Common side effects of lithium
Lithium: medicine to control mood disorders such as mania and bipolar disorder
1. About lithium
Lithium is a type of medicine known as a mood stabiliser.
It's used to treat mood disorders such as:
- mania (feeling highly excited, overactive or distracted)
- hypo-mania (similar to mania, but less severe)
- regular periods of depression, where treatment with other medicines has not worked
- bipolar disorder, where your mood changes between feeling very high (mania) and very low (depression)
Lithium can also help reduce aggressive or self-harming behaviour.
It comes as regular tablets or slow-release tablets (lithium carbonate). It also comes as a liquid that you swallow (lithium citrate).
Lithium is available on prescription.
2. Key facts
- The most common side effects of lithium are feeling or being sick, diarrhoea, a dry mouth and a metallic taste in the mouth.
- Your doctor will carry out regular blood tests to check how much lithium is in your blood. The results will be recorded in your lithium record book.
- Lithium carbonate is available as regular tablets and modified release (brand names include Priadel, Camcolit and Liskonium).
- Lithium citrate comes as a liquid and common brands include Priadel and Li-Liquid.
3. Who can and cannot take lithium
Lithium can be taken by adults and children over the age of 12 years.
Lithium may not be suitable for some people. Tell your doctor if:
- you have ever had an allergic reaction to lithium or other medicines in the past
- you have heart disease
- you have severe kidney problems
- have an underactive thyroid gland (hypothyroidism) that is not being treated
- you have low levels of sodium in your body – this can happen if you're dehydrated or if you're on a low-sodium (low-salt) diet
- you have Addison's disease, a rare disorder of the adrenal glands
- you have, or someone in your family has, a rare condition called Brugada syndrome – a condition that affects your heart
- you need to have surgery in hospital
- you are trying to get pregnant, are pregnant or breastfeeding
Before prescribing lithium, your doctor will do some blood tests to check your kidney and thyroid are OK.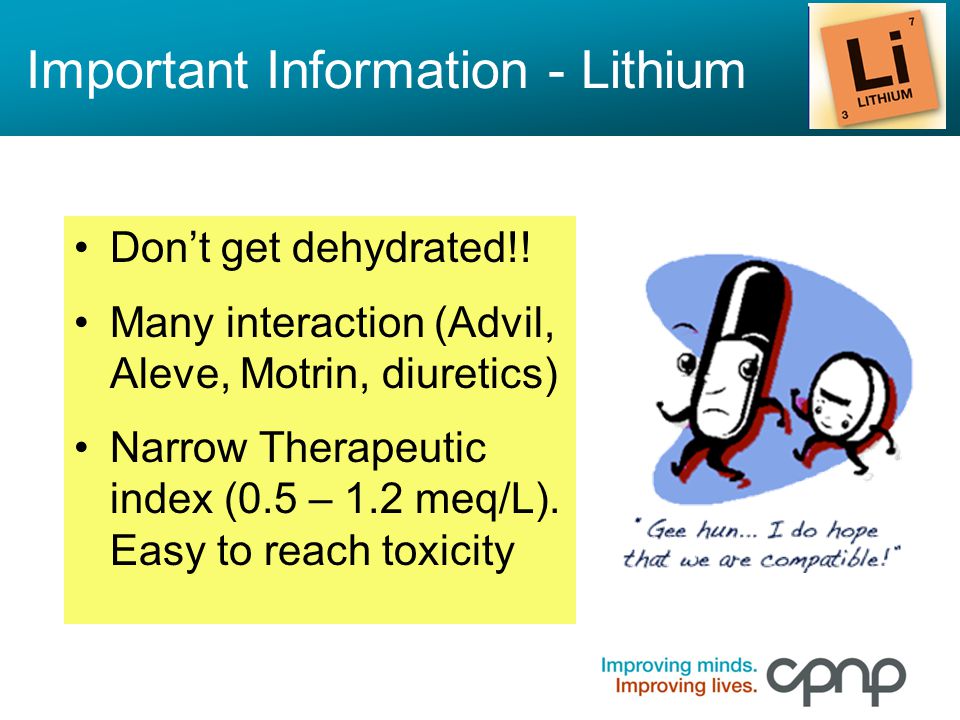 The doctor will also check your weight (and check this throughout your treatment).
The doctor will also check your weight (and check this throughout your treatment).
If you have a heart condition, the doctor may also do a test that measures the electrical activity of your heart (electrocardiogram).
4. How and when to take lithium
It's important to take lithium as recommended by your doctor.
There are 2 different types of lithium – lithium carbonate and lithium citrate. It's important not to change to a different type unless your doctor has recommended it. This is because different types are absorbed differently in the body.
Lithium carbonate comes as regular tablets and slow-release tablets – where the medicine is released slowly over time.
Lithium citrate comes as a liquid. This is usually only prescribed for people who have trouble swallowing tablets .
Doses vary from person to person. Your starting dose will depend on your age, what you're being treated for and the type of lithium your doctor recommends.
Your starting dose will depend on your age, what you're being treated for and the type of lithium your doctor recommends.
If you have kidney problems your doctor will monitor the level of lithium in your blood even more closely and change your dose if necessary.
You will usually take your lithium once a day, at night. This is because when you have your regular blood test, you need to have it 12 hours after taking your medicine. You can choose when you take your lithium – just try to keep to the same time every day.
How to take it
Swallow tablets whole with a drink of water or juice. Do not chew them. You can take lithium with or without food.
If you're taking liquid, use the plastic syringe or spoon that comes with your medicine to measure the correct dose. If you do not have one, ask your pharmacist. Do not use a kitchen teaspoon as you will not get the right amount.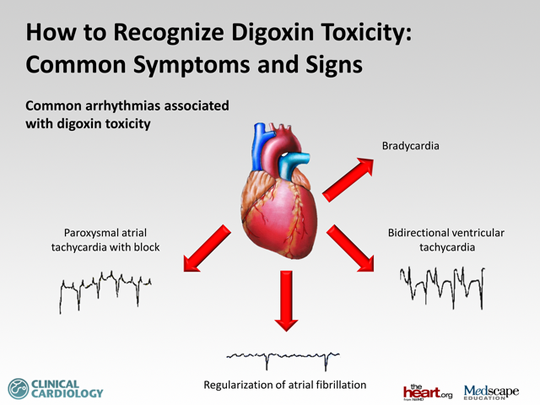
Information about your lithium treatment
When you start taking lithium, you will get a lithium treatment pack (usually a purple folder or book) with a record booklet. You need to show your record booklet every time you see your doctor, go to hospital, or collect your prescription.
When you go to the doctor for blood tests, you or your doctor will write in the record booklet:
- your dose of lithium
- your lithium blood levels
- any other blood test results
- your weight
The treatment pack also has a lithium alert card. You'll need to carry this card with you all the time. It tells healthcare professionals that you're taking lithium. This can be useful for them to know in an emergency.
Tell your doctor or pharmacist if you've lost your treatment pack or did not get one.
Will my dose go up or down?
When you start your treatment you'll need to have a blood test every week to make sure the level of lithium in your blood is not too high or too low. Your doctor may change your dose depending on the results of your blood test.
Once the doctor is happy you'll have a blood test every 3 to 6 months to check the level remains steady.
Once you find a dose that suits you, it will usually stay the same – unless your condition changes, or your doctor prescribes another medicine that may interfere with lithium.
Important
Do not stop taking lithium suddenly or change your dose without speaking to your doctor first. It's important you keep taking it, even if you feel better. If you stop taking it suddenly you could become unwell again very quickly.
What if I'm ill while taking lithium?
Infections and illnesses like colds and flu can make you dehydrated, this can affect the level of lithium in your blood.
Talk to your doctor or pharmacist if you:
- have an illness that causes severe diarrhoea, vomiting, a high temperature or sweating
- have a urinary tract infection (UTI)
- are not eating and drinking much
What if I forget to take it?
If you usually take:
- tablets or slow-release tablets – if it's less than 6 hours since you were supposed to take your lithium, take it as soon as you remember. If it is more than 6 hours, just skip the missed dose and take your next one at the usual time
- liquid – if you forget to take a dose, just skip the missed dose and take your next one at the usual time
Never take 2 doses at the same time. Never take an extra dose to make up for a forgotten one.
If you forget doses often, it may help to set an alarm to remind you. You could also ask your pharmacist for advice on other ways to help you remember to take your medicine.
You could also ask your pharmacist for advice on other ways to help you remember to take your medicine.
What if I take too much?
Immediate action required: Call 999 or go to A&E if:
- you take too much lithium, even if you do not feel any different
This is because very high amounts of lithium can cause problems with your kidneys and other organs. It can cause symptoms such as:
- feeling or being sick
- problems with your eyesight (blurred vision)
- increased need to pee, lack of control over pee or poo
- feeling faint, lightheaded or sleepy
- confusion and blackouts
- shaking or muscle weakness, muscle twitches, jerks or spasms affecting the face, tongue, eyes or neck
If you need to go to A&E, take the lithium packet or the leaflet inside it, plus any remaining medicine, with you.
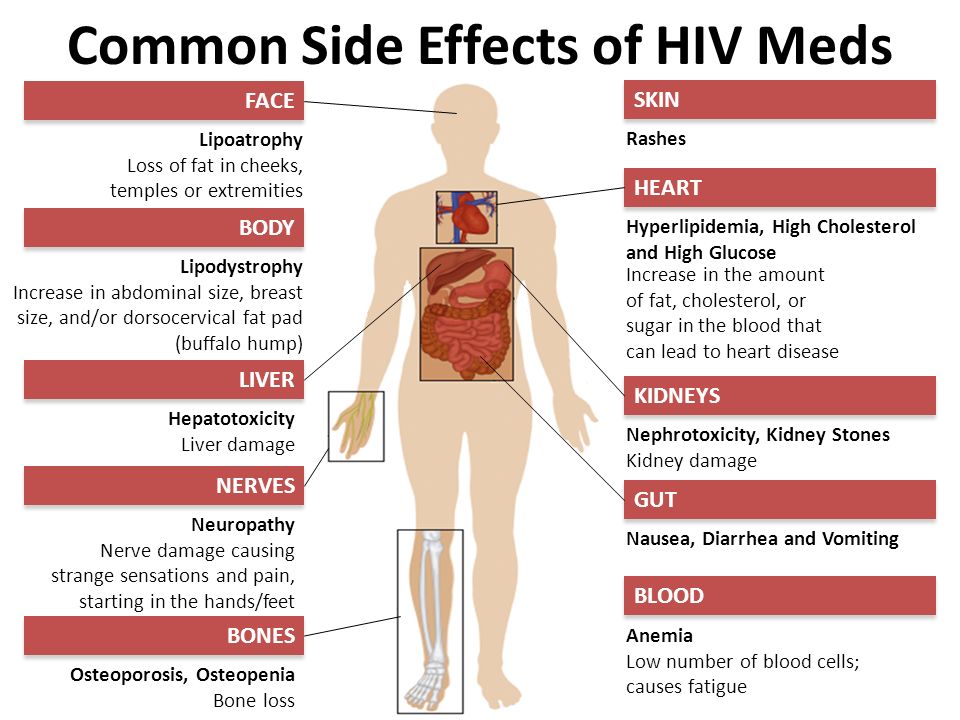
5. Side effects
If you're on the right dose and the level of lithium in your blood is right, you may not have any problems taking this medicine.
However, some people find lithium slows down their thinking or makes them feel a bit "numb".
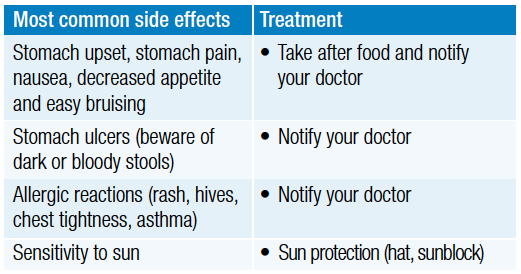
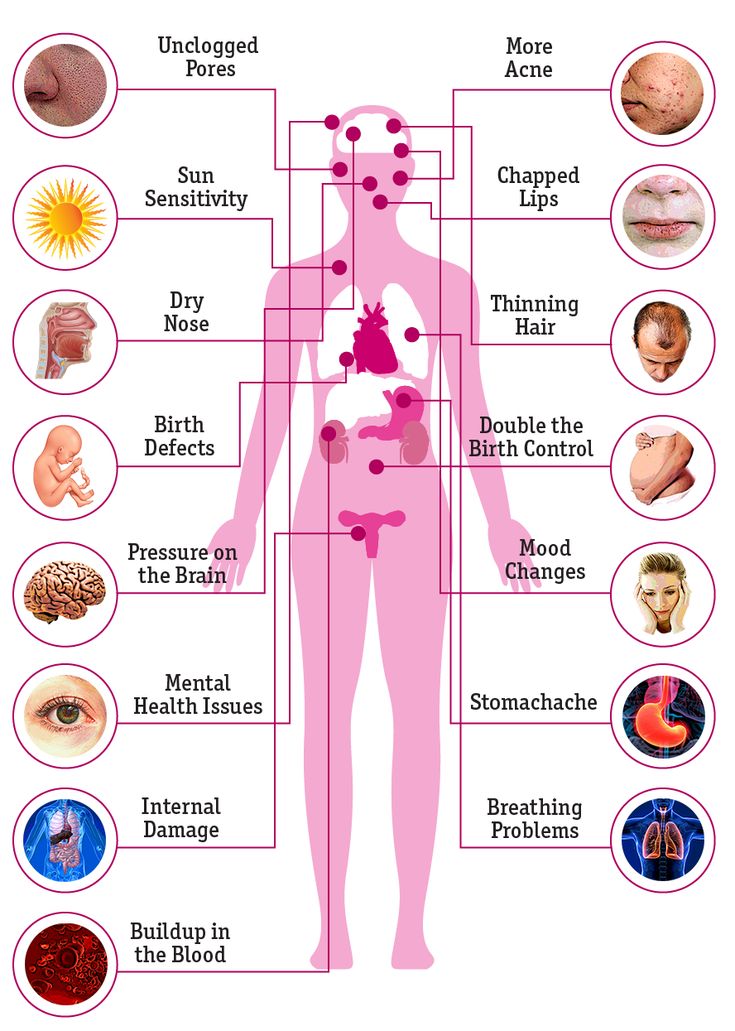
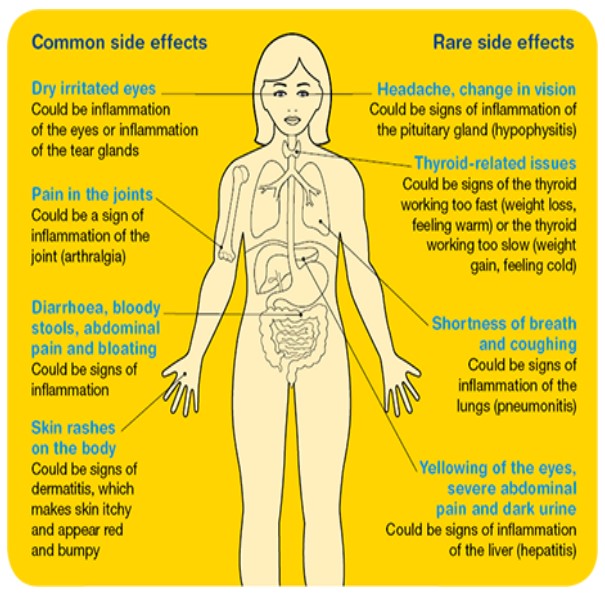
Common side effects
These are usually mild and go away by themselves. They are more likely to happen when you start taking lithium.
Keep taking the medicine but talk to your doctor or pharmacist if any of the following side effects get worse or do not go away after a few days:
- feeling sick (nausea)
- diarrhoea
- a dry mouth and/or a metallic taste in the mouth
- feeling thirsty and needing to drink more and pee more than usual
- slight shaking of the hands (mild tremor)
- feeling tired or sleepy
- weight gain (this is likely to be very gradual)
Serious side effects:
The level of lithium in your blood is checked regularly. But rarely, you may get side effects because there's too much lithium in your blood.
But rarely, you may get side effects because there's too much lithium in your blood.
Immediate action required: Call 999 or go to A&E now if:
You have 1 or more of these symptoms:
- loss of appetite, feeling or being sick (vomiting)
- problems with your eyesight (blurred vision)
- feeling very thirsty, needing to pee more than normal, and lack of control over pee or poo
- feeling lightheaded or drowsy
- confusion and blackouts
- shaking, muscle weakness, muscle twitches, jerks or spasms affecting the face, tongue, eyes or neck
- difficulty speaking
These are signs of lithium toxicity. Lithium toxicity is an emergency. Stop taking lithium straight away.
How to avoid high lithium levels in your blood
Make sure that you go for the blood tests arranged by your doctor.
It's important not to reduce your salt intake suddenly. Talk to your doctor if you want to reduce the amount of salt in your diet.
Drink plenty of fluids, especially if you are doing intense exercise or in hot weather when you will sweat more.
Drinking alcohol causes your body to lose water. It's best not to drink too much as it's likely to make you dehydrated, especially in hot weather when you will sweat more.
Always tell any doctor or pharmacist that you are taking lithium before you take any new medicines.
Serious allergic reaction:
In rare cases, lithium may cause a serious allergic reaction (anaphylaxis).
Immediate action required: Call 999 or go to A&E if:
- you get a skin rash that may include itchy, red, swollen, blistered or peeling skin
- you're wheezing
- you get tightness in the chest or throat
- you have trouble breathing or talking
- your mouth, face, lips, tongue or throat start swelling
You could be having a serious allergic reaction and may need immediate treatment in hospital.
These are not all the side effects of lithium. For a full list, see the leaflet inside your medicine packet.
You can report any suspected side effect to the UK safety scheme.
6. How to cope with side effects
What to do about:
- feeling or being sick – take lithium with or after a meal or snack. It may also help if you do not eat rich or spicy food. If you are being sick, take sips of water to avoid dehydration.
- diarrhoea – drink plenty of fluids to avoid dehydration. Signs of dehydration include peeing less than usual or having dark, strong-smelling pee. Do not take any other medicines to treat diarrhoea without speaking to a pharmacist or doctor.
- a dry mouth and/or a metallic taste in the mouth – try sugar-free gum or sweets, or sipping cold drinks.
 If this does not help, talk to your pharmacist or doctor. Try not to have drinks with a lot of calories in as this might also mean you put on weight.
If this does not help, talk to your pharmacist or doctor. Try not to have drinks with a lot of calories in as this might also mean you put on weight. - slight shaking of the hands (mild tremor) – talk to your doctor if this is bothering you or does not go away after a few days. These symptoms can be a sign that the dose is too high for you. Your doctor may change your dose or recommend taking your medicine at a different time of day.
- feeling tired or sleepy – as your body gets used to lithium, these side effects should wear off. If these symptoms do not get better within a week or two, your doctor may either reduce your dose or increase it more slowly. If that does not work you may need to switch to a different medicine.
- weight gain – try to eat well without increasing your portion sizes so you do not gain too much weight. Regular exercise will help to keep your weight stable and help you feel better.
7. Pregnancy and breastfeeding
Lithium and pregnancy
Lithium is not usually recommended in pregnancy, especially during the first 12 weeks (first trimester) where the risk of problems to the baby is highest. However, you may need to take lithium during pregnancy to remain well. Your doctor may advise you to take it in pregnancy if the benefits of the medicine outweigh the risks.
If you become pregnant while taking lithium, speak to your doctor. It could be dangerous to you and your unborn baby if you stop taking it suddenly. Do not stop taking it or make any change to your dose unless your doctor tells you to.
Talk to your doctor before taking this medicine if you plan to get pregnant, or think you may be pregnant. Your doctor can explain the risks and the benefits and will help you decide which treatment is best for you and your baby.
Lithium and breastfeeding
If your doctor or health visitor says your baby is healthy, you can take lithium while breastfeeding.
Lithium passes into breast milk in small amounts. However, it has been linked with side effects in very few breastfed babies.
It's important to continue taking lithium to keep you well. Breastfeeding will also benefit both you and your baby.
If you notice that your baby is not feeding as well as usual, or seems unusually sleepy, or if you have any other concerns about your baby, talk to your health visitor or doctor as soon as possible.
Non-urgent advice: Talk to your doctor if you:
- are trying to get pregnant
- are already pregnant
- would like to breastfeed
For more information about how lithium can affect you and your baby during pregnancy, read this leaflet on the Best Use of Medicines in Pregnancy (BUMPS) website.
8.
 Cautions with other medicines
Cautions with other medicines This are some medicines that may interfere with how lithium works and this can affect the levels of lithium in your blood.
Check with your doctor or pharmacist if you're taking (or before you start taking):
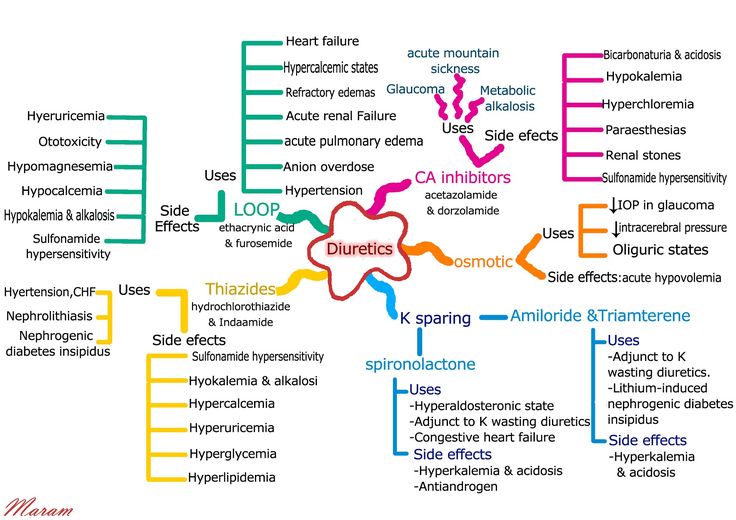
- tablets that make you pee (diuretics) such as furosemide or bendroflumethiazide
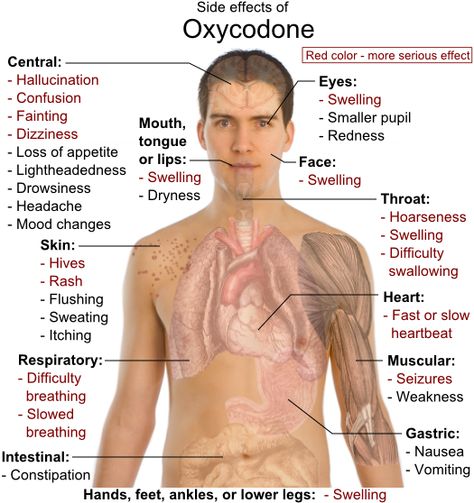
- non-steroidal anti-inflammatory drugs (NSAIDs) – used for pain relief and swelling such as aspirin, ibuprofen, celecoxib or diclofenac
- medicines used for heart problems or high blood pressure such as enalapril, lisinopril or ramipril (ACE inhibitors)
- some medicines used for depression such as fluvoxamine, paroxetine or fluoxetine
- antibiotics such as oxytetracycline, metronidazole, co-trimoxazole, trimethoprim
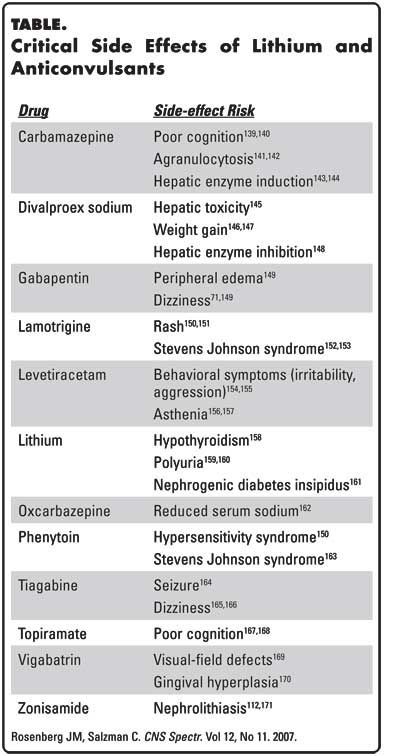
- medicines for epilepsy such as carbamazepine or phenytoin
These are not all the medicines that can affect the way lithium works. Always check with your doctor before you start or stop taking any medicine.
Always check with your doctor before you start or stop taking any medicine.
Mixing lithium with herbal remedies or supplements
It's not possible to say whether complementary medicines and herbal supplements are safe to take with lithium.
They're not tested in the same way as pharmacy and prescription medicines. They're generally not tested for the effect they have on other medicines.
Important
For safety, tell your doctor or pharmacist if you're taking any other medicines, including herbal remedies, vitamins or supplements.
9. Common questions
How does lithium work?Lithium is a metal. Tiny amounts of lithium are found naturally in rocks, and in our food and bodies.
We do not really know exactly how lithium works for mental health conditions, though we do know it's very effective.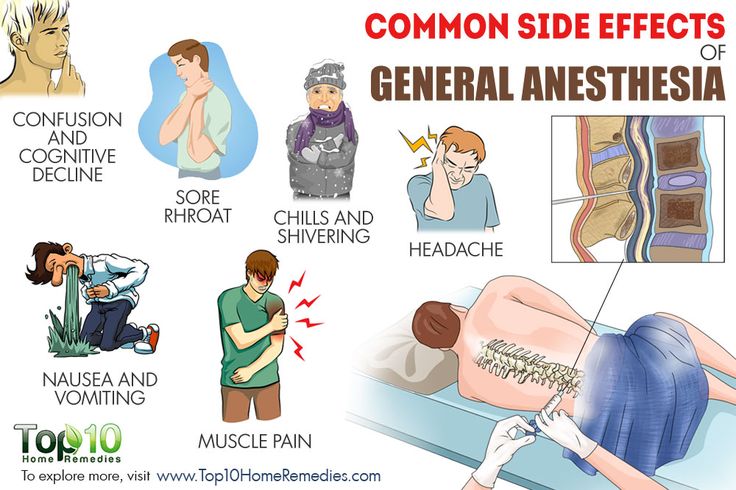
There are a number theories about how it works. One is that it works by protecting and helping to create neurons (the cells that pass messages in your brain).
How long does it take to work?Lithium may take several weeks or months to work.
How will it make me feel?If the amount of lithium in your blood is right, you probably will not have any problems taking this medicine.
However, some people find it slows down their thinking or makes them feel a bit "numb". Sometimes it's hard to know whether this is because the lithium is doing its work to control your mood (if you have mania).
Talk to your doctor if you're worried that lithium is slowing down your thinking or numbing your emotions. You may need to have your lithium levels checked again.
How long will I take it for?As long as it is working well to control your condition, you will generally take lithium for a long time.
Some people need to take lithium for many years.
What will happen if I stop taking it?If you or your doctor decide to stop lithium, it must be reduced gradually over a number of weeks or months. If you stop taking it suddenly the symptoms of your condition are likely to come back.
Do not stop taking lithium suddenly even if you feel better, or because you think the dose is too little or too much.
Your doctor will help you to reduce your medicine and stop completely, if you need to.
However, if you think you have lithium toxicity, or are having an allergic reaction, it's important to stop taking lithium straight away and get medical help.
Immediate action required: Call 999 or go to A&E now (and stop taking lithium) if:
- you’re having an allergic reaction
- you have lithium toxicity
Lithium is generally safe to take for a long time.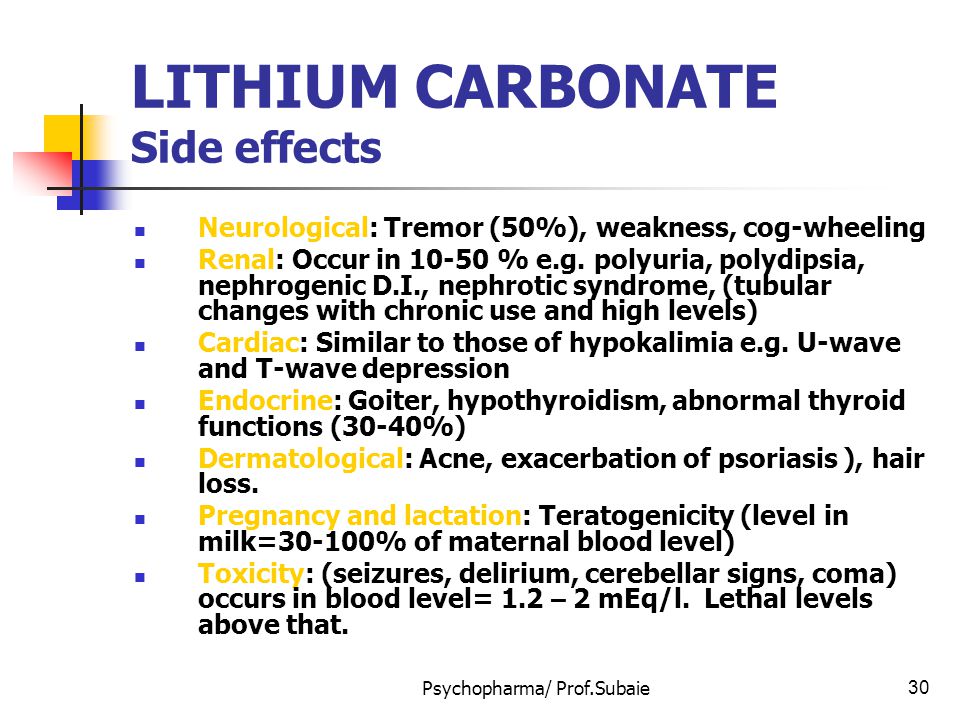 Most people take it for years with no problems.
Most people take it for years with no problems.
If you've been taking lithium for some time, it can cause weight gain. It can also cause problems with your kidneys or thyroid gland.
Common signs of an underactive thyroid are tiredness, weight gain and feeling depressed. Signs of kidney problems include swollen hands or ankles, feeling tired and short of breath, changes in your pee and feeling sick. Tell your doctor if you get any these symptoms. Your doctor will test your thyroid and kidneys every 6 months to check for any changes.
If you find you're putting on weight after taking lithium for a while, try to have a healthy balanced diet. Regular exercise will also help you keep your weight stable. Your doctor will usually monitor your weight while you're taking this medicine.
Your doctor may discuss topping up levels of the hormone that the thyroid gland normally produces (thyroxine) with a tablet.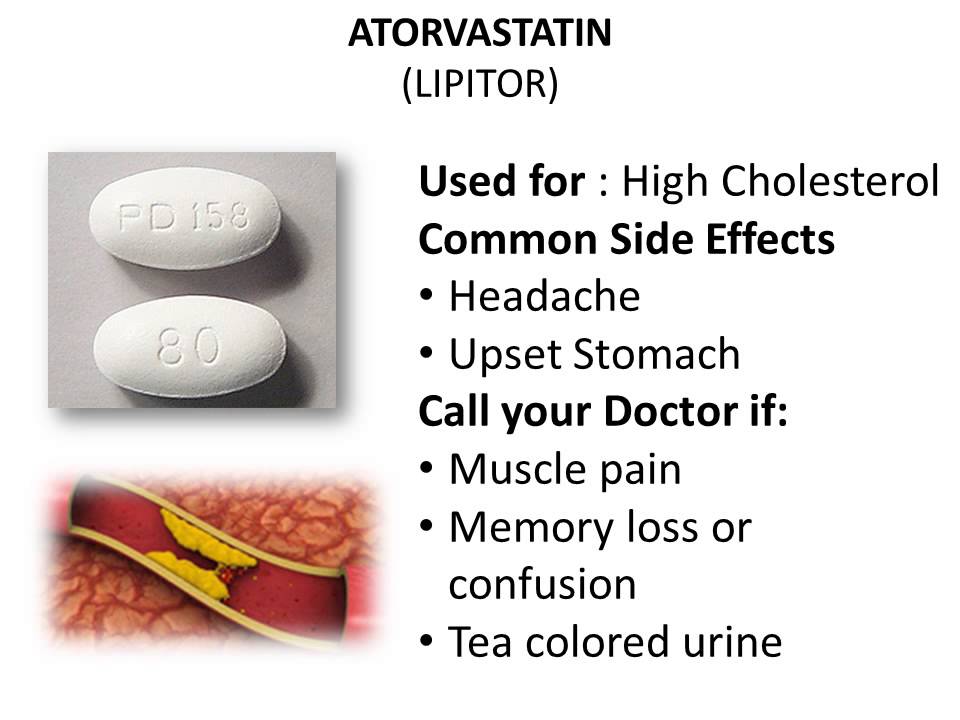
Lithium is not an antipsychotic medicine, it's known as a mood stabiliser. However, your doctor might prescribe an antipsychotic medicine with lithium.
How well does lithium treat depression?Usually, if you have depression, you'll be prescribed an antidepressant medicine first as they are considered more effective for depression than lithium.
However, when antidepressants have not worked, your doctor might prescribe lithium as well. This may be more effective and help your symptoms get better.
Can I drink alcohol with it?Lithium can make you drowsy so it's best to stop drinking alcohol during the first few days of taking lithium, or if your dose is increased.
If you feel OK after this, you can drink alcohol but it's best not to drink too much it's likely to make you dehydrated. This can increase the chance of high levels of lithium in your blood. It's important to remember this, especially in hot weather when you will sweat more and your body loses water.
This can increase the chance of high levels of lithium in your blood. It's important to remember this, especially in hot weather when you will sweat more and your body loses water.
Lithium does not affect contraception including the combined pill or emergency contraception.
However, if you have severe diarrhoea for more than 24 hours, your combined pill may not protect you from pregnancy. Look on the pill packet to find out what to do.
Read more about what to do if you're on the pill and you have diarrhoea
Will it affect my fertility?There is no clear evidence that lithium affects female fertility. However, there is small chance that it can reduce sperm count in men.
Speak to your doctor if you're trying for a baby.
Is there any food or drink I need to avoid?You can eat and drink normally while taking lithium.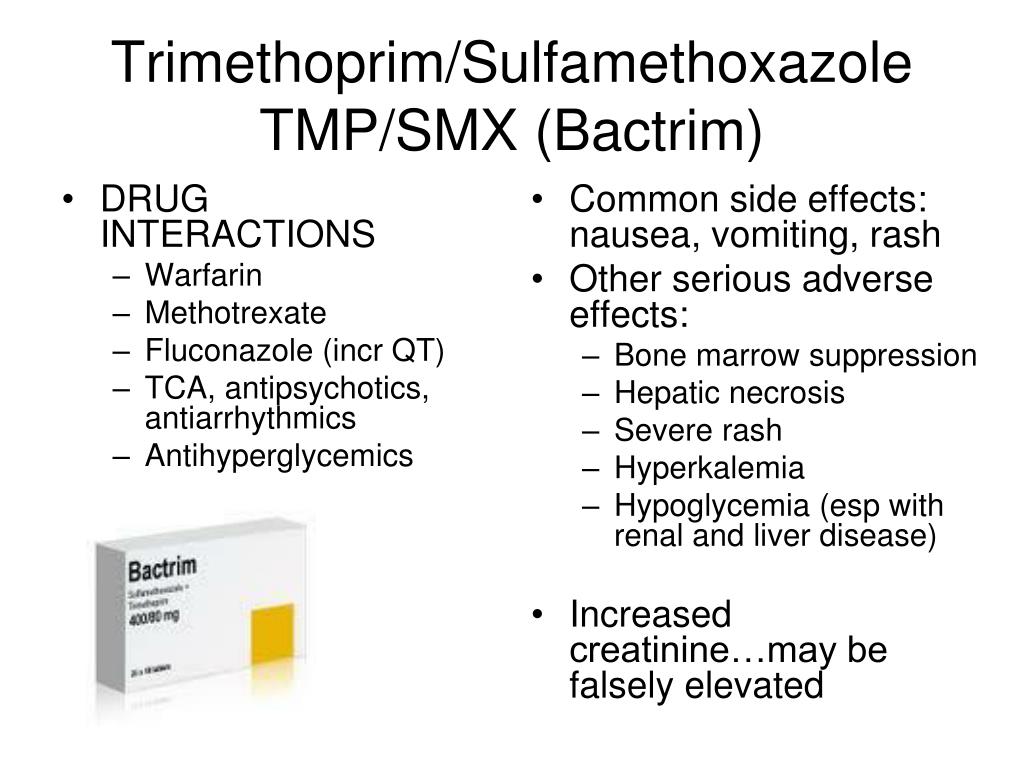
However, it's best to avoid a low-sodium (low-salt) diet as this can increase the levels of lithium in your blood and increase the chance of getting side effects.
The amount of fluids you drink is very important as it can affect the levels of lithium in your blood. Getting dehydrated will affect the levels so it's good to drink plenty of fluids.
Some people may put on weight when taking lithium. Try to eat well without increasing your portion sizes. Regular exercise can also help to keep your weight stable.
Can I drive or ride a bike?When you first start taking lithium – or if the dose has recently been changed – it may make you feel tired, dizzy, sleepy and make your hands shake.
This could affect you if you drive a car, ride a bike, or do anything else that needs focus.
You're recommended to stop doing these things for the first few days, until you know how lithium affects you and until you feel more alert.
If you have been diagnosed with bipolar disorder you must tell the Driver and Vehicle Licensing Agency (DVLA).
Can I take lithium with recreational drugs?Using recreational drugs can affect the level of lithium in the body.
Taking ecstasy while you're on lithium can make you dehydrated, which can lead to lithium toxicity.
Tell your doctor if you think you may take recreational drugs while you're on lithium.
NAMI: National Alliance on Mental Illness
Download PDF
Generic name: lithium (LITH ee um)
- Tablets: 300 mg
- Capsules: 150 mg, 300 mg, 600 mg
- Extended-release tablets: 300 mg, 450 mg
- Oral lithium citrate solution (liquid): 8 mEq/5 mL
Brand names:
- Lithobid®
- Extended-release tablets: 300 mg, 450 mg
- Eskalith®, Eskalith CR®: discontinued
All FDA black box warnings are at the end of this fact sheet. Please review before taking this medication.
Please review before taking this medication.
What Is Lithium And What Does It Treat?
Lithium is a mood stabilizer medication that works in the brain. It is approved for the treatment of bipolar disorder (also known as manic depression). Bipolar disorder involves episodes of depression and/or mania.
Symptoms of depression include:
- Depressed mood — feeling sad, empty, or tearful
- Feeling worthless, guilty, hopeless, or helpless
- Loss of interest or pleasure in normal activities
- Sleep and eat more or less than usual (for most people it is less)
- Low energy, trouble concentrating, or thoughts of death (suicidal thinking)
- Psychomotor agitation (‘nervous energy’)
- Psychomotor retardation (feeling like you are moving in slow motion)
Symptoms of mania include:
- Feeling irritable or “high”
- Having increased self esteem
- Feeling like you don’t need to sleep
- Feeling the need to continue to talk
- Feeling like your thoughts are too quick (racing thoughts)
- Feeling distracted
- Getting involved in activities that are risky or could have bad consequences (e.
 g., excessive spending)
g., excessive spending)
Lithium may also be helpful when prescribed “off-label” for depression, especially when combined with antidepressant medications. “Off-label” means that it hasn’t been approved by the Food and Drug Administration for this condition. Your mental health provider should justify his or her thinking in recommending an “off-label” treatment. They should be clear about the limits of the research around that medication and if there are any other options.
What Is The Most Important Information I Should Know About Lithium?
Bipolar disorder requires long-term treatment. Do not stop taking lithium, even when you feel better. With input from you, your health care provider will assess how long you will need to take the medication. Missing doses of lithium may increase your risk for a relapse in your mood symptoms.
Do not stop taking lithium or change your dose without talking to with your health care provider first.
In order for lithium to work properly, it should be taken every day as ordered by your health care provider.
Periodically, your health care provider may ask you to provide a blood sample to make sure the appropriate level of medication is in your body and to assess for side effects, such as changes in blood cell counts or kidney function.
Are There Specific Concerns About Lithium And Pregnancy?
If you are planning on becoming pregnant, notify your health care provider so that he/she can best manage your medications. People living with bipolar disorder who wish to become pregnant face important decisions. It is important to discuss the risks and benefits of treatment with your doctor and caregivers.
Lithium has been associated with an increased risk of Ebstein’s anomaly, a heart valve defect. Even though data suggest that the risk of Ebstein’s anomaly from first trimester use of lithium is very low, an ultrasound of the heart is recommended at 16 to 20 weeks of gestation. Lithium levels should be monitored monthly in early pregnancy and weekly near delivery. Do not stop taking lithium without first speaking to your health care provider. Discontinuing mood stabilizer medications during pregnancy has been associated with a significant increase in symptom relapse.
Lithium levels should be monitored monthly in early pregnancy and weekly near delivery. Do not stop taking lithium without first speaking to your health care provider. Discontinuing mood stabilizer medications during pregnancy has been associated with a significant increase in symptom relapse.
Regarding breastfeeding, caution is advised since lithium does pass into breast milk. In general, breastfeeding is not recommended while taking lithium.
What Should I Discuss With My Health Care Provider Before Taking Lithium?
- Symptoms of your condition that bother you the most
- If you have thoughts of suicide or harming yourself
- Medications you have taken in the past for your condition, whether they were effective or caused any adverse effects
- If you experience side effects from your medications, discuss them with your provider. Some side effects may pass with time, but others may require changes in the medication.
- Any other psychiatric or medical problems you have
- All other medications you are currently taking (including over the counter products, herbal and nutritional supplements) and any medication allergies you have
- Other non-medication treatment you are receiving, such as talk therapy or substance abuse treatment.
 Your provider can explain how these different treatments work with the medication.
Your provider can explain how these different treatments work with the medication. - If you are pregnant, plan to become pregnant, or are breastfeeding
- If you drink alcohol or use illegal drugs
How Should I Take Lithium?
Lithium is usually taken 1-3 times per day with or without food.
Typically patients begin at a low dose of medication and the dose is increased slowly over several weeks.
The dose usually ranges from 600 mg to 1200 mg daily, but some people may require higher doses depending on weight or symptoms. Only your health care provider can determine the correct dose for you.
Extended release tablets: Swallow the tablet whole. Do not crush or chew extended release tablets.
Liquid: Measure with a dosing spoon or oral syringe, which you can get from your pharmacy.
Use a calendar, pillbox, alarm clock, or cell phone alert to help you remember to take your medication. You may also ask a family member a friend to remind you or check in with you to be sure you are taking your medication.
What Happens If I Miss A Dose Of Lithium?
If you miss a dose of lithium, take it as soon as you remember, unless it is closer to the time of your next dose. Discuss this with your healthcare provider. Do not double your dose or take more than what is prescribed.
What Should I Avoid While Taking Lithium?
Avoid drinking alcohol or using illegal drugs while you are taking lithium. They may decrease the benefits (e.g., worsen your condition) and increase adverse effects (e.g., sedation) of the medication.
Avoid low sodium diets and dehydration because this can increase the risk of lithium toxicity.
Avoid over the counter and prescription pain medications that contain nonsteroidal anti-inflammatory medications (NSAIDS) such as ibuprofen (Motrin®, Advil®) or naproxen (Aleve®, Naprosyn®) because these medications can increase the risk of toxicity from lithium.
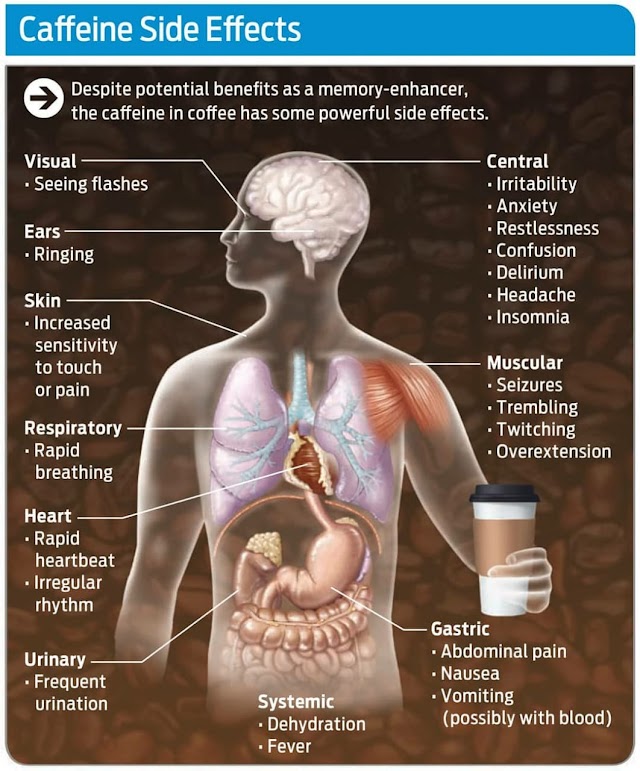
Avoid excessive intake of caffeinated beverages, such as coffee, tea, cola or energy drinks, since these may decrease levels of lithium and decrease effectiveness of the medication. Discontinuing caffeine use may increase lithium levels. Consult your health care provider before reducing or stopping caffeine use.
Discontinuing caffeine use may increase lithium levels. Consult your health care provider before reducing or stopping caffeine use.
What Happens If I Overdose With Lithium?
If an overdose occurs call your doctor or 911. You may need urgent medical care. You may also contact the poison control center at 1-800-222-1222.
A specific treatment to reverse the effects of lithium does not exist, but there are treatments to decrease the effects of the medication. Only a doctor can determine if you require treatment.
What are the possible side effects of lithium?
Common side effects
- Headache
- Nausea or vomiting
- Diarrhea
- Dizziness or drowsiness
- Changes in appetite
- Hand tremors
- Dry mouth
- Increased thirst
- Increased urination
- Thinning of hair or hair loss
- Acne-like rash
Rare/serious side effects
Signs of lithium toxicity include severe nausea and vomiting, severe hand tremors, confusion, vision changes, and unsteadiness while standing or walking. These symptoms need to be addressed immediately with a medical doctor to ensure your lithium level is not dangerously high.
These symptoms need to be addressed immediately with a medical doctor to ensure your lithium level is not dangerously high.
In rare cases, lithium may lead to a reversible condition known as diabetes insipidus. If this occurs you would notice a significant increase in thirst and how much fluid you drink and how much you urinate. Talk to your doctor if you notice you are urinating more frequently than usual.
Are There Any Risks For Taking Lithium For Long Periods Of Time?
Hypothyroidism (low levels of thyroid hormone) may occur with long-term lithium use.
Rare kidney problems have been associated with long-term use of lithium. The risk increases with high levels of lithium. Your doctor will monitor your kidney function at routine check-ups to ensure this does not occur.
What Other Medications May Interact With Lithium?
The following medications can increase the levels and effects of lithium:
- Diuretics, such as: hydrochlorothiazide (Microzide®), furosemide (Lasix®), bumetanide (Bumex®), torsemide (Demadex®), acetazolamide (Diamox®), chlorthiazide (Diuril®), and chlorthalidone (Thalitone®)
- Non-steroidal anti-inflammatory medications (NSAIDs) including: Ibuprofen (Advil®, Motrin®), naproxen (Naprosyn®), celecoxib (Celebrex®), diclofenac (Voltaren®), and nabumetone (Relafen®)
- Certain blood pressure medications, called angiotensin receptor blockers or angiotensin converting enzyme inhibitors.
- Angiotensin receptor blockers (ARBs): valsartan (Diovan®), olmesartan (Benicar®), candesartan (Atacand®), losartan (Cozaar®)
- Angiotensin converting enzyme (ACE) inhibitors: enalapril (Vasotec®), captopril (Capoten®), benazepril (Lotensin®), fosinopril (Monopril®)
- Certain antidepressants, known as monoamine oxidase inhibitors (MAOIs). Examples include phenelzine (Nardil®), tranylcypromine (Parnate®), selegiline (Eldepryl®, Emsam®), and isocarboxazid (Marplan®)
The following medications may decrease the levels and effect of lithium:
- Caffeine
- Sodium chloride (table salt)
- A medication used to treat breathing problems called theophylline (Theo–Dur®, Slo–Bid®)
How Long Does It Take For Lithium To Work?
It is very important to tell your doctor how you feel things are going during the first few weeks after you start taking lithium. It will probably take several weeks to see big enough changes in your symptoms to decide if lithium is the right medication for you.
Mood stabilizer treatment is generally needed lifelong for persons with bipolar disorder. Your doctor can best discuss the duration of treatment you need based on your symptoms and illness.
Summary of Black Box Warnings
Lithium toxicity
Lithium toxicity is closely related to lithium blood levels and can occur at doses close to therapeutic levels; lithium levels should be monitored closely when starting the medication or if individuals experience side effects of the medication.
Provided by
(January 2023)
©2022 The American Association of Psychiatric Pharmacists (AAPP) and the National Alliance on Mental Illness (NAMI). AAPP and NAMI make this document available under the Creative Commons Attribution-No Derivatives 4.0 International License. Last Updated: January 2016.
This information is being provided as a community outreach effort of the American Association of Psychiatric Pharmacists. This information is for educational and informational purposes only and is not medical advice. This information contains a summary of important points and is not an exhaustive review of information about the medication. Always seek the advice of a physician or other qualified medical professional with any questions you may have regarding medications or medical conditions. Never delay seeking professional medical advice or disregard medical professional advice as a result of any information provided herein. The American Association of Psychiatric Pharmacists disclaims any and all liability alleged as a result of the information provided herein.
This information is for educational and informational purposes only and is not medical advice. This information contains a summary of important points and is not an exhaustive review of information about the medication. Always seek the advice of a physician or other qualified medical professional with any questions you may have regarding medications or medical conditions. Never delay seeking professional medical advice or disregard medical professional advice as a result of any information provided herein. The American Association of Psychiatric Pharmacists disclaims any and all liability alleged as a result of the information provided herein.
Lithium carbonate - description of the substance, pharmacology, use, contraindications, formula
Contents
- Structural formula
- Russian name
- English name
- Latin name of the substance Lithium carbonate
- Chemical name
- Gross formula
- Pharmacological group of the substance Lithium carbonate
- Nosological classification
- CAS code
- Pharmacological action
- Characteristic
- Pharmacology
- Substance use Lithium carbonate
- Contraindications
- Use in pregnancy and lactation
- Side effects of the substance Lithium carbonate
- Interaction
- Overdose
- Dosage and administration
- Precautions
- Trade names with active substance Lithium carbonate
Structural formula
Russian name
Lithium carbonate
English name
Lithium carbonate
Latin name of the substance Lithium carbonateLithium carbonate Normotimics
Nosological classification
ICD-10 code list
- H81.
 0 Meniere's disease
0 Meniere's disease - F31 Bipolar affective disorder
- F30.0 Hypomania
- G43 Migraine
- Y57.9 Medicines and medicaments, unspecified
- F10.2 Alcohol dependence syndrome
- F30 Manic episode
- F65 Disorders of sexual preference
- F25 Schizoaffective disorders
CAS code
554-13-2
Pharmacological action
Pharmacological action - antipsychotic , normothymic , sedative .
Characteristics
White granular powder, odorless. Slightly soluble in water, practically insoluble in alcohol.
Slightly soluble in water, practically insoluble in alcohol.
Pharmacology
Blocks sodium channels in neurons and muscle cells, causes a shift in the intraneuronal metabolism of catecholamines.
Sufficiently absorbed in the gastrointestinal tract, T max is 6-12 hours. T 1/2 increases from 1.3 days after the first dose to 2.4 days after 1 year of regular intake. Passes through the BBB, the placental barrier, penetrates into breast milk.
Use of the substance Lithium carbonate
Manic phase and prevention of exacerbations of bipolar affective disorder, schizoaffective disorders, manic and hypomanic states of various origins, affective disorders in chronic alcoholism, drug dependence (some forms), sexual deviations, Meniere's syndrome, migraine.
Contraindications
Hypersensitivity, major surgery, severe cardiovascular disease (may worsen, lithium excretion may be impaired), epilepsy and parkinsonism (may worsen, neurotoxic effect of lithium may be masked), history of leukemia (lithium may exacerbate leukemia) , kidney failure, severe dehydration (increased risk of lithium toxicity), pregnancy, breast-feeding.
Use in pregnancy and lactation
Contraindicated in pregnancy.
FDA fetal category D.
Stop breastfeeding during treatment.
Side effects of the substance Lithium carbonate
From the side of the nervous system and sensory organs: hand tremor, drowsiness, weakness.
From the side of the cardiovascular system and blood (hematopoiesis, hemostasis): cardiac arrhythmia, leukocytosis, inhibition of hematopoiesis.
From the digestive tract: diarrhea, nausea, vomiting, dry mouth.
From the genitourinary system: polyuria, kidney dysfunction.
Other: myasthenia gravis, increased thirst, weight gain, hypothyroidism, allergic reactions, alopecia, acne.
Interactions
The combination of carbamazepine with lithium increases the risk of neurotoxic effects. Metronidazole, fluoxetine, diuretics, NSAIDs, ACE inhibitors slow down the excretion of Li 9 by the kidneys0180 + and increase its toxic effects (careful monitoring of the concentration of lithium in the blood serum is recommended). The combined use of lithium with ampicillin and tetracycline can lead to an increase in the concentration of lithium in plasma. CCBs increase the incidence of neurotoxic complications (caution should be exercised). With simultaneous use with methyldopa, the risk of developing lithium toxicity may increase even when its concentrations in the blood serum remain within the recommended therapeutic limits. Urea, aminophylline, caffeine, theophylline increase the excretion of Li + by the kidneys and reduce its pharmacological action.
The combined use of lithium with ampicillin and tetracycline can lead to an increase in the concentration of lithium in plasma. CCBs increase the incidence of neurotoxic complications (caution should be exercised). With simultaneous use with methyldopa, the risk of developing lithium toxicity may increase even when its concentrations in the blood serum remain within the recommended therapeutic limits. Urea, aminophylline, caffeine, theophylline increase the excretion of Li + by the kidneys and reduce its pharmacological action.
Lithium preparations reduce the pressor effect of norepinephrine (an increase in the dose of norepinephrine may be required), increase or prolong the blockade of neuromuscular transmission when used together with atracurium besylate, pancuronium bromide, suxamethonium; enhance the neurotoxic effects of haloperidol, reduce the absorption of chlorpromazine (and possibly other phenothiazines) from the gastrointestinal tract, which leads to a decrease in its concentration in the blood serum by 40%.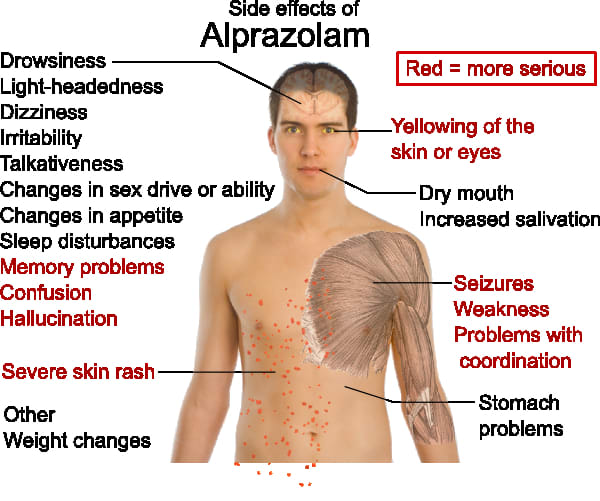 Sodium-containing drugs or foods reduce the effectiveness of lithium preparations (high sodium intake increases the excretion of lithium).
Sodium-containing drugs or foods reduce the effectiveness of lithium preparations (high sodium intake increases the excretion of lithium).
When administered concomitantly with antipsychotics and antidepressants, an increase in body weight is possible. Incompatible with ethanol-containing drinks.
Overdose
Symptoms: speech disorder, hyperreflexia, tonic and epileptic convulsions, oliguria, loss of consciousness, collapse, coma.
Treatment: symptomatic.
Dosage and administration
Inside . Adults are prescribed in a dose, the regular intake of which provides an equilibrium concentration in the blood in the range of 0.6–1.2 mmol / l for more than 6 months to manifest a preventive effect; at a dose of 1 g / day, the concentration stabilizes after 10-14 days. Even with a marked improvement, treatment should not be interrupted in order to avoid relapse. In children, the concentration of lithium in the blood should be in the range of 0. 5–1.0 mmol / l.
5–1.0 mmol / l.
Precautions
Missed doses will not be reimbursed. It is recommended to gradually cancel treatment by increasing the intervals between doses and gradually reducing the dose.
Do not use in violation of the water-salt balance (salt-free diet, sodium deficiency, diarrhea, vomiting). Use with caution in diabetes mellitus (the concentration of insulin in the blood serum may increase), hypothyroidism.
Before treatment, it is necessary to determine Cl creatinine (should be no more than 0.17 ml / s) and the amount of residual nitrogen, conduct an ECG analysis and a complete blood count with the determination of ESR, and then regularly at least 1 time per month, control the level of lithium in the blood 12 hours after the last dose.
Trade names with active substance Lithium carbonate
Reset filters
Lek. form All lek. forms substance substance-powder tablets, film-coated
Dosage All dosages 300 mg No dosage
Manufacturer All manufacturers Altaipharm Pharmstandard-Leksredstva Hemetal Changzhou Yabang Pharmaceutical Co.
Lithium: Pediatric Medication | Memorial Sloan Kettering Cancer Center
Pediatric Medication
ShareProvided by Lexicomp ® , this document provides all the information you need to know about this medicine, including indications, directions for use, side effects, and when your healthcare provider should be contacted.
Trade names: USA
Lithobid
Trade names: Canada
APO-Lithium Carbonate; Carbolith; DOM-Lithium Carbonate; Lithane; Lithmax; PMS-Lithium Carbonate
Warning
- This drug in doses close to standard doses can cause serious side effects. In rare cases, this may include death. Do not exceed the prescribed dosage of the drug when giving it to your child. Your child will need blood tests to measure the level of this drug in the blood. There are many symptoms of elevated lithium levels in the blood. Carefully read the section of this leaflet that tells you which situations require you to contact your child's doctor.
What is this drug used for?
- This medicine is used to treat bipolar disorder.
- This drug can be given to children for other indications. Consult your doctor.
What do I need to tell the doctor BEFORE my child takes this drug?
- If your child has an allergy to this drug, any of its ingredients, other drugs, foods, or substances. Tell the doctor about the allergy and how it manifested itself in the child.
- If your child suffers from any of the following: dehydration (dehydration), heart disease, kidney disease, low salt levels in the blood, or severe weakness or illness.
- If your child has a certain heart disorder called Brugada syndrome or has ever passed out for no known reason.
- If a member of your family has Brugada Syndrome, or someone in your family has died suddenly before the age of 45.
- If your child is taking medicines to control blood pressure or heart problems.
 Your child may need to have blood samples taken for a more thorough analysis.
Your child may need to have blood samples taken for a more thorough analysis.
This list of drugs and conditions that may interact with this drug is not exhaustive.
Talk to your doctor or pharmacist about all medicines your child is taking (prescription and over-the-counter, natural, and vitamins) and any health problems. You need to make sure that this drug is safe to use for your child's illnesses and in combination with other drugs he or she is already taking. Do not start, stop taking, or change the dosage of any drug your child is taking without the doctor's approval.
What do I need to know or do while my child is taking this drug?
- Tell all health care providers who care for your child that your child is taking this drug. These are your child's doctors, nurses, pharmacists and dentists.
- Perform blood tests as directed by your doctor. Consult with your doctor.
- Tell your doctor if your child starts on a low-salt diet.
 This changes the metabolism of lithium in the child's body.
This changes the metabolism of lithium in the child's body. - Have your child avoid tasks or activities that require attention until you see how this drug works for your child. This includes cycling, playing sports, or using items such as scissors, lawn mowers, electric scooters, toy cars, or motorized vehicles.
- Alcohol can interact with this drug. Make sure your child does not drink alcohol.
- An increase in body temperature, infection, vomiting, diarrhea or increased sweating can lead to a change in the concentration of the drug in the blood. If any of these symptoms occur, consult your doctor.
- Make sure your child is careful in hot weather or during active activities. Make sure your child drinks plenty of fluids to avoid dehydration.
- Some people who take this drug have a certain heart disorder (Brugada syndrome). These people had the disorder before but were unaware of it. People with Brugada syndrome have abnormal heart rhythms and are at risk of sudden death.
 Consult your doctor.
Consult your doctor. - People who take this drug with some other drugs, such as haloperidol, have rarely had brain problems. Sometimes these brain disorders have led to long-term brain damage. Consult your doctor.
- If your daughter is of childbearing age, a pregnancy test should be done before starting this medicine to make sure she is NOT pregnant.
If your daughter is pregnant or breastfeeding:
- If your daughter takes this medicine during pregnancy, it could harm the fetus. If your daughter is pregnant or becomes pregnant while taking this drug, call your doctor right away.
- If your daughter is breastfeeding, tell your daughter's doctor. This drug passes into breast milk and may harm your daughter's baby.
What side effects should I report to my child's doctor right away?
WARNING/CAUTION: Although rare, some people may have very serious and sometimes deadly side effects from this drug. Call your child's doctor right away or get medical help if your child has any of the following signs or symptoms that could be associated with a very bad side effect:
Call your child's doctor right away or get medical help if your child has any of the following signs or symptoms that could be associated with a very bad side effect:
- Signs of an allergic reaction, such as rash, hives, itching, red and swollen skin with blisters or peeling, possibly accompanied by fever, wheezing or wheezing, tightness in the chest or throat, difficulty breathing, swallowing or speaking, unusual hoarseness, swelling in the mouth, face, lips, tongue or throat.
- Symptoms of increased acidity in the blood (acidosis), such as confusion, rapid breathing, tachycardia, irregular heartbeat, very severe abdominal pain, nausea or vomiting, severe drowsiness, shortness of breath, increased fatigue or weakness.
- Thyroid symptoms such as weight changes, nervousness, agitation, anxiety, weakness, thinning hair, depression, swelling in the eyes or neck, difficulty concentrating, temperature control problems, menstrual changes, tremors, or sweating.
- Signs of fluid and electrolyte imbalances such as mood changes, confusion, muscle pain or weakness, fast or irregular heart rate, severe dizziness or loss of consciousness, extreme thirst, seizures, feeling very tired or weak, decreased appetite, inability to urinate or change in the amount of urine produced, dry mouth, dry eyes, severe nausea or vomiting.
- Signs of kidney problems, including not passing urine, changes in the volume of urine, blood in the urine, or rapid weight gain.
- Signs of high blood sugar such as confusion, drowsiness, unusual thirst and hunger, increased urination, flushing, rapid breathing, and fruity breath.
- Bloating.
- Diarrhea.
- Dizziness.
- Difficulties with walking.
- Uncontrolled body movements, jerky movements, balance problems, difficulty swallowing or speaking.
- Muscle weakness.
- Feeling sluggish.
- Loss of control over eye movements.

- Mood changes.
- Heat.
- Hallucinations (a person sees or hears something that is not in reality).
- Impairment or loss of memory.
- Anxiety.
- Shortness of breath, sudden weight gain, or swelling of the arms or legs.
- Unexplained fluctuations in weight.
- Inability to control the bladder.
- Loss of control over bowel movements.
- A severe and sometimes deadly complication called serotonin syndrome can occur. This risk may be increased if the child is also taking certain other drugs. Call your child's healthcare provider right away if your child has agitation, balance problems, confusion, hallucinations, high fever, tachycardia or abnormal heart rhythm, flushing, muscle twitching or stiffness, seizures, tremors or tremors, excessive sweating, severe diarrhea, nausea or vomiting, a very severe headache.
- This drug has been associated with increased intracranial pressure and eye inflammation.
 This can lead to visual disturbances, such as loss of vision. Call your doctor right away if your child has a very bad headache, ringing in the ears, or visual problems such as blurred vision, double vision, or loss of vision.
This can lead to visual disturbances, such as loss of vision. Call your doctor right away if your child has a very bad headache, ringing in the ears, or visual problems such as blurred vision, double vision, or loss of vision.
If your child is or may be sexually active:
- Violation of sexual function.
What are some other side effects of this drug?
Any drug can cause side effects. However, for many people, side effects are either minor or non-existent. Contact your child's doctor or seek medical attention if any of these or other side effects bother your child or if they persist:
- Feeling dizzy, drowsy, tired or weak.
- Nausea.
- Decreased appetite.
- Pain in the intestines.
- Increased salivation.
- Gas formation.
- Dry mouth.
- Headache.
- Dry or thin hair.
- Hair loss.
- Change in the ability to perceive taste.
- Joint pain.
This list of possible side effects is not exhaustive. If you have any questions about side effects, ask your child's doctor. Talk to your child's doctor about side effects.
You can report side effects to the National Health Board.
What is the best way to give this drug?
Give this drug to your child as directed by your doctor. Read all the information provided to you. Strictly follow all instructions.
All forms:
- Give this drug with or without food. If the drug causes stomach upset, give it with food.
- Your child should consume the same amount of salt.
- Follow your child's doctor's instructions about the recommended types and amounts of fluids to drink while taking this drug.
Modified release tablets:
- Ask your child to swallow whole. Ask your child not to chew or crumble.
Liquid (solution):
- Liquid doses should be measured with caution.
 Use the dispenser that comes with the medication. If the dispenser is not provided in the package, ask the pharmacist for a dosing agent for this drug.
Use the dispenser that comes with the medication. If the dispenser is not provided in the package, ask the pharmacist for a dosing agent for this drug.
What if my child misses a dose of medication?
- Give the missed dose as soon as possible.
- If it is time for your child to take the next dose, do not take the missed dose and then go back to your child's normal schedule.
- Do not give a double dose at the same time or additional doses.
- If you are not sure what to do if your child misses a dose, contact your doctor.
How do I store and/or discard this drug?
- Store at room temperature in a dry place. Do not store in the bathroom.
- Keep all medicines in a safe place. Keep all medicines out of the reach of children and pets.
- Dispose of unused or expired drugs. Do not empty into a toilet or sewer unless instructed to do so. If you have any questions about disposing of medicines, ask your pharmacist.
 Drug disposal programs may be in place in your area.
Drug disposal programs may be in place in your area.
General information about drugs
- If your child's symptoms or health problems do not improve, or worsen, contact your child's doctor.
- Do not share your child's medicine with others and do not give anyone else's medicine to your child.
- Some medicines may come with other patient information leaflets. If you have questions about this drug, talk with your child's doctor, nurse, pharmacist, or other health care professional.
- If you think you have overdosed, call a poison control center or get medical help right away. Be prepared to tell or show what drug you took, how much, and when it happened.
Consumer Use of Information and Limitation of Liability
This summary information includes a summary of the diagnosis, treatment, and/or drug product. It is not intended to be a comprehensive source of data and should be used as a tool to help the user understand and/or evaluate potential diagnostic and treatment options.