Can ptsd cause hallucinations
Post-Traumatic Stress Disorder (Symptoms) | Center for the Treatment and Study of Anxiety
- Symptoms
- Onset & Course
- What causes PTSD?
- More Information
Symptoms
Posttraumatic Stress Disorder (PTSD) is a pathological anxiety disorder resulting after exposure to a traumatic event. Current literature estimates that 8% of the U.S. population meets the criteria for PTSD and while PTSD cases commonly involve combat or assault experiences, there is a wide range of events capable of triggering PTSD symptoms. These events include car accidents, kidnappings, terrorist attacks, natural disasters, and any other traumatic experience where an individual experienced or witnessed an event that involved death or the threat of physical harm.
For example, should a car accident occur, PTSD could result in the drivers, the passengers, or a witness; yet, the development of PTSD in one individual does not imply the development of PTSD in others involved in the incident. How one responds to an event is dependent on a variety of factors that lie outside the traumatic experience itself.
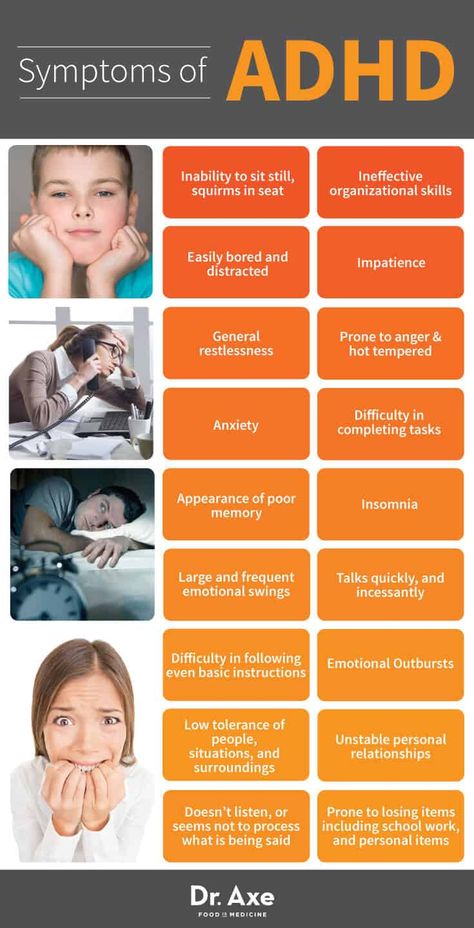
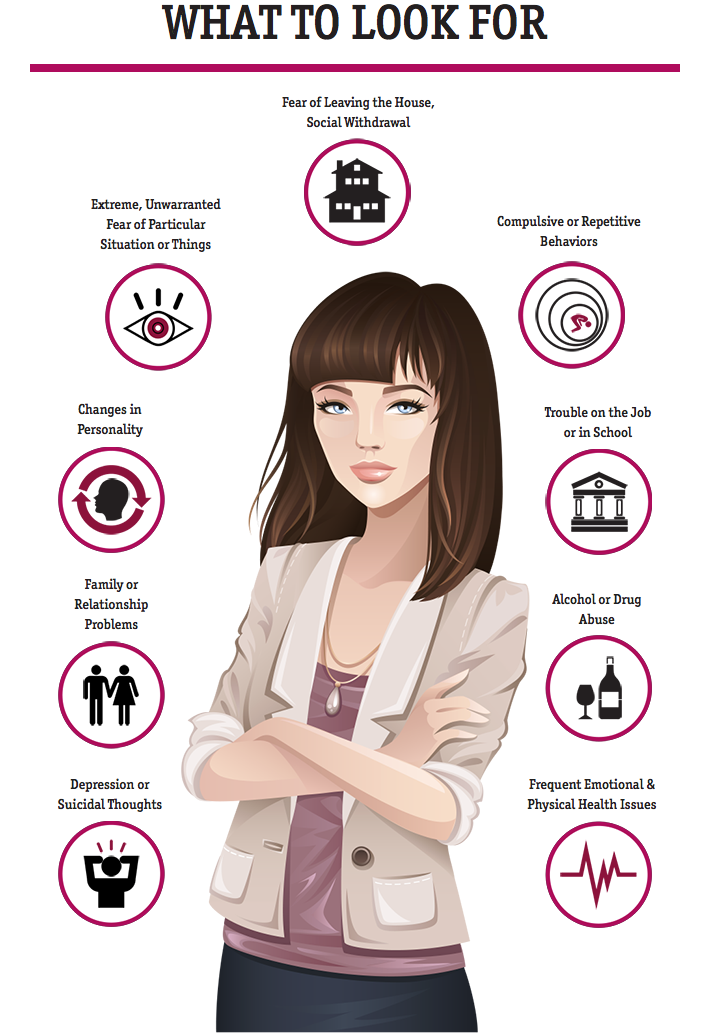
Common Symptoms
According to the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), PTSD is characterized by the following primary symptom areas (applies only for adults and children over age 6):
- Exposure to a traumatic event: Exposure to actual or threatened death, serious injury, or sexual violence in one or more ways, including:
- Directly experiencing the event
- Witnessing the event occur in person
- Learning that the event happened to a close family member or close friend
- Experiencing repeated or extreme exposure to distressing details of the event
- Intrusion or re-experiencing: Recurrent recollections of the event
- Dreams, intrusive memories, and discernable prolonged distress and physical reactions to cues that resemble the traumatic event
- Avoidance: Fear and avoidance behavior
- Avoidance of people, places, thoughts, feelings, or activities closely associated with the traumatic event
- Changes in Mood and Cognition: Negative alterations in emotions or thoughts
- Exaggerated negative beliefs and self-blame for the traumatic event, detachment from others, loss of interest, persistent negative emotional state, reduced ability to feel positive emotions
- Arousal and Hyper-reactivity: Agitation, state of constant wakefulness and alertness
- Hypervigilance, being easily startled, acting irritable or aggressive, recklessness, sleep disturbances, difficulty concentrating
Take, for example, somebody who witnesses a major car accident on a highway by their home.![]() Over the following week, the individual begins to avoid driving on that highway and over the next month, avoids driving all together - either as a driver or a passenger. He/she may become irritable or angry while watching high-speed car chase scenes or avoid conversations about driving; yet, despite the apparent discomfort, the individual may refuse to discuss his/her fear. Moreover, although the witness is unwilling to discuss the fear or the traumatic event itself, he/she may still be haunted by the memory of the accident with segments of the event on “constant replay” in his/her mind.
Over the following week, the individual begins to avoid driving on that highway and over the next month, avoids driving all together - either as a driver or a passenger. He/she may become irritable or angry while watching high-speed car chase scenes or avoid conversations about driving; yet, despite the apparent discomfort, the individual may refuse to discuss his/her fear. Moreover, although the witness is unwilling to discuss the fear or the traumatic event itself, he/she may still be haunted by the memory of the accident with segments of the event on “constant replay” in his/her mind.
Young children do not experience the same reliving of the experience as adults. The progression of PTSD in young children may initially involve dreams about the traumatic event, however, these dreams frequently transform into more generalized nightmares about monsters or different threatening situations where they or another person is in danger. It is more difficult for children to express their sentiments verbally. Therefore, it is necessary for parents or teachers or other adult observers to recognize behavioral changes such as a decreased interest in activity or an altered sense of the future (i.e. the child now believing that he/she will no longer live to become an adult). Other signs of childhood PTSD may occur in the form of repetitive play if the child begins to recreate the incident with toys or may occur through the emergence of physical symptoms such as headaches or stomach aches.
Therefore, it is necessary for parents or teachers or other adult observers to recognize behavioral changes such as a decreased interest in activity or an altered sense of the future (i.e. the child now believing that he/she will no longer live to become an adult). Other signs of childhood PTSD may occur in the form of repetitive play if the child begins to recreate the incident with toys or may occur through the emergence of physical symptoms such as headaches or stomach aches.
An individual’s PTSD might include symptoms such as feelings of shame, or less commonly, compulsive or aggressive behaviors, or self-destructive behavior. These cases often interfere with an individual’s personal life and thus, they are also associated with certain social patterns. These patterns may include sexual dysfunction, marital conflicts, and job loss. There are also strong feelings of guilt and despair that lead to social withdrawal and substance abuse.
Rare cases of PTSD may involve auditory hallucinations and paranoid ideation. Individuals who experience auditory hallucinations may experience tinnitus, a constant ringing in one’s ears, or they may hear a voice or set of voices that are not physically present. Individuals who are experiencing paranoid ideation are highly guarded and constantly suspicious of being harmed and harassed by those around them. When the trauma involves violent death, symptoms of both complicated grief and PTSD may be present.
Individuals who experience auditory hallucinations may experience tinnitus, a constant ringing in one’s ears, or they may hear a voice or set of voices that are not physically present. Individuals who are experiencing paranoid ideation are highly guarded and constantly suspicious of being harmed and harassed by those around them. When the trauma involves violent death, symptoms of both complicated grief and PTSD may be present.
Back to Top
Onset & Course
The development of PTSD is somewhat unpredictable and can occur at any age. The severity and timing of PTSD symptoms differ with each individual; while symptoms usually begin within the first 3 months after the trauma, there can be a delay of months or even years before a person meets criteria to be diagnosed with PTSD.
PTSD typically develops immediately after the trauma. Nonetheless, in some cases symptoms may not emerge until years have passed since the event. Additionally, a traumatic incident may cause mild PTSD symptoms in one individual while chronically debilitating another. Duration of symptoms also varies, with some people recovering from trauma naturally in the first 3 months, and others experiencing symptoms for months or years.
Duration of symptoms also varies, with some people recovering from trauma naturally in the first 3 months, and others experiencing symptoms for months or years.
All PTSD sufferers usually experience a range of symptoms after a traumatic episode. These symptoms are maintained through avoidance behavior and treatment must be actively pursued in order for complete recovery. Particular variables surrounding the traumatic event may, however, influence the development of PTSD. Elements that are known to make PTSD more likely are the following:
- Perceived life threat
- Personal injury
- Interpersonal violence, particularly perpetrated by a caregiver
- Past and present vulnerability, including genetics, childhood trauma, insufficient emotional support, concurrent causes of stress
Example: Childhood abuse and rape
Symptoms of PTSD may emerge later in life. Example: “When I was child, I was abused by my uncle. I was scared by it at first but I eventually came to accept it. He stopped when I was twelve (I have not seen him since). I tried to forget him and blocked the memory from my mind. I had a healthy romantic life throughout high school and college. I dated numerous people and have been involved in two serious relationships. Last year, however, my best friend was raped by a co-worker. I consoled her and she recovered from the experience but since then, I have not been able to stop thinking about my uncle..."
I was scared by it at first but I eventually came to accept it. He stopped when I was twelve (I have not seen him since). I tried to forget him and blocked the memory from my mind. I had a healthy romantic life throughout high school and college. I dated numerous people and have been involved in two serious relationships. Last year, however, my best friend was raped by a co-worker. I consoled her and she recovered from the experience but since then, I have not been able to stop thinking about my uncle..."
Back to Top
What causes PTSD?
Why one person gets PTSD and not another is not completely understood. However, a traumatic experience is required for a diagnosis. Trauma events frequently associated with the development of PTSD include the following:
- Physical, emotional, or sexual abuse
- Combat experiences
- Terrorist attacks
- Natural disasters such as tornados, floods, earthquakes, or fires
- Life-threatening accidents, such as automobile accidents, airplane crashes, or boating accidents both experienced or witnessed
- Violent crimes, both experienced or witnessed
Epidemiological information
The prevalence of PTSD differs according to both gender and ethnicity.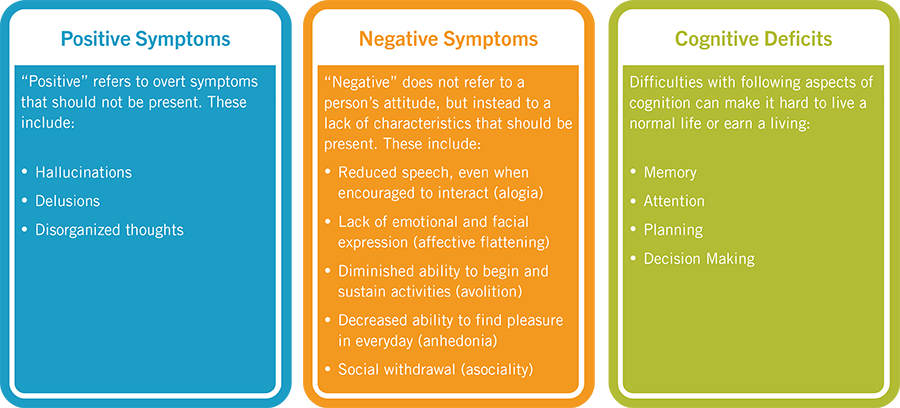 An estimated 8.7% of the U.S. adult population matches the criteria for PTSD with women more likely to develop symptoms than men. Compared with non-Latino European Americans within the U.S., elevated rates of PTSD have been reported mainly among U.S. Latinos, African Americans, and American Indians. Research also suggests that Asian-Americans have the lowest rates of PTSD within the country. These differences are attributed to a variety of cultural and socioeconomic phenomena.
An estimated 8.7% of the U.S. adult population matches the criteria for PTSD with women more likely to develop symptoms than men. Compared with non-Latino European Americans within the U.S., elevated rates of PTSD have been reported mainly among U.S. Latinos, African Americans, and American Indians. Research also suggests that Asian-Americans have the lowest rates of PTSD within the country. These differences are attributed to a variety of cultural and socioeconomic phenomena.
Lower estimates are seen in Europe and most Asian, Latin American, and African countries, ranging from around 0.5% to 1%. This follows the general finding that developed countries have significantly lower rates of PTSD than the developing world. The prevalence of PTSD in the developing world is, however, reasonable given the harsher political and economic climates.
Back to Top
More Information
National Institute of Mental Health (NIMH) - An organization with the National Institute of health dedicated to mental health research:
http://www. nimh.nih.gov/health/topics/post-traumatic-stress-disorder-ptsd/index.shtml
nimh.nih.gov/health/topics/post-traumatic-stress-disorder-ptsd/index.shtml
Army Behavioral Health - A PTSD informational website provided by the U.S. Army Medical Department for the support of Soldiers and their families:
http://armymedicine.mil/Pages/behavioralhealth.aspx
National Center for PTSD (NCPTSD) - A center established by the U.S. Department of Veteran Affairs to improve the well-being of U.S. veterans through PTSD research and education:
www.ncptsd.va.gov/
All About PTSD and Hallucinations
Could those elusive sounds you’re hearing actually be post-traumatic stress disorder (PTSD) hallucinations?
There are many anticipated symptoms that can accompany a post-traumatic stress disorder (PTSD) diagnosis. You might experience anything from flashbacks and avoidant behaviors to sleep disturbance.
What you might not expect to experience, however, are reality-altering changes like hallucinations.
While hallucinations are not typically considered one of the “classic” symptoms of PTSD, a growing body of research indicates these sensory experiences aren’t uncommon in trauma-spectrum disorders.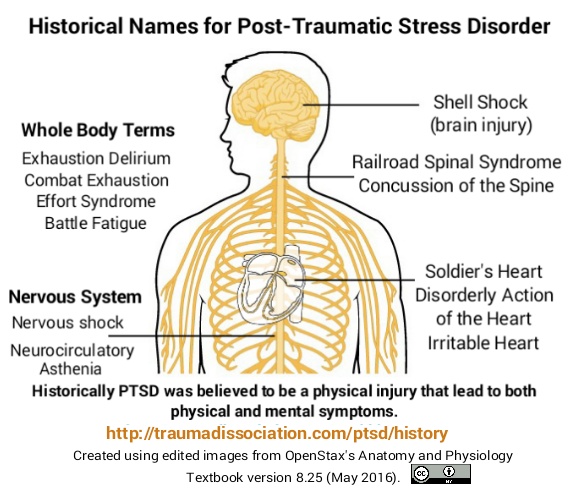
PTSD is a mental health condition that can occur when you’ve experienced or witnessed trauma, such as physical harm or threat.
PTSD can be an impairing disorder characterized by reexperiencing traumatic events and engaging in avoidance behaviors that can impact almost every aspect of daily functioning.
Not everyone who is exposed to a dangerous or traumatic experience will develop PTSD. For many people, the body’s natural reactions to trauma fade over time.
In a moment of danger, your heart rate and breathing may quicken, for example, and you might feel fear or other overwhelming negative emotions.
Afterward, you’re typically able to move on from the trauma. And while you may never forget it, you don’t necessarily experience the effects for a prolonged period of time.
But if you’re living with PTSD, you may still feel the effects. For someone with PTSD, some of those fight, flight, or freeze responses last long after the event, almost as if you’re stuck in perpetual survival mode.
PTSD occurs as the result of a traumatic experience. You may have played an active role in the event, or you might have witnessed a traumatic situation unfold.
Anyone, at any age, can develop PTSD.
Common causes of PTSD can include:
- physical danger
- injury
- near-death experience
- combat
- sexual or physical assault
- abuse
- illness
- natural disaster
- death of a loved one
- crime
- violence
What causes PTSD in your brain?
While PTSD is caused by a traumatic experience, the reason why your brain remains in survival mode is less obvious.
Research from 2022 suggests changes to the brain’s structure and neurophysiology may be responsible for many of the symptoms seen in PTSD.
These changes can create a unique dynamic where some regions of the brain might become hyperresponsive, while others may go into a state of reduced function.
The Diagnostic and Statistical Manual of Mental Disorders, 5th edition (DSM-5) lists four categories of symptoms that appear in a PTSD diagnosis:
- Intrusive.
 Symptoms that cause reexperiencing, such as distressing dreams, flashbacks, unwelcome memories, and intrusive thoughts.
Symptoms that cause reexperiencing, such as distressing dreams, flashbacks, unwelcome memories, and intrusive thoughts. - Avoidant. Actively working to avoid people, places, and things that may remind you of the traumatic event. You may also attempt to avoid talking about it or thinking about it.
- Cognitive or mood. Experiencing changes in mood, an inability to recall events around the trauma, or developing distorted beliefs.
- Arousal or reactivity. Feeling irritable or participating in risky behaviors. You may be prone to outbursts, be easily startled, feel constantly on edge, or experience hypervigilance or feelings of “high alertness.” You may also experience sleep disturbance.
PTSD, and the traumatic experience it arises from, can be very personal. You may not have every symptom listed in the DSM-5.
For some people, you may even experience symptoms not considered criteria in the DSM-5 — like PTSD hallucinations.
Flashbacks vs. hallucinations
Experiencing flashbacks and hallucinations are not the same thing. And while flashbacks are often portrayed as a common symptom of PTSD in media and used for storytelling, they are not a usual feature of this condition.
Yes, you can experience hallucinations with PTSD.
While this symptom isn’t a part of the DSM-5 criteria for post-traumatic stress disorder, expanding research suggests hallucinations may be more common than originally thought among trauma-spectrum disorders.
In a 2020 study among women living with PTSD, researchers found that 46% reported clear auditory hallucinations in the form of voices.
Similar findings were reported in an earlier study from 2000, which found that 30% to 40% of combat veterans living with PTSD reported auditory or visual hallucinations and delusions.
Psychosis
Traditionally, hallucinations and delusions are classified as symptoms of psychosis. Psychosis is characterized by your brain’s inability to distinguish between what’s real and what isn’t.
However, psychotic-like experiences with PTSD are not necessarily considered classic psychosis.
A study from 2005 examined the prevalence of psychosis symptoms among people living with PTSD or trauma exposure. Researchers found that an array of psychosis symptoms were noted among participants.
The severity of a traumatic event was associated with the severity of symptoms experienced. When it came to PTSD hallucinations, they were most commonly associated with experiences of sexual abuse.
However, this research is far from conclusive. It’s important to note that this study was conducted on a sample of people with a preexisting psychotic disorder, and only half of all participants were living with PTSD.
Hallucinations are sensory experiences that can arise from an interruption in reality. They can involve any of your senses, meaning you can see, smell, hear, taste, or feel things that aren’t really there.
Clinically, sensory types of hallucinations are referred to as:
- auditory (hearing)
- olfactory (smell)
- tactile (external touch)
- gustatory (taste)
- visual (sight)
- somatic (internal sensation)
However, auditory hallucinations may be the most common among people with PTSD.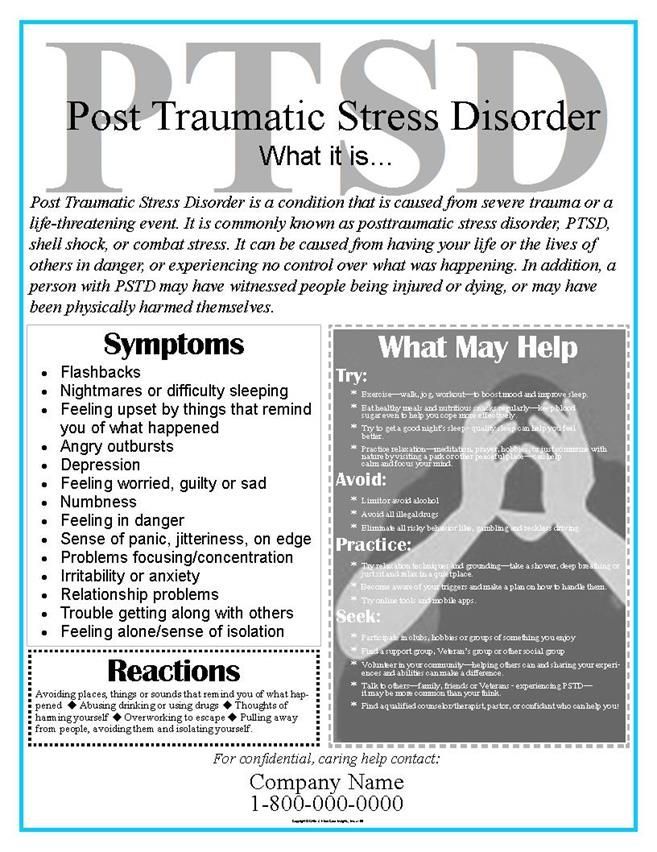
In general, hallucinations may be the result of:
- PTSD
- schizophrenia
- affective disorders (severe depression)
- postpartum psychosis
- psychoactive substances
- delirium tremens
- alcoholic hallucinosis
- brain injury
- delirium
- Alzheimer’s disease
- Lewy body dementia
- Parkinson’s disease
- ear diseases
- eyes diseases
- grief
People with borderline personality disorder (BPD) may also experience hallucinations, though this might be less common. Only 29% of participants with BPD in a 2010 study reported experiencing hallucinations.
Predictive coding in the brain
A 2017 study showed significant genetic commonalities between PTSD and schizophrenia.
While this doesn’t explain the exact mechanism that creates PTSD hallucinations, like in schizophrenia, experts believe these altered perceptions of reality may come from skewed predictive coding in the brain.
Predictive coding is a theoretical concept suggesting that your brain is in a constant state of updating based on anticipated (or predicted) sensory inputs.
Research from 2020 on predictive coding and PTSD hallucinations indicates that incorrect assumptions from the brain may contribute to skewed sensory perception.
In other words, if your brain ignores the correct sensory input in favor of a trauma-informed response, you might experience a hallucination.
Hallucinations can be a symptom of underlying PTSD.
Treating PTSD hallucinations often means addressing your PTSD first. Long-term relief from PTSD often requires guidance from a mental health care professional.
PTSD treatment
If you have PTSD, there is an array of treatment options to help you manage symptoms.
Therapy is often a foundational method for treating PTSD. Medication is also sometimes prescribed to take the edge off of anxiety or hyperarousal from PTSD, but it is not considered as effective in treating other PTSD symptoms.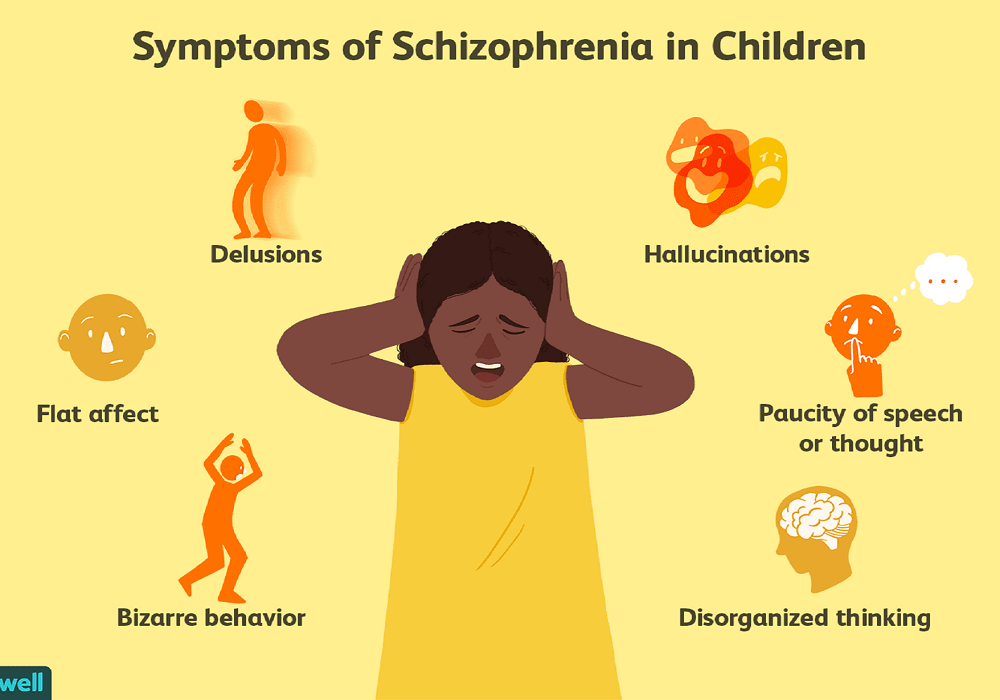
PTSD treatment may involve:
- prolonged exposure therapy (PE)
- cognitive behavioral therapy (CBT)
- cognitive processing therapy (CPT)
- Eye Movement Desensitization and Reprocessing (EMDR)
- brief eclectic psychotherapy (BEP)
- narrative exposure therapy (NET)
- eclectic psychotherapy
Treating PTSD with hallucinations
You may also be prescribed an antipsychotic medication to help manage hallucinations during your PTSD treatment process.
For PTSD with hallucinations, you may also benefit from:
- transcranial magnetic stimulation (TMS)
- psychoeducation
- ABC analysis of voices
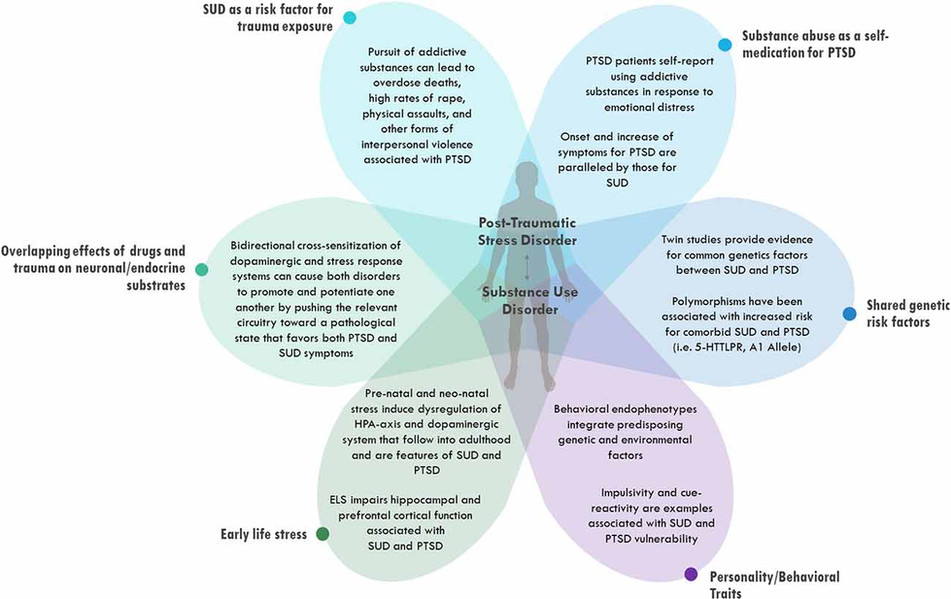
PTSD commonly occurs alongside other mental health conditions, especially:
- depressive disorders, particularly major depressive disorder (MDD)
- anxiety disorders
- substance use disorders
Which one comes first is typically debatable and often depends on the individual.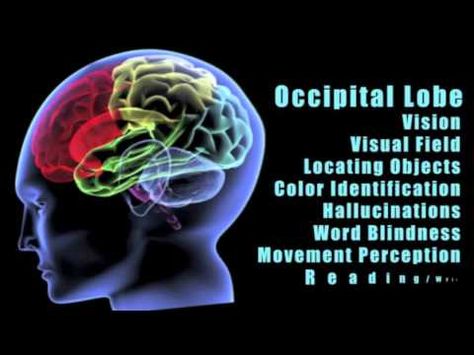
Since PTSD is the result of trauma, it can be found as a precursor to substance use disorders, which may result from unhelpful coping strategies.
The cause-and-effect relationship goes both ways, however.
Living with an anxiety disorder or another mental health condition prior to a traumatic experience may increase your risk of experiencing PTSD.
Sometimes, the stress of living with a mental health condition may contribute to PTSD development.
A 2021 systematic review of PTSD and psychosis found that experiencing psychosis could be considered traumatic enough to cause PTSD.
After a traumatic event, living with PTSD can be a challenging reminder of your experience.
You may display symptoms of reexperiencing and avoidance, and you may also live with co-occurring mental health conditions, like anxiety and depression.
PTSD hallucinations can be an intimidating and unexpected addition to the other symptoms you may be dealing with. You may even feel reluctant to tell those closest to you, especially if you aren’t even sure yourself what’s happening.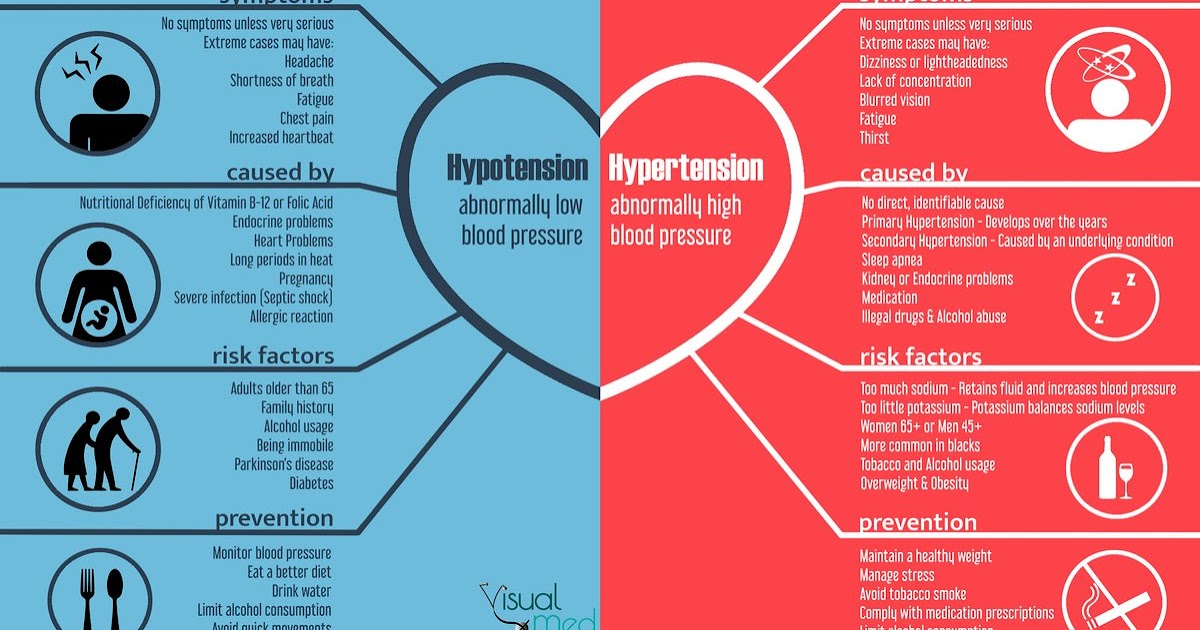
But if you’re experiencing PTSD with hallucinations or psychosis, you can know that you aren’t alone.
You don’t have to live with PTSD or hallucinations forever. The right treatment can make PTSD manageable. And when PTSD is managed, PTSD hallucinations often go away as well.
Finding relief often begins with seeking help from a doctor or therapist to address the underlying PTSD. If you’re ready to get help but don’t know where to begin, you can check out Psych Central’s guide to finding mental health care.
Suicide prevention
Everyone’s trauma is unique. If you’re considering self-harm or suicide, it’s important to remember that you’re not alone and resources are available to you. If you need to talk with someone right away, you can:
- Call the National Suicide Prevention Lifeline, available 24 hours a day at 800-273-8255.
- Text “HOME” to the Crisis Text Line at 741741.
Not in the United States? You can find a helpline in your country with Befrienders Worldwide.
PTSD
") end if %>
Variant of Acrobat Samana Gaze | Acrobat Reader Samana Download
PTSD is a normal response
for severe traumatic events.
This booklet deals with signs,
symptoms and treatments for PTSD.
New York State
Department of Mental Health
Have you experienced a terrible and dangerous event? Note please, those cases in which you recognize yourself.
- Sometimes, out of the blue, everything that happened to me is happening again. I never know when to expect it again.
- I have nightmares and memories of the terrible incident which I have experienced.
- I avoid places that remind me of that incident. nine0024
- I jump on the spot and feel uneasy at any sudden movement or surprise. I feel alert all the time.
- It's hard for me to trust someone and get close to someone.

- Sometimes I just feel emotionally drained and deaf.
- I get angry very easily.
- I am tormented by guilt that others died, but I survived.
- I sleep poorly and experience muscle tension. nine0024
PTSD is a very serious condition that needs to be treated.
Many people who have experienced terrible events suffer from this disease.
It is not your fault that you fell ill, and you should not suffer from it.
Read this booklet to find out how you can be helped.
You can get well and enjoy life again!
What is post-traumatic stress disorder (PTSD/PTSD)?
PTSD is a very serious condition. PTSD symptoms may occur in a person who has experienced a terrible traumatic event. This disease is susceptible medical and therapeutic treatment. nine0003
PTSD can occur after you:
- Have been a victim of sexual abuse
- Have been a victim of physical or emotional domestic violence
- Victim of a violent crime
- Been in a car accident or plane crash
- Survived a hurricane, tornado, or fire
- Were at war
- Survived a life-threatening event
- Witnessed any of the above events
If you have post-traumatic stress disorder, you often have nightmares or memories associated with the event.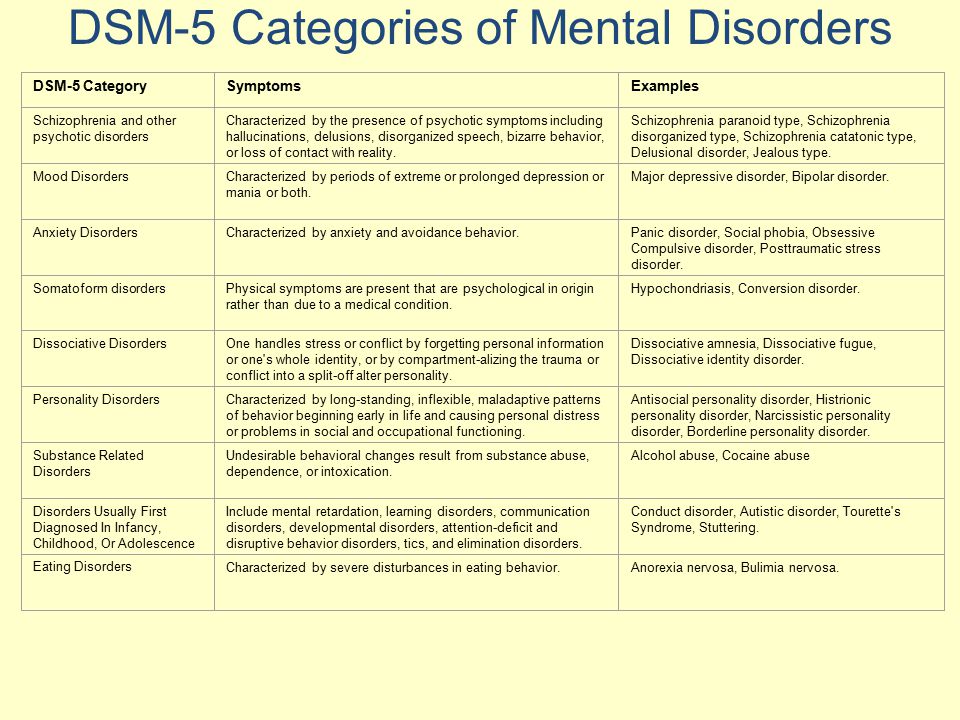 you try to hold on away from anything that might remind you of the experience.
you try to hold on away from anything that might remind you of the experience.
You are bitter and unable to trust or care for others. You are always on your guard and see a hidden threat in everything. You become not by itself, when something happens suddenly and without warning.
When does PTSD start and how long does it last? nine0011
In most cases, post-traumatic stress manifests itself approximately three months after the traumatic event. In some cases, signs Post-traumatic stress symptoms only show up years later. Post-traumatic Stress affects people of all ages. Even children are not immune from it.
Some get better after six months, others may suffer from it illness for much longer.
Am I the only one with this disease? nine0011
No, you are not alone. Every year, 5.2 million Americans suffer from PTSD.
Women suffer from this disease two and a half times more often than men. The most common traumatic events that cause PTSD in men are: rape, participation in hostilities, abandonment and abuse in childhood.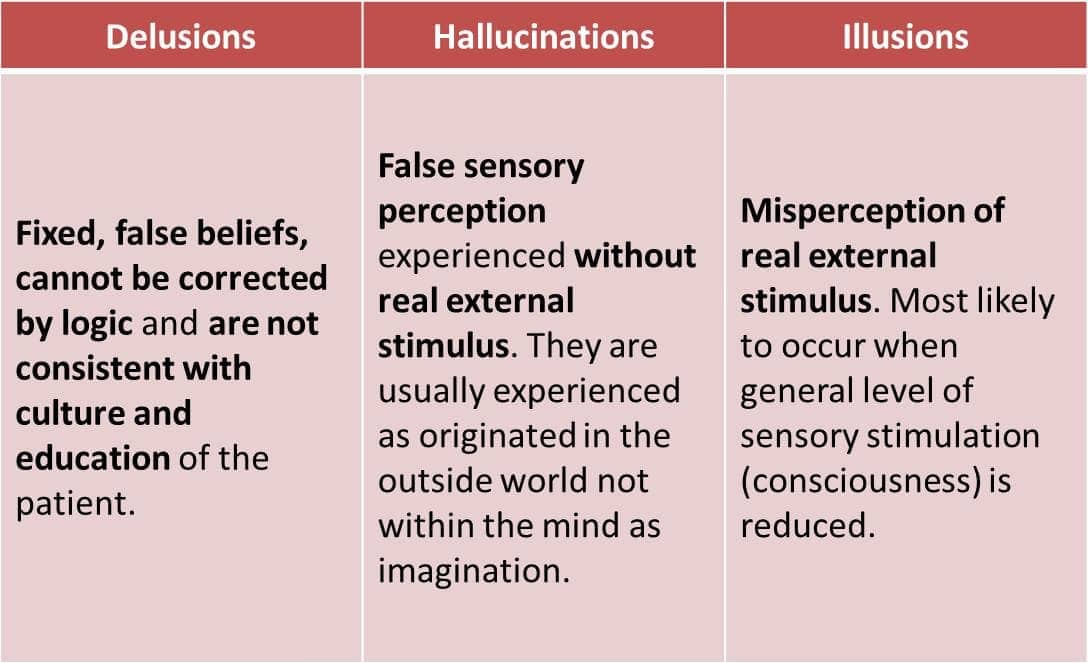 The most traumatic events in women are rape, sexual molestation, physical assault, threat weapons and childhood abuse. nine0003
The most traumatic events in women are rape, sexual molestation, physical assault, threat weapons and childhood abuse. nine0003
What other conditions can accompany PTSD?
Common depression, alcoholism and drug addiction, or other anxiety disorders. The likelihood of successful treatment increases if these comorbidities to identify and treat in time.
Frequent headaches, gastroenterological problems, problems with the immune system, dizziness, chest pain or discomfort in other parts of the body. It often happens that a doctor treats physical symptoms, unaware that their cause lies in PTSD. nine0003
The National Institute of Mental Health (NIMH) recommends therapists to learn from patients about experiences of violence, recent losses and traumatic events, especially when symptoms persist are returning. After diagnosing PTSD, it is recommended to refer patient to a mental health specialist who has experience in the treatment of patients with PTSD.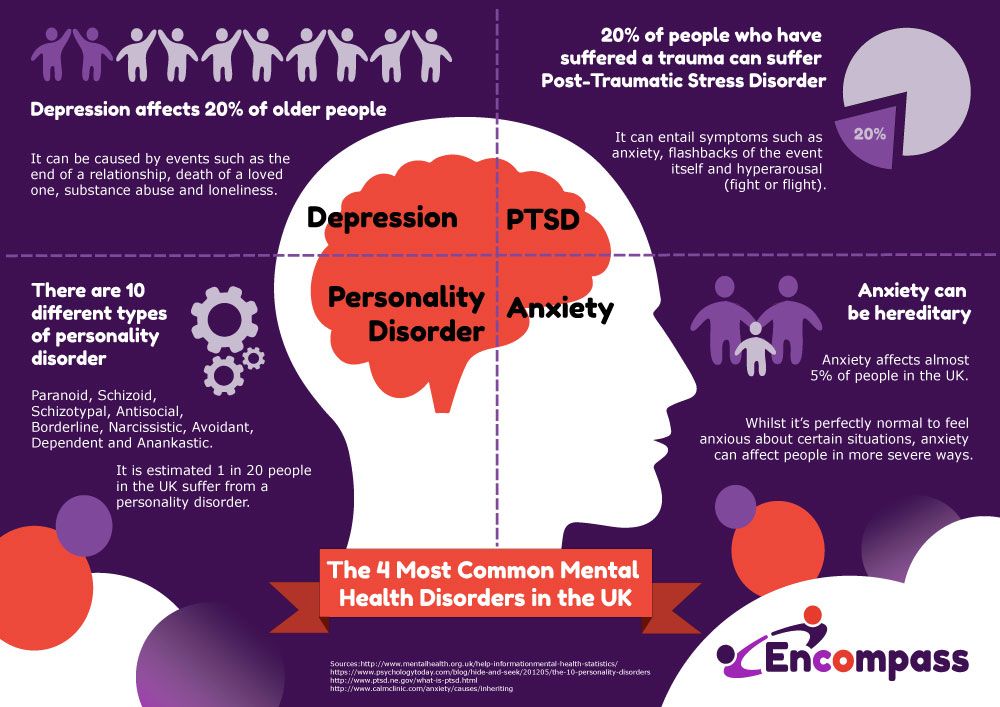
What should I do to help myself in this situation? nine0011
Talk to your doctor and tell him about your experience, and how you feel. If you are visited by terrible memories, overcomes depression and sadness if you have trouble sleeping and constantly embittered - you should tell your doctor about all this. Tell him Are any of these conditions preventing you from doing your daily activities? lead a normal life. You may want to show this booklet to your doctor. This may help explain to him how you feel. Ask your doctor examine you to make sure there are no physical illnesses. nine0003
Ask your doctor if he has had patients with post-traumatic stress. If your doctor does not have a special preparation, ask him for directions to doctor with relevant experience.
How can a doctor or psychotherapist help me?
Your doctor may prescribe medicine to help reduce your fear or tension. However, it should be borne in mind that usually several weeks before the medicine starts to work.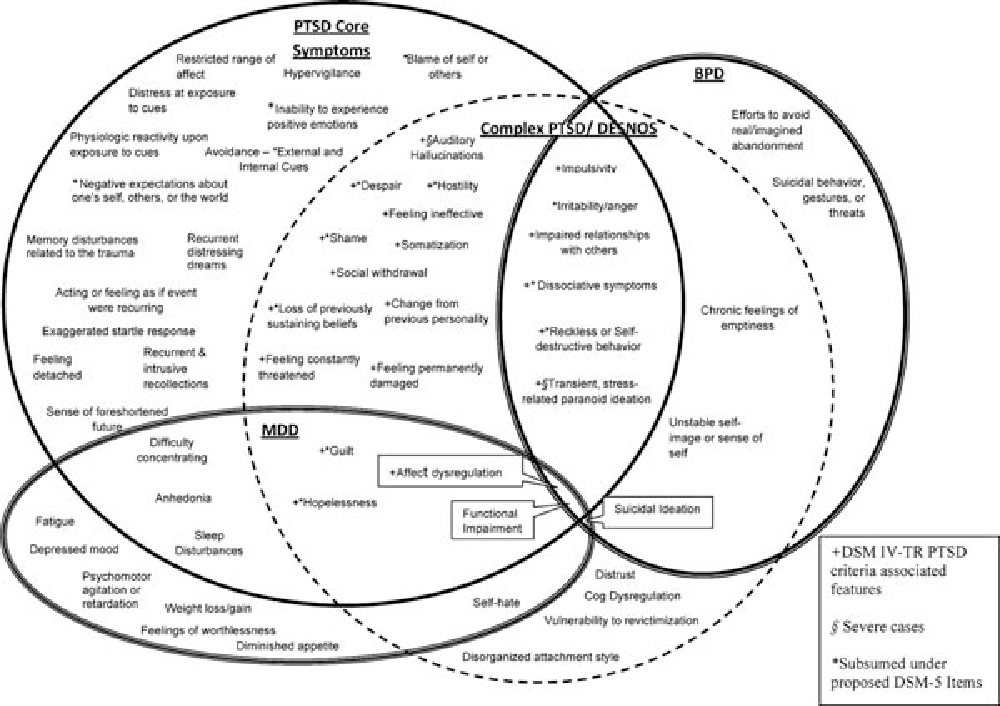 nine0003
nine0003
Many PTSD sufferers benefit from talking with a professional or other people who have experienced traumatic events. This is called "therapy". Therapy will help you get over your nightmare.
One man's story:
"After I was attacked, I He constantly felt fear and depression, became irritable. I couldn't sleep well and lost my appetite. Even when I tried not think about what happened, I was still tormented nightmares and terrible memories. nine0003
“I was completely at a loss and didn't know what to do. one buddy advised to see a doctor. My doctor helped me find a specialist in post-traumatic stress."
“I needed a lot of strength, but after medication and a course of therapy, I gradually come to my senses. It’s good that I called my doctor then.”
PTSD and the military
If you are in the military, you have probably been in combat. You, probably got into terrible and life-threatening situations.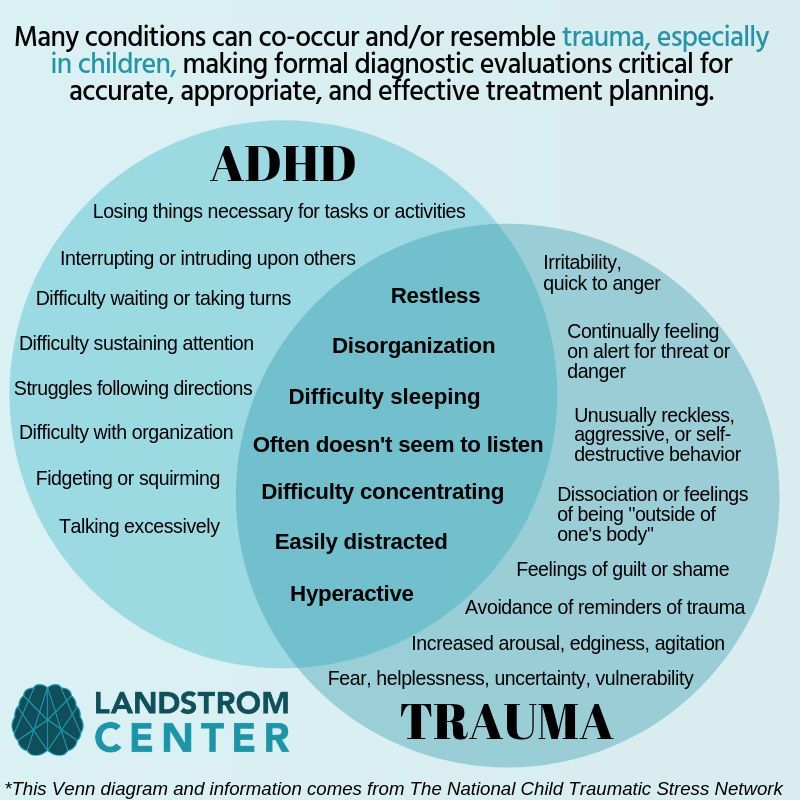 They shot at you you have seen your friend shot, you have seen death. experienced you events can cause PTSD. nine0003
They shot at you you have seen your friend shot, you have seen death. experienced you events can cause PTSD. nine0003
Experts say that PTSD occurs:
- Nearly 30% of Vietnam War veterans
- Nearly 10% of Gulf War veterans (Operation Desert Storm)
- Almost 25% of veterans of the war in Afghanistan (operations "Introducing freedom") and veterans of the war in Iraq (operations "Iraqi Freedom")
Other factors of the military situation can serve as an additional stress to and so stressful situation and can contribute to the development of PTSD and other mental problems. Among these factors are the following: your military specialty, the political aspects of the war, where the battle takes place and who your enemy is. nine0003
Another reason that contributes to PTSD in military personnel can be Military Sexual Assault (MST) – any form of sexual harassment or sexual abuse while serving in the military. MST can happen with men and women, and can occur in peacetime, during war training or during the war.
MST can happen with men and women, and can occur in peacetime, during war training or during the war.
Veterans Affairs (VA) health care approximately:
- 23 out of 100 women (23%) report sexual violence during military service
- 55 out of 100 women (55%) and 38 out of 100 men (38%) were exposed to sexual harassment while serving in the army
Although the trauma of sexual assault is more common in the military among women, more than half of veterans who have experienced sexual trauma violence in the army - it's men.
Remember, you can get the help you need right now:
Tell your doctor about your experience and how you feel. If your doctor does not have special training in the treatment of PTSD, ask him for a referral to a doctor who has relevant experience.
PTSD research
To help those suffering from PTSD, the National Institute of Conservation Mental Health (NIMH) supports research into the study of PTSD, as well as other thematically related to PTSD research on problems anxiety and fear.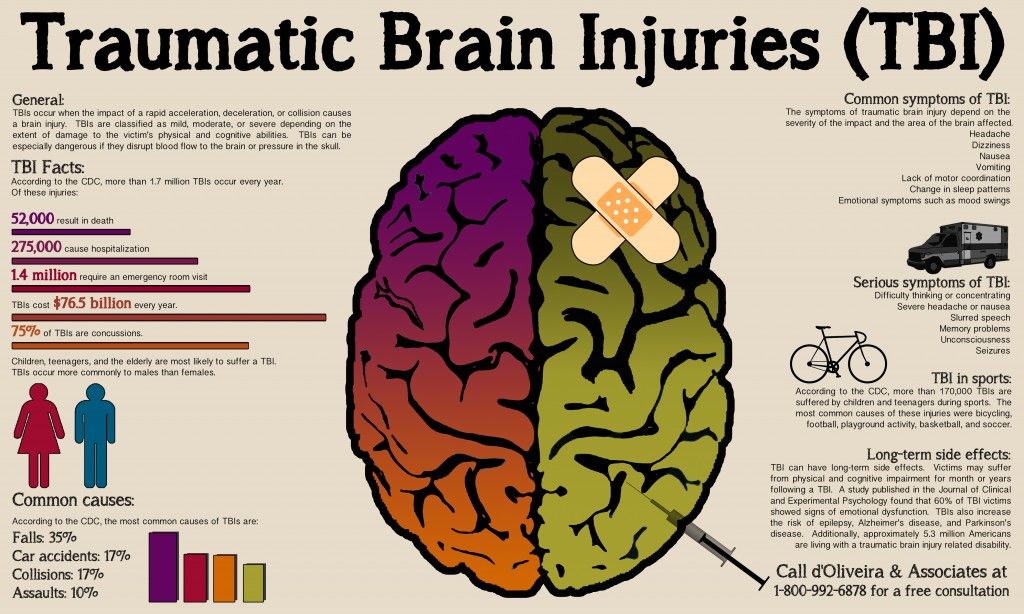 The challenge for research is to find new ways to help people cope with trauma, as well as find new treatment options and, The main thing is to prevent disease. nine0003
The challenge for research is to find new ways to help people cope with trauma, as well as find new treatment options and, The main thing is to prevent disease. nine0003
Research on possible risk factors for PTSD
Today, the attention of many scientists is focused on genes that play a role in having terrible memories. Understanding the mechanism of "creation" of scary memories can help improve or find new ways to alleviate symptoms of PTSD. For example, PTSD researchers have identified genes that are responsible for:
Statmin is a protein involved in the formation of terrible memories. During one experiment, mice were placed in environment designed to instill fear in them. In this situation mice lacking the statmin gene, in contrast to normal mice were less likely to "freeze" - i.e. exercise natural defensive response to danger. Also in the environment designed to evoke innate fear in them, they demonstrated it to a lesser extent than normal mice, more willingly mastering the open "dangerous" space.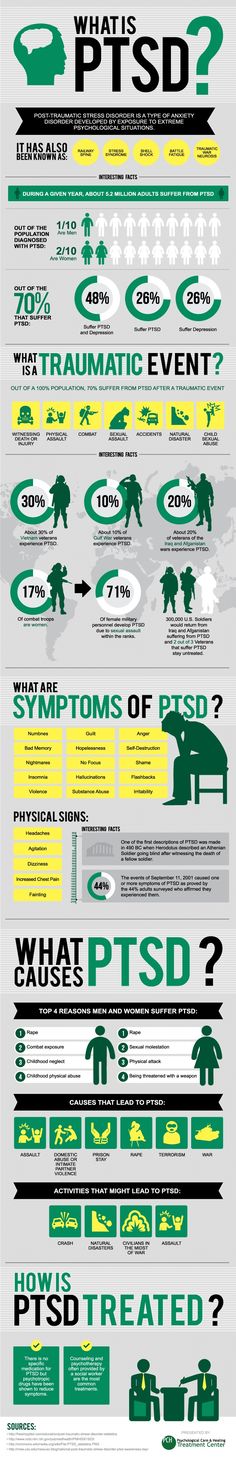 nine0184 1
nine0184 1
GRP (gastrin-releasing peptide/GRP) - signal substance brain released during emotional events. At in mice, GWP helps control the fear response, and lack of GWP can lead to a longer memory of fear. 2
Scientists have also discovered a variant of the 5-HTTLPR gene that controls serotonin (a brain substance associated with mood), which, as it turns out, feeds the fear response. nine0184 3 It seems that, like in the case of other mental disorders, in the development of PTSD different genes are involved, each of which contributes to the formation of the disease.
Understanding the causes of PTSD can also be helped by studying different areas brain responsible for fear and stress. One of these areas is cerebellar amygdala, responsible for emotions, learning and memory. It turned out that she plays an active role in the emergence of fear (or other words, "teaches" to be afraid of something, for example, to touch a hot stove), as well as in the early phases of fear repayment (or in other words, "teaches" Do not be scared). nine0184 4
nine0184 4
The retention of faded memories and the weakening of the initial fear reaction are associated with the prefrontal cortex (PFC / PFC) of the brain, 4 responsible for decision making, problem solving and situation assessment. Each zone PFC has its own role. For example, when the PFC believes that a stressor is amenable to control, the medial prefrontal zone of the PFC suppresses the anxiety center deeply in the brainstem and controls the response to stress. nine0184 5 Ventromedial PFC helps maintain long-term fading of fearful memories, and her ability to perform this feature can be affected by its size. 6
Individual differences in genes or characteristics of regions of the brain brain can only set the stage for PTSD, but by themselves do not cause no symptoms. environmental factors such as childhood trauma, head trauma or mental illness in family, favor the development of the disease and increase the risk of disease, affecting the brain in the early stages of its growth. nine0184 7 Except In addition, how people adapt to trauma is likely to be influenced by and characteristics of character and behavior, such as optimism and a tendency to consider problems in a positive or negative way, as well as social factors such as availability and use of social support. 8 Further research may show what combination of these factors or what other factors will allow ever predict who has a traumatic event cause PTSD, and who doesn't. nine0003
nine0184 7 Except In addition, how people adapt to trauma is likely to be influenced by and characteristics of character and behavior, such as optimism and a tendency to consider problems in a positive or negative way, as well as social factors such as availability and use of social support. 8 Further research may show what combination of these factors or what other factors will allow ever predict who has a traumatic event cause PTSD, and who doesn't. nine0003
PTSD research
Currently, psychotherapy is used in the treatment of PTSD ("talk" therapy), drugs or drug-therapeutic combination.
Psychotherapy
Cognitive behavioral therapy (CBT) helps you learn differently think and react to frightening events that are the impetus for development PTSD, and can help bring the symptoms of the disease under control. There are several types cognitive behavioral therapy, including:
"Push" method - uses mental images, notes or visiting a place experienced trauma to help those affected face the overwhelming their fear and take control of it.
Behavior restructuring (cognitive restructuring) - encourages survivors of a traumatic event express depressing (often erroneous) thoughts about experienced trauma, challenge these thoughts and replace them with more balanced and appropriate. nine0003
Implementation in a stressful situation - teaches ways to reduce anxiety and the ability to cope with it, helping to reduce the symptoms of PTSD, and helps to correct the erroneous train of thought associated with the trauma experienced. NIMH is currently conducting research to study the reaction brain response to cognitive behavioral therapy versus response sertraline (Zoloft) - one of two drugs recommended and approved US Food and Drug Administration funds (FDA) for the treatment of post-traumatic stress. This research may help find out why some people respond better to medications, and others for psychotherapy
Drugs
Recently, in a small study, NIMH scientists found that if patients who are already taking a dose of prazosin (Minipress) at bedtime, add a daily dose, then this weakens the general symptoms of PTSD and stress reaction to reminders of the trauma experienced.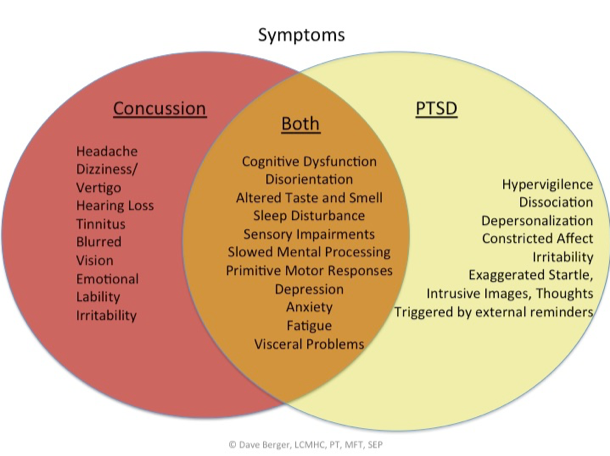 9
9
Another drug of interest is D-cycloserine (Seromycin), which increases the activity of a brain substance called N-methyl-D-aspartate, needed to pay off fear. During the study, which was attended by 28 people suffering from a fear of heights, scientists found that patients who received "push" therapy before a session D-cycloserine, showed lower levels of fear during the session compared to those who did not receive the drug. nine0184 10 Currently scientists study the effectiveness of the combined use of D-cycloserine and therapy for the treatment of post-traumatic stress.
Propranolol (Inderal), a beta-blocker drug, also under study whether it can be used to reduce post-traumatic stress and break the chain of scary memories. First experiments gave consoling results: it was possible to successfully weaken and, it seems, prevent PTSD in a small number of victims of traumatic events. nine0184 11
For example, in one preliminary study, scientists created a website self-help, based on the use of a psychotherapeutic method implementation in a stressful situation. First, patients with PTSD meet in person with doctor. After this meeting, participants can go to the site to find more information about PTSD and how to deal with the problem; their doctors may also visit the site to give advice or briefing. In general, scientists believe that therapy in this form - promising treatment for a large number of people suffering from PTSD. nine0184 12
First, patients with PTSD meet in person with doctor. After this meeting, participants can go to the site to find more information about PTSD and how to deal with the problem; their doctors may also visit the site to give advice or briefing. In general, scientists believe that therapy in this form - promising treatment for a large number of people suffering from PTSD. nine0184 12
Scientists are also working to improve methods for testing early treatment and monitoring of survivors of massive trauma, on developing ways to teach them self-assessment skills and introspection and referral mechanism to psychiatrists (if necessary).
Prospects for PTSD research
In the last decade, rapid progress in the study of mental and biological PTSD has led scientists to conclude that there is a need to focus on prevention, as the most realistic and important goal. nine0003
For example, in order to find ways to prevent PTSD, with funding NIMH conducts research to develop new and orphan drugs, aimed at combating the underlying causes of the disease.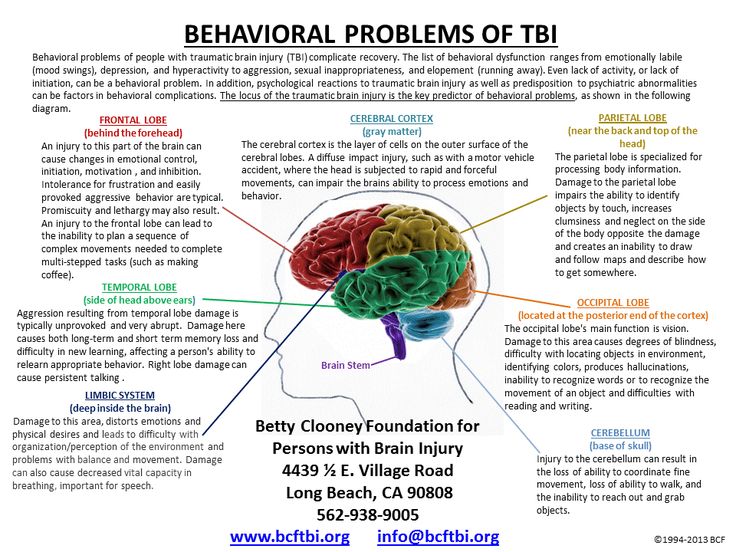 During another research scientists are looking for ways to enhance behavioral, personality and social protective factors and minimizing risk factors for prevent the development of PTSD after trauma. Another study is studying the question of what factors influence the difference in response to one or another method of treatment, which will help in the development of more individual, effective and productive methods of treatment. nine0003
During another research scientists are looking for ways to enhance behavioral, personality and social protective factors and minimizing risk factors for prevent the development of PTSD after trauma. Another study is studying the question of what factors influence the difference in response to one or another method of treatment, which will help in the development of more individual, effective and productive methods of treatment. nine0003
Where can I find more information?
MedlinePlus - resource from the American National Library of Medicine (U.S. National Library of Medicine and the National Institutes of Health) - offers the latest information on many health issues. Information about You can find PTSD at: www.nlm.nih.gov/medlineplus/posttraumaticstressdisorder.html.
National Institute of Mental Health
Office of Science Policy, Planning, and Communications
[National Institute of Mental Health
Science Policy Division research, planning and communications]
6001 Executive Boulevard
Room 8184, MSC 9663
Bethesda, MD 20892-9663
Phone: 301-443-4513; Fax: 301-443-4279
fax answering system Free answering machine: 1-866-615-NIMH (6464)
Text phone: 1-866-415-8051 toll-free
Email: nimhinfo@nih. gov
gov
National Center for Post-traumatic Stress Disorder
[National PTSD Center]
VA Medical Center (116D)
215 North Main Street
White River Junction, VT 05009
802-296-6300
www.ncptsd.va.gov
NOTES
- Shumyatsky GP, Malleret G, Shin RM, et al. Stathmin, a Gene Enriched in the Amygdala, Controls Both Learned and Innate Fear. cell. Nov 18 2005;123(4):697-709.
- Shumyatsky GP, Tsvetkov E, Malleret G, et al. Identification of a signal network in lateral nucleus of amygdala important for inhibiting memory specifically related to learned fear. cell. Dec 13 2002;111(6):905-918.
- Hariri AR, Mattay VS, Tessitore A, et al. Serotonin transporter genetic variation and the response of the human amygdala.Science. Jul 192002;297(5580):400-403.
- Milad MR, Quirk GJ. Neurons in medial prefrontal cortex signal memory for fear extinction.
 Nature. Nov 7 2002;420(6911):70-74.
Nature. Nov 7 2002;420(6911):70-74. - 5 Amat J, Baratta MV, Paul E, Bland ST, Watkins LR, Maier SF. Medial prefrontal cortex determines how stressor controllability affects behavior and dorsal raphe nucleus. Nat Neurosci. Mar 2005;8(3):365-371.
- Milad MR, Quinn BT, Pitman RK, Orr SP, Fischl B, Rauch SL. Thickness of ventromedial prefrontal cortex in humans is correlated with extinction memory. Proc Natl Acad Sci USA. Jul 26 2005;102(30):10706-10711. nine0024
- Gurvits TV, Gilbertson MW, Lasko NB, et al. Neurological soft signs in chronic posttraumatic stress disorder.Arch Gen Psychiatry. Feb 2000;57(2):181-186.
- Brewin CR. Risk factor effect sizes in PTSD: what this means for intervention. J Trauma Dissociation. 2005;6(2):123-130.
- Taylor FB, Lowe K, Thompson C, et al. Daytime Prazosin Reduces Psychological Distress toTrauma Specific Cues in Civilian Trauma Posttraumatic stress disorder.
 Biol Psychiatry. Feb 3 2006.
Biol Psychiatry. Feb 3 2006. - Ressler KJ, Rothbaum BO, Tannenbaum L, et al. Cognitive enhancers as adjuncts to psychotherapy: use of D-cycloserine in phobic individuals to facilitate extinction of fear. Arch Gen Psychiatry. Nov 2004;61(11):1136-1144.
- Pitman RK, Sanders KM, Zusman RM, et al. Pilot study of secondary prevention of posttraumatic stress disorder with propranolol.Biol Psychiatry. Jan 15 2002;51(2):189-192.
- Litz BTWL, Wang J, Bryant R, Engel CC.A therapist-assisted Internet self-help program for traumatic stress. Prof Psychol Res Pr. December 2004;35(6):628-634. nine0024
New York State Department of Mental Health expresses thanks to the National Institute of Mental Health for the information, used in this booklet.
Published by the State Department of Mental Health New York, June 2008.
New York State
Andrew M. Cuomo Governor
Mental Health
Head of Department Michael F.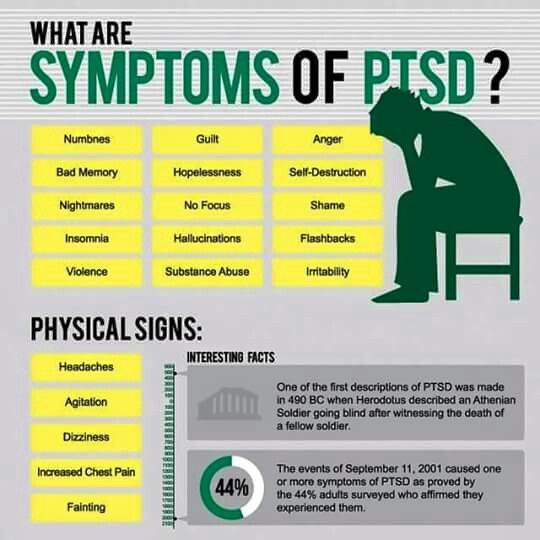 Hogan, PhD
Hogan, PhD
For more information about this edition contact:
New York State Office of Mental Health
Community Outreach and Public Education Office
[New York State Department of Mental Health
Public Relations and Community Education Department]
44 Holland Avenue
Albany, NY 12229
866-270-9857 (toll free)
www.omh.ny.gov
For questions and complaints about mental health services Health in New York contact:
New York State Office of Mental Health
Customer Relations
[New York State Department of Mental Health
Customer Service ]
44 Holland Avenue
Albany, NY 12229
800-597-8481 (toll-free)
For information about mental health services in your neighborhood, contact
nearest New York State Department of Mental Health (NYSOMH) regional office:
Western New York Field Office
[Western New York Regional Office]
737 Delaware Avenue, Suite 200
Buffalo, NY 14209
(716) 885-4219
Central New York Field Office
[Central New York Regional Office]
545 Cedar Street, 2nd Floor
Syracuse, NY 13210-2319
(315) 426-3930
Hudson River Field Office
[Hudson River Regional Office]
4 Jefferson Plaza, 3rd Floor
Poughkeepsie, NY 12601
(845) 454-8229
Long Island Field Office
[Long Island Regional Office]
998 Crooked Hill Road, Building #45-3
West Brentwood, NY 11717-1087
(631) 761-2508
New York City Field Office
[NYC Regional Office]
330 Fifth Avenue, 9th Floor
New York, NY 10001-3101
(212) 330-1671
what is it, why switch and how to apply for
What is an electronic PTS
EPTS is an electronic vehicle passport.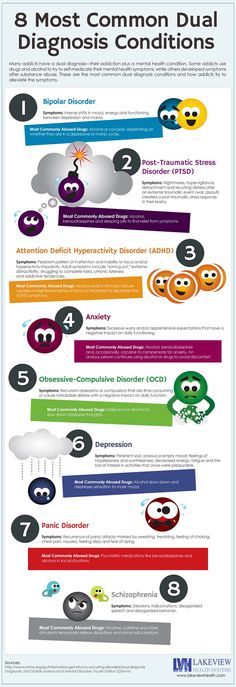 It contains more information than the paper counterpart, and the data is presented in a more convenient form. nine0003
It contains more information than the paper counterpart, and the data is presented in a more convenient form. nine0003
The final transition to EPTS in Russia should be completed by November 2019, so from December the document will be issued exclusively in electronic form. At the moment, however, electronic PTS for car owners are already available for owners of Haval cars.
EPTS looks like a record of all reliable information about the car in a single system. If earlier the buyer received a paper passport in his hands, now the passport number will fit into the registration certificate. At the same time, the owner can at any time check the status of the passport by this unique number in the electronic passport system. nine0003
Why you need EPTS
An electronic passport is an analogue of a paper one. It contains all the information about the car, including the history of its life: from the moment of production and import into the territory of the Customs Union to disposal or export from the vehicle.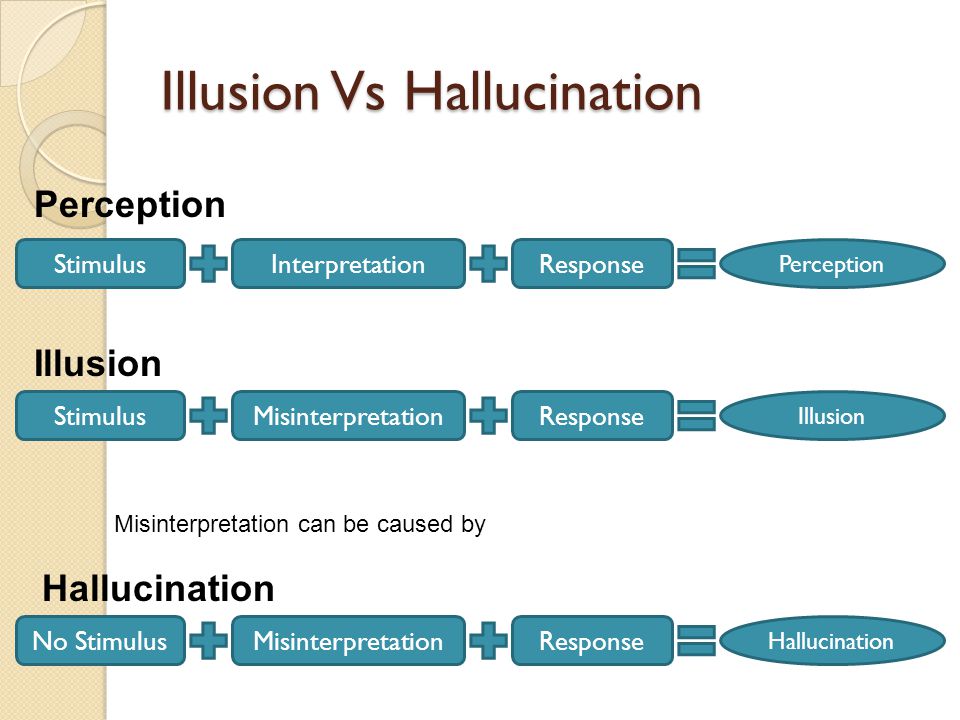 All maintenance, design modifications, new owners, legal restrictions and accidents are reflected in one document. This is its obvious advantage over the paper version. Also:
All maintenance, design modifications, new owners, legal restrictions and accidents are reflected in one document. This is its obvious advantage over the paper version. Also:
- New passport cannot be lost. All information about the car is stored in a single register - AS SEP. nine0024
- It does not need to be replaced if the owner changes, as was the case with a paper passport. All owners fit into one document.
- At any time, you can request an extract from the AS SEP or find out the history of the car.
The main advantages of EPTS are transparency and completeness of information, ease of use.
How to issue an electronic PTS
When buying a new car at a Haval dealership, you do not need to issue an EPTS yourself: the car will already be equipped with it. nine0003
The situation is different for owners of already registered cars. To change an existing paper passport to a digital one, you need to contact authorized organizations, for example, a Russian technical inspection operator. There is no need to urgently replace paper PTS with electronic ones. Old passports are valid indefinitely in the Russian Federation. This is only a matter of convenience and reliability, which motorists decide for themselves.
There is no need to urgently replace paper PTS with electronic ones. Old passports are valid indefinitely in the Russian Federation. This is only a matter of convenience and reliability, which motorists decide for themselves.
What EPTS consists of
There are two blocks of information in the electronic PTS for a car:
- Basic information, which contains the type, number and status of the EPTS, distinguishing features of the car, general technical information and other characteristics. These 13 sections must be completed. If any information is missing, the passport will not be valid.
- Additional information. This includes information about the owner, information about repairs, insurance, accidents, theft or arrest.
EPTS statuses
To register a car with the traffic police, the EPTS must be valid. This means that all sections of the main part are completed and the disposal fee is paid. nine0003
Here are some other statuses that an electronic PTS can have:
- incomplete: basic data is provided, but the disposal fee has not been paid;
- active;
- canceled: assigned when the type of vehicle changes;
- canceled occurs when important vehicle parameters are incorrectly specified;
- scrapped: the status changes automatically after the car is scrapped.
- Main page
- OWNERS
- Service
-
Electronic PTS
Vladimir, st. Traktornaya, 33
+7 (4922) 779-747
Book a test drive
Book a service
Call me
* Price for the HAVAL JOLION model in the Comfort configuration with a 1.5T, 2WD engine manufactured in 2022. The offer is limited, is not an offer and is valid from 09/19/2022.
* Price for the updated HAVAL F7 model in the Comfort configuration with a 1.5T, 2WD engine manufactured in 2022. The offer is limited, is not an offer and is valid from 10/01/2022. nine0483 * Price for the updated HAVAL F7x in the Comfort package with a 1.5T engine, 2WD in 2022. The offer is limited, is not an offer and is valid from 10/01/2022.
* Price for HAVAL DARGO in Comfort package with 2.0T 2WD petrol engine. The offer is limited, is not an offer and is valid from 10/01/2022.
* Price for the GWM Wingle 7 model in the Comfort package with a 2.0T 150 diesel engine, 4WD. The offer is limited, is not an offer and is valid from 19.09.2022.
* Price for GWM POER model in Comfort package with diesel engine 2.0T 150, 4WD. The offer is limited, is not an offer and is valid from 10/01/2022.
* The price for the HAVAL H9 model in the Elite configuration (Elite) with a 2.0 petrol engine, 4WD, manufactured in 2022 is valid from 09/19/2022. The offer is limited, is not an offer and is valid from 09/19/2022.
**** Some HAVAL vehicles may not have an in-vehicle emergency call system / device (ERA-GLONASS unit). nine0003
1 Havale Dargo
2 Havale Jolyon
All information presented on the site regarding cars and service is for informational purposes and is not a public offer. All prices indicated on this site are for informational purposes and are the maximum recommended retail prices according to the distributor's calculations (LLC "Haveil Motor Rus").