Best treatments for borderline personality disorder
Borderline personality disorder - Diagnosis and treatment
Diagnosis
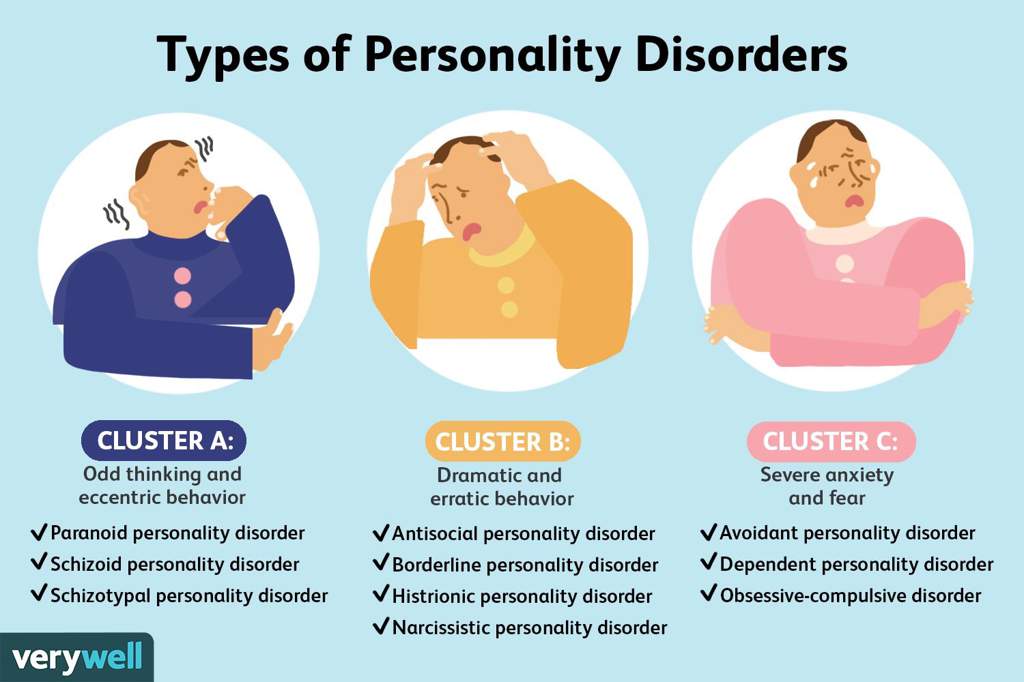
Personality disorders, including borderline personality disorder, are diagnosed based on a:
- Detailed interview with your doctor or mental health provider
- Psychological evaluation that may include completing questionnaires
- Medical history and exam
- Discussion of your signs and symptoms
A diagnosis of borderline personality disorder is usually made in adults, not in children or teenagers. That's because what appear to be signs and symptoms of borderline personality disorder may go away as children get older and become more mature.
Treatment
Borderline personality disorder is mainly treated using psychotherapy, but medication may be added. Your doctor also may recommend hospitalization if your safety is at risk.
Treatment can help you learn skills to manage and cope with your condition. It's also necessary to get treated for any other mental health disorders that often occur along with borderline personality disorder, such as depression or substance misuse. With treatment, you can feel better about yourself and live a more stable, rewarding life.
Psychotherapy
Psychotherapy — also called talk therapy — is a fundamental treatment approach for borderline personality disorder. Your therapist may adapt the type of therapy to best meet your needs. The goals of psychotherapy are to help you:
- Focus on your current ability to function
- Learn to manage emotions that feel uncomfortable
- Reduce your impulsiveness by helping you observe feelings rather than acting on them
- Work on improving relationships by being aware of your feelings and those of others
- Learn about borderline personality disorder
Types of psychotherapy that have been found to be effective include:
- Dialectical behavior therapy (DBT). DBT includes group and individual therapy designed specifically to treat borderline personality disorder. DBT uses a skills-based approach to teach you how to manage your emotions, tolerate distress and improve relationships.
- Schema-focused therapy. Schema-focused therapy can be done individually or in a group. It can help you identify unmet needs that have led to negative life patterns, which at some time may have been helpful for survival, but as an adult are hurtful in many areas of your life. Therapy focuses on helping you get your needs met in a healthy manner to promote positive life patterns.
- Mentalization-based therapy (MBT). MBT is a type of talk therapy that helps you identify your own thoughts and feelings at any given moment and create an alternate perspective on the situation. MBT emphasizes thinking before reacting.
- Systems training for emotional predictability and problem-solving (STEPPS). STEPPS is a 20-week treatment that involves working in groups that incorporate your family members, caregivers, friends or significant others into treatment. STEPPS is used in addition to other types of psychotherapy.
- Transference-focused psychotherapy (TFP).
 Also called psychodynamic psychotherapy, TFP aims to help you understand your emotions and interpersonal difficulties through the developing relationship between you and your therapist. You then apply these insights to ongoing situations.
Also called psychodynamic psychotherapy, TFP aims to help you understand your emotions and interpersonal difficulties through the developing relationship between you and your therapist. You then apply these insights to ongoing situations. - Good psychiatric management. This treatment approach relies on case management, anchoring treatment in an expectation of work or school participation. It focuses on making sense of emotionally difficult moments by considering the interpersonal context for feelings. It may integrate medications, groups, family education and individual therapy.
Medications
Although no drugs have been approved by the Food and Drug Administration specifically for the treatment of borderline personality disorder, certain medications may help with symptoms or co-occurring problems such as depression, impulsiveness, aggression or anxiety. Medications may include antidepressants, antipsychotics or mood-stabilizing drugs.
Talk to your doctor about the benefits and side effects of medications.
Hospitalization
At times, you may need more-intense treatment in a psychiatric hospital or clinic. Hospitalization may also keep you safe from self-injury or address suicidal thoughts or behaviors.
Recovery takes time
Learning to manage your emotions, thoughts and behaviors takes time. Most people improve considerably, but you may always struggle with some symptoms of borderline personality disorder. You may experience times when your symptoms are better or worse. But treatment can improve your ability to function and help you feel better about yourself.
You have the best chance for success when you consult a mental health provider who has experience treating borderline personality disorder.
More Information
- Psychotherapy
Request an appointment
From Mayo Clinic to your inbox
Sign up for free, and stay up to date on research advancements, health tips and current health topics, like COVID-19, plus expertise on managing health. Click here for an email preview.
Click here for an email preview.
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Coping and support
Symptoms associated with borderline personality disorder can be stressful and challenging for you and those around you.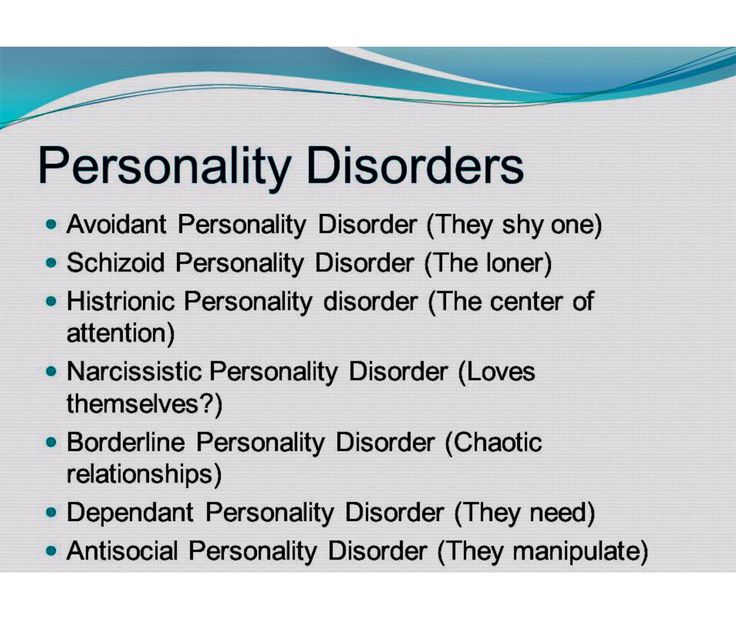 You may be aware that your emotions, thoughts and behaviors are self-destructive or damaging, yet you feel unable to manage them.
You may be aware that your emotions, thoughts and behaviors are self-destructive or damaging, yet you feel unable to manage them.
In addition to getting professional treatment, you can help manage and cope with your condition if you:
- Learn about the disorder so that you understand its causes and treatments
- Learn to recognize what may trigger angry outbursts or impulsive behavior
- Seek professional help and stick to your treatment plan — attend all therapy sessions and take medications as directed
- Work with your mental health provider to develop a plan for what to do the next time a crisis occurs
- Get treatment for related problems, such as substance misuse
- Consider involving people close to you in your treatment to help them understand and support you
- Manage intense emotions by practicing coping skills, such as the use of breathing techniques and mindfulness meditation
- Set limits and boundaries for yourself and others by learning how to appropriately express emotions in a manner that doesn't push others away or trigger abandonment or instability
- Don't make assumptions about what people are feeling or thinking about you
- Reach out to others with the disorder to share insights and experiences
- Build a support system of people who can understand and respect you
- Keep up a healthy lifestyle, such as eating a healthy diet, being physically active and engaging in social activities
- Don't blame yourself for the disorder, but recognize your responsibility to get it treated
Preparing for your appointment
You may start by seeing your primary care doctor. After an initial appointment, your doctor may refer you to a mental health provider, such as a psychologist or psychiatrist. Here's some information to help you prepare for your appointment.
After an initial appointment, your doctor may refer you to a mental health provider, such as a psychologist or psychiatrist. Here's some information to help you prepare for your appointment.
What you can do
Before your appointment, make a list of:
- Any symptoms you or people close to you have noticed, and for how long
- Key personal information, including traumatic events in your past and any current major stressors
- Your medical information, including other physical or mental health conditions
- All medications you take, including prescription and over-the-counter medications, vitamins and other supplements, and the doses
- Questions you want to ask your doctor so that you can make the most of your appointment
Take a family member or friend along, if possible. Someone who has known you for a long time may be able to share important information with the doctor or mental health provider, with your permission.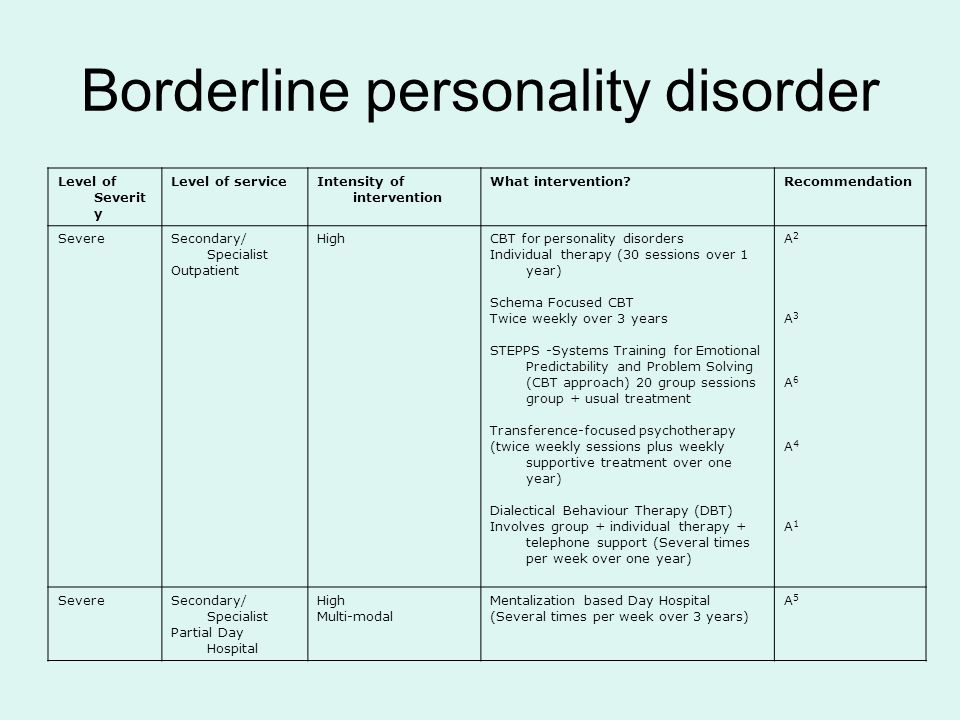
Basic questions to ask your doctor or a mental health provider include:
- What's likely causing my symptoms or condition?
- Are there any other possible causes?
- What treatments are most likely to be effective for me?
- How much can I expect my symptoms to improve with treatment?
- How often will I need therapy sessions and for how long?
- Are there medications that can help?
- What are the possible side effects of the medication you may prescribe?
- Do I need to take any precautions or follow any restrictions?
- I have these other health conditions. How can I best manage them together?
- How can my family or close friends help me in my treatment?
- Do you have any printed material that I can take? What websites do you recommend?
Don't hesitate to ask questions during your appointment.
What to expect from your doctor
A doctor or mental health provider is likely to ask you a number of questions. Be ready to answer them to save time for topics you want to focus on. Possible questions include:
Be ready to answer them to save time for topics you want to focus on. Possible questions include:
- What are your symptoms? When did you first notice them?
- How are these symptoms affecting your life, including your personal relationships and work?
- How often during the course of a normal day do you experience a mood swing?
- How often have you felt betrayed, victimized or abandoned? Why do you think that happened?
- How well do you manage anger?
- How well do you manage being alone?
- How would you describe your sense of self-worth?
- Have you ever felt you were bad, or even evil?
- Have you had any problems with self-destructive or risky behavior?
- Have you ever thought of or tried to harm yourself or attempted suicide?
- Do you use alcohol or recreational drugs or misuse prescription drugs? If so, how often?
- How would you describe your childhood, including your relationship with your parents or caregivers?
- Were you physically or sexually abused or were you neglected as a child?
- Have any of your close relatives or caregivers been diagnosed with a mental health problem, such as a personality disorder?
- Have you been treated for any other mental health problems? If yes, what diagnoses were made, and what treatments were most effective?
- Are you currently being treated for any other medical conditions?
By Mayo Clinic Staff
Related
Associated Procedures
Products & Services
What Works in the Treatment of Borderline Personality Disorder
1. Bateman A, Fonagy P. Effectiveness of partial hospitalization in the treatment of borderline personality disorder: a randomized controlled trial. American journal of Psychiatry. 1999. [PubMed]
Bateman A, Fonagy P. Effectiveness of partial hospitalization in the treatment of borderline personality disorder: a randomized controlled trial. American journal of Psychiatry. 1999. [PubMed]
2. Giesen-Bloo J, Van Dyck R, Spinhoven P, Van Tilburg W, Dirksen C, Van Asselt T, et al. Outpatient psychotherapy for borderline personality disorder: randomized trial of schema-focused therapy vs transference-focused psychotherapy. Arch Gen Psychiatry. 2006;63(6):649–658. doi: 10.1001/archpsyc.63.6.649. [PubMed] [CrossRef] [Google Scholar]
3. Clarkin JF, Levy KN, Lenzenweger MF, Kernberg OF. Evaluating three treatments for borderline personality disorder: a multiwave study. American Journal of Psychiatry. 2007. [PubMed]
4. Blum N, St. John D, Pfohl B, Stuart S, McCormick B, Allen J, et al. Systems Training for Emotional Predictability and Problem Solving (STEPPS) for outpatients with borderline personality disorder: a randomized controlled trial and 1-year follow-up. Am J Psychiatr. 2008;165(4):468–478. doi: 10.1176/appi.ajp.2007.07071079. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
2008;165(4):468–478. doi: 10.1176/appi.ajp.2007.07071079. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
5. Stoffers JM, Völlm BA, Rücker G, Timmer A, Huband N, Lieb K. Psychological therapies for people with borderline personality disorder. The Cochrane Library. 2012. [PMC free article] [PubMed]
6. Ingenhoven T. Pharmacotherapy for borderline patients: business as usual or by default? The Journal of clinical psychiatry. 2015;76(4):522–523. doi: 10.4088/JCP.14com09522. [PubMed] [CrossRef] [Google Scholar]
7. Lieb K, Völlm B, Rücker G, Timmer A, Stoffers JM. Pharmacotherapy for borderline personality disorder: Cochrane systematic review of randomised trials. Br J Psychiatry. 2010;196(1):4–12. doi: 10.1192/bjp.bp.108.062984. [PubMed] [CrossRef] [Google Scholar]
8. • Gunderson JG, Links PS. Handbook of good psychiatric management for borderline personality disorder. American Psychiatric Pub; 2014. This is a practical handbook of how to employ a generalist model of BPD care.
9. Koons CR, Robins CJ, Tweed JL, Lynch TR, Gonzalez AM, Morse JQ, et al. Efficacy of dialectical behavior therapy in women veterans with borderline personality disorder. Behav Ther. 2001;32(2):371–390. doi: 10.1016/S0005-7894(01)80009-5. [CrossRef] [Google Scholar]
10. Linehan MM, Tutek DA, Heard HL, Armstrong HE. Interpersonal outcome of cognitive behavioral treatment for chronically suicidal borderline patients. Am J Psychiatry. 1994;151(12):1771–1776. doi: 10.1176/ajp.151.12.1771. [PubMed] [CrossRef] [Google Scholar]
11. Linehan MM, Armstrong HE, Suarez A, Allmon D, Heard HL. Cognitive-behavioral treatment of chronically parasuicidal borderline patients. Arch Gen Psychiatry. 1991;48(12):1060–1064. doi: 10.1001/archpsyc.1991.01810360024003. [PubMed] [CrossRef] [Google Scholar]
12. Carter GL, Willcox CH, Lewin TJ, Conrad AM, Bendit N. Hunter DBT project: randomized controlled trial of dialectical behaviour therapy in women with borderline personality disorder. Aust N Z J Psychiatry. 2010;44(2):162–173. doi: 10.3109/00048670903393621. [PubMed] [CrossRef] [Google Scholar]
Aust N Z J Psychiatry. 2010;44(2):162–173. doi: 10.3109/00048670903393621. [PubMed] [CrossRef] [Google Scholar]
13. Priebe S, Bhatti N, Barnicot K, Bremner S, Gaglia A, Katsakou C, et al. Effectiveness and cost-effectiveness of dialectical behaviour therapy for self-harming patients with personality disorder: a pragmatic randomised controlled trial. Psychother Psychosom. 2012;81(6):356–365. doi: 10.1159/000338897. [PubMed] [CrossRef] [Google Scholar]
14. Steil R, Krüger A, Dyer A, Priebe K, Feldmann RE, Jr, Bohus M. DBT-PTSD. Trauma und Gewalt. 2010;4(2):106–117. [Google Scholar]
15. Bohus M, Dyer AS, Priebe K, Krüger A, Kleindienst N, Schmahl C, et al. Dialectical behaviour therapy for post-traumatic stress disorder after childhood sexual abuse in patients with and without borderline personality disorder: a randomised controlled trial. Psychother Psychosom. 2013;82(4):221–233. doi: 10.1159/000348451. [PubMed] [CrossRef] [Google Scholar]
16. Rossouw TI, Fonagy P. Mentalization-based treatment for self-harm in adolescents: a randomized controlled trial. Journal of the American Academy of Child & Adolescent Psychiatry. 2012;51(12):1304–1313. doi: 10.1016/j.jaac.2012.09.018. [PubMed] [CrossRef] [Google Scholar]
Mentalization-based treatment for self-harm in adolescents: a randomized controlled trial. Journal of the American Academy of Child & Adolescent Psychiatry. 2012;51(12):1304–1313. doi: 10.1016/j.jaac.2012.09.018. [PubMed] [CrossRef] [Google Scholar]
17. Davidson K, Norrie J, Tyrer P, Gumley A, Tata P, Murray H, et al. The effectiveness of cognitive behavior therapy for borderline personality disorder: results from the borderline personality disorder study of cognitive therapy (BOSCOT) trial. J Personal Disord. 2006;20(5):450. doi: 10.1521/pedi.2006.20.5.450. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
18. Weinberg I, Gunderson JG, Hennen J, Cutter CJ., Jr Manual assisted cognitive treatment for deliberate self-harm in borderline personality disorder patients. J Personal Disord. 2006;20(5):482–492. doi: 10.1521/pedi.2006.20.5.482. [PubMed] [CrossRef] [Google Scholar]
19. Bos EH, van Wel EB, Appelo MT, Verbraak MJ. A randomized controlled trial of a Dutch version of systems training for emotional predictability and problem solving for borderline personality disorder. J Nerv Ment Dis. 2010;198(4):299–304. doi: 10.1097/NMD.0b013e3181d619cf. [PubMed] [CrossRef] [Google Scholar]
J Nerv Ment Dis. 2010;198(4):299–304. doi: 10.1097/NMD.0b013e3181d619cf. [PubMed] [CrossRef] [Google Scholar]
20. Gregory RJ, Chlebowski S, Kang D, Remen AL, Soderberg MG, Stepkovitch J, et al. A controlled trial of psychodynamic psychotherapy for co-occurring borderline personality disorder and alcohol use disorder. Psychother Theory Res Pract Train. 2008;45(1):28. doi: 10.1037/0033-3204.45.1.28. [PubMed] [CrossRef] [Google Scholar]
21. Linehan MM, Comtois KA, Murray AM, Brown MZ, Gallop RJ, Heard HL, et al. Two-year randomized controlled trial and follow-up of dialectical behavior therapy vs therapy by experts for suicidal behaviors and borderline personality disorder. Arch Gen Psychiatry. 2006;63(7):757–766. doi: 10.1001/archpsyc.63.7.757. [PubMed] [CrossRef] [Google Scholar]
22. Doering S, Hörz S, Rentrop M, Fischer-Kern M, Schuster P, Benecke C, et al. Transference-focused psychotherapy v. treatment by community psychotherapists for borderline personality disorder: randomised controlled trial. Br J Psychiatry. 2010;196(5):389–395. doi: 10.1192/bjp.bp.109.070177. [PubMed] [CrossRef] [Google Scholar]
Br J Psychiatry. 2010;196(5):389–395. doi: 10.1192/bjp.bp.109.070177. [PubMed] [CrossRef] [Google Scholar]
23. Sachdeva S, Goldman G, Mustata G, Deranja E, Gregory RJ. Naturalistic outcomes of evidence-based therapies for borderline personality disorder at a university clinic a quasi-randomized trial. J Am Psychoanal Assoc. 2013;61(3):578–584. doi: 10.1177/0003065113490637. [PubMed] [CrossRef] [Google Scholar]
24. McMain SF, Links PS, Gnam WH, Guimond T, Cardish RJ, Korman L et al. A randomized trial of dialectical behavior therapy versus general psychiatric management for borderline personality disorder. American Journal of Psychiatry. 2009. [PubMed]
25. Bateman A, Fonagy P. Randomized controlled trial of outpatient mentalization-based treatment versus structured clinical management for borderline personality disorder. American Journal of Psychiatry. 2009. [PubMed]
26. Jørgensen CR, Freund C, Bøye R, Jordet H, Andersen D, Kjølbye M. Outcome of mentalization-based and supportive psychotherapy in patients with borderline personality disorder: a randomized trial. Acta Psychiatr Scand. 2013;127(4):305–317. doi: 10.1111/j.1600-0447.2012.01923.x. [PubMed] [CrossRef] [Google Scholar]
Acta Psychiatr Scand. 2013;127(4):305–317. doi: 10.1111/j.1600-0447.2012.01923.x. [PubMed] [CrossRef] [Google Scholar]
27. Gabbard GO. Do all roads lead to Rome? New findings on borderline personality disorder. Am J Psychiatr. 2007;164(6):853–855. doi: 10.1176/ajp.2007.164.6.853. [PubMed] [CrossRef] [Google Scholar]
28. Bateman AW, Krawitz R. Borderline personality disorder: an evidence-based guide for generalist mental health professionals. Oxford, United Kingdom: Oxford University Press; 2016.
29. Choi-Kain LW, Albert EB, Gunderson JG. Evidence-based treatments for borderline personality disorder: implementation, integration, and stepped care. Harvard Review of Psychiatry. 2016;24(5):342–356. doi: 10.1097/HRP.0000000000000113. [PubMed] [CrossRef] [Google Scholar]
30. Linehan MM, Korslund KE, Harned MS, Gallop RJ, Lungu A, Neacsiu AD, et al. Dialectical behavior therapy for high suicide risk in individuals with borderline personality disorder: a randomized clinical trial and component analysis. JAMA psychiatry. 2015;72(5):475–482. doi: 10.1001/jamapsychiatry.2014.3039. [PubMed] [CrossRef] [Google Scholar]
JAMA psychiatry. 2015;72(5):475–482. doi: 10.1001/jamapsychiatry.2014.3039. [PubMed] [CrossRef] [Google Scholar]
31. Farrell JM, Shaw IA, Webber MA. A schema-focused approach to group psychotherapy for outpatients with borderline personality disorder: a randomized controlled trial. J Behav Ther Exp Psychiatry. 2009;40(2):317–328. doi: 10.1016/j.jbtep.2009.01.002. [PubMed] [CrossRef] [Google Scholar]
32. Pennay A, Cameron J, Reichert T, Strickland H, Lee NK, Hall K, et al. A systematic review of interventions for co-occurring substance use disorder and borderline personality disorder. J Subst Abus Treat. 2011;41(4):363–373. doi: 10.1016/j.jsat.2011.05.004. [PubMed] [CrossRef] [Google Scholar]
33. Kröger C, Schweiger U, Sipos V, Kliem S, Arnold R, Schunert T, et al. Dialectical behaviour therapy and an added cognitive behavioural treatment module for eating disorders in women with borderline personality disorder and anorexia nervosa or bulimia nervosa who failed to respond to previous treatments: an open trial with a 15-month follow-up. J Behav Ther Exp Psychiatry. 2010;41(4):381–388. doi: 10.1016/j.jbtep.2010.04.001. [PubMed] [CrossRef] [Google Scholar]
J Behav Ther Exp Psychiatry. 2010;41(4):381–388. doi: 10.1016/j.jbtep.2010.04.001. [PubMed] [CrossRef] [Google Scholar]
34. Barnicot K, Priebe S. Post-traumatic stress disorder and the outcome of dialectical behaviour therapy for borderline personality disorder. Personal Ment Health. 2013;7(3):181–190. doi: 10.1002/pmh.1227. [PubMed] [CrossRef] [Google Scholar]
35. Harned MS, Chapman AL, Dexter-Mazza ET, Murray A, Comtois KA, Linehan MM. Treating co-occurring Axis I disorders in recurrently suicidal women with borderline personality disorder: a 2-year randomized trial of dialectical behavior therapy versus community treatment by experts. J Consult Clin Psychol. 2008;76(6):1068–1075. doi: 10.1037/a0014044. [PubMed] [CrossRef] [Google Scholar]
36. Harned MS, Korslund KE, Linehan MM. A pilot randomized controlled trial of Dialectical Behavior Therapy with and without the Dialectical Behavior Therapy Prolonged Exposure protocol for suicidal and self-injuring women with borderline personality disorder and PTSD.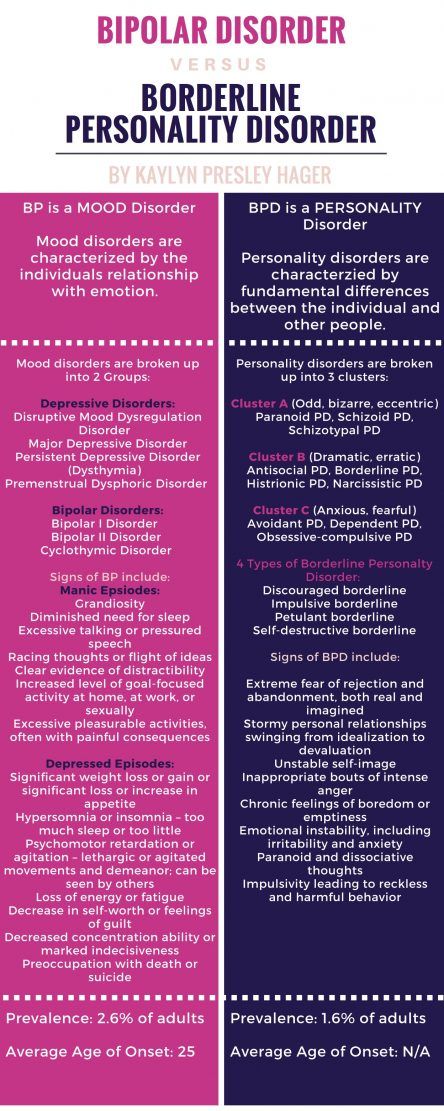 Behav Res Ther. 2014;55:7–17. doi: 10.1016/j.brat.2014.01.008. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
Behav Res Ther. 2014;55:7–17. doi: 10.1016/j.brat.2014.01.008. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
37. Robinson P, Barrett B, Bateman A, Hakeem A, Hellier J, Lemonsky F, et al. Study protocol for a randomized controlled trial of mentalization based therapy against specialist supportive clinical management in patients with both eating disorders and symptoms of borderline personality disorder. BMC psychiatry. 2014;14(1):1. doi: 10.1186/1471-244X-14-1. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
38. Lee NK, Cameron J, Jenner L. A systematic review of interventions for co-occurring substance use and borderline personality disorders. Drug and alcohol review. 2015;34(6):663–672. doi: 10.1111/dar.12267. [PubMed] [CrossRef] [Google Scholar]
39. Linehan MM. Cognitive-behavioral treatment of borderline personality disorder: Guilford Press; 1993.
40. Linehan MM. Skills training manual for treating borderline personality disorder: Guilford Press; 1993.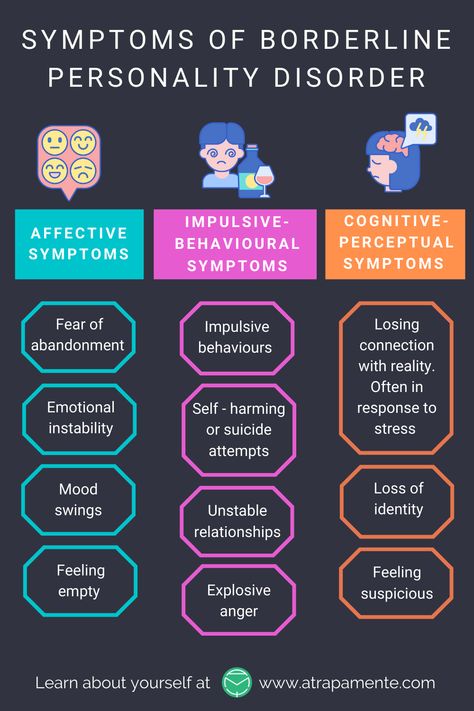
41. Bateman A, Fonagy P. Mentalization-based treatment for borderline personality disorder: a practical guide. OUP Oxford; 2006.
42. Kernberg O. Borderline personality organization. J Am Psychoanal Assoc. 1967;15(3):641–685. doi: 10.1177/000306516701500309. [PubMed] [CrossRef] [Google Scholar]
43. Gunderson JG, Lyons-Ruth K. BPD's interpersonal hypersensitivity phenotype: a gene-environment-developmental model. J Personal Disord. 2008;22(1):22. doi: 10.1521/pedi.2008.22.1.22. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
44. McMain SF, Guimond T, Streiner DL, Cardish RJ, Links PS. Dialectical behavior therapy compared with general psychiatric management for borderline personality disorder: clinical outcomes and functioning over a 2-year follow-up. American Journal of Psychiatry. 2012. [PubMed]
45. Wnuk S, McMain S, Links PS, Habinski L, Murray J, Guimond T. Factors related to dropout from treatment in two outpatient treatments for borderline personality disorder.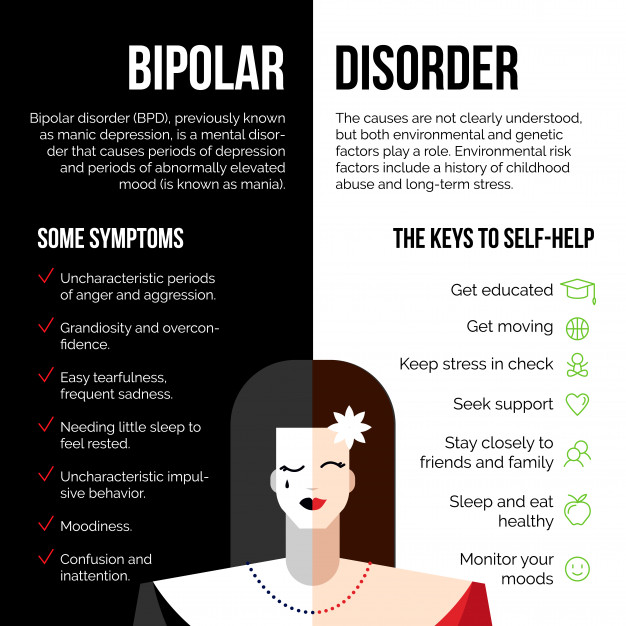 J Personal Disord. 2013;27(6):716. doi: 10.1521/pedi_2013_27_106. [PubMed] [CrossRef] [Google Scholar]
J Personal Disord. 2013;27(6):716. doi: 10.1521/pedi_2013_27_106. [PubMed] [CrossRef] [Google Scholar]
46. Keuroghlian AS, Palmer BA, Choi-Kain LW, Borba CP, Links PS, Gunderson JG. The effect of attending good psychiatric management (GPM) workshops on attitudes toward patients with borderline personality disorder. J Personal Disord. 2015;1-10 [PMC free article] [PubMed]
47. Bateman A, Krawitz R. Borderline personality disorder: an evidence-based guide for generalist mental health professionals. Oxford: Oxford University Press; 2016. [Google Scholar]
48. Black DW, Simsek-Duran F, Blum N, McCormick B, Allen J. Do people with borderline personality disorder complicated by antisocial personality disorder benefit from the STEPPS treatment program? Personal Ment Health. 2016;10(3):205–215. doi: 10.1002/pmh.1326. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
49. Zanarini MC, Frankenburg FR, Hennen J, Reich DB, Silk KR. Axis I comorbidity in patients with borderline personality disorder: 6-year follow-up and prediction of time to remission.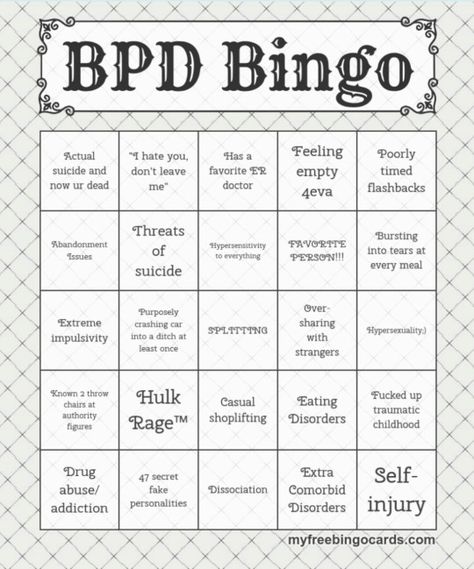 Am J Psychiatr. 2004;161(11):2108–2114. doi: 10.1176/appi.ajp.161.11.2108. [PubMed] [CrossRef] [Google Scholar]
Am J Psychiatr. 2004;161(11):2108–2114. doi: 10.1176/appi.ajp.161.11.2108. [PubMed] [CrossRef] [Google Scholar]
50. Zimmerman M, Mattia JI. Axis I diagnostic comorbidity and borderline personality disorder. Compr Psychiatry. 1999;40(4):245–252. doi: 10.1016/S0010-440X(99)90123-2. [PubMed] [CrossRef] [Google Scholar]
51. Gunderson JG, Stout RL, Shea MT, Grilo CM, Markowitz JC, Morey LC, et al. Interactions of borderline personality disorder and mood disorders over 10 years. J Clin Psychiatry. 2014;75(8):829–834. doi: 10.4088/JCP.13m08972. [PubMed] [CrossRef] [Google Scholar]
52. Bateman A, Fonagy P. Impact of clinical severity on outcomes of mentalisation-based treatment for borderline personality disorder. Br J Psychiatry. 2013;203(3):221–227. doi: 10.1192/bjp.bp.112.121129. [PubMed] [CrossRef] [Google Scholar]
53. Boritz T, Barnhart R, McMain SF. The influence of posttraumatic stress disorder on treatment outcomes of patients with borderline personality disorder.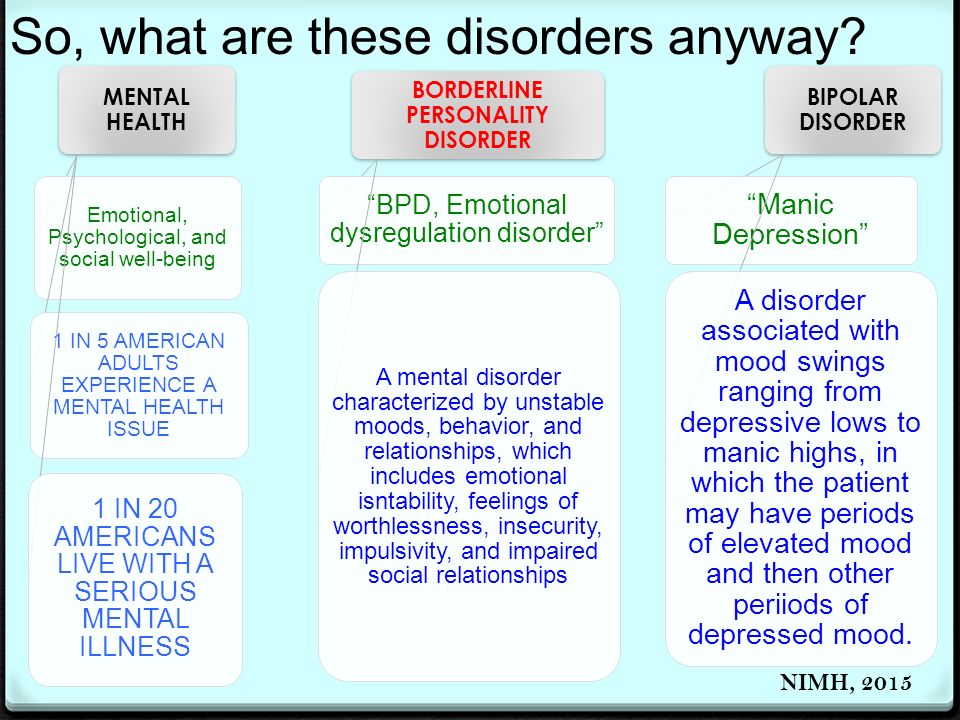 J Personal Disord. 2016;30(3):395–407. doi: 10.1521/pedi_2015_29_207. [PubMed] [CrossRef] [Google Scholar]
J Personal Disord. 2016;30(3):395–407. doi: 10.1521/pedi_2015_29_207. [PubMed] [CrossRef] [Google Scholar]
54. Linehan MM, Dimeff LA, Reynolds SK, Comtois KA, Welch SS, Heagerty P, et al. Dialectical behavior therapy versus comprehensive validation therapy plus 12-step for the treatment of opioid dependent women meeting criteria for borderline personality disorder. Drug Alcohol Depend. 2002;67(1):13–26. doi: 10.1016/S0376-8716(02)00011-X. [PubMed] [CrossRef] [Google Scholar]
55. Gregory RJ, Remen AL. A manual-based psychodynamic therapy for treatment-resistant borderline personality disorder. Psychotherapy: Theory, Research, Practice, Training. 2008;45(1):15. doi: 10.1037/0033-3204.45.1.15. [PubMed] [CrossRef] [Google Scholar]
56. Telch CF, Agras WS, Linehan MM. Dialectical behavior therapy for binge eating disorder. J Consult Clin Psychol. 2001;69(6):1061. doi: 10.1037/0022-006X.69.6.1061. [PubMed] [CrossRef] [Google Scholar]
57. Foa EB, Keane TM, Friedman MJ, Cohen JA. Effective treatments for PTSD: practice guidelines from the International Society for Traumatic Stress Studies. New York, NY: Guilford Press; 2009. [Google Scholar]
Effective treatments for PTSD: practice guidelines from the International Society for Traumatic Stress Studies. New York, NY: Guilford Press; 2009. [Google Scholar]
58. Zanarini MC, Frankenburg FR, Harned A, Fitzmaurice G. Rates of psychotropic medication use reported by borderline patients and axis II comparison subjects over 16 years of prospective follow-up. J Clin Psychopharmacol. 2015;35(1):63–67. doi: 10.1097/JCP.0000000000000232. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
59. Zanarini MC, Frankenburg FR, Reich DB, Conkey LC, Fitzmaurice GM. Treatment rates for patients with borderline personality disorder and other personality disorders: a 16-year study. Psychiatr Serv. 2014;66(1):15–20. doi: 10.1176/appi.ps.201400055. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
60. Martinho E, Jr, Fitzmaurice GM, Frankenburg FR, Zanarini MC. Pro re nata (as needed) psychotropic medication use in patients with borderline personality disorder and subjects with other personality disorders over 14 years of prospective follow-up. J Clin Psychopharmacol. 2014;34(4):499–503. doi: 10.1097/JCP.0000000000000132. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
J Clin Psychopharmacol. 2014;34(4):499–503. doi: 10.1097/JCP.0000000000000132. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
61. APA. Practice guideline for the treatment of patients with borderline personality disorder. American Psychiatric Association: American Psychiatric Pub; 2001. [PubMed]
62. Kendall T, Burbeck R, Bateman A. Pharmacotherapy for borderline personality disorder: NICE guideline. Br J Psychiatry. 2010;196(2):158–159. doi: 10.1192/bjp.196.2.158. [PubMed] [CrossRef] [Google Scholar]
63. National Institute for Clinical Excellence. Borderline personality disorder, treatment and management. The British Psychological society and the Royal College of Psychiatrists., London. 2009. https://www.nice.org.uk/guidance/cg78/chapter/1-Guidance. Accessed 09/02 2016.
64. Ingenhoven T, Lafay P, Rinne T, Passchier J, Duivenvoorden H. Effectiveness of pharmacotherapy for severe personality disorders: meta-analyses of randomized controlled trials. The Journal of clinical psychiatry.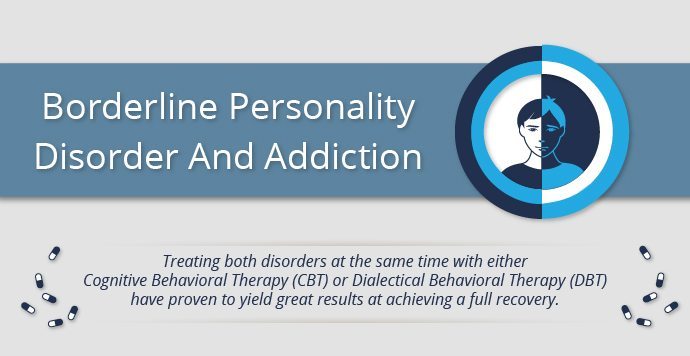 2009;71(1):14–25. doi: 10.4088/JCP.08r04526gre. [PubMed] [CrossRef] [Google Scholar]
2009;71(1):14–25. doi: 10.4088/JCP.08r04526gre. [PubMed] [CrossRef] [Google Scholar]
How to treat borderline personality disorder in adolescents?
The diagnosis of "borderline personality disorder" is often made by specialists who cannot accurately determine the patient's illness. They attribute to this disorder symptoms that are characteristic of other syndromes: bipolar disorder, depression, anxiety disorder, panic attacks, etc. The symptoms of borderline personality disorder resemble a critical manifestation of normal behavior during adolescence. As a rule, this disease begins to be diagnosed in patients aged 12-13 years. The symptoms are most pronounced by the age of 16-25, and by the age of 40-45 their intensity decreases, although the disorder itself can remain for life.
The main symptoms of borderline personality disorder are emotional instability and severe mood swings. These differences also apply to relationships with other people. One moment a person may be nice to another, and the next, hate him. Another common symptom is inner existential emptiness. A person feels emptiness and does not know how to fill himself. This condition can lead to depression or an anxiety disorder. A person can try to solve these problems by showing suicidal tendencies - hurting himself and thus filling the inner emptiness. Often teenagers in this condition may start taking drugs and drinking alcohol. Sometimes this behavior can lead to alcoholism, drug addiction, or suicide.
These differences also apply to relationships with other people. One moment a person may be nice to another, and the next, hate him. Another common symptom is inner existential emptiness. A person feels emptiness and does not know how to fill himself. This condition can lead to depression or an anxiety disorder. A person can try to solve these problems by showing suicidal tendencies - hurting himself and thus filling the inner emptiness. Often teenagers in this condition may start taking drugs and drinking alcohol. Sometimes this behavior can lead to alcoholism, drug addiction, or suicide.
The therapy process accepts the suffering of the patient, but does not accept destructive behavior, drug or alcohol use.
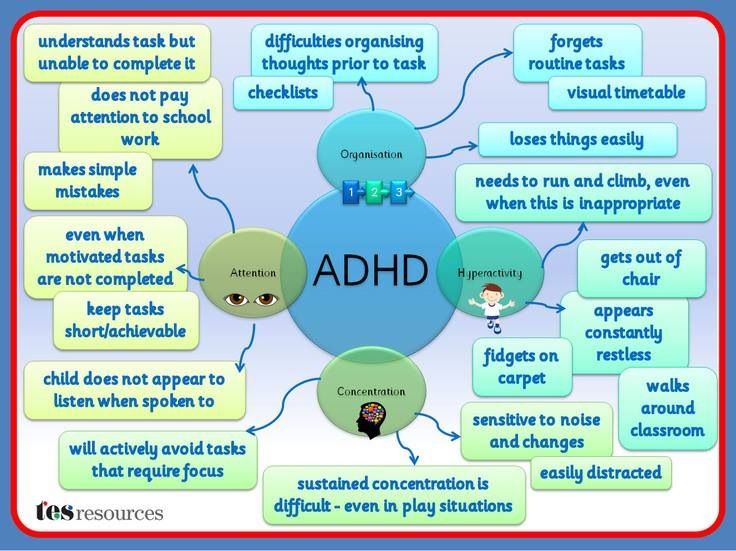
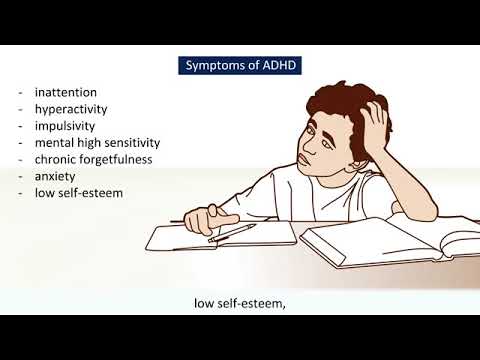
Relatives usually do not know what to do with such people, and psychologists do not always understand how to properly approach their treatment. As a rule, borderline personality disorder appears in adolescents from dysfunctional families, where there was a lot of aggression, screaming, quarrels, and sometimes violence. Such patients may have attention-deficit/hyperactivity disorder as a comorbid disorder.
Such patients may have attention-deficit/hyperactivity disorder as a comorbid disorder.
See also
What is borderline personality disorder?
The most effective treatment for borderline personality disorder is dialectical behavior therapy. The therapy process accepts the suffering of the patient, but does not accept destructive behavior, drug or alcohol use. During the behavioral part of therapy, a strict program is built to avoid the patient's suicidal tendencies or the use of illegal substances. Specialists give behavioral techniques that replace what, in a state of disorder, the patient determines effective for himself.
Also, for the treatment of this syndrome, family instruction is required, in which relatives are explained how to properly respond to human behavior and set boundaries. Medication is also an important part of the program. Unfortunately, at the moment there are no drugs that can completely cure borderline personality disorder, but there are drugs that reduce emotional instability, depression and anxiety.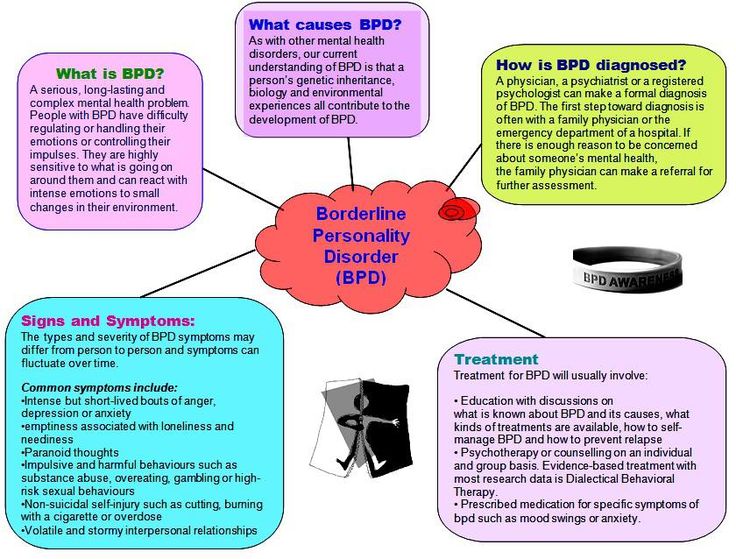 Such treatment helps the patient to socialize in society and receive tools that change his attitude towards himself and others.
Such treatment helps the patient to socialize in society and receive tools that change his attitude towards himself and others.
- Diseases and disorders
Share:
BPD treatment: effective and useless methods - Empathy
BPD treatment: effective and useless methods - Empathy - mental health center- Home
- Articles
- BPD treatment: effective and ineffective methods
We continue to talk about borderline personality disorder. Earlier we touched on such a topic as the mental problems associated with BPD, today's topic is the treatment of BPD.
The main treatment for borderline personality disorder is psychotherapeutic , specifically Dialectical Behavior Therapy (DBT).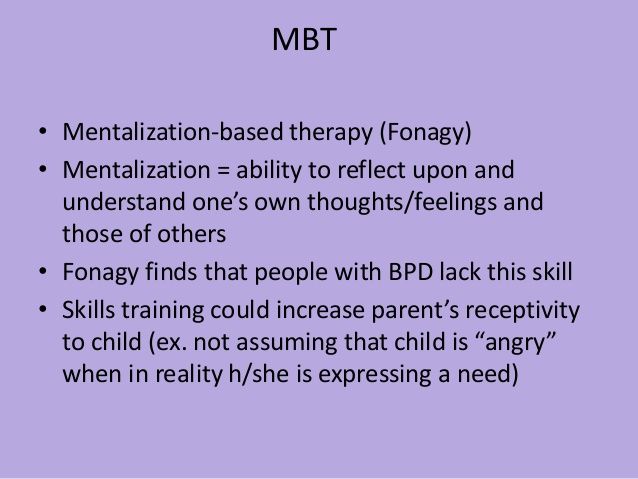 The essence of this method lies in the fact that the patient trains to look at what is happening from different angles, abandoning the simplified, black and white perception of the world. After the patient has realized all the variety of points of view on the same events, the specialist helps him choose the most optimal variant of behavior, in which there will be no place for self-damaging actions and other destructive reactions.
The essence of this method lies in the fact that the patient trains to look at what is happening from different angles, abandoning the simplified, black and white perception of the world. After the patient has realized all the variety of points of view on the same events, the specialist helps him choose the most optimal variant of behavior, in which there will be no place for self-damaging actions and other destructive reactions.
Regarding psychopharmacotherapy in BPD, it is usually used symptomatically and in the presence of comorbid disorders, but often taking pills is as important as psychotherapeutic correction. The main groups of drugs used in BPD are antidepressants, antipsychotics, and mood stabilizers.
Antidepressants
Most often, antidepressants are used when BPD is associated with major depressive disorder or anxiety disorders. When borderline personality disorder occurs without depressive symptoms, antidepressants are useless.
Most often, selective serotonin reuptake inhibitors (SSRIs) are prescribed to patients with BPD, such as fluvoxamine , fluoxetine and sertraline .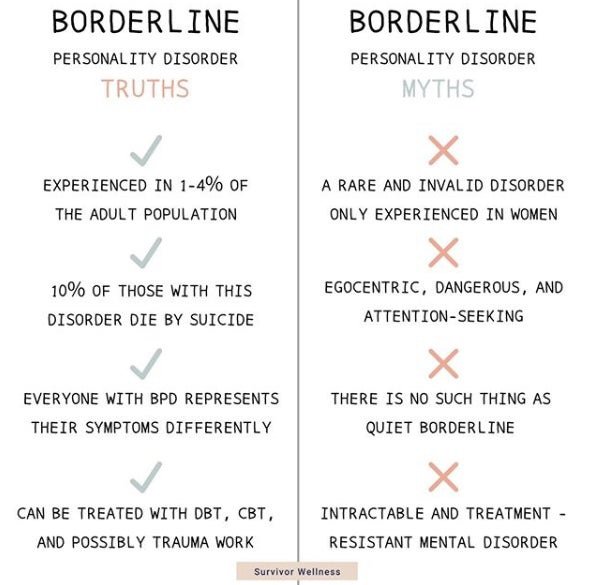 The mixed-acting drug venlafaxine is also effective, and tricyclic antidepressants (amitriptyline) are used for severe depressive symptoms and pharmacological resistance. The effect of antidepressants is greatly enhanced if the patient undergoes psychotherapy in parallel.
The mixed-acting drug venlafaxine is also effective, and tricyclic antidepressants (amitriptyline) are used for severe depressive symptoms and pharmacological resistance. The effect of antidepressants is greatly enhanced if the patient undergoes psychotherapy in parallel.
Atypical antipsychotics
Of the atypical antipsychotics, , aripiprazole , is most effective for the main symptoms of BPD, such as impulsivity, anger, and interpersonal difficulties. Aripiprazole is also effective in relation to comorbidities, for example, it can significantly reduce anxiety and reduce the manifestation of depressive symptoms and symptoms of obsessive-compulsive disorder (OCD). Similar effect to aripiprazole is shown quetiapine and olanzapine . However, researchers have not yet come to an unequivocal opinion about the effectiveness of these drugs in relation to symptoms such as self-harm, suicidal thoughts and attempts.
Mood stabilizers
Among mood stabilizers, topiramate, valproic acid, and lamotrigine are the most effective in relieving the main symptoms of BPD and side effects. Carbamazepine did not show significant positive effects in the treatment of such patients.
Carbamazepine did not show significant positive effects in the treatment of such patients.
Separately, it is worth noting lithium preparations . Although there is not much research on the effectiveness of lithium in BPD, when applied in practice, it shows a decrease in impulsivity and aggression, as well as suppression of suicidal tendencies. When BPD is complicated by bipolar disorder (BAD), the effectiveness of lithium is undeniable.
How can we help?
| If you have found some of the described symptoms in yourself or your loved ones, this may indicate the development of a mental disorder. In this case, it is necessary to consult a psychiatrist for diagnosis and initiation of timely treatment. Beyond face-to-face communication , we offer remote consultation service (online reception) , which is not inferior to a face-to-face meeting in quality. Thus, you can get qualified help from a high-level specialist , no matter where you are. |