Behavioral health service codes
CPT Codes for Behavioral Health Billing [Updated for 2022]
Current procedural terminology (CPT) codes are essential components of the health insurance billing process. It's critical to use the appropriate procedure codes to receive reimbursement for your services and avoid an audit. However, using the correct CPT codes for medical billing involves understanding a complex system.
There are thousands of codes to choose from and many different guidelines to follow. Nevertheless, it is possible to use medical codes properly and receive maximum reimbursement rates for your services.
This post will cover some basics of CPT codes for mental health, and provide tips for avoiding claim denials. The better you understand current procedural terminology, the more time you'll have to care for patients, and the easier it will be to get paid.
What are CPT Codes?CPT is a uniform coding system developed by the American Medical Association (AMA). The AMA first established this system in 1966 to standardize terminology and simplify record-keeping for physicians and staff. Since its development, CPT has undergone several changes. The most recent edition focuses on using CPT codes to report physician services.
CPT codes describe medical procedures — such as tests, evaluations, surgeries, and other practices — performed by a physician on a patient. For example, behavioral health CPT codes describe the length of a psychotherapy session with a client or a diagnostic interview. CPT codes are necessary to receive reimbursement from health insurance companies.
Why CPT Codes Are Essential for Clinicians
CPT codes are essential parts of practice management for clinicians and health care staff because they determine compensation and the practice's overall success. To receive the correct reimbursement rates, clinicians must ensure the codes on insurance claim forms accurately reflect the services they provided before submitting the claims to insurance companies.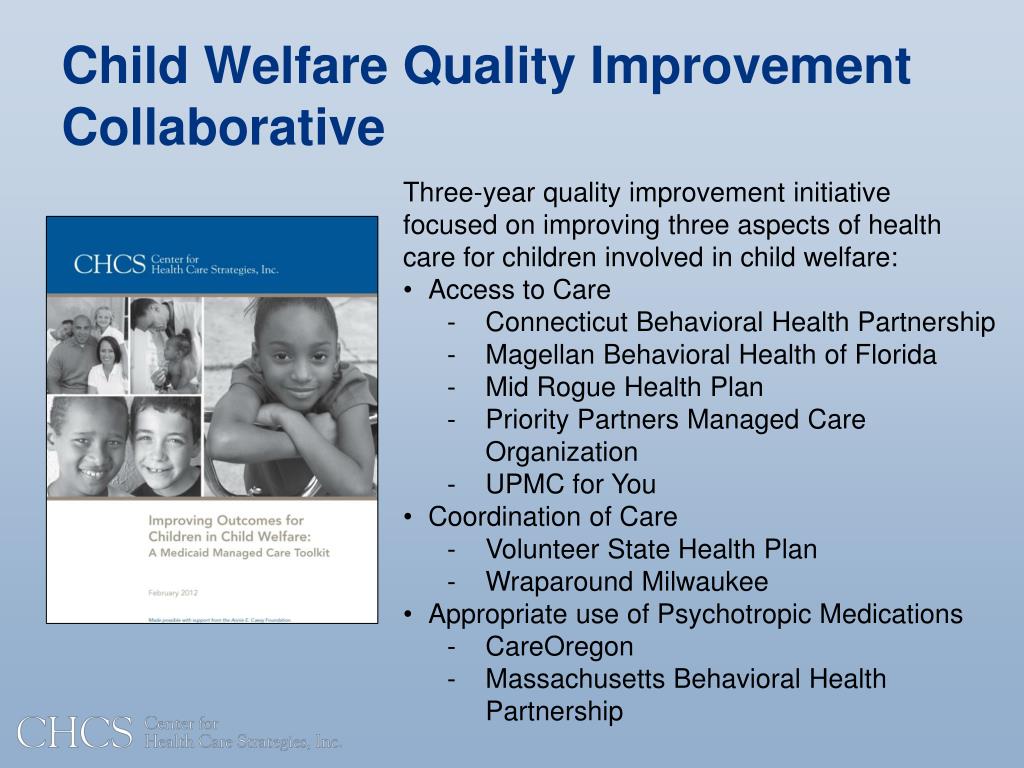
CPT coding tells insurance payers what you would like to get paid for. Along with the International Classification of Diseases codes, CPT codes paint a complete picture for health insurance companies, and you need both types for reimbursement.
The ICD code set describes the diagnosis and why the treatment was necessary, and the CPT code explains the services provided. Examples of mental health ICD codes include the following.
- F41.9: Anxiety disorder
- F31.31: Bipolar disorder, current episode depressed, mild
- F42: Obsessive-compulsive disorder
- F43.11: Post-traumatic stress disorder, acute
For example, a social worker might use F41.9 with CPT code 90832, which is the code for individual psychotherapy for 30 minutes, to bill for a session with a client experiencing anxiety. You would include both codes on a health insurance claims form.
There are three distinct categories of CPT codes, which we will look at next.
What Are the Three Categories of CPT Codes?
The three categories of CPT codes are as follows.
- Category I: Most coders spend the majority of their time working with Category I codes. There are different sections of these codes based on the field of healthcare. The six sections of the CPT codebook are Evaluation and Management, Medicine, Surgery, Radiology, Anesthesiology and Pathology, and Laboratory. Each has a unique set of guidelines. The CPT codes under Category I are five digits long.
- Category II: Category II codes contain four digits, followed by the letter F. Category II codes are optional. They provide additional information and are not a replacement for Category I or Category III codes.
- Category III: Category III codes are temporary and represent new or experimental procedures or technology.
 For example, if you can't find a new practice in Category I, you might use a Category III code. Category III codes are four digits long and end in the letter T.
For example, if you can't find a new practice in Category I, you might use a Category III code. Category III codes are four digits long and end in the letter T.
Since Category I is the most frequently used, here's a look at the numerical range of codes within this category.
- Evaluation and Management: 99202 to 99499
- Anesthesia: 00100 to 01999 and 99100 to 99150
- Surgery: 10021 to 69990
- Radiology: 70010 to 79999
- Pathology and Laboratory: 80047 to 89398
- Medicine: 90281 to 99199 and 99500 to 99607
Each of these sections contains subfields to correspond to a particular healthcare field and include guidelines to follow. For example, therapists commonly use psychotherapy CPT codes falling in the range of 90832 to 90853 under the Medicine's psychiatry section. Psychiatrists, primary care physicians, and other authorized prescribers might use evaluation and management codes for providing general medical services.
CPT codes also have various modifiers. Modifiers have two numbers or letters, and you can add them to a CPT code. They describe specific critical parts of a procedure.
Some codes have instructions below them in parentheses to tell the coder there may be a better code to use. Codes must be as specific as possible for a mental health billing claim to get accepted.
How to Use the
Correct CPT Code in PsychiatryThe CPT code set is a complex system. It is not always easy to determine if you've met the required elements to code appropriately for the maximum reimbursement amount. It may help to break the process down into steps for new and established patients.
First, you might bill two types of psychiatric service or procedure CPT codes for new patient office visits. These are:
- E/M codes
- Psychiatric diagnostic evaluation codes
Depending on the situation and time involved, it may be appropriate to bill for both codes. Here are a few guidelines to follow.
Here are a few guidelines to follow.
- E/M: Use E/M codes when evaluating a new medical issue. With the AMA's 2021 coding changes, you can select an E/M code based on the complexity of medical decision-making or the total time you spent on the patient's care on the day of the encounter. If you provide E/M services with a psychotherapy add-on code, you must choose a code based on medical decision-making and not total time.
- Psychiatric diagnostic evaluation: Use psychiatric diagnostic evaluation codes for a diagnostic assessment. You may need to use these codes more than once if it takes more time to complete the initial evaluation.
Regarding established patients, the rules allow you to bill an E/M service with every psychotherapy visit, but they don't require you to do so with every encounter. Only bill E/M services if you addressed and documented a separate medical issue during the visit.
For example, if you address medication's side effects during an encounter, you might bill for an E/M visit in addition to a psychotherapy session.
However, if a patient has been stable and on the same medication for years and attends a psychotherapy visit, you can only bill for the psychotherapy session. You cannot bill for E/M because there are no medical or medication concerns expressed during the visit.
Also, to bill for E/M, your documentation must prove your active management or discussion of a medical or medication problem distinct from the psychotherapy service.
The 3 Major Components of E/M DocumentationAccording to the Centers for Medicare and Medicaid Services, insurance companies might want to see documentation to ensure the client's policy covers necessary services and confirm the following pieces of information:
- The service site
- The medical necessity of the services provided
- The accuracy of the services reported
Your client's medical records must include the following three components to support the E/M codes you choose.
- History: The history section must include the history of present illness, a review of body systems, and the family and social history.
- Examination: The examination section includes the type of examination performed based on your judgment and the nature of the problem. According to the CMS, the levels of E/M services derive from problem-focused, expanded problem-focused, detailed, or comprehensive exams.
- Medical decision-making: The medical decision-making section includes the number and complexity of problems addressed during the specific encounter, the complexity of the data reviewed, and the risk of complications.
When selecting an E/M code with psychotherapy, you'll base your choice on medical decision-making. It's also necessary to choose a CPT code that reflects the service site and whether the patient is new or established. Take these steps:
- Select the type and level of E/M service based on medical decision-making.
- Choose timed psychotherapy add-on codes based on the time spent providing psychotherapy.
For example, if you choose E/M code 99202 to evaluate and manage a new patient in an outpatient setting with straightforward decision-making and need to bill for 30 minutes of psychotherapy, you would include the add-on code 90833.
Make sure to keep your E/M code and psychotherapy codes separate. The time associated with the E/M service cannot count toward the time of the psychotherapy service. The E/M service must be significant and distinct from psychotherapy.
The Most Common
Psychotherapy CPT CodesWhile family therapists and counselors may not use E/M codes like psychiatrists or primary care physicians, they will bill for psychotherapy services. The American Psychological Association lists standard CPT codes used by therapists.
- 90832: 30 minutes of individual psychotherapy
- 90834: 45 minutes of individual psychotherapy
- 90837: 60 minutes of individual psychotherapy
- 90845: Psychoanalysis
- 90846: 50 minutes of family psychotherapy without the client present
- 90847: 50 minutes of family psychotherapy with the client present
- 90849: Multiple-family group psychotherapy
- 90853: Group psychotherapy
Though CPT codes describe specific times, such as 30, 45, and 60 minutes, therapists have some flexibility, since sessions might go over or under that exact amount.
When choosing a psychotherapy CPT code, therapists must select the closest one to the time spent in the session. The APA lists the following psychotherapy session durations.
- 90832: Choose this code for sessions that run between 16 and 37 minutes.
- 90834: Select this code for sessions that are 38 to 52 minutes long.
- 90837: This code is appropriate for sessions lasting 53 minutes or longer.
- 90846 or 90847: Choose these codes for 26 minutes or more of family psychotherapy.
Psychotherapy
Crisis CodesCPT codes for crises allow behavioral health professionals to bill for emergency sessions. Care providers typically use the following crisis codes for patients in great distress who require immediate attention or are in a life-threatening situation.
- 90839: First 60 minutes of psychotherapy for crisis
- 90840: Add-on code for each additional 30 minutes of psychotherapy for crisis
- 99050: Add-on code for services provided when the office is usually closed
- 99051: Add-on code for services provided during regularly scheduled hours on evenings, weekends, or holidays
If a crisis session falls below 60 minutes, you will bill for a regular psychotherapy code, such as 90834.
Other
Add-On CodesProviders may use add-on codes to describe additional services. Behavioral health clinicians can only apply add-on codes in combination with psychotherapy and diagnostic evaluation services. Providers must include the principal CPT code and add-on code on the billing form, and list them separately. Add-on codes include the following.
- 90785: Interactive complexity
- 90863: Psychopharmacology with psychotherapy
- 90833: 30 minutes of psychotherapy with E/M service
- 90836: 45 minutes of psychotherapy with E/M service
- 90838: 60 minutes of psychotherapy with E/M service
Clinicians might use code 90785 for factors that complicate service delivery, such as a client's angry family member or a third party like a probation officer. Psychologists might use code 90863 when reviewing or prescribing medication on the same day as delivering psychotherapy services. Psychiatrists do not use code 90863.
Psychiatrists do not use code 90863.
Mental Health Test and
Assessment CodesCPT codes for mental health tests and assessments include the following.
- 96105: Aphasia assessment
- 96110: Developmental screening
- 96112: Developmental test administration with interpretation
- 96113: Each additional 30 minutes of developmental test administration with interpretation
- 96116: Neurobehavioral status exam, 60 minutes
- 96121: Each additional hour of neurobehavioral status examination
- 96125: Standardized cognitive performance testing, 60 minutes
- 96127: Brief emotional or behavioral assessment
- 96130: Psychological testing evaluation services provided by a physician or qualified health professional, 60 minutes
- 96131: Each additional hour of psychological testing evaluation services performed
- 96132: Neuropsychological testing services, 60 minutes
- 96133: Each additional hour of neuropsychological testing services performed
- 96136: Psychological or neuropsychological test administration and scoring by a physician or qualified health professional, 30 minutes
- 96137: Each additional 30 minutes of neuropsychological test administration and scoring by a physician or qualified health professional
- 96138: Psychological or neuropsychological test administration and scoring by a technician, 30 minutes
- 96139: Each additional 30 minutes of neuropsychological test administration and scoring by a technician
- 96146: Psychological or neuropsychological test administration via an electronic platform with automated results
- 96156: Health assessment or reassessment
- 96160: Patient-focused health risk assessment
- 96161: Caregiver-focused health risk assessment
Psychiatry
CPT CodesPsychiatrists use CPT codes to bill for psychiatric diagnostic evaluations, psychotherapy, and other psychiatric services. CPT codes for psychiatric services include the following.
CPT codes for psychiatric services include the following.
- 90791: Psychiatric diagnostic evaluation without medical services
- 90792: Psychiatric diagnostic evaluation with medical services
- 90865: Narcosynthesis
- 90867: Therapeutic repetitive transcranial magnetic stimulation
- 90870: Electroconvulsive therapy
- 90875: 30 minutes of individual psychophysiological therapy with biofeedback
- 90876: 45 minutes of individual psychophysiological therapy with biofeedback
- 90880: Hypnotherapy
- 90899: Unlisted psychiatric procedure or service
Psychiatry Evaluation and
Management CodesPsychiatrists may use E/M codes to bill for evaluation and management services either alone or with psychotherapy. For psychiatrists and other physicians, psychotherapy is an add-on code to the primary E/M service.
- 99202 to 99205: Outpatient E/M services for a new patient
- 99211 to 99215: Outpatient E/M services for an established patient
- 99241 to 99245: Consultations for a new or established patient in an outpatient setting
- 99221 to 99223: Initial hospital E/M services for a new or established patient
- 99231 to 99233: Hospital E/M services for a new or established patient after initial visit
- 99251 to 99255: Inpatient consultations
Common Behavioral Health
Case Management CPT CodesLike licensed counselors, clinical social workers who provide psychotherapy services use CPT codes to get reimbursed. Here's a CPT description list of frequently used codes, according to the National Association of Social Workers:
- 90832: 30 minutes of psychotherapy
- 90834: 45 minutes of psychotherapy
- 90837: 60 minutes of psychotherapy
- 90785: Interactive complexity add-on
- 90839: 60 minutes of psychotherapy for crisis
- 90840: Each additional 30 minutes of psychotherapy for crisis
- 90791: Psychiatric diagnostic evaluation
- 90845: Psychoanalysis
- 90846: 50 minutes of family psychotherapy without the patient present
- 90847: 50 minutes of family psychotherapy with the patient present
- 90853: Group psychotherapy
Telehealth
CPT Medical Coding ListWith an increasing number of behavioral health professionals moving their practices online, it helps to know CPT codes for virtual therapy. Telehealth CPT codes are especially relevant today under the Coronavirus Preparedness and Response Supplemental Appropriations Act, which expands access to Medicare telehealth services.
Telehealth CPT codes are especially relevant today under the Coronavirus Preparedness and Response Supplemental Appropriations Act, which expands access to Medicare telehealth services.
According to the Centers for Medicare and Medicaid Services, telehealth visits are the same as in-person visits and get paid at the same rates. Therefore, you will use the identical CPT code for a virtual therapy session as you would if you were billing for a face-to-face meeting. For example, if you meet with a patient online, you would still use the code 90832 for 30 minutes of psychotherapy. However, you would apply different modifiers for telehealth services, as follows.
- 95 modifier: Add the modifier 95 to the appropriate CPT code. This modifier describes a real-time interaction between a clinician and patient via a telecommunications system, such as through video conferencing. You may also use the modifier GT instead.
- 02 for place of service: Use Code 02 to describe the place of service (POS) as a telecommunications system. It may replace the commonly used POS code 11, which describes providing therapy in an office.
As you'll see, some telehealth codes belong to the Healthcare Common Procedural Coding System (HCPCS). HCPCS codes are not part of the CPT set, and they cover specific services and products needed to provide care. HCPCS codes consist of a single letter followed by four numbers. Here are codes you might use specifically for telehealth.
- G2012: Virtual check-in or brief, patient-initiated visit
- G2010: Remote evaluation of a recorded video or image provided by an established patient
- 99421: Online digital evaluation and management service conducted via a patient portal for an established patient, five to 10 minutes of cumulative time over seven days
- 99422: Online digital evaluation and management service conducted via a patient portal for an established patient, 11 to 20 minutes of cumulative time over seven days
- 99423: Online digital evaluation and management service conducted via a patient portal for an established patient, 21 or more minutes of cumulative time over seven days
Non-physician healthcare professionals may use the codes G2061, G2062, or G2063 to provide an online assessment and management service for an established patient.
New CPT Codes for
Behavioral Health ServicesEvery year, health professionals can expect revised or new mental health CPT codes. According to the American Psychological Association, as of Jan. 1, 2020, psychologists must use new therapy CPT codes to get reimbursed for health behavior assessment and intervention services from third-party payers. Providers use these services to address psychological, emotional, cognitive, or behavioral issues that impact the treatment of a physical health problem. Psychologists may provide these services to an individual, group, or a patient's family to help the client cope with physical health conditions.
HBAI codes require a physical health diagnosis or an ICD code and are not for mental health services. Here are the code revisions.
- Code 96156 replaces codes 96150 and 96151: Clinicians must now use code 96156 to bill for a health and behavior assessment or reassessment.
 The new code for assessment services is now event-based rather than time-based.
The new code for assessment services is now event-based rather than time-based. - Code 96152 is now 96158 plus 96159: Code 96152 for an individual, face-to-face health behavior intervention is now 96158 for the first 30 minutes. List code 96159 separately for each additional 15 minutes of the intervention.
- Code 96153 is now 96164 plus 96165: Code 96153 for a face-to-face group health behavior intervention is now 96164 for the first 30 minutes. Tack on the code 96165 for each additional 15 minutes of service.
- Code 96154 is now 96167 plus 96168: Code 96154 for a face-to-face family health behavior intervention with the patient present is now code 96167 for the first 30 minutes. Use code 96168 for each additional 15 minutes.
- Code 96155 is now 96170 plus 96171: Code 96155 for a face-to-face family health behavior intervention without the patient present is now 96170 for the first 30 minutes. Use code 96171 for each additional 15 minutes.
For additional information about the 2021 E/M coding changes, check out our blog post here.
How CPT Code Changes
Impact the Reimbursement ProcessReimbursement rates change all the time, and a lot depends on the decisions made by the CMS. The CMS accepts the American Medical Association's CPT code recommendations and makes the final decisions regarding code values.
The code selection process also impacts how much clinicians get paid. For example, with the recent E/M coding changes, clinicians can bill for the total time they spend in one day on an encounter, which includes non-face-to-face time, and gets credit for tasks like interpreting exams performed by other physicians.
Clinicians can also choose an E/M code based on total time or medical decision-making, selecting the one that makes the most financial sense.
CPT Code
Reimbursement RatesReimbursement rates depend on the insurance payer, location, and practitioner level. For instance, a psychiatrist will receive a higher reimbursement rate than a social worker.
For instance, a psychiatrist will receive a higher reimbursement rate than a social worker.
The CPT code you choose also affects compensation. In general, the longer you spend with a patient delivering services, the more you'll get paid. For example, according to the Mississippi Division of Medicaid's 2020 fee schedule, psychotherapy rates were:
- 90832: $60.07
- 90834: $79.90
- 90837: $119.68
If you're concerned you're not getting the highest reimbursement rate possible, let us know at ICANotes. We've designed our electronic health record software to help behavioral health specialists maximize reimbursement.
ICANotes keeps track of documentation elements in clinical notes and automatically calculates the highest-level E/M code supported by a note. ICANotes makes it easy to establish all the required details of accurate E/M documentation by providing pre-templated buttons and an easy-to-use interface. With ICANotes, clinicians can stay up to date on CPT changes and make sure they comply with the Health Insurance Portability and Accountability Act.
With ICANotes, clinicians can stay up to date on CPT changes and make sure they comply with the Health Insurance Portability and Accountability Act.
Tips for Maximizing Reimbursement and
Avoiding Insurance Claim Denials
If you hope to avoid issues with claims, you mostly want to remember that medical necessity determines the level of service to bill. It would not be appropriate to document a higher level of service if it is unnecessary. Always make sure the documentation supports the level of care you are billing. Here are a few more tips to keep in mind.
1. Ensure Correct Coding
To receive reimbursement, a clinician must complete accurate coding. Coding errors can lead to payment delays or rejected claims. Frequent or consistent errors could lead to an audit or charges of fraud. Strive for the highest accuracy, and cut down on simple errors like incorrect patient information or policy number mistakes. Always refer to the AMA’s most recent CPT manual to make sure you use the right codes in your practice.
Also, make it a habit to check and recheck work, and thoroughly read all the therapy notes included with the codes. Encourage staff members to do the same. One of the most common causes of claim denials is the improper use of modifiers. Therefore, make sure to familiarize yourself with modifiers before using them. Modifiers can be the difference between maximum reimbursement and reduced reimbursement, so it's crucial to review the rules.
2. Claim Only What's Medically Necesarry
Medicare and other payers define what's medically necessary in different ways, but in general, it's about doing what's best for the patient at the right time. A claim for a service that is not a medical necessity will likely get denied.
To help demonstrate a medically necessary claim, make sure to choose the appropriate ICD code and link it to the associated CPT codes that are valid for the visit. Doing so enables staff and insurance payers to see the reason for each service.
3. File Claims on Time
You must submit claims by a specific deadline. For example, Medicare requires you to file no later than 12 months after the date of service. These dates can vary depending on the payer, and some claims may be due within 90 days or 180 days after service. By meeting deadlines, you'll ensure you receive adequate reimbursement.
4. Emphasize Quality Documentation
Inadequate documentation can affect the reimbursement process. Make sure everyone in your practice understands the value of correct, legible, and complete documentation. Otherwise, it will be challenging to make an accurate or complete claim.
5. Identify and Educate
Identify coding errors, review past mistakes, and aim to correct the errors by educating staff and staying current on any code changes. Schedule regular training meetings to keep information fresh and share any updates.
Use ICANotes for Fast and Accurate BillingProper coding requires knowledge and practice. Most behavioral health clinicians want to spend their time and energy providing patient care — not worrying about coding and claims. ICANotes can step in and take care of the work for you, so you can get back to doing what you love.
Most behavioral health clinicians want to spend their time and energy providing patient care — not worrying about coding and claims. ICANotes can step in and take care of the work for you, so you can get back to doing what you love.
With ICANotes, you can expect automatic coding at the highest reimbursement level possible to ensure claims get accepted and you get paid. Without the need to fix errors or resubmit claims, you’ll save time, money, and energy. To experience the benefits of ICANotes behavioral health EHR software firsthand, sign up for a free trial today!
SCHEDULE A DEMO
Sources:
- https://www.cdc.gov/wtc/pdfs/policies/cms-1500-P.pdf
- https://www.icanotes.com/2021/01/15/what-to-know-new-e-m-coding-changes/
- https://www.psychiatry.org/psychiatrists/practice/practice-management/coding-reimbursement-medicare-and-medicaid/coding-and-reimbursement
- https://www.
 apaservices.org/practice/reimbursement/health-codes/psychotherapy
apaservices.org/practice/reimbursement/health-codes/psychotherapy - https://www.aapc.com/resources/medical-coding/cpt.aspx
- https://en.wikipedia.org/wiki/Current_Procedural_Terminology
- https://psychcentral.com/lib/cpt-codes-for-psychology-services#3
- https://www.cms.gov/files/document/medicare-mental-health.pdf
- https://blog.therapynotes.com/understanding-crisis-codes-90839-and-90840
- https://therathink.com/cpt-code-90839/
- https://www.aappublications.org/news/2017/06/21/Coding062117
- https://www.aacap.org/App_Themes/AACAP/Docs/member_resources/aacap_news/2018/AACAP-News-May-June-2018-CPT-Screening-Codes.pdf
- https://www.aap.org/en-us/Documents/coding_factsheet_developmentalscreeningtestingandEmotionalBehvioraassessment.pdf
- https://www.apaservices.org/practice/reimbursement/health-codes/testing/neuropsychological-testing.pdf
- https://www.asha.org/practice/reimbursement/medicare/slp_coding_rules/
- https://www.
 apaservices.org/practice/reimbursement/health-codes/testing/webinar.pdf
apaservices.org/practice/reimbursement/health-codes/testing/webinar.pdf - https://www.cms.gov/outreach-and-education/medicare-learning-network-mln/mlnproducts/downloads/eval-mgmt-serv-guide-icn006764.pdf
- https://www.facs.org/-/media/files/advocacy/practice-management/2020_emcoding.ashx
- https://www.medscape.com/courses/section/880390
- https://www.apaservices.org/practice/reimbursement/health-codes/crosswalk.pdf
- https://www.apaservices.org/practice/reimbursement/health-codes/testing/codes-descriptions.pdf
- https://www.apaservices.org/practice/reimbursement/health-codes/reminder-new-codes
- https://www.apaservices.org/practice/reimbursement/government/psychotherapy-services
- https://therathink.com/insurance-reimbursement-rates-for-psychotherapy/
- https://medicaid.ms.gov/wp-content/uploads/2014/03/CommunityMentalHealthCenter.pdf
- https://www.medicaleconomics.com/view/e-m-changes-take-effect-january-2021
Top CPT Codes for Mental Health Billing – My Clients Plus
While precision in how you use CPT codes may not seem of utmost significance, in fact, using the correct CPT codes for the mental health services you provide is important for two major reasons. When your claims include the right codes, they’ll be accepted in a more timely manner, ensuring you have the necessary cash flow to operate your practice. Perhaps more urgently, coding mistakes could cause your practice to be audited, and errors could result in fines. In this post, we’ll cover what you need to know about using CPT codes and the most common codes you should become familiar with.
When your claims include the right codes, they’ll be accepted in a more timely manner, ensuring you have the necessary cash flow to operate your practice. Perhaps more urgently, coding mistakes could cause your practice to be audited, and errors could result in fines. In this post, we’ll cover what you need to know about using CPT codes and the most common codes you should become familiar with.
What are CPT Codes for Mental Health?
The Current Procedural Terminology (CPT) code set describes tests, evaluations, treatments, and other medical procedures used in the spectrum of healthcare. The set contains over 8,000 codes and is published and updated annually by the American Medical Association. It was created to track healthcare trends and issues as well to use in the claims submission process. The codes communicate to payers what procedures you need to be reimbursed for as a provider.
The codes related to mental health (codes 90785-90899) are found in the Psychiatry section of the CPT code set and cover services provided by medical professionals, such as psychiatrists, as well as services that can be delivered by non-medical professionals such as licensed clinical psychologists, licensed professional counselors, licensed marriage and family therapists, and licensed clinical social workers.
Categories of Mental Health CPT Codes
The mental health CPT codes used by therapists are organized into four distinct categories. These categories make it easier to find the code you’re looking for.
Psychiatric Diagnostic Interview
- Code 90801: Psychiatric diagnostic interview examination
- Code 90802: Interactive psychiatric diagnostic interview examination
Psychiatric Therapeutic Services
- Codes 90804-90809: Insight-oriented, behavior modifying and/or supportive psychotherapy
- Codes 90810-90815: Interactive psychotherapy
Family Medical Psychotherapy
- 90846: Family psychotherapy (without the patient present)
- 90847: Family psychotherapy (with the patient present)
- 90849: Multiple-family group psychotherapy
Group Psychotherapy
- 90853: Group psychotherapy (other than a multiple-family group)
- 90857: Interactive group psychotherapy
Common Mental Health CPT Codes
While there are many codes that may be applicable to mental health services more broadly, in a therapy setting, you’ll probably find yourself using only a relatively small subset of these codes. Learning the most common CPT codes for mental health will help you choose the best code for each service you provide. Here are the most common codes that you’ll encounter as a therapist.
Learning the most common CPT codes for mental health will help you choose the best code for each service you provide. Here are the most common codes that you’ll encounter as a therapist.
90837 — Psychotherapy, 60 minutes
Description: Individual psychotherapy, 60 minutes, with client and/or family member.
Time: 60 minutes (functionally between 53 and 60 minutes)
90834 — Psychotherapy, 45 minutes
Description: Individual psychotherapy, 45 minutes, with client and/or family member.
Time: 45 minutes (functionally between 38 and 52 minutes)
90791 — Psychiatric diagnostic evaluation without medical services
Description: Initial diagnostic interview exam that does not include any medical services. Includes a chief complaint, history of present illness, family and psychosocial history, and complete mental status examination. (Use code 90792 for an initial evaluation with medical services.)
Time: Not time-based
90847 — Family psychotherapy (with client present), 50 minutes
Description: Family psychotherapy (conjoint psychotherapy) (with client present). (Can also be used for couples therapy.)
(Can also be used for couples therapy.)
Time: 50 minutes
90853 — Group psychotherapy (other than of a multiple-family group)
Description: Group psychotherapy (other than of a multiple-family group). Relies on the use of interactions of group members to examine the pathology of each individual within the group. The dynamics of the entire group are noted and used to modify behaviors and attitudes of the client members. (Used to report per-session services for each group member.)
Time: Not time-based
90846 – Family psychotherapy (without client present), 50 minutes
Description: Therapy session intended to aid the treatment of the client, where the family of a client is present without the client being present.
Time: 50 minutes
90875 – Under other psychiatric services or procedures
Description: Individual psychophysiological therapy incorporating biofeedback training by any modality (face-to-face with the client), with psychotherapy (e. g., insight-oriented, behavior modifying, or supportive psychotherapy).
g., insight-oriented, behavior modifying, or supportive psychotherapy).
Time: 20-30 minutes
90832 – Psychotherapy, 30 minutes
Description: Individual psychotherapy, 30 minutes
Time: 30 minutes (functionally between 16 – 37 mins)
90838 – Psychotherapy, 60 minutes, with E/M service
Description: Individual psychotherapy, 60 minutes with client and/or family member when performed with an evaluation and management (E/M) service.
Time: 60 minutes (functionally between 53 and 60 minutes)
99404 — Under preventive medicine, individual counseling services
Description: Preventive medicine counseling and/or risk factor reduction intervention(s) provided to an individual (separate procedure)
Time: 60 minutes (functionally between 53 and 60 minutes)
CPT Code Modifiers
Code modifiers provide additional information to a payer. Modifiers can describe the license level of provider, when services were provided, and how the services were provided, among other things. Here are four modifiers that you may encounter.
Here are four modifiers that you may encounter.
- Modifier 25 — Typically, a single code will accurately describe a session. But occasionally, you may find that a fully separate E/M service is needed (performed by the same provider) on the same day. Modifier 25 is used in these situations, as it calls out that service as separate and reimbursable. Note that you can only attach modifier 25 to codes 99201-99215, 99341-99350.
- Modifier 59 — Similar to modifier 25, this modifier is used to describe a distinct non-E/M procedural service done on the same day. Note that your documentation must support a separate session.
- Modifier GT — Used for telehealth sessions involving interactive audio and video.
- Modifier UT — Used when the provider sees a patient in crisis.
When you understand how CPT codes work and have a firm knowledge of the codes you’ll use most often in your therapy practice, you’ll increase your claims submission rate and reduce the likelihood of being flagged for inappropriate coding. Beyond the practicality of improving cash flow, accurate coding delivers peace of mind since you won’t have to worry about whether or not you’re using CPT codes correctly.
Beyond the practicality of improving cash flow, accurate coding delivers peace of mind since you won’t have to worry about whether or not you’re using CPT codes correctly.
Provision of private security services (Setting up a security post) for the needs of the Research Institute of Mental Health of the Tomsk National Research Medical Center
For control
Placement completed
To the source
Placed: 10.11.2022
Submission of applications: 10.11.2022 2022 9:00)
003
| Goods/services | KTR code | Unit. rev. | Quantity | Unit price | Cost |
|---|---|---|---|---|---|
| Private security services (Setting up a security post) Security officers have weapons No , Mobile group employees have weapons Yes , Use of special means Yes , | 80. 10.12.000 10.12.000 | Man-hour | 0 7002 180 | 1260000 | |
| Private security services (Setting up a security post) Security officers have weapons No , Mobile group employees have weapons Yes , Use of special means Yes , | 80.10.12.000 | Man-hour | 8760 | 180 | 1576800 |
| Availability of special security equipment, Yes employees have weapons , | 80.10.12.000 | Human-hour | 6760 | 180 | 1216800 |
Appendix 1 to the NMC)
11/11/2022
Appendix 2 to the notice (Draft contract)
11/11/2022
Appendix 3 to the notice (Description of the procurement object)
11. 11.2022
11.2022
obligations
11.11.2022
Appendix 4 to the notice (Requirements for the content, composition of the application)
11.11.2022
Protocols, contracts (agreements)
3-23EA-44
0042
 12.2022
12.2022 10 key steps on how to build a mental health app without code?
Are you looking to develop a health or mental health application using a no-code method? If YES, this guide can help you create a mental health app with custom features of your choice. Finding the perfect mental health app or designing apps from scratch can be intimidating, especially in a world driven by technology platforms that need to provide a lot of possibilities.
In this era of busy life, technology platforms have replaced many daily responsibilities for the sake of convenience and simplicity. The busier and busier a person's life becomes, the less time they have left to take care of their physical and mental health. Each person is in a period of superiority to each other, and the search for the best in one way or another worsens his mental health. In this scenario, the role of mental health apps is evident in how health app technology platforms have opened up unique frontiers in mental health support and information display. Mobile apps allow people, clinicians and researchers to use uncharted methods to access care, track improvements, track mood, and improve the interpretation of mental health through health app development.
Human-related mental health applications may collect related information. It has a built-in sensor that detects mood and changes in normal behavior and provides support by alerting you when help is needed to connect to the appropriate healthcare provider. They also have the ability to improve sleep and memory and control negative thoughts.
They also have the ability to improve sleep and memory and control negative thoughts.
Most mental health apps allow you to access and connect with a psychiatrist through these apps even if you don't want to reveal your identity and they help you in a positive relationship with online articles, daily reminders, etc. In short , the mental health app is a great tool for dealing with mental health issues.
Why is a mental health app needed?
The mental health app is a must for anyone in any field or any part of the world because global stress and mental health issues have increased in the age of technology. A good mental health app should be available on every mobile phone to keep mental health on track.
Mental health apps provide support to people during a mental crisis, or if someone is diagnosed with a mental illness, both can benefit from a mental health app. These apps provide useful access to advanced advice and help for symptoms and stress. Mental health apps would be a great option for users who are short on time and need help or need additional resources to address their mental health issues.
Not only for patients with mental illness, these mental health apps are also a great source and platform for healthcare providers. They can easily connect to the app with their patient and update their knowledge to take better care of their patients. Also, the doctor can offer his patient a good nutrition and exercise regimen; Tracking the progress of patients as well as symptoms, mood and medication monitoring can also be done with a good mental health app. In addition, these healthcare providers can contact patients via online sessions when needed. All of this has one goal: to improve patient care and reduce the overall burden on mental health on Earth.
Benefits of a mental health app
A mental health app or therapy app is great for both the user and the healthcare provider. There are many mental health apps available on the market, but they all share some common benefits, which are: health.
Obscurity
With the mental health app, users can choose their mental health rehabilitation options without disturbing anyone around them.
Introduction to care
The mental health app is a good initiative for those who have not received any help or avoided it. The reason can be anything, including difficulty making an appointment or connecting with people.
Economy
Many of the best mental health apps with basic features for free or in-app purchases will cost patients less than traditional mental health care.
Remote and extensive care
The mental health app can help mental health experts access help for people in remote areas or large numbers of people who need impulsive help, such as in the event of a natural disaster, etc.
More attractive
The mental health mobile app is a more attractive and engaging treatment than conventional, which can encourage patients to continue treatment.
24/7 care
The mental health app can provide 24/7, anytime, anywhere help and mental health support every day.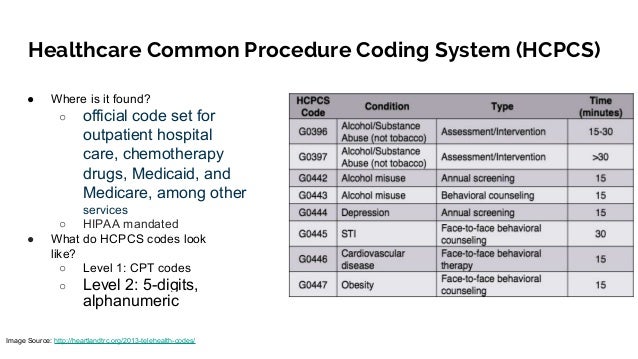
Consistent method
Mental health app and app platforms can provide consistency and equality for every person.
Personalized support
The mental health app is designed so that all people and patients can receive a personalized session that will not only provide support, but also improve and support people's new skills.
Evidence collection
What makes mental health apps unique, unlike conventional therapy, is the collection of factual data that can be accessed with a single click, including patient movement, mood, location and other important information.
Top 3 Mental Health Apps
If someone were to try to compile a definitive list of the best mental health apps, it would be much more difficult because the market is quite competitive. However, the first 3 on the list below have the best user retention and experience, including:
Mood Fit - great for general mental health
This is one of the top and best on the list.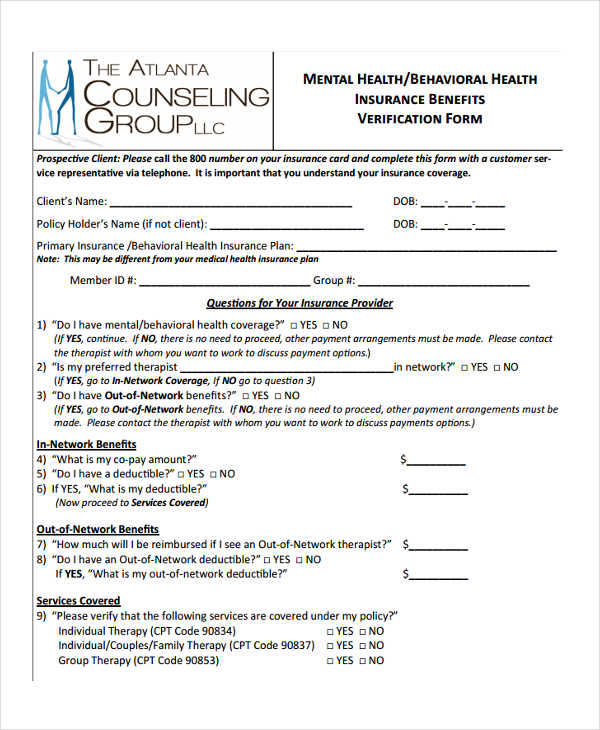 The main feature of the app and choosing it as the best is that it is free to use and provides general mental health help through the app to those who need it. It helps track mood and gives users tips on what they can do next to get over it. However, it does not offer consultations with registered therapists and does not have in-app purchases. This is:
The main feature of the app and choosing it as the best is that it is free to use and provides general mental health help through the app to those who need it. It helps track mood and gives users tips on what they can do next to get over it. However, it does not offer consultations with registered therapists and does not have in-app purchases. This is:
- Modifiable according to the user's goals.
- Ability to monitor daily progress.
- Illustrated understanding with recommended workouts.
- Daily reminders.
Better Help - Great for Mental Health Therapy
Better Help is a mental health app that's great for Online Mind Therapy delivered by Registered Therapists via Video or Audio Conversations ranging from $240 to $600 per month. However, this app does not offer any medication adjustments or free consultations. This is:
- Available on both iOS and Android.
- Allow communication via audio, video or text messages.
- Allow unlimited messages.
Calm is a great meditation tool
Third on the list is Calm, which offers customizable programs and activities that help users overcome anxiety, stay calm, and enable them to better meditate. It offers a 1 week trial plan and an annual subscription for $70 or $400 for life. This is:
- Offering personalized workouts and meditation plans for individual users.
- Soothing music and sound effects.
- Simple and convenient.
How do I create a mental health app?
10 Key Steps to Consider
Building a mental health app is usually done through technique and planning. It differs from other apps in that it covers the sensitive topic of mental health. The steps in developing a mental health app include the following 10 key steps:
Do your market research
The first important step in developing a mental health app is research. You must be aware of the market. How many users does the mental health app have? What disadvantages do they face in the current application setup? What are the main must-have features that other applications in the market use so that you can provide users with better quality and additional features?
How many users does the mental health app have? What disadvantages do they face in the current application setup? What are the main must-have features that other applications in the market use so that you can provide users with better quality and additional features?
Choose your audience
The second step is to set the desired target audience. For example, who are you willing to develop an app for, such as a specific age group? Specific gender? People with specific goals? Patients with a specific disease or application for targeting a general audience.
Choose Your Platforms
The third and most important step is choosing platforms based on several factors. Most applications are developed for the iOS and Android platforms. But initially, it's also a great approach to reach your audience and choose one app development platform.
List the features you want
Make a list of the most basic features you need for a mental health app. You should add what other popular apps offer as a new app. As a new app, you should add some extra features to the basic features to increase your marketing and popularity.
As a new app, you should add some extra features to the basic features to increase your marketing and popularity.
Prototype
The next step in developing an application is to create a prototype or MVP for each feature you have listed above so you can get an idea of the design and make adjustments before it goes into actual development so that the product works to its full potential. measure and could be sure. This will save you money to make sure everything is ready before you go directly to the development of the application.
Code or no code
Now it's time to decide if you want to build your mental health app with a coding team of developers and programmers, or with a no code platform like AppMaster.
Coding
Developing applications using programming languages, also called coding, is a traditional method of developing any online resource, be it a website or an application. It takes a lot of time, money and effort. Often development teams are involved in the development of a single application. The creation of a mental health app through coding must contain all the necessary features, and the development of the application must be based on cybersecurity rules in accordance with HIPAA.
Often development teams are involved in the development of a single application. The creation of a mental health app through coding must contain all the necessary features, and the development of the application must be based on cybersecurity rules in accordance with HIPAA.
No code technology
No code is the new option when it comes to application development. If you choose this option for your mental health development, you won't need a development team working on the same project. In addition, it will be cost effective, time efficient, require less manpower, and will not be technically complex. Even if you have a bit of knowledge, you can easily create your desired mental health app by yourself. AppMaster is a no-code platform that offers a back-end for working with visual programming. With this, you can build your mental health app with drag and drop method with less time and cost.
Pre-launch test
Once the development of the mental health app is complete, the next part of the development process is to test the mental health app before it is finally launched to avoid any future issues. To effectively test your application, you need to follow these test methods and fix if any problems occur:
To effectively test your application, you need to follow these test methods and fix if any problems occur:
- Unit Testing
- Performance Testing
- Functional testing
- Load testing
Promote your application
Whenever a new application is released to the market, there are two types of marketing phases: one is performed before the final launch, and the other after the full launch of the application. When an app is new to your brand awareness, you should promote your app and raise awareness of what it is and what it will be good for.
Launch App
Your mental health apps are now ready to run and you can run them on the appropriate platform or on iOS and Android if you have created a hybrid compatible app.
Keep updating
Once the application is on the market, track its progress, user response and the performance it gives. According to this, you can continue to update the application and stay in it.
What should I add to my mental health app?
Mental health or mood tracking apps should have some basic functionality. Some features are customizable, others are required on platforms such as mental health applications, including:
- Dashboard (separate for user and healthcare professional)
- Registration page (creating user profiles)
Average build time for a traditional coding app or a mental health app is 2 to 5 months with basic features. However, for more advanced features and applications on a larger scale, the application development time can be more than 6 months. Whereas if you use no-code platforms like AppMaster it can only take a few weeks to develop a fully functional mental health or therapy app.
How much does it cost to create a mental health app?
The average app cost to build a mental health app will vary depending on the app's scope, what platform it's for, how many features you're adding, and whether you're going to use coding or non-coding platforms to develop the app.
 application. The average cost of a mental health teletherapy app will be at least around $60,000-$80,000 with basic mental health app features. This amount of money is for the traditional method of developing applications through coding. With a code-free platform like AppMaster, your app costs a lot less and you can always get it back through monetization. You can get acquainted with flexible tariff plans.
application. The average cost of a mental health teletherapy app will be at least around $60,000-$80,000 with basic mental health app features. This amount of money is for the traditional method of developing applications through coding. With a code-free platform like AppMaster, your app costs a lot less and you can always get it back through monetization. You can get acquainted with flexible tariff plans. Do I need to provide certificates to list my mental health solution in app stores?
No, it is not currently required to provide any certifications in your mental health solution app, but it must comply with the HIPAA cybersecurity guidelines.
Are mental health apps regulated?
Personal data is collected for the proper functioning of teletherapy or mental health applications. It contains confidential and personal information about the health of a patient or individual. Thus, in order to regulate mental health apps, it is necessary to comply with all data protection requirements according to the governing bodies in order to ensure the safety of the app and the user and prevent theft.

Unfortunately, most mental health apps and other health apps do not have separate legislatures overseeing this particular issue. However, the owner and creator of the application must develop the mental health application in accordance with data protection authorities and laws, but this may differ in each country.
The legislative governing body on the above issue in the United States of America is the Health Insurance Portability and Accountability Act (HIPAA). It shares federal law on how personal health information is protected.
People and institutions in the medical field or mental health app or therapy app. Below are the main criteria by which a mental health app owner should adjust the app and make corrections as needed:
- Health-related services requiring data entry.
- Storage of personal health data.
- Sharing personal health data.
To avoid fraud, misleading details, or breaches of information, mental health app developers must evaluate several aspects.
 The follow-up must be followed at all times or the owner of a mental health or teletherapy app may face severe legal consequences. Mental health apps or teletherapy apps must meet the following requirements:
The follow-up must be followed at all times or the owner of a mental health or teletherapy app may face severe legal consequences. Mental health apps or teletherapy apps must meet the following requirements: - Confirm that the applications are not medical devices.
- Incorrect data calculation.
- Limit permissions and permissions.
- Remember about authentication.
- Measure that third party service providers are shielding data.
- Secure by design.
- Change the way you communicate and treat users in your health apps and the safety protocols you follow.
What tools should I consider to build an AI-powered mental health app?
AI or artificial intelligence can be useful for developing your therapy or mental health application. This is because mental health development and mood tracking can rely entirely on understanding artificial intelligence as a substitute for a real health care professional or face-to-face patient.
 Artificial intelligence. AI is a great tool to consider when you want to develop a mental health app or when it comes to health app development. The best reason to use AI is that over time, AI-based applications can better adapt to the needs of the user.
Artificial intelligence. AI is a great tool to consider when you want to develop a mental health app or when it comes to health app development. The best reason to use AI is that over time, AI-based applications can better adapt to the needs of the user. AI tools such as AppMaster enable users to develop any type of application with a smart approach, low cost and source code. AppMaster App Builder that quickly and efficiently creates apps.
Monetization Strategies - Making Money With Mental Health Apps
The good thing about app development is that it can get monetized through which you can make some money from your apps. Monetization is a way to earn money through apps or websites and the following methods can be used to monetize:
- ADS
The first and best monetization method is to run in-app ads. - In-app purchases
The second popular monetization method is through in-app purchases and retaining some premium features.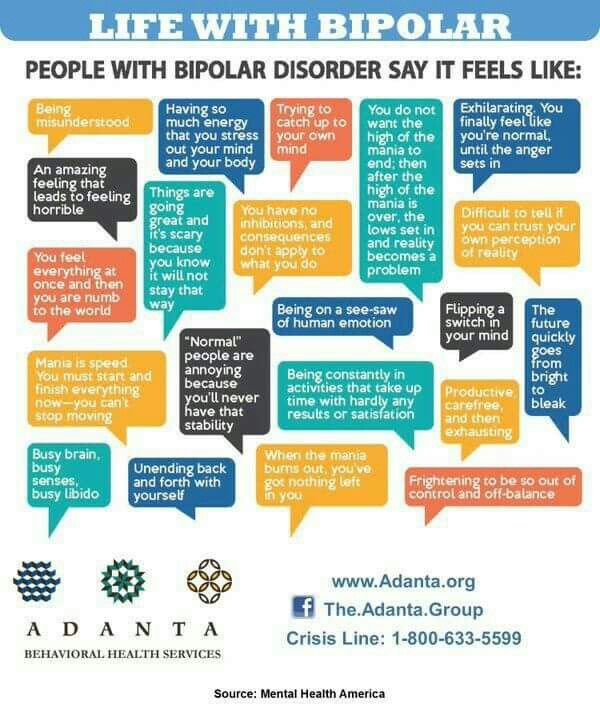
- Paid App
The third monetization method is to make your app paid rather than free.
bottom line
Mental health app, mental health app or therapy app is a type of mobile app that is urgently needed by everyone nowadays due to the increased stress and anxiety among people. This application is downloaded on their mobile phone; people will help them better and more productively control their emotions. These apps help increase reach time for those in need. The mental health app is also a great resource for patients diagnosed with some mental illness like depression, anxiety, etc.
Not only that, if you are a healthcare professional and especially if you are a psychologist or psychiatrist, these mental health apps will also be a great resource for you as the app will allow you to keep track of patient records and help those in need on time, to avoid major crises.
In this way, these mental health apps will reduce the overall burden of stress and anxiety and allow people to get better mental health care anytime, anywhere.