Chest pain no other symptoms
Noncardiac Chest Pain: Symptoms, Causes and Treatments
Overview
What is noncardiac chest pain?
Noncardiac chest pain is defined as recurring pain in your chest — typically, behind your breast bone and near your heart — that is not related to your heart. In most people, noncardiac chest pain is actually related to a problem with their esophagus, most often gastroesophageal reflux disease (GERD). Stress, anxiety and depression can also manifest as chronic chest pain. Other conditions can cause short-term, acute chest pain, including lung problems and musculoskeletal injuries. But noncardiac chest pain (NCCP) is diagnosed as a chronic condition.
What does noncardiac chest pain feel like?
Noncardiac chest pain is often described as feeling like angina, the chest pain caused by heart disease. It feels like a painful squeezing or tightness in your chest, or like pressure or heaviness, particularly behind your sternum. You may feel it on the right side or the left side or in the middle.
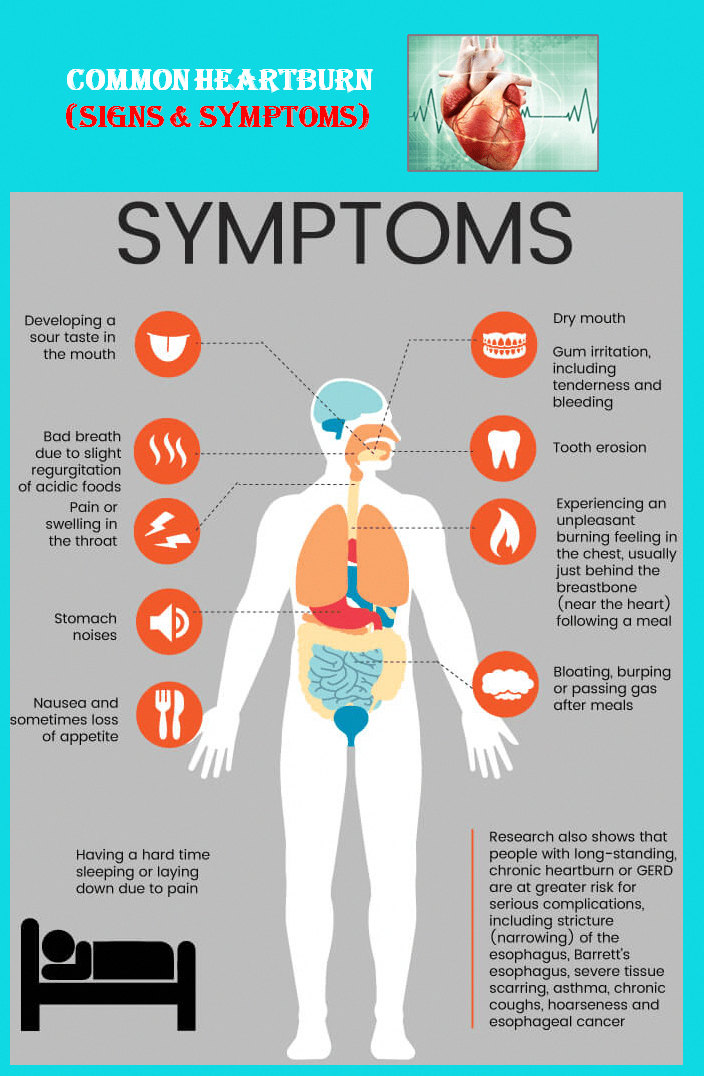
Sometimes the pain radiates to your neck, left arm or back. You may notice that it occurs after eating, or that it is accompanied by heartburn, a burning sensation in the chest. It can last for a few minutes or a few hours.
Why does pain in the esophagus feel like heart pain?
Inside your chest cavity (thorax), your esophagus actually runs right alongside the heart. The same sensory nerves send pain signals from both organs to your brain. It can be difficult to distinguish between the two based on symptoms alone. If you have other symptoms of esophageal reflux, such as stomach fluid coming back up through your esophagus, that can be a clue. Other esophageal disorders, such as muscle spasms or visceral hypersensitivity, might be trickier to identify.
How common is noncardiac chest pain?
Noncardiac chest pain affects up to 25% of adults in the U.S. Between 50% and 75% of chest pain cases presenting to emergency rooms are discharged without a cardiac diagnosis. These cases are classified either as unexplained, as stress- or anxiety-induced or as NCCP.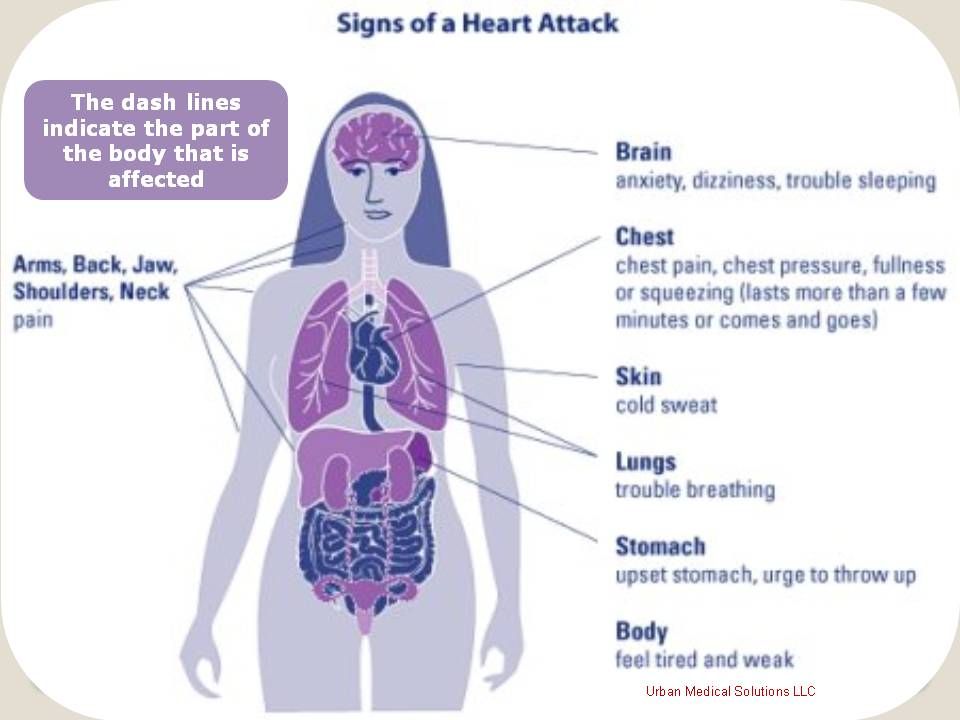
How do I know if my chest pain is serious?
You may not be able to tell the difference between a heart attack and noncardiac chest pain. For this reason, you should always take chest pain seriously. If it is sudden or new and lasts longer than five minutes, go to the emergency room. If it goes away after a few minutes, it may not be an emergency, but you should still see your healthcare provider as soon as possible to determine the cause. Noncardiac chest pain, whatever the cause, can always occur again, and can end up affecting your quality of life.
Symptoms and Causes
People who have certain risk factors are more likely to experience noncardiac chest pain.What are the most common causes of noncardiac chest pain?
Noncardiac chest pain is most commonly related to a problem with your esophagus, the “swallowing tube” that connects your mouth to your stomach. There are several different esophageal disorders that can cause noncardiac chest pain, including:
- Gastroesophageal reflux disease (GERD)
.
 Otherwise known as chronic acid reflux, this is the most common cause of noncardiac chest pain, accounting for 50% to 60% of cases.
Otherwise known as chronic acid reflux, this is the most common cause of noncardiac chest pain, accounting for 50% to 60% of cases. - Esophageal muscle spasms. Abnormal contractions or squeezing of your esophagus.
- Achalasia. This is a rare disorder in which your lower esophageal sphincter doesn’t relax and open to allow food into your stomach, causing food to back up into your esophagus.
- Esophageal hypersensitivity. This is a sensory disorder in which the muscles, nerves and receptors of your esophageal wall are overly sensitive. People with this condition experience normal tension, pressure changes, and acid contents as painful.
- Inflammation of the esophagus. This can result from an immune response to infection or food allergies (eosinophilic esophagitis,) or from peptic ulcer disease.
- Abnormal esophageal tissue. This creates constrictions, such as rings and webs.
When healthcare providers can’t determine the cause but have ruled out other possible factors, they diagnose “functional chest pain of presumed esophageal origin."
What other problems can cause noncardiac chest pain?
Some less common causes of noncardiac chest pain include:
- Muscle or bone problems in the chest, chest wall, or spine (back).
- Chronic lung diseases, including diseases of the pleura, the tissue that covers your lungs.
- Stomach problems, such as ulcers.
- Psychological problems, including pain disorders, stress, anxiety and depression.
Do people with noncardiac chest pain have other symptoms?
People with noncardiac chest pain commonly have other symptoms of GERD, including heartburn and acid reflux. They also report a higher incidence of other gastrointestinal (GI) complaints, including sore throat, regurgitation and difficulty swallowing. Up to 80% of those with functional noncardiac chest pain report other functional GI disorders with no obvious explanation, especially IBS (27%) and functional abdominal bloating (22%).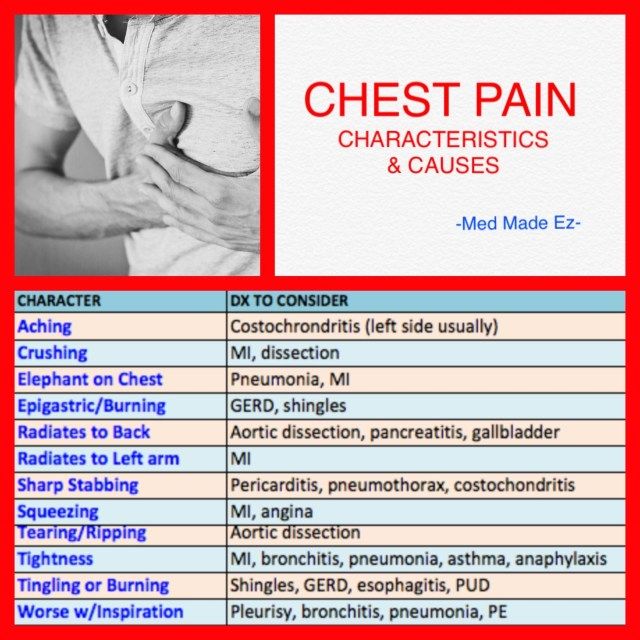
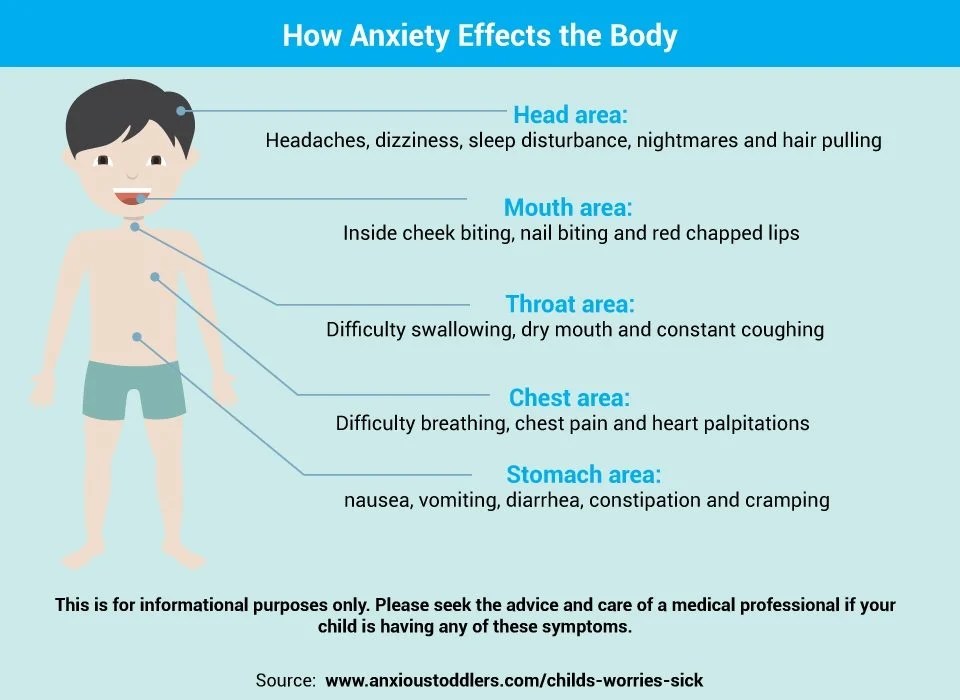
For some people, noncardiac chest pain is associated with psychological symptoms, such as stress, anxiety and depression. This is true even when the cause is determined to be something else. In fact, there is a significant crossover between psychological symptoms and symptoms of esophageal hypersensitivity, as well as heartburn. Psychological stress can trigger gastrointestinal symptoms, and vice versa. Doctors have speculated that this is due to a disorder of the gut-brain connection.
What risk factors are associated with noncardiac chest pain?
Correlation, but not causation, has been shown between noncardiac chest pain and:
- High BMI.
- Smoking or tobacco use.
- NSAIDs.
- Anxiety.
Diagnosis and Tests
How is noncardiac chest pain diagnosed?
If you experience chest pain that resembles cardiac chest pain, you should go to the emergency room. On arrival, you'll receive a complete physical exam that measures all of your vital signs, including blood pressure and heart rate. Then you’ll be screened for heart attack or heart disease. Tests include an electrocardiogram (EKG) — a noninvasive test that records your heart’s electrical activity — and blood tests. Your heart releases certain proteins when a heart attack occurs that will show up in a blood test. Only when cardiac factors have been ruled out will you be diagnosed with noncardiac chest pain.
Then you’ll be screened for heart attack or heart disease. Tests include an electrocardiogram (EKG) — a noninvasive test that records your heart’s electrical activity — and blood tests. Your heart releases certain proteins when a heart attack occurs that will show up in a blood test. Only when cardiac factors have been ruled out will you be diagnosed with noncardiac chest pain.
Once a cardiologist or your primary care provider has ruled out cardiac causes, you’ll likely be referred to a gastroenterologist next. They’ll test you for esophagus-based causes, starting with GERD. One way of testing is to send you home with a proton-pump inhibitor (PPI), a highly effective medicine for GERD. If the PPI relieves your symptoms, it can also confirm their cause. Other tests may include a PH study of the esophagus, an esophageal motility test, an upper endoscopy or ultrasound. In addition to physical tests, your healthcare provider will take a medical history and ask about your stress and emotional factors.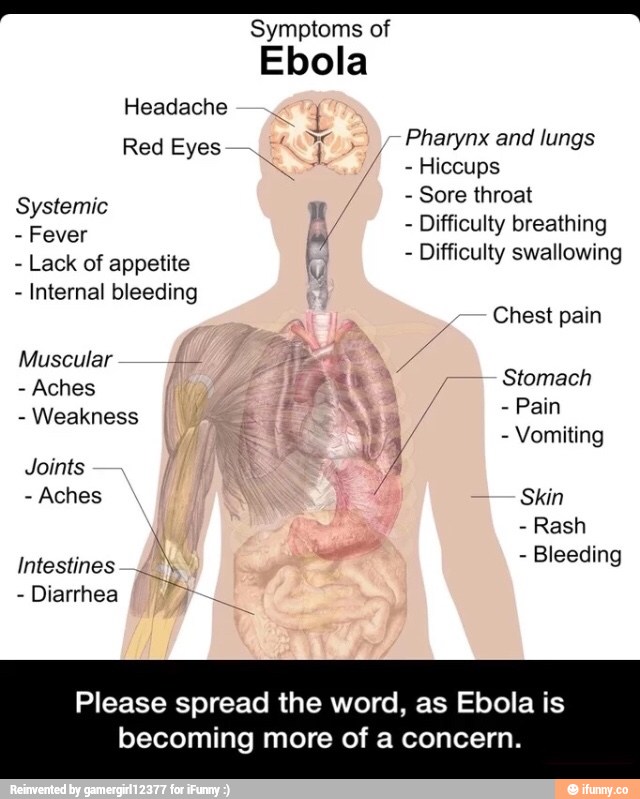
Management and Treatment
How is noncardiac chest pain treated?
Effective treatment depends on identifying the cause of your noncardiac chest pain. Some options include:
Acid reflux treatments
If your noncardiac chest pain is, like most people’s, from GERD, treatment is usually simple and effective. Proton-pump inhibitors (PPI) are the most commonly used medicine to treat GERD. PPIs reduce the amount of stomach acid that your glands secrete, which also allows ulcers and acidic corrosion to heal. Treatment usually begins with a high dosage to control your symptoms, then continues with a low dosage for two to four months. PPIs are about 90% effective in treating GERD and its side effects. If they are ineffective, it probably means that your NCCP is caused by something else.
Pain blockers
The next most common and effective treatment for noncardiac chest pain is a medicine that blocks the pain signals. These are usually from a class of drugs known as tricyclic antidepressants (TCAs), used in much lower dosages than they are used to treat depression.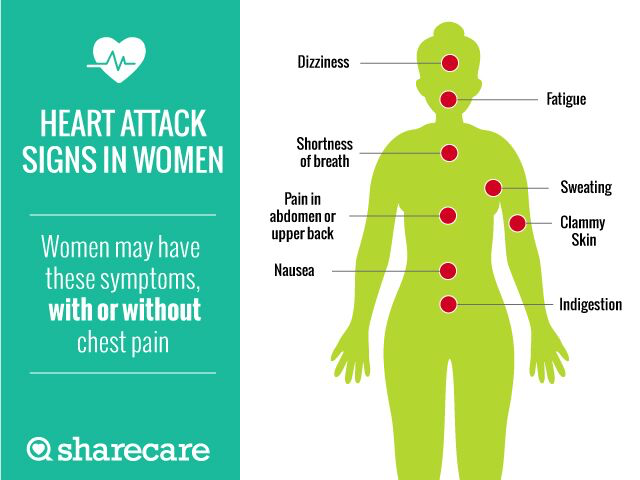 If side effects prevent you from tolerating TCAs, other categories of antidepressants might work. Selective serotonin reuptake inhibitors (SSRI) have shown some promise in treating NCCP, although they are less well-established than TCAs.
If side effects prevent you from tolerating TCAs, other categories of antidepressants might work. Selective serotonin reuptake inhibitors (SSRI) have shown some promise in treating NCCP, although they are less well-established than TCAs.
Emotional and behavioral therapies
Noncardiac chest pain can be related to depression, anxiety or stress. Psychotherapy can help you to work through these problems to reduce the occurrence of chest pain. Cognitive behavioral therapy can teach you how to change or eliminate the thought patterns that trigger stress or anxiety. Biofeedback is a guided mind-body therapy that can help you change the way your body responds to certain stimuli, including thoughts. You can also try stress management techniques at home, such as meditation, exercise and relaxation.
A note from Cleveland Clinic
Noncardiac chest pain can be scary, especially when it feels like cardiac chest pain. Recurring episodes can be frustrating and interfere with your quality of life. Always take chest pain seriously. Finding the cause of your chest pain might take some investigation, but it’s worthwhile. Most causes, when they are identified, are simple to treat. When they are complex, there is a lot to be learned about how your body responds to foods, stress and thoughts that can put you on the path to long-term recovery.
Always take chest pain seriously. Finding the cause of your chest pain might take some investigation, but it’s worthwhile. Most causes, when they are identified, are simple to treat. When they are complex, there is a lot to be learned about how your body responds to foods, stress and thoughts that can put you on the path to long-term recovery.
Symptoms, Treatment, Causes & What it Is
Overview
Visceral Hypersensitivity: Symptoms, Treatment, Causes & What it IsWhat is visceral hypersensitivity syndrome?
Visceral hypersensitivity refers to your experience of pain or discomfort in your visceral organs — the soft, internal organs that live in your chest, abdomen and pelvic cavity. If you have visceral hypersensitivity, your threshold for pain in these organs is lower than normal.
Healthcare providers have been able to measure the visceral pain threshold in certain patients with tests that apply small amounts of internal pressure to some of these organs.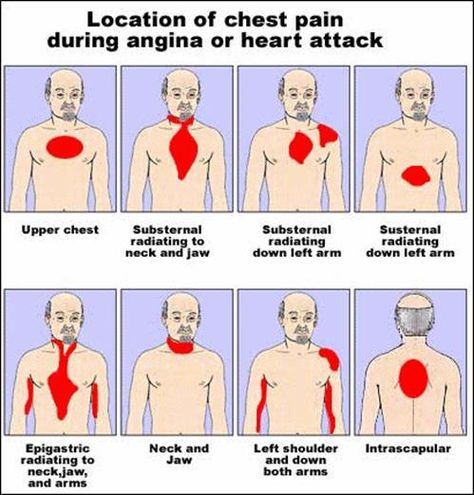 Most people don't experience discomfort from these tests, but those with visceral hypersensitivity do. They also may feel discomfort from the normal functioning of the organs that other people wouldn’t notice.
Most people don't experience discomfort from these tests, but those with visceral hypersensitivity do. They also may feel discomfort from the normal functioning of the organs that other people wouldn’t notice.
How does visceral sensitivity affect my body?
Your visceral organs include your heart and lungs, your bladder and reproductive organs and the organs in your digestive system. Visceral hypersensitivity (VH) can make the normal functioning of one or several of these organs feel uncomfortable. Many people with visceral hypersensitivity are also diagnosed with functional disorders, especially gastrointestinal ones.
Functional disorders cause pain and discomfort in the internal organs in response to normal amounts of internal pressure from gas, fluids or solids moving through. Healthcare providers believe that visceral sensitivity plays a role in how these functional disorders develop (their etiology).
Is visceral hypersensitivity the same as IBS?
No, but it's often involved in IBS, and people who have IBS are the ones most commonly evaluated for visceral hypersensitivity. About 40% of people with IBS are diagnosed with VH. Healthcare providers believe that visceral hypersensitivity may result from and/or contribute to chronic IBS symptoms. It's also involved in other functional disorders, but most of the research on visceral hypersensitivity is related to IBS.
About 40% of people with IBS are diagnosed with VH. Healthcare providers believe that visceral hypersensitivity may result from and/or contribute to chronic IBS symptoms. It's also involved in other functional disorders, but most of the research on visceral hypersensitivity is related to IBS.
How common is this condition?
Visceral hypersensitivity is a relatively new diagnosis. We don’t know yet exactly how common it is. We do know that functional disorders are common. IBS alone affects at least 20% of the population, and up to 40% of people with IBS have visceral hypersensitivity. Considering how many other functional disorders may involve visceral hypersensitivity, it’s easy to estimate that VH affects at least 10% of the population.
Who does visceral hypersensitivity affect?
Visceral hypersensitivity usually accompanies another functional disorder. However, not everyone with a functional disorder appears to have visceral hypersensitivity. It also has a significant overlap with stress-related mood disorders. And there is some evidence that it may run in families. VH is twice as common in people assigned female at birth as it is in those assigned male at birth.
And there is some evidence that it may run in families. VH is twice as common in people assigned female at birth as it is in those assigned male at birth.
You may be more likely to have visceral hypersensitivity if you have:
- Irritable bowel syndrome (IBS).
- Functional dyspepsia.
- Noncardiac chest pain.
- Anismus.
- Interstitial cystitis.
- Fibromyalgia.
- Dysmenorrhea.
- Anxiety disorders.
- Depression.
- A family history of functional pain disorders.
- History of “colic” as a baby.
- Assigned female sex.
Symptoms and Causes
What does visceral hypersensitivity feel like?
In language, the word “visceral” implies a deep-down, intuitive feeling, as in “a visceral reaction." It's also closely associated with your gut, as in a “gut feeling." Visceral pain has these qualities.
It can be diffuse, or not as precisely located as somatic pain from an injury, even when it is intense.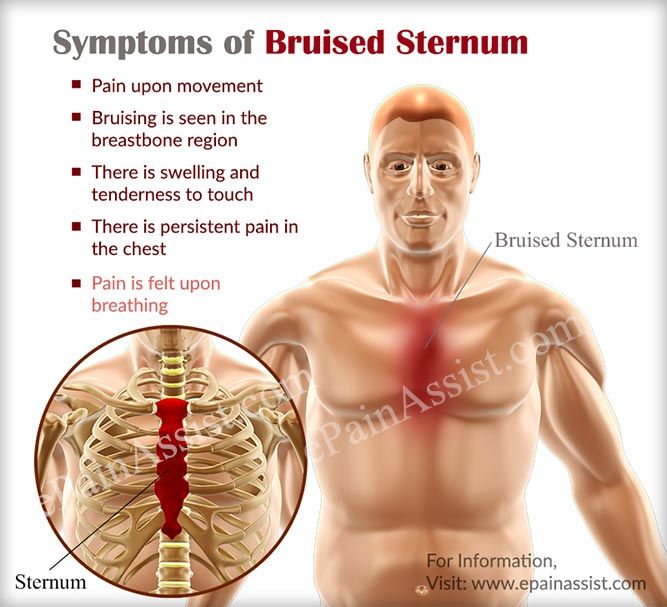 It commonly affects the gut, causing symptoms of abdominal pain, nausea and indigestion, even when the source of the pain is located elsewhere. It also may feel closely tied to your emotional or mental state. Pain in the visceral organs can both trigger and be triggered by mental/emotional distress.
It commonly affects the gut, causing symptoms of abdominal pain, nausea and indigestion, even when the source of the pain is located elsewhere. It also may feel closely tied to your emotional or mental state. Pain in the visceral organs can both trigger and be triggered by mental/emotional distress.
What are visceral symptoms?
People with visceral hypersensitivity tend to feel chronic discomfort in their chest, tummy or lower organs. Chronic pain is defined as lasting consistently for more than three months. It may come and go, or it may be triggered by certain bodily functions, such as a full bladder or swallowing food. The organs affected may include your:
- Esophagus.
- Heart.
- Lungs.
- Stomach.
- Pancreas.
- Small Intestine.
- Large Intestine.
- Bladder.
- Urethra.
- Uterus.
- Rectum.
Visceral pain can be diffused or difficult to localize, and it can sometimes radiate somewhere else.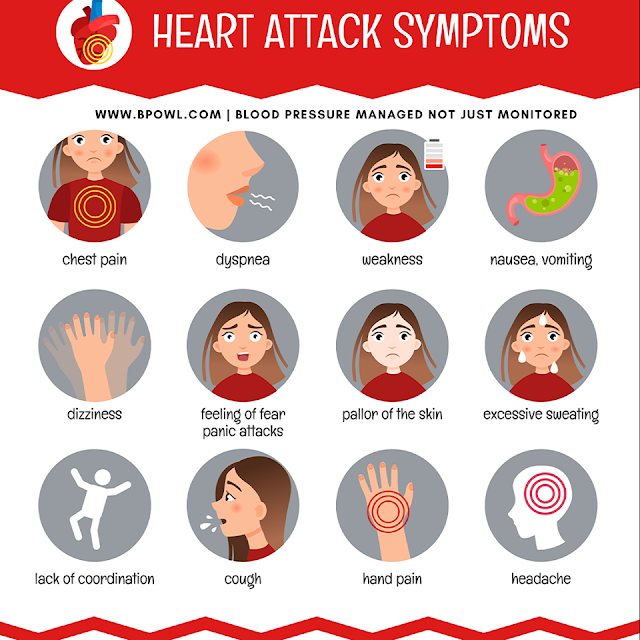 This can make it tricky to pin down and diagnose. One telltale feature of visceral pain is that it may produce strong autonomic responses from your body, such as:
This can make it tricky to pin down and diagnose. One telltale feature of visceral pain is that it may produce strong autonomic responses from your body, such as:
- Pallor.
- Sweating.
- Whole-body motor responses.
- Changes in body temperature.
- Changes in blood pressure.
- Changes in heart rate.
People with VH may also have other symptoms of functional gastrointestinal disorders. These disorders exhibit the same symptoms as inflammatory diseases, such as GERD, peptic ulcer disease and inflammatory bowel disease. The only difference is that with functional disorders, healthcare providers can’t detect any organic cause for them — no ulcers, no acid reflux, and no chronic inflammation.
Typical symptoms of functional GI disorders include:
- Heartburn.
- Chest pain.
- Indigestion.
- Bloated stomach.
- Abdominal pain.
- Nausea & vomiting.
- Diarrhea.
- Constipation.

Healthcare providers have also noted some less typical symptoms reported by people with IBS that may be related to visceral hypersensitivity. For example:
- Pain response to a light touch on your abdomen.
- Burning sensations referred to different parts of your body.
- Hypersensitivity to cold.
- Pain referred to your upper and lower extremities.
These symptoms suggest that, beyond simply physical irritants, the nervous system is involved.
What causes visceral hypersensitivity?
Researchers are still working to understand exactly how visceral hypersensitivity develops. They speculate that the neurological response to pain may become overly sensitized by either severe or repeated exposure to physical, mental and/or emotional stress. Researchers have found several factors that may combine to lead to this response to pain. Some of these factors include:
- Genes. Certain people may be genetically predisposed to develop hypersensitive responses that are biased toward enhanced pain perception.
- Early life trauma. Early childhood is a crucial period for the development of the brain circuitry that regulates stress and pain perception. Early life trauma is one factor that could change the way this circuitry develops, especially if there is already a genetic predisposition toward hypersensitivity. This could include mental/emotional trauma or a significant illness, infection or injury in childhood.
- Psychological disorders. Some of the same mechanics that predispose toward pain disorders can also predispose toward psychological disorders such as anxiety and depression. By the same token, people with psychological disorders are more frequently activating their pain and stress circuitry, driving it toward sensitization.
- Social stress factors. Adult life has many common stress factors, but with adequate social support and physical resilience, most people can weather them. Some adults are more vulnerable, however, because of the many factors listed above.
 Without adequate coping mechanisms, some develop chronic pain syndromes.
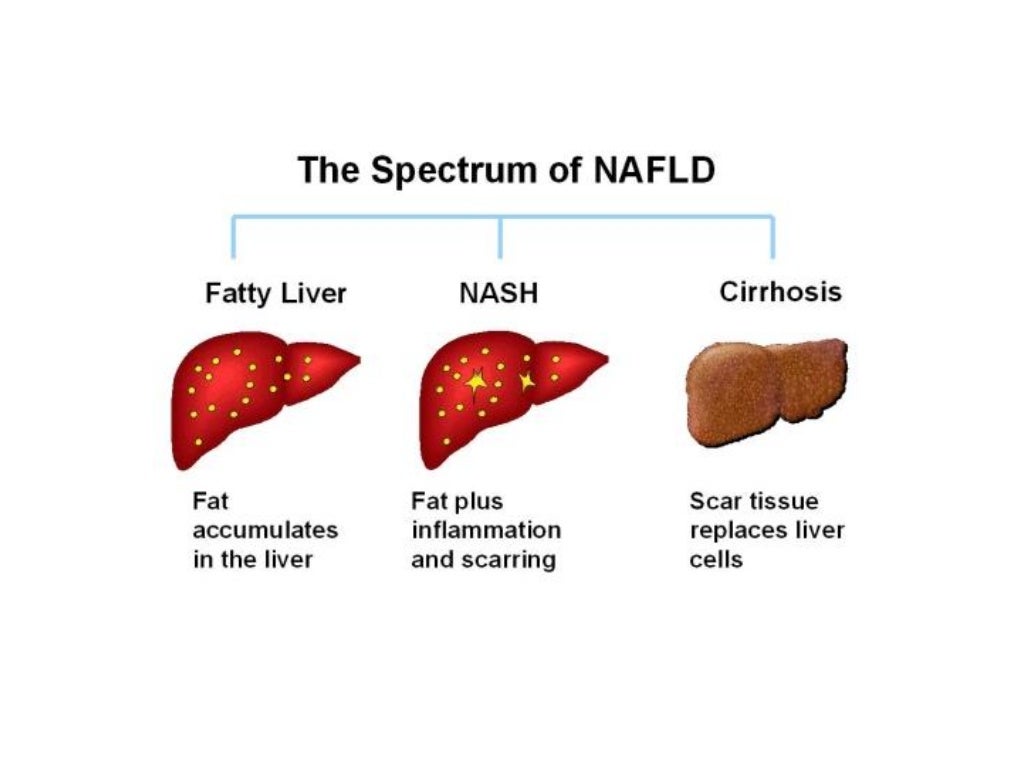
Without adequate coping mechanisms, some develop chronic pain syndromes. - Leaky gut syndrome. Several organic causes, as well as chronic stress, may cause chronic low-grade inflammation in the gut. This can erode the protective lining in your GI tract. One theory is that this may allow inflammatory agents to permeate the gut barrier and activate the central nervous system.
- Bad gut microbiome. The balance of bacteria that live in your gut can affect your visceral pain sensitivity. Gut bacteria communicate with the central nervous system about how your gut is doing. Though it’s unclear why, overgrowth of the wrong kind, or eradication of beneficial bacteria by antibiotics, is associated with visceral hypersensitivity.
When your nervous system has already been primed for a hyper-reactive pain response, visceral pain may begin either at the site of the organ or in the brain as a pathophysiologic response to stress. Healthcare providers have noted that visceral hypersensitivity often develops following a specific event.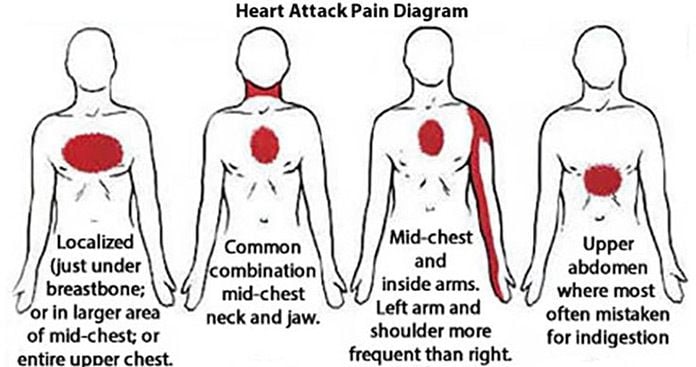 For example, an injury or infection or severe stress may have caused acute pain and inflammation in one of your organs. But after the emergency passed, your nerves continued to interpret normal sensations as pain and send those pain signals to your brain.
For example, an injury or infection or severe stress may have caused acute pain and inflammation in one of your organs. But after the emergency passed, your nerves continued to interpret normal sensations as pain and send those pain signals to your brain.
These nerves send pain signals to the part of your brain that registers pain, which signals to your brain regions that process the emotional part of the pain. An emotional response is part of your body’s way of teaching you to avoid whatever injured you. But this neural pathway also works in the reverse, where stress and emotions can enhance the perception of physical pain or irritation in the visceral organs. With visceral hypersensitivity, physical pain and emotional stress can constantly reinforce each other. Your brain responds to both with stress hormones, which make symptoms worse.
How does visceral sensitivity contribute to functional gastrointestinal disorders such as IBS?
Your digestive system has its own nervous system, the enteric nervous system, which extends throughout the gastrointestinal tract. This is sometimes referred to as your “second brain” or the “brain in your gut." The enteric nervous system has nerve endings in every layer of the digestive organs. These nerve endings are activated by all kinds of things: digestive contents, bacteria and bacterial byproducts, stretch and distension, inflammation and chemical stress signals.
This is sometimes referred to as your “second brain” or the “brain in your gut." The enteric nervous system has nerve endings in every layer of the digestive organs. These nerve endings are activated by all kinds of things: digestive contents, bacteria and bacterial byproducts, stretch and distension, inflammation and chemical stress signals.
These nerves communicate discomfort to your brain, but they also signal your body to respond to the perceived threat in various ways: slowing or accelerating the digestive processes, purging out infectious agents and so on. If these nerves become chronically overexcited, they may perpetually trigger these kinds of responses, leading to symptoms of illness. Alternatively, VH may simply cause you to interpret normal gastrointestinal function as painful.
Diagnosis and Tests
How is visceral hypersensitivity diagnosed?
Although a variety of tests are used to diagnose VH in clinical studies, they aren’t normally given to patients seeking medical care.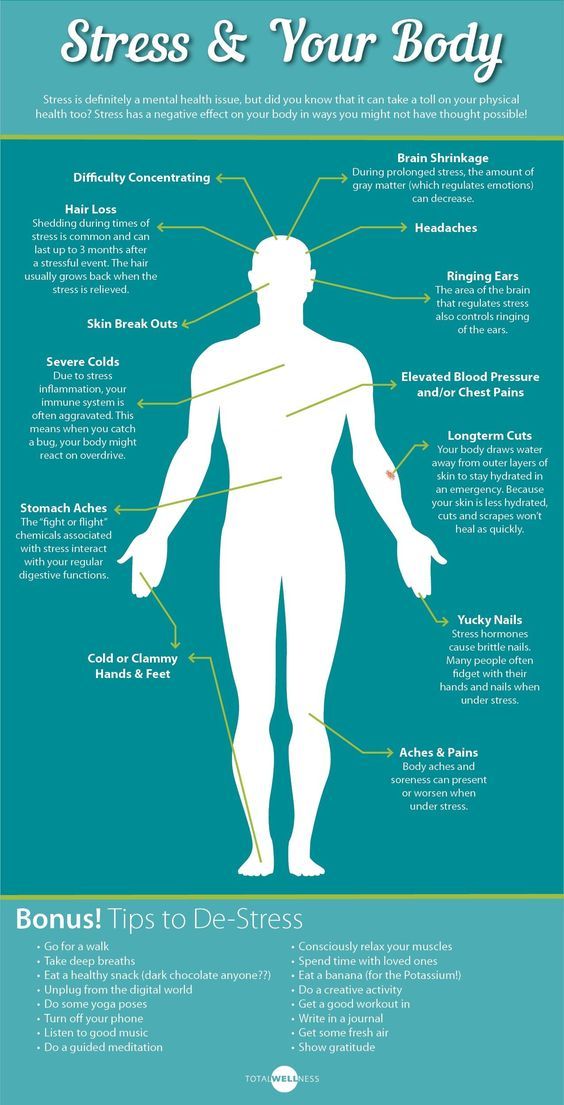 Visceral hypersensitivity is more often diagnosed the way other functional disorders are: by observing your symptoms and ruling out any structural causes for them. You’ll give a complete medical history and receive a complete exam before any standard tests are ordered. If these come back negative, you may be diagnosed with VH.
Visceral hypersensitivity is more often diagnosed the way other functional disorders are: by observing your symptoms and ruling out any structural causes for them. You’ll give a complete medical history and receive a complete exam before any standard tests are ordered. If these come back negative, you may be diagnosed with VH.
Management and Treatment
What treatment is available for visceral hypersensitivity?
Researchers are still investigating new ways of targeting visceral hypersensitivity. Currently, treatment usually involves a combination of pharmaceutical and mind/body therapies. Since this condition equally involves your physical organs and your brain, approaching it from both sides is more pragmatic and has a better chance of long-term success.
Medications
Medications for VH are targeted to calm your nervous system. Typical pain medications don’t work for this type of pain. Heavy pain blockers like narcotics and opioids are not recommended because their side effects can make things worse.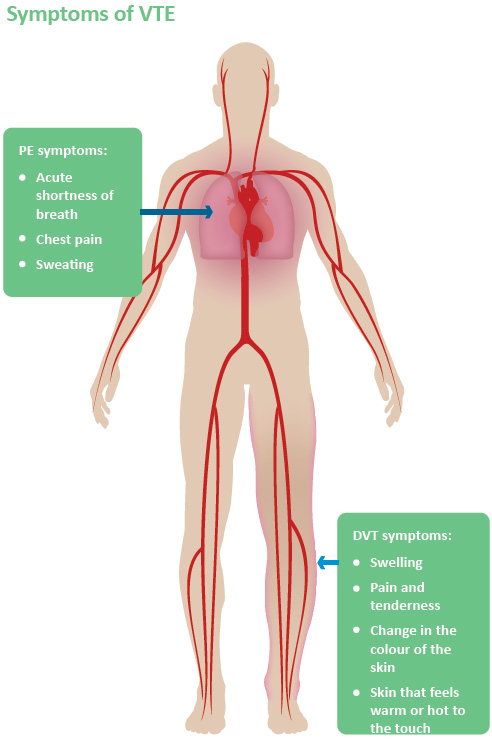 Instead, healthcare providers typically prescribe the same medications they would for psychological mood disorders such as anxiety and depression, only in much lower doses.
Instead, healthcare providers typically prescribe the same medications they would for psychological mood disorders such as anxiety and depression, only in much lower doses.
This isn't because they are presuming that you have mood disorders. Some people with VH do, but some don’t. If psychological symptoms are enhancing your pain threshold, these medications will help raise that threshold. But they also help numb the pain signals from the nerves themselves. Treating the pain itself can help reduce stress hormones and put your body and brain in a better place to benefit from mind/body therapies.
Antidepressants include:
- Tricyclic antidepressants.
- Selective serotonin reuptake inhibitors (SSRIs).
- Selective noradrenaline and serotonin inhibitors (SNRI).
Other medications that may help with nerve pain include:
- Histamine h2 receptor antagonists.
- Anti-epileptic drugs.
Mind/body therapies
Medications can help treat your symptoms, but they don’t treat the underlying condition. That’s what mind/body therapies try to do. Taking advantage of neuroplasticity — the ability of your nervous system and brain to learn new patterns — these therapies attempt to stop nerve pain from initiating in the first place. Recommended therapies include:
That’s what mind/body therapies try to do. Taking advantage of neuroplasticity — the ability of your nervous system and brain to learn new patterns — these therapies attempt to stop nerve pain from initiating in the first place. Recommended therapies include:
- Cognitive behavioral therapy. This is a long-term, systematic way of retraining your nervous system’s response to sensation from the “top down” — that is, from the level of the mind.
- Hypnotherapy. The power of suggestion in a hypnotic state may help to calm nervous pain response.
- Biofeedback. This therapy method uses equipment to measure your physical responses to pain and draw your attention to those responses. Then you can work on changing them.
Complimentary medicine
These recommendations have not been thoroughly tested but have shown promise for helping to treat visceral hypersensitivity.
- Probiotics.
 Following the theory that an imbalanced gut microbiome may contribute to visceral hypersensitivity, probiotics and prebiotics may help symptoms.
Following the theory that an imbalanced gut microbiome may contribute to visceral hypersensitivity, probiotics and prebiotics may help symptoms. - Acupuncture. Acupuncture has been shown effective in treating chronic pain in some people.
- Psychotherapy. If it’s indicated, psychotherapy for related anxiety and depression may help relieve mental/emotional stress and affect your pain perception.
Outlook / Prognosis
Can visceral hypersensitivity be cured?
We don’t know. There have been inspiring reports of certain therapies significantly improving the condition for certain people. But this likely depends on many factors, including the original cause of their symptoms and how many other contributing factors are affecting their hypersensitivity. The good news is that research is ongoing and many promising avenues are being explored for targeting visceral hypersensitivity.
Living With
Can diet help with my visceral hypersensitivity symptoms?
Diet is often recommended to help with IBS symptoms.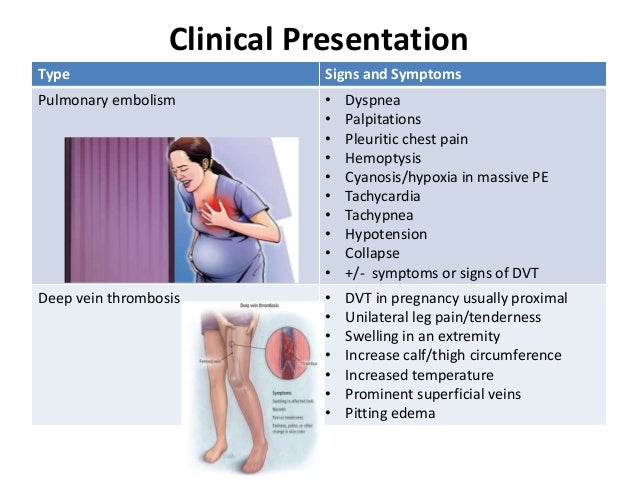 If your visceral sensitivity occurs in your GI tract, diet may help by reducing the discomfort associated with poor digestion.
If your visceral sensitivity occurs in your GI tract, diet may help by reducing the discomfort associated with poor digestion.
Digestion is not necessarily a component of visceral hypersensitivity. However, if you do have intolerances to certain foods, they could cause chronic low-grade inflammation, eroding your gut barrier, and over-feeding bad gut bacteria that feed on the carbohydrates that you can’t digest. All of these effects have been suggested as contributing causes of visceral hypersensitivity. In this case, the following diets might help:
- Elimination diet. This is a temporary diet to identify food intolerances. It removes common trigger foods and then adds them gradually back in as you watch your symptoms.
- Low FODMAP diet. This is a specific elimination diet that targets the carbohydrates that most commonly cause digestive distress. If you have bacterial overgrowth, the low FODMAP diet will help reduce it by starving them of the carbohydrates they depend on.

- Probiotic foods. If a bad gut microbiome is contributing to your troubles, probiotics may help. One of the best ways to get your daily probiotics is through probiotic foods, such as yogurt and cottage cheese, sauerkraut and miso soup.
A note from Cleveland Clinic
Visceral hypersensitivity is a complex problem, and treating it requires a holistic approach. Healthcare providers increasingly recognize the importance of the gut-brain connection. Researchers are working to better understand the ways that our brains, organs and nervous systems communicate with each other, and how this might go wrong.
One thing’s for sure: Visceral pain isn’t “all in your head." But it is a little bit. That makes it trickier to target than a mechanical problem, but it also gives you some power. By activating the power of your brain, you can work to change your own neural pathways to reduce pain.
Chest pain - causes, symptoms and diagnosis, indications for seeking medical attention
Almost everyone perceives chest pain as a potential heart problem. However, there can be many reasons for discomfort. In any case, it is impossible to determine on your own what caused the discomfort. Only a qualified doctor can determine the cause.
Wrong diagnosis, lack of treatment, uncontrolled attempts to anesthetize the place of discomfort often lead to the development of severe pathologies.
To make sure that the pain is not a sign of a serious illness or to choose a treatment for an identified pathology, it is better to visit a doctor. Causes of pain can be caused by diseases of the heart, lungs, gastrointestinal tract and neurological problems. If you do not know which doctor to make an appointment with first of all, come to the Kutuzov Medical and Diagnostic Center. We have all the experts who will help you make an accurate diagnosis. Start by making an appointment with a therapist and follow his instructions.
Such different chest pains
Thoracalgia is a term for chest pain (from the words "torax" - chest and "algia" - pain).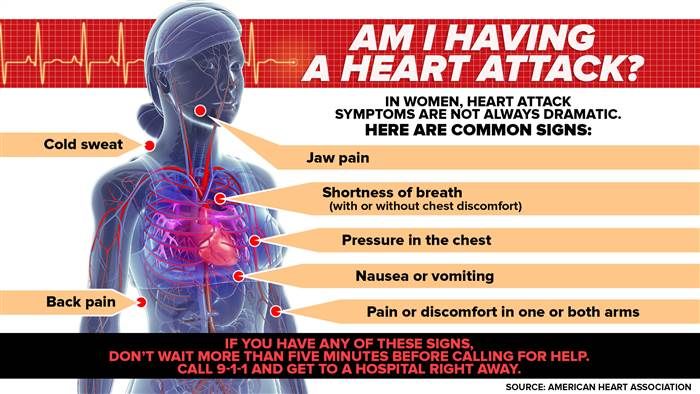
It can hurt, both on one side of the chest, and in the middle, in the upper or lower part. The nature of the pain is:
- Pungent and burning.
- Dull and aching.
- Stab.
- Compressive.
Among the main causes of a disturbing symptom in the chest are diseases, injuries and pathologies:
- Heart and vessels.
- Lungs.
- Musculoskeletal system - muscles, ribs and spine.
- Nervous system
- Gastrointestinal tract.
Let's dwell on them in more detail.
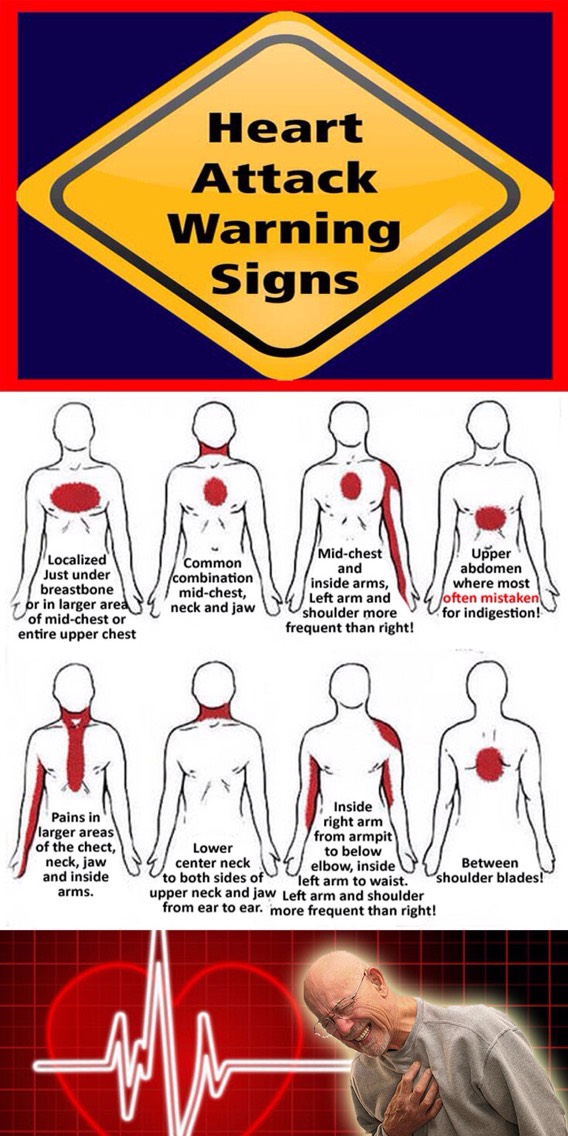
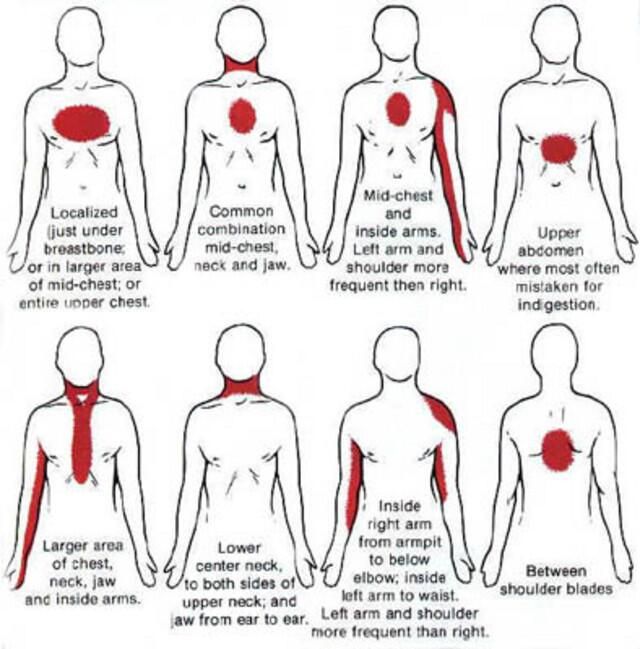
Heart problems
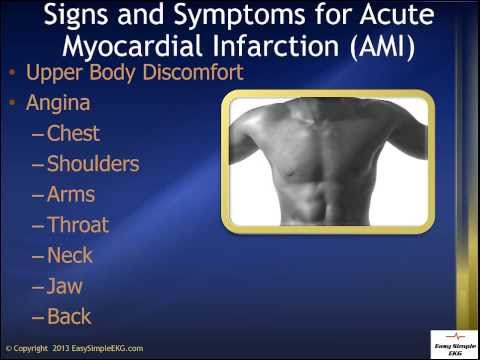
Pain in the chest in the middle or in its left side occurs in various diseases of the heart:
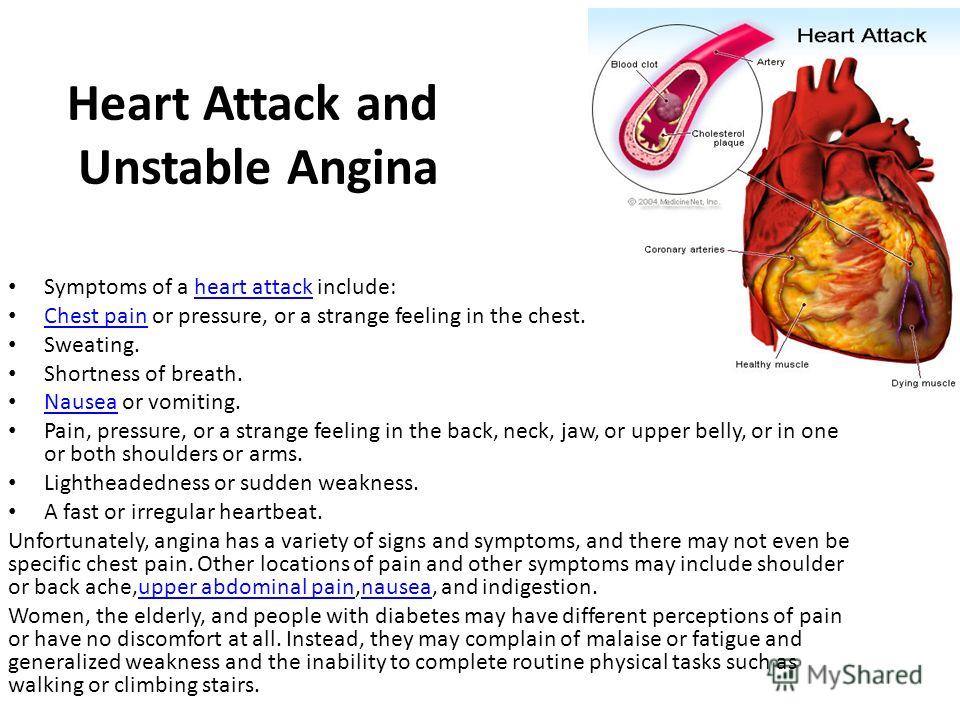
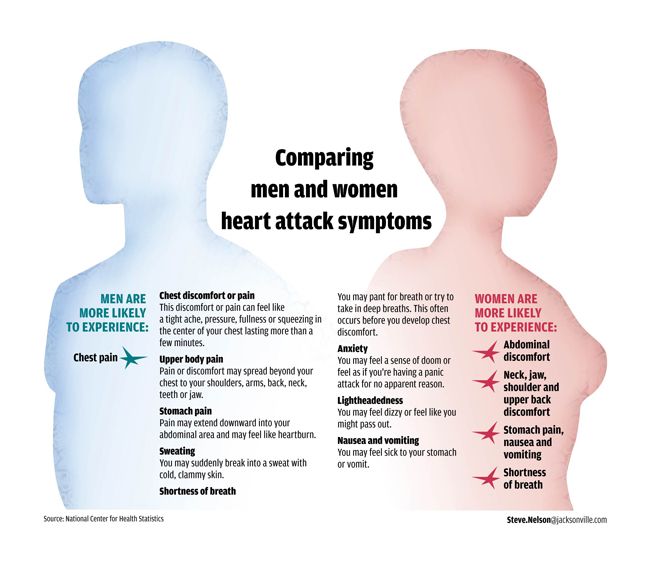
- coronary artery disease, angina pectoris - impaired blood flow in the heart arteries. Often an attack of sharp pain lasts up to 15 minutes. Occurs during physical exertion, stress, excitement, disappears after rest.
- Myocardial infarction - cell death and scarring of the heart muscle.
 It is characterized by severe pain in the chest on the left and in the middle, which does not go away after 15-20 minutes. Additional symptoms include weakness, fear of death.
It is characterized by severe pain in the chest on the left and in the middle, which does not go away after 15-20 minutes. Additional symptoms include weakness, fear of death. - Pericarditis or myocarditis is an inflammatory process in the muscle or lining of the heart. They are characterized by acute or aching pain in the chest when inhaling in the middle of the chest, which are aggravated by eating or lying down.
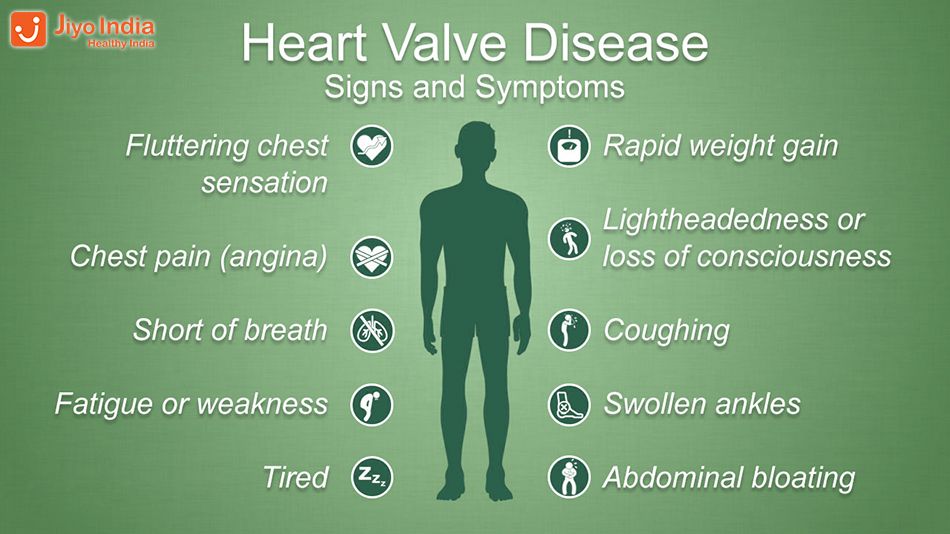
- Mitral valve prolapse - in addition to chest pain, it causes shortness of breath, dizziness, up to fainting.
- Pulmonary hypertension - increased pressure in the pulmonary arteries, the attack is similar to a heart attack.
A characteristic feature of heart pain is that it often occurs against the background of emotional or physical stress, accompanied by a feeling of panic, fear of death.
Lung diseases
This is a common cause of chest discomfort. Main causes and characteristic symptoms:
- Inflammation or abscess of the lung - the process proceeds with severe pain in the chest (right or both parts of the chest), fever, cough.
- Pleurisy (inflammation of the pleura) - there is pain with a deep breath, usually accompanied by fever, cough.
- Thromboembolism of the pulmonary artery with a blood clot - there is a sharp pain in the chest, tachycardia, difficulty breathing.
- Pneumothorax - accumulation of air in the pleural cavity when the lungs are damaged due to injuries of the ribs, spine. There is pain when inhaling, shortness of breath, dry cough, blood pressure may decrease.
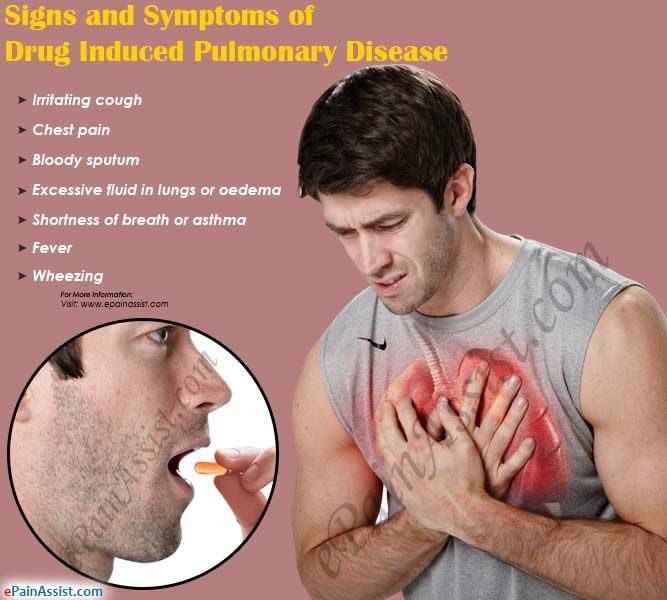
- Bronchial asthma - acute spasms resolve with chest pain and wheezing, wet cough, bouts of shortness of breath
Diseases of the gastrointestinal tract
Major diseases that cause pain in the esophagus or may spread from the abdomen to the chest area:
- Gastroesophageal reflux disease (GERD) - irritation of the esophageal mucosa due to reflux of gastric contents.
- Dyskinesia or perforation of the esophagus - increased pressure in the esophagus due to the slow movement of food or rupture due to injury.
- Gastric ulcers.
Gastrointestinal diseases are characterized by pain that occurs before, after or during meals, and may be accompanied by heartburn and other symptoms.
Injuries and diseases of the musculoskeletal system
Thoracalgia appears due to injuries, diseases of the spine, aggravated after physical exertion. Main causes and symptoms:
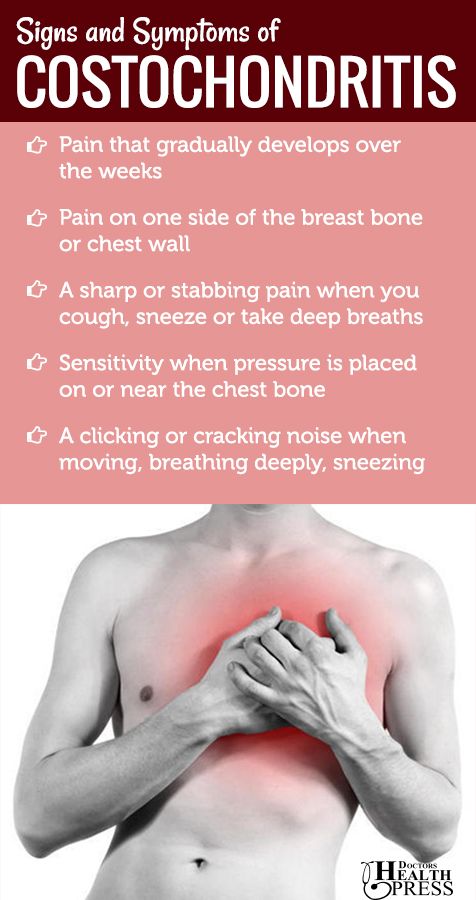
- Osteochondrosis, herniation and protrusion of the intervertebral discs in the thoracic spine, scoliosis cause chest pain, which is aggravated by movement or prolonged immobility.
- Rib fractures.
- Muscle spasms, sprains, intercostal neuralgia - cause pain in the chest on the right or left, depending on the place where the pathology has arisen.
- Tietze's syndrome or inflammation of the costocartilaginous joints.
- Pain of a neurological nature - from "goosebumps" in the chest to severe pain occurs due to mental disorders, with panic attacks.

Pain in the right or left side of the chest may have other causes: neoplasms in the lungs or breast, shingles and other diseases.
The doctor's task is to make a diagnosis in time and correctly. This will help: heart examinations, ultrasound, radiography and other diagnostic procedures.
Medical emergency needed if:
- Acute chest pain does not improve after 15 minutes and after rest.
- There is dizziness, shortness of breath, increased sweating, palpitations.
In other cases, it is also advisable not to postpone the consultation with the doctor for a long time. Who to contact - a cardiologist, a neurologist, a gastroenterologist - depends on the symptoms. But this is not always possible to determine independently. In this case, start with a consultation with a therapist who will help you understand the issue and, if necessary, refer you to a specialist.
In other cases, it is also advisable not to postpone the consultation with a doctor for a long time.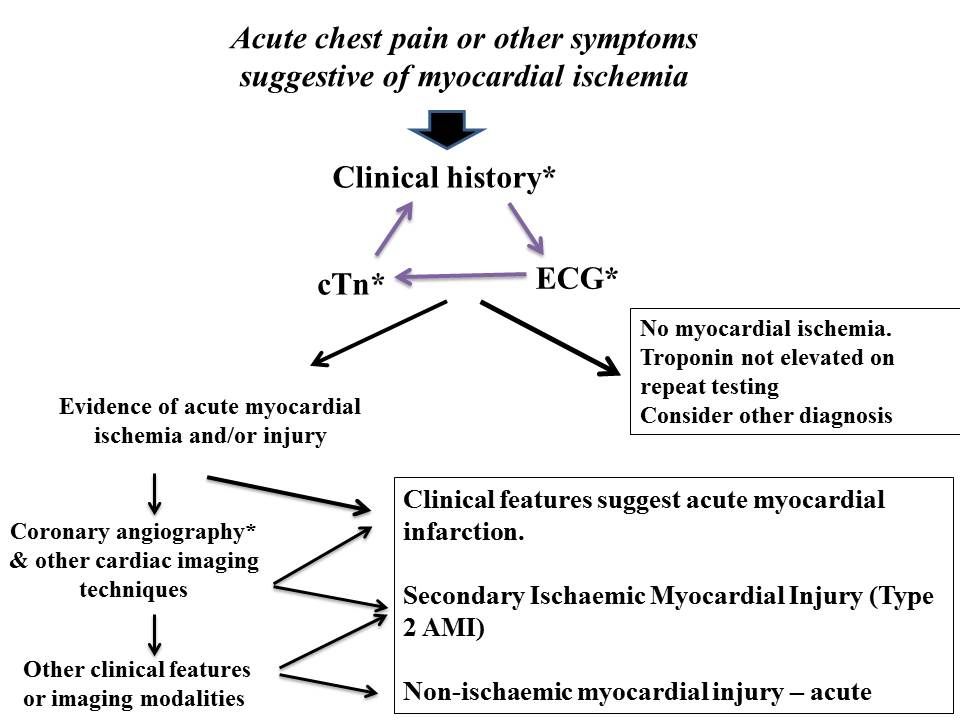 Who to contact - a cardiologist, a neurologist, a gastroenterologist - depends on the symptoms. But this is not always possible to determine independently. In this case, start with a consultation with a therapist who will help you understand the issue and, if necessary, refer you to a specialist. Be healthy!
Who to contact - a cardiologist, a neurologist, a gastroenterologist - depends on the symptoms. But this is not always possible to determine independently. In this case, start with a consultation with a therapist who will help you understand the issue and, if necessary, refer you to a specialist. Be healthy!
Diagnosis of any disease requires modern equipment and vast medical experience. Especially when it comes to chest pain.
Our clinic offers its patients a full range of medical examinations on high-precision equipment. Our doctors select the most informative and safe diagnostic methods.
Turning to us, you can be sure that the cause of the pain will be established as quickly and accurately as possible. High-tech diagnostic devices allow you to monitor the work of all organs and systems without causing you unnecessary discomfort.
We value the time of our patients, so all consultations and procedures are by appointment. By booking an appointment, you can be sure that the doctor will be waiting for you.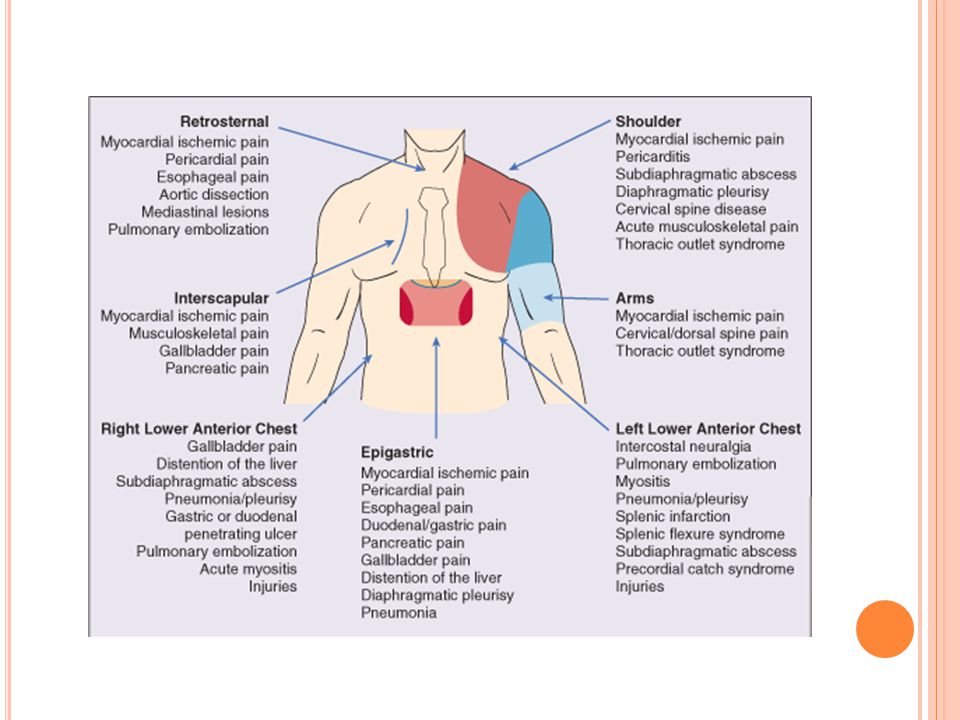 Come to the clinic to find out the cause of pain and discuss treatment options.
Come to the clinic to find out the cause of pain and discuss treatment options.
Chest pain treatment prices
| Title | Price | |
|---|---|---|
| Reception (examination, consultation) of a general practitioner primary | 2200 ₽ | Enroll |
| Repeated appointment (examination, consultation) with a general practitioner | 1900 ₽ | Enroll |
Publication checked:
Pilenitsyn Andrey Yurievich
Experience: 24 years old
Cardiologist of the highest qualification category, general practitioner
Make an appointment
Make an appointment
Name
Phone
By clicking on the "Sign up" button, you consent to the processing of personal data
Chest pain as a symptom of other diseases: which doctor to consult
Chest pain can be a symptom of dozens of diseases related to the heart, stomach, lungs, musculoskeletal and neurological problems.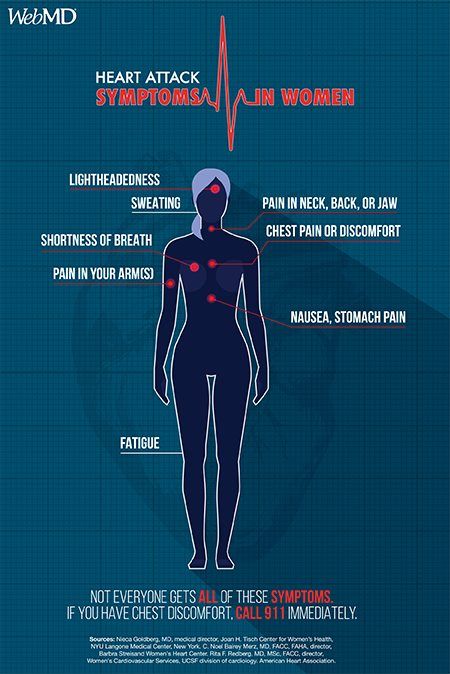 Some situations require urgent medical attention, others do not need treatment. But only a specialist after a comprehensive diagnosis can determine the danger of the cause of pain. For any pain in the chest, contact the NeoMed diagnostic center in Anapa. Here the source of anxiety will be determined and a treatment plan will be drawn up.
Some situations require urgent medical attention, others do not need treatment. But only a specialist after a comprehensive diagnosis can determine the danger of the cause of pain. For any pain in the chest, contact the NeoMed diagnostic center in Anapa. Here the source of anxiety will be determined and a treatment plan will be drawn up.
What can hurt in the chest
Pain in the chest area is familiar to people of all ages. Painful sensations occur in the middle of the chest, on the left, on the right, in the lower or upper part. They are aching, burning, sharp, growing. They last several minutes or for a long time, return periodically, accompanying some specific actions: coughing, inhaling, increased stress.
Inside the breast cage are large vessels, heart, lungs, esophagus, muscles and ligaments. All this can cause pain of a different nature.
It is customary to classify two types of chest pains :
- Vertebrogenic - associated with the pathology of the spine.
- Non-vertebrogenic - caused by diseases of the vessels and internal organs, as well as those of a psychogenic nature.
But it is often very difficult to determine what exactly hurts and where in the chest. After all, pain can occur next to the problem area from pinched nerves or an inflammatory process, be radiating or wandering.
Causes of chest pain
Although chest pain is not always due to cardiac disorders, these problems can rightly be put in the first place.
The nature of pain in heart disease :
- Angina pectoris - compressive nature, radiating to the shoulder, occurs with increased exertion, for example, when walking fast or climbing stairs.
- Heart attack - prolonged (more than 20 minutes) intense chest pain of a pressing nature, shortness of breath, fear of death. Need urgent help.
- Myocarditis - not strong, but pressing, combined with an accelerated heartbeat.
- Pericarditis - acute, exacerbated by the horizontal position of the body.
- Cardiomyopathy - moderate, appears after exercise and eating.
Cardiac pains are usually difficult to localize and intermittent in cases of slowly progressive disease.
Problems of the respiratory system cause different types of pain in the chest:
- Bronchitis - tense, aggravated by coughing.
- Pulmonary embolism - acute, similar to a heart attack, urgent medical attention is required.
- Collapsed lung - accompanied by severe dyspnea.
- Pneumonia - stabbing, worse on inspiration.
- Pleurisy - accompanies every breath, becomes more noticeable when coughing.
- COPD - pressing with wheezing and cough.
- Lung cancer - irregular, may be accompanied by cough with sputum and hemoptysis.
It is important to know that there are no pain receptors in the lungs, so the muscles in the chest hurt from tension or inflammation. Sensations can be localized in the middle or intensified by inflammation.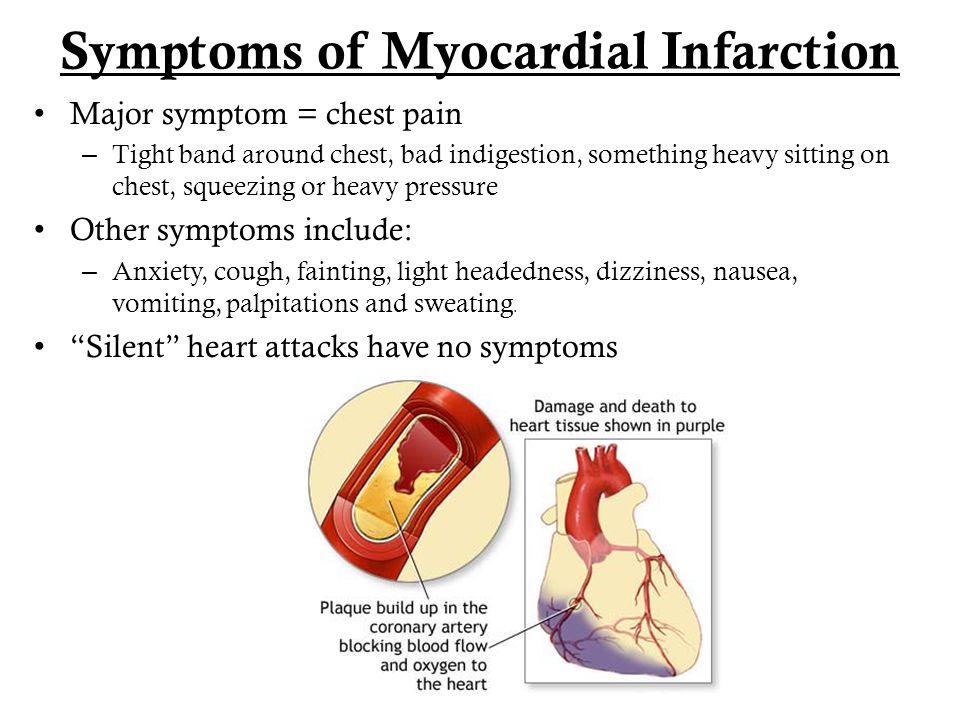
Causes and types of pain in the chest with problems with the digestive system :
- Disorders of the esophagus - appear in the process of swallowing.
- Diseases of the gallbladder and pancreas - accompanied by pain in the upper abdomen.
- Gastroesophageal reflux - accompanied by heartburn: burning behind the sternum.
- Gastritis, gastric ulcer - aching dull pain on the left under the ribs or on the left in the sternum.
Musculoskeletal pain in the chest area causes rib injuries, scoliosis, cartilage disease, thoracic osteochondrosis, the symptoms of which are very similar to a heart attack. A pinched nerve is accompanied by numbness of the problem area. Muscular dull pains of an unknown nature can disturb a long period of time. They are safe, but it is important to rule out life-threatening causes.
Pain in the chest also with panic attacks and intercostal neuralgia, which is characterized by pinching sensations in the middle of the sternum. In women, diseases of the mammary glands and cyclic changes in the hormonal background can provoke painful conditions.
In women, diseases of the mammary glands and cyclic changes in the hormonal background can provoke painful conditions.
Which doctor to contact for diagnosis
The variety of causes makes it difficult to diagnose, but in case of intermittent or long-term disturbing pains, it is important to establish their true cause. Taking painkillers can only aggravate the situation, because chest pain is just a symptom, behind which there is some process that destroys the body.
Since there are many diseases, it is best to consult a general practitioner first. After listening to complaints, he will prescribe preliminary studies: a blood test, ECG, fluorography (X-ray), if necessary, a CT scan of the chest, he will refer to narrow specialists for a more detailed examination. You may need to do an ultrasound, gastroscopy, bronchoscopy, mammography (for women).
If you are concerned about chest pain or other discomfort in the chest, come for a consultation at the NeoMed Medical Center in Anapa.