Bupropion interactions with supplements
Bupropion (Wellbutrin, Zyban) Interactions: What You Need to Know
Bupropion is a prescription-only medication. Under the brand names Wellbutrin® and Wellbutrin XL®, it’s used to treat major depressive disorder. Wellbutrin XL is also used to help treat seasonal affective disorder (SAD). And sold under the brand name Zyban®, it’s used as a smoking cessation aid.
Overall, bupropion is a safe and effective medication when it’s used as directed. However, like many other medications, it can interact with other drugs. Some of these interactions can result in side effects, and some can even be dangerous.
Below, we’ve explained the basics of how bupropion works as a medication. We’ve also listed the interactions that can occur when bupropion is used with other medications, supplements and certain herbal products.
How Does Bupropion Work?
Bupropion is an antidepressant. It works by changing the levels of certain neurotransmitters in your brain. More specifically, bupropion increases the amount of dopamine and norepinephrine that are active in your body at any time.
Dopamine is an important neurotransmitter. It’s responsible for a range of functions within your body, including helping you feel motivated, boosting your mood and regulating your ability to learn, move and display emotional responses.
Norepinephrine, on the other hand, is responsible for regulating your sleep-wake cycle, keeping you alert, allowing you to focus and helping you store new memories.
Although there’s debate about the precise cause of depression, research indicates that it might be linked to disturbances in serotonin, dopamine and norepinephrine levels.
As an antidepressant, bupropion works by inhibiting reuptake of the neurotransmitters dopamine and norepinephrine. This can help to improve your mood and treat the symptoms of depression and conditions such as seasonal affective disorder.
Interestingly, dopamine levels are affected by nicotine, with your body’s production of dopamine rising sharply after you smoke a cigarette. Due to bupropion’s effects on dopamine, it can make the cravings associated with quitting less intense — a topic we’ve covered in more detail here.
Learn how to tell if Wellbutrin is working for you in our blog: 6 Signs Wellbutrin® is Working
online mental health assessment
your mental health journey starts here
Bupropion (Wellbutrin, Zyban) Drug Interactions
Overall, bupropion is a safe, effective medication when it’s used as prescribed. However, like other antidepressants, bupropion can interact with other medications.
Some drug interactions may increase or decrease the effects of bupropion in the body. Others may have dangerous side effects, including potentially serious, life-threatening reactions that can occur when bupropion is used with other medications.
For any medication, including bupropion, the easiest way to avoid interactions is to inform your healthcare provider about all medications you currently use and have recently used. They will be able to review the safety of using bupropion and recommend the safest course of action for you.
We’ve listed these interactions below, along with more information on the risks associated with each drug combination.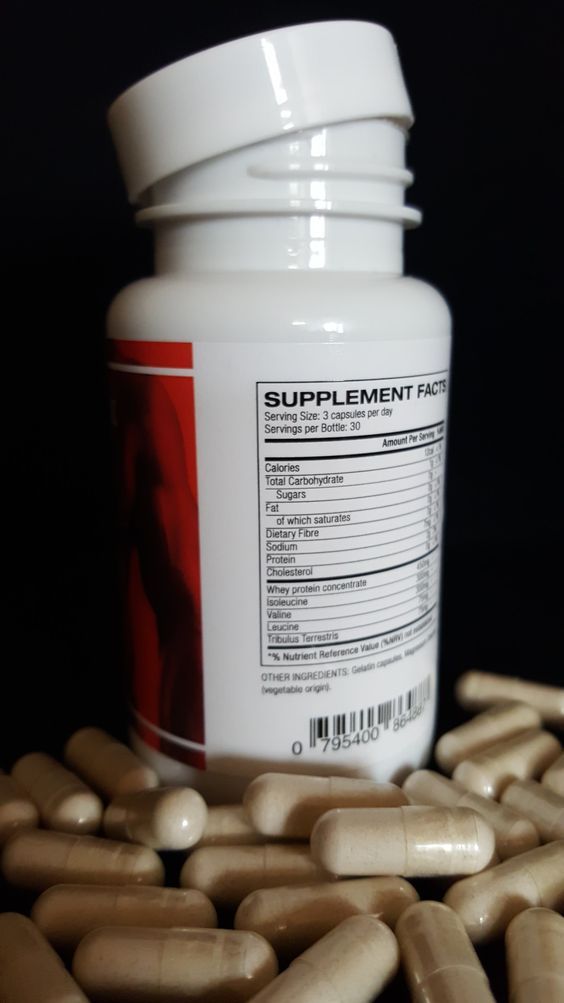
Bupropion (Wellbutrin, Zyban)
Bupropion is sold under several brand names as both a depression treatment (Wellbutrin) and as a medication for smokers interested in quitting (Zyban).
Although it’s technically not an interaction, the FDA warns patients not to accidentally use more than one medication containing bupropion at the same time, as doing so may increase your risk of experiencing side effects such as seizures.
If you’re prescribed Wellbutrin, Zyban or a generic form of bupropion, make sure to check your other medications (particularly antidepressants or smoking aids) to ensure you aren’t using the same drug under a different brand name.
Other brand names used for bupropion include Aplenzin®, Forfivo XL® and several others. Bupropion is also an ingredient in the weight loss medication Contrave®.
Monoamine Oxidase Inhibitors (MAOIs)
Monoamine oxidase inhibitors (MAOIs) are a class of older antidepressants, many of which are still used to treat depression and several other conditions. Some commonly prescribed MAOIs include the following medications:
Some commonly prescribed MAOIs include the following medications:
Phenelzine (Nardil®)
Isocarboxazid (Marplan®)
Tranylcypromine (Parnate®)
Selegiline (Emsam®)
Bupropion can interact with MAOIs, leading to an elevated risk of several side effects, including dangerously high blood pressure. As such, bupropion should not be used if you currently use a MAOI to treat depression or any other condition.
You should also avoid using bupropion if you’ve taken any MAOI medications within the past 14 days. Likewise, if you’re recently stopped using bupropion, avoid using any MAOIs until at least 14 days have passed since your most recent dose of bupropion.
CYP2B6 Inducers
Bupropion is metabolized by the enzyme CYP2B6. Medications that increase the activity of the CYP2B6 enzyme, called CYP2B6 inducers, may make bupropion less effective in the body and necessitate a higher dosage.
CYP2B6 inducers include the antiretroviral medications ritonavir, lopinavir and efavirenz, which are commonly used in combination with other medications to treat HIV/AIDS.
Other medications that can induce CYP2B6 and interact with bupropion include anticonvulsants such as carbamazepine (Tegretol®), phenytoin (Dilantin®) and phenobarbital.
If you’re prescribed any of these medications, it’s important to mention this to your healthcare provider before using bupropion.
CYP2B6 Inhibitors
Likewise, medications that reduce the activity of the CYP2B6 enzyme, called CYP2B6 inhibitors, may increase the concentration of bupropion and other medications metabolized by CYP2B6 in the body.
Medications metabolized by CYP2B6 include several other antidepressants, such as paroxetine (Paxil®), sertraline (Zoloft®), fluoxetine (Prozac®), venlafaxine (Effexor®), desipramine (Norpramin® or Pertofrane®), imipramine (Tofranil®), nortriptyline (Pamelor®) and others.
Talk to your healthcare provider before using bupropion if you’re prescribed any other antidepressants. They may adjust your dosage of bupropion or recommend using a different medication.
Other medications that can affect CYP2B6 levels and interact with bupropion include:
Antipsychotics, such as haloperidol (Haldol®), risperidone (Risperdal®) and thioridazine (Mellaril®).
Beta-blockers, including metoprolol (Lopressor®) and others.
Type 1C antiarrhythmics, such as propafenone (Rythmol®), flecainide and others.
If you’re prescribed any of the medications listed above, or other medications in any of the drug classes listed above, make sure that you inform your healthcare provider before using bupropion.
Dopaminergic Medications
Medications that affect dopamine, called dopaminergic medications, can interact with bupropion and cause central nervous system (CNS) toxicity. This could cause reactions such as dizziness, vertigo, agitation, tremor, restlessness, gait disturbance and loss of control over movement.
Common dopaminergic medications include levodopa, or l-DOPA, and amantadine (Gocovri®), a medication used to treat certain viruses. Inform your healthcare provider if you currently use or have recently used either of these medications before using bupropion.
Inform your healthcare provider if you currently use or have recently used either of these medications before using bupropion.
Alcohol
Although rare, there have been reports of people experiencing a reduced alcohol tolerance or neuropsychiatric events after drinking alcohol while taking bupropion.
If you’re prescribed bupropion, drinking alcohol may increase your risk of experiencing negative side effects from both alcohol and bupropion. As such, it’s best to limit your alcohol consumption or avoid alcohol entirely while you take bupropion.
We’ve covered this topic in more detail, as well as what you can do to protect yourself from side effects associated with drinking while using bupropion, in our guide to bupropion and alcohol.
Drug Tests
Bupropion may affect certain drug tests, causing false-positives. For example, some tests used to check for usage of amphetamines may show a false positive if you’re currently using or have recently used bupropion.
If you’re screened for illicit drugs as part of your employment, education or for any other reason, make sure to let the tester know that you’re prescribed bupropion.
Bupropion (Wellbutrin, Zyban) Disease Interactions
If you have a pre-existing health condition or disease, you may be more at risk of experiencing side effects from bupropion. We’ve listed these interactions below, along with more information on what you can do to minimize your risk of experiencing an adverse reaction from bupropion.
Liver and/or Kidney Problems
Bupropion is metabolized in the liver and kidneys. It may lead to temporarily elevated levels of aminotransferase, an enzyme found in the liver and kidneys that, in some cases, can indicate damage to the liver.
If you have liver and/or kidney problems, you may have a higher risk of experiencing negative side effects from bupropion. To avoid this, your healthcare provider may recommend taking bupropion at a reduced dosage, or for you to use a different medication.
Seizure Disorders and/or Epilepsy
If you have a seizure disorder or epilepsy, using bupropion for any condition may increase your risk of experiencing seizures. As such, you should not use bupropion. Make sure to inform your healthcare provider if you have any seizure-related condition and want to use antidepressants.
Anorexia and Bulimia Nervosa
If you currently have or previously had an eating disorder, such as anorexia or bulimia nervosa, you may have an elevated risk of seizures if you use bupropion.
As such, your healthcare provider may recommend an alternative medication to bupropion.
Alcohol and/or Sedative Withdrawal
If you regularly drink a lot of alcohol and suddenly stop drinking, you may have an elevated risk of experiencing seizures if you use bupropion. This increase risk may also be present if you use the following medications and abruptly stop before using bupropion:
Sedatives, including sleeping pills such as zolpidem (sold as Ambien®), eszopiclone and zopiclone.

Benzodiazepines, including alprazolam (sold as Xanax®), diazepam (Valium®), lorazepam (Ativan®), clonazepam (Klonopin®) and others.
Epilepsy and anti-seizure medications, such as carbamazepine (Tegretol) and other anticonvulsants.
As such, do not use bupropion if any of the above applies to you, and make sure you talk to your healthcare provider if they’re considering prescribing you bupropion.
High Blood Pressure (Hypertension)
Bupropion may cause increased blood pressure. If you have a history of high blood pressure, or currently use medication to lower your blood pressure, it’s important to talk to your healthcare provider about this before using bupropion.
Based on your overall health, your healthcare provider may recommend a different medication or ask you to occasionally monitor your blood pressure while using bupropion.
Other Interactions
Bupropion may potentially interact with other medications and/or health conditions in addition to those listed above. Make sure to inform your healthcare provider about any medications you use, any health conditions you have or any other relevant information before using bupropion.
Make sure to inform your healthcare provider about any medications you use, any health conditions you have or any other relevant information before using bupropion.
psych meds online
psychiatrist-backed care, all from your couch
Learn More About Bupropion
Used as prescribed, bupropion is a safe and effective treatment for depression that can assist in your recovery. It’s also a proven, effective smoking cessation aid that can make it easier to deal with nicotine cravings when you’re trying to quit.
Interested in learning more about bupropion online? Our guide to bupropion lists everything you need to know about this medication, from how it works in your body to dosages, side effects, common questions and much more.
This article is for informational purposes only and does not constitute medical advice. The information contained herein is not a substitute for and should never be relied upon for professional medical advice. Always talk to your doctor about the risks and benefits of any treatment. Learn more about our editorial standards here.
Learn more about our editorial standards here.
Can you take medicine and vitamins together? 6 vitamin interactions
Adding vitamins and supplements to your daily care regimen can help improve your general health and stave off ailments. But many don’t realize that vitamins and supplements can also affect prescription medications when mixed. According to a national Wakefield Research survey, nearly 40% of Americans who take prescription medications are unaware of vitamin interactions.
Can you take medicine and vitamins together?
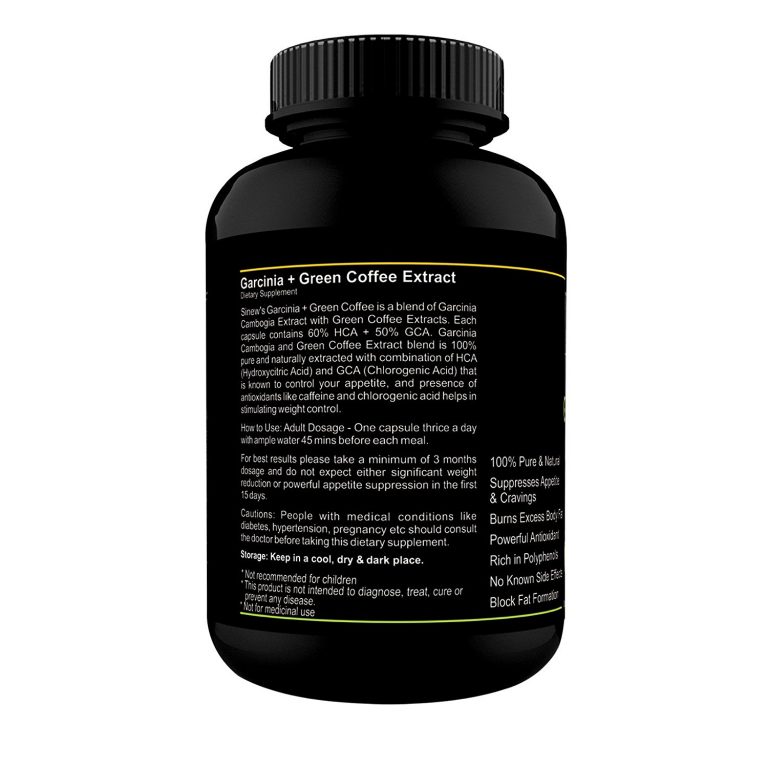
When it comes to supplements, you may think that because they’re natural, they’re safe but that’s not necessarily true. Companies that produce vitamin supplements are not required to get approval from the Food and Drug Administration before selling their products, so it can be hard to determine whether they are safe or effective—even if they contain the exact ingredients listed. And it can be risky to take certain supplements with prescription medications.
Although the FDA requires all supplements to be labeled correctly, not all companies follow these guidelines or report the amounts contained accurately. What’s more, the majority of these supplements lack scientific evidence to support their claims to foster good health. Before you start taking any vitamins or supplements, discuss their safety and possible drug interactions with your doctor or pharmacist. And remember, your best bet to get the required vitamins and minerals is by eating a well-rounded, healthy diet. These are a few examples of how supplements and medications can negatively impact one another.
Vitamin interactions with antidepressants
The combination of SSRI antidepressant medications with supplements can be especially dangerous. If you have an anxiety disorder or depression, your healthcare provider may prescribe a selective serotonin reuptake inhibitor (SSRI). Common SSRIs are Lexapro, Prozac, Paxil, and Zoloft. These are safe for most people, but when taken with supplements or vitamins, the results can be risky. Brandi Cole, Pharm.D., a medical advisory board member for Persona Nutrition, explains what supplements you can’t take with SSRIs, and why.
Brandi Cole, Pharm.D., a medical advisory board member for Persona Nutrition, explains what supplements you can’t take with SSRIs, and why.
- St. John’s wort may decrease a medication’s effectiveness: “Most SSRIs are extensively metabolized by liver enzymes, and supplements that affect these enzymes could potentially change the way your body eliminates SSRIs,” Cole says. “For example; St. John’s wort induces liver enzymes—meaning it makes the liver eliminate certain prescription drugs more quickly than normal.” Translation: St. John’s wort causes your system to clear SSRIs sooner than intended, and without the correct amount of medication in your system, your medication can’t work as well.
- 5HTP (5-hydroxytryptophan) can increase the risk of serotonin syndrome: Supplements that contain serotonin or alter serotonin metabolism—such as 5HTP (a serotonin precursor), SAMe, or St. John’s wort can cause (the potentially life-threatening) serotonin syndrome when taken with SSRIs.

You may be wondering if you can take multivitamins with antidepressants. While multivitamins may seem like a safe bet, it’s best to consult with your healthcare provider to find out before you start taking any vitamin, mineral or herbal supplements.
RELATED: Lexapro details | Prozac details | Paxil details | Zoloft details
Vitamin interactions with birth control
But it’s not just SSRIs. If you are a woman who uses oral contraceptives for birth control, beware of St. John’s wort. “St. John’s wort can render contraceptives useless if you’re taking it regularly,” Cole says. “In fact, taking St. John’s wort can decrease norethindrone and ethinyl estradiol levels by 13% to 15%, which can result in an unplanned pregnancy.”
Iron supplement interactions
Iron supplements can interact with a few different types of medications.
- Antibiotics and iron: Taking iron alongside certain antibiotics, such as ciprofloxacin, tetracycline, or minocycline, may decrease your body’s absorption of the antibiotic prescription.

- Thyroid hormone and iron: Additionally, those taking synthetic thyroid hormone replacement such as Synthroid (levothyroxine) should be sure to discuss with your healthcare provider all vitamin and mineral supplements that contain iron—also soy, and calcium, which, “if taken within four hours of taking a synthetic thyroid hormone, may reduce the absorption rate,” Dr. Cole says.
Vitamin E and blood thinners
Vitamin E thins the blood. If you’re taking aspirin or a prescription blood thinner (such as warfarin), your risk of internal bleeding is increased, which may even be life-threatening. The same is true of the supplement ginkgo biloba–it’s important not to combine these products.
Magnesium interactions
Magnesium supplements can disrupt the efficacy of several medications.
- Magnesium and antibiotics: The efficacy of quinolones such as ciprofloxacin and tetracycline antibiotics such as doxycycline can be decreased when combined with magnesium supplements.
 To avoid this interaction, take the antibiotic more than 2 hours before or 6 hours after you take magnesium (or a vitamin or supplement that contains magnesium).
To avoid this interaction, take the antibiotic more than 2 hours before or 6 hours after you take magnesium (or a vitamin or supplement that contains magnesium). - Magnesium and calcium channel blockers: Taking magnesium along with a calcium channel blocker like nifedipine, amlodipine, diltiazem, felodipine, or verapamil can increase your odds of dizziness and low blood pressure.
- Magnesium and diabetes medications: Taking antacids that contain magnesium hydroxide can increase the absorption of the diabetes medications glipizide or glyburide, which can cause low blood sugar. Consult with your provider before combining the two.
- Magnesium and digoxin: If you’ve been prescribed Lanoxin (digoxin), your provider will carefully monitor your digoxin levels. That’s because magnesium can decrease digoxin levels, making digoxin less effective.
- Magnesium and levothyroxine: Antacids or vitamins/supplements that contain magnesium may decrease the efficacy of the thyroid medication levothyroxine, so discuss the risks of this combination with your provider if you are taking this drug.
 In most cases, the interaction can be avoided by separating when you take each medicine for at least 4 hours.
In most cases, the interaction can be avoided by separating when you take each medicine for at least 4 hours. - Magnesium and osteoporosis drugs: If you’re taking alendronate for osteoporosis, magnesium may reduce its absorption. If you’re combining the two, take magnesium at least 30 minutes after you take alendronate.
Certain drugs can make supplements less effective too. For example, antibiotics such as gentamicin, the antifungal amphotericin B, corticosteroids including prednisone, antacids, and insulin may reduce magnesium levels in the body when combined. Both loop diuretics such as furosemide and thiazide diuretics like hydrochlorothiazide can also decrease your magnesium levels, so your doctor may advise you to supplement with magnesium while taking these drugs.
Vitamin C interactions
Vitamin C can interact with several different types of prescription and over-the-counter medications.
- Vitamin C and OTC pain relievers: Aspirin or other NSAIDs like ibuprofen or naproxen can cause your levels of vitamin C to be depleted.
 What’s more, taking high doses of vitamin C can increase the levels of NSAIDs as well as the over-the-counter pain medication acetaminophen in the body, so it’s best to consult with your doctor before combining vitamin C with these medications.
What’s more, taking high doses of vitamin C can increase the levels of NSAIDs as well as the over-the-counter pain medication acetaminophen in the body, so it’s best to consult with your doctor before combining vitamin C with these medications. - Vitamin C and barbiturates: Anti-seizure medications such as phenobarbital can decrease the effectiveness of vitamin C.
- Vitamin C and chemotherapy: If you’re receiving chemotherapy, check with your doctor before taking vitamin C supplements as it may impact the effectiveness of your treatment.
- Vitamin C and nitrate medications: Taking nitrate medications can cause tolerance over time, meaning that your body gets used to the drug and it has less of an effect. When combined with the heart medications nitroglycerin, isosorbide dinitrate, or isosorbide mononitrate, vitamin C may impact your body’s tolerance to the drugs, where you possibly do not build up a tolerance.

- Vitamin C and oral contraceptives: If you’re taking estrogen-containing birth control pills or hormone replacement therapy (HRT), supplementing with vitamin C may raise your estrogen levels.
- Vitamin C and antibiotics: Taking vitamin C in conjunction with antibiotics including tetracycline, minocycline, or doxycycline can increase blood levels of the medication and decrease the effectiveness of vitamin C.
RELATED: Tetracycline details | Minocycline details
Vitamin interactions chart
6 safety tips for taking supplements and medication
“Prescription medications can deplete nutrients from the body or provide additional nutrients based on the makeup of the medications you’re taking—and that can be helpful or hurtful,” Dr. Cole says. “That’s why it’s important to have an understanding of drug-nutrient interactions if you’re taking both supplements and prescription medications. ”
”
1. Talk to your provider
How certain vitamin interactions occur is largely on a case-by-case basis. Before starting any new vitamins or supplements, be sure to discuss them with your doctor. If you’re already taking supplements, it’s important to let your provider know so that they can advise you of any potential interactions and safety concerns. Make a list of all of the supplements you are taking, including the dose and the frequency.
2. Avoid unsafe supplements
To be sure you’re not taking any supplements or herbal remedies that may be dangerous, it’s best to avoid those that claim to treat medical conditions in the same way prescription medicines would. A good rule of thumb is to avoid anything that’s marketed to treat, prevent, or cure diseases.
3. Take as directed
Be sure not to take more of a dietary supplement than recommended. Doing so can increase the risk of serious side effects–for example, fat-soluble vitamins (such as vitamin A, vitamin D, vitamin E, and vitamin K) can accumulate in the body over time, reaching toxic levels. It’s also important to take the supplement as directed; for example, with or without food. Consult with your doctor for information about potential medication interactions– you may need to adjust your medication’s timing so that absorption issues do not occur.
It’s also important to take the supplement as directed; for example, with or without food. Consult with your doctor for information about potential medication interactions– you may need to adjust your medication’s timing so that absorption issues do not occur.
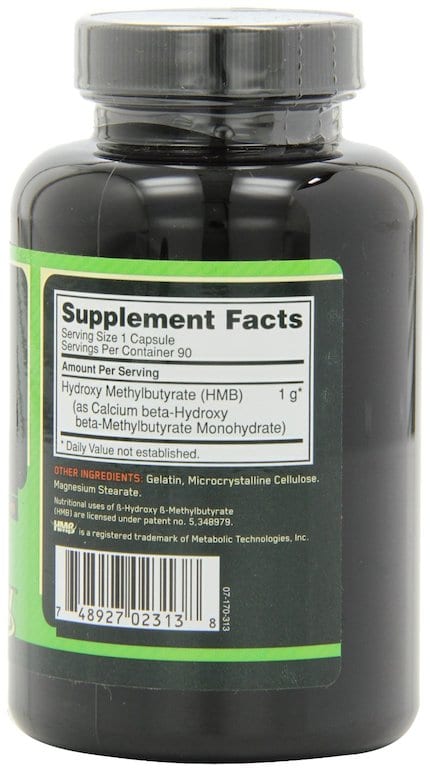
4. Read labels carefully
Because supplements are held to different standards than prescription medications–they are not regulated by the FDA–it’s important for consumers to read product labels carefully. A supplement’s label is required to list its active and inactive ingredients as well as the dosage. Before starting the supplement, have a conversation with your healthcare provider. It may also be helpful to research product reviews.
5. Review supplements before and after surgery
If you are having a surgical procedure, be sure to discuss any vitamins and herbal supplements that you are taking with your doctor beforehand, even common supplements that you may think are harmless. Some supplements may increase the risk of bleeding in patients, and you may be advised to stop them for a period of time before and after surgery.
6. Use extra caution if you’re pregnant or nursing
Pregnant or nursing women should take a prenatal vitamin that contains folic acid. Consult your healthcare provider for guidance on a prenatal vitamin that is right for you. Besides that, take extra precautions when taking any kind of dietary supplement, including herbal products, if you are pregnant or breastfeeding. Always check with your healthcare provider before starting any new vitamins or supplements.
It’s also important to consult the pediatrician before giving any supplements to a child, because dietary supplements are often not sufficiently tested among these populations.
Do antidepressants help smokers trying to quit
This translation is out of date. Please click here for the latest English version of this review.
Relevance and issues addressed in the review
Some medications used to treat depression (antidepressants) have been investigated to see if they can help people trying to quit smoking. Two antidepressants, bupropion (Zyban) and nortriptyline, are sometimes prescribed to help people quit smoking. In this review, we set out to investigate whether the use of antidepressants increases the likelihood of successful smoking cessation for six months or more, and to determine the safety of using these drugs to assist in smoking cessation.
Two antidepressants, bupropion (Zyban) and nortriptyline, are sometimes prescribed to help people quit smoking. In this review, we set out to investigate whether the use of antidepressants increases the likelihood of successful smoking cessation for six months or more, and to determine the safety of using these drugs to assist in smoking cessation.
Study profile
Evidence current to July 2013. This update includes 24 new studies, for a total review of 90 studies. Both smokers and people who recently quit smoking took part in the studies. 65 studies have been conducted with bupropion, which is approved for use as a smoking cessation drug under the trade name Zyban. Ten studies have been done with nortriptyline, a tricyclic antidepressant drug that is not approved for use in smoking cessation aids. We included only those studies that reported a long-term outcome (regardless of whether study participants stopped smoking within six months of study entry or not).
Main findings and quality of evidence
Trials using bupropion (Zyban) for smoking cessation showed high-quality evidence that this drug increases the likelihood of a successful quit attempt for at least six months (44 trials, over 13,000 participants). Side effects of bupropion include insomnia, dry mouth, nausea, and rarely (1:1000) seizures and possibly various psychiatric problems, but the latter is not clear. Moderate-quality evidence, limited by the relatively small number of included studies and participants, indicates that use of the antidepressant nortriptyline also increases smoking cessation rates (six trials, 975 participants). Side effects of using this medicine include: dry mouth, constipation, nausea and sedation, and this drug can be dangerous in overdose. Serotonin reuptake inhibitor antidepressants (eg, fluoxetine), MAOIs (eg, selegiline), and the antidepressant venlafaxine have not been shown to help quit smoking, nor has herbal medicine with St. John's wort or S-adenosyl-L-methionine, a dietary supplement which is believed to have antidepressant properties.
John's wort or S-adenosyl-L-methionine, a dietary supplement which is believed to have antidepressant properties.
Talk
The mechanism of action of bupropion and nortriptyline is not well understood. Both drugs help to quit smoking, regardless of whether patients had previous depression or depressive symptoms at the time of quitting. The likelihood of successful smoking cessation with bupropion or nortriptyline was similar to that of nicotine replacement therapy, but lower than with varenicline.
Translation notes:
Translation: Yakov Petrovich Nizhnik. Editing: Ziganshina Lilia Evgenievna. Project coordination for translation into Russian: Cochrane Russia - Cochrane Russia (branch of the Northern Cochrane Center on the basis of Kazan Federal University). For questions related to this transfer, please contact us at: [email protected]
Bupropion (wellbutrin) interactions: what you need to know
Disclaimer
If you have any medical questions or concerns, contact your doctor. Articles in the Health Guide are based on peer-reviewed research and information from medical societies and government agencies. However, they are not a substitute for professional medical advice, diagnosis or treatment.
Articles in the Health Guide are based on peer-reviewed research and information from medical societies and government agencies. However, they are not a substitute for professional medical advice, diagnosis or treatment.
Bupropion is an FDA-approved prescription drug for the treatment of depression, seasonal affective disorder, and smoking cessation. It belongs to a class of antidepressants known as norepinephrine dopamine reuptake inhibitors (NDRIs) and works by increasing the chemical activity. in the brain (NIH, no data).
Before taking bupropion, it is important to know which medicines may interact with it. Drug interactions happen when you take something along with a drug—such as another drug, food, drink, or supplement—and it changes the potency or effectiveness of that drug. Some medicines may increase the risk of side effects, while others may make bupropion less effective. Here's what you need to know.
Vitals
- Bupropion is an FDA-approved prescription drug for the treatment of depression, seasonal affective disorder, and smoking cessation.
- Some drugs can cause side effects when taken with bupropion.
- Side effects of bupropion include restlessness, dizziness and loss of appetite.
- The FDA has issued a black box warning for bupropion and other antidepressants because they increase the risk of suicidal thoughts and behavior in children, adolescents and young adults. Patients of any age taking antidepressants should tell their healthcare provider if their symptoms worsen or they experience suicidal thoughts or behavior.
What drugs interact with bupropion?
Before you start taking bupropion, be sure to check with your doctor about any other medicines or supplements you are taking to avoid possible drug interactions.
The following drugs may interact with bupropion (DailyMed, 2019):
- CYP2B6 inducers : You may need a higher dose of bupropion if you are taking CYP2B6 inducers, drugs that stimulate liver enzymes that help the body break down certain drugs ( e.
 g. ritonavir, lopinavir, efavirenz, carbamazepine, phenobarbital and phenytoin). These drugs speed up the breakdown of bupropion, which lowers the effective concentration in the body.
g. ritonavir, lopinavir, efavirenz, carbamazepine, phenobarbital and phenytoin). These drugs speed up the breakdown of bupropion, which lowers the effective concentration in the body. - Drugs metabolized by CYP2D6 : Bupropion inhibits CYP2D6, an enzyme that helps the liver metabolize certain drugs. It can increase the concentration of some drugs that are broken down by the CYP2D6 enzyme. Examples include antidepressants (including venlafaxine, nortriptyline, imipramine, desipramine, paroxetine, fluoxetine, sertraline), antipsychotics (eg, haloperidol, risperidone, thioridazine), beta-blockers (eg, metoprolol), for example, and type 1C antiarrhythmics (antiarrhythmic drugs). type 1C) flecainide). Your doctor may need to adjust the dose of your medicine.
- Digoxin : Bupropion may lower blood levels of digoxin, a medicine used to treat heart failure and arrhythmias. If you are taking digoxin, your digoxin level should be monitored by your doctor.

- Drugs that lower seizure threshold : Bupropion increases the likelihood of a seizure. It should be used with caution if you are taking other drugs that also lower the seizure threshold (eg, other bupropion drugs, neuroleptics, antidepressants, theophylline, or systemic corticosteroids).
- Dopaminergic drugs (levodopa and amantadine) : When used with bupropion, toxic effects on the central nervous system may occur. Adverse reactions may include restlessness, agitation, tremor, ataxia (impaired coordination), gait disturbance, dizziness, and vertigo.
- MAOIs (monoamine oxidase inhibitors) : Taking bupropion with MAOIs may increase the risk of hypertensive reactions (high blood pressure). You must wait at least 14 days after stopping an MAOI inhibitor before taking bupropion and 14 days after stopping bupropion and starting treatment with an MAOI inhibitor. Examples of MAOIs include phenelzine (trade name Nardil), tranylcypromine (trade name Parnate), isocarboxazid (trade name Marplan) and selegiline (trade name Emsam).

- Interactions with drugs and laboratory tests : Bupropion may cause false positive urine test results for amphetamines.
Advertisement
Over 500 Generics at $5/month
Go to Ro Pharmacy for prescriptions for only $5/month each (no insurance).
Learn more
How does bupropion work?
As we have noted, bupropion (brand name Wellbutrin) affects certain chemicals. in the brain (NIH, no data). As the name suggests, it slows the brain's uptake of two chemicals (neurotransmitters), norepinephrine and dopamine. Bupropion increases the levels of these neurotransmitters, improving mental health and mood. Norepinephrine helps the body respond to stress, and dopamine is released when the brain expects a reward.
what are the benefits of vitamin K
Bupropion is not an SSRI (selective serotonin reuptake inhibitor). Unlike this class of antidepressants, which include sertraline (brand name Zoloft), fluoxetine (brand name Prozac), and paroxetine (brand name Paxil), bupropion does not act on serotonin (also known as the feel-good hormone) receptors in the brain (Patel , 2016).
Bupropion use
Bupropion FDA approved for major depressive disorder (MDD), seasonal affective disorder (SAD) and smoking cessation (Huecker, 2020). It is also sometimes used to treat bipolar disorder, but this is an off-label use - meaning that the FDA has not approved bupropion for that specific purpose (Li, 2016).
As an antidepressant, its brand names include Aplenzin, Wellbutrin, Wellbutrin SR and Wellbutrin XL. Zyban is a brand name for smoking cessation.
Off-label uses of bupropion without FDA approval include:
- Sexual dysfunction caused by certain antidepressants
- Attention deficit/hyperactivity disorder (ADHD)
- Depression associated with bipolar disorder
- Obesity0002 In children, it is used off-label for ADHD (Hücker, 2020).
Dosages of bupropion
Bupropion is available as a regular table, sustained release (SR) and extended release (ER) tablets for oral administration. Depending on the dosage prescribed, you can take bupropion one to four times a day.
The regular tablet is usually taken three or four times a day at regular intervals. The sustained release tablet is usually taken twice a day at least eight hours apart. Extended release tablets (Aplenzin, Wellbutrin XL) are usually taken once daily in the morning. For the treatment of seasonal affective disorder, it is usually taken once a day in the morning from early autumn to early spring.
The maximum daily dose of bupropion is 450 mg (NIH, 2018).
Bupropion side effects
Bupropion can cause mild to severe side effects.
The FDA has issued a black box warning for bupropion (DailyMed, 2019) and other antidepressants, reporting that they increase the risk of suicidal thoughts and behavior in children, adolescents, and young adults in short-term trials. Patients of any age taking antidepressants should tell their healthcare provider if their symptoms worsen or they experience suicidal thoughts or behavior.
This is some of the side effects of people who take Bupropion (NIH, 2018):
- Driving
- Anxiety
- Problems of falling asleep or sleep
- Dry Dry
- 9004 Vomiting
- Abdominal pain
- Shaking
- Loss of appetite
- Weight loss
- Constipation
- Excessive sweating
- Tinnitus (ringing in the ears)
- Changes in taste sensation
- Frequent urination
- Sore throat
This list does not include all possible side effects.
 Talk to your pharmacist or doctor for more information about medicines.
Talk to your pharmacist or doctor for more information about medicines. Who should not use bupropion
People with certain medical conditions should avoid using bupropion (DailyMed, 2019): head, stroke, infection, etc.).
- People with a current or previous diagnosis of an eating disorder such as bulimia or anorexia nervosa should not take bupropion as they are at increased risk of seizures.
- Bupropion should not be taken if you are abruptly stopping alcohol, benzodiazepines, barbiturates, or antiepileptic drugs.
- Do not take an MAOI at the same time as bupropion or within 14 days of stopping bupropion due to the risk of hypertension (high blood pressure) reactions. Wait 14 days after stopping an MAOI before taking bupropion. People taking reversible MAOIs (such as linezolid or intravenous methylene blue) should not take bupropion.
- Do not take bupropion if you have an allergic reaction to the medicine.
Bupropion is category C in pregnancy; this means there is not enough data to say if bupropion is safe during pregnancy. It has been found in breast milk so be careful if breastfeeding. Talk to your doctor to see if you should avoid using this medication.
It has been found in breast milk so be careful if breastfeeding. Talk to your doctor to see if you should avoid using this medication.
Recommendations
- DailyMed - BUPROPION HYDROCHLORIDE tablet. (2019). Retrieved August 19, 2020, from https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=e4100232-a25d-4468-9057-af7e66205154
- Hücker M. R., Smiley A. and Saadabadi A. (2020). Bupropion. At Stat Pearls. Stat Pearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK470212/
- Li, D.J., Tseng, P.T., Chen, Y.W., Wu, K.K., and Lin , P. Yu. (2016). Significant treatment effect of bupropion in patients with bipolar disorder, but similar rate of phase shift as other antidepressants: a meta-analysis following the PRISMA guidelines. Medicine, 95(13), e3165. https://doi.org/10.1097/MD.0000000000003165
- National Institutes of Health. Bupropion: MedlinePlus Medication Information (2018). Retrieved August 19, 2020, from https://medlineplus.gov/druginfo/meds/a695033.

Learn more