Celiac disease bipolar disorder
The Burden of Depressive and Bipolar Disorders in Celiac Disease
1. Carta M.G., Hardoy M.C., Boi M.F., Mariotti S., Carpiniello B., Usai P. Association between panic disorder, major depressive disorder and celiac disease: a possible role of thyroid autoimmunity. J. Psychosom. Res. 2002;53(3):789–793. doi: 10.1016/S0022-3999(02)00328-8. [PubMed] [CrossRef] [Google Scholar]
2. Zingone F., Swift G.L., Card T.R., Sanders D.S., Ludvigsson J.F., Bai J.C. Psychological morbidity of celiac disease: A review of the literature. United European Gastroenterol. J. 2015;3(2):136–145. doi: 10.1177/2050640614560786. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
3. Hernanz A., Polanco I. Plasma precursor amino acids of central nervous system monoamines in children with coeliac disease. Gut. 1991;32(12):1478–1481. doi: 10.1136/gut.32.12.1478. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
4. Postal M., Appenzeller S. The importance of cytokines and autoantibodies in depression. Autoimmun. Rev. 2015;14(1):30–35. doi: 10.1016/j.autrev.2014.09.001. [PubMed] [CrossRef] [Google Scholar]
5. Hardoy M.C., Cadeddu M., Serra A., Moro M.F., Mura G., Mellino G., Bhat K.M., AltoA(c) G., Usai P., Piga M., Carta M.G. A pattern of cerebral perfusion anomalies between major depressive disorder and Hashimoto thyroiditis. BMC Psychiatry. 2011;11:148. doi: 10.1186/1471-244X-11-148. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
6. Hamdani N., Doukhan R., Kurtlucan O., Tamouza R., Leboyer M. Immunity, inflammation, and bipolar disorder: diagnostic and therapeutic implications. Curr. Psychiatry Rep. 2013;15(9):387. doi: 10.1007/s11920-013-0387-y. [PubMed] [CrossRef] [Google Scholar]
7. Carta M.G., Carpiniello B., Kovess V., Porcedda R., Zedda A., Rudas N. Lifetime prevalence of major depression and dystymia. Eur. Neuropsychopharmacol. 1995;5:103–107. doi: 10.1016/0924-977X(95)00036-O. [PubMed] [CrossRef] [Google Scholar]
8. Hardoy M.C., Carta M.G., Marci A.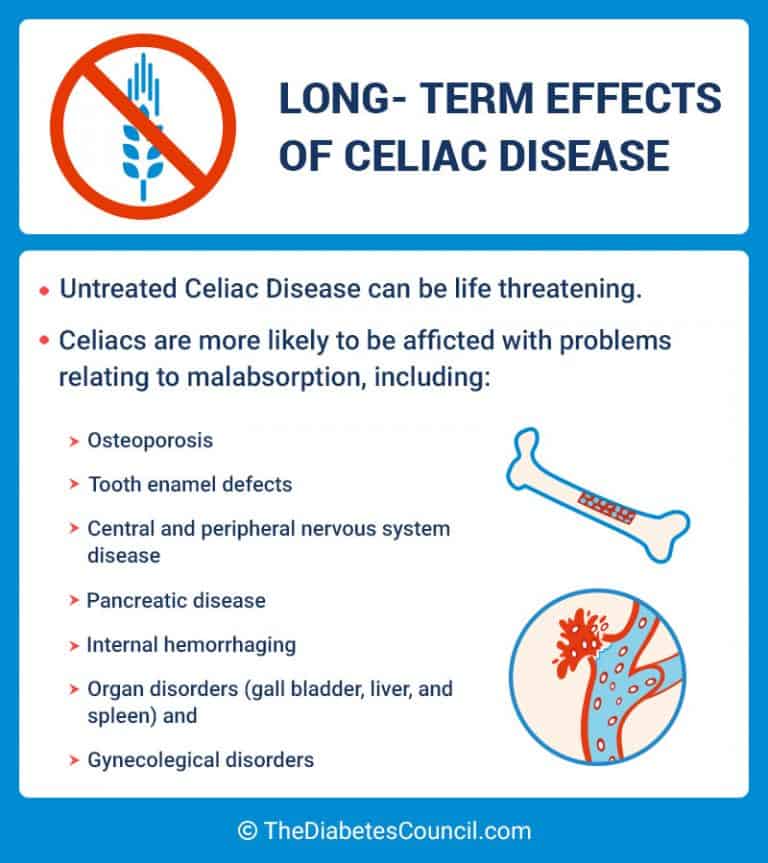 R., Carbone F., Cadeddu M., Kovess V., Dell 'Osso L., Carpiniello B. Exposure to aircraft noise and risk of psychiatric disorders: the Elmas survey--aircraft noise and psychiatric disorders. Soc. Psychiatry Psychiatr. Epidemiol. 2005;40(1):24–26. doi: 10.1007/s00127-005-0837-x. [PubMed] [CrossRef] [Google Scholar]
R., Carbone F., Cadeddu M., Kovess V., Dell 'Osso L., Carpiniello B. Exposure to aircraft noise and risk of psychiatric disorders: the Elmas survey--aircraft noise and psychiatric disorders. Soc. Psychiatry Psychiatr. Epidemiol. 2005;40(1):24–26. doi: 10.1007/s00127-005-0837-x. [PubMed] [CrossRef] [Google Scholar]
9. LA vdahl H., BA,en E., Malt E.A., Malt U.F. Somatic and cognitive symptoms as indicators of potential endophenotypes in bipolar spectrum disorders: an exploratory and proof-of-concept study comparing bipolar II disorder with recurrent brief depression and healthy controls. J. Affect. Disord. 2014;166:59–70. doi: 10.1016/j.jad.2014.04.056. [PubMed] [CrossRef] [Google Scholar]
10. Carta M.G., Aguglia E., Balestrieri M., Calabrese J.R., Caraci F., Dell 'Osso L., Di Sciascio G., Drago F., Faravelli C., Lecca M.E., Moro M.F., Nardini M., Palumbo G., Hardoy M.C. The lifetime prevalence of bipolar disorders and the use of antidepressant drugs in bipolar depression in Italy.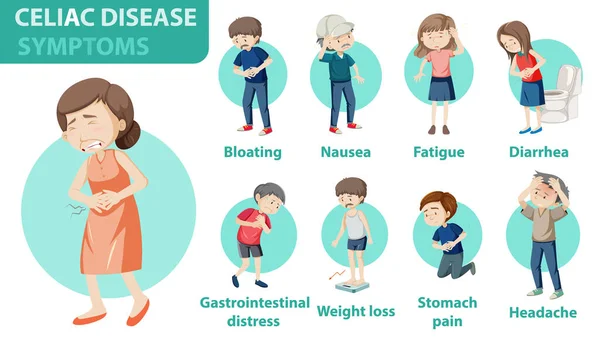 J. Affect. Disord. 2012;136(3):775–780. doi: 10.1016/j.jad.2011.09.041. [PubMed] [CrossRef] [Google Scholar]
J. Affect. Disord. 2012;136(3):775–780. doi: 10.1016/j.jad.2011.09.041. [PubMed] [CrossRef] [Google Scholar]
11. Mantovani G., Astara G., Lampis B., Bianchi A., Curreli L., OrrA1 W., Carta M.G., Carpiniello B., Contu P., Rudas N. Evaluation by multidimensional instruments of health-related quality of life of elderly cancer patients undergoing three different ?opsychosocial ?? treatment approaches. A randomized clinical trial. Support. Care Cancer. 1996;4(2):129–140. doi: 10.1007/BF01845762. [PubMed] [CrossRef] [Google Scholar]
12. Mantovani G., Astara G., Lampis B., et al. Impact of psychosocial intervention on the quality of life of elderly cancer patients. Psychooncology. 1996;5:127–135. doi: 10.1002/(SICI)1099-1611(199606)5:2<127::AID-PON220>3.0.CO;2-L. [CrossRef] [Google Scholar]
13. Carta M.G., Aguglia E., Bocchetta A., Balestrieri M., Caraci F., Casacchia M., Dell 'osso L., Sciascio G.D., Drago F., Faravelli C., Lecca M.E., Moro M.F., Morosini P.L., Nardini M. , Palumbo G., Hardoy M.C. The use of antidepressant drugs and the lifetime prevalence of major depressive disorders in Italy. Clin. Pract. Epidemol Ment. Health. 2010;6:94–100. doi: 10.2174/1745017901006010094. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
, Palumbo G., Hardoy M.C. The use of antidepressant drugs and the lifetime prevalence of major depressive disorders in Italy. Clin. Pract. Epidemol Ment. Health. 2010;6:94–100. doi: 10.2174/1745017901006010094. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
14. First M., Spitzer R., Gibbon M., Williams J. Structured clinical interview for DSM-IV axis I disorders, research version, non-patient edition (SCID-I/NP). New York: Biometrics Research, New York State Psychiatric Institute; 1997. [Google Scholar]
15. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4 th ed., Text Revision. Washington, DC: APA Press; 2000. [Google Scholar]
16. Hirschfeld R.M., Calabrese J.R., Weissman M.M., Reed M., Davies M.A., Frye M.A., Keck P.E., Jr, Lewis L., McElroy S.L., McNulty J.P., Wagner K.D. Screening for bipolar disorder in the community. J. Clin. Psychiatry. 2003;64(1):53–59. doi: 10.4088/JCP.v64n0111. [PubMed] [CrossRef] [Google Scholar]
17. Hardoy M.C., Cadeddu M., Murru A., Dell Osso B., Carpiniello B., Morosini P.L., Calabrese J.R., Carta M.G. Validation of the Italian version of the ?oMood Disorder Questionnaire ?? for the screening of bipolar disorders. Clin. Pract. Epidemol Ment. Health. 2005;1:8. doi: 10.1186/1745-0179-1-8. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
Hardoy M.C., Cadeddu M., Murru A., Dell Osso B., Carpiniello B., Morosini P.L., Calabrese J.R., Carta M.G. Validation of the Italian version of the ?oMood Disorder Questionnaire ?? for the screening of bipolar disorders. Clin. Pract. Epidemol Ment. Health. 2005;1:8. doi: 10.1186/1745-0179-1-8. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
18. Ware J., Jr, Kosinski M., Keller S.D. A 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Med. Care. 1996;34(3):220–233. doi: 10.1097/00005650-199603000-00003. [PubMed] [CrossRef] [Google Scholar]
19. Fasano A, Catassi C. Clinical practice. Celiac disease. . N Engl J Med . 2001;367(25):2419–26. [PubMed] [Google Scholar]
20. Chow M.A., Lebwohl B., Reilly N.R., Green P.H. Immunoglobulin A deficiency in celiac disease. J. Clin. Gastroenterol. 2012;46(10):850–854. doi: 10.1097/MCG.0b013e31824b2277. [PubMed] [CrossRef] [Google Scholar]
21. Loft D.E., Marsh M.N., Crowe P.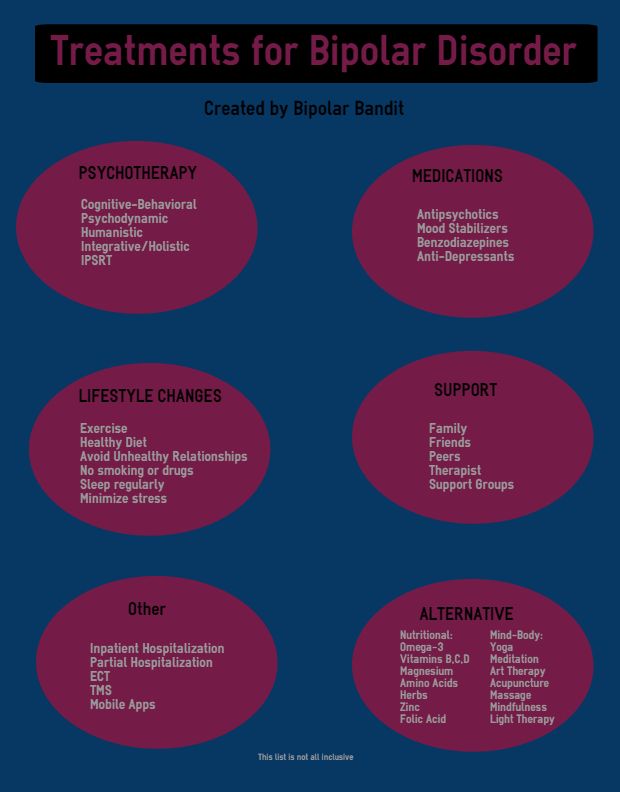 T. Rectal gluten challenge and diagnosis of coeliac disease. Lancet. 1990;336(8720):953. doi: 10.1016/0140-6736(90)92331-B. [PubMed] [CrossRef] [Google Scholar]
T. Rectal gluten challenge and diagnosis of coeliac disease. Lancet. 1990;336(8720):953. doi: 10.1016/0140-6736(90)92331-B. [PubMed] [CrossRef] [Google Scholar]
22. Setty M., Hormaza L., Guandalini S. Celiac disease: risk assessment, diagnosis, and monitoring. Mol. Diagn. Ther. 2008;12(5):289–298. doi: 10.1007/BF03256294. [PubMed] [CrossRef] [Google Scholar]
23. Carta M.G., Sorbello O., Moro M.F., Bhat K.M., Demelia E., Serra A., Mura G., Sancassiani F., Piga M., Demelia L. Bipolar disorders and Wilson's disease. BMC Psychiatry. 2012;12(1):52. doi: 10.1186/1471-244X-12-52. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
24. Carta M.G., Moro M.F., Aguglia E., Balestrieri M., Caraci F., Dell Osso L., Di Sciascio G., Drago F., Hardoy M.C., D Aloja E., Machado S., Roncone R., Faravelli C. The attributable burden of panic disorder in the impairment of quality of life in a national survey in Italy. Int. J. Soc. Psychiatry. 2015;61(7):693–699. doi: 10.1177/0020764015573848.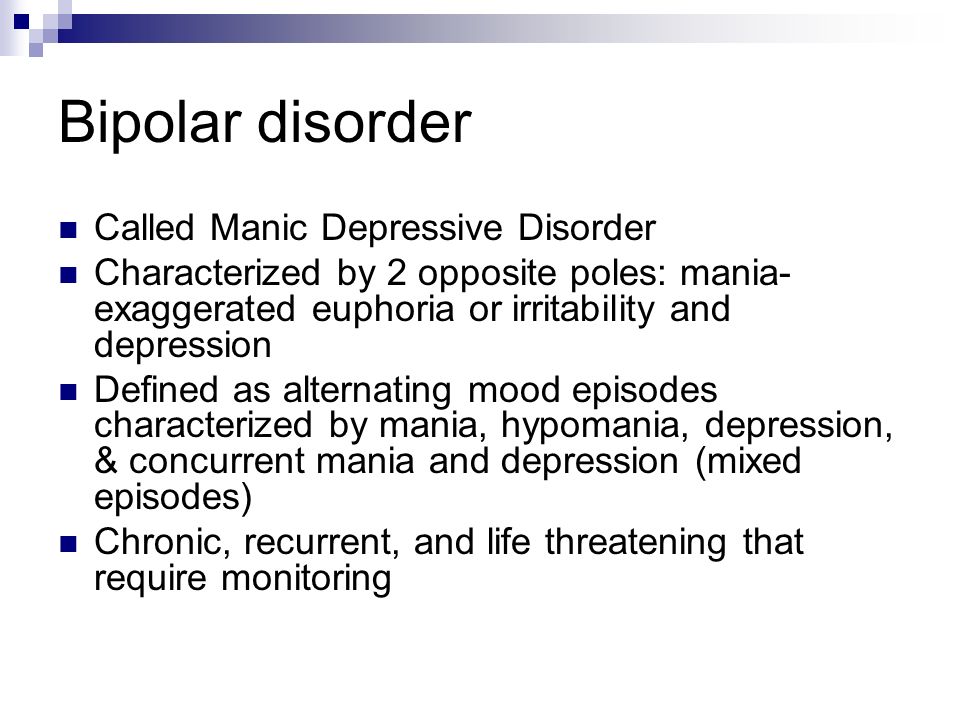 [PubMed] [CrossRef] [Google Scholar]
[PubMed] [CrossRef] [Google Scholar]
25. Carta M.G., Preti A., Moro M.F., Aguglia E., Balestrieri M., Caraci F., Dell (tm)Osso L., Di Sciascio G., Drago F., Faravelli C., Hardoy M.C., D (tm)Aloja E., Cossu G., CalA S., Palumbo G., Bhugra D. Eating disorders as a public health issue: prevalence and attributable impairment of quality of life in an Italian community sample. Int. Rev. Psychiatry. 2014;26(4):486–492. doi: 10.3109/09540261.2014.927753. [PubMed] [CrossRef] [Google Scholar]
26. Carta M.G., Moro M.F., Lorefice L., Picardi A., Trincas G., Fenu G., Cocco E., Floris F., Bessonov D., Akiskal H.S., Marrosu M.G. Multiple sclerosis and bipolar disorders: the burden of comorbidity and its consequences on quality of life. J. Affect. Disord. 2014;167:192–197. doi: 10.1016/j.jad.2014.05.024. [PubMed] [CrossRef] [Google Scholar]
27. Lecca M.E., Saba L., Sanfilippo R., et al. The role of co-morbid mood disorders. Clin Pract Psychiatr Epidemiol. in Press. [PMC free article] [PubMed] [Google Scholar]
28. Ludvigsson J.F., Reutfors J., Osby U., Ekbom A., Montgomery S.M. Coeliac disease and risk of mood disorders--a general population-based cohort study. J. Affect. Disord. 2007;99(1-3):117–126. doi: 10.1016/j.jad.2006.08.032. [PubMed] [CrossRef] [Google Scholar]
Ludvigsson J.F., Reutfors J., Osby U., Ekbom A., Montgomery S.M. Coeliac disease and risk of mood disorders--a general population-based cohort study. J. Affect. Disord. 2007;99(1-3):117–126. doi: 10.1016/j.jad.2006.08.032. [PubMed] [CrossRef] [Google Scholar]
29. Zimmerman M. Screening for bipolar disorder: confusion between case-finding and screening. Psychother. Psychosom. 2014;83(5):259–262. doi: 10.1159/000362564. [PubMed] [CrossRef] [Google Scholar]
30. Dickerson F., Stallings C., Origoni A., Vaughan C., Khushalani S., Alaedini A., Yolken R. Markers of gluten sensitivity and celiac disease in bipolar disorder. Bipolar Disord. 2011;13(1):52–58. doi: 10.1111/j.1399-5618.2011.00894.x. [PubMed] [CrossRef] [Google Scholar]
31. Saleem A., Connor H.J., Regan P.O. Adult coeliac disease in Ireland: a case series. Ir. J. Med. Sci. 2012;181(2):225–229. doi: 10.1007/s11845-011-0788-z. [PubMed] [CrossRef] [Google Scholar]
32. Avramopoulos D., Pearce B.D., McGrath J., Wolyniec P. , Wang R., Eckart N., Hatzimanolis A., Goes F.S., Nestadt G., Mulle J., Coneely K., Hopkins M., Ruczinski I., Yolken R., Pulver A.E. Infection and inflammation in schizophrenia and bipolar disorder: a genome wide study for interactions with genetic variation. PLoS One. 2015;10(3):e0116696. doi: 10.1371/journal.pone.0116696. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
, Wang R., Eckart N., Hatzimanolis A., Goes F.S., Nestadt G., Mulle J., Coneely K., Hopkins M., Ruczinski I., Yolken R., Pulver A.E. Infection and inflammation in schizophrenia and bipolar disorder: a genome wide study for interactions with genetic variation. PLoS One. 2015;10(3):e0116696. doi: 10.1371/journal.pone.0116696. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
33. Carta M.G., Norcini-Pala A., Moro M.F., Balestrieri M., Caraci F., Dell (tm)Osso L., Sciascio G.D., Faravelli C., Hardoy M.C., Aguglia E., Roncone R., Nardi A.E., Drago F. Does Mood Disorder Questionnaire identify sub-threshold bipolarity? Evidence studying worsening of quality of life. J. Affect. Disord. 2015;183:173–178. doi: 10.1016/j.jad.2015.04.058. [PubMed] [CrossRef] [Google Scholar]
34. Carta M.G., Moro M.F., Lorefice L., Trincas G., Cocco E., Del Giudice E., Fenu G., Colom F., Marrosu M.G. The risk of bipolar disorders in multiple sclerosis. J. Affect. Disord. 2014;155:255–260. doi: 10.1016/j.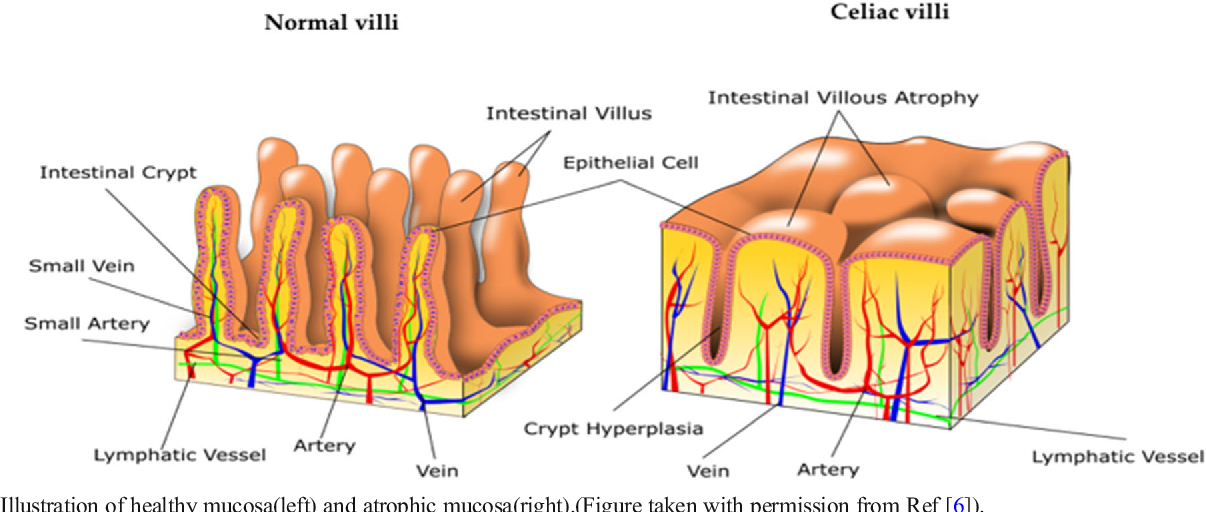 jad.2013.11.008. [PubMed] [CrossRef] [Google Scholar]
jad.2013.11.008. [PubMed] [CrossRef] [Google Scholar]
35. Angeli G., Pasquini R., Panella V., Pelli M.A. An epidemiologic survey of celiac disease in the Terni area (Umbria, Italy) in 2002-2010. J. Prev. Med. Hyg. 2012;53(1):20–23. [PubMed] [Google Scholar]
Mood Disorders and Gluten: It’s Not All in Your Mind! A Systematic Review with Meta-Analysis
1. Depression. [(accessed on 22 October 2018)]; Available online: http://www.who.int/news-room/fact-sheets/detail/depression
2. NHS . Statistics for England, 2002–2012. NHS; London, UK: 2013. Prescriptions Dispensed in the Community. [Google Scholar]
3. World Health Organization . Depression and Other Common Mental Disorders. World Health Organization; Geneva, Switzerland: 2017. Global Health Estimates. [Google Scholar]
4. Sapone A., Bai J.C., Ciacci C., Dolinsek J., Green P.H., Hadjivassiliou M., Kaukinen K., Rostami K., Sanders D.S., Schumann M., et al. Spectrum of gluten-related disorders: Consensus on new nomenclature and classification.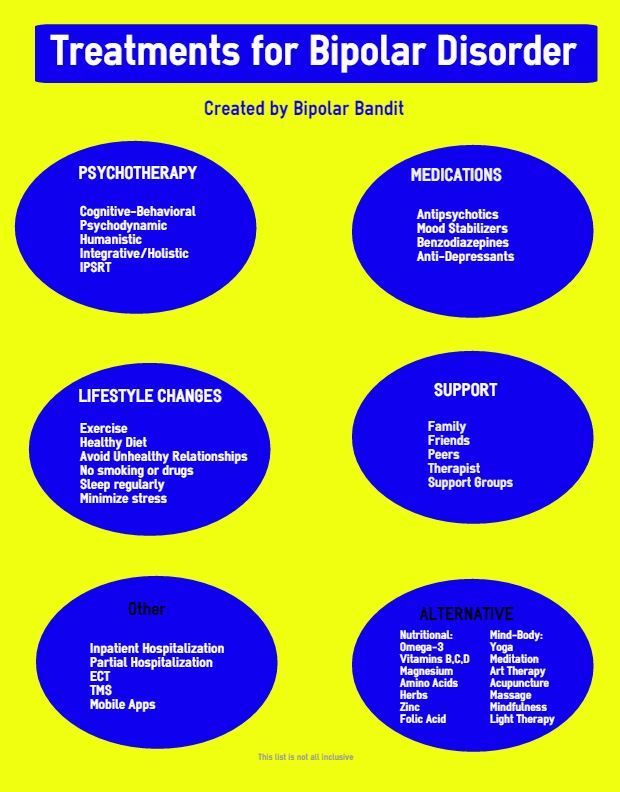 BMC Med. 2012;10:13. doi: 10.1186/1741-7015-10-13. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
BMC Med. 2012;10:13. doi: 10.1186/1741-7015-10-13. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
5. NIH In Proceedings of the NIH Consensus Development Conference on Celiac Disease; Bethesda, MD, USA. 28–30 June 2004; pp. 1–23. [Google Scholar]
6. Black J.L., Orfila C. Impact of coeliac disease on dietary habits and quality of life. J. Hum. Nutr. Diet. 2011;24:582–587. doi: 10.1111/j.1365-277X.2011.01170.x. [PubMed] [CrossRef] [Google Scholar]
7. Tack G.J., Verbeek W.H.M., Schreurs M.W.J., Mulder C.J.J. The spectrum of celiac disease: Epidemiology, clinical aspects and treatment. Nat. Rev. Gastroenterol. Hepatol. 2010;7:204–213. doi: 10.1038/nrgastro.2010.23. [PubMed] [CrossRef] [Google Scholar]
8. Addolorato G., Di Giuda D., De Rossi G., Valenza V., Domenicali M., Caputo F., Gasbarrini A., Capristo E., Gasbarrini G. Regional cerebral hypoperfusion in patients with celiac disease. Am. J. Med. 2004;116:312–317. doi: 10.1016/j.amjmed.2003.09.037. [PubMed] [CrossRef] [Google Scholar]
9. Smith D.F., Gerdes L.U. Meta-analysis on anxiety and depression in adult celiac disease: Anxiety and depression in celiac disease. Acta Psychiatr. Scand. 2012;125:189–193. doi: 10.1111/j.1600-0447.2011.01795.x. [PubMed] [CrossRef] [Google Scholar]
Smith D.F., Gerdes L.U. Meta-analysis on anxiety and depression in adult celiac disease: Anxiety and depression in celiac disease. Acta Psychiatr. Scand. 2012;125:189–193. doi: 10.1111/j.1600-0447.2011.01795.x. [PubMed] [CrossRef] [Google Scholar]
10. Ludvigsson J.F., Leffler D.A., Bai J., Biagi F., Fasano A., Green P.H., Hadjivassiliou M., Kaukinen K., Kelly C., Leonard J.N., et al. The Oslo definitions for coeliac disease and related terms. Gut. 2013;62:43. doi: 10.1136/gutjnl-2011-301346. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
11. Simsek S., Baysoy G., Gencoglan S., Uluca U. Effects of Gluten-Free Diet on Quality of Life and Depression in Children with Celiac Disease. J. Pediatr. Gastroenterol. Nutr. 2015;61:303. doi: 10.1097/MPG.0000000000000799. [PubMed] [CrossRef] [Google Scholar]
12. Liester M.B., Liester M.G. A Review of Psychiatric Disorders Associated with Celiac Disease. Dual Diagn. Open Access. 2017;3 doi: 10.21767/2472-5048.100035. [CrossRef] [Google Scholar]
13. Catassi C., Elli L., Bonaz B., Bouma G., Carroccio A., Castillejo G., Cellier C., Cristofori F., de Magistris L., Dolinsek J., et al. Diagnosis of Non-Celiac Gluten Sensitivity (NCGS): The Salerno Experts’ Criteria. Nutrients. 2015;7:4966–4977. doi: 10.3390/nu7064966. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
Catassi C., Elli L., Bonaz B., Bouma G., Carroccio A., Castillejo G., Cellier C., Cristofori F., de Magistris L., Dolinsek J., et al. Diagnosis of Non-Celiac Gluten Sensitivity (NCGS): The Salerno Experts’ Criteria. Nutrients. 2015;7:4966–4977. doi: 10.3390/nu7064966. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
14. Catassi C. Gluten Sensitivity. Ann. Nutr. Metab. 2015;67(Suppl. S2):16–26. doi: 10.1159/000440990. [PubMed] [CrossRef] [Google Scholar]
15. Volta U., Tovoli F., Cicola R., Parisi C., Fabbri A., Piscaglia M., Fiorini E., Caio G. Serological tests in gluten sensitivity (nonceliac gluten intolerance) J. Clin. Gastroenterol. 2012;46:680–685. doi: 10.1097/MCG.0b013e3182372541. [PubMed] [CrossRef] [Google Scholar]
16. Daynes G. Bread and Tears—Naughtiness, Depression and Fits Due to Wheat Sensitivity. Proc. R. Soc. Med. 1956;49:391–394. [PMC free article] [PubMed] [Google Scholar]
17. Carroccio A., Giambalvo O., Blasca F.L., Iacobucci R., D’Alcamo A. , Mansueto P. Self-Reported Non-Celiac Wheat Sensitivity in High School Students: Demographic and Clinical Characteristics. Nutrients. 2017;9:771. doi: 10.3390/nu9070771. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
, Mansueto P. Self-Reported Non-Celiac Wheat Sensitivity in High School Students: Demographic and Clinical Characteristics. Nutrients. 2017;9:771. doi: 10.3390/nu9070771. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
18. Harper L., Bold J.S. An exploration into the motivation for gluten avoidance in the absence of coeliac disease. Gastroenterol. Hepatol. Bed Bench. 2018 doi: 10.22037/ghfbb.v0i0.1268. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
19. Porcelli B., Verdino V., Ferretti F., Bizzaro N., Terzuoli L., Cinci F., Bossini L., Fagiolini A. A study on the association of mood disorders and gluten-related diseases. Psychiatry Res. 2018;260:366–370. doi: 10.1016/j.psychres.2017.12.008. [PubMed] [CrossRef] [Google Scholar]
20. Karakula-Juchnowicz H., Gałęcka M., Rog J., Bartnicka A., Łukaszewicz Z., Krukow P., Morylowska-Topolska J., Skonieczna-Zydecka K., Krajka T., Jonak K., et al. The Food-Specific Serum IgG Reactivity in Major Depressive Disorder Patients, Irritable Bowel Syndrome Patients and Healthy Controls.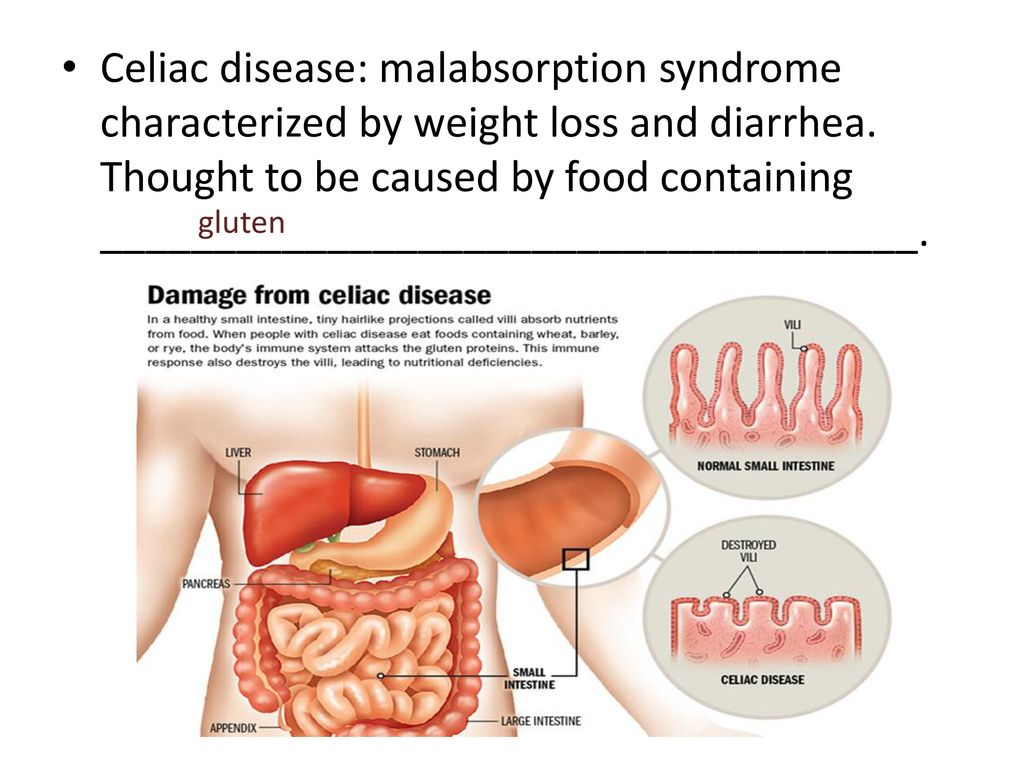 Nutrients. 2018;10:548. doi: 10.3390/nu10050548. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
Nutrients. 2018;10:548. doi: 10.3390/nu10050548. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
21. Jackson J., Eaton W., Cascella N., Fasano A., Santora D., Sullivan K., Feldman S., Raley H., McMahon R.P., Carpenter W.T.J., et al. Gluten sensitivity and relationship to psychiatric symptoms in people with schizophrenia. Schizophr. Res. 2014;159:539–542. doi: 10.1016/j.schres.2014.09.023. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
22. Dickerson F., Stallings C., Origoni A., Vaughan C., Khushalani S., Yolken R. Markers of gluten sensitivity in acute mania: A longitudinal study. Psychiatry Res. 2012;196:68–71. doi: 10.1016/j.psychres.2011.11.007. [PubMed] [CrossRef] [Google Scholar]
23. Karakuła-Juchnowicz H., Szachta P., Opolska A., Morylowska-Topolska J., Gałęcka M., Juchnowicz D., Krukow P., Lasik Z. The role of IgG hypersensitivity in the pathogenesis and therapy of depressive disorders. Nutr. Neurosci. 2017;20:110–118. doi: 10.1179/1476830514Y. 0000000158. [PubMed] [CrossRef] [Google Scholar]
0000000158. [PubMed] [CrossRef] [Google Scholar]
24. Fera T., Cascio B., Angelini G., Martini S., Guidetti C. Affective disorders and quality of life in adult coeliac disease patients on a gluten-free diet. Eur. J. Gastroenterol. Hepatol. 2003;15:1287–1292. doi: 10.1097/00042737-200312000-00006. [PubMed] [CrossRef] [Google Scholar]
25. Roos S., Kärner A., Hallert C. Gastrointestinal symptoms and well-being of adults living on a gluten-free diet: A case for nursing in celiac disease. Gastroenterol. Nurs. 2009;32:196–201. doi: 10.1097/SGA.0b013e3181a85e7b. [PubMed] [CrossRef] [Google Scholar]
26. Ruepert L., Quartero A.O., de Wit N.J., van der Heijden G.J., Rubin G., Muris J.W. Bulking agents, antispasmodics and antidepressants for the treatment of irritable bowel syndrome. Cochrane Database Syst. Rev. 2011:CD003460. doi: 10.1002/14651858.CD003460.pub3. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
27. Hallert C., Svensson M., Tholstrup J., Hultberg B. Clinical trial: B vitamins improve health in patients with coeliac disease living on a gluten-free diet.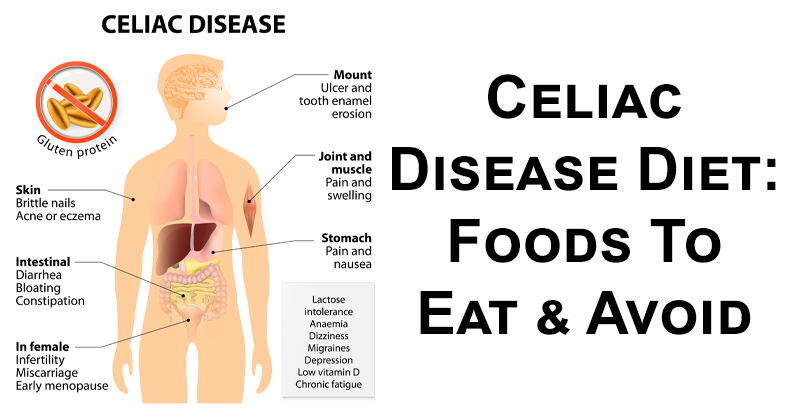 Aliment. Pharmacol. Therapeut. 2009;29:811–816. doi: 10.1111/j.1365-2036.2009.03945.x. [PubMed] [CrossRef] [Google Scholar]
Aliment. Pharmacol. Therapeut. 2009;29:811–816. doi: 10.1111/j.1365-2036.2009.03945.x. [PubMed] [CrossRef] [Google Scholar]
28. Biesiekierski J.R., Peters S.L., Newnham E.D., Rosella O., Muir J.G., Gibson P.R. No effects of gluten in patients with self-reported non-celiac gluten sensitivity after dietary reduction of fermentable, poorly absorbed, short-chain carbohydrates. Gastroenterology. 2013;145:320–328. doi: 10.1053/j.gastro.2013.04.051. [PubMed] [CrossRef] [Google Scholar]
29. Dieterich W., Schuppan D., Schink M., Schwappacher R., Wirtz S., Agaimy A., Neurath M.F., Zopf Y. Influence of low FODMAP and gluten-free diets on disease activity and intestinal microbiota in patients with non-celiac gluten sensitivity. Clin. Nutr. 2018 doi: 10.1016/j.clnu.2018.03.017. [PubMed] [CrossRef] [Google Scholar]
30. Horvath-Stolarczyk A., Sidor K., Dziechciarz P., Siemińska J. Assessment of emotional status, selected personality traits and depression in young adults with celiac disease. Pediatr. Wspolczesna. 2002;4:241–246. [Google Scholar]
Pediatr. Wspolczesna. 2002;4:241–246. [Google Scholar]
31. Cicarelli G., Della Rocca G., Amboni M., Ciacci C., Mazzacca G., Filla A., Barone P. Clinical and neurological abnormalities in adult celiac disease. Neurol. Sci. 2003;24:311–317. doi: 10.1007/s10072-003-0181-4. [PubMed] [CrossRef] [Google Scholar]
32. Burger J.P.W., de Brouwer B., IntHout J., Wahab P.J., Tummers M., Drenth J.P.H. Systematic review with meta-analysis: Dietary adherence influences normalization of health-related quality of life in coeliac disease. Clin. Nutr. 2017;36:399–406. doi: 10.1016/j.clnu.2016.04.021. [PubMed] [CrossRef] [Google Scholar]
33. Shahbazkhani B., Sadeghi A., Malekzadeh R., Khatavi F., Etemadi M., Kalantri E., Rostami-Nejad M., Rostami K. Non-Celiac Gluten Sensitivity Has Narrowed the Spectrum of Irritable Bowel Syndrome: A Double-Blind Randomized Placebo-Controlled Trial. Nutrients. 2015;7:4542–4554. doi: 10.3390/nu7064542. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
34. Caio G., Volta U., Tovoli F., De Giorgio R. Effect of gluten free diet on immune response to gliadin in patients with non-celiac gluten sensitivity. BMC Gastroenterol. 2014;14:26. doi: 10.1186/1471-230X-14-26. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
Caio G., Volta U., Tovoli F., De Giorgio R. Effect of gluten free diet on immune response to gliadin in patients with non-celiac gluten sensitivity. BMC Gastroenterol. 2014;14:26. doi: 10.1186/1471-230X-14-26. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
35. Sainsbury K., Marques M.M. The relationship between gluten free diet adherence and depressive symptoms in adults with coeliac disease: A systematic review with meta-analysis. Appetite. 2018;120:578–588. doi: 10.1016/j.appet.2017.10.017. [PubMed] [CrossRef] [Google Scholar]
36. Vazquez-Roque M.I., Camilleri M., Smyrk T., Murray J.A., Marietta E., O’Neill J., Carlson P., Lamsam J., Janzow D., Eckert D., et al. A controlled trial of gluten-free diet in patients with irritable bowel syndrome-diarrhea: Effects on bowel frequency and intestinal function. Gastroenterology. 2013;144:903–911. doi: 10.1053/j.gastro.2013.01.049. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
37. Soares F.L.P., de Oliveira Matoso R. , Teixeira L.G., Menezes Z., Pereira S.S., Alves A.C., Batista N.V., de Faria A.M.C., Cara D.C., Ferreira A.V.M., et al. Gluten-free diet reduces adiposity, inflammation and insulin resistance associated with the induction of PPAR-alpha and PPAR-gamma expression. J. Nutr. Biochem. 2013;24:1105–1111. doi: 10.1016/j.jnutbio.2012.08.009. [PubMed] [CrossRef] [Google Scholar]
, Teixeira L.G., Menezes Z., Pereira S.S., Alves A.C., Batista N.V., de Faria A.M.C., Cara D.C., Ferreira A.V.M., et al. Gluten-free diet reduces adiposity, inflammation and insulin resistance associated with the induction of PPAR-alpha and PPAR-gamma expression. J. Nutr. Biochem. 2013;24:1105–1111. doi: 10.1016/j.jnutbio.2012.08.009. [PubMed] [CrossRef] [Google Scholar]
38. Mulloy A., Lang R., O’Reilly M., Sigafoos J., Lancioni G., Rispoli M. Gluten-free and casein-free diets in the treatment of autism spectrum disorders: A systematic review. Res. Autism Spectr. Disord. 2010;4:328–339. doi: 10.1016/j.rasd.2009.10.008. [CrossRef] [Google Scholar]
39. Piwowarczyk A., Horvath A., Łukasik J., Pisula E., Szajewska H. Gluten- and casein-free diet and autism spectrum disorders in children: A systematic review. Eur. J. Nutr. 2018;57:433–440. doi: 10.1007/s00394-017-1483-2. [PubMed] [CrossRef] [Google Scholar]
40. Brietzke E., Cerqueira R.O., Mansur R.B., McIntyre R.S. Gluten related illnesses and severe mental disorders: A comprehensive review. Neurosci. Biobehav. Rev. 2018;84:368–375. doi: 10.1016/j.neubiorev.2017.08.009. [PubMed] [CrossRef] [Google Scholar]
Neurosci. Biobehav. Rev. 2018;84:368–375. doi: 10.1016/j.neubiorev.2017.08.009. [PubMed] [CrossRef] [Google Scholar]
41. Losurdo G., Principi M., Iannone A., Amoruso A., Ierardi E., Leo A.D., Barone M. Extra-intestinal manifestations of non-celiac gluten sensitivity: An expanding paradigm. World J. Gastroenterol. 2018;24:1521–1530. doi: 10.3748/wjg.v24.i14.1521. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
42. Peters S.L., Biesiekierski J.R., Yelland G.W., Muir J.G., Gibson P.R. Randomised clinical trial: Gluten may cause depression in subjects with non-coeliac gluten sensitivity—An exploratory clinical study. Aliment. Pharmacol. Therapeut. 2014;39:1104–1112. doi: 10.1111/apt.12730. [PubMed] [CrossRef] [Google Scholar]
43. Joelson A.M., Geller M.G., Zylberberg H.M., Green P.H.R., Lebwohl B. The Effect of Depressive Symptoms on the Association between Gluten-Free Diet Adherence and Symptoms in Celiac Disease: Analysis of a Patient Powered Research Network. Nutrients. 2018;10:538. doi: 10.3390/nu10050538. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
2018;10:538. doi: 10.3390/nu10050538. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
44. Wolf R.L., Lebwohl B., Lee A.R., Zybert P., Reilly N.R., Cadenhead J., Amengual C., Green P.H.R. Hypervigilance to a Gluten-Free Diet and Decreased Quality of Life in Teenagers and Adults with Celiac Disease. Digest. Dis. Sci. 2018;63:1438–1448. doi: 10.1007/s10620-018-4936-4. [PubMed] [CrossRef] [Google Scholar]
45. The Cochrane Collaboration . In: Cochrane Handbook for Systematic Reviews of Interventions. Higgins J., Green S., editors. The Cochrane Collaboration; London, UK: 2011. [Google Scholar]
46. Higgins J., Sterne J.A., Savović J., Page M., Hróbjartsson A., Boutron I., Reeves B.C., Eldridge S. A revised tool for assessing risk of bias in randomized trials. Cochrane Database Syst. Rev. 2016;10(Suppl. S1) doi: 10.1002/14651858.CD201601. [CrossRef] [Google Scholar]
47. Sterne J.A., Hernán M.A., Reeves B.C., Savović J., Berkman N.D., Viswanathan M., Henry D., Altman D.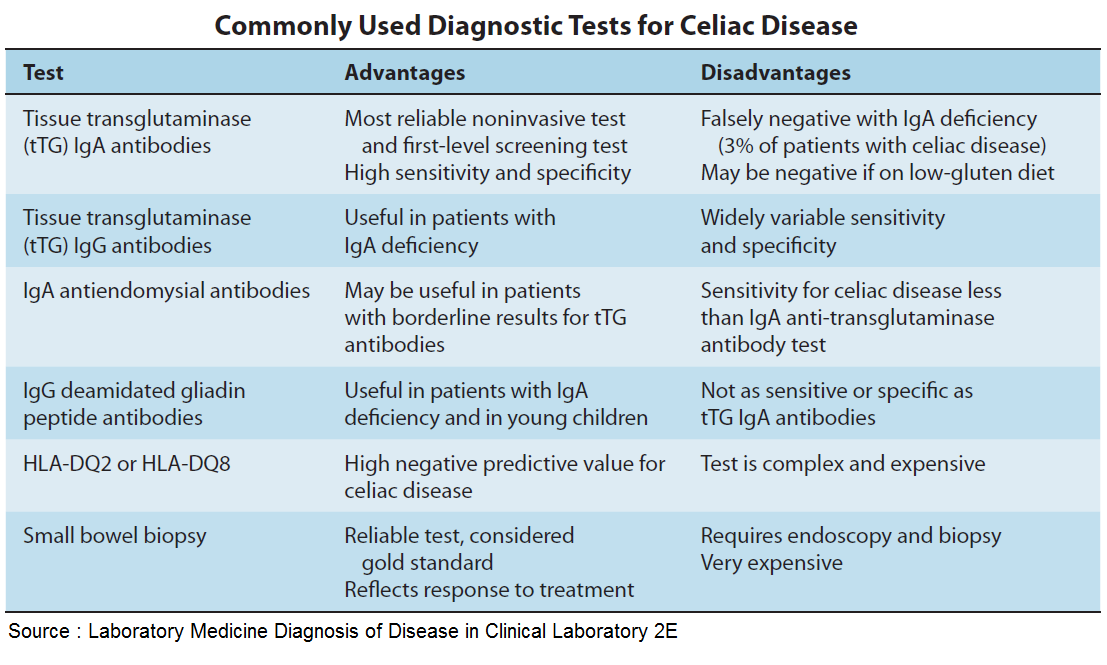 G., Ansari M.T., Boutron I., et al. ROBINS-I: A tool for assessing risk of bias in non-randomised studies of interventions. BMJ. 2016;355:i4919. doi: 10.1136/bmj.i4919. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
G., Ansari M.T., Boutron I., et al. ROBINS-I: A tool for assessing risk of bias in non-randomised studies of interventions. BMJ. 2016;355:i4919. doi: 10.1136/bmj.i4919. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
48. Guyatt G.H., Oxman A.D., Vist G.E., Kunz R., Falck-Ytter Y., Alonso-Coello P., Schünemann H.J. GRADE: An emerging consensus on rating quality of evidence and strength of recommendations. BMJ. 2008;336:924–926. doi: 10.1136/bmj.39489.470347.AD. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
49. The GRADE Working Group . In: GRADE Handbook for Grading Quality of Evidence and Strength of Recommendations. Schünemann H., Brożek J., Guyatt G., Oxman A., editors. The GRADE Working Group; Hamilton, ON, Canada: 2013. Updated October 2013. [Google Scholar]
50. Evidence Prime, Inc. GRADEpro GDT: GRADEpro Guideline Development Tool [Software] McMaster University; Hamilton, ON, Canada: 2015. [Google Scholar]
51. Higgins J.P.T., Thompson S.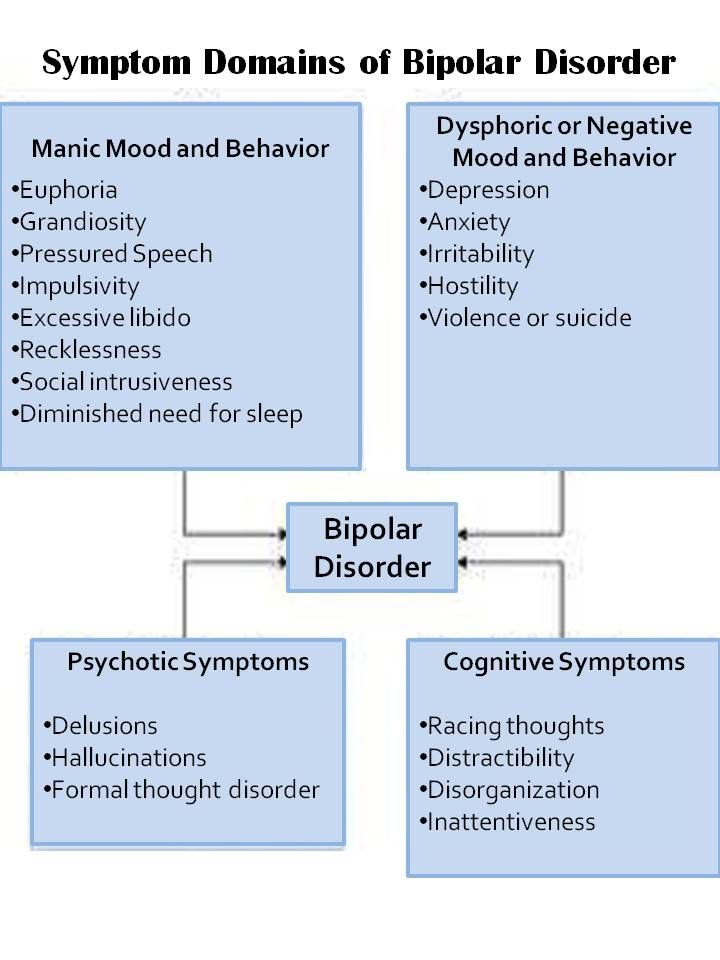 G., Deeks J.J., Altman D.G. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–560. doi: 10.1136/bmj.327.7414.557. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
G., Deeks J.J., Altman D.G. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–560. doi: 10.1136/bmj.327.7414.557. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
52. Rohatgi A. WebPlotDigitizer. [(accessed on 22 October 2018)]; Available online: https://automeris.io/WebPlotDigitizer/
53. Kurppa K., Paavola A., Collin P., Sievänen H., Laurila K., Huhtala H., Saavalainen P., Mäki M., Kaukinen K. Benefits of a gluten-free diet for asymptomatic patients with serologic markers of celiac disease. Gastroenterology. 2014;147:610–617. doi: 10.1053/j.gastro.2014.05.003. [PubMed] [CrossRef] [Google Scholar]
54. Elli L., Tomba C., Branchi F., Roncoroni L., Lombardo V., Bardella M.T., Ferretti F., Conte D., Valiante F., Fini L., et al. Evidence for the Presence of Non-Celiac Gluten Sensitivity in Patients with Functional Gastrointestinal Symptoms: Results from a Multicenter Randomized Double-Blind Placebo-Controlled Gluten Challenge. Nutrients. 2016;8 doi: 10.3390/nu8020084. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
[PMC free article] [PubMed] [CrossRef] [Google Scholar]
55. Paavola A., Kurppa K., Ukkola A., Collin P., Lähdeaho M.-L., Huhtala H., Mäki M., Kaukinen K. Gastrointestinal symptoms and quality of life in screen-detected celiac disease. Dig. Liver Dis. 2012;44:814–818. doi: 10.1016/j.dld.2012.04.019. [PubMed] [CrossRef] [Google Scholar]
56. Di Sabatino A., Volta U., Salvatore C., Biancheri P., Caio G., De Giorgio R., Di Stefano M., Corazza G.R. Small Amounts of Gluten in Subjects With Suspected Nonceliac Gluten Sensitivity: A Randomized, Double-Blind, Placebo-Controlled, Cross-Over Trial. Clin. Gastroenterol. Hepatol. 2015;13:1604–1612. doi: 10.1016/j.cgh.2015.01.029. [PubMed] [CrossRef] [Google Scholar]
57. Nachman F., del Campo M.P., González A., Corzo L., Vázquez H., Sfoggia C., Smecuol E., Sánchez M.I.P., Niveloni S., Sugai E., et al. Long-term deterioration of quality of life in adult patients with celiac disease is associated with treatment noncompliance. Dig. Liver Dis. 2010;42:685–691. doi: 10.1016/j.dld.2010.03.004. [PubMed] [CrossRef] [Google Scholar]
2010;42:685–691. doi: 10.1016/j.dld.2010.03.004. [PubMed] [CrossRef] [Google Scholar]
58. Nachman F., Mauriño E., Vázquez H., Sfoggia C., Gonzalez A., Gonzalez V., del Campo M.P., Smecuol E., Niveloni S., Sugai E., et al. Quality of life in celiac disease patients. Prospective analysis on the importance of clinical severity at diagnosis and the impact of treatment. Dig. Liver Dis. 2009;41:15–25. doi: 10.1016/j.dld.2008.05.011. [PubMed] [CrossRef] [Google Scholar]
59. Bella R., Lanza G., Cantone M., Giuffrida S., Puglisi V., Vinciguerra L., Pennisi M., Ricceri R., D’Agate C.C., Malaguarnera G., et al. Effect of a Gluten-Free Diet on Cortical Excitability in Adults with Celiac Disease. PLoS ONE. 2015;10:1–11. doi: 10.1371/journal.pone.0129218. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
60. Kurppa K., Collin P., Sievänen H., Huhtala H., Mäki M., Kaukinen K. Gastrointestinal symptoms, quality of life and bone mineral density in mild enteropathic coeliac disease: A prospective clinical trial. Scand. J. Gastroenterol. 2010;45:305–314. doi: 10.3109/00365520903555879. [PubMed] [CrossRef] [Google Scholar]
Scand. J. Gastroenterol. 2010;45:305–314. doi: 10.3109/00365520903555879. [PubMed] [CrossRef] [Google Scholar]
61. Ukkola A., Mäki M., Kurppa K., Collin P., Huhtala H., Kekkonen L., Kaukinen K. Diet Improves Perception of Health and Well-being in Symptomatic, but Not Asymptomatic, Patients With Celiac Disease. Clin. Gastroenterol. Hepatol. 2011;9:118–123. doi: 10.1016/j.cgh.2010.10.011. [PubMed] [CrossRef] [Google Scholar]
62. Vilppula A., Kaukinen K., Luostarinen L., Krekelä I., Patrikainen H., Valve R., Luostarinen M., Laurila K., Mäki M., Collin P. Clinical benefit of gluten-free diet in screen-detected older celiac disease patients. BMC Gastroenterol. 2011;11 doi: 10.1186/1471-230X-11-136. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
63. Aziz I., Trott N., Briggs R., North J.R., Hadjivassiliou M., Sanders D.S. Efficacy of a Gluten-Free Diet in Subjects With Irritable Bowel Syndrome-Diarrhea Unaware of Their HLA-DQ2/8 Genotype. Clin. Gastroenterol. Hepatol. 2016;14:696–703. doi: 10.1016/j.cgh.2015.12.031. [PubMed] [CrossRef] [Google Scholar]
2016;14:696–703. doi: 10.1016/j.cgh.2015.12.031. [PubMed] [CrossRef] [Google Scholar]
64. Collin P., Kaukinen K., Mattila A.K., Joukamaa M. Psychoneurotic symptoms and alexithymia in coeliac disease. Scand. J. Gastroenterol. 2008;43:1329–1333. doi: 10.1080/00365520802240248. [PubMed] [CrossRef] [Google Scholar]
65. Addolorato G., Capristo E., Ghittoni G., Valeri C., Mascianà R., Ancona C., Gasbarrini G. Anxiety but not depression decreases in coeliac patients after one-year gluten-free diet: A longitudinal study. Scand. J. Gastroenterol. 2001;36:502–506. doi: 10.1080/00365520119754. [PubMed] [CrossRef] [Google Scholar]
66. Fuchs V., Kurppa K., Huhtala H., Mäki M., Kekkonen L., Kaukinen K. Delayed celiac disease diagnosis predisposes to reduced quality of life and incremental use of health care services and medicines: A prospective nationwide study. United Eur. Gastroenterol. J. 2018;6:567–575. doi: 10.1177/2050640617751253. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
67. Peters S., Yelland G., Moore J., Ward M. No effect of gluten on anxiety or depression in patients with NCGS, but could it be brain fog? J. Gastroenterol. Hepatol. 2016;31:175–176. doi: 10.1016/S0016-5085(16)32515-X. [CrossRef] [Google Scholar]
Peters S., Yelland G., Moore J., Ward M. No effect of gluten on anxiety or depression in patients with NCGS, but could it be brain fog? J. Gastroenterol. Hepatol. 2016;31:175–176. doi: 10.1016/S0016-5085(16)32515-X. [CrossRef] [Google Scholar]
68. Sterne J.A.C., Sutton A.J., Ioannidis J.P.A., Terrin N., Jones D.R., Lau J., Carpenter J., Rücker G., Harbord R.M., Schmid C.H., et al. Recommendations for examining and interpreting funnel plot asymmetry in meta-analyses of randomised controlled trials. BMJ. 2011;343:d4002. doi: 10.1136/bmj.d4002. [PubMed] [CrossRef] [Google Scholar]
69. Moher D., Liberati A., Tetzlaff J., Altman D.G. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. BMJ. 2009;339:b2535. doi: 10.1136/bmj.b2535. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
70. Cohen J. Statistical Power Analysis in the Behavioral Sciences. 2nd ed. Routledge; Hillsdale, MJ, USA: 1988. [Google Scholar]
71. Admou B., Essaadouni L.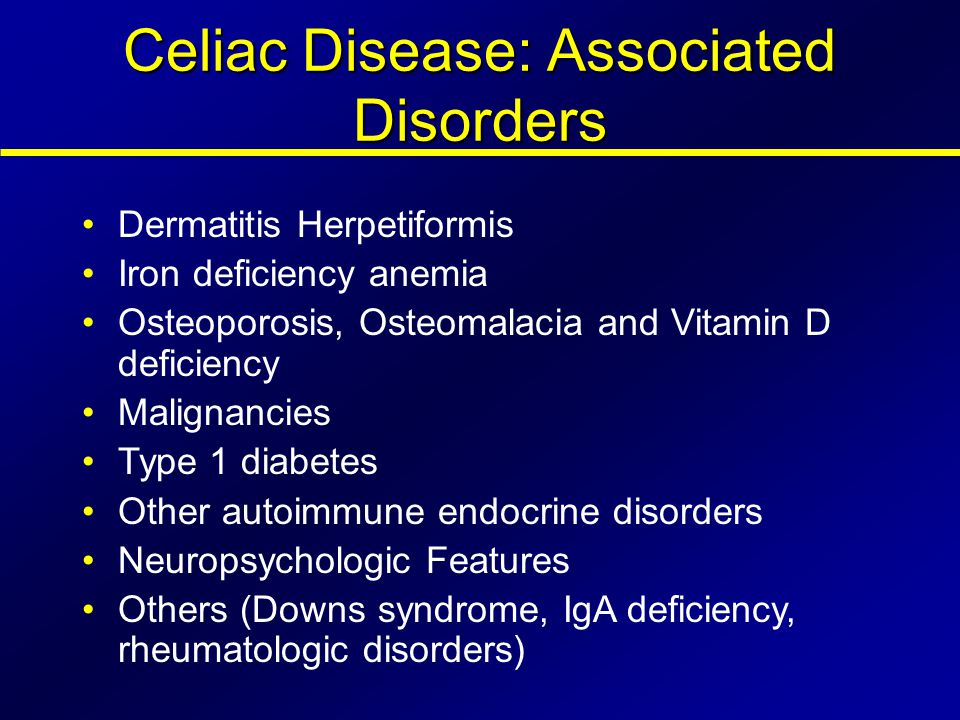 , Krati K., Zaher K., Sbihi M., Chabaa L., Belaabidia B., Alaoui-Yazidi A. Atypical Celiac Disease: From Recognizing to Managing. Gastroenterol. Res. Pract. 2012;2012 doi: 10.1155/2012/637187. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
, Krati K., Zaher K., Sbihi M., Chabaa L., Belaabidia B., Alaoui-Yazidi A. Atypical Celiac Disease: From Recognizing to Managing. Gastroenterol. Res. Pract. 2012;2012 doi: 10.1155/2012/637187. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
72. Concerto C., Lanza G., Cantone M., Pennisi M., Giordano D., Spampinato C., Ricceri R., Pennisi G., Aguglia E., Bella R. Different patterns of cortical excitability in major depression and vascular depression: A transcranial magnetic stimulation study. BMC Psychiatry. 2013;13:300. doi: 10.1186/1471-244X-13-300. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
73. Hall N.J., Rubin G., Charnock A. Systematic review: Adherence to a gluten-free diet in adult patients with coeliac disease. Aliment. Pharmacol. Therapeut. 2009;30:315–330. doi: 10.1111/j.1365-2036.2009.04053.x. [PubMed] [CrossRef] [Google Scholar]
74. Zysk W., Głąbska D., Guzek D., Zysk W., Głąbska D., Guzek D. Social and Emotional Fears and Worries Influencing the Quality of Life of Female Celiac Disease Patients Following a Gluten-Free Diet.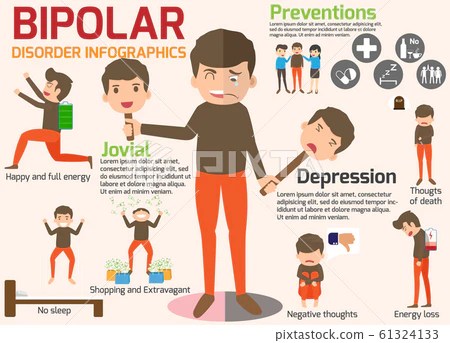 Nutrients. 2018;10:1414. doi: 10.3390/nu10101414. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
Nutrients. 2018;10:1414. doi: 10.3390/nu10101414. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
75. Leonard M., Cureton P., Fasano A., Leonard M.M., Cureton P., Fasano A. Indications and Use of the Gluten Contamination Elimination Diet for Patients with Non-Responsive Celiac Disease. Nutrients. 2017;9:1129. doi: 10.3390/nu9101129. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
76. Hollon J.R., Cureton P.A., Martin M.L., Puppa E.L.L., Fasano A. Trace gluten contamination may play a role in mucosal and clinical recovery in a subgroup of diet-adherent non-responsive celiac disease patients. BMC Gastroenterol. 2013;13:40. doi: 10.1186/1471-230X-13-40. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
77. Rostami K., Bold J., Parr A., Johnson M., Rostami K., Bold J., Parr A., Johnson M.W. Gluten-Free Diet Indications, Safety, Quality, Labels, and Challenges. Nutrients. 2017;9:846. doi: 10.3390/nu9080846. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
78. Roncoroni L., Bascuñán K., Doneda L., Scricciolo A., Lombardo V., Branchi F., Ferretti F., Dell’Osso B., Montanari V., Bardella M., et al. A Low FODMAP Gluten-Free Diet Improves Functional Gastrointestinal Disorders and Overall Mental Health of Celiac Disease Patients: A Randomized Controlled Trial. Nutrients. 2018;10:1023. doi: 10.3390/nu10081023. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
Roncoroni L., Bascuñán K., Doneda L., Scricciolo A., Lombardo V., Branchi F., Ferretti F., Dell’Osso B., Montanari V., Bardella M., et al. A Low FODMAP Gluten-Free Diet Improves Functional Gastrointestinal Disorders and Overall Mental Health of Celiac Disease Patients: A Randomized Controlled Trial. Nutrients. 2018;10:1023. doi: 10.3390/nu10081023. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
79. Jiang H., Ling Z., Zhang Y., Mao H., Ma Z., Yin Y., Wang W., Tang W., Tan Z., Shi J., et al. Altered fecal microbiota composition in patients with major depressive disorder. Brain Behav. Immun. 2015;48:186–194. doi: 10.1016/j.bbi.2015.03.016. [PubMed] [CrossRef] [Google Scholar]
80. Majeed M., Nagabhushanam K., Arumugam S., Majeed S., Ali F. Bacillus coagulans MTCC 5856 for the management of major depression with irritable bowel syndrome: A randomised, double-blind, placebo controlled, multi-centre, pilot clinical study. Food Nutr. Res. 2018;62 doi: 10.29219/fnr.v62.1218.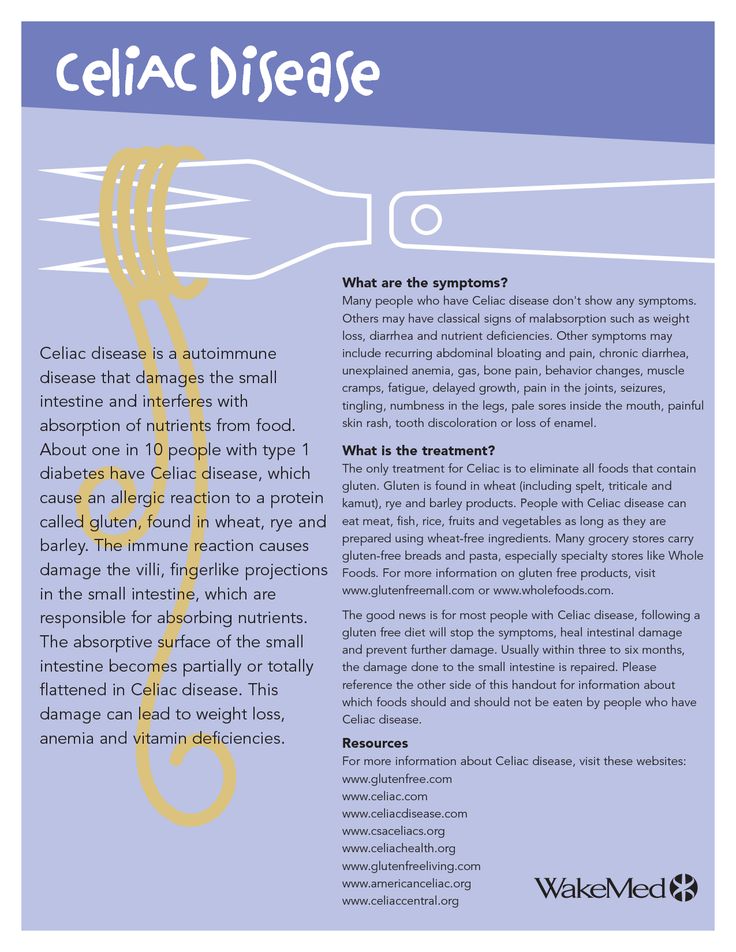 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
[PMC free article] [PubMed] [CrossRef] [Google Scholar]
81. Garcia-Mazcorro J., Noratto G., Remes-Troche J., Garcia-Mazcorro J.F., Noratto G., Remes-Troche J.M. The Effect of Gluten-Free Diet on Health and the Gut Microbiota Cannot Be Extrapolated from One Population to Others. Nutrients. 2018;10:1421. doi: 10.3390/nu10101421. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
82. Biesiekierski J.R., Newnham E.D., Irving P.M., Barrett J.S., Haines M., Doecke J.D., Shepherd S.J., Muir J.G., Gibson P.R. Gluten Causes Gastrointestinal Symptoms in Subjects Without Celiac Disease: A Double-Blind Randomized Placebo-Controlled Trial. Am. J. Gastroenterol. 2011;106:508–514. doi: 10.1038/ajg.2010.487. [PubMed] [CrossRef] [Google Scholar]
83. Skodje G.I., Sarna V.K., Minelle I.H., Rolfsen K.L., Muir J.G., Gibson P.R., Veierød M.B., Henriksen C., Lundin K.E.A. Fructan, Rather Than Gluten, Induces Symptoms in Patients With Self-Reported Non-Celiac Gluten Sensitivity. Gastroenterology.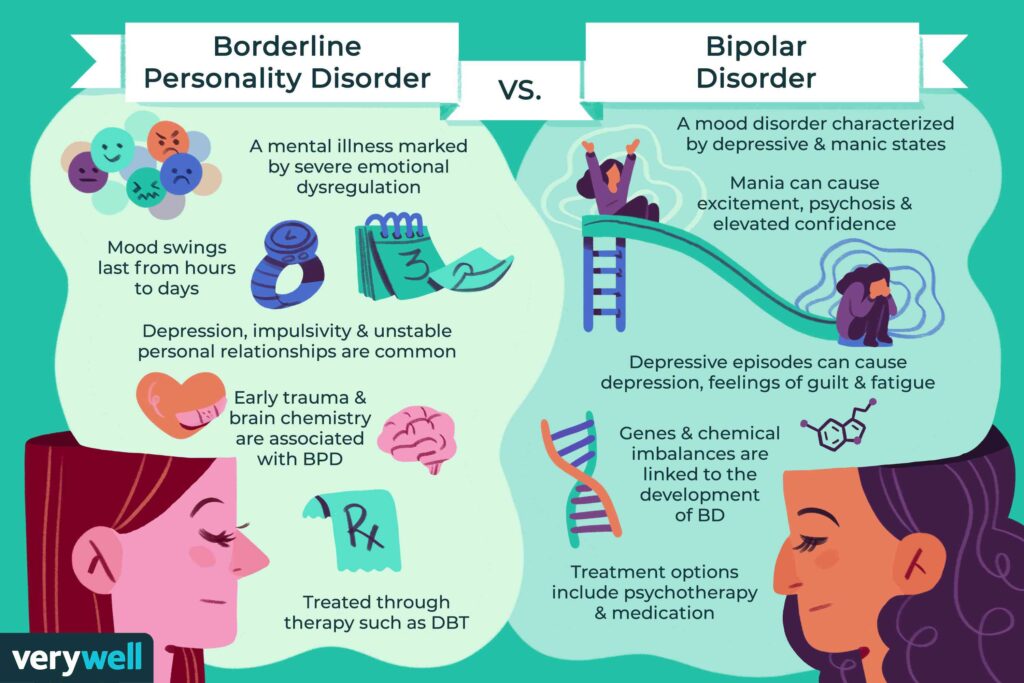 2018;154:529–539. doi: 10.1053/j.gastro.2017.10.040. [PubMed] [CrossRef] [Google Scholar]
2018;154:529–539. doi: 10.1053/j.gastro.2017.10.040. [PubMed] [CrossRef] [Google Scholar]
84. Catassi C., Alaedini A., Bojarski C., Bonaz B., Bouma G., Carroccio A., Castillejo G., De Magistris L., Dieterich W., Di Liberto D., et al. The Overlapping Area of Non-Celiac Gluten Sensitivity (NCGS) and Wheat-Sensitive Irritable Bowel Syndrome (IBS): An Update. Nutrients. 2017;9:1268. doi: 10.3390/nu9111268. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
85. Aziz I., Hadjivassiliou M., Sanders D.S. The spectrum of noncoeliac gluten sensitivity. Nat. Rev. Gastroenterol. Hepatol. 2015;12:516–526. doi: 10.1038/nrgastro.2015.107. [PubMed] [CrossRef] [Google Scholar]
86. Ford R.P.K. The gluten syndrome: A neurological disease. Med. Hypotheses. 2009;73:438–440. doi: 10.1016/j.mehy.2009.03.037. [PubMed] [CrossRef] [Google Scholar]
87. Morales-Muñoz I., Koskinen S., Partonen T. Differences in clinical and cognitive variables in seasonal affective disorder compared to depressive-related disorders: Evidence from a population-based study in Finland. Eur. Psychiatry. 2017;44:9–16. doi: 10.1016/j.eurpsy.2017.03.003. [PubMed] [CrossRef] [Google Scholar]
Eur. Psychiatry. 2017;44:9–16. doi: 10.1016/j.eurpsy.2017.03.003. [PubMed] [CrossRef] [Google Scholar]
88. Kurppa K., Lauronen O., Collin P., Ukkola A., Laurila K., Huhtala H., Mäki M., Kaukinen K. Factors Associated with Dietary Adherence in Celiac Disease: A Nationwide Study. DIG. 2012;86:309–314. doi: 10.1159/000341416. [PubMed] [CrossRef] [Google Scholar]
89. Addolorato C., De Lorenzi C., Abenavoli L., Leccio L., Capristo E., Casbarrini C. Psychological support counselling improves gluten-free diet compliance in coeliac patients with affective disorders. Aliment. Pharmacol. Therapeut. 2004;20:777–782. doi: 10.1111/j.1365-2036.2004.02193.x. [PubMed] [CrossRef] [Google Scholar]
90. Fueyo-Díaz R., Magallón-Botaya R., Gascón-Santos S., Asensio-Martínez Á., Palacios-Navarro G., Sebastián-Domingo J.J. Development and Validation of a Specific Self-Efficacy Scale in Adherence to a Gluten-Free Diet. Front. Psychol. 2018;9 doi: 10.3389/fpsyg.2018.00342. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
Diagnosis of a mental disorder and gluten as the main culprit essay example
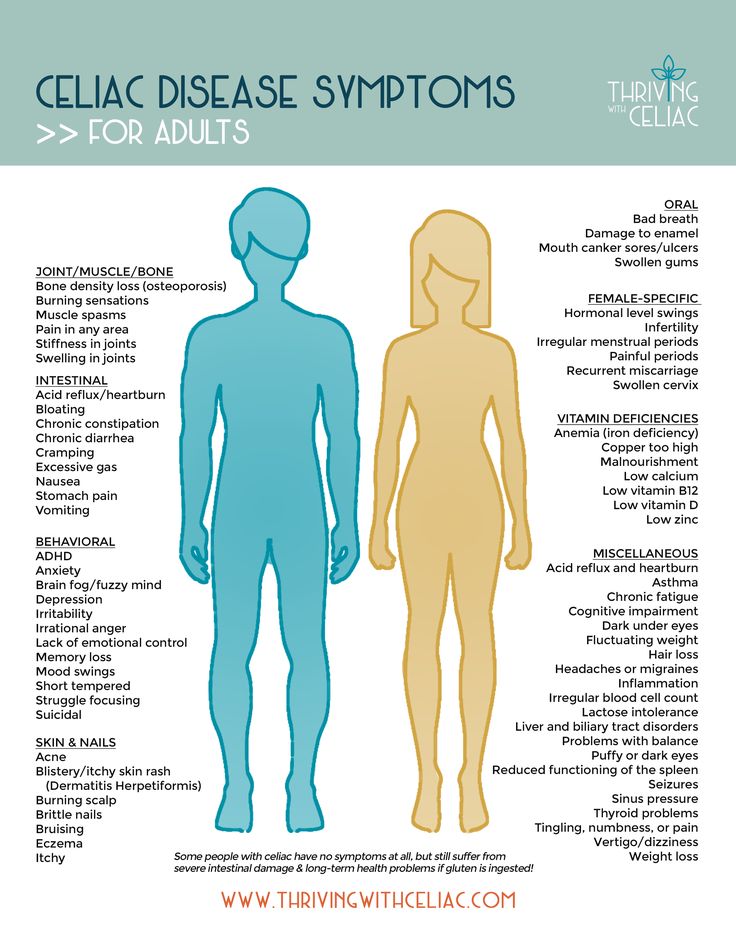
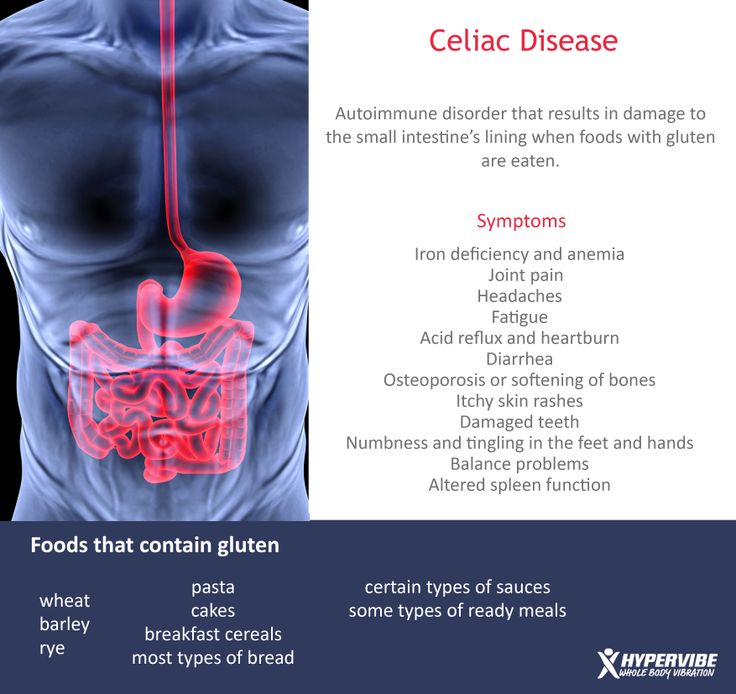
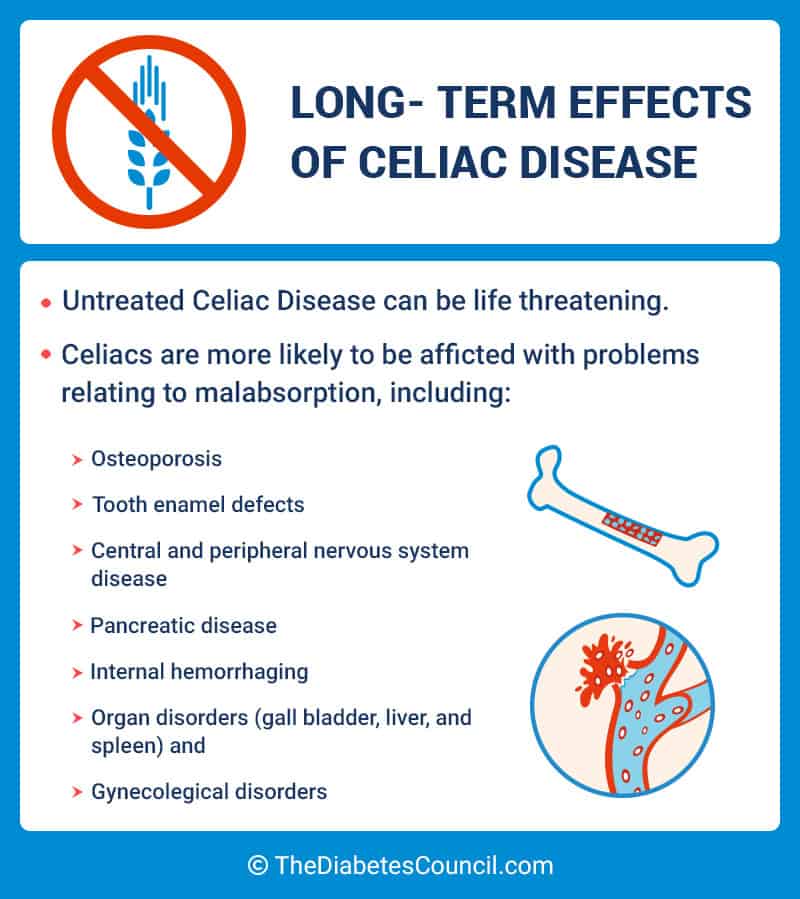
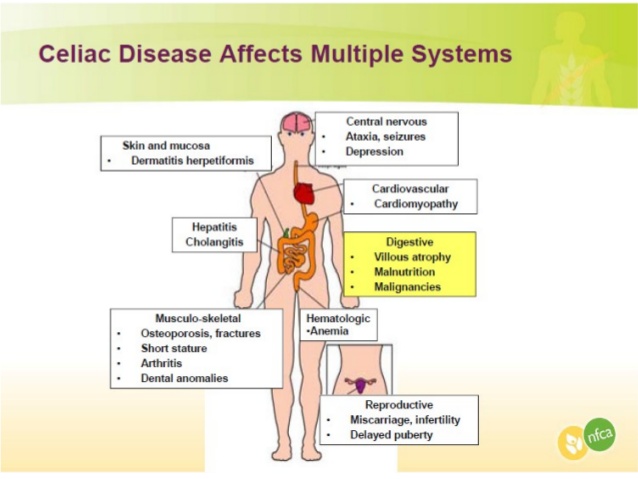
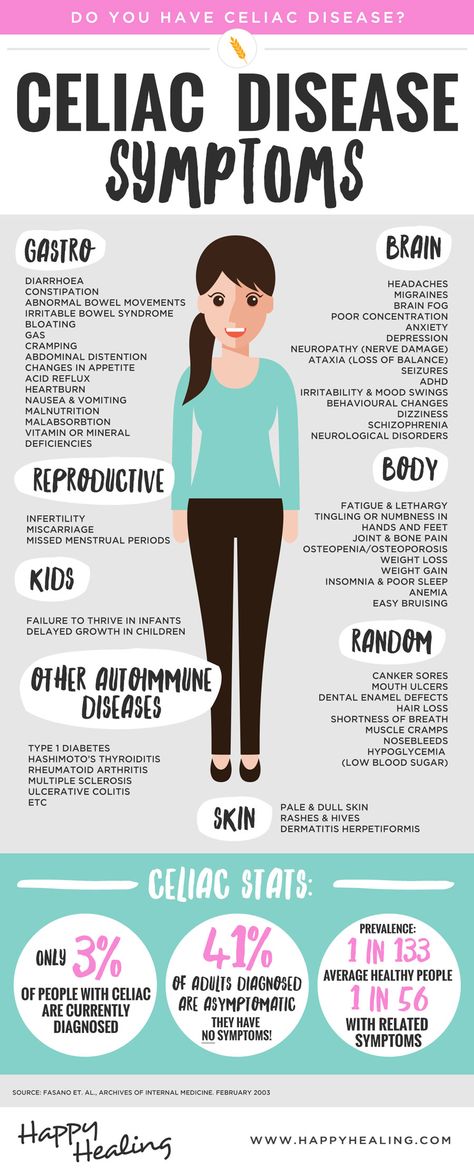
When a doctor makes a diagnosis of "brain / mental disorder", the first drug after the diagnosis is the drug that the patient must prescribe. While medications are necessary for most and effective treatments, what the average person doesn't know is that many of the symptoms associated with mental illness can also be caused by a gluten allergy. It's also important to recognize that celiac disease isn't the only gluten-related disease, it's just the most famous. Gluten has a wide range of effects, especially on the brain and its daily functioning. Disorders, including depression, anxiety, bipolar disorder, insomnia, and brain fog, may be the result of an allergy to gluten or only to it. For many, a gluten-free diet has eased the symptoms of these disorders, prompting physicians to begin this approach when treating a patient. This is because allergies are caused by an immunological reaction. Testing for this can be difficult, so research must continue to help detect these reactions. More people are becoming aware of gluten sensitivity, and it's important to understand that gluten can also greatly affect the brain; Gluten can be the source of many mental illnesses associated with the brain, and it has been proven that a gluten-free diet can relieve the symptoms of these disorders.
While medications are necessary for most and effective treatments, what the average person doesn't know is that many of the symptoms associated with mental illness can also be caused by a gluten allergy. It's also important to recognize that celiac disease isn't the only gluten-related disease, it's just the most famous. Gluten has a wide range of effects, especially on the brain and its daily functioning. Disorders, including depression, anxiety, bipolar disorder, insomnia, and brain fog, may be the result of an allergy to gluten or only to it. For many, a gluten-free diet has eased the symptoms of these disorders, prompting physicians to begin this approach when treating a patient. This is because allergies are caused by an immunological reaction. Testing for this can be difficult, so research must continue to help detect these reactions. More people are becoming aware of gluten sensitivity, and it's important to understand that gluten can also greatly affect the brain; Gluten can be the source of many mental illnesses associated with the brain, and it has been proven that a gluten-free diet can relieve the symptoms of these disorders.
Gluten-free labels can be seen on almost every trip to the grocery store, gluten-free sections are on almost every restaurant menu, and it's not uncommon to hear someone say they're gluten-free almost everywhere. Everyone has heard this phrase, but what exactly is gluten and why does it negatively affect the brain? Gluten is made up of proteins and is found in foods containing wheat, barley and rye. When looking at celiac disease, allergies are caused by an adverse immunological reaction to wheat proteins. In gluten sensitivity (not celiac disease), the symptoms are caused by an increased immune response to gluten, and this reaction usually comes from genetics as well. Gluten specifically degenerates the brain and nerve tissue to a large extent for allergy sufferers, causing neurological problems. to (Gaesser). Because of people hearing about these allergies, they may assume that a gluten-free diet is appropriate for a healthy person. Many people prefer a gluten-free diet, believing that due to common allergies and celiac disease, they immediately assume that gluten is bad in general.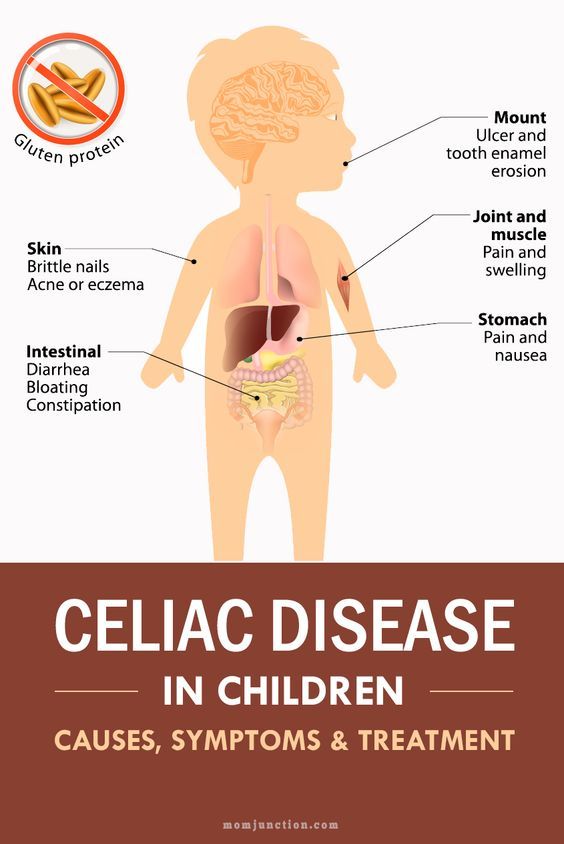 This is not always the case as many of the problems are related to genetics. It's extremely important to assume that a gluten-free diet is for everyone's holiday because there are benefits to gluten if you're healthy and don't suffer from allergies.
This is not always the case as many of the problems are related to genetics. It's extremely important to assume that a gluten-free diet is for everyone's holiday because there are benefits to gluten if you're healthy and don't suffer from allergies.
In addition to spreading the trend based on these assumptions, the benefits of diet for a person who is struggling with mental health is very important information to pass on.
When looking at depression, gluten symptoms can stem from symptoms. In an article published in the journal Functional Medicine Patient Education, the author states: “… the intestinal wall becomes excessively porous. This allows undigested food, toxins, and bacteria to enter the bloodstream, where they cause inflammation throughout the body and brain" ("Gluten can cause depression, anxiety, brain fog, and other brain disorders"). There are many different reactions that can cause brain damage. This article looks at bacteria found in gluten that cannot be digested by most. This is why many celiac patients may also struggle with depression; there is a direct correlation. In addition to this method, there is also a reaction called gluten cross-reactivity. Gluten has a structure similar to brain tissue. The immune system can then confuse gluten in the bloodstream with brain tissue and attack the brain. All of these gluten-related reactions cause an imbalance with bacteria (good and bad) in the digestive tract. Because many nutrients needed for brain health are absorbed in the digestive tract, many nutrients end up not being absorbed, which slows or stops the chemicals needed to prevent mental illness. In fact, these processes are very complex and can be difficult to detect. Either testing or testing of a gluten-free diet will usually determine the diagnosis of gluten allergy due to complexity.
This is why many celiac patients may also struggle with depression; there is a direct correlation. In addition to this method, there is also a reaction called gluten cross-reactivity. Gluten has a structure similar to brain tissue. The immune system can then confuse gluten in the bloodstream with brain tissue and attack the brain. All of these gluten-related reactions cause an imbalance with bacteria (good and bad) in the digestive tract. Because many nutrients needed for brain health are absorbed in the digestive tract, many nutrients end up not being absorbed, which slows or stops the chemicals needed to prevent mental illness. In fact, these processes are very complex and can be difficult to detect. Either testing or testing of a gluten-free diet will usually determine the diagnosis of gluten allergy due to complexity.
To test gluten-related disorders and treatments, the University of Maryland conducted a six-year study on 347 patients. This study tested the symptoms of these patients and how they are related, as well as the treatment.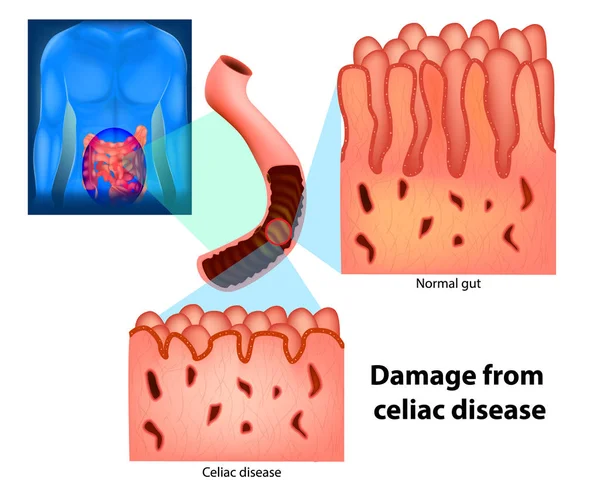 The results showed that "the two most common extracellular manifestations with gluten load were 'foggy mind' (42%) and fatigue (36%)" (Reese Parish 44). Of the 347 patients, these numbers are very important in assessing symptoms. These symptoms are also found in people with depression, anxiety, insomnia, and many other brain disorders. It is also important to recognize that the majority of these subjects did not know that these symptoms could be caused by gluten, they were randomly selected. Thirty-seven patients with similar symptoms were then included in the study and treated by removing gluten from their diet, and all symptoms were reduced. It is still extremely studied and discussed by many scientists, but research and studies have proven the mental health benefits of a gluten-free diet and that allergies are actually common throughout the world.
The results showed that "the two most common extracellular manifestations with gluten load were 'foggy mind' (42%) and fatigue (36%)" (Reese Parish 44). Of the 347 patients, these numbers are very important in assessing symptoms. These symptoms are also found in people with depression, anxiety, insomnia, and many other brain disorders. It is also important to recognize that the majority of these subjects did not know that these symptoms could be caused by gluten, they were randomly selected. Thirty-seven patients with similar symptoms were then included in the study and treated by removing gluten from their diet, and all symptoms were reduced. It is still extremely studied and discussed by many scientists, but research and studies have proven the mental health benefits of a gluten-free diet and that allergies are actually common throughout the world.
Many other studies support the validity of doctors recommending gluten-free diets to patients suffering from mental illness. The Gastroenterological Research Publication includes another study of a five-year-old girl with extreme psychiatric problems. Until the age of four, the girl was healthy, but she suddenly began to have visual and auditory hallucinations. This girl suffered from hallucinations of fairies to horrible scenes of a young boy. Her mother first tried eliminating soy, corn, and dairy products from her diet, but to no avail. While attending lectures on nutrition when she was older, she came up with the idea of eliminating gluten, which caused her hallucinations to completely disappear. “She talks about how, for the first time in her life, she was able to focus on her studies, which allowed her to get a degree in biology and get a job” (Genuis). Without a gluten-free diet, this girl may never be able to continue her studies and become successful. A second case study also confirms the improvement. This study was conducted in Melbourne, Australia by Monash University. The researchers specifically focused on the brain fog associated with gluten sensitivity and whether aspects such as memory, attention, processing efficiency, and motor function would improve after eliminating gluten.
Until the age of four, the girl was healthy, but she suddenly began to have visual and auditory hallucinations. This girl suffered from hallucinations of fairies to horrible scenes of a young boy. Her mother first tried eliminating soy, corn, and dairy products from her diet, but to no avail. While attending lectures on nutrition when she was older, she came up with the idea of eliminating gluten, which caused her hallucinations to completely disappear. “She talks about how, for the first time in her life, she was able to focus on her studies, which allowed her to get a degree in biology and get a job” (Genuis). Without a gluten-free diet, this girl may never be able to continue her studies and become successful. A second case study also confirms the improvement. This study was conducted in Melbourne, Australia by Monash University. The researchers specifically focused on the brain fog associated with gluten sensitivity and whether aspects such as memory, attention, processing efficiency, and motor function would improve after eliminating gluten.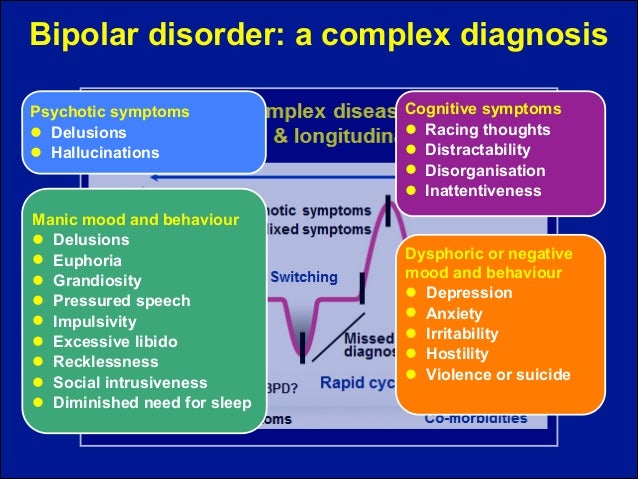 The results of the study concluded: "Patients showed significant improvement in 4 of the cognitive tests, and improvement in measures of verbal fluency, attention, and motor function at 52 weeks was highly correlated with Bolot's scores and increased anti-tissue transglutaminase antibodies" (Laidman). The second time, brain function improved significantly after he experienced brain fog before he was put on a diet. The study also showed that in some patients, the symptoms did not improve, suggesting that these symptoms are not always the result of gluten, but they are very common. This study also showed how many tests are needed to really know the effects of gluten. In the future, we hope that these studies and scientists will find more effective tests and methods for detecting allergies.
The results of the study concluded: "Patients showed significant improvement in 4 of the cognitive tests, and improvement in measures of verbal fluency, attention, and motor function at 52 weeks was highly correlated with Bolot's scores and increased anti-tissue transglutaminase antibodies" (Laidman). The second time, brain function improved significantly after he experienced brain fog before he was put on a diet. The study also showed that in some patients, the symptoms did not improve, suggesting that these symptoms are not always the result of gluten, but they are very common. This study also showed how many tests are needed to really know the effects of gluten. In the future, we hope that these studies and scientists will find more effective tests and methods for detecting allergies.
Gluten-free diets have been a fad for a considerable period of time, but not many people realize that this diet may be necessary for some when trying to treat mental health problems.
Although celiac disease is the most common gluten allergy, general psychiatric/mental disorders are also associated with gluten allergy. The reactions that cause these symptoms are complex and testing is difficult, which is why many doctors immediately prescribe a gluten-free diet to see if symptoms disappear or improve. Countless case studies prove the effectiveness of a gluten-free diet for mental health problems. This is still a widely discussed issue and is still being researched, so it's good to spread the word about the benefits of a gluten-free diet for those who are not completely healthy or have mental health problems. This discussion needs to continue so that more technologies and less complex testing can be found to help people with gluten allergies.
Genital tuberculosis
10/30/2020 No Comments
Genital TB is the cause of infertility in women It is likely that each of us has had a family member or acquaintance affected by TB. Tuberculosis is serious
Read more »
Swaddling at NICU
10/30/2020 No Comments
Many children in the neonatal intensive care unit face many health problems that involve risky and painful procedures in everyday life in the hospital.
Read more »
Colorectal and breast cancer
10/30/2020 No Comments
This study included 30 patients with colorectal and breast cancer who used capecitabine. Patients were asked to bring any medicine left during the
Read more »
Gluten and Anxiety: Is There a Link?
The term gluten refers to a group of proteins found in various grains, including wheat, rye and barley.
Although most people can tolerate gluten, it can cause a number of harmful side effects in people with celiac disease or gluten sensitivity.
Some say that gluten not only causes indigestion, headaches, and skin problems, but it can also contribute to psychological symptoms such as anxiety (1).
This article discusses research in more detail to determine if gluten may be a concern.
Share on Pinterest
content
Celiac disease
In patients with celiac disease, eating gluten causes inflammation in the intestines, causing symptoms such as bloating, gas, diarrhea, and fatigue.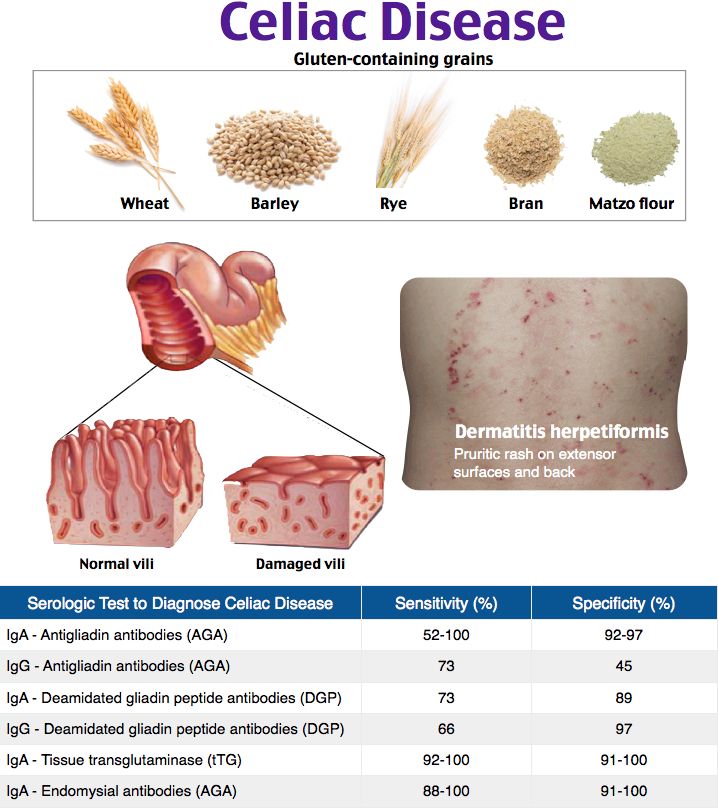 2).
2).
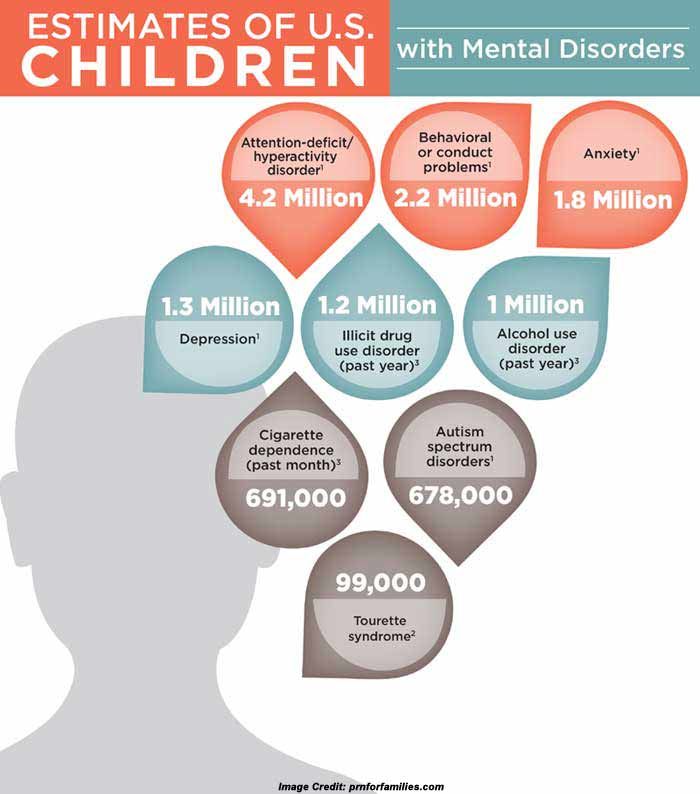
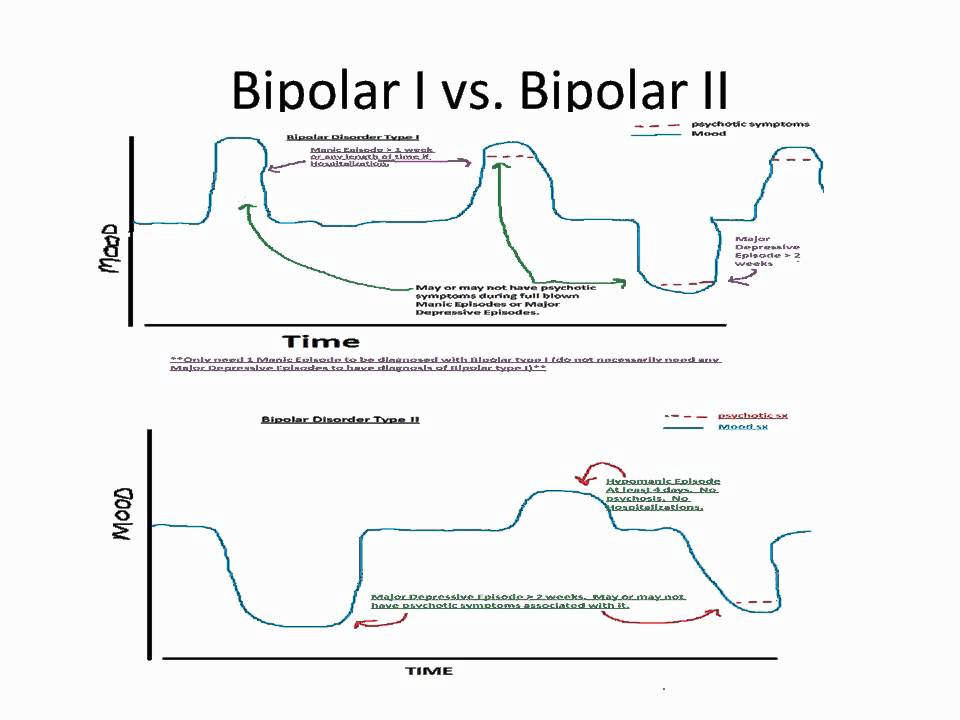
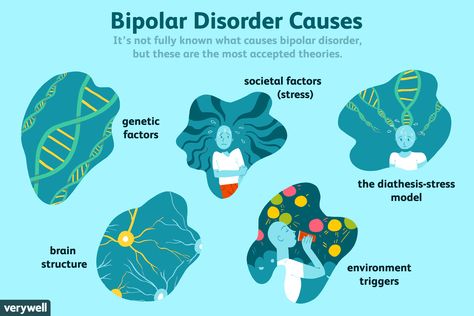
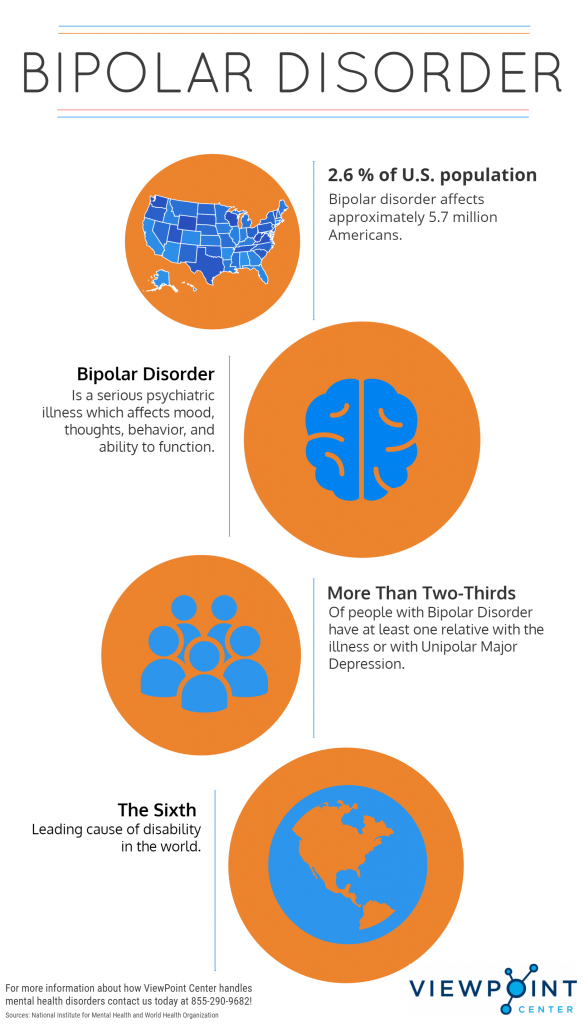
Some research suggests that celiac disease may be associated with a higher risk of certain psychiatric disorders, including anxiety, depression, bipolar disorder, and schizophrenia.3).
A gluten-free diet can not only relieve symptoms of celiac disease, but also reduce anxiety.
In fact, a 2001 study showed that after a gluten-free diet for 1 year, anxiety decreased in 35 people with celiac disease.4).
Another small study of 20 people with celiac disease reported that participants experienced higher levels of anxiety before starting a gluten-free diet than after following it for 1 year.5).
However, conflicting results have been noted in other studies.
For example, one study found that women with celiac disease were more likely to have anxiety compared to the general population, even after completing a gluten-free diet.6).
Notably, homestay was also associated with a higher risk of anxiety disorders in the study, which may be related to the stress of buying and preparing meals for family members with and without celiac disease.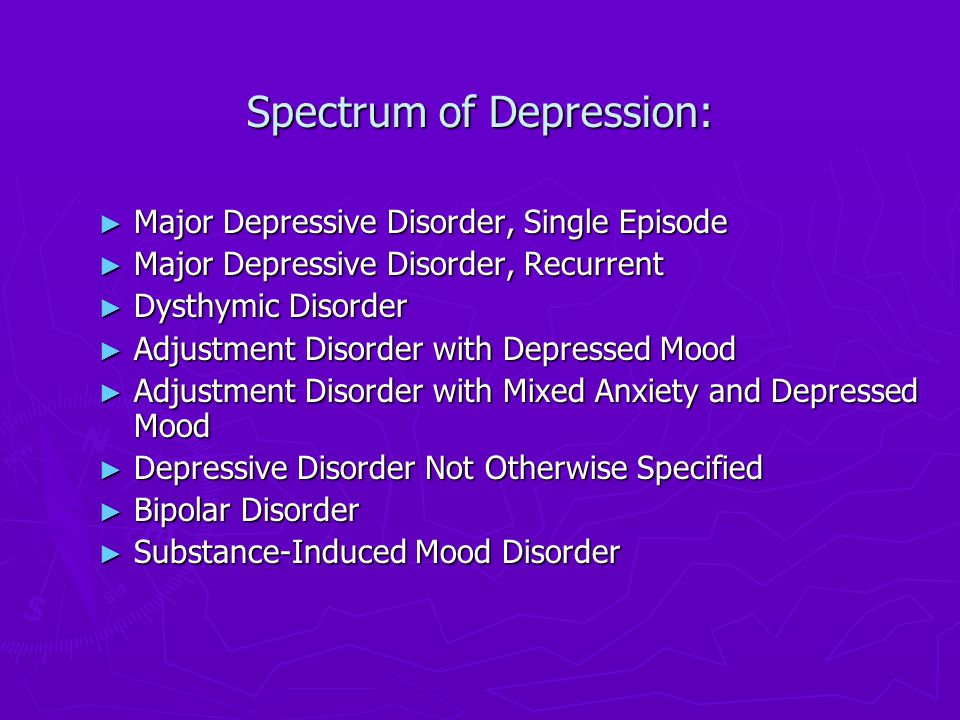 6).
6).
Moreover, a 2020 study of 283 people with celiac disease reported a high frequency of anxiety in people with celiac disease and found that following a gluten-free diet did not significantly improve anxiety symptoms.
So while a gluten-free diet may reduce anxiety in some people with celiac disease, it may not reduce anxiety or even contribute to stress and anxiety in others.
More research is needed to evaluate the effect of a gluten-free diet on anxiety in people with celiac disease.
Gluten sensitivity
People with gluten sensitivity to gluten may also experience harmful side effects from consuming gluten, including symptoms such as fatigue, headaches and muscle pain.7).
In some cases, people who are not sensitive to celiac disease may also experience psychological symptoms such as depression or anxiety.7).
Although more qualitative research is needed, some studies suggest that removing gluten from the diet may be beneficial in these conditions.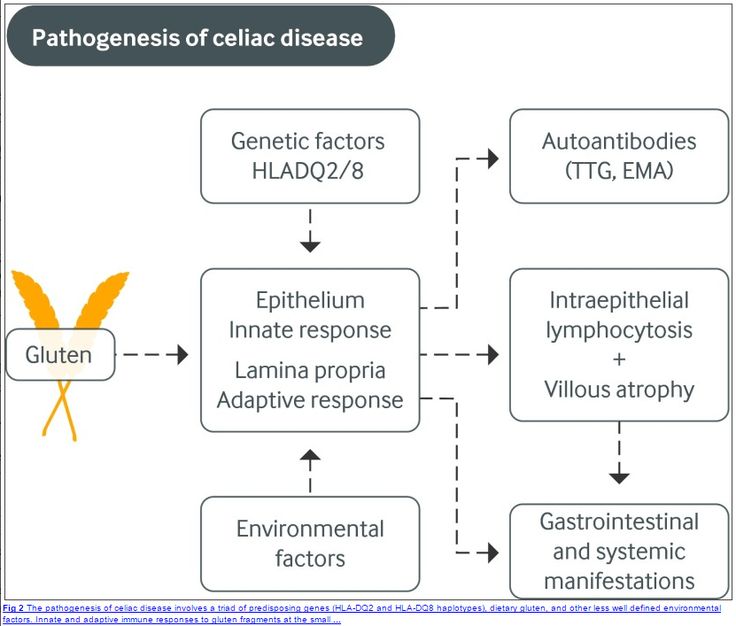
In one study of 23 people, 13% of participants reported that their subjective anxiety decreased after a gluten-free diet (8).
Another study in 22 people with gluten sensitivity without celiac disease found that eating gluten for 3 days resulted in increased feelings of depression compared to controls.9).
Although the cause of these symptoms is still unclear, some research suggests that the effect may be due to changes in the gut microbiome, a community of beneficial bacteria in the digestive tract that are involved in several aspects of health.10,11).
Unlike celiac disease or wheat allergy, there is no specific test used to diagnose gluten sensitivity.
However, if you experience anxiety, depression, or any other negative symptoms after eating gluten, consult your doctor to determine if a gluten-free diet is right for you.
Essence
Anxiety is often associated with celiac disease and gluten sensitivity.
Although studies have shown mixed results, several studies show that monitoring a gluten-free diet can help reduce anxiety symptoms in people with celiac disease or gluten sensitivity.