Dating someone schizophrenia
What to Expect — Talkspace
Dating is challenging, no matter who you are or who you pick as a partner. However, for people in relationships with one of the nearly 1% of the population who struggles with schizophrenia, dating can be exceptionally challenging.
Schizophrenia is a mental health condition hallmarked by unpredictable emotions, hallucinations, and delusions. While dating someone with this disorder can sometimes be difficult, learning as much as you can about schizophrenia can help shape your relationship in a meaningful way.
Keep reading to learn more about the challenges that come with dating someone who has schizophrenia.
Before Diagnosis
Symptoms of schizophrenia tend to manifest when a person is in their late teens into the 30s. Women are more likely to be diagnosed with the disorder than men. Schizophrenia tends to be progressive, meaning it gets worse as time goes on. For this reason alone, it’s important to begin treatment as soon as symptoms first appear.
Treatment will ensure the best outcome and the most likely chance that rewarding, healthy relationships are possible in the future. The challenging part is that people with schizophrenia often don’t realize that they need help.
The key symptoms of schizophrenia include hallucinations, which involve seeing or hearing things that aren’t real (although they seem real to the person experiencing them).
Experiencing delusions is another common symptom that involves believing things that aren’t real — for example, believing you’re the President of the United States. Delusions can also involve believing scenarios that aren’t based on fact, like thinking something happened that didn’t.
People with schizophrenia can also:
- Have difficulty showing emotions
- Might withstand emotionally or socially
- Have a hard time expressing themselves
- Find it hard at times to process what they’re told
- Have abnormal movements
- Speak in disorganized patterns
- Maintain odd or unhealthy eating and sleeping habits
“One of the most common symptoms that is often ignored or misunderstood is disorganized speech.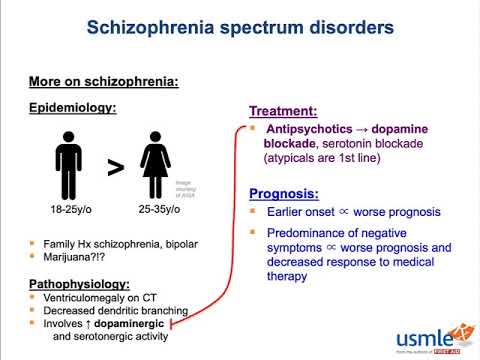 It can be seen as a result of other issues, but is not always connected to schizophrenia.”
It can be seen as a result of other issues, but is not always connected to schizophrenia.”
Talkspace therapist Cynthia V. Catchings, LCSW-S
If your partner begins to exhibit signs of schizophrenia or any other mental health condition, it’s important to support them. If you think their actions are bizarre, they’re likely having difficulty coping also.
The best thing you can do is have them evaluated by a mental health professional who can diagnose them and recommend a treatment plan. We can’t say often enough that early treatment of schizophrenia is essential for the best outcome.
After DiagnosisThe time after a schizophrenia diagnosis can be scary for you and your partner. Learning effective ways to help them is the best support you can provide right now.
3 Ways to support your partner after schizophrenia diagnosisThere are dozens of ways to help someone with schizophrenia, but a few strategies will be more helpful than others.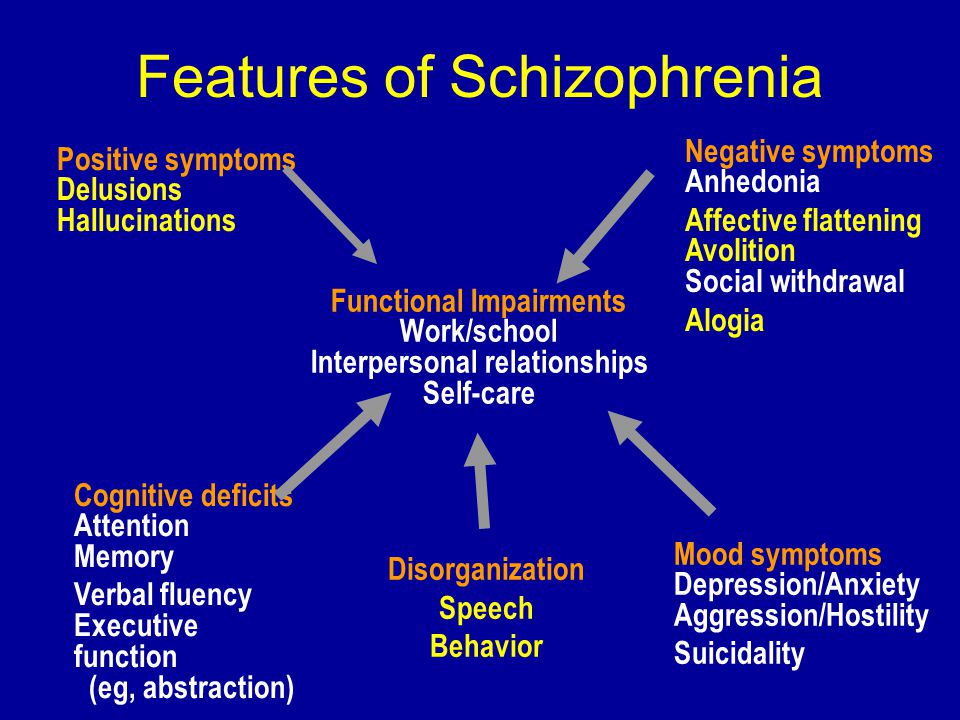
- Fight (or at least acknowledge) the stigma. Unfortunately, mental health conditions — especially serious ones like schizophrenia — carry a stigma in our society. Acknowledging this with your partner, and letting them know that you support them unconditionally, can go a long way in boosting their self-esteem and helping them stay with a treatment plan.
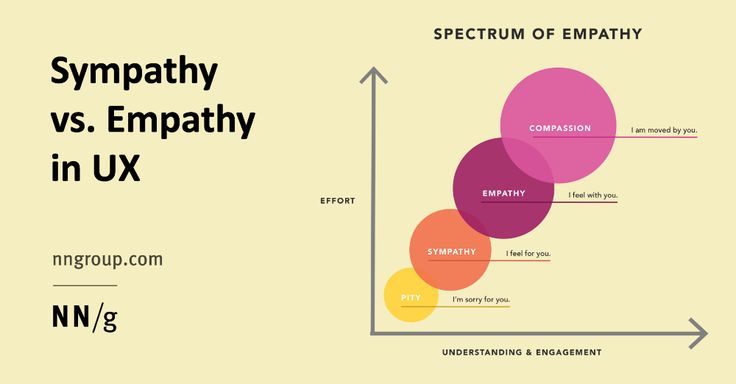
- Learn as much as you can about their condition. Educating yourself about your partner’s condition means you can be a better health advocate for them. It can also help you in general, as when you have a better understanding of what they’re going through, you’ll be able to lead with compassion, not frustration or misunderstanding.
- Be empathetic. Keep in mind, especially when things are really challenging, this is difficult for them, too. Bring empathy to any conversation you have about their mental health.
“Educating yourself and joining online or in-person support groups can be helpful and good ways to support your partner.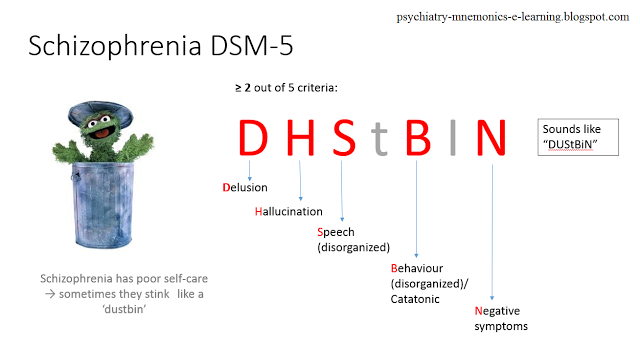 Remember that they act the way they do due to their diagnosis and that your support can make a true difference.”
Remember that they act the way they do due to their diagnosis and that your support can make a true difference.”
Talkspace therapist Cynthia V. Catchings, LCSW-S
Any mental health diagnosis complicates a relationship. However, a diagnosis of schizophrenia can make communication and meeting each other’s needs even more difficult. The good news is that with a diagnosis, you can put a name and a cause to the symptoms your partner is experiencing. Then, you can work together to get them the treatment they need to improve and strengthen your relationship.
Challenges you may faceSchizophrenia can present several challenges in a relationship. Knowing these upfront, and being able to understand them, means you can hopefully avoid frustration and keep things calm and in perspective. For example:
1. Finances can be challenging if your partner cannot work because of their diagnosis.
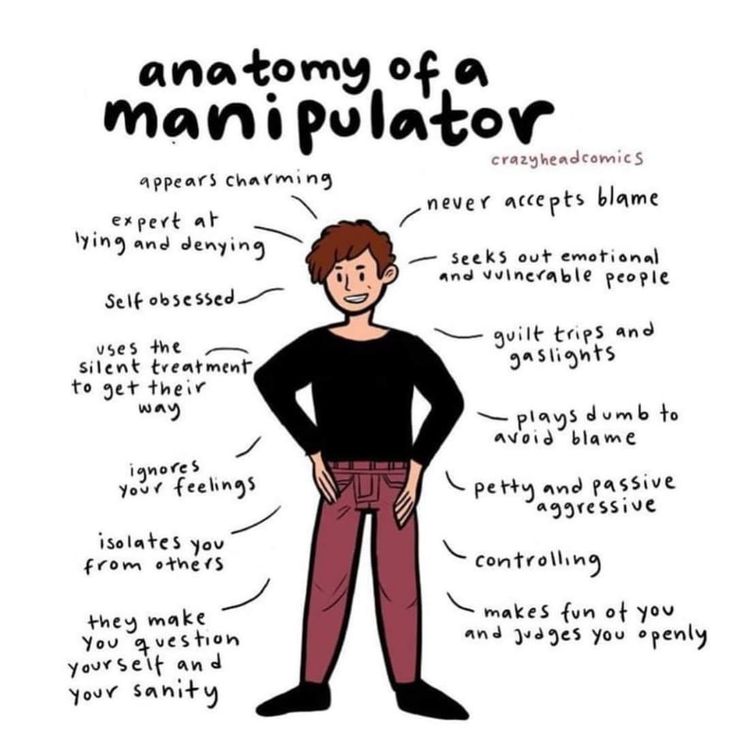
2. Communication, always critical in a relationship, can be complicated by hallucinations and delusions or by your partner shutting down emotionally.
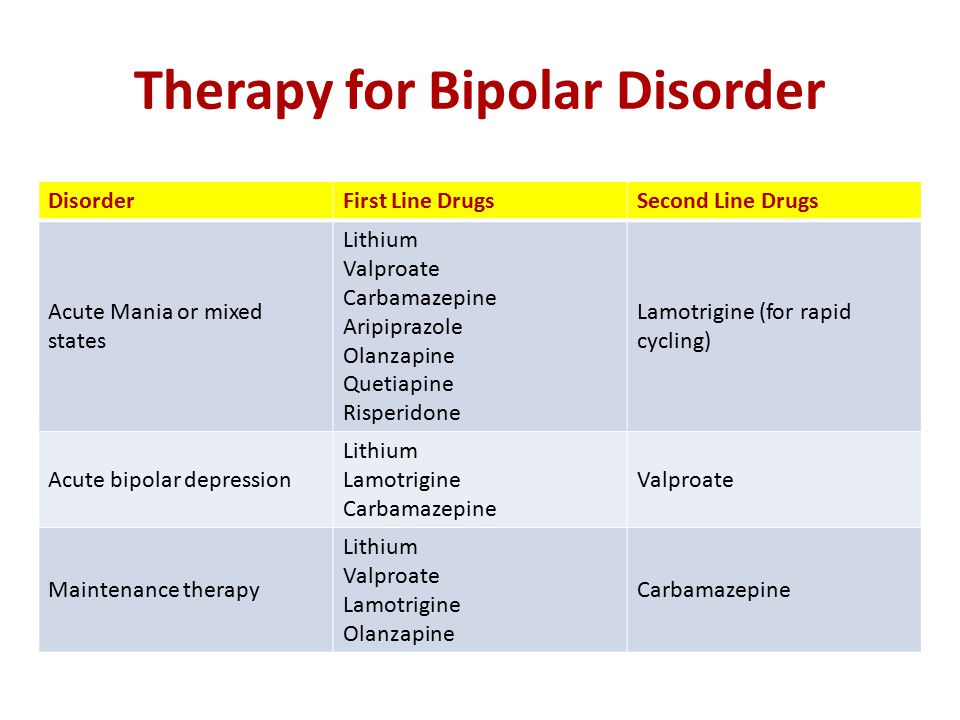
3. Medication used to control and ease symptoms of schizophrenia can cause mood swings, unexpected behavior, and changes in libido. Often, it takes a while before a mental health team finds a schizophrenia medication that works well for someone.
4. Treatment can often bring out unresolved feelings and childhood trauma that can be difficult for both partners to deal with.
How to manage the challengesThere are several ways you can successfully navigate the challenging aspects of a relationship with someone who has schizophrenia.
1. Work on your communication skills. Good listening skills are essential to any healthy relationship. That’s especially true when you’re involved with someone who has paranoid schizophrenia. Listen to what your partner is experiencing, but also be sure to communicate your own needs.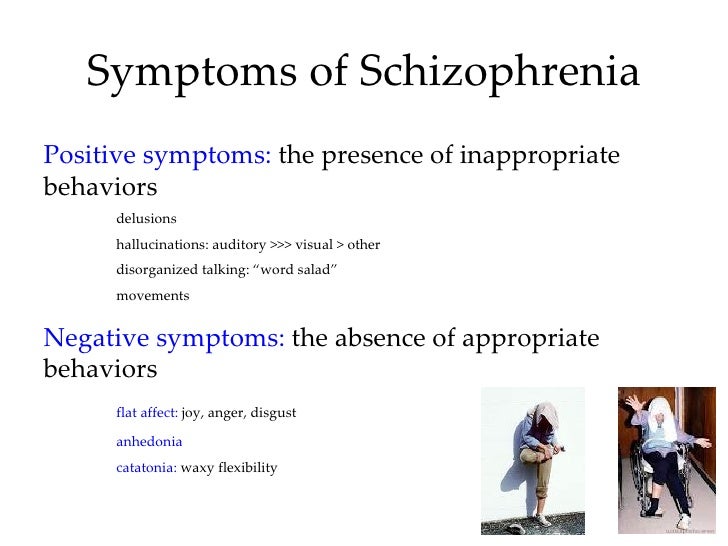 It doesn’t have to be all about the person with the condition.
It doesn’t have to be all about the person with the condition.
2. Be patient. Medication can cause a myriad of symptoms, especially while your partner’s mental health team is trying to find the right combination. Symptoms and stress from treatment can cause moodiness, disrupt sex drive, and make your partner act impulsively. Try to be patient.
3. Don’t let your partner stop treatment to work on your relationship. Early treatment and therapy for schizophrenia are essential for a long-term positive outcome when dealing with schizophrenia. Assure your partner that you can take on the challenges of treatment (or other treatment options) and that you’ll be there for them throughout the process.
4. Suggest couples therapy. Dating someone with schizophrenia can present a few more challenges than some other relationships might. You can find mutual support for the both of you when you start couples therapy. If nothing else, it might show your partner you’re committed to the health of your relationship.
“People diagnosed with schizophrenia struggle to start relationships and show their emotions. That can make it difficult for them, and later on for their partners, due to the lack of emotional response. Talking to a mental health professional about ways to overcome this issue can help a couple in many ways.”
Talkspace therapist Cynthia V. Catchings, LCSW-S
The good news if you’re dating someone with schizophrenia is that there are many resources available designed to help both the person diagnosed as well as those who care about them.
Your partner’s mental health team can point you towards good support groups in your area.
You can still have a rewarding relationship when you’re dating someone with schizophrenia. It helps if you’re able to educate yourself, so you’re prepared for the unexpected, and getting support is always a good first step.
Talkspace is an online therapy platform that aims to make access to mental health care simple and affordable. We have skilled therapists available to help you and your partner successfully manage any condition or challenge in your relationship, including schizophrenia. There isn’t a cure for schizophrenia, but with the right tools and coping skills, you can learn to maintain a healthy, mutually rewarding relationship with a loved one with schizophrenia. Talkspace can help.
We have skilled therapists available to help you and your partner successfully manage any condition or challenge in your relationship, including schizophrenia. There isn’t a cure for schizophrenia, but with the right tools and coping skills, you can learn to maintain a healthy, mutually rewarding relationship with a loved one with schizophrenia. Talkspace can help.
See references
- Schizophrenia. National Institute of Mental Health (NIMH).
- What is Schizophrenia?. American Psychiatric Association.
Finding Love When You Have Schizophrenia: Tips on Dating
Written by Camille Noe Pagán
Dating can be tough for anyone. A serious mental health condition like schizophrenia adds even more challenges to the mix. At times, it can cause psychotic behaviors, like hallucinations and delusional thought processes. In severe cases, dating is probably out of the question. Even if your condition is well-treated, you may have trouble enjoying activities. It might be difficult for you to show your emotions, too.
It might be difficult for you to show your emotions, too.
As a result, many people with schizophrenia find it hard to start relationships and keep them. Others avoid it all together. But some are able to have healthy relationships. If you have schizophrenia or you’re romantically involved with someone who does, here’s what you need to know.
It May Not Be Right for You
You may not ever feel like or be able to pursue a romantic relationship -- and that’s OK. “Your symptoms might get in the way of socializing or make you anxious,” says Lionel S. Wininger, PhD, a psychologist at Montefiore Medical Center in New York City.
But if you’re in treatment and your condition is well-controlled, it could be something to try. Though many people with schizophrenia do get worse, others do improve and can have successful relationships.
It can take a while to find a treatment plan that works. You may have to wait weeks or even months before it fully takes effect. Ask the doctor who treats your schizophrenia if they feel your plan is working and you’re ready.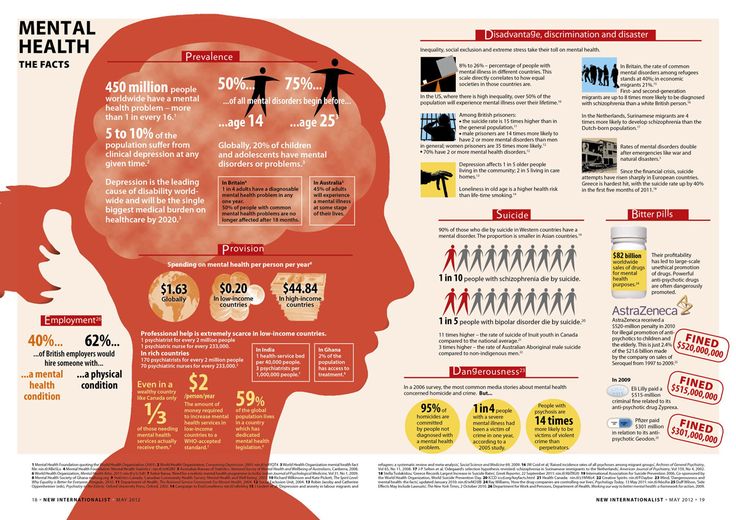 Besides medication, you’ll want to discuss lifestyle issues. “For example, if you spend the night at someone else’s house, do you have a plan for making sure you’re able to take your medication on schedule?” says Alex Dimitriu, MD, a psychiatrist and the founder of Menlo Park Psychiatry & Sleep Medicine in California.
Besides medication, you’ll want to discuss lifestyle issues. “For example, if you spend the night at someone else’s house, do you have a plan for making sure you’re able to take your medication on schedule?” says Alex Dimitriu, MD, a psychiatrist and the founder of Menlo Park Psychiatry & Sleep Medicine in California.
You also need think about how the rest of your life is going. “Regularity is important if you have schizophrenia, and dating can disrupt that,” Dimitriu says. If you’re dealing with another big change, like a new job, location, or treatment plan, you may want to wait until you’re settled to try dating.
How Do You Let Them Know?
There have been major advances in treatment for this condition over the past several decades.
But the person you’re seeing may have wrong ideas about what it is. For example, they may think you have multiple personalities or that you frequently hallucinate.
They may not know that most people who live with it aren’t violent and that treatment can ease and even prevent psychosis.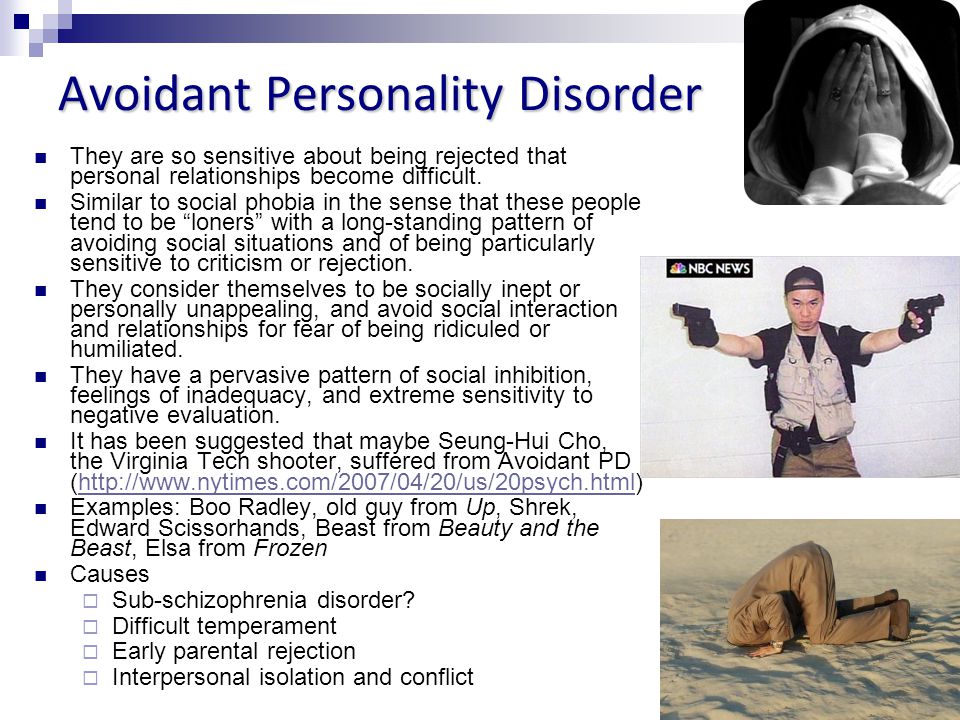
That’s why you may want to wait until you’ve gone out with someone a few times to tell them you have it. “Once the person has gotten to know you a little, it may be easier for them to see that you don’t fit the stereotype of someone with schizophrenia,” Wininger says.
When you’re ready, let them know you’d like to discuss something personal. You might say something like, “I want to share something important with you. It’s tough to talk about, and I hope you’ll hear me out.” Dimitriu says to stay honest and emphasize the positive.
For example, you could say, “I have schizophrenia, but it’s well-managed and I’ve been symptom-free for X number of months or years.” Explain that it’s a lasting mental disorder that can affect how you think, feel, and behave. Also let them know that while it can cause severe symptoms, you can also treat it so that you avoid these problems in the future.
It’s possible that your partner may have a negative reaction after they find out. Know that surprise and discomfort are normal. If the person cares for you and wants to keep seeing you, they’ll find a way to support you.
Know that surprise and discomfort are normal. If the person cares for you and wants to keep seeing you, they’ll find a way to support you.
Tips to Make Dating Better
If your doctor gives you the green light and you feel ready:
Keep your expectations in check. Even if your condition is well-managed and you feel good, keep in mind that it may cause social anxiety and other issues that can make it a challenge to date. You could have trouble with focus or flat affect (when your voice and facial expressions don’t express your emotions). You may not speak as much as other people do, which can make it tough to communicate. It can help to work through some of these issues with a therapist. You’ll find ways to feel better about yourself and your condition.
Take it slow. Stress can make schizophrenia harder to manage. That’s why it’s smart to ease into a relationship. You may want to choose low-key activities, like a meetup for coffee or a walk together, for your early dates.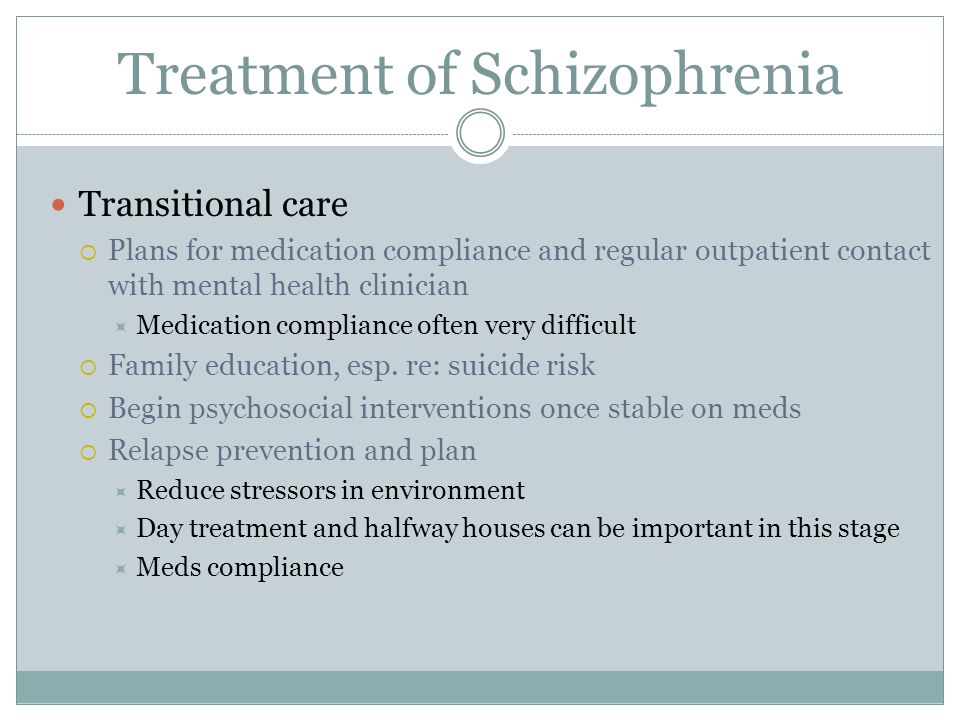 If it heats up, “It’s important to try to keep the rest of your life as regular as possible so you can stick with your treatment plan,” Dimitriu says.
If it heats up, “It’s important to try to keep the rest of your life as regular as possible so you can stick with your treatment plan,” Dimitriu says.
Know that sexual side effects are common. Your medications may impact your interest in sex or ability to get aroused or achieve orgasm. If you do have sexual side effects from medication, talk to your doctor and partner about them. It could help to switch medications.
Take a team approach. If you and your partner get serious, you may want to bring them to a doctor’s appointments or therapy sessions. “A committed partner probably knows you better than your health care provider does,” Wininger says. “They can check in with you and help you pay attention to important signs [that you need to adjust your treatment], like feeling more down than usual.” A partner’s support can be one more way to live better with schizophrenia.
how people with schizophrenia work in Russia
People diagnosed with schizophrenia told ASI how to get an education and get a job in Russia if you have a chronic psychiatric illness.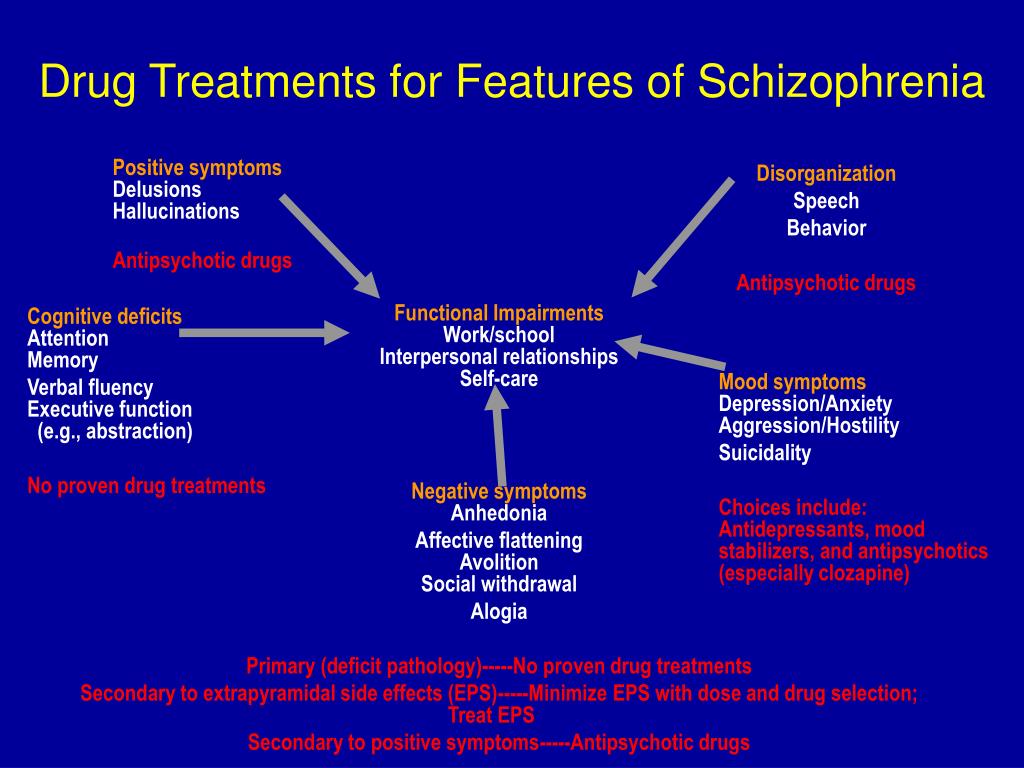
Anna Malenko Health, People with Disabilities 26.05.2020
Photo: Unsplash.comSergey (name changed), 38 years old. The diagnosis was made at the age of 23
When psychosis first occurred, I was studying at MEPhI in my last year at the Department of Applied Nuclear Physics. He left the hospital, wrote and defended his thesis. A month later, on the site "Rabota.ru" I responded to the vacancy of a system administrator in the company "Lira Keramika". I was invited for an interview and immediately got hired. I never told anyone that I had schizophrenia. After three months, he decided to quit from there - he wanted to find a better place. nine0003
I was going through a three-day probationary period at the Optima company, but then I started to get aggravated.
Walked the floors of the office, asked strangers inappropriate questions - of course, they noticed that I was not all right. I was invited to the personnel department, where a psychologist talked to me.
I had to talk about the disease. I went to the hospital, they refused me a job.
At the age of 25, I ended up at the Russian House Center for Social Initiatives, where they rehabilitate people with mental disorders, help them get an education and get a job. At the Center, I began to actively help repair computers, set up a network, and later organized computer literacy courses. He taught lessons for my own friends, other members of the Russia House. Even before the disease, while studying at MEPhI, I worked as a computer science teacher at school. I like teaching very much. nine0003
A year after my rehabilitation, Russia House offered me a job at Moscow State University (Moscow State University): to type texts in English and Russian for the department of foreign languages on a computer, to monitor the work of computers at the department, to help teachers learn new things for them programs.
After two years of work at Moscow State University, Russia House helped me get a job as a copywriter at Saatchi&Saatchi. And at home, I independently studied programming languages for writing websites. Two years later, I returned to Moscow State University as an engineer. Made a website for the Department of Foreign Languages, helped teachers work with the new system "Truth" ( system for evaluating the activities of employees and accounting for the teaching load - Approx. Ed.) .
And at home, I independently studied programming languages for writing websites. Two years later, I returned to Moscow State University as an engineer. Made a website for the Department of Foreign Languages, helped teachers work with the new system "Truth" ( system for evaluating the activities of employees and accounting for the teaching load - Approx. Ed.) .
Four years ago, a dacha neighbor offered me to administer two online stores that sell spare parts. This is my first job, where I got myself a job after rehabilitation. Already without the support of the "Russian House", but still by acquaintance. I am a full service of these stores, on one site I completely changed the design.
Schizophrenia did not prevent me from getting a job, the boss knows everything. But, I think, the disease did not become an obstacle just because my neighbor knows me well, who advised me to find a job. nine0003
I was at an interview at VTB Capital, the head of the IT department liked me, he said that they need specialists like me.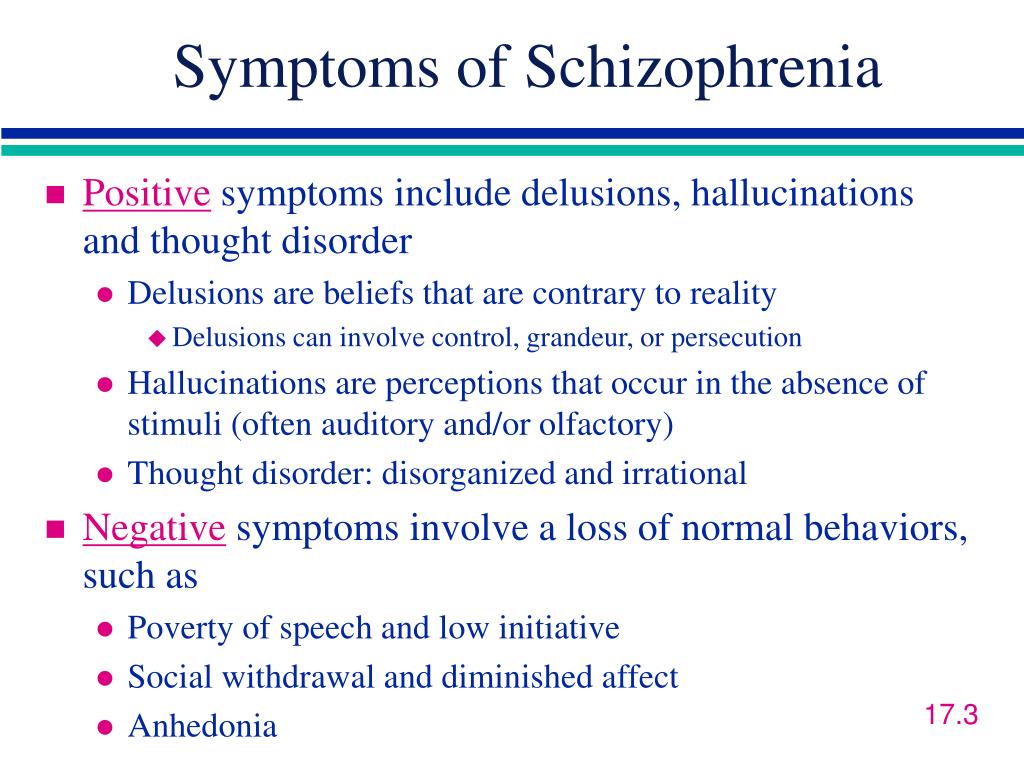 But I failed to pass the second interview in the personnel department. HR and a psychologist talked to me.
But I failed to pass the second interview in the personnel department. HR and a psychologist talked to me.
I said that I had schizophrenia, after that they completely changed their faces and said that they would call back later.
After a week of silence, I contacted them myself, they told me that the office is now moving, it may take several months, "we will contact you." But of course no one got in touch. nine0003
After VTB Capital, I had a Skype interview at the Skolkovo Foundation. When I said that I had a mental disability, I was told goodbye again.
Unsuccessful attempts at employment did not discourage my desire. I want to work for a big company. I also dream of opening my own online school for teaching programming to children in the future. And the experience of working in a large company would help me, but I understand that due to the disease it will be difficult for me to get such a job. nine0003 Photo: unsplash.com
Dmitry (name changed), 31 years old.
 I was diagnosed at the age of 18
I was diagnosed at the age of 18 I studied at the Moscow Pedagogical University at the Faculty of Sociology. I fell ill immediately after the first course. I took an academic one to be treated. After I completed another course, and then my condition worsened. I avoided social contacts, mostly sat at home, it was very difficult for me to go somewhere to find a job. My aunt was looking for a job. She got me a job as a freight forwarder for a construction company for the summer. I worked for this company for several years in a row. The disease affected my work - it was difficult for me to contact people. For me, it was an overload. nine0003
Then again, through my relatives, I got a job at the Polygraphic Resources company, in the customs department. I helped customs brokers, processed documents. I think that my colleagues saw that something was wrong with me, but as cultured people they did not say anything.
Anyway, work was a lot of stress for me. I didn't have clearly defined responsibilities that I had to fulfill. I didn't feel like a full-fledged worker. I constantly thought that I was there because of the pull, that in fact I was not really needed, there was little sense from me. A year later, everything ended with the fact that our customs post and department were closed. nine0003
I didn't feel like a full-fledged worker. I constantly thought that I was there because of the pull, that in fact I was not really needed, there was little sense from me. A year later, everything ended with the fact that our customs post and department were closed. nine0003
After that, I stayed at home for a year and a half. Then, through relatives, he also got a job in a logistics company in a warehouse. There was a heavy schedule: 12-hour shifts, including night shifts. I managed to endure only 3.5 months.
Tried to get a job through the Perspektiva organization. They had few offers for people with mental illness. But I was sent for an interview for a merchandiser position.
I was received very well. But the security service did not like that I was registered in a psycho-neurological dispensary. They asked what my disease was. He answered that I have obsessive thoughts, obsessive rituals, for example, I can wash my hands for a long time. They did not understand this and asked if I had seizures.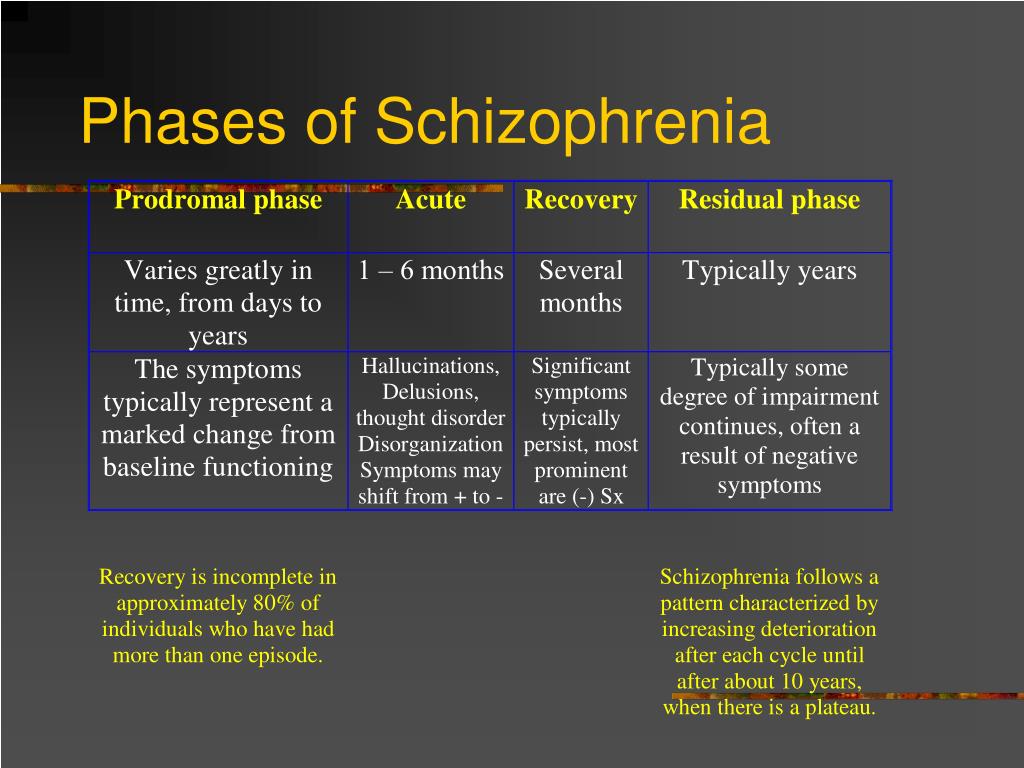 I answered that I am not an epileptic ... In general, the security service said that I should provide them with a certificate from the PND ( neuropsychiatric dispensary - Approx. ASI ) that I can work for them. I realized that it is useless.
I answered that I am not an epileptic ... In general, the security service said that I should provide them with a certificate from the PND ( neuropsychiatric dispensary - Approx. ASI ) that I can work for them. I realized that it is useless.
At the end of 2015, I ended up at the Russian House Center for Social Initiatives. In 2018, the Center helped me get a job in the interregional public organization "Equal Opportunities" as an administrator.
I really liked it there, but I always had anxiety that I wasn't doing well enough. I think I did my job, but looked dull compared to the senior students who worked as other administrators. I'm not very good with a computer, I often asked how to do something, I worked slower than the others. nine0003
Another problem is that when I work, it is difficult for me to take medicines, some of them cause drowsiness. In past jobs, I often reduced the dosage of the drug or even completely canceled it, but this led to the return of the disease.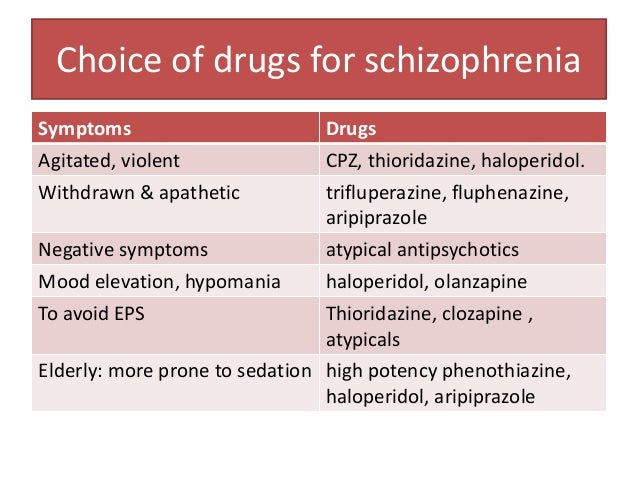
Then Russkiy Dom reported that a vacancy for a laboratory assistant had appeared at Moscow State University. When I began to collect documents for official employment, I had to provide a certificate from the psychiatric clinic. There I was told that people with mental illness cannot work in medical and educational institutions. nine0003
Last year, Russkiy Dom helped me enter the College of Technology in the correspondence department, majoring in Management Documentation and Archiving. At the end, I want to find a job where there will be no hard deadlines, I don’t have to communicate with people a lot. So that it was not very difficult and I could handle it.
Reference
Autonomous non-profit organization "Center for Social Initiatives "Russian House" is a rehabilitation center for adults with mental disorders, which operates according to the internationally recognized model of social and labor rehabilitation "Club House". You can learn more about the Club House model and its three-level program of labor rehabilitation and employment on the Russia House website. nine0003
nine0003
The program of labor rehabilitation and employment is implemented by Russia House with the financial support of the Presidential Grants Fund within the framework of the project “Together towards inclusive employment!”.
Subscribe to the ASI channel at Yandex.Zen
Dear readers, colleagues, friends of ASI.
Your support is very important to us. Together we can make the news better and more interesting.
Contribute
Tags: people with mental disorders, education and employment of people with disabilities, schizophrenia
NGOs: Autonomous non-profit organization "Center for Social Initiatives "Russian House", Regional Public Organization of People with Disabilities "Perspektiva"
Services of organizations
Autonomous non-profit organization "Center for Social Initiatives "Russian House"
Center "Russian House" is engaged in social and labor rehabilitation of adults with mental problems: instills skills for independent living, helps with employment, provides legal, psychological and domestic assistance. All services are provided free of charge. nine0003
All services are provided free of charge. nine0003
Regional Public Organization of People with Disabilities “Perspektiva”
Regional Public Organization of People with Disabilities “Perspektiva” helps adults with disabilities get a job, and children and teenagers with disabilities find a place to study, supports and develops inclusive education, conducts educational trainings, seminars, festivals, implements projects for the development of leadership qualities of adolescents with disabilities.
Recommended
Recommended
Newsletter subscription
The latest news and our best materials in your mailbox
Subscribe by email
Announcements
-
Tropical Winter Exhibition
Sun, 01.01.2023, 14:00 Moscow
-
Master classes "Creativity with a mustache"
Mon, 02.01.2023, 12:00 Online
-
Charity exhibition "Adopt a cat from a shelter"
nine0002 Thu, 05.01.2023, 14:00 Moscow -
Extra-curricular readings: meeting with Veniamin Smekhov
Thu, 01/05/2023, 19:00 Moscow
-
"Nostalgia": games on paper
Thu, 05.
 01.2023, 16:00 Moscow
01.2023, 16:00 Moscow
All events
Send news
Editor's choice
Examples of the treatment of patients with schizophrenia //Psychological newspaper
Chapter from the book of a neuropsychiatrist, psychotherapist V.V. Madorsky "Practical psychotherapy of schizophrenia":
Example one
Patient A., 23 years old. Heredity is psychopathologically burdened: the father suffered from depression, became alcoholic, hanged himself at the age of 37 (his son was 10 years old). The suicide of his father, with whom he had no emotionally significant relationship, endured calmly. Mother by nature is strong-willed, stubborn, prone to dominance, an entrepreneur. One child in the family. As a child, by nature he was passive, subordinate. He was brought up according to the mechanism of dominant hyper-custody. He studied well at school, but had few friends. After leaving school, he graduated from a university with a degree in manager (the educational institution was chosen by the mother).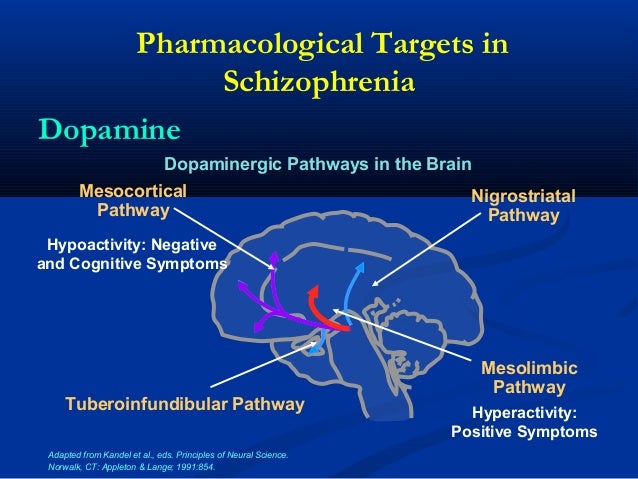 I studied averagely - having good abilities, I was lazy. Communicated in a student company, where he was on the sidelines. He lived off his mother's income. Sexual life from the age of 20, the first sexual intercourse initiated by a more experienced partner 5 years older. I didn’t build serious relationships, the connections were random, mostly at parties while intoxicated. Periodically drank, on the mechanisms of imitation smoked marijuana. During one of these episodes in the 4th year, I unexpectedly experienced an attack of strong fear, it seemed that someone terrible was hiding behind the wall, in the next room. He was afraid to go and see, the horror did not pass, even when his friends made fun of him. nine0003
I studied averagely - having good abilities, I was lazy. Communicated in a student company, where he was on the sidelines. He lived off his mother's income. Sexual life from the age of 20, the first sexual intercourse initiated by a more experienced partner 5 years older. I didn’t build serious relationships, the connections were random, mostly at parties while intoxicated. Periodically drank, on the mechanisms of imitation smoked marijuana. During one of these episodes in the 4th year, I unexpectedly experienced an attack of strong fear, it seemed that someone terrible was hiding behind the wall, in the next room. He was afraid to go and see, the horror did not pass, even when his friends made fun of him. nine0003
After that, he became anxious, began to avoid companies, fearing that the smoke of marijuana smoked by someone could cause him a similar reaction. I stopped going to the institute, fearing that someone who had recently smoked marijuana might be nearby. Insomnia appeared, fears began to be noted at home, the patient began to suspect that he was smoking marijuana and deliberately blows smoke into his apartment in order to drive him crazy, one of the neighbors, in connection with which he began to try to look into the neighbor's windows . Six months later, on the recommendation of friends, the mother turned to the Nadezhda rehabilitation center for help. nine0003
Six months later, on the recommendation of friends, the mother turned to the Nadezhda rehabilitation center for help. nine0003
Mental status on examination: Consciousness is formally clear, fully oriented. Closed, anxious, does not fully disclose his experiences. In the psychiatrist's office, he sniffs around, trying to determine if there is a marijuana smell. He claims that his neighbor, having learned about his poor health, is trying to deliberately drive him crazy by smoking marijuana and blowing smoke into his apartment, thereby seeking revenge for the fact that the patient was listening to loud music. Thinking with elements of fragmentation, concentration of attention is significantly reduced, intelligence is preserved, memory is reduced for psychotraumatic events. There is no criticism. In the neurological status - without features. EPI is a borderline variant of the schizophrenic pathopsychological symptom complex. The diagnosis was made: Schizophrenia, paroxysmal-progressive type of course, manifest affective-delusional attack (according to ICD-10 - schizoaffective disorder, depressive type F 25.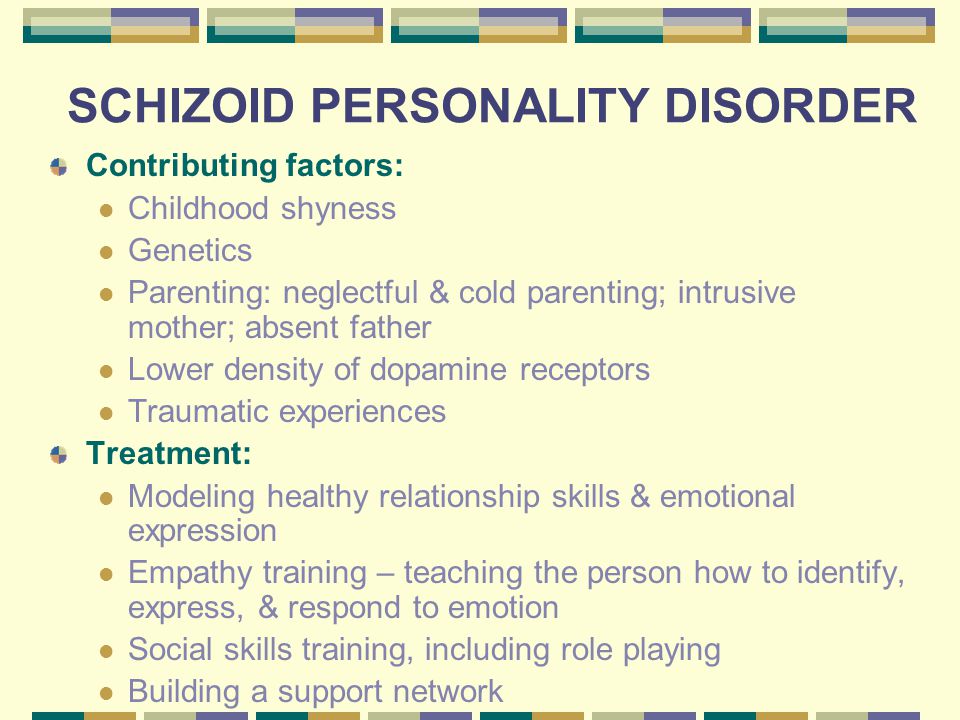 18). nine0003
18). nine0003
Work with the patient began with a family meeting. The aunt, the cousin of the patient's mother, was also invited to the meeting, on whose initiative the family came to the center - it was important from the very beginning to break the symbiotic relationship between the patient and the mother. The family meeting was organized before the start of psychopharmacotherapy, because it is at this moment of the crisis, against the background of the patient's disordered behavior, that the family is most ready for change. The patient and relatives were informed about the nature of the disease and methods of its treatment. During a family meeting, using the information received from the aunt, the pathological nature of family relationships was clarified. nine0003
Clear rules of conduct for the patient and responsibility for their violation in the form of an increased amount of homework were established. During the conversation, it was clarified that the main thing in the family is the mother, and the patient is obliged to strictly follow all her instructions.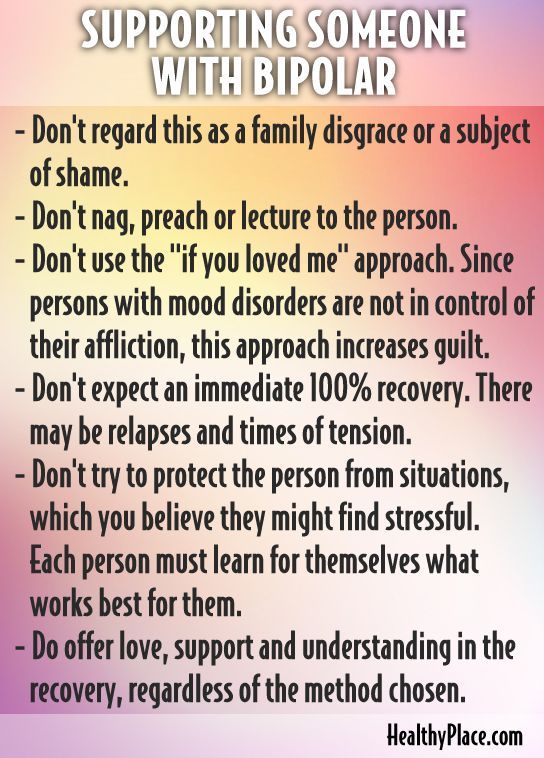 In case of refusal of this, the mother had to hospitalize the patient in a psychiatric hospital. Thus, conditions were built that counteract the patient's sliding into the habitual niche of schizophrenic communication with the refusal to determine intentions, actions and feelings. nine0003
In case of refusal of this, the mother had to hospitalize the patient in a psychiatric hospital. Thus, conditions were built that counteract the patient's sliding into the habitual niche of schizophrenic communication with the refusal to determine intentions, actions and feelings. nine0003
The patient was started on pharmacological treatment at home... The patient's mental state began to gradually improve, he was emotionally compensated, his behavior became orderly, his thinking became more harmonious, criticism of his condition began to form. The patient did not violate the rules established for him, although sometimes he verbally expressed dissatisfaction with their severity. After 2 weeks the dose of drugs was reduced and individual psychotherapy was started with the patient 2 times a week. The work began with cognitive training in the visualization of visual images, followed by their sketching. Due to the rapid exhaustion of the patient's psyche, the first sessions lasted no more than 30 minutes, but subsequently, as the state was further compensated, the duration of the session was 1 hour.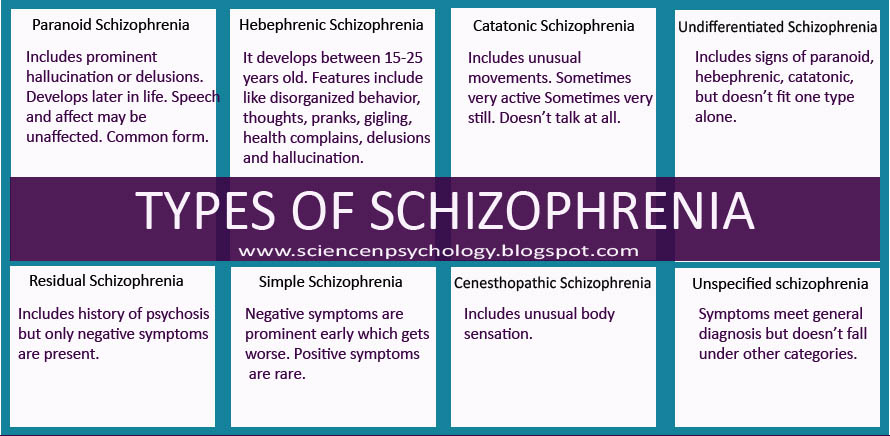 nine0003
nine0003
In the experienced images, a pronounced anxiety was projected: the meadow was flooded with water all the time, the stream was thin and disappeared in the sands, instead of one mountain it presented two frightening magnitudes, which for a long time could not climb. In the image of the edge of the forest, the patient was pursued by ferocious predators, and the house presented was old and falling apart, beyond repair.
The patient was recommended to imagine the image of the Scout "in order to learn to understand all this." The scout was cowardly, inept, for some reason dragging an outdated Maxim machine gun on his back, tearing under his weight, and having no idea where he was going and why. At the next session, the scout was assigned to the cadets of the reconnaissance school, where experienced mentors taught him the mind, and in the subsequent scout coped with the matter much more professionally. Then came the time of the Defender, the Knight, who won the knightly tournament and won back the beautiful girl from the evil dragon .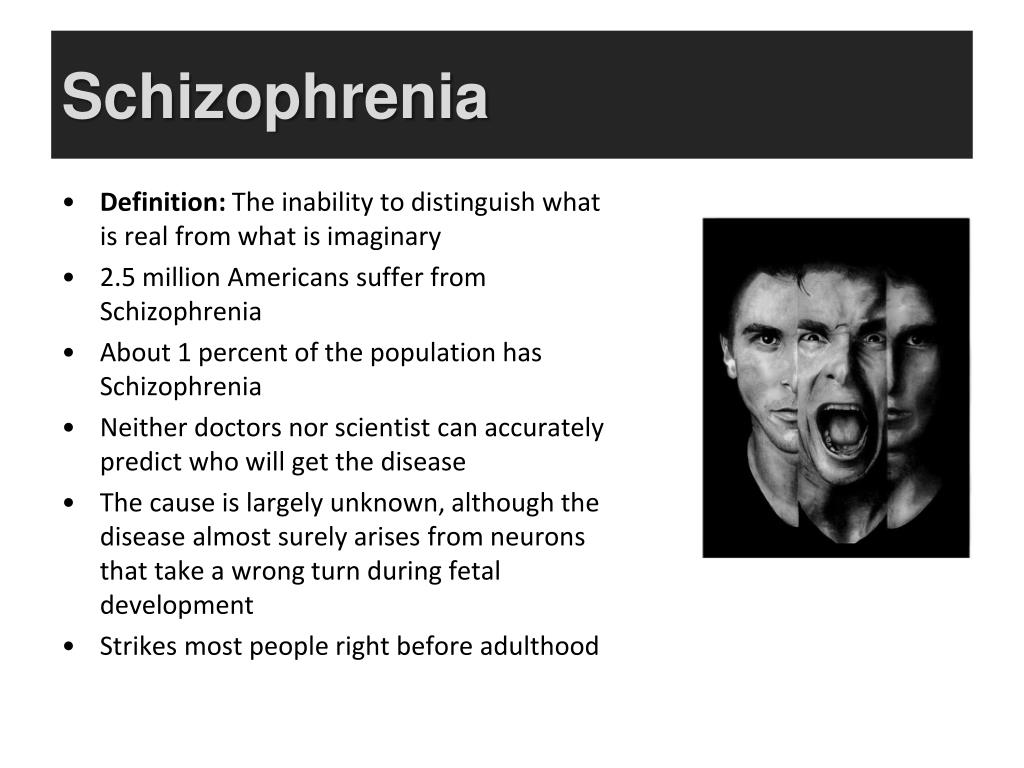 .. However, the dragon that appeared was extremely vicious and stupid (he himself was exposed to the blow of the knight), as, however, the liberated princess, who poutedly did not say a word to the knight gratitude, and then, when he went to drink in a tavern, biting her elbows in anger at a potential groom who did not pay attention to her. After presenting this image, it was explained to the patient that all the characters presented were images of parts of his own subconscious. Together we managed to figure out that the Dragon is his fears, the stupid puffed up young lady is his idea of women who, as it seemed to the patient, are just waiting to offend him, and the brave but inconsistent Knight, who does not receive anything from his heroism, is his the image of a man. This important occupation opened the way to work with female images and their interaction with male ones. nine0003
.. However, the dragon that appeared was extremely vicious and stupid (he himself was exposed to the blow of the knight), as, however, the liberated princess, who poutedly did not say a word to the knight gratitude, and then, when he went to drink in a tavern, biting her elbows in anger at a potential groom who did not pay attention to her. After presenting this image, it was explained to the patient that all the characters presented were images of parts of his own subconscious. Together we managed to figure out that the Dragon is his fears, the stupid puffed up young lady is his idea of women who, as it seemed to the patient, are just waiting to offend him, and the brave but inconsistent Knight, who does not receive anything from his heroism, is his the image of a man. This important occupation opened the way to work with female images and their interaction with male ones. nine0003
Against the background of this work, the patient's condition improved ... As these topics were gradually worked out, cognitive-behavioral classes were also connected, in which the patient learned to cope with his affects, communicate, organize his day correctly, etc.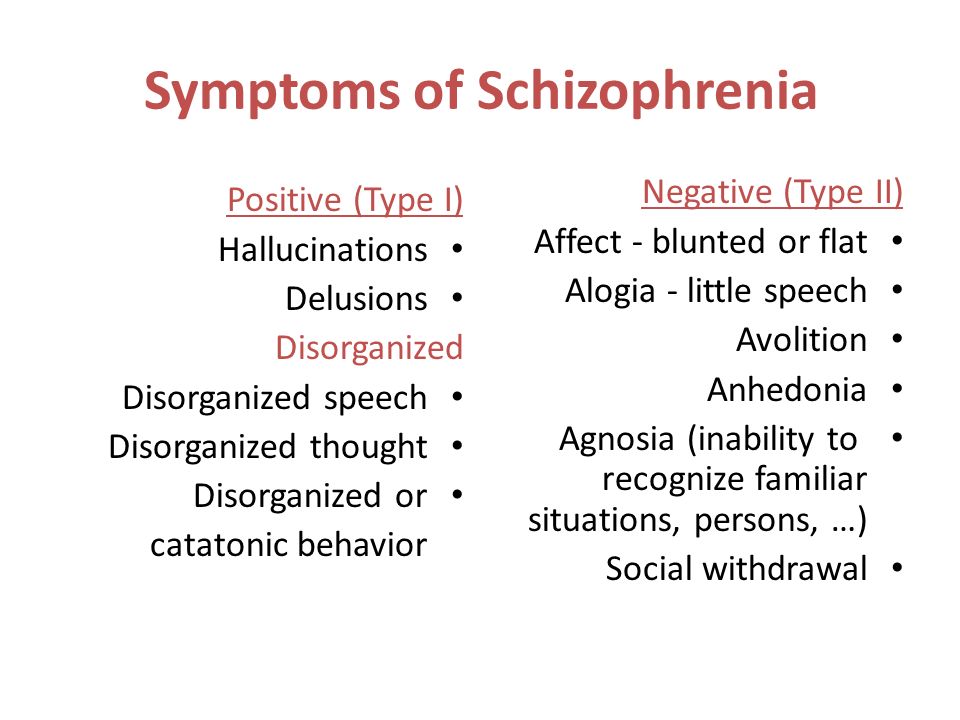 His condition was gradually compensated, and through six months after starting work, he went to study.
His condition was gradually compensated, and through six months after starting work, he went to study.
At the beginning of training, the condition worsened: anxiety, weakness increased sharply, the patient began to skip classes. This was corrected by changing the doses of drugs, visualizing and sketching the image of a frightening erupting and then calming volcano, and a behavioral task, when for every day when the patient did not go to school, he had to wash the entire staircase in the entrance. The condition stabilized again, the patient successfully passed the session, the circle of contacts expanded. Against the background of discussing the relationship between visualized male and female images, the patient began to meet with girls. nine0003
Separately, work was carried out with the patient's mother, as a result of which her anxiety significantly decreased, she became prettier and found a man for herself. The son began to go on his dates, and the mother went on hers. A year and a half after the start of work, the patient and his girlfriend went to live in an apartment, getting a job as a waiter. His mental state was stable. Taking medication in maintenance dosages ... continued for another six months.
A year and a half after the start of work, the patient and his girlfriend went to live in an apartment, getting a job as a waiter. His mental state was stable. Taking medication in maintenance dosages ... continued for another six months.
Follow-up after 5 years: the patient successfully works as a personnel manager, is married, has good family relations, he has 2 daughters who do not show signs of mental disorders. nine0003
Second example
Patient A. 19 years old. Data for the presence of mental illness in relatives could not be identified. Mother is soft, anxious by nature, works as an accountant. The father is unsure of himself, often gets sick - there are frequent exacerbations of stomach ulcers and sciatica; works as a turner at the same enterprise as his mother. Proband is the youngest child in the family. The 5-year-old brother is distinguished by emphatically sthenic forms of response, graduated from a military school, serves as an officer in the Strategic Missile Forces, communicates little with members of the parental family, treats his parents with emphatic contempt, reproaching them for weakness and gentleness.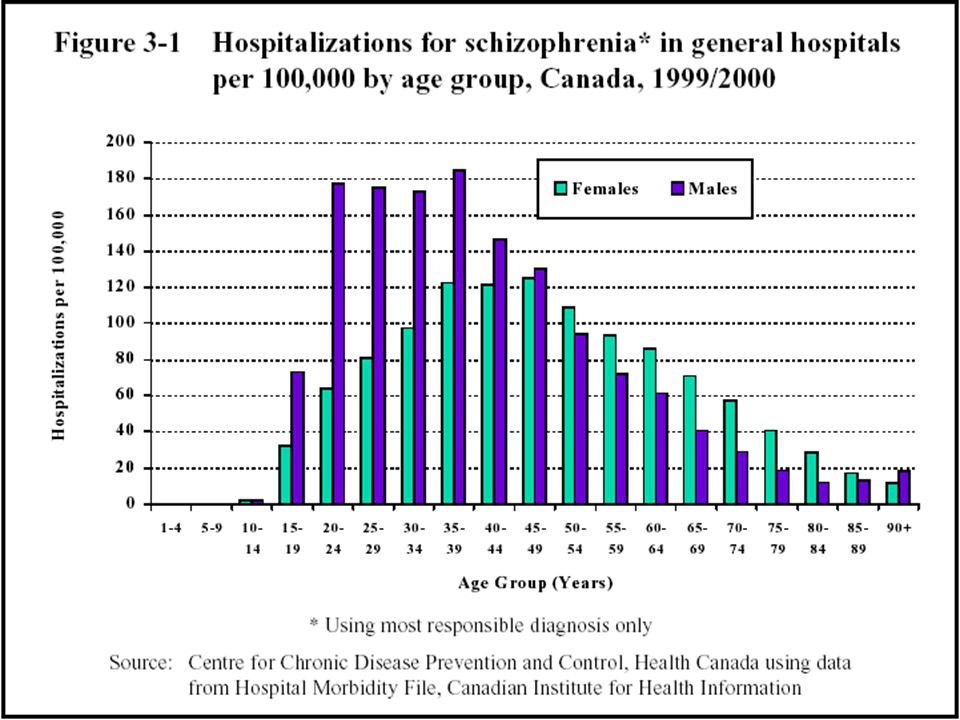 From childhood, the patient was distinguished by traits of vulnerability, resentment, and uncertainty. She preferred to play herself, she was very worried if she saw dead or suffering animals. The suffering of people did not cause such feelings in her, she was indifferent to this. Since childhood, she often suffered from headaches, for which she regularly received treatment from a neurologist with a diagnosis of vegetative-vascular dystonia. At school she was closed, she had only one girlfriend, but she studied well. She didn’t get acquainted with the boys - in her words, she was not interested in it. I never worried about the narrow circle of communication, it was not comfortable for her to communicate. Relations with parents were good and warm. After graduating from school, on the recommendation of her mother, she entered a financial institution. She finished her first year with flying colours, but contacts with other students were extremely formal, she was known as a "nerd" among her peers.
From childhood, the patient was distinguished by traits of vulnerability, resentment, and uncertainty. She preferred to play herself, she was very worried if she saw dead or suffering animals. The suffering of people did not cause such feelings in her, she was indifferent to this. Since childhood, she often suffered from headaches, for which she regularly received treatment from a neurologist with a diagnosis of vegetative-vascular dystonia. At school she was closed, she had only one girlfriend, but she studied well. She didn’t get acquainted with the boys - in her words, she was not interested in it. I never worried about the narrow circle of communication, it was not comfortable for her to communicate. Relations with parents were good and warm. After graduating from school, on the recommendation of her mother, she entered a financial institution. She finished her first year with flying colours, but contacts with other students were extremely formal, she was known as a "nerd" among her peers. I sat on the Internet for a long time, where I read on one of the sites that in order to attract good luck, you need to perform certain actions: get up from a certain foot, step over one tile in the bathroom, etc. I got carried away with this, she had whole morning and evening rituals to attract good luck, in which she began to involve her parents under the pretext of taking care of them. When parents tried to refuse to perform rituals, the patient's anxiety and headaches sharply increased, for which she reproached her parents. nine0003
I sat on the Internet for a long time, where I read on one of the sites that in order to attract good luck, you need to perform certain actions: get up from a certain foot, step over one tile in the bathroom, etc. I got carried away with this, she had whole morning and evening rituals to attract good luck, in which she began to involve her parents under the pretext of taking care of them. When parents tried to refuse to perform rituals, the patient's anxiety and headaches sharply increased, for which she reproached her parents. nine0003
Because of the rituals, she began to be late for school more and more often, and as a result, she completely stopped attending the university, motivating this by having more important things to do: performing rituals to attract good luck and health and clear the karma of her and her loved ones. She refused to visit a doctor, considering herself healthy, but simply busy with extremely important matters. Relations with parents deteriorated significantly, scandals arose more and more often in the house, to which she reacted with resentment, general weakness and headache. In this regard, the doctors turned to the Nadezhda Center for help. nine0003
In this regard, the doctors turned to the Nadezhda Center for help. nine0003
Upon admission, she complains of weakness and headaches, but believes that these are all natural difficulties in her work to attract good luck and purify karma, and considers herself perfectly healthy. In mental status: consciousness is clear, fully oriented.
Emotionally monotone. She speaks in an emphatically calm voice, claims that the meaning of her life is to attract good luck and cleanse the karma of others. This is very important, and therefore they must endure the inconvenience associated with it, for example, provide for it financially, citing the practice of monastics in this regard as an example. However, she does not consider herself religious, she says that “everything is wrong” in the church. Her philosophical constructions are a mixture of different currents, from which the patient chose what suited her. When you try to argue with her arguments, she falls silent, becomes indifferent, saying that she is sure of her rightness, but she is not interested in proving something. A conversation in a friendly, interested tone about her philosophical research can be maintained for quite a long time. Obviously does not express delusional ideas, the presence of deceptions of perception denies. Intelligence, memory preserved, criticism is extremely formal. In neurological and somatic status - without features. nine0003
A conversation in a friendly, interested tone about her philosophical research can be maintained for quite a long time. Obviously does not express delusional ideas, the presence of deceptions of perception denies. Intelligence, memory preserved, criticism is extremely formal. In neurological and somatic status - without features. nine0003
Assistance to the patient began with a family meeting. At first, only one mother could come to a meeting with a psychotherapist with a patient, but the doctor had to explain that the case was complex and that it was necessary to collect as much information as possible. The meeting was postponed for a week so that the father and brother could also come (struggle for structure and initiative). During the first meeting, all those present were asked to tell what they see as problems. Since the purpose of the first meeting is to intensify the family crisis, the first word was given to the older brother who was most opposed to the parental family. nine0003
The patient was heard last. It was clarified that, in fact, the family was led by her symptoms by the youngest daughter, who threatened to worsen her condition if her demands were not met. Further, all family members were asked to formulate what should happen in order for everything to become good (clarification of relations and intentions). The first word this time was given to the daughter, and in the form of a Socratic dialogue it was made clear to her that if her parents fulfilled all her requirements for conducting rituals, then there would be nothing to eat in the house. The daughter was also asked if she could be happy if the rest of the family was unhappy, and after her answer no, the parents and brother also said that they in the family currently feel unhappy. When questioning other family members, the psychotherapist drew everyone's attention to the fact that, by and large, everyone wanted the same thing: respect for each other, love, understanding, joy. The psychotherapist emphasized that different paths can lead to this, but none of these paths can be successfully passed in the absence of a clear, clear hierarchy in the family.
It was clarified that, in fact, the family was led by her symptoms by the youngest daughter, who threatened to worsen her condition if her demands were not met. Further, all family members were asked to formulate what should happen in order for everything to become good (clarification of relations and intentions). The first word this time was given to the daughter, and in the form of a Socratic dialogue it was made clear to her that if her parents fulfilled all her requirements for conducting rituals, then there would be nothing to eat in the house. The daughter was also asked if she could be happy if the rest of the family was unhappy, and after her answer no, the parents and brother also said that they in the family currently feel unhappy. When questioning other family members, the psychotherapist drew everyone's attention to the fact that, by and large, everyone wanted the same thing: respect for each other, love, understanding, joy. The psychotherapist emphasized that different paths can lead to this, but none of these paths can be successfully passed in the absence of a clear, clear hierarchy in the family.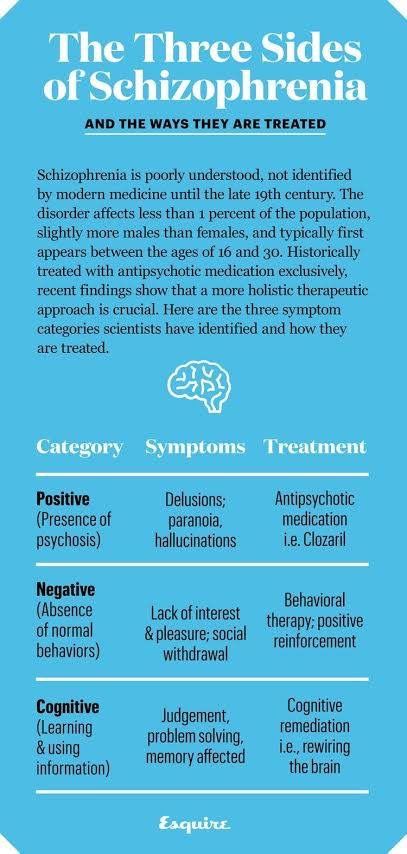 The best head of the family, the doctor emphasized, is the one under whose wise rule all family members satisfy all their needs. The question was raised: who could be the head of the family (the establishment of a hierarchy)? nine0003
The best head of the family, the doctor emphasized, is the one under whose wise rule all family members satisfy all their needs. The question was raised: who could be the head of the family (the establishment of a hierarchy)? nine0003
This position was first offered to the patient (a paradoxical prescription aimed at destroying the unconscious game that maintained the pathological family hierarchy). At first she was delighted, but then, when it turned out that at the same time she had to think about how to earn money, build a family budget, etc., she categorically refused. The mother was asked to become the head of the family; everyone promised to comply with her demands. The patient at first resisted, but then she was faced with a choice: you can command everything yourself and be responsible for it, you can obey the head of the family, you can go live on your own. nine0003
Next, it is time to clarify family laws. It was established that family members should either study, or work, or, if they cannot do this for health reasons, then be treated.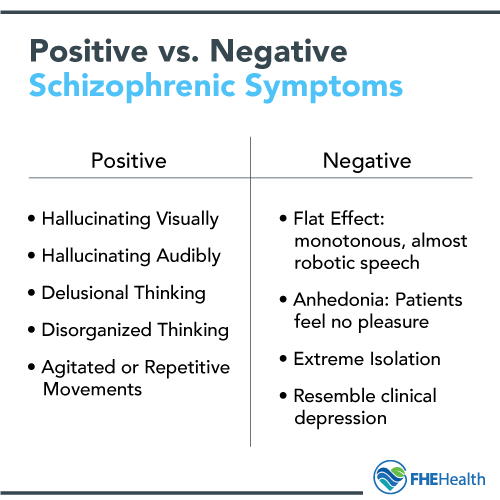 In order to objectively understand what is happening, the patient underwent an experimental psychological study. The EPI revealed a borderline variant of the schizophrenic pathopsychological symptom complex. The psychologist who tested the patient was invited as a “black messenger” to the next family meeting, where she explained in detail the essence of the problems to the patient and her family members. Using the criteria for diagnosing schizophrenia from ICD-10, together with family members, the diagnosis was clarified: low-progressive schizophrenia with paranoid syndrome (according to ICD-10, paranoid schizophrenia, F22.82). nine0003
In order to objectively understand what is happening, the patient underwent an experimental psychological study. The EPI revealed a borderline variant of the schizophrenic pathopsychological symptom complex. The psychologist who tested the patient was invited as a “black messenger” to the next family meeting, where she explained in detail the essence of the problems to the patient and her family members. Using the criteria for diagnosing schizophrenia from ICD-10, together with family members, the diagnosis was clarified: low-progressive schizophrenia with paranoid syndrome (according to ICD-10, paranoid schizophrenia, F22.82). nine0003
Psychoeducational work was started, it was explained that without treatment, schizophrenia leads to dementia and various severe disorders of behavior, thinking and perception, but at the current level of medical knowledge it is quite possible to cope with it. To do this, it is necessary to ensure regular medication, psychotherapy to teach the patient to cope with her problems on her own, stable consistent relationships in the family, and social and labor readaptation. The patient was explained that the treatment can be carried out at home, following all the instructions of the parents, or in a hospital, where orderlies will seek obedience, and it was described in detail which components of the treatment solve which problems. nine0003
The patient was explained that the treatment can be carried out at home, following all the instructions of the parents, or in a hospital, where orderlies will seek obedience, and it was described in detail which components of the treatment solve which problems. nine0003
All this helped to destroy the domestic myth about the incurability of schizophrenia. The home care option was chosen…
The parents prescribed a clear daily routine for the patient, devoting a lot of space to housework there. An individual psychotherapy was started with the girl, during which the psychotherapist, having shown interest in her practicing magic, promised to teach her how to do it professionally, emphasizing that all experienced magicians can work with visual images in a trance. From this, classes of projective hypnotherapy were started, followed by sketching of images (therapy with creative self-expression). At first, the work was carried out with landscape images, and then the psychotherapist suggested being in a trance as a sorceress.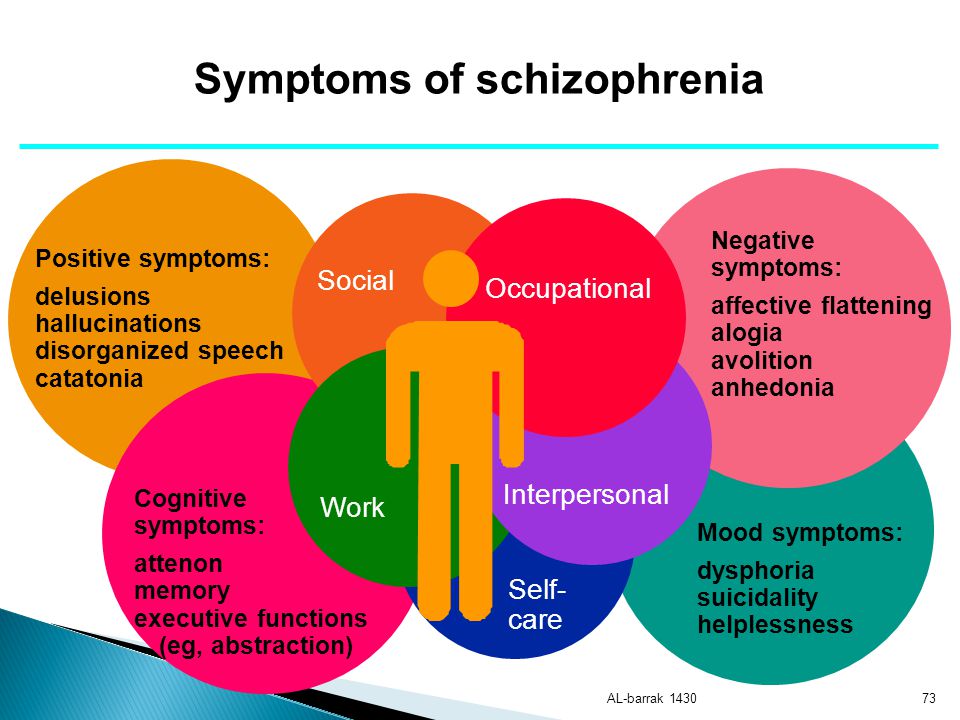 This proposal caused considerable embarrassment in the patient, but the psychotherapist was persistent, arguing that if she was seriously going to practice magic, then it was absolutely necessary to be able to be, even in a trance, a sorceress. It turned out to be difficult to imagine the image - it was a girl who was unsure of herself, collecting medicinal herbs and not owning anything particularly magical. In the process of interpreting and discussing this and other images, it became clear that the girl had an unconscious ban on aggressive or feminine behavior, and the libido was unconsciously directed towards self-destruction of the personality. In view of this, work began with aggressive images, and at first with male ones (Warrior on the battlefield, Lion, Defender, Executioner), to which female images were later added (Witch, Amazon, Geisha), and the interaction between them was also studied in trance. As the initiating images were worked out, the girl became more and more interested in real relationships, and the topic of performing magical rituals gradually became deactivated - the schizophrenic initiation of the mythological-ritual complex "death-rebirth" began to change to the initiation of the development of a unique, successful, happy woman.
This proposal caused considerable embarrassment in the patient, but the psychotherapist was persistent, arguing that if she was seriously going to practice magic, then it was absolutely necessary to be able to be, even in a trance, a sorceress. It turned out to be difficult to imagine the image - it was a girl who was unsure of herself, collecting medicinal herbs and not owning anything particularly magical. In the process of interpreting and discussing this and other images, it became clear that the girl had an unconscious ban on aggressive or feminine behavior, and the libido was unconsciously directed towards self-destruction of the personality. In view of this, work began with aggressive images, and at first with male ones (Warrior on the battlefield, Lion, Defender, Executioner), to which female images were later added (Witch, Amazon, Geisha), and the interaction between them was also studied in trance. As the initiating images were worked out, the girl became more and more interested in real relationships, and the topic of performing magical rituals gradually became deactivated - the schizophrenic initiation of the mythological-ritual complex "death-rebirth" began to change to the initiation of the development of a unique, successful, happy woman. Approximately six months after the start of work, the psychotherapist began to give tasks for the real establishment of relationships with young people. The patient began preparations for continuing her studies. nine0003
Approximately six months after the start of work, the psychotherapist began to give tasks for the real establishment of relationships with young people. The patient began preparations for continuing her studies. nine0003
Against this background, conflicts between the parents began to become more pronounced, based on the dissatisfaction of the patient's father with the dictates of her mother, and the mother's dissatisfaction with the lack of will and irresponsibility of the father. The attention in the monthly sessions of family therapy was shifted to this. The psychotherapist suggested handing over the reins of the family to the father, with which, to the great surprise of the mother, he began to cope successfully. Even more surprising for my mother was that she began to like not to solve problems herself, but to shift them onto her husband's shoulders. To strengthen the position of the father in the family, several classes were held with him in a cognitive-behavioral manner. The parents were instructed to learn how to better relax together, and the patient was asked if she was ready to help them with the accurate fulfillment of her duties.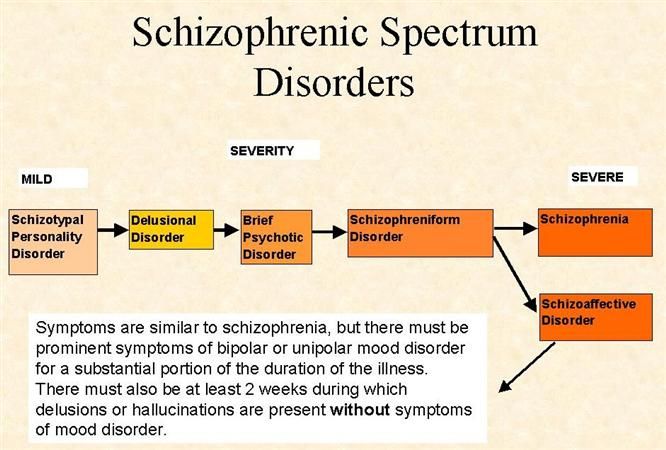 The patient responded with great enthusiasm, she emphasized that she could never figure out how to make her parents happy. nine0003
The patient responded with great enthusiasm, she emphasized that she could never figure out how to make her parents happy. nine0003
Also, the family was given a directive injunction to soon worsen the patient's condition, and then successfully solve the problems arising from this. This was very useful when later, not 10 months later, when the patient went to study, her anxiety and headaches recurred. The family and the patient were not frightened, but, calmly increasing the doses of drugs and intensifying psychotherapeutic work, they successfully coped with the problems, continuing to study.
It was explained to the girl: she is already an adult and should be able to regularly go to school or work, regardless of how she feels, except for especially serious conditions, such as acute poisoning, high temperature or pressure. In these cases, she should contact the local doctor and take a sick leave. If there is no sick leave, then she must get to the place of study or work and serve there a full day, trying to cope with the duties assigned to her as best as she can.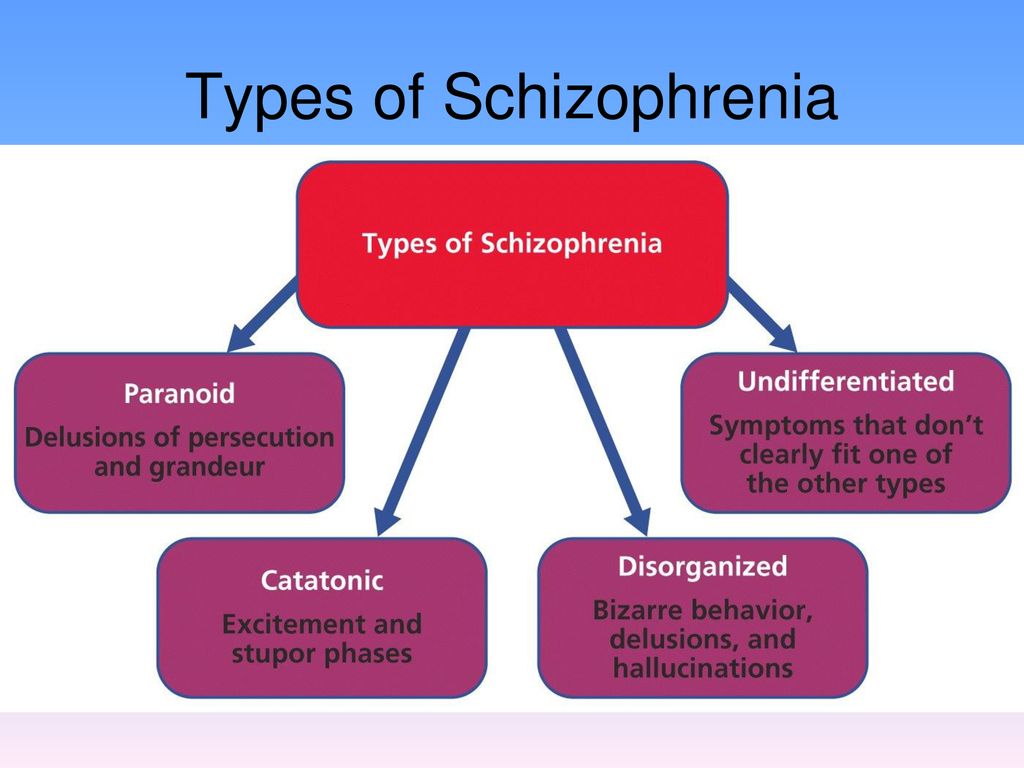 (It is clear that such a requirement should not be applied to all patients. But with a hystero-hypochondriac syndrome with symptoms of hospitalism, which at that moment determined the severity of the patient's condition, this recommendation is often very effective). nine0003
(It is clear that such a requirement should not be applied to all patients. But with a hystero-hypochondriac syndrome with symptoms of hospitalism, which at that moment determined the severity of the patient's condition, this recommendation is often very effective). nine0003
The rehabilitation work continued, and the emphasis in it shifted more and more from psychiatric to psychological issues ... One of her fellow practitioners became interested in the patient, and this first relationship in her life caused her many experiences that she had to constantly work through with a psychotherapist. In addition to cognitive-behavioral approaches, the continuation of initiatory therapy played an important role (images of "The Little Mermaid", "Disenchantment of Femininity", "Aphrodite", "Geisha"). Of great importance were the symbolic "battles" in trance, carried out to free the patient from her complexes and prohibitions ("Kill the Dragon", "Kill the Villain", "Battle with the Great Spider", "Battle with Koshchey"). And yet, the first relationship in her life ended unsuccessfully, together with a psychotherapist, she had to “lick her wounds” and learn, using past experience, to build new ones. nine0003
And yet, the first relationship in her life ended unsuccessfully, together with a psychotherapist, she had to “lick her wounds” and learn, using past experience, to build new ones. nine0003
After going through a series of superficial relationships, after 2 years from the start of work, the girl, on her own initiative, met a guy she liked. They decided to live together, and here again they had to work with their parents. By helping them deal with their fears, the therapist helped them give the patient a much-needed blessing to start an independent life. Regular individual therapy and medication continued for another six months (2.5 years in total). After that, the patient and I saw each other once a month, and once every 3 months, and then - once every six months, the entire parental family gathered. This went on for another year. After that, the patient occasionally (1-2 times a year) comes in for advice on how to optimize relationships in the family and at work. She does not show any signs of mental illness. nine0003
nine0003
Example three
Patient R., 43 years old. He applied at the insistence of his relatives, in whose care he has been for the last year and a half. Anamnesis: heredity is psychopathologically burdened by father's alcoholism. When the patient was 18 years old, his father drowned at the age of 42. The proband endured this calmly - he did not have significant relationships with his father. By nature, the proband was kind, hardworking, but vulnerable. He studied well, had many friends, but relations with girls did not work out - he did not know how to be strong, assertive, he was very worried about female tantrums. After graduating from college, he worked as an engineer. Was in good standing, promoted. At 29married for years, the relationship began at the initiative of a woman to whom he seemed like a promising man. However, the relationship did not work out. Scandals constantly arose in the family, connected with the fact that, from the point of view of his wife, the proband earned little, devoting too much time to science.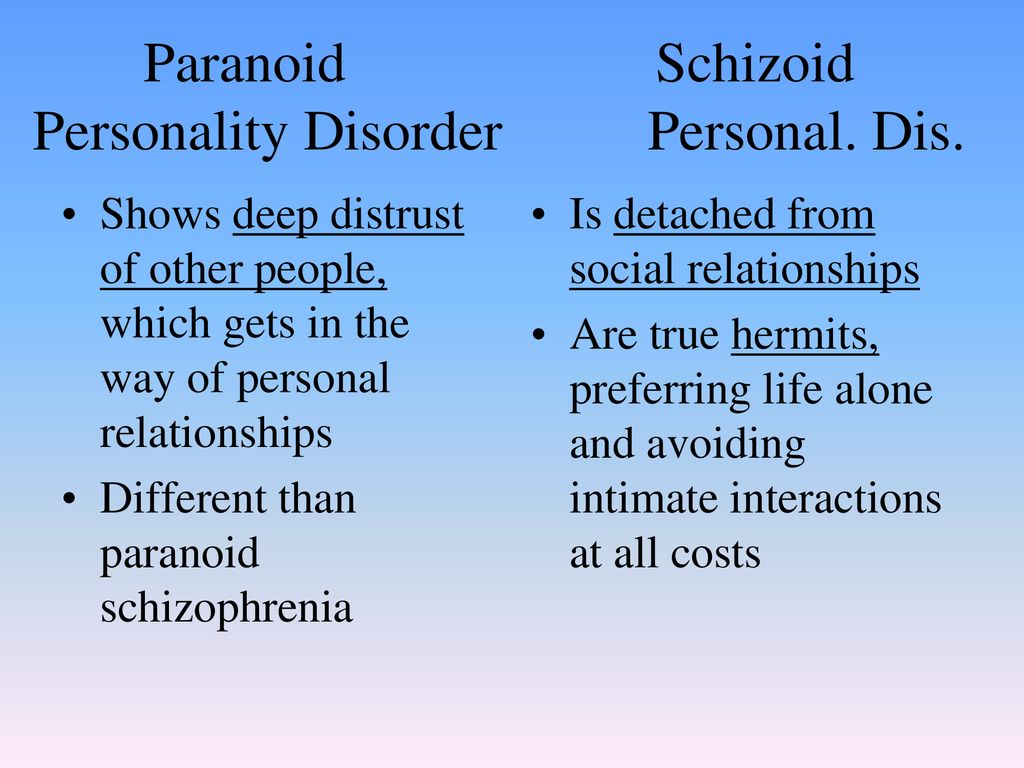 When he was 38 years old, his wife left, taking her beloved son with her. The patient plunged into depression, began to drink alcohol. At the initiative of his mother, he turned to the district psychiatrist, received antidepressants. The patient's condition improved, the patient started to work, but after 3 months his night's sleep was disturbed, he became aggressive, quarreled with his mother, threatened physical violence against his ex-wife because she allegedly put poison in his food so that he "did not stand up". In this regard, he was hospitalized in a psychiatric hospital, where he received treatment for paranoid schizophrenia with an episodic course for six months. Was discharged in good condition, went to work. After the attack, he became more withdrawn, more often sat at home, there were fewer friends. But he got the job done. At the initiative of his mother, he began to meet with another woman, quite quickly, on her initiative, he got married, a child was born. However, the patient stopped taking the medicines prescribed for him, and when he was 40 years old, he developed another attack of schizophrenia - he plunged into depression, claimed that he had no arms, legs, lower jaw, and because of this he could not walk on work, talk and eat.
When he was 38 years old, his wife left, taking her beloved son with her. The patient plunged into depression, began to drink alcohol. At the initiative of his mother, he turned to the district psychiatrist, received antidepressants. The patient's condition improved, the patient started to work, but after 3 months his night's sleep was disturbed, he became aggressive, quarreled with his mother, threatened physical violence against his ex-wife because she allegedly put poison in his food so that he "did not stand up". In this regard, he was hospitalized in a psychiatric hospital, where he received treatment for paranoid schizophrenia with an episodic course for six months. Was discharged in good condition, went to work. After the attack, he became more withdrawn, more often sat at home, there were fewer friends. But he got the job done. At the initiative of his mother, he began to meet with another woman, quite quickly, on her initiative, he got married, a child was born. However, the patient stopped taking the medicines prescribed for him, and when he was 40 years old, he developed another attack of schizophrenia - he plunged into depression, claimed that he had no arms, legs, lower jaw, and because of this he could not walk on work, talk and eat.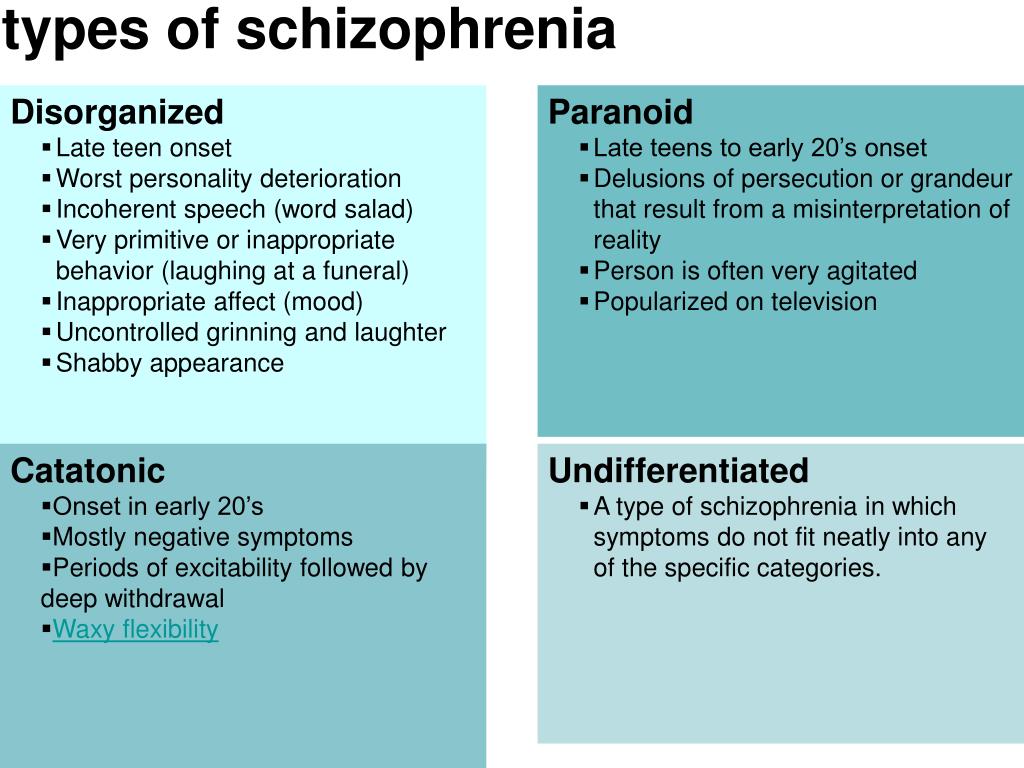 The wife and child, maintaining good relations with him, left him and went to her parents. He walked around with a scarf wrapped around his neck and lower part of his face, trying to hide from others the absence of his throat and lower jaw. For six months he was treated in a hospital, then at the local psychiatrist. The improvement was insignificant, the disability of the second group was issued. nine0003
The wife and child, maintaining good relations with him, left him and went to her parents. He walked around with a scarf wrapped around his neck and lower part of his face, trying to hide from others the absence of his throat and lower jaw. For six months he was treated in a hospital, then at the local psychiatrist. The improvement was insignificant, the disability of the second group was issued. nine0003
Mental status at admission: formally clear consciousness. Fully oriented. Closed, inactive, immersed in their experiences. Answers questions briefly, formally, after a long latent pause, not always in terms of the given. Claims that he has no throat and lower jaw, which prevents him from speaking and eating. Thinking with severe fragmentation, which makes it difficult to understand in detail the nature of the patient's experiences. Depressive. The concentration of attention is reduced. The memory is preserved, there is no criticism. In somatic and neurological status - no pathology. In the EPI data - a schizophrenic pathological symptom complex between moderate and severe severity. nine0003
In the EPI data - a schizophrenic pathological symptom complex between moderate and severe severity. nine0003
The treatment began with a family meeting, which was mainly devoted to psychoeducational work. The psychotherapist insisted that not only the patient and his mother, but also his niece and her husband, who knew about the situation and periodically tried to help, come to her. The diagnosis of paranoid schizophrenia with an episodic type of course was confirmed (according to ICD-9 - schizophrenia, paroxysmal-progressive type of course, prolonged affective-delusional attack with a pronounced change in personality). The patient and his family members were explained what schizophrenia is and what are the methods of its treatment. Separately, the nature of schizophrenic communication was described. Noting the patient's inability to name his feelings, the doctor suggested that he determine them using an emotion chart. With great difficulty, the patient was able to determine that he had melancholy, anxiety and uncertainty. “So you feel like you feel like you really didn’t have a throat and lower jaw?” - clarified the psychotherapist, and when the patient confirmed this, the doctor explained to him and family members that, using delusional metaphors, the patient sought to express his feelings when he was unable to do it otherwise, and then he began to believe in his metaphors. The patient and family members were advised to tell others about their feelings at least 2 times a day and stop talking in metaphors, learning to name all their experiences, clearly defining them as feelings, sensations, sounds, visual images, smells, taste, etc. For example When the patient started talking again about body defects, the relatives had to stop him and offer to say the same thing, but not with the help of metaphors, but correctly naming his feelings and sensations. In addition, the family hierarchy was clearly defined (the head of the family at this stage is the mother of the patient, the patient must clearly follow her instructions, and in case of his refusal to fulfill the necessary help, the niece and her husband should have helped restore order), the patient's obligations to maintain order and repair at home, exercise.
“So you feel like you feel like you really didn’t have a throat and lower jaw?” - clarified the psychotherapist, and when the patient confirmed this, the doctor explained to him and family members that, using delusional metaphors, the patient sought to express his feelings when he was unable to do it otherwise, and then he began to believe in his metaphors. The patient and family members were advised to tell others about their feelings at least 2 times a day and stop talking in metaphors, learning to name all their experiences, clearly defining them as feelings, sensations, sounds, visual images, smells, taste, etc. For example When the patient started talking again about body defects, the relatives had to stop him and offer to say the same thing, but not with the help of metaphors, but correctly naming his feelings and sensations. In addition, the family hierarchy was clearly defined (the head of the family at this stage is the mother of the patient, the patient must clearly follow her instructions, and in case of his refusal to fulfill the necessary help, the niece and her husband should have helped restore order), the patient's obligations to maintain order and repair at home, exercise.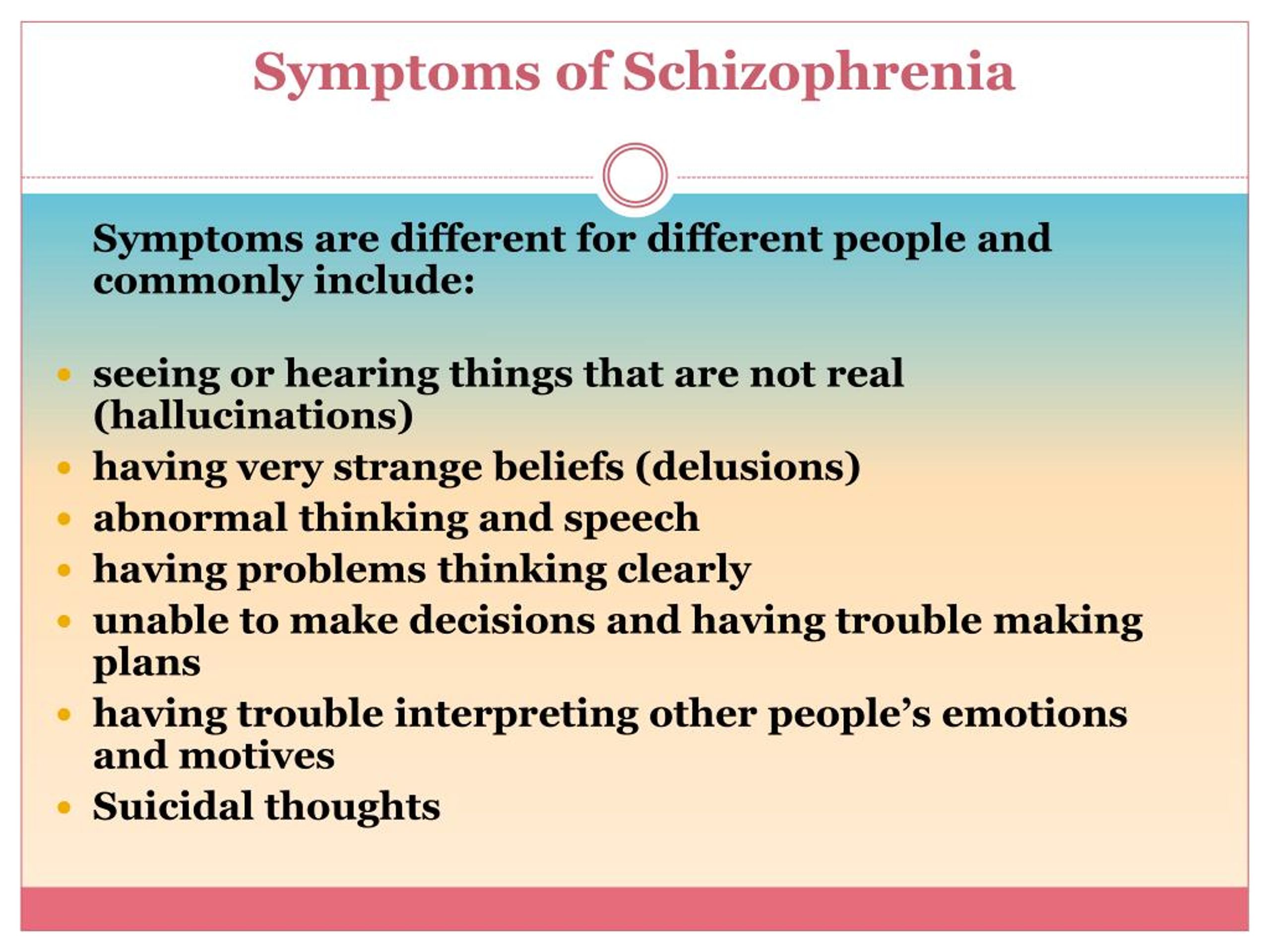 Pharmacological treatment was prescribed... Cognitive training in the visualization of visual images was started with the patient. At first, it proceeded with difficulties due to the pronounced fragmentation of thinking, but later, as the work continued, the visualization of images began to be easier for the patient. nine0003
Pharmacological treatment was prescribed... Cognitive training in the visualization of visual images was started with the patient. At first, it proceeded with difficulties due to the pronounced fragmentation of thinking, but later, as the work continued, the visualization of images began to be easier for the patient. nine0003
The condition began to gradually improve, after 2 months of treatment the patient became more active, thinking became noticeably more productive. He began to perceive his body adequately, actively engaged in work on repairing the house, however, he had to face pronounced problems with finding a job, which was also associated with the mother’s fears about the possible deterioration of his condition during intensive work and her conviction that a good job you will not find (of course, the repressed fears of the mother herself played a significant role here). The issue of finding a job was not resolved until after 4 months the patient's condition worsened. It was quickly stopped by the correction of drugs, and from that moment the mother, taught by bitter experience, began to actively demand from the patient to look for work.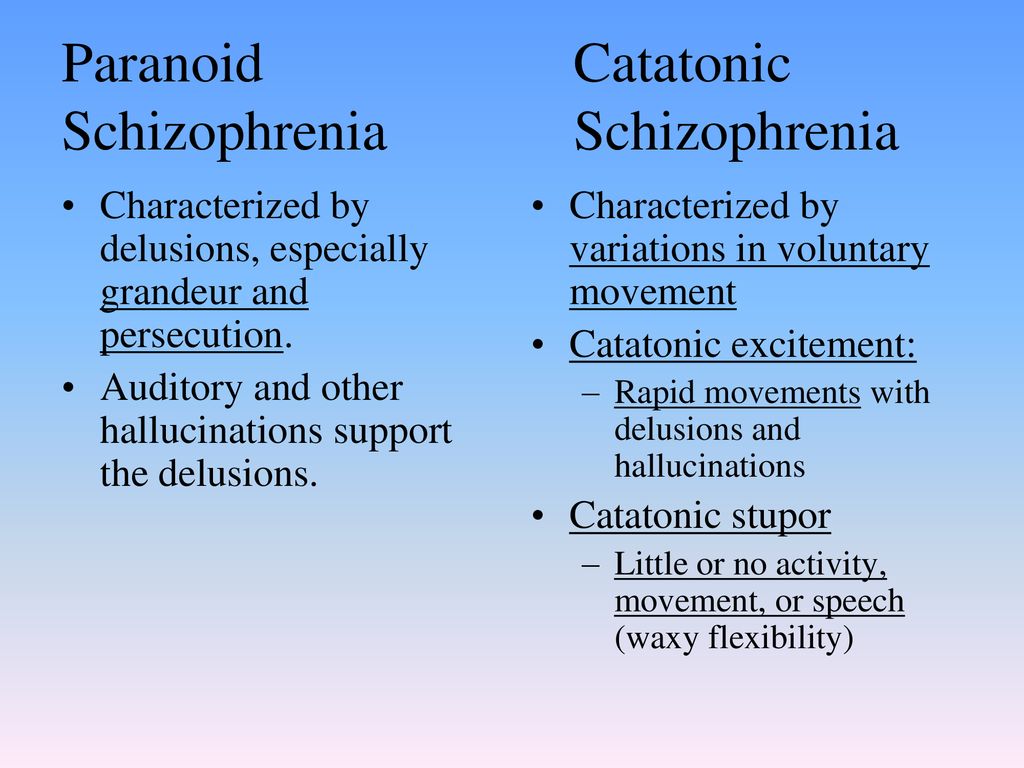 nine0003
nine0003
Psychotherapeutic work at this stage was carried out 2 times a month. For the first 30 minutes, a family conversation was held, to which the patient’s niece periodically joined (in family work, symbiotic “twos” must be turned into “triples”), and the second 30 minutes we discussed his problems with the patient and worked with images that were then sketched at home. An important role was played by images in which the patient played a dominant role in the relationship, at first symbolically (Climbing the mountain), and then more and more directly (Lion, Bull, Gardener, Breadwinner, King). Gradually, the patient found a job, but a month later he quit because of non-payment of wages. Subsequent attempts were more successful, and gradually the patient reached the position of chief specialist of the company in a year and a half. Convinced by the changes for the better, the second wife and child returned to him. In the process of preparing for the family reunion, the patient's representation of himself in female images (Witch, Amazon.