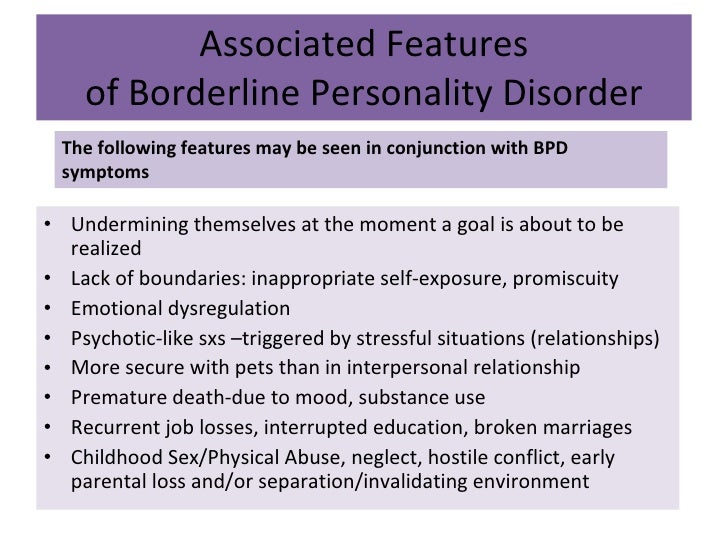
Borderline personality disorder psychotic
Hallucinations and Other Psychotic Symptoms in Patients with Borderline Personality Disorder
1. Black DW, Blum N, Pfohl B, Hale N. Suicidal behavior in borderline personality disorder: prevalence risk factors, prediction and prevention. J Personality Disord. 2004;18:226–239. [PubMed] [Google Scholar]
2. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Washington, DC: American Psychiatric Association; 2013. [Google Scholar]
3. Knight RP. Borderline states. Bull Menninger Clin. 1953;17:1–12. [PubMed] [Google Scholar]
4. Kernberg O. Borderline personality organization. J Am Psychoanal Assoc. 1967;15(3):641–685. [PubMed] [Google Scholar]
5. Zandersen M, Henriksen MG, Parnas J. A recurrent question: what is borderline? J Personal Disord. 2019;33:341–369. [PubMed] [Google Scholar]
6. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 3 ed. Washington, DC: American Psychiatric Association; 1980. [Google Scholar]
7. Decker HS. The Making of DSM-IIIJ: A Diagnostic Manual’s Conquest of American Psychiatry. New York, NY: Oxford University Press; 2013. [Google Scholar]
8. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4 ed. Arlington, VA: American Psychiatric Publishing; 1994. [Google Scholar]
9. World Health Organization. The ICD-10 Classification of Mental and Behavioural Disorders: Clinical Descriptions and Diagnostic Guidelines. Geneva: World Health Organization; 1992. [Google Scholar]
10. World Health Organization. International Statistical Classification of Diseases and Related Health Problems. 11. World Health Organization; 2019. [Google Scholar]
11. Zanarini MC, Gunderson JG, Frankenburg FR. Cognitive features of borderline personality disorder. Am J Psychiatry. 1990;147:57–63. [PubMed] [Google Scholar]
12. Pope HG. The validity of DSM-III borderline personality disorder: a phenomenologic, family history, treatment response, and long-term follow-up study. Arch Gen Psychiatry. 1983;40:23. [PubMed] [Google Scholar]
Pope HG. The validity of DSM-III borderline personality disorder: a phenomenologic, family history, treatment response, and long-term follow-up study. Arch Gen Psychiatry. 1983;40:23. [PubMed] [Google Scholar]
13. Chopra HD, Beatson JA. Psychotic symptoms in borderline personality disorder. Am J Psychiatry. 1986;143:1605–1607. [PubMed] [Google Scholar]
14. Links PS, Steiner M, Mitton J. Characteristics of psychosis in borderline personality disorder. Psychopathology. 1989;22:188–193. [PubMed] [Google Scholar]
15. Kingdon DG, Ashcroft K, Bhandari B, et al. Schizophrenia and borderline personality disorder: similarities and differences in the experience of auditory hallucinations, paranoia, and childhood trauma. J Nerv Ment Dis. 2010;198:399–403. [PubMed] [Google Scholar]
16. Merrett Z, Rossell SL, Castle DJ. Comparing the experience of voices in borderline personality disorder with the experience of voices in a psychotic disorder: a systematic review. Aust N Z J Psychiatry. 2016;50:640–648. [PubMed] [Google Scholar]
Aust N Z J Psychiatry. 2016;50:640–648. [PubMed] [Google Scholar]
17. Niemantsverdriet MBA, Slotema CW, Blom JD, et al. Hallucinations in borderline personality disorder: prevalence, characteristics and associations with comorbid symptoms and disorders. Sci Rep. 2017;7:13920. [PMC free article] [PubMed] [Google Scholar]
18. Lindley SE, Carlson E, Sheikh J. Psychotic symptoms in posttraumatic stress disorder. CNS Spectr. 2000;5:52–57. [PubMed] [Google Scholar]
19. Larøi F, Sommer IE, Blom JD, et al. The characteristic features of auditory verbal hallucinations in clinical and non-clinical groups: state-of-The-art overview and future directions. Schizophr Bull. 2012;38:724–733. [PMC free article] [PubMed] [Google Scholar]
20. Slotema CW, Daalman K, Blom JD, Diederen KMJ, Hoek HW, Sommer IEC. Auditory verbal hallucinations in patients with borderline personality disorder are similar to those with schizophrenia. Psychol Med.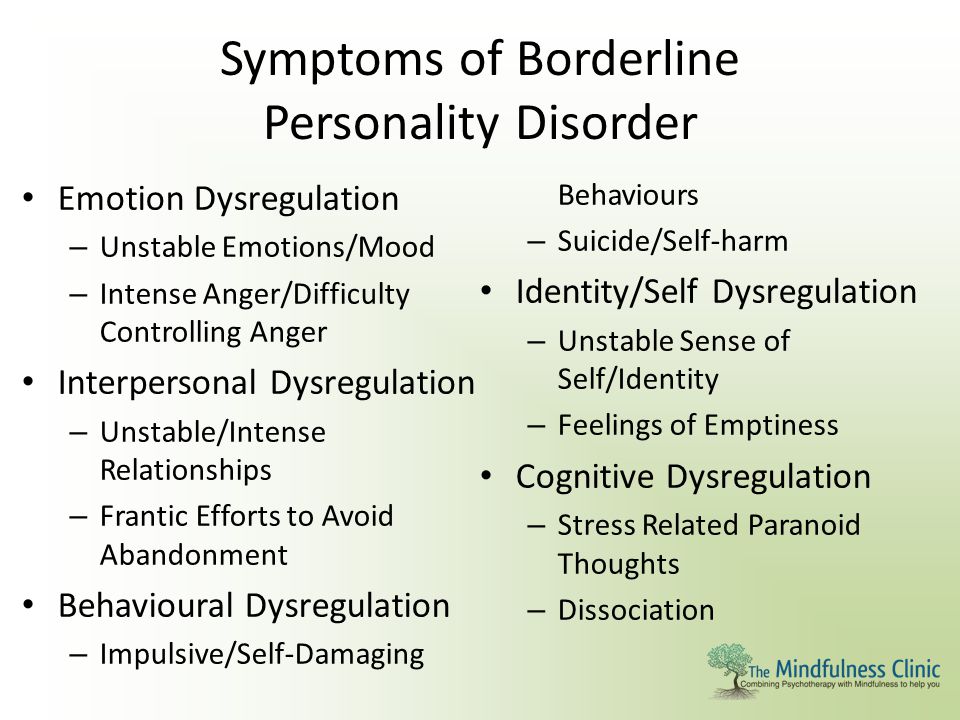 2012;42:1873–1878. [PubMed] [Google Scholar]
2012;42:1873–1878. [PubMed] [Google Scholar]
21. Schroeder K, Fisher HL, Sch€afer I. Psychotic symptoms in patients with borderline personality disorder: prevalence and clinical management. Curr Opin Psychiatry. 2013;26:113–119. [PubMed] [Google Scholar]
22. Beatson J, Broadbear JH, Duncan C, Bourton D, Rao S. Avoiding misdiagnosis when auditory verbal hallucinations are present in borderline personality disorder. J Nerv Ment Dis. 2019;207:1048–1055. [PubMed] [Google Scholar]
23. D’Agostino A, Rossi Monti M, Starcevic V. Psychotic symptoms in borderline personality disorder: an update. Curr Opin Psychiatry. 2018;1:12. [PubMed] [Google Scholar]
24. Slotema CW, Blom JD, Niemantsverdriet MBA, Deen M, Sommer IEC. Comorbid diagnosis of psychotic disorders in borderline personality disorder: prevalence and influence on outcome. Front Psychiatry. 2018;9:84. [PMC free article] [PubMed] [Google Scholar]
25. Pearse LJ, Dibben C, Ziauddeen H, Denman C, McKenna PJ.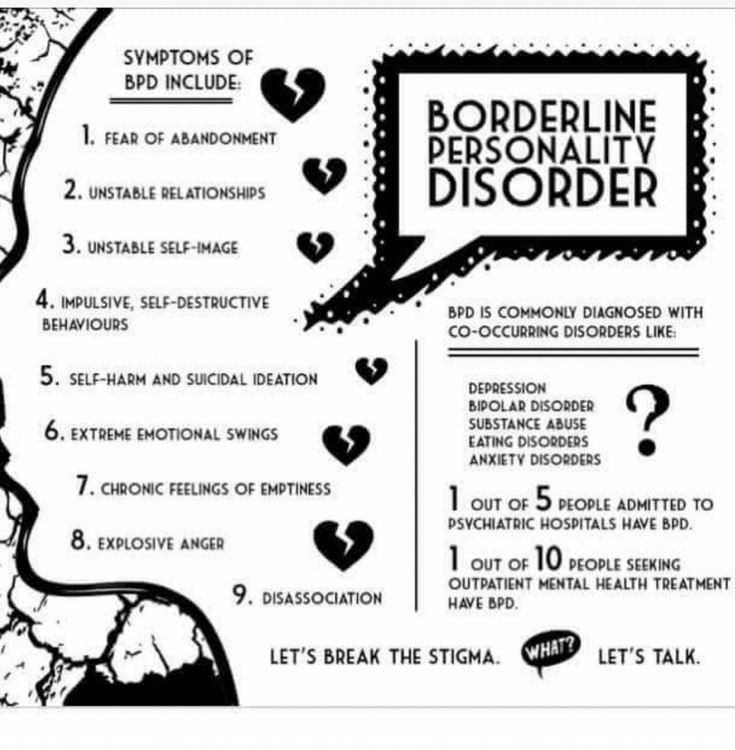 A study of psychotic symptoms in borderline personality disorder. J Nerv Ment Dis. 2014;202:368–371. [PubMed] [Google Scholar]
A study of psychotic symptoms in borderline personality disorder. J Nerv Ment Dis. 2014;202:368–371. [PubMed] [Google Scholar]
26. Tschoeke S, Steinert T, Flammer E, Uhlmann C. Similarities and differences in borderline personality disorder and schizophrenia with voice hearing. J Nerv Ment Dis. 2014;202:544–549. [PubMed] [Google Scholar]
27. Yee L, Korner AJ, McSwiggan S, Meares RA, Stevenson J. Persistent hallucinosis in borderline personality disorder. Compr Psychiatry. 2005;46:147–154. [PubMed] [Google Scholar]
28. Slotema CW, Bayrak H, Linszen MMJ, Deen M, Sommer IEC. Hallucinations in patients with borderline personality disorder: characteristics, severity, and relationship with schizotypy and loneliness. Acta Psychiatr Scand. 2019;139:434–442. [PubMed] [Google Scholar]
29. Rom O, Reznick AZ. The Stress Reaction: a Historical Perspective. Adv Exp Med Biol. 2016;905:1–4. [PubMed] [Google Scholar]
30. Howes OD, Murray RM.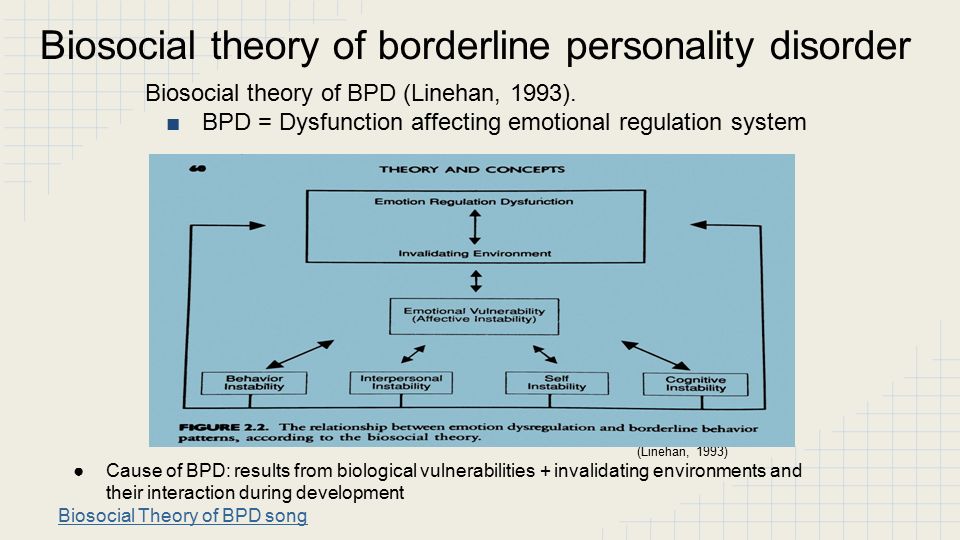 Schizophrenia: an integrated sociodevelopmental-cognitive model. Lancet. 2014;383(9929):1677–1687. [PMC free article] [PubMed] [Google Scholar]
Schizophrenia: an integrated sociodevelopmental-cognitive model. Lancet. 2014;383(9929):1677–1687. [PMC free article] [PubMed] [Google Scholar]
31. Glaser J-P, Van Os J, Thewissen V, Myin-Germeys I. Psychotic reactivity in borderline personality disorder. Acta Psychiatr Scand. 2010;121:125–134. [PubMed] [Google Scholar]
32. Daalman K, Diederen KM, Derks EM, van Lutterveld R, Kahn RS, Sommer IE. Childhood trauma and auditory verbal hallucinations. Psychol Med. 2012;42:2475–2484. [PubMed] [Google Scholar]
33. Varese F, Barkus E, Bentall RP. Dissociation mediates the relationship between childhood trauma and hallucination-proneness. Psychol Med. 2012;42:1025–1036. [PubMed] [Google Scholar]
34. Whitfield CL, Dube SR, Felitti VJ, Anda RF. Adverse childhood experiences and hallucinations. Child Abuse Negl. 2005;29:797–810. [PubMed] [Google Scholar]
35. De Jong Gierveld J, Kamphuis FH. The development of a Rasch-type loneliness-scale.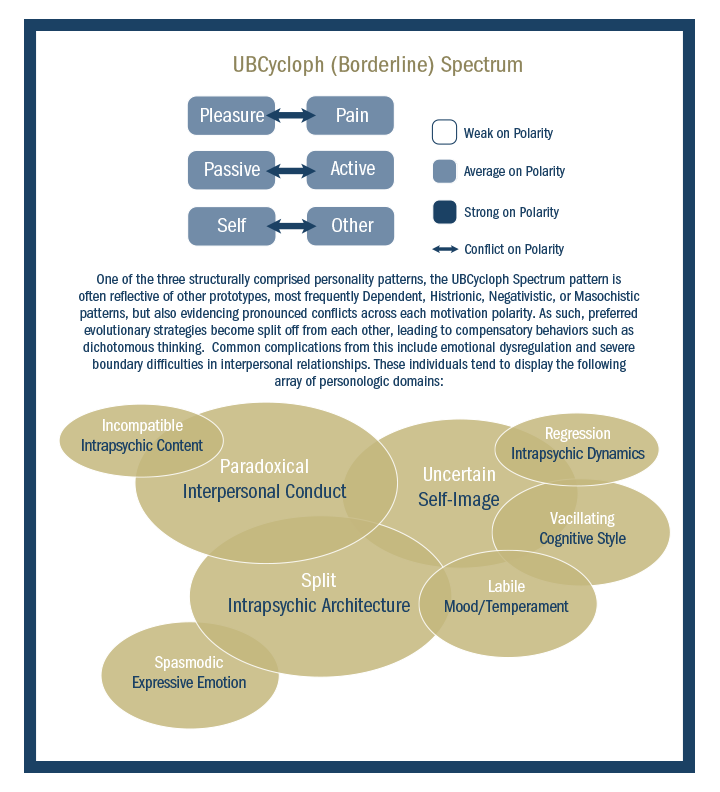 App Psychol Meas. 1985;9:289–299. [Google Scholar]
App Psychol Meas. 1985;9:289–299. [Google Scholar]
36. Mushtaq R, Shoib S, Shah T, Mushtaq S. Relationship between loneliness, psychiatric disorders and physical health? A review on the psychological aspects of loneliness. J Clin Diagn Res. 2014;8:WE01–4. [PMC free article] [PubMed] [Google Scholar]
37. Hoffman RE. A social deafferentation hypothesis for induction of active schizophrenia. Schiz Bull. 2007;33:1066–1070. [PMC free article] [PubMed] [Google Scholar]
38. Hoffman RE. Auditory verbal hallucinations, speech perception neurocircuitry, and the social deafferentation hypothesis. Clin EEG Neurosci. 2008;39:87–90. [PubMed] [Google Scholar]
39. Epley N, Akalis S, Waytz A, Cacioppo JT. Creating social connection through inferential reproduction: loneliness and perceived agency in gadgets, gods, and greyhounds. Psychol Sci. 2008;19:114–120. [PubMed] [Google Scholar]
40. Tan HY, Ang YG. First-episode psychosis in the military: a comparative study of prodromal symptoms.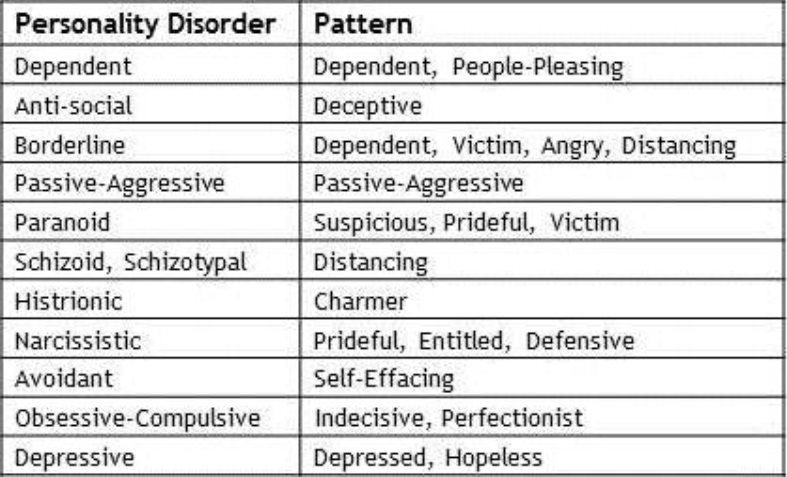 Aust N Z J Psychiatry. 2001;35:512–519. [PubMed] [Google Scholar]
Aust N Z J Psychiatry. 2001;35:512–519. [PubMed] [Google Scholar]
41. Nayani TH, David AS. The auditory hallucination: a phenomenological survey. Psychol Med. 1996;26:177–189. [PubMed] [Google Scholar]
42. Da Rocha MB, Rhodes S, Vasipoulou E, Hutton P. Loneliness in psychosis: a meta-analytic review. Schizophr Bull. 2017;44:114–125. [PMC free article] [PubMed] [Google Scholar]
43. Meltzer H, Bebbington P, Dennis MS, Jenkins R, McManus S, Brugha TS. Feelings of loneliness among adults with mental disorder. Soc Psychiatry Psychiatr Epidemiol. 2013;48:5–13. [PubMed] [Google Scholar]
44. Stain HJ, Galletly CA, Clark S, et al. Understanding the social costs of psychosis: the experience of adults affected by psychosis identified within the second Australian National Survey of Psychosis. Aust N Z J Psychiatry. 2012;46:879–889. [PubMed] [Google Scholar]
45. Klonsky ED. What is emptiness? Clarifying the 7th criterion for borderline personality disorder.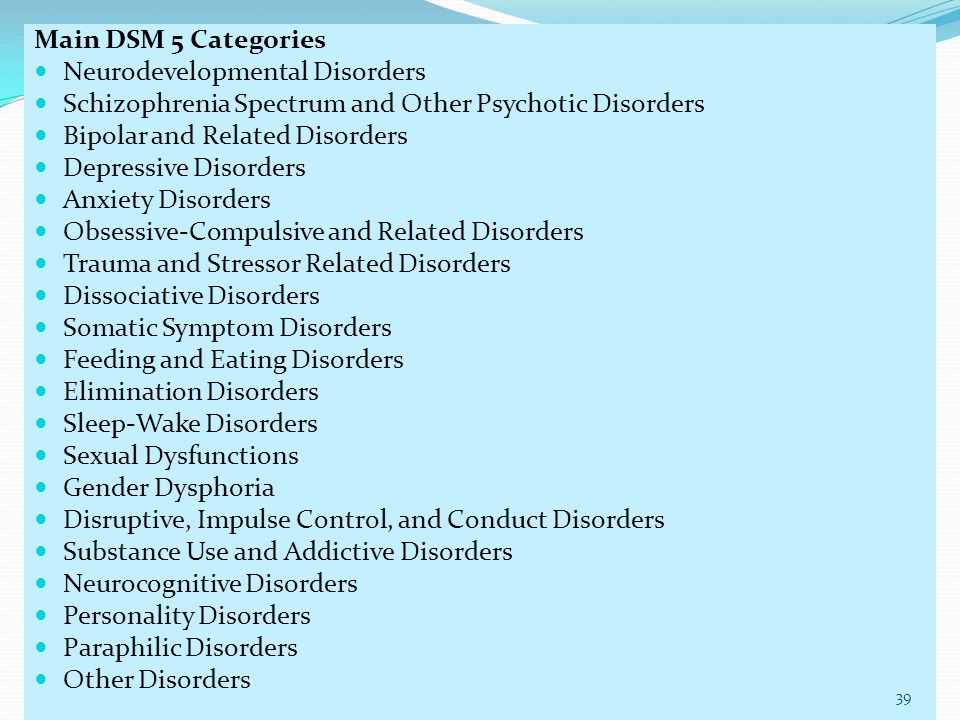 J Pers Dis. 2008;22:418–426. [PubMed] [Google Scholar]
J Pers Dis. 2008;22:418–426. [PubMed] [Google Scholar]
46. Liebke L, Bungert M, Thome J, Hauschild S, Gescher DM, Schmahl C. Loneliness, social networks, and social functioning in borderline personality disorder. Pers Dis. 2017;8:349–356. [PubMed] [Google Scholar]
47. Zanarini MC, Frankenburg FR, Reich BD, Silk KR, Hudson JI, McSweeney LB. The subsyndromal phenomenology of borderline personality disorder: a 10-year follow-up study. Am J Psychiatry. 2007;164:929–935. [PubMed] [Google Scholar]
48. Modenato D. The concept of schizotypy — a computational anatomy perspective. Schizophrenia Research. 2015;2(2):89–892. [PMC free article] [PubMed] [Google Scholar]
49. George A, Soloff PH. Schizotypal symptoms in patients with borderline personality disorders. Am J Psychiatry. 1986;143:212–215. [PubMed] [Google Scholar]
50. Kavoussi RJ, Siever LJ. Overlap between borderline and schizotypal personality disorders. Compr Psychiatry. 1992;33:7–12. [PubMed] [Google Scholar]
1992;33:7–12. [PubMed] [Google Scholar]
51. van Riel L, Ingenhoven TJM, van Dam QD, et al. Borderline or schizotypal? Differential psychodynamic assessment in severe personality disorders. J Psychiatr Practice. 2017;23:101–113. [PubMed] [Google Scholar]
52. Raine A. The SPQ: a Scale for the Assessment of Schizotypal Personality Based on DSM-III-R Criteria. Schizophr Bull. 1991;17(4):555–564. [PubMed] [Google Scholar]
53. Vollema MG, Sitskoorn MM, Appels MC, Kahn RS. Does the Schizotypal Personality Questionnaire reflect the biological-genetic vulnerability to schizophrenia? Schizophr Res. 2002;1:39–45. [PubMed] [Google Scholar]
54. Sommer IE, Daalman K, Rietkerk T, et al. Healthy individuals with auditory verbal hallucinations; who are they? Psychiatric assessments of a selected sample of 103 subjects. Schizophr Bull. 2010;36:633–641. [PMC free article] [PubMed] [Google Scholar]
55. Hummelen B, Pedersen G, Karterud S. Some suggestions for the DSM-5 schizotypal personality disorder construct.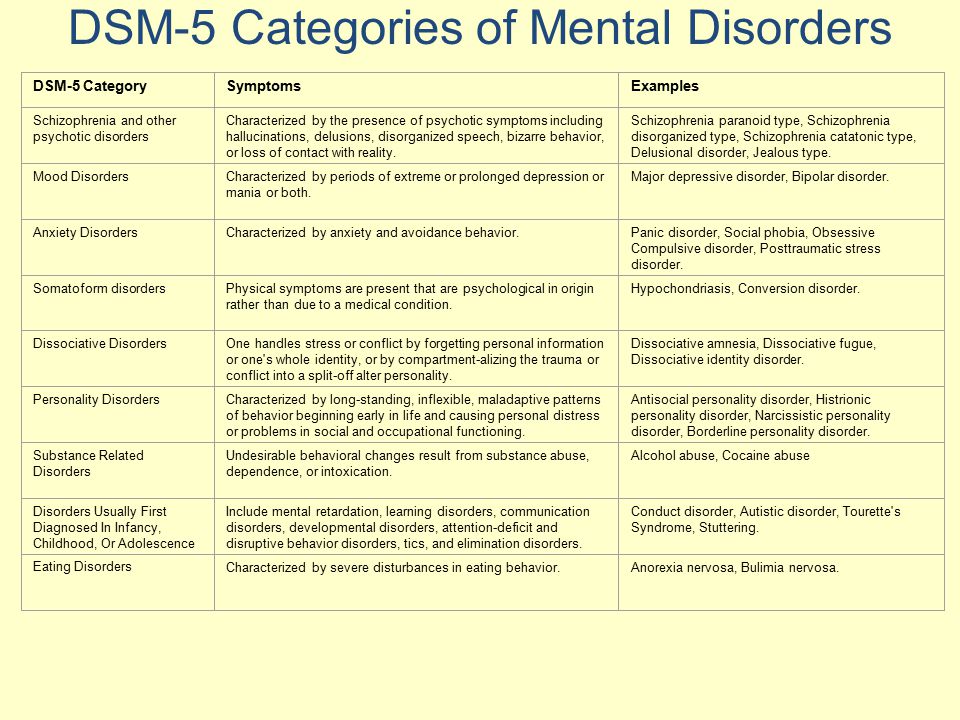 Compr Psychiatry. 2012;53:341–349. [PubMed] [Google Scholar]
Compr Psychiatry. 2012;53:341–349. [PubMed] [Google Scholar]
56. Zanarini MC, Frankenburg FR, Dubo ED, et al. Axis II comorbidity of borderline personality disorder. Compr Psychiatry. 1998;39:296–302. [PubMed] [Google Scholar]
57. Chanen AM, McCutcheon L. Prevention and early intervention for borderline personality disorder: current status and recent evidence. Br J Psychiatry. 2013;202:s24–s29. [PubMed] [Google Scholar]
58. Sharp C, Wall K. Personality pathology grows up: adolescence as a sensitive period. Curr Opin Psychol. 2018;21:111–116. [PubMed] [Google Scholar]
59. McGorry PD, Purcell R, Goldstone S, Amminger GP. Age of onset and timing of treatment for mental and substance use disorders: implications for preventive intervention strategies and models of care. Curr Opin Psychiatry. 2011;24:301–306. [PubMed] [Google Scholar]
60. Winsper C, Wolke D, Scott J, Sharp C, Thompson A, Marwaha S. Psychopathological outcomes of adolescent borderline personality disorder symptoms.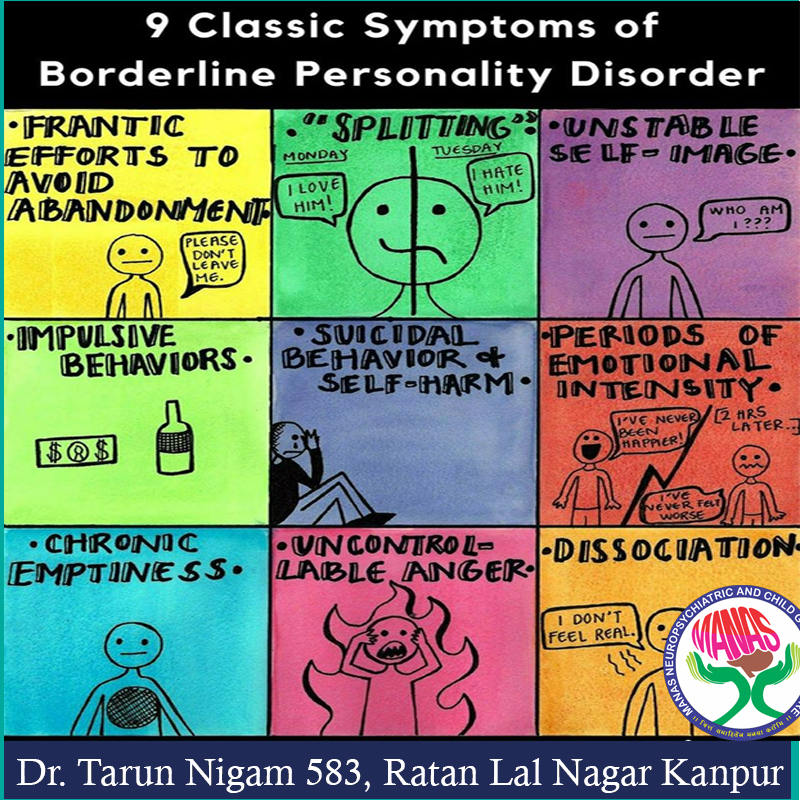 Aust N Z J Psychiatry. 2020;54:308–317. [PubMed] [Google Scholar]
Aust N Z J Psychiatry. 2020;54:308–317. [PubMed] [Google Scholar]
61. Paust T, Theodoridou A, Muller M, et al. Borderline personality pathology in an at-risk mental state sample. Front Psychiatry. 2019;10:838. [PMC free article] [PubMed] [Google Scholar]
62. Ryan J, Graham A, Nelson B, Yung A. Borderline personality pathology in young people at ultra-high risk of developing a psychotic disorder: borderline personality pathology. Early Interv Psychiatry. 2017;11:208–214. [PubMed] [Google Scholar]
63. Schultze-Lutter F, Klosterkötter J, Michel C, Winkler K, Ruhrmann S. Personality disorders and accentuations in at-risk persons with and without conversion to first-episode psychosis: personality disorders and psychosis risk. Early Interv Psychiatry. 2012;6:389–398. [PubMed] [Google Scholar]
64. Thompson A, Nelson B, Bechdolf A, et al. Borderline personality features and development of psychosis in an ‘Ultra High Risk’ (UHR) population: a case control study: borderline personality and psychosis risk. Early Interv Psychiatry. 2012;6:247–255. [PubMed] [Google Scholar]
Early Interv Psychiatry. 2012;6:247–255. [PubMed] [Google Scholar]
65. Caspi A, Houts RM, Belsky DW, et al. The p factor: one general psychopathology factor in the structure of psychiatric disorders? Clin Psychol Sci. 2014;2:119–137. [PMC free article] [PubMed] [Google Scholar]
66. Sharp C, Vanwoerden S, Wall K. Adolescence as a sensitive period for the development of personality disorder. Psychiatr Clin North Am. 2018;41:669–683. [PubMed] [Google Scholar]
67. Cavelti M, Thompson K, Chanen AM, Kaess M. Psychotic symptoms in borderline personality disorder: developmental aspects. Current Opinion in Psychology. 2021;37:26–31. [PubMed] [Google Scholar]
68. Thompson KN, Cavelti M, Chanen AM. Psychotic symptoms in adolescents with borderline personality disorder features. Eur Child Adolesc Psychiatry. 2019;28:985–992. [PubMed] [Google Scholar]
69. Cavelti M, Thompson KN, Hulbert C, et al. Exploratory comparison of auditory verbal hallucinations and other psychotic symptoms among youth with borderline personality disorder or schizophrenia spectrum disorder.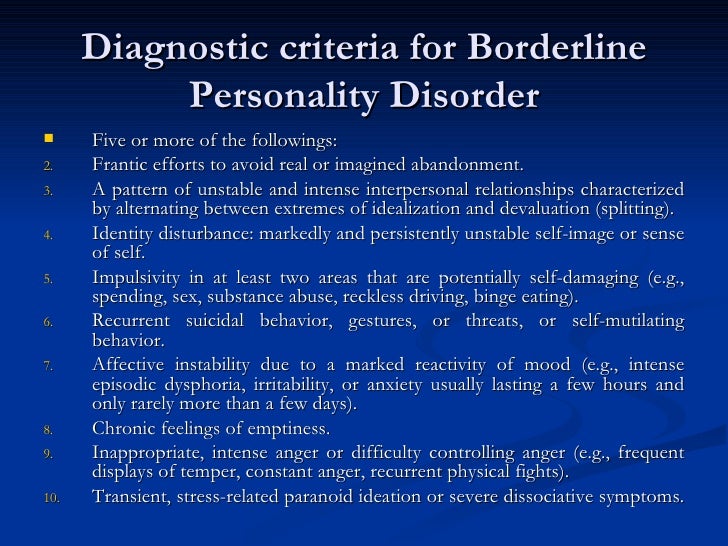 Early Interv Psychiatry. 2019;13:1252–1262. [PubMed] [Google Scholar]
Early Interv Psychiatry. 2019;13:1252–1262. [PubMed] [Google Scholar]
70. Zandersen M, Parnas J. Identity disturbance, feelings of emptiness, and the boundaries of the schizophrenia spectrum. Schizophr Bull. 2019;45:106–113. [PMC free article] [PubMed] [Google Scholar]
71. Bachmann S. Epidemiology of Suicide and the Psychiatric Perspective. Int J Environ Res Public Health. 2018;15(7):1425. [PMC free article] [PubMed] [Google Scholar]
72. Kelleher I, Ramsay H, DeVylder J. Psychotic experiences and suicide attempt risk in common mental disorders and borderline personality disorder. Acta Psychiatr Scand. 2017;135:212–218. [PubMed] [Google Scholar]
73. Slotema CW, Niemantsverdriet MB, Blom JD, et al. Suicidality and hospitalisation in patients with borderline personality disorder who experience auditory verbal hallucinations. Eur Psychiatry. 2017;41:47–52. [PubMed] [Google Scholar]
74. Schroeder K, Schätzle A, Kowohl P, Leske L, Huber CG, Schafer I.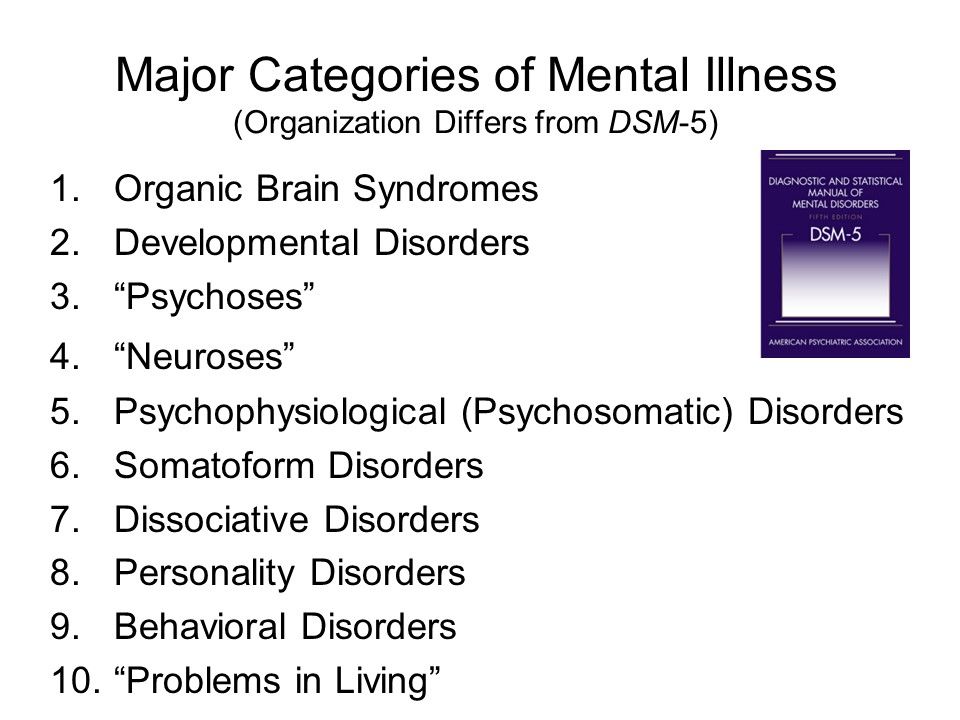 Prevalence and phenomenology of psychotic-like symptoms in borderline personality disorders – associations with suicide attempts and use of psychiatric inpatient treatment. Psychother Psychosom Med Psychol. 2018;68:516–524. [PubMed] [Google Scholar]
Prevalence and phenomenology of psychotic-like symptoms in borderline personality disorders – associations with suicide attempts and use of psychiatric inpatient treatment. Psychother Psychosom Med Psychol. 2018;68:516–524. [PubMed] [Google Scholar]
75. Furnes D, Gjestad R, Mehlum L, et al. Personality disorder: what predicts acute psychiatric readmissions? J Personal Disord. 2019;1:1–13. [PubMed] [Google Scholar]
76. Slotema CW, Blom JD, Niemantsverdriet MBA, Sommer IEC. Auditory verbal hallucinations in borderline personality disorder and the efficacy of antipsychotics: a systematic review. Front Psychiatry. 2018;9:347. [PMC free article] [PubMed] [Google Scholar]
77. Pope HG, Jonas JM, Hudson JI, Cohen BM, Tohen M. An empirical study of psychosis in borderline personality disorder. Am J Psychiatry. 1985;142:1285–1290. [PubMed] [Google Scholar]
78. Nishizono-Maher A, Ikuta N, Ogiso Y, Moriya N, Miyake Y, Minakawa K. Psychotic symptoms in depression and borderline personality disorder. J Affect Disord. 1993;28:279–285. [PubMed] [Google Scholar]
J Affect Disord. 1993;28:279–285. [PubMed] [Google Scholar]
79. Miller FT, Abrams T, Dulit R, Fyer M. Psychotic symptoms in patients with borderline personality disorder and concurrent axis I disorder. Hosp Community Psychiatry. 1993;44:59–61. [PubMed] [Google Scholar]
80. Benvenuti A, Rucci P, Ravani L, et al. Psychotic features in borderline patients: is there a connection to mood dysregulation? Bipolar Disord. 2005;7:338–343. [PubMed] [Google Scholar]
81. Francey SM, Jovev M, Phassouliotis C, Cotton SM, Chanen AM. Does co-occurring borderline personality disorder influences acute-phase treatment for first-episode psychosis? Early Interv Psychiatry. 2018;12:1166–1172. [PubMed] [Google Scholar]
82. Hepworth CR, Ashcroft K, Kingdon D. Auditory hallucinations: a comparison of beliefs about voices in individuals with schizophrenia and borderline personality disorder: auditory hallucinations. Clin Psychol Psychother. 2013;20:239–245. [PubMed] [Google Scholar]
[PubMed] [Google Scholar]
83. Ingenhoven T, Lafay P, Rinne T, Passchier J, Duivenvoorden H. Effectiveness of pharmacotherapy for severe personality disorders: meta-analyses of randomized controlled trials. J Clin Psychiatry. 2010;71:14–25. [PubMed] [Google Scholar]
84. Ingenhoven TJ, Duivenvoorden HJ. Differential effectiveness of antipsychotics in borderline personality disorder: meta-analyses of placebo-controlled, randomized clinical trials on symptomatic outcome domains. J Clin Psychopharmacol. 2011;31:489–496. [PubMed] [Google Scholar]
85. Lieb K, Völlm B, Rucker G, Timmer A, Stoffers JM. Pharmacotherapy for borderline personality disorder: Cochrane systematic review of randomised trials. Br J Psychiatry. 2010;196:4–12. [PubMed] [Google Scholar]
86. Lim MH, Gleeson JFM, Alvarez-Jimenez M, Penn DL. Loneliness in psychosis: a systematic review. Soc Psychiatry Psychiatr Epid. 2018;53:221–238. [PubMed] [Google Scholar]
87. Longden E, Branitsky A, Moskowitz A, Berry K, Bucci S, Varese F. The relationship between dissociation and symptoms of psychosis: a meta-analysis. Schizophr Bull. 2020;1:sbaa037. [PMC free article] [PubMed] [Google Scholar]
Longden E, Branitsky A, Moskowitz A, Berry K, Bucci S, Varese F. The relationship between dissociation and symptoms of psychosis: a meta-analysis. Schizophr Bull. 2020;1:sbaa037. [PMC free article] [PubMed] [Google Scholar]
88. Stanton KJ, Denietolis B, Goodwin BJ, Dvir Y. Childhood trauma and psychosis. Child Adolesc Psychiatr Clin N Am. 2020;29:115–129. [PubMed] [Google Scholar]
89. El Haj M, Jardri R, Larøi F, Antoine P. Hallucinations, loneliness, and social isolation in Alzheimer’s disease. Cogn Neuropsychiatry. 2016;21:1–13. [PubMed] [Google Scholar]
90. Sommer IEC, Slotema CW, Daskalakis ZJ, Derks EM, Blom JD, van der Gaag M. The treatment of hallucinations in schizophrenia spectrum disorders. Schizophr Bull. 2012;38:704–714. [PMC free article] [PubMed] [Google Scholar]
91. McCarthy-Jones S, Smailes D, Corvin A, et al. Occurrence and co-occurrence of hallucinations by modality in schizophrenia-spectrum disorders. Psychiatry Res.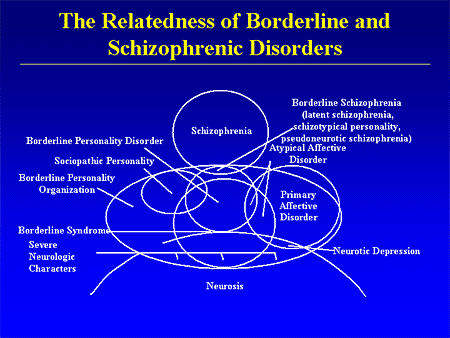 2017;252:154–160. [PubMed] [Google Scholar]
2017;252:154–160. [PubMed] [Google Scholar]
92. Waters F, Fernyhough C. Hallucinations: a Systematic Review of Points of Similarity and Difference Across Diagnostic Classes. Schizophr Bull. 2017;43(1):32–43. [PMC free article] [PubMed] [Google Scholar]
93. Niemantsverdriet MBA, Slotema CW, van der Veen FM, et al. Sensory processing deficiencies in patients with borderline personality disorder who experience auditory verbal hallucinations. Psychiatry Res. 2019;281:112545. [PubMed] [Google Scholar]
94. Davies G, Hayward M, Evans S, Mason O. A systematic review of structural MRI investigations within borderline personality disorder: identification of key psychological variables of interest going forward. Psychiatry Res. 2020;286:112864. [PubMed] [Google Scholar]
95. Chanen AM, Betts J, Jackson H, et al. Aripiprazole compared with placebo for auditory verbal hallucinations in youth with borderline personality disorder: protocol for the VERBATIM randomized controlled trial. Early Interv Psychiatry. 2019;13(6):1373–1381. [PubMed] [Google Scholar]
Early Interv Psychiatry. 2019;13(6):1373–1381. [PubMed] [Google Scholar]
96. Slotema CW, Blom JD, Deen M, et al. Negative beliefs about voices in patients with borderline personality disorder are associated with distress: a plea for cognitive-behavioural therapy? Psychopathology. 2017;50:255–261. [PubMed] [Google Scholar]
97. Cavelti M, Thompson KN, Hulbert C, et al. Preliminary evidence for the cognitive model of auditory verbal hallucinations in youth with borderline personality disorder. Front Psychiatry. 2019b;10:292. [PMC free article] [PubMed] [Google Scholar]
98. Cavelti M, Thompson KN, Hulbert C, et al. Testing the interpersonal-cognitive model of auditory verbal hallucinations in youths with either early-stage borderline personality disorder or first-episode schizophrenia Spectrum disorder. Psychopathology. 2020;1:1–13. [PubMed] [Google Scholar]
99. Thomas N, Hayward M, Peters E, et al. Psychological therapies for auditory hallucinations (Voices): current status and key directions for future research. Schizophr Bull. 2014;40:S202–S212. [PMC free article] [PubMed] [Google Scholar]
Schizophr Bull. 2014;40:S202–S212. [PMC free article] [PubMed] [Google Scholar]
100. Fielding-Smith SF, Hayward M, Strauss C, Fowler D, Paulik G. Thomas N: bringing the “self” into focus: conceptualising the role of self-experience for understanding and working with distressing voices. Front Psychol. 2015;6:1129. [PMC free article] [PubMed] [Google Scholar]
101. Chanen AM, Berk M, Thompson KN. Integrating early intervention for borderline personality disorder and mood disorders. Harv Rev Psychiatry. 2016;24:330–341. [PubMed] [Google Scholar]
102. Hutsebaut J, Videler AC, Verheul R, Van Alphen SPJ. Managing borderline personality disorder from a life course perspective: clinical staging and health management. Personal Disord. 2019;10:309–316. [PubMed] [Google Scholar]
Borderline personality disorder and psychosis: a review
Review
. 2010 Jun;12(3):186-95.
doi: 10.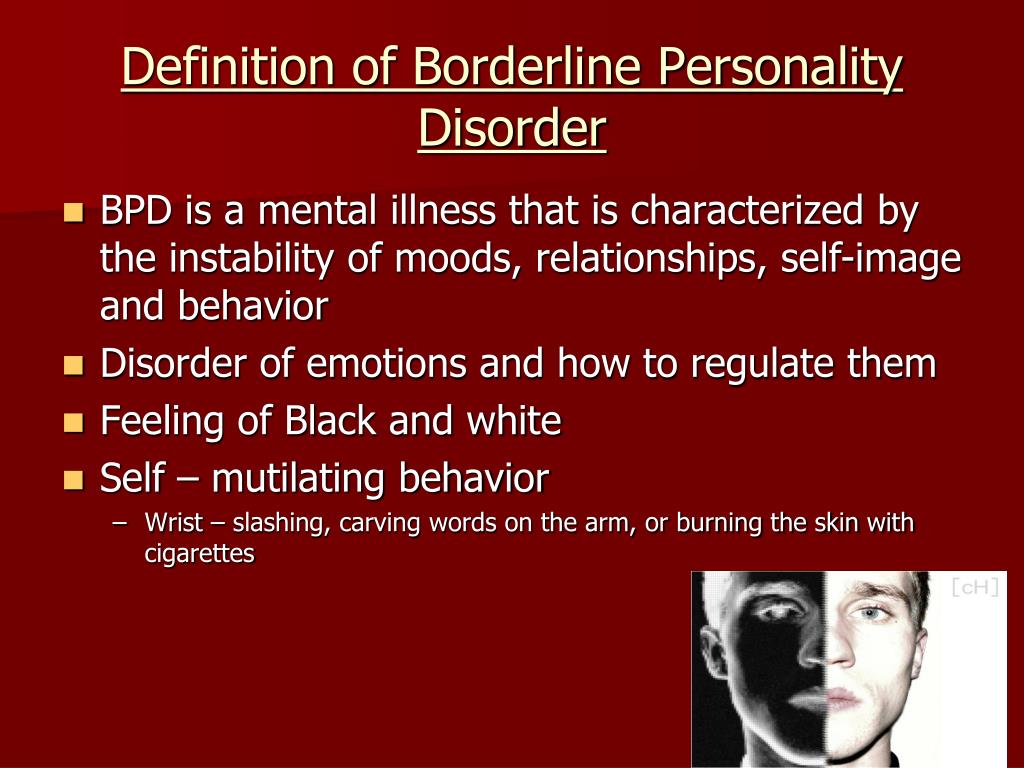 1007/s11920-010-0107-9.
1007/s11920-010-0107-9.
Sven Barnow 1 , Elisabeth A Arens, Simkje Sieswerda, Ramona Dinu-Biringer, Carsten Spitzer, Simone Lang
Affiliations
Affiliation
- 1 Department of Clinical Psychology and Psychotherapy, Psychological Institute, Ruprecht-Karls University Heidelberg, Hauptstr. 47-51, Heidelberg 69117, Germany. [email protected]
- PMID: 20425279
- DOI: 10.1007/s11920-010-0107-9
Review
Sven Barnow et al. Curr Psychiatry Rep. 2010 Jun.
. 2010 Jun;12(3):186-95.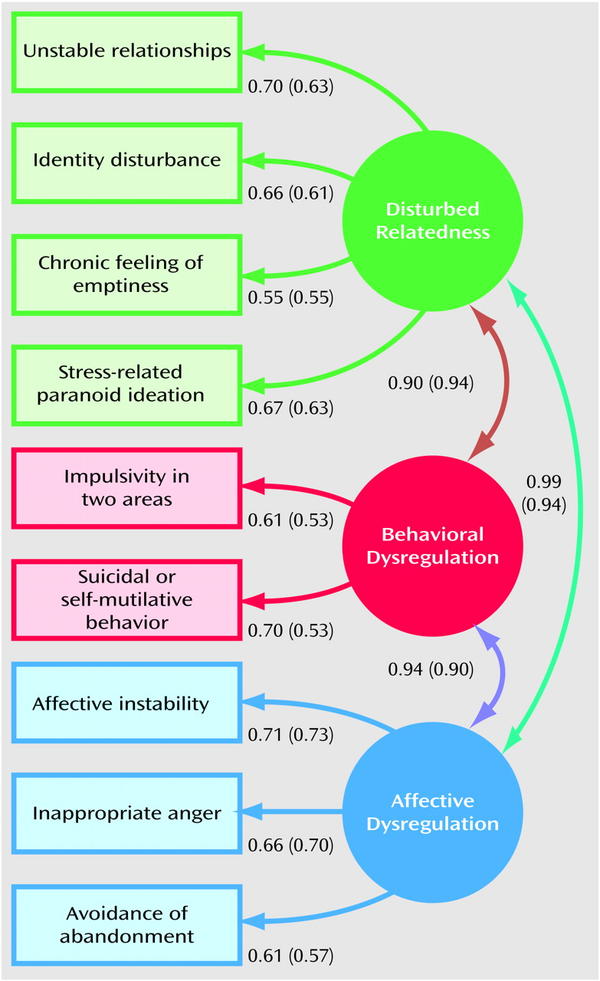
doi: 10.1007/s11920-010-0107-9.
Authors
Sven Barnow 1 , Elisabeth A Arens, Simkje Sieswerda, Ramona Dinu-Biringer, Carsten Spitzer, Simone Lang
Affiliation
- 1 Department of Clinical Psychology and Psychotherapy, Psychological Institute, Ruprecht-Karls University Heidelberg, Hauptstr. 47-51, Heidelberg 69117, Germany. [email protected]
- PMID: 20425279
- DOI: 10.1007/s11920-010-0107-9
Abstract
Early views of borderline personality disorder (BPD) were based on the idea that patients with this pathology were "on the border" of psychosis. However, more recent studies have not supported this view, although they have found evidence of a malevolent interpersonal evaluation and a significant proportion of BPD patients showing psychotic symptoms. For example, in one study, 24% of BPD patients reported severe psychotic symptoms and about 75% had dissociative experiences and paranoid ideation. Thus, we start with an overview regarding the prevalence of psychotic symptoms in BPD patients. Furthermore, we report findings of studies investigating the role of comorbidity (eg, post-traumatic stress disorder) in the severity and frequency of psychotic symptoms in BPD patients. We then present results of genetic and neurobiological studies comparing BPD patients with patients with schizophrenia or nonschizophrenic psychotic disorders. In conclusion, this review reveals that psychotic symptoms in BPD patients may not predict the development of a psychotic disorder but are often permanent and severe and need careful consideration by clinicians.
However, more recent studies have not supported this view, although they have found evidence of a malevolent interpersonal evaluation and a significant proportion of BPD patients showing psychotic symptoms. For example, in one study, 24% of BPD patients reported severe psychotic symptoms and about 75% had dissociative experiences and paranoid ideation. Thus, we start with an overview regarding the prevalence of psychotic symptoms in BPD patients. Furthermore, we report findings of studies investigating the role of comorbidity (eg, post-traumatic stress disorder) in the severity and frequency of psychotic symptoms in BPD patients. We then present results of genetic and neurobiological studies comparing BPD patients with patients with schizophrenia or nonschizophrenic psychotic disorders. In conclusion, this review reveals that psychotic symptoms in BPD patients may not predict the development of a psychotic disorder but are often permanent and severe and need careful consideration by clinicians.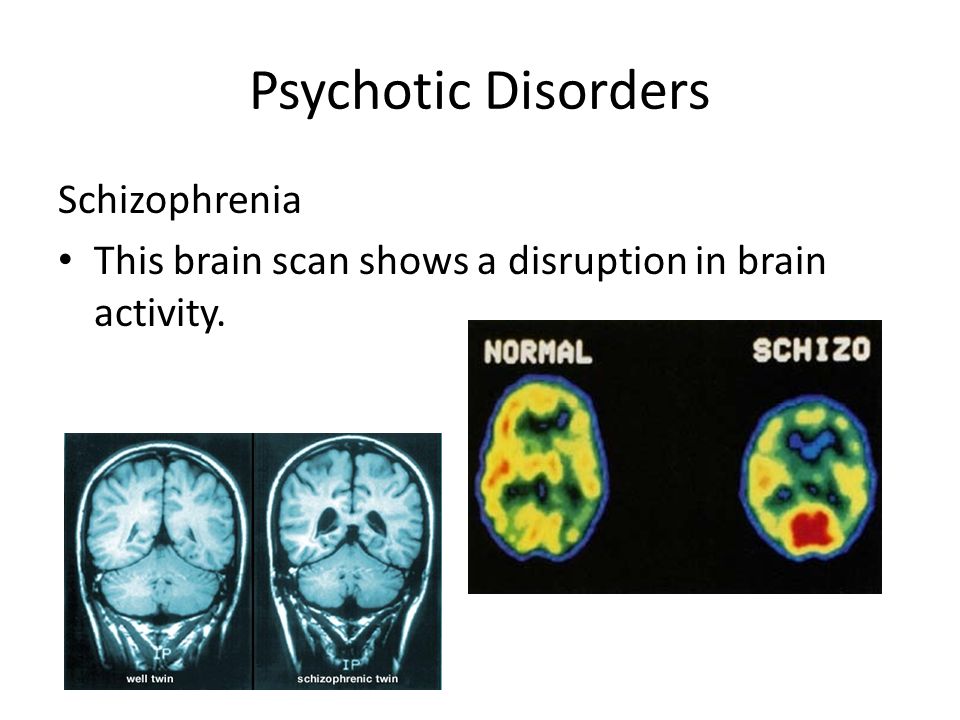 Therefore, adequate diagnosis and treatment of psychotic symptoms in BPD patients is emphasized.
Therefore, adequate diagnosis and treatment of psychotic symptoms in BPD patients is emphasized.
Similar articles
-
Psychotic symptoms in patients with borderline personality disorder: prevalence and clinical management.
Schroeder K, Fisher HL, Schäfer I. Schroeder K, et al. Curr Opin Psychiatry. 2013 Jan;26(1):113-9. doi: 10.1097/YCO.0b013e32835a2ae7. Curr Opin Psychiatry. 2013. PMID: 23168909 Review.
-
Psychotic reactivity in borderline personality disorder.
Glaser JP, Van Os J, Thewissen V, Myin-Germeys I. Glaser JP, et al. Acta Psychiatr Scand. 2010 Feb;121(2):125-34. doi: 10.1111/j.1600-0447.2009.01427.x. Epub 2009 Jun 25. Acta Psychiatr Scand. 2010. PMID: 19555465
-
[Hallucinations and borderline personality disorder: a review].
Gras A, Amad A, Thomas P, Jardri R. Gras A, et al. Encephale. 2014 Dec;40(6):431-8. doi: 10.1016/j.encep.2014.07.002. Epub 2014 Jul 22. Encephale. 2014. PMID: 25063345 Review. French.
-
Psychosis in borderline personality disorder.
Jonas JM, Pope HG. Jonas JM, et al. Psychiatr Dev. 1984 Winter;2(4):295-308. Psychiatr Dev. 1984. PMID: 6396640 Review.
-
Features of borderline personality disorder as a mediator of the relation between childhood traumatic experiences and psychosis-like experiences in patients with mood disorder.
Baryshnikov I, Aaltonen K, Suvisaari J, Koivisto M, Heikkinen M, Joffe G, Isometsä E. Baryshnikov I, et al. Eur Psychiatry. 2018 Mar;49:9-15.
 doi: 10.1016/j.eurpsy.2017.12.005. Epub 2018 Jan 30. Eur Psychiatry. 2018. PMID: 29353179
doi: 10.1016/j.eurpsy.2017.12.005. Epub 2018 Jan 30. Eur Psychiatry. 2018. PMID: 29353179
See all similar articles
Cited by
-
Demystifying borderline personality disorder in primary care.
Wu T, Hu J, Davydow D, Huang H, Spottswood M, Huang H. Wu T, et al. Front Med (Lausanne). 2022 Nov 3;9:1024022. doi: 10.3389/fmed.2022.1024022. eCollection 2022. Front Med (Lausanne). 2022. PMID: 36405597 Free PMC article. Review.
-
Borderline personality disorder: associations with psychiatric disorders, somatic illnesses, trauma, and adverse behaviors.
Tate AE, Sahlin H, Liu S, Lu Y, Lundström S, Larsson H, Lichtenstein P, Kuja-Halkola R. Tate AE, et al. Mol Psychiatry.
 2022 May;27(5):2514-2521. doi: 10.1038/s41380-022-01503-z. Epub 2022 Mar 18. Mol Psychiatry. 2022. PMID: 35304564 Free PMC article.
2022 May;27(5):2514-2521. doi: 10.1038/s41380-022-01503-z. Epub 2022 Mar 18. Mol Psychiatry. 2022. PMID: 35304564 Free PMC article. -
A Dimensional Understanding of Borderline Personality Disorder Using MMPI-2 PSY-5 Scales in Clinical Samples.
Jin MJ, Lee HJ, Hwang KS, Lee JH, Yang CM, Jang SH, Lee SY. Jin MJ, et al. Psychiatry Investig. 2021 Dec;18(12):1164-1170. doi: 10.30773/pi.2021.0164. Epub 2021 Dec 8. Psychiatry Investig. 2021. PMID: 34872242 Free PMC article.
-
Self-report screening instruments differentiate bipolar disorder and borderline personality disorder.
Palmer BA, Pahwa M, Geske JR, Kung S, Nassan M, Schak KM, Alarcon RD, Frye MA, Singh B. Palmer BA, et al. Brain Behav. 2021 Jul;11(7):e02201.
 doi: 10.1002/brb3.2201. Epub 2021 May 30. Brain Behav. 2021. PMID: 34056864 Free PMC article.
doi: 10.1002/brb3.2201. Epub 2021 May 30. Brain Behav. 2021. PMID: 34056864 Free PMC article. -
Personality Traits as Markers of Psychosis Risk in Kenya: Assessment of Temperament and Character.
Mamah D, Cloninger CR, Mutiso VN, Gitonga I, Tele A, Ndetei DM. Mamah D, et al. Schizophr Bull Open. 2020 Jan;1(1):sgaa051. doi: 10.1093/schizbullopen/sgaa051. Epub 2020 Sep 19. Schizophr Bull Open. 2020. PMID: 33215089 Free PMC article.
See all "Cited by" articles
References
-
- Hosp Community Psychiatry. 1993 Jan;44(1):59-61 - PubMed
-
- J Psychiatr Res.
 2009 Mar;43(6):592-9 - PubMed
2009 Mar;43(6):592-9 - PubMed
- J Psychiatr Res.
-
- Compr Psychiatry. 2005 Mar-Apr;46(2):147-54 - PubMed
-
- J Pers Disord. 2009 Aug;23(4):357-69 - PubMed
-
- Cereb Cortex. 2004 Jan;14(1):91-6 - PubMed
Publication types
MeSH terms
Substances
Borderline personality disorder: what it is, symptoms and signs of BPD
Borderline personality disorder is characterized by emotional instability, impulsive behavior and low self-control. Forbes Life figured out what causes this disease, how to diagnose borderline personality disorder and how to help people who have experienced it
Forbes Life figured out what causes this disease, how to diagnose borderline personality disorder and how to help people who have experienced it
Mental personality disorders differ from other types of disorders in their intensity. They cannot be treated like an ordinary illness, as a temporary mental disorder, because personality disorders affect a set of personal characteristics formed in childhood. There are a number of problems with diagnosing such diseases: their symptoms are quite individual, although there are a number of common signs. For borderline personality disorder (BPD), these may include difficulties with self-image, extreme mood swings, risky behavior, and self-harm. The good news is that personality disorders can still be managed—there is a cure. nine0005
Finished reading here
Now officially: BPD is a diagnosis
Borderline personality disorder is one of the ten types of personality disorders in modern psychotherapy, which is expressed in problems of awareness and formation of personal identity.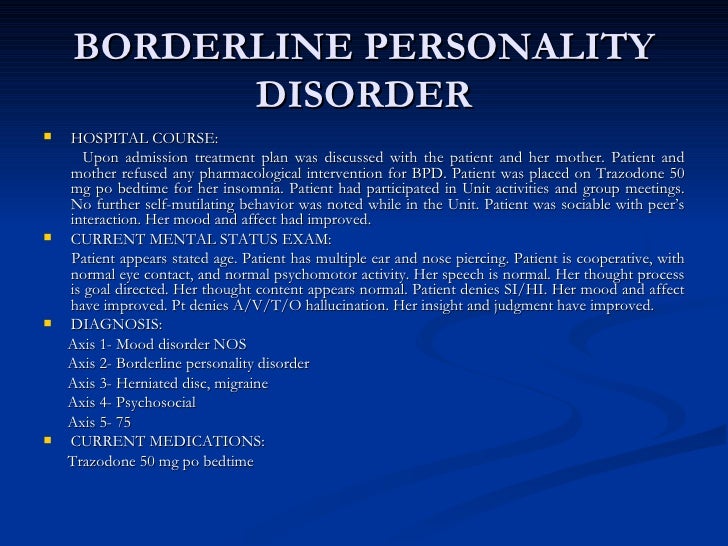 Psychologist, Gestalt therapist Valentin Oskin notes that this mental illness is associated with strong, uncontrollable and often painful emotions that lead to a distorted sense of self and unstable interpersonal relationships. nine0005
Psychologist, Gestalt therapist Valentin Oskin notes that this mental illness is associated with strong, uncontrollable and often painful emotions that lead to a distorted sense of self and unstable interpersonal relationships. nine0005
People with BPD are reverse solipsists: they are convinced of the inviolability of the surrounding world, but doubt the reality of their own existence - their image of the inner “I” is so mobile and unstable. In addition to depersonalization, "borderguards" are characterized by impulsiveness, dependence on other people, unstable behavior, a tendency to a chaotic life, and even a need to harm themselves and injure themselves. "Border guards" are characterized by chronic suicidality: 75% of people with BPD try to commit suicide, of which about 10% die as a result of suicide. Moreover, a third of all completed suicides were committed by those suffering from borderline personality disorder. nine0005
Despite the statistics, until 2022 the diagnosis of BPD in Russia could not be officially diagnosed - borderline personality disorder in psychiatry was defined as a disease only in foreign classifications of diseases.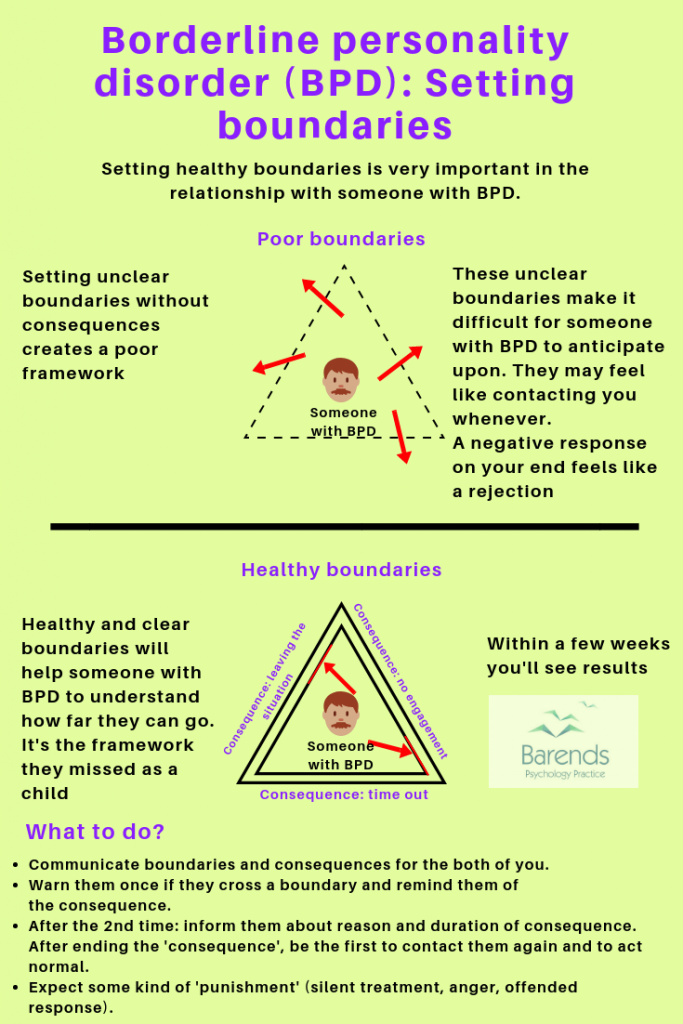 It was often called impulsive personality disorder or generally diagnosed as sluggish schizophrenia: the diseases are similar in symptoms, among the signs of BPD there are no hallucinations and delusions. BPD also resembles bipolar affective disorder (up to 40% of "border guards" get an erroneous diagnosis of bipolar disorder), only periods of depressive and elated mood are replaced with bipolar disorder less often. The transition to the International Classification of Diseases of the 11th revision will finally allow doctors to make an accurate diagnosis for Russian citizens and prescribe the appropriate treatment. nine0005
It was often called impulsive personality disorder or generally diagnosed as sluggish schizophrenia: the diseases are similar in symptoms, among the signs of BPD there are no hallucinations and delusions. BPD also resembles bipolar affective disorder (up to 40% of "border guards" get an erroneous diagnosis of bipolar disorder), only periods of depressive and elated mood are replaced with bipolar disorder less often. The transition to the International Classification of Diseases of the 11th revision will finally allow doctors to make an accurate diagnosis for Russian citizens and prescribe the appropriate treatment. nine0005
Diagnosis is not a sentence, the boundary between the norm and pathology is very flexible: “Each of us has borderline responses. For some, they are deeply hidden and appear only in crises, traumas, stressful situations. And for some, life as such is stressful, and therefore the ways of responding turn into what psychologists could call the borderline organization of the personality,” notes Irina Mlodik, Candidate of Psychological Sciences, in the book “House of Cards. Psychotherapeutic assistance to clients with borderline disorders. nine0005
Psychotherapeutic assistance to clients with borderline disorders. nine0005
Related material
Ghost hints
Most people with BPD are unaware of their diagnosis and do not seek medical attention. And it's not just that BPD in psychology does not have a clear definition. The disease does not allow you to objectively assess your mental state and understand that the indomitable monster inside is raging not because of the permanent retrograde Mercury and the fatal force of circumstances. The absence of obvious mental abnormalities like hallucinations makes it possible to attribute emotional behavior to character traits. Colleagues, friends and relatives often believe that behind the disgusting behavior of such a person is hysteria and selfishness. Therefore, systematic treatment of borderline personality disorder begins in most cases after a suicide attempt.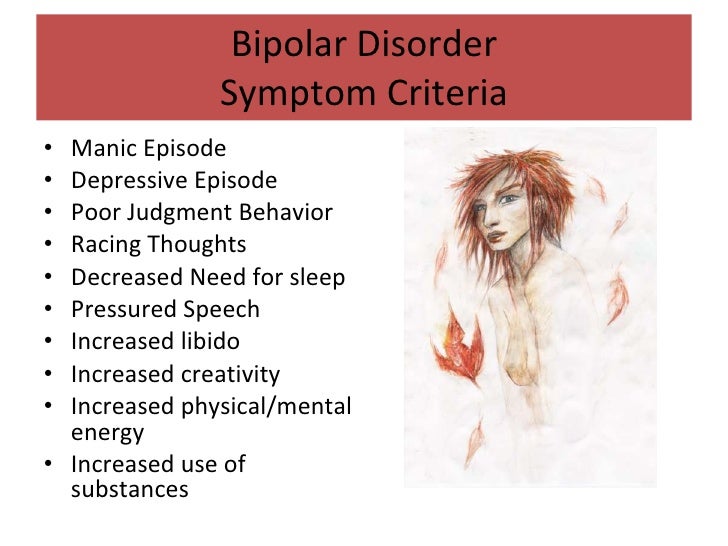 nine0005
nine0005
The most striking and obvious sign of borderline personality disorder is a craving for auto-aggression, or self-harm. This is not only the infliction of bodily harm (cuts, blows or burns), but also the intention to deprive oneself of sleep, nutrition. This practice is not necessarily a consequence of suicidal behavior: physical pain serves as a way to drown out inner pain, to switch attention from uncontrollable emotions to those that have become the result of an effort of will. The problem is that self-harm is either carefully hidden by people with BPD because it is not normal in our culture, or they perceive it as controlled behavior (eg, exhausting workouts in the gym, striving to do work tasks in their free time). nine0005
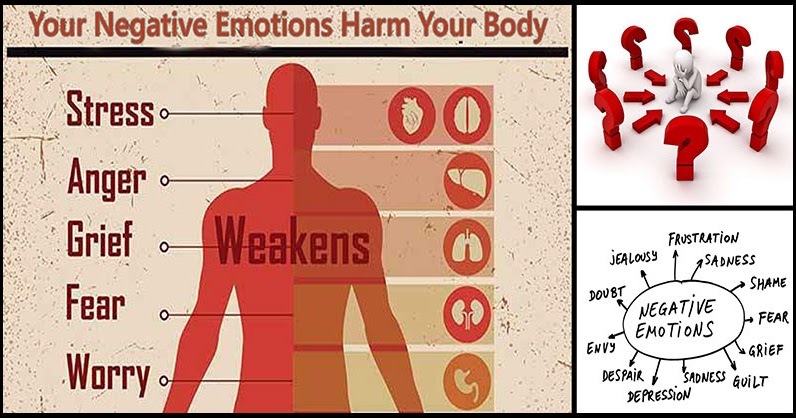
Borderline personality disorder may be accompanied by alcohol, drug, gambling and a number of other diseases. “For example, depression, anxiety disorders, eating disorders are common in people with BPD.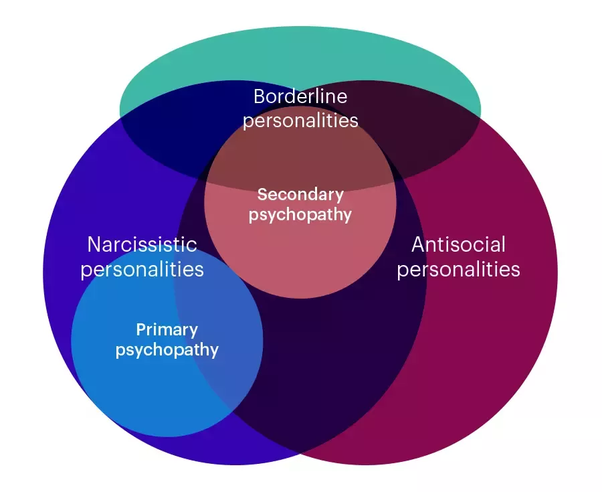 Often, a history of PTSD or CPTSD is found, ”notes Valentin Oskin. That is, constant panic attacks or overeating in the evenings can be a sign of more serious mental disorders than just a reaction to stress.
Often, a history of PTSD or CPTSD is found, ”notes Valentin Oskin. That is, constant panic attacks or overeating in the evenings can be a sign of more serious mental disorders than just a reaction to stress.
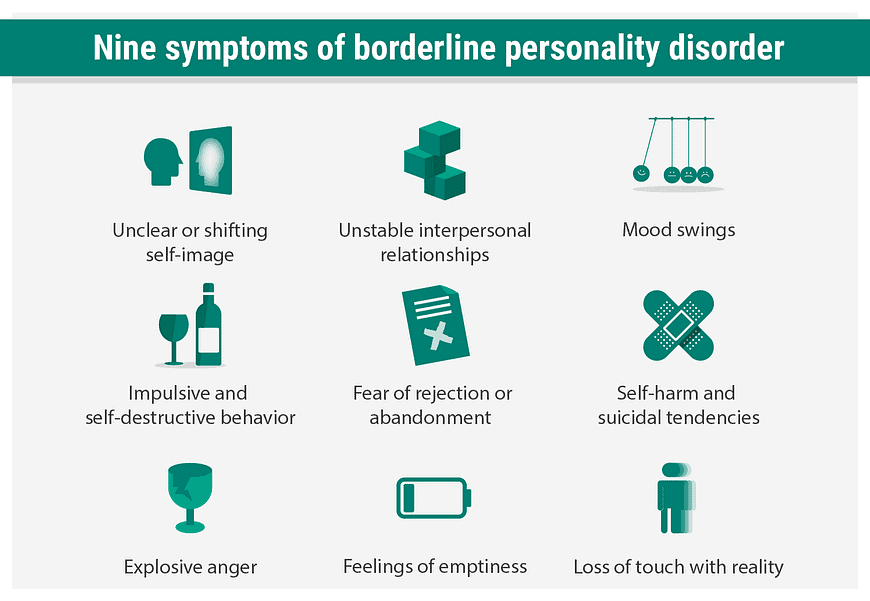
Mind, a British mental health resource, highlights the following symptoms that may indicate borderline personality disorder. If they last long enough and have a negative impact on your life, it makes sense to consult a psychotherapist or psychiatrist:
- Fear of being alone. You constantly worry about people leaving you and are ready to do everything to prevent this from happening.
- Impulsivity and affectivity. You are overcome by strong emotions that last from several hours to several days and can change quickly (for example, from feelings of happiness and confidence to sudden depression and sadness). This is especially evident in a state of anger, which is difficult to control.
 In a state of severe stress, you may also experience paranoia or dissociation (as if everything is not happening to you, but to someone else). nine0034
In a state of severe stress, you may also experience paranoia or dissociation (as if everything is not happening to you, but to someone else). nine0034 - Depersonalization. There is no clear idea of who you really are: the sense of self and behavior changes radically depending on where and with whom you are. As an option - a constant feeling of emptiness inside, boredom, misunderstanding of one's true desires and values.
- Communication problems. It is very difficult for you to create and maintain stable relationships, you are prone to masochistic communication, cyclically idealize and devalue even the closest people, and do not always correctly interpret the motives of the actions of others. nine0034
“Borderline personality disorder can manifest itself in a wide range of signs,” says Valentin Oskin, “the symptoms of borderline personality disorder are most fully described in the DSM-5 and ICD-11 reference books. If grouped together, the symptoms will reflect a lack of control in the emotional, behavioral, cognitive spheres, as well as a distortion of the sense of self and a violation of interpersonal relationships. According to the psychologist, it is extremely difficult for people with BPD to break off relationships, even those that need to be broken off. Instead, they may go to great lengths to keep the people who matter to them around them. nine0005
If grouped together, the symptoms will reflect a lack of control in the emotional, behavioral, cognitive spheres, as well as a distortion of the sense of self and a violation of interpersonal relationships. According to the psychologist, it is extremely difficult for people with BPD to break off relationships, even those that need to be broken off. Instead, they may go to great lengths to keep the people who matter to them around them. nine0005
At the same time, “border guards” tend to involuntarily throw out their emotions on those who are dear to them: “Often this ends with interruption of communication, because not everyone is able to endure such a bolt from the blue. And even more so if this thunder rumbles once every couple of months, ”Ksenia Ivanenko notes in her Telegram channel, where she describes her personal experience in dealing with BPD.
Related material
To determine if you are at risk, you can take several tests for borderline personality disorder that are publicly available. It is important to understand that the result obtained is not a final diagnosis, it can only be made by a qualified doctor after analyzing the symptoms. nine0005
It is important to understand that the result obtained is not a final diagnosis, it can only be made by a qualified doctor after analyzing the symptoms. nine0005
The Root of the Problem: What Causes Borderline Personality Disorder
Effective treatment for most mental illnesses requires the cause to be identified. Borderline personality disorder is problematic in that it arises from a number of factors and affects the basic components of the personality. That is, there is simply no specific reason that triggers the PRL processes. “While BPD is one of the most researched personality disorders, there is no consensus on what exactly causes it. Severe stresses experienced by children and adolescents, such as neglect, prolonged painful separation, loss of a parent, violence, are common in people with BPD. There is also evidence of a genetic predisposition: among first-line relatives of a person with borderline disorder, the likelihood of developing a similar disorder is 3-5 times higher when compared with the general population,” notes Valentin Oskin.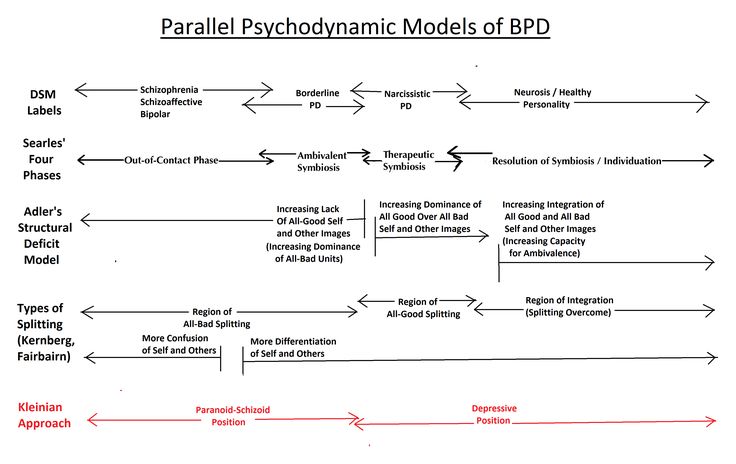 nine0005
nine0005
Any person can be at risk, especially if he is going through a difficult stressful situation. It is known that this diagnosis is made more often in women than in men, and that in almost all cases of BPD it is driven by a deep emotional shock. Most researchers agree that the development of BPD is promoted by a combination of two groups of factors:
- Stress and traumatic life situations. For example, sexual, physical or emotional abuse, persistent feelings of fear or abandonment in childhood, family problems, repressed feelings of anger, anxiety, and sadness. Stress or trauma in adulthood can trigger the onset of borderline personality disorder. nine0034
- Genetic predisposition and environmental influences. The disease can be inherited, but more often borderline occurs as a pattern of behavior unconsciously borrowed from parents or close people, reactions to external stimuli.
Related material
No reason to cut ties
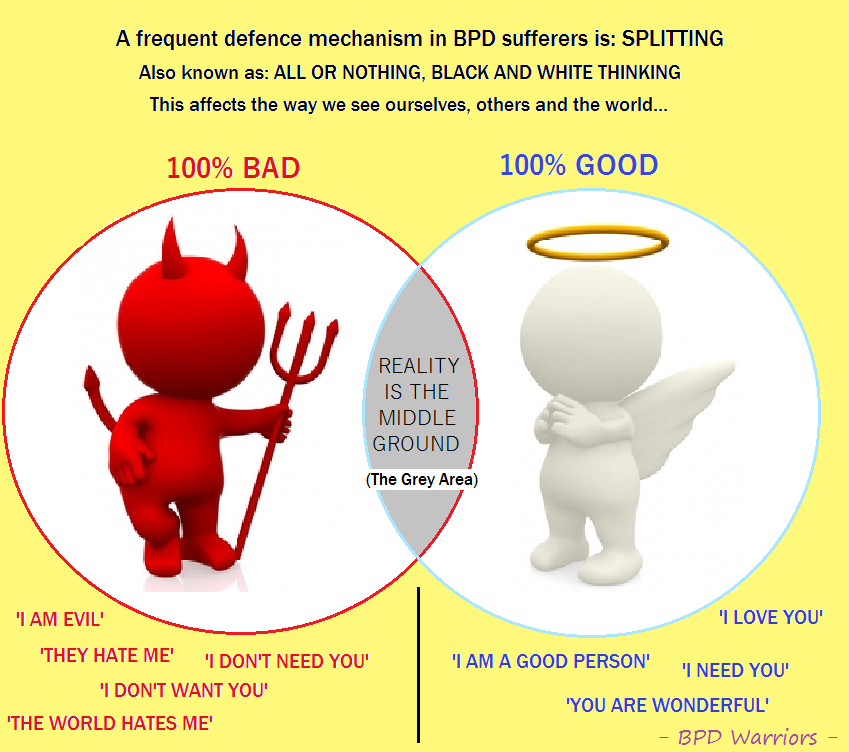
If there is a “border guard” in your environment, you can build constructive communication with him, although this will require a lot of effort. “It is important to understand that a person with borderline personality disorder takes criticism extremely hard, for him it sounds like rejection, which he is terribly afraid of. At the same time, emotional jumps do not allow him to get the desired intimacy. Relations with such a person are usually like a swing between the poles "I love you, don't leave me - I hate you, I'll leave you." It is important to understand that with borderline personality disorder it is impossible to consciously change your behavior, thinking, emotional reactions and response patterns to certain situations, ”says Valentin Oskin. nine0005
Many "border guards" live with a constant oppressive feeling of guilt, they feel broken, bad and unworthy of normal communication, which they badly need. They are unable to correctly read the reactions of others and the motives of their actions. This determines their strange behavior and repels potential partners and friends. Often, people with borderline personality disorder have a Favorite Person - a person on whom the "borderguard" is extremely dependent and who replaces not only everyone around him, but also himself. If this person is busy or there is a conflict with him, the “border guard” literally collapses the world: he drowns in a storm of emotions, reflects on death and looks for thousands of reasons why he was rejected. nine0005
They are unable to correctly read the reactions of others and the motives of their actions. This determines their strange behavior and repels potential partners and friends. Often, people with borderline personality disorder have a Favorite Person - a person on whom the "borderguard" is extremely dependent and who replaces not only everyone around him, but also himself. If this person is busy or there is a conflict with him, the “border guard” literally collapses the world: he drowns in a storm of emotions, reflects on death and looks for thousands of reasons why he was rejected. nine0005
There are a number of rules that psychologists have developed for those who seek to communicate as "border guards", minimizing chaos, conflicts and the possibility of a tragic denouement: could end in disaster.
 nine0034
nine0034 Related material
How to get rid of BPD
The main way to deal with borderline personality disorder is psychotherapy, in which work is done on the accompanying manifestations of an unstable mental state (depression, addictions, eating disorders, etc.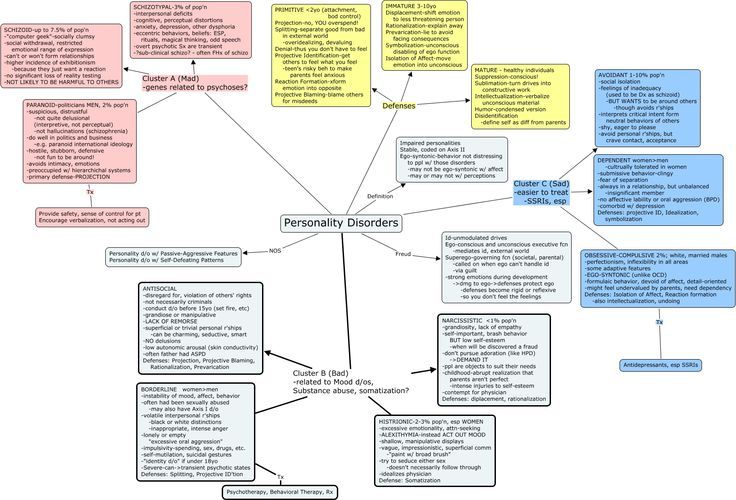 ) and syndromes (it is often necessary to treat alcohol withdrawal symptoms). syndrome). This is a long and complicated process, but statistics show that 70% of the “border guards” get rid of the main symptoms during therapy within six years, and remission occurs in a third of patients after two years. nine0005
) and syndromes (it is often necessary to treat alcohol withdrawal symptoms). syndrome). This is a long and complicated process, but statistics show that 70% of the “border guards” get rid of the main symptoms during therapy within six years, and remission occurs in a third of patients after two years. nine0005
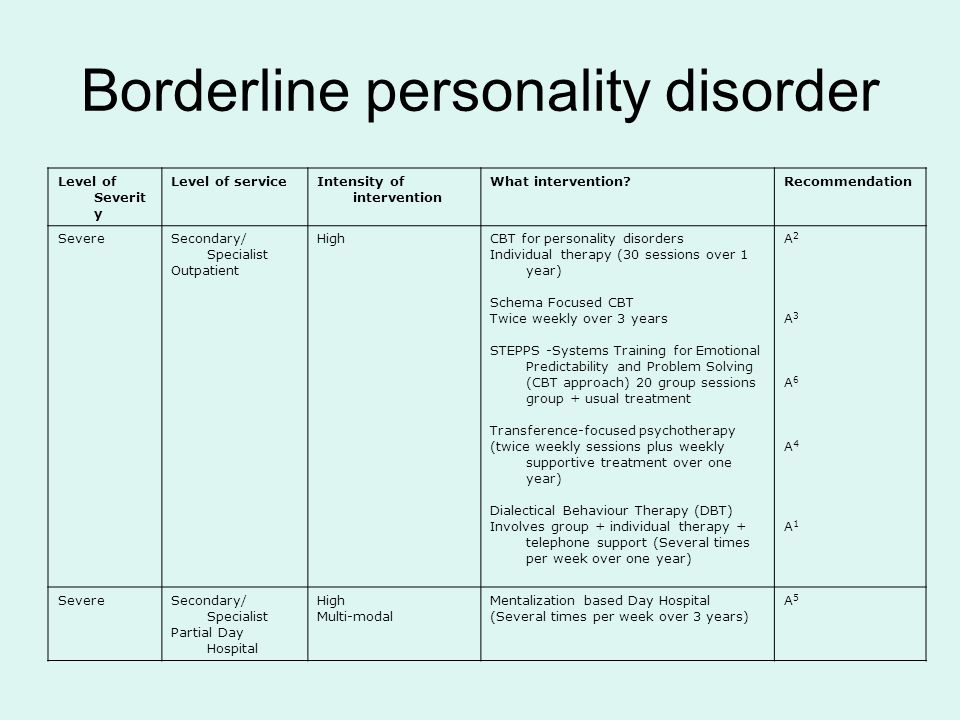
“In therapy, people with BPD are primarily trained in emotional control, responsibility, and interpersonal skills. Dialectico-behavioral psychotherapy, a specially developed method for the treatment of BPD based on cognitive behavioral therapy, is well suited for this. No less effective is schema therapy, which also has special developments for the treatment of BPD. In the course of treatment, pharmacotherapy can also be prescribed, for example, for the treatment of associated depression or anxiety disorder, ”says Valentin Oskin. nine0005
Comprehensive treatment may include the following therapies:
- Dialectical Behavioral Therapy (DBT).
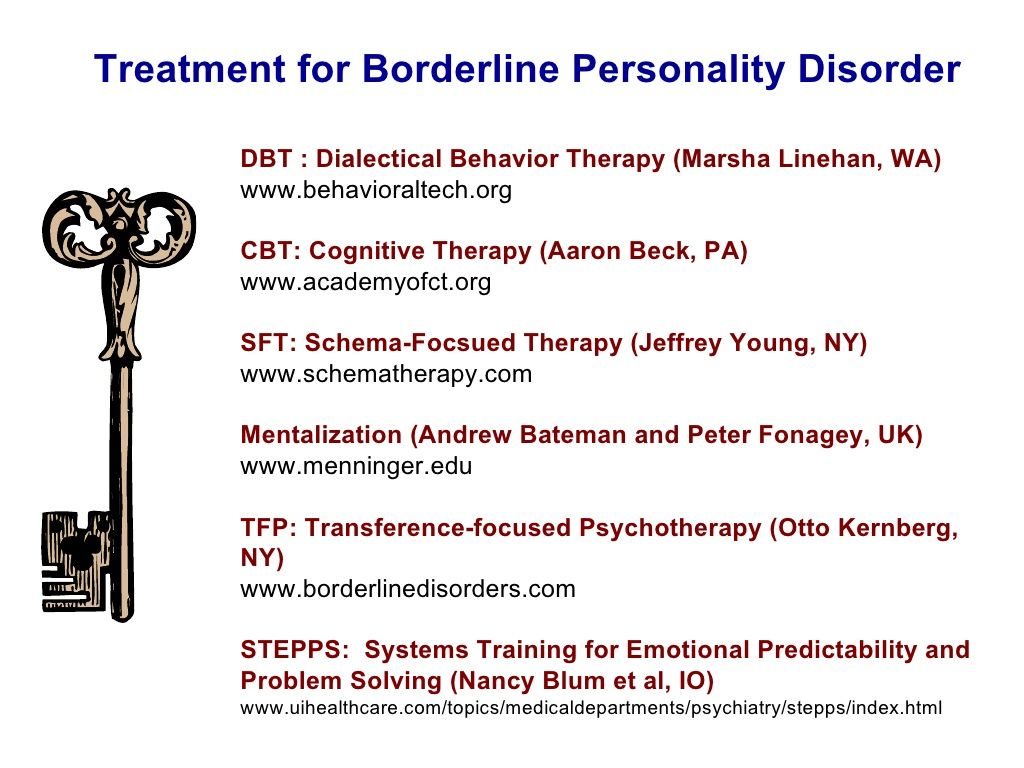 Allows the "border guard" to realize that problems can be viewed from different angles, eliminates black and white thinking.
Allows the "border guard" to realize that problems can be viewed from different angles, eliminates black and white thinking. - Mentalization (MBT). It helps to explain to oneself the behavior of other people, logically argue their motives and work to improve interpersonal interaction.
- Transference Therapy (TFP) teaches to perceive positive and negative qualities at the same time, to get out of the “deification/devaluation” paradigm. nine0034
- Cognitive Behavioral Therapy helps to change the way of thinking, reactions to stress and correct affective patterns of behavior.
- Schematic therapy is a complex treatment based on psychoanalysis and gestalt therapy. It changes the behavioral patterns laid down in childhood or adolescence.
- Self-help. It consists in tracking the dynamics of emotions, asking yourself questions like “how do I feel now?”, “What does he (a) specifically want from me?”, “Is this reality or my fiction?”. nine0034
To improve their inner state, people with BPD are advised to start meditating, exercising, walking more often in the fresh air, trying to rationalize their own mood swings, learning self-soothing techniques and training willpower in order to stop emotional breakdowns in time.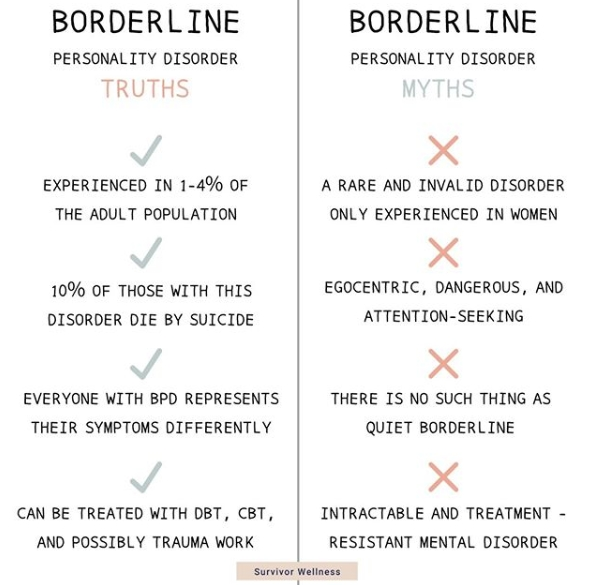
Related material
Borderline personality disorder, symptoms, causes, diagnosis, treatment
Borderline personality disorder (abbreviated as PRL ) - today it is increasingly common among children. The pathogenesis of this type of psychopathy is usually accompanied by a complex of unfavorable factors.
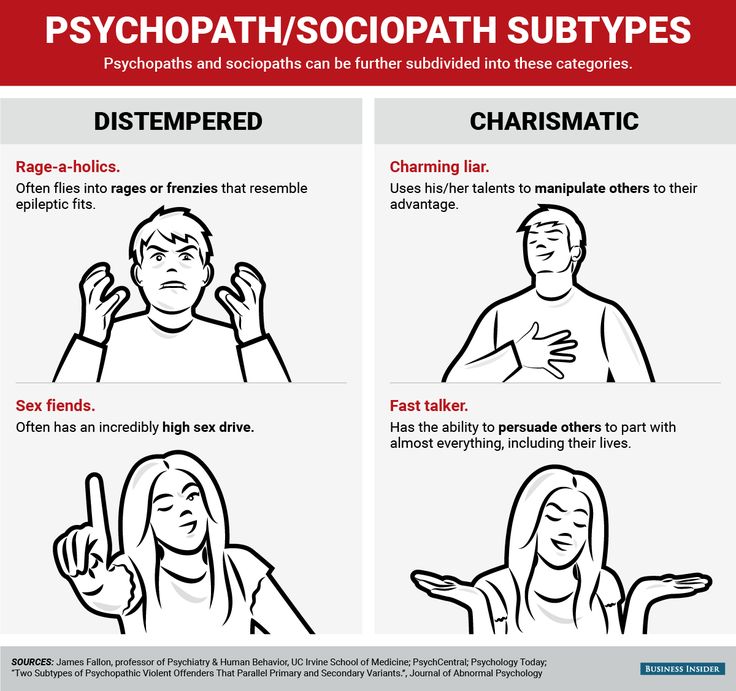
It is quite difficult to recognize this type of disease in everyday life. Often, it is confused with narcissism or simply the bad character of the individual, since the behavior of the "border guards" can be characterized by an extreme degree of unpredictability and hysteria, as well as a tendency to manipulation. For example, they confess their love to a partner, and after a couple of hours they leave “forever”, they can sincerely sympathize with someone, and then hit. It is also very common for patients of this type to constantly violate the boundaries of other people, shifting their problems onto them, and avoiding responsibility. Consider the symptoms of borderline in more detail. nine0005
Consider the symptoms of borderline in more detail. nine0005
Symptoms of borderline personality disorder (BPD)
The main symptomatic difference of this type of disorder is prolonged abnormal behavior of the patient .
While in many other psychopathy periods of instability alternate with remission, in the case of BPD the patient behaves destructively over a long period of time. In the field of psychological anomalies are such manifestations as:
- aggressive behavior leading to problems in relationships,
- unstable emotional background and inadequate self-image,
- high anxiety,
- total fear of loneliness and permanent feeling of boredom,
- dichotomous thinking and changeable mood, dividing the world only into "black and white" (today I love, but tomorrow I hate).
Also among the main symptoms can be noted: sociopathy and fear of society associated with low self-esteem and, as a result, separation anxiety (it is experienced by a person when separated from home or loved ones).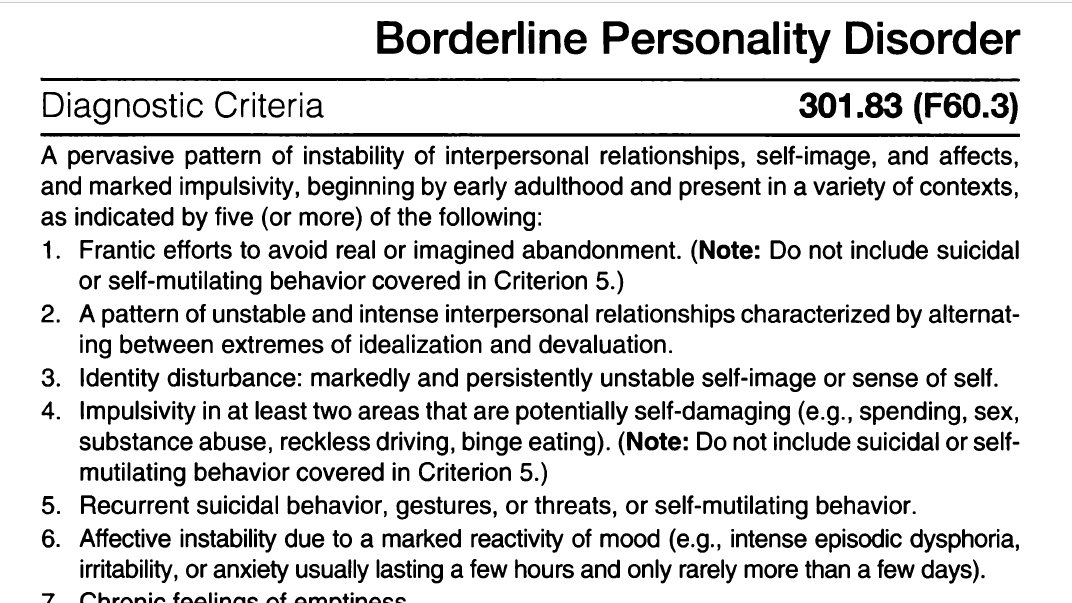 Patients often exhibit reckless irresponsible "risky" behavior, the extreme form of which may be self-harm or suicide attempt. nine0005
Patients often exhibit reckless irresponsible "risky" behavior, the extreme form of which may be self-harm or suicide attempt. nine0005
Types of spontaneous actions that accompany mental borderline personality disorders
Due to difficulties in self-identification, lack of one's own opinion and a tendency to polarity, spontaneous destructive actions are characteristic of BPD sufferers.
Panic fear of loneliness and the lack of an inner core pushes them into contact with sociopathic personalities who are characterized by destructive behavior: gambling, theft, vandalism, promiscuous relationships, drug addiction. This also includes self-harm, which was mentioned above. nine0005
One of the reasons for this uncontrolled behavior is the problem with holding the internal impulse. The level of impulsivity is so high that a person is not able to control it.
Cherednichenko Andrey Nikolaevich
Chief physician of the Korsakov medical centers network, psychiatrist-narcologist
- Experience more than 11 years
Consultation
Record for reception
Emotively unstable personality disorder
in the MKB of the 10 personality disorder is defined as "Emotionally unstable personality disorder (F60.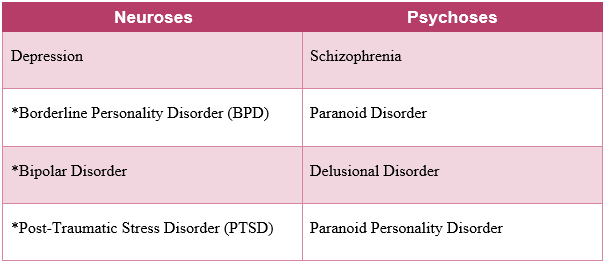 3)". In the clinical community on the territory of the Russian Federation, this name is used quite often and is used due to the fact that the main symptom, as described above, manifests itself in the form of an emotionally unstable mental state of a person. nine0005
3)". In the clinical community on the territory of the Russian Federation, this name is used quite often and is used due to the fact that the main symptom, as described above, manifests itself in the form of an emotionally unstable mental state of a person. nine0005
BPD pathogenesis
In the pathogenesis of the disease lies an incorrectly or incompletely formed intrapersonal self-awareness, in other words, “self-identification”. Border guards hardly realize how they relate to the main areas of life. They have problems with the concept of their opinions, interests, hobbies, and their character as well. Hence the more common definition of the disorder - "borderline". In this aspect, it means maneuvering on the verge between psychopathy and a stable state. The word "borderline" in a particular case means a precarious state between the norm and deviation, as if a person lives on the verge between "mental illness" (psychosis) and "mental health". That is why, the slang name for patients of this type is “borderliners” (from the English expression “border line”, which literally translates as “border”). nine0005
nine0005
In classical psychiatry, borderline personality disorder is also classified as a type of ego syntonic disorder. Ego syntonicity implies that the patient does not assess his condition as painful, is not critical of him and calmly accepts deviations in behavior, not believing that they harm him in any way. Moreover, the patient, as it were, “defends” his symptom, preventing his own cure due to the difficulty in identifying his own “I”.
Causes of BPD
The underlying causes of BPD are currently not clearly defined, however, like most other disorders, BPD is caused by a group of factors. nine0005
Hereditary (genetic determinism), physiological (disturbances in the brain) and social factors (low stress resistance and psychological traumatic factor).
Unfavorable social environment
According to statistics, groups of people exposed to an unfavorable social environment, for example, in the family, are more susceptible to the disease. These include:
- difficult childhood,
- abuse, nine0033 tyranny,
It is worth noting that "borderliness" occurs 3 times more often among women than among men.
Post-traumatic stress disorder (PTSD) , as a variation of an unfavorable social factor, can act not only as a cause, but also as a concomitant individual disease that is in a pathogenetic relationship with the diagnosis in question. nine0005
Childhood chronic emotional trauma may contribute to the development of BPD, but in rare cases it is the only cause. Personal qualities that are responsible for the ability to cope with a stressful situation in this aspect also play a big role. Here it is worth noting that, according to statistics, an injury received in childhood (especially before the age of 10) can lead to a subsequent disorder much more likely than an injury received at an older age. Also, scientists note that situations not associated with direct violence, such as natural disasters or catastrophes, are less likely to lead to the development of post-traumatic syndrome. nine0005
nine0005
Physiology
Another group of factors considers a possible cause of the development of the disease - disorders in the work of neural brain connections, namely the destruction of the functioning of the frontal-limbic neurons
Heredity
diagnosis. It is quite difficult to achieve clear indicators in this vein, however, according to European studies, BPD is located in 3rd place out of 10 in terms of the genetic determinant among personality disorders. It is logical to note that deviations in the work of certain parts of the brain can be inherited and lead to a number of psychological problems, the development of which is aggravated by the social factor. Most studies show that most often borderlineness is transmitted from the mother. nine0005
Borderline mental state in psychiatry and severity of personality disorders
In clinical psychiatry, three levels of mental disorder are traditionally distinguished:
- Neurotic .
 These include neuroses of a different nature, implying reversible temporary conditions that can be treated.
These include neuroses of a different nature, implying reversible temporary conditions that can be treated. - Psychopathic level . In its plane lie personality disorders, which include anomalies in the nature of various pathogenesis or painful changes in its features, with which nothing can be done, since they relate to the personality structure of the individual. nine0034
- And finally, the deepest lesion of the psyche manifests itself at the psychotic level . This includes such manifestations as delirium, hallucinations, twilight consciousness.
Modern psychoanalysis distinguishes 4 levels of deviations. Between the state of psychosis and neurosis, it is conditionally located just “ borderline level”, also called borderline state . A borderline state can mean both the disorder itself and the designation of the level of mental damage. nine0005
How to reliably identify borderline personality disorder (BPD)
Borderline personality disorder is extremely difficult to diagnose and differentiate, as it has a high level of comorbidity, in other words, it is combined with a large number of concomitant disorders. For example, panic anxiety, eating disorders, bipolar affective disorder, attention deficit disorder, sociopathy, and so on. In connection with the above, the patient has to undergo a long diagnostic process and special tests. nine0005
For example, panic anxiety, eating disorders, bipolar affective disorder, attention deficit disorder, sociopathy, and so on. In connection with the above, the patient has to undergo a long diagnostic process and special tests. nine0005
Borderline personality disorder BPD test
One of the fairly popular tools for detecting the presence of psychopathy are tests, which are, in fact, a personality questionnaire. Used in modern clinical psychology, a test for screening for the bright signs of BPD was developed in 2012 by a group of scientists. In their work, the authors relied on the basic criteria for differentiating borderline disorder.
The questionnaire edited by them is a fairly effective tool for diagnostic verification and confirmation of symptoms. It is used both in psychiatric and general clinical, and in other practices that are not directly related to medicine. nine0005
The test itself consists of 20 questions and asks the subject to answer only yes or no.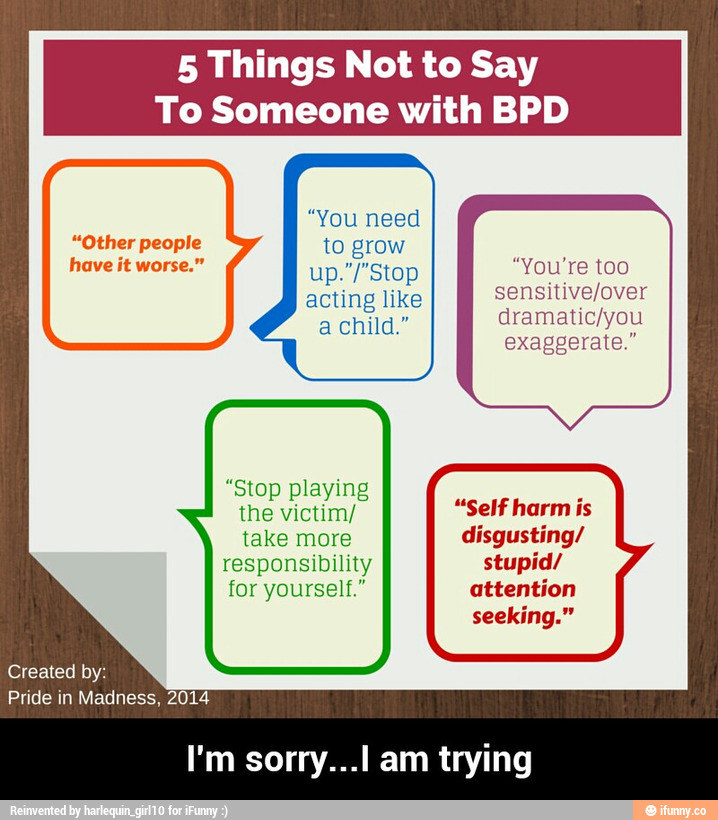 For each answer, the system counts a certain number of points. The probability of diagnosing BPD appears if the respondent scored more than 25 points.
For each answer, the system counts a certain number of points. The probability of diagnosing BPD appears if the respondent scored more than 25 points.
Treatment of borderline personality disorder (BPD)
Cherednichenko Andrey Nikolaevich
Head physician of the network of medical centers "Korsakov", psychiatrist-narcologist
- Experience over 11 years
Consultation
Appointment
Like most other mental disorders, borderline disorder is not treated at home and requires complex occupational therapy, including both medication (taking antidepressants and antipsychotics) and psychotherapy. And only a psychiatrist, often in tandem with a clinical psychologist, can competently develop an effective course of treatment.
The drug course is developed in accordance with the individual characteristics of the patient's body and includes the following drug groups:
- Selective inhibitors of are aimed at preventing depressive episodes and reducing anxiety/panic/borderline states.
- Mood stabilizers .
One of the most popular remedies is Lamotrigine. It is also used to neutralize depression, mood lability and impulsivity.
- Atypical antipsychotics .
Now the 2nd generation of drugs of this cluster has already been developed, which have proven themselves in neutralizing the symptoms of the cognitive sphere, such as: aggression, distortion of the perception of reality, paranoia, thought dichotomy and disorganization. nine0005
As for the group of benzodiazepines and stimulants, they are used in modern therapy extremely rarely due to the high risk of dependence and, accordingly, overdose.
Thus, the main task of drug therapy in borderline personality disorder is to reduce the severity of symptoms and alleviate the general condition of the patient.
It is worth noting that BPD is the most difficult to treat due to the patient's ego syntony, which we discussed above.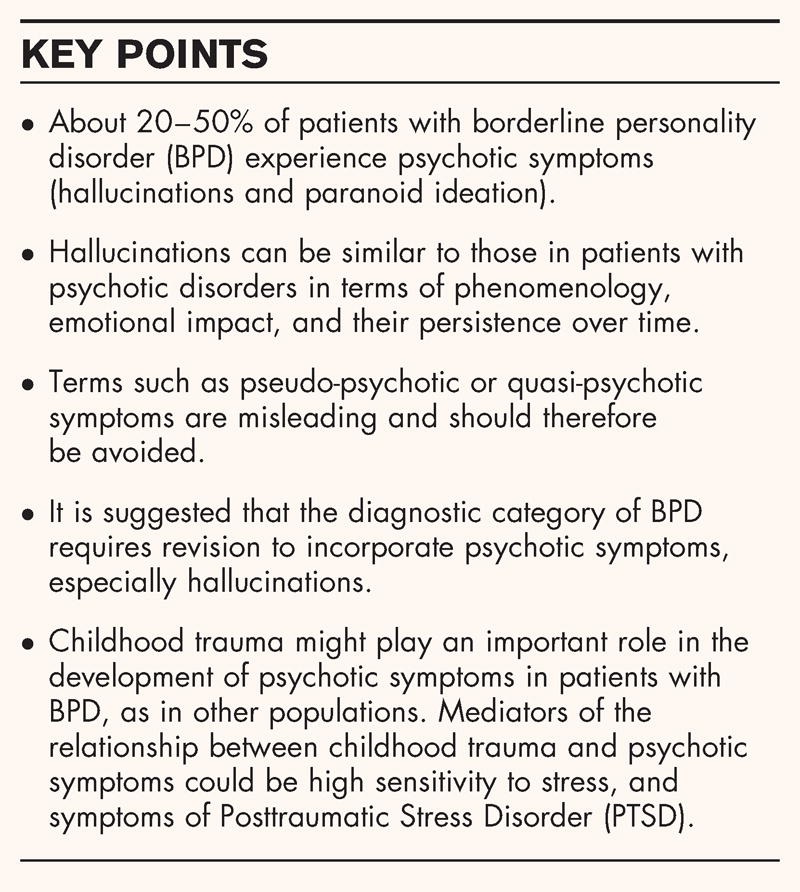 It is the patient with BPD who is the most difficult to respond to any therapy due to the rigidity of the psyche and the clear conviction that everything is generally normal with them. nine0005
It is the patient with BPD who is the most difficult to respond to any therapy due to the rigidity of the psyche and the clear conviction that everything is generally normal with them. nine0005
However, when it comes to Selective Inhibitors, Dialectical Behavioral Therapy (DBT), one of the varieties of Cognitive Behavioral Therapy (CBT), is considered the most effective method in the modern clinical community. As part of the treatment, the patient is taught to look at the problem from different points of view and evaluate the causal relationship in different ways. Due to satisfaction with their symptoms and rigidity, "border guards" are difficult to treat, so the psychotherapeutic process can be lengthy. nine0005
Most often, relatives suffer the most from relationships with patients with BPD, so another parameter that the specialist works on is the patient's socialization and adaptation, aimed at developing fundamental life skills and developing an adequate behavior for the situation.