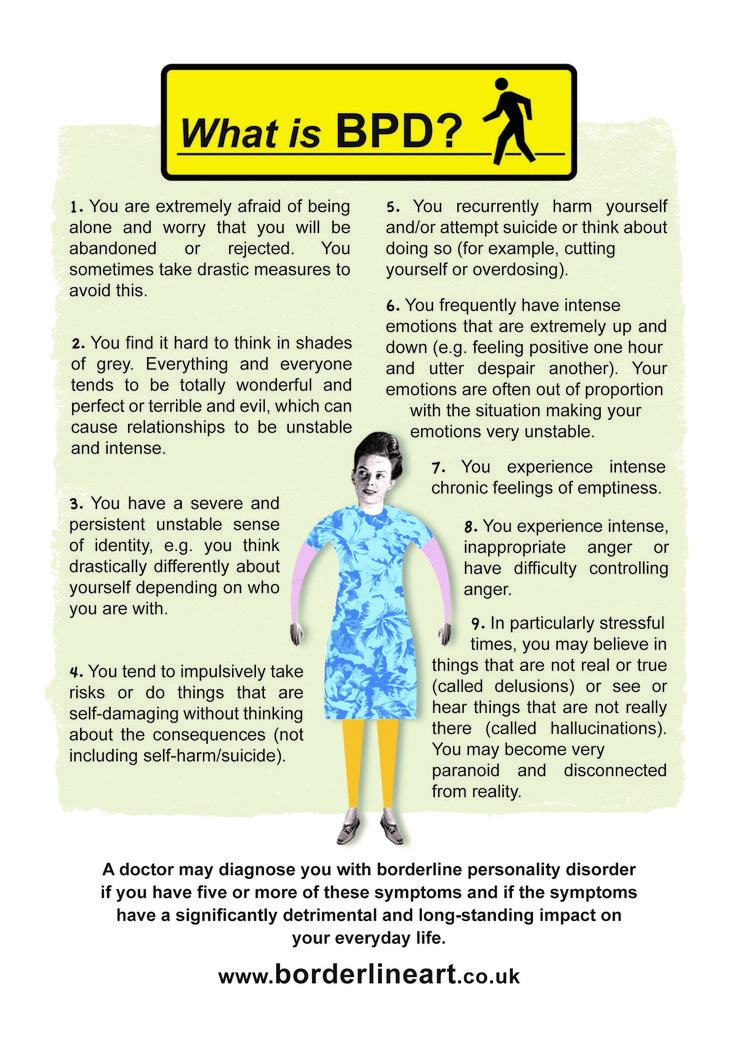 Triangles are a necessary attribute of the life of dependent-codependent. S. Karpman, developing the ideas of E. Bern, showed that the whole variety of roles underlying the "games that people play" can be reduced to three main ones - the Rescuer, the Persecutor and the Victim. The triangle that unites these roles symbolizes both their connection and constant change. This triangle can be viewed both interpersonally and intrapersonally. Each role position can be described by a set of feelings, thoughts, and characteristic behaviors.
Triangles are a necessary attribute of the life of dependent-codependent. S. Karpman, developing the ideas of E. Bern, showed that the whole variety of roles underlying the "games that people play" can be reduced to three main ones - the Rescuer, the Persecutor and the Victim. The triangle that unites these roles symbolizes both their connection and constant change. This triangle can be viewed both interpersonally and intrapersonally. Each role position can be described by a set of feelings, thoughts, and characteristic behaviors.
A victim is one whose life is ruined by a tyrant. The victim is unhappy, does not achieve what he could if he were released. She is forced to control the tyrant all the time, but she does not succeed well. Usually the victim suppresses his aggression, but it can manifest itself in the form of outbursts of rage or auto-aggression. To support a pathological relationship, the victim needs external resources in the form of help from the rescuer.
A tyrant is one who persecutes the victim, often believing that the latter is to blame and provokes him to "bad" behavior. He is unpredictable, not in charge of his own life, and needs the other person's sacrificial behavior in order to survive. Only the departure of the victim or a steady change in his behavior can lead to a change in the tyrant.
He is unpredictable, not in charge of his own life, and needs the other person's sacrificial behavior in order to survive. Only the departure of the victim or a steady change in his behavior can lead to a change in the tyrant.
Rescuer is an important part of the triangle, which gives “bonuses” to the victim in the form of support, participation, various types of assistance. Without a rescuer, this triangle would fall apart, since the victim would not have enough of his own resources to live with a partner. The rescuer also benefits from participating in this project in the form of the gratitude of the victim and the feeling of his own omnipotence from being in a position "on top". The psychologist/therapist is initially assigned the role of a rescuer, but in the future he can be included in other roles - a tyrant and even a victim.
Analyzing the therapeutic relationship in work with the described clients, it should be noted that they (relationships) are quite unstable due to resistance in work on the part of both the client (addicted-codependent) and the therapist.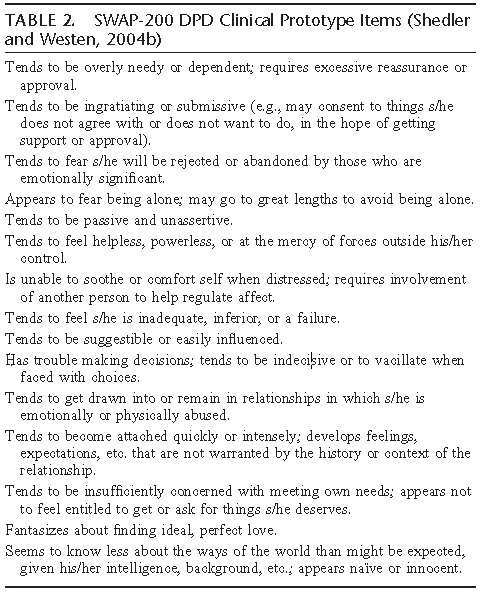
The co-dependent (most often the customer of therapy) is dissatisfied with the results of the work, because the psychologist/psychotherapist does not do what he would like. He most often consciously resists therapy, prevents it in every possible way, using an arsenal of the most harmless methods - excuses of the addicted to therapy, to quite serious ones - threats to both the client of therapy and the therapist himself.
The addict (client) - on the one hand, consciously wants changes, on the other hand, unconsciously resists it in every possible way, since he is pathologically attached to the codependent. He is infantile, lacking initiative, he is held back by guilt and fear. He often unconsciously connects the objects of the system to the resistance.
The psychologist/therapist may also unconsciously turn on the mechanisms of resistance to work. The feelings that he experiences for the client can hardly be classified as positive: fear, anger, hopelessness...
Fear of arises as a result of the fact that the position of the psychologist/therapist is quite vulnerable, it can easily be harmed, since the content of psychological assistance is not clear enough to ordinary people. There are no clear objective criteria for the success of therapy in the work of a psychologist/therapist. The position of a psychologist/therapist is also vulnerable in legal terms - often he does not have a license for this kind of activity due to legislative peculiarities. The position of a specialist is also unstable in terms of competition with medical colleagues - "psychotherapists in law". Any complaint from a dissatisfied customer can create many difficulties for a psychologist / psychotherapist.
There are no clear objective criteria for the success of therapy in the work of a psychologist/therapist. The position of a psychologist/therapist is also vulnerable in legal terms - often he does not have a license for this kind of activity due to legislative peculiarities. The position of a specialist is also unstable in terms of competition with medical colleagues - "psychotherapists in law". Any complaint from a dissatisfied customer can create many difficulties for a psychologist / psychotherapist.
Despair is due to the fact that working with such clients is long and slow, and the changes are small and unstable.
Anger is due to the fact that the client is a manipulator, a borderline personality, he is a great specialist in breaking psychological boundaries, including the boundaries of therapy and the therapist.
When working with clients with a dependent personality structure, it is important to remember a number of important points.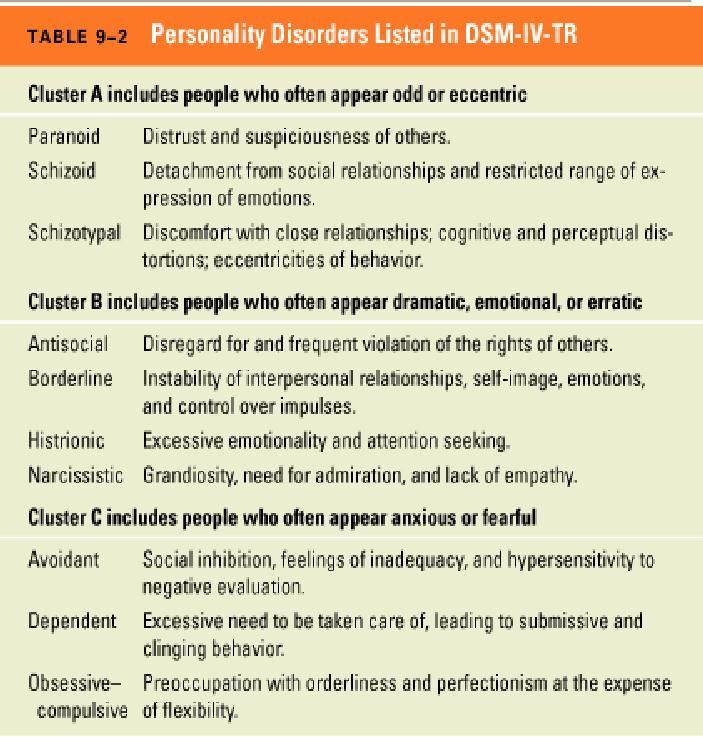
In the case where the client is an addict, the therapist does not work with the client, but with a systemic phenomenon, the client is a symptom of a dysfunctional system. In this regard, it is impossible to work with the client as a symptom in individual therapy. In this case, the best thing a psychologist/psychotherapist can do is to try to bring the codependent into therapy. In working with a co-addict, it will be strategically important not to be included in systemic relationships (the system is stronger), but to maintain his psychological autonomy in the client. The general strategy in working with both addicts and co-addicts is to focus on their psychological maturation.
Codependent personality therapy is a maturation therapy. The origins of codependency, as we noted earlier, lie in early childhood. The therapist needs to remember that he is working with a client who, in terms of his psychological age, corresponds to a child of 2-3 years old. Consequently, the goals of therapy will be determined by the developmental tasks characteristic of this age period.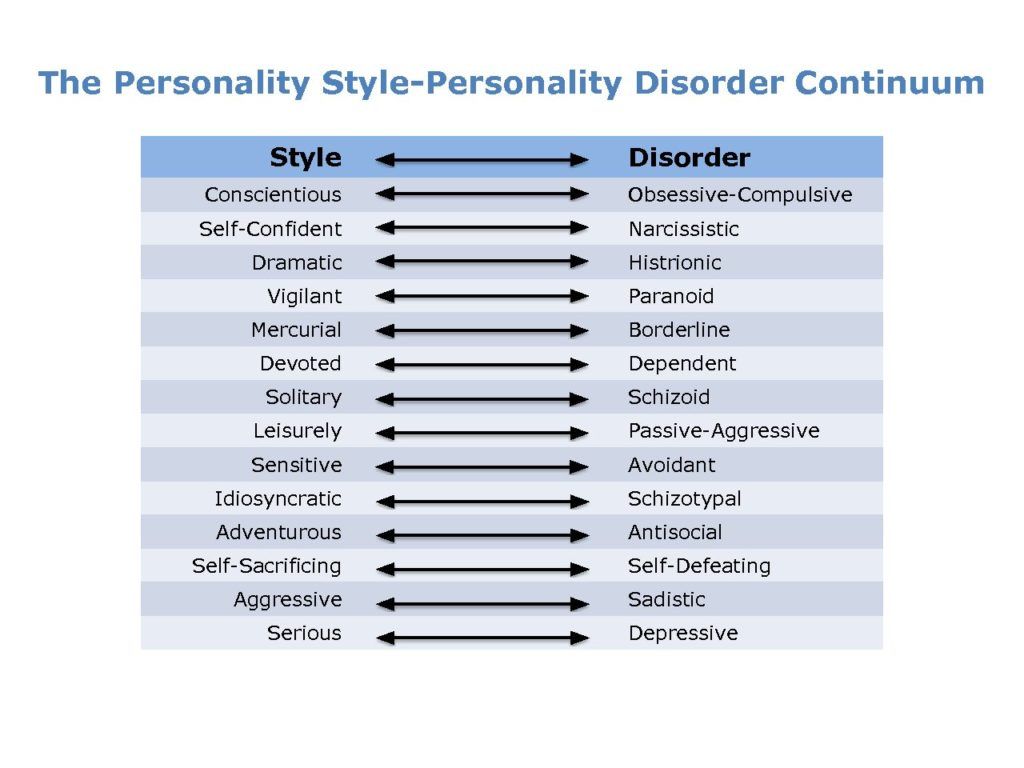 Therapy with clients with a dependent personality structure can be seen as a client “growing” project; such therapy can be metaphorically thought of as a mother-child relationship. This idea is not new. Even D. Winnicott wrote that in “therapy we are trying to imitate the natural process that characterizes the behavior of a particular mother and her child. … it is the “mother-infant” couple that can teach us the basic principles of working with children whose early communication with their mother was “not good enough” or turned out to be interrupted” [3, p.31].
Therapy with clients with a dependent personality structure can be seen as a client “growing” project; such therapy can be metaphorically thought of as a mother-child relationship. This idea is not new. Even D. Winnicott wrote that in “therapy we are trying to imitate the natural process that characterizes the behavior of a particular mother and her child. … it is the “mother-infant” couple that can teach us the basic principles of working with children whose early communication with their mother was “not good enough” or turned out to be interrupted” [3, p.31].
The main goal of therapy with clients with a dependent personality structure is to create conditions for the "psychological birth" and development of one's own "I", which is the basis for its psychological autonomy. To do this, it is necessary to solve a number of tasks in psychotherapy: restoring boundaries, gaining the client's sensitivity, primarily to aggression, contact with their needs, desires, learning new models of free behavior.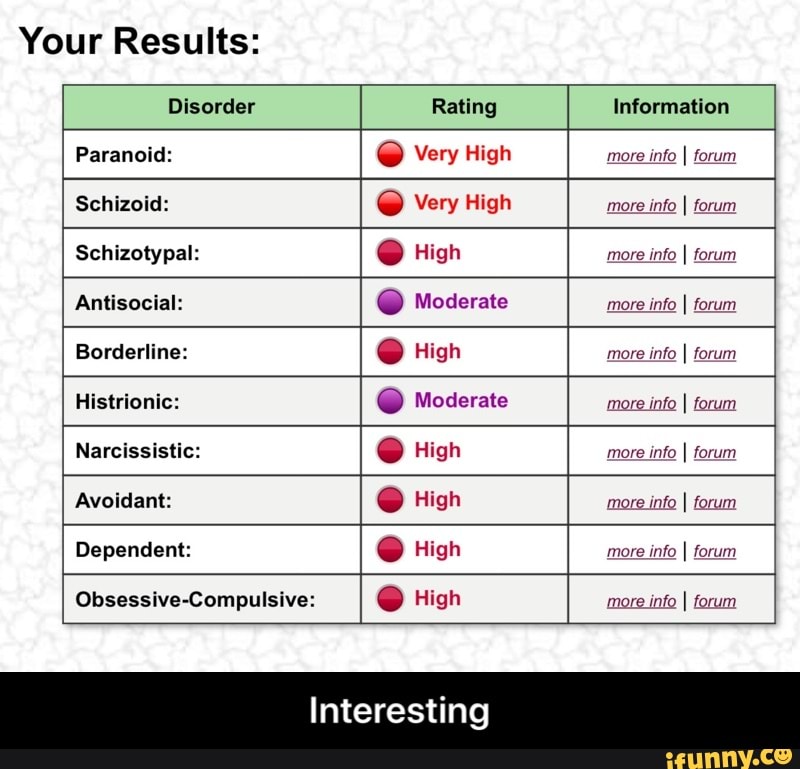
The use of the metaphor "parent-child" in the psychotherapy of codependent clients allows us to determine the strategy for working with them. The psychologist/therapist should be nonjudgmental and accepting of the various manifestations of the client's Self. This makes special demands on the therapist's awareness and acceptance of the rejected aspects of his own Self, his ability to withstand manifestations of various feelings, emotions and states of the client, primarily his aggression. The development of destructive aggression makes it possible to get out of pathogenic symbiosis and delimit one's own identity [1, p.111].
The psychologist/therapist will have to put in a lot of effort in building a trusting relationship before the client allows himself more freedom to express his own feelings and experiences. The appearance at the next stage of the work of the client's counter-dependent tendencies with aggressive reactions towards the therapist - negativism, aggression, depreciation - must be welcomed in every possible way.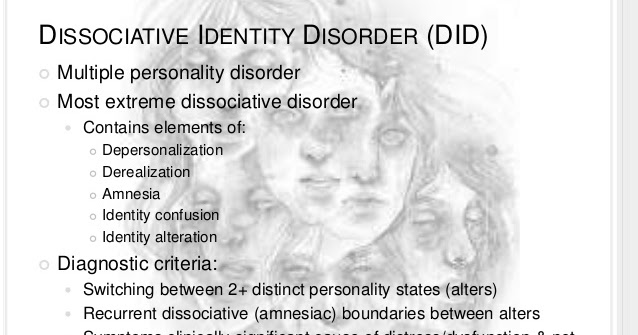 The client has a real opportunity to experience in therapy the manifestation of his “bad” part, while maintaining the relationship and not receiving rejection. This new experience of accepting yourself as a significant Other can become the basis for accepting yourself, which will serve as a condition for building healthy relationships with clear boundaries. The therapist, at this stage of therapy, needs to stock up on a capacious "container" for "storage" of the client's negative feelings.
The client has a real opportunity to experience in therapy the manifestation of his “bad” part, while maintaining the relationship and not receiving rejection. This new experience of accepting yourself as a significant Other can become the basis for accepting yourself, which will serve as a condition for building healthy relationships with clear boundaries. The therapist, at this stage of therapy, needs to stock up on a capacious "container" for "storage" of the client's negative feelings.
A separate and important part of the therapeutic work should be devoted to the client becoming sensitive to his Self and integrating it. For clients with a dependent personality structure, selective alexithymia is characteristic, which consists in the inability to recognize and accept the rejected aspects of one's Self - feelings, desires, thoughts. As a result, the co-dependent, according to the definition of G. Ammon, has a “structural narcissistic defect”, which manifests itself in the existence of a “defect of the boundaries of the Self” or “holes of the Self”.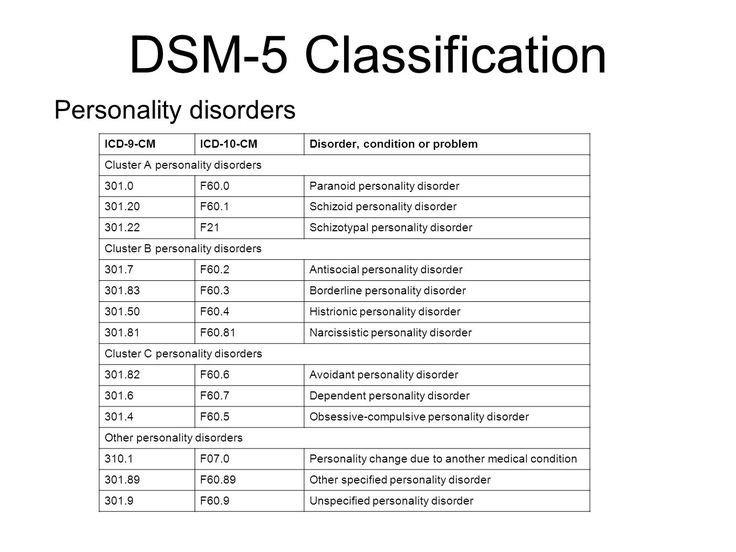 The task of therapy at this stage of work is the awareness and acceptance of the rejected aspects of the Self, which contributes to “patching holes” in the client's Self. The discovery of the positive potential of "negative" feelings is the client's invaluable insights in this work, and their acceptance is a condition for the integration of his identity.
The task of therapy at this stage of work is the awareness and acceptance of the rejected aspects of the Self, which contributes to “patching holes” in the client's Self. The discovery of the positive potential of "negative" feelings is the client's invaluable insights in this work, and their acceptance is a condition for the integration of his identity.
The criterion for successful therapeutic work is the emergence in the client of his own desires, the discovery of new feelings in himself, the experience of new qualities of his Self on which he can rely, as well as the ability to remain alone.
An important point in the therapy of clients with a dependent personality structure is the focus in work not on the symptoms of dependent behavior, but on the development of the client's identity. It must be remembered that the Other, as described above, performs a structure-forming function that gives the codependent a sense of the integrity of his Self, and in general - the meaning of life. F. Alexander spoke about the "emotional gap" that remains in the patient after the elimination of the symptom. He also emphasized the danger of psychotic disintegration that may follow. This "emotional gap" just means a "hole in the Self", a structural deficit in the border of the patient's Self. Therefore, the goal of therapy should be to assist the patient in the formation of a functionally effective boundary of the self, which leads to the uselessness of dependent behavior that replaces or protects this boundary .
F. Alexander spoke about the "emotional gap" that remains in the patient after the elimination of the symptom. He also emphasized the danger of psychotic disintegration that may follow. This "emotional gap" just means a "hole in the Self", a structural deficit in the border of the patient's Self. Therefore, the goal of therapy should be to assist the patient in the formation of a functionally effective boundary of the self, which leads to the uselessness of dependent behavior that replaces or protects this boundary .
An important criterion for the success of working with such clients is to overcome their egocentric position. This is manifested in the fact that the client begins to notice in the therapist and in other people their humanity - vulnerability, sensitivity. One of the markers of such a neoplasm is the appearance of a feeling of gratitude in the client.
Psychotherapy of a client with a dependent personality structure is a long-term project. There is an opinion that its duration is calculated at the rate of one month of therapy for each year of the client's life.