Citalopram when pregnant
Pregnancy, breastfeeding and fertility while taking citalopram
Citalopram and pregnancy
Citalopram can be used in pregnancy. Some studies have suggested that citalopram might occasionally affect the development of a baby’s heart. However, if there is any risk, it is small, and most babies born to women taking citalopram have a normal heart.
When citalopram is taken in the weeks before delivery it can sometimes cause short-term withdrawal symptoms and, very rarely, breathing problems in the baby. Your baby will be checked after birth and given extra care if needed.
Taking citalopram in the last month of pregnancy may slightly increase your risk of bleeding after delivery. However, because this side-effect is rare and treatable, it is not a reason to stop taking citalopram for most pregnant women.
It is important that mental health problems are well treated since these can affect both you and your baby’s wellbeing. Depression and anxiety can sometimes get worse during pregnancy, and after the baby’s born.
Speak to your doctor if you get pregnant. They will help you weigh up the risks and benefits so you can decide on the best treatment for you and your baby.
Citalopram and breastfeeding
If your doctor or health visitor says your baby is healthy, you can take citalopram while breastfeeding.
Citalopram passes into breast milk in fairly small amounts. It has often been used during breastfeeding without any problems but has been linked with side effects, including poor feeding, colic, and being unusually sleepy, irritable or restless, in a very small number of breastfed babies.
If you notice that your baby has any of these side effects, or you have any other concerns about them, talk to your health visitor, midwife, pharmacist or doctor as soon as possible.
Although other medicines that pass into breast milk in smaller amounts might be preferred while you are breastfeeding, it is important you take the medicine that works for you. If you are breastfeeding, or planning to breastfeed, talk to your doctor or pharmacist to help you decide what is best for you.
If you are breastfeeding, or planning to breastfeed, talk to your doctor or pharmacist to help you decide what is best for you.
It's important to continue taking citalopram to keep you well. Breastfeeding will also benefit both you and your baby.
Citalopram and fertility
Citalopram may possibly reduce sperm quality, but it's not known whether this reduces male fertility or not. Speak to your doctor if you're having difficulty conceiving a baby.
For women, there's no evidence to suggest that taking citalopram will reduce your fertility. Speak to a pharmacist or your doctor if you're trying to get pregnant as they may want to review your treatment.
Non-urgent advice: Tell your doctor if you're:
- trying to get pregnant
- pregnant
- breastfeeding
Find out more about how citalopram can affect you and your baby on the Best Use of Medicines in Pregnancy (BUMPS) website.
Page last reviewed: 9 February 2022
Next review due: 9 February 2025
Citalopram use in pregnancy: prospective comparative evaluation of pregnancy and fetal outcome
Comparative Study
. 2005 Dec;193(6):2004-9.
doi: 10.1016/j.ajog.2005.05.012.
Anna Sivojelezova 1 , Samar Shuhaiber, Lorig Sarkissian, Adrienne Einarson, Gideon Koren
Affiliations
Affiliation
- 1 The Motherisk Program, Division of Clinical Pharmacology and Toxicology, The Hospital for Sick Children, Ontario, Canada. [email protected]
- PMID: 16325604
- DOI: 10.
 1016/j.ajog.2005.05.012
1016/j.ajog.2005.05.012
Comparative Study
Anna Sivojelezova et al. Am J Obstet Gynecol. 2005 Dec.
. 2005 Dec;193(6):2004-9.
doi: 10.1016/j.ajog.2005.05.012.
Authors
Anna Sivojelezova 1 , Samar Shuhaiber, Lorig Sarkissian, Adrienne Einarson, Gideon Koren
Affiliation
- 1 The Motherisk Program, Division of Clinical Pharmacology and Toxicology, The Hospital for Sick Children, Ontario, Canada. [email protected]
- PMID: 16325604
- DOI: 10.
 1016/j.ajog.2005.05.012
1016/j.ajog.2005.05.012
Abstract
Objective: Citalopram is a selective serotonin reuptake inhibitor indicated for depression. The safety of this medication in pregnancy has not been fully established. The purpose of this study was to investigate whether citalopram is associated with an increased incidence of adverse pregnancy outcomes.
Study design: Pregnant women who contacted the Motherisk Program, a Teratogen Information Center in Toronto, Ontario, with regard to the safety of citalopram in pregnancy were enrolled in the study. The exposed women were matched to a disease-matched group of women and a nonteratogenic group. All women were matched for age (+/- 2 years) and gestational age at time of first call to the Motherisk (+/- 2 weeks). A structured telephone follow-up interview was conducted following the expected date of confinement.
Results: The total number of pregnant women enrolled in this study was 396 (132 women in each group). A total of 125 women took citalopram at least in the first trimester. Seventy-one (54%) women continued to take the drug throughout pregnancy. One hundred fourteen women (86%) had live births, 14 (11%) had spontaneous abortions, 2 (1.5%) had elective terminations, and 2 (1.5%) experienced stillbirths. Fetal survival rates, mean birth weights, and duration of pregnancy were not statistically different among the 3 groups. Of 108 live-born infants whose mothers were exposed to citalopram in the first trimester, there was 1 (0.9%) male infant born with a major malformation. There was a relative risk of 4.2 (95% confidence interval 1.71-10.26) in neonates exposed to citalopram close to term to be admitted to special-care nurseries as compared with the unexposed infants.
Conclusion: Citalopram use during the period of embryogenesis in pregnancy is not associated with an apparent major teratogenic risk. Late pregnancy use of citalopram is associated with increased risk of poor neonatal adaptation syndrome, recently described with other selective serotonin reuptake inhibitors.
Late pregnancy use of citalopram is associated with increased risk of poor neonatal adaptation syndrome, recently described with other selective serotonin reuptake inhibitors.
Similar articles
-
Neonatal outcomes after prenatal exposure to selective serotonin reuptake inhibitor antidepressants and maternal depression using population-based linked health data.
Oberlander TF, Warburton W, Misri S, Aghajanian J, Hertzman C. Oberlander TF, et al. Arch Gen Psychiatry. 2006 Aug;63(8):898-906. doi: 10.1001/archpsyc.63.8.898. Arch Gen Psychiatry. 2006. PMID: 16894066
-
Risks associated with selective serotonin reuptake inhibitors in pregnancy.
Malm H, Klaukka T, Neuvonen PJ. Malm H, et al. Obstet Gynecol. 2005 Dec;106(6):1289-96.
 doi: 10.1097/01.AOG.0000187302.61812.53. Obstet Gynecol. 2005. PMID: 16319254
doi: 10.1097/01.AOG.0000187302.61812.53. Obstet Gynecol. 2005. PMID: 16319254 -
Pregnancy outcome of women exposed to bupropion during pregnancy: a prospective comparative study.
Chun-Fai-Chan B, Koren G, Fayez I, Kalra S, Voyer-Lavigne S, Boshier A, Shakir S, Einarson A. Chun-Fai-Chan B, et al. Am J Obstet Gynecol. 2005 Mar;192(3):932-6. doi: 10.1016/j.ajog.2004.09.027. Am J Obstet Gynecol. 2005. PMID: 15746694
-
Safety of newer antidepressants in pregnancy.
Way CM. Way CM. Pharmacotherapy. 2007 Apr;27(4):546-52. doi: 10.1592/phco.27.4.546. Pharmacotherapy. 2007. PMID: 17381382 Review.
-
[The safety profile of escitalopram in pregnancy and breastfeeding].

Bellantuono C, Orsolini L, Bozzi F. Bellantuono C, et al. Riv Psichiatr. 2013 Nov-Dec;48(6):407-14. doi: 10.1708/1379.15335. Riv Psichiatr. 2013. PMID: 24441517 Review. Italian.
See all similar articles
Cited by
-
Machine learning to predict metabolic drug interactions related to cytochrome P450 isozymes.
Wang NN, Wang XG, Xiong GL, Yang ZY, Lu AP, Chen X, Liu S, Hou TJ, Cao DS. Wang NN, et al. J Cheminform. 2022 Apr 15;14(1):23. doi: 10.1186/s13321-022-00602-x. J Cheminform. 2022. PMID: 35428354 Free PMC article.
-
Use of Herbal Medicines for the Treatment of Mild Mental Disorders and/or Symptoms During Pregnancy: A Cross-Sectional Survey.
Gantner G, Spiess D, Randecker E, Quack Lötscher KC, Simões-Wüst AP.
 Gantner G, et al. Front Pharmacol. 2021 Oct 8;12:729724. doi: 10.3389/fphar.2021.729724. eCollection 2021. Front Pharmacol. 2021. PMID: 34690768 Free PMC article.
Gantner G, et al. Front Pharmacol. 2021 Oct 8;12:729724. doi: 10.3389/fphar.2021.729724. eCollection 2021. Front Pharmacol. 2021. PMID: 34690768 Free PMC article. -
A Review on the Vagus Nerve and Autonomic Nervous System During Fetal Development: Searching for Critical Windows.
Cerritelli F, Frasch MG, Antonelli MC, Viglione C, Vecchi S, Chiera M, Manzotti A. Cerritelli F, et al. Front Neurosci. 2021 Sep 20;15:721605. doi: 10.3389/fnins.2021.721605. eCollection 2021. Front Neurosci. 2021. PMID: 34616274 Free PMC article.
-
Duloxetine Exposure During Pregnancy and the Risk of Spontaneous and Elective Abortion: A Danish Nationwide Observational Study.
Ankarfeldt MZ, Petersen J, Andersen JT, Fernandes MFS, Li H, Motsko SP, Fast T, Jimenez-Solem E.
 Ankarfeldt MZ, et al. Drugs Real World Outcomes. 2021 Sep;8(3):289-299. doi: 10.1007/s40801-021-00252-9. Epub 2021 May 18. Drugs Real World Outcomes. 2021. PMID: 34008161 Free PMC article.
Ankarfeldt MZ, et al. Drugs Real World Outcomes. 2021 Sep;8(3):289-299. doi: 10.1007/s40801-021-00252-9. Epub 2021 May 18. Drugs Real World Outcomes. 2021. PMID: 34008161 Free PMC article. -
Affective disorders: A question of continuing treatment during pregnancy (Review).
Trifu SC, Popescu A, Marian MA. Trifu SC, et al. Exp Ther Med. 2020 Oct;20(4):3474-3482. doi: 10.3892/etm.2020.8989. Epub 2020 Jul 13. Exp Ther Med. 2020. PMID: 32905103 Free PMC article. Review.
See all "Cited by" articles
Publication types
MeSH terms
Substances
FGBNU NTsPZ. ‹‹Depression in General Medicine: A Guide for Physicians››
The choice between the need for pharmacotherapy, on the one hand, and the prevention of risks to the health of the fetus or newborn (the risk of congenital malformations, pre- and neonatal complications, etc. ) on the other, is required from the doctor in case of depression that manifests or worsens during the period pregnancy.
) on the other, is required from the doctor in case of depression that manifests or worsens during the period pregnancy.
When deciding on such an alternative (the proportion of benefit to the mother and the potential risk to the child), a number of circumstances are taken into account, including the possibility of a negative impact on the development of the fetus by the mother's severe mental state during pregnancy. nine0003
Psychotropic drugs for pregnant women are prescribed if absolutely necessary according to strict clinical indications:
- with pronounced affective manifestations with anxiety, agitation, sleep and appetite disorders, aggravating the somatic condition of pregnant women and women in childbirth;
- with suicidal thoughts and tendencies.
However, in some cases, such as unplanned pregnancy, antidepressants are taken out of ignorance - a depressed woman, not yet aware of the pregnancy, may continue to take psychotropic drugs and be exposed to them. nine0003
nine0003
Penetrating through the placenta or with mother's milk, psychotropic drugs can have an adverse effect on the fetus or newborn. Microsomal enzymes of the fetal liver are less active and are in a lower concentration compared to the liver of adults, which prolongs and enhances the effect of drugs. In the prenatal period, the blood-brain barrier is not yet fully formed and the immature CNS is generally more sensitive to the action of drugs. At the stage of embryogenesis, as well as in the early postnatal (neonatal) period of ontogenesis, the development of these vital structures is not completed, which can enhance the toxic effect of psychotropic drugs on both the fetus and the newborn. Such effects include potentially reversible, dose-dependent effects that may be exacerbated by the fact that metabolic systems have not yet fully formed. The constant use of drugs by a pregnant woman can lead to drug dependence of the fetus and, ultimately, to a withdrawal syndrome in the newborn [Vybornykh D. E., 1996].
E., 1996].
During lactation, taking antidepressants due to the possibility of the neonatal complications listed above is also highly undesirable. The mother should be convinced that in this situation it is more appropriate to feed with donor milk or artificial mixtures.
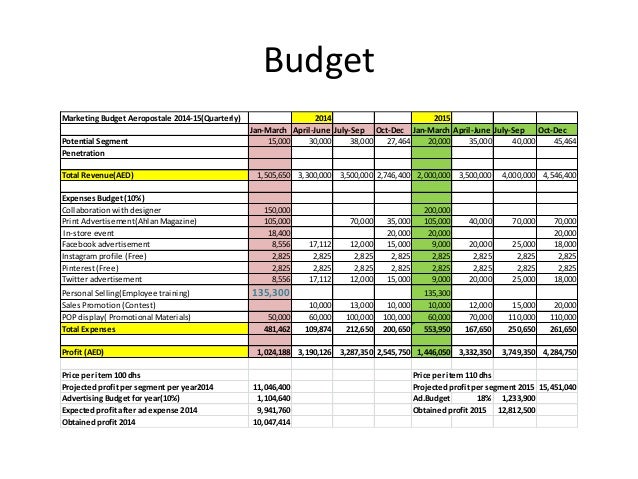
Differentiation of antidepressants in accordance with the degree of risk of developing toxic effects for infants fed by a mother taking psychotropic drugs of this class is shown in Table. 16. nine0003
Table 16 Risk of developing toxic effects in infants breastfed by mothers taking antidepressants
| Level of risk | ||
| short | average | tall |
| Mianserin | SSRI | Doxepin |
| TCAs (majority) | ||
When deciding on the use of antidepressants during pregnancy, it is necessary to take into account data on the risk of teratogenic effects of antidepressants. The teratogenic effects of antidepressants cannot be completely ruled out from laboratory animal data and some very limited clinical observations. nine0003
The teratogenic effects of antidepressants cannot be completely ruled out from laboratory animal data and some very limited clinical observations. nine0003
There are 3 classes of teratogenicity of psychotropic drugs: class A - no teratogenicity in animals, no studies of the risk of teratogenicity in humans, or teratogenicity in animals has been established, but not in humans;
class B - known to be teratogenic in animals, no risk of teratogenicity in humans, or no risk of teratogenicity in animals or humans;
class B - teratogenicity has been proven, but the benefits associated with prescribing drugs sometimes outweigh the risks (eg, in a life-threatening situation). nine0003
The distribution of drugs by teratogenicity classes is presented in Table. 17. Data are given for the first trimester of pregnancy.
Table 17. Distribution of psychotropic drugs by teratogenicity class Psychotropic Drug Directory, 1997]

 N., 1995; Winn, 1995; Stowe Z. N., Nemeroff S. V., 1996; Yoshida K. et al., 1997; Piontek C. M., 2001].
N., 1995; Winn, 1995; Stowe Z. N., Nemeroff S. V., 1996; Yoshida K. et al., 1997; Piontek C. M., 2001].  The use of psychotropic drugs in such cases is also the prevention of postpartum depression. nine0003
The use of psychotropic drugs in such cases is also the prevention of postpartum depression. nine0003  The literature also describes the possibility of an increase in the risk of other defects (anal atresia, hypospadias, craniosynostosis, etc.), but with a much smaller evidence base.
The literature also describes the possibility of an increase in the risk of other defects (anal atresia, hypospadias, craniosynostosis, etc.), but with a much smaller evidence base. 
 48, and in the analysis of siblings - 0.56. nine0003
48, and in the analysis of siblings - 0.56. nine0003