Can stress cause sleepwalking
Why Do People Sleepwalk? Causes, Symptoms, Dangers, More
Have you ever gone to sleep in your bed and woken up on the living room sofa? Or, perhaps you’ve woken up with mysterious crumbs sprinkled over your pajamas with no recollection of a midnight snack?
If so, you may be one of the 6.9 percent of people who’ve experienced at least one episode of sleepwalking in their life.
Although the prevalence of sleepwalking is significantly higher in children, about 1.5 percent of adults have had a sleepwalking episode beyond their childhood years.
Sleepwalking, or somnambulism, can be caused by medications, genetics, or health conditions that disrupt your sleep.
Here’s what we know about why some people sleepwalk.
Sleepwalking is a sleeping disturbance that occurs in the deepest part of your nonrapid eye movement (NREM) sleep. It most often occurs within 1 to 2 hours of falling asleep.
During an episode of sleepwalking, you may sit up, walk around, and even perform ordinary activities — all while sleeping. Your eyes are open, but you’re actually still in a deep state of sleep.
The American Psychiatric Association does not consider sleepwalking to be a disorder unless it happens often enough to cause you distress and it disturbs your ability to function during the day.
More common in children than adults, sleepwalking is often outgrown by the teen years. But not everyone stops sleepwalking once they’re adults. Although rare, some people may only start sleepwalking in their adult years.
Sleep researchers have identified several health conditions, activities, and substances that are known to trigger sleepwalking episodes.
It’s also possible that you inherited your tendency to sleepwalk. Sleepwalking sometimes runs in families.
Stress
Stress and anxiety are known to interfere with a good night’s rest. Some sleep scientists also think daytime stress can contribute to somnambulism.
One study of 193 patients in a sleep clinic found that one of the main triggers of sleepwalking episodes was stressful events experienced during the day.
If you want to decrease your daily stress levels so you can rest at night, you may want to try stress-reduction techniques such as these:
- get regular exercise
- practice mindfulness
- limit caffeine
- do breathing exercises
- try yoga
Sleep deprivation
People who don’t get enough sleep are more vulnerable to sleepwalking.
Researchers who studied MRI brain scans of people with a history of sleepwalking found that being sleep-deprived increased the number of sleepwalking episodes people experienced.
Migraine
If you have chronic migraine, you may be more vulnerable to sleepwalking.
In 2015, a group of sleep scientists interviewed 100 patients who routinely sleepwalk, and found a strong association between sleepwalking and lifelong headaches, particularly migraine.
Fever
Sleepwalking has been associated with illnesses that cause fever, especially in children.
Fevers can also cause night terrors, which are sleep disturbances during which you might scream, thrash your arms about, or try to escape from fearful things you perceive in your sleep.
Breathing disorders
Obstructive sleep apnea is a breathing disorder that causes you to stop breathing for short periods while you sleep. It’s more than just snoring.
Among other things, severe sleep apnea can lead to daytime fatigue, high blood pressure, stroke, and heart disease.
If you have severe obstructive sleep apnea, your likelihood of sleepwalking is higher than people with mild sleep apnea.
There have also been reports of sleepwalking among children who have asthma. Asthma can lead to sleep deprivation, and the medication montelukast has triggered sleepwalking in some children.
Gastroesophageal reflux disease (GERD)
If you have GERD, the contents of your stomach can come back up through your esophagus, causing uncomfortable burning sensations. For many people, symptoms are worse at night.
People with GERD and other gastric disorders are more prone to many kinds of sleep disorders, including sleepwalking.
Because GERD interferes with sleep, it can cause long-term exhaustion, which also makes you more vulnerable to sleepwalking episodes.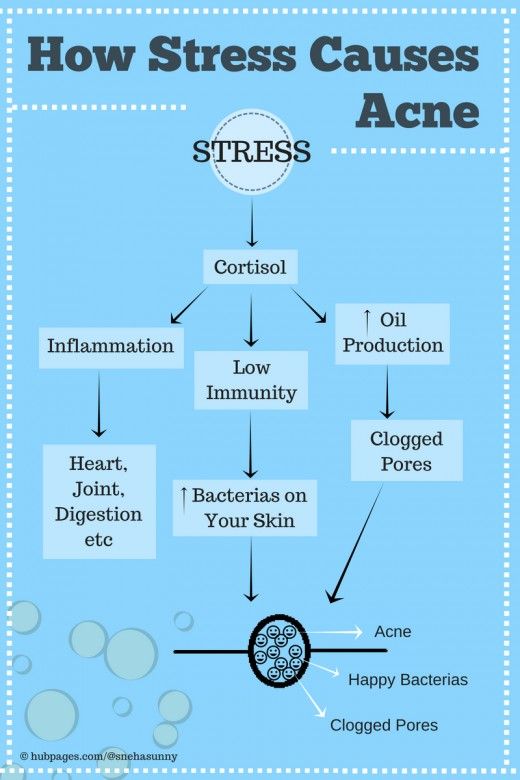
Parkinson’s disease
Parkinson’s disease is a nerve condition that affects your body’s ability to move. As the disease progresses, it can affect parts of the brain stem that control movement as well as parts of the brain that control sleep.
Normally, when you dream during REM sleep, your brain temporarily paralyzes some muscles to keep you from acting on your dreams and hurting yourself or others in the process.
Some studies indicate that Parkinson’s disease may keep that sleep paralysis from happening completely. This, in turn, may lead to sleepwalking and other sleep disturbances.
Restless leg syndrome
There’s some debate among sleep researchers about whether restless leg syndrome (RLS) causes sleepwalking.
Some studies indicate that people with RLS are no more likely to sleepwalk than other people. Other studies point to a connection between sleepwalking and the medications used to treat restless leg syndrome.
Certain medications
Some sleep medications have caused people to sleepwalk, including the sleep-inducing drug zolpidem, which is also sold under the names Ambien and Edluar.
Other medications linked to sleepwalking include:
- sodium oxybate used to treat narcolepsy
- benzodiazepine receptor agonists
- antidepressants
- antipsychotics used to treat psychiatric disorders
- beta-blockers used to treat heart disease and anxiety
People who are sleepwalking usually do not respond when you try to get their attention. They may have a glazed or distant look in their eyes.
According to sleep experts, sleepwalkers can also engage in other activities while they’re in their sleepwalking state, including:
- eating
- talking
- preparing food
- urinating in places that aren’t toilets
- trying to leave the house
- having sex
Most of the time, people do not remember an episode of sleepwalking when they wake up. If you wake someone up while they’re sleepwalking, they may be confused about what’s going on.
Although most episodes of sleepwalking end without injury, sleepwalking can be quite dangerous. Some people may attempt to drive or perform other tasks without being able to perceive what’s really going on around them.
Some people may attempt to drive or perform other tasks without being able to perceive what’s really going on around them.
In one study involving 100 patients with a history of repeated sleepwalking, 57.9 percent had been injured or had injured someone else during an episode of sleepwalking.
Injuries were the result of accidents like falling down the stairs, or bumping into objects like walls or furniture.
Because someone could hurt themselves or others while they’re sleepwalking, it’s a good idea to wake up someone who’s sleepwalking. Just do it gently, because a sleepwalking person may be startled by being awakened.
Most children grow out of sleepwalking by the time they reach their teenage years, without ever needing treatment.
However, if your sleepwalking didn’t begin until you were an adult, you may want to talk to your doctor to rule out underlying conditions that can cause you to sleepwalk.
If you sleepwalk often, or if your sleepwalking is causing problems with your daily functioning or your relationships, it’s a good idea to talk to a doctor.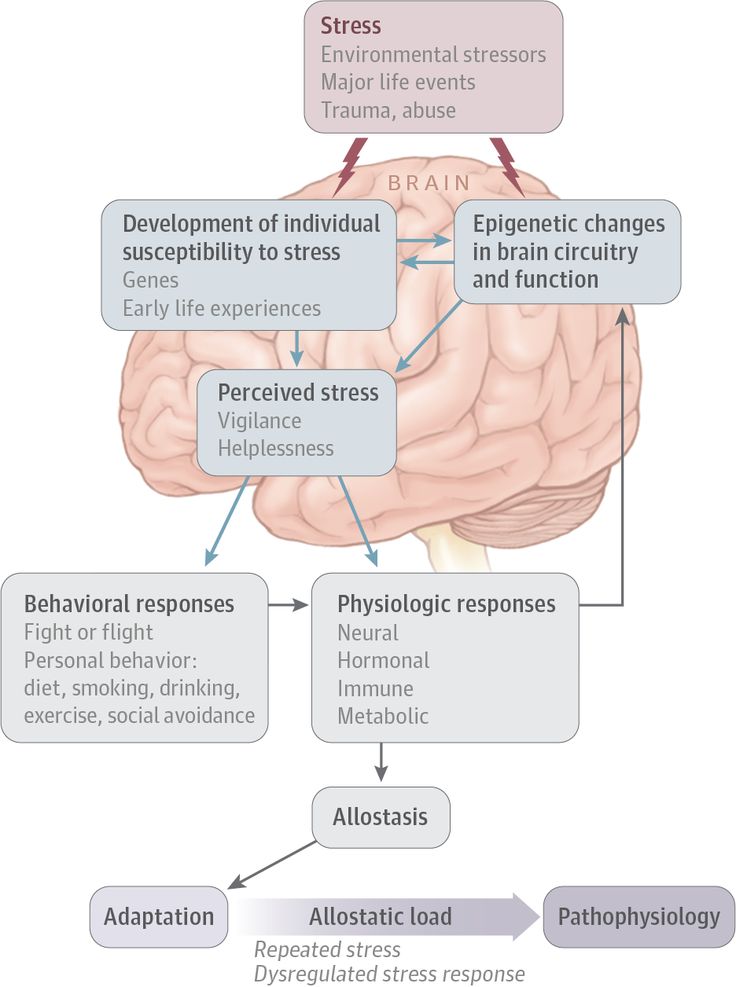
The most common way for sleepwalking to be diagnosed is when someone else sees it firsthand. Since most sleepwalking occurs during childhood, parents are the ones who most often report sleepwalking to healthcare providers.
If your doctor is concerned about your sleepwalking, a sleep study could reveal more about your condition.
During the sleep study, your healthcare team will check your blood oxygen levels, brain waves, breathing, and movements while you’re asleep.
If your sleepwalking isn’t severe, you may be able to prevent it by reducing stress in your daily life and improving your sleep habits.
If those methods don’t work well enough, your doctor may prescribe medications to help.
Clonazepam (Klonopin) and diazepam (Valium) have been shown to reduce sleepwalking. Antidepressants and benzodiazepines may help you with your stress levels so you can rest.
For most children, treatment usually isn’t necessary because sleepwalking often goes away on its own as the child matures.
Sleepwalking is a sleep disturbance in which you walk, talk, or do other activities while you’re in a deep state of sleep. It happens in the deepest part of your sleep cycle, usually within an hour or two of going to sleep.
More common in children than adults, sleepwalking is often outgrown by the teen years. But not everyone stops sleepwalking once they’re adults.
Sleepwalking often runs in families. It can also be caused by stress, sleep deprivation, certain medications, breathing disorders, neurological conditions, stress, fever, and migraine.
If you sleepwalk often, or if your nighttime wandering is causing problems — either at night or during the day — it’s a good idea to follow up with your doctor.
Why Do People Sleepwalk? Causes, Symptoms, Dangers, More
Have you ever gone to sleep in your bed and woken up on the living room sofa? Or, perhaps you’ve woken up with mysterious crumbs sprinkled over your pajamas with no recollection of a midnight snack?
If so, you may be one of the 6. 9 percent of people who’ve experienced at least one episode of sleepwalking in their life.
9 percent of people who’ve experienced at least one episode of sleepwalking in their life.
Although the prevalence of sleepwalking is significantly higher in children, about 1.5 percent of adults have had a sleepwalking episode beyond their childhood years.
Sleepwalking, or somnambulism, can be caused by medications, genetics, or health conditions that disrupt your sleep.
Here’s what we know about why some people sleepwalk.
Sleepwalking is a sleeping disturbance that occurs in the deepest part of your nonrapid eye movement (NREM) sleep. It most often occurs within 1 to 2 hours of falling asleep.
During an episode of sleepwalking, you may sit up, walk around, and even perform ordinary activities — all while sleeping. Your eyes are open, but you’re actually still in a deep state of sleep.
The American Psychiatric Association does not consider sleepwalking to be a disorder unless it happens often enough to cause you distress and it disturbs your ability to function during the day.
More common in children than adults, sleepwalking is often outgrown by the teen years. But not everyone stops sleepwalking once they’re adults. Although rare, some people may only start sleepwalking in their adult years.
Sleep researchers have identified several health conditions, activities, and substances that are known to trigger sleepwalking episodes.
It’s also possible that you inherited your tendency to sleepwalk. Sleepwalking sometimes runs in families.
Stress
Stress and anxiety are known to interfere with a good night’s rest. Some sleep scientists also think daytime stress can contribute to somnambulism.
One study of 193 patients in a sleep clinic found that one of the main triggers of sleepwalking episodes was stressful events experienced during the day.
If you want to decrease your daily stress levels so you can rest at night, you may want to try stress-reduction techniques such as these:
- get regular exercise
- practice mindfulness
- limit caffeine
- do breathing exercises
- try yoga
Sleep deprivation
People who don’t get enough sleep are more vulnerable to sleepwalking.
Researchers who studied MRI brain scans of people with a history of sleepwalking found that being sleep-deprived increased the number of sleepwalking episodes people experienced.
Migraine
If you have chronic migraine, you may be more vulnerable to sleepwalking.
In 2015, a group of sleep scientists interviewed 100 patients who routinely sleepwalk, and found a strong association between sleepwalking and lifelong headaches, particularly migraine.
Fever
Sleepwalking has been associated with illnesses that cause fever, especially in children.
Fevers can also cause night terrors, which are sleep disturbances during which you might scream, thrash your arms about, or try to escape from fearful things you perceive in your sleep.
Breathing disorders
Obstructive sleep apnea is a breathing disorder that causes you to stop breathing for short periods while you sleep. It’s more than just snoring.
Among other things, severe sleep apnea can lead to daytime fatigue, high blood pressure, stroke, and heart disease.
If you have severe obstructive sleep apnea, your likelihood of sleepwalking is higher than people with mild sleep apnea.
There have also been reports of sleepwalking among children who have asthma. Asthma can lead to sleep deprivation, and the medication montelukast has triggered sleepwalking in some children.
Gastroesophageal reflux disease (GERD)
If you have GERD, the contents of your stomach can come back up through your esophagus, causing uncomfortable burning sensations. For many people, symptoms are worse at night.
People with GERD and other gastric disorders are more prone to many kinds of sleep disorders, including sleepwalking.
Because GERD interferes with sleep, it can cause long-term exhaustion, which also makes you more vulnerable to sleepwalking episodes.
Parkinson’s disease
Parkinson’s disease is a nerve condition that affects your body’s ability to move. As the disease progresses, it can affect parts of the brain stem that control movement as well as parts of the brain that control sleep.
Normally, when you dream during REM sleep, your brain temporarily paralyzes some muscles to keep you from acting on your dreams and hurting yourself or others in the process.
Some studies indicate that Parkinson’s disease may keep that sleep paralysis from happening completely. This, in turn, may lead to sleepwalking and other sleep disturbances.
Restless leg syndrome
There’s some debate among sleep researchers about whether restless leg syndrome (RLS) causes sleepwalking.
Some studies indicate that people with RLS are no more likely to sleepwalk than other people. Other studies point to a connection between sleepwalking and the medications used to treat restless leg syndrome.
Certain medications
Some sleep medications have caused people to sleepwalk, including the sleep-inducing drug zolpidem, which is also sold under the names Ambien and Edluar.
Other medications linked to sleepwalking include:
- sodium oxybate used to treat narcolepsy
- benzodiazepine receptor agonists
- antidepressants
- antipsychotics used to treat psychiatric disorders
- beta-blockers used to treat heart disease and anxiety
People who are sleepwalking usually do not respond when you try to get their attention. They may have a glazed or distant look in their eyes.
They may have a glazed or distant look in their eyes.
According to sleep experts, sleepwalkers can also engage in other activities while they’re in their sleepwalking state, including:
- eating
- talking
- preparing food
- urinating in places that aren’t toilets
- trying to leave the house
- having sex
Most of the time, people do not remember an episode of sleepwalking when they wake up. If you wake someone up while they’re sleepwalking, they may be confused about what’s going on.
Although most episodes of sleepwalking end without injury, sleepwalking can be quite dangerous. Some people may attempt to drive or perform other tasks without being able to perceive what’s really going on around them.
In one study involving 100 patients with a history of repeated sleepwalking, 57.9 percent had been injured or had injured someone else during an episode of sleepwalking.
Injuries were the result of accidents like falling down the stairs, or bumping into objects like walls or furniture.
Because someone could hurt themselves or others while they’re sleepwalking, it’s a good idea to wake up someone who’s sleepwalking. Just do it gently, because a sleepwalking person may be startled by being awakened.
Most children grow out of sleepwalking by the time they reach their teenage years, without ever needing treatment.
However, if your sleepwalking didn’t begin until you were an adult, you may want to talk to your doctor to rule out underlying conditions that can cause you to sleepwalk.
If you sleepwalk often, or if your sleepwalking is causing problems with your daily functioning or your relationships, it’s a good idea to talk to a doctor.
The most common way for sleepwalking to be diagnosed is when someone else sees it firsthand. Since most sleepwalking occurs during childhood, parents are the ones who most often report sleepwalking to healthcare providers.
If your doctor is concerned about your sleepwalking, a sleep study could reveal more about your condition.
During the sleep study, your healthcare team will check your blood oxygen levels, brain waves, breathing, and movements while you’re asleep.
If your sleepwalking isn’t severe, you may be able to prevent it by reducing stress in your daily life and improving your sleep habits.
If those methods don’t work well enough, your doctor may prescribe medications to help.
Clonazepam (Klonopin) and diazepam (Valium) have been shown to reduce sleepwalking. Antidepressants and benzodiazepines may help you with your stress levels so you can rest.
For most children, treatment usually isn’t necessary because sleepwalking often goes away on its own as the child matures.
Sleepwalking is a sleep disturbance in which you walk, talk, or do other activities while you’re in a deep state of sleep. It happens in the deepest part of your sleep cycle, usually within an hour or two of going to sleep.
More common in children than adults, sleepwalking is often outgrown by the teen years. But not everyone stops sleepwalking once they’re adults.
But not everyone stops sleepwalking once they’re adults.
Sleepwalking often runs in families. It can also be caused by stress, sleep deprivation, certain medications, breathing disorders, neurological conditions, stress, fever, and migraine.
If you sleepwalk often, or if your nighttime wandering is causing problems — either at night or during the day — it’s a good idea to follow up with your doctor.
What are the causes of sleepwalking? | Emergency Live
If so, you may be one of the 6.9% of people who have experienced sleepwalking at least once in their lives.
Although the prevalence in children is much higher, about 1.5% of adults have experienced episodes of sleepwalking outside of childhood.
This may be due to medications, genetics, or medical conditions that interfere with sleep.
Here's what we know about why some people sleepwalk.
What is sleepwalking?
This is a sleep disorder that occurs in the deepest part of non-REM sleep (NREM).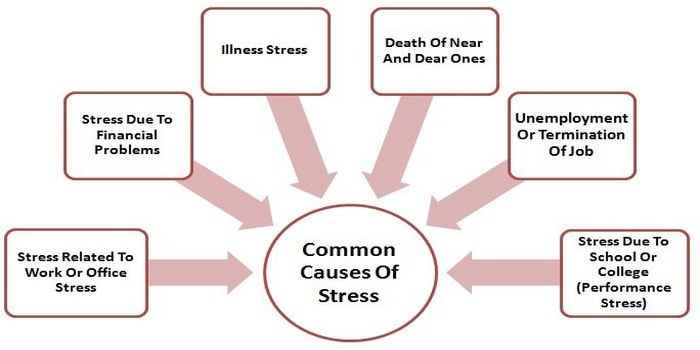
Most often this occurs within 1-2 hours after falling asleep.
During the episode, you can sit, walk, and even do normal activities in your sleep.
Your eyes are open, but in reality you are still in deep sleep.
The American Psychiatric Association does not consider it a disorder unless it occurs frequently enough to cause distress and impair your ability to function throughout the day.
What are the causes of sleepwalking?
More often in children than in adults, sleepwalking is often overcome by adolescence.
But not everyone stops sleepwalking as adults.
Although rare, some people may not begin sleepwalking until adulthood.
Sleep researchers have identified several health conditions, activities, and substances known to trigger seizures.
Stress and sleepwalking
Stress and anxiety are known to interfere with a good night's rest.
Some sleep experts also believe that daytime stress can contribute to sleepwalking.
A study of 193 patients in a sleep clinic found that one of the main triggers for episodes was stressful events experienced during the day.
If you want to reduce your daily stress so that you can rest at night, you can try stress reduction methods such as these:
- regular exercise
- practicing mindfulness
- caffeine restriction
- do breathing exercises
- try yoga
Lack of sleep
People who do not get enough sleep are more vulnerable.
Researchers who studied MRI brain scans of people with a history of sleepwalking found that sleep deprivation increases the number of sleepwalking episodes in people.
migraine
If you have a chronic migraine, you may be more vulnerable.
In 2015, a team of sleep specialists examined 100 patients who constantly sleepwalk and found a strong link between sleepwalking and lifelong headaches, especially migraines.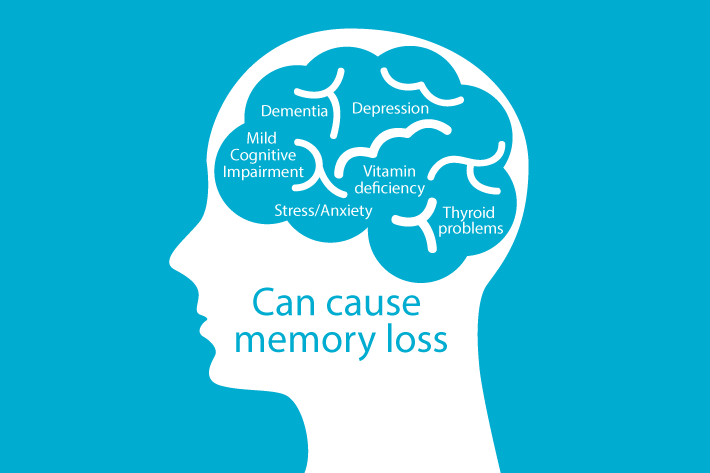
Fever and sleepwalking
Sleepwalking has been associated with illnesses that cause fever, especially in children.
Fever can also cause nightmares, which are sleep disturbances during which you may scream, wave your arms, or try to run away from the scary things you see in your dreams.
Breathing disorder
Obstructive sleep apnea is a breathing disorder in which a person stops breathing for short periods of time while sleeping.
More than just snoring.
Severe sleep apnea can lead to daytime fatigue, high blood pressure, stroke, and heart disease, among other things.
If you have severe obstructive sleep apnea, you are more likely to sleepwalk than people with mild sleep apnea.
There have also been reports of sleepwalking among children with asthma.
Asthma can lead to sleep deprivation and the drug montelukast has caused this problem in some children.
Gastroesophageal reflux disease (GERD) and sleepwalking
If you have GERD, stomach contents can back up into your esophagus, causing an uncomfortable burning sensation.
In many people, the symptoms are worse at night.
People with GERD and other stomach problems are more prone to many types of sleep disorders.
Because GERD interferes with sleep, it can cause prolonged exhaustion, which also makes you more vulnerable to seizures.
Parkinson's disease
Parkinson's disease is a nerve disease that affects your body's ability to move.
As the disease progresses, the parts of the brain stem that control movement and the parts of the brain that control sleep can be affected.
Usually when you dream during REM sleep, your brain temporarily paralyzes certain muscles so that you cannot act on your dreams and harm yourself or others in the process.
Some research suggests that Parkinson's disease may prevent sleep paralysis altogether.
This in turn can lead to sleepwalking and other sleep disorders.
Restless Leg Syndrome
There is debate among sleep researchers about whether sleepwalking causes restless leg syndrome (RLS).
Some studies show that people with RLS are no more prone to sleepwalking than other people.
Other studies point to a link between sleep problems and medications used to treat restless leg syndrome.
Some drugs can cause sleepwalking.
Some sleeping pills cause sleepwalking, including the sleep-inducing drug zolpidem, also sold under the names Ambien and Edluar.
Other drugs associated with sleepwalking include:
- sodium oxybate used to treat narcolepsy
- benzodiazepine receptor agonists
- antidepressants
- Antipsychotics used to treat mental disorders
- beta blockers used to treat heart disease and anxiety
How do you know if someone is sleepwalking?
Sleepwalkers usually don't respond when you try to get their attention.
They may have a glassy or distant look.
According to sleep experts, sleepwalkers may also engage in other activities in their condition, including:
- eating
- talk
- cook food
- urination in places other than the toilet
- trying to leave the house
- sex
Most of the time people don't remember the episode when they wake up.
If you wake someone up while they are sleepwalking, they may be confused by what is going on.
Is sleepwalking dangerous?
Although most episodes end without injury, sleepwalking can be quite dangerous.
Some people may try to drive or perform other tasks without being aware of what is actually going on around them.
In a study of 100 patients with a history of recurrent sleepwalking, 57.9% were injured or injured someone else during the episode.
Injuries were the result of accidents such as falling down stairs or hitting objects such as walls or furniture.
Because someone may harm themselves or others while sleepwalking, it is recommended to wake the sleepwalker.
Just do it carefully, because the sleepwalker might get scared when he wakes up.
When is it important to see a doctor for sleepwalking?
Most children outgrow this problem by the time they reach adolescence without even needing treatment.
However, if sleepwalking does not start before adulthood, you can talk to your doctor to rule out underlying conditions that may be causing sleepwalking.
If you often sleepwalk or if sleepwalking is causing problems in your daily activities or relationships, it is recommended that you talk to your doctor.
How is it diagnosed and treated?
The most common way to diagnose sleepwalking is to see it first hand.
Because sleepwalking most often occurs during childhood, it is parents who are most likely to report sleepwalking to healthcare professionals.
If your doctor is concerned, a sleep study can provide more information about your condition.
During the sleep study, your medical team will check your blood oxygen levels, brain waves, breathing, and movements while you sleep.
If your sleepwalking is not serious, you can prevent it by reducing stress in your daily life and improving your sleep habits.
If these methods don't work well enough, your doctor may prescribe medications to help.
Clonazepam (Klonopin) and diazepam (Valium) have been shown to reduce sleepwalking.
Antidepressants and benzodiazepines can help reduce stress levels so you can rest.
Most children do not usually need treatment because sleepwalking often goes away on its own as the child gets older.
Read also:
Emergency Live More... Live: download your newspaper's new free app for IOS and Android
Obstructive sleep apnea: what it is and how to treat it
Grinding teeth in sleep: symptoms and remedies bruxism
Long-term Covid and insomnia: "Sleep disorders and fatigue after infection"
Sleep disorders: signs that should not be underestimated
Sleepwalking: what it is, what are its symptoms and how to treat it
source:
Health line
Sleepwalking: causes, symptoms and treatment | PHARMACY
Sleepwalking (somnambulism) is a type of parasomnia, a behavioral disorder that occurs during sleep.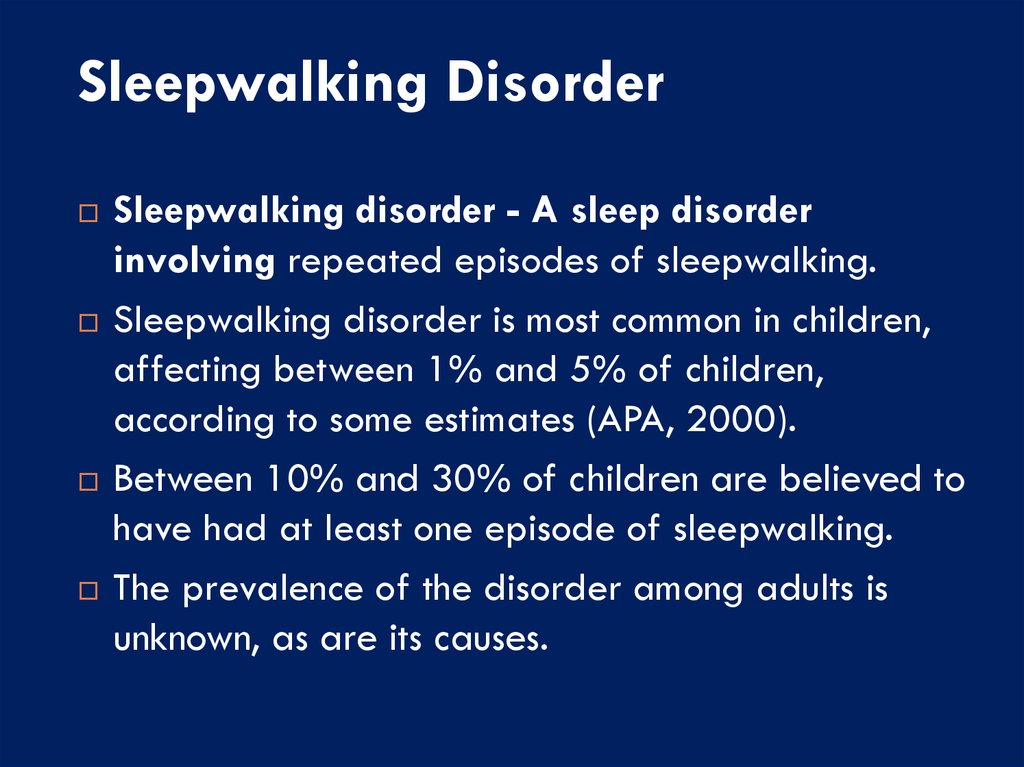 Most often detected in children aged 3-8 years. Sleepwalking is inherited and usually resolves spontaneously during adolescence.
Most often detected in children aged 3-8 years. Sleepwalking is inherited and usually resolves spontaneously during adolescence.
Sleepwalkers may get out of bed, walk, or even perform various activities such as eating or rearranging furniture, leaving the house, and driving. As a rule, persons with sleepwalking do not remember what they were doing at the time when they were supposed to sleep.
The causes of sleepwalking have not been studied in detail. Sometimes this condition is associated with any serious concomitant somatic or mental problems. Treatment for sleepwalking is about improving sleep hygiene, identifying and managing potential triggers, and keeping the patient healthy from the harm they can do to themselves during their nightly wanderings.
Sleepwalking usually occurs during incomplete awakening from deep non-REM sleep. Thus, the brain is in a transitional state between sleep and wakefulness. During sleepwalking, a person is usually clumsy and can easily stumble, fall, which can cause injury. Individuals with sleepwalking may react to the people around them, and upon awakening are usually disoriented and confused. The frequency of episodes varies from person to person. Some experience this condition on rare occasions, while others experience it several times a night.
Individuals with sleepwalking may react to the people around them, and upon awakening are usually disoriented and confused. The frequency of episodes varies from person to person. Some experience this condition on rare occasions, while others experience it several times a night.
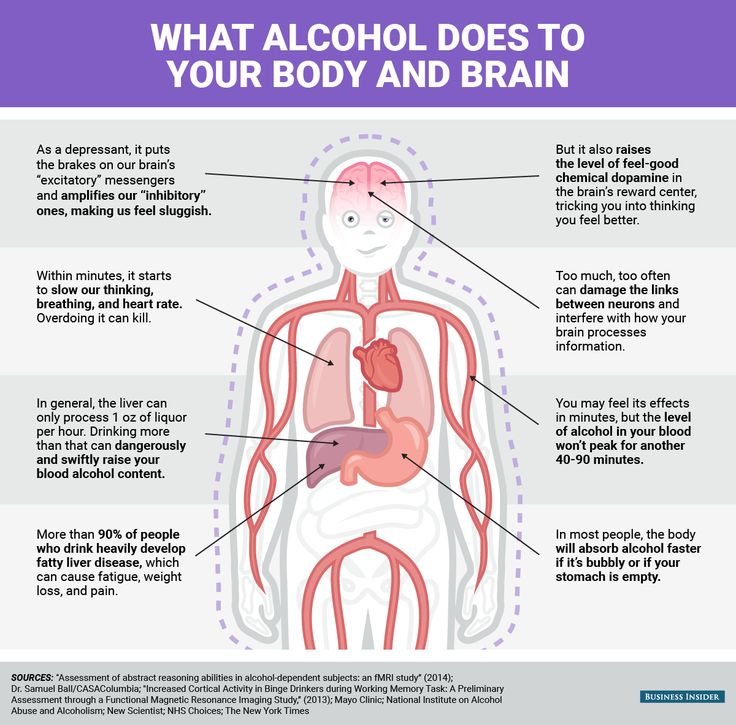
Known triggers for sleepwalking are: comorbid sleep disorders, especially obstructive sleep apnea, sleep deprivation, alcohol use, fever, pregnancy, extreme exercise or extreme fatigue, environmental stimuli, bladder filling, sleeping in a strange place, emotional or situational stress , childhood separation anxiety, medications, including phenothiazines, chloral hydrate, zolpidem, and lithium. Some pathologies, such as stroke, traumatic brain injury, migraine, or epilepsy, can also contribute to sleepwalking.
Persons who have at least a few episodes of sleepwalking should consult a doctor for advice. To establish the diagnosis of "sleepwalking", a specialist can keep a diary of sleep and awakening, which reflects the events that occur with the patient during the night.